Abstract
People with mental illness experience increased chronic disease burden, contributed to by a greater prevalence of modifiable chronic disease risk behaviours. Policies recommend mental health services provide preventive care for such risk behaviours. Provision of such care has not previously been synthesised. This review assessed the provision of preventive care for modifiable chronic disease risk behaviours by mental health services. Four databases were searched from 2006 to 2017. Eligible studies were observational quantitative study designs conducted in mental health services, where preventive care was provided to clients for tobacco smoking, harmful alcohol consumption, inadequate nutrition, or inadequate physical activity. Two reviewers independently screened studies, conducted data extraction and critical appraisal. Results were pooled as proportions of clients receiving or clinicians providing preventive care using random effects meta-analyses, by risk behaviour and preventive care element (ask/assess, advise, assist, arrange). Subgroup analyses were conducted by mental health service type (inpatient, outpatient, other/multiple). Narrative synthesis was used where meta-analysis was not possible. Thirty-eight studies were included with 26 amenable to meta-analyses. Analyses revealed that rates of assessment were highest for smoking (78%, 95% confidence interval [CI]:59%–96%) and lowest for nutrition (17%, 95% CI:1%–35%); with variable rates of care provision for all behaviours, care elements, and across service types, with substantial heterogeneity across analyses. Findings indicated suboptimal and variable provision of preventive care for modifiable chronic disease risk behaviours in mental health services, but should be considered with caution due to the very low quality of cumulative evidence.
PROSPERO registration: CRD42016049889.
Keywords: Mental health services, Care provision, Smoking, Alcohol, Nutrition, Physical activity
Highlights
-
•
First meta-analysis of chronic disease preventive care provided by mental health service settings
-
•
Assessed preventive care for smoking, alcohol, nutrition, and physical activity in mental health settings
-
•
Provision of preventive care varied across risk behaviours, care elements, and service types.
-
•
Findings indicate suboptimal provision of preventive care for health risk behaviours.
1. Introduction
People with a mental illness experience greater rates of preventable morbidity, mortality, and a reduced life expectancy up to 30 years compared to people without such an illness (Brown et al., 2010; Laursen et al., 2013; Wahlbeck et al., 2011; Chang et al., 2011; Lawrence et al., 2013; Walker et al., 2015; Olfson et al., 2015; Erlangsen et al., 2017). In high income countries, such disparities are primarily due to a greater prevalence of chronic disease (Brown et al., 2010; Walker et al., 2015; Callaghan et al., 2014; Markkula et al., 2012). This inequitable disease burden is consistently reported to be associated with a greater prevalence of four leading modifiable chronic disease risk behaviours: tobacco smoking, harmful alcohol consumption, inadequate nutrition, and inadequate physical activity (Callaghan et al., 2014; Scott and Happell, 2011; Stanley and Laugharne, 2014; Australian Institute of Health and Welfare, 2012; World Health Organization, 2013).
Care to support and facilitate improvements or reductions in such modifiable chronic disease risk behaviours has been termed ‘preventive care’ (Hensrud, 2000; Woolf et al., 2006; Hulscher et al., 1997). A recommended strategy for addressing such behaviours is the provision of preventive care by health care providers, (Australian Health Ministers' Advisory Council, 2017) with Cochrane systematic review evidence supporting provision of preventive care for such behaviours in general health care settings for risk behaviour improvement (Rees et al., 2013; Hillsdon et al., 2005; Rice et al., 2013; Rigotti et al., 2012; Brunner et al., 2007; Foster et al., 2005). Systematic review evidence demonstrates significant improvements in prevalence of such behaviours among people with a mental illness following the receipt of health promotion programs provided by mental health services (Verhaeghe et al., 2011; Cabassa et al., 2010; Naslund et al., 2017; Happell et al., 2012a). The provision of systematic preventive care is recommended in all health care settings, including mental health services, to all adult clients; (NSW Department of Health, 2017a; NSW Department of Health, 2017b; NSW Mental Health Commission, 2014; National Preventive Health Taskforce, 2008; Royal Australian College of General Practitioners, 2004; Agency for Healthcare Research and Quality, 2010; National Institute for Health and Care Excellence, 2010; National Institute for Health and Care Excellence, 2013; Glasgow et al., 2004; US Department of Health and Human Services, 2009) with tobacco smoking, harmful alcohol consumption, inadequate nutrition, and inadequate physical activity often addressed together in clinical guidelines and recommendations (Royal Australian College of General Practitioners, 2004). The ‘5As’ framework is one recommended approach to facilitate the routine delivery of preventive care (‘ask’ about engagement in risk behaviours; ‘assess’ behaviour risk status and interest in change; ‘advise’ changing/reducing risk behaviours; provide behaviour change ‘assistance’; and ‘arrange’ or refer to other services for behaviour change support (Glasgow et al., 2004).
Despite the effectiveness of preventive care provision in addressing chronic disease risk behaviours in health services, little research has focused on the extent to which any elements of preventive care are delivered by mental health settings. A review of the literature identified two previous reviews of the provision of preventive care within mental health services (Wye et al., 2011; Dickens et al., 2019). A narrative review exploring the provision of care to address smoking within psychiatric inpatient settings cited four studies from the USA and Australia, reported provision of care narratively (Wye et al., 2011). A more recent review (2019) explored mental health nurses' experiences of providing physical health care, with a focus on their attitudes rather than provision of care (Dickens et al., 2019). The review included 41 studies examining general physical health care, sexual health, smoking, physical activity, and nutrition. Six included studies reported advise on regular exercise was provided ‘always or very often’ by 50.4% to 79.7% of participants, advise on healthy diet was provided ‘always or very often’ by 43.4% to 86.7% of participants, and 30.6% to 66.7% of participants reported aiding smoking cessation ‘always or very often’ (Dickens et al., 2019). Whilst the review utilised a broad definition of physical healthcare, limitations included: only exploring mental health nurses' provision of care; outcomes not reported by service type; no meta-analysis due to the broad inclusion criteria and different study methodologies (Dickens et al., 2019). A number of additional individual observational studies have examined preventive care provision for all four risk behaviours in mental health services, utilising varied methodologies (client and clinician self-report, and cross-sectional, pre-post, and interrupted time series surveys; and retrospective medical record audits), however findings have not been quantitatively synthesised previously (Stanley and Laugharne, 2013; Bartlem et al., 2015; Bartlem et al., 2014a; Happell et al., 2013a; Howard and Gamble, 2011). As findings have not been synthesised by mental health service type, it is unknown whether rates of preventive care provision are consistent across service types or otherwise. A systematic synthesis of the extent to which preventive care is provided for all four health risk behaviours to clients of mental health services is lacking. An identification of risk behaviours that receive inadequate care provision, or identifying which elements of care are provided least often could inform the tailoring of future interventions to increase the provision and benefits of preventive care by mental health services.
Given the limitations of previous research, a systematic review and meta-analysis was conducted of the prevalence of preventive care provision for four modifiable chronic disease risk behaviours (tobacco smoking, harmful alcohol consumption, inadequate nutrition, and inadequate physical activity) by mental health services. A secondary aim was to quantify pooled prevalence estimates of preventive care provision for each risk behaviour by care element and service type, and conduct a narrative synthesis where meta-analysis was not possible.
2. Methods
Review methods and protocol were prospectively registered with PROSPERO [reference number CRD42016049889]. The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) informed the development of the review protocol (Moher et al., 2015) and reporting of findings (Moher et al., 2009; Stroup et al., 2000).
2.1. Search methods
Four databases were searched from January 2006 to August 2017: Medline, PsycINFO, EMBASE, and CINAHL. As clinical practice guidelines for the provision of preventive care have only been introduced recently, (Fiore et al., 2008; Department of Health N, 2009) the search commenced from 2006. Search terms pertained to mental illness and mental health service settings, eligible study designs, four chronic disease risk behaviours of interest, and preventive care practices. Search terms for preventive care practices used a variety of terms to capture care provided by the 5A care elements and any reports of individual care components to account for differences in terminology internationally (Appendix A). Additional sources searched for eligible studies included: first 200 articles from Google Scholar; hand searching of articles published between 2015 and 2017 from Preventive Medicine and Psychiatric Services; and reference lists of included studies. Authors of included studies were contacted and any related publications were requested and screened for eligibility. JBa developed and executed the search strategies with assistance from a research librarian.
2.2. Study eligibility criteria
Study type: Descriptive studies including: observational and cross-sectional surveys; retrospective medical record audits; and longitudinal repeated measures were included. Only baseline data from experimental study designs were included.
Setting: Eligible studies were conducted in services with the primary objective of delivering mental health care to adult clients (≥18 years), and could consist of: bed-based (inpatient) mental health services; specialised community (outpatient) mental health services; or community psychosocial support services (non-clinical mental health services). Dual diagnosis services (mental health and substance use treatment) were included if mental health care was a primary care objective. Studies were eligible if preventive care was provided by mental health service staff in the context of routine care delivery.
Outcome measures: Eligible measures included quantitative reporting of the provision or receipt of any elements of preventive care provision for any of four chronic disease risk behaviours (tobacco smoking, harmful alcohol consumption, inadequate nutrition, inadequate physical activity). The World Health Organisation (WHO) has released guidelines for each of the four modifiable risk behaviours, (World Health Organization, 2017; World Health Organization, 2018; World Health Organization, 2011; World Health Organization, 2003) and Australia, (National Health and Medical Research Council, 2009; National Health and Medical Research Council, 2013; Department of Health, 2014; Ministerial Council on Drug Strategy, 2011) and other nations (Piercy et al., 2018; Her Majesty's Government, 2011; Canadian Society for Exercise Physiology, 2011; Ministry of Health, 2015; U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015; Public Health England, 2016; Health Canada, 2019; Centers for Disease Control and Prevention, 2014; Centers for Disease Control and Prevention, n.d.; Department of Health, 2016; Department of Health and Social Care, 2018; Health Canada, 2018; Ministry of Health, 2007; Butt et al., 2011) similarly have developed ‘country specific’ definitions or guidelines as to what constitutes risk. In the present review, eligible studies were not required to report the definition of risk used for each risk behaviour and variations were expected across countries and studies.
2.3. Study selection process
Identified citations were compiled in Endnote, (Anon, 2016) duplicates removed, and remaining citations and abstracts uploaded to Covidence (Anon, n.d.). Two independent reviewers screened titles and abstracts (any of JBa, TB, PW, ES, DT, JD, RC, KB, RH, TR) and relevant full texts (JBa and one of: TB, PW, KB, AM, TR, DT, JD, RH) against predetermined eligibility criteria. Disagreements regarding study eligibility were resolved via consensus or a third reviewer (PW or KB). Corresponding authors were contacted where reported study characteristics were insufficient to determine eligibility, or where outcome data were missing or insufficiently reported.
