Abstract
Background
The long time from exposure to potentially harmful chemicals until breast cancer occurrence poses challenges for designing etiologic studies and for implementing successful prevention programs. Growing evidence from animal and human studies indicates that distinct time periods of heightened susceptibility to endocrine disruptors exist throughout the life course. The influence of environmental chemicals on breast cancer risk may be greater during several windows of susceptibility (WOS) in a woman’s life, including prenatal development, puberty, pregnancy, and the menopausal transition. These time windows are considered as specific periods of susceptibility for breast cancer because significant structural and functional changes occur in the mammary gland, as well as alterations in the mammary micro-environment and hormone signaling that may influence risk. Breast cancer research focused on these breast cancer WOS will accelerate understanding of disease etiology and prevention.
Main text
Despite the plausible heightened mechanistic influences of environmental chemicals on breast cancer risk during time periods of change in the mammary gland’s structure and function, most human studies of environmental chemicals are not focused on specific WOS. This article reviews studies conducted over the past few decades that have specifically addressed the effect of environmental chemicals and metals on breast cancer risk during at least one of these WOS. In addition to summarizing the broader evidence-base specific to WOS, we include discussion of the NIH-funded Breast Cancer and the Environment Research Program (BCERP) which included population-based and basic science research focused on specific WOS to evaluate associations between breast cancer risk and particular classes of endocrine-disrupting chemicals—including polycyclic aromatic hydrocarbons, perfluorinated compounds, polybrominated diphenyl ethers, and phenols—and metals. We outline ways in which ongoing transdisciplinary BCERP projects incorporate animal research and human epidemiologic studies in close partnership with community organizations and communication scientists to identify research priorities and effectively translate evidence-based findings to the public and policy makers.
Conclusions
An integrative model of breast cancer research is needed to determine the impact and mechanisms of action of endocrine disruptors at different WOS. By focusing on environmental chemical exposure during specific WOS, scientists and their community partners may identify when prevention efforts are likely to be most effective.
Keywords: Breast neoplasms, Puberty, Pregnancy, Menopause, Environment
Background
Despite the considerable personal and societal burden from breast cancer, primary prevention efforts encounter challenges. Unlike other cancers that are linked to a predominant risk factor (e.g., smoking and lung cancer [1], human papillomavirus, and cervical cancer [2]), most established breast cancer risk factors have modest associations; moreover, many risk factors are not conducive to population-level intervention. The American Cancer Society guidelines for breast cancer prevention include limiting alcohol intake, avoiding post-menopausal hormone use, increasing physical activity, and maintaining a healthy body weight [3]. Yet even considering these factors, estimates indicate that a substantial proportion of breast cancer risk remains unexplained [4, 5].
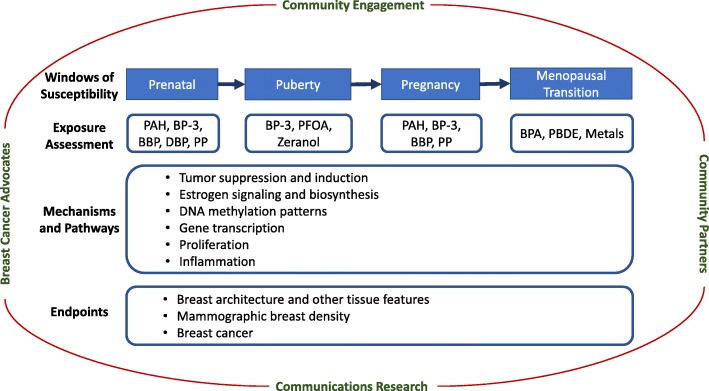
Migrant studies, atomic bomb survivor studies, and experimental model studies reinforce the concept that exposures during certain periods in a woman’s life are important to later breast cancer risk [6–9]. These time intervals represent windows of susceptibility (WOS) and coincide with landmark events when a woman’s breast tissue changes in structure and function including the prenatal, pubertal, pregnancy, and menopausal WOS. Epidemiologic data support that both medications [10] and medical conditions [11, 12] during these WOS may affect breast cancer risk; more limited evidence addresses specific environmental chemicals and metals during these same WOS. In 2003, the National Institute for Environmental Health Sciences (NIEHS) initiated the Breast Cancer and the Environment Research Program (BCERP) with support from the National Cancer Institute (NCI) to specifically examine whether environmental exposures during the pubertal WOS affect the timing of puberty, a risk factor for breast cancer. Since 2009, BCERP expanded the WOS to include the prenatal, pregnancy, and menopausal transition WOS. In addition, studies of mammographic breast density (MBD), breast tissue measurements, and other intermediate biomarkers of the effects of environmental exposures were included. The BCERP consortium unites basic and population scientists in advancing our understanding of the role of environmental chemicals during WOS in breast cancer risk. Scientific research in BCERP also builds from community partnerships and collaborations with communication scientists within the consortium to facilitate direct translation to the public (Fig. 1).
Fig. 1.
BCERP framework. A model of transdisciplinary community-engaged research by epidemiologists, basic scientists, communication researchers, and advocates to examine environmental causes of breast cancer, as conducted by the Breast Cancer and the Environment Research Program (BCERP)
Numerous previous studies examined environmental chemical exposure and breast cancer risk; however, most research in humans has not specifically focused on measuring environmental chemical exposures during WOS (for review, see [13, 14]). For example, of the 146 epidemiologic reports published in 2006–2016 on environmental chemicals and incident breast cancer, only 16 (11%) report on exposures measured during a specific WOS [14]. In this review, we outline the scientific evidence generated by experimental and epidemiologic scientists including (but not limited to) those in BCERP addressing the link between breast cancer risk and environmental chemicals and metals within four WOS—prenatal, puberty, pregnancy, and the menopausal transition—to inform breast cancer etiology and future interventions.
Windows of susceptibility (WOS)
Breast cancer etiology appears to be driven in part by perturbations to breast tissue as well as alterations of the mammary gland micro-environment during critical windows. Here we briefly summarize breast tissue changes occurring during each WOS, review evidence that addresses environmental carcinogenesis during each WOS, and outline the motivation for ongoing research on the chemicals and metals targeted in BCERP.
Prenatal WOS
The prenatal period is a particularly vulnerable WOS because breast tissue begins to develop in the embryonic stage when epidermal cells in concert with embryonic mesenchyme become breast buds [15–18]. Faster fetal growth and greater birth-weight increase breast cancer risk later in life [19–21]. Proposed mechanisms by which chemicals can alter normal mammary development trajectories [15, 18, 19, 22, 23] include changes in maternal hormone levels regulating development and sex differentiation, high levels of growth factors, potential DNA damage and mutations in germ cells, and other genetic or epigenetic processes [24].
Pregnancy and birth cohorts reveal possible associations between environmental chemicals during the prenatal period and breast cancer. The Child Health and Development Studies (CHDS) found high levels of maternal exposure to dichlorodiphenyltrichloroethane (DDT) during pregnancy increased the daughters’ later breast cancer risk to age 52 nearly fourfold compared to daughters of women with low levels of exposure (Table 1) [25]. Although production of many of the organochlorine chemicals—including dioxins, polychlorinated biphenyls (PCBs), and pesticides such as DDT—stopped in the 1970s, there is continued exposure to these complex mixtures with diverse biological activity. Animal fats and fish from contaminated waters are on-going sources of human exposure as a result of bioaccumulation [26]; PCB exposure also persists through inhalation both outdoors and of indoor air and dust from caulk, building materials, and floor finishes [27]. Organochlorines are hormonally active and may contribute to breast cancer by altering mammary gland development or hormone responsiveness early in life, or by promoting tumor growth [25]. Epidemiologic studies of DDT exposure measured outside of a WOS and breast cancer risk were less likely to report consistent findings [14, 19].
Table 1.
Epidemiologic studies investigating environmental exposures during three windows of susceptibility in relation to an intermediate marker of breast cancer risk or breast cancer
| First author (Year) | Exposure | Outcome | Population | Sample size | Risk estimate | 95% CI | Notes |
|---|---|---|---|---|---|---|---|
| Exposure during prenatal window | |||||||
| Bonner (2005) [33] | Regional total suspended particulates | Breast cancer | Women 35–79, New York | 1166 cases and 2105 controls | OR 2.42 | 0.97–6.09 | > 140 vs < 84 μg/m3 TSP, postmenopausal women |
| OR 1.78 | 0.62–5.10 | > 140 vs < 84 μg/m3 TSP, premenopausal women | |||||
| Bocskay (2005) [32] | Personal airborne PAH; PAH DNA adducts | Chromosomal aberrations from cord blood | Newborns in Northern Manhattan; Bronx | 60 (32 female, 28 male) | Data not shown for PAH adducts | “No strong association” | |
|
Airborne PAH β = 0.14 |
p = 0.006 | Linear regression line slope | |||||
| Cohn (2015) [25] | Maternal o,p’-DDT | Daughter breast cancer | Mothers and adult daughters in Alameda County, CA | 118 cases and 354 controls | OR 3.7 | 1.5–9.0 | Fourth vs first quartile (> 0.78 vs < 0.27 ng/mL) |
| Exposure during puberty window | |||||||
| Tsai (2015) [82] | Serum PFOA | log-transformed SHBG | Taiwanese girls aged 12–17 | 65 | 2.96 (SE 0.34) vs 3.50 (SE 0.24) | p < 0.05 | Mean PFOA levels 90th vs 50th percentile (> 9.80 vs < 3.63 ng/mL) |
| Data not shown | p > 0.05 | FSH and testosterone | |||||
| Wolff (2015) [57] | Urinary phenols | Age at breast development | US girls aged 6–8 followed for 7 years | 1239 girls |
Enterolactone: HR 0.79 Benzophenone-3: HR 0.80 Triclosan: HR 1.17 2,5-dichlophenol: HR 1.37 |
0.64–0.98 0.65–0.98 0.96–1.43 1.09–1.72 |
5th vs 1st quintiles of biomarkers |
| Wolff (2014) [58] | Low and high molecular weight phthalate (MWP) metabolites from urine | Age of breast and pubic hair development | US girls aged 6–8 followed for 7 years | 1239 girls |
Pubic hair development age: HR 0.91 Breast development age: HR 0.99 |
0.84–0.99 0.91–1.08 |
5th vs 1st quintiles of high MWP metabolites. Results null for low MWP metabolites. |
| Wolff (2010) [59] | Low and high molecular weight phthalate (MWP) metabolites from urine | Stage of breast and pubic hair development | US girls aged 6–8 followed for 1 year | 1151 girls |
Pubic hair development: PR 0.94 Breast development: PR 1.03 |
0.88–1.00 0.97–1.10 |
5th vs 1st quintiles of high MWP metabolites. Results attenuated for low MWP metabolites (p = 0.08). |
| Windham (2015) [60] | PBDE, PCB, OCP | Tanner stage 2+ vs 1 (breast development) | US girls aged 6–8 followed for 7 years | 645 girls |
PBDE: TR 1.05 PCB: TR 1.05 OCP: TR 1.10 |
1.02–1.08 1.01–1.08 1.06–1.14 |
4th vs 1st quartile. Results similar for pubic hair development. |
| Cohn (2007, 2019) [67, 68] | p,p’-DDT metabolites in serum taken after giving birth (initial DDT exposure likely before age 14 years) | Breast cancer before age 50 | Women in Child Health and Development Studies cohort | 129 cases and 129 matched controls | OR 5.4 | 1.7–17.1 | Highest vs lowest tertile (> 13.90 vs < 8.09 μg/L) |
| Breast cancer diagnosis during ages 50–54 | 153 cases and 432 matched controls | OR 1.88 | 1.37–2.59 | One-unit change in log2 (p,p’-DDT), approximately equal to a 2-fold increase | |||
| Exposure during pregnancy | |||||||
| Nie (2007) [115] | Regional total suspended particulates at time of first birth | Post-menopausal breast cancer | Women 35–79 in Erie and Niagara Counties | 220 cases and 301 controls | OR 2.57 | 1.16–5.69 | Highest vs lowest quartile |
| Bonefeld-Jorgensen (2014) [83] | 16 serum PFAS during pregnancy including 10 PFCA, 5 PFSA, and PFOSA | Breast cancer | Danish National Birth Cohort | 250 cases and 233 controls |
PFOSA: RR 1.04 PFHxS: RR 0.66 |
0.99–1.08 0.47–0.94 |
Continuous per ng/ml. All other PFAS were null. |
| Cohn (2012) [110] | Serum PCB during early postpartum | Breast cancer before age 50 | Women in Child Health and Development Studies cohort | 112 cases with matched controls |
PCB 167: OR 0.24 PCB 187: OR 0.35 PCB 203: OR 6.34 |
0.07–0.79 0.11–1.14 1.85–21.7 |
Highest vs lowest quartile (> 0.30 vs < 0.08 mmol/l) (> 0.66 vs < 0.38 mmol/l) (> 0.42 vs < 0.34 mmol/l) |
Abbreviations: AA African American, BMI body mass index, FSH follicle-stimulating hormone, HR hazard ratio, IRR incidence rate ratio, NHANES National Health and Nutrition Examination Survey, OR odds ratio, PAH polycyclic aromatic hydrocarbons, PFAS perfluoroalkylated substances, PFHxS perfluorohexanesulfonate, PFOA perfluorooctanoic acid, PFOSA perflurooctane-sulfonamide, PR prevalence ratio, RR relative risk, SHBG sex hormone-binding globulin, TR time ratio of median ages across quantile groups
Another class of chemical exposures of concern during the prenatal WOS is polycyclic aromatic hydrocarbons (PAH). PAH are produced as a result of combustion of hydrocarbons. Some of the common sources of PAH exposure include consuming grilled meats and certain other food items [28], inhaling cigarette smoke and motor vehicle exhaust [29], and exposure to industrial processes [29–31]. PAH are widespread and enter the body largely through ingestion and inhalation of suspended particulate matter [32, 33]. The International Agency for Research on Cancer classifies PAH as probable carcinogens; the US Environmental Protection Agency lists PAH as possible carcinogens [34, 35].
