Abstract
Introduction
Erectile dysfunction is a highly prevalent condition. Existing guidelines provide recommendations for diagnosis and treatment, but they are often disregarded in clinical practice in favor of a “patient-tailored” approach.
Objectives
We planned a Delphi consensus method to bridge the gap between evidence-based medicine and the real-life approach in daily practice.
Materials and Methods
The Advisory Board prepared 15 statements on debated topics in andrology, each including 4–6 items designed as a 5-point Likert scale. After a validation phase, the questionnaire was sent by e-mail to a panel of experts for a first round of voting; members of the panel were later invited to a second round of voting, preceded by discussion of the “hot topics” identified in the first round.
Results
The first round of the Delphi consensus involved 101 experts; 71 (70%) also took part in the second round of voting. The Advisory Board deemed 22 items to be worthy of debate, and these underwent the second round of voting. “Real-life” results from the survey proved quite different from evidence-based recommendations.
Conclusion
Although guidelines suggest the best approach for a “standard” patient, real-life settings require flexibility. Diagnostic and therapeutic approaches should be tailored to the patients’ needs. Phosphodiesterase type 5 inhibitors are recognized as the first-line therapy in both settings, including the newly introduced sildenafil orodispersible film. Indications from the panel might help close the gap between recommendations from guidelines and real-life practice in relation to the diagnosis and treatment of erectile dysfunction.
Isidori AM, Giammusso B, Corona G, et al. Diagnostic and Therapeutic Workup of Erectile Dysfunction: Results From a Delphi Consensus of Andrology Experts. Sex Med 2019;7:292–302.
Key Words: Erectile Dysfunction, PDE5 Inhibitors, Treatment, Delphi, Consensus
Introduction
Erectile dysfunction (ED) is an increasingly important health issue, with epidemiological data demonstrating its high prevalence and overall increasing incidence worldwide. Several guidelines have been published by international scientific associations that summarize the current evidence for the diagnosis and treatment of patients suffering from ED.1, 2, 3, 4 In routine clinical practice, however, decisions are often challenging, often because of time constraints, limited personnel, and lack of resources. Gaps between real-life practice and evidence from clinical trials arise from both a diagnostic and a therapeutic point of view. For example, is a diagnostic classification with specialized examinations always necessary? Is it really now possible to offer our patients a "tailor-made" therapeutic approach? How should we approach the commercial innovations that are proposed to us but that do not always have a solid scientific basis?
When evidence-based medicine does not provide a clear answer to a clinical problem, consensus methods may enhance decision-making and support expert opinion guidelines.5 These consist in gathering the opinion of experts to obtain a formal agreement on debated topics.
Several research methods have been developed that are directed at problem-solving, idea-generation, or determining priorities, and, among these, the most common are the nominal group technique and the Delphi technique.6 The latter is based on the establishment of a panel comprising a large number of participants that uses a multistage self-completed questionnaire, with individual feedback to determine consensus from a larger group of “experts” without the need for face-to-face contact.7 In this article, we report the results of a Delphi consensus panel that was organized to address multiple clinically relevant but unanswered questions about the clinical management of patients with ED.
Materials and methods
Identification, Selection of the Topics and Questionnaire Drafting
After a literature research the Advisory Board prepared a Delphi questionnaire containing a list of 15 statements focusing on debated topics in the andrology community, divided into 2 main parts (general topics and clinical cases), and each statement is expanded to from 4 to 6 items. The statements focus on diagnostic and therapeutic management problems with different types of ED patient; adherence to treatment; rehabilitation therapies after surgery; therapeutic approaches after iatrogenic problems; and therapeutic approach to comorbid patients. The full questionnaire is reported in the supplementary appendix.
Delphi Method
A modified Delphi method8 was used to achieve a consensus among a group of Italian andrology specialists (Figure 1). Delphi is a structured method generally used in medicine to obtain consensus among experts and to develop recommendations, clinical guidelines, questionnaires or clinical indicators.9 The participants provide their opinion freely, individually, and anonymously through ≥1 rounds of discussion. The process usually ends when an agreement on the discussed topic has been achieved.
Figure 1.
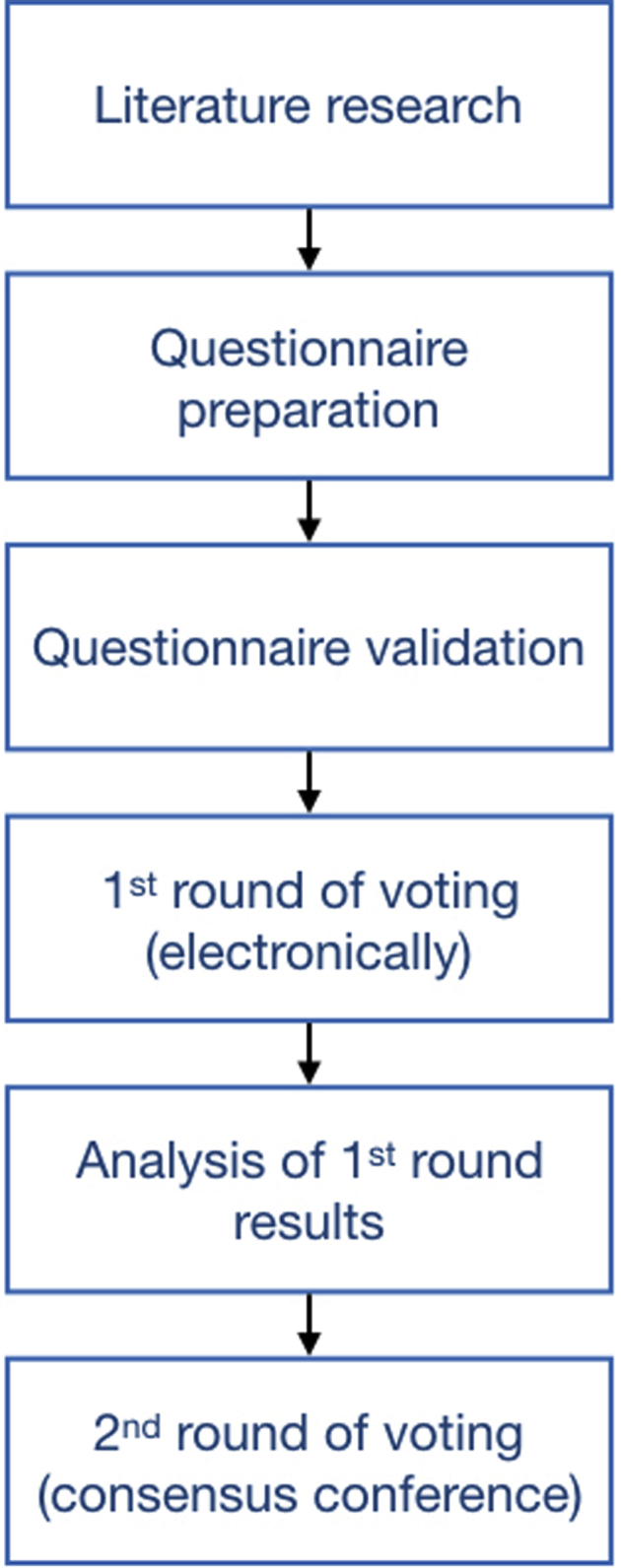
The modified Delphi method used in this Consensus.
