Abstract
Objectives:
To clarify the etiology of substance-induced psychotic disorder (SIPD) and its progression to schizophrenia in a national Swedish sample.
Method:
7,606 cases of SIPD, registered 1997-2015, had a mean follow-up of 84 months. Family risk scores (FRS) for nonaffective psychosis (NAP), drug abuse (DA) and alcohol use disorder (AUD) were calculated from first through third-degree relatives utilizing medical, criminal and pharmacy registries.
Results:
Cases of SIPD had large elevations in their standardized FRS for DA (+1.09 95% CIs 1.02-1.15) and AUD (+0.98, 0.93-1.03) and modest elevations for NAP (+0.35, 0.30-0.41). The cumulative hazard for progression to schizophrenia was 11.3%, lowest for alcohol-and highest for cannabis-induced PD, and was predicted from early age at SIPD, male sex, and further DA, AUD, and SIPD episodes. A risk prediction model found 47% of conversions in the upper 20%. FRS for DA and AUD did not discriminate converters and non-converters while FRS for NAP did: 0.67 (0.40-0.95) and 0.33 (0.28-0.39) (P<0.0001), respectively. FRS for NAP were indistinguishable in cases of schizophrenia with and without prior SIPD. Early retirement from the Swedish Social Insurance Agency strongly discriminated cases of SIPD with and without schizophrenia.
Conclusions:
SIPD results from substantial drug exposure in individuals at high familial risk for substance abuse and a moderately elevated familial liability to psychosis. Familial risk for psychosis, but not substance abuse, predicts progression from SIPD to schizophrenia. Schizophrenia following SIPD is likely a drug-precipitated disorder in highly vulnerable individuals, not a syndrome predominantly “caused” by drug exposure.
Substance-induced psychotic disorders (SIPD) have been a focus of clinical and research interest in psychiatry for decades, with Kraepelin describing cases of alcoholic paranoia, alcoholic hallucinosis and cocaine delusional insanity, the latter often demonstrating flagrant schizophrenia-like bizarre delusions and passivity experiences (1;2) and Connell describing amphetamine psychosis in his classic 1957 monograph (3).
Kraepelin noted that although most patients recover quickly from cocaine delusional insanity, delusions could persist long after cessation of use ((1) p. 144). More systematic modern studies suggest that an appreciable proportion of cases of SIPD go on to develop schizophrenia (4–7) with the best evidence coming from follow-up studies of epidemiological cohorts in Finland (8) and Scotland (9).
Clarifying the etiology of SIPD is of interest because it can provide insights generalizable to other psychotic syndromes (10). Two etiologic questions are paramount. First, does the emergence of psychotic symptoms result solely from the pharmacological effects of the drug of abuse or also from the individual’s vulnerability to psychosis? Given the strong influence of familial/genetic factors in nonaffective psychoses (NAP)(11;12), this question could be addressed by examining the familial liability to NAP in cases of SIPD. If the psychosis resulted solely from drug exposure, familial risk to NAP would not be elevated in SIPD cases. If, however, a psychotic diathesis played an important role in the emergence of SIPD, then, such cases would have increased familial liability for NAP.
Second, what is the etiology of schizophrenia that emerges after SIPD? Such cases could arise i) from sustained pharmacologic exposure to drugs of abuse, ii) from a mixture of drug exposure and modest individual liability to psychosis, or iii) from a strong genetic diathesis where illness is simply precipitated by drug abuse. These three hypotheses predict, respectively, that the familial risk to NAP in cases of SIPD who go on to develop schizophrenia should i) not differ from controls, ii) be in between levels seen in controls and typical cases of schizophrenia, and iii) not differ from levels seen in typical schizophrenia.
Our analyses focus on three major questions. First, can we, in Swedish National Registries, obtain descriptive results for SIPD and its potential progression to schizophrenia, in line with the two prior registry-based longitudinal studies (8;9)? Second, could we clarify how familial risk scores (FRS) calculated from first, second and third-degree relatives for non-affective psychosis (NAP), drug abuse (DA) and alcohol use disorder (AUD), distinguish those who first develop SIPD from the general population and among those who develop SIPD who does versus does not progress to schizophrenia? Third, could we develop a risk calculator from available data to predict development of schizophrenia in cases of SIPD?
METHODS
This prospective cohort study utilized several Swedish population-based registers with national coverage that were linked using each person’s unique identification number. To preserve confidentiality, this number was replaced by a serial number. We secured ethical approval for this study from the Regional Ethical Review Board of Lund University (No. 2008/409). From the Swedish Hospital Discharge Register (national coverage between 1987 and 2015), the Outpatient Care Register (national coverage between 2001 and 2015) and the Primary Care Registry (based on visits to the primary health care in 18 county councils in Sweden with partial coverage from 1997 and onwards), all of whom over these years used ICD-10 codes, we selected all individuals with a registration of SIPD defined as: F10.5 (Due to Alcohol), F11.5 (Opioids), F12.5 (Cannabis), F13.5 (Hypnotics), F14.5 (Cocaine), F15.5 (Other stimulants), F16.5 (Hallucinogens), F17.5 (Tobacco), F18.5 (volatile solvents), and F19.5 (multiple drug use) between 1st January 1997 and 31st December 2015. Furthermore, we required that the individual was born in Sweden and had a first SIPD registration between ages 15-50. We included registrations for schizophrenia during the follow-up period: from date of SIPD registration until death, emigration of patient or end of follow-up (31 Dec 2015). All individuals with a registration of Nonaffective Psychosis (NAP) prior to their SIPD were excluded from the sample. Schizophrenia was defined based on the following ICD-codes in the medical registers: ICD10: F20.0; F20.1; F20.2; F20.3; F20.5; F20.9; ICD9: 295,1, 295,2, 295,3, 295,6, 295,9; ICD8: 295,1, 295,2, 295,3, 295,6, 295,9; NAP was defined in the same registers based on the following ICD-codes: ICD10: F20; F22; F23; F24; F25; F28; F29; ICD9: 295, 297, 298,3, 298,9; ICD8: 295, 297, 298,3, 298,9. For all individuals in the sample, we also include information on Alcohol Use Disorder registrations (AUD), Drug Abuse registrations (DA) and assignment of early retirement by the Swedish Social Insurance Agency (for definitions, see appendix).
