Abstract
Background:
Physical inactivity is a leading risk factor for cardiovascular disease worldwide. Group sport participation offers a unique, engaging approach for delivering physical activity interventions, but its overall effect on cardiometabolic risk factors is unclear.
Objective:
To estimate the pooled effects of community-based, recreational-level group sports on cardiometabolic risk factors and fitness parameters among adults.
Methods and Results:
We systematically searched electronic databases for English articles reporting the effectiveness of recreational-level group sports, published between January 1, 1965 and January 17, 2017. We extracted baseline and end of intervention means for cardiometabolic and fitness parameters. Random- or fixed-effects meta-analyses were used to obtain pooled pre/post change in outcome means within intervention participants and between groups. From 2,491 screened titles, 23 publications were included (N=902, age [mean±SD] 46.6±11.7 yrs), comprised of 21 soccer and two rugby interventions. Intervention participants achieved larger improvements compared to control subjects in weight (−1.44 kg [−1.79, −1.08]), BMI (−0.88 kg/m2 [−1.73, −0.03]), waist circumference (−0.77 cm [−1.21, −0.33]), body fat % (−1.80% [−3.12, −0.49]), total cholesterol (−0.33 mmol/L [−0.53, −0.13]), LDL cholesterol (−0.35 mmol/L [−0.54, −0.15]), systolic blood pressure (BP) (−5.71 mmHg [−7.98, −3.44]), diastolic BP (−3.36 mmHg [−4.93, −1.78]), VO2 max (3.93 mL/min/kg [2.96, 4.91]), and RHR (−5.51 beats/min [−7.37, −3.66]). Most studies (n=16) were classified as high-quality, and we found no evidence of publication bias.
Conclusions:
We found significant cardiometabolic and fitness improvements following group sport participation, primarily recreational soccer. Findings suggest group sport interventions are promising strategies for reducing cardiometabolic risk in adults.
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide and physical inactivity is a highly-prevalent risk factor for CVD and over forty major non-communicable chronic diseases (NCDs)1–3. Although the general population recognizes the health benefits of physical activity, including prevention of NCDs4, population engagement in physical activity is suboptimal. In the U.S., only 52% of adults report meeting the aerobic physical activity (PA) guidelines while only 20% of adults report meeting both the aerobic and muscle-strengthening components of the guidelines5. Globally, 25% of adults are insufficiently active and as a risk factor, inactivity accounts for 6% to 10% of the global premature mortality from CVD, type 2 diabetes, colon, and breast cancer6, 7
Many obstacles exist for sustained PA participation including environmental and intrapersonal barriers such as low motivation to exercise individually or insufficient adherence to traditional lifestyle interventions8–10. Recreational group sports offers an alternative to individual sports or traditional exercise options by introducing a competitive aspect and a social component that can lead to increased PA motivation for participants of different ages, genders, and fitness levels8. A variety of training mechanisms integrated within group sports (sprinting, loading, various aerobic intensities) are associated with improvements in metabolic, cardiovascular, and musculoskeletal fitness11, 12. Such interventions may also have broad acceptability given the popularity of group sports and growing access to sports facilities. Coupled with the high adherence rates reported in previous studies, there is potential for considering group sports interventions as feasible cardiometabolic risk reduction strategies13, 14
Previous reviews evaluating group sport interventions have focused on specific components of physical fitness and a single sport15–17; however, no previous meta-analysis has comprehensively evaluated the effects of multiple recreational group sport interventions on a variety of cardiometabolic biomarkers and physical fitness components. Therefore, the objective of this systematic review and meta-analysis was to estimate the pooled effects of community-based, recreational-level group sports on cardiometabolic risk factors and fitness among adults.
Methods
Literature Search Strategy
This systematic review and meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines18 and is registered with the International Prospective Register of Systematic Reviews (PROSPERO, registration number: CRD42017055325). We systematically searched Pubmed, Embase, PsychInfo, CINAHL, and Web of Science electronic databases for English articles reporting on the effectiveness of recreational-level group sports, published between January 1, 1965 and January 17, 2017.
Group sports included in our search were based on the current list of Olympic team sports and were then cross-referenced with a PA compendium for a MET value >3.5, equivalent to moderate-intensity PA19, 20. Due to the novelty of the topic, general search terms were employed to capture as many articles by title as possible. Cardiovascular and cardiometabolic terms were searched in combination with “and” statements for each group sport (Appendix 1). Additionally, reference lists of included studies and relevant reviews were examined to further identify articles.
Study Selection
Two reviewers independently screened all titles, abstracts, and full texts. Eligible articles were those including adults (18 years or older) participating in a recreational level group sport intervention comparing pre-/post-intervention measurements of cardiometabolic outcomes. We included studies that used single-arm pre/post, randomized controlled trial, or quasi-experimental designs. Control groups consisted of participants with baseline PA levels similar to the intervention group and that continued their current lifestyle. Articles were excluded if participants were extensively treated for chronic conditions such as chemotherapy or dialysis in order to better understand the pooled effects of group sport interventions for primary and secondary prevention of cardiometabolic diseases. The kappa statistic based on initial screening of abstracts and full texts was 0.89, indicating excellent agreement21. Any discrepancies between reviewers were settled through discussion with a third reviewer.
Data Extraction and Outcomes
Two reviewers independently extracted data regarding participant demographic characteristics, study protocol, and cardiometabolic outcomes using a standardized form. Primary outcomes in this review were categorized into the following groups: 1) body composition: weight, body mass index (kg/m2), body fat percent, and waist circumference; 2) Lipid profile: total cholesterol, low density lipoproteins (LDL), high density lipoproteins (HDL), and triglycerides (TG); 3) blood pressure: systolic blood pressure (SBP) and diastolic blood pressure (DBP); 4) aerobic fitness indicators: maximal oxygen consumption (VO2 maximum) and resting heart rate (RHR), and 5) glucose homeostasis factors: fasting blood glucose (FBG), fasting insulin, homeostatic model assessment for insulin resistance (HOMA-IR), hemoglobin A1c (HbA1c). For each outcome, data was extracted from published reports for mean baseline and end of intervention values and calculated or extracted mean change. If an outcome was reported in multiple publications from the same population, the corresponding data was extracted only once. Study level data was also extracted including location of the intervention, study design, duration of the intervention, frequency of the intervention, and PA dose. Study quality was assessed using a scale proposed by Juni et al.22 and adapted to evaluate the translatability and methodological strength of controlled trials and lifestyle interventions with three criterion22,23. The first criterion in the Juni scale assessed the methods used to minimize bias and had to have used one of the following: an intention to treat analysis, an attrition rate ≤20%, or compared characteristics of completers and non-completers. The second criterion assessed aspects related to the translatability of the program. To meet high-quality standards for the second criterion, the study had to include four or more of the following: description of the program design process, description of the enrollment process, documentation of session attendance, reporting costs and/or resource inputs, documentation of training process or qualifications of intervention personnel, or description of qualitative feedback from participants. The third criterion assessed the presence of a control group that was randomized, matched, or an unmatched comparison. To qualify as a high-quality study (i.e. low risk of bias due to strong internal validity), each study had to meet two or more of the three criterion above.
Data synthesis and analysis
Random- or fixed-effects meta-analyses weighted by the inverse variance were conducted on all outcomes that were reported by three or more studies. We estimated the aggregate mean differences from baseline to end of intervention within intervention participants and between intervention and control groups for all outcomes. A difference in differences analysis was used for between-group comparisons that contrasted change from baseline to post-intervention between intervention and control participants.
We explored heterogeneity of effects across studies by computing I2, and random effects models were employed in cases where I2 >50%. For studies with significant heterogeneity (I2>75%), meta-regressions were used to explore whether participant- or intervention-level characteristics explained heterogeneity in treatment effects. We conducted subgroup meta-analyses stratified by participant sex, studies enrolling participants at high-risk of CVD (defined as studies that enrolled only participants with diagnosed hypertension or type 2 diabetes), and intervention duration (≤6 months). We conducted sensitivity analyses to estimate intervention effects according to study quality category. Finally, publication bias was assessed by visually examining funnel plots for symmetry.
Cochrane Review Manager Software (version 5.3; Copenhagen, Denmark) was used to calculate meta-analyses and SAS (Version 9.4, Cary, NC) to conduct multivariate meta-regression.
