Abstract
Introduction
The objective of this study was to define current assistive technology and telecare (ATT) practice for people with dementia living at home.
Methods
This is a randomized controlled trial (N = 495) of ATT assessment and ATT installation intervention, compared with control (restricted ATT package). ATT assessment and installation data were collected. Qualitative work identified value networks delivering ATT, established an ATT assessment standard.
Results
ATT was delivered by public and not-for-profit telecare networks. ATT assessments showed 52% fidelity to the ATT assessment standard. Areas of assessment most frequently leading to identifying ATT need were daily activities (93%), memory (89%), and problem-solving (83%). ATT needs and recommendations were weakly correlated (τ = 0.242; P < .000), with ATT recommendations and installations moderately correlated (τ = −0.470; P < .000). Half (53%) of recommended technology was not installed. Safety concerns motivated 38% of installations.
Discussion
Assessment recommendations were routinely disregarded at the point of installation. ATT was commonly recommended for safety and seldom for supporting leisure.
Keywords: Dementia, Assistive technology, Telecare, ATTILA, Assessment of need, Community-dwelling
1. Background
Approximately 46.8 million people are living with dementia worldwide [1]. As the disease progresses, it can be a challenge for people with dementia to live safely in their own homes [2]. Assistive technology and telecare (ATT) offer a means of managing the risks facing older people with dementia who wish to remain living independently at home. The first use of electronic ATT in the UK was to provide support for people with dementia and their caregivers [3]. Within a decade, interest in ATT prompted the development of a Department of Health strategy [4] and, increasingly, ATT moved into the mainstream. However, as interest in ATT has increased, the specific focus on its application for those living with dementia has diminished [5]. Early studies of ATT for dementia highlighted the importance of assessment [6] to construct a sufficiently detailed picture of an individual's life to enable assistive technology to meet needs and maximize good outcomes [7], [8]. However, to date, there is scant evidence on the effectiveness of usual ATT provision and associated practices for people with dementia. The Assistive Technology and Telecare to maintain Independent Living At home for people with dementia (ATTILA) trial was a pragmatic randomized controlled trial, comparing outcomes for people with dementia receiving ATT and those receiving equivalent community services but not ATT [9].
1.1. Aim
A detailed exploration of the intervention under investigation is needed to give insight into the fidelity of the intervention and to allow for replication [10].We aimed to provide an investigation of routine ATT practice and the systems in place to deliver ATT for people with dementia.
2. Method
We adhered to the Template for Intervention Description and Replication (TIDieR) [11] in describing the components of the ATTILA intervention, in terms of what happened, who was involved, how, where, and when did the intervention happen, how much was provided, and whether it was tailored to participants.
2.1. Assistive technology and telecare
The ATT intervention was defined for the purposes of the ATTILA trial as a two-stage process:
-
1.
an ATT assessment, with subsequent ATT recommendation(s),
-
2.
the installation of ATT devices alongside monitoring services as appropriate.
ATT devices included simple, battery-operated, stand-alone technologies, and/or telecare, that is, a range of devices and sensors, which communicate and relay messages to an external call center where an appropriate response is arranged. Participants were randomized to receive an ATT assessment followed by either installation of ATT as indicated by the assessment (intervention arm), or an ATT package restricted to only nonmonitored smoke and carbon monoxide detectors and pendant alarm (control arm) [9].
2.2. Participants
People with either a diagnosis of dementia (early or late onset) or evidence of cognitive difficulties suggesting presence of dementia were eligible for ATTILA. Those lacking capacity could participate with the consent of a personal consultee. In addition, participants had to meet eligibility criteria for access to social care services, live in an ordinary community dwelling (including sheltered accommodation) and have a working telephone line at home. Exclusions from the study included having already received ATT (excluding smoke, carbon monoxide, or pendant alarms); having previously received ATT and not used it; or having a perceived urgent need for a package of care [9].
