Abstract
Objective
Obesity is preventable and yet continues to be a major risk factor for chronic disease. Multiple prevention approaches have been proposed across multiple settings where people live, work, learn, worship, and play. This review searched the vast literature on obesity prevention interventions to assess their effects on daily energy consumed and energy expended.
Methods
This systematic review (PROSPERO registration CRD42017077083) searched seven databases for systematic reviews and studies reporting energy intake and expenditure. Two independent reviewers screened 5,977 citations; data abstraction supported an evidence map, comprehensive evidence tables, and meta‐analysis; critical appraisal assessed risk of bias; and the quality of evidence was evaluated using Grading of Recommendations Assessment, Development and Evaluation (GRADE).
Results
Hundreds of published reviews were identified. However, few studies reported on energy intake and expenditure to determine intervention success. Ninety‐nine studies across all intervention domains were identified. Few areas demonstrated statistically significant effects across studies; school‐based approaches and health care initiatives reduced energy consumed, education reduced energy consumed and increased energy expended, and social‐group approaches increased energy expenditure.
Conclusions
Despite the amount of research on obesity prevention interventions, very few studies have provided relevant information on energy intake and expenditure, two factors determining weight gain. Future research needs to fill this gap to identify successful public health policies.
Introduction
Estimated global obesity prevalence doubled from 1980 to 2008 1, 2. In the United States, obesity prevalence has reached 35% in men, 40% in women 3, and 17% in children 4; severe obesity may still be increasing 5, 6. The U.S. National Institutes of Health has provided approximately $9.5 billion to obesity prevention and intervention research over the past decade 7. While much work has been done in clinical and educational interventions, dietary and physical activity patterns are influenced by environments. The Foresight Programme used a mapping approach, indicating that obesity is likely determined by a complex multifaceted system with multiple drivers 8. As researchers recognize different obesogenic environmental determinants, numerous distinct research subfields have been launched. Putting a multitude of isolated data points into a coherent picture is challenging but necessary to assess whether proposed solutions are promising or not. There is a need for a cohesive thread to understand findings across subfields because eventually preventing obesity requires changes in either energy intake or energy expenditure.
This review searched the literature on obesity prevention interventions to assess their effects on daily energy consumed and energy expended. We assessed evidence across approaches that are being tested and implemented in public health areas in the United States and Mexico. Focusing on a few would ignore the myriad of ways that changes in economic, physical, and social environments can impact obesity. We included studies of food labeling, fiscal measures, physical environment and transportation, food supply and lifestyle commodities, work site interventions, population‐based health care initiatives, school‐based interventions, education and public health campaigns, and social‐group approaches. We focused on obesity prevention strategies aimed at general populations. We summarized effectiveness in meta‐analyses to determine intervention effects, and formal quality‐of‐evidence assessments provided a comprehensive overview.
Methods
The systematic review protocol is registered in PROSPERO (CRD42017077083). We chose intervention categories in order to parameterize a microsimulation model of obesity policies that incorporates energy balance and the interplay between diet and physical activity in the development of obesity.
Data sources and searches
We searched PubMed (biomedical literature), Cochrane Database of Systematic Reviews (Cochrane Collaboration reviews of health interventions), CAB (applied life sciences), ERIC (education research), Cumulative Index to Nursing and Allied Health Literature, Campbell Systematic Reviews (Campbell Collaboration reviews addressing social and economic topics), and Web of Science (multidisciplinary scientific research collection). The search strategy is documented in Supporting Information Table S1, and it combined known diet and physical activity interventions and general search terms to identify novel approaches.
The search identified systematic reviews and primary research studies with concurrent or historic comparators to estimate effects of obesity prevention approaches. Systematic reviews provided comprehensive summaries of the literature for defined topics by combining thorough and comprehensive searches and synthesis of the available evidence. Searches built on a comprehensive review by the World Health Organization of studies evaluating diet and/or physical activity interventions for children and/or adults published in 2009 9, and updated searches targeted studies not yet summarized in the World Health Organization review.
Study selection
The eligibility criteria are documented in a population, intervention, comparator, outcome, timing, setting, and study design framework (Supporting Information Table S2). Two independent reviewers screened publications; disagreements were resolved through discussion.
Data abstraction and critical appraisal
Data were abstracted by a systematic reviewer and checked for accuracy by a second reviewer. We abstracted the reported daily calorie intake and daily energy expenditure in the intervention and the comparator group. We assessed selection bias and confounding, performance bias, detection bias, attrition bias, and other sources of bias. The results of the risk of bias assessments were incorporated into the quality of evidence summary. The critical appraisal criteria and results are presented in Supporting Information Figure S1.
Obesity prevention intervention categories
We categorized interventions according to their primary aim using mutually exclusive categories (see Supporting Information Table S3).
Data synthesis and analysis
The evidence synthesis was based on primary research studies that report on energy consumed and/or energy expended. In addition, we provided an evidence map to document the published systematic reviews on the topic. The systematic reviews were used to provide a broader overview of the existing literature and as a source to identify primary research studies.
We converted intervention effects to standardized mean differences (SMD) together with the 95% CIs in order to compare effects across individual studies. Studies exclusively targeting children were analyzed separately from studies addressing adults only or children and adults. We stratified studies with concurrent comparators (e.g., controlled trials) and those with historic comparators (e.g., pre‐post evaluations). Where a sufficient number of studies was available, we conducted sensitivity analyses to test the robustness of the intervention effect estimates. Meta‐analysis was based on random‐effects models using the Hartung‐Knapp correction.
The quality of evidence was assessed for each summary statement using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach. The initial assessment for the quality of evidence was based on study design. Randomized controlled trials (RCTs) comparing an intervention to a concurrent comparator start at high quality of evidence, whereas studies with historic comparators start at low quality of evidence. Eight criteria were used to assess the quality of the evidence. Five criteria were used to downgrade where applicable (study limitations, inconsistency, indirectness, imprecision, and publication bias), and three criteria (presence of a large effect, documented dose‐response relationship, and residual confounding would reduce the effect) were used to potentially upgrade the quality of evidence. We categorized our confidence in the summary as high, moderate, low, or very low using the GRADE criteria.
Results
We identified 5,977 citations and obtained 1,565 publications. We identified 99 unique studies and 338 systematic reviews meeting the inclusion criteria. The literature flow diagram is in Supporting Information Figure S2, and we include a list of the included systematic reviews (Supporting Information Table S4).
We identified a large number of systematic reviews. Figure 1 shows the distribution of topics addressed in published reviews, and they are described in Supporting Information Table S5.
Figure 1.
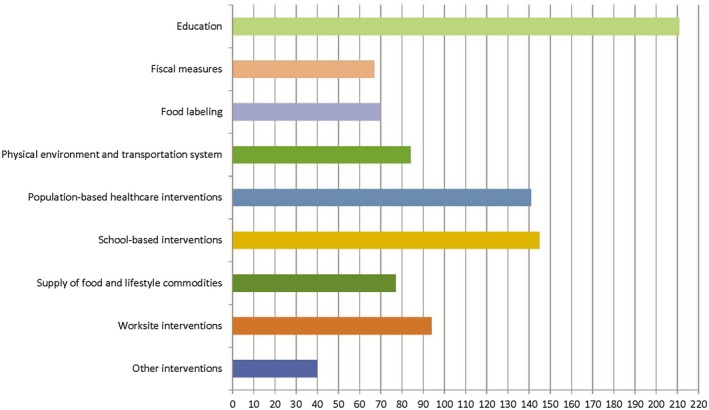
Overview of interventions targeted in published systematic reviews. [Colour figure can be viewed at wileyonlinelibrary.com]
The 99 primary research studies reporting on energy consumption and/or expenditure are documented in a detailed evidence table in Supporting Information Table S6. The table is stratified by obesity prevention approach and provides a comprehensive overview. The results across studies are summarized in the Table 1, which documents the presence and absence of evidence for all intervention categories of interest, the number of studies per intervention, the study design the results are based on, and the summary across studies. The following provides a synthesis for the different obesity prevention strategies across the identified evidence. Citations and review or study details are documented in Supporting Information Table S6.
