Abstract
Background:
Urinary incontinence (UI) is defined as any involuntary urine loss that predominantly affects older women. There is evidence that pelvic floor muscles training (PFMT) program is effective on the treatment of pelvic floor (PF) dysfunctions and is considered to be first-line treatment. The evaluation of pelvic floor muscles (PFM) function and strength is central to validate the effectiveness of the training protocol in UI decrease. The Oxford Grading Scale and manometry are fundamental to evaluate the PFM function and strength.
Objective:
The aim of the study was to systematize the scientific evidence about the effects of PFMT in older women, assessing the PF function and strength through Oxford Grading Scale and manometry.
Methods:
The research of randomized controlled clinical trials was performed through B-on, EBSCO, PEDro, Pubmed, and SciELO data carried out from 2003 to 2016.
Results:
A total of 35 studies were identified, 26 of these were selected and fully analyzed. From the analyzed studies (n = 26), 20 were excluded for not meeting the criteria for inclusion, and only 6 studies were classified as high methodological quality, scoring an overall 4 points according the PEDro scale.
Conclusion:
The PFMT seems to be effective in treating UI in older women; the Oxford Grading Scale and manometry are considered the most reliable in the random and controlled clinical trials results. However, future investigations with high methodological quality with older women are necessary to support these results.
Keywords: older, manometry, Oxford Grading Scale, pelvic floor muscles training, urinary incontinence
Introduction
Urinary incontinence (UI), according to the International Continence Society (ICS), is defined as a condition of any involuntary loss of urine.1,2 Although not considered a cause of morbidity or mortality, UI has a serious negative impact on aspects of the social, emotional, and well-being life of the population, and may even result in depression, isolation, and physical inactivity, affecting the health-related quality of life.3,6–12
The prevalence of UI increases with age; it is estimated that 20% to 40% of the older women present involuntary loss of urine.13,14 Stress urinary incontinence (SUI) is the most common type of UI in women; this type of voluntary urinary loss occurs during coughing, sneezing, and exertion.3,9,10
In the pathophysiology of UI, several risk factors such as increased age, obesity, pregnancy, menopause, pelvic surgeries, postmenopausal estrogen deficiency, and collagen fibers decrease. These are the causes of the weakening of the pelvic floor muscles (PFM).9,15 The atrophic changes that occur with aging of PFM through endocrine, enzymatic, neural, and energetic alterations are possibly genetically driven, resulting in the reduction of muscle mass by degradation and its replacement by adipocytes, contributing to the weakening of the pelvic floor (PF).15,16 Studies have shown with advancing age the functional and anatomical deterioration of PFM striated muscles could be at the origin of UI.17,18 Exercise practice seems to contribute to a better PF function, as reported in Ree et al study, arguing that physical exercise potentiates the volume of PFM making them more capable of contraction during abdominal pressure.7,19
Sherburn et al15 reported that with advancing age the maximum urethral closure pressure and the number of periurethral fibers decreased, being a risk factor for UI development, due to changes in PF structures and their response to increase in intra-abdominal pressure.
Some studies have shown that the pelvic floor muscles training (PFMT) is highly effective in the treatment of PF dysfunctions, and it is considered a first-line therapy, covering 56% to 75% success rates in the treatment of SUI and mixed urinary incontinence (MUI).9–11,20,21
The PFMT is based on 3 primary objectives: strengthen PFM, improves the mechanism that allows urethral closure, and inhibits the reflex contraction of the detrusor muscle in the MUI.5 According to some authors, as reported in Bernards et al,9 Bø,22 and Hay-Smith et al,23 the PFMT is based particularly on the increase of force (maximum force generated by a muscle in a single contraction); endurance (ability of continuous contractions or maintain muscle contraction over a longer period of time); and coordination of muscle activity (precontraction of PFM anticipating an increase in intra-abdominal pressure), adherence, and motivation to the treatment program.