2.3. ATT delivery systems
To describe the delivery systems for ATT deployment, interviews were conducted by C.H. with key informants from local authority operational/commissioning teams and telecare monitoring center managers in the seven sites from which most trial participants were recruited (N = 484). Invitations were sent to 21 potential key informants, resulting in 14 interviews covering six sites (no key informants were available for interview in one site) between June and September 2016. Interviews were not recorded but written notes were taken; interviewees were also asked for supporting documentation that might help to understand the policies and procedures in relation to ATT deployment. Data were also collected on ATT assessment and delivery processes via pro formas completed by local researchers in 2015 and via a follow-up desk-based search in 2017. Data were examined using NVIVO qualitative data analysis software (version 11) by C.H. Data were first structured into five production stages within a framework analysis [12]: assessment, equipment procurement/ordering, installation, call monitoring, and response to sensor activations. To identify commonalities in local systems for delivering ATT to trial participants, we took an approach based on value network role analysis [13], [14]. Production inputs and processes observed in each site were mapped onto value network frameworks.
2.4. Baseline participant characteristics
Local trial researchers collected data on characteristics of participants (age, gender, ethnic background, marital status, living situation [living with another, living alone], and caregivers (ethnic background, marital status, caregiver). They completed Standardized Mini–Mental State Examinations (SMMSE) [15] with participants, and rated participants' risk of wandering (low, moderate, high), and safety risk within the home (low, moderate, high).
2.5. Local baseline ATT assessments/recommendations
We assumed that Social Services Departments in each ATTILA site had distilled local and national guidelines on best practice in ATT assessment when constructing local assessment templates. To establish a practice standard for ATT assessments in the ATTILA sites, ATT assessment templates and guidance were sourced from each site between August 2013 and August 2016. Sites were asked to resend documentation if there were changes during the lifetime of the study; as a result, two sets of new documentation were submitted. Framework analysis [12] to identify common assessment themes across sites was applied to this documentation (by K.F.), using the Model of Human Occupation Screening Tool [16]. The Model of Human Occupation Screening Tool is designed to detail people's values, insight, interests, routines, communication, cognitive and physical skills, and physical and social environment to gain a detailed picture of an individual's life. The resultant ATT assessment standard consisted of a set of 14 ATT assessment areas (see Supplementary Materials 1). A four-point scale was developed for each assessment area within the ATT assessment standard, where 4 = no risk when doing daily activity, 3 = mostly risk free when doing daily activity, 2 = some risk when doing daily activity, and 1 = significant multiple risks when doing daily activity. Specific definitions were developed for rating each assessment area (see Supplementary Materials 2). ATT needs were identified when an assessment area received a rating of 1 (significant multiple risks when doing daily activity) or 2 (some risk when doing daily activity).
Locally completed ATT assessments for each participant were reviewed against the ATT assessment standard to assess whether these addressed the ATT assessment areas identified by the templates across ATTILA sites. Fidelity to this standard was determined by two trial practitioners with experience in dementia care and ATT assessment (K.F., E.C.), who independently classified the content of each locally completed ATT assessment against the ATT assessment standard and assigned risk-ratings. They then reviewed ratings together and resolved discrepancies.
There is no recognized taxonomy of ATT for people with dementia; therefore, a taxonomy was developed in collaboration with Trent Dementia Services Development Centre and the “atdementia” initiative (www.atdementia.org.uk), an independent online ATT resource. This taxonomy was then developed into two identical Technology Checklist forms (one for recommended ATT and one for installed ATT) which covered the following ATT functions: (1) reminder or prompting devices; (2) devices to support safety; (3) safer walking technologies; (4) communication devices and (5) devices that support meaningful use of leisure time; (6) monitoring and response information. The form also recorded data about which type of assessor had assessed for ATT (ATT assessor, health or social care professional, other), method of assessment (in-person at-home, in-person not-at-home, telephone assessment, using case notes, other), whether ATT was monitored (yes/no), who would respond to ATT alerts (direct to responder or via a call center). Two trial practitioners with experience in dementia care and ATT assessment (K.F., B.D.) collaboratively classified each device recommended within the locally completed ATT needs assessment using the technology checklist (for recommended ATT).