Results
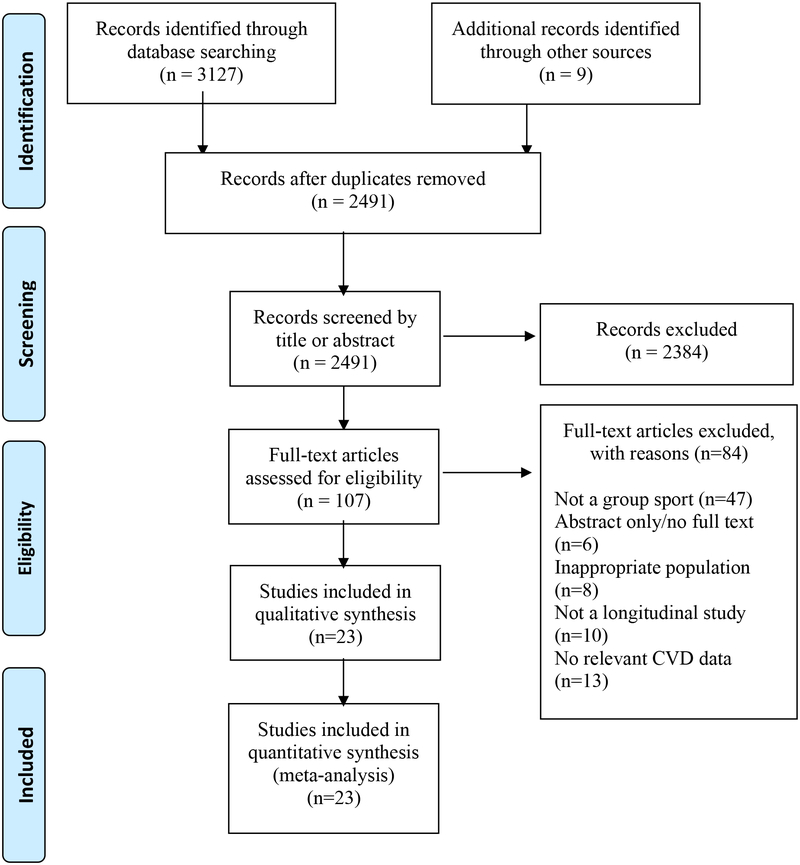
The electronic search identified 3,127 titles; nine additional articles were identified through reference lists. Of these, 107 full texts were screened and 23 studies met inclusion criteria for this review (Figure 1). The final studies included 902 participants with an average age of 46.6 years (SD=11.7 yrs; range, 30–69.1 years) and 55.4% male. Average intervention duration was 5.9 months (range, 2–16 months) and average PA dose was 133.8 minutes/week (range, 30–180 minutes/week). Of the 23 studies, 21 used soccer as the group sport intervention and two studies used rugby. The majority of the studies (87.0%) took place in Europe in a community setting (Table 1). Participant attrition rate ranged from 0% to 56% (average, 11%), the highest rate of attrition was reported in a study of homeless men participating in recreational soccer24.
Figure 1:
PRISMA flow chart for study selection.
Table 1.
Baseline characteristics and changes in cardiovascular related variables
| Study Authors | Population Mean age (yrs)/Sex/n | Intervention | Training Program Duration (months); Dose (mins/week) | Location (Country) |
|---|---|---|---|---|
| Andersen et al. 201026 | 46.7/ M/ 13 | Soccer | 3; 120 | Denmark |
| 47.8/ M/ 9 | Control | - | Denmark | |
| Andersen et al. 2014 – A25 | 45.8/ M/ 20 | Soccer | 6; 120 | Denmark |
| 46.9/ M/ 11 | Control | - | Denmark | |
| Andersen et al. 2014 – B31 | 50.6/ M/ 10 | Soccer | 6; 120 | Denmark |
| 48.7/ M/ 8 | Control | - | Denmark | |
| Andersen et al. 2014 – C33 | 68/ M/ 9 | Soccer | 4; 120 | Denmark |
| 69.1/ M/ 9 | Strength Training | 4; 120 | Denmark | |
| 67.4/ M/ 8 | Control | - | Denmark | |
| Andersen et al. 201634 | 68/ M/ 9 | Soccer | 12; 120–180 | Denmark |
| 69.1/ M/ 9 | Resistance Training | 12; 120–180 | Denmark | |
| 67.4/ M/ 8 | Control | - | Denmark | |
| Bangsbo et al. 201076 | 37/ M/ 21 | Soccer | 4; 120 | Denmark |
| 37/ M/ 18 | Running | 4; 120 | Denmark | |
| 33/M/ 12 | Control | - | Denmark | |
| Barene et al. 2014 – A35 | 44.1/ F/ 37 | Soccer | 3;120–180 | Norway |
| 45.9/ F/ 35 | Zumba | 3;120–180 | Norway | |
| 47.4/ F/ 35 | Control | - | Norway | |
| Barene et al. 2014 – B36 | 44.1/ F/37 | Soccer | 10; 60–120 | Norway |
| 45.9/ F/ 35 | Zumba | 10; 60–120 | Norway | |
| 47.4/ F/ 35 | Control | - | Norway | |
| Connolly et al. 201437 | 39/ F/ 13 | Soccer | 4; 30 | - |
| 40/ F/ 17 | Vibration Training | 4; 30 | - | |
| 40/ F/ 14 | Control | - | - | |
| de Sousa et al. 201432 | 61/ F-9 M-10 | Soccer + Dietary Counseling | 3; 120 | Brazil |
| 61/ F-10 M-5 | Dietary Counseling | 3; 120 | Brazil | |
| Filliau et al. 201477 | 44.4/ F-10 M-10 | Rugby | 3; 90 | France |
| Knoepfli-Lenzin et al. 201027 | 37/ M/ 15 | Soccer | 3; 180 | Switzerland |
| 36/M/ 15 | Running | 3; 180 | Switzerland | |
| 38/ M/ 17 | Control | - | Switzerland | |
| Krustrup et al. 200972 | 30/ M/ 12 | Soccer | 3; 180 | Denmark |
| 31/ M/10 | Running | 3; 180 | Denmark | |
| 30/ M/ 10 | Control | - | Denmark | |
| Krustrup et al. 2010 – A39 | 40/ F/ 7 | Soccer | 16;120 | Denmark |
| 40/ F/ 8 | Running | 16;120 | Denmark | |
| 38/ F/ 7 | Control | - | Denmark | |
| Krustrup et al. 2010 – B78 | 37/ F/21 | Soccer | 4; 120 | Denmark |
| 37/ F/ 17 | Running | 4; 120 | Denmark | |
| 33/ F/ 14 | Control | - | Denmark | |
| Krustrup et al. 201328 | 46/ M/ 22 | Soccer | 6; 120 | Denmark |
| 47/ M/ 11 | Control | - | Denmark | |
| Milancovic et al. 201541 | -/ M/ 20 | Soccer | 3; 180 | Serbia |
| -/ M/ 21 | Running | 3; 180 | Serbia | |
| -/ M/ 23 | Control | - | Serbia | |
| Mendham et al. 201540 | 46.8/ M/ 10 | Rugby | 2; 180 | Australia |
| 49.5/ M/ 11 | Cycling | 2; 180 | Australia | |
| 49.2/ M/ 11 | Control | - | Australia | |
| Mohr et al. 201429 | 45/ F/ 21 | Soccer | 3.75; 180 | - |
| 43/ F/ 20 | Control | - | - | |
| Randers et al. 201079 | 31/ M/10 | Soccer | 16;120 | Denmark |
| 32/ M/ 7 | Control | - | Denmark | |
| Randers et al. 201224 | 37/ M/ 22 | Soccer | 3; 180 | Denmark |
| 43/ M/ 10 | Control | - | Denmark | |
| Schmidt et al. 201330 | 50.6/ M/ 10 | Soccer | 6; 120 | Denmark |
| 48.7/ M/ 8 | Control | - | Denmark | |
| Schmidt et al. 201442 | 68/ M/ 9 | Soccer | 12;120–180 | Denmark |
| 69.1/ M/ 9 | Resistance Training | 12; 120–180 | Denmark | |
| 67.4/ M/ 8 | Control | - | Denmark | |
| Abbreviations: yrs-years - Denotes that data was not reported, not applicable, or insufficient to carry out analyses. Some studies included an additional intervention arm of an alternative exercise; these were not included in any pooled effect estimates. | ||||
| Study Authors | Weight (kg) | BMI (kg/m2) | WC (cm) | Body Fat (%) | LDL (mmol/L) | HDL (mmol/L) |
|---|---|---|---|---|---|---|
| Andersen et al. 201026 | −1.4 (4.3) | 0.1 (1.1) | 0 (0.4) | |||
| - | - | - | −0.1 (6.2) | 0.6 (0.9) | 0.1 (0.3) | |
| Andersen et al. 2014 – A25 | - | - | - | - | - | - |
| - | - | - | - | - | - | |
| Andersen et al. 2014 – B31 | −1.1 (13.4) | −0.3 (3.2) | - | −1.5 (3.6) | - | - |
| 0.5 (18) | 0.3 (6.5) | - | −0.2 (10.8) | - | - | |
| Andersen et al. 2014 – C33 | −1.1 (9.3) | −0.4 (3.6) | - | −1.1 (7.2) | −0.2 (0.8) | 0.1 (0.3) |
| −0.3 (11.8) | −0.1 (2.9) | - | −1.5 (6.6) | −0.1 (0.6) | 0.1 (0.3) | |
| −0.5 (12.1) | −0.2 (4.4) | - | −0.2 (5.1) | −0.2 (0.6) | 0 (0.3) | |
| Andersen et al. 201634 | −2.3 (9.3) | −0.8 (3.5) | - | −1.6 (7.1) | 0 (0.9) | 0.2 (0.3) |
| −0.2 (12) | −0.1 (2.9) | - | −1.2 (6.9) | 0.2 (0.6) | 0.3 (0.5) | |
