Abstract
Introduction:
Few studies investigated the combined patterns of individual assets (e.g., social competence, positive identity) and mental health symptoms (MHS) in adolescents. This study examined the patterns of early adolescents’ individual assets and MHS and whether identified patterns were associated with later adolescents’ outcomes.
Methods:
Participants were 352 (164 boys, 188 girls) adolescents who were primarily African-American and from low socioeconomic status families, participating in a prospective study of the effects of prenatal cocaine exposure from birth in the Midwest United States. Individual assets, using the Developmental Assets Profile, and MHS, using the Youth Self-Report, were assessed at age 12. Substance use, via self-report and biologic assays, early (before age 15) sexual behaviors, and behavioral adjustment were assessed at age 15.
Results:
Latent profile analysis indicated four distinctive profiles: low assets with elevated MHS (P1, n=54, 15.3%); adequate assets with thought and social problems (P2, n=84, 23.9%); low assets without MHS (P3, n=101, 28.7%); and high assets without MHS (P4, n=113, 32.1%). Children in the profile with high assets without MHS (P4) were more likely to have a higher IQ and to be in a more optimal environment (higher parental monitoring and less family conflict) than those in other profiles. Although profiles with MHS were associated with adolescent risk behaviors, this relationship was more pronounced for girls than for boys.
Conclusions:
Girls in the low assets with elevated MHS (P1) should be a primary concern for preventive intervention. Our study demonstrates the heterogeneity of individual patterns of adaptation and maladaptation.
Keywords: Individual assets, Mental health symptoms, Latent Profile Analysis, Gender, Adolescents
Introduction
Adolescence is a period of rapid growth and learning. Marked by physical maturation, identity exploration, expanded social and peer relationships, academic challenges, and the drive for independence, adolescents are exposed to opportunities for both enrichment and risk experimentation (Schwartz, Pantin, Coatsworth, & Szapocznik, 2007; Warren, Wray-Lake, Rote, & Schubert, 2016). Studies on adolescence have tended to be problem-focused, attending to mental health symptoms (MHS) such as delinquency, depression, and substance use, in keeping with a “stress-and-storm” view of adolescence (Hall, 1904). From this perspective, the absence of problems is indicative of optimal adolescence development, and problem reduction is the focus of the intervention. In the 1990s, an alternative approach emphasizing the strength of youth and the plasticity of human development began to gain prominence (Lerner, 1998). In this approach, individual assets, such as school engagement (Li & Lerner, 2011), social competence (Burt & Roisman, 2010; Sørlie, Hagen, & Ogden, 2008), positive identity reflecting an optimistic future outlook and sense of purpose (Schmid, Phelps, & Lerner, 2011), positive values of honesty, integrity, responsibility, and caring that form a young person’s inner guidance system (Lerner et al, 2012), are expected to reduce the risk of MHS (Scales & Leffert, 2004; Schwartz et al., 2010).
Although MHS and individual strengths/assets tend to be inversely related to each other (Jelicic, Bobek, Phelps, Lerner, & Lerner, 2007), the magnitude of the correlation is modest at best (Kokko, Temblay, La course, Nagin, & Vitaro, 2006). Further, some behaviors typically thought to be risky (e.g., aggressive behaviors) may have adaptive values, especially in a resource-deprived, urban, inner-city with diminished opportunities and prospects (Ellis et al., 2012; Miller & Sperry, 1987; Min, Minnes, Kim, Yoon, & Singer., 2018), complicating further efforts to understand and promote optimal adolescent development. Using the 4-H study of Positive Youth Development (PYD) sample, Arbeit et al. (2014) demonstrated that higher levels of confidence and competence were found not only in adolescents showing fewer depressive symptoms and engagement in problem behaviors (bullying, delinquency, sexual activity), but also in adolescents reporting alcohol and marijuana use. This co-occurrence of adaptive functioning (conceptualized as self-esteem, life satisfaction, connection with others) and risk behavior (delinquency and substance use) was also observed in a subgroup of adolescents using a nationally representative United States sample (Warren et al. 2016), suggesting that the presence of strengths may not necessarily imply an absence of risk or MHS (Min et al., 2018a).
Although these studies represent an endeavor to understand adolescent development in a more comprehensive and integrative way (Masten & Curtis, 2000; Schwartz et al., 2007), relatively few studies have examined the combined patterns of both dimensions of MHS and individual assets as a whole, especially in at-risk adolescents. Assessing the totality of attributes, comprising both individual assets/strength and MHS in the context of each other rather than in isolation, is crucial for understanding the course of development (Cicchetti, 2013; Magnusson, 2003). The presence of any one attribute, whether it is strength or liability, will have different developmental implications depending on the complex matrix of individuals’ other characteristics. For example, child externalizing behavior problems may have different developmental implications depending on whether the child is socially competent or not. Only two empirical studies (Orpinas, Raczynski, Peter, Colman, & Bandalos, 2015; Rose, Lindsey, Xio, Finigan-Carr, & Joe, 2017), to our knowledge, examined different patterns across both strengths/assets and MHS within individual adolescents by identifying distinct groups via indicators of positive assets and MHS. Using the 6th-grade sample of the Healthy Teens Longitudinal Study data, Orpinas et al. (2015) examined teachers’ ratings on adaptive skills (i.e., leadership, social skills, and study skills), school problems (i.e., attention and learning problems), internalizing symptoms (i.e., anxiety, depression, and somatization), and externalizing symptoms (i.e., aggression, hyperactivity, and conduct) to identify meaningful groups with different configurations of adolescent assets and risks. Seven latent groups were identified. Two groups (“well-adapted” and “average”) did not have any problems, but the “well-adapted” had better study skills and fewer attention problems than the “average.” The “average, social skills deficit” group demonstrated lower leadership and study skills, but otherwise functioned at the level of the normative average. The “internalizing” group had borderline scores in anxiety and somatization, while functioning at the normal range in all other domains. Three groups were identified based on the severity of externalizing behavior problems-the “externalizing,” “disruptive behavior with school problems,” and “severe problems” groups- with children of severe problems having more pervasive problems across multiple domains, as indicated by greater internalizing and school problems and less adaptive skills.
Similarly, the Rose and colleagues’ study (2017) on a national probability sample of 1,170 Black adolescents aged 13–17 years, identified four groups: “troubled,” “vulnerable,” “symptomatic but content,” and “positive mental health.” Both the “troubled” and “vulnerable” groups had low levels of internal assets (defined as self-esteem, mastery, life satisfaction, and social integration), but the “troubled” group had high levels of psychopathology (defined as depressive symptoms and severity of mental disorder), while the “vulnerable” had low psychopathology. Both “symptomatic but content” and “positive mental health” had higher levels of internal assets but differed by the levels of psychopathology. Adolescents in the “symptomatic but content” group exhibited high levels of psychopathology, whereas those in the “positive mental health” group exhibited no psychopathology. Although both studies identified two typical common groups of well-adjusted/normative and maladjusted/troubled, differences in the nature of the samples, informants, operationalization of internal assets and MHS, and ages at assessment might yield variability in the number of subgroups and their nature.
The purpose of the current study is to identify the underlying classes of similar “profiles” on the basis of internal assets and MHS in at-risk urban children at 12 years through a person-oriented analytic approach (Lanza, Flaherty, & Collins, 2003). The person-centered approach allows detection of subgroups with distinct patterns of high and low scores across components of assets and MHS, which may not fit the average patterns generated by traditional variable-centered approaches. Thus, it is especially useful for identifying atypical subgroup such as children with positive assets yet MHS or children with no assets yet no MHS.