Evaluation of PFM's function and strength is fundamental to instruct and obtain feedback regarding the participant's ability to contract PFM's, as well as to evaluate changes in the parameters in question. The intervention program aims to verify the effectiveness of the protocol. There are several methods of evaluating PFM function such as digital palpation, manometry, ultrasound, electromyography, and magnetic resonance imaging.10 However, according to the International Association of Urogynecological (IUGA) and ICS, it recommends the evaluation of voluntary contraction and relaxation of PFM through digital palpation and manometry.4,10 Digital palpation is considered a simple, inexpensive method, golden-standard, and mostly used in the evaluation of PFM contraction capacity. Laycock and Jerwood24 developed through the digital palpation, the Oxford Grading Scale, that aims to evaluate and grade the PFM contraction capacity in 6 points: 0, absence of muscular response; 1, unsustained muscular contraction; 2, presence of contraction of low intensity, but not sustained; 3, moderate contraction, felt as an increase in intravaginal pressure; 4, satisfactory contraction; and 5, strong contraction.10 Likewise, manometry (also known as perineometry) evaluates the contraction of PFM, but more objectively through an intravaginal balloon device. The Perineometer is considered a high reproducibility method, and widely used in conjunction with other methods to analyze PFM activity.9,10,24
The aim of this study is to systematize the scientific evidence regarding the effects of PFMT in older women through the evaluation of the function and strength of the PFM, and determination of the maximum voluntary contraction through Oxford Grading Scale and manometry.
Methods
This study consisted of systematizing the scientific evidence on the effects of PFMT in older women, analyzing the function and strength of PFM through the Oxford Grading Scale and manometry. A systematic review of publications was carried out from 2003 to 2016.
Inclusion and exclusion criteria
From the screening of all titles and abstracts, the articles were read completely, assessing the eligibility according to the following inclusion criteria: randomized controlled trials; PFMT as a dependent variable including participants with UI; older women; articles in English language; methodological quality assessed by PEDro Scale with a classification superior to 4. Exclusion criteria are as follows: studies addressing surgical interventions; prolapsed ≥4 “Pelvic Organ Prolapse Quantification” (POP-Q); pregnant women and women who have recently given birth; pharmacological treatment of UI; case studies; systematic reviews; animal studies; meta-analyses; and low methodological quality.
Search strategy
Initially, this systematic review was conducted in accordance with the statement of the items of the preferential report for systematic reviews and meta-analyses (PRISMA), which aims to improve the reporting pattern of systematic reviews and meta-analyses.26
A search was made in the databases of B-on, EBSCO, PEDro, Pubmed, and SciELO, carried out between 2003 and 2016. The keywords were combined, and the research strategies were physical exercise (AND; OR) training of pelvic floor muscles, urinary incontinence, elderly (AND; OR) postmenopausal women, pelvic floor, pelvic floor muscles, manometry (AND; OR) perineometry, digital palpation (AND; OR) Modified Oxford Test (AND; OR) Oxford Grading Scale, evaluation of pelvic floor (AND; OR) evaluation of pelvic floor muscles.
Methodological quality assessment
The methodological quality of the studies was evaluated by the PEDro Scale,27 which is based on 11 questions about the study, of which 10 are scored (external validity, internal validity, and statistical reporting). The final score is obtained by the sum of all positive responses, and the classification of the result ranges from 0 to 10. The studies were classified independently by an evaluator and a second evaluator whose aim was to resolve potential disagreements that might arise in quality of selected studies.
