Abstract
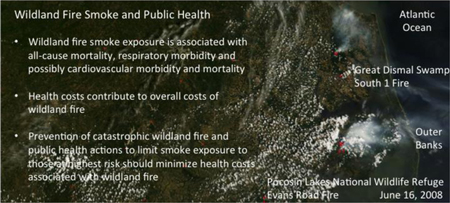
The natural cycle of landscape fire maintains the ecological health of the land, yet adverse health effects associated with exposure to emissions from wildfire produce public health and clinical challenges. Systematic reviews conclude that a positive association exists between exposure to wildfire smoke or wildfire particulate matter (PM2.5) and all-cause mortality and respiratory morbidity. Respiratory morbidity includes asthma, chronic obstructive pulmonary disease (COPD), bronchitis and pneumonia. The epidemiological data linking wildfire smoke exposure to cardiovascular mortality and morbidity is mixed, and inconclusive. More studies are needed to define the risk for common and costly clinical cardiovascular outcomes. Susceptible populations include people with respiratory and possibly cardiovascular diseases, middle-aged and older adults, children, pregnant women and the fetus. The increasing frequency of large wildland fires, the expansion of the wildland-urban interface, the area between unoccupied land and human development; and an increasing and aging U.S. population are increasing the number of people at-risk from wildfire smoke, thus highlighting the necessity for broadening stakeholder cooperation to address the health effects of wildfire. While much is known, many questions remain and require further population-based, clinical and occupational health research. Health effects measured over much wider geographical areas and for longer periods time will better define the risk for adverse health outcomes, identify the sensitive populations and assess the influence of social factors on the relationship between exposure and health outcomes. Improving exposure models and access to large clinical databases foreshadow improved risk analysis facilitating more effective risk management. Fuel and smoke management remains an important component for protecting population health. Improved smoke forecasting and translation of environmental health science into communication of actionable information for use by public health officials, healthcare professionals and the public is needed to motivate behaviors that lower exposure and protect public health, particularly among those at high risk.
Keywords: Wildfire emissions, smoke, health effects, air pollution, particulate matter, PM2.5
Graphical Abstract
1. Introduction
The natural cycle of wildland fire plays an important role for maintaining the ecological health of the landscape. Yet, the emission and atmospheric transport of combustion products from wildland fire, namely smoke represents a costly and growing global public health problem impacting vulnerable communities, and individuals who are more sensitive to the adverse health effects of smoke exposure. A contemporary estimate of the annual global mortality from landscape fire smoke is 339,000 deaths (Fig. 1, Johnston et al., 2012). Despite this shockingly high estimate, extreme weather events and drought are further increasing the risk of wildland fire and its attendant risks to health (Flannigan, et al. 2009). As the intensity and size of wildland fires increase, so do the associated costs and the vulnerable and at-risk populations adversely impacted by wildland fire smoke. Accordingly, the public health impacts of wildland fire smoke are taking on greater importance and merit the attention of all who have responsibility for land and air quality management decisions and wildland fire policy, who protect the health of the public and at-risk populations, and the stakeholders who are impacted by wildland fire policy. Consequently, the range of decision-makers and stakeholders needed to address this issue is vast and includes local, state, federal and Tribal governments and agencies/offices responsible for land and forest use and fire management, environmental quality and public health. Health care systems, health care professionals, and health insurers as well as city and regional planners should also take an active role in formulating and implementing solutions to mitigate the adverse health impacts of wildland fire emissions.
Figure 1. Global fire map corresponding to September 8 to 17, 2015.
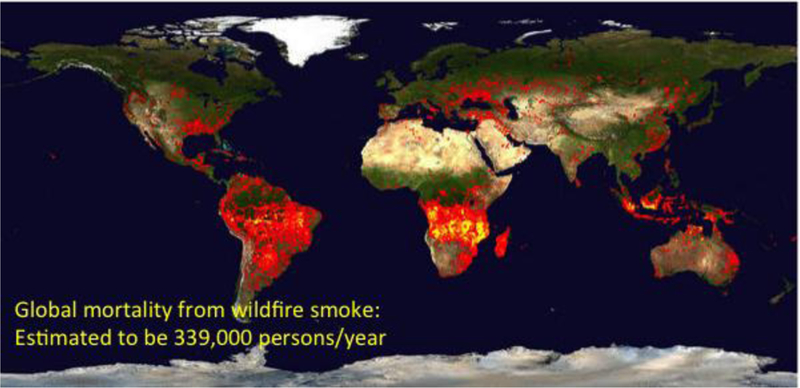
The global fire map (https://lance.modaps.eosdis.nasa.gov/cgi-bin/imagery/firemaps.cgi?period=2015251–2015260) reports the location of fires detected by MODIS (Moderate Resolution Image Spectroradiometer) on board NASA’s Terra and Aqua research satellites and shows the global expanse of wildfires. Each colored dot indicates a location where MODIS detected a fire during the 10-day period. Red dots indicate low fire counts, whereas yellow dots indicate larger numbers of fires. Global mortality from wildfire smoke is estimated to be 339,000 deaths annually (Johnson et al., 2012).
The review that follows expands on the plenary session titled, “Wildland Fire Smoke and Health: What’s new since the 1st International Smoke Symposium” presented at the 2nd International Smoke Symposium 2016 in Long Beach, CA on November 15, 2016. The purpose of the plenary session was to communicate the state of our knowledge of the human health effects of wildland fire smoke exposure. The presentation integrated new epidemiological studies and recent systematic reviews of the health effects of wildland fire smoke exposure (Youssouf et al., 2014, Liu et al., 2015, Reid et al., 2016a). This paper also broadens the discussion to consider the health costs of catastrophic wildfire and the role of public health and healthcare professionals for mitigating the adverse health effects of wildland fire smoke. Such information is critically important for risk assessment, policy analysis, and decision-making regarding air quality, land use and fuel management.
2. Wildland Fire Emissions and Smoke
Wildland fire emissions are complex both physically and chemically, and attendant smoke formation, physiochemical aging and atmospheric transport are influenced by many factors including but not limited to the type of fuel, the type of fire, the characteristics of the landscape, the rate of fuel consumption, and meteorological conditions. The key primary emissions from wildland fires that worsen air quality include ambient air particles such as fine and coarse particulate matter (PM), and gases, carbon monoxide (CO), methane, nitrous oxide (N2O), nitrogen oxides (NOx), volatile organic carbon (VOC) as well as many other air toxics (Urbanski et al., 2009). Emissions also contain a number of trace metals. Air quality is further affected by the formation of secondary pollutants such as organic aerosols, and ozone generated by the photoreaction of NOx and VOCs in the atmosphere (Jaffe et al. Atmos Environ 2012).
Particulate matter, NO2, CO, and O3, are National Ambient Air Quality Standard (NAAQS) criteria pollutants regulated under the Clean Air Act, and the health impacts of these pollutants are well established. Yet, the extent to which air pollutants generated by wildland fires affect health is less well quantified, and the study of such effects represents an emerging and rapidly advancing field. So, while much has been learned over the last decade and will be briefly summarized here, much is still unknown and further research is needed to better define the short-term and long-term impacts of wildfire emissions on health while being mindful of the ecological benefits of wildland fire. Such knowledge is critically important for policy development and decision-making vis-à-vis fuel management that includes prescribed fire, smoke forecasting (Yao et al., 2013), and public health and clinical interventions intended to limit exposure to smoke and protect population health.
3. Health Effects of Wildland Fire Smoke and Wildfire-Related PM2.5
Recent systematic reviews (Youssouf et al., 2014; Liu et al., 2015; Reid et al., 2016a) conclude that a strong association exists between exposure to wildland fire smoke or wildfire-PM2.5 and all-cause mortality and respiratory morbidity (see Table1). Strong positive associations are present between wildland fire smoke exposure and exacerbations of asthma and COPD, bronchitis and pneumonia (Youssouf et al., 2014; Liu et al., 2015; Reid et al., 2016a). Wildland fire smoke exposure and respiratory mortality do not appear to be associated. The epidemiological data linking wildfire smoke exposure to cardiovascular mortality and morbidity is mixed, and as yet inconclusive. More data is needed to accurately define the risk of cardiovascular health effects including common, life-threatening, disabling and costly clinical outcomes that include myocardial infarction, stroke, heart failure, heart rhythm disturbances, and sudden death. Health data including clinical outcomes collected over much wider geographical areas with larger numbers of exposed people and for longer periods of time would better define the risk of adverse health effects. Additionally, the study of larger and diverse populations will help define the most sensitive populations and the evaluation of the influence of non-chemical stressors and social factors on the relationship between exposure and the health effects of wildland fire smoke.