In order to better understand different profiles derived, we examined multiple socio-demographic characteristics shown to be related to individual assets and MHS, including child IQ (Harden et al., 2017), maternal education (Hughes, Toro, Harding, Way, & Rarick, 2016) and psychological distress (LaGasse et al., 2016; Singer et al., 1997; Min, Singer, Minnes, Kim, & Short, 2013), quality of the home environment (Min et al., 2014a; Singer et al., 2008), and adoptive/foster care placement (Linares et al., 2005; Singer et al., 2004). Also, we assessed variables characterizing the interpersonal developmental contexts in which adolescents transact (Cicchetti & Rogosch, 2002), such as parental attachment (Min, Minnes, Yoon, Short, & Singer, 2014b) and monitoring (Dittus et al., 2015), family conflict (Fosco, Stormshak, Dishion, & Winter, 2012), violence exposure (Kobulsky et al., 2016; Minnes et al., 2014), and maltreatment (Min et al., 2016; Min et al., 2018b).
The clinical significance and validity of each profile were evaluated by comparing adolescent substance use, early sexual risk behavior, and behavioral adjustment assessed at age 15. Interactions between the identified profiles and gender were explored due to well-known gender differences in patterns of drug use (Becker, McClellan, & Reed, 2016), sexual behaviors (Dir, Coskunpinar, & Cyders, 2014; Zimmer-Gembeck & Helfand, 2008; Min, Minnes, Lang, Yoon, & Singer, 2015), and mental health status (Else-Quest, Hyde, Goldsmith, & Van Hulle, 2006; Salk, Hyde, & Abramson, 2017). We hypothesized that: 1) heterogeneous profiles exist in at-risk urban children and can be identified as distinct subgroups; and 2) a more problematic profile (e.g., low assets with MHS) would be related to adolescent substance use, early sexual behavior, and poorer mental health.
Method
Sample and Procedure
The study sample consisted of 352 children (164 boys, 188 girls) recruited at birth (September 1994 to June 1996) from a large, urban, teaching hospital in the Midwest United States for a longitudinal investigation of the developmental effects of prenatal cocaine exposure (Min et al., 2014; Minnes et al., 2010; Minnes, et al., 2014; Singer et al., 2004; Singer et al., 2008). Drug toxicology screenings were administered to 647 mothers and infants at delivery who were identified to be high risk due to lack of prenatal care, maternal behavior suggesting intoxication, self-admitted drug use, or a history of involvement with the Department of Children and Family Services. Women with a psychiatric history of severe depression, bipolar disorder or schizophrenia, low intellectual functioning indicated in medical chart, HIV positive status or chronic medical illness were excluded, as were infants with Down syndrome, fetal alcohol syndrome or congenial heart defects. Of the 593 eligible participants, 415 infants enrolled in the study. Twelve children died after enrollment from sudden infant death syndrome (6), respiratory distress syndrome (2), cardiopulmonary arrest (1), pneumonia (1), accidental asphyxia (1), and unknown illness (1). The present study utilized data from 352 adolescents who completed a behavioral assessment at age 12, representing 87% retention of the 403 living participants. The 51 non-participating children (21 drop-out, 17 lost contact, 3 low intellectual functioning (IQ < 50), and 10 incomplete data) were more likely to be white (p < .04) and to have birth mothers who graduated from high school (p < .03) than the 352 participants. There were no other differences in sociodemographic and prenatal drug exposure characteristics.
The Institutional Review Board of the participating hospital approved all research procedures. The longitudinal follow-up assessments on children and their caregiver were conducted at the university-based developmental research lab at 1, 6, 12, and 18 months and 2, 4, 6, 9, 10, 11, 12, and 15 years of age postpartum. Parental written informed consent was obtained at each visit, with child assent beginning at age 9. At each follow up visit, a trained research assistant blind to cocaine exposure status, as well as other prenatal exposure, administered the behavioral and cognitive assessment protocol to the children. A different research assistant conducted caregiver interviews privately. All participants were given a monetary stipend, lunch, and transportation costs if needed. A Certificate of Confidentiality number (DA-98–91) was obtained from U.S. Department of Health and Human Services to protect the release of drug-related information.
Participating adolescents were primarily African American (n = 284, 80.7%), with an additional 11.3% White (n=40), 3.7% Hispanic (n=13), and 4.3% (n=15) biracial (n=13) or Asian (n=2). On average, adolescents were 12.09 (SD = .25) years of age at assessment. Forty-two percent of their mothers (n = 146) had not finished high school, with a mean of 11.73 years of education (SD = 1.56). A majority of the adolescents (n = 304, 86%) were prenatally exposed to at least one substance and two-thirds (n = 232) to ≥ 2 substances. Half of the children (n = 177) were prenatally exposed to cocaine, 64% (n = 217) to tobacco, 77% (n = 261) to alcohol, and 31% (n = 105) to marijuana. The majority of the sample reported being recipients of free lunch (n = 279, 84%) and Medicaid (n = 266, 80%) at age 15.
Measures
Child individual assets
Individual assets were assessed at age 12 using the 32-item Internal Assets subscale of the widely used Developmental Assets Profile (DAP; Search Institute, 2005). It is a youth self-report designed to assess 11 to 18 year-old adolescents’ positive experiences and qualities within the last 3 months using a 4-point Likert scale (0 = not at all/rarely; 1 = somewhat/sometimes; 2 = very/often; and 3 = extremely/always). The internal assets scale identifies characteristics and behaviors that reflect positive personal and psychosocial growth, including commitment to learning (7 items, α = .82; e.g., “I do my homework,” “I care about school”), positive values (11 items, α = .82; e.g., “I stand up for what I believe in,” “I stay away from tobacco, alcohol, and other drugs”), social competencies (8 items, α = .76; e.g., “I express my feelings in proper ways,” “I plan ahead and make good choices”), and positive identity (6 items, α = .70; e.g., “I feel good about myself,” “I feel in control of my life and future”), with a possible range of 0–30. Higher scores indicate greater assets, with scores < 15 indicating challenged, 15 – 20 vulnerable, 21 – 25 adequate, and > 25 indicating thriving assets (Scales, 2011).
Child mental health symptoms
Internalizing (anxious or depressed, withdrawn, somatic complaints; α= .86), externalizing (aggression and rule-breaking behaviors; α= .87), attention problems (α= .74), thought problems (α= .71), and social problems (α= .67) were assessed at age 12 using the Youth Self Report (YSR; Achenbach & Rescorla, 2001), a 105-item youth self-rating of emotional, behavioral and social problems in the last 6 months. Items were written at the 5th grade reading level and rated on a 3-point scale (0 = not true to 2= very often or often true). T-scores were standardized for gender and age, with higher scores indicating more MHS. T-scores < 60 in broadband (internalizing and externalizing) scores are considered in the normal range; 60–63 represent borderline scores; and scores > 63 are in the clinical range. T-scores < 65 in syndrome scale scores are considered in the normal range; 65–69 borderline scores; and scores > 69 are in the clinical range (Achenbach, 1991).
Adolescent outcomes at age 15
Adolescent substance use was assessed at age 15 using self-report and biologic assays. Self-reported alcohol, tobacco, and marijuana use were assessed using the Youth Risk Behavior Surveillance System (YRBSS; Centers for Disease Control and Prevention, 2009). Research nurses from the university’s NIH-funded Clinical Research Unit collected samples of participants’ urine, hair, and/or bloodspots, and sent them to the United States Drug Testing Laboratory for analysis (See Minnes et al., 2014 for a complete description of adolescent drug use assessment). Respondents positive on either self-report or biologic assays for a particular drug were coded 1 (yes) for that drug. Early sexual intercourse, defined as sexual intercourse prior to 15th birthday, was assessed at age 15 using the YRBSS. Behavioral adjustment was assessed at age 15 with the Problem Oriented Screening Instrument for Teenagers (POSIT), a self-report, multi-problem screening instrument composed of 139 yes/no questions designed to identify substance abuse and related problems in adolescents ages 12–19 years (Rahdert, 1991). Two subscales, Mental Health and Aggressive/Delinquent Behavior, were used in this study. The Mental Health subscale (α= .87) consists of 22 items representing emotional problems (e.g., feeling alone/nervous/sad most of the time, frustrated easily). The Aggressive/Delinquent behavior subscale (α= .74) consists of 16 items (e.g., threatening to hurt people, stealing, fighting a lot).