In the present consensus, experts anonymously expressed their level of agreement according to the following 5-point Likert scale: 1 = completely disagree, 2 = disagree, 3 = agree, 4 = strongly agree, 5 = completely agree. Consensus was reached when the sum of items 1 and 2 (Disagree, negative consensus) or 3, 4 and 5 (Agree, positive consensus) reached at least 66%. No consensus was reached when the sum of the responses for a negative consensus or a positive consensus was <66%.
The questionnaire was submitted to 5 external validators and then sent by e-mail to 101 Italian andrology specialists with at least 5 years’ experience in andrology, selected according their predominant andrological clinical activity. The recruited clinicians were uniformly distributed among various clinical centers in Italy and were representative of different professional settings, including academia, hospitals, and private practice.
A first round of voting was performed via a web-based anonymous survey. Members of the panel were later invited to a second round of voting, preceded by discussion of the “hot topics” identified in first round.
Results
Round 1: Web-Based Survey
As previously stated, 101 experts were involved in the first round of voting. The 15 statements investigating the diagnostic and therapeutic management of ED patients received mixed answers from the panel, suggesting that in the clinical practice opinions often diverge among experts. Detailed results of the first round are reported in the Supplementary File 1. At the end of this first round of voting, several items were identified as “hot topics” requiring further investigation, including items patently in contrast with existing guidelines and those for which no definite consensus was reached.
Statement 1: Diagnostic Tests Necessary for Assessment of Erectile Function
Assessment of glucose and lipid profile (item 1.1), total testosterone and sex hormone binding globulin (item 1.2), penile Doppler ultrasound scanning before and after intracavernous prostaglandin injection (ICI) (item 1.3) reached positive consensus. Nocturnal penile tumescence test (item 1.4) and testicular and transrectal prostate ultrasound scanning (item 1.5) reached negative consensus.
Statement 2: Non-Medical Interventions to Improve Erectile Function
Positive agreement was reached for all lifestyle changes, namely 5% weight loss for obese and overweight patients (item 2.1, 99% agreement), transition to a well-balanced Mediterranean diet (item 2.2, 96% agreement), stopping smoking (item 2.3, 100% agreement), and complete abstinence from alcohol consumption (item 2.4, 73% agreement).
Statement 3: First-Line Treatments for Young, “Naïve” Patients in a Stable Relationship
Members of the panel were asked about their common approach to treating young patients with no history of phosphodiesterase type 5 (PDE5) inhibitor use. Positive consensus was reached on recommending sexual counseling alone for mild ED (item 3.1) or sexual counseling, possibly followed by PDE5 inhibitors (PDE5i) for moderate ED (item 3.2). No definite consensus was reached concerning the possibility of treating with either “on demand” (item 3.3) or daily (item 3.4) PDE5i, possibly followed by other therapeutic options. Likewise, no consensus was reached concerning whether to start with an initial high dose of PDE5i, followed by a dose reduction (item 3.5), or vice versa (item 3.6).
Statement 4: Treatments for “Non-Naïve” Patients
Panelists did not reach consensus on the efficacy of switching from an on-demand to a daily treatment when the former is no longer effective (item 4.1). However, they agreed that either switching to a different compound (item 4.2) or route of administration (item 4.3) could improve erectile function after treatment failure. Experts were also asked to describe their choice of prostaglandin use (via ICI): no consensus was reached regarding the need to switch to ICI for patients not responding adequately to PDE5i (item 4.4), there was a negative consensus on the tolerability of transurethral vs. ICI administration (item 4.5), and no consensus was reached for combining PDE5i and prostaglandins (item 4.6).
Statement 5: Refractory Erectile Dysfunction
Members of the panel were asked about their treatment of choice for patients no longer responding to PDE5i. Panelists agreed on the use of prostaglandins ICI, with or without phentolamine and papaverine (item 5.1), patient rehabilitation via daily administration of PDE5i, possibly coupled with sexual counseling (item 5.2) and penile prosthesis (item 5.4). No consensus was reached on penile venous ligation surgery (item 5.3).
Statement 6: Reasons for Choosing a Specific PDE5 Inhibitor
Members of the panel agreed that penile rigidity (item 6.1), partner’s preference (item 6.2) and tolerability profiles (item 6.5) were all possible criteria driving their choice when prescribing PDE5i. Experts did not agree about ignoring possible interactions between PDE5i and other drugs, except for nitrates (item 6.3), and about patient’s preference for daily rather than on-demand treatment (item 6.4).
Statement 7: External Conditioning Factors Involved in Treatment Choice
Most experts thought that the Internet (item 7.1), the pharmacist (item 7.2), or the general practitioner (item 7.3) had influenced the patients’ choice of treatment. No consensus was reached when asked about whether to leave treatment unchanged unless patently wrong (item 7.4). 2 more questions investigated whether the experts believed that ≤10% of their patients might have bought PDE5i on the “black market” (item 7.5) and whether they considered buying online appropriate for the patient, to increase treatment availability while reducing costs and embarrassment (item 7.6). No consensus was reached for the former, whereas negative agreement was reached for the latter.
Statement 8: Generic Equivalent Drugs for ED
Experts agreed that external conditioning factors, such as suggestion by the pharmacist, might affect the patient’s choice of treatment (item 8.1) and that drugs from selected, trustworthy companies should be preferred (item 8.3). No consensus was reached on whether competition could reduce the costs of generic equivalent PDE5i (item 8.2); however, experts agreed that branded drugs should be preferred despite the higher cost (item 8.4).