Table 1.
Associations between Wildfire-PM or Smoke Exposure and Health Outcomes
| Outcome | Direction of Association | Strength of Evidence | New Studies Published Since Reid et al., 2016a | |||
|---|---|---|---|---|---|---|
| Mortality | ||||||
| All | Increased | Strong | − Zu et al., 2016, − Kollanus et al., 2016 | |||
| Respiratory | No assoc. | − Zu et al., 2016, − Kollanus et al., 2016 | ||||
| Cardiovascular | Increased | Inconclusive | − Zu et al., 2016, ± Kollanus et al., 2016* | |||
| Morbidity | ||||||
| Respiratory | Increased | Very Strong | + Liu et al., 2017a; Lui et al., 2017b; + Tinling et al., 2016; + Reid et al., 2016b; + Parthum et al., 2017; + Le et al., 2014* | |||
| Asthma | Increased | Very Strong | + Vicedo-Cabrera et al., 2016; + Reid et al., 2016b; + Alman et al., 2016; + Parthum et al., 2017, − Kollanus et al., 2016 | |||
| COPD | Increased | Very Strong | + Reid et al., 2016b; Alman et al., 2016; + Parthum et al., 2017, − Kollanus et al., 2016; +Le et al., 2014* | |||
| Infection | Increased | Strong | + Tinling et al., 2016; + Parthum et al., 2017 | |||
| Cardiovascular | Increased | Inconclusive | + Tinling et al., 2016; − Alman et al., 2016; − Reid et al., 2016a; − Kollanus et al., 2016; + Le et al., 2014* | |||
| Acute MI | Mixed | Inconclusive | + Le et al., 2014* | |||
| Heart Failure | Mixed | Inconclusive | + Parthum et al., 2017; +Le et al., 2014* | |||
| Cardiac arrest | Mixed | Inconclusive | ||||
| Hypertension | Mixed | Inconclusive | + Tinling et al., 2016; + Reid et al., 2016b (women); + Le et al., 2014* | |||
| Arrhythmia | No assoc. | + Le et al., 2014* | ||||
| IHD | Increased | Inconclusive | + Alman et al., 2017, + Le et al., 2014* | |||
| Angina | Increased | Inconclusive | ||||
| Cerebro-vascular | Mixed | Inconclusive | + Le et al., 2014* | |||
COPD = Chronic obstructive pulmonary disease; IHD = Ischemic heart disease; MI=myocardial infarction, No Assoc. = No association; + indicates statistically significant positive association with wildfire-PM2.5; - indicates no association with wildfire-PM2.5. ± indicates borderline positive association with wildfire-PM2.5.
For individuals ≥65 years.
Table 1 summarizes the associations between wildfire-PM or smoke exposure and health outcomes based on the most recent critical review (Reid et al., 2016a). Each outcome is listed along with the direction and strength of the association. Recently published studies are provided and are marked as either showing a positive association between wildfire-PM or smoke and the health outcome of interest or no association.
Epidemiological studies have defined populations of individuals who might be at greater risk from the adverse health effects of wildland fire smoke or PM2.5. Susceptible populations probably include people with pre-existing respiratory disease, middle-aged and older adults (Lui et al., 2015; Reid et al., 2016a), children, pregnant women and fetuses (Reid et al. 2016a), although not all studies are consistent (Reid et al., 2016b). A recent study provides evidence that risks are greater for older women and African-Americans (Lui et al., 2017b) and those with indicators of lower socio-economic status (Reid et al., 2016b; Lui et al., 2017b).
Since the publication of the most recent systematic review (Reid et al., 2016a) several epidemiological studies have been published further describing the impacts of wildland fire smoke on the health of the exposed population (Table 1, right hand column). Health outcomes associated with wildland fires were described for Colorado in 2012 (Alman et al., 2016), California in 2008 (Reid et al., 2016b), the western U.S. between 2004 and 2009 (Liu et al., 2017b), North Carolina in 2008 (Parthum et al., 2017) and 2011 (Tinling et al., 2016), the northeastern and Mid-Atlantic States of the U.S. (Le et al., 2014) and Boston and New York in 2002 (Zu et al., 2016), Europe in 2005 and 2008 (Kollanus et al., 2017) and Valencia, Spain in 2012 (Vicedo-Cabrera et al., 2016). The findings of these studies further corroborate the conclusions of the previous published systematic reviews. Three recent studies describing the health effects of long-range transport of wildfire related-PM2.5 from Quebec, Canada in 2002 (Zu et al., 2016; Le et al., 2014) and the Helsinki metropolitan area, Finland between 2001 and 2010 (Kollanus et al., 2016). No evidence of all-cause mortality was found in either of the studies that examined mortality (Zu et al., 2016, Kollanus et al., 2016). By contrast the study examining the health effects of long-range transported wildfire smoke from the Quebec, Canada wildfires in 2002 (Le et al., 2014) did show positive associations for respiratory and cardiovascular hospitalizations in a Medicare population in the northeastern and Mid-Atlantic States of the United States.
Reid and colleagues (Reid et al., 2016b) studied a long-lived, large wildfire complex in northern California that occurred in the summer of 2008. Daily wildfire-PM exposure was modeled using a data-adaptive machine learning approach with spatiotemporal data sets. The main findings were that for each 5µg/m3 increase in wildfire-PM2.5, the risk of emergency department visits for asthma [RR=1.06, 95% CI=(1.05, 1.07)] and COPD [RR=1.02 (95% CI=(1.01, 1.04)], and hospitalizations [RR=1.07, 95% CI=(1.05, 1.10)] increased. In this study and in another recent study by Lui and colleagues, effects were more prominent in women, in people living in areas with the lowest median income (Liu et al., 2017b), or among aged adults (Lui et al., 2017a). Rappold and colleagues during the 2008 Pocosin Lakes National Wildlife Refuge fire in North Carolina also found that poor socioeconomic conditions increased the association between exposure to wildland fire PM2.5 and emergency department visits for asthma, and heart failure (Rappold et al., 2012).
Like the previous studies, Tinling and colleagues (Tinling et al., 2016) found positive associations between wildfire-PM and respiratory health effects during the 2012 Pains Bay peat fire in eastern North Carolina, a fire that was located very close to the 2008 Pocosin National Wildlife Refuge Fire. As exposure to wildfire-PM2.5 increased, respiratory/other chest symptoms and upper respiratory infections increased in adults and children. The sensitivity of children, particularly those with asthma or rhinitis to the respiratory effects of wildfire-PM2.5 were also observed in the Valencia birth cohort when surveyed for health effects after the 2012 wildfire in Valencia Spain (Vicedo-Cabrera et al., 2016). By contrast to the previous studies Tinling and colleagues showed that as daily wildfire-PM2.5 increased, hypertension and ‘all-cause’ cardiac outcomes increased on the day of exposure and up to two days after exposure (Tinling et al., 2016). The observation of cardiovascular health effects during the 2012 Pains Bay peat fire in eastern North Carolina largely confirmed the findings reported on the 2008 Pocosin Lakes National Wildlife Refuge peat fire (Rappold et al., 2011; Rappold et al., 2012).
Alman and colleagues (Alman et al., 2016) studied the effect of wildfire smoke on respiratory and cardiovascular emergency department visits and hospitalizations over a 2-day period in Colorado in 2012. Exposure to PM2.5 was modeled with a Weather Research and Forecasting Model. PM2.5 exposure was associated with asthma and wheeze, and COPD for lag day 0 and with a 2-day or 3-day moving average lag period. Neither the Reid et al. (Reid et al., 2016b) nor the Alman et al. (Alman et al., 2016) study identified an effect of wildfire PM on cardiovascular outcomes.
