Key Points
Question
What were the trends in medical imaging from 2000 through 2016 in the United States and Ontario, Canada?
Findings
In this retrospective cohort study of 135 million imaging examinations conducted in 7 US integrated health care systems and in Ontario, annual growth in imaging rates among US adults and older adults slowed over time for computed tomography (CT; from an 11.6% annual percentage increase among adults and 9.5% among older adults in 2000-2006 to 3.7% among adults in 2013-2016 and 5.2% among older adults in 2014-2016) and for magnetic resonance imaging (MRI; from 11.4% in 2000-2004 in adults and 11.3% in 2000-2005 in older adults to 1.3% in 2007-2016 in adults and 2.2% in 2005-2016 in older adults). Patterns in Ontario were similar. Among children, annual growth for CT stabilized or declined (United States: from 10.1% in 2000-2005 to 0.8% in 2013-2016; Ontario: from 3.3% in 2000-2006 to −5.3% in 2006-2016), but patterns for MRI were similar to adults. Changes in annual growth in ultrasound were smaller among adults and children in the United States and Ontario.
Meaning
From 2000 to 2016 in 7 US integrated health care systems and Ontario, CT and MRI rates continued to increase among adults, but at a slower pace in more recent years compared with earlier years; in children, CT rates stabilized or declined in recent years.
Abstract
Importance
Medical imaging increased rapidly from 2000 to 2006, but trends in recent years have not been analyzed.
Objective
To evaluate recent trends in medical imaging.
Design, Setting, and Participants
Retrospective cohort study of patterns of medical imaging between 2000 and 2016 among 16 million to 21 million patients enrolled annually in 7 US integrated and mixed-model insurance health care systems and for individuals receiving care in Ontario, Canada.
Exposures
Calendar year and country (United States vs Canada).
Main Outcomes and Measures
Use of computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and nuclear medicine imaging. Annual and relative imaging rates by imaging modality, country, and age (children [<18 years], adults [18-64 years], and older adults [≥65 years]).
Results
Overall, 135 774 532 imaging examinations were included; 5 439 874 (4%) in children, 89 635 312 (66%) in adults, and 40 699 346 (30%) in older adults. Among adults and older adults, imaging rates were significantly higher in 2016 vs 2000 for all imaging modalities other than nuclear medicine. For example, among older adults, CT imaging rates were 428 per 1000 person-years in 2016 vs 204 per 1000 in 2000 in US health care systems and 409 per 1000 vs 161 per 1000 in Ontario; for MRI, 139 per 1000 vs 62 per 1000 in the United States and 89 per 1000 vs 13 per 1000 in Ontario; and for ultrasound, 495 per 1000 vs 324 per 1000 in the United States and 580 per 1000 vs 332 per 1000 in Ontario. Annual growth in imaging rates among US adults and older adults slowed over time for CT (from an 11.6% annual percentage increase among adults and 9.5% among older adults in 2000-2006 to 3.7% among adults in 2013-2016 and 5.2% among older adults in 2014-2016) and for MRI (from 11.4% in 2000-2004 in adults and 11.3% in 2000-2005 in older adults to 1.3% in 2007-2016 in adults and 2.2% in 2005-2016 in older adults). Patterns in Ontario were similar. Among children, annual growth for CT stabilized or declined (United States: from 10.1% in 2000-2005 to 0.8% in 2013-2016; Ontario: from 3.3% in 2000-2006 to −5.3% in 2006-2016), but patterns for MRI were similar to adults. Changes in annual growth in ultrasound were smaller among adults and children in the United States and Ontario compared with CT and MRI. Nuclear medicine imaging declined in adults and children after 2006.
Conclusions and Relevance
From 2000 to 2016 in 7 US integrated and mixed-model health care systems and in Ontario, rates of CT and MRI use continued to increase among adults, but at a slower pace in more recent years. In children, imaging rates continued to increase except for CT, which stabilized or declined in more recent periods. Whether the observed imaging utilization was appropriate or was associated with improved patient outcomes is unknown.
This study evaluates trends in utilization of computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and nuclear medicine imaging between 2000 and 2016 in 7 US health care networks and in Ontario, Canada.
Introduction
Use of computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound in the United States increased rapidly from 2000 to 2006.1,2 Among Medicare beneficiaries, the increase in utilization was higher for medical imaging than other physician-provided services.3,4 Steep increases in imaging can be attributed to technical improvements, physician and patient demand, and strong financial incentives. Medical imaging contributes to accurate disease diagnosis and improved treatment; however, imaging can also increase costs and patient harms, such as incidental findings, overdiagnosis, anxiety, and radiation exposure associated with increased risk of cancer. It has been estimated that 30% or more of imaging examinations may be unnecessary, costing approximately $30 billion annually in the United States.5 In addition, in a recent study that compared the United States with 10 other countries on various metrics, the United States ranked 1 or 2 in the number of CT and MRI scans performed per 1000 individuals.6
Potential overuse of diagnostic testing has been addressed by the American Board of Internal Medicine Foundation’s Choosing Wisely campaign7 and by initiatives by payers to reduce imaging through payment reductions.8,9 These efforts are frequently cited to have reduced imaging rates among Medicare beneficiaries.10,11 Most analyses, however, have focused on costs rather than utilization, and changing billing practices, including the bundling of common examinations, makes assessment of utilization and costs different. Costs may not accurately reflect utilization or potential harms associated with imaging. To date, no large studies have determined recent imaging utilization rates across different patient populations, such as populations in integrated health care systems, and few studies have assessed imaging patterns over time.6
This study examined medical imaging rates from 2000 through 2016 among individuals enrolled in diverse US integrated health care systems and among individuals residing in Ontario, Canada, and assessed changes in medical imaging utilization over time by country, health system, and patient demographic factors.
Methods
Utilization data of CT, MRI, ultrasound, and nuclear medicine were obtained from 2000 through 2016 for individuals enrolled in 7 US health care systems and individuals living in Ontario who were eligible for the Ontario Health Insurance Plan. These sites were selected to provide a sample of US health care systems with sociodemographic and geographic diversity. The US systems included Kaiser Permanente (KP) Hawaii, KP Northern California, and KP Northwest (Oregon), each of which are fully integrated staff model health maintenance organizations (HMOs); KP Washington (which was Group Health Cooperative until 2016), Geisinger (Pennsylvania), Harvard Pilgrim Health Care (Boston, Massachusetts), and Marshfield Clinic Health System (Wisconsin), all of which are mixed-model insurance plans in which patients received care within an HMO or a preferred provider organization under a fee-for-service model of care. One of the health plans contributed data after 2003. The institutional review boards of all collaborating institutions and the University of California, Davis, Statistical Coordinating Center approved the study, and a waiver of individual consent was obtained.
Data Sources
The US health care systems are members of the National Cancer Institute–supported Health Care Systems Research Network,12 and all sites have available electronic health care information stored in a virtual data warehouse.13,14 The virtual data warehouse is a collaborative data model structure consisting of a series of data tables with information on all medical care utilization, including imaging, among enrollees. Imaging is stored across settings (inpatient, outpatient, and emergency departments) from clinical and administrative data sources, including electronic health records. For imaging done outside the health care system, information is captured via claims data. For Ontario, the Registered Persons Database was used to identify an eligible population. Imaging utilization data were obtained from physician billing records, inpatient imaging from the Discharge Abstract Database, surgery-related imaging from the Same-Day Surgery Database, and emergency department imaging from the National Ambulatory Care Reporting System. These data sets were linked using unique encoded identifiers and analyzed at ICES, Toronto, Ontario, before being aggregated with the US data at the University of California, Davis.
Imaging Utilization
For each calendar year, individuals who were born, continuously enrolled, or died during that year were included. United States imaging examinations were coded using a combination of Current Procedural Terminology15; International Classification of Diseases, Ninth Revision, Clinical Modification16 and International Statistical Classification of Diseases, Tenth Revision, Clinical Modification17; and Healthcare Common Procedure Coding System18 billing codes, including modifiers for the technical, physician, or global components. Examinations were included irrespective of the physician specialty billing for the study. Some billing codes changed over time, and all codes were mapped to an anatomic area and imaging modality to ensure consistency over time, updating a previously used map.2 For Ontario data, Canadian Classification of Health Interventions19 codes were used to create a relational table of codes from the United States with codes from Canada to compare imaging rates by imaging modality and anatomic area. A nonspecific ultrasound code was frequently used in Ontario, making it inaccurate to compare ultrasound within anatomic areas between the United States and Ontario.