Using the Swedish Multi-Generation register, we calculated a familial risk score (RFS) for NAP using first, second and third-degree relatives (for details, see appendix). For our main analyses, Kaplan–Meier survival curves were calculated to examine the cumulative hazard for schizophrenia for the different SIPD types. For comparison of FRSs between different groups, we used a non-parametric approach -- Van der Waerden Scores (13) – which ranks all values (the familial risks scores in the two groups) and then standardizes them (0 mean and 1 SD). Next, a Cox Regression model was performed with time to schizophrenia as outcome. As exposure variables we used: i) the different types of SIPDs as exposure variables (with Alcohol-Induced Psychosis as reference); ii) location of SIPD diagnosis (Primary Care, Outpatient Specialist Care or Inpatient Care); iii) registrations for DA, AUD, or SIPD after the initial SIPD episode. Among individuals registered in inpatient care, we constructed a separate model that also included length of hospitalization. In all models, we controlled for age at registration for SIPD and gender. Finally, we fitted a multivariate logistic regression model to a random half of our SIPD subjects as a training-sample. Results from that model were then applied to the second random half as the test sample. We divided this sample into 10 risk groups and fitted a Cox regression model with time to SZ as outcome and the 10 risk groups as exposure variables. All statistical analyses were performed using SAS 9.4 (14).
RESULTS
Descriptive Results
Table 1 provides details of the 7,606 cases of SIPD ascertained in individuals born in Sweden 1940-1995 who had no prior recorded NAP diagnosis as well as for the four forms of SIPD with greater than 1,000 subjects: alcohol, cannabis, stimulants, and multiple. The group was predominantly male (78%) with a mean age at first SIPD registration of 32.1 and a mean follow-up of 84 months. SIPD registrations occurred most frequently in hospitals (59.5%) and out-patient specialty care (23.9%).
Table 1.
Descriptive Statistics for Cases of Substance-Induced Psychotic Disorder (SIPD)
| All | F10.5 (Alcohol) | F12.5 (Cannabis) | F15.5 (Stimulants) | F19.5 (Multiple/Other) | |
|---|---|---|---|---|---|
| N* | 7,606 | 2,121 | 1,000 | 1,677 | 2,373 |
| % Males | 78.2 | 77.4 | 83.4 | 75.7 | 78.9 |
| Mean Age At SIPD | 32.1 | 39.4 | 25.2 | 31.8 | 29.3 |
| % SZ | 5.85 | 2.36 | 9.90 | 7.22 | 6.11 |
| Cumulative hazard Schizophrenia (95% Cls)# | 11.3 (10.0; 12.8) | 4.7 (3.1; 7.1) | 18.0 (14.5; 22.3) | 12.9 (10.4; 15.9) | 13.0 (10.5; 16.1) |
| Months to Schizophrenia (25-50-75 p-tile) | 18-39-72 | 14-27-65 | 14-30-59 | 16-47-84 | 21-43-71 |
| Mean Follow-up time for Schizophrenia (Months) | 83.9 | 87.9 | 67.0 | 99.4 | 75.6 |
| Inpatient Registrations % | 59.5% | 39.6% | 55.4% | 73.2% | 69.8% |
| Hospitalization days (25-50-75 percentile) | 1-3-7 | 1-2-6 | 1-4-12 | 1-2-5 | 1-3-8 |
| Outpatient Registration % | 23.9% | 14.0% | 38.1% | 21.5% | 27.5% |
| Primary Care Registration % | 16.2% | 46.5% | 6.5% | 5.3% | 2.7% |
| Prior DA registrations (%) | 63.2 | 32.9 | 61.8 | 77.5 | 80.8 |
| Prior AUD registrations (%) | 52.4 | 75.2 | 20.2 | 54.4 | 47.5 |
| # DA Registrations SIPD → Schizophrenia** | 2.86 | 1.22 | 2.25 | 4.44 | 4.09 |
| # AUD Registrations SIPD → Schizophrenia** | 2.24 | 3.83 | 0.62 | 2.26 | 2.85 |
Without prior non-affective psychosis registrations;
Number of registrations between SIPD and SZ Cases not shown in the table: F11. 5 (Opioids) n = 88; F13.5 (Sedatives) n = 94; F14.5 (Cocaine) n = 52; F16.5 (Hallucinogens) n = 197; F17.5 (Tobacco) n = 3; F18.5 (Solvents) n=ll
% SZ in the general population born 1940-1995: 0.45%
Prior to their first SIPD registration, 84% and 63% of the sample had been previously registered for DA and AUD, respectively. The mean age at registration for SIPD was earliest for cannabis (25.2 years) and latest for alcohol (39.4 years).