While the associations between wildfire smoke and cardiovascular effects remain mixed, one study assessing the health impacts of intense wildfires in Victoria, Australia from December 2006 through January 2007 (Haikerwal et al., 2015) is of particular interest. This study showed a positive association between exposure to wildfire-related PM2.5 and important clinical cardiovascular events. The major findings included a positive association between wildfire-PM2.5 exposure of the total population and out-of-hospital cardiac arrests. Significant positive associations were also observed between wildfire-PM2.5 exposure and out-of-hospital cardiac arrests among older adults and men. Increased risk was also observed for hospitalizations for ischemic heart disease and myocardial infarction with statistically significant positive associations for the total population, older adults and women (Haikerwal et al., 2015)(see Fig. 2). Such associations of wildfire PM2.5 with health outcomes are very similar to what is known about the health effects of ambient air PM2.5 exposure. Another recent study (Kollanus et al. 2016) published after the systematic reviews also provides borderline evidence of cardiovascular morality among the aged, that is those individuals 65 years of age or greater on the day of exposure to smoke related PM2.5. The effect estimate was a 13.8% (Confidence interval: −0.6 to 30.4) increase in mortality for each 10µg/m3 increase in smoke-affected day PM2.5. Wildfire smoke has also been associated with low birth weight (Holstius et al., 2012) when wildfire smoke exposure, as estimated by ambient PM10 concentrations occurs during the third trimester.
Figure 2. Cardiovascular health effects during wildfires in Victoria, Australia, December 1, 2006 to January 31, 2007.
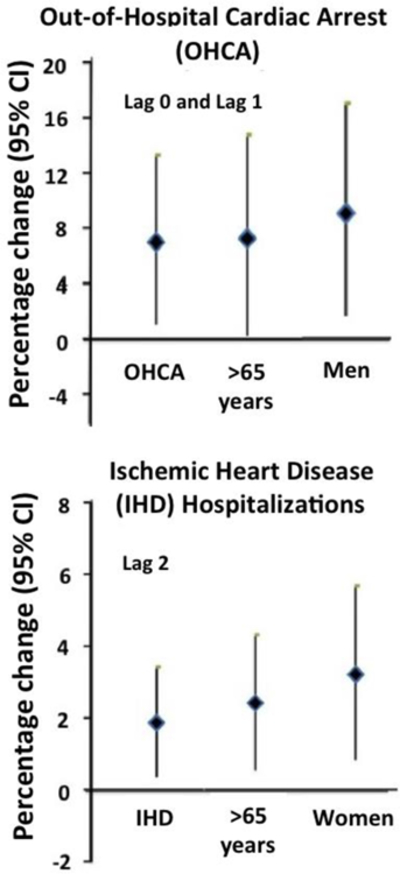
The upper panel shows the percent change in out-of-hospital cardiac arrest (OHCA) and the lower panel ischemic heart disease (IHD) hospitalizations for a 9µg/m3 interquartile range increase in wildfire-PM2.5 exposure. Lag 0: effect occurs on the day of exposure. Lag 0 to 1: Health effects occur on the day of exposure and a day after exposure. [Adapted from Haikerwal et al., 2015].
Many epidemiological studies estimating the health effects of PM2.5 (US EPA, 2009) have identified the populations most susceptible to the adverse health effects of PM2.5 as individuals with pre-existing respiratory and cardiovascular disease, adults 65 years of age and older, populations with lower socio-economic status, children and developing fetuses. Other populations suspected to be at greater risk include people with chronic inflammatory diseases (e.g., diabetes, obesity) and those with specific genetic polymorphisms (e.g., GSTM1) that mediate physiologic response to air pollution. To date no data has been presented to suggest higher risk among those with diabetes, obesity or specific genetic polymorphisms. Future research should consider such possibilities.
So given that the young, the old and people with respiratory and cardiovascular diseases are possibly at higher risk, just what percentage of the U.S. population do these conditions represent? And how many people might be potentially at-risk in the population. Currently in the United States 14.9 percent of the population is over the age of 65 years (U.S. Census Bureau, 2017a), and 22.8% are children (less than 18 years old)(U.S. Census Bureau, 2017b). Heart disease and lung disease also contribute to the population at-risk with heart disease, accounting for about 28.4 million (11.7%)(US CDC, 2015a) and COPD 12.8 million (5.3%) (CDC, 2015b). Asthma adds an additional 24.6 million (9%) persons (CDC, 2015b). There are about 4 million births in the U.S. each year (Martin et al., 2017). Consequently, even though the relative risks of wildfire-PM2.5 and smoke are small, the very large number of at-risk individuals across the U.S. has the potential to produce a large number of serious adverse health outcomes during wildland fire events.
The reader should also keep in mind that wildland fire smoke or wildfire-related PM2.5 while serving as a metric of exposure represents only a surrogate of the actual aerosols to which populations are exposed and is not likely to fully characterize the exposure to toxic constituents of the atmosphere unique to each wildland fire. The incomplete characterization of exposure might in part explain the inconsistencies in the epidemiological data particularly for cardiovascular outcomes. Apart from methodological limitations related to study design, exposure misclassification, and statistical power, a real consideration is that differential toxicity of wildland fires emissions based on the multitude of conditions that modify the chemical characteristics of such emission might contribute to these inconsistencies.
4. Mechanisms Proposed to Explain Health Effects
Substantial progress has been made over the last decade identifying the key biological pathways accounting for health effects of inhaled particulate matter and gases (Newby et al., 2015). Currently there are three principal pathways supported by epidemiological, clinical and toxicological data that explain the observed biochemical, physiological and clinical effects of air particulate pollutant exposure. First, inhaled particulates can react with neural receptors in the lung and activate a reflex involving chemical and electrical communication between the lung and the nervous system. Return signals from the brain traveling through the autonomic nervous system result in increases in blood pressure and changes in heart rhythm. Second, air pollutants interact with the alveolar-capillary cells generating oxidative stress reactions and local and systemic inflammatory responses. The consequences of these responses include decreased nitric oxide availability, oxidation and alteration of the function of blood lipids, platelet activation, and prothrombotic changes in blood proteins that affect the function of blood vessels and increase the likelihood that blood will clot. Third, the smallest fraction of particulate matter, the ultra-fine fraction, defined as particles less that 0.1 µm, can translocate across the alveolar membrane and move systemically acting at a distance from the lung. The biochemical and physiological responses contribute to a number of functional changes including endothelial dysfunction, endothelial activation, and injury. Local changes in the lung promote pulmonary responses affecting airway function, and resistance to viruses and bacteria increasing the risk of infection, for example upper respiratory tract infections, bronchitis, and pneumonia. Systemically, the sequence of biochemical and physiological changes associated with urban-PM2.5 increases the risk of cardiac ischemia, and acute coronary syndrome, stroke, arrhythmia and heart failure, yet such outcomes have not been established with certainty after wildland fire smoke exposure suggesting that chemical differences might yield differential health effects. Should cardiovascular health effects ultimately be confirmed, the mechanism of such effects is likely to be similar to that described for urban-PM.
Limited toxicological data exists that can relate directly to epidemiological observations. However, Kim and colleagues (Kim et al., 2014) studied the differential pulmonary and cardiovascular system effects in an in vivo study in mice in response to PM collected during the 2008 Pocosin Lakes National Wildlife Refuge fire in eastern North Carolina, a fire extensively studied for its health effects by Rappold and colleagues (Rappold et al., 2011; Rappold et al., 2012). PM was collected during the smoldering and “glowing and nearly extinguished” phase of the fire and the PM was divided into fine and coarse fractions. Lung and systemic markers of injury and inflammation were measured after oropharyngeal aspiration of 100 μg PM/mouse. Fig. 3 shows the toxicological responses of the lung tissue to fine and coarse wildfire-PM, and provides direct evidence of the differential biological effects of the two size fractions of PM in lung tissue. Coarse particle exposure causes inflammatory effects in the lung driven by endotoxin, a constituent of bacterial cell walls and present in coarse PM. Exposure to the fine PM fraction did not produce pulmonary effects in the mouse, but did produce cardiovascular effects (Kim et al., 2014).