Imaging performed in combination with radiation treatment planning, image processing (ie, manipulation of images after they were obtained), and imaging reinterpretation were not included. The final map included 4774 unique billing codes. Overall, both professional and technical billing claims were used to assess utilization, but to avoid overcounting, only a single imaging examination per modality and anatomic region per day were included. This analysis was restricted to CT, MRI, ultrasound, and nuclear medicine examinations. Within these modalities, all examination types were included. For example, all angiographic studies were included if they used CT, MRI, ultrasound, or nuclear medicine, and these study types were included with the specific imaging modality. The full billing code list of included studies is available from the authors.
Statistical Analyses
All analyses were stratified by country, imaging modality, and age group (<18 years [children]; 18-64 years [adults]; and ≥65 years [older adults]) and account for follow-up time for individuals born or dying that year. Utilization rates were modeled using overdispersed Poisson regression including main effects for examination year, country, and US system and an interaction term between examination year and country. Absolute annual rates per 1000 person-years and relative rates (US vs Canada and 2016 vs 2000) with 95% confidence intervals were estimated from the Poisson regression models. Absolute rates for the United States were averaged over the US health care systems using equal weights. Annual rates per 1000 person-years are similar to rates per 1000 persons except that individuals contributed less than a full year during years they were born or died.
Joinpoint regression20,21 was used to identify years with significant changes in imaging trends over time and to calculate the average annual percentage change (growth) within fixed time periods (2000-2005, 2006-2011, and 2012-2016) by imaging modality and anatomic area. Rates and standard errors estimated from the Poisson regression model were entered into the software, which determined the optimal number of change points and identified up to 3 joinpoints based on the recommended maximum for the number of observations. A permutation test was used to select the best model and determine the number of joinpoints for each subgroup, applying a Bonferroni correction to the type I error to correct for multiple testing. Annual percentage changes and 95% confidence intervals were estimated assuming that the rates change at a constant percentage every year on a log scale.
As exploratory analyses, annual imaging rates were graphed and relative imaging rates with 95% confidence intervals were calculated by imaging modality for each individual health plan, by anatomic area for CT and MRI for the United States and Ontario, and for nuclear medicine and ultrasound overall, and stratified by US plan type (integrated vs mixed-model plans) after adjusting for the annual mean Elixhauser comorbidity score22 and sex. Joinpoint regression was performed using Joinpoint version 4.7.0.0, and remaining analyses were performed using SAS version 9.4 (SAS Institute Inc).
Results
Overall, 135 774 532 imaging examinations were included over 310 093 012 person-years; 5 439 874 (4%) in children (49.5% female), 89 635 312 (66.0%) in adults (50.8% female), and 40 699 346 (30%) in older adults (50.0% female) (Table 1). Distributions of demographic variables were similar across health care systems; 51% of individuals were female, the Elixhauser comorbidity score ranged from 0.07 to 0.09 in children (mean, 0.08), from 0.13 to 0.24 in adults (mean, 0.17), and from 0.83 to 1.50 in older adults (mean, 0.96), and the percentage of pregnant women ranged from 0.83% to 1.14% across US health care systems and 0.95% in Ontario. Rates of CT, MRI, and ultrasound imaging increased over time in the United States and Ontario, whereas nuclear medicine imaging declined over time (Table 1). For example, in the US health care systems, CT imaging increased from 56 per 1000 person-years in 2000 to 141 per 1000 person-years in 2016, MRI from 16 to 64 per 1000 person-years, ultrasound from 177 to 347 per 1000 person-years, and nuclear medicine from 28 to 22 per 1000 person-years (Table 1). The patterns were similar in Ontario: CT increased from 52 per 1000 person-years in 2000 to 135 per 1000 person-years in 2016, MRI from 10 to 60 per 1000 person-years, ultrasound from 188 to 386 per 1000 person-years, and nuclear medicine from 33 to 25 per 1000 person-years.
Table 1. Characteristics of Study Population by Health Care Systema.
| Characteristics | Overall No. (%) | Ontario | All US Sites | Mixed Model | Integrated | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| US Site A | US Site B | US Site C | US Site D | US Site E | US Site F | US Site G | ||||
| Total No. of person-years | 310 093 012 | 226 280 059 | 83 812 954 | 11 512 495 | 7 882 429 | 2 489 571 | 2 811 040 | 48 903 156 | 6 975 790 | 3 238 473 |
| No. of person-years by age group | ||||||||||
| Children (<18 y) | 66 932 670 (22) | 48 838 155 | 18 094 514 | 2 664 365 | 1 432 029 | 575 104 | 571 319 | 10 673 313 | 1 468 324 | 710 060 |
| Adults (18-64 y) | 198 554 403 (64) | 145 251 413 | 5 302 991 | 7 933 096 | 5 108 928 | 1 426 853 | 1 576 744 | 30 797 362 | 4 427 181 | 2 032 827 |
| Older adults (≥65 y) | 44 605 939 (14) | 32 190 491 | 12 415 449 | 915 034 | 1 341 472 | 487 614 | 662 977 | 7 432 481 | 1 080 285 | 495 586 |
| Total No. of tests | ||||||||||
| Children (<18 y) | 5 439 874 (4) | 4 100 110 | 1 339 764 | 294 865 | 120 086 | 60 179 | 73 323 | 621 964 | 110 159 | 59 188 |
| Adults (18-64 y) | 89 635 312 (66) | 67 833 889 | 21 801 423 | 4 563 830 | 2 155 108 | 622 092 | 1 009 847 | 10 970 397 | 1 684 310 | 795 839 |
| Older adults (≥65 y) | 40 699 346 (30) | 29 384 193 | 11 315 153 | 1 161 587 | 1 305 356 | 516 591 | 772 244 | 6 139 781 | 950 233 | 469 361 |
| No. of person-years by sex | ||||||||||
| Male | 151 812 172 (49) | 111 646 603 | 40 165 571 | 5 533 333 | 3 651 049 | 1 192 240 | 1 354 264 | 23 384 056 | 3 334 575 | 1 585 642 |
| Female | 158 275 573 (51) | 114 633 456 | 43 642 118 | 5 979 163 | 4 231 311 | 1 297 331 | 1 456 352 | 25 384 056 | 3 641 074 | 1 652 831 |
| Unknown/other | 5267 (0.002) | NA | 5266 | NA | 69 | NA | 424 | 4632 | 141 | NA |
| Pregnancies, % | 2 985 128 (0.96) | 0.95 | 1.02 | 1.14 | 0.83 | 1.01 | NA | 1.06 | 0.97 | 1.08 |
| Elixhauser score, mean | ||||||||||
| Children (aged <18 y) | NA | 0.08 | 0.08 | 0.07 | 0.08 | 0.09 | 0.09 | 0.08 | 0.09 | |
| Adults (aged 18-64 y) | NA | 0.17 | 0.18 | 0.16 | 0.24 | 0.19 | 0.15 | 0.17 | 0.13 | |
| Older adults (aged ≥65 y) | NA | 0.96 | 1.10 | 0.70 | 1.50 | 0.95 | 0.96 | 0.88 | 0.83 | |
| Total No. of tests per 1000 person-years in sample years | ||||||||||
| Computed tomography | ||||||||||
| 2000 | 52 | 56 | 76 | 82 | 81 | NA | 57 | 68 | 65 | |
| 2004 | 75 | 82 | 122 | 115 | 110 | 138 | 94 | 105 | 107 | |
| 2008 | 101 | 106 | 127 | 150 | 145 | 171 | 106 | 126 | 145 | |
| 2012 | 111 | 116 | 128 | 139 | 156 | 175 | 125 | 132 | 129 | |
| 2016 | 135 | 141 | 156 | 165 | 179 | 225 | 142 | 150 | 167 | |
| Magnetic resonance imaging | ||||||||||
| 2000 | 10 | 16 | 53 | 33 | 41 | NA | 27 | 31 | 29 | |
| 2004 | 20 | 29 | 88 | 62 | 57 | 93 | 40 | 42 | 46 | |
| 2008 | 40 | 45 | 99 | 83 | 71 | 92 | 44 | 60 | 82 | |
| 2012 | 50 | 55 | 99 | 77 | 77 | 83 | 57 | 76 | 61 | |
| 2016 | 60 | 64 | 105 | 80 | 71 | 89 | 65 | 72 | 81 | |
| Ultrasound | ||||||||||
| 2000 | 188 | 177 | 210 | 157 | 185 | NA | 124 | 160 | 122 | |
| 2004 | 218 | 207 | 265 | 188 | 217 | 285 | 151 | 160 | 174 | |
| 2008 | 283 | 263 | 287 | 231 | 228 | 319 | 180 | 176 | 212 | |
| 2012 | 325 | 301 | 307 | 249 | 283 | 351 | 211 | 212 | 220 | |
| 2016 | 386 | 347 | 331 | 256 | 295 | 396 | 224 | 223 | 243 | |
| Nuclear medicine | ||||||||||
| 2000 | 33 | 28 | 28 | 28 | 35 | NA | 25 | 27 | 30 | |
| 2004 | 34 | 34 | 34 | 33 | 39 | 56 | 25 | 26 | 32 | |
| 2008 | 36 | 28 | 28 | 23 | 36 | 52 | 25 | 22 | 35 | |
| 2012 | 29 | 22 | 22 | 29 | 35 | 40 | 20 | 18 | 26 | |
| 2016 | 25 | 22 | 22 | 22 | 30 | 34 | 16 | 16 | 23 | |
Abbreviation: NA, not available.
