Abstract
Objective
It is recognised that ketamine treatment can reduce suicidal ideation (SI) in people with depression, at least in the short term. However, information is lacking on patients’ perspectives on such effects. Studying these can contribute to greater understanding of the mechanisms underlying impact of ketamine treatment on SI. The aim of this study was to investigate patients’ reports of the impact of treatment on their SI, the duration of effects and possible mechanisms.
Design and setting
This qualitative study consisted of semi-structured interviews with patients who had received ketamine treatment for depression. Interview data were analysed thematically.
Participants
Fourteen patients (8 females, 6 males, aged 24–64 years) who had received treatment with ketamine for treatment-resistant depression, and had SI at the initiation of treatment. Two participants also had a diagnosis of bipolar type 1 and two of emotionally unstable personality disorder. Eight had a history of self-harm.
Results
SI reduced following ketamine treatment in 12 out of 14 participants for periods of a few hours following a single treatment to up to three years with ongoing treatment. Reduction of SI was variable in terms of extent and duration, and re-emergence of suicidal thoughts often occurred when treatment ceased. Participants’ accounts indicated that reduced SI was associated with improved mood and reduced anxiety, as were clarity of thought, focus and concentration, and ability to function. Participants reported experiencing some or all of these effects in various orders of occurrence.
Conclusion
Generally, ketamine treatment was experienced as effective in reducing SI, although duration of effects varied considerably. Patients’ perspectives indicated similarities in the mechanisms of reduction in SI, but some differences in their manifestation, particularly in relation to chronology. Experiences of this cohort suggest that reduced anxiety and improvement in ability to think and function were important mechanisms alongside, or in some cases independently of, improvement in mood. Further studies of patients’ experiences are required to gain enhanced understanding of the variability of effects of ketamine on SI and functionality.
Keywords: ketamine, suicidal ideation, treatment-resistant depression, mechanisms, self-harm
Strengths and limitations of this study.
This is one of the first studies of the impact of ketamine on suicidal ideation based on qualitative investigation of patients’ experiences.
Participants comprised a heterogeneous group in terms of gender, age, and number and routes of treatments with ketamine.
The study is limited by the relatively small number of participants.
Suicidal ideation was identified through a single item on a depression scale.
Some patients declined participation.
Introduction
Suicide is a major public health problem globally.1 It often occurs in the context of depression.2 3 While both pharmacological and psychological treatments can reduce depression and suicidality,4 there is an important group of individuals who have treatment-resistant depression in whom suicidal thinking is common and who have increased risk of a suicidal act.5 Ketamine has received increasing attention as a rapid-acting antidepressant, with studies suggesting that a single low-dose infusion has a beneficial although transitory effect for patients with depression, including treatment-resistant unipolar and bipolar depression.6–8 Multiple mechanisms have been described for the antidepressant action of ketamine: NMDA antagonism, reduced inhibitory interneuron GABAergic transmission, a glutamate surge, an AMPA-mediated increase in BDNF release and mTOR-dependent neuroplasticity.9 In terms of beneficial effects of ketamine on suicidality there are several potential pathways, but the effects on the glutaminergic system may predominate.10
There is accumulating evidence from clinical and randomised controlled trials (RCTs) that ketamine can reduce suicidal ideation (SI), at least in the short term.11–13 However, there is uncertainty as to the mechanisms which might underlie this effect.14 Reduction in SI mediated by improvement in overall depressive symptoms may be one factor,15 but it also seems that improvements can occur independently from changes in mood.16–18
As far as we are aware, research to date has not examined patient views regarding the impact of ketamine treatment on SI or sought to understand how patients think that ketamine has reduced their SI. The aim of this qualitative study was to explore patients' perspectives on the impact of ketamine treatment on SI in the context of treatment-resistant depression, including perceived benefits and how these might occur.
Method
Participants
Inclusion criteria consisted of a diagnosis of unipolar or bipolar treatment-resistant depression, age 18 years or over, English speaking and SI at commencement of ketamine treatment. All participants had received ketamine treatment within the past year apart from one who had last received it 22 months prior to interview. SI was assessed by a score of 1 or above on the SI question of the Beck Depression Inventory (BDI).19 Exclusion criteria were a lack of mental capacity, significant impairment of intellectual functioning and lack of fluency in spoken English. Participants were in receipt of a range of other antidepressant, anxiolytic, mood stabiliser and psychological treatments, which were not prescribed by the ketamine clinic.