Figure 3. Toxicology of Wildland Fire Emissions.
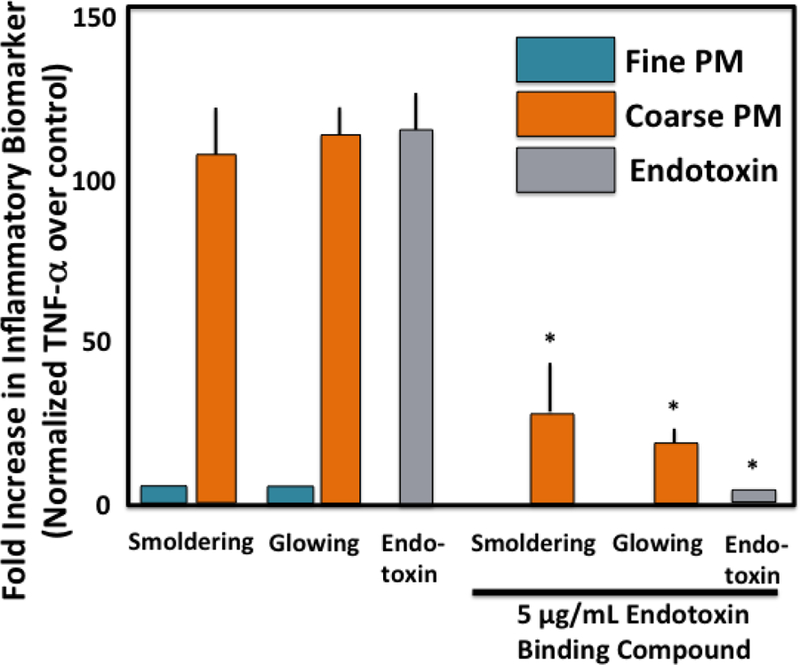
Murine lungs were exposed to fine (blue bars) and coarse (orange bars) PM collected at the 2008 Pocosin Lakes National Wildlife Refuge fire and endotoxin in the presence and absence of polymixin B (PMB) an antibiotic that binds endotoxin and blocks the effect of endotoxin, a key component of the outer membrane of Gram-negative bacteria. Murine lungs responded with an inflammatory response to exposure to endotoxin (Gray bar) as shown by the increase in the pro-inflammatory cytokine TNF-alpha. The effect of endotoxin was blocked by the addition of polymixin B. Coarse PM (orange bars) induced a pro-inflammatory response as indicated by the increased TNF-alpha, an effect blocked by polymyxin B. Inhibition of the TNF-alpha response by polymyxin B confirms that endotoxin probably plays a role in the inflammatory response induced by the coarse PM fraction. By contrast fine PM (blue bars) did not induce an inflammatory response in this model. (Kim et al., 2014)
The toxicological findings in this study (Kim et al., 2014) provide some biological plausibility for the increase in emergency department visits for pulmonary and cardiovascular health outcomes among those exposed to emissions from the Pocosin Lakes National Wildlife Refuge fire in 2008 (Rappold et al., 2011). The toxicological studies further suggested that cardiovascular effects might be mediated by the wildfire smoke’s fine fraction of PM, while the pulmonary responses appear to be related to coarse PM’s endotoxin content. The possible role of endotoxin as a biologically active component of the coarse fraction of wildfire smoke was strengthened by a controlled human exposure study of 50 healthy adults who were exposed to concentrated ambient fine and coarse PM exposure at 200 µg/m3 for 130 minutes (Zhong et al., 2015). Inhalation of coarse PM caused increases in blood pressure and heart rate and the response was associated with the endotoxin and ß-1,3-d-glucan content of the coarse PM. While wildfire smoke was not the specific source of the concentrated air particles used in the controlled human exposure study, the observations taken within the context of the in vivo murine study implicates endotoxin as an active component of coarse particles affecting biological responses in man.
5. Hidden Costs of Wildfires
Federal wildfire suppression costs have quadrupled between the late 1980s and the last five years (https://www.fs.fed.us/sites/default/files/2015-Fire-Budget-Report.pdf), because of the location of wildfires, the increasing size and intensity of fires, the expansion of the wildland-urban interface, and base camp and personnel support. Such costs are straining the federal wildfire suppression budget (https://www.usda.gov/media/press-releases/2017/09/14/forest-service-wildland-fire-suppression-costs-exceed-2-billion) and highlight the importance of land use and fuel management decisions. However, these costs only partially account for the total costs of catastrophic wildfires. Wildfires are also associated with many other costs including those associated with premature mortality (Johnston et al., 2012; Rappold et al., 2014; Kollanus et al., 2017), health care utilization, lost productivity, impacts on the quality of life (Jones, 2017b), compromised stream, river and drinking water quality (Hohner et al., 2016; Bladon et al., 2014), and damage to critical infrastructure. Estimates of direct and indirect costs of wildfire to health related costs are emerging as new and important sources of data to be considered when making fuel management and land use decisions. Such estimates also have the potential to be used to estimate health costs associated with fuel management approaches such as prescribed fire that provide ecological benefits and mitigate catastrophic wildfires (Fernandes et al., 2003), yet impair air quality.
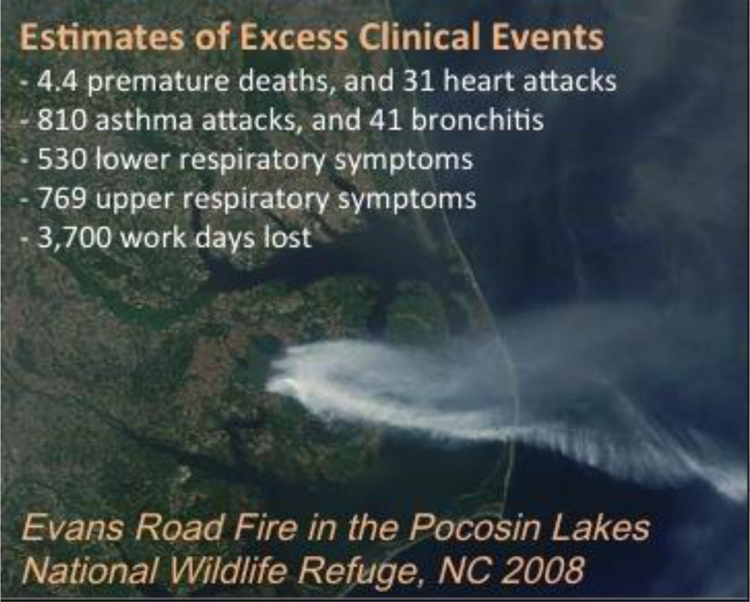
The 2008 wildland fire in the Pocosin Lakes National Wildlife Refuge in eastern North Carolina (Fig. 4) offered an opportunity to estimate the total health costs of a wildland fire that burned more than 40,000 acres of peat bogs over 202 days. Suppression costs of this fire totaled $20 million, required 2 billion gallons of water and over 400 people to control the fire (Rappold et al., 2011). Health cost estimates based on excess adverse health impacts and deaths attributable to smoke exposure were $48.4 million. Health cost estimates were based on 4 to 5 premature deaths, 31 non-fatal heart attacks, 41 episodes of bronchitis, 810 asthma attacks, 530 lower respiratory symptoms, 769 upper respiratory symptoms and 3,700 work days lost. The cost of excess emergency department visits for asthma and heart failure alone were estimated to be $1 million (Rappold et al., 2014). Therefore, in this example the estimated costs associated with deaths, lost workdays and healthcare costs were two-fold higher than the costs of suppression. The health costs were also estimated for peat fires in the Great Dismal Swamp that occurred in 2008 in Virginia (Parthum et al., 2017). The clinical observations noted in Table 1 were similar to those observed by Rappold et al. (Rappold et al., 2011). The estimated health costs attributed only to morbidity were $3.69 million (Parthum et al., 2017) with fire suppression costs exceeding $10 million (https://fws.gov/refuge/Great_Dismal_Swamp/what_we_do/firesuppression.html). While the cost attributed to the peat fires of Virginia and North Carolina during 2008 was high, the size of these fires is dwarfed by the catastrophic wildfires of the west. In a third example, Jones and Berrens (Jones et al., 2017a) estimated the health costs of morbidity and morality associated with PM2.5 smoke in the Western US between 2005 and 2015. Their analysis suggests that wildfire smoke in the Western US contributes as much as $165 million in annual health costs attributable to morbidity and mortality (Jones et al., 2017a). Fann and colleagues estimated the morbidity, mortality and economic burden of wildland fires for the continental U.S. between the years 2008 and 2012(Fann et al., 2018). The economic burden of these fires over the five years studied ranged from $63 million (95% CI:$6-$170 million) for short-term exposures, to $450 million (CI: $42 - $1,000 million) for long-term exposures.