Sites are listed in order of increasing rates of computed tomography imaging in 2016.
Adults
Annual imaging rates by imaging modality, age, and country are shown in Table 2. Imaging rates were higher in 2016 than in 2000 in adults and older adults for CT, MRI, and ultrasound in both the United States and Ontario. For example, among older adults in the United States, CT increased from 204 per 1000 person-years in 2000 to 428 per 1000 person-years in 2016 (relative rate for 2016 compared with 2000, 2.1; 95% CI, 2.0-2.2), and in Ontario, CT increased from 161 to 409 per 1000 person-years (relative rate, 2.5; 95% CI, 2.4-2.7). Magnetic resonance imaging increased from 62 to 139 per 1000 person-years in the United States (relative rate, 2.3; 95% CI, 2.0-2.6) and from 13 to 89 per 1000 person-years in Ontario (relative rate, 6.7; 95% CI, 5.7-7.8), and ultrasound increased from 324 to 495 per 1000 person-years in the United States (relative rate, 1.5; 95% CI, 1.4-1.7) and from 332 to 580 per 1000 person-years in Ontario (relative rate, 1.7; 95% CI, 1.7-1.8). Among older adults, nuclear medicine declined from 94 to 64 per 1000 person-years in the United States (relative rate, 0.68; 95% CI, 0.63-0.74) and from 87 to 74 per 1000 person-years in Ontario (relative rate, 0.84; 95% CI, 0.80-0.89).
Table 2. Absolute and Relative Imaging Rates in Ontario and US Health Care Systems by Imaging Modality, Age, and Country, Based on Joinpoint Analysis.
| Older Adults (Aged ≥65 y) | Adults (Aged 18-64 y) | Children (Aged <18 y) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Rate per 1000 Person-Years (95% CI) | Relative Rate (95% CI) | Rate per 1000 Person-Years (95% CI) | Relative Rate (95% CI) | Rate per 1000 Person-Years (95% CI) | Relative Rate (95% CI) | ||||
| United States | Ontario | United States | Ontario | United States | Ontario | ||||
| Computed Tomography | |||||||||
| 2000 | 204 (192-216) | 161 (154-167) | 1.3 (1.2-1.4) | 63 (58-68) | 46 (43-48) | 1.4 (1.2-1.5) | 18 (16-19) | 12 (11-12) | 1.5 (1.4-1.7) |
| 2006 | 352 (338-367) | 277 (269-285) | 1.3 (1.2-1.4) | 119 (112-126) | 79 (76-82) | 1.5 (1.4-1.6) | 29 (28-31) | 14 (14-15) | 2.1 (1.9 2.2) |
| 2012 | 376 (362-390) | 344 (336-352) | 1.1 (1.0-1.1) | 120 (113-127) | 89 (86-92) | 1.3 (1.3-1.4) | 22 (21-24) | 10 (10-11) | 2.2 (2.0-2.4) |
| 2016 | 428 (415-441) | 409 (402-418) | 1.0 (1.0-1.1) | 134 (127-141) | 103 (100-107) | 1.3 (1.2-1.4) | 22 (19-22) | 9 (8-9) | 2.3 (2.1-2.5) |
| 2016 vs 2000, relative rate (95% CI) | 2.1 (2.0-2.2) | 2.5 (2.4-2.7) | 2.1 (1.9-2.4) | 2.3 (2.1-2.4) | 1.2 (1.1-1.3) | 0.8 (0.7-0.8) | |||
| Magnetic Resonance Imaging | |||||||||
| 2000 | 62 (55-69) | 13 (12-15) | 4.6 (3.8-5.6) | 42 (37-47) | 12 (11-14) | 3.4 (2.9-4.0) | 9 (9-10) | 4 (3.7-4.4) | 2.3 (2.0-2.6) |
| 2006 | 112 (103-121) | 43 (40-47) | 2.6 (2.9-3.8) | 72 (66-78) | 34 (32-36) | 2.1 (1.9-2.3) | 15 (14-16) | 8 (7-8) | 1.9 (2.1-2.5) |
| 2012 | 127 (119-137) | 73 (69-77) | 1.7 (1.6-1.9) | 81 (75-87) | 57 (54-59) | 1.4 (1.3-1.6) | 21 (19-22) | 14 (14-15) | 1.4 (1.3-1.5) |
| 2016 | 139 (131-147) | 89 (85-93) | 1.6 (1.5-1.7) | 85 (80-91) | 66 (63-69) | 1.3 (1.2-1.4) | 21 (20-23) | 16 (15-17) | 1.3 (1.2-1.4) |
| 2016 vs 2000, relative rate (95% CI) | 2.3 (2.0-2.6) | 6.7 (5.7-7.8) | 2.0 (1.8-2.3) | 5.4 (4.8-6.1) | 2.3 (2.0-2.5) | 4.0 (3.6-4.3) | |||
| Ultrasound | |||||||||
| 2000 | 324 (302-347) | 332 (320-345) | 1.0 (0.9-1.1) | 174 (165-184) | 216 (201-221) | 0.8 (0.8-0.9) | 30 (28-32) | 36 (34-37) | 0.8 (0.8-0.9) |
| 2006 | 415 (392-439) | 409 (397-423) | 1.0 (1.0-1.1) | 226 (217-237) | 286 (280-293) | 0.8 (0.8-0.8) | 40 (37-43) | 48 (47-50) | 0.8 (0.9-1.0) |
| 2012 | 494 (472-518) | 510 (497-523) | 1.0 (0.9-1.0) | 262 (252-272) | 362 (355-369) | 0.7 (0.7-0.8) | 54 (51-58) | 73 (71-75) | 0.7 (0.7-0.8) |
| 2016 | 495 (475-515) | 580 (567-593) | 0.9 (0.8-0.9) | 278 (268-288) | 428 (421-436) | 0.6 (0.6-0.7) | 59 (56-63) | 85 (83-87) | 0.7 (0.7-0.7) |
| 2016 vs 2000, relative rate (95% CI) | 1.5 (1.4-1.7) | 1.7 (1.7-1.8) | 1.6 (1.5-1.7) | 2.0 (1.9-2.1) | 2.0 (1.8-2.2) | 2.4 (2.3-2.5) | |||
| Nuclear Medicine | |||||||||
| 2000 | 94 (88-100) | 87 (84-91) | 1.1 (1.0-1.2) | 28 (27-30) | 32 (32-33) | 0.9 (0.8-0.9) | 4 (3.7-4.3) | 5 (4.5-4.9) | 0.9 (0.8-0.9) |
| 2006 | 101 (95-106) | 97 (94-100) | 1.0 (1.0-1.2) | 30 (29-32) | 34 (33-35) | 0.9 (0.8-0.9) | 3 (3.2-3.7) | 4 (4.1-4.4) | 0.8 (0.8-1.0) |
| 2012 | 76 (72-80) | 84 (82-87) | 0.9 (0.8-1.0) | 20 (19-21) | 25 (24-25) | 0.8 (0.8-0.9) | 2 (1.9-2.4) | 3 (2.5-2.8) | 0.8 (0.7-0.9) |
| 2016 | 64 (61-68) | 74 (72-76) | 0.9 (0.8-0.9) | 16 (15-17) | 20 (19-20) | 0.8 (0.7-0.9) | 2 (1.3-1.6) | 2 (1.7-1.9) | 0.8 (0.7-0.9) |
| 2016 vs 2000, relative rate (95% CI) | 0.68 (0.63-0.74) | 0.84 (0.80-0.89) | 0.55 (0.51-0.60) | 0.61 (0.58-0.63) | 0.37 (0.32-0.42) | 0.39 (0.36-0.41) | |||