Results
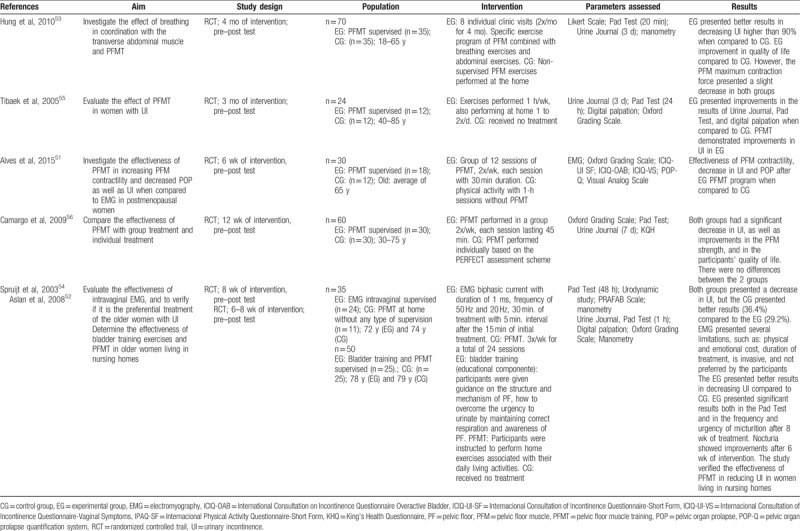
Thirty-five studies were found in the databases, of which 26 were analyzed in their entirety, and about 6 were selected for eligibility, after the exclusion of 8 articles from the literature review.3,11,28–33 The reasons for exclusion are presented in the PRISMA flowchart (Fig. 1). The excluded studies did not present the criteria for evaluation of the PEDro Scale,25,34–37 have a very large age range or lack of age data,38–42 one pilot study,12 sample of young athletes,43,44 and pregnant women.45,46 Although 5 studies present a classification between 4 and 8 in the PEDro Scale, only 1 study does not present a description of the digital palpation,8 and the remaining participants have an average age of 44 to 60 years.47–50 Only 6 studies are included in the PEDro Scale (score between 4 and 8), and meet the inclusion criteria (Table 1).51–56 PFM contraction was assessed in 4 studies by digital vaginal examination using the Oxford Grading Scale51,52,55,56; 3 studies used manometry as an evaluation method. Of the selected studies, 1 study reported to assess maximal vaginal squeeze pressure and holding time through a manometer53; 1 study evaluated the contractility of PFM using a vaginal probe of surface eletromyography51; and 1 study assessed the average maximum intravaginal pressure by a perineometer.54 The articles selected for the elaboration of the systematic review are represented in Table 2.
Figure 1.
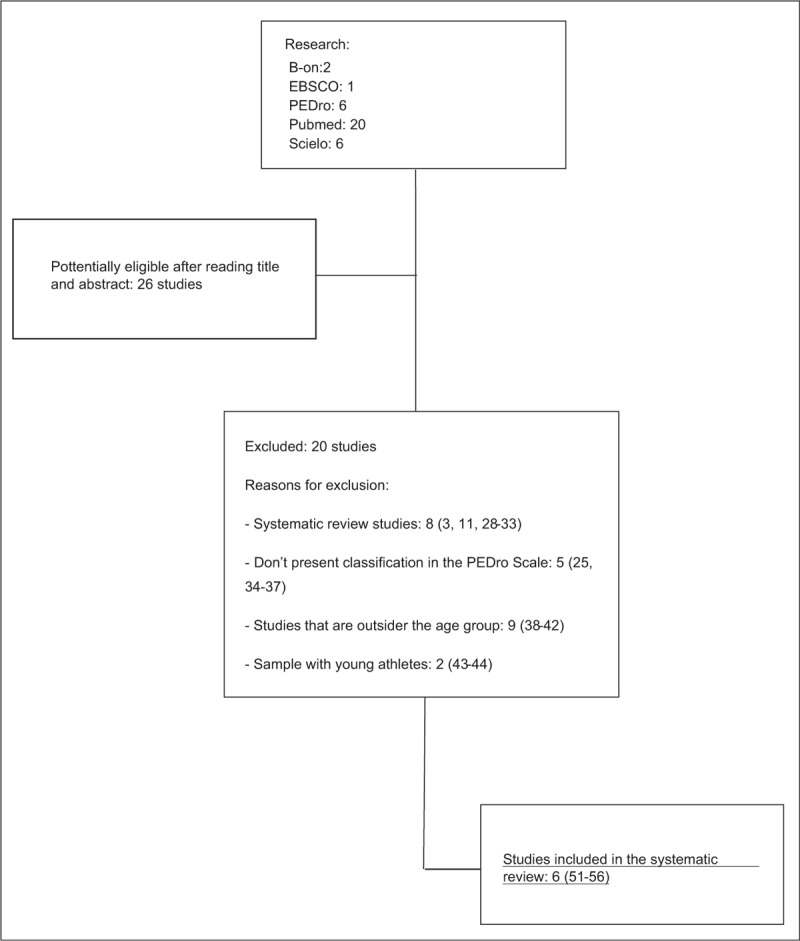
PRISMA flow diagram of the eligibility process.
Table 1.