Figure 4. Satellite image showing the location of Evans Road Fire in the Pocosin Lakes National Wildlife Refuge, NC in 2008.
6. Population Vulnerabilities
The 24-hour NAAQS for PM2.5 and PM10 are established to protect the health of the public during short-term exposure to ambient PM, whereas the annual PM2.5 standard is intended to provided public health protection against long-term exposures. As has been described, large wildland fires generate massive emissions into the atmosphere over a short period of time and increase local and even distant ambient air PM concentrations that exceed the 24-hour PM standard and are associated with adverse health effects in the most sensitive populations (Navarro et al., 2016).
While it is easy for one to appreciate that wildland fires produce short-term increases in ambient PM, less well appreciated is the fact that wildland fire and prescribe burning of the landscape contribute substantially to the average annual PM2.5. Figure 5 was adapted from a recent paper by Rappold and colleagues (Rappold et al., 2017) and illustrates the important point that wildland fires contribute to both short-term and long-term increases in ambient air particle pollution. The annual average daily fire-PM2.5 footprint by county in the U.S. between 2008 and 2012 is shown in the left-hand panel of the map in Fig. 5. Large fire perimeters are shown in black. The figure shows that wildland fire smoke contributes substantially to total PM in some areas of the United States. By contrast, the right-hand panel of Fig. 5 shows the number of days by county with wildfire-PM2.5 above the 24 hour EPA NAAQS of 35 μg/m3. Interestingly, while the southeastern and western US wildland fires produce similar elevations of the annual average PM2.5 concentrations (Fig. 5, Left hand panel), the number of days exceeding the 24-hour average PM2.5 NAAQS is far fewer in the southeast where prescribed fire is used to a greater extant (Fig. 5, Right hand panel).
Figure 5.
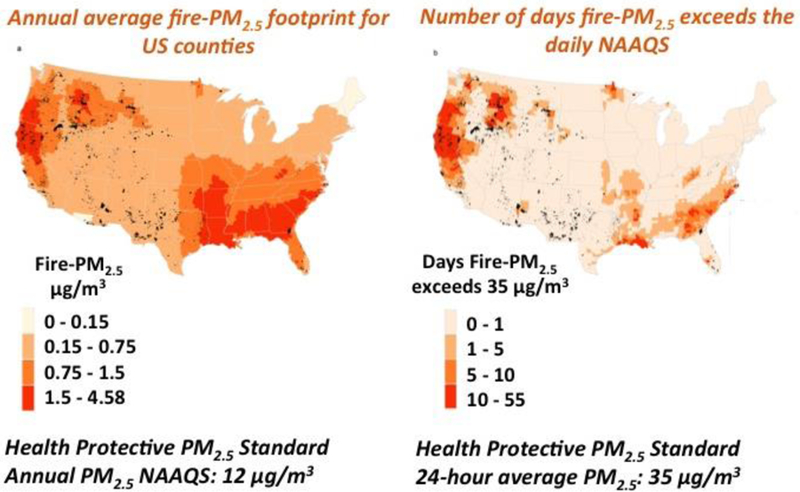
Left-hand panel. Annual average daily fire- PM2.5 footprint by counties of continental U.S. and perimeters of area burned by large fires in black between 2008 and 2012. Right-hand panel. Number of days with fire-PM2.5 above 35 μg/m3 by counties of continental U.S.. Adapted from Rappold et al., 2017.
The maps depicted in Fig. 5 illustrate the non-uniform spatial distribution of wildland fire smoke exposure across the United States. Likewise, the health characteristics of the population are also distributed unequally across the landscape. For example, Fig. 6 shows the spatial distribution across the U.S. of chronic obstructive pulmonary disease, a population known to be at increased risk for the adverse health effects from wildfire smoke. The prevalence of COPD is greater in the eastern United States. When simultaneously considering the distribution of populations at risk and the distribution of wildfire smoke exposure it becomes apparent that some regions of the U.S. are predicted to have a higher likelihood of adverse health effects during wildland fire events.
Figure 6. Chronic obstructive pulmonary disease prevalence by county in the U.S. in 2014.
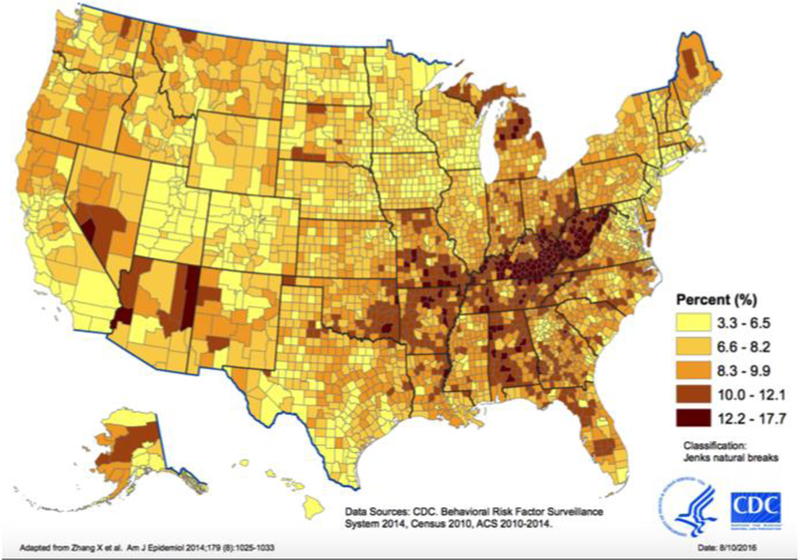
Age-standardized prevalence of chronic obstructive pulmonary disease (COPD) among adults aged ≥ 18 years. Source: CDC, Behavioral Risk Factor Surveillance System, 2014, Census 2010, ACS 2010–2014. www.cdc.gov/copd/pdfs/COPD_cnty2014_saeColor_2.pdf
The Community health-vulnerability Index (Rappold et al., 2017, see Fig. 7) provides an index at the county-level based on factors that increase risk such as respiratory and vascular disease, age, diabetes and obesity and SES parameters as well as the magnitude of annual exposure from the distribution of wildfire-PM2.5 as shown in Fig. 5. The map is instructive because it shows that the county-level risks for adverse health impacts are greatest in the southeastern United States. Even though the western states experience more large fires, the presence of a healthier population appears to lower the overall risk when compared to the counties in the southeastern and mid-Atlantic states.
Figure 7. Community Health-Vulnerability Index.
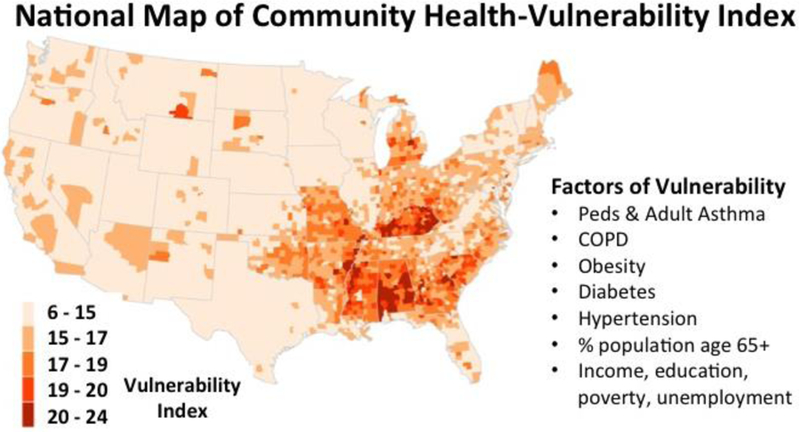
Adapted from Rappold et al., 2017.