Imaging Rates Among Adults by Joinpoint Analysis
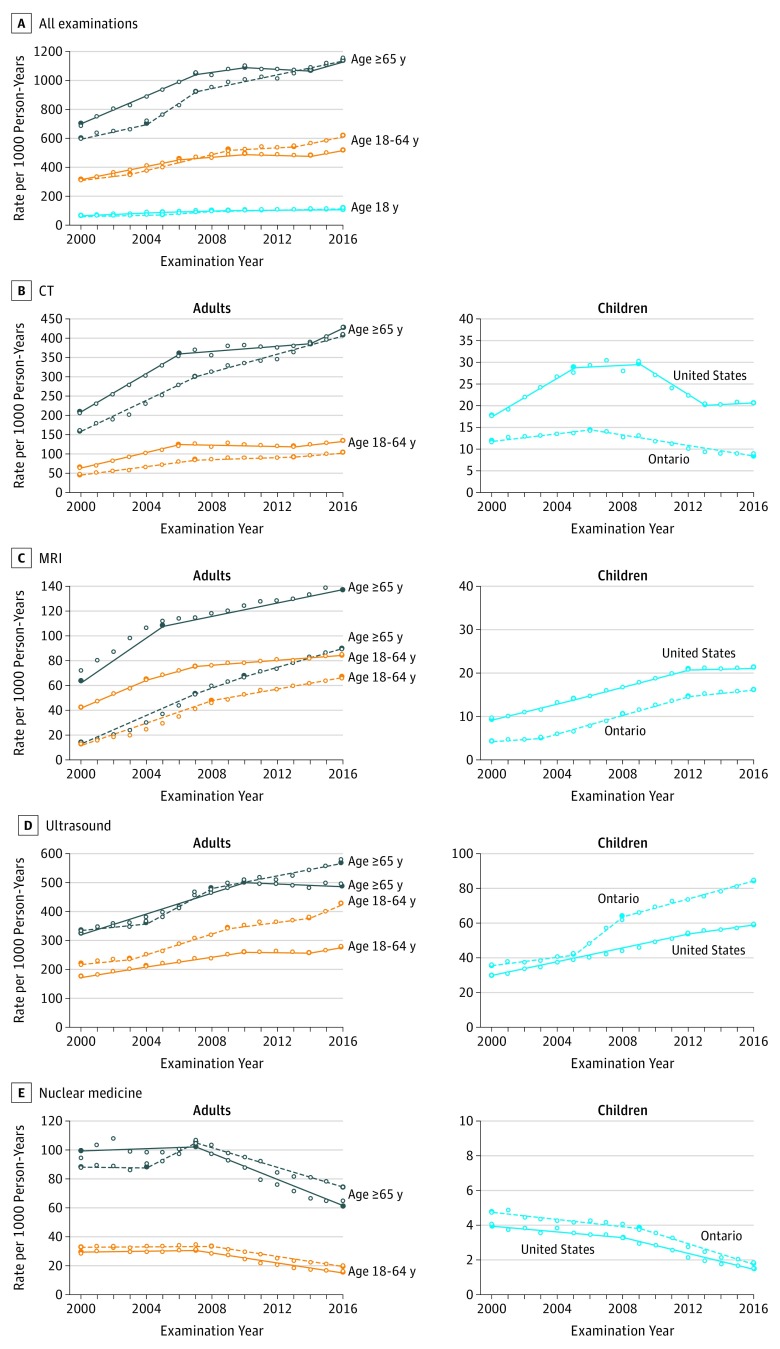
Annual growth in imaging was similar in the US health care systems and Ontario (Figure 1 and eFigure 1 in the Supplement). Imaging rates for CT among adults and older adults increased most rapidly in the early 2000s; in adults, annual growth in CT was 11.6% in the US sites (2000-2006) and 9.2% in Ontario (2000-2007), and in older adults, annual growth was 9.5% in both the United States (2000-2006) and Ontario (2000-2007). Growth during the next period continued at a slower pace or was flat (−0.5% among adults [2006-2013] and 0.9% among older adults [2006-2014] in the United States and 1.3% among adults [2007-2013] and 3.4% among older adults [2007-2016] in Ontario). This was followed by a reacceleration in growth during recent years for most groups (annual growth, 3.7% among adults [2013-2016] and 5.2% among older adults [2014-2016] in the United States and 3.7% among adults in Ontario [2013-2016]) (Figure 1 and eFigure 1).
Figure 1. Annual Change in Imaging Rates per 1000 Person-Years by Imaging Modality, Age, and Country, Based on Joinpoint Analysis.
CT indicates computed tomography; MRI, magnetic resonance imaging. All US data are shown as solid curves; Ontario data are shown as dashed curves. Annual percentage changes with 95% confidence intervals are shown in eFigure 1 in the Supplement.
Patterns of MRI use among adults and older adults in the US health care systems and Ontario were similar to those observed for CT. The greatest annual growth in MRI occurred during the earlier period (11.4% among adults [2000-2004] and 11.3% among older adults [2000-2005] in the United States and 18.5% among adults [2000-2008] and 22% among older adults [2000-2007] in Ontario). There was ongoing but slower annual growth in MRI during the most recent periods (1.3% in adults [2007-2016] and 2.2% in older adults [2005-2016] in the United States and 4.3% in adults [2008-2016] and 4.9% in older adults [2010-2016] in Ontario) (Figure 1 and eFigure 1 in the Supplement).
Ultrasound imaging increased over time, with less variation in annual growth over time across adults and older adults (range, −0.4% to 7.6%) than observed for CT and MRI (Figure 1 and eFigure 1 in the Supplement). The absolute rates of ultrasound imaging were higher than for CT and MRI combined among both adults and older adults. In contrast to the other modalities, nuclear medicine imaging declined consistently after 2008 among adults in Ontario (−6.7% annually) and after 2007 in other groups (annual percentage change, −3.8% to −7.6%) (Figure 1 and eFigure 1).
When all imaging tests were combined, there was significant ongoing growth in imaging in the most recent time interval (annual percentage change, 4.0% in adults and 3.0% in older adults [2014-2016] in the United States and 4.3% in adults [2013-2016] and 3.0% in older adults [2007-2016] in Ontario (Figure 1 and eFigure 1 in the Supplement).
Comparison by Country and Anatomic Area Among Adults
Imaging rates of CT and MRI were higher in US health care systems compared with Ontario, but these differences diminished over time. For example, among older adults, in 2000, CT imaging was 204 per 1000 person-years in the United States and 161 per 1000 person-years in Ontario (relative rate, 1.3; 95% CI, 1.2-1.4), whereas in 2016, it was 428 per 1000 person-years in the United States and 409 per 1000 person-years in Ontario (relative rate, 1.0; 95% CI, 1.0-1.1) (Table 2). Similarly, among older adults, in 2000, MRI use was 62 per 1000 in the United States and 13 per 1000 in Ontario (relative rate, 4.6; 95% CI, 3.8-5.6), whereas in 2016, it was 139 per 1000 person-years in the United States and 89 per 1000 person-years in Ontario (relative rate, 1.6; 95% CI, 1.5-1.7) (Table 2). In contrast, ultrasound and nuclear medicine imaging was the same or lower in the United States, and the difference in relative imaging rates increased over time. In older adults, the relative rate for ultrasound was 1.0 (95% CI, 0.9-1.1) in 2000 and 0.9 (95% CI, 0.8-0.9) in 2016; the relative rate for nuclear medicine was 1.1 (95% CI, 1.0-1.2) in 2000 and 0.9 (95% CI, 0.8-0.9) in 2016.
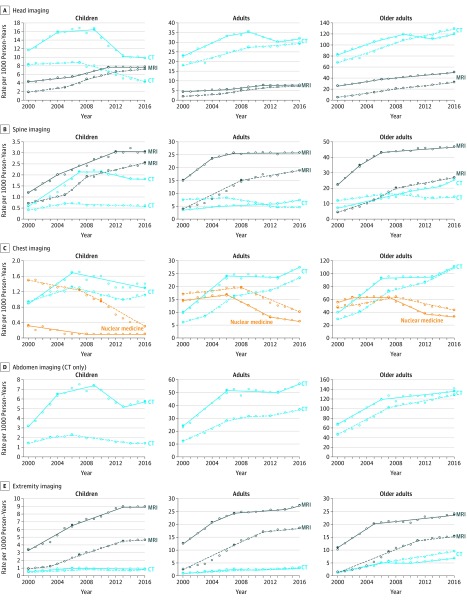
Imaging rates within anatomic areas were similar to the overall results; CT, MRI, and ultrasound increased and nuclear medicine declined over time (Figure 2). In 2016, in most anatomic areas imaged with CT or MRI, imaging rates were higher in the United States compared with Ontario (Table 3). For example, in 2016, the relative rate for the United States vs Ontario for MRI of the spine was 1.36 (95% CI, 1.23-1.59) in adults and 1.75 (95% CI, 1.59-1.91) in older adults.