Recruitment
All participants were recruited from a UK ketamine clinic. Standard treatment at this clinic is an initial three intravenous ketamine treatments (infusions) (0.5 mg/kg) followed by oral ketamine or a combination of oral and intravenous treatments as needed.
Forty eligible participants were approached by the ketamine clinic staff (HT and RM) by email or in person at the clinic. Participant information sheets were provided and interested individuals were referred to the researcher (KL), who then provided further information before undergoing the informed consent process (see the online supplementary appendix for further information in the completed Consolidated Criteria for Reporting Qualitative Research Checklist). Patients approached included both those who had responded positively to ketamine treatment and patients who had not experienced any tangible benefit or who had stopped treatment due to side effects.
bmjopen-2019-029108supp001.pdf (57.6KB, pdf)
Data collection
Data collection was through one-to-one semistructured interviews carried out by the researcher (KL) at the hospital site where the ketamine clinic is based. All interviews were carried out face to face, although two longer interviews were carried out in two parts, with the second parts by phone or Skype. Topics included history of depression and suicidality, the circumstances under which participants started ketamine treatment, their experiences of treatment and perspectives on impact of ketamine on mood and SI. In addition, participants were asked to complete the BDI before the interview commenced (only the pretreatment score was used to determine eligibility). They also completed benefits and side effects checklists during the interview to gather structured information about frequency and duration of effects.
The length of interviews ranged from 1 to 2.5 hours. All interviews were tape recorded. Participants were advised that they could withdraw from the study at any time and provided with information about sources of support in case they became distressed following the interview.
Analysis
Interview data were transcribed verbatim and participants were given the opportunity to review their anonymised transcripts. Six participants took up this opportunity but none suggested changes. Thematic analysis was carried out to report participants’ experiences, meanings and realities using an inductive and semantic approach, following the six stages of analysis recommended by Braun and Clarke20: (1) becoming familiar with the data; (2) generating initial codes; (3) searching for themes; (4) reviewing themes; (5) defining and naming themes; and (6) write-up. Final identification of themes was based on consensus discussion between two researchers (KL and FB), and was supported by NVivo software (V.11 QSR 2008). Main themes and subthemes were first identified in relation to separate participants, and then across the whole sample. The qualitative analysis was supervised by LM.
Patient and public involvement
A former patient of the ketamine clinic was involved in reviewing and providing feedback on the interview schedule and participant information literature prior to submission to the local research ethics committee.
Results
Participants
In total, 40 current and past patients were approached (21 females and 19 males). Eighteen individuals expressed initial interest in the study and 14 (35%, 8 females and 6 males) went on to participate. Of the 4/18 patients who did not go on to take part, three did not respond to invitations to meet with the researcher and one withdrew before the informed consent process. One of the final 14 participants had stopped treatment 16 months prior to commencement of the study (22 months prior to interview) due to non-response but was included in the sample to ensure a range of perspectives. Participants were predominantly White British (13/14), with one classed as White Other. Ages ranged from 24 to 64 years, with a median age of 41 years. Most (11) participants lived with others (spouses, partners, parents, house share, student accommodation), with three living alone. Six participants were registered as sick or disabled at the time of their interviews.
All 14 participants met criteria for treatment-resistant depression.5 Two had a primary diagnosis of bipolar affective disorder type 1, two a diagnosis of emotionally unstable personality disorder and the remaining 10 a primary diagnosis of depression. BDI scores for the SI question at the start of ketamine treatment and at interview are shown in table 1.
Table 1.
Characteristics of the participants (n=14)
| Characteristics | n=14 |
| Gender (male/female) | 6/8 |
| Age (years) | 24–64; median 41 |
| Past self-harm | 8 |
| Family history of self-harm or suicide | 4 |
| BDI suicidal ideation score* | |
| At commencement of treatment | 1 n=7 2 n=5 3 n=2 |
| At interview | 0 n=6 1 n=4 2 n=3 3 n=1 |
*= 0=No thoughts of killing self; 1=Thoughts of killing self, but would not carry them out; 2=Would like to kill self; 3=Would kill self if had the chance
BDI, Beck Depression Inventory.