A total of 445 SIPD cases received, during our follow-up, one or more diagnosis of schizophrenia and of these 314 (70.6%) had ≥ 2 schizophrenia diagnoses. The cumulative hazard (± 95% CIs) for cases of SIPD converting to schizophrenia was 11.3% (10.0-11.8). Controlling for year of birth and gender, a diagnosis of SIPD carried a strong risk for a subsequent diagnosis of schizophrenia: hazard rate (HR)±95% CIs of 118.3 (104.7-133.7).
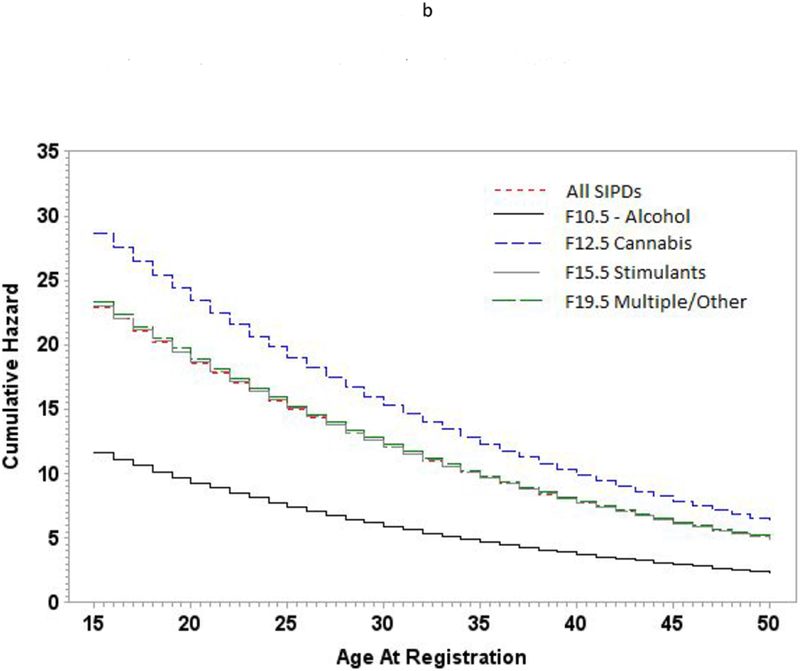
Examining the individual forms of SIPD, the cumulative hazard for schizophrenia was lowest for alcohol (4.7%, 3.1-7.1) and highest for cannabis: 18.0% (14.5-22.3). The cumulative hazard for schizophrenia onset for our four common SIPD classes are see in figure 1. Because of age at onset differences of SIPD across substance classes, we also examined the HR for schizophrenia controlling for age at registration (figure 1b). A higher risk for schizophrenia onset for cannabis-induced psychosis was seen at all ages.
Figure 1.
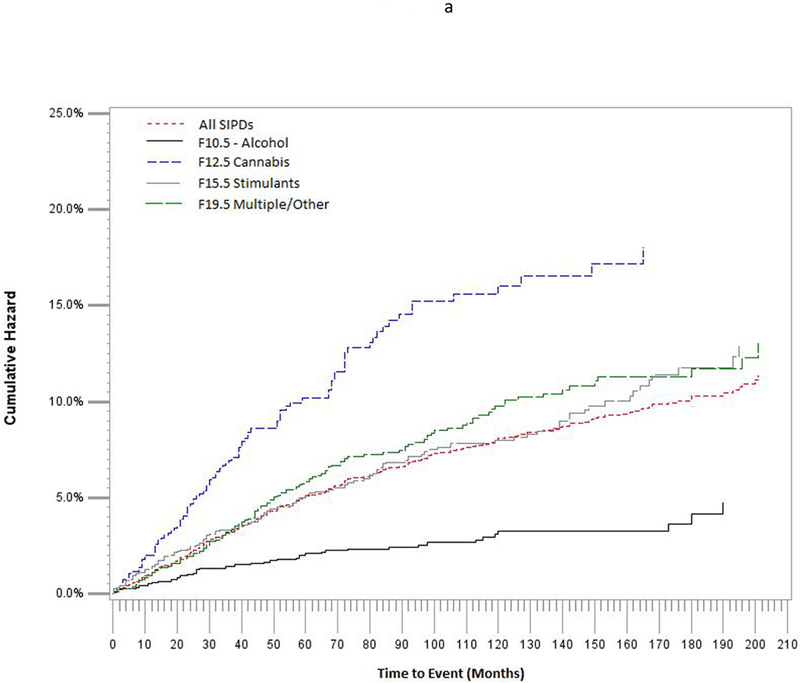
a Survival Curves for Schizophrenia in Cases of Substance Induced Psychotic Disorder as a Function of Time Since First Onset
b Cumulative Hazard for Schizophrenia in Cases of Substance Induced Psychotic Disorder as a Function of Age at SIPD Registration
c Rates of Receipt of Early Retirement for All Cases with Substance-Induced Psychotic Disorders Who Did versus Did Not Receive a Subsequent Schizophrenia (SZ) Diagnosis. Dotted Lines Indicate 95% Confidence Intervals
The mean time to schizophrenia conversion was 39 months. These converters had, during the period between their first SIPD and first schizophrenia diagnosis, a mean number 2.86 DA and 2.24 AUD registrations. We examined, in the general population, the correlations between our three FRS scores which were as follows: DA-AUD +0.34, DA-NAP +0.10 and DA-AUD +0.09.