Like DDT and other organochlorines, PAH are lipophilic and stored in fat tissue including breast tissue [36]. Most PAH compounds are weakly estrogenic and may induce cell proliferation via activation of the estrogen receptor (ER) [37]. Exposure to PAH was linked to mammary cancer in rodents [38]. PAH exposure has been measured directly in both blood [39] and breast tissue [40], and higher levels of PAH-DNA adducts have been found in breast cancer cases compared with women without breast cancer [41]. Similarly, breast cancer cases reported higher levels of PAH exposures than controls based on questionnaire assessments of indirect exposure [42–46]. For all these epidemiologic studies, specific WOS were not investigated. Because experimental and epidemiologic associations implicate prenatal PAH exposure in multiple adverse health effects including obesity [47–49], one focus of BCERP is the impact of PAH exposure during the prenatal WOS. BCERP research specifically addresses how exposure to PAH during the prenatal and pregnancy WOS may increase the development of mammary tumors in mice. Concurrent human studies within BCERP evaluate how prenatal PAH exposure alters breast tissue development and tissue composition in adolescent girls.
Pubertal window of susceptibility
The female breast undergoes rapid changes and growth during puberty. The highest density of proliferating terminal end buds that mediate ductal elongation and establishment of the ductal tree and primitive lobular structures form during puberty [50, 51]. This time period is considered highly estrogen sensitive based on evidence in mice where pubertal growth is almost completely stunted in mice lacking ERα [52, 53]. The profound hormonal changes, including a dramatic increase in endogenous estrogen biosynthesis by stimulating hormones from the hypothalamus and pituitary gland, culminate in the onset of menarche. Endocrine-disrupting chemicals (EDC) in the environment may affect the interaction of endogenous estrogens and progestogens with their receptors and together have carcinogenic impact. Exposure to EDC may reprogram normal stem cells which are subsequently transformed by additional estrogen exposures [54]. The number of mammary stem cells expands during this period of proliferation, and these cells distribute throughout the ductal tree [55]. Three previous BCERP puberty cohorts examined exposure to several environmental chemicals in relation to pubertal timing as endpoints and reported that higher levels of some (but not all) chemicals, including various phenols (including bisphenol A [BPA]), parabens, phthalates, and persistent organohalogenated compounds, were associated with delayed median puberty endpoints by 5–11 months when comparing extreme categories of exposure (Table 1) [56–60].
Epidemiologic and experimental evidence from investigators outside of BCERP suggest environmental exposures during the pubertal WOS are associated with an increase in breast cancer risk. Human studies have examined high doses of radiation from medical treatment or atomic bomb exposure [61, 62] and nutritional exposures during puberty and adolescence [63–66]. DDT exposure during infancy and puberty was associated with increased breast cancer risk [67, 68]. In experimental studies of rats, exposure to a carcinogen (dimethylbenz [a] anthracene, DMBA) resulted in the highest number of tumors when administered to rodents during “puberty” possibly through induction of proinflammatory responses [50, 51, 69–74]. Excessive signaling through the ER appears to be another primary mechanism for mammary carcinogenesis as modest overexpression of ERα in response to endogenous estrogen during puberty in transgenic mice resulted in mammary hyperplasia and tumors [75, 76].
BCERP members are studying the effect of pubertal levels of perfluorooctanoic acid (PFOA) and per- and polyfluoralkyl substances (PFAS) on breast development and breast density. PFAS are used in many commercial products because of their non-stick, stain-resistant, and waterproof characteristics. Sources of human exposure include production facilities, firefighting training, consumer products, diet, and drinking water. Dietary sources include seafood [77] and food packaging [78]. PFAS enhance the estrogenic effects of 17β-estradiol in T47D human breast cancer cells [79] and promote the proliferation, migration and invasion potential of human breast epithelial cells [80]. Animal studies provide evidence that PFOA affects the developing mammary gland [81], although limited human epidemiologic data have been less conclusive when PFOA and PFAS exposure was examined in relation to intermediate breast cancer markers (hormone levels) [82] or measured during adulthood [83]. Because environmental chemicals may influence the timing and duration of the pubertal trajectory, studies including breast tissue biomarkers that can be reliably measured to provide greater information than a single event in time, such as age at menarche, are critical to move the field forward.
Pregnancy window of susceptibility
Pregnancy is another period of rapid breast tissue and micro-environmental changes during which susceptibility to environmental exposures may increase the risk of breast cancer [8]. During pregnancy, breast tissue changes rapidly in size and function to prepare for lactation. Estrogen, progesterone, and prolactin are the major drivers of branching and development of the lobuloalveolar structures’ characteristic of the mature breast [84]. Pregnancy also decreases the number of mammary stem cells [85, 86]. However, the protective pathways activated during pregnancy can be eroded by prolonged exposure to exogenous 17β-estradiol which restores sensitivity to carcinogen-induced mammary tumors [87–89]. These observations may explain why pregnancy is accompanied by a short-term increase in breast cancer risk [12, 90]; “pregnancy-associated breast cancer” has poorer overall survival [91, 92]. However, in the long term after a pregnancy, breast cells are less sensitive to carcinogenesis with the lifetime risk of breast cancer reduced by up to 50% [93–96]. Thus, the mechanisms mediating the competition between tumor-promoting and tumor-suppressive effects of estrogens in the breast provide fundamental insights into mechanisms underlying risk and resistance in the presence of environmental chemicals.
In mice, there is a greater than 100-fold increase in the number of mammary epithelial cells during pregnancy demonstrating the rapid changes that occur in mammary tissue. Despite the rapid proliferation, a full-term pregnancy renders the mammary epithelium resistant to tumorigenesis subsequent to the pregnancy. This is observed in studies of exposure to carcinogens [70, 97–99] as well as inherited genetic risk alleles [100–103]. Administering exogenous estrogen, either alone or in combination with progesterone to rodents at an early age, sufficiently mimics the effect of pregnancy in reducing tumors in rodents [104–106]. Lobuloalveolar structures may be less susceptible to carcinogens [107, 108], in part, through more robust p53-dependent responses to DNA damage [109].
Epidemiologic evidence directly linking environmental exposures during pregnancy and breast cancer risk arises from the previously mentioned prospective CHDS which measured PCB and DDT soon after pregnancy and confirmed breast cancer diagnoses with medical records. Relative risk estimates for breast cancer comparing upper to lower quartiles of 16 individual PCB congeners ranged from 0.2 to 6.3; a composite score of exposure was associated with an odds ratio of 2.8 (95% CI 1.1–7.1) (Table 1) [110]. Other epidemiologic studies suggest no association between breast cancer and organochlorine pesticide residues in blood collected near the time of diagnosis [111, 112], but these measurements may not be representative of exposure to the parent chemical during the relevant WOS [113].
The BCERP consortium is studying the effects of exposure during pregnancy on maternal breast cancer risk by examining breast tissue changes in the mothers of daughters participating in studies at the Columbia’s Children Center for Environmental Health [32, 114]. The design of this mother-daughter cohort, similar to CHDS, facilitates efficient examination of exposure to PAH during two WOS (pregnancy and prenatal) in the two generations [115]. As a complement to this epidemiologic study, other BCERP members aim to elucidate the mechanisms for the dual effect of pregnancy on breast cancer risk by examining chemicals that are found in higher levels among pregnant women [116, 117] and their potential to impair the protective pathways associated with breast development during pregnancy. These pathways include the activity of p53 [109] and limiting the stem cell populations [118].
Menopausal transition window of susceptibility
Although menopause is often defined as the cessation of menstrual periods for at least 1 year, the menopausal transition begins a number of years prior to menopause. During the menopausal transition, micro-environment changes occur in the breast tissue along with declining systemic levels of endogenous estrogen and progesterone [119]. As the majority of breast cancers are responsive to these two sex steroid hormones, their decline explains the leveling-off of the age-specific rate curve of breast cancer after menopause [120]. Later age at menopause is associated with a higher risk of developing breast cancer due to a longer period of exposure to higher levels of sex steroid hormones [121]. Despite the leveling in the age-specific rate curve of breast cancer, the vast majority of breast cancers are diagnosed after menopause, in part through enhanced hormone receptor sensitivity during the menopausal transition. Mammary tissue may be more responsive to lower levels of estrogen and progesterone, as well as to hormone mimics, by adapting to the abrupt reduced production of ovarian hormones [122, 123].
Analyses of data from the Women’s Health Initiative (WHI) showed that the increased incidence of breast cancer with use of exogenous estrogen and progesterone [124–127] was mediated through the change in mammographic breast density that occurred in the first year of use [128]. A biologically based breast tumor growth rate model [129] suggests that hormone therapy promotes growth of pre-existing occult lesions and minimally initiated de novo tumors. EDCs with estrogen-like and/or progesterone-like activities or those modifying aromatase expression/activity including polybrominated diphenyl ethers (PBDE), BPA, or selected metals may act in a similar manner and promote the growth of occult disease to clinically detectable tumors during the menopausal transition.
PBDE are a class of over 200 organohalogenated compounds widely used as flame retardants and may modulate steroidogenesis including expression of aromatase [130–136]. BPA is an industrial chemical found in polycarbonate plastics, epoxy resins, dental sealants, and thermal paper [137, 138]. Both PBDE [136] and BPA [139] have been shown to act as ligands of ERα. While experimental studies suggest that PBDE and BPA cause breast cancer and biomonitoring studies confirm that women are exposed, epidemiologic studies have not to-date measured exposure during relevant WOS, used methods that reflect long-term exposure, or included measures of mammographic density or other intermediate markers of breast cancer risk [138, 140, 141].
Metalloestrogens are metals that activate the ER, leading to estrogen-like changes. Metalloestrogens are prevalent environmental contaminants with multiple routes of human exposure. They often accumulate in tissues and organs (reviewed in [142, 143]). Most breast cancer studies have focused on cadmium which induces the proliferation of estrogen-dependent breast cancer cells [144–147], increases the transcription and expression of estrogen-regulated genes such as the PR [144, 148], activates ERα in transfection assays [144–146, 149, 150], and increases signaling through the ERK1/2 and Akt pathways [148, 151, 152]. The reported associations between metalloestrogen exposures and breast cancer risk to date have been inconsistent in part due to the variety of techniques used to assess exposure. Studies of dietary cadmium measured from self-reported dietary assessments and breast cancer risk have on the most part found minimal if any associations due in part to the difficulty in determining exposure [153–159]. The studies of neighborhood airborne levels did not distinguish differences between breast cancer cases and controls [160, 161]. The studies measuring individual cadmium levels from blood, urine, or toenails are not necessarily measuring the same timing of exposure. Most [153–155, 159, 162, 163], but not all [158, 164], epidemiologic studies of postmenopausal women or all ages combined show risk estimates in the 0.73 to 1.01 range (Table 2). Two studies show greater risk associated with cadmium exposure for premenopausal women than for postmenopausal women [156, 165], whereas two other studies show the reverse [157, 166], with additional studies describing generally null associations for both groups [160, 161, 167, 168]. Stratification by estrogen receptor status does not reveal a consistent pattern. Studies of cadmium and mammographic breast density as an intermediate marker of breast cancer risk also have mixed findings possibly due to differences in assessment of cadmium or breast density in terms of methods and in timing relative to WOS [168–171]. Exposure to cadmium or other metalloestrogens during any of the WOS may impact a woman’s risk of breast cancer by activation of the hormone receptors; however, no studies as of yet have carefully examined whether metalloestrogens may have the greatest impact during the menopausal transition when endogenous hormone levels are declining.
Table 2.