Socio-demographic variables
Infant sex and race were extracted from hospital birth records. Prenatal cocaine exposure was identified based on positive results of maternal or infant urine assay, infant meconium assay, or maternal self-report of cocaine use during pregnancy to medical or research staff at the newborn visit (coded as 1). Non-cocaine-exposed infants were negative on all indicators, but may have been exposed to alcohol, tobacco, and/or marijuana. Birth mothers also asked to recall frequency and amount of drug use for the month prior to and for each trimester of pregnancy at the newborn visit. The number of tobacco cigarettes and marijuana joints smoked per day, and the number of drinks of beer, wine, or hard liquor per week were computed, with each drink equivalent to 0.5 oz. of absolute alcohol. Frequency of use was recorded for each drug on a Likert-type scale ranging from 0 (not at all) to 7 (daily use) to reflect the average number of days per week the given drug was used, except for cigarettes, which was collected as the number smoked per day. The drug assessment was updated with the child’s current caregiver at each follow-up visit to assess recent (prior 30-day period) postpartum, caregiver drug use (See Singer et al., 2004 for a complete description of maternal drug use assessment during pregnancy). Maternal education in years was collected via research interview. Maternal psychological distress was assessed at the newborn visit and at each follow-up visit using the Global Severity Index (α= .95), a summary scale of the Brief Symptom Inventory (Derogatis, 1992). At each visit, the child’s placement (with either biological mother/relative or non-kinship adoptive/foster caregiver) and changes (defined by a change in both primary caregiver and physical setting lasting greater than one month) were also noted. Child Full Scale IQ was assessed at the 11-year visit using the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV; Wechsler, 2003).
At age 12 years, the quality of the caregiving environment was assessed via interview using the Home Observation of the Environment-Early Adolescent (HOME; α = .83; Caldwell & Bradley, 2003). Parental attachment and monitoring, family conflict, and violence exposure were also assessed using the Assessment of Liability and Exposure to Substance Use and Antisocial Behavior (ALEXSA; Ridenour et al., 2009), an illustration-based, audio, computer-assisted self-report of antisocial behavior, substance involvement and associated risk factors for children ages 9–12. The parental attachment scale is a 5-item questionnaire using a 4-point Likert scale (α = .79), assessing the youth’s perceived closeness with parents. The parental monitoring scale, a 5-item questionnaire using a 4-point Likert scale (α = .75), assesses the youths’ perceptions of whether their parent(s) usually is (are) aware of the youths’ activities and whereabouts. The family conflict index is a 10-item questionnaire assessing family conflict tactics, such as yelling, threatening to hurt, throwing, or hitting; the variable was a total count of these incidents. The violence exposure scale is an 8-item questionnaire using a 5-point Likert scale (α = .76), measuring lifetime exposure to violence (e.g., beating, robbery, stabbing, shooting), either as a direct victim or witness, with higher scores indicating greater exposure. At age 17, childhood maltreatment and sexual victimization were assessed (1= yes; 0= no) retrospectively using the Juvenile Victimization Questionnaire (JVQ)- Adult Retrospective Version (Hamby, Finkelhor, Ormrod, & Turner, 2004; Finkelhor, Hamby, Ormrod, & Turner, 2005).
Analyses
Latent profile analysis (LPA) was conducted to classify children into discrete profiles that share common characteristics of assets and MHS indexed by the nine continuous indicators from the DAP and the YSR. The assumption of local independence (i.e., no residual correlation among indicators within each latent class) of LPA was examined using standardized residuals (Collins& Lanza, 2010; Tein, Coxe, & Cham, 2013). Multivariate normality for the indicators within each profile and equal variances across latent profiles were examined using the plot distribution within each profile (Nylund, Asparouhov, & Muthén, 2007; Tein, Coxe, & Cham, 2013). Using Mplus v. 7.11 with the maximum likelihood estimator with robust standard errors, a series of LPAs were conducted to determine the optimal number of latent profiles by specifying 2-, 3-, 4-, 5-, and 6-profile solutions. Each solution was evaluated with multiple model fit indices, including Akaike Information Criterion (AIC), Bayesian Information Criteria (BIC), Adjusted BIC (ABIC), entropy (precision of the class), and the bootstrap likelihood ratio test (BLRT). The lower absolute value of AIC, BIC, and ABIC, as well as high entropy (close to 1) indicate a better fit for the data (Collins & Lanza, 2010; Jung & Wickrama, 2008; Nylund, Asparaouhov, & Muthén, 2007). The BLRT compares the target model’s fit with one less class, with p > .05 indicating the model with one fewer class to be a better fit (Nylund, Asparouhov, & Muthen, 2007). We also considered the meaning of each latent class (interpretability) and minimum class sizes to capture small but meaningful groups for the practical usefulness. As the number of profiles is determined, the most likely class variable was determined for each individual using the posterior probabilities of class membership obtained from LPA. Due to the different distribution of the DAP and the YSR, z-scores were calculated for comparison and used in a graphical illustration.
Validity of the LPA-derived profiles were examined by comparing profiles on sample characteristics using the AUXILIARY function in Mplus, which provides a chi-square test of the equality of means across classes, accounting for the uncertainty in classifying an individual in a group. We also examined how different profiles were associated with later adolescent outcomes using logistic regression analysis and ANOVA. When a profile had an overall significant effect, all pairwise profile differences were probed. Gender was tested for interaction with profiles. Adjusted least square means and standard errors were calculated from the estimated models.
Results
The means and standard deviations, along with zero-order correlations(r) and reliability (Cronbach’s α), for study variables are presented in Table 1. On average, the internal asset scores on the DAP were hovering in the lower end of the “adequate” range (~ 21), with T-scores on the YSR within the normative (> 60) range. Indicators of individual assets were substantially correlated with each other, from r = .54 between commitment to learning and positive identity to r = .74 between positive values and social competencies. Indicators of MHS on the YSR were also correlated to each other, from r = .52 between externalizing problems and social problems to r = .68 between externalizing problems and internalizing problems. All indicators of individual assets were inversely correlated to the indicators of MHS, with r = - .12 between commitment to learning and social problems to r = - .42 between social competencies and externalizing problems.
Table 1.