Figure 2. Imaging Rates per 1000 Person-Years by Anatomic Area, Imaging Modality, Age, and Country, Based on Joinpoint Analysis.
CT indicates computed tomography; MRI, magnetic resonance imaging. All US data are shown as solid curves; Ontario data are shown as dashed curves. Children are aged <18 years; adults, 18 to 64 years, and older adults, ≥65 years. See Table 3 for relative rates of imaging for United States compared with Ontario.
Table 3. Relative Rates of Imaging for United States vs Ontario by Age and Anatomic Area in 2016.
| Anatomic Area | Relative Rate (95% CI) | ||
|---|---|---|---|
| Older Adults (Aged ≥65 y) | Adults (Aged 18-64 y) | Children (Aged <18 y) | |
| Head | |||
| Computed tomography | 0.94 (0.90-0.97) | 1.07 (1.01-1.14) | 2.14 (1.95-2.35) |
| Magnetic resonance imaging | 1.58 (1.45-1.72) | 1.21 (1.12-1.30) | 1.08 (1.00-1.16) |
| Spine | |||
| Computed tomography | 1.81 (1.51-2.17) | 1.63 (1.25-2.12) | 2.96 (2.60-3.36) |
| Magnetic resonance imaging | 1.75 (1.59-1.91) | 1.36 (1.23-1.50) | 1.22 (1.09-1.35) |
| Chest | |||
| Computed tomography | 1.02 (0.98-1.07) | 1.17 (1.10-1.24) | 1.32 (1.19-1.48) |
| Nuclear medicine | 0.77 (0.69-0.86) | 0.63 (0.56-0.70) | 0.25 (0.15-0.40) |
| Abdomen | |||
| Computed tomography | 1.09 (1.04-1.15) | 1.56 (1.45-1.67) | 4.06 (3.59-4.59) |
| Extremity | |||
| Computed tomography | 0.73 (0.66-0.80) | 0.92 (0.84-1.01) | 1.22 (1.08-1.37) |
| Magnetic resonance imaging | 1.59 (1.45-1.75) | 1.47 (1.34-1.61) | 1.96 (1.76-2.18) |
The average annual percentage changes in imaging within fixed time periods stratified by anatomic area are shown in Table 4. These results stratified by anatomic area are similar to the overall results; the largest growth occurred between 2000 and 2005, more modest growth between 2006 and 2011, and ongoing or reacceleration of growth between 2012 and 2016. For example, between 2000 and 2005, annual growth in CT overall among adults aged 18 to 64 years was 11.6% in the United States and 9.2% in Ontario; for specific anatomic areas, it was 13.6% and 14.8% for CT of the abdomen, 15.8% and 14.1% for CT of the chest, 6.4% and 4.8% for CT of the head, and 7.4% and 1.7% for CT of the spine in the United States and Ontario, respectively. Annual growth rates among adults aged 18 to 64 years declined (in the United States) or were lower than earlier (in Ontario) between 2006 and 2011, and for CT overall and in nearly all anatomic areas, there was ongoing growth or reacceleration of growth from 2012 to 2016, with a single exception. Between 2012 and 2016, annual growth in CT overall imaging among adults aged 18 to 64 years was 2.6% in the United States and 3.4% in Ontario; for specific anatomic areas, it was 3.0% and 3.6% for CT of the abdomen, 3.9% and 6.1% for CT of the chest, 0.4% and 1.0% for CT of the head, and 5.8% and −2.7% for CT of the spine in the United States and Ontario, respectively. The same pattern was observed for MRI: between 2012 and 2016, in adults, there was ongoing growth in MRI overall (1.3% in the United States and 4.3% in Ontario), MRI of the head (1.2% in the United States and 4.2% in Ontario), and MRI of the spine in Ontario (2.9%; with no growth in MRI of the spine in the United States).
Table 4. Average Annual Percentage Changes in Imaging Rates by Age, Country, and Anatomic Area.
| Average Annual Change From Prior Period, % (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Older Adults (Aged ≥65 y) | Adults (Aged 18-64 y) | Children (Aged <18 y) | ||||
| United States | Ontario | United States | Ontario | United States | Ontario | |
| Computed Tomography | ||||||
| Overall | ||||||
| 2000-2005 | 9.5 (8.2 to 10.8) | 9.5 (8.5 to 10.6) | 11.6 (9.7 to 13.5) | 9.2 (8.2 to 10.3) | 10.1 (7.8 to 12.5) | 3.3 (1.2 to 5.4) |
| 2006-2011 | 0.9 (0.2 to 1.6) | 4.6 (4.2 to 5.0) | −0.5. (−1.8 to 0.8) | 2.9 (1.9 to 3.8) | −3.4 (−5.7 to −1.0) | −5.3 (−6.2 to −4.3) |
| 2012-2016 | 3.0 (1.1 to 4.9) | 3.4 (3.0 to 3.9) | 2.6 (0.2 to 5.1) | 3.4 (1.6 to 5.3) | −1.8 (−4.5 to 1.1) | −5.3 (−6.2 to −4.3) |
| Abdomen | ||||||
| 2000-2005 | 9.9 (7.7 to 12.1) | 11.9 (10.8 to 12.9) | 13.6 (10.8 to 16.3) | 14.8 (13.4 to 16.2) | 16.1 (11.8 to 20.6) | 9.1 (5.5 to 12.8) |
| 2006-2011 | 1.3 (0.7 to 2.0) | 4.4 (4.0 to 4.7) | −0.4 (−2.2 to 1.4) | 2.4 (−0.6 to 5.6) | −2.0 (−5.2 to 1.3) | −5.8 (−6.9 to −4.8) |
| 2012-2016 | 1.3 (0.7 to 2.0) | 2.6 (2.1 to 3.0) | 3.0 (−0.3 to 6.5) | 3.6 (2.1 to 5.2) | 0.3 (−4.1 to 4.9) | −3.0 (−5.7 to −0.3) |
| Chest | ||||||
| 2000-2005 | 15.9 (12.8 to 19.0) | 13.3 (11.2 to 15.4) | 15.8 (13.6 to 18.0) | 14.1 (12.1 to 16.2) | 11.3 (6.7 to 16.1) | 5.8 (3.9 to 7.8) |
| 2006-2011 | 0.3− (−0.5 to 1.2) | 5.8 (4.9 to 6.8) | −0.3 (−1.6 to 1.0) | 5.4 (4.5 to 6.4) | −2.7 (−3.8 to −1.5) | −4.0 (−5.6 to −2.4) |
| 2012-2016 | 4.1 (2.8 to 5.3) | 6.0 (4.9 to 7.0) | 3.9 (1.4 to 6.4) | 6.1 (4.9 to 7.3) | −2.7 (−3.8 to −1.5) | 1.9 (−1.7 to 5.6) |
| Head | ||||||
| 2000-2005 | 5.1 (3.9 to 6.3) | 5.4 (4.8 to 5.9) | 6.4 (5.5 to 7.3) | 4.8 (4.0 to 5.6) | 6.6 (4.2 to 9.1) | 0.7 (−1.0 to 2.4) |
| 2006-2011 | 1.1 (−0.1 to 2.4) | 4.2 (3.9 to 4.6) | −0.4 (−2.5 to 1.8) | 3.2 (2.7 to 3.8) | −4.2 (−6.4 to −2.0) | −6.0 (−6.9 to −5.1) |
| 2012-2016 | 1.5 (0.3 to 2.6) | 2.5 (1.9 to 3.1) | 0.4 (−0.8 to 1.7) | 1.0 (0.1 to 1.9) | −3.9 (−7.5 to −0.1) | −7.6 (−8.8 to −6.4) |
| Spine | ||||||
| 2000-2005 | 9.9 (8.8 to 10.9) | 4.9 (3.0 to 6.7) | 7.4 (4.9 to 9.8) | 1.7 (0.4 to 3.1) | 20.5 (19.2 to 21.9) | 11.4 (8.8 to 14.0) |
| 2006-2011 | 8.6 (7.7 to 9.6) | −1.7 (−3.5 to 0.1) | 2.4 (1.3 to 3.6) | −7.2 (−9.8 to −4.6) | 3.0 (0.5 to 5.53.5) | −1.6 (−2.7 to −0.6) |
| 2012-2016 | 6.8 (3.7 to 9.9) | 0.4 (−3.0 to 3.9) | 5.8 (3.4 to 8.2) | −2.7 (−6.1 to 0.9) | −2.1 (−4.7 to 0.4) | −1.6 (−2.7 to −0.6) |