2.4. Data extraction
Data were extracted independently by two authors (JBa and one of: TB, AM, DT, KB, TR) using an Excel-based extraction form, with any inconsistencies resolved by a third reviewer (PW, KB, ES). Where reported, extracted data included study year, setting, sample size, data source (client report, clinician report, medical record audit), study eligibility criteria, clinical and demographic characteristics of mental health service clients and clinicians, clinician engagement in risk behaviours, policies of the mental health service related to preventive care provision, outcome measures, and information required to conduct assessment of methodological quality. Data were extracted separately for each relevant preventive care element and for each risk behaviour (smoking, alcohol, nutrition, physical activity). For intervention studies, only baseline data were extracted. For longitudinal studies, the most recent data were extracted as it was considered to most closely represent current practice.
2.5. Data analysis and synthesis
Outcome measures were grouped by data type: clinician reported; client reported; or medical record audit. Preventive care reported in any form/terminology was categorised into the relevant 5A care elements (ask, assess, advise, assist, arrange/refer), and findings were reported using the framework for ease of reporting. The ‘ask’ and ‘assess’ elements of care were combined for analysis. Client reported and audit data were combined for analysis as they represented care provided to individual clients, whereas clinician reported data was reported separately as they represent the proportion of clinicians providing care to an unknown number of clients, consistent with a previous review of smoking care provision in hospitals (Freund et al., 2008).
To facilitate meta-analyses clinician reported data were converted to a common variable of ‘care provision to at least 50% of clients’. For instance, studies reporting care provision to a specific proportion of clients (such as 78%)(Price et al., 2007; Etter et al., 2008; Schacht et al., 2012; Zabeen et al., 2015) were combined with studies reporting care to ‘more than 60% of clients’, (Anderson et al., 2013) ‘50–100%’, (Bartlem et al., 2014a; Chwastiak et al., 2013) and ‘80–100%’ (Bartlem et al., 2014a). Clinician data utilising categorical responses to describe the frequency of care provision (for example, ‘always’) were not pooled in meta-analysis due to the subjective and nonspecific nature. Where a study reported multiple data points for a single care element and behaviour (for instance, 0% of clients were referred to a smoking cessation quitline, and 12% were referred to smoking cessation group education or treatment)(Williams et al., 2015) both the highest and lowest proportions of care provided/received were utilised in separate meta-analyses to reflect the most and least optimistic estimations of care provision. If outcome data were incomplete (missing numerators, denominators, or proportions), data were calculated and backfilled using available data from the studies.
Pre-specified meta-analyses were conducted in RStudio, (RStudio Team, 2015) by JBa with the assistance of a statistician and guidance of ES and RH, where comparable outcome measures were pooled. Random-effects models were utilised to determine pooled prevalence estimates for each preventive care element by each risk behaviour; calculated as proportions and 95% confidence intervals (CIs). Random-effects models were selected as heterogeneity between studies was expected given the different contexts, settings, and delivery of preventive care reported (Deeks et al., 2017; Borenstien et al., 2009). Meta-analyses were conducted where at least two studies contributed data for an outcome measure (Deeks et al., 2017). Heterogeneity in the pooled estimates was assessed via visual inspection of forest plots and consideration of the I2 statistic (Deeks et al., 2017). Where substantial, heterogeneity was explored via subgroup and sensitivity analyses. Where data could not be combined for meta-analysis, narrative summary was undertaken.
2.6. Assessment of methodological quality
The methodological quality of each study was assessed independently by two reviewers (JBa and one of: AM, TR, RC, DT, JD, KB) using the Joanna Briggs Institute Critical Appraisal tool: Checklist for Prevalence Studies (Appendix B) (Munn et al., 2015). The following nine domains were assessed: appropriateness of sample frame; appropriateness of participant recruitment; adequacy of sample size; sufficient description of subjects and setting; analysis conducted with sufficient coverage of subgroups; measurement or classification bias; reliable measurement of condition; appropriateness of statistical analysis; and adequacy of response rate. Disagreements were resolved through consensus via discussion or with a third reviewer (KB, JBo).
2.7. Subgroup and sensitivity analyses
Where possible, pre-specified subgroup analyses were conducted by: mental health service type: inpatient setting; outpatient setting; and other/multiple service settings. Where heterogeneity was substantial (I2 > 50%; chi-square p < 0.1)(Deeks et al., 2017) post-hoc subgroup analyses were conducted by data type, analysing client reported and medical record audit data separately to explore this. Post-hoc subgroup analyses were also conducted by country.
Pre-specified sensitivity analyses were conducted to exclude studies categorised as high risk of bias (scoring>1 ‘no’ response on methodological quality tool) (Munn et al., 2015). Additional sensitivity analyses were conducted to exclude any studies utilising data that were calculated by the reviewers for the purpose of the review. Furthermore, sensitivity analyses were conducted on clinician reported data to exclude studies reporting any data not in the form of an exact proportion of care provision (for example, ‘80–100%’).
2.8. Assessment of confidence in cumulative evidence
Confidence in the cumulative evidence of the primary review outcomes (pre-specified meta-analyses of the provision of care elements by each risk behaviour) were assessed by JBa using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach (GRADE Working Group, 2004; Guyatt et al., 2008a; Guyatt et al., 2008b; Ryan and Hill, n.d.).
2.9. Differences between protocol and review
Studies published in languages other than English were originally excluded at full text screening due to inadequate funding for translation as stated in the protocol. However, those studies were subsequently translated to determine eligibility; with consultation from corresponding authors where requested. Data extraction was conducted by two reviewers independently rather than by one reviewer, with a second reviewer checking for consistency, as stated in the protocol. Additionally, the assessment of the cumulative evidence of the main outcomes through the GRADE approach was planned post protocol registration.
3. Results
3.1. Study selection
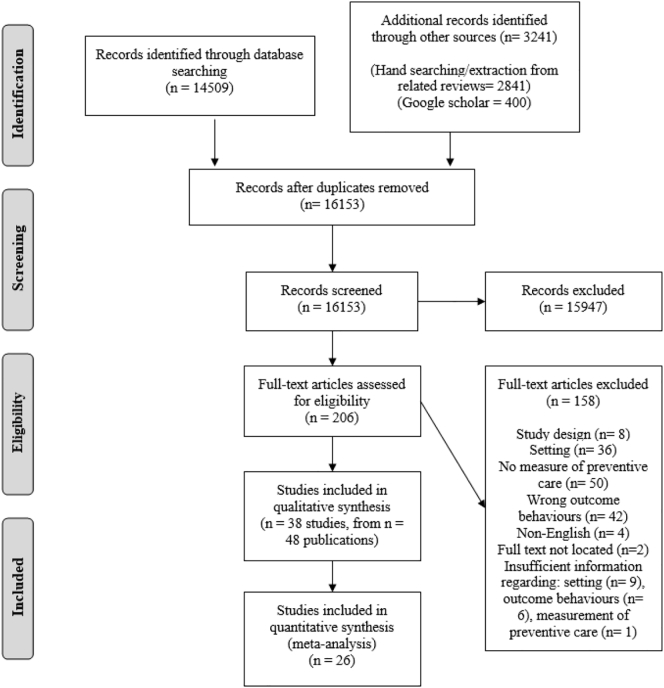
After duplicates were removed, 16,153 titles and abstracts were screened, 206 studies underwent full-text screening, with 38 studies eligible for inclusion in the review across 48 publications (Fig. 1). Twenty-one studies reported data amenable to meta-analyses; data from 12 studies, which could not be combined for meta-analysis, were summarised narratively; and 5 studies contributed data to both meta-analyses and narrative summaries.
Fig. 1.
PRISMA study flow diagram of studies published from 2006 to 2017.
3.2. Characteristics of included studies
The majority of the 38 studies were conducted in either Australia (14)(Stanley and Laugharne, 2013; Bartlem et al., 2015; Bartlem et al., 2014a; Happell et al., 2013a; Anderson et al., 2013; Ashton et al., 2010; Siru et al., 2010; Stanton et al., 2015; Stockings et al., 2015; Stockings et al., 2014; Tso et al., 2017; Wye et al., 2010; Wye et al., 2009; Wye et al., 2017) or the USA (11) (Price et al., 2007; Schacht et al., 2012; Chwastiak et al., 2013; Williams et al., 2015; Bolton et al., 2016; Himelhoch et al., 2014; Kilbourne et al., 2011; Leyro et al., 2013; Maki and Bjorklund, 2013; Prochaska et al., 2006; Sarna et al., 2009). Eight described client reported receipt of preventive care, (Bartlem et al., 2015; Etter et al., 2008; Siru et al., 2010; Stockings et al., 2015; Stockings et al., 2014; Leyro et al., 2013; Prochaska et al., 2006; Etter and Etter, 2007) 21 described clinician reported provision of care, (Bartlem et al., 2014a; Happell et al., 2013a; Price et al., 2007; Etter et al., 2008; Schacht et al., 2012; Zabeen et al., 2015; Anderson et al., 2013; Chwastiak et al., 2013; Williams et al., 2015; Ashton et al., 2010; Stanton et al., 2015; Wye et al., 2009; Bolton et al., 2016; Himelhoch et al., 2014; Sarna et al., 2009; Johnson et al., 2009; Haddad et al., 2016; Keizer et al., 2014; Ballbe et al., 2012; Guo et al., 2015; Robson et al., 2013a) and 12 described medical record audit data; (Stanley and Laugharne, 2013; Howard and Gamble, 2011; Williams et al., 2015; Tso et al., 2017; Wye et al., 2010; Wye et al., 2017; Kilbourne et al., 2011; Maki and Bjorklund, 2013; Prochaska et al., 2006; Corradi-Webster et al., 2009; Wu et al., 2013; Parker et al., 2012) where some studies utilised more than one method of data type. Eighteen studies reported data collected in psychiatric inpatient settings; (Howard and Gamble, 2011; Etter et al., 2008; Schacht et al., 2012; Zabeen et al., 2015; Siru et al., 2010; Stanton et al., 2015; Stockings et al., 2015; Stockings et al., 2014; Wye et al., 2010; Wye et al., 2009; Wye et al., 2017; Leyro et al., 2013; Prochaska et al., 2006; Sarna et al., 2009; Etter and Etter, 2007; Haddad et al., 2016; Keizer et al., 2014; Parker et al., 2012) 12 in outpatient settings; (Bartlem et al., 2015; Bartlem et al., 2014a; Price et al., 2007; Anderson et al., 2013; Chwastiak et al., 2013; Tso et al., 2017; Himelhoch et al., 2014; Maki and Bjorklund, 2013; Johnson et al., 2009; Corradi-Webster et al., 2009; Wu et al., 2013; Parker et al., 2012) and 10 in other or multiple mental health service types (Table 1) (Stanley and Laugharne, 2013; Happell et al., 2013a; Williams et al., 2015; Ashton et al., 2010; Bolton et al., 2016; Kilbourne et al., 2011; Ballbe et al., 2012; Guo et al., 2015; Robson et al., 2013a; Parker et al., 2012). Of the 20 studies that utilised client or audit data, 11 reported information on client psychiatric diagnosis; (Bartlem et al., 2015; Howard and Gamble, 2011; Williams et al., 2015; Siru et al., 2010; Stockings et al., 2015; Stockings et al., 2014; Tso et al., 2017; Wye et al., 2017; Leyro et al., 2013; Prochaska et al., 2006; Corradi-Webster et al., 2009) where mood and psychotic disorders were commonly reported (Appendix C). Of the 21 studies that examined clinician reported data, 20 reported clinician profession; (Bartlem et al., 2014a; Happell et al., 2013a; Price et al., 2007; Schacht et al., 2012; Zabeen et al., 2015; Anderson et al., 2013; Chwastiak et al., 2013; Williams et al., 2015; Ashton et al., 2010; Stanton et al., 2015; Wye et al., 2009; Bolton et al., 2016; Himelhoch et al., 2014; Sarna et al., 2009; Johnson et al., 2009; Haddad et al., 2016; Keizer et al., 2014; Ballbe et al., 2012; Guo et al., 2015; Robson et al., 2013a) with clinical/unit managers, and nursing staff frequently surveyed.