7. Public Health Guidance and Interventions
One of the potential benefits of the Community Health-Vulnerability Index (Rappold, et al. 2017) is that its use could increase awareness of local wildland fire health risks among public health officials and healthcare professionals responsible for the wellbeing of the affected communities. Researchers in the U.S. Center for Disease Control and Prevention’s National Center for Environmental Health are currently developing a similar tool for integration into the Environmental Tracking Network as a national online tool for identifying at-risk populations, and providing public health guidance during wildland fire events (Vaidyanathan et al., 2017). Increased awareness of health risk is more likely to prompt public health officials and health care professionals to advise at-risk individuals to take action to avoid exposures to wildland fire smoke. One source of readily available and up-to-date information to assist public health and health care professionals is the “Wildfire Smoke: Guide for Public Health Officials”. The guide is a comprehensive summary of information available at the US EPA’s AirNow.gov website (URL: ttps://www3.epa.gov/airnow/wildfire_may2016.pdf) to assist public health officials to prepare for wildland fire smoke, and provides information to share with the public to protect them during such events. The guide offers specific strategies to reduce smoke exposure as well as how to communicate particulate matter concentrations and recommendations for public health action.
While recommending interventions to limit exposure to wildland fire smoke is prudent, particularly among those at highest risk, studies are needed to evaluate the benefits of such interventions. Considering the available data portable air filters have been advocated as a public health response to wildfire smoke (Barn et al., 2016). Fisk and Chan (Fisk and Chan, 2016) further advanced this concept by estimating the health benefits expected of in-home interventions that improve the quality of the indoor air during wildfires. Their analysis indicated that particle filtration in the homes of people at highest risk from the adverse effects of smoke is expected to be economically beneficial (Fisk and Chan, 2016).
A study conducted in Taipei between 2013 and 2014 tested the effect of air home air filtration on biomarkers of inflammation, oxidative stress and blood pressure. The crossover intervention study showed that increased exposure to PM2.5 and total VOCs increased inflammation, oxidant stress and blood pressure, and that in-home air filtering decreased biomarkers of inflammation, oxidative stress and the acute phase reactant fibrinogen (Chuang et al., 2017). This study provides biological plausibility for the modeled outcomes predicted by Fisk and Chan (Fisk and Chan, 2016).
It is imperative that effective public health communication strategies be developed in conjunction with communities, public health officials, health care professionals and state officials because the public health impacts of wildland fire smoke will continue to increase (Liu et al., 2016).
8. Knowledge Gaps and Research Opportunities
To effectively study the health effects of wildfire smoke or wildfire-related PM requires three key components: (1) an adequate assessment of exposure, (2) the availability of reliable data for the health metrics of interest, and (3) an exposed population of sufficient size and exposure gradients to have the statistical power to yield estimates of the association of exposure-health outcome having statistical confidence. Prior to the last decade, epidemiological studies of the health effects of wildland fires were very limited because the occurrences of wildland fires are for the most part unpredictable and occur in sparsely populated wilderness or rural areas that are not typically included in the ambient air pollutant monitoring network.
At a minimum, exposure assessment requires the location, the pollutants present at that location and their concentration, and the duration of exposure. Exposures have been estimated by a number of methods that include comparison of smoky versus non-smoky days, monitored PM, modeled PM, satellite indicators of smoke, temporal and spatial comparisons, and integration of PM monitoring, statistical modeling and satellite imaging (Reid et al., 2016a). Importantly, health effect estimates can be affected by the methods used to estimate exposure (Gan et al., 2017). Thus, the accuracy of the measured relationship between wildfire emissions and health effects depends on our ability to accurately estimate the exposure of an individual to one or more pollutants. More research is needed to integrate measurements and modeling to improve exposure assessments. Ideally, such assessments would also include both indoor and outdoor exposures, the constituents of the emissions and activity.
A more detailed and realistic assessment of the health impacts of wildfire smoke exposure has been made possible by the recent technological advances such as estimates of the temporal and spatial distribution of wildfire-PM concentrations and exposure afforded by satellite imaging of aerosol optical density, and the integration of satellite-based data with other sources of directly measures or modeled air pollution data (van Donkelaar, et al., 2010), GIS coding of residences of exposed individuals, and the availability of large health data sets to test associations. A literature search in Pubmed.gov of the terms “(((wildland fire or wildfire or forest fire or prescribed fire))) AND ((air pollution or particulate matter or smoke or PM2.5))) AND health” identified 207 publications between 1990 and November 21, 2017, of which 176 were published during or after 2006. The dramatic increase in epidemiological studies over the last decade highlights just how recent the developments in exposure modeling and epidemiology have allowed the study of the relationship between wildfire smoke and health effects.
Health outcomes have been expressed in many different forms and include: mortality, hospitalizations, emergency department visits, physician office visits, and medication usage (Reid et al., 2016a). Figure 8 illustrates the wide variety of health effects attributed to wildfire smoke density or wildfire-PM. Responses range from asymptomatic subclinical biological and physiological responses affecting a large number of exposed individuals to smaller numbers demonstrating worsened clinical manifestations requiring medication use, healthcare system utilization, and even death. Associations between wildfire smoke density or wildfire-PM and health effects are best defined for mortality, hospitalizations, and emergency department utilization because of the accessibility of such health data. On the other hand an assessment of the full public health impact and societal burden of wildfire emissions are not known because data corresponding to symptoms contributing to impaired function, discomfort, lost work and productivity is not readily available.
Figure 8.
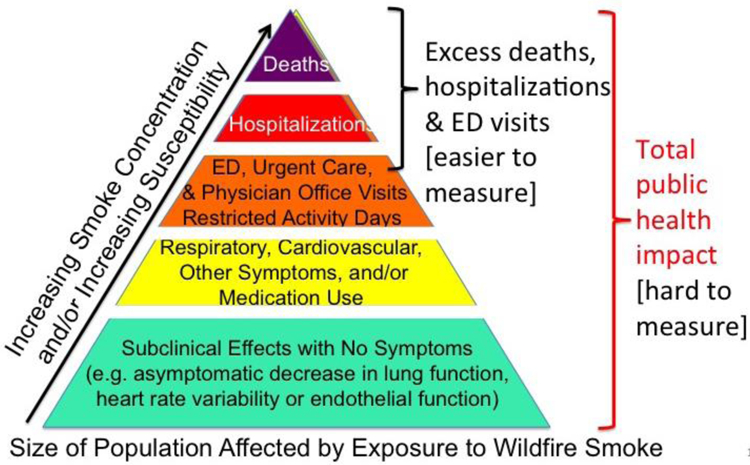
Clinical and Sub-Clinical Impacts of Wildfire Smoke or PM2.5
As we look the future, satellite imaging and atmospheric modeling of smoke concentrations are anticipated to improve. Other pollutants are likely to be included offering opportunities to explore co-pollutant interaction. Lower cost, portable PM monitors are expected to be available for deployment to sample real-time ground-level concentrations and increase the spatial resolution of ground-based PM2.5 measurements and enhance the value of integrated exposure models. Availability of more health information perhaps through access to electronic health records will further increase the temporal and spatial resolution and statistical power of the epidemiology studies.
More large-scale epidemiology studies will help better define health effect estimates and the public health burden of wildland fires with particular attention to common and costly health conditions such as heart and vascular disease and vulnerable populations. Such large-scale epidemiology studies also have an important role to play when comparing the aggregated health effects of large and less frequent wildland fires to small and more frequent prescribed fires.