| Magnetic Resonance Imaging | ||||||
| Overall | ||||||
| 2000-2005 | 11.3 (10.1 to 12.5) | 22 (20.6 to 23.4) | 10.1 (8.9 to 11.3) | 18.5 (17.3 to 19.8) | 8.7 (7.2 to 10.3) | 9.9 (8.5 to 11.4) |
| 2006-2011 | 2.2 (2.0 to 2.4) | 10.1 (7.3 to 12.9) | 2.1 (1.4 to 2.7) | 9.8 (9.2 to 10.3) | 5.9 (5.0 to 6.8) | 11.8 (10.9 to 12.7) |
| 2012-2016 | 2.2 (2.0 to 2.4) | 4.9 (4.2 to 5.6) | 1.3 (1.0 to 1.6) | 4.3 (3.7 to 5.0) | 0.5 (−1.0 to 1.9) | 2.5 (1.6 to 3.4) |
| Head | ||||||
| 2000-2005 | 6.6 (5.4 to 7.8) | 23.1 (20.5 to 25.7) | 6.9 (6.0 to 7.8) | 13.4 (12.6 to 14.1) | 3.9 (2.6 to 5.3) | 9.7 (8.0 to 11.4) |
| 2006-2011 | 3.0 (2.6 to 3.4) | 8.7 (6.6 to 11.0) | 2.5 (1.6 to 3.3) | 7.8 (7.4 to 8.2) | 7.1 (5.2 to 9.1) | 11.8 (9.2 to 14.5) |
| 2012-2016 | 3.0 (2.6 to 3.4) | 5.8 (5.3 to 6.3) | 1.2 (0.8 to 1.6) | 4.2 (3.7 to 4.7) | 0.1 (−1.1 to 1.3) | 2.2 (0.7 to 3.8) |
| Spine | ||||||
| 2000-2005 | 12.5 (10.1 to 15.0) | 22.8 (19.8 to 25.8) | 10.0 (8.7 to 11.3) | 18.5 (16.9 to 20.0) | 12.0 (9.1 to 15.0) | 9.1 (4.9 to 13.6) |
| 2006-2011 | 0.8 (0.5 to 1.1) | 9.1 (6.6 to 11.8) | 0.6 (−0.1 to 1.3) | 8.9 (8.2 to 9.5) | 5.4 (3.5 to 7.4) | 10.2 (6.2 to 14.3) |
| 2012-2016 | 0.8 (0.5 to 1.1) | 3.7 (3.2 to 4.3) | 0.0 (−0.3 to 0.3) | 2.9 (2.1 to 3.7) | −0.1 (−3.7 to 3.7) | 3.5 (2.7 to 4.4) |
| Ultrasound | ||||||
| Overall | ||||||
| 2000-2005 | 4.5 (4.0 to 5.0) | 2.9 (1.1 to 4.8) | 4.6 (3.6 to 5.7) | 4.1 (2.6 to 5.5) | 5.0 (4.8 to 5.3) | 3.4 (2.1 to 4.6) |
| 2006-2011 | 3.5 (3.1 to 3.9) | 4.2 (3.0 to 5.5) | 2.8 (2.1 to 3.5 | 4.6 (4.0 to 5.3) | 5.0 (4.8 to 5.3) | 8.0 (6.3 to 9.7) |
| 2012-2016 | −0.4 (−1.2 to 0.4) | 2.1 (1.5 to 2.7) | 1.8 (0.2 to 3.4) | 4.1 (2.4 to 5.8) | 2.2 (1.2 to 3.3) | 3.5 (3.1 to 4.0) |
| Nuclear Medicine | ||||||
| Overall | ||||||
| 2000-2005 | 0.4 (−1.1 to 2.0) | 1.1 (−0.6 to 2.9) | 0.5 (−1.0 to −2.0) | 0.3 (−0.2 to 0.9) | −2.3 (−3.4 to −1.1) | −2.3 (−3.1 to −1.6) |
| 2006-2011 | −4.5 (−5.1 to −3.6) | −1.9 (−2.9 to −0.8) | −6.0 (−6.8 to −5.2) | −3.9 (−4.3 to −3.6) | −5.7 (−7.4 to −6.0) | −5.7 (−6.3 to −5.0) |
| 2012-2016 | −5.5 (−6.5 to −4.6) | −3.8 (−4.3 to −3.3) | −7.6 (−8.6 to −6.5) | −6.7 (−7.3 to −6.1) | −10.1 (−10.7 to −8.4) | −10.5 (−11.9 to −9.1) |
Children
Annual imaging rates in children by modality and country are shown in Table 2. Imaging rates were higher in 2016 than in 2000 for CT, MRI, and ultrasound, with a single exception: CT imaging in Ontario was lower in 2016 than in 2000. In the United States, CT increased from 18 to 22 per 1000 person-years (relative rate, 1.2; 95% CI, 1.1-1.3), MRI increased from 9 to 21 per 1000 person-years (relative rate, 2.3; 95% CI, 2.0-2.5), and ultrasound increased from 30 to 59 per 1000 person-years (relative rate, 2.0; 95% CI, 1.8-2.2). In Ontario, CT declined from 12 to 9 per 1000 person-years (relative rate, 0.8; 95% CI, 0.7-0.8), MRI increased from 4 to 16 per 1000 person-years (relative rate, 4.0; 95% CI, 3.6-4.3), and ultrasound increased from 36 to 85 per 1000 person-years (relative rate, 2.4; 95% CI, 2.3-2.5).
Imaging Rates Among Children by Joinpoint Analysis
Imaging trends in children were similar to adults, with the notable exception of a recent decline in CT. For CT, imaging rates increased most rapidly in the early 2000s; the annual percentage change in CT was 10.1% in the United States (2000-2005) and 3.3% in Ontario (2000-2006). In the United States, CT imaging during the next period continued at a slower pace (0.7% annual growth between 2005 and 2009), followed by a large reduction in imaging (−9.1% annual growth), followed by relative stable imaging after 2013 (0.8% annual growth; 95% CI, −3.6% to 5.5%) (Figure 1 and eFigure 1 in the Supplement). In Ontario, CT imaging in children declined consistently after 2006 (−5.3% annual growth). During all periods, CT imaging in children was higher in the United States.
Use of MRI had a similar pattern in children and adults: more rapid increase in imaging use during the earlier periods with ongoing but more modest growth after 2012. In the United States, annual growth in MRI in children was 8.7% (2000-2005), 5.9% (2005-2012), and 0.5% (2012-2016); annual growth in Ontario was 5.9% (2000-2003), 16.3% (2003-2008), 8.9% (2008-2012), and 2.5% (2012-2016) (Figure 1 and eFigure 1 in the Supplement). Ultrasound use in children increased over time in both the United States and Ontario. Although the growth in ultrasound was slower than observed for CT or MRI, the absolute rates of ultrasound imaging were higher than for CT and MRI combined (Figure 1 and eFigure 1). Nuclear medicine declined over the entire observed time period, but declines were largest after 2009 in the United States (−10.5%) and after 2008 in Ontario (−9.6%).
When rates of CT, MRI, ultrasound, and nuclear medicine imaging were combined, there was significant ongoing growth in imaging in children in the most recent time interval (Figure 1 and eFigure 1). Annual growth was 0.8% in the United States and 2.4% in Ontario.
Comparison by Country and Anatomic Area Among Children
Rates of CT and MRI were higher in US health care systems compared with Ontario. The differences increased over time for CT and diminished over time for MRI. Among children in 2000, CT imaging was 18 per 1000 person-years in the United States and 12 per 1000 person-years in Ontario (relative rate, 1.5; 95% CI, 1.4-1.7), whereas in 2016 it was 22 per 1000 person-years in the United States and 9 per 1000 person-years in Ontario (relative rate, 2.3; 95% CI, 2.1-2.5) (Table 2). The larger difference in CT utilization between countries in 2016 reflects both the increase in the United States and the decrease in Ontario in the absolute rate of CT imaging.