Ketamine treatment
Ten participants were engaged in ongoing ketamine treatment at the time of interview. Of the remaining four, one had received ketamine a month prior to interview, two 9 months before and one 22 months prior to interview. Reasons for cessation of treatment were non-response (n=1), treatment becoming ineffective over time (n=1), severe side effects (n=1) and a lack of supply of oral ketamine (n=1).
There was considerable variation in the length of time participants were involved in treatment. Two individuals received between one and three infusions over a few weeks, five had between 6 and 88 infusions and up to 199 oral doses over a year or more (19 months to 6 years, three consistently and two periodically). The length of treatment and number of doses for the remaining seven was somewhere between these points (3–6 infusions and up to 46 oral doses over 4–9 months).
Impact of ketamine on SI
Twelve participants reported a reduction in SI at some stage following ketamine treatment. The onset and duration of this effect varied; onset ranged from immediate to a day or more after treatment, and duration from less than 24 hours to 3 years with ongoing treatment (table 2). One patient who reported a reduction in SI had treatment stopped after one infusion due to adverse side effects (see below). Of the two participants who did not report a reduction in SI, one did not experience any noticeable benefit from ketamine at all apart from a mild and transient improvement in mood; the other experienced improved energy levels and cognitive function but only rarely any improvement in mood.
Table 2.
Impact of ketamine on suicidal ideation (SI) in those patients who experienced benefit (n=12)
| Onset of reduced SI | n=12 |
| Immediate/during treatment | 2 |
| Within an hour of treatment | 5 |
| A few hours after treatment | 2 |
| A day or more after treatment | 3 |
| Duration of reduced SI | |
| 0–24 hours | 2 |
| Several days | 4 (3–6 days) |
| A week or more | 0 |
| A month or more | 1 |
| Ongoing | 5 |
Four participants experienced sustained elimination of SI on both intravenous and oral ketamine.
And the strongest thing that’s come out of the ketamine is that it doesn’t matter how down I’ve got, after maybe the first one, maybe two, the idea of suicide is not there. (P3)
Two of these four participants (three of whom were receiving ketamine at the time of interview) noticed a return of SI during periods they were without treatment (between intravenous and oral treatment, or when they ran out of oral treatment), although stated that the ideation was less intense.
[SI returned] Only when I’ve been off it for two months…. but not quite as bad as I’ve experienced it before… the fact that the thought had flashed into my mind at all was like, ah and now it’s time to get in contact. (P6)
Three participants experienced an elimination of SI following intravenous treatment, which lasted from 6 hours to 9 months (6 hours; 6–8 days; 3–9 months). One of these participants had only ever received intravenous ketamine; the others had received both intravenous and oral treatment but experienced elimination of SI only with intravenous administration, although they reported a reduced intensity of SI on oral ketamine.
I thought if it doesn’t work, on the way back, because we were staying in a hotel, and I was going to kill myself there… I actually went and had dinner with my dad in the hotel room on the way back, which I’ve never done before. Usually I wouldn’t be up to doing that mood wise. And I was able to eat and enjoy the food… [The oral] never had the impact of reducing the suicidal thoughts to the extent that the infusion did…. on the infusion they disappeared. (P8)
A further participant had only one full intravenous treatment before stopping due to side effects (exacerbated hallucinations and intrusive unpleasant and paranoid thoughts), but reported a period of a few hours of relief from persistent SI on the third day after the first treatment, which they attributed to the ketamine.
A reduction in SI was reported by six participants, which manifested as a reduction in intensity rather than frequency, with content unchanged.
The intensity of the thought is definitely reduced…I can cope with the frequency, lots of them at a small level, I’m so used to them that it doesn’t bother me. But if I get lots at a high intensity, this is when things start to break down. So reducing the intensity is the first step for me. (P2)
The intravenous ketamine treatment was experienced as considerably stronger and, for most participants, more effective than oral treatment in reducing SI, although eight of the nine individuals who had oral treatment did report some benefit from it.