Table 1.
Summary of findings
| Intervention outcome | Number of studies and study design | Reason for downgraded quality | Effect estimate and direction of effects | GRADE |
|---|---|---|---|---|
| Food labeling | ||||
| Energy consumed | None | NA | NA | NA |
| Energy expended | None | NA | NA | NA |
| Fiscal measures | ||||
| Energy consumed | 1 RCT | Consistency could not be assessed, study limitations | No statistically significant difference (SMD, 0.10; 95% CI: −0.24 to 0.44) | Very low |
| Energy expended | None | NA | NA | NA |
| Physical environment and transportation | ||||
| Energy consumed | 1 CT | Inconsistency | ES could not be calculated for the CT (but favored the intervention group); the control group had lower intake in the cohort study (SMD, 0.41; 95% CI: 0.14 to 0.69; 1 cohort study) | Very low |
| 1 cohort study | ||||
| Energy expended | None | NA | NA | NA |
| Supply of food and lifestyle commodities | ||||
| Energy consumed | 3 RCTs | Inconsistency, study limitations | RCTs report positive but not statistically significant differences (SMD, −0.23; 95% CI: −0.45 to −0.00; 3 RCTs); the CT reported insufficient data | Low |
| 1 CT | ||||
| Energy expended | None | NA | NA | NA |
| Work site interventions | ||||
| Energy consumed | 2 RCTs | Inconsistency, study limitations | 2 studies reported positive results, but ES could not be computed; 2 studies reported conflicting results and were based on diverse study designs (SMD, −0.20; 95% CI: −0.53 to 0.13; 1 RCT; SMD, −0.98; 95% CI: −1.32 to −0.65; 1 pre‐post study) | Very low |
| 1 CT | ||||
| 1 pre‐post study | ||||
| Energy expended | 6 RCTs | Inconsistency, imprecision | 4 RCTs found no statistically significant difference (SMD, 0.22; 95% CI: −0.17 to 0.61; 4 RCTs); 2 pre‐post studies reported improvements but could not be combined in a summary estimate | Low |
| 1 CT | ||||
| 2 pre‐post studies | ||||
| Population‐based health care initiatives | ||||
| Energy consumed | 15 RCTs | Inconsistency (sensitivity analysis) | Reduced consumption (SMD, −0.13; 95% CI: −0.18 to −0.08; 9 RCTs) | Moderate |
| Energy consumed, children only | 2 RCTs | Imprecision | No statistically significant difference (SMD, −0.19; 95% CI: −0.61 to 0.24; 2 RCTs) | Low |
| Energy expended | 5 RCTs | Study limitations, inconsistency | Studies could not be combined; effect varied | Very low |
| School‐based interventions | ||||
| Energy consumed, children | 10 | Inconsistency | Significant reduction (SMD, −0.11; 95% CI: −0.19 to −0.04; 6 studies) | Moderate |
| 6 RCTs | ||||
| 3 CTs | ||||
| 1 cohort study | ||||
| Energy expended, children | 5 RCTs | Inconsistency | No systematic effect (SMD, −0.08; 95% CI: −0.65 to 0.49; 6 trials) | Low |
| 1 CT | ||||
| 2 pre‐post studies | ||||
| Health education campaigns | ||||
| Energy consumed | 17 RCTs | Inconsistency | RCTs showed a statistically significant effect (SMD, −0.17; 95% CI: −0.26 to −0.08; 10 RCTs); pre‐post studies both positive but could not be combined | Moderate |
| 3 pre‐post studies | ||||
| Energy consumed, children only | 3 RCTs | Inconsistency, imprecision | SMD, −0.20; 95% CI: −0.41 to 0.01; 3 RCTs | Very low |
| Energy expended | 13 RCTs | Inconsistency | Positive pooled effects but individual results varied (SMD, 0.37; 95% CI: 0.07 to 0.67; 10 RCTs; SMD, 0.48; 95% CI: 0.16 to 0.79; 2 pre‐post studies) | Low |
| 2 pre‐post studies | ||||
| Energy expended, children only | 2 RCTs | Inconsistency, imprecision | Difference not statistically significant (SMD, 0.06; 95% CI: −0.41 to 0.52; 2 RCTs) | Very low |
| Social‐group approaches | ||||
| Energy consumed | 2 RCTs | Inconsistency, imprecision | Studies could not be combined; conflicting results | Very low |
| 1 CT | ||||
| Energy expended | 7 RCTs | Inconsistency | Statistically significant increase (SMD, 0.26; 95% CI: −0.07 to 0.44; 8 trials) | Moderate |
| 1 CT | ||||
| 1 pre‐post study | ||||
| Energy expended, children only | 3 RCTs | Imprecision | Not statistically significant (SMD, 0.17; 95% CI: −0.17 to 0.51; 3 RCTs) | Low |
CT, controlled trial; ES, effect size; NA, not applicable; RCT, randomized controlled trial; SMD, standardized mean difference.
Food labeling
We identified 69 systematic reviews in which the scope of the review included food‐labeling initiatives. Six of these exclusively addressed food labeling such as calorie labeling in restaurants. The reviews reported on a variety of acceptability outcomes and obesity measures.
We did not identify any individual study that met inclusion criteria and reported on daily energy consumed or expended with food‐labeling initiatives.
Financial incentives
We identified 68 systematic reviews in which the scope of the review included financial incentives. Of these, six exclusively targeted financial incentives.
Our literature searches in databases and reference mining of the systematic reviews identified one relevant study that reported on daily energy consumed.
Energy consumed
The study evaluated whether incentivizing the purchase of fruits and vegetables and prohibiting the purchase of less nutritious food in a food‐benefit program improves the nutritional quality of participants’ diets. The study reported reduced intake of energy (−96 kcal per day; SE, 59.9), but the difference between the intervention and control group was not statistically significant (SMD, 0.10; 95% CI: −0.24 to 0.44; one RCT) 10. The quality of the evidence was downgraded because the result is based on a single study and the consistency across studies could not be assessed.
None of the identified studies reported on children alone.
Energy expended
None of the identified studies reported on energy expended.
Physical environment and transportation system
We identified 83 systematic reviews that covered physical environment interventions. Four of the systematic reviews exclusively addressed physical environment changes and transportation system approaches.
Two studies reporting on physical environment interventions met inclusion criteria, and both reported on energy consumed.
Energy consumed
One of the studies assessed the effect of introducing a supermarket in a “food desert” on daily calorie intake compared with participants in a comparison neighborhood 11. The study reported a decrease in the intervention group; however, the study reported no measure of dispersion, and therefore the effect size could not be calculated. The other study assessed the impact of a new government‐subsidized supermarket on children’s dietary intake 12. Dietary recall data showed more calories consumed in the intervention group (SMD, 0.41; 95% CI: 0.14‐0.69; one cohort study), and the authors concluded that further research is needed to determine whether healthy food retail expansions can improve food choices of children and their families. Given the inconsistent findings in the small number of studies, the quality of evidence was downgraded to very low quality.
Energy expended
We did not identify studies reporting on energy expended.
Supply of food and lifestyle commodities
Of all identified systematic reviews, 76 included interventions that involved supply of food or lifestyle commodities. Of these, six addressed only supply of food (e.g., diet approaches with pre‐prepared food) or product placement (e.g., changing shops and supermarkets to promote healthier options).