| 1 (12) | 0.3 (4.5) | - | 0.4 (4.8) | 0.1 (0.7) | 0 (0.3) | |
| Bangsbo et al. 201076 | - | - | - | - | - | - |
| - | - | - | - | - | - | |
| - | - | - | - | - | - | |
| Barene et al. 2014 – A35 | 2 (0.3) | - | - | 2.2 (0.4) | - | - |
| 1.9 (0.3) | - | - | 2.3 (0.4) | - | - | |
| - | - | - | - | - | - | |
| Barene et al. 2014 – B36 | −1.1 (3.5) | - | - | −1.2 (2.8) | −0.1 (0.8) | 0 (0.3) |
| −2.1 (3.7) | - | - | −1.3 (2.9) | −0.2 (0.9) | 0 (0.3) | |
| - | - | - | - | - | - | |
| Connolly et al. 201437 | −0.6 (2.7) | - | - | −1.7 (2.4) | - | - |
| 0.2 (2.1) | - | - | 0.4 (1.8) | - | - | |
| 0 (2.1) | - | - | −0.2 (2) | - | - | |
| de Sousa et al. 201432 | 3.7 (0.6) | −1.4 (4.4) | −5.4 (0.9) | 2.4 (0.4) | −0.4 (0.2) | 0 (0.4) |
| 4.7 (0.7) | −1.8 (4.3) | −6.2 (0.4) | 2.4 (0.4) | 0.3 (1.2) | 0 (0.4) | |
| Filliau et al. 201477 | 0 (10.6) | - | - | 0 (7.4) | - | - |
| Knoepfli-Lenzin et al. 201027 | −1.6 (1.8) | - | −3.3 (8) | −2 (4.3) | −0.1 (1) | 0.1 (0.4) |
| −1.5 (2.1) | - | −1.3 (8.1) | −1.4 (4.2) | 0 (0.8) | 0 (0.4) | |
| −0.2 (13.4) | - | −0.4 (10.6) | 0.1 (7.2) | −0.1 (0.9) | 0.1 (0.4) | |
| Krustrup et al. 200972 | −1.1 (9.7) | −0.3 (2.8) | - | −2.9 (7.6) | −0.4 (0.6) | 0.1 (0.3) |
| −1 (17) | −0.3 (4.6) | - | −1.7 (5.2) | −0.1 (0.8) | 0.1 (0.3) | |
| 0 (11.8) | 0 (3.5) | - | −0.2 (8.7) | 0 (0.6) | 0 (0.3) | |
| Krustrup et al. 2010 - A39 | −0.5 (8.3) | −0.3 (3.3) | - | −1.7 (4.9) | - | - |
| −1.5 (7.5) | −0.7 (2.6) | - | −1.9 (7.2) | - | - | |
| −0.5 (11) | −0.2 (3.9) | - | −0.8 (6.9) | - | - | |
| Krustrup et al. 2010 - B78 | 0.3 (10.5) | 0.2 (4.1) | - | −2 (5.7) | −0.2 (0.8) | 0.1 (0.5) |
| 0.2 (7.4) | −1 (3.4) | - | −1.7 (6.8) | 0 (0.8) | 0.1 (0.4) | |
| −0.7 (9) | −0.2 (3.2) | - | −0.8 (6.2) | 0.1 (0.7) | 0.1 (0.4) | |
| Krustrup et al. 201328 | - | - | - | −2.2 (21.5) | −0.3 (0.8) | −0.1 (0.4) |
| - | - | - | −1 (21.1) | 0.3 (0.9) | 0.1 (0.3) | |
| Milancovic et al. 201541 | −5.8 (8.3) | −1.9 (2.2) | - | −4.7 (3) | - | - |
| −5.7 (5.4) | −1.8 (1.9) | - | −4.4 (2.9) | - | - | |
| 2.6 (12.3) | 0.8 (3) | - | −1.6 (4) | - | - | |
| Mendham et al. 201540 | −0.2 (13.5) | 0 (2.9) | −2.8 (7.1) | −1(3.1) | - | 0 (0.3) |
| −0.5 (12.4) | −0.2 (3.9) | −1.3 (8.9) | −0.8 (6.2) | - | 0 (0.3) | |
| 0.2 (11) | −0.1 (3.2) | −0.6 (8.6) | 1 (7) | - | 0 (0.5) | |
| Mohr et al. 201429 | −1.4 (0.5) | - | - | −2.1 (3.2) | - | - |
| 1 (1.4) | - | - | −0.5 (1.8) | - | - | |
| Randers et al. 201079 | −1.5 (7.1) | - | - | −3.8 (8.1) | −0.2 (0.6) | 0.1 (0.3) |
| 0.7 (18.2) | - | - | −0.6 (12.7) | 0.2 (1) | 0 (0.5) | |
| Randers et al. 201224 | −0.7 (16.6) | −0.3 (3.8) | - | −1.9 (8.6) | −0.4 (0.6) | 0 (0.4) |
| 0.6 (16.1) | 0.2 (4.2) | - | 0.1 (8) | −0.1 (0.8) | −0.1 (0.1) | |
| Schmidt et al. 201330 | −1.1 (14.7) | −0.4 (3.4) | - | - | −0.3 (0.9) | 0.1 (0.3) |
| 0.5 (19.1) | 0.3 (7) | - | - | 0.2 (1) | 0.1 (0.3) | |
| Schmidt et al. 201442 | - | - | - | - | - | - |
| - | - | - | - | - | - | |
| - | - | - | - | - | - | |
| Abbreviations: BMI- Body mass index, WC- waist circumference, LDL- low density lipoprotein, HDL:-high density lipoprotein | ||||||
| Study Authors | Total Cholesterol (mmol/L) | Triglycerides (mmol/L) | SBP (mm Hg) | DBP (mm Hg) | RHR (beats/min) | VO2 Max (mL/min/kg) |
|---|---|---|---|---|---|---|
| Andersen et al. 201026 | 0 (1.1) | −0.2 (0.7) | −12 (10.8) | −7 (3.6) | −12 (7.2) | 2.5 (5.3) |
| 0.5 (1.1) | −0.3 (1.2) | −5 (7.9) | −3 (6) | 1 (9) | −1.1 (5.7) | |
| Andersen et al. 2014 – A25 | - | - | - | - | −8 (12.5) | 8 (12.2) |
| - | - | - | - | −3 (4.5) | 2 (11.6) | |
| Andersen et al. 2014 – B31 | - | - | - | - | - | 3.6 (9.9) |
| - | - | - | - | - | 0.2 (7.1) | |
| Andersen et al. 2014 – C33 | −0.1 (1.1) | 0.1 (0.3) | - | - | - | 3.8 (6) |
| −0.3 (0.8) | 0.1 (0.3) | - | - | - | 0.8 (4.9) | |
| −0.3 (0.7) | 0.1 (0.5) | - | - | - | −0.7 (5.9) | |
| Andersen et al. 201634 | −0.5 (0.9) | 0 (0.3) | - | - | - | - |
| −0.5 (0.6) | 0.1 (0.5) | - | - | - | - | |
| −0.1 (0.8) | 0.2 (0.7) | - | - | - | - | |
| Bangsbo et al. 201076 | - | - | - | - | - | 5 (5) |
| - | - | - | - | - | 3.6 (5.7) | |
| - | - | - | - | - | - | |
| Barene et al. 2014 – A35 | - | - | 10.7 (1.8) | 7.8 (1.3) | - | 3.9 (0.6) |
| - | - | 10.6 (1.8) | 7.5 (1.3) | - | 3.8 (0.6) | |
| - | - | - | - | - | - | |
| Barene et al. 2014 – B36 | 0 (0.9) | 0 (0.6) | −0.3 (11.6) | 0.8 (8.2) | - | 1.1 (4) |
| −0.2 (0.9) | 0.1 (0.9) | −2.1 (11.5) | 0.6 (8) | - | 2.2 (3.9) | |
| - | - | - | - | - | - | |
| Connolly et al. 201437 | - | - | 2 (14.1) | 1 (10.5) | −4 (8) | - |
| - | - | −3 (15.4) | −1 (10.1) | −2 (11) | - | |
| - | - | 1 (16.5) | 0 (10.5) | −3 (7.9) | - | |
| de Sousa et al. 201432 | −0.6 (0.9) | −0.4 (0.4) | - | - | - | - |
| 0.4 (1.2) | 0.1 (1) | - | - | - | - | |
| Filliau et al. 201477 | - | - | −19 (20.4) | −7.5 (12) | −4.8 (10.4) | 2.3 (6.6) |
| Knoepfli-Lenzin et al. 201027 | −0.3 (1.1) | - | - | −9 (5) | −7 (10.6) | 4 (4.5) |
| −0.1 (0.9) | - | - | −4 (6) | −9 (6.2) | 5.5 (5) | |
| −0.2 (1.1) | - | - | - | −6 (8) | 0.4 (5.7) | |
| Krustrup et al. 200972 | −0.2 (0.7) | - | −8 (6.9) | −5 (6.9) | −6 (6) | 5 (4.7) |
| −0.3 (1.1) | - | −8 (11.4) | −2 (8.4) | −6 (6.3) | 2.9 (7.1) | |
| 0 (0.8) | - | −2 (8.4) | 2 (9.5) | 1 (9.5) | −0.3 (8.1) | |
| Krustrup et al. 2010 – A39 | - | - | −3 (11.5) | −3 (12.1) | −7 (7) | 4.8 (4.4) |
| - | - | −6 (10.2) | 0 (8.5) | −7 (7.5) | 4.5 (6.9) | |
| - | - | −6 (9.5) | −4 (7.9) | −1 (10.6) | 0.5 (4.9) | |
| Krustrup et al. 2010 – B78 | −0.1 (0.8) | −0.1 (0.5) | −7 (9.2) | −4 (9.2) | −5 (4.6) | - |