Statement 9: Factors Affecting Adherence to Treatment
Members of the panel agreed that up to 50% of patients discontinue treatment with PDE5i during the first year (item 9.1), or during the first 2 years when using ICI or vacuum devices (item 9.4, 93% agreement). To improve adherence to treatment, the experts agreed that patients should receive adequate information on the different pharmacokinetics and pharmacodynamics of PDE5i (item 9.2). They also agreed that switching to a different product might improve treatment efficacy (item 9.3).
Statement 10: Factors Involved in Treatment Discontinuation
The panel agreed that efficacy of any PDE5 inhibitor should be valued only after ≥6 consecutive attempts (item 10.1). In cases of treatment failure, they agreed on assessing mode of use (eg, sexual stimulation, inadequate doses, counterfeit drugs; item 10.2) and on proposing treatment “re-education” (item 10.3) before changing drug. They agreed that “combined” treatment with both low-dose daily tadalafil and high-dose short-acting on-demand PDE5i might be suggested to patients reporting unsatisfying response to daily treatment alone (item 10.4). No consensus was reached on the use of low-intensity shockwave therapy for ED as a mid-step between PDE5i and ICI (item 10.5).
Statement 11: Sexual Rehabilitation After Pelvic Surgery: General Considerations
The panel agreed on all items of this statement: early initiation of treatment (item 11.1), lasting duration of treatment (item 11.2), factors affecting recovery, such as age, pre-operative erectile function quality and degree of nerve sparing during surgery (item 11.3) and the progressive structural damage resulting from the absence of erectile activity (item 11.4). They also agreed that a long-term therapeutic scheme (daily use or several times per week) is no better than on-demand treatment for all therapies, including ICI and vacuum devices (item 11.5).
Statement 12: Sexual Rehabilitation After Pelvic Surgery: Treatment Choice
There was agreement on using PDE5i as a first-line treatment after nerve-sparing surgery (item 12.1), with therapeutic success depending on the choice and dose of PDE5 inhibitor and extent of any nerve damage (item 12.2), efficacy of ICI or vacuum devices (despite higher drop-out rates) in non-responders to PDE5i (item 12.3), and penile prosthesis as a last resort treatment for patients who either do not fully recover erectile function or wish for a permanent solution (item 12.4).
Statement 13: Clinical Case 1
This statement described a man with diabetes mellitus, treated with cordarone and with a medical history of moderate kidney failure (glomerular filtration rate 40 mL/min), chronic heart disease, and myocardial infarction. The patient was in a stable relationship and had normal serum testosterone. Members of the panel failed to reach consensus on treatment with daily long-acting PDE5i (item 13.1) or with on-demand ICI (item 13.3); however, the majority agreed on treatment with the on-demand sildenafil orodispersible film (item 13.2). No consensus was reached on delaying treatment in favor of a referral to a cardiologist (item 13.4).
Statement 14. Clinical Case 2
This statement described a 45-year-old man whose marriage had recently failed. He was undergoing treatment with sotalol for tachyarrhythmias, had normal serum testosterone, and reported casual sexual relationships. Members of the panel reached agreement on all items of this statement: short-acting PDE5i, namely sildenafil orodispersible film (item 14.1) and vardenafil sublingual tablets (item 14.4, 70% agreement), were considered as the best treatments, whereas there was a negative consensus on daily administration of long-acting PDE5i (item 14.2). The panel also agreed that psychological assessment was needed before starting treatment with PDE5i (item 14.3).
Statement 15. Clinical Case 3
This statement described a 67-year-old man with uncontrolled type 2 diabetes mellitus undergoing treatment with oral hypoglycemic agents (fasting glucose 210 mg/dL, hemoglobin A1c [HbA1c] 8.5%). The patient also had obliterating atherosclerosis of the lower extremities. During 4 consecutive attempts with Sildenafil 100 mg, the patient failed to achieve a fully rigid erection. The panel agreed on either trying the same treatment after achieving satisfactory metabolic control (item 15.1) or suspending PDE5i and switching to ICI, penile prosthesis, or low-intensity shockwave therapy (item 15.4). No consensus was reached concerning switching treatment to another PDE5i, whether on demand (item 15.2) or daily (item 15.3).
Round 2: Consensus Conference
A second Delphi round was then performed in a Consensus conference held in Rome on April 20, 2018; 70% of the online first-round responders (n = 71) also took part in the second round. During the meeting, the results from the first round of voting were presented (as reported in Supplementary File 1); the participants were then divided into 4 groups and discussed selected items and statements reported below with all members of the Advisory Board before a second round of voting. Items 1.3, 2.4, 3.1, 6.2, 15.1, and 15.4 (positive consensus after first round), items 3.3, 3.4, 3.5, 3.6, 5.2, 7.4, 7.5, 8.2 (no consensus after the first round), and statements 13 and 14 were re-voted. The results of the second round are shown in Table 1. The Advisory Board reminded all participants to answer based on their actual clinical practice, rather than on their “best-case scenario”: as a result, after the second round, consensus was different for several items. The results of the 2 Delphi rounds are discussed below.
Table 1.