Studies are needed to evaluate the health and economic benefit of interventions intended to decrease emissions and exposure. Mitigation of the health effects caused by exposure to smoke includes management of emissions as well as avoidance of exposure. For example does smoke management during prescribed fire mitigate the adverse health effects of wildland fire by optimizing the timing and environmental conditions at the time of the fire? To achieve the best outcomes of interventions, the public and especially those individuals at greatest risk must understand their risk and be willing to take action to avoid smoke exposure. Does increasing awareness among those at greatest risk motivate behavioral actions that limit exposure and mitigate adverse health impacts? Research in the social sciences is needed to better understand the modifying effects of non-chemical and social stressors or conditions and use this information to develop more effective communication strategies (Olsen, et al., 2014) that will increase awareness and willingness to take actions to protect health (Wells et al., 2012). It is important to learn what people are willing to do to decrease their risk from air pollution accompanying wildland fire. Are they willing to stay indoors, use in-home HEPA filtering, and wear an N-95 respirator when outdoors? Will pharmacological or dietary supplements taken before and during exposure curtail the health effects of wildland fire smoke? Health care professionals, hospital systems, and even health insurers also have a role to play in increasing the awareness of their at-risk patients about actions they can take to limit exposure to smoke from landscape fire.
9. Final Comments
In summary, exposure to wildfire emissions is an important and growing public health and clinical problem affecting tens of millions of people in the United States. Changing weather patterns including drought are increasing risks of wildland fire and risks of co-morbidity. Populations at greatest risk include people with chronic lung disease, older individuals, children, pregnant women and fetuses. Individuals with pre-existing heart disease are also likely to be at increased risk. An expanding wildland-urban interface and an aging U.S. population are increasing the size of vulnerable and sensitive populations. Studies are now providing estimates of health costs associated with wildland fire events and such information will likely be very valuable when considering the relative benefits of various land management policies and practices to prevent catastrophic wildland fires. Yet, knowledge gaps persist and require ongoing research related to population health effects. Effective smoke management is an important component of maintaining population health. Better communication of actionable information by public health officials and health care professionals is needed to more effectively improve the response of the public particularly those at highest risk.
For more information regarding wildfire smoke, wildfire science and health visit the following websites: EPA AirNow (www.airnow.gov) and Fires: Current Conditions webpage (https://airnow.gov/index.cfm?action=topics.smoke_wildfires), U.S. Forest Service, Wildfire (www.fs.fed.us/managing-land/fire), Centers for Disease Control and Prevention, Wildfire Smoke (www.cdc.gov/disasters/wildfires/smoke.html), NASA, Wildfire and Smoke (https://www.nasa.gov/mission_pages/fires/main/index.html), NOAA, Smoke Forecasting System (http://www.arl.noaa.gov/smoke.php), National Interagency Fire Center (www.nifc.gov), and Joint Fire Science Program (www.firescience.gov), and Department of the Interior Office of Wildland Fire (https://www.doi.gov/wildlandfire).
Highlights.
Wildland fire smoke exposure is an important and growing risk to public health.
The size of the population at-risk from wildland fire smoke is increasing.
Averting catastrophic wildfire and personal exposure will likely improve health.
Stakeholder cooperation is needed to limit the health effects of wildland fire.
Research is needed to assess the health benefits of avoiding smoke exposure.
Acknowledgements:
The review was supported by the U.S. Environmental Protection Agency, Office of Research and Development.
Footnotes
Publisher's Disclaimer: Disclaimer: The research described in this article has been reviewed by the National Health and Environmental Effects Research Laboratory, U.S. Environmental Protection Agency, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the Agency, nor does the mention of trade names of commercial products constitute endorsement or recommendation for use.
The author declares no competing financial interest.
References:
- Alman BL, Pfister G, Hao H, Stowell J, Hu X, Liu Y, Strickland MJ, 2016. The association of wildfire smoke with respiratory and cardiovascular emergency department visits in Colorado in 2012: a case crossover study. Environ. Health 15, 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barn PK, Elliott CT, Allen RW, Kosatsky T, Rideout K, Henderson SB, 2016. Portable air cleaners should be at the forefront of the public health response to landscape fire smoke. Environ. Health 15, 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bladon KD, Emelko MB, Silins U, Stone M, 2014. Wildfire and the future of water supply. Environ Sci. Technol 48, 8936–43. [DOI] [PubMed] [Google Scholar]
- Chuang HC, Ho KF, Lin LY, Chang TY, Hong GB, Ma CM, Liu IJ, Chuang KJ, 2017. Long-term indoor air conditioner filtration and cardiovascular health: A randomized crossover intervention study. Environ. Int 106, 91–96. [DOI] [PubMed] [Google Scholar]
- Fann N, Alman B, Broome RA, Morgan GG, Johnston FH, Pouliot G, Rappold AG, 2018. The health impacts and economic value of wildland fire episodes in the U.S.: 2008–2012. Sci. Total Environ 610–611, 802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes PM, Botelho HS, 2003. A review of prescribed burning effectiveness in fire hazard reduction. Int. J. Wildland Fire 12 117–28. [Google Scholar]
- Fisk WJ, Chan WR, 2017. Health benefits and costs of filtration interventions that reduce indoor exposure to PM2.5 during wildfires. Indoor Air 27, 191–204. [DOI] [PubMed] [Google Scholar]
- Flannigan MD, Krawchuk MA, de Groot WJ, Wotton BM, Gowman LM, 2009. Implications of changing climate for global wildland fire. Int. J. Wildland Fire 18, 483–507. [Google Scholar]
- Gan RW, Ford B, Lassman W, Pfister G, Vaidyanathan A, Fischer E, Volckens J, Pierce JR, Magzamen S, 2017. Comparison of wildfire smoke estimation methods and associations with cardiopulmonary-related hospital admissions. Geohealth 1, 122–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haikerwal A, Akram M, Del Monaco A, Smith K, Sim MR, Meyer M, Tonkin AM, Abramson MJ, Dennekamp M, 2015. Impact of fine particulate matter (PM2.5) exposure during wildfires on cardiovascular health outcomes. J. Am. Heart Assoc 4, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hohner AK, Cawley K, Oropeza J, Summers RS, Rosario-Ortiz FL, 2016. Drinking water treatment response following a Colorado wildfire. Water Res 105, 187–198. [DOI] [PubMed] [Google Scholar]
- Holstius DM, Reid CE, Jesdale BM, Morello-Frosch R, 2012. Birth weight following pregnancy during the 2003 Southern California wildfires. Environ. Health Perspect 120, 1340–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe DA, Wigder NL, 2012. Ozone from wildfires: A critical review. Atmos. Environ 51, 1–10. [Google Scholar]
- Johnston FH, Henderson SB, Chen Y, Randerson JT, Marlier M, Defries RS, Kinney P, Bowman DM, Brauer M, 2012. Estimated global mortality attributable to smoke from landscape fires. Environ. Health Perspect 120, 695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BA, Berrens RP, 2017a. Application of an original wildfire smoke health cost benefits transfer protocol to the Western US, 2005–2015. Environ. Manage 60, 809–22. [DOI] [PubMed] [Google Scholar]
- Jones BA, 2017b. Are we underestimating the economic costs of wildfire smoke? An investigation using the life satisfaction approach. J. For. Econ 27, 80–90. [Google Scholar]
- Kim YH, Tong H, Daniels M, Boykin E, Krantz QT, McGee J, Hays M, Kovalcik K, Dye JA, Gilmour MI, 2014. Cardiopulmonary toxicity of peat wildfire particulate matter and the predictive utility of precision cut lung slices. Part. Fibre Toxicol 11, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollanus V, Tiittanen P, Niemi JV, Lanki T, 2016. Effects of long-range transported air pollution from vegetation fires on daily mortality and hospital admissions in the Helsinki metropolitan area, Finland. Env. Res 151, 351–358. [DOI] [PubMed] [Google Scholar]
