Abstract
BACKGROUND:
Vitamin D deficiency is the most common nutritional deficiency worldwide in all ages. Prolonged and severe vitamin D deficiency can result in secondary hyperparathyroidism and osteomalacia. Vitamin D deficiency can be caused by various factors included here institutionalisation, malabsorption, inadequate exposure to sunlight etc. Osteomalacia is a disorder of decreased mineralisation of newly formed osteoid at sited of bone turnover, which can be manifested with symptoms such as diffuse body aches and pain. Muscles weakness from vitamin D deficiency causes difficulty in walking, developing proximal myopathy. Nearly 30-50% of all age groups are Vitamin D deficient worldwide.
CASE PRESENTATION:
We report a case of 51-years-old woman, with a religious garment, with slowly progressing weakness of the proximal limb muscles, extreme fatigue, chest and lower spine pain, paresthesia, depression, difficulties in walking and waddling gait. On whole-body bone scintigraphy diffuse metabolic changes were present, and in DXA osteoporosis was shown due to severe vitamin D deficiency and secondary hyperparathyroidism. Treatment with high doses of vitamin D and calcium replacement improved clinical manifestation of osteomalacia for few months. Absent of waddling gait with no pain was evident due to the better muscle and bone performance after the treatment.
CONCLUSION:
Suspicious cases for osteomalacia in population wearing a religious garment and those that are not adequately exposed to the sunlight, laboratory evaluation should include measurement of 25 (OH) vitamin D, PTH, calcium, alkaline phosphatase and performing of DXA in order such cases do not get undiagnosed.
Keywords: Osteomalacia, Myopathy, Vitamin D deficiency
Introduction
Vitamin D deficiency is the most common nutritional deficiency worldwide in both children and adults. It has been defined and recently recommended by the Institute of Medicine (IOM) as a 25(OH) vitamin D less than 20 ng/mL. Nearly 30-50% of all age groups are Vitamin D deficient worldwide [1].
Osteomalacia is a disorder of decreased mineralisation of newly formed osteoid at sited of bone turnover, which can be manifested with symptoms such as diffuse body aches and pain. Prolonged and severe vitamin D deficiency can result in secondary hyperparathyroidism and osteomalacia.
Vitamin D deficiency can be caused by various factors as nutritional, inadequate exposure to sunlight or concealing clothing, malabsorption resulting from intestinal inflammation, celiac disease or gastric surgery, prolonged use of anticonvulsants and corticoids, at hospitalised persons, as well at institutionalised persons and others [2]. Vitamin D is crucial for calcium, phosphorus and bone metabolism. Low 25(OH), vitamin D status, leads to reduced efficiency in intestinal calcium and phosphorus absorption, and the body reacts by increasing the secretion of parathyroid hormone (PTH) [3]. To maintain serum calcium in the normal range, secondary hyperparathyroidism is activated mobilising calcium from the skeleton and increasing phosphorus wasting in the kidneys. High level of PTH increases osteoclastic activity resulting from the inadequate calcium-phosphorus product, causing mineralisation defect in the skeleton (local foci), which can contribute to a generalised decrease in bone mineral density (BMD), resulting in osteopenia and osteoporosis. Alkaline Phosphatase (ALP) levels are usually elevated in secondary hyperparathyroidism due to osteomalacia.
Vitamin D deficiency and increased serum PTH concentration, in the children, can result with rickets, in adults when epiphysis plates are closed, this defect in mineralisation, bone turnover and bone loss, can result as osteomalacia. Muscles weakness from vitamin D deficiency causes difficulty in walking from the abnormal muscle contraction and increasing their risk of fracture. And decreased muscle strength is observed at the level below 30 nmol/l of 25(OH)Vitamin D.
Vitamin D receptor (VDR) is a member of the nuclear receptor, located in various tissues and cells in the body, revealing different biological effects based on different molecular pathways [4]. Based on the results of different studies, it was shown that vitamin D is implicated in the regulation of the immune system, the cardiovascular system, oncogenesis [5], and cognitive functions. More than 30 years ago, Yoshikawa et al., showed in their study a direct link between hypovitaminosis and muscle function at the patients with rickets and developing proximal myopathy in osteomalacia [7].
Women who wear concealing clothing like hijab may be at greater risk for vitamin D deficiency and have poor bone status and also can adversely affect muscle function [6].
Case Presentation
We report the case of a 51 years old woman admitted in our Clinic on April 2014, with several years’ history of extreme fatigue, pain in lower extremities, pelvis, lower spine and the chest, paresthesia, depression, weight loss and difficulties in walking (waddling gait). The patient has no history of metabolic diseases, married and 2 healthy children and 1 child dead from leukaemia. Before two years she was hospitalised and treated as fibromyalgia (with NSAIDs etc.), but with no improvement in her clinical manifestation. In physical examination, demineralisation of teeth, Trendelenburg sign positive (waddling gait) was detected. Twenty-five (OH) vitamin D3 was extremely low 3 ng/mL and parathyroid hormone level was found to be very high (PTH) 423 pg/mL (Table 1) which shows severe Vitamin D deficiency.
Table 1.
