ABSTRACT
Background: Young children may be adversely impacted by separation from and loss of caregivers and other loved ones. Such experiences often co-occur with interpersonal violence, unpredictability and other traumas. Whether separation/loss has unique effects independent of those other adversities is not known.
Objective: This study aimed to establish whether separation/loss is associated with trauma-related symptoms, psychiatric disorders, and functional impairment in 18- to 48-month-old children independent of other adversities.
Methods: Data from a cross-sectional community and clinical cohort were analyzed. Recruitment occurred in pediatric primary care, mental health, and developmental services sites. Children (33% female) were heterogeneous in ethnic background (55% minority) and family socioeconomic status (40% living in poverty).
Results: Separation/loss was common (30.9% single type, 15.0% multiple types) and frequent amongst violence-exposed children (84.4% of violence-exposed children had experienced separation/loss from a loved one). However, violence exposure was uncommon amongst children with separation/loss experiences (only 23.9% were violence-exposed). Separation/loss was significantly associated with symptoms of posttraumatic stress and reactive attachment, as well as impairment and psychiatric disorders in models that controlled for sociodemographic and contextual risks, including other traumas. Psychiatric disorders were approximately 2.5 times more likely in children who had experienced multiple separations/losses, after accounting for interpersonal violence which was also significant.
Conclusion: Professionals working with young children, policy-makers and caregivers should be aware that an accumulation of caregiver separations/losses, irrespective of violence and other traumatic exposure, may have detrimental effects on young children especially in the context of prior separations/losses or disruptions in their lives.
KEYWORDS: Separation, loss, interpersonal violence, non-interpersonal trauma, trauma symptoms, psychiatric disorder, impairment, infant, toddler
HIGHLIGHTS
• Findings link multiple separations from or losses of primary caregivers and other loved ones with trauma-related symptoms, reactive attachment symptoms, impairment, and psychiatric disorders in 18–48 month-olds.• Associations are independent of the effects of interpersonal violence and other traumas.• Routine screening may be warranted to identify young children who have experienced multiple separations/losses and are manifesting enduring symptoms that merit referral to mental health professionals for further evaluation of the need for trauma-informed therapeutic services.
Abstract
Antecedentes: los niños pequeños pueden verse afectados negativamente por la separación y la pérdida de los cuidadores y otros seres queridos. Tales experiencias a menudo se producen conjuntamente con la violencia interpersonal, la imprevisibilidad y otros traumas. Se desconoce si la separación/pérdida tiene efectos únicos independientes de esas otras adversidades.
Objetivo: Este estudio tuvo como objetivo establecer si la separación/pérdida está asociada con síntomas relacionados con el trauma, trastornos psiquiátricos y deterioro funcional en niños de 18 a 48 meses de edad, independientemente de otras adversidades.
Métodos: Se analizaron datos de una comunidad de corte transversal y una cohorte clínica. El reclutamiento se realizó en los centros de atención primaria pediátrica, salud mental y servicios de desarrollo. Los niños (33% mujeres) eran heterogéneos en cuanto a antecedentes étnicos (55% de minorías) y estatus socioeconómico familiar (40% que viven en la pobreza). Resultados: la separación/pérdida fue común (30.9% tipo único, 15.0% tipos múltiples) y frecuente entre los niños expuestos a la violencia ((84.4% de los niños expuestos a la violencia habían experimentado la separación/pérdida de un ser querido). Sin embargo, la exposición a la violencia fue poco frecuente entre los niños con experiencias de separación/pérdida (solo el 23,9% estaba expuesto a la violencia). La separación/pérdida se asoció significativamente con los síntomas de estrés postraumático y el apego reactivo, así como con el deterioro y los trastornos psiquiátricos en modelos que controlaban riesgos sociodemográficos y contextuales, incluidos otros traumas. Los trastornos psiquiátricos fueron aproximadamente 2.5 veces más probables en los niños que habían sufrido múltiples separaciones/pérdidas, después de considerar la violencia interpersonal, que también fue importante.
Conclusión: Los profesionales que trabajan con niños pequeños, políticos y cuidadores deben ser conscientes de que una acumulación de separaciones/pérdidas de cuidadores, independientemente de la violencia y otras exposiciones traumáticas, puede tener efectos perjudiciales en los niños pequeños, especialmente en el contexto de separaciones/pérdidas previas o interrupciones en sus vidas.
PALABRAS CLAVE: Separación, pérdida, violencia interpersonal, trauma no interpersonal, síntomas de trauma, desorden psiquiátrico, discapacidad, infantil, lactante
儿童与自然灾害
背景:远离和丧失照顾者和其他亲人可能会使幼儿受到不利影响。这些经历经常与人际暴力,不可预测性和其他创伤一同发生。这种分离或丧失是否具有独立于其他暴露的独特效应尚不清楚。
目的:本研究旨在确定18-48个月大的儿童中,分离或丧失是否独立于其他暴露,与创伤相关的症状、精神障碍及功能损伤有关。
方法:分析的横断面数据来自于社区和临床人群。在儿科初级护理、心理健康和发展服务站点招募参与者。招募儿童(33%为女童)的种族背景(55%为少数民族)和家庭社会经济地位(40%生活贫困)具有异质性。
结果:分离或丧失在遭受过暴力的儿童中普遍(30.9%为单一类型,15.0%为多种类型)且频发(84.4%遭受过暴力的儿童经历过与亲人分离或丧失亲人)。然而,在有分离或丧失经历的儿童中,遭受暴力并不普遍(只有23.9%遭受过暴力)。在控制了社会人口学和包括其他创伤的情境风险的模型中,分离或丧失与创伤后应激及反应性依恋的症状、损伤和精神障碍显著相关。在排除了同时也显著的人际暴力的影响之后,经历过多次分离或丧失的儿童罹患精神障碍的可能性大约是正常儿童的2.5倍。
结论:与幼儿、政策制定者和照顾者一起工作的专业人员应该意识到,无论是否遭受暴力和其他创伤暴露,与照顾者的分离或丧失的暴露叠加都可能对幼儿产生不利影响,特别是在以前经历过分离或丧失或者生活中的干扰事件的情况下。
关键词: 分离, 丧失, 人际暴力, 非人际创伤, 创伤症状, 精神障碍, 损伤, 婴儿, 幼儿
1. Introduction
Loss of and separation from primary caregivers may profoundly impact young children’s mental health. Traumatic loss refers to the sudden, unexpected loss of a loved one due to death, harm or illness or abandonment. Serious negative effects on mental health have been documented in young children who have experienced traumatic losses such as institutionalization, parental death or abandonment, or separation from parents due to war and civil unrest (Bowlby, 1982, 1980, 1973; Feldman & Vengrober, 2011; Lieberman, Compton, Van Horn, & Ghosh Ippen, 2003; Zeanah et al., 2009). Prolonged separations have been shown to negatively affect the emotional and behavioral functioning of young children following maternal incarceration (age 2–7 years) and parental military deployment (age 0–4 years) (Barker & Berry, 2009; Poehlmann, 2005). The adverse psychosocial impact on children of immigration-related family separations have also been documented (Gindling & Poggio, 2012; Santa-Maria & Cornille, 2007; Suárez-Orozco, Bang, & Kim, 2011), but the effects on young children have not been systematically investigated. Young children also may be affected by separations that do not rise to the DSM-based definition of traumatic loss, such as separation due to caregiver travel, caregiver hospitalization, or parental divorce/separation. While adults may perceive these types of separation as predictable, they may be very stressful for young children because their developing cognitive capacities limit their understanding that separations are temporary and the loved one will return. For young children these experiences may be analogous to physical ambiguous loss, which includes situations of unclear and unresolved loss in which a loved one is absent and their return is uncertain because the family does not know if they are dead or alive (Boss, 2016). Available data, though very limited, suggest that such separations may increase children’s risk for emotional and behavioral problems (Adam & Chase-Lansdale, 2002; Crawford, Cohen, Chen, Anglin, & Ehrensaft, 2009; Howard, Martin, Berlin, & Brooks-Gunn, 2011). In one study, infants and toddlers who were separated from their mothers for a week or longer subsequently showed modestly elevated aggression and negativity toward their mothers as preschoolers (Howard et al., 2011). Other research has shown that infants/toddlers who were exposed to repeated laboratory separations show greater distress upon later separations, suggesting that they retain memories of and are distressed by these brief separations, and that they may have a cumulative impact (Mueller et al., 2018). However, the effects on young children’s mental health of single or multiple incidents of separations have not been well investigated.