| −0.1 (0.7) | 0.1 (0.2) | −7 (8.2) | −3 (8.2) | −6 (8.2) | - | |
| 0.2 (0.7) | 0.1 (0.6) | −2 (7.5) | −2 (7.5) | 0 (7.5) | - | |
| Krustrup et al. 201328 | - | - | −13 (9) | 8 (6) | −8 (11) | 2.8 (2.9) |
| - | - | - | - | −3 (9) | −0.8 (1.8) | |
| Milancovic et al. 201541 | - | - | - | - | - | - |
| - | - | - | - | - | - | |
| - | - | - | - | - | - | |
| Mendham et al. 201540 | −0.2 (1) | 0.1 (0.7) | - | - | - | 4.2 (2.7) |
| −0.2 (0.8) | 0 (0.6) | - | - | - | 3.9 (3.8) | |
| 0 (0.9) | 0.2 (0.6) | - | - | - | −0.8 (5.3) | |
| Mohr et al. 201429 | −0.4 (0.5) | −0.2 (0.5) | −12 (13.7) | −6 (9.2) | −7 (9.2) | - |
| 0.1 (0.9) | 0.3 (0.9) | −1 (4.5) | 1 (8.9) | −3 (8.9) | - | |
| Randers et al. 201079 | 0 (0.6) | −0.2 (0.7) | −8 (6.3) | −3 (6.3) | −8 (8.4) | 3.1 (3.6) |
| 0.1 (1) | −0.4 (1.4) | −2 (7.3) | 3 (7.9) | 3 (7) | −0.9 (8.7) | |
| Randers et al. 201224 | −0.1 (1.3) | 0.1 (0.6) | 0 (11.5) | −2 (9) | 4 (9.5) | 3.9 (3.5) |
| 0.1 (1.2) | 0.1 (0.8) | 3 (14.8) | 1 (9.2) | 3 (13.5) | −0.3 (1.9) | |
| Schmidt et al. 201330 | −0.2 (0.9) | 0.3 (0.7) | −9 (15.5) | −8 (7) | −6 (8.7) | 3.6 (3.1) |
| 0.3 (1.2) | 0.3 (0.7) | 3 (16.4) | 0 (9.8) | 2 (19) | 0.5 (7.8) | |
| Schmidt et al. 201442 | - | - | - | - | −8 (9.2) | - |
| - | - | - | - | −2 (4.4) | - | |
| - | - | - | - | −2 (5.3) | - | |
| Abbreviations: TG-triglycerides, SBP-systolic blood pressure, DBP-diastolic blood pressure | ||||||
| Study Authors | Fasting Blood Glucose (mmol/L) | Fasting Insulin (umol/L) | HbAlc (%) | HOMA-IR |
|---|---|---|---|---|
| Andersen et al. 201026 | ||||
| - | - | - | - | |
| Andersen et al. 2014 – A25 | - | - | - | - |
| - | - | - | - | |
| Andersen et al. 2014 – B31 | −1 (2.1) | −6.7 (27.1) | −0.4 (0.9) | −0.9 (1.7) |
| 0.9 (2.3) | −1.3 (22.4) | 0 (1.1) | 0.8 (1.7) | |
| Andersen et al. 2014 – C33 | 0.1 (0.5) | −7 (13.1) | 0.1 (0.3) | −0.3 (0.5) |
| −0.1 (0.5) | −6 (15.9) | 0 (0.3) | −0.3 (0.8) | |
| 0.1 (0.6) | −8 (25.1) | 0.1 (0.3) | −0.3 (1.2) | |
| Andersen et al. 201634 | 0 (0.5) | −9 (13.1) | 0 (0.3) | −0.4 (0.5) |
| 0.1 (0.5) | −5 (16.7) | 0 (0.3) | −0.2 (0.8) | |
| 0.2 (0.5) | 0 (33.3) | 0 (0.3) | 0 (1.6) | |
| Bangsbo et al. 201076 | - | - | - | |
| - | - | - | - | |
| - | - | - | - | |
| Barene et al. 2014 – A35 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| Barene et al. 2014 – B36 | 0.1 (0.8) | - | - | - |
| −0.2 (1.4) | - | - | - | |
| - | - | - | - | |
| Connolly et al. 201437 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| de Sousa et al. 201432 | −0.4 (0.4) | −2.2 (7.3) | −1 (1.2) | −1.7 (2.7) |
| −0.4 (0.8) | −0.8 (8.3) | −0.8 (1) | −1.2 (3.1) | |
| Filliau et al. 201477 | - | - | - | - |
| Knoepfli-Lenzin et al. 201027 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| Krustrup et al. 200972 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| Krustrup et al. 2010 - A39 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| Krustrup et al. 2010 - B78 | 0 (0.8) | 2.2 (20.8) | - | - |
| −0.4 (0.8) | 2 (11.8) | - | - | |
| 0.1 (0.7) | 11.9 (17.6) | - | - | |
| Krustrup et al. 201328 | 0 (0.8) | −4 (37.2) | - | - |
| −0.3 (0.9) | 19 (58.9) | - | - | |
| Milancovic et al. 201541 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| Mendham et al. 201540 | −0.3 (0.6) | −15.3 (41.6) | −0.3 (0.4) | −0.6 (1.5) |
| −0.1 (0.7) | −4.9 (44.1) | −0.3 (0.6) | −0.1 (1.9) | |
| 0 (0.9) | 9 (52.7) | 0 (0.4) | 0.3 (2) | |
| Mohr et al. 201429 | - | - | - | - |
| - | - | - | - | |
| Randers et al. 201079 | −0.2 (0.5) | - | - | - |
| 0 (0.6) | - | - | - | |
| Randers et al. 201224 | 0.1 (0.6) | 5 (25.2) | - | - |
| −0.2 (0.6) | 11 (30.3) | - | - | |
| Schmidt et al. 201330 | - | - | −0.4 (1.2) | - |
| - | - | 0 (1.2) | - | |
| Schmidt et al. 201442 | - | - | - | - |
| - | - | - | - | |
| - | - | - | - | |
| Abbreviations: Hba1c-hemoglobin A1c, HOMA-IR-homeostatic model assessment for insulin resistance | ||||
Most control groups continued their current lifestyle with one control group receiving dietary advice. Twenty-two of the studies included at least one control group; 13 studies included an additional arm of an alternative intervention (i.e., running, strength training, cycling). Eight studies enrolled participants with high CVD risk: five studies enrolled hypertensive participants and three enrolled participants diagnosed with type 2 diabetes25–32.
Quality Assessment
Of the 23 studies included in the systematic review, 16 were classified as high quality24–29, 33–42 (Supplemental Table 1). These studies had a low attrition rate and included a control group. Furthermore, the studies had similar interventions characterized by aerobic sport activities and collected data at baseline and end of the intervention on a wide range of health outcomes using comparable measures. Based on these results, we deemed it appropriate to carry out a meta-analysis on reported cardiometabolic-related outcomes.
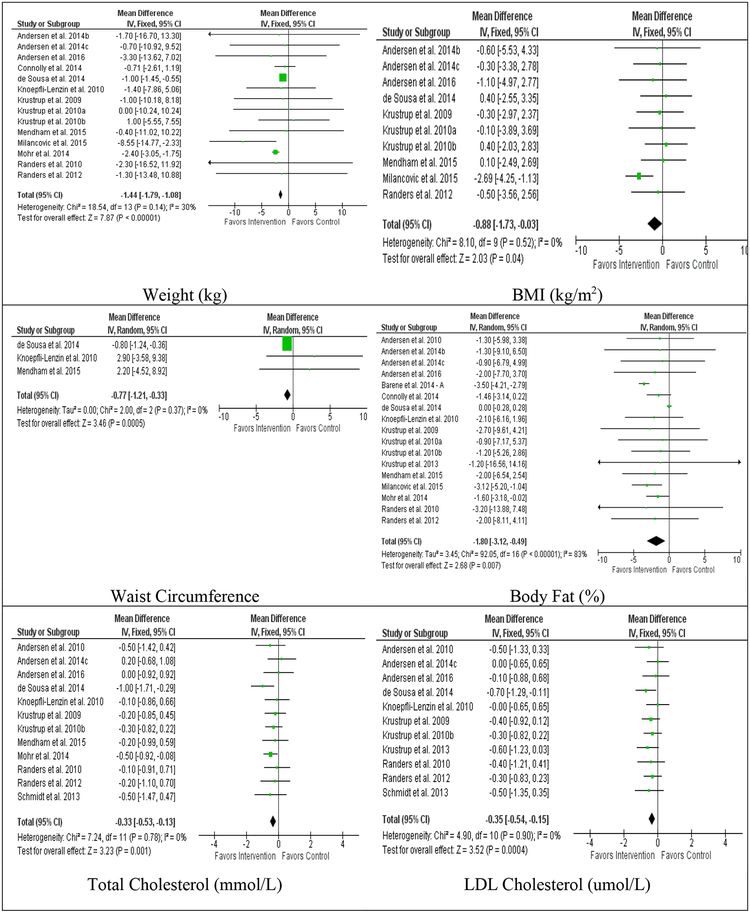
Body Composition
In 18 studies reporting weight change in intervention participants, there was a pooled reduction of 1.53 kg (−3.12, 0.06; I2=0%). In 14 controlled studies, intervention participants lost 1.44 kg more than the control participants (−1.79, −1.08; I2=30%) (Figure 2). In subgroup analyses of controlled studies, significant reductions in weight were also observed in the male-only studies, female-only studies, and studies with a duration ≤6 months (Table 2).
Figure 2:
Forest plots for between group comparisons of body composition and lipid outcomes
Table 2.