The larger differences in CT imaging between the United States and Ontario in recent years are reflected in results stratified by anatomic area (Figure 2 and Table 3). In 2016, relative imaging rates for specific anatomic areas were as follows: for CT of the head, relative rate, 2.14 (95% CI, 1.95-2.35; 9.8 per 1000 person-years in the United States vs 4.6 per 1000 person-years in Ontario); for CT of the spine, relative rate, 2.96 (95% CI, 2.60-3.36; 1.8 per 1000 person-years in the United States vs 0.6 per 1000 person-years in Ontario); for CT of the chest, relative rate, 1.32 (95% CI, 1.19-1.48; 1.3 per 1000 person-years in the United States vs 1.1 per 1000 person-years in Ontario); for CT of the abdomen, relative rate, 4.06 (95% CI, 3.59-4.59; 5.6 per 1000 person-years in the United States vs 1.4 per 1000 person-years in Ontario); and for CT of the extremities, relative rate, 1.22 (95% CI, 1.08-1.37; 0.9 per 1000 person-years in the United States vs 0.8 per 1000 person-years in Ontario).
The average annual percentage change in imaging within fixed time periods and by anatomic area are shown in Table 4. For CT overall, growth was positive between 2000 and 2006 (10.1% annual growth in the United States and 3.3% annual growth in Ontario); in the subsequent time intervals, CT use declined (−3.4% in the United States and −5.3% in Ontario between 2006 and 2011; −1.8% and −5.3%, respectively, between 2012 and 2016). The patterns were similar by anatomic area, with declines or no change between 2006 and 2016, except for spine imaging in the United States. Use of MRI in each anatomic area increased in Ontario between 2012 and 2016 (overall annual growth, 2.5%; head, 2.2%; spine, 3.5%), whereas in the United States there was no significant growth during this period.
Variation Across Health Care Systems
Absolute imaging rates varied across US health care systems, but patterns over time were similar across systems: CT and ultrasound increased, nuclear medicine decreased, and all but 1 health care system showed increasing MRI use over time (eFigure 2 in the Supplement). Site-specific imaging rates for hospitals and imaging centers in Ontario were not available. Imaging rates in Ontario for CT and MRI were near or below those at the US site with the lowest rates, whereas for ultrasound and nuclear medicine, rates were near or below those at the US site with the highest rates.
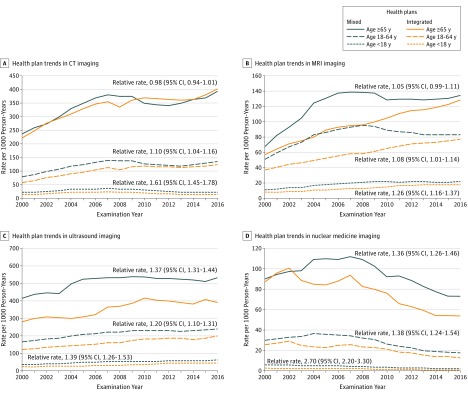
Imaging rates for CT, MRI, ultrasound, and nuclear medicine by type of US health care system insurance model (mixed-model vs fully integrated) are shown in Figure 3. Among older adults, there were no significant differences in imaging rates for CT or MRI by type of plan. However, rates were slightly higher for mixed-model plans among adults. Specifically, in 2016, imaging rates for CT in mixed compared with integrated plans were 392 vs 401 per 1000 person-years in older adults (relative rate, 0.98; 95% CI, 0.94-1.01) and 136 vs 124 per 1000 person-years in adults (relative rate, 1.10; 95% CI, 1.04-1.16). For MRI, rates were 135 vs 129 per 1000 person-years in older adults (relative rate, 1.05; 95% CI, 0.99-1.11) and 83 vs 77 per 1000 person-years in adults (relative rate, 1.08; 95% CI. 1.01-1.14). Relative imaging rates were higher among the mixed-model health care plans for ultrasound in older adults (536 vs 390 per 1000 person-years; relative rate, 1.37; 95% CI, 1.31-1.44) and in adults (240 vs 201 per 1000 person-years; relative rate, 1.20; 95% CI, 1.10-1.31) and for nuclear medicine in older adults (73 vs 54 per 1000 person-years; relative rate, 1.36; 95% CI, 1.26-1.46) and in adults (18 vs 13 per 1000 person-years; relative rate, 1.38; 95% CI, 1.24-1.54). For children, imaging rates were significantly higher in the mixed-model plans for CT (23.5 vs 14.6 per 1000 person-years; relative rate, 1.61; 95% CI, 1.45-1.78), MRI (22.2 vs 17.6 per 1000 person-years; relative rate, 1.26; 95% CI, 1.16-1.37), ultrasound (63.3 vs 45.6 per 1000 person-years; relative rate, 1.39; 95% CI, 1.26-1.53), and nuclear medicine (2.0 vs 0.8 per 1000 person-years; relative rate, 2.70; 95% CI, 2.20-3.30).
Figure 3. Imaging Rates per 1000 Person-Years by Imaging Modality, Stratified by Type of US Health Care System.
CT indicates computed tomography; MRI, magnetic resonance imaging. Relative rates are for 2016.
Discussion
Use of CT, MRI, and ultrasound in 7 US integrated health care systems and in Ontario has continued to increase in recent years. Annual growth in CT, MRI, and ultrasound was highest in the earlier years (ie, between 2000 and 2006), but utilization continued to rise between 2012 and 2016 (1%-5% annually) for most age groups both in the US sites and in Ontario. The notable exception is for pediatric CT (<18 years old), which has declined since 2006. In contrast, nuclear medicine imaging demonstrated a consistent decline in every age category and health care system.
These results differ from some reports that suggest recent declines in imaging.10,23,24,25 Differences could be due to how imaging examinations were counted, as the results presented in this study focus on utilization of tests rather than payer costs. These results reflect imaging across all age groups, while several prior studies focused on Medicare patients. Nonetheless, even among adults aged 65 years or older, the results presented show ongoing annual growth in CT and MRI use of 2.2% to 4.9% in the US sites and Ontario. A recent increase in imaging was also noted in a study of a privately insured population, which showed imaging utilization starting to rise in 2011 after a downturn in 2010.24 Declines in CT, MRI, and ultrasound have been described in widely cited market research reports,23 but no details are available regarding sampling of facilities or counting of examinations, thus preventing a direct comparison with the current study results.
Imaging use was significantly greater in mixed-model compared with fully integrated HMO health care plans in children and adults for all imaging modalities and for older adults for ultrasound and nuclear medicine but not for CT or MRI. This may suggest that imaging rates are lower within systems that have stronger incentives to constrain imaging (and cost). However, these differences were not seen to the same degree in older adults. This result must be considered with caution, as this study included a limited sample of health care plans of each type and could control for only a limited number of possible confounding variables.
Ideally, use of any health care service should be guided by a balanced consideration of benefits and harms, yet for imaging, few relevant data quantifying either are available. Although guidelines have been developed for imaging, they are primarily based on expert opinion rather than evidence26,27 and have not been shown to reduce imaging.28 Imaging examinations are frequently adopted into clinical practice before evidence supports their use, and once incorporated into practice, withdrawing their use is difficult. Thus, it is not surprising that imaging rates have not declined substantially despite multiple policy and clinical efforts focused on reducing imaging use. In addition, what is acceptable clinical practice changes over time. For example, in the past, for children with suspected appendicitis, it was acceptable to have both false-positive and false-negative surgical rates of 10%. Use of ultrasound and CT have lowered those rates to less than 5%.
Public health concerns about radiation exposure from medical imaging have intensified with publicity regarding the rapid increase in imaging utilization. The focus is primarily on CT because of the relatively high ionizing radiation exposure per examination and large numbers of individuals exposed.29 Adults and children are sensitive to radiation.30,31,32,33 In adults, CT use continued to rise, albeit more slowly than seen previously. The decline of CT in children and greater increase in MRI may reflect greater awareness of the concern regarding radiation exposure and harm in children. The less frequent CT use in adults in Ontario may reflect greater awareness of issues of ionizing radiation exposure in adults.
This study has several strengths, including its large size, inclusion of imaging data from 7 US sites and from Ontario, inclusion of all age groups, and accurate assessment of utilization, including examinations conducted outside health care plans with reimbursement claims. Imaging data were mapped across settings, modalities, and anatomic areas to prevent examination double counting and influences from changes in billing practices over time.