The oral dose, I suppose is stopping me from doing a suicide attempt even though I still have those suicidal feelings …it lessened the intensity of them so I would think I’ll hold on for a bit longer and see what, thinking more of other people. (P8)
Notwithstanding the greater effect of intravenous ketamine, one participant preferred the regime of having the more regular, although lower, doses permitted by taking ketamine orally. Another favoured oral treatment because, although it did not eradicate SI as the intravenous treatment did, there was not such a significant drop in mood when the effects wore off and improved functionality was more sustained.
Dissociative and euphoric effects
Dissociative effects during ketamine treatment were experienced some or all of the time by the 12 participants who reported a positive impact on SI (and also by the two participants who did not experience reduced SI). For one participant, who went on to stop treatment due to side effects, this was experienced as malevolent hallucinations and an acute increase in pre-existing intrusive and disturbing thoughts and mental images. These effects continued for 2 days after treatment and the participant reported a sustained worsening of the pre-existing thoughts and images even at the point of interview. Dissociative effects were more common and stronger with intravenous treatment and one participant reported no dissociative effects at all with oral treatment. To describe the difference one participant likened the oral ketamine to drinking a glass of wine and the intravenous to consuming a bottle of vodka.
Participants were not asked specifically if they thought the reduction in their SI was linked to the dissociative effects they experienced. However, when asked if they had discovered ways of maximising the overall benefit of ketamine, five participants said they would take oral ketamine on an empty stomach to achieve a stronger sense of dissociation and derive more benefit, suggesting they believed there was such a link, although two participants noted that in practice this was not always the case.
Sometimes I won’t get as much of a kick from taking it, almost not notice … and I’m like did I get any? … and then the next week will be fine. Sometimes I’d get a really powerful thing and the next week felt down, so there was definitely some stuff going on there that was beyond my ability to make sense of. (P6)
One participant reported getting the giggles and feeling like a ‘happy drunk’ during intravenous ketamine treatment and two others described clear euphoric effects.
It was like a weight had been lifted off my shoulders. It was like I’d let go of a big weight, like a heavy weight had shifted from me. It was absolutely amazing. (P1)
These three participants all experienced an eradication of SI following ketamine infusions. For two this was transitory and for one it was longer lasting (for some months following a course of four infusions).
Other side effects
All participants experienced some side effects, including the effects during ketamine administration, ranging from rarely to always (the most frequently reported of which were feeling strange or unreal (n=14), abnormal sensations such as seeing or hearing unusual things (n=11), tiredness (n=11), blurred vision (n=8) and headaches (n=7)). One participant reported severe side effects resulting in cessation of treatment (see above). For the rest of the participants (n=13), however, side effects were not considered major and six explicitly stated that the side effects they experienced from ketamine were much less severe than those they had experienced with conventional antidepressants. No participant described an association between side effects and impact of ketamine on SI, nor did any individual require prescribed medication to address side effects.
Perceived mechanisms contributing to reduced SI
Participants rated the frequency with which they experienced benefits following ketamine treatment using a structured checklist (table 3). Of the 12 participants whose SI was reduced by ketamine, five reported that they always experienced a reduction in SI following treatment, although improved mood, reduced anxiety and increased energy were experienced less regularly. This suggests that in some cases SI was reduced independently of mood and anxiety.
Table 3.
Participants’ responses regarding specific impacts of ketamine
| Participants with reduced suicidal ideation (n=12) | Participants with no reduction in suicidal ideation (n=2) | |
| Ketamine reduced suicidal ideation | ||
| Always | 5* | |
| Often | 5 | |
| Sometimes | 2 | |
| Never | 2 | |
| Ketamine improved mood | ||
| Always | 3* | 1 |
| Often | 7 | |
| Sometimes | 2 | 1 |
| Ketamine reduced anxiety | ||
| Always | 2* | |
| Often | 8 | 1 |
| Sometimes | 1 | |
| Rarely | 1 | |
| Never | 1 | |
| Ketamine increased energy levels | ||
| Always | 2 | |
| Often | 5 | 1 |
| Sometimes | 5* | |
| Rarely | 1 | |
*One of these participants had only one full intravenous treatment due to severe side effects.