Sensitivity analyses for high quality studies and subgroup analysesa
| Outcome | High Quality | High Risk | Males-only |
|---|---|---|---|
| Weight (kg) | −1.64 (−2.14, −1.13)* | −0.83 (−3.79, 2.14) | −3.68 (−7.19, −0.18)* |
| BMI (kg/m2) | −1.36 (−2.43, −0.30)* | −1.32 (−2.33, −0.32)* | |
| Body Fat (%) | −1.88 (−2.77, −0.99)* | −0.06 (−0.33, 0.21) | −2.46 (−3.94, −0.98)* |
| WC (cm) | |||
| Total Cholesterol (mmol/L) | −0.29 (−0.56, −0.01)* | −0.53 (−0.83, −0.23)* | −0.18 (−0.47, 0.12) |
| LDL (mmol/L) | −0.30 (−0.57, −0.03)* | −0.47 (−0.78, −0.16)* | −0.34 (−0.58, −0.11)* |
| HDL (mmol/L) | 0.04 (−0.06, 0.14) | −0.06 (−0.18, 0.06) | 0.03 (−0.05, 0.12) |
| TG (mmol/L) | −0.22 (−0.47, 0.03) | −0.34 (−0.62, −0.05)* | −0.04 (−0.26, 0.18) |
| SBP (mm Hg) | −3.81 (−6.19, −1.42)* | −7.43 (−10.76, −4.11)* | −5.76 (−8.65, −2.88)* |
| DBP (mm HG) | −3.12 (−4.84, −1.40)* | −5.21 (−7.12, −3.31)* | −5.05 (−7.11, −2.98)* |
| VO2 Max (mL/min/kg) | 3.92 (2.93, 4.94)* | 3.65 (2.29, 5.02)* | 3.97 (2.92, 5.01)* |
| RHR (beats/min) | −5.01 (−7.28, −2.74)* | −5.29 (−8.11, −2.48)* | −7.59 (−10.22, −4.96)* |
| Fasting Blood Glucose (mmol/L) | 0.04 (−0.22, 0.29) | 0.03 (−0.32, 0.38) | −0.06 (−0.13, 0.01) |
| Fasting Insulin (umol/L) | −9.81 (−21.75, 2.14) | −1.99 (−7.13, 3.14) | −6.84 (−17.01, 3.33) |
| HbA1c (%) | −0.14 (−0.34, 0.07) | −0.30 (−0.82, 0.22) | −0.09 (−0.25, 0.08) |
| HOMA-IR | - | - | -0.50 (−1.10, 0.10) |
| *Indicates statistically significant finding (P<.05) a If an outcome was reported in <3 studies, a meta-analysis was not conducted (denoted by -); all effect estimates are presented as mean difference estimates and 95% confidence interval Abbreviations: BMI- Body mass index, WC- waist circumference, LDL- low density lipoprotein, HDL:-high density lipoprotein, SBP-systolic blood pressure, DBP-diastolic blood pressure, RHR-resting heart rate, Hba1c-hemoglobin A1c, HOMA-IR-homeostatic model assessment for insulin resistance | |||
| Outcome | Females-only | Duration (≤6 months) |
|---|---|---|
| Weight (kg) | −2.18 (−2.80, −1.57)* | −1.25 (−1.58, −0.92)* |
| BMI (kg/m2) | 0.23 (−1.74, 2.19) | −0.91 (−1.81, −0.02)* |
| Body Fat (%) | −1.49 (−2.57, −0.40)* | −1.80 (−3.20, −0.41)* |
| WC (cm) | ||
| Total Cholesterol (mmol/L) | −0.37 (−0.58, −0.15)* | |
| LDL (mmol/L) | −0.36 (−0.56, −0.15)* | |
| HDL (mmol/L) | 0.01 (−0.08, 0.09) | |
| TG (mmol/L) | −0.16 (−0.34, 0.01) | |
| SBP (mm Hg) | −5.36 (−8.98, −1.75)* | −6.10 (−8.58, −3.63)* |
| DBP (mm HG) | −2.89 (−6.18, 0.41) | −3.32 (−4.95, −1.69)* |
| VO2 Max (mL/min/kg) | 3.77 (2.77, 4.77)* | |
| RHR (beats/min) | −3.99 (−6.80, −1.18)* | −5.03 (−7.06, −2.99)* |
| Fasting Blood Glucose (mmol/L) | 0.04 (−0.17, 0.24) | |
| Fasting Insulin (umol/L) | −7.82 (−16.24, 0.59) | |
| HbA1c (%) | −0.14 (−0.34, 0.06) | |
| HOMA-IR | −0.53 (−1.19, 0.13) | |
| High-quality studies were determined based on adopted Juni22 score. High-risk populations were recognized as populations at high risk for developing CVD. Participants in these studies exclusively included participants with clinically diagnosed hypertension or type 2 diabetes. | ||
In 11 studies reporting BMI, intervention participants had a pooled change of −0.38 kg/m2 (−1.25, 0.48; I2=25%). BMI was reported in 10 controlled studies and intervention participants lost 0.88 kg/m2 more than control participants (−1.73, −0.03; I2=0%) (Figure 2). In subgroup analyses of controlled studies, male-only studies and studies with a duration ≤6 months had significant observed changes in BMI (Table 2).
In 19 studies reporting body fat percent measurements for intervention participants, there was a pooled change of −2.26% (−3.06, −1.46 I2=0%). In controlled studies (n=17), intervention participants had a 1.8% greater reduction in body fat percent than control subjects (−3.12, −0.49; I2=83%) (Figure 2). In subgroup analyses of controlled studies, male-only studies, female-only studies, and studies with a duration ≤6 months had significant observed reductions in body fat percent (Table 2). A multivariate meta-regression with participant baseline age, intervention duration, and percent of male participants did not explain heterogeneity of effects.
Waist circumference was reported in 3 controlled studies. Intervention participants achieved a pooled change of −3.78 cm (−7.29, −0.26; I2=0%) and lost 0.77 cm more than control participants (−1.21, −0.33; I2=0%) (Figure 2). Data was insufficient to conduct further analyses.
Lipids
In 13 studies reporting total cholesterol, a pooled change of 0.14 mmol/L (−0.31, 0.04; I2=0%) was observed in intervention participants. In 12 controlled studies reporting total cholesterol, intervention participants had a 0.33 mmol/L greater reduction than control participants (−0.53, −0.13; I2=0%) (Figure 2). In subgroup analyses of controlled studies, significant reductions were observed among studies enrolling participants at high-risk of CVD and studies with a duration ≤6 months (Table 2).
In 12 studies reporting LDL cholesterol measures among intervention participants, a pooled change of −0.23 mmol/L (−0.39, −0.08; I2=0%) was observed. In 11 controlled studies reporting LDL cholesterol outcomes, intervention participants decreased LDL cholesterol by0.35 mmol/L more than control participants (−0.54, −0.15; I2=0%) (Figure 2). In subgroup analyses of controlled studies, significant reductions were observed among male-only studies, studies enrolling participants at high-risk of CVD, and studies with a duration ≤6 months (Table 2).
In 13 studies reporting measures of HDL cholesterol in intervention participants, there was a pooled increase of 0.04 mmol/L (−0.02, 0.11, I2=0%). HDL cholesterol was reported in 12 controlled studies and no significant differences were observed in between group or subgroup analyses pooled estimates (Figure 2, Table 2).
In 13 studies reporting TG measures in intervention participants, there was a pooled decrease of −0.05 mmol/L (−0.16, 0.06, I2=0%). In 10 controlled studies reporting TG, intervention participants had a pooled change of −0.37 mmol/L (−0.74, 0.01; I2=0%) (Figure 2). In subgroup analyses of controlled studies, studies enrolling high-risk populations had significant observed reductions in TG (Table 2).
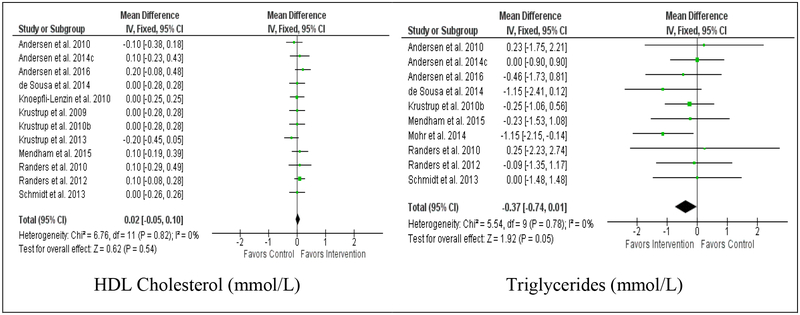
Blood Pressure
In 12 studies reporting SBP measures, intervention participants had a pooled change in SBP of −7.28 mm Hg (−9.29, −5.26; I2=56%). In controlled studies (n=10), intervention participants had a 5.71 mm Hg greater reduction than control participants (−7.98, −3.44; I2=0%) (Figure 3). All subgroup analyses of controlled studies showed significant reductions in SBP (Table 2).
Figure 3:
Forest plots for between group comparisons of blood pressure, fitness parameters, and glucose homeostasis indicators
In 13 studies reporting DBP measures, intervention participants had a pooled change of −3.6 mm Hg (−5.03, −2.17; I2=49%). In controlled studies (n=11), intervention participants reduced DBP 3.36 mm Hg more than control participants (−4.93, −1.78; I2=29%) (Figure 3). In subgroup analyses of controlled studies, male-only studies, studies enrolling participants at high-risk of CVD, and studies with a duration ≤6 months had significant observed reductions (Table 2).