Limitations
This study has several limitations. First, the study was limited by including US patients enrolled in a limited number of health care systems, all of which used HMO models of care either in part or in total. Patterns of imaging over time among these patients may not represent patterns among individuals covered by fee-for-service plans with different incentives and disincentives. Second, the indication for imaging was not available; thus, it is not possible to determine whether imaging was appropriate or inappropriate for any given test or whether imaging utilization was associated with improved patient outcomes. Third, because of differences in billing practices, it was not possible to accurately estimate anatomic areas imaged with ultrasound or to make detailed comparisons between the United States and Ontario that accounted for imaging during pregnancy. It is possible that the greater use of ultrasound in Canada reflects its more frequent use in pregnancy; however, this would only affect and explain imaging in adults and not imaging in children and older adults. Fourth, in Canada, imaging was assessed only in the province of Ontario. Although Ontario is Canada’s largest province, it may not reflect practices in other provinces or territories. Fifth, by using electronic health record data, the majority of imaging was most likely captured, but if examinations were conducted outside of the health care system and the primary insurer was not billed, there may be missing data on imaging utilization.
Conclusions
From 2000 to 2016 in 7 US integrated and mixed-model health care systems and in Ontario, rates of CT and MRI use continued to increase among adults, but at a slower pace in more recent years. In children, imaging rates continued to increase except for CT, which stabilized or declined in more recent periods. Whether the observed imaging utilization was appropriate or was associated with improved patient outcomes is unknown.
eFigure 1. Annual Change in Imaging Rates per 1000 Person-Years by Modality, Age, and Country Based on Joinpoint Analysis Showing the Annual Percent Change in Each Segment and 95% Confidence Intervals Around These Rates
eFigure 2. Imaging Rates per 1000 Persons by Modality, Age, Country and Individual Healthcare System
References
- 1.Government Accountability Office Report to congressional requesters: Medicare Part B imaging services: rapid spending growth and shift to physician offices indicated need for CMS to consider additional management practices [GAO-08-452]. https://www.gao.gov/new.items/d08452.pdf. Accessed June 3, 2019.
- 2.Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307(22):2400-2409. doi: 10.1001/jama.2012.5960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iglehart JK. Health insurers and medical-imaging policy—a work in progress. N Engl J Med. 2009;360(10):1030-1037. doi: 10.1056/NEJMhpr0808703 [DOI] [PubMed] [Google Scholar]
- 4.Winter A, Stensland J Introduction: expert panel on new research on use of imaging services [presentation to Medicare Payment Advisory Commission]. September 5, 2008. http://67.59.137.244/transcripts/imaging%20expert%20panel_Sept%2008_public.pdf. Accessed June 3, 2019.
- 5.Institute of Medicine Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: Institute of Medicine; September 6, 2012. [DOI] [PubMed] [Google Scholar]
- 6.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024-1039. doi: 10.1001/jama.2018.1150 [DOI] [PubMed] [Google Scholar]
- 7.Choosing Wisely: an initiative of the American Board of Internal Medicine Foundation. http://www.choosingwisely.org/. Accessed June 3, 2019.
- 8.Deficit Reduction Act of 2005, S 1932, 109th Cong. Pub L No. 109-171 §5102. https://www.congress.gov/bill/109th-congress/senate-bill/1932. Accessed August 7, 2019.
- 9.Protecting Access to Medicare Act of 2014, HR 4302, 113th Cong. Pub L No. 113-93. https://www.congress.gov/bill/113th-congress/house-bill/4302. Accessed August 2, 2019.
- 10.Levin DC, Parker L, Palit CD, Rao VM. After nearly a decade of rapid growth, use and complexity of imaging declined, 2008-14. Health Aff (Millwood). 2017;36(4):663-670. doi: 10.1377/hlthaff.2016.0836 [DOI] [PubMed] [Google Scholar]
- 11.Levin DC, Parker L, Rao VM. The recent losses in Medicare imaging revenues experienced by radiologists, cardiologists, and other physicians. J Am Coll Radiol. 2017;14(8):1007-1012. doi: 10.1016/j.jacr.2017.02.044 [DOI] [PubMed] [Google Scholar]
- 12.Ross TR, Ng D, Brown JS, et al. The HMO Research Network virtual data warehouse: a public data model to support collaboration. EGEMS (Wash DC). 2014;2(1):1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner EH, Greene SM, Hart G, et al. Building a research consortium of large health systems: the Cancer Research Network. J Natl Cancer Inst Monogr. 2005;(35):3-11. doi: 10.1093/jncimonographs/lgi032 [DOI] [PubMed] [Google Scholar]
- 14.Chubak J, Ziebell R, Greenlee RT, et al. The Cancer Research Network: a platform for epidemiologic and health services research on cancer prevention, care, and outcomes in large, stable populations. Cancer Causes Control. 2016;27(11):1315-1323. doi: 10.1007/s10552-016-0808-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirschner CG, Coy JA, Edwards NK, et al. CPT 1993: Physicians’ Current Procedural Terminology. Chicago, IL: American Medical Association; 1993. [Google Scholar]
- 16.World Health Organization International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Geneva, Switzerland: World Health Organization; 1977. [Google Scholar]
- 17.American Medical Association ICD-10-CM 2018: The Complete Official Codebook. Chicago, IL: American Medical Association; 2017. [Google Scholar]
- 18.American Medical Association HCPCS Level II 2018 Professional Edition. Chicago, IL: American Medical Association; 2018. [Google Scholar]
- 19.Canadian Classification of Health Interventions Volume 3 Ottawa, ON: Canadian Institute for Health Information; 2012.
- 20.Kim HJ, Luo J, Kim J, Chen HS, Feuer EJ. Clustering of trend data using Joinpoint regression models. Stat Med. 2014;33(23):4087-4103. doi: 10.1002/sim.6221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 22.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626-633. doi: 10.1097/MLR.0b013e31819432e5 [DOI] [PubMed] [Google Scholar]
- 23.IMV Medical Information Division 2018 CT Benchmark Report. Des Plaines, IL: IMV; 2017. [Google Scholar]
- 24.Horný M, Burgess JF Jr, Horwitt J, Cohen AB. Advanced diagnostic imaging in privately insured patients: recent trends in utilization and payments. J Am Coll Radiol. 2014;11(7):692-697. doi: 10.1016/j.jacr.2014.01.019 [DOI] [PubMed] [Google Scholar]
- 25.Raja AS, Ip IK, Sodickson AD, et al. Radiology utilization in the emergency department: trends of the past 2 decades. AJR Am J Roentgenol. 2014;203(2):355-360. doi: 10.2214/AJR.13.11892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith-Bindman R, Bindman AB. Imaging more wisely—already at work [letter reply]. JAMA Intern Med. 2016;176(6):870-871. doi: 10.1001/jamainternmed.2016.2075 [DOI] [PubMed] [Google Scholar]
- 27.Smith-Bindman R, Bindman AB. Imaging more wisely. JAMA Intern Med. 2016;176(2):168-170. doi: 10.1001/jamainternmed.2015.7113 [DOI] [PubMed] [Google Scholar]
- 28.Centers for Medicare & Medicaid Services Medicare imaging demonstration evaluation report to Congress. November 5, 2014. https://innovation.cms.gov/Files/reports/MedicareImagingDemoRTC.pdf. Accessed August 5, 2019.
- 29.Smith-Bindman R. Is computed tomography safe? N Engl J Med. 2010;363(1):1-4. doi: 10.1056/NEJMp1002530 [DOI] [PubMed] [Google Scholar]
- 30.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499-505. doi: 10.1016/S0140-6736(12)60815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Preston DL, Ron E, Tokuoka S, et al. Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat Res. 2007;168(1):1-64. doi: 10.1667/RR0763.1 [DOI] [PubMed] [Google Scholar]
- 32.Board of Radiation Effects Research, Division on Earth and Life Sciences, National Research Council of the National Academies Health Risks From Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 33.Shuryak I, Sachs RK, Brenner DJ. Cancer risks after radiation exposure in middle age. J Natl Cancer Inst. 2010;102(21):1628-1636. doi: 10.1093/jnci/djq346 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Annual Change in Imaging Rates per 1000 Person-Years by Modality, Age, and Country Based on Joinpoint Analysis Showing the Annual Percent Change in Each Segment and 95% Confidence Intervals Around These Rates
eFigure 2. Imaging Rates per 1000 Persons by Modality, Age, Country and Individual Healthcare System