Separations/losses may occur in combination with or as a consequence of traumatic experiences. For example, partner violence may lead a caregiver to leave the home, divorce/separation, caregiver incarceration or caregiver hospitalization. Illness or injuries from non-interpersonal traumas, such as accidents, may lead to caregiver hospitalization. Considerable research now documents post-traumatic stress symptoms and other emotional and behavioral problems in young children exposed to violence (Bogat, DeJonghe, Levendosky, Davidson, & von Eye, 2006; Briggs-Gowan et al., 2010; Briggs-Gowan, Carter, & Ford, 2012; Briggs-Gowan et al., 2018; Grasso, Ford, & Briggs-Gowan, 2013; Grasso et al., 2016; Koolick et al., 2016; Levendosky, Huth-Bocks, Semel, & Shapiro, 2002; Lieberman, 2007; Mongillo, Briggs-Gowan, Ford, & Carter, 2009; Schechter, Willheim, Suardi, & Serpa, 2019) and non-interpersonal traumas (Briggs-Gowan et al., 2010; Meiser-Stedman, Smith, Glucksman, Yule, & Dalgleish, 2008; Scheeringa, 2009), highlighting the need to also consider the impact of these experiences when studying the effects of separation/loss.
This study tests the hypothesis that an accumulation of experiences of separations/losses from caregivers and other loved ones is associated with trauma-related symptoms, psychiatric disorders, and impairment in young children, independent of sociodemographic covariates and other trauma exposures known to increase mental health symptoms.
2. Methods
2.1. Participants
Participants were 246 parents and their 18- to 48-month-old children. Families were recruited from clinical sites (mental health, developmental assessment/service) (n= 111) and community settings in the same communities (n= 135) in the Northeastern and Midwestern U.S. Children with Autism Spectrum disorders, neurological conditions, global cognitive delays were ineligible, and other severe developmental or medical conditions (e.g., congenital diaphragmatic hernia, cancer) were excluded. Parents of 306 eligible children consented, 270 participated, and 24 were excluded from analyses due to incomplete exposure or symptom data. The final sample of 246 represented 80.4% of eligible consented participants.
Mean child age was 32.5 months (±8.0). The majority were boys (67.1%). Participants were diverse ethnoracially (45.1% non-Hispanic White, 28.1% African American/Black, 14.2% Hispanic/Latino, 12.6% other minority) and socioeconomically (40.4% with family incomes below or within 180% of the poverty level). Most children came from two-parent homes (70.9%). Parents were primarily biological parents (86.5% biological mother, 4.5% biological father, 5.7% adoptive/foster parent, 3.3% grandparent/other). Mean parental age was 33.9 years (Std = 7.8). Respondent education varied (11.4% <high school, 18.7% high school/GED, 25.6% some college, 42.7% >college degree, 1.6% not reported). Mean child intelligence quotient was 94.7 (Std = 19.9) on the Mullen Scales of Early Learning, according to chart reviews and study testing; thus, average developmental scores were in the normative range despite some of the sample being recruited from clinical sites. Children from clinical and community sites were similar in ethnicity, poverty status, two-parent home status, and respondent education, as well as separation/loss, violence, harsh parenting, and non-interpersonal trauma exposures (p > .05); as referral status was not significantly associated with any independent variable of interest, it was not included as a covariate in analyses. Children from clinical sites were on average 2.2 months older and more likely to be male (73.6% vs. 61.8%) (p < .05).
2.2. Procedures
Families learned about the study from clinic staff, research assistants, and posted fliers. Parents completed questionnaires and diagnostic interviews. Ethical guidelines for mandated reporting were followed. Informed consent was obtained, participants were compensated, and procedures were approved by Institutional Review Boards.
2.3. Measures
2.3.1. Trauma exposure
Lifetime exposure to interpersonal and non-interpersonal traumatic events (Table 1) was assessed with the Preschool-Age Psychiatric Assessment (PAPA) (Egger et al., 2006) PTSD section and two Child Life Events Scale (CLES) (Carter & Briggs-Gowan, 1998) questions describing witnessing physical violence or weapon-use towards family members. Interpersonal trauma included physical abuse, sexual abuse, and witnessed violence. As only one child had experienced sexual abuse only, we refer to children who had experienced any form of interpersonal trauma as violence-exposed. Non-interpersonal trauma included accidental fall, burn, vehicular accident, poisoning, near drowning, animal attack, natural disaster and fire. Few children had experienced multiple types of either non-interpersonal (n = 6) or interpersonal trauma (n = 3). Therefore, binary variables reflecting any non-interpersonal trauma and any violent trauma were generated.
Table 1.
Frequencies of separation/loss, violence exposure, and non-interpersonal trauma events.
| N | % | |
|---|---|---|
| Non-interpersonal Trauma | ||
| Serious accidental fall | 12 | 4.9 |
| Accidental burn | 16 | 6.5 |
| Vehicular accident | 4 | 1.6 |
| Poisoning | 4 | 1.6 |
| Near drowning | 2 | 0.8 |
| Animal attack | 1 | 0.4 |
| Natural disaster or Fire | 2 | 0.8 |
| Total Number of Types of Non-interpersonal Trauma | ||
| 0 | 211 | 85.8 |
| 1 | 29 | 11.8 |
| 2 | 6 | 2.4 |
| Interpersonal Violence | ||
| Witnessed violence | 29 | 11.8 |
| Physical violence/abuse or sexual abuse | 6 | 2.4 |
| Total Number of Types of Interpersonal Violence | ||
| 0 | 214 | 87.0 |
| 1 | 29 | 11.8 |
| 2 | 3 | 1.2 |
| Separation/loss in the Full Sample | ||
| Caregiver separation (separated from parent ≥1 week or parent hospitalized for > 24 hours) | 81 | 32.9 |
| Death of loved one | 38 | 14.1 |
| Separation/divorce | 26 | 10.6 |
| Other separation/loss (caregiver or other loved one moved without further contact) | 9 | 3.7 |
| ‘Any’ prolonged loss/separation (death, separation/divorce, other) | 63 | 25.6 |
| Total Number of Types of Separation/Loss in the Full Sample | ||
| 0 | 133 | 54.1 |
| 1 | 76 | 30.9 |
| 2 | 34 | 13.8 |
| 3 | 3 | 1.2 |
| Separation/loss in the Single Occurrence Group (N = 76) | ||
| Caregiver separation | 50 | 65.8 |
| Death of loved one | 15 | 19.7 |
| Separation/divorce | 8 | 10.5 |
| Other separation/loss | 3 | 4.0 |
| ‘Any’ prolonged separation/loss (death, separation/divorce, other) | 26 | 34.2 |
| Separation/loss in the multiple occurrence group (N = 37) | ||
| Caregiver separation | 31 | 83.8 |
| Death of adult loved one | 22 | 59.5 |
| Separation/divorce | 18 | 48.7 |
| Other separation/loss | 6 | 16.2 |
| ‘Any’ prolonged separation/loss (death, separation/divorce, other) | 37 | 100.0 |
2.3.2. Harsh parenting
Parents’ responses on the 7 item O’Leary Parenting Scale (Arnold, O’Leary, Wolff, & Acker, 1993) provided an indicator of their own harsh, over-reactive parenting in the past month (Cronbach’s Alpha [α] = .68). High scores reflect a tendency to use spanking and other forms of physical punishment, yelling, and out of control behaviors. Analyses utilized continuous and clinical cut-scores (defined as scores 1.5 standard deviations above the mean). All 14 children with harsh parenting scores above the cut-score were reported to have experienced frequent verbal aggression (yelling, insults) and 8 had experienced physical aggression (spank, slap, grab, hit) more than ‘rarely.’
2.3.3. Separation/loss
Separation/loss was defined as a period of separation from or permanent loss of parental caregiver or other significant loved one. Lifetime experiences of death of a loved one, separation from a parent for a week or longer, and divorce/separation of the child’s parents were assessed with the PAPA and CLES. The PAPA Life Stressors Section assessed recent (past 3 months) parental hospitalization for longer than 24 hours, parental arrest, or the loss of a relationship deemed by the parent to be important to the child (e.g., parent, grandparent, other adult, sibling) due to a permanent move without possibility of further contact. A cumulative separation/loss variable was generated (0 = none, 1 = one type, 2 = multiple types). The distribution of types of loss (and non-interpersonal trauma and violence exposure) are shown in Supplemental Figures.