Four studies met inclusion criteria, and all reported on daily energy intake. The details of each of the studies are documented in Supporting Information Table S6 and summarized in this section.
Energy consumed
An RCT evaluated the effects of health coaches targeting the home food and activity environment compared with families receiving only educational material 13. A second RCT evaluated the effect of a 1‐year intervention of home delivery of noncaloric beverages 14. An RCT delivered in Mexico provided women with overweight with bottled water for 9 months to increase water intake compared with a group receiving education alone 15. The pooled school‐based result showed a small treatment effect showing a statistically significant reduction compared with control (SMD, −0.23; 95% CI: −0.45 to 0.00; three RCTs) (Supporting Information Figure S3). I 2 estimated no heterogeneity. Restricting to US studies did not substantially change the effect estimate but increased the CI so that the effect was not statistically significant (SMD, −0.26; 95% CI: −0.99 to 0.48; two RCTs).
A further study could not be combined with the RCTs (Supporting Information Table S7).
The quality of the evidence was downgraded to low quality because of inconsistency and study limitation. Only one of the three studies reported a statistically significant effect, and excluding one study resulted in no statistically significant effect.
Energy expended
None of the studies reported a measure of energy expended.
Work site interventions
Ninety‐four of the identified systematic reviews included work site intervention evaluations. Fourteen of these reviewed only work site interventions.
Ten primary research studies met all inclusion criteria. Studies addressed a range of interventions implemented in the work site context. The individual studies are described in detail in Supporting Information Table S6.
Energy consumed
Four of the work site studies reported on daily energy consumption. The studies were difficult to combine, and it was not possible to estimate a summary effect across studies. An RCT evaluating a work site chronic disease prevention program reported no statistically significant differences between intervention and control groups (SMD, −0.20; 95% CI: −0.53 to 0.13; one RCT) 16. A second study compared two active interventions without a control group 17. The study reported no difference between the two interventions. The study indicated improvement in energy intake at follow‐up; however, the effect size could not be computed because the study did not report the standard error (SE) of the difference (or provide the information that allowed it to be calculated). The third study evaluated the program America on the Move implemented as a research study at a university 18. The study reported a positive effect on participants during the intervention week (SMD, −0.98; 95% CI: −1.32 to −0.65; one pre‐post study). The fourth study was a cluster RCT evaluating an obesity prevention intervention for metropolitan transit workers 19. The study reported insufficient detail to compute an effect size.
The quality of the evidence for work site interventions on energy consumed was downgraded to very low quality because of inconsistency and study limitations that prevented estimating a summary effect.
Energy expended
Nine of the work site studies reported on energy expenditure. Four RCTs reported effect size estimates compared with a passive control group and were combined in a meta‐analysis. The studies evaluated an activity monitoring interventions for physicians in training 20, a walking program for employees 21, booster breaks and physical activity computer prompts 22, and a work site chronic disease prevention program 16. Although three studies favored the intervention, only one reported a statistically significant improvement. The difference between intervention and control groups was not statistically significant across studies (SMD, 0.22; 95% CI: −0.17 to 0.61; four RCTs) (Supporting Information Figure S4). Two additional RCTs and a controlled trial could not be included in the analysis (insufficient data, comparative effectiveness); the studies are described in Supporting Information Table S7.
Two pre‐post studies could be combined in a meta‐analysis to estimate the effect of the intervention to the status before the intervention 18, 23. The studies evaluated an implementation of the America on the Move program at a university 18 and an intervention to increase walking for women at rural work sites 23. Although both studies reported positive effects of the intervention, the effect size estimates varied so widely that a pooled effect showed a wide CI that did not support a statistically significant summary estimate. In addition, the width of the CI did not indicate that a summary estimate is meaningful.
Based on RCT evidence, work site interventions did not have a statistically significant effect on energy expended compared with concurrent control groups. However, the quality of the evidence was downgraded to low because of inconsistency and imprecision, and it remains unclear whether work site interventions do have an effect on energy expended.
Population‐based health care interventions
We identified 139 systematic reviews that included health care interventions in their scope. Of these, 23 focused exclusively on health care interventions such as prevention programs implemented in primary care.
Sixteen studies in total met inclusion criteria. The studies recruited participants through health care settings (Supporting Information Table S6).
Energy consumed
All but three of the included studies reported on energy consumed. Nine RCTs assessed the effectiveness of the intervention compared with no intervention or other passive control groups. Interventions were described as dietary modification 24, using weight loss strategies from successful weight losers 25, culturally tailored lifestyle intervention 26, behavioral intervention for postpartum weight loss 27, internet‐based program for low‐income postpartum women 28, clinic‐based weight management program 29, health behavior intervention for adolescents 30, mentorship model for urban adolescents 31, and tailored lifestyle modification 32. Across studies, health care interventions resulted in a small effect favoring the interventions (SMD, −0.13; 95% CI: −0.18 to −0.08; nine RCTs) (Figure 2). The majority of studies reported a positive effect, although only one individual study was statistically significant. Effect estimates varied somewhat, but all CIs overlapped and I 2 was negligible (7%). There was no evidence of publication bias (Begg P = 0.90, Egger P = 0.27). Excluding Beresford et al. 24 in a sensitivity analysis showed that the result was primarily driven by this large study; the estimate without the study was not statistically significant (SMD, −0.09; 95% CI: −0.19 to 0.02; eight RCTs).
Figure 2.
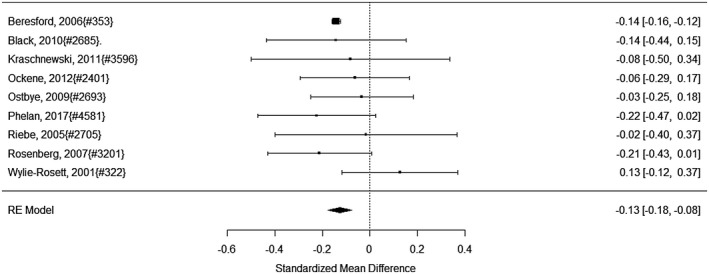
Estimated effects of population‐based health care interventions on energy consumed.
Two of the studies included children 30, 31. A subgroup analysis for these found a similar effect estimate, albeit not statistically significant (SMD, −0.19; 95% CI: −0.61 to 0.24; two RCTs).
Several studies assessed the comparative effectiveness of different interventions; these are described in Supporting Information Table S7.
We judged the quality of evidence to be moderate for a small effect on reduced energy consumed (downgraded because of inconsistency across studies).
Energy expended
Five studies reported on energy expended. Two studies had passive control groups that allowed estimating the intervention effect. One RCT evaluated the effect on a mentorship model among urban, black adolescents 31. A cluster RCT investigated an internet‐based program for low‐income postpartum women 28.
The two studies reported very different results, one favoring the intervention and one the control group, indicating that a combined effect estimate is not appropriate (SMD, 0.02; 95% CI: −1.93 to 1.98; two RCTs). Two health care studies reported comparative effectiveness data, and one reported insufficient data (Supporting Information Table S6).
The quality of evidence was rated very low (downgraded for study limitations and inconsistency) because it was not possible to determine with confidence whether health care interventions increased expended energy.
School‐based interventions
A large number (n = 145) of the identified systematic reviews included school interventions in their scope. Of these, 32 focused exclusively on school‐setting interventions for various age groups (childcare setting to high school).
We identified 22 studies in schoolchildren that met inclusion criteria.