2.6. Trial instruments (week 12–104)
Local trial researchers administered the Technology Checklist (for installed ATT) during home visits at weeks 12, 24, 52, and 104.
2.7. Statistical analyses
Categorical data were summarized in percentages and numbers of observations. Correlations between count variables were tested using nonparametric methods (Kendall Tau Rank Correlation Coefficient τ). The Kruskal-Wallis test was used to assess if there were statistically significant differences between multiple groups for outcomes. Freidman's test was used to determine significance of change over time in the count variables. In the case of categorical variables, differences between observed and expected frequencies were tested using Pearson's chi square test for independence, or alternatively Fisher's exact test, when the assumption of minimum expected cell count in contingency tables was not met [17]. SMMSE scores were categorized into stages of dementia [18] for the purposes of analysis (30 = no dementia, 26–29 = questionable dementia, 21–25 = mild dementia, 11–20 = moderate dementia, 0–10 = severe dementia). Effective tailoring of the intervention was described through the strength of the correlation [19] between ATT needs and ATT recommendations at the baseline and between ATT recommendations and ATT installation by 24 weeks. We also compared the ATT recommended in the baseline assessment with subsequent installations for each participant in the intervention arm up to 24 weeks. Any installation after 24 weeks was considered unrelated to the baseline ATT assessment.
2.8. Ethical approval
The ATTILA trial was approved by the NHS Health Research Authority National Research Ethics Committee (REC reference number 12/LO/186) and is registered with the ISRCTN (http://www.controlled-trials.com/ISRCTN86537017).
3. Results
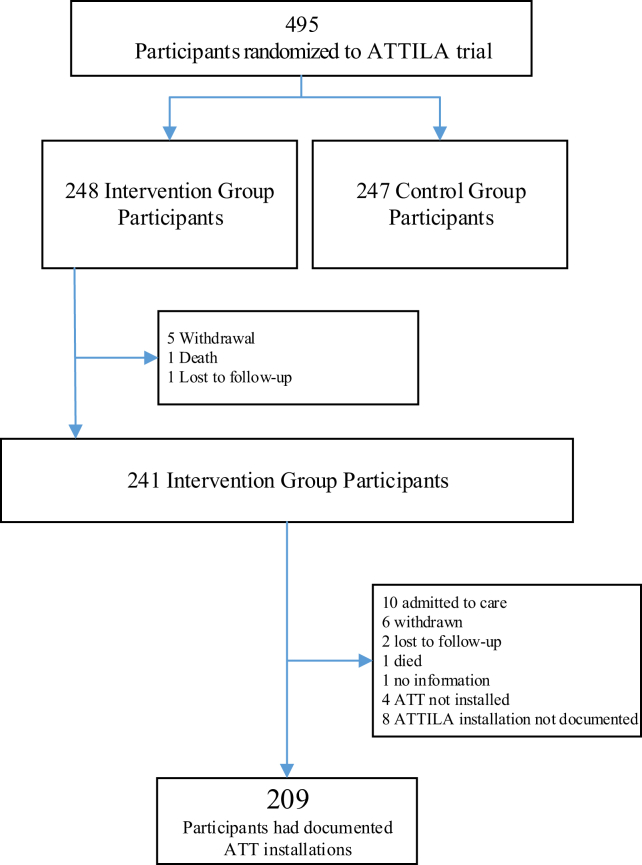
In total, 495 people were randomized into the ATTILA trial between August 2013 and October 2016 (247 control, 248 intervention). Most participants were >80 years old, female, widowed, white British, did not live alone, had moderate dementia, were at low risk for wandering, and of being considered a safety risk within the home. Most caregivers were aged over 65 years, married, and spouses or daughters of participants (Table 1). Of the 451 documented baseline ATT assessments available, 413 contained an ATT recommendation. Of the 248 participants recruited to the intervention arm, data from 209 participants was available for analysis of ATT installations (Fig. 1).
Table 1.