Table 1.
Included studies reporting the provision of preventive care in mental health services from 2006 to 2017.
| Author/year published/country | Year undertaken/setting/sample size (participation rate) | Data source | Chronic disease risk behaviours/preventive care elements* |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Smoking |
Alcohol |
Nutrition |
Physical activity |
|||||||||||||||
| As | Ad | At | Ar | As | Ad | At | Ar | As | Ad | At | Ar | As | Ad | At | Ar | |||
| Outpatient settings | ||||||||||||||||||
| Andersonb 2013 Australia |
2009 79 community mental health services 79 (94%) service managers |
Clinician report | ||||||||||||||||
| Bartlem (Bartlem et al., 2015) 2015 Australia |
2011–2012 12 community mental health services from one health district in NSW 558 (72%) clients |
Client report | ||||||||||||||||
| Bartlem (Bartlem et al., 2014a) 2014 Australia |
2010 All public community mental health services in one local health district in NSW 151 (89%) clinicians |
Clinician report | ||||||||||||||||
| Chwastiakb 2013 USA |
2011 1 community mental health centre 154 (71.6%) clinicians |
Clinician report | ||||||||||||||||
| Himelhock (Himelhoch et al., 2014) 2014 USA |
2011 9 community mental health settings 95 (100%) clinicians |
Clinician report | ||||||||||||||||
| Johnson (Johnson et al., 2009) 2009 Canada |
2006 8 community mental health teams and 14 contracted community agencies 282 (32–38%) clinicians |
Clinician report | ||||||||||||||||
| Price (Price et al., 2007) 2007 USA |
2005 78 community mental health centres with Ohio Department of Mental Health certification 80 (53%) psychiatrists |
Clinician report | ||||||||||||||||
| Corradi-Webster (Corradi-Webster et al., 2009) 2009 Brazil |
2000–2004 1 psychiatric outpatient clinic 127 records |
Medical record audit | ||||||||||||||||
| Makib 2013 USA |
nr 1 community mental health centre 129 records |
Medical record audit | ||||||||||||||||
| Tso (Tso et al., 2017) 2017 Australia |
2014–2015 Community mental health clinics at 2 public hospitals 251 records |
Medical record audit | ||||||||||||||||
| Wu (Wu et al., 2013) 2013 UK |
2008–2011 South London and Maudsley (SLaM) Case Register 5588 records |
Medical record audit | ||||||||||||||||
| Inpatient settings | ||||||||||||||||||
| Etterb 2008 Switzerland |
2003–2006 2 inpatient psychiatric units within a hospital 2006–77 (67.5%) patients |
Client report | ||||||||||||||||
| 2005–2006 2 inpatient psychiatric units within a hospital 2006–57 (91.9%) clinicians |
Clinician report | |||||||||||||||||
| Etterb 2007 Switzerland |
2003–2004 2 inpatient psychiatric units within a hospital 49 (86%) patients |
Client report | ||||||||||||||||
| Leyro (Leyro et al., 2013) 2013 USA |
2006–2010 2 psychiatric hospitals 324 (71% and 79% per hospital) patients |
Client report | ||||||||||||||||
| Prochaska (Prochaska et al., 2006) 2006 USA |
nr 1univeristy-based inpatient psychiatry unit 100 (87%) patients |
Client report | ||||||||||||||||
| 100 records | Medical record audit | |||||||||||||||||
| Siru (Siru et al., 2010) 2010 Australia |
2008 Department of Psychiatry in a major teaching hospital 64 (nr) patients |
Client report | ||||||||||||||||
| Stockings (Stockings et al., 2014) 2014 Australia |
2010–2011 3 psychiatric inpatient units in a large, regional public hospital 205 (69%) patients |
Client report | ||||||||||||||||
| Stockings (Stockings et al., 2015) 2015 Australia |
2009–2010 3 psychiatric inpatient units in a large, regional public hospital 181 (90.9%) patients |
Client report | ||||||||||||||||
| Haddad (Haddad et al., 2016) 2016 UK |
nr 1 low secure forensic psychiatric inpatient unit 57 (90.5%) clinicians |
Clinician report | ||||||||||||||||
| Keizer (Keizer et al., 2014) 2014 Switzerland |
2009 Department of Mental Health and Psychiatry in a large hospital 155 (72.4%) clinicians |
Clinician report | ||||||||||||||||
| Sarna (Sarna et al., 2009) 2009 USA |
nr Adult psychiatric inpatient settings in a Magnet-designated health care facility 100 (100%) nurses |
Clinician report | ||||||||||||||||
| Schacht (Schacht et al., 2012) 2012 USA |
2011 206 state inpatient psychiatric facilities 165 (80%) facility directors |
Clinician report | ||||||||||||||||
| Stanton (Stanton et al., 2015) 2015 Australia |
nr inpatient psychiatric facilities in a regional city in QLD 34 (nr) nurses |
Clinician report | ||||||||||||||||
| Wye (Wye et al., 2009) 2009 Australia |
2006 All publicly funded psychiatric inpatient units in NSW 123 (94%) nurse unit managers |
Clinician report | ||||||||||||||||
| Zabeenb 2015 UK |
2010 Random sample of inpatient psychiatric units across England 147 (67%) unit managers |
Clinician report | ||||||||||||||||
| Howard (Howard and Gamble, 2011) 2011 UK |
nr 2 acute wards from a large mental health trust 28 records |
Medical record audit | ||||||||||||||||
| Wye (Wye et al., 2010) 2010 Australia |
2005–2006 1 large adult psychiatric hospital 1000 (99%) records |
Medical record audit | ||||||||||||||||
| Wye (Wye et al., 2017) 2017 Australia |
2009–2010 2 general locked adult inpatient psychiatric facilities in one health district in NSW 1054 records |
Medical record audit | ||||||||||||||||
| Other settings | ||||||||||||||||||
| Ashton (Ashton et al., 2010) 2010 Australia |
2007 45 government and non-government mental health organisations in Adelaide, SA 324 (60%) team members |
Clinician report | ||||||||||||||||
| Ballbe (Ballbe et al., 2012) 2012 Spain |
2008–2009 186 Inpatient and outpatient mental health services in Catalonia 186 (96.9%) Clinical managers |
Clinician report | ||||||||||||||||
| Boltona 2016 USA |
2015 Members of the American Psychiatric Nurses Association 26 (nr) clinicians |
Clinician report | ||||||||||||||||
| Guo (Guo et al., 2015) 2015 Taiwan |
nr 2 community psychiatric hospitals providing inpatient and outpatient services 193 (96.9%) clinicians |
Clinician report | ||||||||||||||||
| Happella 2013 Australia |
2012 Members of the Australian College of Mental Health Nurses 559 (19.6%) mental health nurses |
Clinician report | ||||||||||||||||
| Robson (Robson et al., 2013a) 2013 UK |
2006–2007 Mental health nurses recruited from a large National Health Service Mental Health Trust in the UK 585 (52%) mental health nurses |
Clinician report | ||||||||||||||||
| Williams (Williams et al., 2015) 2015 USA |
2012 30 outpatient or partial-hospitalisation settings of state-wide behavioural health agency 18 (90%) clinicians |
Clinician report | ||||||||||||||||
| 100 records | Medical record audit | |||||||||||||||||
| Kilbourne (Kilbourne et al., 2011) 2011 USA |
2006–2007 VA Mental Health Programs with and without colocated general medical services 7514 (7.1%) records |
Medical record audit | ||||||||||||||||
| Parker (Parker et al., 2012) 2012 UK |
2010–2011 Adult mental health treatment services in the United Kingdom's largest Mental Health Trust 85 inpatient records 2028 community patient records |
Medical record audit | ||||||||||||||||
| Stanley (Stanley and Laugharne, 2013) 2013 Australia |
2011–2012 1 Fremantle adult psychiatric hospital with inpatient and outpatient services, 1 Kimberley rural mental health and drug service 56 Kimberley records 228 Fremantle records |
Medical record audit | ||||||||||||||||
Total  c c
|
23/41 | 22/41 | 25/41 | 12/41 | 7/41 | 3/41 | 1/41 | 2/41 | 4/41 | 8/41 | 0/41 | 2/41 | 4/41 | 9/41 | 0/41 | 4/41 | ||
*As- Ask/ Assess, Ad- Advise, At- Assist, Ar- Arrange.
 - Assessed.
- Assessed.
 - Not assessed.
- Not assessed.
nr = Not reported.
Data not reported in paper, analysed for review purposes.
Study reported incomplete outcome data where either the numerator or denominator of care provision/receipt was not reported and calculations were assumed.
Total number of data sources (Stanley and Laugharne, 2013) from 38 studies reporting on the provision of preventive care.
3.3. Provision of preventive care
Most (36) studies reported the receipt/provision of smoking cessation care, with fewer reporting the receipt/provision of care for: inadequate physical activity (10); inadequate nutrition (9); and harmful alcohol consumption (8; Table 1).
With regard to elements of care provision: the proportions of clients reporting being asked/clinicians reporting ‘asking’ about and/or ‘assessing’ extent of client risk behaviour was reported in 23 studies; ‘advising’ the modification of risk behaviours was reported in 25 studies; ‘assisting’ with behaviour change was reported in 22 studies; and ‘arranging’ referral or further behaviour change support was reported in 13 studies (Table 1).
3.4. Assessment of methodological quality
Most studies were of low methodological quality; 25/38 classified as high risk of bias. Most studies adequately described the subjects and setting, and had adequate response rates. Just two studies utilised appropriate statistical analysis, and no studies utilised a valid measurement of care provision; nor did data analysis provide sufficient coverage of subgroups-that is, coverage bias resulting from differing response rates among subgroups (where applicable; Appendix D).
3.5. Meta-analysis of prevalence of preventive care provision
Due to space constraints, meta-analysis results presented below reflect the highest estimations of care provision across clinician, client and audit reported data. Refer to Table 2 for results of the lowest estimations, and Appendix E for all Forest plots.
Table 2.