Energy consumed
Ten of the 22 studies reported on energy consumed. Figure 3 shows six trials that could be combined in a meta‐analysis for the outcome energy consumed. One cluster RCT compared a multicomponent intervention for American Indian schoolchildren with no intervention 33. Casazza et al. 34 focused on the method of delivery of nutrition and physical activity information for adolescents in a nonrandomized investigator‐controlled trial (compared with no intervention). A cluster RCT assessed a multicomponent intervention‐based school intervention to prevent obesity compared with control schools 35. An additional cluster RCT for high schools compared nurse‐delivered cognitive‐behavioral counseling plus after‐school exercise with information alone 36. A (nonrandomized) trial evaluated the effects of a cooking program for fifth graders 37. A natural experiment assessed the effect of state laws governing fat, sugar, and caloric content of foods sold in schools 38. The interventions varied in duration, ranging from 3 months 34 to 3 years 33. Across studies, we found a small effect in these school interventions compared with no intervention or information only (SMD, −0.11; 95% CI: −0.19 to −0.04; six studies) (Figure 3). I 2 was negligible (10%); however, one study 37 came to a different effect estimate than the other studies (the CIs did not overlap). There was no evidence of publication bias (Begg P = 0.48, Egger P = 0.43). Four RCTs could not be pooled with the others (Supporting Information Table S7).
Figure 3.
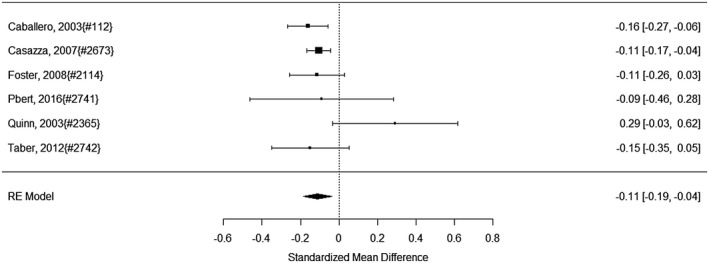
Estimated effects of school‐based initiatives on energy consumed.
All studies addressed the effects of the intervention on children and none on adults.
The quality of evidence was determined to be moderate that school interventions have a small effect on daily energy consumed (downgraded because of inconsistency).
Energy expended
Twelve included school‐based intervention studies reported on an objective measure of daily energy expended. Supporting Information Figure S5 shows those that we were able to combine in a meta‐analysis. Aburto et al. 39 randomized 27 Mexican schools to either a physical activity intervention or control. One cluster RCT evaluated educational materials for schools and families aiming to decrease screen time, increase fruit and vegetable consumption, and increasing physical activity 40. A further cluster RCT evaluated an interactive multimedia curriculum for promoting physical activity compared with an educational CD 41. A (nonrandomized) trial compared a pedometer intervention program in middle schoolers with control children 42. A cluster RCT compared a physical activity intervention for middle school girls with delayed intervention 43. One RCT assessed the effect of a 3‐week pedometer intervention with set goals compared with wearing pedometers alone 44. Studies varied, and not all favored the intervention arm. Across studies, there was no statistically significant difference between intervention and control participants (SMD, −0.08; 95% CI: −0.65 to 0.49; six trials) (Supporting Information Figure S5).
Four additional RCTs reported on energy expended, but the effect size could not be calculated (Supporting Information Table S7).
One pre‐post study reported a statistically significant effect of a school health approach for Appalachian youth (SMD, 0.65; 95% CI: 0.38‐0.91; one pre‐post study) 45. One pre‐post study could not be combined with the previous study (Supporting Information Table S7).
We rated the quality of evidence as low because of the large variation in the studies that did not indicate that the effects are intervention specific.
Health education campaigns
Most identified systematic reviews (n = 211) included education interventions. Sixty‐two of these focused exclusively on education approaches such as public health campaigns in mass media or social media.
We identified 27 education studies meeting inclusion criteria. While the content of the intervention varied widely, participants in the studies were recruited through advertisements or mass mailings (i.e., not directly approached by their health care provider or recruited through school or work sites), and the studies did not involve any structural changes implemented in the physical environment.
Energy consumed
Of the included studies, 18 reported on energy consumed. This included an RCT evaluating the effects of an intensive diet and physical activity modification program, Complete Health Improvement Program (CHIP), compared with wait list 46. A further RCT investigated whether video games designed to promote behavior change enable children to learn healthier behaviors 47. One RCT explored the maintenance of weight loss in middle‐aged women with overweight using an internet‐based intervention 48. One RCT compared personalized dietary counseling via lay health advisors plus tailored print materials delivered via the mail in Latinas compared with targeted, mailed, “off‐the‐shelf” materials 49. An RCT studied the effect of diet and exercise in postmenopausal women compared with a control group 50. One of the identified RCTs addressed the efficacy of a 2‐year obesity prevention program in African American girls compared with a control group 51. One RCT evaluated the effect of dietary counseling compared with information material only 52. A further RCT assessed the effect of a lifestyle intervention to prevent weight gain during menopause compared with no intervention 53. In one of the included RCTs, the intervention group participated in a 4‐hour prevention program, whereas the control group received only an educational brochure 54. A family‐based community‐centered program of skills‐building sessions was evaluated in another RCT 55. The pooled result showed a small effect for reduced energy consumed (SMD, −0.17; 95% CI: −0.26 to −0.08; 10 RCTs) (Figure 4). The I 2 statistic indicated negligible heterogeneity (18%). There was no evidence of publication bias (Begg P = 0.29, Egger P = 0.52). The graph included three studies that were exclusively in children 47, 51, 55. The effect was similar but not statistically significant in this subgroup (SMD, −0.20; 95% CI: −0.41 to 0.01; three RCTs). Other identified studies evaluated the comparative effectiveness of different obesity prevention interventions (Supporting Information Table S7).
Figure 4.
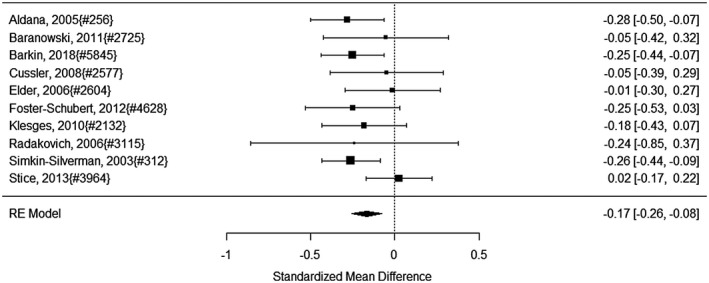
Estimated effects of health education campaigns on energy consumed.
Three included studies did not report on a concurrent comparator. A pre‐post study evaluated a Web‐based intervention to influence health behavior 56. A further pre‐post study assessed energy consumed in the context of a weight management program using the food‐exchange system 57. Although both pre‐post studies reported positive effects, the estimates varied widely, and the pooled estimate was not statistically significant (SMD, −0.54; 95% CI: −3.76 to 2.69; two pre‐post studies). One pre‐post study could not be combined with the other studies because no measure of dispersion was reported (Supporting Information Table S7).
We determined that a moderate‐quality body of evidence supports a small effect of reduced consumed energy (downgraded because of inconsistency).
Energy expended
In total, 12 studies evaluating educational interventions reported on daily energy expended. This included five of the RCTs already described that also reported on energy consumed and that compared with a passive control group 46, 47, 50, 51, 53. In addition, an RCT randomizing older adults to a pedometer and interactive website‐based intervention compared with control contributed to this analysis 58. One RCT evaluated an automated intervention for multiple health behaviors using conversational agents that also reported on energy expended 59. Furthermore, one RCT evaluated a peer‐guided intervention for mothers participating in the Special Supplemental Nutrition Program for Women, Infants, and Children 60. One RCT randomized older participants to volunteering in public school or a low‐activity control group 61. An additional RCT investigated the impact of a brief intervention for working mothers compared with waiting list control 62. The effects of the interventions varied widely, but the pooled effect was statistically significantly different from the control arm (SMD, 0.37; 95% CI: 0.07 to 0.67; 10 RCTs). There was substantial heterogeneity (I 2 83%) but no indication of publication bias (Begg P = 0.86, Egger P = 0.70). The two studies exclusively enrolling children did not find differences between groups (SMD, 0.06; 95% CI: −0.41 to 0.52; two RCTs) 47, 51. Two comparative effectiveness studies and one RCT not adjusted for clustering are described in Supporting Information Table S6.