Methodological quality of the included studies
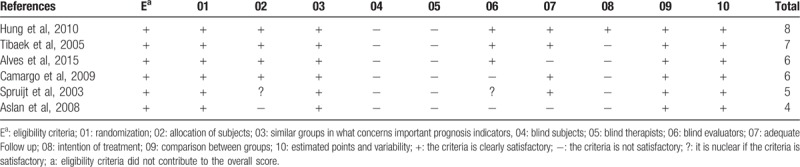
Table 2.
Characteristics and main results of the included studies
Discussion
This systematic review demonstrates that independently of the type of UI, PFMT is recommended by ICS as a first-line conservative therapy in older women, and is fundamental to increase strength and correct contraction of PFM.8–10 However, it is essential to evaluate the function and strength of PFM, before and after, the PFMT to determine the effects of the established training protocol. The physical evaluation is considered fundamental in the determination of UI and should include visual analysis of the urogenital region, vaginal palpation, and verification of the function of the PFM.9,10,25
There are several methods to evaluate the function and strength of PFM, but digital palpation and manometry are considered the standardized and highly reproducible methods in the clinical evaluation.4
Digital palpation is fundamental in the PF evaluation process. The determination of muscle strength and endurance provides indispensable information about the condition of the muscular strength of the patient, which allows the physiotherapist to establish a specific training program appropriate to the patient.9,10
All studies selected showed improvements in UI symptoms; however, the results of PFM evaluation are divergent. In the study performed by Hung et al,53 70 women were randomly allocated in a training group (TG) and control group (CG). The TG was subjected to individual clinical visits twice a month during 4 months and a training program that consists of exercises: diaphragmatic breathing; tonic activation of transversus abdominis and PFM; strengthening of transversus abdominis, PFM and internal oblique; functional expiratory exercises; and impact activities. The subjects in CG followed the oral instruction and the normal information that was composed of UI, bladder hygiene, and PFMT program. The participants performed self-monitored PFMT program at home. PF assessment was performed by a physiotherapist through digital palpation to assess maximal voluntary contraction, and teach women to contract PFM correctly. Together, it was performed through manometry in which participants were instructed to contract PP 3 times, taking into account the last 2 contractions (mean of the 2 measurements). Although there was improvement in PFM strengthening in the treatment group when compared with the CG, a slight decrease in the maximum contraction pressure (effect size 0.36) was observed through manometry. This can be explained by the fact that the patient cannot maintain the PFM's maximum contraction for a long time, keeping only enough to hold the device. Studies indicate that increased abdominal pressure resulting from abdominal transverse contraction may cause PFM to weaken in women with UI.57 Hung et al53 advocate that physiotherapists supervise the co-contraction of the abdominal transverse with PFM, to prevent PFM weakening resulting from increased intra-abdominal pressure.
Camargo et al56 evaluated the PFM maximum strength through Oxford Grading Scale. The endurance has been defined as a time interval of up to 10 seconds, where a maximum vaginal contraction may be maintained before a force decreases to approximately 35% or more occurs. Another hypothesis indicator of muscular fatigue is the simultaneous contraction of the adductor muscle of the hip, buttocks, and a strong co-contraction of the transverse abdominal. According to the principle of the biomechanics of the pelvic structure, Alves et al51 believe that PFMT should not only be based on PFM but should also highlight the interaction and harmony of all the structures that are involved in the function of PF.
Some authors suggest that there is not a correlation between strength weakening during a maximal voluntary contraction of PFM and UI symptoms. However, in the study Da Roza et al44 reported a significant moderate correlation between the Oxford Grading Scale score and peak pressure on manometry (r = 0.646, P = .002).
Despite improvements in the decrease in UI, some authors point out limitations to the study of Hung et al,53 one of which was the fact that most participants did not present involuntary loss of urine at the baseline. In addition, both groups did not receive a structured PFMT program. Another limitation of the investigation was that participants in the CG were instructed how to perform the PFM exercises protocol on one occasion, without continuous supervision or feedback, for that reason the control intervention was not considered the best practice.3
In the study of Tibaek,55 Oxford Grading Scale was used in the evaluation of the maximum voluntary contraction and 3 measurements were made, being considered only the best result. Mattiasson and Tibaek,55,58 refer to digital palpation as a simple and important method that provides the necessary information about the structure and function of PF, compared with electromyography and manometry. The Oxford Grading Scale is considered a simple, low-cost, and widely used method in clinical practice, which presents as its main disadvantage subjectivity by including only 1 examiner.55
Alves et al51 observed on increased strength and contractility of PFM after the PFMT program in the TG, evaluated both by digital palpation (P = .001) and electromyography (P = .003).