Correlations, descriptive statistics, and profile means for all study variables
| Internal Assets | Mental Health Symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| 1. Commitment, to learning | - | ||||||||
| 2. Positive values | .68*** | - | |||||||
| 3. Social competencies | .63*** | .74*** | - | ||||||
| 4. Positive identity | .54*** | .60*** | .66*** | - | |||||
| 5. Attention problems | − .27*** | − .28*** | − .30*** | − .26*** | - | ||||
| 6. Thought problems | − .17** | − .18** | − .21*** | − .15** | .56*** | - | |||
| 7. Social problems | − .12* | − .15** | − .27*** | − .24*** | .58*** | .62*** | - | ||
| 8. Internalizing problems | − .21*** | − .23*** | − .34*** | − .31*** | .54*** | .65*** | .68*** | - | |
| 9. Externalizing problems | − .39*** | − .42*** | − .42*** | − .29*** | .58*** | .54*** | .52*** | .54*** | - |
| Mean (Standard deviation) |
22.09 (5.88) |
20.75 (5.14) |
21.33 (5.50) |
20.66 (5.64) |
56.56 (7.59) |
57.31 (6.48) |
57.63 (7.29) |
53.34 (9.47) |
48.98 (9.99) |
| Cronbach’s alpha | .82 | .82 | .76 | .70 | .74 | .71 | .67 | .86 | .87 |
| Estimated means | |||||||||
| Profile 1 (n = 54) | 16.53 | 16.30 | 15.63 | 15.79 | 66.72 | 65.46 | 66.41 | 63.69 | 59.85 |
| Profile 2 (n = 84) | 24.07 | 22.17 | 22.97 | 22.01 | 59.31 | 61.66 | 61.95 | 59.30 | 53.26 |
| Profile 3 (n = 101) | 18.49 | 17.01 | 17.49 | 17.17 | 54.24 | 54.23 | 54.63 | 51.67 | 48.74 |
| Profile 4 (n = 113) | 26.42 | 25.07 | 26.18 | 25.02 | 51.72 | 52.97 | 52.93 | 45.60 | 40.93 |
Note.
p < .05;
p < .01;
p < .001
Latent profiles of adolescent assets and mental health symptoms
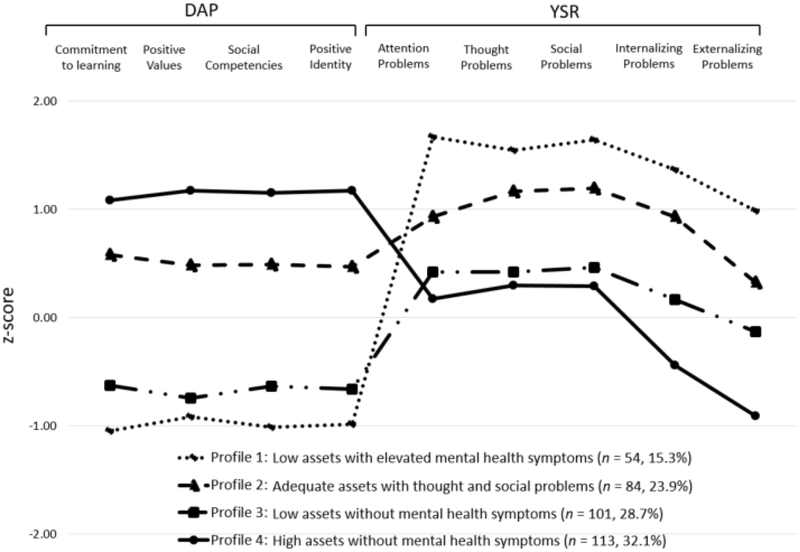
Table 2 summarizes model fit indices for each LPA model with different numbers of latent profiles. Although all likelihood information criterion (AIC, BIC, ABIC), along with the BLRT, indicated an improvement in model fit from the one-profile to the six-profile solution, the five and six-profile models included a profile with < 4% membership. Thus, the four-class solution was selected as the best fitting model. Figure 1 shows the levels of individual assets and MHS for each profile using estimated z-scores for a better comparison, with the mean raw scores of individual assets and T-scores of MHS presented in the last part of Table 1.
Table 2.
Model fit indices for latent profiles
| Class | Log likelihood | AIC | BIC | ABIC | Entropy | BLRT | Smallest class % |
|---|---|---|---|---|---|---|---|
| 1 | −10351.56 | 20739.12 | 20808.66 | 20751.56 | --- | --- | --- |
| 2 | −9949.16 | 19954.31 | 20062.50 | 19973.67 | .85 | < .001 | 47.7 |
| 3 | −9786.21 | 19648.41 | 19795.23 | 19674.68 | .84 | < .001 | 29.0 |
| 4 | −9691.61 | 19479.22 | 19664.68 | 19512.40 | .85 | < .001 | 15.3 |
| 5 | −9625.76 | 19367.53 | 19591.62 | 19407.62 | .88 | < .001 | 2.3 |
| 6 | −9571.51 | 19279.02 | 19541.74 | 19326.02 | .87 | < .001 | 3.7 |
Note. AIC=Akaike Information Criterion; BIC=Bayesian Information Criteria; ABIC=Sample-adjusted BIC; BLRT=Bootstrapped parametric likelihood ratio test
Figure 1.
Latent profiles of individual assets and mental health symptoms at age 12. z-scores for the DAP variables = Observed score – M / SD; z-scores for the YSR variables = (T scores – 50) / 10
The first profile (P1), comprising the smallest group (n=54, 15.3% of the sample), was named low assets with elevated MHS, as it was characterized by all indicators of individual assets below the mean (ranged from 15.63 in social competencies to 16.53 in commitment to learning) and all indicators of MHS, aside from externalizing problems, above the clinical cut-off, with externalizing problems on the clinical cut-off (T score 60). The second profile (P2), adequate assets with thought and social problems (n=84, 23.9%), exhibited individual assets above the mean (ranged from 22 in positive identity to 24 in commitment to learning) with elevated thought and social problem scores close to the clinical borderline (T score 65). The third profile (P3), low assets without MHS (n=101, 28.7%), had no MHS despite the similar lower levels of individual assets (from 17.01 in positive value to 18.49 in commitment to learning) with P1. The fourth profile (P4), high assets without MHS, accounting the biggest group (n=113, 32.1%), reported the highest levels of individual assets (> 25) and the lowest levels of MHS. All means of the nine indicators differed by the profile except the four indicators of indicators of individual assets between P1 and P3.
Characteristics by the latent profiles
Table 3 compares characteristics by the four identified profiles. Although no overall profile differences were found in socio-demographic, prenatal exposure to substances, placement (birth parents’ care, non-kinship care), and caregiver substance use characteristics, children in the high assets without MHS profile (P4) were less likely to have lower (< 80) IQ than children in the two MHS profiles (P1 and P2). Further, variables characterizing the interpersonal developmental contexts in which adolescents transact were found to have overall profile differences. Children in the high assets without MHS profile (P4) reported higher parental attachment than children in the two low assets profiles (P1 and P3), greater parental monitoring and fewer family conflicts than children in all other profiles, and lower violence exposure and child maltreatment than children in the two MHS profiles (P1 and P2). Children in the low assets with elevated MHS profile (P1) reported lower parental attachment than those in the adequate assets with thought and social problems profile (P2) and higher violence exposure and child maltreatment than those in the low assets without MHS profile (P3).
Table 3.