Two of the pre‐post studies reported on energy expended 56, 63. One evaluated the effect of a statewide campaign to increase activity levels 63. The other study evaluated a Web‐based intervention to influence health behavior 56. Both studies reported a positive effect, and across studies, we estimated a small to medium effect on energy expended (SMD, 0.48; 95% CI: 0.16‐0.79; two pre‐post studies) (Figure 5). Heterogeneity was low (I 2 6%). Publication bias could not be assessed because of the small number of studies.
Figure 5.
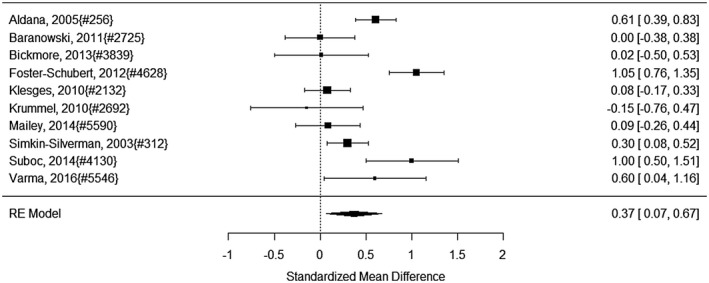
Estimated effects of health education campaigns on energy expended.
Education interventions may have a small effect on daily energy expended, but the quality of evidence was very low (the pooled effect in RCTs was not statistically significant, and the pre‐post studies showed wide CIs).
Social‐group approaches
The identified studies included 13 studies in which participants were recruited through existing social groups or community institutions, such as churches, Boy Scout groups, or established community programs.
Energy consumed
Of these social‐group interventions to prevent obesity, two reported on energy consumed 64, 65. One reported on a nutrition education program for women evaluated in an investigator‐controlled nonrandomized trial (Expanded Food and Nutrition Education Program) 64, and the other evaluated a faith‐based cardiovascular health promotion intervention for African American women in a cluster RCT 65. The studies reported conflicting results, and the large CI did not suggest that a mean effect estimate is appropriate (SMD, −0.05; 95% CI: −3.60 to 3.50; two trials).
The quality of evidence was rated as very low because of the lack of consistency in results in the small number of studies that reported on the outcome dietary consumption.
Energy expended
Social‐group interventions reported on energy expended (11 studies). Figure 6 shows studies that compared interventions with a concurrent control group. One study evaluated a faith‐based, behavior‐change, physical activity intervention for African Americans 66. One RCT compared the effect of a pedometer‐based intervention for older adults with a wait list group 67. One study evaluated a YMCA after‐school food and fitness program in a cluster RCT 68. Another cluster RCT evaluated a Boy Scout badge intervention to increase physical activity skills, self‐efficacy, and goal setting compared with a control condition 69. One RCT evaluated a lifestyle behavior intervention for Hispanic women 70. A nonrandomized controlled trial focused on physical activity levels in low‐income women 71. A cluster RCT used an intervention in churches to improve nutrition and physical activity 72. Another cluster RCT compared an intervention of culturally tailored dance and reducing screen time in low‐income African American girls compared with information alone 73. Across studies, we found a medium effect of increased daily expenditure (SMD, 0.26; 95% CI: 0.07 to 0.44; eight trials). There was little evidence of heterogeneity (I 2 44%) and no indication of publication bias (Egger P = 0.37, Begg P = 0.28). Some of the studies targeted adults, and others targeted children 68, 69, 73. The effect estimate for the studies in children was lower, and the effect was not statistically significant (SMD, 0.17; 95% CI: −0.17 to 0.51; three RCTs) (Figure 6). A cluster RCT, a comparative effectiveness study, and a pre‐post study could not be combined with the other studies (Supporting Information Table S7).
Figure 6.
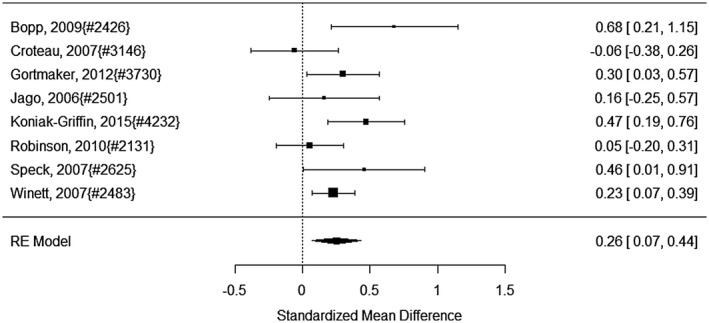
Estimated effects of social‐group approaches on energy expended.
We determined the quality of evidence to be moderate that interventions increase physical activity using established social groups (downgraded because of inconsistency).
Other studies
Supporting Information Table S7 lists the individual studies not contributing to the effect estimates and shows studies categorized as “other” interventions because they did not describe how participants were recruited or they paid university students to participate in an experiment. The references for these interventions are listed in Supporting Information Table S8.
Discussion
This systematic review included 99 studies across a diverse set of public health approaches to prevent obesity. Despite the major efforts these studies represent, we found limited evidence that interventions impacted energy intake and expenditure. Empirical evidence for changes in energy consumption or expenditure was sparse within intervention categories, and findings across studies often varied considerably. In many cases, we were unable to estimate effect sizes because studies provided insufficient details.
Health education campaigns made up the largest proportion of studies. The small pooled effect in reduced energy intake and the estimated effect of increasing energy expenditure suggest education programs reaching unselected participant samples can impact energy consumed and physical activity. Education programs are appealing because they can largely be delivered across large populations with relatively low cost. Yet the lack of tailoring to different groups of people with varying priorities and barriers to healthy lifestyles likely limits their ability to change behavior.
Despite literature searches in multiple sources, we did not identify food‐labeling studies reporting on outcomes of interest. Existing food‐labeling studies primarily focused on changes in food purchasing. While some promising evidence suggests that changing food labeling may improve food purchasing choices 74 without assessing changes in diet, it remains unknown whether and to what extent such interventions might reduce obesity. This lack of evidence is especially relevant given the US Food and Drug Administration Commissioner’s recent statement introducing federal food‐labeling legislation 75.
Energy expenditure and intake outcomes were not reported across all intervention types. The intervention delivery approach drives which side of the energy balance equation can be targeted. For example, interventions that modified the physical environment and mode of transportation assessed impacts only on physical activity. However, the interventions that employed education and behavior‐change support in broad social and situational contexts where people spend significant amounts of time were able to assess impacts on both energy intake and expenditure. These interventions included work site interventions, population health care interventions, school‐based interventions, health education, and social‐group interventions.
Population‐based health care initiatives had the largest effect on reducing energy expenditure. The dietary interventions reached large audiences and were delivered either through clinics or online, but all were tailored to target behavior change for specific groups, such as low‐income postpartum women 28 or urban adolescents 31.
Social‐group interventions also showed promising effects on energy expenditure. This is consistent with conceptual behavior‐change models (e.g., social‐ecological model) 76, 77 that address the importance of social factors and support for maintaining or increasing physical activity. Understanding how dietary choices are made in the context of personal and social influences that interact is critical to reducing obesity.