I think it’s separate [from mood]. Because there’s still days where I feel very low and normally the suicide thing would be at the back of my head or be there, but it, without any thought process, it’s gone, and I can’t reason that one. (P3)
Themes derived from participants’ narratives reflect the checklist findings and indicate that while improved mood and reduced anxiety were both associated with a reduction in SI, clarity of thought, improved focus and concentration, and improved ability to function were additional factors involved in the alleviation of SI (figure 1; table 4). These perceptions were consistent across the sample, and accounts of individuals with diagnoses of bipolar disorder or emotionally unstable personality disorder did not appear to differ from those of participants with a primary diagnosis of depression.
Figure 1.
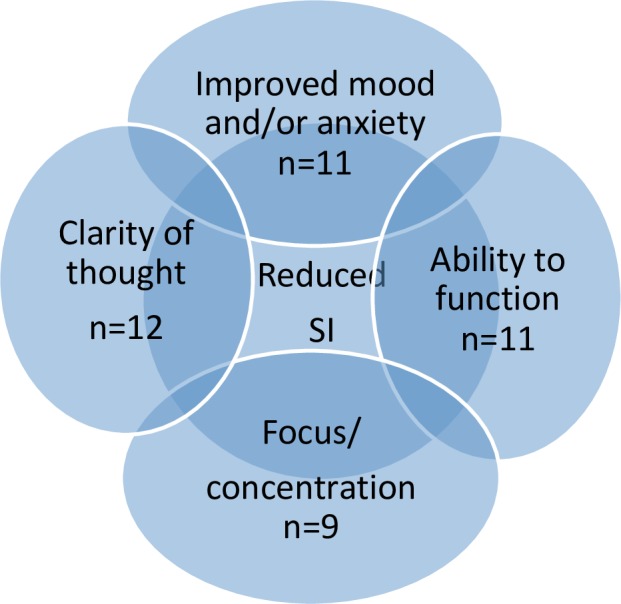
Participants’ perspectives of mechanisms associated with reduced suicidal ideation (SI) (n=12).
Table 4.
Key themes, subthemes and perceived impact of subthemes
| Main themes | Subthemes | Perceived subthemes |
| 1. Clarity of thought | Reduced intrusive thoughts Relief from slowed thoughts Reaching new understandings |
Getting a break |
| 2. Focus and concentration | Able to make decisions Motivation and energy |
Choosing not to act on SI Able to let go Seeing other options |
| 3. Ability to function | Activities of daily living Socialisation |
Doing normal stuff Improved connection with others |
SI, suicidal ideation.
Participants reported similar perceptions of the mechanisms involved in reduction of SI but some differences in experiences of order of occurrence. Most (n=8) perceived that an improvement in mood resulted in reduced SI, but for others the improvement in mood was itself a result of improved clarity of thought and the associated ability to focus.
I think it may be more ways, not necessarily my mood, maybe that I could have a gap in thinking without the thoughts coming in. So I could distract and therefore look at other things that could help my mood, which then I suppose reduces the suicidality, because when the mood goes really low I can’t concentrate on anything or think about other things. So basically, the ketamine helps to give you a different perspective at looking outwards and being interested in different things so I’m not being wound in constant thoughts. (P8)
Improved clarity of thought was experienced by some participants (n=7) as a reduction in intrusive thoughts or depressive ruminations. Such thoughts were negative and frequently suicidal in nature and described as ‘constant thoughts’, ‘tornado of thoughts’, ‘rapid fire thoughts’, ‘head swimming’ and ‘ruminations’.
The day after [ketamine treatment] I maybe have more clarity of thought. I think instead of maybe being so locked into the pattern of kind of cyclical thinking and rumination, I think it does maybe break that up a bit and maybe make you a bit more open to possibilities (P4)
Other participants (n=3) described a process of making sense of thoughts and reaching new understandings or gaining new perspectives. Two of these participants used the same metaphor (‘it’s like rinsing my brain out’, ‘it’s like having your brain jet washed’) to describe this experience. The remaining two participants experienced a relief from slowed thinking and used the same descriptors for their state before treatment with ketamine (‘nothingness’, ‘this blank nothing’) and the metaphor of ‘the fog lifting’ to describe how they felt ketamine enabled clarity of thought.
Ketamine’s positive effect on anxiety was noticed by most participants who experienced a reduction in SI (n=11/12). Some put this down to the reduction in intrusive negative and suicidal thoughts whereas others described a general reduction in anxiety that was associated with improved ability to focus, which in turn prevented intrusive thoughts.