Aerobic Fitness
In 16 studies reporting measures of VO2 maximum, there was a pooled increase of 3.43 mL/min/kg (2.63, 4.22; I2=0%) for intervention participants. In 11 controlled studies reporting VO2 maximum change, intervention participants increased VO2 maximum 3.93 mL/min/kg more than control participants (2.96, 4.91; I2=0%) (Figure 3). In subgroup analyses of controlled studies, improvements were similar and all analyses showed statistically significant improvements (Table 2).
In 15 studies reporting measures of RHR, there was a pooled change of −6.13 beats/min (−7.61, −4.65; I2=0%) for intervention participants. In controlled studies (n=13), intervention participants decreased RHR by 5.51 beats/min more than control participants (−7.37, −3.66; I2=0%) (Figure 3). All subgroup analyses of controlled studies showed significant reductions (Table 2).
Glucose Homeostasis Indicators
There were no statistically significant improvements in FBG, fasting insulin, or HbA1c% measures observed within intervention participants or between intervention and control participants (Figure 3, Table 2). In 5 studies reporting baseline to post-intervention measures of HOMA-IR, there was a pooled change of −0.43 (−0.72, −0.14; I2=0%) in intervention participants. No significant effects were observed in controlled studies or subgroup analyses (Figure 3, Table 2).
Sensitivity Analyses
In a sensitivity analysis of the 16 high-quality studies, effects were consistent (i.e., in the same direction) and generally greater than estimates obtained when including all studies (Table 2, Supplemental Table 1). Compared to overall between-group pooled estimates, high-quality studies had greater effects for weight (−1.64 kg, [−2.14, −1.13]), BMI (−1.36 kg/m2, [−2.43, −0.30]), and body fat percent (−1.88%, [−2.77, −0.99]). Estimates were smaller and remained statistically significant for SBP (−3.81 mm Hg [−6.19, −1.42]), DBP (−3.12 mm Hg [−4.84, −1.40]), total cholesterol (−0.29 mmol/L [−0.56, −0.01]), LDL cholesterol (−0.30 mmol/L [−0.57, −0.03]), RHR (−5.01 beats/min [−7.28, −2.74]), and VO2 maximum (3.92 mL/min/kg [2.93, 4.94]).
Discussion
To our knowledge, this is the first meta-analysis to comprehensively evaluate the effects of recreational, community-based group sport participation on cardiometabolic risk factors in adults. We found that group sport participation, primarily recreational soccer, was associated with broad reaching and clinically significant improvements in body composition, lipid profiles, blood pressure, and aerobic fitness. Overall, intervention participants reduced weight by 1.44 kg, BMI by 0.88 kg/m2, SBP by 5.71 mm Hg, DBP by 3.36 mm Hg, total cholesterol by 0.33 mmol/L, LDL cholesterol by 0.35 mmol/L, waist circumference by 0.77 cm, body fat percent by 1.80%, resting heart rate by 5.51 beats/min, and increased VO2 maximum by 3.93 mL/min/kg more than the control participants (Table 2).
Lifestyle interventions have been proven effective for primary and secondary prevention of NCDs such as type 2 diabetes and CVD43–46. Interventions that utilize a combination of diet, PA, and behavior change approaches often have stronger effects than interventions utilizing individual lifestyle components44, 45, 47 Despite this, our meta-analysis shows that PA-centric programs delivered using group sports are an effective lifestyle intervention to improve cardiometabolic-related outcomes and stronger effects may be seen if combined with dietary and behavioral interventions.
Body Composition
Our analyses revealed significant reductions in body weight, BMI, waist circumference, and body fat percentage in intervention compared to control participants. Male-only studies had an averaged observed weight change of −3.68 kg (−7.19, −0.18), which equated to a 4.6% body weight reduction from baseline. This is close to the American Diabetes Association recommendations for prevention/delay of diabetes and CVD48. Previous reviews have shown significant improvement in body composition in the absence of body weight loss following resistance training or high intensity interval training (HIIT)49, 50. The observed reductions in weight, waist circumference, and body fat percentage in this meta-analysis demonstrate that these interventions are an effective approach for reducing total weight and fat mass.
Lipids
We found significant improvements for total and LDL cholesterol in intervention participants compared to control participants. Previous findings show that greater exercise intensity is often needed to improve lipid profiles51, 52, indicating that participants were engaged in high intensity activity12. No significant improvements were observed for HDL cholesterol, which is known to respond variably to exercise and require a relatively large volume of PA to induce positive changes (over 1,500 kcal energy expenditure/week)53. Meta-analyses of exercise randomized controlled trials and lipid levels have reported similar changes in triglycerides but differing results for HDL, LDL and total cholesterol54, 55. Group sport interventions lead to more modest reductions in lipids compared to medications56–59; however, the observed reductions may be clinically meaningful, especially when considering the pleiotropic effect of PA on multiple cardiometabolic parameters and low number of negative side effects60.
Blood Pressure
Our results show significant improvements in SBP and DBP with group sport interventions. We found greater BP reductions in the high CVD risk population subgroup analysis, which is expected as hypertensive participants have greater potential for BP reduction compared to normotensive participants50. Greater BP reductions were found with group sport interventions compared to commonly used anti-hypertensive medications61, and the mean BP reductions observed in this meta-analysis are notable. Previous modelling has shown that BP reduction of this magnitude may reduce stroke risk by up to 20%46, 62.
Aerobic Fitness
Cardiorespiratory fitness, along with body fat percent, are known predictors of CVD and all-cause mortality63. We found significant improvements in VO2 max in each of the analyses conducted, showing group sport interventions are effective for increasing fitness in a variety of populations and are superior or comparable to traditional aerobic training11, 12. Other reviews have found recreational soccer was effective in improving VO2 maximum across populations of differing age, sex, and health status compared to strength training and no exercise15–17. Furthermore, recreational soccer produced greater improvements in VO2 max compared to endurance running and strength training15,17.
Glucose Homeostasis
Although all glucose homeostasis variables trended towards improvement, there were no significant reductions in FBG, fasting insulin, HbA1c, or HOMA-IR for the intervention participants compared to controls; however, there was a significant improvement in HOMA-IR among intervention participants from baseline to end of intervention. These findings may be due to the small samples sizes and limited of statistical power of several of the included trials in this review. There is strong evidence that PA participation fosters improvement in insulin sensitivity and non-insulin mediated glucose transport60. Meta-analyses focusing on mixed exercise regimens have found varied results45, 49, 55, 64 and changes in glucose homeostasis markers may vary depending on the population; however, there is biological plausibility that recreational group sports, similar to HIIT, positively impacts glucose homeostasis markers32, 65.
Group sport interventions constitute a unique way to engage participants and overcome barriers. Among intervention participants, average attrition rate was lower than traditional exercise interventions66. Furthermore, PA interventions compare favorably in terms of compliance and effectiveness for hard outcomes (mortality) versus drug interventions and have less adverse effects reported55, 57, 60, 66. The variety of training categories and movement patterns inherent to group sport participation (high-intensity runs, muscle loading, intense actions such as dribbles, shots, jumps and various aerobic intensity activities) result in broad-ranging physiological effects such as reduced insulin resistance, chronic inflammation, and arterial stiffness12, 32. Although heart rate often exceeds 80% of age-estimated maximum during recreational soccer participation irrespective of age, fitness status and previous training, participants report lower rates of perceived exertion compared to jogging, interval running, and strength training participants11, 12, which may foster engagement in more vigorous and continued PA participation67. Evidence indicates that HIIT modalities such as recreational soccer and other group sports are not only highly efficacious but also safe with low rates and risk of injury and engaging interventions for cardiometabolic risk reduction, even in populations at high risk of CVD such as participants diagnosed with hypertension or type 2 diabetes65, 68, 69. Our findings indicated stronger pooled effects than recently published data on HIIT49. Although, HIIT typically has a shorter duration compared to group sports (<30 mins versus one-hour); to our knowledge, there has been no direct comparison of group sport interventions and HIIT. In addition, group sport interventions also build social capital and are associated with positive motivational factors70.
Group sport interventions have the potential for broad public health impact as 75% of adults report ever playing sports, although only 25% report current participation71. In addition, 5 out of 10 of the most popular sports in the U.S. are group sports which include basketball, baseball/softball, soccer, football, and volleyball71 and worldwide, over 500 million people participate in recreational soccer72.
We observed low heterogeneity across included studies and 16 out of 23 included studies ranked as high quality, and we did not find evidence of publication bias based on visual inspection of funnel plots as symmetrical (Supplemental Figure 1). Thus, we believe the evidence in this meta-analysis is strong, although greater precision of effect estimates may be gained through addition of more studies and increased number of participants. Quality assessment indicated that studies incorporated a study design to minimize bias and all but one study included a control group for comparison. Inclusion of studies that used baseline and post-intervention assessment of participants also adds strength to the findings of this meta-analysis.