Epidemiologic studies investigating cadmium exposure in relation to breast cancer risk according to the menopause window of susceptibility (WOS)
| First author (year) | Exposure | Population | Sample size | Risk estimate | 95% CI | Notes |
|---|---|---|---|---|---|---|
| Cadmium exposure stratified by menopausal status | ||||||
| McElroy (2006) [165] | Urinary cadmium | Women aged 20–69 years | 246 cases and 254 controls |
All ages OR 2.29 20–56 years OR 2.34 57–69 years OR 1.36 |
1.3–4.2 1.1–5.0 0.5–3.4 |
Highest (≥ 0.58) vs lowest (< 0.263 μg/g) quartile |
| Gallagher (2010) [166] | Urinary cadmium | Long Island (LI), NY and NHANES women aged ≥ 30 years |
LI 100 cases and 98 controls NHANES 99 cases and 3120 non-cases |
All ages OR 2.81 n.s. difference by age All ages OR 2.32 30–54 years OR n.s. ≥ 55 years OR 7.25 |
1.11–7.13 0.92–5.84 n.s. 1.04–50.7 |
Highest (≥ 0.60) vs lowest (< 0.22 μg/g creatinine) quartile |
| Itoh (2014) [157] | Dietary cadmium | Japanese women aged 20–74 years | 212 cases and 253 controls |
All cases OR 1.04 Premeno. OR 1.01 Postmeno. OR 1.06 Post. ER+ OR 1.08 Post. ER− OR 0.99 |
1.00–1.08 0.96–1.07 1.06–1.11 1.03–1.14 0.92–1.06 |
Continuous cadmium intake (μg/day) |
| Amadou (2019) [160] | Long-term airborne exposure to cadmium | E3N French cohort aged 40–65 years | 4059 cases and 4059 controls |
Overall OR 0.98 Premeno OR 0.72 Postmeno. OR 1.06 ER+ OR 1.00 ER− OR 0.63 |
0.84–1.14 0.45–1.15 0.89–1.27 0.82–1.22 0.41–0.95 |
Highest (> 5.47) vs lowest (≤ 0.033 mg/m2) quintile |
| Grioni (2019) [156] | Dietary cadmium | Italian cohort aged 34–70 years | 8924 total in cohort with 481 cases |
Overall HR 1.54 Premeno HR 1.73 Postmeno HR 1.29 ER+ HR 1.64 ER− HR 1.30 |
1.06–2.22 1.10–2.71 0.68–2.44 1.06–2.54 0.60–2.83 |
Highest (≥ 8.82) vs lowest (< 6.73 μg/day) quintile |
| O’Brien (2019) [167] | Cadmium from toenail clippings | Sister and two-sister studies aged < 50 years | 1217 sister-pairs of cases and controls | OR 1.15 | 0.82–1.60 | Highest (> 0.011) vs lowest (< 0.003 μg/g) quartile |
|
White (2019) [161] |
Residential census tract airborne exposure to cadmium at baseline | Sister study aged 35–74 years | 50,884 total in cohort with 2587 cases |
Overall HR 1.1 Premeno 1.0 Postmeno 1.1 |
0.96– 1.3 0.78– 1.4 0.96– 1.3 |
Highest vs lowest quintile |
| Postmenopausal women only | ||||||
| Julin (2012) [158] | Dietary cadmium | Swedish postmenopausal women | 55,987 total in cohort with 2112 cases |
All cases RR 1.21 ER+ cases RR 1.19 ER− cases RR 1.33 |
1.07–1.36 1.03–1.36 0.95–1.87 |
Highest (> 16) vs lowest (< 13 μg/day) tertile |
| Adams (2012) [153] | Dietary cadmium | Postmenopausal women in VITamines And Lifestyle cohort | 30,543 total in cohort with 899 cases |
HR 1.00 n.s. difference by ER status (p = 0.11) |
0.72–1.41 | Highest (> 13.3) vs lowest (< 7.48 μg/day) quartile |
| Eriksen (2014) [155] | Dietary cadmium | Danish postmenopausal women | 23,815 total in cohort with 1390 breast cancer cases |
All cases IRR 0.99 ER+ IRR 1.00 ER− IRR 0.88 |
0.87–1.13 0.85–1.15 0.62–1.22 |
Per 10 μg/day increase in intake |
| Adams (2014) [154] | Dietary cadmium | Postmenopausal women aged 50–79 years | 155,069 total in cohort with 6658 cases |
HR 0.90 n.s. difference by ER status |
0.81–1.00 | Highest (> 14.21) vs lowest (< 7.10 μg/day) quintile |
| Adams (2016) [162] | Urinary cadmium | Postmenopausal women ages ≥ 50 years in Women’s Health Initiative | 12,701 total in cohort with 508 cases and 1050 controls |
All HR 0.80 ER+ HR 0.98 ER−/PR- HR 0.88 |
0.56–1.14 0.87–1.07 0.70–1.11 |
Highest (> 0.748) vs lowest (< 0.325 μg/g creatinine) quartile |
| All ages | ||||||
| Sawada (2012) [159] | Dietary cadmium | Japanese women aged 45–74 years | 48,351 females total in cohort with 402 breast cancer cases | HR 0.87 | 0.61–1.23 | Highest (median 32.3) vs lowest (median 19.2 μg/day) tertile |
| Nagata (2013) [164] | Urinary cadmium | Japanese women ages ≥ 25 years | 153 cases from one hospital and 431 controls invited for breast cancer screening | OR 6.05 | 2.90–12.62 | Highest (> 2.620) vs lowest (< 1.674 μg/g creatinine) tertile |
| Gaudet (2018) [163] | Blood cadmium | Cancer Prevention Study II women 47–85 years of age | 816 cases and 816 controls |
All RR 1.01 ER+ RR 0.89 ER− RR 0.96 |
0.76–1.34 0.62–1.27 0.44–2.09 |
Continuous per μg/L |
| Italian women aged 35–70 years | 292 cases and 294 controls | RR 0.80 | 0.61–1.03 | Continuous per μg/L | ||
| Swedish women aged 30–61 years | 325 cases and 325 controls | RR 0.73 | 0.54–0.97 | Continuous per μg/L | ||
| Combined 3 nested case-cohort studies | 1433 cases and 1435 controls | RR 0.84 | 0.69–1.01 | Continuous per μg/L | ||
Abbreviations: BCSC Breast Cancer Surveillance Consortium, CI confidence interval, EPA Environmental Protection Agency, ER estrogen receptor, HR hazard ratio, IRR incidence rate ratio, NHANES National Health and Nutrition Examination Survey, n.s. not statistically significant, OR odds ratio, RR relative risk
BCERP members are examining whether exposure to PBDEs, BPA, or selected metals during the menopausal transition is associated with breast cancer risk in humans, and evaluating potential mechanisms to explain these associations in rodent models.
Strategies to address long latency
The long time between exposures during the early WOS (prenatal, puberty, pregnancy) and breast cancer occurrence has multiple implications for breast cancer research. First, because many environmental exposures are stored long-term in adipose tissue, even compounds now banned, such as DDT and PBDE, may continue to be relevant for breast cancer risk. Bioaccumulation of lipophilic chemicals and their long-term storage also means studies incorporating biomarkers in breast tissue need to consider both the effects on adipose tissue as well as epithelial and stromal tissues.
Second, because it may be decades after the relevant windows of exposure before breast cancer is diagnosed, the examination and validation of intermediate biomarkers of response, apparent closer to the timing of exposure and before diagnosis, are imperative, particularly in prospective human studies. BCERP first started as a cohort study of the environmental exposures that may accelerate puberty. The main outcome of the cohort study was based on Tanner Stages [172]. As BCERP expanded to include other WOS, additional measures of breast tissue composition and breast density were added. BCERP investigators are now using a variety of intermediate markers—as both outcomes in relation to chemical exposures and as predictors of breast and mammary cancers—conducted in parallel human and rodent studies including epigenetic biomarkers, altered tumor suppression and induction, and altered estrogen signaling and biosynthesis (Fig. 1) [173].
One intermediate outcome is mammographic breast density (MBD), defined as the fraction of connective and glandular tissue to adipose tissue on a mammogram [174–181]. MBD is one of the strongest predictors of breast cancer risk with a four- to sixfold elevation in risk comparing ≥ 75% MBD to < 5% [182], but the mechanisms explaining how environmental chemicals affect the overall level and rate of change of MBD are uncertain. While MBD declines with age in many women, particularly around the time of menopause [183–185], this pattern does not occur uniformly for all women [8, 186, 187].
Little is known of the drivers of breast tissue changes across adolescence, early adulthood, and the menopausal transition and thus the contributors to breast density. Most of what is known about normal breast tissue characteristics is from mammography data in women over 40 years of age. In women under 40 years, two alternative imaging methods have been used to assess breast composition including three studies of magnetic resonance imaging (MRI) in women aged 15–30 years [188–190] and two of dual X-ray absorptiometry (DXA) in girls aged 10–16 years [191, 192]. In addition, optical spectroscopy (OS) provides a compositional view of the breast capturing variation in the amount of water, lipid, hemoglobin, and collagen, as well as overall cellular and connective tissue density [174–176]. Collagen density may promote epithelial cell proliferation and increase tumor mobility and invasion, while hemoglobin is associated with angiogenesis [193–195]. OS has been used to measure differences in adolescent breast tissue across developmental stages as assessed by Tanner stage [196]. Thus, MRI, DXA, and OS provide novel intermediate outcomes to measure breast tissue changes across the developmental trajectory of adolescence and early adulthood and may be important tools for examining environmental effects during these life stages. Mammography techniques now include digital breast tomosynthesis measures as well as the use of ultrasound in measuring breast density without radiation exposure [181]. While density of the adult breast is highly correlated with breast cancer risk, longitudinal measures of pubertal density are currently lacking but are being collected in BCERP.
Conclusions
Given the changes in mammary tissue architecture and hormone signaling during the prenatal, pubertal, pregnancy, and menopausal transition windows, these critical time periods may reflect windows of heightened risk. Thus, measuring the impact of environmental chemical and metal exposures during these WOS is essential to understand their roles in breast cancer risk; these issues have not been addressed by the majority of epidemiologic studies to date.
Experimental studies in cell lines and animals are providing causative mechanistic links between environmental exposures and altered mammary carcinogenesis, particularly during key WOS. Increasingly, epidemiologic studies are able to link the human exposure of chemicals and metals during relevant WOS through the use of intermediate breast outcomes including specific breast tissue characteristics and breast density in adolescence and adulthood to address the challenge of long latency time posed in cancer research.
For many of the studies described here, community engagement strengthens the research design as well as the dissemination and implementation of study findings. To address knowledge gaps and accelerate translation of environmental breast cancer research findings related to WOS, BCERP integrates basic and population researchers with communication scientists and representatives of community-based organizations (Fig. 1). Community partnerships are vital, because both the sources and the remedies for environmental exposures are outside of clinical settings. Community input also can identify issues of concern to the community, motivate participation in studies, and translate findings to public audiences. Scientists need to disseminate research findings to the public to enable people to make informed choices in their personal lives and workplaces, and to influence health policies as voters and community leaders. For example, participation of community partners in BCERP has led to the development of strategies to provide reports of personal chemical exposures to individuals who donated biological samples, so they can learn about environmental health and make informed decisions regarding possible behavioral modification in general and with particular reference to WOS [197, 198]. Digital methods using libraries of vetted exposure and health information and decision rules, set by the study team, make personalized results practical [199]. In addition, communication scientists within BCERP are testing different messages and channels for future outreach efforts [200]. Scholarship about community-engaged research shows that this approach improves the “rigor, relevance, and reach” of research [201].
Although the median age when women are diagnosed with breast cancer is 62 years [202], primary prevention of potentially hazardous environmental exposures during earlier WOS is critical [13], particularly when considering that exposure to environmental chemicals may contribute to cancer health disparities [203–206]. Furthermore, just as family-based studies facilitated the discovery of breast cancer genes relevant to all women, studies during specific WOS will facilitate the assessment of the effects from environmental exposures that will be relevant outside of these WOS. As evidence from WOS accumulates, the paradigm for breast cancer needs to expand beyond the secondary prevention efforts of screening and mid-life risk assessment to primary prevention efforts with involvement of community partners, educators and school districts, families, and primary care providers including pediatricians for lifelong impact [207].
Acknowledgements
The authors would like to thank Natalia Arroyo, Julie McGregor, and Eileen McGuine for their assistance with this manuscript. The funders had no role in the design of the study, the writing of the manuscript, or the decision to submit the manuscript for publication.
The Breast Cancer and the Environment Research Program includes Mary Pat Berry, Jennifer Bird, Christopher Bradfield, Ronald Gangnon, Michael Gould, John Hampton, Sara Lindberg, Sarah Luongo, Kristen Malecki, Betsy Rolland, and James Shull (University of Wisconsin-Madison); Mia Gaudet (American Cancer Society); Mark Thornquist (Fred Hutchinson Cancer Research Center); Mark D. Aupperlee, Sandra Z. Haslam, Reyhane Hoshyar, Anastasia Kariagina, Juliana R. Lopes, Karen J. Miller, Olena Morozova, Cathy J. Newkirk, Richard C. Schwartz, Brandon Thomas, Daniel Totzkay, and Fang Xie (Michigan State University); Kami J. Silk (University of Delaware); Frank M. Biro (Cincinnati Children’s Hospital); Cecily S. Fassler, Courtney M. Giannini, and Susan Pinney (University of Cincinnati); Melissa A. Troester (University of North Carolina Chapel Hill); Kimberly Burke, Julie Herbstman, Rebecca Kehm, Jasmine McDonald, Rachel Miller, Sabine Oskar, Frederica Perera, Debeshish Sahay, Parisa Tehranifar, Mary Beth Terry, Desiree Walker, and Nur Zeinomar (Columbia University); Milagros de Hoz and Peggy Shepard (WeACT); Julia Knight (Lunenfeld-Tanenbaum Research Institute); Lothar Lilge (University Health Network); Alexandra Binder, Karin Michels (University of California Los Angeles); Vincent Bessonneau, Julia Brody, Vanessa De La Rosa, Jennifer Ohayon, and Ruthann Rudel (Silent Spring Institute); Camila Corvalan, Ana Pereira, and Rosario Toro-Campos (University of Chile); Julia Pereira, Jose Russo, and Su Yanrong (Fox Chase Cancer Center); John Shepherd (University of Hawaii Cancer Center); Lucile Adams-Campbell, Chiranjeev Dash, Bassem Haddad, Rhonda Hamilton, Mary Beth Martin, and Brenda Richardson (Georgetown University); Celia Byrne and Hristina Denic-Roberts (Uniformed Services University of the Health Sciences); Gregory Chang, Shiuan Chen, Yuan Chun Ding, Noriko Kanaya, Susan Neuhausen, Michele Rakoff, Kohei Saeki, and Mayra Serrano (City of Hope); Peggy Reynolds (University of California San Francisco); Karen Dunphy, Joseph Jerry, Anna Symington, and Laura Vandenberg (University of Massachusetts Amherst); Sallie Schneider (Baystate Medical Center); Swann Arp Adams, Heather M. Brandt, Daniela Friedman, and Jamie R. Lead (University of South Carolina); Xiaomei Cai, Gary Kreps, Camella J. Rising, and Kevin B. Wright (George Mason University); Amelia Burke-Garcia (University of Chicago); Dasha Afanaseva (Westat); and Carla L. Fisher and Michaela Devyn Mullis (University of Florida).