Summary of effects of all meta-analyses of included studies published from 2006 to 2017.
| Outcomea |
% (95% CI) | I2 (%) | p | n | n of studies |
|---|---|---|---|---|---|
| Meta-analysis results: | |||||
| Overall clinician reported data- highest estimates of care provision | |||||
| Ask/assess | |||||
| Smoking | 78 (59%–96%) | 97.7 | <0.01 | 515 | 4 |
| Advise | |||||
| Smoking | 46 (31%–61%) | 88.5 | <0.01 | 384 | 3 |
| Nutrition | 54 (48%–59%) | 0 | 0.78 | 305 | 2 |
| Physical activity | 72 (49%–95%) | 95.4 | <0.01 | 304 | 2 |
| Assist | |||||
| Smoking | 52 (31%–73%) | 94.2 | <0.01 | 339 | 4 |
| Arrange | |||||
| Smoking | 30 (1%–59%) | 95.6 | <0.01 | 211 | 2 |
| Overall clinician reported data- lowest estimates of care provision | |||||
| Ask/Assess | |||||
| Smoking | 78 (59%–96%) | 97.7 | <0.01 | 515 | 4 |
| Advise | |||||
| Smoking | 43 (32%–54%) | 78.5 | <0.01 | 384 | 3 |
| Nutrition | 54 (48%–59%) | 0 | 0.78 | 305 | 2 |
| Physical activity | 72 (49%–95%) | 95.4 | <0.01 | 304 | 2 |
| Assist | |||||
| Smoking | 39 (12%–67%) | 97.8 | <0.01 | 339 | 4 |
| Arrange | |||||
| Smokingb | 7 (0%–20%) | 90.0 | <0.01 | 229 | 2 |
| Overall client and audit reported data- highest estimates of care provision | |||||
| Ask/assess | |||||
| Smoking | 54 (38%–71%) | 99.7 | <0.01 | 10,574 | 12 |
| Alcohol | 62 (42%–81%) | 99.0 | <0.01 | 3240 | 6 |
| Nutritionb | 17 (0%–35%) | 98.6 | <0.01 | 813 | 3 |
| Physical activityb | 35 (0%–72%) | 99.6 | <0.01 | 641 | 3 |
| Advise | |||||
| Smoking | 28 (14%–42%) | 98.4 | <0.01 | 1880 | 10 |
| Alcoholb | 42 (0%–100%) | 98.8 | <0.01 | 228 | 2 |
| Nutrition | 47 (5%–90%) | 95.6 | <0.01 | 152 | 2 |
| Physical activityb | 46 (0%–100%) | 99.5 | <0.01 | 190 | 2 |
| Assist | |||||
| Smoking | 37 (13%–61%) | 99.7 | <0.01 | 3141 | 8 |
| Arrange | |||||
| Smokingb | 21 (0%–49%) | 98.9 | <0.01 | 388 | 3 |
| Physical activity | 35 (10%–59%) | 87.8 | <0.01 | 190 | 2 |
| Overall client and audit reported data- lowest estimates of care provision | |||||
| Ask/Assess | |||||
| Smoking | 41 (22%–61%) | 99.6 | <0.01 | 10,574 | 12 |
| Alcohol | 62 (42%–81%) | 99.0 | <0.01 | 3240 | 6 |
| Nutritionb | 17 (0%–35%) | 98.6 | <0.01 | 813 | 3 |
| Physical activityb | 35 (0%–72%) | 99.6 | <0.01 | 641 | 3 |
| Advise | |||||
| Smoking | 25 (10%–40%) | 99.2 | <0.01 | 1880 | 10 |
| Alcoholb | 42 (0%–100%) | 98.8 | <0.01 | 228 | 2 |
| Nutrition | 47 (5%–90%) | 95.6 | <0.01 | 152 | 2 |
| Physical activityb | 46 (0%–100%) | 99.5 | <0.01 | 190 | 2 |
| Assist | |||||
| Smoking | 31 (7%–56%) | 99.8 | <0.01 | 3141 | 8 |
| Arrange | |||||
| Smokingb | 3 (0%–7%) | 85.5 | <0.01 | 388 | 3 |
| Physical activityb | 10 (0%–29%) | 84.0 | 0.01 | 190 | 2 |
Meta-analyses were not possible for all health behaviours by all care elements due to insufficient numbers of studies (n < 2) contributing data.
In some cases approximate confidence intervals for the proportion gave limits outside 0 and 1. These cases have been truncated to 0 or 1 as appropriate.
Ask/Assess: Client and audit reported care data were available for meta-analysis for all four behaviours, however clinician reported data were only available for smoking. According to the combined client and audit reported data, assessment was most likely to occur for alcohol use (62%, 95% CI: 42%–81%; I2 99%; participants = 3240; studies = 6), followed by smoking (54%, 95% CI: 38%–71%; I2 99.7%; participants = 10,574; studies = 12; Fig. 2), physical activity (35%, 95% CI: −1%-72%; I2 99.6%; participants = 641; studies = 3), and nutrition (17%, 95% CI: 1%–35%; I2 98.6%; participants = 813; studies = 3). Assessment of smoking via clinician report was somewhat higher (78%, 95% CI: 59%–96%; I2 97.7%; participants = 515; studies = 4). Heterogeneity in pooled estimates was substantial (I2 > 50%; Appendices E, F).
Fig. 2.
Forest plots of the overall client and audit reported highest estimates of smoking cessation care provision by care element: a) ask/assess, b) advise, c) assist, and d) arrange.
Note: Error-bars represent 95% confidence intervals; included studies published from 2006 to 2017. At times, 95% confidence intervals exceed the boundaries of the proportion (between 0 and 1), as the random effects binomial proportion interval (Wald interval) assumes a normal distribution.
Advise: Client and audit reported data for “advice” were available for meta-analyses for all behaviours, and clinician reported data for all behaviours except alcohol. The receipt of client and audit reported advice to change at risk behaviours was similar for nutrition (47%, 95% CI: 5%–90%; I2 95.6%; participants = 152; studies = 2), physical activity (46%, 95% CI: −30%-123%; I2 99.5%; participants = 190; studies = 2), and alcohol (42%, 95% CI: −19%-102%; I2 98.8%; participants = 228; studies = 2), yet lower for smoking (28%, 95% CI: 14%–42%; I2 98.4%; participants = 1880; studies = 10; Fig. 2). Similar proportions of advice were provided via clinician report for smoking (46%, 95% CI: 31%–61%; I2 88.5%; participants = 384; studies = 3) and nutrition (54%, 95% CI: 48%–59%; I2 0%; participants = 305; studies = 2), with advice for physical activity somewhat higher (72%, 95% CI: 49%–95%; I2 95.4%; participants = 211; studies = 2). Heterogeneity was substantial, with the exception of clinician reported nutrition advice; however this value is a probable underestimation of heterogeneity due to the small number of data points (Appendices E, F) (von Hippel, 2015).
Assist: Meta-analyses were conducted for clinician and client/audit reported data and were possible for the provision of assistance for smoking only. The pooled prevalence of clinician reported provision of assistance for smoking was 52% (95% CI: 31%–73%; I2 94.2%; participants = 339; studies = 4), whilst client and audit reported receipt was 37% (95% CI 13%–61%; I2 99.7%; participants = 3141; studies = 8; Fig. 2). Heterogeneity was substantial (Appendices E, F).
Arrange: Client and audit reported data enabled meta-analysis for smoking and physical activity outcomes, whilst clinician reported data were available for meta-analysis of smoking only. The pooled prevalence of clinician reported arrangement of smoking cessation care was 30% (95% CI: 1%–59%; I2 95.6%; participants = 211; studies = 2), whilst the client and audit reported receipt was 21% (95% CI: −7%-49%; I2 98.9%; participants = 388; studies = 3; Fig. 2). Client and audit reported receipt of care arranged for physical activity was 35% (95% CI: 10%–59%; I2 87.8%; participants = 190; studies = 2). Heterogeneity was substantial (Appendices E, F).
3.6. Assessment of confidence in cumulative evidence
GRADE ratings for outcome measures were initially classified as ‘low’ as the included data were observational (Guyatt et al., 2008b). The quality of evidence (GRADE) in all meta-analyses for all elements of care provision, across all four risk behaviours, was downgraded to ‘very low’ due to risk of bias, and/or inconsistency, and/or imprecision of results (Appendix F) (Ryan and Hill, n.d.).
3.7. Narrative synthesis
Seventeen studies reported data not conducive to meta-analysis. Thirteen of these studies reported data using categorical responses describing the frequency of clinician care provision (for example, ‘always’) (Happell et al., 2013a; Williams et al., 2015; Ashton et al., 2010; Stanton et al., 2015; Wye et al., 2009; Bolton et al., 2016; Himelhoch et al., 2014; Sarna et al., 2009; Johnson et al., 2009; Haddad et al., 2016; Keizer et al., 2014; Ballbe et al., 2012; Robson et al., 2013a). Two of the 17 studies, one utilising client reported data and one clinician report, were not included in the meta-analyses as no other studies reported data points for the same risk behaviour and care element (Bartlem et al., 2015; Bartlem et al., 2014a). Five of the 17 studies, also utilised categorical responses, reporting preventive care outcomes in mean scores rather than proportions: for smoking: ask/assess; (Price et al., 2007; Ashton et al., 2010) advise; (Price et al., 2007) assist; (Happell et al., 2013a; Price et al., 2007; Bolton et al., 2016; Guo et al., 2015) and arrange; (Price et al., 2007) and advice for nutrition and physical activity; (Bolton et al., 2016) and assistance for alcohol, nutrition, and physical activity (Appendix C) (Happell et al., 2013a).
Ask/Assess: The proportions of clinicians reporting ‘often’ or ‘always’ providing assessment care for smoking was 26.1–100% (Williams et al., 2015; Ashton et al., 2010; Himelhoch et al., 2014; Sarna et al., 2009; Johnson et al., 2009; Ballbe et al., 2012). Proportions of clinicians reporting providing 80–100% of clients with assessment was greatest for alcohol (89.4%), followed by physical activity (59.6%), and nutrition (13.2%) (Bartlem et al., 2014a).
Advise: The highest proportions of clinicians reporting ‘often’ or ‘always’ providing advice were found for nutrition (61–100%)(Happell et al., 2013a; Bolton et al., 2016; Haddad et al., 2016; Robson et al., 2013a) and physical activity (53–100%), (Happell et al., 2013a; Stanton et al., 2015; Bolton et al., 2016; Haddad et al., 2016; Robson et al., 2013a) with a more variable range for smoking (16–100%) (Williams et al., 2015; Wye et al., 2009; Himelhoch et al., 2014; Sarna et al., 2009; Johnson et al., 2009). Additionally, 80.1% of clinicians were reported to provide advice to reduce alcohol consumption to 80–100% of clients (Bartlem et al., 2014a).