2.3.4. Trauma related symptoms
Parents completed the Trauma Related Symptoms Scales (TRSS) of the Infant-Toddler Social and Emotional Assessment (ITSEA), a developmentally-sensitive measure for children ages 12 to 48 months (Carter & Briggs-Gowan, 2006; Carter, Briggs-Gowan, Jones, & Little, 2003; Mongillo et al., 2009). The TRSS includes subscales for re-experiencing (9 items, α = .47), avoidance/numbing (10 items, α = .66), and hyperarousal (20 items, α = .85) and a total score (39 items, α = .88). Model fit, reliability and validity of the TRSS has been supported in independent research (Briggs-Gowan et al., 2012; Mongillo et al., 2009). The re-experiencing score had marginal internal consistency; such lower reliability may be tolerated when caused by low loadings of items that describe clinically-important but rare behaviors (Achenbach, Edelbrock, & Howell, 1987) as observed here for behaviors such as freezing and regression. Clinically significant (‘Of concern’) trauma-related symptoms were indicated by total scores above the 80th percentile in a normative sample (Mongillo et al., 2009).
2.3.5. PAPA
The PAPA is a developmentally-sensitive, semi-structured interview with established algorithms for assessing psychiatric disorders among children who are 2 to 5 years of age (Briggs-Gowan, Godoy, Heberle, & Carter, 2016; Egger et al., 2006). The PAPA integrates parent-report information with glossary-driven interviewer coding, as such it integrates parent perspectives with clinical judgement. Prior work has established the reliability and validity of the PAPA (Briggs-Gowan et al., 2016; Egger et al., 2006). Common DSM-IV childhood internalizing disorders [Separation Anxiety, Social Phobia, Specific Phobia, Depression/Dysthymia, Depression Not Otherwise Specified (NOS)] and externalizing disorders [Attention-Deficit Hyperactivity Disorder, Disruptive Behavior Disorders (DBDS), i.e., Oppositional Defiant and DBD-NOS] were assessed. Diagnostic data are not available for 1-year-old participants because algorithms are not available for children younger than 2 years. Diagnostic algorithms required full symptom, duration and onset criteria but did not require associated impairment because of our interest in emergent psychopathology in this very young sample; nonetheless, children who met criteria for ‘any’ disorder were substantially more impaired (MN = .57, SD = .05) than those who did not (MN = .25, SD = .03), with very large effect size (η = .1547, p < .0001). A binary variable representing the presence of any psychiatric disorder versus none was constructed for the study.
The PAPA also was used to assess research domain criteria symptoms of Reactive Attachment Disorder (RAD); disorder status is not determined due to the need for clinical data to determine the presence of pathogenic care and rule-out developmental delay/PDD. The Inhibited Symptoms score was based on 7 items (α = .79) reflecting the failure to initiate or respond in a developmentally appropriate manner to most social interactions, as manifested by inhibited behavior, restricted affect, failure to seek comfort when distressed, resistance of comfort, approach/avoidance behavior toward caregivers, and difficulty being affectionate. The Disinhibited Symptoms score was based on 3 items (α = .74) reflecting indiscriminate behavior toward adults, as manifested in minimal checking with caregiver in unfamiliar settings, indiscriminant willingness to leave with an unfamiliar adult and indiscriminant behavior toward adults.
2.3.6. Family Life Impairment Scale (FLIS) (Briggs-Gowan, Horowitz, & Carter, 1998; Mian, Soto, Briggs-Gowan, & Carter, 2018)
Parents completed the FLIS to assess the extent to which the child’s difficult behavior and/or special needs were perceived to interfere with functioning in three areas. Family Impairment assessed limitations in daily routines and social activities typical of families with young children (6 items, α = .85). Childcare Impairment assessed limitations in the use of formal or informal childcare and difficulty finding or retaining appropriate care (4 items, α = .66). Parental Impairment assessed problems in caregiver functioning (4 items, α = .75). Impairment was defined as a continuous score based on the number of FLIS items endorsed (14 items, α = .86). Prior research in other samples of young children has demonstrated acceptable reliability and validity for the FLIS (Mian et al., 2018).
2.3.7. Sociodemographics
Child age and sex, ethnicity, parental education, marital status, income, and receipt of public assistance were assessed by parent report. Poverty status was defined based on Federal income-to-need ratio and/or receipt of public assistance supports requiring incomes below 180% of the poverty line.
2.4. Analytic plan
Sociodemographic characteristics that were significantly associated with both the given dependent variable and one or more independent variable were considered for inclusion as covariates in hypothesis-testing models. Poverty status and minority ethnicity met this criterion (see Table 2). However, the two were highly correlated and only poverty status remained significant when the other variable was controlled in partial correlations; for parsimony, only poverty was a covariate in models. Hypotheses for continuous measures were tested with general linear models with separation/loss (none, single, multiple) as the group variable and continuous symptom or impairment scores as the dependent variables. Models included child age, sex, and poverty status as demographic covariates. To test the specificity of effects to separation/loss versus other traumas and interpersonal adversity, these models also included non-interpersonal trauma, harsh parenting, and violence exposure. To minimize the likelihood of chance findings, we first tested the model for the total score for a given dependent variable (ITSEA, FLIS) and subsequently examined models for individual subscales only if the total score was significant. Pairwise group comparisons were adjusted with the Bonferroni correction. Hypotheses for binary dependent variables reflecting diagnostic status and clinically-concerning trauma symptoms were examined with logistic regression models. Single and multiple separations/losses were included as dummy variables. Due to the low rate of positives for interpersonal violence and clinically-significant harsh parenting, a composite harsh parenting/violence variable was used in these models. To conserve power, the logistic regression models included violence/harsh parenting and non-interpersonal trauma only if they were significantly associated with the outcome on a bivariate basis.
Table 2.
Correlations among study variables.
| |
Demographics |
Exposures |
ITSEA Trauma |
RAD Symptoms |
FLIS Impairment |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Min | Pov | Loss | Viol | Harsh Parent | Non-Int. | Total | Re- exp |
Ars | Avoid | RAD Inhib | RAD Disinh |
Total | Child care |
Family | Parent | |
| Age (older) | .13* | .02 | .05 | .24*** | .12 | .03 | .08 | .06 | .12 | .02 | .03 | .07 | .18*** | .10 | .06 | .07 | .10 |
| Sex (male) | .01 | .04 | .03 | .01 | .04 | .06 | .03 | −.11 | .06 | .12 | .07 | .09 | .03 | .00 | −.01 | .08 | |
| Minority | .45**** | .09 | .16* | −.08 | .02 | .04 | .01 | .01 | .10 | −.06 | −.02 | .10 | .14* | .10 | .00 | ||
| Poverty | .09 | .29**** | −.07 | .07 | .24**** | .16* | .20** | .24**** | .02 | −.05 | .20** | .21*** | .26**** | .03 | |||
| Loss | .39**** | .03 | .06 | .21** | .24**** | .19** | .06 | .13* | .03 | .17** | .15* | .12 | .14* | ||||
| Violence | .08 | .15* | .26**** | .22*** | .23*** | .15* | .13* | .09 | .12 | .13* | .12 | .03 | |||||
| Harsh Parenting | .08 | .26**** | .05 | .31**** | .23*** | .15* | .16* | .21** | .00 | .13* | .36**** | ||||||
| Non-int. Trauma | .15* | .16* | .07 | .15* | .12 | .02 | .06 | .04 | .00 | .10 | |||||||
| Total Trauma Sx | .73**** | .87**** | .77**** | .41**** | .20** | .47**** | .37**** | .46**** | .30**** | ||||||||
| Re-experiencing | .45**** | .32**** | .18** | .05 | .19** | .18** | .11 | .17** | |||||||||
| Arousal | .58**** | .42**** | .21*** | .53**** | .39**** | .38**** | .50**** | ||||||||||
| Avoidance | .37**** | .20** | .37**** | .28**** | .36**** | .25*** | |||||||||||
| RAD Inhibited | .40**** | .29**** | .23*** | .20*** | .25**** | ||||||||||||
| RAD Disinhibited | .27**** | .19** | .27**** | .21** | |||||||||||||
| Total Impairment | .85**** | .80**** | .76**** | ||||||||||||||
| Childcare Impairment | .60**** | .42**** | |||||||||||||||
| Family Impairment | .37**** | ||||||||||||||||
| N | 246 | 246 | 246 | 246 | 246 | 246 | 246 | 246 | 246 | 246 | 246 | 245 | 245 | 241 | 241 | 241 | 241 |
| MN (SD) | .67 (.47) | .55 (.50) | .43 (.49) | .61 (.74) | .13 (.34) | 2.32 (.81) | .14 (.35) | .41 (.23) | .38 (.26) | .65 (.35) | .21 (.24) | .31 (.79) | .12 (.45) | .34 (.37) | .38 (.47) | .26 (.42) | .38 (.48) |
Non-Int. Trauma = non-interpersonal trauma exposure, Re-exp = re-experiencing symptoms, Ars = Arousal symptoms, RAD = Reactive Attachment Disorder.