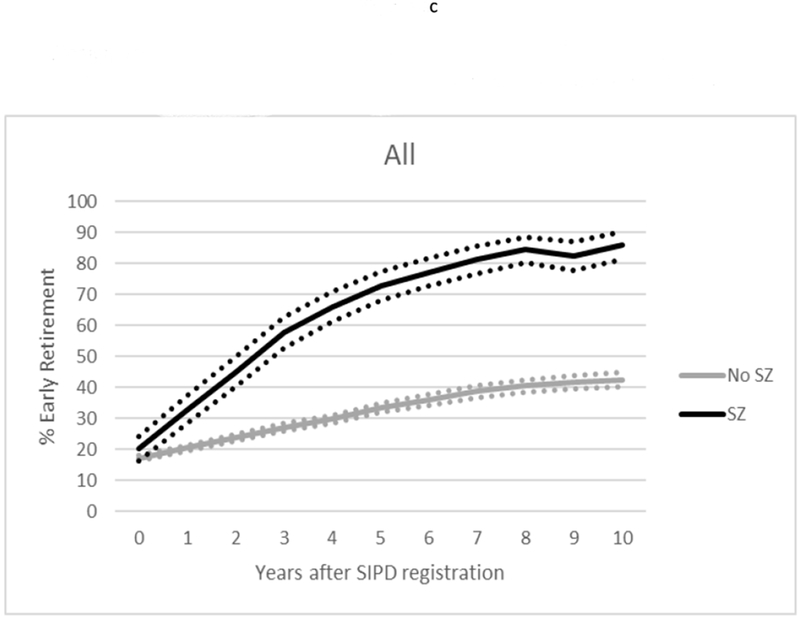
We evaluated differences in the occupational competence of SIPD cases who did versus did not receive a subsequent schizophrenia diagnosis by examining rates of receipt of early retirement in the 10 years after first SIPD diagnosis (figure 1c.). Such status is awarded by the Swedish Social Insurance Agency to individuals whose work capacity is judged to be substantially reduced for a long-term period or permanently. These rates differed significantly within one year of the first SIPD diagnosis and further diverged over the subsequent decade.
Familial Risk Scores and Prediction of Substance Induced Psychotic Disorder
As seen in table 2 (top half), the standardized FRS for DA, AUD and NAP were significantly increased for all SIPD cases. The FRS elevation was greatest for DA (mean standardized score = +1.09) which was significantly greater than the FRS in all non-SIPD cases of DA in the population (+0.82)(p <0.0001). The elevation in the AUD FRS in SIPD cases was slightly lower (+0.98) but also significantly greater than that seen in all non-SIPD AUD cases in the population (0.53)(p<0.0001). The mean elevation in FRS for NAP in SIPD cases was more modest (+0.35) and significantly lower than that seen in all non-SIPD cases of schizophrenia (+0.77)(p<0.0001).
Table 2.
Mean Standardized Familial Risk Scores for Drug Abuse (DA), Alcohol Use Disorder (AUD) and Non-Affective Psychosis (NAP) in Cases of Substance-Induced Psychotic Disorder (SIPD) Compared to the General Population and that Did versus Did Not Convert to Schizophrenia
| Prediction of | Conversion to Schizophrenia | All | F10.5 Alcohol | F12.5 Cannabis | F15.5 Stimulants | F19.5 (Multiple/Other) | P value across 4 specific forms of SIPD | |
|---|---|---|---|---|---|---|---|---|
| DA Familial Risk Score | SIPD in total population | -- | 1.09 1.02; 1.15 | 0.41 0.34; 0.49 | 1.25 1.06; 1.45 | 1.19 1.06; 1.32 | 1.57 1.43; 1.71 | <0.0001 |
| P-value difference* | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||
| AUD Familial Risk Score | SIPD in total population | -- | 0.98 0.93; 1.03 | 0.91 0.82; 0.99 | 0.61 0.50; 0.73 | 1.19 1.08; 1.31 | 1.09 0.99; 1.19 | <0.0001 |
| P-value difference* | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||
| NAP Familial Risk Score | SIPD in total population | -- | 0.35 0.30; 0.41 | 0.25 0.14; 0.37 | 0.47 0.32; 0.61 | 0.40 0.29; 0.52 | 0.39 0.30; 0.48 | <0.0001 |
| P-value difference* | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||
| DA Familial Risk Score | Schizophrenia in SIPD Cases | Yes | 1.11 0.85; 1.37 | 0.15 −0.12; 0.42 | 1.03 0.50; 1.55 | 1.59 0.98; 2.20 | 1.21 0.76; 1.67 | 0.0022 |
| DA Familial Risk Score | No | 1.08 1.02; 1.15 | 0.42 0.34; 0.50 | 1.28 1.08; 1.49 | 1.16 1.02; 1.30 | 1.60 1.45; 1.74 | <.0001 | |
| P-value difference | 0.3496 | 0.2227 | 0.0905 | 0.1147 | 0.1911 | |||
| AUD Familial Risk Score | Schizophrenia in SIPD Cases | Yes | 1.09 0.87; 1.32 | 1.01 0.40; 1.61 | 0.76 0.32; 1.21 | 1.39 0.91; 1.86 | 1.06 0.66; 1.46 | 0.0238 |
| AUD Familial Risk Score | No | 0.97 0.92; 1.02 | 0.90 0.82; 0.99 | 0.60 0.48; 0.71 | 1.18 1.06; 1.29 | 1.09 0.99; 1.19 | <.0001 | |
| P-value difference | 0.3531 | 0.1804 | 0.4909 | 0.1255 | 0.2209 | |||
| NAP Familial Risk Score | Schizophrenia In SIPD Cases | Yes | 0.67 0.40; 0.95 | 0.81 0.27; 1.35 | 0.79 0.20; 1.38 | 0.78 0.11; 1.45 | 0.58 0.12; 1.03 | 0.6270 |
| NAP Familial Risk Score | No | 0.33 0.28; 0.39 | 0.24 0.12; 0.36 | 0.43 0.28; 0.58 | 0.37 0.27; 0.48 | 0.38 0.29; 0.47 | <.0001 | |
| P-value difference | <0.0001 | <0.0001 | 0.0931 | 0.0011 | 0.0164 |
Compared with the general population born 1940-1995. The p-values are calculated using a non-parametric approach; the Van der Waerden Scores.