In this review, the interventions that included children were population health care, school‐based, education, and social‐group approaches. Despite possible plateaus in the prevalence of childhood obesity 78, rates are still high, and severe obesity is emerging as the fastest growing category of childhood obesity 79, 80, 81. Thus, effective interventions to improve energy balance for children early in life are still needed to prevent child and adult obesity. The only significant effect for children was reducing energy intake through school‐based interventions. The school‐based studies that examined effects on energy consumption were one of the few areas in which the quality of evidence was graded as moderate. School‐based interventions may have more traction than other types of interventions to effect behavior change. Children must attend school, and if the intervention is part of a curriculum, then their participation is essentially guaranteed. Moreover, schools are settings where children spend the majority of their day, consume about 30% of their calories from the school lunch alone 82, and have opportunities for physical activity. All these reasons point to schools as being potent settings to intervene on diet and physical activity. Moreover, parental involvement, beyond consent, in an obesity intervention has been suggested to improve its effectiveness 83, 84. Parents have integral relationships with schools and may be more inclined to participate with their child in an intervention if it is embedded within a school with school leadership support. While we did not see a significant effect of the school‐based interventions on physical activity, these studies had inconsistent findings and were graded as low. The variation could reflect the limited opportunities students have to be physically active at school (e.g., recess, physical education), so there is less time to increase child activity during their school day.
Even the statistically significant effect estimates were relatively small in magnitude. This may follow from the unique nature of the interventions. Modifying the built and social environments will change energy balance only distally. That is, many steps or choices happen between the environmental change and a person’s decision to consume what type of and how much food and how physically active they will be. Small effects will be difficult to detect without adequate samples; therefore, many of the studies we reviewed may be underpowered. That is not to say that investigators did not present adequate power estimates. All RCTs included power calculations; however, BMI was often the primary outcome assessed. It may be that because BMI is a consequence of energy balance and further downstream from the intervention, proximal energy intake and expenditure should be considered the primary outcome in power and sample size estimates.
The studies we reviewed relied on recruited participants, so findings may be vulnerable to selection bias. Socially disadvantaged populations have historically been underrepresented in health research 85, 86 which not only threatens generalizability but, often, the missing groups are also those with a high burden of disease. An assessment of selection bias in the reviewed studies is beyond the scope of this paper; however, the evidence should be considered in light of this limitation. We also recognize that our energy intake and expenditure reporting requirement excluded other types of relevant population‐level interventions (e.g., advertising restrictions) 87.
In addition to estimating the effects of included studies, our review identified a critical gap in the literature. Out of hundreds of potentially relevant studies, we had to exclude more than 90% because they did not meet our inclusion criteria, primarily because they did not measure or report energy consumption or expenditure. However, understanding effects on energy consumption and expenditure is needed if we are to understand obesity intervention effects and potential intervention targets.
A major challenge is to measure energy intake and expenditure accurately. In particular, population‐based studies rely on self‐reported food intake. Even 24‐hour dietary recalls that are considered to be the best method to collect usual intakes are very limited by misreporting 88 and the limited nutrient databases relative to the massive number of items available for consumption 89. Thus, developing new technologies to collect the types and amounts of foods and beverages people eat in real time is sorely needed to significantly improve the accuracy with which we can measure diet. Moreover, we acknowledge that even measurement accuracy is not all that is needed to understand effects of environmental change on energy balance. We noted how the intervention target determined whether energy intake or expenditure was measured. Changes in energy balance and body weight cannot be predicted from a change in a single component of energy balance. People’s physical activity and dietary behaviors are intertwined, and an intervention that targets either energy intake or expenditure could lead to compensation such that people change their behavior in the other energy balance component. Thus, studies to reduce obesity need affordable methods to objectively measure both physical activity and energy intake simultaneously across all types of studies accurately.
With technological advances, researchers may be able to better collect dietary and activity data in real time. Linking people in place and time by capturing high‐quality space‐time‐behavior data (e.g., using global positioning systems) is a promising approach. For example, ecological momentary assessment is a technique to collect repeated samples of people’s behaviors and experiences in real time and in their natural environment 90, and it can integrate psychosocial aspects with contextual experiences, such as who is with the subject and current feelings. Linking ecological momentary assessment with mobile dietary recording or accelerometry may facilitate collecting these critical data across all intervention settings.
New methods may also help assess multiple cross‐sectoral and environmental efforts with small effects. For example, mental models approach is a multistage, mixed methods approach to understanding and influencing people’s decision processes 91 and can provide a framework to conceptualize where, what, why, and with whom people purchase and consume food or choose an activity. By building a model of influences for a particular choice or set of choices, researchers can better understand the chain of events and decisions (e.g., diet, physical activity) in complex environments.
Conclusion
Understanding the impact of public health obesity interventions on energy balance is critical to reducing obesity. Despite current research on obesity prevention, very few studies provide relevant information on energy intake and expenditure. Existing evidence with statistically significant effects to inform policies is limited. We found school‐based approaches and health care initiatives reduced energy consumed, education reduced energy consumed and increased energy expended, and social‐group approaches increased energy expenditure, but effects were small to moderate. We recommend future research address the divide between public health obesity interventions and energy balance to clarify how prevention and treatment efforts fail and succeed.
Supporting information
Acknowledgments
We thank Patty Smith for administrative assistance and Laura Raaen for her assistance reviewing the literature.
Funding agencies: This paper was supported by the National Institute of Child Health and Human Development grant R01HD087257.
Disclosure: The authors declared no conflicts of interest.