*p < .05, **p < .01, ***p < .001, ****p < .0001.
3. Results
3.1. Descriptive analyses
In this young sample, child age and sex were minimally and inconsistently associated with symptoms and impairment (see Table 1). However, psychiatric disorders were more common in 3-year-olds (43.8%) than in 2-year-olds (20.9%) (Χ2 = 10.75, p = .0010) and trended toward being more common in boys (33.1%) than girls (18.5%) (Χ2 = 3.40, p = .0653).
3.2. Exposure history
Nearly half of children had experienced separation/loss (30.9% single type, 15.0% multiple types) (see Table 1). Separation from a parent for ≥1 week or parent hospitalization were most common (32.9%), followed by prolonged loss/separation (25.6%). Approximately 13% of children were violence-exposed and 14.2% had experienced non-interpersonal trauma. Separation/loss and violence exposure were positively associated: 84.4% of violence-exposed children had experienced separation/loss (34.4% single separation/loss, 50.0% multiple), Χ2(1,246) = 36.63, p < .0001. However, only 23.9% of children who had experienced separation/loss were violence-exposed (14.5% of single separation/loss, 43.2% of multiple). Non-interpersonal trauma was not associated with separation/loss, Χ2(1,246) = 0.82, but was associated with violence exposure, Χ2(1,246) = 7.08, p = .0291. On-line supplemental Figures 1–3 detail the overlap of separations/losses with types of trauma exposure.
3.3. Bivariate associations
Separation/loss, violence exposure and harsh parenting correlated positively with trauma-related symptoms and impairment. Non-interpersonal trauma correlated significantly with trauma-related symptoms but not impairment (see Table 2).
3.4. Trauma related symptoms
The results of the initial model (see Table 3) for total trauma-related symptoms revealed a significant effect of separation/loss on ITSEA total trauma-related symptoms, with moderate effect size, controlling for demographic covariates, F(2,240) = 6.45, p = .0019, partial η2 = .0510. Patterns were similar with violence exposure, non-interpersonal trauma, and harsh parenting controlled, F(2,246) = 4.02, p = .0192, partial η2 = .0328. Trauma-related symptoms were significantly associated with poverty and harsh parenting [F(1,237) = 12.19, p = .0006 and F(1,237) = 18.43, p < .0001, respectively] but not non-interpersonal trauma or interpersonal violence [F(1,237) = 2.48, p = .1168 and F(1, 237) = 1.84, p = .1765, respectively]. Within specific symptom domains, there were significant effects of separation/loss on arousal and re-experiencing symptoms, controlling for the same variables. As shown in Figure 1(a), parents reported greater total symptoms, re-experiencing and arousal symptoms in children with multiple separations/losses compared with those with no history of separation/loss (Bonferroni-adjusted p < .05). Total trauma-related symptoms and arousal were also higher in the multiple separation/loss group than in the single loss group. Avoidance symptoms were not related to separation/loss.
Table 3.
Psychiatric disorders linked with multiple separations/losses.
| |
Adjusted Odds Ratios (95% Confidence Interval) |
|||
|---|---|---|---|---|
| Independent Variables | Any Disorder | Any Externalizing | Disruptive Behavior Disorders | Any Internalizing |
| Child age | 1.06 (1.01–1.12) | 1.06 (1.00–1.12) | 1.06 (0.99–1.12) | 1.03 (0.97–1.10) |
| Child sex | 2.47 (1.07–5.70) | 2.67 (1.10–6.47) | 2.58 (0.99–6.70) | 1.85 (0.69–4.90) |
| Poverty | 1.64 (0.84–3.22) | 1.61 (0.80–3.27) | 2.40 (1.11–5.17) | 0.98 (0.43–2.21) |
| Non-interpers. Trauma | - | - | - | - |
| Violence/Harsh Parenting | 2.49 (1.01–6.22) | 2.19 (0.89–5.37) | 2.01 (0.79–5.13) | 2.34 (0.87–6.33) |
| Single Separation/Loss | 1.50 (0.72–3.17) | 1.39 (0.63–3.07) | 1.38 (0.58–3.29) | 1.58 (0.63–3.96) |
| Multiple Separations/Losses | 2.61 (1.01–6.75) | 2.40 (0.91–6.31) | 3.33 (1.21–9.16) | 2.32 (0.77–6.99) |
For ease of interpretation, significant effects are bolded. Child age and sex were included in all models. For parsimony, models included non-interpersonal trauma only when a significant bivariate association with the outcome was present. Violence/Harsh Parenting variable was positive if violent interpersonal trauma was reported or the child experienced very harsh parenting incorporating physical and/or verbal aggression.
Figure 1.
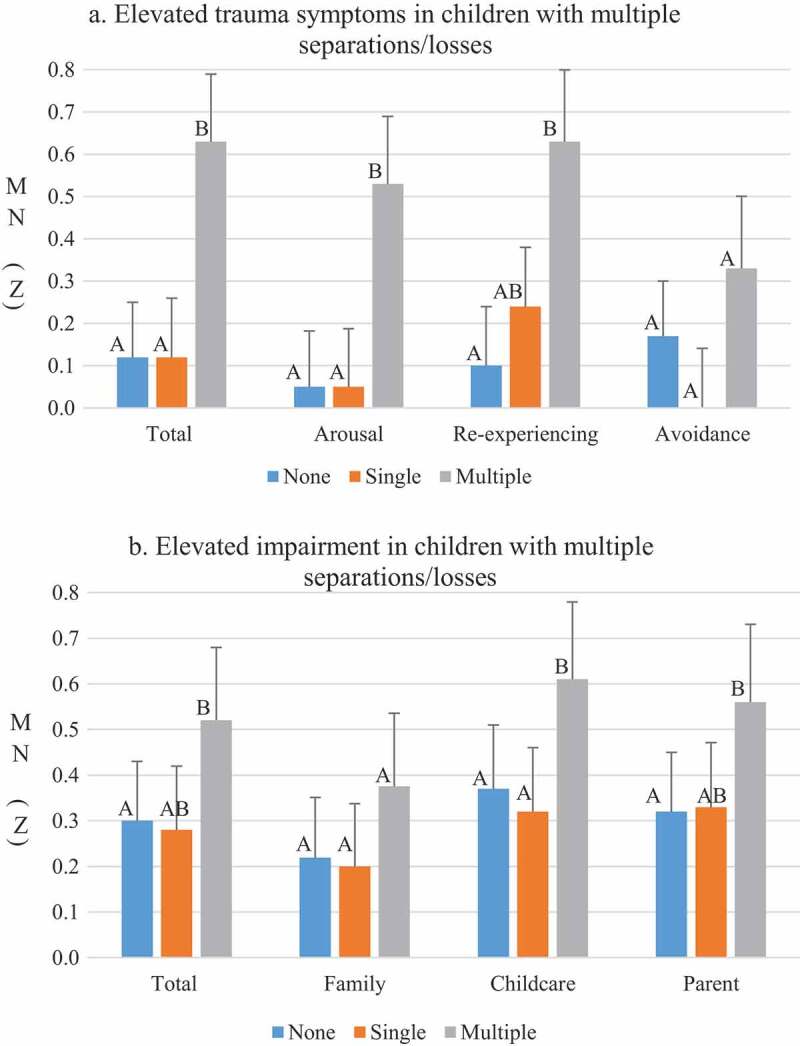
Multiple separations/losses associated with trauma symptoms and impairment.