Second-round voting
| Statements and Items | Score Distribution |
Consensus |
|||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Disagree | Agree | |
| Statement 1. When diagnosing a patient complaining of erectile dysfunction, I always evaluate the following items: | |||||||
| 1.3 Penile color Doppler scanning to be done before and after prostaglandin stimulation | 17% | 45% | 31% | 2% | 5% | 62% | 38% |
| Statement 2. To a patient complaining of erectile dysfunction, I would recommend 1 of the following options, in addition to a possible pharmacologic therapy: | |||||||
| 2.4 Complete abstinence from alcohol, which leads to improved sexual function | 25% | 53% | 15% | 2% | 5% | 78% | 22% |
| Statement 3. With regard to the first line of treatment of erectile dysfunction in young patients (with a stable relationship, "naïve" to treatment), I think that: | |||||||
| 3.1 It is appropriate to start with sexual counseling alone if erectile dysfunction is mild. | 11% | 43% | 21% | 8% | 17% | 54% | 46% |
| 3.3 It is appropriate to start immediately with an on-demand PDE5i (<3 times per week) before adding other therapies. | 6% | 34% | 26% | 24% | 10% | 40% | 60% |
| 3.4 It is appropriate to start immediately with a PDE5i administered as long-term therapy (≥3 times per week) and then add other therapies, if needed. | 22% | 46% | 18% | 3% | 11% | 68% | 32% |
| 3.5 When prescribing a PDE5i, it is usually better to start with a medium- to high-dose regimen that can be reduced afterward, if the patient responds well. | 16% | 48% | 13% | 10% | 13% | 64% | 36% |
| 3.6 When prescribing a PDE5i, it is usually better to start with a medium- to low-dose regimen that can be increased if the patient does not respond well. | 8% | 32% | 18% | 21% | 21% | 40% | 60% |
| Statement 5. With regard to the treatment of “refractory” erectile dysfunction (long-term erectile dysfunction, not responding to PDE5i at the maximum dosage after repeated attempts), I think that: | |||||||
| 5.2 It is appropriate to try patient rehabilitation, by proposing long-term PDE5i, possibly daily, for a prolonged period of time, associated to a psychological counseling (or external device), if needed. | 3% | 37% | 37% | 20% | 3% | 40% | 60% |
| Statement 6. When I prescribe a PDE5i to a patient with ED: | |||||||
| 6.2 I think that the opinion of the patient's partner, regardless of whether she is present during the visit, is crucial for the patient's treatment preference | 5% | 41% | 52% | 2% | 0% | 46% | 54% |
| Statement 7. With regard to external influences on the selection of the treatment for erectile dysfunction, I think that | |||||||
| 7.4 A therapy suggested by the patient— based on the information collected externally (web, general practitioner, pharmacist)—should not be changed, unless it is evidently wrong. | 3% | 12% | 70% | 12% | 3% | 15% | 85% |
| 7.5 Up to 10% of my patients may have purchased drugs for the treatment of erectile dysfunction from unofficial websites (black market). | 6% | 40% | 36% | 12% | 6% | 46% | 54% |
| Statement 8. With regard to the use of generic drugs for the treatment of erectile dysfunction, I think that: | |||||||
| 8.2 Generic drugs are all the same, so a competition based on price reduction is likely to occur. | 31% | 56% | 10% | 3% | 0% | 87% | 13% |
| Statement 13. In a patient with diabetes, post-MI ischemic heart disease, well compensated but receiving prophylaxis with cordarone, moderate CKD (glomerular filtration rate of 40 mL/min), in a stable relationship, and with normal testosterone values, I would choose the following therapy: | |||||||
| 13.1 Long-term administration of long half-life PDE5i | 27% | 63% | 8% | 2% | 0% | 90% | 10% |
| 13.2 On-demand rabestrom | 3% | 3% | 40% | 24% | 30% | 6% | 94% |
| 13.3 On-demand prostaglandin | 18% | 55% | 21% | 6% | 0% | 73% | 27% |
| 13.4 No drugs, but referral to cardiologist before prescribing a PDE5i, if any | 14% | 69% | 17% | 0% | 0% | 83% | 17% |
| Statement 14. In a 45-year-old patient with erectile dysfunction in good state of health, under treatment with sotalol for tachyarrhythmias, with a recently failed marriage and current occasional intercourse, with normal testosterone values, I would choose the following therapy: | |||||||
| 14.1 On-demand rabestrom | 3% | 0% | 47% | 20% | 30% | 3% | 97% |
| 14.2 Long-term administration of long half-life PDE5-I | 12% | 54% | 25% | 6% | 3% | 66% | 34% |
| 14.3 Treatment with PDE5-I must be secondary to a psychological evaluation to exclude issues related to the previous marriage. | 0% | 47% | 37% | 8% | 8% | 47% | 53% |
| 14.4 On-demand sublingual Vardenafil | 41% | 46% | 13% | 0% | 0% | 87% | 13% |
| Statement 15. In a 67-year-old patient, heavy smoker, with type 2 diabetes treated with oral hypoglycemic agents, fasting blood glucose levels of 210 mg/dL, HbA1c of 8.5%, with obliterative arterial disease of the lower limbs, who took Sildenafil 100 mg on 4 occasions without achieving rigidity sufficient for penetration: | |||||||
| 15.1 I would prescribe another attempt with the same drug after adequate glycometabolic compensation. | 7% | 26% | 39% | 15% | 13% | 33% | 67% |
| 15.4 I would discontinue the oral therapy and switch to another treatment (alprostadil, ESWT, prosthesis). | 16% | 48% | 13% | 10% | 13% | 64% | 36% |
| 14.1 On-demand rabestrom | 3% | 0% | 47% | 20% | 30% | 3% | 97% |
| 14.2 Long-term administration of long half-life PDE5i | 12% | 54% | 25% | 6% | 3% | 66% | 34% |
| 14.3 Treatment with PDE5i must be secondary to a psychological evaluation to exclude issues related to the previous marriage. | 0% | 47% | 37% | 8% | 8% | 47% | 53% |
| 14.4 On-demand sublingual Vardenafil | 41% | 46% | 13% | 0% | 0% | 87% | 13% |
| Statement 15. In a 67-year-old patient, heavy smoker, with type 2 diabetes treated with oral hypoglycemic agents, fasting blood glucose levels of 210 mg/dL, HbA1c of 8.5%, with obliterative arterial disease of the lower limbs, who took Sildenafil 100 mg on 4 occasions without achieving rigidity sufficient for penetration: | |||||||
| 15.1 I would prescribe another attempt with the same drug after adequate glycometabolic compensation. | 7% | 26% | 39% | 15% | 13% | 33% | 67% |
| 15.4 I would discontinue the oral therapy and switch to another treatment (alprostadil, ESWT, prosthesis). | 16% | 48% | 13% | 10% | 13% | 64% | 36% |
| 14.1 On-demand rabestrom | 3% | 0% | 47% | 20% | 30% | 3% | 97% |
| 14.2 Long-term administration of long half-life PDE5i | 12% | 54% | 25% | 6% | 3% | 66% | 34% |
| 14.3 Treatment with PDE5i must be secondary to a psychological evaluation to exclude issues related to the previous marriage. | 0% | 47% | 37% | 8% | 8% | 47% | 53% |
| 14.4 On-demand sublingual Vardenafil | 41% | 46% | 13% | 0% | 0% | 87% | 13% |
| Statement 15. In a 67-year-old patient, heavy smoker, with type 2 diabetes treated with oral hypoglycemic agents, fasting blood glucose levels of 210 mg/dL, HbA1c of 8.5%, with obliterative arterial disease of the lower limbs, who took Sildenafil 100 mg on 4 occasions without achieving rigidity sufficient for penetration: | |||||||
| 15.1 I would prescribe another attempt with the same drug after adequate glycometabolic compensation. | 7% | 26% | 39% | 15% | 13% | 33% | 67% |
| 15.4 I would discontinue the oral therapy and switch to another treatment (alprostadil, ESWT, prosthesis). | 16% | 48% | 13% | 10% | 13% | 64% | 46% |
ESWT = extracorporeal shockwave therapy; HbA1c = hemoglobin A1c; CKD = chronic kideny disease; MI = myocardial infarction; PDE5i = phosphodiesterase type 5 inhibitor.