References
- 1. Finucane MM, Stevens GA, Cowan MJ, et al.; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index). National, regional, and global trends in body‐mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country‐years and 9.1 million participants. Lancet 2011;377:557‐567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Flegal KM, Kruszon‐Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284‐2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806‐814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes (Lond) 2013;37:889‐891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hales CMCM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015‐2016. NCHS Data Brief, no. 288. Hyattsville, MD: National Center for Health Statistics; 2017. [Google Scholar]
- 7. National Institutes of Health . Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). Research Portfolio Online Reporting Tools (RePORT) website. https://report.nih.gov/categorical_spending.aspx. Published April 19, 2019. [Google Scholar]
- 8. Butland B, Jebb S, Kopelman P, et al.; Government Office for Science. Tackling Obesities: Future Choices – Project Report. 2nd ed. London, UK: Department of Innovation Universities and Skills; 2007. [Google Scholar]
- 9. World Health Organization . Interventions on Diet and Physical Activity: What Works. Geneva: WHO; 2009. [PubMed] [Google Scholar]
- 10. Harnack L, Oakes JM, Elbel B, Beatty T, Rydell S, French S. Effects of subsidies and prohibitions on nutrition in a food benefit program: a randomized clinical trial. JAMA Intern Med 2016;176:1610‐1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dubowitz T, Ghosh‐Dastidar M, Cohen DA, et al. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Aff (Millwood) 2015;34:1858‐1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elbel B, Moran A, Dixon LB, et al. Assessment of a government‐subsidized supermarket in a high‐need area on household food availability and children's dietary intakes. Public Health Nutr 2015;18:2881‐2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kegler MC, Haardorfer R, Alcantara IC, et al. Impact of improving home environments on energy intake and physical activity: a randomized controlled trial. Am J Public Health 2016;106:143‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ebbeling CB, Feldman HA, Chomitz VR, et al. A randomized trial of sugar‐sweetened beverages and adolescent body weight. New Engl J Med 2012;367:1407‐1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rodriguez‐Ramirez S, Gonzalez de Cosio T, Mendez MA, et al. A water and education provision intervention modifies the diet in overweight Mexican women in a randomized controlled trial. J Nutr 2015;145:1892‐1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aldana SG, Greenlaw RL, Diehl HA, Salberg A, Merrill RM, Ohmine S. The effects of a worksite chronic disease prevention program. J Occup Environ Med 2005;47:558‐564. [DOI] [PubMed] [Google Scholar]
- 17. Touger‐Decker R, Denmark R, Bruno M, O'Sullivan‐Maillet J, Lasser N. Workplace weight loss program; comparing live and internet methods. J Occup Environ Med 2010;52:1112‐1118. [DOI] [PubMed] [Google Scholar]
- 18. Stroebele N, de Castro JM, Stuht J, Catenacci V, Wyatt HR, Hill JO. A small‐changes approach reduces energy intake in free‐living humans. J Am Coll Nutr 2009;28:63‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. French SA, Harnack LJ, Hannan PJ, Mitchell NR, Gerlach AF, Toomey TL. Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev Med 2010;50:180‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thorndike AN, Mills S, Sonnenberg L, et al. Activity monitor intervention to promote physical activity of physicians‐in‐training: randomized controlled trial. PLoS One 2014;9:e100251. doi: 10.1371/journal.pone.0100251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Poirier J, Bennett WL, Jerome GJ, et al. Effectiveness of an activity tracker‐ and internet‐based adaptive walking program for adults: a randomized controlled trial. J Med Internet Res 2016;18:e34. doi: 10.2196/jmir.5295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Taylor WC, Paxton RJ, Shegog R, et al. Impact of booster breaks and computer prompts on physical activity and sedentary behavior among desk‐based workers: a cluster‐randomized controlled trial. Prev Chronic Dis 2016;13:E155. doi: 10.5888/pcd13.160231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Warren BS, Maley M, Sugarwala LJ, Wells MT, Devine CM. Small steps are easier together: a goal‐based ecological intervention to increase walking by women in rural worksites. Prev Med 2010;50:230‐234. [DOI] [PubMed] [Google Scholar]
- 24. Beresford SA, Johnson KC, Ritenbaugh C, et al. Low fat dietary pattern and risk of colorectal cancer: the Women’s Health Initiative Randomised Controlled Dietary Modification Trial. J Am Med Assoc 2006;295:643‐654. [DOI] [PubMed] [Google Scholar]
- 25. Kraschnewski JL, Stuckey HL, Rovniak LS, et al. Efficacy of a weight‐loss website based on positive deviance. A randomized trial. Am J Prev Med 2011;41:610‐614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ockene IS, Tellez TL, Rosal MC, et al. Outcomes of a Latino community‐based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. Am J Public Health 2012;102:336‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ostbye T, Krause KM, Lovelady CA, et al. Active Mothers Postpartum: a randomized controlled weight‐loss intervention trial. Am J Prev Med 2009;37:173‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Phelan S, Hagobian T, Brannen A, et al. Effect of an internet‐based program on weight loss for low‐income postpartum women: a randomized clinical trial. JAMA 2017;317:2381‐2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Riebe D, Blissmer B, Greene G, et al. Long‐term maintenance of exercise and healthy eating behaviors in overweight adults. Prev Med 2005;40:769‐778. [DOI] [PubMed] [Google Scholar]
- 30. Rosenberg DE, Norman GJ, Sallis JF, Calfas KJ, Patrick K. Covariation of adolescent physical activity and dietary behaviors over 12 months. J Adolesc Health 2007;41:472‐478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Black MM, Hager ER, Le K, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics 2010;126:280‐288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wylie‐Rosett J, Swencionis C, Ginsberg M, et al. Computerized weight loss intervention optimizes staff time: the clinical and cost results of a controlled clinical trial conducted in a managed care setting. J Am Diet Assoc 2001;101:1155‐1162; quiz 1163‐1164. [DOI] [PubMed] [Google Scholar]
- 33. Caballero B, Clay T, Davis SM, et al. Pathways: a school‐based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr 2003;78:1030‐1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Casazza K, Ciccazzo M. The method of delivery of nutrition and physical activity information may play a role in eliciting behavior changes in adolescents. Eat Behav 2007;8:73‐82. [DOI] [PubMed] [Google Scholar]
- 35. Foster GD, Sherman S, Borradaile KE, et al. A policy‐based school intervention to prevent overweight and obesity. Pediatrics 2008;121:e794‐e802. [DOI] [PubMed] [Google Scholar]
- 36. Pbert L, Druker S, Barton B, et al. A school‐based program for overweight and obese adolescents: a randomized controlled trial. J Sch Health 2016;86:699‐708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Quinn LJ, Horacek TM, J. C. The impact of COOKSHOP on the dietary habits and attitudes of fifth graders. Top Clin Nutr 2003;18:42‐48. [Google Scholar]
- 38. Taber DR, Chriqui JF, Chaloupka FJ. Differences in nutrient intake associated with state laws regarding fat, sugar, and caloric content of competitive foods. Arch Pediatr Adolesc Med 2012;166:452‐458. [DOI] [PubMed] [Google Scholar]
- 39. Aburto NJ, Fulton JE, Safdie M, Duque T, Bonvecchio A, Rivera JA. Effect of a school‐based intervention on physical activity: cluster‐randomized trial. Med Sci Sports Exerc 2011;43:1898‐1906. [DOI] [PubMed] [Google Scholar]
- 40. Morgan PJ, Saunders KL, Lubans DR. Improving physical self‐perception in adolescent boys from disadvantaged schools: psychological outcomes from the Physical Activity Leaders randomized controlled trial. Pediatr Obes 2012;7:e27‐e32. [DOI] [PubMed] [Google Scholar]
- 41. Goran MI, Reynolds K. Interactive multimedia for promoting physical activity (IMPACT) in children. Obes Res 2005;13:762‐771. [DOI] [PubMed] [Google Scholar]
- 42. Manley D, Cowan P, Graff C, et al. Self‐efficacy, physical activity, and aerobic fitness in middle school children: examination of a pedometer intervention program. J Pediatr Nurs 2014;29:228‐237. [DOI] [PubMed] [Google Scholar]
- 43. Webber LS, Catellier DJ, Lytle LA, et al. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med 2008;34:173‐184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zizzi A, Vitullo E, Rye J, et al. Impact of a three‐week pedometer intervention on high school students0 daily step counts and perceptions of physical activity. Am J Health Educ 2006;37:35‐40. [Google Scholar]
- 45. Schetzina KE, Dalton WT 3rd, Lowe EF, et al. A coordinated school health approach to obesity prevention among Appalachian youth: the Winning with Wellness Pilot Project. Fam Community Health 2009;32:271‐285. [DOI] [PubMed] [Google Scholar]