Our meta-analysis is subject to several limitations. First, we were not able to explore differences in cardiometabolic improvement by each group sport. The majority of included studies used soccer as the sport intervention and took place in Europe. There is a need for implementation of these interventions in more locations and investigating a broader range of group sports such as volleyball, basketball, rugby, and field or ice hockey and future studies should investigate the comparisons of group sports to traditional exercise interventions (i.e. running, cycling) and/or in combination with dietary and other behavioral interventions. Second, the various target populations included in the individual studies limited subgroup analyses to smaller sample sizes. Third, our findings are subject to inherent weaknesses of the individual included studies and possible publication bias, although visual inspection of funnel plots for each outcome did not indicate publication bias. Fourth, race/ethnicity of participants was rarely reported so the generalizability to various racial/ethnic groups is unknown. Despite these limitations, this study also has strengths as it is the first meta-analysis to comprehensively examine the effects of group sport participation on CVD and metabolic risk factors and physical fitness components from multiple studies with low heterogeneity.
In conclusion, the findings of this meta-analysis support the implementation of lifestyle interventions utilizing group sports as promising strategies for reducing cardiometabolic risk with potential for broad public health impact. Group sport interventions are highly engaging, have low attrition rates and broad-ranging beneficial effects on cardiometabolic and fitness parameters across populations of differing sex, in studies with durations less than 6 months, and in those at high risk of developing CVD risk (i.e. hypertension and type 2 diabetes). Significant increases in the proportion of the population achieving ideal levels of PA constitute a critical aspect of the new 2017 Hypertension prevention guidelines and overall cardiometabolic risk reduction guidelines73–75. Group sport interventions can be applied to primordial, primary, and secondary prevention of CVD and the results of this study provide support for scaling-up sports-based programs to help participants reduce physical inactivity, one of the most prevalent NCD risk factors globally.
Supplementary Material
Acknowledgements:
All authors approved of the final version of this manuscript.
Abbreviations
- BMI
Body mass index
- CVD
Cardiovascular disease
- DBP
Diastolic blood pressure
- HbA1c
Hemoglobin A1c/Glycated hemoglobin
- HDL cholesterol
High density lipoprotein cholesterol
- HOMA-IR
Homeostatic model assessment—Insulin resistance
- LDL cholesterol
Low density lipoprotein cholesterol
- NCD
Non-communicable chronic disease
- PA
Physical activity
- RHR
Resting heart rate
- SBP
Systolic blood pressure
- TG
Triglycerides
- VO2 maximum
Maximum rate of oxygen consumption
Appendix 1: Search Terms
Each of the following searches was completed in PubMed, EMBASE, PsycINFO, Web of Science, CINAHL, and Cochrane Library
Cardiovascular +
Sport
Volleyball
Soccer
Football
Basketball
Futbol
Rugby
Handball
Hockey
Softball
Baseball
Cardiometabolic +
Sport
Volleyball
Soccer
Football
Basketball
Futbol
Rugby
Handball
Hockey
Softball
Baseball
Footnotes
Conflict of interest statement: None
Financial disclosure: None
Publisher's Disclaimer: Disclaimer: All authors conduct an active lifestyle including participation in group sports primarily volleyball (Bellissimo, Paskert), soccer (Galaviz, Lobelo) and basketball (Lobelo). However, the authors are not advocates or activists of any specific group sports interventions or exercise programs.
References:
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–360. [DOI] [PubMed] [Google Scholar]
- 2.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40:181–188. [DOI] [PubMed] [Google Scholar]
- 3.Blair SN. Physical inactivity: the biggest public health problem of the 21st century. British journal of sports medicine. 2009;43:1–2. [PubMed] [Google Scholar]
- 4.Loprinzi PD, Darnell T, Hager K, Vidrine JI. Physical activity-related beliefs and discrepancies between beliefs and physical activity behavior for various chronic diseases. Physiology & behavior. 2015;151:577–582. [DOI] [PubMed] [Google Scholar]
- 5.Prevention CfDCa. State Indicator Report on Physical Activity. Atlanta, GA: US Dpeartment of Health and Human Services; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organization WH. Physical Activity Fact Sheet. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 7.Organization WH. Global Health Risks Mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: 2009:1–70. [Google Scholar]
- 8.Pringle A, Zwolinsky S, McKenna J, Daly-Smith A, Robertson S, White A. Reducing CVD Risk Factors for Men/Hard-to-Reach Men Using English Premier League Soccer Clubs. Medicine and Science in Sports and Exercise. 2014;46:595–595. [Google Scholar]
- 9.McGuire AM, Anderson DJ, Fulbrook P. Perceived barriers to healthy lifestyle activities in midlife and older Australian women with type 2 diabetes. Collegian (Royal College of Nursing, Australia). 2014;21:301–310. [DOI] [PubMed] [Google Scholar]
- 10.Capili B, Anastasi JK, Chang M, Ogedegbe O. Barriers and facilitators to engagement in lifestyle interventions among individuals with HIV. The Journal of the Association of Nurses in AIDS Care : JANAC. 2014;25:450–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krustrup P, Aagaard P, Nybo L, Petersen J, Mohr M, Bangsbo J. Recreational football as a health promoting activity: a topical review. Scandinavian journal of medicine & science in sports. 2010;20 Suppl 1:1–13. [DOI] [PubMed] [Google Scholar]
- 12.Bangsbo J, Hansen PR, Dvorak J, Krustrup P. Recreational football for disease prevention and treatment in untrained men: a narrative review examining cardiovascular health, lipid profile, body composition, muscle strength and functional capacity. British journal of sports medicine. 2015;49:568–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Nassau F, van der Ploeg HP, Abrahamsen F, et al. Study protocol of European Fans in Training (EuroFIT): a four-country randomised controlled trial of a lifestyle program for men delivered in elite football clubs. BMC public health. 2016;16:598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunt K, Wyke S, Gray CM, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet. 2014;383:1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milanovic Z, Pantelic S, Covic N, Sporis G, Krustrup P. Is Recreational Soccer Effective for Improving VO2max A Systematic Review and Meta-Analysis. Sports medicine (Auckland, N.Z.). 2015;45:1339–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oja P, Titze S, Kokko S, et al. Health benefits of different sport disciplines for adults: systematic review of observational and intervention studies with meta-analysis. Br J Sports Med. 2015;49:434–440. [DOI] [PubMed] [Google Scholar]
- 17.Milanovic Z, Pantelic S, Covic N, Sporis G, Mohr M, Krustrup P. Broad-spectrum physical fitness benefits of recreational football: a systematic review and meta-analysis. British journal of sports medicine. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Medicine and science in sports and exercise. 2011;43:1575–1581. [DOI] [PubMed] [Google Scholar]
- 20.Games O. Sports. Lausanne, Switzerland: International Olympic Committee; 2017. [Google Scholar]
- 21.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Family medicine. 2005;37:360–363. [PubMed] [Google Scholar]
- 22.Juni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ (Clinical research ed.). 2001;323:42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mudaliar U, Zabetian A, Goodman M, et al. Cardiometabolic Risk Factor Changes Observed in Diabetes Prevention Programs in US Settings: A Systematic Review and Meta-analysis. PLoS medicine. 2016;13:e1002095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Randers MB, Petersen J, Andersen LJ, et al. Short-term street soccer improves fitness and cardiovascular health status of homeless men. Eur J Appl Physiol. 2012;112:2097–2106. [DOI] [PubMed] [Google Scholar]
- 25.Andersen LJ, Randers MB, Hansen PR, et al. Structural and functional cardiac adaptations to 6 months of football training in untrained hypertensive men. Scand J Med Sci Sports. 2014;24 Suppl 1:27–35. [DOI] [PubMed] [Google Scholar]
- 26.Andersen LJ, Randers MB, Westh K, et al. Football as a treatment for hypertension in untrained 30–55-year-old men: a prospective randomized study. Scand J Med Sci Sports. 2010;20 Suppl 1:98–102. [DOI] [PubMed] [Google Scholar]
- 27.Knoepfli-Lenzin C, Sennhauser C, Toigo M, et al. Effects of a 12-week intervention period with football and running for habitually active men with mild hypertension. Scandinavian journal of medicine & science in sports. Vol 20 Suppl 1 2010:72–79. [DOI] [PubMed] [Google Scholar]
- 28.Krustrup P, Randers MB, Andersen LJ, Jackman SR, Bangsbo J, Hansen PR. Soccer improves fitness and attenuates cardiovascular risk factors in hypertensive men. Med Sci Sports Exerc. 2013;45:553–560. [DOI] [PubMed] [Google Scholar]
- 29.Mohr M, Lindenskov A, Holm PM, et al. Football training improves cardiovascular health profile in sedentary, premenopausal hypertensive women. Scandinavian journal of medicine & science in sports. Vol 24 Suppl 1 2014:36–42. [DOI] [PubMed] [Google Scholar]
- 30.Schmidt JF, Andersen TR, Horton J, et al. Soccer training improves cardiac function in men with type 2 diabetes. Med Sci Sports Exerc. 2013;45:2223–2233. [DOI] [PubMed] [Google Scholar]
- 31.Andersen TR, Schmidt JF, Thomassen M, et al. A preliminary study: effects of football training on glucose control, body composition, and performance in men with type 2 diabetes. Scandinavian journal of medicine & science in sports. 2014;24 Suppl 1:43–56. [DOI] [PubMed] [Google Scholar]
- 32.de Sousa MV, Fukui R, Krustrup P, et al. Positive effects of football on fitness, lipid profile, and insulin resistance in Brazilian patients with type 2 diabetes. Scandinavian journal of medicine & science in sports. 2014;24 Suppl 1:57–65. [DOI] [PubMed] [Google Scholar]