Laboratory analyses before and after the treatment
| Baseline data | Data after the treatment | Reference values | |
|---|---|---|---|
| Vitamin D (25-OH Vitmanin D) | 3 | 30.1 | < 9.9 ng/mL severe deficiency |
| iPTH | 423.6 | 97.8 | 12.0-72.0 pg/mL |
| Total Calcium | 2.0 | 2.1 | 2.15-2.57 mmol/L |
| Ionized Calcium | 1.0 | 1.1 | 1.12-1.32 mmol/L |
| Alkaline phosphatase | 200 | 324 | 53-128 U/L |
| Phosphorus | 0.6 | 0.98 | 0.48-2.26 mmol/L |
Inflammation markers and thyroid hormones were normal. Antibodies for celiac disease were negative, renal and hepatic functions were normal. In electrocardiography (ECG), no signs were evident for coronary insufficiency. On whole-body bone scintigraphy (Figure 1) diffuse metabolic changes were present (characteristic looser zones in chest ribs and knees bones). In dual-energy X-ray absorptiometry scan (DXA) were shown marked changes as low body mass density and severe osteoporosis (Table 2). Biopsy through gastroesophagoscopy-revealed-chronic gastroduodenitis – lymphoplasmacytic inflammatory infiltrates. Thyroid and parathyroid ultrasound were normal, and no signs and symptoms for cardiovascular diseases (CVD).
Figure 1.
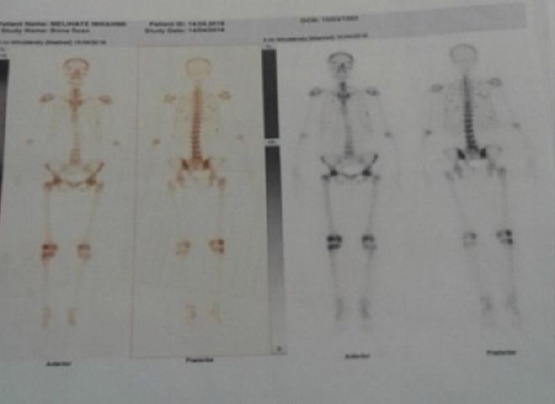
Whole-body bone scintigraphy before the treatment with characteristic chest and knees bone looser zones
Table 2.
DXA* before and after the treatment
| Baseline data | Data after the treatment | |||||
|---|---|---|---|---|---|---|
| Region | BMD** | T- | Z- | BMD | T- | Z- |
| Right femur | 0.521 | -3.4 | -2.9 | 0.787 | -1.3 | 0.7 |
| Left femur | 0.586 | -2.9 | -2.4 | 0.819 | -1.3 | -0.6 |
| L-spine | 0.686 | -3.3 | -2.5 | 0.919 | -1.2 | -0.6 |
DXA-dual-energy X-ray absorptiometry scan;
BMD-bone mineral density.
The patient was wearing the religious garment (hijab) and had almost no exposure to the sunlight for years.
In the following are presented laboratory investigation that revealed a severe deficiency of 25(OH) vitamin D, high PTH, low calcium and high alkaline phosphatase before the treatment and improvement of these data six months after the treatment (Table 1). In the meantime, DXA revealed low BMD in all relevant part of both femur region and L-spine and an impressive improvement of these data after the treatment for the same period (Table 2).
In the lumbosacral radiography, there were revealed the sign of osteomalacia like biconcave vertebral bodies (fish vertebrae) and upper anterior fracture of the 5th lumbar vertebra (probably fracture of osteophyte (Figure 2).
Figure 2.

Biconcave vertebral bodies (fish vertebrae) and upper anterior fracture of the 5th lumbar vertebra osteophyte
To avoid malabsorption of vitamin D due to gastrointestinal lymphoplasmacytic inflammatory infiltrates, it was initiated Cholecalciferol (vitamin D3) i.m. 300 000 UI at once, followed by vitamin D3 50 000 UI/per week oral solution and, calcium 1000 mg 1x1 daily together with dairy products for one month, then followed with 25 000 UI/per week oral solution for other two months. Appropriate sun exposure in daily bases was recommended and other necessary treatment. Last three months, appropriate doses of Vitamin D were ordered in oral tablets.
After 6 months of the treatment, she gains 3 kg and impressive improvement in walking were evident (no Trendelenburg sing and waddling gait), no pain and paraesthesia, and no signs and complaints of depression were observed. The last DXA revealed normal values of BMD and T score (Table 2).
Discussion
In this report, we described our female patient, which was admitted with muscles weakness, pain in a different part of the body and waddling gait due to osteomalacia. Latest evidence showed the very important role of vitamin D in muscle growth, strength and gait, confirming that hypovitaminosis D is always associated with a decrease in muscle function and performance and an increase in disability. Progressive difficulties in changing the body position, or rising from a chair followed with diffuse muscle pain are all symptoms of myopathy from osteomalacia [8]. Effect of active form of vitamin D, calcitriol or 1, 25-dihydroxy vitamin D3 on the muscle tissue is based in two molecular mechanism by binding to the nuclear receptors (genomic effect) and protein synthesis through RNA messenger to drive cellular differentiation and proliferation [8], [9] and by binding to a membrane-bound receptors (non-genomic effect) which in turn lead to a rapid influx of calcium into the cell [9].