It’s linked with the focus right, so if you’re focused on your task or what’s in front of you at the time, there’s no place for neurotic and other thoughts to kick in and actually then lead you to suicidal thoughts. (P12)
Clarity of thought and the ability to focus along with increased energy levels were linked to improved functionality in relation to activities of daily living and socialisation.
By the thoughts being slowed down you automatically gain more control because you can isolate them…everything seems more manageable at a slower pace… the mood is able to go up and the suicidal thinking comes down… It means I can do things. I can get out of bed. I can take my kids to school. I can have a shower… (P2)
Although participants were not specifically prompted about hopelessness, some accounts suggested that this reduced somewhat as mood improved and the treatment was experienced as being effective, for example:
I think it’s because my mood improved and I had a reason to keep going. There wasn’t this black hole that was always going to be there. And, you know, as soon as somebody says ‘well you’re drug resistant to this’ you do, you go oh, bloody hell. So that’s it. (P7)
Self-harm
Two of the 14 study participants had self-harmed while undergoing ketamine treatment. One of these reported an overall reduction in intensity of SI. A third participant, who had ketamine periodically over some years, had episodes of self-harm when in a mental health crisis, while not receiving ketamine, which led to further courses of ketamine treatment. A fourth participant had self-harmed since cessation of ketamine treatment (due to side effects). All of these participants had a history of self-harm prior to commencement of ketamine treatment.
Discussion
In this study we explored patients’ accounts of the impact of ketamine treatment on their suicidal thinking and perspectives of the associated mechanisms. Treatment with ketamine was reported as reducing SI in 12 out of 14 participants. However, the intensity and duration of effects on SI varied greatly. In most clinical trials which have shown an impact of a single treatment with ketamine on SI, this effect has not usually persisted beyond 72 hours,13 21 22 although has had longer effects in some patients. In the present study, some participants who reported benefits in terms of reduced SI identified a relatively long duration of effect. Grunebaum et al12 found an effect on SI up to 6 weeks following a single infusion of ketamine.12 Also, in our study all but one individual had received multiple ketamine treatments. Some of these reported that beneficial effects on SI persisted with continuation of treatment, but that this effect was lost if treatment was discontinued.
Differences between individual experiences of impact of ketamine on suicidality have been noted by other authors, such as Ballard et al18 who found that those least likely to have reduced SI following ketamine were those with the most severe SI and a history of self-injury.18 Of the eight participants in our study who scored 2 or above in the BDI SI question, six had a history of self-harm. Five of these reported a beneficial impact on SI; one complete elimination, two elimination with ketamine infusion and reduction with oral treatment and two an overall reduction. These findings indicate that most participants who had stronger SI and a history of self-harm experienced a reduction in SI following ketamine treatment. The rest of the participants (n=6) had less severe SI and fewer (n=2) had a history of self-harm. However, responses of this group were similar to the group with higher SI; one reported no response; two reduced SI; and three elimination of SI.
One possibility for optimising improvement in thought processes and functionality experienced following ketamine treatment, and hence longer term benefits for both depression and SI, could be additional use of intensive psychological therapy. Some participants in this study spontaneously mentioned the need for psychological treatment and the fact that ketamine made them feel more amenable to therapy or more able to use skills learnt in previous therapy. Repeated treatment with ketamine, as was the case for several participants in this study, is another approach.
Previous research has indicated that a single dose of ketamine has a short-term positive effect on hopelessness as well as SI.23 24 In our study some participants’ accounts suggested that reduced hopelessness was experienced alongside or subsequent to improvement in mood and due to the relief of finding a treatment that was more effective than those previously tried. However, hopelessness was not systematically explored in this study.
Potential mechanisms of impact of ketamine on SI
Participants’ accounts indicated that they regarded the beneficial effects of ketamine on SI to be partly related to improvements in depression and anxiety. However, some also related the impact on SI to improved clarity of thinking and functionality. This is in keeping with findings from other studies that improvements in SI following a single treatment with ketamine can occur partly independently of improvements in mood, with improvement in depression explaining about 50% of the improvement in SI.12 13 Grunebaum et al12 found that reduced SI largely continued up to 6 weeks after infusion and explained that this is likely to be partly due to concomitant treatment with other psychotropic medication, although the participants were not necessarily suffering from treatment-resistant depression.12
Research implications
The variety of responses found in this study and other investigations indicate that measures of impact should be monitored frequently in trials assessing the impact of ketamine on SI and behaviour. Further work is needed to try to identify likely responders. This will be particularly important should ketamine be used for management of SI in emergency situations. Our findings, and those of others,12 18 suggest that there should be more focus on investigating the mechanisms involved in beneficial effects of ketamine on SI. We would encourage deployment of mixed-methods studies, including nested qualitative studies within RCTs, for this purpose and for obtaining a more nuanced appraisal of the effects of ketamine than may be possible by only using scales to assess impact.