Vaginal electrical stimulation does not seem to be the most effective treatment for UI reduction. Spriujt et al54 verified through manometry, there is no significant improvement in urinary loss in women treated with vaginal electrostimulation, when compared with the group submitted to PFMT. Vaginal electrostimulation presents several limitations, such as physical and emotional cost, duration of treatment, and invasive.
One of the criticisms attributed to the Oxford Grading Scale is the difficulty in obtaining valid and reproducible measures because it is not able to correctly classify women who present diminished muscle strength when compared with pressure measurement (manometry). To limit this difficulty, it is suggested to associate with other methods of evaluation, such as manometry and ultrasound.56 Camargo et al56 reported that one of the limitations of their study was the assessment of PFM function and strength. The validity and reproducibility of the evaluation is very difficult to reach only by digital palpation, requiring a more objective evaluation such as manometry, to better understand the relationship between PFM strength and involuntary loss of urine in the research area, but in clinical practice digital palpation is considered a standard method.
In the study performed by Aslan,52 it was verified that there was an improvement in UI comparing the PFMT group to the CG, but it was limited in its sample because 30% of the older women did not accept to be evaluated by digital palpation as well as by manometry. The selected test was the digital palpation and performed with repetitions of 4 to 5 times, not being mentioned how the measurements were calculated.
Several studies have demonstrated good intrarater reproducibility using manometry with intragroup correlation; the mean coefficient ranges from 0.88 to 0.97 in the maximal voluntary contraction, but few studies have reported inter-rater reproducibility.45,59 Although the limited sample size, in the study by Da Roza et al44 with a group of young nulliparous athletes with UI, compared the maximum pressure values of manometry with the scores of the Oxford Grading Scale, determined a moderate inter-rater reproducibility of 0.65, considering differences between the measures of maximum voluntary contraction between continent and incontinent women. Another limitation of the study was that the data obtained should only be validated for young athletes and the results should be different in older women with PF dysfunctions. In the study by Hung et al,53 the test–retest reproducibility of manometry was established as being good with a correlation coefficient of 0.95.
Currently, the assessment of PFM strength and function seems to be better when determined through a combination of observation, palpation, and vaginal tightening pressure. There are several factors that make it difficult to evaluate the function of PF among which stand out, location of the PF within the pelvic cavity, volume and anatomy. To overcome this problem, we may have the association of other methods such as ultrasonography and magnetic resonance.10
Digital palpation is a very common procedure in the evaluation of PFM contraction in pelvic dysfunctions. Although it is a subjective assessment, the Oxford Grading Scale is a qualitative method (if there was contraction or not), useful, low cost and simple to perform. Digital palpation is adequate for clinical evaluations. Proper testing of the patient, standardization of instruction, motivation, and the patient's position are key issues in order for the test to occur properly.
Manometry is the method chosen when evaluating the strength of PFM because it is considered less invasive, without risk of infection and more reliable to use in research assessment when compared to urodynamic evaluation. However, both methods require a lot of experience and training of the examiner due to the variation of sensitivity by the test taker.10
The evaluation of PFM is essential in clinical practice as in scientific research, but there are limitations to studies, such as the number of evaluations of maximum voluntary contraction. Some of these studies do not mention the calculation of these measurements. The rest time between evaluations is divergent. The existence of having an examiner or more may be a factor of subjectivity. The different types of instruments may be a confounding variable in the results of the evaluation of the maximal voluntary contraction of PFM.
Although it is considered a first-line treatment in the treatment and prevention of urogynecological dysfunctions, and the literature has shown that PFMT have high success rates in the treatment of PF dysfunction, studies conducted in PFMT are still scarce and present some methodological problems (eg, insufficient sample, nonappropriate study designs). These limitations prevent the establishment recommendations regarding the type, frequency, and duration of training, thus standardized PFMT protocols are required.
Conclusion
In conclusion, the Oxford Grading Scale and manometry are considered the ones that present a greater reproducibility in the results of the studies carried out in the research area. As a limitation to the study, we can present several factors, such as: type and severity of incontinence, exercise intensity, duration of intervention, adherence of participants, measurement instruments, sample size, and standardized test evaluations. These factors make it difficult to compare several studies. In addition, we observed the need for randomized controlled trials of high methodological quality that compare the results of the Oxford Grading Scale with manometry evaluation in older women.