Assist: Between 5 and 92.9% of clinicians reported ‘often’ or ‘always’ providing clients with assistance for smoking, (Happell et al., 2013a; Williams et al., 2015; Wye et al., 2009; Bolton et al., 2016; Himelhoch et al., 2014; Sarna et al., 2009; Johnson et al., 2009; Haddad et al., 2016; Ballbe et al., 2012; Robson et al., 2013a) and 86.2% reported ‘often’ or ‘always’ providing assistance for alcohol consumption (Happell et al., 2013a). No studies reported on assistance for nutrition or physical activity.
Arrange: Between 8 and 94% of clinicians reported ‘often’ or ‘always’ arranging care for smoking for clients (Williams et al., 2015; Wye et al., 2009; Himelhoch et al., 2014; Sarna et al., 2009; Ballbe et al., 2012). Higher proportions of clinicians reported arranging care for 80–100% of clients for alcohol consumption (60.9%), compared to physical activity (40.1%) and nutrition (22.5%) (Bartlem et al., 2014a). Additionally, 38% of clients reported receiving care for alcohol, and 43% reported receiving care for nutrition (Appendix C) (Bartlem et al., 2015).
3.8. Subgroup and sensitivity analyses
Service type: Pre-specified subgroup analyses were conducted by mental health service type: inpatient; outpatient; and other/multiple settings (Appendix E, F). With respect to subgroup analyses of clinician reported data, provision of care did not differ significantly in inpatient or outpatient settings relative to the overall pooled estimate.
Subgroup analyses of client and audit reported data of care provision by setting revealed non-significant trends of variability in pooled prevalence estimates between settings. Client and audit reported care for smoking ask/assessment was lower in inpatient settings (31%), and higher in outpatient (70%) and other settings (68%) relative to the overall pooled estimate (54%). Ask/assessment of alcohol consumption was lower in outpatient settings (49%) and higher in other settings (83%) compared to the pooled estimate (62%). Additionally, receipt for smoking cessation assistance was lower in other settings (23%) and higher in inpatient settings (45%) relative to the overall polled estimate (37%; Appendix F).
Heterogeneity remained substantial for all individual subgroup analyses with the exception of: clinician reported provision of nutrition advice in outpatient settings (I2 0%); and client receipt of alcohol ask/assessment in other settings (I2 0%; Appendix F), however these values are likely an underestimation of heterogeneity due to small number of data points (von Hippel, 2015). To explore substantial heterogeneity, a further post-hoc subgroup analysis of client and audit data separately by setting type was conducted, however heterogeneity remained substantial with the exception of audit data of smoking advice in inpatient settings (I2 0%; Appendix F).
Post-hoc subgroup analyses were conducted by country, where possible (Australia only for clinician reported data; and Australia, UK, and US for client and audit data). With respect to Australian clinician reported data, no significant differences were found compared to the overall meta-analyses. Moreover, subgroup analyses using client and audit reported data yielded no significant differences between the countries or the overall estimates (Appendix F).
Sensitivity analyses: Pre-specified sensitivity analyses were conducted to exclude studies at high risk of bias. All studies reporting clinician data were assessed at high risk of bias; therefore analysis was not possible. Sensitivity analyses of client and audit reported care excluding studies at high risk of bias revealed a similar pooled prevalence to all possible comparisons (within 6%) with the overall meta-analyses results (Appendix F).
Post-hoc sensitivity analyses were conducted to exclude any data calculated by the authors for the purpose of the review. This eliminated all clinician reported analyses bar one, where clinician reported ask/assess of smoking was similar to overall care provision estimates; as were all client and audit reported sensitivity analyses excluding calculated data (Appendix F).
Finally, sensitivity analyses utilising only exact proportions of clinician reported care provision estimates yielded just one analysis, where the pooled prevalence of provision of assistance for smoking did not differ from the overall estimate (Appendix F).
4. Discussion
This is the first review to comprehensively synthesise the international evidence on the provision of preventive care by mental health services for four modifiable chronic disease risk behaviours by individual preventive care elements and by service type. Meta-analysis revealed sub-optimal levels of care provision (defined as <80% of clients in receipt of care in previous research)(Bartlem et al., 2014b; McElwaine et al., 2014; Freund et al., 2005) across clinician and client/audit reported data for each of the four risk behaviours and all analysed care elements. Relatively few of the included studies examined the provision of care for behaviours other than smoking and across all care elements. Estimations of care provision by care element varied across risk behaviours revealing no clear patterns. Similarly, subgroup analyses did not reveal any consistent trends across settings or country, likely due to the small number of studies available. Further research is needed to explore the extent to which different mental health settings provide preventive care for harmful alcohol consumption, inadequate nutrition, and inadequate physical activity.
One of the key findings of the review was the wide variation in how care was measured across the included studies; hampering comparisons across studies. Moreover, the creation of the pooled clinician measure lacked specificity whereby estimates of care could only be calculated for ‘at least 50% of clients’. Despite these constraints, pooled estimates of care provision suggest between one-third and three-quarters (36–78%) of clinicians are providing at least 50% of clients with preventive care for the behaviours and care elements analysed. Whilst these findings suggest overall sub-optimal levels of care provision, many clinicians are currently providing care to at least 50% of clients suggesting an attempt to incorporate preventive care into service practice where clinicians are aware of the requirement (NSW Department of Health, 2017a; NSW Department of Health, 2017b; NSW Mental Health Commission, 2014; National Preventive Health Taskforce, 2008; Agency for Healthcare Research and Quality, 2010; National Institute for Health and Care Excellence, 2010; National Institute for Health and Care Excellence, 2013; US Department of Health and Human Services, 2009). However, less than a third of studies reported any details on any policies or procedures operational within the settings studied regarding the requirements of preventive care provision (Stanley and Laugharne, 2013; Bartlem et al., 2015; Bartlem et al., 2014a; Stockings et al., 2015; Stockings et al., 2014; Wye et al., 2010; Leyro et al., 2013; Etter and Etter, 2007; Keizer et al., 2014; Parker et al., 2012).
Another key finding of the review was the dearth of previous research assessing the extent to which care is provided for behaviours other than smoking in mental health services. No included studies reported on the provision of assistance for improving nutrition or physical activity by clinician nor client, nor audit reported data. Similarly no studies reported provision of assistance for alcohol consumption by client or audit report, and only one study (in the narrative synthesis report)(Happell et al., 2013a) reported on the provision of assistance for alcohol consumption by clinician reported data. As such, the current provision of care in the form of assistance to address nutrition, physical activity, and alcohol consumption is largely unknown and requires further investigation in subsequent research.
The findings of this review confirm sub-optimal reports of the provision of preventive care reported in individual identified studies and the previous narrative review of smoking cessation care provision in inpatient settings; (Wye et al., 2011) suggesting a need for further research to address barriers to the provision of preventive care. Previous research conducted in mental health settings has identified multiple barriers to the provision preventive care at the clinician and service level (Price et al., 2007; Anderson et al., 2013; Chwastiak et al., 2013; Ashton et al., 2010; Johnson et al., 2009; Johnson and Fry, 2013; Robson et al., 2013b; Happell et al., 2012b; Hyland et al., 2003; Organ et al., 2010; Happell et al., 2013b; Dunbar et al., 2010; Nash, 2005). To address such barriers, various strategies have been tested and demonstrated to reduce clinician burden in providing preventive care and increase the provision of care such as: reduction of the ‘5As’ model to ‘2As and R’; (Schroeder, 2005; Revell and Schroeder, 2005) incorporation of tools such as prompts, recording and arrange/referral protocols; (Shojania et al., 2009; Wolfenden et al., 2009; Krist et al., 2008) and training in the provision of care and referral options (Sheffer et al., 2012). Alternatively, the institution of a specialist preventive care provider embedded in mental health services, relieving mental health clinicians of the role of preventive care provision, has been trialled through limited research and found to increase care provision (Osborn et al., 2010; McKenna et al., 2014; Cunningham et al., 2013). Further research could focus on the design of practice change interventions to address identified barriers and increase the provision of care across mental health services. Additionally, the review investigated care provision for the four leading modifiable chronic disease risk behaviours. Future research could examine the provision of care by mental health services for other modifiable risk behaviours, such as sleep; more recently recognised as a risk factor for chronic disease (von Ruesten et al., 2012; Liu et al., 2013).
4.1. Study limitations and strengths
This is the first review to comprehensively synthesise the international published evidence on the provision of preventive care by mental health services for four health risk behaviours by individual preventive care elements and by service type.
The review is limited by the variability and heterogeneity of included individual studies. Substantial heterogeneity remained throughout the majority of meta-analyses and subgroup analyses, contributing to the very low quality assessment of the cumulative evidence. As included studies were observational to reflect real-world practice and not conducted under strict controlled conditions, some heterogeneity is to be expected. Such heterogeneity might be explained by between-study differences in methodology including measurements and definitions of care elements used to assess care provision, or by population characteristics such as country; clinician qualification/profession; or psychiatric diagnosis of clients (Hippokratia, 2010; Glasziou and Sanders, 2002). Heterogeneity may also result from true differences in provision of care impacted by unknown characteristics, such as whether or not the settings studied operated under specific preventive care policies; as changes in smoke-free policies have resulted in changes in smoking cessation care provision (Etter et al., 2008). As mentioned above, limited studies provided information on whether or not a service operated under specific preventive care policies, and few studies that mentioned active policies or procedures provided any description of such procedures (Stanley and Laugharne, 2013; Bartlem et al., 2015; Bartlem et al., 2014a; Stockings et al., 2015; Stockings et al., 2014; Keizer et al., 2014). Future research on preventive care provision in mental health settings could seek to utilise uniformed measurements of preventive care provision and elucidate the preventive care policy and procedural contexts in which services operate.
Review findings should be considered with caution due to the very low quality of cumulative evidence, suggesting future studies are likely to change the estimates; and in light of the following limitations. The majority of studies were categorised as high risk of bias. Data relied on self-report measures and medical record audit; where clinician self-report may over-estimate care provision, whilst audit data may reflect an underestimation of care provision; (Hrisos et al., 2009) suggesting client reported data may be a useful additional measure in future research where feasible (Hrisos et al., 2009). However, client report may also be susceptible to recall bias (Hrisos et al., 2009). Future research could seek to compare the accuracy of such measures in the context of preventive care in mental health services.
The variability in assessment and reporting of outcome measures by included studies limited comparability and resulted in many meta-analysis outcomes being based on a limited number of studies. Clinician reported data could not be pooled to create an estimate of care provision to all clients, rather the more conservative estimate of care provision to at least 50% of clients was analysed. Finally, heterogeneity remained substantial despite subgroup and sensitivity analyses suggesting between-study differences that could not be explored due to inconsistencies or insufficient reporting of study measures and characteristics.
5. Conclusion
This review found suboptimal provision of preventive care for tobacco smoking, harmful alcohol consumption, inadequate nutrition, and inadequate physical activity in mental health settings across all analysed care elements. These findings are important to mental health service clinicians and managers as they suggest current preventive care is suboptimal across risk behaviours and service types; suggesting a need to improve the quality of interventions to increase the provision of preventive care. Utilisation of consistent care provision and reporting measures across all mental health services, relating to care provided to individual clients, would facilitate further synthesis of the prevalence of care provision. Future studies need to investigate methods to increase clinician delivery of preventive care in mental health services, which have an organisational culture and service issues that pose idiosyncratic challenges to the field of implementation science (Sandstrom et al., 2015; Michie et al., 2007).