- 46. Aldana SG, Greenlaw RL, Diehl HA, et al. Effects of an intensive diet and physical activity modification program on the health risks of adults. J Am Diet Assoc 2005;105:371‐381. [DOI] [PubMed] [Google Scholar]
- 47. Baranowski T, Baranowski J, Thompson D, et al. Video game play, child diet, and physical activity behavior change a randomized clinical trial. Am J Prev Med 2011;40:33‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cussler EC, Teixeira PJ, Going SB, et al. Maintenance of weight loss in overweight middle‐aged women through the Internet. Obesity (Silver Spring) 2008;16:1052‐1060. [DOI] [PubMed] [Google Scholar]
- 49. Elder JP, Ayala GX, Campbell NR, et al. Long‐term effects of a communication intervention for Spanish‐dominant Latinas. Am J Prev Med 2006;31:159‐166. [DOI] [PubMed] [Google Scholar]
- 50. Foster‐Schubert KE, Alfano CM, Duggan CR, et al. Effect of diet and exercise, alone or combined, on weight and body composition in overweight‐to‐obese postmenopausal women. Obesity (Silver Spring) 2012;20:1628‐1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Klesges RC, Obarzanek E, Kumanyika S, et al. The Memphis Girls' health Enrichment Multi‐site Studies (GEMS): an evaluation of the efficacy of a 2‐year obesity prevention program in African American girls. Arch Pediatr Adolesc Med 2010;164:1007‐1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Radakovich K, Heilbrun LK, Venkatranamamoorthy R, Lababidi S, Klurfeld DM, Djuric Z. Women participating in a dietary intervention trial maintain dietary changes without much effect on household members. Nutr Cancer 2006;55:44‐52. [DOI] [PubMed] [Google Scholar]
- 53. Simkin‐Silverman LR, Wing RR, Boraz MA, Kuller LH. Lifestyle intervention can prevent weight gain during menopause: results from a 5‐year randomized clinical trial. Ann Behav Med 2003;26:212‐220. [DOI] [PubMed] [Google Scholar]
- 54. Stice E, Rohde P, Shaw H, Marti CN. Efficacy trial of a selective prevention program targeting both eating disorders and obesity among female college students: 1‐ and 2‐year follow‐up effects. J Consult Clin Psychol 2013;81:183‐189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Barkin SL, Heerman WJ, Sommer EC, et al. Effect of a behavioral intervention for underserved preschool‐age children on change in body mass index a randomized clinical trial. JAMA 2018;320:450‐460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Anderson‐Bill ES, Winett RA, Wojcik JR, Winett SG. Web‐based guide to health: relationship of theoretical variables to change in physical activity, nutrition and weight at 16‐months. J Med Internet Res 2011;13:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Benezra LM, Nieman DC, Nieman CM, et al. Intakes of most nutrients remain at acceptable levels during a weight management program using the food exchange system. J Am Diet Assoc 2001;101:554‐561. [DOI] [PubMed] [Google Scholar]
- 58. Suboc TB, Strath SJ, Dharmashankar K, et al. Relative importance of step count, intensity, and duration on physical activity's impact on vascular structure and function in previously sedentary older adults. J Am Heart Assoc 2014;3:e000702. doi: 10.1161/JAHA.113.000702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bickmore TW, Schulman D, Sidner C. Automated interventions for multiple health behaviors using conversational agents. Patient Educ Couns 2013;92:142‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Krummel D, Semmens E, MacBride AM, Fisher B. Lessons learned from the mothers' overweight management study in 4 West Virginia WIC offices. J Nutr Educ Behav 2010;42(3 suppl):S52‐S58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Varma VR, Tan EJ, Gross AL, et al. Effect of community volunteering on physical activity: a randomized controlled trial. Am J Prev Med 2016;50:106‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mailey E, McAuley E. Impact of a brief intervention on physical activity and social cognitive determinants among working mothers: a randomized trial. J Behav Med 2014;37:343‐355. [DOI] [PubMed] [Google Scholar]
- 63. Leahey TM, Crane MM, Pinto AM, Weinberg B, Kumar R, Wing RR. Effect of teammates on changes in physical activity in a statewide campaign. Prev Med 2010;51:45‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Burney J, Haughton B. EFNEP: a nutrition education program that demonstrates cost‐benefit. J Am Diet Assoc 2002;102:39‐45. [DOI] [PubMed] [Google Scholar]
- 65. Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep 2001;116(suppl 1):68‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bopp M, Wilcox S, Laken M, et al. 8 Steps to Fitness: a faith‐based, behavior change physical activity intervention for African Americans. J Phys Act Health 2009;6:568‐577. [DOI] [PubMed] [Google Scholar]
- 67. Croteau KA, Richeson NE, Farmer BC, Jones DB. Effect of a pedometer‐based intervention on daily step counts of community‐dwelling older adults. Res Q Exerc Sport 2007;78:401‐406. [DOI] [PubMed] [Google Scholar]
- 68. Gortmaker SL, Lee RM, Mozaffarian RS, et al. Effect of an after‐school intervention on increases in children's physical activity. Med Sci Sports Exerc 2012;44:450‐457. [DOI] [PubMed] [Google Scholar]
- 69. Jago R, Baranowski T, Baranowski JC, et al. Fit for Life Boy Scout badge: outcome evaluation of a troop and Internet intervention. Prev Med 2006;42:181‐187. [DOI] [PubMed] [Google Scholar]
- 70. Koniak‐Griffin D, Brecht ML, Takayanagi S, Villegas J, Melendrez M, Balcazar H. A community health worker‐led lifestyle behavior intervention for Latina (Hispanic) women: feasibility and outcomes of a randomized controlled trial. Int J Nurs Stud 2015;52:75‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Speck BJ, Hines‐Martin V, Stetson BA, Looney SW. An environmental intervention aimed at increasing physical activity levels in low‐income women. J Cardiovasc Nurs 2007;22:263‐271. [DOI] [PubMed] [Google Scholar]
- 72. Winett RA, Anderson ES, Wojcik JR, Winett SG, Bowden T. Guide to health: nutrition and physical activity outcomes of a group‐randomized trial of an Internet‐based intervention in churches. Ann Behav Med 2007;33:251‐261. [DOI] [PubMed] [Google Scholar]
- 73. Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low‐income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med 2010;164:995‐1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sturm R, Huang HC, Tsang F, et al. Examining Consumer Responses to Calorie Information on Restaurant Menus in a Discrete Choice Experiment. Santa Monica, CA: RAND Corporation; 2018. [Google Scholar]
- 75. US Food and Drug Administration . Statement from FDA Commissioner Scott Gottlieb, M.D., on the public health benefits from enactment of menu labeling. https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-public-health-benefits-enactment-menu-labeling. Published May 7, 2018.
- 76. Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol 1977;32:513‐531. [Google Scholar]
- 77. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351‐377. [DOI] [PubMed] [Google Scholar]
- 78. Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988‐1994 through 2013‐2014. JAMA 2016;315:2292‐2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007‐2008. JAMA 2010;303:242‐249. [DOI] [PubMed] [Google Scholar]
- 80. Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr 2009;9:322‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Claire Wang Y, Gortmaker SL, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976‐2006. Int J Pediatr Obes 2011;6:12‐20. [DOI] [PubMed] [Google Scholar]
- 82. Food and Nutrition Service . School Nutrition Dietary Assessment Study‐III: Volume II: Student Participation and Dietary Intakes. Alexandria, VA: U.S. Department of Agriculture; 2007. [Google Scholar]
- 83. Golley RK, Hendrie GA, Slater A, Corsini N. Interventions that involve parents to improve children's weight‐related nutrition intake and activity patterns ‐ what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obes Rev 2011;12:114‐130. [DOI] [PubMed] [Google Scholar]
- 84. Stice E, Shaw H, Marti CN. A meta‐analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull 2006;132:667‐691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. National Institutes of Health . NIH Policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research; https://grants.nih.gov/policy/inclusion/women-and-minorities/guidelines.htm. Published October 9, 2001. [Google Scholar]
- 86. Heiat A, Gross CP, Krumholz HM. Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med 2002;162:1682‐1688. [DOI] [PubMed] [Google Scholar]
- 87. World Cancer Research Fund International . NOURISHING database. https://www.wcrf.org/int/policy/nourishing-database. 2019.
- 88. Johnson RK. Dietary intake ‐ how do we measure what people are really eating? Obes Res 2002;10(suppl 1):63S‐68S. [DOI] [PubMed] [Google Scholar]
- 89. Poti JM, Yoon E, Hollingsworth B, et al. Development of a food composition database to monitor changes in packaged foods and beverages . J Food Compost Anal 2017;64:18‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol 2008;4:1‐32. [DOI] [PubMed] [Google Scholar]
- 91. Morgan MG, Fischhoff B, Bostrom A, Atman CJ. Risk Communication: A Mental Models Approach. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