(a) Total Trauma Symptoms, Arousal, and Re-experiencing were significantly higher in the multiple separations/losses group than the none group. This group also had higher Total Symptoms and Arousal than the single separation/loss group. Means are adjusted for age, sex, poverty, violence exposure, harsh parenting, and non-interpersonal trauma. Pairwise comparisons significant at p < .05 with Bonferroni correction. Means that share the same letter do not differ.(b) Total Impairment, Childcare Impairment and Parent Impairment were significantly higher in the multiple separations/losses group than the none group. This group also had significantly higher Childcare Impairment than the single separation/loss group. Means presented are adjusted for age, sex, poverty, violence exposure, harsh parenting, and non-interpersonal trauma. Pairwise comparisons significant at p < .05 with Bonferroni correction. Means that share the same letter do not differ.
Clinically concerning trauma-related symptoms provide an indication of the extent to which trauma-related symptoms were of sufficient severity to warrant clinical concern, and were reported by 62.2% of children with multiple separations/losses, but only 32.0% of the single separation/loss group and 33.1% of those with no separation/loss, Χ2(2, 245) = 11.30, p = .0035. Children with multiple separations/losses were nearly 3 times more likely (OR = 2.77, 95% CI = 1.16–6.60) to have clinically concerning trauma-related symptoms than all other children, after controlling for age, sex, poverty, harsh parenting/violence exposure and exposure to non-interpersonal trauma in a logistic regression analysis. Single separation/loss was not a significant predictor (OR = 0.90, CI = 0.47–1.69).
3.5. Reactive attachment disorder symptoms
RAD Inhibited-type symptoms were associated with separation/loss (see Table 2). These symptoms were relatively rare, with 14.7% of children reported to have 1 symptom, 2.9% two symptoms, and 2.9% three or more symptoms. However, the distribution of these symptoms was associated with loss group (Mantel-Haenszel Χ2 = 4.18, p = .0409), with 13.9% of the repeated separations/losses group having 2 or more symptoms, compared with 2.6% in the single loss group and 5.3% in the no separation/loss group.
Results of the general linear models indicated that separation/loss was associated with RAD Inhibited symptoms in the initial model with demographic covariates, and once harsh parenting, non-interpersonal trauma, and interpersonal violence were included [F(2,236) = 4.81, p = .0089, partial η2 = .0387 and F(2,236) = 3.67, p = .0269, partial η2 = .0302, respectively]. These symptoms also were associated with harsh parenting, F(2,236) = 4.38, p = .0373, partial η2 = .0182, but not violence exposure or non-interpersonal trauma. Children with multiple separations/losses (adjusted MN = 0.75, SE = 0.14) had significantly higher levels of symptoms than children with a single separation/loss (adjusted MN = 0.31, SE = 0.12, p = .0217), but the comparison with children with no losses did not achieve significance (adjusted MN = 0.41, SE = 0.11, p = .1113). RAD Disinhibited symptoms were not significantly associated with separation/loss, consistent with the bivariate analysis.
3.6. Impairment
Separation/loss was associated with total impairment controlling for age, sex, and poverty F(2,235) = 5.08, p = .0070, partial η2 = .0414, as well as when harsh parenting, non-interpersonal trauma, and interpersonal violence were added to the model, F(2, 232) = 5.18, p = .0063, partial η2 = .0427. Harsh parenting and poverty also explained unique variance in total impairment, F(1, 232) = 12.55, p = .0005, partial η2 = .0515, and F(1, 232) = 10.93, p = .0011, partial η2 = .0450, respectively. Violence exposure and non-interpersonal trauma were not associated with impairment. Within specific impairment areas, separation/loss was positively related to childcare and parent impairment, F(2,232) = 4.55, p = .0115, partial η2 = .0378, and F(2,232) = 3.47, p = .0328, partial η2 = .0290, respectively. As shown in Figure 1(b), all three impairment measures were significantly higher in the multiple separation/loss group than in the no separation/loss group. The multiple separation/loss group also had greater childcare impairment than the single loss group. Separation/loss was not related to family impairment, F(2,232) = 2.09, p = .1265.
3.7. Psychiatric disorders
Fifty-nine children had one or more psychiatric disorders, 49 had an externalizing disorder (42 DBD, 21 ADHD), and 32 an internalizing disorder (15 anxiety, 19 depressive). Separation/loss was associated with problems in all diagnostic areas except ADHD and depressive disorders, in unadjusted bivariate analyses (see Figure 2). Results of multivariate analyses revealed that children with multiple separations/losses were approximately 2.5 times more likely than other children to have at least one disorder (OR = 2.61, CI = 1.01–6.75, p = .0478), after controlling for age, sex, poverty status and violence/harsh parenting (see Table 3). Violence/harsh parenting also was associated with an increased likelihood of a psychiatric disorder in this model (OR = 2.49, CI = 1.01–6.22, p = .0498). Examination of models for specific diagnostic areas suggested that this pattern was primarily driven by greater likelihood of DBDs in children with multiple separations/losses relative to other children (OR = 3.33, CI = 1.21–9.16, p = .0199). For internalizing disorders, none of the variables was significant; however, power for this analysis was constrained due to the limited number of children with internalizing disorders and those findings should be interpreted cautiously.
Figure 2.
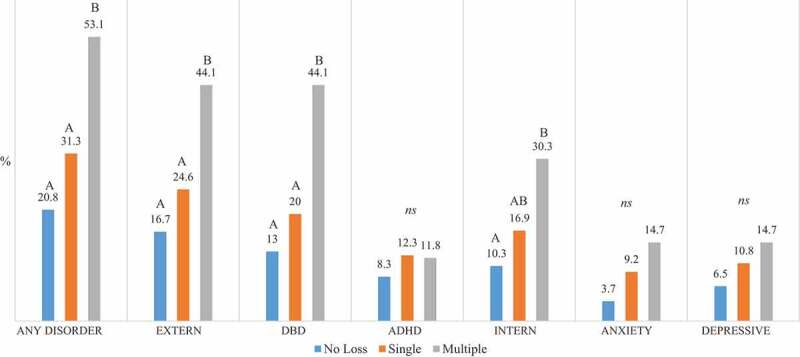
Psychiatric disorders by separation/loss group.
Separation/loss group was significantly related to presence of any disorder, externalizing disorders, disruptive behavior disorders, and internalizing disorders (Χ2 = 7.42 to 13.66, p = .0064 to .0005). There also was a modest association with anxiety disorders (Χ2 = 5.19, p = .0228) but no significant association with ADHD or depressive disorders (Χ2 = 0.59 to 2.37, ns). In pairwise tests, children with multiple separations/losses were significantly more likely than children with no separation/loss to have any disorder, externalizing disorders, DBDs, and internalizing disorders (p < .05 to p < .005). Any disorder, externalizing disorders, and DBDs were also more common in children with multiple losses/separations compared to those in the single separation/loss group (p < .05). Means that share the same letter do not differ significantly.
4. Discussion
In an ethnoracially and socioeconomically diverse sample drawn from community and clinical sites, separations and losses of parental caregivers and other loved ones were common in early childhood, occurring in almost half (45.9%) of the current sample of children aged 18 to 48 months. Thirty-one percent of infants and toddlers had experienced a single separation or loss. These single experiences were most often related to a caregiver being apart from the child for more than a week or being hospitalized. However, approximately 15% of children had experienced repeated separations, which also most often involved caregiver separation for more than a week or caregiver hospitalization (84%), but also reflected more prolonged losses due to death of a loved one (60%) or divorce (49%). Although most children who had experienced violence or non-interpersonal trauma also experienced caregiver separation/loss (and half of them had experienced multiple separations/losses), there was a unique association between multiple separations/losses and trauma-related symptoms, reactive attachment symptoms, functional impairment, and psychiatric disorders even after accounting for the effects of violence, non-interpersonal trauma exposure and contextual risks such as poverty and harsh parenting.