Systematic review protocol and registration
Systematic review of the prevalence of preventive care provision for chronic disease risk behaviours in mental health services. PROSPERO 2016:CRD42016049889 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=49889
Acknowledgments
Acknowledgements
The authors would like to acknowledge the assistance of Ms. Debbie Booth in the development and execution of search strategies, Ms. Joanna Latter's assistance with screening full texts for eligibility, and Mr. Paul Rippon's assistance in the organisation of data for meta-analysis, conduct and interpretation of meta-analyses. The authors would also like to thank the authors of included studies who provided additional clarifications and/or data for the purposes of the review. Forest plots for additional subgroup analyses and sensitivity analyses, not presented in Appendix E, are available upon request from the corresponding author.
Funding
The project received funding from the University of Newcastle Australia Priority Research Centre for Health Behaviour. The funding source had no role in study design, data collection and analysis, interpretation of the results, writing the report or the decision to submit the paper for publication. Ms. Jacqueline Bailey receives financial support through an Australian Government Research Training Program Scholarship. Drs Kate Bartlem and Emily Stockings are funded by National Health and Medical Research Council Early Career Fellowships (#1142272; #1104600). No other financial disclosures were reported by the authors of this paper.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2019.100969.
Appendix A. Supplementary data
Supplementary material
References
- Agency for Healthcare Research and Quality . 2010. Guide to Clinical Preventive Services 2010–2011. (AHRQ Publication No. 10–05145). Rockville, MD. [PubMed] [Google Scholar]
- Anderson A.E., Bowman J.A., Knight J. Smoking cessation care provision and support procedures in Australian community mental health centers. Psychiatr. Serv. 2013;64(7):707–710. doi: 10.1176/appi.ps.201200213. [DOI] [PubMed] [Google Scholar]
- Anon . Clarivate Analytics; Philadelphia: 2016. EndNote X8 [Computer Program] [Google Scholar]
- Anon Covidence systematic review software [Computer Program]. Melbourne, Australia: Veritas Health Innovation.
- Ashton M., Lawn S., Hosking J.R. Mental health workers' views on addressing tobacco use. Australian & New Zealand Journal of Psychiatry. 2010;44(9):846–851. doi: 10.3109/00048674.2010.488637. [DOI] [PubMed] [Google Scholar]
- Australian Health Ministers' Advisory Council . Australian Government; Canberra: 2017. National Strategic Framework for Chronic Conditions. [Google Scholar]
- Australian Institute of Health and Welfare . AIHW; Canberra: 2012. Risk Factors Contributing to Chronic Disease. Cat No. PHE157. [Google Scholar]
- Ballbe M., Nieva G., Mondon S. Smoke-free policies in psychiatric services: identification of unmet needs. Tob. Control. 2012;21(6):549–554. doi: 10.1136/tobaccocontrol-2011-050029. [DOI] [PubMed] [Google Scholar]
- Bartlem K.M., Bowman J.A., Freund M. Care provision to prevent chronic disease by community mental health clinicians. Am. J. Prev. Med. 2014;47(6):762–770. doi: 10.1016/j.amepre.2014.08.003. [DOI] [PubMed] [Google Scholar]
- Bartlem K., Bowman J., Freund M. Care provision to prevent chronic disease by community mental health clinicians. Am. J. Prev. Med. 2014;47(6):762–770. doi: 10.1016/j.amepre.2014.08.003. [DOI] [PubMed] [Google Scholar]
- Bartlem K., Bowman J., Freund M. Acceptability and receipt of preventive care for chronic-disease health risk behaviors reported by clients of community mental health services. Psychiatr. Serv. 2015;66(8):857–864. doi: 10.1176/appi.ps.201400360. [DOI] [PubMed] [Google Scholar]
- Bolton P.S., Knight M., Kopeski L.M. Metabolic syndrome. J. Psychosoc. Nurs. Ment. Health Serv. 2016;54(11):44–53. doi: 10.3928/02793695-20161026-01. [DOI] [PubMed] [Google Scholar]
- Borenstien M., Hedges L.V., Higgins J.P.T., Rothstein H.R. John Wiley & Sons, Ltd.; West Sussex, UK: 2009. Introduction to Meta-Analysis. [Google Scholar]
- Brown S., Kim M., Mitchell C., Inskip H. Twenty-five year mortality of a community cohort with schizophrenia. Br. J. Psychiatry J. Ment. Sci. 2010;196(2):116–121. doi: 10.1192/bjp.bp.109.067512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner E., Rees K., Ward K., Burke M., Thorogood M. Cochrane Database of Systematic Reviews. 2007. Dietary advice for reducing cardiovascular risk. Issue 4. CD002128; [DOI] [PubMed] [Google Scholar]
- Butt P., Berirness D., Gliksman L., Paradis C., Stockwell T. Ottawa; Canadian Centre on Substance Abuse: 2011. Alcohol and Health in Canada: A Summary of Evidence and Guidelines for Low Risk Drinking. [Google Scholar]
- Cabassa L.J., Ezell J.M., Lewis-Fernandez R. Lifestyle interventions for adults with serious mental illness: a systematic literature review. Psychiatr. Serv. 2010;61(8):774–782. doi: 10.1176/appi.ps.61.8.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan R.C., Veldhuizen S., Jeysingh T. Patterns of tobacco-related mortality among individuals diagnosed with schizophrenia, bipolar disorder, or depression. J. Psychiatr. Res. 2014;48(1):102–110. doi: 10.1016/j.jpsychires.2013.09.014. [DOI] [PubMed] [Google Scholar]
- Canadian Society for Exercise Physiology . Canadian Society for Exercise Physiology; Ottawa: 2011. Canadian Physical Activity Guidelines: For Adults 18–64 Years. [Google Scholar]
- Centers for Disease Control and Prevention . Centres for Disease Control and Prevention; Atlanta: 2014. Best Practices for Comprehensive Tobacco Control Programs - 2014 : U.S. Department of Health and Human Services CfDCaP, ed. [Google Scholar]
- Centers for Disease Control and Prevention. (n.d.) Alcohol Use and your Health Factsheet. In. (CDC2018).
- Chang C.K., Hayes R.D., Perera G. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One. 2011;6(5) doi: 10.1371/journal.pone.0019590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chwastiak L., Cruza-Guet M.C., Carroll-Scott A., Sernyak M., Ickovics J. Preventive counseling for chronic disease: missed opportunities in a community mental health center. Psychosomatics. 2013;54(4):328–335. doi: 10.1016/j.psym.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corradi-Webster C.M., Laprega M.R., Furtado E.F. Do psychiatry residents document outpatients' alcohol problems? Revista de Psiquiatria do Rio Grande do Sul. 2009;31(3):187–191. [Google Scholar]
- Cunningham C., Peters K., Mannix J. Physical health inequities in people with severe mental illness: identifying initiatives for practice change. Issues in mental health nursing. 2013;34(12):855–862. doi: 10.3109/01612840.2013.832826. [DOI] [PubMed] [Google Scholar]
- Deeks J.J., Higgins J.P.T., Altman D.G., on behalf of the Cochrane Statistical Methods Group . Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins J.P.T., Churchill R., Chandler J., Cumpston M.S., editors. Cochrane handbook for systematic reviews of interventions. Version 5.2.0 [updated June 2017]. The Cochrane Collaboration. 2017. [Google Scholar]
- Department of Health . Commonwealth of Australia; Canberra: 2014. Make your Move-Sit Less Be Active for Life! [Google Scholar]
- Department of Health . Department of Health; London: 2016. UK Chief Medical Officers' Low Risk Drinking Guidelines. [Google Scholar]
- Department of Health and Social Care . Department of Health and Social Care; London: 2018. Tobacco Control Plan: Delivery Plan: 2017–2022. [Google Scholar]
- Department of Health N . In: Physical Health Care within Mental Health Services. Office MHaDaA, editor. NSW Health; Sydney: 2009. [Google Scholar]
- Dickens G.L., Ion R., Waters C., Atlantis E., Everett B. Mental health nurses' attitudes, experience, and knowledge regarding routine physical healthcare: systematic, integrative review of studies involving 7,549 nurses working in mental health settings. BMC Nurs. 2019;18(16) doi: 10.1186/s12912-019-0339-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar L., Brandt T., Wheeler A., Harrison J. Barriers and solutions to implementing metabolic risk assessment in a secondary mental health service. Australasian Psychiatry. 2010;18(4):322–325. doi: 10.3109/10398561003692571. [DOI] [PubMed] [Google Scholar]
- Erlangsen A., Andersen P.K., Toender A., Laursen T.M., Nordentoft M., Canudas-Romo V. Cause-specific life-years lost in people with mental disorders: a nationwide, register-based cohort study. Lancet Psychiatry. 2017;4(12):937–945. doi: 10.1016/S2215-0366(17)30429-7. [DOI] [PubMed] [Google Scholar]
- Etter M., Etter J.F. Acceptability and impact of a partial smoking ban in a psychiatric hospital. Prev. Med. 2007;44(1):64–69. doi: 10.1016/j.ypmed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Etter M., Khan A.N., Etter J.F. Acceptability and impact of a partial smoking ban followed by a total smoking ban in a psychiatric hospital. Prev. Med. 2008;46(6):572–578. doi: 10.1016/j.ypmed.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Fiore M.C., Jaen C.R., Baker T.B. US Department of Health and Human Services. Public Health Service; Rockville, MD: 2008. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guidelines. [Google Scholar]
- Foster C., Hillsdon M., Thorogood M. Cochrane Reviews. 2005. Interventions for promoting physical activity. Issue 1. CD003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freund M., Campbell E., Paul C., Sakrouge R., Wiggers J. Smoking care provision in smoke-free hospitals in Australia. Prev. Med. 2005;41:151–158. doi: 10.1016/j.ypmed.2004.09.044. [DOI] [PubMed] [Google Scholar]
- Freund M., Campbell E., Paul C. Smoking care provision in hospitals: a review of prevalence. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2008;10(5):757–774. doi: 10.1080/14622200802027131. [DOI] [PubMed] [Google Scholar]
- Glasgow R.E., Goldstein M.G., Ockene J.K., Pronk N.P. Translating what we have learned into practice. Principles and hypotheses for interventions addressing multiple behaviors in primary care. Am. J. Prev. Med. 2004;27(2 Suppl):88–101. doi: 10.1016/j.amepre.2004.04.019. [DOI] [PubMed] [Google Scholar]
- Glasziou P.P., Sanders S.L. Investigating causes of heterogeneity in systematic reviews. Stat. Med. 2002;21:1503–1511. doi: 10.1002/sim.1183. [DOI] [PubMed] [Google Scholar]
- GRADE Working Group Grading quality of evidence and strength of recommendations. Bmj. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo S.-E., Wang A.-L., Shu B.-C. Self-efficacy in providing smoking-cessation services among psychiatric nurses in central and southern Taiwan: an exploratory study. Int. J. Ment. Health Nurs. 2015;24(2):158–168. doi: 10.1111/inm.12119. [DOI] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Vist G.E. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Schunemann H.J. GRADE: what is "quality of evidence" and why is it important to clinicians? Bmj. 2008;336:995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad M., Llewellyn-Jones S., Yarnold S., Simpson A. Improving the physical health of people with severe mental illness in a low secure forensic unit: an uncontrolled evaluation study of staff training and physical health care plans. Int. J. Ment. Health Nurs. 2016;25(6):554–565. doi: 10.1111/inm.12246. [DOI] [PubMed] [Google Scholar]
- Happell B., Davies C., Scott D. Health behaviour interventions to improve physical health in individuals diagnosed with a mental illness: a systematic review. Int. J. Ment. Health Nurs. 2012;21(3):236–247. doi: 10.1111/j.1447-0349.2012.00816.x. [DOI] [PubMed] [Google Scholar]
- Happell B., Scott D., Platania-Phung C., Nankivell J. Should we or shouldn't we? Mental health nurses' views on physical health care of mental health consumers. Int. J. Ment. Health Nurs. 2012;21(3):202–210. doi: 10.1111/j.1447-0349.2011.00799.x. [DOI] [PubMed] [Google Scholar]
- Happell B., Platania-Phung C., Scott D. Are nurses in mental health services providing physical health care for people with serious mental illness? An Australian perspective. Issues in mental health nursing. 2013;34(3):198–207. doi: 10.3109/01612840.2012.733907. [DOI] [PubMed] [Google Scholar]