Statement 1: Diagnostic Tests
Guidelines do not recommend penile Doppler ultrasound scanning after ICI on a routine basis.1, 2, 3, 4 In the second vote, no consensus was reached, but agreement was lower.
Statement 2: Non-Medical Interventions
Light alcohol consumption has shown effects in reducing anxiety and might, therefore, improve erectile function in some patients.10, 11 Because item 2.5 suggested complete abstinence from alcohol, the Advisory Board suggested reviewing this item in round 2. A negative consensus was reached when asking experts whether they actually suggest complete abstinence from alcohol in their clinical practice.
Statement 3: First-Line Treatments for Young, “Naïve” Patients
Several items in this statement were discussed. The aim of item 3.1 was to assess whether experts actually recommend sexual counseling alone for mild ED—not whether they agree with guidelines suggesting it. After explanation, agreement dropped markedly, and consensus was no longer reached. The Advisory Board suggested using PDE5i together with psychological interventions as a first line of treatment.12 When asked to re-vote, participants failed to reach a consensus on the use of on-demand inhibitors before any other interventions and disagreed with daily administration before other interventions. For items 3.5 and 3.6, the guidelines suggest starting with low dosages and then titrate to the maximum dosage to increase efficacy 2, 3; however, no consensus for either item was reached after discussion.
Statement 5: When PDE5i Fail
The Advisory Board reported no solid evidence for “rehabilitation” of erectile function with daily PDE5i 13; on re-voting, there was still no consensus.
Statement 6: Reasons for Choosing a Specific PDE5 Inhibitor
Concerning item 6.2, the Advisory Board asked experts to vote based on their own clinical practice, rather than guidelines suggestions; consensus was not reached.
Statement 7: External Influences Involved in Treatment Choice
Items 7.4 and 7.5 were re-voted, asking experts to express whether they agree or disagree based on their clinical practice: a vast majority agreed that they do not change treatment, unless patently wrong. No consensus was reached on item 7.5 during round 2.
Statement 8: Generic Equivalent Drugs for ED
Most experts expressed doubts regarding the reliability of minor pharmaceutical companies.
Statement 13: Clinical Case 1
All items of this statement underwent discussion and a second round of voting. In clinical practice, most experts agreed on treatment with on-demand sildenafil orodispersible film, rather than ICI or daily administration of long-acting PDE5i. They also disagreed with the need to delay treatment in favor of an assessment by a cardiologist.
Statement 14: Clinical Case 2
All items of this statement underwent discussion and a second round of voting. Treatment with on-demand sildenafil orodispersible film (item 14.1) reached positive consensus by the panel, whereas there was a negative consensus on the use of long-acting PDE5i (item 14.2) and on-demand vardenafil orodispersible tablets (item 14.4), due, respectively, to the reduced frequency of sexual intercourse and the possible side effects associated with sotalol use presented in the clinical case.14 There was a positive consensus in round 1 on item 14.3, suggesting psychological assessment before prescribing PDE5i, but no consensus on this item in round 2.
Statement 15: Clinical Case 3
Items 15.1 and 15.4 were discussed in round 2 and subsequently re-voted on. Members of the Advisory Board stressed the presence of severe vascular damage and its possible negative effects on erectile function; no changes in agreement were observed for item 15.1, whereas a consensus was no longer reached for item 15.4.
Discussion
The treatment of ED has been discussed in several guidelines and standard operating procedures.1, 2, 3, 4 However, real life is often different from the “ideal” setting described in recommendations. This limits the applicability of evidence-based medicine, leaving some “gaps” that might only be bridged by a consensus of expert clinicians based on their daily practice. The Delphi technique is 1 of the most reliable consensus methods for healthcare 7 and has been used to develop therapeutic management indicators for several conditions.15 For this study, the statements proposed by the Advisory Board were designed with the intention of providing a current picture of how ED is actually treated by Italian andrologists.
Sexual dysfunctions are common complaints in men of all ages. Although premature ejaculation is relatively more prevalent in the general population, ED is frequently perceived by the patient as a more serious condition and is often the prime reason for consultation. A large body of evidence has documented that ED is a possible symptom of future cardiovascular (CV) events, due to its association with several traditional CV risk factors.16 Hence, the general agreement on the routine assessment of glucose and lipid profile is not surprising and is in line with the available guidelines.1, 2, 3, 4 The same is true for the assessment of total testosterone and sex hormone binding globulin.
It has been reported that ED patients are a population with a higher proportion of hypogonadism and metabolic diseases.17 Because the symptoms of male hypogonadism are non-specific and affected by age, comorbidities, and duration of testosterone deficiency, diagnosis based on clinical features is not always possible; therefore, blood tests are necessary to reach diagnosis. Measuring fasting serum total testosterone on 2 separate mornings (between 8 and 11 am) is recommended to exclude possible circadian and day-to-day variations in serum testosterone concentrations.18 Guidelines suggest against routinely performing more-specialized diagnostic tests, such as penile Doppler ultrasound scanning after ICI, in the first-line clinical evaluation.1, 2 Results from the 2 rounds suggest that clinicians often disregard guidelines in these regards; although we cannot answer on behalf of the experts involved in the panel, we hypothesize that the rationale for performing penile Doppler ultrasound scanning after ICI would be to reduce the time for diagnosis or to exclude vascular causes.
Psychological intervention, although recommended, is not always feasible and often requires several sessions before bearing any results for the patient. It is, therefore, unsurprising that no consensus was reached in the second round on whether clinicians actually suggest psychological assessment (or perform it themselves) in their clinical practice. However, a recent meta-analysis suggested that the combination of psychological intervention and PDE5i yields better outcomes than either treatment alone,12 even for the shortest duration.
Considering the close correlation between ED and CV risk factors, lifestyle modifications should be considered as the first step for the treatment of ED subjects. Weight loss and a Mediterranean-style diet high in fruits, vegetables, and fish have been shown to improve ED.19 Similar observations have been reported for smoking cessation.19 The experts were, in fact, in agreement on these points.
The relationship between alcohol consumption and ED is not completely clarified. However, it has been reported that light alcohol consumption could help improve sexual function, acting psychologically to reduce anxiety and improving endothelial function.20 Conversely, heavier consumption is associated with impaired sexual function and increased CV risk.19, 20 This evidence was reflected by the panelists with their negative consensus during the second round.