- 33.Andersen TR, Schmidt JF, Nielsen JJ, et al. Effect of football or strength training on functional ability and physical performance in untrained old men. Scandinavian journal of medicine & science in sports. 2014;24 Suppl 1:76–85. [DOI] [PubMed] [Google Scholar]
- 34.Andersen TR, Schmidt JF, Pedersen MT, Krustrup P, Bangsbo J. The Effects of 52 Weeks of Soccer or Resistance Training on Body Composition and Muscle Function in +65-Year-Old Healthy Males--A Randomized Controlled Trial. PloS one. 2016;11:e0148236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barene S, Krustrup P, Jackman SR, Brekke OL, Holtermann A. Do soccer and Zumba exercise improve fitness and indicators of health among female hospital employees? A 12-week RCT. Scandinavian journal of medicine & science in sports. 2014;24:990–999. [DOI] [PubMed] [Google Scholar]
- 36.Barene S, Krustrup P, Brekke OL, Holtermann A. Soccer and Zumba as health-promoting activities among female hospital employees: a 40-weeks cluster randomised intervention study. Journal of sports sciences. 2014;32:1539–1549. [DOI] [PubMed] [Google Scholar]
- 37.Connolly LJ, Suzanne S, Mohr M, Ermidis G, Julian R, Bangsbo J, Jackman SR, Bowtell JL, Davies RC, Hopkins SJ, Seymour R, Knapp KM, Krustrup P, Fulford J Effects of small-volume soccer and vibration training on body composition, aerobic fitness, and muscular PCr kinetics for inactive women aged 20–45. Journal of Sport and Health Science. 2014;3:284–292. [Google Scholar]
- 38.Krustrup P, Nielsen JJ, Krustrup BR, et al. Recreational soccer is an effective health-promoting activity for untrained men. British journal of sports medicine. 2009;43:825–831. [DOI] [PubMed] [Google Scholar]
- 39.Krustrup P, Hansen PR, Randers MB, et al. Beneficial effects of recreational football on the cardiovascular risk profile in untrained premenopausal women. Scandinavian journal of medicine & science in sports. 2010;20 Suppl 1:40–49. [DOI] [PubMed] [Google Scholar]
- 40.Mendham AE, Duffield R, Coutts AJ, Marino F, Boyko A, Bishop DJ. Rugby-Specific Small-Sided Games Training Is an Effective Alternative to Stationary Cycling at Reducing Clinical Risk Factors Associated with the Development of Type 2 Diabetes: A Randomized, Controlled Trial. PloS one. 2015;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Milanovic Z, Pantelic S, Kostic R, Trajkovic N, Sporis G. Soccer vs. running training effects in young adult men: which programme is more effective in improvement of body composition? Randomized controlled trial. Biol Sport. 2015;32:301–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schmidt JF, Hansen PR, Andersen TR, et al. Cardiovascular adaptations to 4 and 12 months of football or strength training in 65- to 75-year-old untrained men. Scandinavian journal of medicine & science in sports. Vol 24 Suppl 1 2014:86–97. [DOI] [PubMed] [Google Scholar]
- 43.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang X, Devlin HM, Smith B, et al. Effect of lifestyle interventions on cardiovascular risk factors among adults without impaired glucose tolerance or diabetes: A systematic review and meta-analysis. PloS one. 2017;12:e0176436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang X, Imperatore G, Thomas W, et al. Effect of lifestyle interventions on glucose regulation among adults without impaired glucose tolerance or diabetes: A systematic review and meta-analysis. Diabetes research and clinical practice. 2017;123:149–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–443. [DOI] [PubMed] [Google Scholar]
- 47.LeFevre ML. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;161:587–593. [DOI] [PubMed] [Google Scholar]
- 48.Association AAD. Standards of Medical Care in Diabetes-2017 In: Cefalu WT, ed. Diabetes Care. Vol 40 The Journal of Clinical and Applied Research and Education; 2017. [Google Scholar]
- 49.Batacan RB Jr., Duncan MJ, Dalbo VJ, Tucker PS, Fenning AS. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. British journal of sports medicine. 2017;51:494–503. [DOI] [PubMed] [Google Scholar]
- 50.Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension (Dallas, Tex. : 1979). 2011;58:950–958. [DOI] [PubMed] [Google Scholar]
- 51.Stein RA, Michielli DW, Glantz MD, et al. Effects of different exercise training intensities on lipoprotein cholesterol fractions in healthy middle-aged men. American heart journal. 1990;119:277–283. [DOI] [PubMed] [Google Scholar]
- 52.Nybo L, Sundstrup E, Jakobsen MD, et al. High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sports Exerc. 2010;42:1951–1958. [DOI] [PubMed] [Google Scholar]
- 53.Ferguson MA, Alderson NL, Trost SG, Davis PG, Mosher PE, Durstine JL. Plasma lipid and lipoprotein responses during exercise. Scandinavian journal of clinical and laboratory investigation. 2003;63:73–79. [DOI] [PubMed] [Google Scholar]
- 54.Kelley GA, Kelley KS, Roberts S, Haskell W. Comparison of aerobic exercise, diet or both on lipids and lipoproteins in adults: a meta-analysis of randomized controlled trials. Clinical nutrition (Edinburgh, Scotland). 2012;31:156–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lin X, Zhang X, Guo J, et al. Effects of Exercise Training on Cardiorespiratory Fitness and Biomarkers of Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of the American Heart Association. 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Naci H, Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ (Clinical research ed.). 2013;347:f5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Naci H, Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. British journal of sports medicine. 2015;49:1414–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fulcher J, O’Connell R, Voysey M, et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385:1397–1405. [DOI] [PubMed] [Google Scholar]
- 59.Adams SP, Tsang M, Wright JM. Lipid-lowering efficacy of atorvastatin. The Cochrane database of systematic reviews. 2015:Cd008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fiuza-Luces C, Garatachea N, Berger NA, Lucia A. Exercise is the real polypill. Physiology (Bethesda, Md.). 2013;28:330–358. [DOI] [PubMed] [Google Scholar]
- 61.Gao D, Ning N, Niu X, Wei J, Sun P, Hao G. Aliskiren vs. angiotensin receptor blockers in hypertension: meta-analysis of randomized controlled trials. American journal of hypertension. 2011;24:613–621. [DOI] [PubMed] [Google Scholar]
- 62.Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J Hypertens. 2011;29:1253–1269. [DOI] [PubMed] [Google Scholar]
- 63.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. The American journal of clinical nutrition. 1999;69:373–380. [DOI] [PubMed] [Google Scholar]
- 64.Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. Jama. 2011;305:1790–1799. [DOI] [PubMed] [Google Scholar]
- 65.Jung ME, Bourne JE, Beauchamp MR, Robinson E, Little JP. High-intensity interval training as an efficacious alternative to moderate-intensity continuous training for adults with prediabetes. Journal of diabetes research. 2015;2015:191595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pavey T, Taylor A, Hillsdon M, et al. Levels and predictors of exercise referral scheme uptake and adherence: a systematic review. J Epidemiol Community Health. 2012;66:737–744. [DOI] [PubMed] [Google Scholar]
- 67.Nielsen G, Wikman JM, Jensen CJ, Schmidt JF, Gliemann L, Andersen TR. Health promotion: the impact of beliefs of health benefits, social relations and enjoyment on exercise continuation. Scandinavian journal of medicine & science in sports. 2014;24 Suppl 1:66–75. [DOI] [PubMed] [Google Scholar]
- 68.Ramos JS, Dalleck LC, Tjonna AE, Beetham KS, Coombes JS. The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports medicine (Auckland, N.Z.). 2015;45:679–692. [DOI] [PubMed] [Google Scholar]
- 69.Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2004;11:216–222. [DOI] [PubMed] [Google Scholar]
- 70.Blatter JS, Dvorak J. Football for health - science proves that playing football on a regular basis contributes to the improvement of public health. Scandinavian journal of medicine & science in sports. 2014;24 Suppl 1:2–3. [DOI] [PubMed] [Google Scholar]
- 71.NPR RWJF, Harvard T.H. Chan School of Public Health. Sports and Health in America 2015:1–73. [Google Scholar]
- 72.Krustrup P, Bangsbo J. Recreational football is effective in the treatment of non-communicable diseases. British journal of sports medicine. 2015;49:1426–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Whelton PK, Carey RM, Aronow WS, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017. [DOI] [PubMed] [Google Scholar]
- 74.Mozaffarian D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation. 2016;133:187–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Go AS MD, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, F S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, L D, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association 2013:127:e126–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bangsbo J, Nielsen JJ, Mohr M, et al. Performance enhancements and muscular adaptations of a 16-week recreational football intervention for untrained women. Scandinavian journal of medicine & science in sports. 2010;20 Suppl 1:24–30. [DOI] [PubMed] [Google Scholar]
- 77.Filliau C, Younes M, Blanchard AL, et al. Effect of “Touch Rugby” Training on the Cardiovascular Autonomic Control In Sedentary Subjects. Int J Sports Med. 2015;36:567–572. [DOI] [PubMed] [Google Scholar]
- 78.Krustrup P, Hansen PR, Andersen LJ, et al. Long-term musculoskeletal and cardiac health effects of recreational football and running for premenopausal women. Scandinavian journal of medicine & science in sports. Vol 20 Suppl 1 2010:58–71. [DOI] [PubMed] [Google Scholar]
- 79.Randers MB, Nielsen JJ, Krustrup BR, et al. Positive performance and health effects of a football training program over 12 weeks can be maintained over a 1-year period with reduced training frequency. Scand J Med Sci Sports. 2010;20 Suppl 1:80–89. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.