Strengths and limitations
We are unaware of previous qualitative studies of the experiences of depressed patients with suicidal ideas receiving treatment with ketamine. The approach we have used encourages a real-world appraisal of the impact of ketamine and allows highlighting of individual patients’ experiences. However, there are limitations, especially in terms of the small sample size and the potential lack of generalisability associated with the qualitative methodology. In addition, participants who responded to invitations to participate were self-selected and there may be some bias in terms of those agreeing to participate perhaps having experienced a more positive impact on their SI than those who declined. The inclusion criteria included a positive score on a single item on a mood scale, the Beck Depression Inventory. Differences in response to ketamine in terms of SI have been found when different measures of SI have been used.13 The participants all attended a single clinic, which may also influence the generalisability of the findings. Furthermore, the interviews were conducted retrospectively and at varying times following initiation of treatment, with some participants still receiving ketamine and others having ceased treatment.
Conclusions
This study of patients’ experiences of treatment with ketamine has indicated variable responses in terms of changes in SI, both in intensity and duration of benefits. The patients’ perceptions of mechanisms involved in a reduction of SI suggest that improvements in depression and anxiety are just part of the effect, with improved clarity of thinking and functionality also being important. Further studies of patients’ experiences are warranted, especially in terms of understanding variability of effects of ketamine on suicidality, including hopelessness and actual suicidal behaviour, and how benefits of the medication might interact with activities of daily living and other treatments, including possible psychological therapy. Such work should add to knowledge about the suitability of use of ketamine to treat suicidality, especially in potential emergency situations. In addition, while we cannot comment on the effect of ketamine on repeat self-harm of people with emotionally unstable personality disorder, given that individuals with this diagnosis are in receipt of ketamine treatment such study would be judicious.
Supplementary Material
Acknowledgments
The authors thank Suzanne Pullin and Charlie Pullin for their funding, Chris Dammers for his contribution to the research design and the staff of the Ketamine Clinic at Oxford Health NHS Foundation Trust for their support of the research.
Footnotes
Contributors: LM, KH and KL designed the study, with the assistance of HT and RM, who both helped recruit the participants. KL collected the data. KL and FB transcribed and analysed the data. KL and KH wrote the first draft of the report. All authors revised the report and approved the final version. KH is an Emeritus National Institute for Health Research senior investigator.
Funding: This work was supported by the Jim Pullin Trust. RM is supported by the NIHR Oxford Health Biomedical Research Centre and Collaborations for Leadership in Applied Health Research and Care.
Competing interests: RM has received consulting fees from Janssen.
Patient consent for publication: Not required.