Characteristics by the latent profiles, M (SD)
| Profile 1: Low assets with elevated mental health symptoms (n = 54) |
Profile 2: Adequate assets with thought and social problems (n = 84) |
Profile 3: Low assets without mental health symptoms (n = 101) |
Profile 4: High assets without mental health symptoms (n = 113) |
p | Pair-wise difference | |
|---|---|---|---|---|---|---|
| Female, n (%) | 28 (51.9) | 41 (48.8) | 49 (48.5) | 70 (61.9) | .17 | |
| Receiving free lunch at school, n (%) | 38 (76.0) | 74 (90.2) | 74 (80.4) | 93 (86.9) | .09 | |
| Receiving Medicaid, n (%) | 35 (70.0) | 65 (79.3) | 76 (80.9) | 90 (84.1) | .23 | |
| Prenatal substance exposure, n (%) | ||||||
| Cocaine | 31 (57.4) | 40 (47.6) | 50 (49.5) | 56 (49.6) | .71 | |
| Alcohol | 42 (80.8) | 67 (82.7) | 70 (71.4) | 82 (75.2) | .29 | |
| Tobacco | 31 (59.6) | 50 (61.7) | 62 (63.3) | 74 (67.9) | .72 | |
| Marijuana | 15 (28.9) | 27 (33.3) | 30 (30.6) | 33 (30.3) | .95 | |
| African-American, n (%) | 43 (79.6) | 66 (78.6) | 80 (79.2) | 97 (85.8) | .57 | |
| Maternal education | 11.81 (1.82) | 11.49 (1.42) | 11.86 (1.56) | 11.74 (1.52) | .41 | |
| < High school, n (%) | 21 (38.9) | 39 (46.4) | 37 (36.6) | 50 (44.2) | .51 | |
| Maternal psychological distressa | 0.47 (0.30) | 0.44 (0.36) | 0.42 (0.33) | 0.47 (0.35) | .74 | |
| Full Scale IQ at age 11 | 83.54 (13.95) | 84.20 (12.25) | 86.38 (12.87) | 88.23 (12.52) | .07 | |
| < 80 IQ, n (%) | 23 (42.6) | 35 (41.6) | 33 (32.7) | 24 (21.2) | .007 | 4≠1, 2 |
| HOME Scoreb | 47.90 (6.92) | 47.95 (6.40) | 47.96 (6.94) | 49.74 (5.95) | .12 | |
| Parental attachmentb | 1.88 (0.71) | 2.22 (0.62) | 1.99 (0.64) | 2.45 (0.55) | < .001 | 4≠1, 2, 3; 2≠1, 3 |
| Monitoringb | 2.25 (0.60) | 2.43 (0.60) | 2.33 (0.69) | 2.69 (0.44) | < .001 | 4≠1, 2, 3 |
| Family conflictb | 3.91 (2.39) | 3.53 (2.47) | 2.89 (2.54) | 2.00 (2.16) | < .001 | 4≠1, 2, 3; 1≠3 |
| Violence exposureb | 1.03 (1.04) | 0.74 (0.79) | 0.48 (0.68) | 0.38 (0.56) | < .001 | 4≠1, 2; 3≠1, 2 |
| Child maltreatment, n (%)c | 18 (37.5) | 24 (30.8) | 18 (19.2) | 16 (14.8) | .004 | 4≠1, 2; 1≠3 |
| Caregiver substance use in the past 30 daysb,d | ||||||
| Alcohol | 12 (22.2) | 31 (36.9) | 27 (26.7) | 35 (31.0) | .26 | |
| Tobacco | 19 (35.2) | 40 (46.6) | 49 (43.4) | 39 (38.6) | .44 | |
| Marijuana | 1 (1.9) | 4 (4.8) | 4 (1.1) | 3 (2.7) | .76 | |
| Always in birth parents’ care by age 12, n (%) | 26 (52.0) | 47 (58.0) | 56 (58.9) | 74 (61.9) | .23 | |
| Non-kinship care at age 12, n (%) | 11 (22.0) | 12 (14.8) | 12 (12.6) | 9 (8.3) | .11 |
Note.
Assessed at birth,
12 years, and
17 years
All caregivers reported no use of cocaine in the past 30 days
Latent profiles and subsequent adolescent outcomes
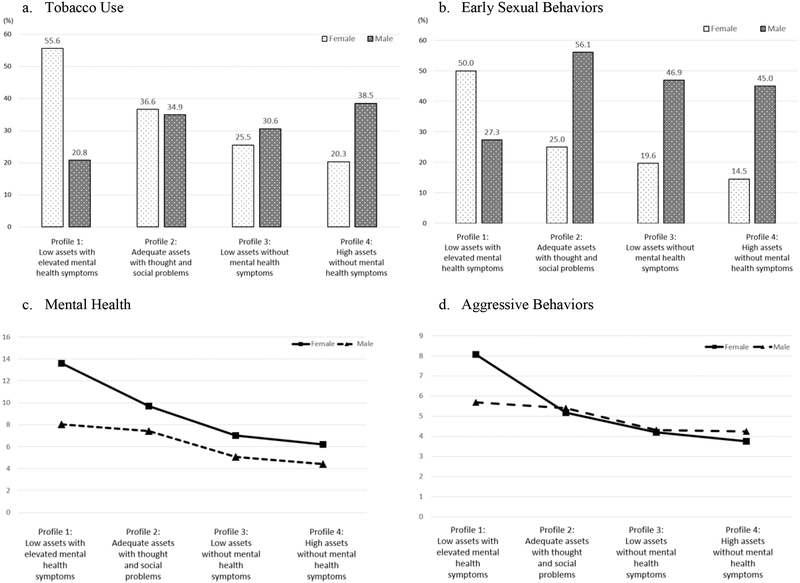
Figure 2 summarizes the results of logistic regression analysis and ANOVA examining latent profiles and gender as predictors of adolescent substance (tobacco, alcohol, marijuana) use, early sexual behaviors, mental health, and aggressive behaviors. Since the latent profiles were not related to adolescent alcohol or marijuana use, our findings are focused on other four adolescent outcomes. Profile by gender interactions (p < .05) were found in all four adolescent outcomes except mental health status (p = .064).
Figure 2.
Adolescent outcomes at age 15 by latent profiles and gender. For tobacco use (a), gender differences in Profile 1 & 4; Profile 1 differs from Profile 3 & 4 in girls, with no class difference in boys. For early sexual behaviors (b), gender differences in all profiles except Profile 1; Profile 1 differs from all other profiles in girls, and Profile 1 differs from Profile 2 in boys. For mental health (c), gender differece in Profile 1; Profile 1 differs from all other classes and Profile 2 differs from Profile 4 difference within each profile; Profile 1 differs from Profile 2, 3, & 4 in girls, with no profile difference in boys.
Tobacco use.
A greater number of girls in the low assets with elevated MHS profile (P1f; 55.6%) smoked tobacco than those in the two profiles with low MHS (P3f; 25.5% and P4f; 20.3%). No profile difference was noted in boys. Gender differences within profile were found in the low assets with elevated MHS profile (P1) and the high assets without MHS (P4), with more girls (55.6%) reporting tobacco use than boys (20.8%) in P1 (20.8%) whereas more boys (38.5%) reporting tobacco use than girls (20.3%) in P4.
Early sexual behaviors.
More girls in the low assets with elevated MHS profile (P1f; 50.0%) engaged in sexual intercourse before age 15 than those in the other three profiles, whereas more boys in the adequate assets with thought and social problems profile (P2m; 56.1%) engaged in early sexual intercourse than those in P1 (27.3%). More boys began to engage in sexual behaviors earlier than girls in all profiles except P1 (Figure 2b).
Mental health status.
Girls in the low assets with elevated MHS profile at age 12 (P1f; M=13.61, SE= 0.84) reported experiencing more emotional problems at age 15 than those in other three profiles; girls in the adequate assets with thought and social problems profile (P2f; M=9.71, SE= 0.70) reported higher emotional problems than those in the high assets without MHS (P4f; M=6.18, SE= 0.54). Boys in P4 (M=4.43, SE= 0.69) reported fewer emotional problems than those in P1 (M=8.04, SE= 0.89) and P2 (M=7.42, SE= 0.68). Although there was no overall gender by profile interaction (p = .064), girls in P1 (M=13.6 SE= 0.84) reported more emotional problems than boys in P1 (M=8.04, SE= 0.89).
Aggressive behaviors.
Girls in the low assets with elevated MHS profile (P1f; M=8.07, SE= 0.58) reported to have more aggressive behavior problems than girls in the other three profiles. Neither profile difference in boys nor gender difference within each profile were found (Figure 2d).