Acknowledgments
None.
Conflicts of interest
The authors report no conflicts of interest.
References
- 1.Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 2010; 29:213–240. [DOI] [PubMed] [Google Scholar]
- 2.Dirk de R, Robert F, Steven S, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 2010; 21:5–26. [DOI] [PubMed] [Google Scholar]
- 3.Bø K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. J Physiother 2013; 59:159–168. [DOI] [PubMed] [Google Scholar]
- 4.Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010; 29:4–20. [DOI] [PubMed] [Google Scholar]
- 5.Hay-Smith J, Herderschee R, Dumoulin C, et al. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women: an abridged Cochrane systematic review. Eur J Phys Rehabil Med 2012; 48:689–705. [PubMed] [Google Scholar]
- 6.Abrams P, Cotterill N, Smith AP. The impact of urinary incontinence on health-related quality of life (HRQoL) in a real-world population of women aged 45-60 years: Results from a survey in France, Germany, the UK and the USA. BJU Int 2015; 115:143–152. [DOI] [PubMed] [Google Scholar]
- 7.Bø K. Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Med 2004; 34:451–464. [DOI] [PubMed] [Google Scholar]
- 8.Sherburn M, Bird M, Carey M, et al. Incontinence improves in older women after intensive pelvic floor muscle training: an assessor-blinded randomized controlled trial. Neurourol Urodyn 2011; 30:317–324. [DOI] [PubMed] [Google Scholar]
- 9.Bernards AT, Berghmans BC, Slieker-Ten Hove MC, et al. Dutch guidelines for physiotherapy in patients with stress urinary incontinence: an update. Int Urogynecol J 2014; 25:171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bø K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther 2005; 85:269–282. [PubMed] [Google Scholar]
- 11.Bø K, Hilde G. Does it work in the long term? A systematic review on pelvic floor muscle training for female stress urinary incontinence. Neurourol Urodyn 2013; 32:215–223. [DOI] [PubMed] [Google Scholar]
- 12.Da Roza T, Araujo M, Viana R, et al. Pelvic floor muscle training to improve urinary incontinence in young, nulliparous sport students: a pilot study. Int Urogynecol J 2012; 23:1069. [DOI] [PubMed] [Google Scholar]
- 13.Van Geelen JM, Hunskaar S. The epidemiology of female urinary incontinence. Eur Clinics Obstet Gynaecol 2005; 1:3–11. [Google Scholar]
- 14.Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008; 300:1311–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherburn M. Bø K, Berghmans B, Morked S, Kampen MV. Evidence for pelvic floor physical therapy in the elderly. Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice. Philadelphia:Churchill Livingstone Elsevier; 2007. 345–368. [Google Scholar]
- 16.Danforth KN, Townsend MK, Lifford K, et al. Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol 2006; 194:339–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perucchini D, DeLancey JO, Ashton-Miller JA, et al. Age effects on urethral striated muscle. I. Changes in number and diameter of striated muscle fibers in the ventral urethra. Am J Obstet Gynecol 2002; 186:351–355. [DOI] [PubMed] [Google Scholar]
- 18.Ashton-Miller JA, DeLancey JO. Functional anatomy of the female pelvic floor. Ann N Y Acad Sci 2007; 1101:266–296. [DOI] [PubMed] [Google Scholar]
- 19.Ree ML, Nygaard I, Bo K. Muscular fatigue in the pelvic floor muscles after strenuous physical activity. Acta Obstet Gynecol Scand 2007; 86:870–876. [DOI] [PubMed] [Google Scholar]
- 20.Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 2010; 1: CD005654. [DOI] [PubMed] [Google Scholar]
- 21.Freeman RM. The role of pelvic floor muscle training in urinary incontinence. BJOG 2004; 111:37–40. [DOI] [PubMed] [Google Scholar]
- 22.Bø K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int Urogynecol J and Pelvic Floor Dysfunct 2004; 15:76–84. [DOI] [PubMed] [Google Scholar]