In cases where is not available DXA, PTH values can be considered for evaluation of cases with severe vitamin D deficiency, [10] and normal renal function. The effects on muscular fibres are based on hypocalcaemia that can impact on decreased inhibition of nerves and muscle fibres depolarisation [11]. In the meantime, high level of PTH has to be considered except on bone tissues, also on progressive muscular weakness. [12]
Vitamin D supplementation is needed for women wearing concealing clothes to reach or maintain a healthy vitamin D status [13] and to avoid osteomalacia.
Severe vitamin D deficiency, along with electrolyte abnormalities such as low calcium and associated elevated PTH would suggest severe osteomalacia which may be manifested as muscular and neurological symptoms such as proximal weakness and paresthesia. Suspicious cases for osteomalacia in population wearing a religious garment and those that are not adequately exposed to the sunlight, laboratory evaluation should include measurement of 25 (OH) vitamin D, PTH, calcium, alkaline phosphatase and performing of DXA in order such cases do not get undiagnosed. In these cases, treatment with high doses of vitamin D and calcium supplements is essential to treat osteomalacia and myopathy.
Acknowledgement
We want to thank Shpresa Azemi, MD, resident of endocrinology for technical help, and Drita Mekuli, MD, department chair for general support.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid BiochemMol Biol. 2014;144:138–45. doi: 10.1016/j.jsbmb.2013.11.003. https://doi.org/10.1016/j.jsbmb.2013.11.003 PMid:24239505 PMCid:PMC4018438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ritu G, Gupta A. Vitamin D deficiency in India:prevalence, causalities and interventions. Nutrients. 2014;6(2):729–75. doi: 10.3390/nu6020729. https://doi.org/10.3390/nu6020729 PMid:24566435 PMCid:PMC3942730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heaney RP1. Toward a physiological referent for the vitamin D requirement. J Endocrinol Invest. 2014;37(11):1127–30. doi: 10.1007/s40618-014-0190-6. https://doi.org/10.1007/s40618-014-0190-6 PMid:25308199. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Zhu J, DeLuca HF. Where is the vitamin D receptor? Arch BiochemBiophys. 2012;523(1):123–33. doi: 10.1016/j.abb.2012.04.001. https://doi.org/10.1016/j.abb.2012.04.001 PMid:22503810. [DOI] [PubMed] [Google Scholar]
- 5.Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80(6 Suppl):1678S–88S. doi: 10.1093/ajcn/80.6.1678S. https://doi.org/10.1093/ajcn/80.6.1678S PMid:15585788. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, DeLuca HF. Is the vitamin d receptor found in muscle? Endocrinology. 2011;152(2):354–63. doi: 10.1210/en.2010-1109. https://doi.org/10.1210/en.2010-1109 PMid:21190957. [DOI] [PubMed] [Google Scholar]
- 7.Yoshikawa S, Nakamura T, Tanabe H, Imamura T. Osteomalacic myopathy. EndocrinolJpn. 1979;26(Suppl):65–72. doi: 10.1507/endocrj1954.26.supplement_65. https://doi.org/10.1507/endocrj1954.26.Supplement_65 PMid:467350. [DOI] [PubMed] [Google Scholar]
- 8.Pfeifer M, Begerow B, Minne HW. Vitamin D and muscle function. OsteoporosInt. 2002;13:187–194. doi: 10.1007/s001980200012. https://doi.org/10.1007/s001980200012 PMid:11991436. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton B. Vitamin D and human skeletal muscle. Scand J Med Sci Sports. 2010;20(2):182–90. doi: 10.1111/j.1600-0838.2009.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emini M, Morina N, Gerqari I, Alimehmeti I. Severe Osteoporosis in a Young Woman With Celiac Diseases due to Vitamin D Deficiency. Journal of Medical Cases. 2016;7(10):467–70. https://doi.org/10.14740/jmc2601w. [Google Scholar]
- 11.Armstrong CM, Cota G. Calcium block of Na+channels and its effect on closing rate. Proceedings of the National Academy of Sciences. 1999;96(7):4154–7. doi: 10.1073/pnas.96.7.4154. https://doi.org/10.1073/pnas.96.7.4154 PMid:10097179 PMCid:PMC22436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karim Hajjar K, Hagenacker T. Neuromuscular disorder as initial manifestation of secondary hyperparathyroidism - a case report. Eur J Transl Myol. 2017;27(1):40–42. doi: 10.4081/ejtm.2017.6100. https://doi.org/10.4081/ejtm.2017.6100 PMid:28458803 PMCid:PMC5391528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ojah RC, Welch JM. Vitamin D and musculoskeletal status in Nova Scotian women who wear concealing clothing. Nutrients. 2012;4(5):399–412. doi: 10.3390/nu4050399. https://doi.org/10.3390/nu4050399 PMid:22690323 PMCid:PMC3367264. [DOI] [PMC free article] [PubMed] [Google Scholar]