Disclosure
Celia Byrne: the views expressed are those of the author(s) and do not necessarily reflect the official views of the Uniformed Services University of the Health Sciences or the Department of Defense.
Abbreviations
- BCERP
Breast Cancer and the Environment Research Program
- BPA
Bisphenol A
- CHDS
Child Health and Development Study
- DDT
Dichlorodiphenyltrichloroethane
- DMBA
Dimethylbenz [a]anthracene
- DNA
Deoxyribonucleic acid
- DXA
Dual X-ray absorptiometry
- EDC
Endocrine-disrupting chemical
- ER
Estrogen receptor
- MBD
Mammographic breast density
- MRI
Magnetic resonance imaging
- NCI
National Cancer Institute
- NIEHS
National Institute of Environmental Health Sciences
- OR
-
Odds ratio OS
optical spectroscopy
- PAH
Polycyclic aromatic hydrocarbons
- PBDE
Polybrominated diphenyl ethers
- PCB
Polychlorinated biphenyl
- PFAS
Per- and poly-fluoroalkyl substances
- PFOA
Perfluorooctanoic acid
- RR
Relative risk
- WHI
Women’s Health Initiative
Authors’ contributions
All authors performed parts of the literature review and wrote drafts of the manuscript. MBT, KBM, and ATD conceptualized the paper and provided overall supervision and coordination of the manuscript preparation. ATD generated the table and figures, which were revised by all authors. All authors were involved in writing the manuscript and approved the final manuscript.
Funding
This work was completed as part of the Breast Cancer and the Environment Research Program (BCERP), supported by the National Institute of Environmental Health Sciences and the National Cancer Institute at the National Institutes of Health (grant numbers U01 ES026119, U01 ES026122, U01 ES026127, U01 ES026130, U01 ES026132, U01 ES026137, U01 ES026140, R03 ES027406, R21 ES027417, and R21 ES027418).
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mary Beth Terry and Karin B. Michels should be considered shared first authors.
Contributor Information
Mary Beth Terry, Email: mt146@columbia.edu.
Karin B. Michels, Email: k.michels@ucla.edu
Julia Green Brody, Email: brody@silentspring.org.
Celia Byrne, Email: celia.byrne@usuhs.edu.
Shiuan Chen, Email: schen@coh.org.
D. Joseph Jerry, Email: jjerry@vasci.umass.edu.
Kristen M. C. Malecki, Email: kmalecki@wisc.edu
Mary Beth Martin, Email: martinmb@georgetown.edu.
Rachel L. Miller, Email: rlm14@cumc.columbia.edu
Susan L. Neuhausen, Email: sneuhausen@coh.org
Kami Silk, Email: kamisilk@udel.edu.
Amy Trentham-Dietz, Email: trentham@wisc.edu.
on behalf of Breast Cancer and the Environment Research Program (BCERP):
Jasmine McDonald, Sabine Oskar, Julia Knight, Rosario Toro-Campos, Xiaomei Cai, Camella J. Rising, Dasha Afanaseva, Michaela Devyn Mullis, Mary Pat Berry, Jennifer Bird, Christopher Bradfield, Ronald Gangnon, Michael Gould, John Hampton, Sara Lindberg, Sarah Luongo, Kristen Malecki, Betsy Rolland, James Shull, Mia Gaudet, Mark Thornquist, Mark D. Aupperlee, Sandra Z. Haslam, Reyhane Hoshyar, Anastasia Kariagina, Juliana R. Lopes, Karen J. Miller, Olena Morozova, Cathy J. Newkirk, Richard C. Schwartz, Brandon Thomas, Daniel Totzkay, Fang Xie, Kami J. Silk, Frank M. Biro, Cecily S. Fassler, Courtney M. Giannini, Susan Pinney, Melissa A. Troester, Kimberly Burke, Julie Herbstman, Rebecca Kehm, Logthar Lilge, Rachel Miller, Frederica Perera, Debeshish Sahay, Parisa Tehranifar, Mary Beth Terry, Desiree Walker, Nur Zeinomar, Milagros de Hoz, Peggy Shepard, Alexandra Binder, Karin Michels, Vincent Bessonneau, Julia Brody, Vanessa De La Rosa, Jennifer Ohayon, Ruthann Rudel, Camila Corvalan, Ana Pereira, Julia Pereira, Jose Russo, Su Yanrong, John Shepherd, Lucile Adams-Campbell, Chiranjeev Dash, Bassem Haddad, Rhonda Hamilton, Mary Beth Martin, Brenda Richardson, Celia Byrne, Hristina Denic-Roberts, Gregory Chang, Shiuan Chen, Yuan Chun Ding, Noriko Kanaya, Susan Neuhausen, Michele Rakoff, Kohei Saeki, Mayra Serrano, Peggy Reynolds, Karen Dunphy, Joseph Jerry, Anna Symington, Laura Vandenberg, Sallie Schneider, Swann Arp Adams, Heather M. Brandt, Daniela Friedman, Jamie R. Lead, Gary Kreps, Kevin Wright, Amelia Burke-Garcia, and Carla Fisher
References
- 1.Lee PN, Forey BA, Coombs KJ. Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer. BMC Cancer. 2012;12:385. doi: 10.1186/1471-2407-12-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Munoz N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 3.Breast Cancer Risk and Prevention. Available at https://www.cancer.org/cancer/breast-cancer/risk-and-prevention.html. Accessed 3 July 2019.
- 4.Colditz GA, Bohlke K. Priorities for the primary prevention of breast cancer. CA Cancer J Clin. 2014;64(3):186–194. doi: 10.3322/caac.21225. [DOI] [PubMed] [Google Scholar]
- 5.Sprague BL, Trentham-Dietz A, Egan KM, Titus-Ernstoff L, Hampton JM, Newcomb PA. Proportion of invasive breast cancer attributable to risk factors modifiable after menopause. Am J Epidemiol. 2008;168(4):404–411. doi: 10.1093/aje/kwn143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.IOM (Institute of Medicine) Breast cancer and the environment: a life course approach. Washington, D.C.: National Academies Press; 2012. [Google Scholar]
- 7.Korenman SG. The endocrinology of breast cancer. Cancer. 1980;46(4 Suppl):874–878. doi: 10.1002/1097-0142(19800815)46:4+<874::AID-CNCR2820461305>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 8.Pike MC, Krailo MD, Henderson BE, Casagrande JT. Hoel DG: ‘Hormonal’ risk factors, 'breast tissue age' and the age-incidence of breast cancer. Nature. 1983;303(5920):767–770. doi: 10.1038/303767a0. [DOI] [PubMed] [Google Scholar]
- 9.Russo J, Russo IH. Toward a physiological approach to breast cancer prevention. Cancer Epidemiol Biomark Prev. 1994;3(4):353–364. [PubMed] [Google Scholar]
- 10.Hilakivi-Clarke L. Maternal exposure to diethylstilbestrol during pregnancy and increased breast cancer risk in daughters. Breast Cancer Res. 2014;16(2):208. doi: 10.1186/bcr3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nechuta S, Paneth N, Velie EM. Pregnancy characteristics and maternal breast cancer risk: a review of the epidemiologic literature. Cancer Causes Control. 2010;21(7):967–989. doi: 10.1007/s10552-010-9524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nichols Hazel B., Schoemaker Minouk J., Cai Jianwen, Xu Jiawei, Wright Lauren B., Brook Mark N., Jones Michael E., Adami Hans-Olov, Baglietto Laura, Bertrand Kimberly A., Blot William J., Boutron-Ruault Marie-Christine, Dorronsoro Miren, Dossus Laure, Eliassen A. Heather, Giles Graham G., Gram Inger T., Hankinson Susan E., Hoffman-Bolton Judy, Kaaks Rudolf, Key Timothy J., Kitahara Cari M., Larsson Susanna C., Linet Martha, Merritt Melissa A., Milne Roger L., Pala Valeria, Palmer Julie R., Peeters Petra H., Riboli Elio, Sund Malin, Tamimi Rulla M., Tjønneland Anne, Trichopoulou Antonia, Ursin Giske, Vatten Lars, Visvanathan Kala, Weiderpass Elisabete, Wolk Alicja, Zheng Wei, Weinberg Clarice R., Swerdlow Anthony J., Sandler Dale P. Breast Cancer Risk After Recent Childbirth. Annals of Internal Medicine. 2018;170(1):22. doi: 10.7326/M18-1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Interagency Breast Cancer and the Environment Research Coordinating Committee. In. Breast cancer and the environment: prioritizing prevention. Bethesda, MD: National Institutes of Health; February 2013. (http://www.niehs.nih.gov/about/assets/docs/ibcercc_full_508.pdf). (Accessed 1 Dec 2014).
- 14.Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: an updated review of epidemiological literature informed by biological mechanisms. Environ Res. 2018;160:152–182. doi: 10.1016/j.envres.2017.08.045. [DOI] [PubMed] [Google Scholar]
- 15.Fenton SE, Reed C, Newbold RR. Perinatal environmental exposures affect mammary development, function, and cancer risk in adulthood. Annu Rev Pharmacol Toxicol. 2012;52:455–479. doi: 10.1146/annurev-pharmtox-010611-134659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russo J, Lynch H, Russo IH. Mammary gland architecture as a determining factor in the susceptibility of the human breast to cancer. Breast J. 2001;7(5):278–291. doi: 10.1046/j.1524-4741.2001.21033.x. [DOI] [PubMed] [Google Scholar]
- 17.Russo J, Russo IH. Development of the human breast. Maturitas. 2004;49(1):2–15. doi: 10.1016/j.maturitas.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt CW. IOM issues report on breast cancer and the environment. Environ Health Perspect. 2012;120(2):a60–a61. doi: 10.1289/ehp.120-a60a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brody JG, Rudel RA, Michels KB, Moysich KB, Bernstein L, Attfield KR, Gray S. Environmental pollutants, diet, physical activity, body size, and breast cancer: where do we stand in research to identify opportunities for prevention? Cancer. 2007;109(12 Suppl):2627–2634. doi: 10.1002/cncr.22656. [DOI] [PubMed] [Google Scholar]
- 20.Michels KB, Xue F, Terry KL, Willett WC. Longitudinal study of birthweight and the incidence of breast cancer in adulthood. Carcinogenesis. 2006;27(12):2464–2468. doi: 10.1093/carcin/bgl105. [DOI] [PubMed] [Google Scholar]
- 21.Warner ET, Hu R, Collins LC, Beck AH, Schnitt S, Rosner B, Eliassen AH, Michels KB, Willett WC, Tamimi RM. Height and body size in childhood, adolescence, and young adulthood and breast cancer risk according to molecular subtype in the Nurses’ Health Studies. Cancer Prev Res (Phila) 2016;9(9):732–738. doi: 10.1158/1940-6207.CAPR-16-0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michels KB, Mohllajee AP, Roset-Bahmanyar E, Beehler GP, Moysich KB. Diet and breast cancer: a review of the prospective observational studies. Cancer. 2007;109(12 Suppl):2712–2749. doi: 10.1002/cncr.22654. [DOI] [PubMed] [Google Scholar]
- 23.Potischman N, Troisi R. In-utero and early life exposures in relation to risk of breast cancer. Cancer Causes Control. 1999;10(6):561–573. doi: 10.1023/A:1008955110868. [DOI] [PubMed] [Google Scholar]
- 24.Xue F, Michels KB. Intrauterine factors and risk of breast cancer: a systematic review and meta-analysis of current evidence. Lancet Oncol. 2007;8(12):1088–1100. doi: 10.1016/S1470-2045(07)70377-7. [DOI] [PubMed] [Google Scholar]
- 25.Cohn BA, La Merrill M, Krigbaum NY, Yeh G, Park JS, Zimmermann L, Cirillo PM. DDT exposure in utero and breast cancer. J Clin Endocrinol Metab. 2015;100(8):2865–2872. doi: 10.1210/jc.2015-1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mrema EJ, Rubino FM, Brambilla G, Moretto A, Tsatsakis AM, Colosio C. Persistent organochlorinated pesticides and mechanisms of their toxicity. Toxicology. 2013;307:74–88. doi: 10.1016/j.tox.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 27.Rudel RA, Seryak LM, Brody JG. PCB-containing wood floor finish is a likely source of elevated PCBs in residents’ blood, household air and dust: a case study of exposure. Environ Health. 2008;7:2. doi: 10.1186/1476-069X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phillips D. Polycyclic aromatic hydrocarbons in the diet. Mutat Res. 1999;443(1–2):139–147. doi: 10.1016/S1383-5742(99)00016-2. [DOI] [PubMed] [Google Scholar]
- 29.Miguel A, Kirchstetter T, Harley R. On-road emissions of particulate polycyclic aromatic hydrocarbons and black carbon from gasoline and diesel vehicles. Environmental Science & Technology. 1998;32(4):450–455. doi: 10.1021/es970566w. [DOI] [Google Scholar]
- 30.IARC: Polynuclear aromatic hydrocarbons. Part 3, Industrial exposures in aluminum production, coal gasification, coke production, and iron and steel founding. International Agency for Research on Cancer Monographs on the Carcinogenic Risk of Chemicals to Humans. Lyon; 1984.