That the preponderance of young children who had experienced significant traumatic experiences also had experienced caregiver separation/loss – and particularly multiple caregiver separations and losses – suggests that what may appear to be symptoms and impairments caused by trauma exposure could be due to or augmented by the distress elicited and biobehavioral adaptations required by separations/losses. The trauma-related symptoms that were uniquely associated with multiple separations and losses, and not with either violence or other trauma exposures, were re-experiencing and arousal symptoms. Repeated experiences of separation/loss may sensitize young children to reminders or indicators of potential threat in their current lives. This is consistent with the crucial role caregivers play in helping young children to both navigate normative stressors and feel safe in the face or aftermath of traumatic stressors (Gray, Forbes, Briggs-Gowan, & Carter, 2015; Hofer, 1994). Early life maternal separations also may lead to sensitization on a neurobiological level, as indicated by findings from animal research of an inflammatory neuroimmune reaction and subsequent depressive-like behavior following repeated maternal separations (Hennessy et al., 2019). Moreover, animal models with rodents and primates have shown that mother-infant interactions play a critical role in regulating infant behavioral and biological systems and that even short separations from an attachment figure can result in disruptions in these systems (Hofer, 1994). Together, these patterns align with Bowlby’s descriptions of the dysregulation that occurs (e.g., protest, despair) with separation from and loss of an attachment figure (Bowlby, 1982, 1980, 1973).
Furthermore, the development of these trauma-related symptoms is consistent with caregiving contexts in which the child experiences not only a threat but also the absence of protective, predictable caregiving (Field, 1996; Meyer, Novak, Bowman, & Harlow, 1975; Sroufe, 1986). Thus, what might appear to be intrusive re-experiencing of the threat or harm posed by violence or other traumas may be a more complex combination of re-experiencing that is related to fear and overwhelming anxiety of the trauma and of the loss of or separation from a protective caregiver. The presence of early arousal symptoms further suggests that repeated experiences of separation/loss of a caregiver may lead to defensive psychobiological mobilization by young children potentially impeding or compromising acquisition of self-regulatory capacities that typically develop in early childhood.
Additional findings for reactive attachment symptoms suggest that for some children repeated separations/losses are associated with disruptions in their ability to engage in secure base behaviors and to be consoled by adult attachment figures. While rare in this sample, inhibited-type RAD symptoms were more common in children with multiple separations/losses than other children: 14% had multiple symptoms in this domain, compared with 3% of children with a single separation/loss and 5% in those with no separation/losses. These symptoms include failure to seek comfort from caregivers, resistance of comfort by caregivers, difficulty being affectionate, and a tendency to approach caregivers for help but then withdraw or not follow through. Such impairments in their ability to make use of attachment figures when stressed likely increases these children’s risk for problems with arousal modulation when faced with new separations/losses, traumas or other stressors.
Avoidance/numbing symptoms were not associated with separation/loss, violence or non-interpersonal trauma exposure. This is consistent with the findings of other studies of posttraumatic stress symptoms in young children (Briggs-Gowan et al., 2016; Levendosky et al., 2002; Scheeringa, 2006) as well as with the reduced emphasis on avoidance symptoms in the diagnostic criteria developed specifically for young children (American Psychiatric Association, 2013). Lower levels of avoidance symptoms may be due to difficulty that parents have in identifying these abstract and predominantly internalized symptoms among young children who are still at an early stage of development of verbal skills and emotional awareness.
Importantly, our data reveal the early emergence of impairment in children exposed to multiple types of separation/loss. Their parents reported greater difficulty obtaining and retaining childcare for them. They also reported greater interference in their own functioning and relationships, for example, more difficulty caring for other children in the family or spending time with a partner. In our prior research in a representative birth cohort of infants and toddlers, the presence of these forms of impairment within the first few years of life appeared to signal the onset of persistent, impairing psychopathology (Briggs-Gowan, Carter, Bosson-Heenan, Guyer, & Horwitz, 2006).
Consistent with the impairment findings, psychiatric disorders were significantly more common in children with multiple separations/losses than other children. Young children with multiple separations/losses were approximately 2.5 times more likely than other children to have at least one psychiatric disorder and more than 3 times more likely to have a disruptive behavior disorder, independent of the effects of important contextual risks, such as poverty, harsh parenting and violence exposure. Converging with the trauma symptom and impairment findings, these diagnostic patterns suggest that multiple separations/losses may place children at-risk for a constellation of problems arising from emotional and behavioral dysregulation. However, given the cross-sectional design of this study, longitudinal research with infant-toddler cohorts will be essential to establish the long-term sequelae of early separations.
We also found that young children who had experienced interpersonal violence showed increased likelihood of psychiatric disorders and clinically-elevated trauma symptoms, after accounting for multiple separations/losses. These patterns align with evidence that interpersonal violence may lead to defensive psychobiological mobilization and hypervigilance to threats in young children (Briggs-Gowan et al., 2012, 2015). It is possible that exposure to trauma and the mobilization of defensive arousal also exacerbates children’s sense of being unprotected and need for more attuned, protective caregiving that appears to be associated with separation/loss in young children. However, this cannot be determined in the current sample because nearly all of the violence-exposed children had also experienced separation/loss. This warrants further investigation given previous evidence that trauma exposure may sensitize young children to subsequent non-traumatic stressors (Grasso et al., 2013).
These data suggest that multiple and often prolonged separations/losses may have particularly adverse effects on young children, but more research is needed to fully understand their impact. It is likely that qualitative features of individual experiences of separation or loss, not captured in the current study, further contribute to their impact. To illustrate, a one week separation from a caregiver might occur following partner violence that was witnessed by the child, resulted in one parent moving out and being incarcerated, the other parent being hospitalized, and the toddler suddenly being cared for in an unfamiliar environment by a relative with little or no knowledge of the child who may be distressed or angered by the situation. In this scenario, the child experiences not only significant threats to and the loss of both caregivers, but also disruption in daily routines and the need to adapt to a new caregiving relationship. In contrast, a planned one week separation due to caregiver travel during which the child is cared for by the second parent in their usual home may be less stressful because it involves less caregiver distress or threat and disruption to the child’s routines, and because the presence of the second parent may buffer the impact of the separation. Relatedly, although anecdotally we know that some children had experienced the prolonged or permanent loss of their biological mother, for example, due to removal due to abuse/neglect or adoption at birth, this specific type of loss is not adequately captured in our data. There is no question that the nature and quality of the young child’s relationship with the caregiver from whom they are separated and with the caregiver(s) who remains or who assumes care of the child are likely play central roles in the child’s adaptation or maladaptation during and following separation/loss. More in-depth investigation of qualitative features of separations and the caregiving contexts in which they occur will be important in future research.
The current findings suggest that mental health and pediatric professionals should screen and identify young children who have experienced multiple types of separation/loss from caregivers, including both relatively brief separations, separations/loss in the context of trauma and also more permanent losses, and carefully screen and monitor them for emerging emotional and behavioral problems. Further, careful screening for caregiver separation/loss is warranted for children with evident mental health problems as trauma-informed interventions may be warranted. In many cases, children currently are not identified because most children who experience caregiver separations – 74% of single separation/loss group and 46% of multiple separation/loss group in this sample – have not experienced violence or non-interpersonal trauma. Parents and professionals may not recognize the potential impact of separations on young children’s functioning. Therefore, while screening and evaluation of children exposed to violence and other traumas are becoming well-recognized as a pediatric and psychiatric standard of care, our findings indicate that similar evaluation and care is warranted for children coping with multiple or significant caregiver separations/losses. Furthermore, the needs of remaining adult caregivers should be addressed as they likely experienced the same separations/losses and may be bereaved or depressed, as has been well-documented in the literature on parental death (Lieberman et al., 2003; Lieberman & Van Horn, 2011). In addition, a parent-child relational approach to therapeutic intervention is highly recommended to help the adult to recognize the needs of the child to be able to play out/talk about their experience. Furthermore, through the therapeutic process of creating a trauma narrative, the affected child and remaining adult caregiver will develop language and support to discuss their individual and mutual experience of separation and loss (Lieberman & Van Horn, 2011; Lieberman, Van Horn, & Ghosh-Ippen, 2015).