Participants' baseline characteristics
| Characteristic | Participants, N (%) |
|---|---|
| Age | |
| <65 years | 15/495 (3) |
| 65–80 years | 182/495 (37) |
| >80 years | 298/495 (60) |
| Gender | |
| Male | 205/495 (41) |
| Female | 290/495 (59) |
| Stage of dementia (SMMSE) | |
| Severe | 59/495 (12) |
| Moderate | 179/495 (36) |
| Mild | 126/495 (25) |
| Questionable | 51/495 (10) |
| No | 0/495 (0) |
| Incomplete responses | 80/495 (16) |
| Marital status of the participant | |
| Single (never married) | 25/495 (5) |
| Married | 191/495 (39) |
| Cohabiting | 8/495 (2) |
| Civil partnership | 0/495 (0) |
| Separated | 5/495 (1) |
| Divorced | 22/495 (4) |
| Widowed | 196/495 (40) |
| Blank | 17/495 (3) |
| Ethnic background of the participant | |
| White British | 357/495 (72) |
| White Irish | 10/495 (2) |
| Other white background | 13/495 (3) |
| Black or black British—Caribbean | 45/495 (9) |
| Black or black British—African | 10/495 (2) |
| Other Black Background | 0/495 (0) |
| Asian or Asian British—Indian | 9/495 (2) |
| Asian or Asian British—Pakistani | 0/495 (0) |
| Asian or Asian British—Bangladeshi | 0/495 (0) |
| Chinese | 1/495 (0) |
| Other Asian background | 4/495 (1) |
| Mixed—white and black Caribbean | 0/495 (0) |
| Mixed—white and black African | 0/495 (0) |
| Mixed—white and Asian | 1/495 (0) |
| Other—mixed background | 4/495 (1) |
| Other ethnic background | 6/495 (1) |
| Blank | 4/495 (1) |
| Living situation | |
| Living with other | 267/495 (54) |
| Living alone | 228/495 (46) |
| Risk of wandering | |
| Low | 358/495 (72) |
| Moderate | 100/495 (20) |
| High | 37/495 (7) |
| Safety risk within the home | |
| Low | 249/495 (50) |
| Moderate | 205/495 (41) |
| High | 41/495 (8) |
| Caregiver age | |
| <65 years | 223/495 (45) |
| 65–80 years | 113/495 (23) |
| 80 + years | 48/495 (10) |
| Blank | 111/495 (22) |
| Caregiver details | |
| Live-in caregiver | 240/495 (48) |
| Caregiver visits at least once/day | 122/495 (25) |
| Caregiver visits less than once/day | 133/495 (27) |
| Marital status of the caregiver | |
| Single (never married) | 59/495 (12) |
| Married | 309/495 (62) |
| Cohabiting | 25/495 (5) |
| Civil partnership | 0/495 (0) |
| Separated | 4/495 (1) |
| Divorced | 35/495 (7) |
| Widowed | 10/495 (2) |
| Blank | 22/495 (4) |
| Relationship of caregiver to participant | |
| Wife/husband | 160/495 (32) |
| Partner | 10/495 (2) |
| Daughter | 153/495 (31) |
| Son | 84/495 (17) |
| Daughter in law | 10/495 (2) |
| Son in law | 1/495 (0) |
| Sister | 2/495 (0) |
| Brother | 2/495 (0) |
| Other relative | 26/495 (5) |
| Neighbor | 5/495 (1) |
| Friend | 7/495 (1) |
| Other | 4/495 (1) |
Abbreviation: SMMSE, Standardized Mini–Mental State Examinations.
Fig. 1.
Cases available for analysis of ATT installations. Abbreviations: ATT, assistive technology and telecare; ATTILA, Assistive Technology and Telecare to maintain Independent Living At home for people with dementia.