These scores differed significantly across our four common forms of SIPD. Alcohol-induced PD and multiple substance induced PD had, respectively, the lowest and highest familial risk for DA. Cannabis PD and stimulant-induced PD had, respectively, the lowest and highest familial risk for AUD. Alcohol- and cannabis-induced PD had, respectively, the lowest and highest familial risk for NAP.
Predictors of Conversion to Schizophrenia
We first examined the following non-familial risk factors for conversion, i) location of SIPD diagnosis, ii) length of hospitalization among those hospitalized, iii) registrations for DA, AUD or SIPD after the initial SIPD episode. All these variables significantly predicted risk for subsequent schizophrenia controlling for sex and age at SIPD registration. Compared to registration occurring in primary care, the HR for schizophrenia was 2.06 (1.13; 3.76) in those diagnosed in specialist care and 2.77 (1.57; 4.88) in hospital. Among those hospitalized for SIPD (n=4,553), compared to those hospitalized for only 1 day, those hospitalized for 2-3, 4-7 days and 8 or more days had the following HRs for developing schizophrenia: 0.87 (0.62; 1.21), 1.00 (0.71; 1.39) and 2.21 (1.70; 2.87). Finally, risk for conversion to schizophrenia was increased by an additional registration, after the first SIPD diagnosis for DA [HR=1.60 (1.27; 2.02)], AUD [1.36 (1.11; 2.65)] or SIPD [2.86 (2.35; 3.47)].
We then explored familial risk factors (table 2 – bottom) examining the standardized FRS for NAP, DA and AUD in the SIPD cases who did versus did not progress to schizophrenia. While these two groups did not differ significantly in their FRS for DA or AUD, the NAP FRS of patients who converted to schizophrenia was twice as high (+0.67) as those who did not convert (+0.33) (p<0.0001). No significant differences were seen in the FRS NAP scores across the four specific forms of SIPD.
Table 3 compares, in the general population, our FRS scores for all cases of DA, AUD and schizophrenia with and without SIPD. Compared to cases of DA without SIPD, cases with SIPD have a 15% and 68% elevation in their FRS for DA and AUD but a 300% increased risk for NAP (all p< 0.0001). Compared to cases of AUD without SIPD, cases with SIPD have a 180% and 75% elevation in their FRS for DA and AUD and a 244% increased risk for NAP (all p< 0.0001).
Table 3.
Mean Standardized Familial Risk Scores for Drug Abuse (DA), Alcohol Use Disorder (AUD) and Non-Affective Psychosis (NAP) in Cases of Schizophrenia, Drug Abuse and Alcohol Use Disorder With and Without a Prior Diagnosis of Substance-Induced Psychotic Disorder (SIPD)
| Genetic Risk Score (NAP) | Genetic Risk Score (DA) | Genetic Risk Score (AUD) | |
|---|---|---|---|
| DA – No SIPD | 0.13 (0.13; 0.14) | 0.82 (0.81; 0.83) | 0.56 (0.55; 0.56) |
| DA – SIPD | 0.39 (0.35; 0.44) | 1.06 (1.01; 1.12) | 0.94 (0.90; 0.98) |
| P-value difference | <0.0001 | <0.0001 | <0.0001 |
| AUD – No SIPD | 0.09 (0.08; 0.09) | 0.25 (0.24; 0.25) | 0.53 (0.53; 0.54) |
| AUD – SIPD | 0.31 (0.27; 0.36) | 0.70 (0.65; 0.74) | 0.93 (0.89; 0.98) |
| P-value difference | <0.0001 | <0.0001 | <0.0001 |
| SZ – No SIPD | 0.77 (0.73; 0.82) | 0.04 (0.03; 0.06) | 0.20 (0.19; 0.22) |
| SZ – SIPD | 0.66 (0.51; 0.80) | 0.78 (0.66; 0.91) | 0.88 (0.76; 1.00) |
| P-value difference | 0.1676 | <0.0001 | <0.0001 |
The p-values (One-sided test) are calculated using a non-parametric approach; the Van der Waerden Scores.