- 31.Pedersen M, Wichmann J, Autrup H, Dang D, Decordier I, Hvidberg M, Bossi R, Jakobsen J, Loft S, Knudsen L. Increased micronuclei and bulky DNA adducts in cord blood after maternal exposures to traffic-related air pollution. Environ Res. 2009;109(8):1012–1020. doi: 10.1016/j.envres.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 32.Bocskay KA, Tang D, Orjuela MA, Liu X, Warburton DP, Perera FP. Chromosomal aberrations in cord blood are associated with prenatal exposure to carcinogenic polycyclic aromatic hydrocarbons. Cancer Epidemiol Biomark Prev. 2005;14(2):506–511. doi: 10.1158/1055-9965.EPI-04-0566. [DOI] [PubMed] [Google Scholar]
- 33.Bonner MR, Han D, Nie J, Rogerson P, Vena JE, Muti P, Trevisan M, Edge SB, Freudenheim JL. Breast cancer risk and exposure in early life to polycyclic aromatic hydrocarbons using total suspended particulates as a proxy measure. Cancer Epidemiol Biomark Prev. 2005;14(1):53–60. [PubMed] [Google Scholar]
- 34.Agency for Toxic Substances and Disease Registry (ATSDR) Toxicological profile for polycyclic aromatic hydrocarbons (PAHs) Atlanta: U.S. Department of Health and Human Services, Public Health Service; 1995. [PubMed] [Google Scholar]
- 35.IARC . IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Lyon: World Health Organization; 2002. Volume 82. Some traditional herbal medicines, some mycotoxins, naphthalene and styrene. [PMC free article] [PubMed] [Google Scholar]
- 36.Obana H, Hori S, Kashimoto T, Kunita N. Polycyclic aromatic hydrocarbons in human fat and liver. Bull Environ Contam Toxicol. 1981;27(1):23–27. doi: 10.1007/BF01610981. [DOI] [PubMed] [Google Scholar]
- 37.Plísková M, Vondrácek J, Vojtesek B, Kozubík A, Machala M. Deregulation of cell proliferation by polycyclic aromatic hydrocarbons in human breast carcinoma MCF-7 cells reflects both genotoxic and nongenotoxic events. Toxicol Sci. 2004;83(2):246–256. doi: 10.1093/toxsci/kfi040. [DOI] [PubMed] [Google Scholar]
- 38.Ambrosone C, Shields P. Molecular epidemiology of breast cancer. In: Aldaz C, Gould M, McLachlan J, Slaga T, editors. Etiology of Breast and gynecological cancers (Progress in clinical and biologic research) New York: Wiley-Liss, Inc.; 1997. pp. 93–99. [Google Scholar]
- 39.Gammon MD, Santella RM, Neugut AI, Eng SM, Teitelbaum SL, Paykin A, Levin B, Terry MB, Young TL, Wang LW, et al. Environmental toxins and breast cancer on Long Island. I. Polycyclic aromatic hydrocarbon DNA adducts. Cancer Epidemiol Biomark Prev. 2002;11(8):677–685. [PubMed] [Google Scholar]
- 40.Rundle A, Tang DL, Hibshoosh H, Estabrook A, Schnabel F, Cao WF, Grumet S, Perera FP. The relationship between genetic damage from polycyclic aromatic hydrocarbons in breast tissue and breast cancer. Carcinogenesis. 2000;21(7):1281–1289. doi: 10.1093/carcin/21.7.1281. [DOI] [PubMed] [Google Scholar]
- 41.Korsh J, Shen A, Aliano K, Davenport T. Polycyclic aromatic hydrocarbons and breast cancer: a review of the literature. Breast Care (Basel) 2015;10(5):316–318. doi: 10.1159/000436956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.White A, Teitelbaum S, Stellman S, Beyea J, Steck S, Mordukhovich I, McCarty K, Ahn J, Rossner P, Santella R, et al. Indoor air pollution exposure from use of indoor stoves and fireplaces in association with breast cancer: a case-control study. Environ Health. 2014;13(1):108. doi: 10.1186/1476-069X-13-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.White AJ, Sandler DP. Indoor wood-burning stove and fireplace use and breast cancer in a prospective cohort study. Environ Health Perspect. 2017;125(7):077011. doi: 10.1289/EHP827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mordukhovich I, Beyea J, Herring AH, Hatch M, Stellman SD, Teitelbaum SL, Richardson DB, Millikan RC, Engel LS, Shantakumar S, et al. Vehicular traffic-related polycyclic aromatic hydrocarbon exposure and breast cancer incidence: the Long Island Breast Cancer Study Project (LIBCSP) Environ Health Perspect. 2016;124(1):30–38. doi: 10.1289/ehp.1307736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Agudo A, Peluso M, Munnia A, Lujan-Barroso L, Barricarte A, Amiano P, Navarro C, Sanchez MJ, Quiros JR, Ardanaz E, et al. Aromatic DNA adducts and breast cancer risk: a case-cohort study within the EPIC-Spain. Carcinogenesis. 2017;38(7):691–698. doi: 10.1093/carcin/bgx047. [DOI] [PubMed] [Google Scholar]
- 46.Lee KH, Shu XO, Gao YT, Ji BT, Yang G, Blair A, Rothman N, Zheng W, Chow WH, Kang D. Breast cancer and urinary biomarkers of polycyclic aromatic hydrocarbon and oxidative stress in the Shanghai Women’s Health Study. Cancer Epidemiol Biomark Prev. 2010;19(3):877–883. doi: 10.1158/1055-9965.EPI-09-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miller RL, Yan Z, Maher C, Zhang H, Gudsnuk K, McDonald J, Champagne FA. Impact of prenatal polycyclic aromatic hydrocarbon exposure on behavior, cortical gene expression and DNA methylation of the Bdnf gene. Neuroepigenetics. 2016;5:11–18. doi: 10.1016/j.nepig.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rundle A, Hoepner L, Hassoun A, Oberfield S, Freyer G, Holmes D, Reyes M, Quinn J, Camann D, Perera F, et al. Association of childhood obesity with maternal exposure to ambient air polycyclic aromatic hydrocarbons during pregnancy. Am J Epidemiol. 2012;175(11):1163–1172. doi: 10.1093/aje/kwr455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yan Z, Zhang H, Maher C, Arteaga-Solis E, Champagne FA, Wu L, McDonald JD, Yan B, Schwartz GJ, Miller RL. Prenatal polycyclic aromatic hydrocarbon, adiposity, peroxisome proliferator-activated receptor (PPAR) gamma methylation in offspring, grand-offspring mice. PLoS One. 2014;9(10):e110706. doi: 10.1371/journal.pone.0110706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Russo J, Tay LK, Russo IH. Differentiation of the mammary gland and susceptibility to carcinogenesis. Breast Cancer Res Treat. 1982;2(1):5–73. doi: 10.1007/BF01805718. [DOI] [PubMed] [Google Scholar]
- 51.Russo J, Wilgus G, Russo IH. Susceptibility of the mammary gland to carcinogenesis: I Differentiation of the mammary gland as determinant of tumor incidence and type of lesion. Am J Pathol. 1979;96(3):721–736. [PMC free article] [PubMed] [Google Scholar]
- 52.Mallepell S, Krust A, Chambon P, Brisken C. Paracrine signaling through the epithelial estrogen receptor alpha is required for proliferation and morphogenesis in the mammary gland. Proc Natl Acad Sci U S A. 2006;103(7):2196–2201. doi: 10.1073/pnas.0510974103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Feng Y, Manka D, Wagner KU, Khan SA. Estrogen receptor-alpha expression in the mammary epithelium is required for ductal and alveolar morphogenesis in mice. Proc Natl Acad Sci U S A. 2007;104(37):14718–14723. doi: 10.1073/pnas.0706933104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prins GS, Calderon-Gierszal EL, Hu WY. Stem cells as hormone targets that lead to increased cancer susceptibility. Endocrinology. 2015;156(10):3451–3457. doi: 10.1210/en.2015-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ercan C, van Diest PJ, Vooijs M. Mammary development and breast cancer: the role of stem cells. Curr Mol Med. 2011;11(4):270–285. doi: 10.2174/156652411795678007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mervish NA, Pajak A, Teitelbaum SL, Pinney SM, Windham GC, Kushi LH, Biro FM, Valentin-Blasini L, Blount BC, Wolff MS, et al. Thyroid antagonists (perchlorate, thiocyanate, and nitrate) and childhood growth in a longitudinal study of U.S. girls. Environ Health Perspect. 2016;124(4):542–549. doi: 10.1289/ehp.1409309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wolff MS, Teitelbaum SL, McGovern K, Pinney SM, Windham GC, Galvez M, Pajak A, Rybak M, Calafat AM, Kushi LH, et al. Environmental phenols and pubertal development in girls. Environ Int. 2015;84:174–180. doi: 10.1016/j.envint.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wolff MS, Teitelbaum SL, McGovern K, Windham GC, Pinney SM, Galvez M, Calafat AM, Kushi LH, Biro FM, Breast C, et al. Phthalate exposure and pubertal development in a longitudinal study of US girls. Hum Reprod. 2014;29(7):1558–1566. doi: 10.1093/humrep/deu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wolff MS, Teitelbaum SL, Pinney SM, Windham G, Liao L, Biro F, Kushi LH, Erdmann C, Hiatt RA, Rybak ME, et al. Investigation of relationships between urinary biomarkers of phytoestrogens, phthalates, and phenols and pubertal stages in girls. Environ Health Perspect. 2010;118(7):1039–1046. doi: 10.1289/ehp.0901690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Windham GC, Pinney SM, Voss RW, Sjodin A, Biro FM, Greenspan LC, Stewart S, Hiatt RA, Kushi LH. Brominated flame retardants and other persistent organohalogenated compounds in relation to timing of puberty in a longitudinal study of girls. Environ Health Perspect. 2015;123(10):1046–1052. doi: 10.1289/ehp.1408778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bhatia S, Robison LL, Oberlin O, Greenberg M, Bunin G, Fossati-Bellani F, Meadows AT. Breast cancer and other second neoplasms after childhood Hodgkin’s disease. N Engl J Med. 1996;334(12):745–751. doi: 10.1056/NEJM199603213341201. [DOI] [PubMed] [Google Scholar]
- 62.Land CE. Studies of cancer and radiation dose among atomic bomb survivors. The example of breast cancer. JAMA. 1995;274(5):402–407. doi: 10.1001/jama.1995.03530050050031. [DOI] [PubMed] [Google Scholar]
- 63.Ahlgren M, Melbye M, Wohlfahrt J, Sorensen TI. Growth patterns and the risk of breast cancer in women. N Engl J Med. 2004;351(16):1619–1626. doi: 10.1056/NEJMoa040576. [DOI] [PubMed] [Google Scholar]
- 64.Harris HR, Willett WC, Vaidya RL, Michels KB. An adolescent and early adulthood dietary pattern associated with inflammation and the incidence of breast cancer. Cancer Res. 2017;77(5):1179–1187. doi: 10.1158/0008-5472.CAN-16-2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Michels KB, Ekbom A. Caloric restriction and incidence of breast cancer. JAMA. 2004;291(10):1226–1230. doi: 10.1001/jama.291.10.1226. [DOI] [PubMed] [Google Scholar]
- 66.van den Brandt PA, Spiegelman D, Yaun SS, Adami HO, Beeson L, Folsom AR, Fraser G, Goldbohm RA, Graham S, Kushi L, et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol. 2000;152(6):514–527. doi: 10.1093/aje/152.6.514. [DOI] [PubMed] [Google Scholar]
- 67.Cohn BA, Wolff MS, Cirillo PM, Sholtz RI. DDT and breast cancer in young women: new data on the significance of age at exposure. Environ Health Perspect. 2007;115(10):1406–1414. doi: 10.1289/ehp.10260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cohn BA, Cirillo PM, Terry MB. DDT and breast cancer: prospective study of induction time and susceptibility windows. J Natl Cancer Inst. 2019;111(8):djy198. doi: 10.1093/jnci/djy198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Russo J, Russo IH. Influence of differentiation and cell kinetics on the susceptibility of the rat mammary gland to carcinogenesis. Cancer Res. 1980;40(8 Pt 1):2677–2687. [PubMed] [Google Scholar]
- 70.Russo J, Russo IH. Susceptibility of the mammary gland to carcinogenesis. II. Pregnancy interruption as a risk factor in tumor incidence. Am J Pathol. 1980;100(2):497–512. [PMC free article] [PubMed] [Google Scholar]
- 71.Russo J, Russo IH. Biological and molecular bases of mammary carcinogenesis. Lab Investig. 1987;57(2):112–137. [PubMed] [Google Scholar]
- 72.Russo J, Tay LK, Ciocca DR, Russo IH. Molecular and cellular basis of the mammary gland susceptibility to carcinogenesis. Environ Health Perspect. 1983;49:185–199. doi: 10.1289/ehp.8349185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Russo J, Wilgus G, Tait L, Russo IH. Influence of age and parity on the susceptibility of rat mammary gland epithelial cells in primary cultures to 7,12-dimethylbenz(a)anthracene. In Vitro. 1981;17(10):877–884. doi: 10.1007/BF02618283. [DOI] [PubMed] [Google Scholar]
- 74.Tay LK, Russo J. Formation and removal of 7,12-dimethylbenz [a]anthracene--nucleic acid adducts in rat mammary epithelial cells with different susceptibility to carcinogenesis. Carcinogenesis. 1981;2(12):1327–1333. doi: 10.1093/carcin/2.12.1327. [DOI] [PubMed] [Google Scholar]