- Happell B., Scott D., Nankivell J., Platania-Phung C. Screening physical health? Yes! But...: nurses' views on physical health screening in mental health care. J. Clin. Nurs. 2013;22(15–16):2286–2297. doi: 10.1111/j.1365-2702.2012.04325.x. [DOI] [PubMed] [Google Scholar]
- Health Canada . Ottawa; Health Canada: 2018. Canada's Tobacco Strategy. [Google Scholar]
- Health Canada . Ottawa; Health Canada: 2019. Canada's Dietary Guidelines. [Google Scholar]
- Hensrud D. Clinical preventive medicine in primary care: background and practice: 1. Rationale and current preventive practices. Mayo Clin. Proc. 2000;75(2):165–172. doi: 10.4065/75.2.165. [DOI] [PubMed] [Google Scholar]
- Her Majesty's Government . In: Factsheet 4: Physical Activity Guidelines for Adults 19–64 Years. Health Do, editor. Her Majesty's Government; London: 2011. [Google Scholar]
- Hillsdon M., Foster C., Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst. Rev. 2005;1 doi: 10.1002/14651858.CD003180.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelhoch S., Riddle J., Goldman H.H. Barriers to implementing evidence-based smoking cessation practices in nine community mental health sites. Psychiatr. Serv. 2014;65(1):75–80. doi: 10.1176/appi.ps.201200247. [DOI] [PubMed] [Google Scholar]
- Haidich AB. Meta-analysis in medical researchHippokratia. 2010;14(1):29–37. [PMC free article] [PubMed] [Google Scholar]
- Howard L., Gamble C. Supporting mental health nurses to address the physical health needs of people with serious mental illness in acute inpatient care settings. Journal of Psychiatric & Mental Health Nursing. 2011;18(2):105–112. doi: 10.1111/j.1365-2850.2010.01642.x. [DOI] [PubMed] [Google Scholar]
- Hrisos S., Eccles M.P., Francis J.J. Are there valid proxy measures of clinical behaviour? A systematic review. Implementation science : IS. 2009;4:37. doi: 10.1186/1748-5908-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulscher M, Wensing M, ven der Weijden T, Grol R. Interventions to implement prevention in primary care. Cochrane Database Syst. Rev.. 1997;1:CD000362. [DOI] [PubMed]
- Hyland B., Judd F., Davidson S., Jolley D., Hocking B. Case managers' attitudes to the physical health of their patients. Aust. N. Z. J. Psychiatry. 2003;37(6):710–714. doi: 10.1080/j.1440-1614.2003.01264.x. [DOI] [PubMed] [Google Scholar]
- Johnson K., Fry C. The attitudes and practices of community managed mental health service staff in addressing physical health: findings from a targeted online survey. Adv. Ment. Health. 2013;11(3):163–171. [Google Scholar]
- Johnson J.L., Malchy L.A., Ratner P.A. Community mental healthcare providers' attitudes and practices related to smoking cessation interventions for people living with severe mental illness. Patient Educ. Couns. 2009;77(2):289–295. doi: 10.1016/j.pec.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Keizer I., Gex-Fabry M., Bruegger A., Croquette P., Khan A.N. Staff representations and tobacco-related practices in a psychiatric hospital with an indoor smoking ban. Int. J. Ment. Health Nurs. 2014;23(2):171–182. doi: 10.1111/inm.12030. [DOI] [PubMed] [Google Scholar]
- Kilbourne A.M., Pirraglia P.A., Lai Z. Quality of general medical care among patients with serious mental illness: does colocation of services matter? Psychiatr. Serv. 2011;62(8):922–928. doi: 10.1176/ps.62.8.pss6208_0922. [DOI] [PubMed] [Google Scholar]
- Krist A., Woolf S., Frazier C. An electronic linkage system for health behavior counseling: effect on delivery of the 5A's. Am. J. Prev. Med. 2008;35(5S):S350–S358. doi: 10.1016/j.amepre.2008.08.010. [DOI] [PubMed] [Google Scholar]
- Laursen T.M., Wahlbeck K., Hallgren J. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS One. 2013;8(6) doi: 10.1371/journal.pone.0067133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D., Hancock K., Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. Bmj. 2013;346:f2539. doi: 10.1136/bmj.f2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro T.M., Hall S.M., Hickman N., Kim R., Hall S.E., Prochaska J.J. Clinical management of tobacco dependence in inpatient psychiatry: provider practices and patient utilization. Psychiatr. Serv. 2013;64(11):1161–1165. doi: 10.1176/appi.ps.201200574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Wheaton A.G., Chapman D.P., Croft J.B. Sleep duration and chronic diseases among U.S. adults age 45 years and older: evidence from the 2010 behavioral risk factor surveillance system. Sleep. 2013;36(10):1421–1427. doi: 10.5665/sleep.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki M., Bjorklund P. Improving cardiovascular disease screening in community mental health centers. Perspectives in Psychiatric Care. 2013;49(3):179–186. doi: 10.1111/j.1744-6163.2012.00348.x. [DOI] [PubMed] [Google Scholar]
- Markkula N., Harkanen T., Perala J. Motality in people with depressive, anxiety and alcohol use disorders in Finland. Br. J. Psychiatry. 2012;200(2):143–149. doi: 10.1192/bjp.bp.111.094904. [DOI] [PubMed] [Google Scholar]
- McElwaine K., Freund M., Campbell E. Clinician assessment, advice and referral for multiple health risk behaviors: prevalence and predictors of delivery by primary health care nurses and allied health professionals. Patient Educ. Couns. 2014;94(2):193–201. doi: 10.1016/j.pec.2013.10.017. [DOI] [PubMed] [Google Scholar]
- McKenna B., Furness T., Wallace E. The effectiveness of specialist roles in mental health metabolic monitoring: a retrospective cross-sectional comparison study. BMC psychiatry. 2014;14:234. doi: 10.1186/s12888-014-0234-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Pilling S., Garety P. Difficulties implementing a mental health guideline: an exploratory investigation using psychological theory. Implement. Sci. 2007;2:8. doi: 10.1186/1748-5908-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministerial Council on Drug Strategy . Commonwealth of Australia; Perth: 2011. National Drug Strategy 2010–2015. [Google Scholar]
- Ministry of Health . Ministry of Health; Wellington: 2007. New Zealand Smoking Cessation Guidelines. [Google Scholar]
- Ministry of Health . Ministry of Health; Wellington: 2015. Eating and Activity Guidelines for New Zealand Adults. [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- Moher D., Shamseer L., Clarke M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(1) doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence-Based Healthcare. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- Nash M. Physical care skills: a training needs analysis of inpatient and community mental health nurses. Ment. Health Pract. 2005;9(4):20–23. [Google Scholar]
- Naslund J.A., Whiteman K.L., McHugo G.J., Aschbrenner K.A., Marsh L.A., Bartels S.J. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: a systematic review and meta-analysis. Gen. Hosp. Psychiatry. 2017;47:83–102. doi: 10.1016/j.genhosppsych.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health and Medical Research Council . Commonwealth of Australia; Canberra: 2009. Australian Guidelines to Reduce Health Risks from Drinking Alcohol. [Google Scholar]
- National Health and Medical Research Council . Australian Government; Canberra: 2013. Eat for Health: Australian Dietary Guidelines Summary. [Google Scholar]
- National Institute for Health and Care Excellence . The British Psychological Society & The Royal College of Psychiatrists; 2010. Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Primary and Secondary Care (Updated Edition) Clinical Guideline 82. [Google Scholar]
- National Institute for Health and Care Excellence . Public Health Guidance 48. NICE; London: 2013. Smoking cessation in secondary care: acute, maternity and mental health services. [Google Scholar]
- National Preventive Health Taskforce . Canberra; Commonwealth of Australia: 2008. Australia: The Healthiest Country by 2020 - a Discussion Paper. In. [Google Scholar]
- NSW Department of Health . NSW Department of Health; Sydney: 2017. Physical Health Care of Mental Health Consumers. [Google Scholar]
- NSW Department of Health . Department of Health; Sydney, NSW: 2017. Physical Health Care within Mental Health Services. [Google Scholar]
- NSW Mental Health Commission . Commission NMH; Sydney: 2014. Living Well: A Strategic Plan for Mental Health in NSW. (ed.) [Google Scholar]
- Olfson M., Gerhard T., Huang C., Crystal S., Stroup T. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiat. 2015;72:1172–1181. doi: 10.1001/jamapsychiatry.2015.1737. [DOI] [PubMed] [Google Scholar]
- Organ B., Nicholson E., Castle D. Implementing a physical health strategy in a mental health service. Australasian psychiatry : bulletin of Royal Australian and New Zealand College of Psychiatrists. 2010;18(5):456–459. doi: 10.3109/10398562.2010.506217. [DOI] [PubMed] [Google Scholar]
- Osborn D.P., Nazareth I., Wright C.A., King M.B. Impact of a nurse-led intervention to improve screening for cardiovascular risk factors in people with severe mental illnesses. Phase-two cluster randomised feasibility trial of community mental health teams. BMC Health Serv. Res. 2010;10:61. doi: 10.1186/1472-6963-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker C., McNeill A., Ratschen E. Tailored tobacco dependence support for mental health patients: a model for inpatient and community services. Addiction. 2012;107(Suppl. 2):18–25. doi: 10.1111/j.1360-0443.2012.04082.x. [DOI] [PubMed] [Google Scholar]
- Piercy K.L., Troiano R.P., Ballard R.M. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price J.H., Ambrosetti L.M., Sidani J.E., Price J.A. Psychiatrists' smoking cessation activities with Ohio community mental health center patients. Community Ment. Health J. 2007;43(3):251–266. doi: 10.1007/s10597-006-9074-3. [DOI] [PubMed] [Google Scholar]
- Prochaska J.J., Fletcher L., Hall S.E., Hall S.M. Return to smoking following a smoke-free psychiatric hospitalization. Am. J. Addict. 2006;15(1):15–22. doi: 10.1080/10550490500419011. [DOI] [PubMed] [Google Scholar]
- Public Health England . Public Health England; London: 2016. Government Dietary Recommendations. [Google Scholar]
- Rees K, Dyakova M, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst. Rev.. 2013(3):Art. No.: CD002128. [DOI] [PubMed]
- Revell C., Schroeder S. Simplicity matters: using system-level changes to encourage clinician intervention in helping tobacco users quit. Nicotine and Tobacco Research. 2005;7(S1):S67–S69. doi: 10.1080/14622200500078162. [DOI] [PubMed] [Google Scholar]
- Rice V.H., Hartmann-Boyce J., Stead L.F. Nursing interventions for smoking cessation. Cochrane Database Syst. Rev. 2013;8 doi: 10.1002/14651858.CD001188.pub4. [DOI] [PubMed] [Google Scholar]
- Rigotti N.A., Clair C., Munafo M.R., Stead L.F. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst. Rev. 2012;5 doi: 10.1002/14651858.CD001837.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robson D., Haddad M., Gray R., Gournay K. Mental health nursing and physical health care: a cross-sectional study of nurses' attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int. J. Ment. Health Nurs. 2013;22(5):409–417. doi: 10.1111/j.1447-0349.2012.00883.x. [DOI] [PubMed] [Google Scholar]
- Robson D., Haddad M., Gray R., Gournay K. Mental health nursing and physical health care: a cross-sectional study of nurses' attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int. J. Ment. Health Nurs. 2013;22(5):409–417. doi: 10.1111/j.1447-0349.2012.00883.x. [DOI] [PubMed] [Google Scholar]
- Royal Australian College of General Practitioners . Royal Australian College of General Practitioners; Melbourne: 2004. Smoking, Nutrition, Alcohol, Physical Activity (SNAP): A Population Health Guide to Behavioural Risk Factors in General Practice. [Google Scholar]
- RStudio Team RStudio: integrated development for R. 2015. http://www.rstudio.com/
- Ryan R., Hill S. How to GRADE the quality of the evidence. http://cccrg.cochrane.org/author-resources Version 3.0. 2016.