Compared to all cases of schizophrenia without SIPD, those with SIPD who develop into schizophrenia have highly significant elevated FRS for DA and AUD, but their level of NAP FRS do not significantly differ. In particular, the mean NAP FRS for alcohol, cannabis and stimulant induced PD that evolve into schizophrenia (respectively +0.81, +0.79 and +0.78) are nearly identical to the observed mean FRS for all non-SIPD cases of schizophrenia (+0.77).
Development of a Risk Calculator
We fitted a multivariate regression model to a random training-half of the cohort including i) location of SIPD diagnosis, ii) registrations for DA, AUD or SIPD after the initial SIPD episode, iii) additional SIPD registrations after the initial SIPD diagnosis, iv) FRS for DA, NAP and AUD, v) Age at SIPD registration, vi) gender, and vii) type of SIPD. Results from that model were then applied to the second random half as the test sample. Dividing our sample into deciles, our predictor obtained a HR for schizophrenia outcome per decile of 1.40 (1.32–1.49). The uniquely significant predictors in this model were: male sex, early age at first registration, high FRS for NAP, first diagnosis in specialist or in-patient care, and additional SIPD diagnoses.
Figure 2 displays the HRs for these deciles compared with the lowest risk group. Compared to the 1st decline, the 9th and 10th deciles of risk had HRs of 15.2 (9.5-24.3) and 21.3 (12.6-36.2), respectively. ROC analysis provided an area under the curve of 0.74 (0.71-0.77) (appendix figure 1).
Figure 2:
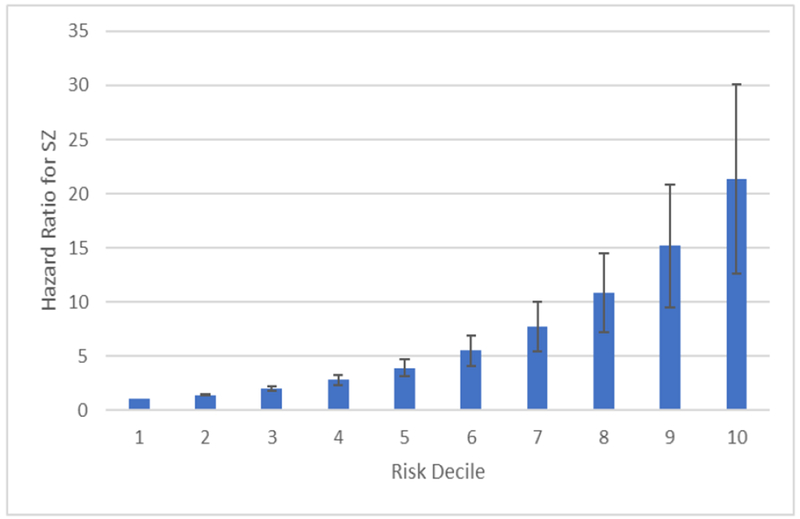
Hazard Ratios (compared to lowest risk group) for Schizophrenia in Patients with Substance Induced Psychotic Disorder Divided into Deciles of Risk
DISCUSSION
This paper had three major goals the first of which was to determine how well results in Sweden replicated the two previous longitudinal cohort studies of SIPD (8;9). The specific conversion rates differed widely across studies (11.3% in this study, 17.3% in Scotland and 46% in Finland), but much of this variation likely resulted from differences in follow-up time and breadth of definition which varied from schizophrenia spectrum in Finland to narrowly defined schizophrenia in our study. These three samples also produced a range of more consilient findings including i) alcohol-induced psychotic disorder (PD) having the latest age at onset of any SIPD type and the lowest conversion rate to schizophrenia, ii) cannabis-induced PD having among the lowest age at onset and highest conversion rate to schizophrenia, iii) male sex and younger age at SIPD diagnosis predicting higher risk of conversion, and iv) shorter SIPD hospitalizations predicting lower conversion risk.
Our second goal was to use information about FRS to evaluate etiologic hypotheses about who develops SIPD and given SIPD who progresses to schizophrenia. Focusing first on SIPD, we could confidently reject the hypothesis that SIPD arises solely from the psychotogenic effects of the substances of abuse. Individuals with SIPD had, on average, one-third of a standard deviation higher FRS for NAP than the general population – a highly significant difference. Our findings are congruent with prior evidence that among methamphetamine users, the risk for schizophrenia, assessed by family history, was significantly higher in those who did versus did not develop methamphetamine-induced psychosis (15).
But our results also support an effect of substances of abuse on SIPD. The mean RFS NAP scores differed significantly across our drug classes, being lowest for alcohol. Compared to the other substances studied, the psychotic symptoms emerging from heavy drinking are more likely to be influenced by direct pharmacologic effects and less by the individual’s liability to psychosis. Our FRS analyses also clarify the familial impact of risks for DA and AUD on SIPD. Cases of SIPD had considerably higher familial risk for DA and AUD than they did for psychosis. Finally, the mean familial DA and AUD risks for our SIPD cohort were higher than that seen in DA and AUD cases without SIPD in Sweden. Thus, an elevated familial risk to DA and AUD plays an important etiologic role in SIPD.