In this young child sample, converging findings across symptoms, impairment, and disorders suggest that multiple separations/losses are associated with clinically-concerning problems rather than with difficulties that are relatively mild or transient. However, while this study utilized developmentally-sensitive, in-depth, methods for assessing children’s functioning and exposure to separation/loss, trauma, and other adversities, some limitations are worth discussion. First, as is often true when assessing mental health in the young child, this study utilized parent/caregiver’s reports, raising the possibility that shared method variance may have contributed to the patterns observed. It will be important to incorporate other sources of information, such as additional informants or observational assessments in future work. Additionally, our methods did not capture the exact duration, developmental timing, or number of separate instances of each specific type of separation/loss or trauma. Thus, we were unable to establish how ‘dose’ of exposure affected findings. Furthermore, as discussed above, the association of multiple separations/losses with symptoms and impairment outcomes could be related to corollary factors such as whether the events were more permanent, involved threat to a critical caregiving figure, were unplanned, or required the child to be cared for outside the familial home, rather than to the number of types of separation/loss per se. Finally, the cross-sectional study design does not permit inferences about causation or the stability of the trauma-related and psychiatric symptoms. Ideally, future research in this area will include a longitudinal design and an even more comprehensive assessment of children’s experiences of separation and loss to more powerfully demonstrate the impact of these experiences on developmental pathways starting early in life.
5. Conclusions
The past two decades have witnessed exponential growth in our understanding that young children can and do suffer from serious and impairing mental health problems. Considerable evidence has documented that infants and toddlers may be especially vulnerable to adversities such as maltreatment, witnessing interpersonal violence, and other traumas (Briggs-Gowan et al., 2010, 2012; Manly, Kim, Rogosch, & Cicchetti, 2001; Schechter et al., 2019; Tottenham, 2014). Our findings extend our understanding of risk for early psychopathology. Indeed, our data show that separations and losses of caregivers may affect young children in ways that are similar to the impact of exposure to violence, with increased trauma symptoms and psychiatric disorders. Early caregiver separation is likely to disrupt caregiver-child co-regulation (Hendrix, Stowe, Newport, & Brennan, 2018) which has been shown to be important for at-risk children in this age range in developing executive functioning capacities and peer acceptance (Hendrix et al., 2018; Herbers, Cutuli, Supkoff, Narayan, & Masten, 2014). Research is needed to determine whether early life separation from caregivers that occur at different ages, for different periods of time, in relation to different caregivers (e.g., primary vs. secondary), and in different contexts (e.g., forced separation due to exposure to violence or during immigration; separation due to caregiver trauma or behavioral health problems) have different impacts on caregiver-child co-regulation or other potential protective factors, and lead to distinct adverse outcomes in childhood and subsequently across the lifespan.
It also is crucial for policy-makers, professionals working with young children, and caregivers to appreciate that these separations/losses of a primary caregiver may have serious, detrimental effects on a young child, especially in the context of prior separations, losses, or disruptions in their lives. Tens of thousands of young children are experiencing separations from caregivers worldwide under highly adverse circumstances that often involve exposure to both interpersonal and non-interpersonal violence (Betancourt et al., 2017; Brown, de Graaff, Annan, & Betancourt, 2017). Interventions to protect these children, promote recovery, and ultimately to prevent separations (especially in the context of violence or other traumas) are a crucial public health and humanitarian priority (Purgato et al., 2018).
Supplementary Material
Acknowledgments
We wish to acknowledge Marilyn Augustyn, MD, Elizabeth Caronna, MD, Audrey Tluczek, PhD, and Danielle Forbes, PhD, for their work engaging and evaluating study families. We especially thank the many families who made this study possible.
Disclosure statement
The first and last authors receive royalties related to the distribution of the ITSEA questionnaire by the MAPI Research Trust.
Supplemental material
Supplemental data for this article can be accessed here.
References
- Achenbach T. M., Edelbrock C., & Howell C. T. (1987). Empirically based assessment of the behavioral/emotional problems of 2- and 3-year-old children. Journal of Abnormal Child Psychology, 15, 629–14. [DOI] [PubMed] [Google Scholar]
- Adam E. K., & Chase-Lansdale P. L. (2002). Home sweet home(s): Parental separations, residential moves, and adjustment problems in low-income adolescent girls. Developmental Psychology, 38(5), 792–805. [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statisical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Arnold D. S., O’Leary S. G., Wolff L. S., & Acker M. M. (1993). The parenting scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment, 5(2), 137–144. [Google Scholar]
- Barker L. H., & Berry K. D. (2009). Developmental issues impacting military families with young children during single and multiple deployments. Military Medicine, 174(10), 1033–1040. [DOI] [PubMed] [Google Scholar]
- Betancourt T. S., Newnham E. A., Birman D., Lee R., Ellis B. H., & Layne C. M. (2017). Comparing trauma exposure, mental health needs, and service utilization across clinical samples of refugee, immigrant, and U.S.-origin children. Journal of Traumatic Stress, 30(3), 209–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogat G. A., DeJonghe E., Levendosky A. A., Davidson W. S., & von Eye A. (2006). Trauma symptoms among infants exposed to intimate partner violence. Child Abuse & Neglect, 30(2), 109–125. [DOI] [PubMed] [Google Scholar]
- Boss P. (2016). The context and process of theory development: The story of ambiguous loss. Journal of Family Theory & Review, 8, 269–286. [Google Scholar]
- Bowlby J. (1973). Attachment and loss (Vol 2): Separation: Anxiety and anger. New York: Basic. [Google Scholar]
- Bowlby J. (1980). Attachment and loss (Vol 3): Sadness and depression. New York: Basic. [Google Scholar]
- Bowlby J. (1982). Attachment and loss (Vol. 1, 2nd ed.). New York: Basic. [Google Scholar]
- Briggs-Gowan M. J., Godoy L., Heberle A., & Carter A. S. (2016). In Cicchetti D. (Ed.), Developmental psychopathology (3rd ed., pp. 1–45). New York: Wiley. [Google Scholar]
- Briggs-Gowan M. J., Carter A. S., Clark R., Augustyn M., McCarthy K. J., & Ford J. D. (2010). Exposure to potentially traumatic events in early childhood: Differential links to emergent psychopathology. Journal of Child Psychology & Psychiatry, 51(10), 1132–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M. J., Carter A. S., & Ford J. D. (2012). Parsing the effects violence exposure in early childhood: Modeling developmental pathways. Journal of Pediatric Psychology, 37(1), 11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M. J., Estabrook R., Henry D., Grasso D. G., Burns J., McCarthy K. J., … Wakschlag L. S. (2018). Parsing dimensions of family violence exposure in early childhood: Shared and specific contributions to emergent psychopathology and impairment. Child Abuse and Neglect, 87, 100–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M. J., Grasso D. J., Bar-Haim Y., Voss J., McCarthy K. J., Pine D. S., & Wakschlag L. S. (2016). Attention bias in the developmental unfolding of post-traumatic stress symptoms in young children at risk. Journal of Child Psychology and Psychiatry, 57(9), 1083–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M. J., Horowitz S., & Carter A. (1998). The family life impairment scale. New Haven, CT: Yale University. [Google Scholar]
- Briggs-Gowan M. J., Pollak S. D., Grasso D., Voss J., Mian N. D., Zobel E., … Pine D. S. (2015). Attention bias and anxiety in young children exposed to family violence. Journal of Child Psychology and Psychiatry, 56(11), 1194–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M. J., Carter A. S., Bosson-Heenan J., Guyer A. E., & Horwitz S. M. (2006). Are infant-toddler social-emotional and behavioral problems transient? Journal of the American Academy of Child & Adolescent Psychiatry, 45(7), 849––858.. doi: 10.1097/01.chi.0000220849.48650.59 [DOI] [PubMed] [Google Scholar]