- 75.Frech MS, Halama ED, Tilli MT, Singh B, Gunther EJ, Chodosh LA, Flaws JA, Furth PA. Deregulated estrogen receptor alpha expression in mammary epithelial cells of transgenic mice results in the development of ductal carcinoma in situ. Cancer Res. 2005;65(3):681–685. [PMC free article] [PubMed] [Google Scholar]
- 76.Jones LP, Tilli MT, Assefnia S, Torre K, Halama ED, Parrish A, Rosen EM, Furth PA. Activation of estrogen signaling pathways collaborates with loss of Brca1 to promote development of ERalpha-negative and ERalpha-positive mammary preneoplasia and cancer. Oncogene. 2008;27(6):794–802. doi: 10.1038/sj.onc.1210674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Christensen KY, Raymond M, Blackowicz M, Liu Y, Thompson BA, Anderson HA, Turyk M. Perfluoroalkyl substances and fish consumption. Environ Res. 2017;154:145–151. doi: 10.1016/j.envres.2016.12.032. [DOI] [PubMed] [Google Scholar]
- 78.Schaider LA, Balan SA, Blum A, Andrews DQ, Strynar MJ, Dickinson ME, Lunderberg DM, Lang JR, Peaslee GF. Fluorinated compounds in US fast food packaging. Environ Sci Technol Lett. 2017;4(3):105–111. doi: 10.1021/acs.estlett.6b00435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sonthithai P, Suriyo T, Thiantanawat A, Watcharasit P, Ruchirawat M, Satayavivad J. Perfluorinated chemicals, PFOS and PFOA, enhance the estrogenic effects of 17beta-estradiol in T47D human breast cancer cells. J Appl Toxicol. 2016;36(6):790–801. doi: 10.1002/jat.3210. [DOI] [PubMed] [Google Scholar]
- 80.Pierozan P, Jerneren F, Karlsson O. Perfluorooctanoic acid (PFOA) exposure promotes proliferation, migration and invasion potential in human breast epithelial cells. Arch Toxicol. 2018;92(5):1729–1739. doi: 10.1007/s00204-018-2181-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rudel RA, Fenton SE, Ackerman JM, Euling SY, Makris SL. Environmental exposures and mammary gland development: state of the science, public health implications, and research recommendations. Environ Health Perspect. 2011;119(8):1053–1061. doi: 10.1289/ehp.1002864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsai MS, Lin CY, Lin CC, Chen MH, Hsu SH, Chien KL, Sung FC, Chen PC, Su TC. Association between perfluoroalkyl substances and reproductive hormones in adolescents and young adults. Int J Hyg Environ Health. 2015;218(5):437–443. doi: 10.1016/j.ijheh.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 83.Bonefeld-Jorgensen EC, Long M, Fredslund SO, Bossi R, Olsen J. Breast cancer risk after exposure to perfluorinated compounds in Danish women: a case-control study nested in the Danish National Birth Cohort. Cancer Causes Control. 2014;25(11):1439–1448. doi: 10.1007/s10552-014-0446-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.David B, Fenton S. Chapter 61 - Mammary gland. In: Hascheck WM, Rousseaux CG, Wallig MA, Bolon B, Ochoa R, Mahler BW, editors. Hascheck and Rousseaux’s handbook of toxicologic pathology, volume III. 3. New York: Academic Press; 2013. [Google Scholar]
- 85.Meier-Abt Fabienne, Bentires-Alj Mohamed. How pregnancy at early age protects against breast cancer. Trends in Molecular Medicine. 2014;20(3):143–153. doi: 10.1016/j.molmed.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 86.Meier-Abt F, Brinkhaus H, Bentires-Alj M. Early but not late pregnancy induces lifelong reductions in the proportion of mammary progesterone sensing cells and epithelial Wnt signaling. Breast Cancer Res. 2014;16(2):402. doi: 10.1186/bcr3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rajkumar L, Arumugam A, Elsayed A, Schecter S, Kotkowski E, Castillo R, de la Torre A, Hernandez C. Long-term hormonal promotion overcomes genetic resistance to mammary cancer. Steroids. 2011;76(1–2):31–37. doi: 10.1016/j.steroids.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 88.Swanson SM, Guzman RC, Collins G, Tafoya P, Thordarson G, Talamantes F, Nandi S. Refractoriness to mammary carcinogenesis in the parous mouse is reversible by hormonal stimulation induced by pituitary isografts. Cancer Lett. 1995;90(2):171–181. doi: 10.1016/0304-3835(95)03712-6. [DOI] [PubMed] [Google Scholar]
- 89.Thordarson G, Van Horn K, Guzman RC, Nandi S, Talamantes F. Parous rats regain high susceptibility to chemically induced mammary cancer after treatment with various mammotropic hormones. Carcinogenesis. 2001;22(7):1027–1033. doi: 10.1093/carcin/22.7.1027. [DOI] [PubMed] [Google Scholar]
- 90.Schedin P. Pregnancy-associated breast cancer and metastasis. Nat Rev Cancer. 2006;6(4):281–291. doi: 10.1038/nrc1839. [DOI] [PubMed] [Google Scholar]
- 91.Azim HA, Jr, Santoro L, Russell-Edu W, Pentheroudakis G, Pavlidis N, Peccatori FA. Prognosis of pregnancy-associated breast cancer: a meta-analysis of 30 studies. Cancer Treat Rev. 2012;38(7):834–842. doi: 10.1016/j.ctrv.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 92.Callihan EB, Gao D, Jindal S, Lyons TR, Manthey E, Edgerton S, Urquhart A, Schedin P, Borges VF. Postpartum diagnosis demonstrates a high risk for metastasis and merits an expanded definition of pregnancy-associated breast cancer. Breast Cancer Res Treat. 2013;138(2):549–559. doi: 10.1007/s10549-013-2437-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Albrektsen G, Heuch I, Hansen S, Kvale G. Breast cancer risk by age at birth, time since birth and time intervals between births: exploring interaction effects. Br J Cancer. 2005;92(1):167–175. doi: 10.1038/sj.bjc.6602302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chie WC, Hsieh C, Newcomb PA, Longnecker MP, Mittendorf R, Greenberg ER, Clapp RW, Burke KP, Titus-Ernstoff L, Trentham-Dietz A, et al. Age at any full-term pregnancy and breast cancer risk. Am J Epidemiol. 2000;151(7):715–722. doi: 10.1093/oxfordjournals.aje.a010266. [DOI] [PubMed] [Google Scholar]
- 95.MacMahon B, Cole P, Lin TM, Lowe CR, Mirra AP, Ravnihar B, Salber EJ, Valaoras VG, Yuasa S. Age at first birth and breast cancer risk. Bull World Health Organ. 1970;43(2):209–221. [PMC free article] [PubMed] [Google Scholar]
- 96.Rosner B, Colditz GA, Willett WC. Reproductive risk factors in a prospective study of breast cancer: the Nurses’ Health Study. Am J Epidemiol. 1994;139(8):819–835. doi: 10.1093/oxfordjournals.aje.a117079. [DOI] [PubMed] [Google Scholar]
- 97.Ronckers CM, Erdmann CA, Land CE. Radiation and breast cancer: a review of current evidence. Breast Cancer Res. 2005;7(1):21–32. doi: 10.1186/bcr970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Russo IH, Russo J. Developmental stage of the rat mammary gland as determinant of its susceptibility to 7,12-dimethylbenz [a]anthracene. J Natl Cancer Inst. 1978;61(6):1439–1449. [PubMed] [Google Scholar]
- 99.Sinha DK, Pazik JE, Dao TL. Prevention of mammary carcinogenesis in rats by pregnancy: effect of full-term and interrupted pregnancy. Br J Cancer. 1988;57(4):390–394. doi: 10.1038/bjc.1988.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.MUNFORD R. E. CHANGES IN THE MAMMARY GLANDS OF RATS AND MICE DURING PREGNANCY, LACTATION AND INVOLUTION. Journal of Endocrinology. 1963;28(1):17–34. doi: 10.1677/joe.0.0280017. [DOI] [PubMed] [Google Scholar]
- 101.Antonio AC, Shenton A, Maher ER, Watson E, Woodward E, Lalloo F, Easton DF, Evans DG. Parity and breast cancer risk among BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2006;8(6):R72. [DOI] [PMC free article] [PubMed]
- 102.Jerry DJ, Kittrell FS, Kuperwasser C, Laucirica R, Dickinson ES, Bonilla PJ, Butel JS, Medina D. A mammary-specific model demonstrates the role of the p53 tumor suppressor gene in tumor development. Oncogene. 2000;19(8):1052–1058. doi: 10.1038/sj.onc.1203270. [DOI] [PubMed] [Google Scholar]
- 103.Milne Roger L., Osorio Ana, Ramón y Cajal Teresa, Baiget Montserrat, Lasa Adriana, Diaz-Rubio Eduardo, de la Hoya Miguel, Caldés Trinidad, Teulé Alex, Lázaro Conxi, Blanco Ignacio, Balmaña Judith, Sánchez-Ollé Gessamí, Vega Ana, Blanco Ana, Chirivella Isabel, Esteban Cardeñosa Eva, Durán Mercedes, Velasco Eladio, Martínez de Dueñas Eduardo, Tejada María-Isabel, Miramar María-Dolores, Calvo María-Teresa, Guillén-Ponce Carmen, Salazar Raquel, San Román Carlos, Urioste Miguel, Benítez Javier. Parity and the risk of breast and ovarian cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Research and Treatment. 2009;119(1):221–232. doi: 10.1007/s10549-009-0394-1. [DOI] [PubMed] [Google Scholar]
- 104.Medina D, Kittrell FS. p53 function is required for hormone-mediated protection of mouse mammary tumorigenesis. Cancer Res. 2003;63(19):6140–6143. [PubMed] [Google Scholar]
- 105.Rajkumar L, Guzman RC, Yang J, Thordarson G, Talamantes F, Nandi S. Short-term exposure to pregnancy levels of estrogen prevents mammary carcinogenesis. ProcNatlAcadSciUSA. 2001;98(20):11755–11759. doi: 10.1073/pnas.201393798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rajkumar L, Kittrell FS, Guzman RC, Brown PH, Nandi S, Medina D. Hormone-induced protection of mammary tumorigenesis in genetically engineered mouse models. Breast Cancer Res. 2007;9(1):R12. doi: 10.1186/bcr1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Russo J, Ao X, Grill C, Russo IH. Pattern of distribution of cells positive for estrogen receptor alpha and progesterone receptor in relation to proliferating cells in the mammary gland. Breast Cancer ResTreat. 1999;53(3):217–227. doi: 10.1023/A:1006186719322. [DOI] [PubMed] [Google Scholar]
- 108.Russo J, Gusterson BA, Rogers AE, Russo IH, Wellings SR, van Zwieten MJ. Comparative study of human and rat mammary tumorigenesis. Lab Investig. 1990;62(3):244–278. [PubMed] [Google Scholar]
- 109.Dunphy KA, Blackburn AC, Yan H, O'Connell LR, Jerry DJ. Estrogen and progesterone induce persistent increases in p53-dependent apoptosis and suppress mammary tumors in BALB/c-Trp53+/− mice. Breast Cancer Res. 2008;10(3):R43. doi: 10.1186/bcr2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cohn BA, Terry MB, Plumb M, Cirillo PM. Exposure to polychlorinated biphenyl (PCB) congeners measured shortly after giving birth and subsequent risk of maternal breast cancer before age 50. Breast Cancer Res Treat. 2012;136(1):267–275. doi: 10.1007/s10549-012-2257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Brody JG, Moysich KB, Humblet O, Attfield KR, Beehler GP, Rudel RA. Environmental pollutants and breast cancer: epidemiologic studies. Cancer. 2007;109(12 Suppl):2667–2711. doi: 10.1002/cncr.22655. [DOI] [PubMed] [Google Scholar]
- 112.Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: an updated review of epidemiological literature informed by biological mechanisms. Environ Res. 2017;160:152–182. doi: 10.1016/j.envres.2017.08.045. [DOI] [PubMed] [Google Scholar]
- 113.Snedeker SM. Pesticides and breast cancer risk: a review of DDT, DDE, and dieldrin. Environ Health Perspect. 2001;109(Suppl 1):35–47. doi: 10.1289/ehp.01109s135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Whyatt RM, Perzanowski MS, Just AC, Rundle AG, Donohue KM, Calafat AM, Hoepner LA, Perera FP, Miller RL. Asthma in inner-city children at 5-11 years of age and prenatal exposure to phthalates: the Columbia Center for Children’s Environmental Health Cohort. Environ Health Perspect. 2014;122(10):1141–1146. doi: 10.1289/ehp.1307670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nie J, Beyea J, Bonner MR, Han D, Vena JE, Rogerson P, Vito D, Muti P, Trevisan M, Edge SB, et al. Exposure to traffic emissions throughout life and risk of breast cancer: the Western New York Exposures and Breast Cancer (WEB) study. Cancer Causes Control. 2007;18(9):947–955. doi: 10.1007/s10552-007-9036-2. [DOI] [PubMed] [Google Scholar]