Since the approval of sildenafil citrate by the Food and Drug Administration in 1998, PDE5i have emerged as the first-line medical treatment for most patients.1, 2, 3, 4 To date, 4 PDE5i have been approved for use in both Europe and the United States, none of which is selective for PDE5 alone but, instead, inhibits several other PDE isoforms.21, 22, 23 These drugs also have different pharmacokinetic parameters, enabling a more-tailored treatment based on the patient’s needs.21, 22, 23 Interestingly, no consensus was reached on the starting dosage and frequency of administration in either naïve or non-naïve PDE5i treated patients. Similarly, the current evidence suggests no difference in efficacy among the available PDE5i.24 In addition, the daily treatment approach did not provide better outcomes when compared with on-demand treatment, even in severe forms of ED, such as those secondary to radical prostatectomy 25 or type 2 diabetes mellitus.26
Current guidelines suggest starting with low dosages, followed by titration to the maximum dosage to increase treatment efficacy and satisfaction. However, it is important to recognize that a recent web survey suggests that, in clinical practice, physicians are more prone to prescribing the highest PDE5i dosage 27 and then possibly down-titrating, an approach that can minimize the risk of PDE5i failure from under-dosing and consequent depression. All of these considerations can explain the lack of consensus, even in the second round.
Patients strongly prefer PDE5i to all other forms of treatment,28 given their ease of use and mild, well-tolerated side effects; however, ≤35% of patients might fail to respond to the suggested treatment.29 Lack of efficacy is among the chief causes for treatment dropout, as well as cost, partner-related problems, and spontaneous recovery of erectile function.30, 31 Several options are available for patients who fail to respond to a PDE5 inhibitor. Although literature in this area is scant, it has been reported that some patients do actually respond better to 1 PDE5 inhibitor than to another: guidelines suggest this approach before abandoning PDE5i in favor of other treatments, most notably ICI, vacuum devices, and penile prosthesis. Although the pharmacokinetics differ between compounds, inhibition of isoforms different from PDE5 might also explain why some patients report greater benefits, different side effects, or both when switching treatment.32 Accordingly, the panelists reached a consensus on this topic in the first round.
To date, there are insufficient data to support any specific regimen as optimal for penile rehabilitation after prostate cancer.33 This point was recognized by the board of the panelists, who achieved a consensus in the first round.
The final 3 statements, each describing a difficult clinical scenario, were the most debated during the consensus conference. The first case (statement 13) described a diabetic man with a previous history of moderate kidney failure and chronic heart disease, undergoing treatment with cordarone, with normal levels of serum testosterone; given his frequency of sexual intercourse, this patient has no need for a daily treatment regimen and should be treated with on-demand PDE5i. On-demand prostaglandins are possibly effective but should not be suggested as a first approach. All members of the panel agreed on these items during the second round, and most experts also agreed that cardiologic consultation should by no means be considered mandatory before starting treatment, because there is no contraindication in relation to concurrent medications and comorbidities. This is in line with the 3rd Princeton Consensus Panel, which does not suggest cardiological consultation in this scenario,34 but which, however, suggests referral to a cardiologist in “high-risk” patients.
The second case (statement 14), which described a 45-year-old man undergoing treatment with sotalol and whose marriage had recently failed, aimed to identify the preferred therapy for a patient with mixed causes of ED; although psychological assessment and intervention were not universally considered useful by the panel, no doubts about the possible side effects of vardenafil due to its possible negative interaction with sotalol 14, 34 emerged during the second round. Given the reduced frequency of intercourse, on-demand sildenafil orodispersible film seemed the best treatment for this patient.
In the last case, involving a 67-year-old man with severe vascular damage and uncontrolled type 2 diabetes mellitus undergoing treatment with oral hypoglycemic agents (statement 15), most experts suggested re-assessing the efficacy of a previously used PDE5 inhibitor after improving metabolic control; no consensus was reached for any of the remaining items, suggesting that only some clinicians would suggest administering “tailored” treatment based on frequency of sexual intercourse and efficacy of different regimens, or switching to other forms of treatment.
Data obtained during the 20 years since the introduction of PDE5i have clarified the close correlation between ED and CV risk, as well as its association with testosterone deficiency. PDE5i are considered the first-line therapy for all subjects with ED, although their correct use in terms of starting dosage and frequency of administration, particularly in more severely affected subjects, needs further elucidation. Results from this Delphi consensus reflect the available evidence: consensus was reached only when the evidence was strong and, in the absence of solid evidence, physicians felt free to make the best choice in relation to the patient and couple’s needs and expectations.
Conclusions
The results of this Delphi consensus clearly demonstrated that, in daily practice, several recommendations from guidelines are often disregarded. Although this could be somewhat expected for some of the investigated items (eg, item 3.1, sexual counseling alone as a first-line treatment), we found that most experts do not follow guidelines on first-line therapies for naïve patients (all items from statement 3, except for 3.2), on drug switching for non-responders before suggesting more-invasive treatments (item 15.4), or even on the use of diagnostic tests (item 1.3).
Mixed results were obtained in relation to topics not entirely covered by the guidelines, such as generic equivalent drugs (item 8.2), the “rehabilitation” of erectile function with daily PDE5i (item 5.2), and the need to involve the patient’s partner in the choice of treatment (item 6.2); although there was a negative consensus for item 8.2, no consensus was reached for items 5.2 and 6.2, even after the second round of voting. The consensus on complete abstinence from alcohol, which was almost fully agreed on during the first round, underwent a dramatic change in the second round, with a 78% negative consensus (item 2.4).
Some items were unequivocally agreed on by the panelists, such as the need to investigate the patient’s metabolic and endocrine status (item 1.1), the importance of weight loss in overweight or obese men (item 1.2), and the suggestion of on-demand sildenafil orodispersible film as a first-line treatment (items 13.2 and 14.1). Likewise, a negative consensus was achieved for other items, such as penile venous ligation surgery (item 5.3) and the use of daily treatment with long-acting PDE5i in difficult patients (items 13.1 and 14.2).
In conclusion, an effort by international societies is required to improve the standards of care for patients with ED. To our knowledge, this study is the first attempt at using the Delphi method to investigate how to close the gap between recommendations and daily clinical practice in andrology. Given the prevalence of this condition and its possible repercussions on quality of life, we believe that all efforts should be made to provide a standard of care that is not only evidence-based, but also clinically feasible in all settings. Different cultural and medical backgrounds might limit the application of our findings to foreign countries, suggesting that large studies with international collaborators might be needed to precisely target the largest gaps between daily clinical practice and recommendations from guidelines.