Discussion
The current study identified four distinctive profiles of individual assets and MHS in a sample of 12-years old children at risk for suboptimal development. About 39% of the children exhibited profiles with MHS. The four heterogeneous profiles are in line with previous studies, demonstrating distinct patterns of adolescents’ assets and MHS. For example, the low assets without MHS (P3) was similar to the “Average, social skills deficit” in Orpinas et al. (2015) and the “Vulnerable” in Rose et al. (2017). Additionally, the adequate assets with thought and social problems (P2) profile shared the similar tendency as Orpinas et al.’s “Internalizing” and Rose et al.’s “Symptomatic but content.” Both the high assets without MHS (P4) and the low assets with elevated MHS (P1) were also aligned with these previous studies (Orpinas et al., 2015; Rose et al., 2017). However, Orpinas and colleagues’ results had more elaborated classes than our study, such as “Externalizing,” “Disruptive behavior with school problems,” and “Severe problems,” which are similar to the low assets with elevated MHS (P1) in this study. The high assets without MHS (P4) was also similar to Rose and colleagues’ “Positive mental health,” although their indicators focused mainly on internalizing symptoms. Despite no overall demographic and prenatal substance exposure differences between profiles, children in P4 (the group with high assets and low MHS) were more likely to have a higher IQ and to be in a more optimal environment, characterized by higher parental attachment and monitoring and less family conflict, violence exposure, and child maltreatment, than those in other profiles.
Our study also indicates that profiles with MHS identified at age 12 were related to subsequent adolescent risk behaviors including tobacco use, early sexual risk behaviors, mental health, and aggressive behaviors at age 15, demonstrating the validity of the profiles. However, this relationship was more robust for girls than for boys, consistent with previous studies reporting poorer outcomes in adulthood in girls with MHS than in boys. For example, Odgers et al. (2008) found that childhood antisocial behaviors were associated with later mental and physical health problems in adulthood more strongly in females than males. Our findings suggest that girls reporting low assets with elevated MHS (P1) should be a primary concern for preventive intervention. Interventions focusing on the enhancement of family functioning and the family’s interface with key social systems such as peers and school (Henggeler, Clingempeel, Brondino, & Pickrel, 2002) and peer-to-peer mentoring (Van Dam et al., 2018) seem promising in reducing risk behaviors. Early interventions that improve neurocognitive functioning may be another avenue, given the relatively lower IQ noted in the two groups with MHS (P1 and P2).
In the present study, boys’ profiles at age 12 were not differentially associated with tobacco use and aggressive behaviors at age 15. These gender divergences may be elucidated by the different social norms and expectations for boys and girls. Boys may perceive tobacco use and aggressive behaviors as masculine and adult-like, and therefore socially desirable, especially in an urban, inner city setting with limited opportunities and outlook (Frankenhuis & Del Giudice, 2012; Ellis et al., 2012). sexual intercourse than boys in the adequate assets but thought and social problems (P2). This may be due to the “double standard” in which adolescent boys’ sexual behaviors are accepted and even rewarded, whereas adolescent girls’ such behaviors are degraded and stigmatized (Kreager & Staff, 2009). Additionally, lower internal assets may reflect the lack of interpersonal confidence and greater shyness (Edwards et al., 2007). Thus, boys in the low assets with elevated MHS (P1) may not have been perceived as attractive mates (Collibee & Furman, 2015; Feiring, Deblinger, Hoch-Espada, & Haworth, 2002), which needs to be replicated and validated by future studies.
More than half of the boys, but not girls, in the adequate assets with thought and social problems profile (P2) engaged in sexual intercourse before 15 years of age. Although additional research is needed to understand the factors that explain the course and prognosis of this profile (e.g., do they go on to develop sexually transmitted disease), it seems reasonable to recommend that these boys should also be a focus of preventive effort.
Limitations should be considered when interpreting the current study’s findings. First, our sample composition and screening criteria limit the generalizability of the findings to low income, urban, predominantly African-American adolescents with a history of prenatal substance exposure. Nonetheless, our study investigating at-risk urban, inner-city youth provides an important glimpse at the early combined patterns of MHS and individual assets, a key strength critical to the development of early intervention programs. Second, the current study relied on adolescents’ self-report, which might be subject to social desirability bias, as well as their ability to assess and reflect on their own strengths and behaviors. Utilizing multiple (e.g., teacher, peer) informants may increase validity. Third, the correlational nature of the data may limit the confidence in the influence of the age 12 profiles on adolescent outcomes at age 15. Latent transition analyses, assessing changes from one latent subgroup to another over time (Lanza, Flaherty, & Collins, 2003), may clarify the impact of preadolescence profile on subsequent adolescnet outcomes. Fourth, the relatively small sample size for multiple group analysis also precluded from the investigation of possible gender variations in the patterns of classification. Lastly, the lack of positive adolescent outcomes (e.g., leadership, competence) at age 15 in this study might limit us from distinguishing and understanding the two profiles without MHS (P3 and P4). Nevertheless, the present study has a number of methodological strengths including its longitudinal prospective design, use of well-validated, widely-used standardized measures, and use of the integrated person-centered approach examining both assets and MHS simultaneously to better characterize the complexity of adolescent development.
In conclusion, this study demonstrates the heterogeneity of individual patterns of adaptation and maladaptation in at-risk, inner-city American adolescents. Different subgroups of youth identified in this study may benefit from different intervention strategies. Girls with low assets and elevated MHS fared poorly in adolescence, raising particular concern for their later adjustment. Continued studies into adulthood will uncover whether the unique combination of individual assets and MHS identified in early adolescence may affect psychosocial and vocational adjustment differently in this high risk population.
Acknowledgements
Portions of this paper were presented at the 80th Annual Meeting of College on Problems of Drug Dependence (CPDD) in San Diego, CA, in June 2018. The authors would like to thank all of our families who participated in our research for 17 years. We would also like to thank Adelaide Lang, PhD, Laurie Ellison, LISW, and Paul Weishampel, MA for research assistance. This research was supported by National Institute on Drug Abuse Grants R01–07957 and R01–042747.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM (1991). Manual for the youth self-report and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry. [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Arbeit MR, Johnson SK, Champine RB, Greenman KN, Lerner JV, & Lerner RM (2014). Profiles of problematic behaviors across adolescence: Covariations with indicators of positive youth development. Journal of Youth and Adolescence, 43(6), 971–990. 10.1007/s10964-014-0092-0. [DOI] [PubMed] [Google Scholar]
- Becker JB, McClellan M, & Reed BG (2016). Sociocultural context for sex differences in addiction. Addiction Biology, 21(5), 1052–1059. 10.1111/adb.12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson PL, & Scales PC (2011). Developmental assets. Encyclopedia of adolescence, 667–683. [Google Scholar]
- Burt KB, & Roisman GI (2010). Competence and psychopathology: Cascade effects in the NICHD study of early child care and youth development. Development and Psychopathology, 22(3), 557–567. doi: 10.1017/S0954579410000271. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, & Bradley RH (2003). HOME Inventory: Administration manual. Little Rock, AR: University of Arkansas for Medical Sciences. [Google Scholar]
- Centers for Disease Control and Prevention (2009). YRBSS: Youth risk behavior surveillance system. Retrieved from http://www.cdc.gov/HealthyYouth/yrbs/index.htm.