- Kollanus V, Prank M, Gens A, Soares J, Vira J, Kukkonen J, Sofiev M, Salonen R,O., Lanki T, 2017. Mortality due to vegetation fire-originated PM2.5 exposure in Europe-assessment for the years 2005 and 2008. Environ. Health Perspect 125, 30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le GE, Breysse PN, McDermott A, Eftim SE, Geyh A, Berman JD, Currierro FC, 2014. Canadian forest fires and effects of long-range transboundary air pollution on hospitalizations among the elderly. ISPRS Int. J. Geo-Inf 3, 713–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Pereira G, Uhl SA, Bravo MA, Bell ML, 2015. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res 136, 120–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Mickley LJ, Sulprizio MP, Dominici F, Yue X, Ebisu K, Anderson GB, Khan RFA, Bravo MA, Bell ML, 2016. Particulate air pollution from wildfires in the Western US under climate change. Clim. Change 138, 655–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Wilson A, Mickley LJ, Dominici F, Ebisu K, Wang Y, Sulprizio MP, Peng RD, Yue X, Son JY, Anderson GB, Bell ML, 2017a. Wildfire-specific fine particulate matter and risk of hospital admissions in urban and rural counties. Epidemiology 28, 77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Wilson A, Mickley LJ, Ebisu K, Sulprizio MP, Wang Y, Peng RD, Yue X, Dominici F, Bell ML, 2017b. Who among the elderly is most vulnerable to exposure and health risks of PM2.5 from wildfire smoke? Am. J. Epidemiol 186, 730–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman M,J.K., Driscoll AK, Matthews TJ, 2017. National Vital Statistics Report: Births Final Data for 2015 66, 1–69. https://www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_01.pdf. (Accessed December 1, 2017) [PubMed] [Google Scholar]
- Navarro KM, Cisneros R, O’Neill SM, Schweizer D, Larkin NK, Balmes JR, 2016. Air-quality impacts and intake fraction of PM2.5 during the 2013 Rim Megafire. Environ. Sci. Technol 50, 11965–11973. [DOI] [PubMed] [Google Scholar]
- Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, Forastiere F, Franchini M, Franco OH, Graham I, Hoek G, Hoffmann B, Hoylaerts MF, Künzli N, Mills N, Pekkanen J, Peters A, Piepoli MF, Rajagopalan S, Storey RF; ESC Working Group on Thrombosis, European Association for Cardiovascular Prevention and Rehabilitation; ESC Heart Failure Association., 2015. Expert position paper on air pollution and cardiovascular disease. Eur Heart J 36, 83–93. doi: 10.1093/eurheartj/ehu458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen CS, Mazzotta DK, Toman E, Fischer AP, 2014. Communicating about smoke from wildland fire: challenges and opportunities for managers. Environ Manage 54, 571–82. [DOI] [PubMed] [Google Scholar]
- Parthum B, Pindilli E, Hogan D, 2017. Benefits of the fire mitigation ecosystem service in The Great Dismal Swamp National Wildlife Refuge, Virginia, USA. J. Environ. Manage 203, 375–382. [DOI] [PubMed] [Google Scholar]
- Rappold AG, Stone SL, Cascio WE, Neas LM, Kilaru VJ, Carraway MS, Szykman JJ, Ising A, Cleve WE, Meredith JT, Vaughan-Batten H, Deyneka L, Devlin RB, 2011. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ. Health Perspect 119, 1415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold AG, Cascio WE, Kilaru VJ, Stone SL, Neas LM, Devlin RB, Diaz-Sanchez D, 2012. Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environ. Health 11, 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold AG, Fann NL, Crooks J, Huang J, Cascio WE, Devlin RB, Diaz-Sanchez D, 2014. Forecast-based interventions can reduce the health and economic burden of wildfires. Environ. Sci. Technol 48, 10571–9. [DOI] [PubMed] [Google Scholar]
- Rappold AG, Reyes J, Pouliot G, Cascio WE, Diaz-Sanchez D, 2017. Community vulnerability to health impacts of wildland fire smoke exposure. Environ. Sci. Technol 51, 6674–6682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT, 2016a. Critical review of health impacts of wildfire smoke exposure. Environ. Health Perspect 124, 1334–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid CE, Jerrett M, Tager IB, Petersen ML, Mann JK, Balmes JR, 2016b. Differential respiratory health effects from the 2008 northern California wildfires: A spatiotemporal approach. Environ. Res 150, 227–35. [DOI] [PubMed] [Google Scholar]
- Tinling MA, West JJ, Cascio WE, Kilaru V, Rappold AG, 2016. Repeating cardiopulmonary health effects in rural North Carolina population during a second large peat wildfire. Environ. Health 15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanski SP, Hao WM, Baker S, 2009. Chemical Composition of Wildland Fire Smoke, in: Arbaugh M, Riebau A, Andersen C (Eds.), Developments in Environmental Science, Volume 8 A Bytnerowicz, Elsevier B.V. pp. 79–107. ISSN: 1474–8177/DOI: 10.1016/S1474-8177(08)00004-1. [DOI] [Google Scholar]
- US Census Bureau, 2017a. Profile America Facts for Features: Older Americans Month: May 2017 March 17, 2917. https://www.census.gov/content/dam/Census/newsroom/facts-for-features/2017/cb17-ff08.pdf (Accessed December 1, 2017)
- US Census Bureau, 2017b. https://www.census.gov/quickfacts/fact/table/US/PST045216. (Accessed December 1, 2017).
- U.S. Centers for Disease Control and Prevention, 2015a. National Center for Statistics https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_A-1.pdf (Accessed December 1, 2017)
- U.S. Centers for Disease Control and Prevention, 2015b. Summary Health Statistics: National Health Interview Survey, 2015 https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_A-2.pdf. (Accessed December 1, 2017)
- US Department of Agriculture, Forest Service, 2015. The rising cost of wildfire operations: Effect on the Forest Service’s Non-Fire Work August 4, 2015 https://www.fs.fed.us/sites/default/files/2015-Fire-Budget-Report.pdf (accessed November 19, 2017)
- US Environmental Protection Agency, 2009. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, Dec 2009) https://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=216546 (accessed November 19, 2017)
- Vaidyanathan A, Yip F, Garbe P., 2017. Developing an online tool for identifying at-risk populations to wildfire smoke hazards. Sci. Total Environ 619-620, 376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Donkelaar A, Martin RV, Brauer M, Kahn R, Robert Levy R, Verduzco C, Villeneuve PJ, 2010. Global estimates of ambient fine particulate matter concentrations from satellite-based aerosol optical depth: Development and application. Environ Health Perspect 118:847–855 (2010). doi: 10.1289/ehp.0901623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicedo-Cabrera AM, Esplugues A, Iñíguez C, Estarlich M, Ballester F, 2016. Health effects of the 2012 Valencia (Spain) wildfires on children in a cohort study. Environ. Geochem. Health 38, 703–12. [DOI] [PubMed] [Google Scholar]
- Wells EM, Dearborn DG, Jackson LW, 2012. Activity change in response to bad air quality, National Health and Nutrition Examination Survey, 2007–2010. PLoS ONE 7, e50526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao J, Brauer M, Henderson SB, 2013. Evaluation of a wildfire smoke forecasting system as a tool for public health protection. Environ. Health Perspect 121, 1142–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youssouf H, Liousse C, Roblou L, Assamoi EM, Salonen RO, Maesano C, Banerjee S, Annesi-Maesano I, 2014. Non-accidental health impacts of wildfire smoke. Int. J Environ. Res. Public Health 11, 11772–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong J, Urch B, Speck M, Coull BA, Koutrakis P, Thorne PS, Scott J, Liu L, Brook RD, Behbod B, Gibson H, Silverman F, Mittleman MA, Baccarelli AA, Gold DR, 2015. Endotoxin and β−1,3-d-glucan in concentrated ambient particles induce rapid increase in blood pressure in controlled human exposures. Hypertension 66, 509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zu. K, Tao G, Long C, Goodman J, Valberg P, 2016. Long-range fine particulate matter from the 2002 Quebec forest fires and daily mortality in Greater Boston and New York City. Air Qual. Atmos. Health 9, 213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]