- 23.Hay-Smith J, Morkved S, Fairbrother KA, et al. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 2008; 4: CD007471. [DOI] [PubMed] [Google Scholar]
- 24.Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy 2001; 87:631–642. [Google Scholar]
- 25.Talasz H, Jansen SC, Kofler M, et al. High prevalence of pelvic floor muscle dysfunction in hospitalized elderly women with urinary incontinence. Int Urogynecol J 2012; 23:1231–1237. [DOI] [PubMed] [Google Scholar]
- 26.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009. 339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 2009; 55:129–133. [DOI] [PubMed] [Google Scholar]
- 28.Ferreira M, Santos P. Princípios da Fisiologia do Exercício no Treino dos Músculos do Pavimento Pélvico. Acta Urológica 2009; 26:31–38. [Google Scholar]
- 29.Jácomo RH, Fitz FF, Alves AT, et al. The effect of pelvic floor muscle training in urinary incontinent elderly women: a sistematic review. Fisioter Mov 2014; 27:675–689. [Google Scholar]
- 30.Pereira VS, Escobar AC, Driusso P. Effects of physical therapy in older women with urinary incontinence: a systematic review. Rev Bras de Fisioter 2012; 16:463–468. [DOI] [PubMed] [Google Scholar]
- 31.Da Roza T, Jorge RN, Mascarenhas T, et al. Urinary incontinence in sport women: from risk factors to treatment—a review. Curr Womens Health Rev 2013; 9:77–84. [Google Scholar]
- 32.Goldstick O, Constantini N. Urinary incontinence in physically active women and female athletes. Br J Sports Med 2014; 48:296–298. [DOI] [PubMed] [Google Scholar]
- 33.Bø K. Pelvic floor muscle training in treatment of female stress urinary incontinence, pelvic organ prolapse and sexual dysfunction. World J Urol 2012; 30:437–443. [DOI] [PubMed] [Google Scholar]
- 34.Tibaek S, Dehlendorff C. Pelvic floor muscle function in women with pelvic floor dysfunction: a retrospective chart review, 1992–2008. Int Urogynecol J 2014; 25:663–669. [DOI] [PubMed] [Google Scholar]
- 35.Gameiro MO, Moreira EC, Ferrari RS, et al. A comparative analysis of pelvic floor muscle strength in women with stress and urge urinary incontinence. Int Braz J Urol 2012; 38:661–666. [DOI] [PubMed] [Google Scholar]
- 36.Virtuoso JF, Mazo GZ, Menezes EC. Urinary incontinence and perineal muscle function in physically active and sedentary elderly women. Braz J Phys Ther 2011; 15:310–317. [DOI] [PubMed] [Google Scholar]
- 37.Langoni CS, Knorst MR, Lovatel GA, et al. Urinary incontinence in elderly women from Porto Alegre: its prevalence and relation to pelvic floor muscle function. Fisioterapia e Pesquisa 2014; 21:74–80. [Google Scholar]
- 38.Talasz H, Himmer-Perschak G, Marth E, et al. Evaluation of pelvic floor muscle function in a random group of adult women in Austria. Int Urogynecol J Pelvic Floor Dysfunct 2008; 19:131–135. [DOI] [PubMed] [Google Scholar]
- 39.Dietz HP, Shek KL. Levator function and voluntary augmentation of maximum urethral closure pressure. Int Urogynecol J 2012; 23:1035–1040. [DOI] [PubMed] [Google Scholar]
- 40.Lacombe AC, Riccobene VM, Nogueira LA. Effectiveness of a program of therapeutic exercises on the quality of life and lumbar disability in women with Stress Urinary Incontinence. J Bodyw Mov Ther 2015; 19:82–88. [DOI] [PubMed] [Google Scholar]
- 41.Botelho S, Martinho NM, Silva VR, et al. Abdominopelvic kinesiotherapy for pelvic floor muscle training: a tested proposal in different groups. Int Urogynecol J 2015; 26:1867–1869. [DOI] [PubMed] [Google Scholar]
- 42.Chevalier F, Fernandez-Lao C, Cuesta-Vargas AI. Normal reference values of strength in pelvic floor muscle of women: a descriptive and inferential study. BMC Womens Health 2014; 14:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Da Roza T, Brandao S, Mascarenhas T, et al. Volume of training and the ranking level are associated with the leakage of urine in young female trampolinists. Clin J Sport Med 2015; 25:270–275. [DOI] [PubMed] [Google Scholar]