- Cicchetti D (2013). An overview of developmental psychopathology In Zelazo PD (Eds.), The Oxford Handbook of Developmental Psychology Vol. 2. Self and Other (pp. 455–480). New York, NY, US: Oxford University Press. [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70(1), 6–20. 10.1037/0022-006X.70.1.6. [DOI] [PubMed] [Google Scholar]
- Collibee C, & Furman W (2015). Quality counts: Developmental shifts in associations between romantic relationship qualities and psychosocial adjustment. Child Development, 86(5), 1639–1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2010). Latent class and latent transition analysis: With applications in the social behavioral, and health sciences. Hoboken, N. J: Wiley. [Google Scholar]
- Derogatis LR (1992). BSI: Administration, scoring, and procedures manual II. Towson, MD: Clinical Psychometric Research. [Google Scholar]
- Dir AL, Coskunpinar A, & Cyders MA (2014). A meta-analytic review of the relationship between adolescent risky sexual behavior and impulsivity across gender, age, andrace. Clinical Psychology Review, 34(7), 551–562. 10.1016/j.cpr.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Dittus PJ, Michael SL, Becasen JS, Gloppen KM, McCarthy K, & Guilamo-Ramos V (2015). Parental monitoring and its associations with adolescent sexual risk behavior: A meta-analysis. Pediatrics, 136(6), e1587–e1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BJ, Del Giudice M, Dishion TJ, Figueredo AJ, Gray P, Griskevicius V, … & Wilson DS (2012). The evolutionary basis of risky adolescent behavior: implications for science, policy, and practice. Developmental Psychology, 48(3), 598–623. 10.1037/a0026220. [DOI] [PubMed] [Google Scholar]
- Else-Quest NM, Hyde JS, Goldsmith HH, & Van Hulle CA (2006). Gender differences in temperament: a meta-analysis. Psychological Bulletin, 132(1), 33–72. http://doi:10.1037/0033-2909.132.1.33. [DOI] [PubMed] [Google Scholar]
- Feiring C, Deblinger E, Hoch-Espada A, & Haworth T (2002). Romantic relationship aggression and attitudes in high school students: The role of gender, grade, and attachment and emotional styles. Journal of Youth and Adolescence, 31(5), 73–385. [Google Scholar]
- Finkelhor D, Hamby SL, Ormrod R, & Turner H (2005). The juvenile victimization questionnaire: Reliability, validity, and national norms. Child Abuse & Neglect, 29(4), 383–412. 10.1016/j.chiabu.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Fosco GM, Stormshak EA, Dishion TJ, & Winter CE (2012). Family relationships and parental monitoring during middle school as predictors of early adolescent problem behavior. Journal of Clinical Child & Adolescent Psychology, 41(2), 202–213. 10.1080/15374416.2012.651989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankenhuis WE, & Del Giudice M (2012). When do adaptive developmental mechanisms yield maladaptive outcomes? Developmental Psychology, 48(3), 628–642. http://doi:10.1037/a0025629. [DOI] [PubMed] [Google Scholar]
- Hall GS (1904). Adolescence: Its psychology and itsi relations to physiology, anthropology, sociology, sex, crime, religion and education. New York: D. Appleton and Company. [Google Scholar]
- Hamby SL, Finkelhor D, Ormrod RK, & Turner HA (2004). The juvenile victimization questionnaire (JVQ): Administration and scoring manual. Durham, NH: Crimes Against Children Research Center. [Google Scholar]
- Harden KP, Kretsch N, Mann FD, Herzhoff K, Tackett JL, Steinberg L, & Tucker-Drob EM (2017). Beyond dual systems: A genetically-informed, latent factor model of behavioral and self-report measures related to adolescent risk-taking. Developmental Cognitive Neuroscience, 25, 221–234. 10.1016/j.dcn.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Clingempeel WG, Brondino MJ, & Pickrel SG (2002). Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child & AdolescentPsychiatry, 41(7), 868–874. [DOI] [PubMed] [Google Scholar]
- Hughes D, Toro JD, Harding JF, Way N, & Rarick JRD (2016). Trajectories of discrimination across adolescence: Associations with academic, psychological, and behavioral outcomes. Child Development, 87(5), 1337–1351. 10.1111/cdev.12591. [DOI] [PubMed] [Google Scholar]
- Jelicic H, Bobek DL, Phelps E, Lerner RM, & Lerner JV (2007). Using positive youth development to predict contribution and risk behaviors in early adolescence: Findings from the first two waves of the 4-H Study of Positive Youth Development. International Journal of Behavioral Development, 31(3), 263–273. 10.1177/0165025407076439. [DOI] [Google Scholar]
- Jung T, & Wickrama KAS (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1751-9004.2007.00054.x [Google Scholar]
- Kobulsky JM, Minnes S, Min MO, & Singer MI (2016). Violence exposure and early substance use in high-risk adolescents. Journal of Social Work Practice in the Addictions, 16(1–2), 46–71. 10.1080/1533256x.2016.1138867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokko K, Tremblay RE, Lacourse E, Nagin DS, & Vitaro F (2006). Trajectories of prosocial behavior and physical aggression in middle childhood: Links to adolescent school dropout and physical violence. Journal of Research on Adolescence, 16(3), 403–428. 10.1111/j.1532-7795.2006.00500.x [DOI] [Google Scholar]
- Kreager DA, & Staff J (2009). The sexual double standard and adolescent peer acceptance. Social Psychology Quarterly, 72(2), 143–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagasse LL, Conradt E, Karalunas SL, Dansereau LM, Butner JE, Shankaran S, … & Lester BM (2016). Transactional relations between caregiving stress, executive functioning, and problem behavior from early childhood to early adolescence. Development and Psychopathology, 28(3), 743–756. 10.1017/S0954579416000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Flaherty BP, & Collins LM (2003). Latent class and latent transition analysis In Schinka JA & Velicer WF(Eds.), Handbook of psychology: Research methods in psychology, Vol. 2 (pp. 663–685). Hoboken, NJ, US: John Wiley & Sons Inc; 10.1002/0471264385.wei0226. [DOI] [Google Scholar]
- Lerner RM (1998). Theories of human development: Contemporary perspectives In Damon W, & Lerner RM (Eds.). Handbook of child psychology: Vol. 1. Theoretical model of human development (pp. 1–24). (5th ed.). New York: Wiley. [Google Scholar]
- Lerner JV, Bowers EP, Minor K, Boyd MJ, Mueller MK, Schmid KL, … Lerner RM (2013). Positive youth development: Processes, philosophies, and programs In Lerner RM, Easterbrooks MA, Mistry, & Weiner IB (Eds.), Handbook of psychology: Developmental psychology (pp. 365–392). Hoboken, NJ, US: John Wiley & Sons Inc. [Google Scholar]
- Lewin-Bizan S, Bower EP, & Lerner RM (2010). One good thing leads to another: Cascades of positive youth development among American adolescents. Development and Psychopathology, 22(4), 759–770. 10.1017/S0954579410000441 [DOI] [PubMed] [Google Scholar]
- Li Y, & Lerner RM (2011). Trajectories of school engagement during adolescence: implications for grades, depression, delinquency, and substance use. Developmental psychology, 47(1), 233. [DOI] [PubMed] [Google Scholar]
- Linares TJ, Singer LT, Kirchner L, Short EJ, Min MO, Hussey P, & Minnes S (2005). Mental health outcomes of cocaine-exposed children at 6 years of age. Journal of Pediatric Psychology, 31(1), 85–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson D (2003). The person approach: Concepts, measurement models, and research strategy. New directions for child and adolescent development, 2003(101), 3–23. [DOI] [PubMed] [Google Scholar]
- Masten AS, & Curtis WJ (2000). Integrating competence and psychopathology: Pathways toward a comprehensive science of adaptation in development. Development and Psychopathology, 12(3), 529–550. [DOI] [PubMed] [Google Scholar]
- Miller P, & Sperry LL (1987). The socialization of anger and aggression. Merrill-Palmer Quarterly (1982-), 1–31. [Google Scholar]