Turning to the conversion of SIPD to schizophrenia, we also obtained clear results. Familiar risk for DA or AUD do not impact on risk for schizophrenia given SIPD as the mean DA and AUD FRS scores did not differ in SIPD cases who did versus did not convert to schizophrenia. However, NAP FRS scores were twice as high in the SIPD cases who did versus did not later receive a schizophrenia diagnosis. Finally, across all our cases, the mean NAP FRS did not differ between individuals with schizophrenia who did not versus did have a prior SIPD diagnosis. That is, with respect to familial risk for psychosis, SIPD patients who develop schizophrenia are indistinguishable from other cases of schizophrenia without a history of SIPD. These results support the hypothesis that in SIPD, drugs of abuse may precipitate the development of schizophrenia but do not typically have a strong causal role in the emergence of the chronic psychosis. If drug exposure caused the schizophrenia disorder, such affected individuals should, on average, have lower familial psychosis risk than typical cases of schizophrenia which they do not. Our findings are consistent with those reported by Tsuang (16) who found that risk for schizophrenia in the first-degree relatives of SIPD closely resembled that found in the relatives of a group of typical schizophrenic probands.
We were able to validate our diagnostic results by comparing receipt of early retirement benefits in SIPD cases. Those subsequently diagnosed with schizophrenia were twice as likely to receive such benefits as those without the diagnosis and this difference emerged quite early in their post-SIPD course, prior to the time that many of them received their schizophrenia diagnosis.
Our third goal was to develop a risk calculator to predict progression for SIPD to schizophrenia. We generated and then testing our model on random split-halves of our sample. The predictive power of our model was substantial, as 47% of converting SIPD cases were found in the upper 2 deciles and our area under the curve results (74%) were substantial.
What can we learn from our analyses about the nature of the cannabis-schizophrenia association (5;17)? Cannabis-associated SIPD stood out from the other subforms in having i) the earliest age at onset, ii) highest risk for conversion to schizophrenia and iii) highest FRS for NAP. Converted cases of cannabis SIPD had the same familial risk for SZ as typical SZ cases. In our multivariate prediction model, where NAP FRS were controlled for, cannabis use no longer predicted an elevated risk for conversion to schizophrenia. Our results suggest that the high conversion rate to schizophrenia in cannabis-induced PD is at least in part a result of the high familial risk for NAP rather than solely a result of the specific pharmacological effect of cannabis. Our findings do not directly contradict claims for a causal relationship between heavy cannabis exposure and schizophrenia (17). But, in accord with our prior findings from a co-relative study of cannabis abuse and schizophrenia in a Swedish national study (18), they do suggest that the observed cannabis abuse-schizophrenia association is not entirely causal but results in part to some sharing of familial/genetic risk for cannabis abuse and schizophrenia (18).
Limitations
Our results should be interpreted in the context of four potential methodological limitations. First, our findings are applicable only to the Swedish population and may or may not extrapolate to other countries. Second, while ascertaining cases of DA, AUD and schizophrenia from registry data has important advantages, especially independence from subject cooperation and accurate recall, it also may have significant limitations. For DA and AUD, there are surely false negatives for individuals who abuse substances but avoid medical or police attention. However, the validity of our detection of these syndromes is supported by evidence for strong associations of cases detected from different registries. The mean OR for case detection across our relevant registries was 52 for DA (19) and 33 for AUD was 33 (20). While diagnoses of schizophrenia were recorded by diverse clinicians, studies have found, using record reviews (21) and diagnostic interviews (22), that 96% and 94% of Swedish cases with hospital schizophrenia diagnoses, respectively, fulfilled DSM-IV criteria. Furthermore, our schizophrenia diagnoses were validated by showing strong associations with assignment of early retirement. Third, our analyses required only one schizophrenia diagnosis to consider an SIPD case a “converter.” Perhaps this is too weak a threshold. We therefore repeated all our major analyses requiring at least two separate diagnosis (see appendix figure 2, tables 1–2). Results did not change appreciably. Fourth, could the high conversion rate of cannabis-SIPD to schizophrenia result from mis-diagnosing cases of true schizophrenia? If this occurred, it would predict that cannabis-SIPD cases should receive a higher rate of early disability than other SIPD cases. This was not seen (figure 1c, appendix figure 3).
Conclusions
SIPD arises in individuals with high familial liability to drug and alcohol abuse and a moderate familial vulnerability to psychosis (roughly mid-way between that seen in the general population and in schizophrenia). Thus, SIPD likely arises from both substantial drug exposure and elevated psychosis liability. Only alcohol-induced psychotic disorder may differ in requiring less familial vulnerability to psychosis. A modest proportion of cases of SIPD “convert” to schizophrenia. The probability of conversion can be well predicted from a range of risk factors including early age at first SIPD, male sex, and further DA, AUD or especially SIPD episodes. Familial liability to psychosis, but not to substance abuse, strongly predicts this conversion. Indeed, the familial psychosis liability to typical schizophrenia and schizophrenia following SIPD are indistinguishable. Schizophrenia following SIPD is better explained as a drug-precipitated disorder in a highly vulnerable individual rather than as a syndrome predominantly caused by drug exposure.
Supplementary Material
Disclosures and Acknowledgments:
None.
Grant Support: This project was supported by grants R01DA030005 and R01AA023534 from the National Institutes of Health, NIAAA grant the Swedish Research Council (K2012-70X-15428-08-3), the Swedish Research Council for Health, Working Life and Welfare (In Swedish: Forte; Reg.nr: 2013-1836), the Swedish Research Council (2012-2378; 2014-10134) and FORTE (2014-0804) as well as Avtal om Läkarutbildning och Forskning (ALF) funding from Region Skåne.
Footnotes
Compliance with Ethical Standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. We secured ethical approval for this study from the Regional Ethical Review Board of Lund University (No. 2008/409).