- 44.Da Roza T, Mascarenhas T, Araujo M, et al. Oxford Grading Scale vs manometer for assessment of pelvic floor strength in nulliparous sports students. Physiotherapy 2013; 99:207–211. [DOI] [PubMed] [Google Scholar]
- 45.Ribeiro JS, Guirro EC, Franco MM, et al. Inter-rater reliability study of the Peritron perineometer in pregnant women. Physiother Theory Pract 2016; 32:209–217. [DOI] [PubMed] [Google Scholar]
- 46.Gameiro MO, Sousa VO, Gameiro LF, et al. Comparison of pelvic floor muscle strength evaluations in nulliparous and primiparous women: a prospective study. Clinics (Sao Paulo) 2011; 66:1389–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gameiro MO, Moreira EH, Gameiro FO, et al. Vaginal weight cone versus assisted pelvic floor muscle training in the treatment of female urinary incontinence. A prospective, single-blind, randomized trial. Int Urogynecol J 2010; 21:395–399. [DOI] [PubMed] [Google Scholar]
- 48.Williams KS, Assassa RP, Gillies CL, et al. A randomized controlled trial of the effectiveness of pelvic floor therapies for urodynamic stress and mixed incontinence. BJU Int 2006; 98:1043–1050. [DOI] [PubMed] [Google Scholar]
- 49.Beuttenmüller L, Cader SA, Macena RHM, et al. Floor muscles contraction in women with stress urinary incontinence underwent to exercises and electric stimulation therapy: a randomized study. Fisioter Pesqui 2011; 18:210–216. [Google Scholar]
- 50.Felicissimo MF, Carneiro MM, Saleme CS, et al. Intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: a randomized comparative trial. Int Urogynecol J 2010; 21:835–840. [DOI] [PubMed] [Google Scholar]
- 51.Alves FK, Riccetto C, Adami DB, et al. A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial. Maturitas 2015; 81:300–305. [DOI] [PubMed] [Google Scholar]
- 52.Aslan E, Komurcu N, Beji NK, et al. Bladder training and Kegel exercises for women with urinary complaints living in a rest home. Gerontology 2008; 54:224–231. [DOI] [PubMed] [Google Scholar]
- 53.Hung HC, Hsiao SM, Chih SY, et al. An alternative intervention for urinary incontinence: retraining diaphragmatic, deep abdominal and pelvic floor muscle coordinated function. Man Ther 2010; 15:273–279. [DOI] [PubMed] [Google Scholar]
- 54.Spruijt J, Vierhout M, Verstraeten R, et al. Vaginal electrical stimulation of the pelvic floor: a randomized feasibility study in urinary incontinent elderly women. Acta Obstet Gynecol Scand 2003; 82:1043–1048. [DOI] [PubMed] [Google Scholar]
- 55.Tibaek S, Gard G, Jensen R. Pelvic floor muscle training is effective in women with urinary incontinence after stroke: a randomised, controlled and blinded study. Neurourol Urodyn 2005; 24:348–357. [DOI] [PubMed] [Google Scholar]
- 56.Camargo FO, Rodrigues AM, Arruda RM, et al. Pelvic floor muscle training in female stress urinary incontinence: comparison between group training and individual treatment using PERFECT assessment scheme. Int Urogynecol J Pelvic Floor Dysfunct 2009; 20:1455–1462. [DOI] [PubMed] [Google Scholar]
- 57.Bø K, Morkved S, Frawley H, et al. Evidence for benefit of transversus abdominis training alone or in combination with pelvic floor muscle training to treat female urinary incontinence: a systematic review. Neurourol Urodyn 2009; 28:368–373. [DOI] [PubMed] [Google Scholar]
- 58.Mattiasson A. Characterisation of lower urinary tract disorders: a new view. Neurourol Urodyn 2001; 20:601–621. [DOI] [PubMed] [Google Scholar]
- 59.Sigurdardottir T, Steingrimsdottir T, Arnason A, et al. Test-retest intra-rater reliability of vaginal measurement of pelvic floor muscle strength using Myomed 932. Acta Obstet Gynecol Scand 2009; 88:939–943. [DOI] [PubMed] [Google Scholar]