- Sandstrom B., Willman A., Svensson B., Borglin G. Perceptions of national guidelines and their (non) implementation in mental healthcare: a deductive and inductive content analysis. Implement. Sci. 2015;10(1):43. doi: 10.1186/s13012-015-0234-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarna L., Bialous S.A., Wells M.J., Kotlerman J. Smoking among psychiatric nurses: does it hinder tobacco dependence treatment? Journal of the American Psychiatric Nurses Association. 2009;15(1):59–67. doi: 10.1177/1078390308330638. [DOI] [PubMed] [Google Scholar]
- Schacht L., Ortiz G., Lane M.B., Jr. National Association of State Mental Health Program Directors Research Institute; Alexandria, VA: 2012. Smoking Policies and Practices in State Psychiatric Facilities: Survey Results From 2011. [Google Scholar]
- Schroeder S.A. What to do with a patient who smokes. J. Am. Med. Assoc. 2005;294(4):482–487. doi: 10.1001/jama.294.4.482. [DOI] [PubMed] [Google Scholar]
- Scott D., Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Ment. Health Nurs. 2011;32(9):589–597. doi: 10.3109/01612840.2011.569846. [DOI] [PubMed] [Google Scholar]
- Sheffer M., Baker T., Fraser D., Adsit R., McAfee T., Fiore M. Fax referrals, academic detailing, and tobacco quitline use: a randomized trial. Am. J. Prev. Med. 2012;42(1):21–28. doi: 10.1016/j.amepre.2011.08.028. [DOI] [PubMed] [Google Scholar]
- . Shojania K, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. In: Cochrane Database Syst. Rev.. Issue 3. Art. No.: CD001096.; 2009. [DOI] [PMC free article] [PubMed]
- Siru R., Hulse G.K., Khan R.J.K., Tait R.J. Motivation to quit smoking among hospitalised individuals with and without mental health disorders. Australian & New Zealand Journal of Psychiatry. 2010;44(7):640–647. doi: 10.3109/00048671003627413. [DOI] [PubMed] [Google Scholar]
- Stanley S.H., Laugharne J. Neurosciences SoPaC. University of Western Australia; Crawley: 2013. Clinical guidelines for the physical care of mental health consumers: multi-site service evaluation project 2013. ed. [Google Scholar]
- Stanley S., Laugharne J. The impact of lifestyle factors on the physical health of people with a mental illness: a brief review. Int. J. Behav. Med. 2014;21(2):275–281. doi: 10.1007/s12529-013-9298-x. [DOI] [PubMed] [Google Scholar]
- Stanton R., Happell B., Reaburn P. Investigating the exercise-prescription practices of nurses working in inpatient mental health settings. Int. J. Ment. Health Nurs. 2015;24(2):112–120. doi: 10.1111/inm.12125. [DOI] [PubMed] [Google Scholar]
- Stockings E.A.L., Bowman J.A., Baker A.L. Impact of a postdischarge smoking cessation intervention for smokers admitted to an inpatient psychiatric facility: a randomized controlled trial. Nicotine and Tobacco Research. 2014;16(11):1417–1428. doi: 10.1093/ntr/ntu097. [DOI] [PubMed] [Google Scholar]
- Stockings E.A., Bowman J.A., Bartlem K.M. Implementation of a smoke-free policy in an inpatient psychiatric facility: patient-reported adherence, support, and receipt of nicotine-dependence treatment. Int. J. Ment. Health Nurs. 2015;24(4):342–349. doi: 10.1111/inm.12128. [DOI] [PubMed] [Google Scholar]
- Stroup D.F., Berlin S.C., Olkin I. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Tso G., Kumar P., Jayasooriya T., Kisely S., Siskind D. Metabolic monitoring and management among clozapine users. Australasian Psychiatry. 2017;25(1):48–52. doi: 10.1177/1039856216665282. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture . 8th edition. U.S. Department of Health and Human Services; In. Washington DC: 2015. 2015–2020 Dietary Guidelines for Americans. [Google Scholar]
- US Department of Health and Human Services . 2009. The Guide to Clinical Preventive Services. In. Rockville MD: Agency for Healthcare Research and Quality. Pub. No. 09-IP006. [Google Scholar]
- Verhaeghe N., De Maeseneer J., Maes L., Van Heeringen C., Annemans L. Effectiveness and cost-effectiveness of lifestyle interventions on physical activity and eating habits in persons with severe mental disorders: a systematic review. The international journal of behavioral nutrition and physical activity. 2011;8:28. doi: 10.1186/1479-5868-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Hippel P.T. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Med. Res. Methodol. 2015;15(35) doi: 10.1186/s12874-015-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Ruesten A., Weikert C., Fietze I., Boeing H. Association of sleep duration with chronic diseases in the European prospective investigation into cancer and nutrition (EPIC)-potsdam study. PLoS One. 2012;7(1):e30972. doi: 10.1371/journal.pone.0030972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlbeck K., Westman J., Nordentoft M., Gissler M., Laursen T.M. Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. Br. J. Psychiatry J. Ment. Sci. 2011;199(6):453–458. doi: 10.1192/bjp.bp.110.085100. [DOI] [PubMed] [Google Scholar]
- Walker E.R., McGee R.E., Druss B.G. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J.M., Miskimen T., Minsky S. Increasing tobacco dependence treatment through continuing education training for behavioral health professionals. Psychiatr. Serv. 2015;66(1):21–26. doi: 10.1176/appi.ps.201300523. [DOI] [PubMed] [Google Scholar]
- Wolfenden L., Wiggers J., Campbell E., Knight J., Kerridge R., Spigelman A. Providing comprehensive smoking cessation care to surgical patients: the case for computers. Drug and alcohol review. 2009;28:60–65. doi: 10.1111/j.1465-3362.2008.00003.x. [DOI] [PubMed] [Google Scholar]
- Woolf S., Krist A., Rothemich S. Center for American Progress; Washington DC: 2006. Joining Hands: Partnerships Between Physicians and the Community in the Delivery of Preventive Care. [Google Scholar]
- World Health Organization . WHO; Geneva: 2003. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation. [Google Scholar]
- World Health Organization . WHO; Geneva: 2011. Global Recommendations on Physical Activity for Health. [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva: 2013. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. [Google Scholar]
- World Health Organization . Monitoring Tobacco Use and Prevention Policies. WHO; In. Geneva: 2017. WHO report on the global tobacco epidemic, 2017. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2018. Global Status Report on Alcohol and Health 2018. 3.0IGO LCB-N-S, ed. [Google Scholar]
- Wu C.Y., Chang C.K., Robson D. Evaluation of smoking status identification using electronic health records and open-text information in a large mental health case register. PLoS ONE [Electronic Resource] 2013;8(9):e74262. doi: 10.1371/journal.pone.0074262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wye P.M., Bowman J.A., Wiggers J.H. Smoking restrictions and treatment for smoking: policies and procedures in psychiatric inpatient units in Australia. Psychiatr. Serv. 2009;60(1):100–107. doi: 10.1176/ps.2009.60.1.100. [DOI] [PubMed] [Google Scholar]
- Wye P., Bowman J., Wiggers J. An audit of the prevalence of recorded nicotine dependence treatment in an Australian psychiatric hospital. Australian & New Zealand Journal of Public Health. 2010;34(3):298–303. doi: 10.1111/j.1753-6405.2010.00530.x. [DOI] [PubMed] [Google Scholar]
- Wye P., Bowman J., Wiggers J., Freund M., Wolfenden L., Stockings E. Treating nicotine dependence in Australian mental health hospitals. Mental Health and Substance Use Journal. 2011;2(130) [Google Scholar]
- . Wye PM, Stockings EA, Bowman JA, Oldmeadow C, Wiggers JH. Effectiveness of a clinical practice change intervention in increasing the provision of nicotine dependence treatment in inpatient psychiatric facilities: an implementation trial. BMC Psychiatry Vol 17 2017, ArtID 56. 2017;17. [DOI] [PMC free article] [PubMed]
- Zabeen S., Tsourtos G., Campion J., Lawn S. Type of unit and population served matters when implementing a smoke-free policy in mental health settings: perceptions of unit managers across England. Int. J. Soc. Psychiatry. 2015;61(7):700–710. doi: 10.1177/0020764015575799. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material