- 116.Mortensen ME, Calafat AM, Ye X, Wong LY, Wright DJ, Pirkle JL, Merrill LS, Moye J. Urinary concentrations of environmental phenols in pregnant women in a pilot study of the National Children’s Study. Environ Res. 2014;129:32–38. doi: 10.1016/j.envres.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Philippat C, Wolff MS, Calafat AM, Ye X, Bausell R, Meadows M, Stone J, Slama R, Engel SM. Prenatal exposure to environmental phenols: concentrations in amniotic fluid and variability in urinary concentrations during pregnancy. Environ Health Perspect. 2013;121(10):1225–1231. doi: 10.1289/ehp.1206335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Meier-Abt F, Milani E, Roloff T, Brinkhaus H, Duss S, Meyer DS, Klebba I, Balwierz PJ, van Nimwegen E, Bentires-Alj M. Parity induces differentiation and reduces Wnt/Notch signaling ratio and proliferation potential of basal stem/progenitor cells isolated from mouse mammary epithelium. Breast Cancer Res. 2013;15(2):R36. doi: 10.1186/bcr3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Benz CC. Impact of aging on the biology of breast cancer. Crit Rev Oncol Hematol. 2008;66(1):65–74. doi: 10.1016/j.critrevonc.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pike MC, Spicer DV, Dahmoush L, Press MF. Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol Rev. 1993;15(1):17–35. doi: 10.1093/oxfordjournals.epirev.a036102. [DOI] [PubMed] [Google Scholar]
- 121.Trichopoulos D, MacMahon B, Cole P. Menopause and breast cancer risk. J Natl Cancer Inst. 1972;48(3):605–613. [PubMed] [Google Scholar]
- 122.Cheng G, Li Y, Omoto Y, Wang Y, Berg T, Nord M, Vihko P, Warner M, Piao YS, Gustafsson JA. Differential regulation of estrogen receptor (ER) alpha and ERbeta in primate mammary gland. J Clin Endocrinol Metab. 2005;90(1):435–444. doi: 10.1210/jc.2004-0861. [DOI] [PubMed] [Google Scholar]
- 123.Khan SA, Rogers MA, Khurana KK, Meguid MM, Numann PJ. Estrogen receptor expression in benign breast epithelium and breast cancer risk. J Natl Cancer Inst. 1998;90(1):37–42. doi: 10.1093/jnci/90.1.37. [DOI] [PubMed] [Google Scholar]
- 124.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results. From the Women's Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 125.Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, Rodabough RJ, Gilligan MA, Cyr MG, Thomson CA, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. JAMA. 2003;289(24):3243–3253. doi: 10.1001/jama.289.24.3243. [DOI] [PubMed] [Google Scholar]
- 126.Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, Anderson G, Howard BV, Thomson CA, LaCroix AZ, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women's Health Initiative randomized trials. JAMA. 2013;310(13):1353–1368. doi: 10.1001/jama.2013.278040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chlebowski RT, Rohan TE, Manson JE, Aragaki AK, Kaunitz A, Stefanick ML, Simon MS, Johnson KC, Wactawski-Wende J, O'Sullivan MJ, et al. Breast cancer after use of estrogen plus progestin and estrogen alone: analyses of data from 2 women’s health initiative randomized clinical trials. JAMA Oncol. 2015;1(3):296–305. doi: 10.1001/jamaoncol.2015.0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Byrne C, Ursin G, Martin CF, Peck JD, Cole EB, Zeng D, Kim E, Yaffe MD, Boyd NF, Heiss G et al: Mammographic density change with estrogen and progestin therapy and breast cancer risk. J Natl Cancer Inst. 2017;109(9). 10.1093/jnci/djx001. [DOI] [PMC free article] [PubMed]
- 129.Santen RJ, Song Y, Yue W, Wang JP, Heitjan DF. Effects of menopausal hormonal therapy on occult breast tumors. J Steroid Biochem Mol Biol. 2013;137:150–156. doi: 10.1016/j.jsbmb.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 130.Allen JG, McClean MD, Stapleton HM, Webster TF. Linking PBDEs in house dust to consumer products using X-ray fluorescence. Environ Sci Technol. 2008;42(11):4222–4228. doi: 10.1021/es702964a. [DOI] [PubMed] [Google Scholar]
- 131.Costa LG, Giordano G, Tagliaferri S, Caglieri A, Mutti A. Polybrominated diphenyl ether (PBDE) flame retardants: environmental contamination, human body burden and potential adverse health effects. Acta Biomed. 2008;79(3):172–183. [PubMed] [Google Scholar]
- 132.Darnerud PO. Brominated flame retardants as possible endocrine disrupters. Int J Androl. 2008;31(2):152–160. doi: 10.1111/j.1365-2605.2008.00869.x. [DOI] [PubMed] [Google Scholar]
- 133.Darnerud PO, Eriksen GS, Johannesson T, Larsen PB, Viluksela M. Polybrominated diphenyl ethers: occurrence, dietary exposure, and toxicology. Environ Health Perspect. 2001;109(Suppl 1):49–68. doi: 10.1289/ehp.01109s149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lorber M. Exposure of Americans to polybrominated diphenyl ethers. J Expo Sci Environ Epidemiol. 2008;18(1):2–19. doi: 10.1038/sj.jes.7500572. [DOI] [PubMed] [Google Scholar]
- 135.U.S. Department of Health and Human Services, Public Health Service: Toxicological Profile for Polybrominated Biphenyls and Polybrominated Diphenyl Ethers. In. Edited by U.S. Department of Health and Human Services Agency for Toxic Substances and Disease Registry. Atlanta; 2004.
- 136.He Y, Murphy MB, Yu RM, Lam MH, Hecker M, Giesy JP, Wu RS, Lam PK. Effects of 20 PBDE metabolites on steroidogenesis in the H295R cell line. Toxicol Lett. 2008;176(3):230–238. doi: 10.1016/j.toxlet.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 137.Sprague BL, Trentham-Dietz A, Hedman CJ, Wang J, Hemming JD, Hampton JM, Buist DS, Aiello Bowles EJ, Sisney GS, Burnside ES. Circulating serum xenoestrogens and mammographic breast density. Breast Cancer Res. 2013;15(3):R45. doi: 10.1186/bcr3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Trabert B, Falk RT, Figueroa JD, Graubard BI, Garcia-Closas M, Lissowska J, Peplonska B, Fox SD, Brinton LA. Urinary bisphenol A-glucuronide and postmenopausal breast cancer in Poland. Cancer Causes Control. 2014;25(12):1587–1593. doi: 10.1007/s10552-014-0461-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen S, Zhou D, Hsin LY, Kanaya N, Wong C, Yip R, Sakamuru S, Xia M, Yuan YC, Witt K, et al. AroER tri-screen is a biologically relevant assay for endocrine disrupting chemicals modulating the activity of aromatase and/or the estrogen receptor. Toxicol Sci. 2014;139(1):198–209. doi: 10.1093/toxsci/kfu023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sprague BL, Trentham-Dietz A, Hedman CJ, Wang J, Hemming JD, Hampton JM, Buist DS, Bowles EJ, Burnside ES. Authors’ response. Breast Cancer Res. 2013;15(5):403. doi: 10.1186/bcr3494. [DOI] [PubMed] [Google Scholar]
- 141.Holtcamp W. Obesogens: an environmental link to obesity. Environ Health Perspect. 2012;120(2):a62–a68. doi: 10.1289/ehp.120-a62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Byrne C, Divekar SD, Storchan GB, Parodi DA, Martin MB. Cadmium--a metallohormone? Toxicol Appl Pharmacol. 2009;238(3):266–271. doi: 10.1016/j.taap.2009.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Byrne C, Divekar SD, Storchan GB, Parodi DA, Martin MB. Metals and breast cancer. J Mammary Gland Biol Neoplasia. 2013;18(1):63–73. doi: 10.1007/s10911-013-9273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Garcia-Morales P, Saceda M, Kenney N, Kim N, Salomon DS, Gottardis MM, Solomon HB, Sholler PF, Jordan VC, Martin MB. Effect of cadmium on estrogen receptor levels and estrogen-induced responses in human breast cancer cells. J Biol Chem. 1994;269(24):16896–16901. [PubMed] [Google Scholar]
- 145.Choe SY, Kim SJ, Kim HG, Lee JH, Choi Y, Lee H, Kim Y. Evaluation of estrogenicity of major heavy metals. Sci Total Environ. 2003;312(1–3):15–21. doi: 10.1016/S0048-9697(03)00190-6. [DOI] [PubMed] [Google Scholar]
- 146.Martinez-Campa C, Alonso-Gonzalez C, Mediavilla MD, Cos S, Gonzalez A, Ramos S, Sanchez-Barcelo EJ. Melatonin inhibits both ER alpha activation and breast cancer cell proliferation induced by a metalloestrogen, cadmium. J Pineal Res. 2006;40(4):291–296. doi: 10.1111/j.1600-079X.2006.00315.x. [DOI] [PubMed] [Google Scholar]
- 147.Siewit CL, Gengler B, Vegas E, Puckett R, Louie MC. Cadmium promotes breast cancer cell proliferation by potentiating the interaction between ERalpha and c-Jun. Mol Endocrinol. 2010;24(5):981–992. doi: 10.1210/me.2009-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Brama M, Gnessi L, Basciani S, Cerulli N, Politi L, Spera G, Mariani S, Cherubini S, Scotto d'Abusco A, Scandurra R, et al. Cadmium induces mitogenic signaling in breast cancer cell by an ERalpha-dependent mechanism. Mol Cell Endocrinol. 2007;264(1–2):102–108. doi: 10.1016/j.mce.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 149.Stoica A, Katzenellenbogen BS, Martin MB. Activation of estrogen receptor-alpha by the heavy metal cadmium. Mol Endocrinol. 2000;14(4):545–553. doi: 10.1210/mend.14.4.0441. [DOI] [PubMed] [Google Scholar]
- 150.Wilson VS, Bobseine K, Gray LE., Jr Development and characterization of a cell line that stably expresses an estrogen-responsive luciferase reporter for the detection of estrogen receptor agonist and antagonists. Toxicol Sci. 2004;81(1):69–77. doi: 10.1093/toxsci/kfh180. [DOI] [PubMed] [Google Scholar]
- 151.Liu Z, Yu X, Shaikh ZA. Rapid activation of ERK1/2 and AKT in human breast cancer cells by cadmium. Toxicol Appl Pharmacol. 2008;228(3):286–294. doi: 10.1016/j.taap.2007.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zang Y, Odwin-Dacosta S, Yager JD. Effects of cadmium on estrogen receptor mediated signaling and estrogen induced DNA synthesis in T47D human breast cancer cells. Toxicol Lett. 2009;184(2):134–138. doi: 10.1016/j.toxlet.2008.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Adams SV, Newcomb PA, White E. Dietary cadmium and risk of invasive postmenopausal breast cancer in the VITAL cohort. Cancer Causes Control. 2012;23(6):845–854. doi: 10.1007/s10552-012-9953-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Adams SV, Quraishi SM, Shafer MM, Passarelli MN, Freney EP, Chlebowski RT, Luo J, Meliker JR, Mu L, Neuhouser ML, et al. Dietary cadmium exposure and risk of breast, endometrial, and ovarian cancer in the Women's Health Initiative. Environ Health Perspect. 2014;122(6):594–600. doi: 10.1289/ehp.1307054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Eriksen KT, Halkjaer J, Sorensen M, Meliker JR, McElroy JA, Tjonneland A, Raaschou-Nielsen O. Dietary cadmium intake and risk of breast, endometrial and ovarian cancer in Danish postmenopausal women: a prospective cohort study. PLoS One. 2014;9(6):e100815. doi: 10.1371/journal.pone.0100815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Grioni S, Agnoli C, Krogh V, Pala V, Rinaldi S, Vinceti M, Contiero P, Vescovi L, Malavolti M, Sieri S. Dietary cadmium and risk of breast cancer subtypes defined by hormone receptor status: a prospective cohort study. Int J Cancer. 2019;144(9):2153–2160. doi: 10.1002/ijc.32039. [DOI] [PubMed] [Google Scholar]
- 157.Itoh H, Iwasaki M, Sawada N, Takachi R, Kasuga Y, Yokoyama S, Onuma H, Nishimura H, Kusama R, Yokoyama K, et al. Dietary cadmium intake and breast cancer risk in Japanese women: a case-control study. Int J Hyg Environ Health. 2014;217(1):70–77. doi: 10.1016/j.ijheh.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 158.Julin B, Wolk A, Bergkvist L, Bottai M, Akesson A. Dietary cadmium exposure and risk of postmenopausal breast cancer: a population-based prospective cohort study. Cancer Res. 2012;72(6):1459–1466. doi: 10.1158/0008-5472.CAN-11-0735. [DOI] [PubMed] [Google Scholar]
- 159.Sawada N, Iwasaki M, Inoue M, Takachi R, Sasazuki S, Yamaji T, Shimazu T, Endo Y, Tsugane S. Long-term dietary cadmium intake and cancer incidence. Epidemiology. 2012;23(3):368–376. doi: 10.1097/EDE.0b013e31824d063c. [DOI] [PubMed] [Google Scholar]
- 160.Amadou A, Praud D, Coudon T, Danjou AMN, Faure E, Leffondre K, Le Romancer M, Severi G, Salizzoni P, Mancini FR, et al. Chronic long-term exposure to cadmium air pollution and breast cancer risk in the French E3N cohort. Int J Cancer. 2019. 10.1002/ijc.32257. [DOI] [PubMed]