Collaborators
Collaborators are listed below in alphabetical order: Albanesi Luca, Antomarchi Francesco, Arcaniolo Davide, Balercia Giancarlo, Barbonetti Arcangelo, Barletta Davide, Barrese Francesco, Bellastella Giuseppe, Biggio Antonio, Bitelli Marco, Botturi Alessandro, Brancato Tommaso, Branchina Antonino, Cai Tommaso, Canale Domenico, Capone Lorenzo, Capone Massimo, Carluccini Alfonso, Citarrella Roberto, Cocci Andrea, Corvese Francesco, Cozza Pietro Paolo, Creta Massimiliano, D'Andrea Settimio, Dalena Giuseppe, Damiano Rocco, Defeudis Giuseppe, Del Grasso Andrea, Delbarba Andrea, Delle Rose Augusto, Di Crosta Giuseppe, Di Filippo Aldo, Di Lena Sebastiano, Di Martino Mario, Di Millo Francesco, Di Palma Paolo, Diazzi Davide, Dicuio Mauro, Diosi Dario, Fabbri Andrea, Fattorini Giorgio, Florio Mirko, Formiconi Andrea, Franco Giorgio, Galdiero Mariano, Giambersio Antonio Marcello, Gianfrilli Daniele, Giovannone Riccardo, Granata Antonio Maria, Iafrate Massimo, Iapicca Gennaro, Iatrino Giuseppe, Ilacqua Nicola, Innocenti Flavio, Italiano Emilio, Izzo Alessandro, Izzo Pierluigi, Lamartina Marcello, Ledda Andrea Francesco, Lepri Luca, Lo Calzo Fabio, Lombardo Francesco, Luca Giovanni, Macchione Luciano, Maga Tommaso Matteo Maria, Malvestiti Gian Mario, Marella Giovanni, Maretti Carlo, Maturo Giovanni, Mazzaferro Daniele, Mazzilli Rossella, Migliorini Filippo, Milardi Domenico, Minardi Vincenzo, Moiso Andrea, Mondaini Nicola, Moretti Marco, Motta Giovanna, Nerva Franco, Pastore Antonio Luigi, Paulis Gianni, Piazza Nicola, Pili Marcello, Pistone Antonio, Pivonello Rosario, Pizzocaro Alessandro, Polverini Marco, Provinzano Vincenzo, Rastrelli Giulia, Risi Oreste, Rocchegiani Andrea, Rolle Luigi, Romanelli Francesco, Romano Giuseppe, Russo Giorgio Ivan, Salemi Giancarlo, Salzano Ciro, Sanna Federica, Sansone Andrea, Santi Daniele, Scalese Gino Alessandro, Scarano Pasquale, Scroppo Fabrizio Ildefonso, Serrao Marco Francesco, Sidoti Giuseppe, Silvestre Gianmarco, Simone Omero, Sorrentino Michelangelo, Tallis Valeria, Tammaro Rosario, Ughi Gianni, Vagnoni Valerio, Vavallo Antonio, Vecchio Daniele, Vita Angela, Zicarelli Paolo, Zucchi Alessandro.
Statement of authorship
Category 1
-
(a)Conception and Design
- Andrea M. Isidori; Bruno Giammusso; Giovanni Corona; Paolo Verze
-
(b)Acquisition of Data
- Andrea M. Isidori; Bruno Giammusso; Giovanni Corona; Paolo Verze
-
(c)Analysis and Interpretation of Data
- Andrea M. Isidori; Bruno Giammusso; Giovanni Corona; Paolo Verze
Category 2
-
(a)Drafting the Article
- Andrea M. Isidori
-
(b)Revising It for Intellectual Content
- Andrea M. Isidori; Bruno Giammusso; Giovanni Corona; Paolo Verze
Category 3
-
(a)Final Approval of the Completed Article
- Andrea M. Isidori; Bruno Giammusso; Giovanni Corona; Paolo Verze
Footnotes
Conflicts of Interest: Andrea M. Isidori has received personal fees and grants from Shire, Novartis, and Ipsen. The other authors report no conflicts of interest.
Funding: None.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.esxm.2019.04.001.
Supplementary Data
References
- 1.Hackett G., Kirby M., Wylie K. British Society for Sexual Medicine Guidelines on the Management of Erectile Dysfunction in Men-2017. J Sex Med. 2018;15:430–457. doi: 10.1016/j.jsxm.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 2.Hatzimouratidis K., Giuliano F., Moncada I. European Association of Urology; The Netherlands: 2016. EAU Guidelines on Erectile Dysfunction, Premature Ejaculation, Penile Curvature and Priapism. Arnhem. [Google Scholar]
- 3.Hatzimouratidis K., Salonia A., Adaikan G. Pharmacotherapy for Erectile Dysfunction: Recommendations From the Fourth International Consultation for Sexual Medicine (ICSM 2015) J Sex Med. 2016;13:465–488. doi: 10.1016/j.jsxm.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Porst H., Burnett A., Brock G. SOP conservative (medical and mechanical) treatment of erectile dysfunction. J Sex Med. 2013;10:130–171. doi: 10.1111/jsm.12023. [DOI] [PubMed] [Google Scholar]
- 5.Campbell S.M., Cantrill J.A., Roberts D. Prescribing indicators for UK general practice: Delphi consultation study. BMJ. 2000;321(7258):425–428. doi: 10.1136/bmj.321.7258.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMillan S.S., King M., Tully M.P. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38:655–662. doi: 10.1007/s11096-016-0257-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boulkedid R., Abdoul H., Loustau M. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS One. 2011;6:e20476. doi: 10.1371/journal.pone.0020476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avella J.R. Delphi panels: Research design, procedures, advantages, and challenges. Int J Doctoral Stud. 2016;11:305–321. [Google Scholar]
- 9.Dalkey N., Brown B., Cochran S. RAND Corporation; Santa Monica, CA: 1969. The Delphi Method, III: Use of self ratings to improve group estimates. [Google Scholar]
- 10.Jiann B.-P. Effect of alcohol consumption on the risk of erectile dysfunction. Urol Sci. 2010;21:163–168. [Google Scholar]
- 11.Yafi F.A., Jenkins L., Albersen M. Erectile dysfunction. Nat Rev Dis Primers. 2016;2:16003. doi: 10.1038/nrdp.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmidt H.M., Munder T., Gerger H. Combination of psychological intervention and phosphodiesterase-5 inhibitors for erectile dysfunction: A narrative review and meta-analysis. J Sex Med. 2014;11:1376–1391. doi: 10.1111/jsm.12520. [DOI] [PubMed] [Google Scholar]