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Location of where work was done: Lund University, Virginia Commonwealth University
Conflicts of Interest: None of the authors have any conflicts of interest to declare.
Reference List
- 1.Kraepelin E: Clinical Psychiatry: A Text-Book for Students and Physicians. (Abstracted and adapted from the sixth German edition of Kraepelin’s “Lehrbuch der Psychiatrie” by A. Ross Diefendorf, MD). New York: The Macmillan Company; 1904. [Google Scholar]
- 2.Kraepelin E: Psychiatry, A Textbook for Students and Physicians (Translation of the 6th Edition of Psychiatrie-Translator Volume 2-Sabine Ayed). Editor: Jaques Quen. ed. Canton MA: Science History Publications; 1990. [Google Scholar]
- 3.Connell PH: Amphetamine Psychosis: Maudsley monographs, No.5, Institute of Psychiatry. London: Chapman and Hall, Ltd.; 1958. [Google Scholar]
- 4.Thirthalli J, Benegal V: Psychosis among substance users. Curr Opin Psychiatry 2006; 19(3):239–45. [DOI] [PubMed] [Google Scholar]
- 5.Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jorgensen P: Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry 2005; 187:510–5. [DOI] [PubMed] [Google Scholar]
- 6.Crebbin K, Mitford E, Paxton R, Turkington D: First-episode drug-induced psychosis: a medium term follow up study reveals a high-risk group. Soc Psychiatry Psychiatr Epidemiol 2009; 44(9):710–5. [DOI] [PubMed] [Google Scholar]
- 7.Kittirattanapaiboon P, Mahatnirunkul S, Booncharoen H, Thummawomg P, Dumrongchai U, Chutha W: Long-term outcomes in methamphetamine psychosis patients after first hospitalisation. Drug Alcohol Rev 2010; 29(4):456–61. [DOI] [PubMed] [Google Scholar]
- 8.Niemi-Pynttari JA, Sund R, Putkonen H, Vorma H, Wahlbeck K, Pirkola SP: Substance-induced psychoses converting into schizophrenia: a register-based study of 18,478 Finnish inpatient cases. J Clin Psychiatry 2013; 74(1):e94–e99. [DOI] [PubMed] [Google Scholar]
- 9.Alderson HL, Semple DM, Blayney C, Queirazza F, Chekuri V, Lawrie SM: Risk of transition to schizophrenia following first admission with substance-induced psychotic disorder: a population-based longitudinal cohort study. Psychol Med 2017; 47(14):2548–55. [DOI] [PubMed] [Google Scholar]
- 10.Murray RM, Paparelli A, Morrison PD, Marconi A, Di FM: What can we learn about schizophrenia from studying the human model, drug-induced psychosis? Am J Med Genet B Neuropsychiatr Genet 2013; 162B(7):661–70. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan PF, Kendler KS, Neale MC: Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 2003; 60(12):1187–92. [DOI] [PubMed] [Google Scholar]
- 12.Lichtenstein P, Yip BH, Bjork C, Pawitan Y, Cannon TD, Sullivan PF, Hultman CM: Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 2009; 373(9659):234–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luepsen H: Comparison of non-parametric analysis of variance methods: A vote for van der Waerden. Commun Stat Simul Comput 2018; 47(9):2547–76. [Google Scholar]
- 14.SAS Institute I. SAS/STAT® Online Documentation, Version 9.4 Cary, N.C.: SAS Institute, Inc; 2012. [Google Scholar]
- 15.Chen CK, Lin SK, Sham PC, Ball D, Loh e, Murray RM : Morbid risk for psychiatric disorder among the relatives of methamphetamine users with and without psychosis. Am J Med Genet B Neuropsychiatr Genet 2005; 136(1):87–91. [DOI] [PubMed] [Google Scholar]
- 16.Tsuang MT, Simpson JC, Kronfol Z: Subtypes of drug abuse with psychosis. Demographic characteristics, clinical features, and family history. Arch Gen Psychiatry 1982; 39(2):141–7. [DOI] [PubMed] [Google Scholar]
- 17.Marconi A, Di FM, Lewis CM, Murray RM, Vassos E: Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis. Schizophr Bull 2016; 42(5):1262–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giordano GN, Ohlsson H, Sundquist K, Sundquist J, Kendler KS: The association between cannabis abuse and subsequent schizophrenia: a Swedish national co-relative control study. Psychol Med 2015; 45(2):407–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kendler KS, Sundquist K, Ohlsson H, Palmer K, Maes H, Winkleby MA, Sundquist J: Genetic and familial environmental influences on the risk for drug abuse: a national Swedish adoption study. Arch Gen Psychiatry 2012; 69(7):690–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kendler KS, Ji J, Edwards AC, Ohlsson H, Sundquist J, Sundquist K: An Extended Swedish National Adoption Study of Alcohol Use Disorders. JAMA Psychiatry 2015; 72(3):211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lichtenstein P, Bjork C, Hultman CM, Scolnick E, Sklar P, Sullivan PF: Recurrence risks for schizophrenia in a Swedish national cohort. Psychol Med 2006; 36(10):1417–25. [DOI] [PubMed] [Google Scholar]
- 22.Ekholm B, Ekholm A, Adolfsson R, Vares M, Osby U, Sedvall GC, Jonsson EG: Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nord J Psychiatry 2005; 59(1):457–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