- Brown F. L., de Graaff A. M., Annan J., & Betancourt T. S. (2017). Annual research review: Breaking cycles of violence - a systematic review and common practice elements analysis of psychosocial interventions for children and youth affected by armed conflict. Journal of Child Psychology and Psychiatry, 58(4), 507–524. [DOI] [PubMed] [Google Scholar]
- Carter A. S., & Briggs-Gowan M. J. (1998). Child life events screener: A manual. New Haven, CT. Unpublished. [Google Scholar]
- Carter A. S., & Briggs-Gowan M. J. (2006). ITSEA Infant-Toddler Social and Emotional Assessment examiner’s manual. San Antonio, TX: Harcourt Assessment, Inc. [Google Scholar]
- Carter A. S., Briggs-Gowan M. J., Jones S. M., & Little T. D. (2003). The Infant-Toddler Social and Emotional Assessment (ITSEA): Factor structure, reliability, and validity. Journal of Abnormal Child Psychology, 31(5), 495–514. [DOI] [PubMed] [Google Scholar]
- Crawford T. N., Cohen P. R., Chen H., Anglin D. M., & Ehrensaft M. (2009). Early maternal separation and the trajectory of borderline personality disorder symptoms. Development & Psychopathology, 21(3), 1013–1030. [DOI] [PubMed] [Google Scholar]
- Egger H. L., Erkanli A., Keeler G., Potts E., Walter B. K., & Angold A. (2006). Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA). Journal of the American Academy of Child and Adolescent Psychiatry, 45(5), 538–549. [DOI] [PubMed] [Google Scholar]
- Feldman R., & Vengrober A. (2011). Posttraumatic stress disorder in infants and young children exposed to war-related trauma. Journal of the American Academy of Child and Adolescent Psychiatry, 50(7), 645–658. [DOI] [PubMed] [Google Scholar]
- Field T. (1996). Attachment and separation in young children. Annual Review of Psychology, 47, 541–561. [DOI] [PubMed] [Google Scholar]
- Gindling T., & Poggio S. (2012). Family separation and reunification as a factor in the educational success of immigrant children. Journal of Ethnic and Migration Studies, 38(7), 155–1173. [Google Scholar]
- Grasso D. J., Ford J. D., & Briggs-Gowan M. J. (2013). Early life trauma exposure and stress sensitivity in young children. Journal of Pediatric Psychology, 38(1), 94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso D. J., Petitclerc A., Henry D. B., McCarthy K. J., Wakschlag L. S., & Briggs-Gowan M. J. (2016). Examining patterns of exposure to family violence in preschool children: A latent class approach. Journal of Traumatic Stress, 29(6), 491–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray S. A., Forbes D., Briggs-Gowan M. J., & Carter A. S. (2015). Caregiver insightfulness and young children’s violence exposure: Testing a relational model of risk and resilience. Attachment & Human Development, 17(6), 615–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrix C. L., Stowe Z. N., Newport D. J., & Brennan P. A. (2018). Physiological attunement in mother-infant dyads at clinical high risk: The influence of maternal depression and positive parenting. Development & Psychopathology, 30(2), 623–634. [DOI] [PubMed] [Google Scholar]
- Hennessy M. B., Deak T., Sensenbaugh J. D., Gallimore D. M., Garybush A. M., Mondello J. E., & Schiml P. A. (2019). Central neuroimmune activity and depressive-like behavior in response to repeated maternal separation and injection of LPS. Physiology & Behavior, 199, 366–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbers J. E., Cutuli J. J., Supkoff L. M., Narayan A. J., & Masten A. S. (2014). Parenting and coregulation: Adaptive systems for competence in children experiencing homelessness. American Journal of Orthopsychiatry, 84(4), 420–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer M. A. (1994). Hidden regulators in attachment, separation, and loss. Monographs of the Society for Research in Child Development, 59(2–3), 192–207. [PubMed] [Google Scholar]
- Howard K., Martin A., Berlin L. J., & Brooks-Gunn J. (2011). Early mother-child separation, parenting, and child well-being in early head start families. Attachment & Human Development, 13(1), 5–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koolick J., Galano M., Grogan-Kaylor A., Clark H., Montalvo-Liendo N., & Graham-Bermann S. (2016). PTSD symptoms in young children exposed to intimate partner violence in four ethno-racial groups. Journal of Child & Adolescent Trauma, 9, 97–107. [Google Scholar]
- Levendosky A. A., Huth-Bocks A. C., Semel M. A., & Shapiro D. L. (2002). Trauma symptoms in preschool-age children exposed to domestic violence. Journal of Interpersonal Violence, 17(2), 150–164. [Google Scholar]
- Lieberman A. F. (2007). Ghosts and angels: Intergenerational patterns in the transmission and treatment of the traumatic sequelae of domestic violence. Infant Mental Health Journal, 28(4), 422–439. [DOI] [PubMed] [Google Scholar]
- Lieberman A. F., Compton N. C., Van Horn P., & Ghosh Ippen C. (2003). Losing a parent to death in the early years: Guidelines for the treatment of traumatic bereavement in infancy and early childhood. Washington DC: ZEROTOTHREE. [Google Scholar]
- Lieberman A. F., & Van Horn P. (2011). Psychotherapy with infants and young children: Repairing the effects of stress and trauma on early attachment. New York, NY: Guilford Press. [Google Scholar]
- Lieberman A. F., Van Horn P., & Ghosh-Ippen C. (2015). Don’t hit my mommy (2nd ed.). Washington DC: ZerotoThree Press. [Google Scholar]
- Manly J. T., Kim J. E., Rogosch F. A., & Cicchetti D. (2001). Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology, 13(4), 759–782. [PubMed] [Google Scholar]
- Meiser-Stedman R., Smith P., Glucksman E., Yule W., & Dalgleish T. (2008). The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. American Journal of Psychiatry, 165(10), 1326–1337. [DOI] [PubMed] [Google Scholar]
- Meyer J. S., Novak M. A., Bowman R. E., & Harlow H. F. (1975). Behavioral and hormonal effects of attachment object separation in surrogate-peer-reared and mother-reared infant rhesus monkeys. Developmental Psychobiology, 8(5), 425–435. [DOI] [PubMed] [Google Scholar]
- Mian N. D., Soto T. W., Briggs-Gowan M. J., & Carter A. S. (2018). The family life impairment scale: Factor structure and clinical utility with young children. Journal of Clinical Child & Adolescent Psychology, 47, S530–S541 Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongillo E. A., Briggs-Gowan M., Ford J. D., & Carter A. S. (2009). Impact of traumatic life events in a community sample of toddlers. Journal of Abnormal Child Psychology, 37(4), 455–468. [DOI] [PubMed] [Google Scholar]
- Mueller I., Snidman N., DiCorcia J., Sravish A., Duffy E., & Tronick E. Z. (2018). In a heartbeat: Infant memory for a stressful social event at 4-months. International Congress of Infant Studies, Philadelphia, PA. [Google Scholar]
- Poehlmann J. (2005). Representations of attachment relationships in children of incarcerated mothers. Child Development, 76(3), 679–696. [DOI] [PubMed] [Google Scholar]
- Purgato M., Gross A. L., Betancourt T., Bolton P., Bonetto C., Gastaldon C., … Barbui C. (2018). Focused psychosocial interventions for children in low-resource humanitarian settings: A systematic review and individual participant data meta-analysis. Lancet Glob Health, 6(4), e390–e400. [DOI] [PubMed] [Google Scholar]
- Santa-Maria M. L., & Cornille T. (2007). Traumatic stress, family separations, and attachment among Latin American immigrants. Traumatology, 13(2), 26–31. [Google Scholar]
- Schechter D. S., Willheim E., Suardi F., & Serpa R. S. (2019). The effects of violent experiences on infants and young children In Zeanah C. H. (Ed.), Handbook of infant mental health (4th ed., pp. 219–238). New York, NY: The Guilford Press. [Google Scholar]
- Scheeringa M. S. (2006). Posttraumatic stress disorder: Clinical guidelines and research findings In Luby J. L. (Ed.), Handbook of preschool mental health: Development, disorders, and treatment (pp. 165–185). New York, NY: Guilford Press. [Google Scholar]
- Scheeringa M. S. (2009). Posttraumatic stress disorder In Zeanah C. H. (Ed.), Handbook of infant mental health (3rd ed., pp. 345–361). New York: The Guilford Press. [Google Scholar]
- Sroufe L. A. (1986). Bowlby’s contribution to psychoanalytic theory and developmental psychology; attachment: Separation: Loss. Journal of Child Psychology & Psychiatry, 27(6), 841–849. [DOI] [PubMed] [Google Scholar]
- Suárez-Orozco C., Bang H. J., & Kim H. Y. (2011). I felt like my heart was staying behind: Psychological implications of family separations & reunifications for immigrant youth. Journal of Adolescent Research, 26(2), 222–257. [Google Scholar]
- Tottenham N. (2014). The importance of early experiences for neuro-affective development. Current Topics in Behavioral Neurosciences, 16, 109–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah C. H., Egger H. L., Smyke A. T., Nelson C. A., Fox N. A., Marshall P. J., & Guthrie D. (2009). Institutional rearing and psychiatric disorders in Romanian preschool children. American Journal of Psychiatry, 166(7), 777–785. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