- 13.Lee K.C., Brock G.B. Daily dosing of PDE5 inhibitors: Where does it fit in? Curr Urol Rep. 2013;14:269–278. doi: 10.1007/s11934-013-0342-9. [DOI] [PubMed] [Google Scholar]
- 14.Corona G., Razzoli E., Forti G. The use of phosphodiesterase 5 inhibitors with concomitant medications. J Endocrinol Invest. 2008;31:799–808. doi: 10.1007/BF03349261. [DOI] [PubMed] [Google Scholar]
- 15.Colonna P., Andreotti F., Ageno W. Clinical conundrums in antithrombotic therapy management: A Delphi Consensus panel. Int J Cardiol. 2017;249:249–256. doi: 10.1016/j.ijcard.2017.09.159. [DOI] [PubMed] [Google Scholar]
- 16.Vlachopoulos C.V., Terentes-Printzios D.G., Ioakeimidis N.K. Prediction of cardiovascular events and all-cause mortality with erectile dysfunction: A systematic review and meta-analysis of cohort studies. Circ Cardiovasc Qual Outcomes. 2013;6:99–109. doi: 10.1161/CIRCOUTCOMES.112.966903. [DOI] [PubMed] [Google Scholar]
- 17.Maseroli E., Corona G., Rastrelli G. Prevalence of endocrine and metabolic disorders in subjects with erectile dysfunction: A comparative study. J Sex Med. 2015;12:956–965. doi: 10.1111/jsm.12832. [DOI] [PubMed] [Google Scholar]
- 18.Sansone A., Romanelli F., Gianfrilli D. Endocrine evaluation of erectile dysfunction. Endocrine. 2014;46:423–430. doi: 10.1007/s12020-014-0254-6. [DOI] [PubMed] [Google Scholar]
- 19.Allen M.S., Walter E.E. Health-related lifestyle factors and sexual dysfunction: A meta-analysis of population-based research. J Sex Med. 2018;15:458–475. doi: 10.1016/j.jsxm.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Boddi V., Corona G., Monami M. Priapus is happier with Venus than with Bacchus. J Sex Med. 2010;7:2831–2841. doi: 10.1111/j.1743-6109.2010.01887.x. [DOI] [PubMed] [Google Scholar]
- 21.Seftel A.D. Phosphodiesterase type 5 inhibitor differentiation based on selectivity, pharmacokinetic, and efficacy profiles. Clin Cardiol. 2004;27(Suppl. 1):I14–I19. doi: 10.1002/clc.4960271305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright P.J. Comparison of phosphodiesterase type 5 (PDE5) inhibitors. Int J Clin Pract. 2006;60:967–975. doi: 10.1111/j.1742-1241.2006.01049.x. [DOI] [PubMed] [Google Scholar]
- 23.Wang R., Burnett A.L., Heller W.H. Selectivity of avanafil, a PDE5 inhibitor for the treatment of erectile dysfunction: Implications for clinical safety and improved tolerability. J Sex Med. 2012;9:2122–2129. doi: 10.1111/j.1743-6109.2012.02822.x. [DOI] [PubMed] [Google Scholar]
- 24.Chen L., Staubli S.E., Schneider M.P. Phosphodiesterase 5 inhibitors for the treatment of erectile dysfunction: A trade-off network meta-analysis. Eur Urol. 2015;68:674–680. doi: 10.1016/j.eururo.2015.03.031. [DOI] [PubMed] [Google Scholar]
- 25.Limoncin E., Gravina G.L., Corona G. Erectile function recovery in men treated with phosphodiesterase type 5 inhibitor administration after bilateral nerve-sparing radical prostatectomy: A systematic review of placebo-controlled randomized trials with trial sequential analysis. Andrology. 2017;5:863–872. doi: 10.1111/andr.12403. [DOI] [PubMed] [Google Scholar]
- 26.Santi D., Giannetta E., Isidori A.M. Therapy of endocrine disease. Effects of chronic use of phosphodiesterase inhibitors on endothelial markers in type 2 diabetes mellitus: A meta-analysis. Eur J Endocrinol. 2015;172:R103–R114. doi: 10.1530/EJE-14-0700. [DOI] [PubMed] [Google Scholar]
- 27.Corona G., Maggi M., Jannini E.A. EDEUS, a real-life study on the users of phosphodiesterase type 5 inhibitors: Prevalence, perceptions, and health care-seeking behavior among European men with a focus on 2nd-generation Avanafil. Sex Med. 2018;6:15–23. doi: 10.1016/j.esxm.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith W.B., 2nd, McCaslin I.R., Gokce A. PDE5 inhibitors: Considerations for preference and long-term adherence. Int J Clin Pract. 2013;67:768–780. doi: 10.1111/ijcp.12074. [DOI] [PubMed] [Google Scholar]
- 29.Shamloul R., Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153–165. doi: 10.1016/S0140-6736(12)60520-0. [DOI] [PubMed] [Google Scholar]
- 30.Carvalheira A.A., Pereira N.M., Maroco J. Dropout in the treatment of erectile dysfunction with PDE5: A study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med. 2012;9:2361–2369. doi: 10.1111/j.1743-6109.2012.02787.x. [DOI] [PubMed] [Google Scholar]
- 31.Corona G., Rastrelli G., Burri A. First-generation phosphodiesterase type 5 inhibitors dropout: A comprehensive review and meta-analysis. Andrology. 2016;4:1002–1009. doi: 10.1111/andr.12255. [DOI] [PubMed] [Google Scholar]
- 32.Ahmad F., Murata T., Shimizu K. Cyclic nucleotide phosphodiesterases: important signaling modulators and therapeutic targets. Oral Dis. 2015;21:e25–e50. doi: 10.1111/odi.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salonia A., Adaikan G., Buvat J. Sexual rehabilitation after treatment for prostate cancer—Part 1: Recommendations from the Fourth International Consultation for Sexual Medicine (ICSM 2015) J Sex Med. 2017;14:285–296. doi: 10.1016/j.jsxm.2016.11.325. [DOI] [PubMed] [Google Scholar]
- 34.Nehra A., Jackson G., Miner M. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clin Proc. 2012;87:766–778. doi: 10.1016/j.mayocp.2012.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