- Min MO, Minnes S, Lang A, Albert JM, Kim JY, & Singer LT (2016). Pathways to adolescent sexual risk behaviors: Effects of prenatal cocaine exposure. Drug and Alcohol Dependence, 161(1), 284–291. 10.1016/j.drugalcdep.2016.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Lang A, Weishampel P, Short EJ, Yoon S, & Singer LT (2014a). Externalizing behavior and substance use related problems at 15 years in prenatally cocaine exposed adolescents. Journal of Adolescence, 37(3), 269–279. 10.1016/j.adolescence.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Lang A, Yoon S, & Singer LT (2015). Effects of prenatal cocaine exposure on early sexual behavior: Gender difference in externalizing behavior as a mediator. Drug and Alcohol Dependence, 153(1), 59–65. 10.1016/j.drugalcdep.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Kim JY, Yoon M, & Singer LT (2018a). Individual assets and problem behaviors in at-risk adolescents: A longitudinal cross-lagged analysis. Journal of Adolescence. 64, 52–61. 10.1016/j.adolescence.2018.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Park H, Ridenour T, Kim JY, Yoon M, & Singer LT (2018b). Developmental trajectories of externalizing behavior from ages 4 to 12: Prenatal cocaine exposure and adolescent correlates. Drug and Alcohol Dependence, 192(1), 223–232. 10.1016/j.drugalcdep.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Yoon S, Short EJ, Singer LT (2014b). Self-reported adolescent behavioral adjustment: Effects of prenatal cocaine exposure. Journal of Adolescent Health, 55(2), 167–174. 10.1016/j.jadohealth.2013.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Singer LT, Minnes S, Kim H, & Short E (2013). Mediating links between maternal childhood trauma and preadolescent behavioral adjustment. Journal of Interpersonal Violence, 28(4), 831–851. 10.1177/0886260512455868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Singer LT, Kirchner HL, Short E, Lewis B, Satayathum S, & Queh D (2010). The effects of prenatal cocaine exposure on problem behavior in children 4–10 years. Neurotoxicology and Teratology, 32(4), 443–451. 10.1016/j.ntt.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Singer L, Min MO, Wu M, Lang A, & Yoon S (2014). Effects of prenatal cocaine/polydrug exposure on substance use by age 15. Drug and Alcohol Dependence, 134(1), 201–210. 10.1016/j.drugalcdep.2013.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray KW, Dwyer KM, Rubin KH, Knighton-Wisor S, & Booth-LaForce C (2014). Parent-child relationships, parental psychological control, and aggression: Maternal and paternal relationships. Journal of Youth and Adolescence, 43(8), 1361–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling, 14(4), 535–569. [Google Scholar]
- Odgers CL, Moffitt TE, Broadbent JM, Dickson N, Hancox RJ, Harrington H, … & Caspi A (2008). Female and male antisocial trajectories: From childhood origins to adult outcomes. Development and Psychopathology, 20(2), 673–716. [DOI] [PubMed] [Google Scholar]
- Orpinas P, Raczynski K, Peters JW, Colman L, & Bandalos D (2015). Latent profile analysis of sixth graders based on teacher ratings: Association with school dropout. School Psychology Quarterly, 30(4), 577–592. 10.1037/spq0000107. [DOI] [PubMed] [Google Scholar]
- Pinquart M (2017). Associations of parenting dimensions and styles with externalizing problems of children and adolescents: An updated meta-analysis. Developmental Psychology, 53(5), 873–932. 10.1037/dev0000295. [DOI] [PubMed] [Google Scholar]
- Phelps E, Balsano AB, Fay K, Peltz JS, Zimmerman SM, Lerner RM, & Lerner JV (2007). Nuances in early adolescent developmental trajectories of positive and problematic/risk behaviors: Findings from the 4-H study of positive youthdevelopment. Child and Adolescent Psychiatric Clinics of North America, 16(2), 473–496. 10.1016/j.chc.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Rahdert E (1991). The Adolescent Assessment and Referral Manual (DHHS Publication ADM-91–1735). Rockville, MD: National Institute on Drug Abuse. [Google Scholar]
- Ridenour TA, Clark DB, & Cottler LB (2009). The illustration-based Assessment of Liability and Exposure to Substance use and Antisocial behavior© for children. The American Journal of Drug and Alcohol Abuse, 35(4), 242–252. 10.1080/00952990902998715. [DOI] [PubMed] [Google Scholar]
- Rose T, Lindsey MA, Xiao Y, Finigan-Carr NM, & Joe S (2017). Mental health and educational experiences among black youth: A latent class analysis. Journal of Youth and Adolescence, 46(11), 2321–2340. 10.1007/s10964-017-0723-3. [DOI] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, & Abramson LY (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822. 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scales PC (2011). Youth developmental assets in global perspective: Results from international adaptions of the developmental assets profile. Child Indicators Research, 4, 619–645. [Google Scholar]
- Scales PC, & Leffert N (2004). Developmental assets: A synthesis of the scientific research on adolescent development (2nd ed.). Minneapolis, MN: Search Iinstitute. [Google Scholar]
- Schmid KL, Phelps E, & Lerner RM (2011). Constructing positive futures: Modeling the relationship between adolescents’ hopeful future expectations and intentional self regulation in predicting positive youth development. Journal of adolescence, 34(6), 1127–1135. [DOI] [PubMed] [Google Scholar]
- Schwartz SJ, Pantin H, Coatsworth JD, & Szapocznik J (2007). Addressing the challenges and opportunities for today’s youth: Toward an integrative model and its implications for research and intervention. Journal of Primary Prevention, 28(2), 117–144. 10.1007/s10935-007-0084-x. [DOI] [PubMed] [Google Scholar]
- Schwartz SJ, Phelps E, Lerner JV, Huang S, Brown CH, Lewin-Bizan S, … Lerner RM (2010). Promotion as prevention: Positive youth development as protective against tobacco, alcohol, illicit drug, and sex initiation. Applied Developmental Science, 14(4), 197–211. 10.1080/10888691.2010.516186. [DOI] [Google Scholar]
- Search Institute (2005). Developmental assets profile: User manual. Minneapolis, MN: Search Institute. [Google Scholar]
- Singer L, Arendt R, Farkas K, Minnes S, Huang J, & Yamashita T (1997). Relationship of prenatal cocaine exposure and maternal postpartum psychological distress to child developmental outcome. Development and Psychopathology, 9(3), 473–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Minnes S, Short E, Arendt R, Farkas K, Lewis B, … Kirchner HL (2004). Cognitive outcomes of preschool children with prenatal cocaine exposure. JAMA, 291(20), 2448–2456. 10.1001/jama.291.20.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Nelson S, Short E, Min MO, Lewis B, Russ S, & Minnes S (2008). Prenatal cocaine exposure: Drug and environmental effects at 9 years. The Journal of Pediatrics, 153(1), 105–111. 10.1016/j.jpeds.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørlie MA, Hagen KA, & Ogden T (2008). Social competence and antisocial behavior: Continuity and distinctiveness across early adolescence. Journal of Research on Adolescence, 18(1), 121–144. doi: 10.1111/j.1532-7795.2008.00553.x. [DOI] [Google Scholar]
- Tein J-Y, Coxe S, & Cham H (2013). Statistical Power to Detect the Correct Number of Classes in Latent Profile Analysis. Structural Equation Modeling: A Multidisciplinary Journal, 20(4), 640–657. 10.1080/10705511.2013.824781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dam L, Smit D, Wildschut B, Branje SJT, Rhodes JE, Assink M, & Stams GJJ (2018). Does Natural Mentoring Matter? A Multilevel Metaffanalysis on the Association Between Natural Mentoring and Youth Outcomes. American journal of community psychology, 62(1–2), 203–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren MT, Wray-Lake L, Rote WM, & Shubert J (2016). Thriving while engaging in risk? Examining trajectories of adaptive functioning, delinqueny, and substance use in a nationally representative sample of U.S. adolescents. Developmental Psychology, 52(2), 296–310. 10.1037/a0039922. [DOI] [PubMed] [Google Scholar]
- Wechsler D (2003). Wechsler intelligence scale for children (4th ed.). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Zimmer-Gembeck MJ, & Helfand M (2008). Ten years of longitudinal research on US adolescent sexual behavior: Developmental correlates of sexual intercourse, and the importance of age, gender and ethnic background. Developmental Review, 28(2), 153–224. 10.1016/j.dr.2007.06.001. [DOI] [Google Scholar]