- 161.White AJ, O'Brien KM, Niehoff NM, Carroll R, Sandler DP. Metallic air pollutants and breast cancer risk in a nationwide cohort study. Epidemiology. 2019;30(1):20–28. doi: 10.1097/EDE.0000000000000917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Adams SV, Shafer MM, Bonner MR, LaCroix AZ, Manson JE, Meliker JR, Neuhouser ML, Newcomb PA. Urinary cadmium and risk of invasive breast cancer in the women’s health initiative. Am J Epidemiol. 2016;183(9):815–823. doi: 10.1093/aje/kwv285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gaudet Mia M., Deubler Emily L., Kelly Rachel S., Ryan Diver W., Teras Lauren R., Hodge James M., Levine Keith E., Haines Laura G., Lundh Thomas, Lenner Per, Palli Domenico, Vineis Paolo, Bergdahl Ingvar A., Gapstur Susan M., Kyrtopoulos Soterios A. Blood levels of cadmium and lead in relation to breast cancer risk in three prospective cohorts. International Journal of Cancer. 2018;144(5):1010–1016. doi: 10.1002/ijc.31805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Nagata C, Nagao Y, Nakamura K, Wada K, Tamai Y, Tsuji M, Yamamoto S, Kashiki Y. Cadmium exposure and the risk of breast cancer in Japanese women. Breast Cancer Res Treat. 2013;138(1):235–239. doi: 10.1007/s10549-013-2414-4. [DOI] [PubMed] [Google Scholar]
- 165.McElroy JA, Shafer MM, Trentham-Dietz A, Hampton JM, Newcomb PA. Cadmium exposure and breast cancer risk. J Natl Cancer Inst. 2006;98(12):869–873. doi: 10.1093/jnci/djj233. [DOI] [PubMed] [Google Scholar]
- 166.Gallagher CM, Chen JJ, Kovach JS. Environmental cadmium and breast cancer risk. Aging (Albany NY) 2010;2(11):804–814. doi: 10.18632/aging.100226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.O'Brien KM, White AJ, Jackson BP, Karagas MR, Sandler DP, Weinberg CR. Toenail-based metal concentrations and young-onset breast cancer. Am J Epidemiol. 2019;188(4):646–655. doi: 10.1093/aje/kwy283. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 168.White AJ, Weinberg CR, O'Meara ES, Sandler DP, Sprague BL. Airborne metals and polycyclic aromatic hydrocarbons in relation to mammographic breast density. Breast Cancer Res. 2019;21(1):24. doi: 10.1186/s13058-019-1110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Adams SV, Hampton JM, Trentham-Dietz A, Gangnon RE, Shafer MM, Newcomb PA. Urinary cadmium and mammographic density. Epidemiology. 2017;28(1):e6–e7. doi: 10.1097/EDE.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 170.Adams SV, Newcomb PA, Shafer MM, Atkinson C, Bowles EJ, Newton KM, Lampe JW. Urinary cadmium and mammographic density in premenopausal women. Breast Cancer Res Treat. 2011;128(3):837–844. doi: 10.1007/s10549-011-1383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Mora-Pinzon MC, Trentham-Dietz A, Gangnon RE, Adams SV, Hampton JM, Burnside E, Shafer MM, Newcomb PA. Urinary magnesium and other elements in relation to mammographic Breast density, a measure of breast cancer risk. Nutr Cancer. 2018;70(3):441–446. doi: 10.1080/01635581.2018.1446094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Biro FM, Pinney SM, Schwartz RC, Huang B, Cattran AM, Haslam SZ. Amphiregulin as a novel serum marker of puberty in girls. J Pediatr Adolesc Gynecol. 2017;30(5):535–539. doi: 10.1016/j.jpag.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Knight JA, Blackmore KM, Wong J, Tharmalingam S, Lilge L. Optical spectroscopy of the breast in premenopausal women reveals tissue variation with changes in age and parity. Med Phys. 2010;37(2):419–426. doi: 10.1118/1.3276737. [DOI] [PubMed] [Google Scholar]
- 175.Blackmore KM, Knight JA, Walter J, Lilge L. The association between breast tissue optical content and mammographic density in pre- and post-menopausal women. PLoS One. 2015;10(1):e0115851. doi: 10.1371/journal.pone.0115851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Walter EJ, Knight JA, Lilge L. A multi-wavelength, laser-based optical spectroscopy device for breast density and breast cancer risk pre-screening. J Biophotonics. 2017;10(4):565–576. doi: 10.1002/jbio.201600033. [DOI] [PubMed] [Google Scholar]
- 177.Blyschak K, Simick M, Jong R, Lilge L. Classification of breast tissue density by optical transillumination spectroscopy: optical and physiological effects governing predictive value. Med Phys. 2004;31(6):1398–1414. doi: 10.1118/1.1738191. [DOI] [PubMed] [Google Scholar]
- 178.Blackmore KM, Knight JA, Lilge L. Association between transillumination breast spectroscopy and quantitative mammographic features of the breast. Cancer Epidemiol Biomarkers Prev. 2008;17(5):1043–1050. doi: 10.1158/1055-9965.EPI-07-2658. [DOI] [PubMed] [Google Scholar]
- 179.Walter E. J., Lilge Lothar. Optical assessment of mammographic breast density by a 12-wavelength vs a continuous-spectrum optical spectroscopy device. Journal of Biophotonics. 2017;11(2):e201700071. doi: 10.1002/jbio.201700071. [DOI] [PubMed] [Google Scholar]
- 180.Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, Hoover R, Haile R. Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995;87(21):1622–1629. doi: 10.1093/jnci/87.21.1622. [DOI] [PubMed] [Google Scholar]
- 181.Sak MA, Littrup PJ, Duric N, Mullooly M, Sherman ME, Gierach GL. Current and future methods for measuring breast density: a brief comparative review. Breast Cancer Manag. 2015;4(4):209–221. doi: 10.2217/bmt.15.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.McCormack VA, dos Santos SI. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev. 2006;15(6):1159–1169. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 183.Maskarinec G, Pagano I, Lurie G, Kolonel LN. A longitudinal investigation of mammographic density: the multiethnic cohort. Cancer Epidemiol Biomark Prev. 2006;15(4):732–739. doi: 10.1158/1055-9965.EPI-05-0798. [DOI] [PubMed] [Google Scholar]
- 184.Boyd N, Martin L, Stone J, Little L, Minkin S, Yaffe M. A longitudinal study of the effects of menopause on mammographic features. Cancer Epidemiol Biomarkers Prev. 2002;11(10 Pt 1):1048–1053. [PubMed] [Google Scholar]
- 185.Lokate M, Stellato RK, Veldhuis WB, Peeters PH, van Gils CH. Age-related changes in mammographic density and breast cancer risk. Am J Epidemiol. 2013;178(1):101–109. doi: 10.1093/aje/kws446. [DOI] [PubMed] [Google Scholar]
- 186.Work ME, Reimers LL, Quante AS, Crew KD, Whiffen A, Terry MB. Changes in mammographic density over time in breast cancer cases and women at high risk for breast cancer. Int J Cancer. 2014;135(7):1740–1744. doi: 10.1002/ijc.28825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kerlikowske K, Ichikawa L, Miglioretti DL, Buist DS, Vacek PM, Smith-Bindman R, Yankaskas B, Carney PA, Ballard-Barbash R. National Institutes of Health Breast Cancer Surveillance Consortium: longitudinal measurement of clinical mammographic breast density to improve estimation of breast cancer risk. J Natl Cancer Inst. 2007;99(5):386–395. doi: 10.1093/jnci/djk066. [DOI] [PubMed] [Google Scholar]
- 188.Boyd N, Martin L, Chavez S, Gunasekara A, Salleh A, Melnichouk O, Yaffe M, Friedenreich C, Minkin S, Bronskill M. Breast-tissue composition and other risk factors for breast cancer in young women: a cross-sectional study. Lancet Oncol. 2009;10(6):569–580. doi: 10.1016/S1470-2045(09)70078-6. [DOI] [PubMed] [Google Scholar]
- 189.Bertrand KA, Baer HJ, Orav EJ, Klifa C, Shepherd JA, Van Horn L, Snetselaar L, Stevens VJ, Hylton NM, Dorgan JF. Body fatness during childhood and adolescence and breast density in young women: a prospective analysis. Breast Cancer Res. 2015;17:95. doi: 10.1186/s13058-015-0601-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Denholm R, De Stavola B, Hipwell JH, Doran SJ, Busana MC, Eng A, Jeffreys M, Leach MO, Hawkes D, Dos Santos SI. Pre-natal exposures and breast tissue composition: findings from a British pre-birth cohort of young women and a systematic review. Breast Cancer Res. 2016;18(1):102. doi: 10.1186/s13058-016-0751-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Novotny R, Daida Y, Morimoto Y, Shepherd J, Maskarinec G. Puberty, body fat, and breast density in girls of several ethnic groups. Am J Hum Biol. 2011;23(3):359–365. doi: 10.1002/ajhb.21145. [DOI] [PubMed] [Google Scholar]
- 192.Gaskins AJ, Pereira A, Quintiliano D, Shepherd JA, Uauy R, Corvalan C, Michels KB. Dairy intake in relation to breast and pubertal development in Chilean girls. Am J Clin Nutr. 2017;105(5):1166–1175. doi: 10.3945/ajcn.116.150359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Lyons TR, O'Brien J, Borges VF, Conklin MW, Keely PJ, Eliceiri KW, Marusyk A, Tan AC, Schedin P. Postpartum mammary gland involution drives progression of ductal carcinoma in situ through collagen and COX-2. Nat Med. 2011;17(9):1109–1115. doi: 10.1038/nm.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Provenzano PP, Inman DR, Eliceiri KW, Knittel JG, Yan L, Rueden CT, White JG, Keely PJ. Collagen density promotes mammary tumor initiation and progression. BMC Med. 2008;6:11. doi: 10.1186/1741-7015-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Brown JQ, Wilke LG, Geradts J, Kennedy SA, Palmer GM, Ramanujam N. Quantitative optical spectroscopy: a robust tool for direct measurement of breast cancer vascular oxygenation and total hemoglobin content in vivo. Cancer Res. 2009;69(7):2919–2926. doi: 10.1158/0008-5472.CAN-08-3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Lilge L, Terry MB, Walter J, Pinnaduwage D, Glendon G, Hanna D, Tammemagi M, Bradbury AR, Buys SS, Daly MB, et al. Non-invasive optical spectroscopic (OS) monitoring of breast development during puberty. Breast Cancer Res. 2017;19(1):12. [DOI] [PMC free article] [PubMed]
- 197.Brody JG, Dunagan SC, Morello-Frosch R, Brown P, Patton S, Rudel RA. Reporting individual results for biomonitoring and environmental exposures: lessons learned from environmental communication case studies. Environ Health. 2014;13:40. doi: 10.1186/1476-069X-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Hernick AD, Brown MK, Pinney SM, Biro FM, Ball KM, Bornschein RL. Sharing unexpected biomarker results with study participants. Environ Health Perspect. 2011;119(1):1–5. doi: 10.1289/ehp.1001988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Boronow KE, Susmann HP, Gajos KZ, Rudel RA, Arnold KC, Brown P, Morello-Frosch R, Havas L, Brody JG. DERBI: a digital method to help researchers offer “right-to-know” personal exposure results. Environ Health Perspect. 2017;125(2):A27–A33. doi: 10.1289/EHP702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Silk KJ, Perrault EK, Neuberger L, Rogers A, Atkin C, Barlow J, Duncan DM. Translating and testing breast cancer risk reduction messages for mothers of adolescent girls. J Health Commun. 2014;19(2):226–243. doi: 10.1080/10810730.2013.811322. [DOI] [PubMed] [Google Scholar]
- 201.Balazs Carolina L., Morello-Frosch Rachel. The Three Rs: How Community-Based Participatory Research Strengthens the Rigor, Relevance, and Reach of Science. Environmental Justice. 2013;6(1):9–16. doi: 10.1089/env.2012.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A et al: SEER Cancer Statistics Review, 1975–2014. In.; National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017.
- 203.ACOG Committee Opinion No 575: Exposure to toxic environmental agents. Obstet Gynecol. 2013;122(4):931–935. doi: 10.1097/01.AOG.0000435416.21944.54. [DOI] [PubMed] [Google Scholar]
- 204.Attina TM, Malits J, Naidu M, Trasande L. Racial/ethnic disparities in disease burden and costs related to exposure to endocrine-disrupting chemicals in the United States: an exploratory analysis. J Clin Epidemiol. 2019;108:34–43. doi: 10.1016/j.jclinepi.2018.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.James W, Jia C, Kedia S. Uneven magnitude of disparities in cancer risks from air toxics. Int J Environ Res Public Health. 2012;9(12):4365–4385. doi: 10.3390/ijerph9124365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.2018–2023 Strategic Plan: Advancing Environmental Health Sciences, Improving Health. In.; NIH Publication No. 18-ES-7935. National Institute of Environmental Health Sciences, National Institutes of Health, US Department of Health and Human Services; 2018. (www.niehs.nih.gov) (Accessed 1 Oct 2018).
- 207.Terry MB, Forman MR. Empowering pediatricians to prevent chronic disease across generations. Pediatrics. 2016;138(Suppl 1):S92–S94. doi: 10.1542/peds.2015-4268M. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.