Ethics approval: The study was approved by the South Central Oxford A Research Ethics Committee and the Health Research Authority (Reference No 17/SC/0106).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1. World Health Organization Preventing suicide: a global imperative. World Health Organization, 2014. [Google Scholar]
- 2. Cavanagh JTO, Carson AJ, Sharpe M, et al. . Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395–405. 10.1017/S0033291702006943 [DOI] [PubMed] [Google Scholar]
- 3. Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatr Scand 2006;113:180–206. 10.1111/j.1600-0447.2005.00702.x [DOI] [PubMed] [Google Scholar]
- 4. Zalsman G, Hawton K, Wasserman D, et al. . Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 2016;3:646–59. 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- 5. Anderson IM. We all know what we mean by treatment-resistant depression – don't we? Br J Psychiatry 2018;212:259–61. 10.1192/bjp.2018.56 [DOI] [PubMed] [Google Scholar]
- 6. Caddy C, Amit BH, McCloud TL, et al. . Ketamine and other glutamate receptor modulators for depression in adults. Cochrane Database Syst Rev 2015;75 10.1002/14651858.CD011612.pub2 [DOI] [PubMed] [Google Scholar]
- 7. McCloud TL, Caddy C, Jochim J, et al. . Ketamine and other glutamate receptor modulators for depression in bipolar disorder in adults. Cochrane Database Syst Rev 2015;14 10.1002/14651858.CD011611.pub2 [DOI] [PubMed] [Google Scholar]
- 8. Katalinic N, Lai R, Somogyi A, et al. . Ketamine as a new treatment for depression: a review of its efficacy and adverse effects. Aust N Z J Psychiatry 2013;47:710–27. 10.1177/0004867413486842 [DOI] [PubMed] [Google Scholar]
- 9. Abdallah CG, Sanacora G, Duman RS, et al. . The neurobiology of depression, ketamine and rapid-acting antidepressants: is it glutamate inhibition or activation? Pharmacol Ther 2018;190:148–58. 10.1016/j.pharmthera.2018.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De Berardis D, Fornaro M, Valchera A, et al. . Eradicating suicide at its roots: preclinical bases and clinical evidence of the efficacy of ketamine in the treatment of suicidal behaviors. Int J Mol Sci 2018;19:2888 10.3390/ijms19102888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bartoli F, Riboldi I, Crocamo C, et al. . Ketamine as a rapid-acting agent for suicidal ideation: a meta-analysis. Neurosci Biobehav Rev 2017;77:232–6. 10.1016/j.neubiorev.2017.03.010 [DOI] [PubMed] [Google Scholar]
- 12. Grunebaum MF, Galfalvy HC, Choo T-H, et al. . Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. Am J Psychiatry 2018;175:327–35. 10.1176/appi.ajp.2017.17060647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wilkinson ST, Ballard ED, Bloch MH, et al. . The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. AJP 2018;175:150–8. 10.1176/appi.ajp.2017.17040472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Price RB, Mathew SJ. Does ketamine have anti-suicidal properties? current status and future directions. CNS Drugs 2015;29:181–8. 10.1007/s40263-015-0232-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Price RB, Iosifescu DV, Murrough JW, et al. . Effects of ketamine on explicit and implicit suicidal cognition: a randomized controlled trial in treatment-resistant depression. Depress Anxiety 2014;31:335–43. 10.1002/da.22253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Phillips JL, Norris S, Talbot J, et al. . Direct effect of ketamine on suicidal ideation independent of its effects on depressive symptoms. Eur Neuropsychopharmacol 2016;26 10.1016/S0924-977X(16)31473-0 [DOI] [Google Scholar]
- 17. Ballard ED, Wills K, Lally N, et al. . Anhedonia as a clinical correlate of suicidal thoughts in clinical ketamine trials. J Affect Disord 2017;218:195–200. 10.1016/j.jad.2017.04.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ballard ED, Yarrington JS, Farmer CA, et al. . Characterizing the course of suicidal ideation response to ketamine. J Affect Disord 2018;241:86–93. 10.1016/j.jad.2018.07.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Beck AT, Schuyler D, Herman I. Development of suicidal intent scales. in: the prediction of suicide. Philadelphia, PA: Charles Press, 1974: 45–56. [Google Scholar]
- 20. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 21. Xu Y, Hackett M, Carter G, et al. . Effects of low-dose and very low-dose ketamine among patients with major depression: a systematic review and meta-analysis. IJNPPY 2016;19 10.1093/ijnp/pyv124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Murrough JW, Iosifescu DV, Chang LC, et al. . Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. AJP 2013;170:1134–42. 10.1176/appi.ajp.2013.13030392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. DiazGranados N, Ibrahim LA, Brutsche NE, et al. . Rapid resolution of suicidal ideation after a single infusion of an N-methyl-D-aspartate antagonist in patients with treatment-resistant major depressive disorder. J Clin Psychiatry 2010;71:1605–11. 10.4088/JCP.09m05327blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Burger J, Capobianco M, Lovern R, et al. . A double-blinded, randomized, placebo-controlled Sub-Dissociative dose ketamine pilot study in the treatment of acute depression and suicidality in a military emergency department setting. Mil Med 2016;181:1195–9. 10.7205/MILMED-D-15-00431 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-029108supp001.pdf (57.6KB, pdf)