3.1. Value networks
Networks delivering services (offering value) to ATTILA participants were classified into two types (Supplementary Materials 3a and 3b). First, “public telecare provider networks” (N = 4), where two assessor roles were identified: the ATT assessor, and the authorized (or trusted) assessor (Health or Social Care Professional). ATT assessors were employed by public agencies (NHS or Councils with Adults Social Services Responsibilities—CASSRs); their primary role was to assess for a full range of ATT devices (“networked”—monitored by a telecare call center or unpaid caregiver; or “standalone”). Authorized assessors could offer first-generation telecare (pendant-only systems) or straightforward ATT (for instance, adding on an additional sensor or providing a memo minder) depending on their level of experience and local permissions; they performed ATT assessment as a secondary role. In these networks, most or all of the ATT infrastructure for procurement, installation, stock control, and maintenance of ATT devices fell to units within the CASSR. Second, there were “not-for-profit provider networks” (NFP) (N = 3). Three assessor roles were identified across these “NFP telecare networks”. Telecare assessors working for NFP telecare providers assessed for AT that was networked to providers' call-monitoring centers. Assessment for standalone AT fell to assessors within the CASSR. A “social care ATT assessor” role was also identified: these assessors could assess for ATT (networked/standalone) and work with a choice of suppliers to procure and arrange installation of ATT devices. Private companies offered combinations of procurement and stock control, installation and maintenance services to the NFP telecare providers.
3.2. Locally completed ATT assessments/recommendations at the baseline
The local ATT assessment fidelity with the ATT assessment standard was 52% (7.2 assessment areas were addressed per assessment) (Table 2). Of ATT assessments reviewed, 99/451 (22%) addressed 0-2 areas of assessment. There was higher fidelity to assessment areas relating to “mobility” (74%), “social support” (72%), “daily activity” (71%), and “memory” (71%). Fidelity varied across sites: the mean number of assessment areas addressed ranged from 2 to 13 per site (P < .000) with public telecare providers addressing more assessment areas than not-for-profit telecare providers (P < .026). Health and social care (HSC) professionals addressed more assessment areas than ATT assessors (P < .046). Fidelity varied across assessment methods (P < .000), with the in-person at-home assessment method addressing more assessment areas than in-person but not-at-home (P = .003), telephone assessment (P < .000), and case notes methods (P = .003). Women had more assessment areas addressed than men (P = .027). More assessment areas were addressed for participants at medium risk of wandering than for participants at low risk of wandering (P = .028).
Table 2.
Fidelity with ATT assessment standard and identified ATT needs
| Sites ATT assessment areas/standard | Fidelity with ATT assessments standard | ATT needs (i.e., responses rated as some risk or significant multiple risk) | ||
|---|---|---|---|---|
| 1. Insight | 241/451 | 53% | 151/241 | 63% |
| 2. Values | 245/451 | 54% | 100/245 | 41% |
| 3. Wandering/disorientation | 284/451 | 63% | 219/284 | 77% |
| 4. Daily activity | 321/451 | 71% | 298/321 | 93% |
| 5. Conversation | 226/451 | 50% | 100/226 | 44% |
| 6. Express needs | 175/451 | 39% | 24/175 | 14% |
| 7. Memory | 320/451 | 71% | 284/320 | 89% |
| 8. Problem-solving | 218/451 | 48% | 181/218 | 83% |
| 9. Mobility | 335/451 | 74% | 224/335 | 67% |
| 10. Grip/dexterity | 147/451 | 33% | 18/147 | 12% |
| 11. Space | 140/451 | 31% | 47/140 | 34% |
| 12. Resources | 128/451 | 28% | 26/128 | 20% |
| 13. Social support | 325/451 | 72% | 183/325 | 56% |
| 14. The way the activity completed | 162/451 | 36% | 118/162 | 73% |
| Total responses | 3267/6314 | 52% | 1973/3267 | 60% |
| Fidelity with ATT assessments standard |
Number ATT needs |
|||||
|---|---|---|---|---|---|---|
| Median | Mean | % | Median | Mean | % | |
| Participant characteristics | ||||||
| Gender | ||||||
| Female | 8 | 7.67 | 62 | 4 | 4.46 | 60 |
| Male | 5 | 6.65 | 38 | 3 | 4.25 | 40 |
| P = .027 | P = .337 | |||||
| Risk of wandering | ||||||
| Low | 7 | 6.93 | 70 | 4 | 4.10 | 68 |
| Medium | 9 | 8.37 | 23 | 5 | 5.04 | 23 |
| High | 6 | 7.24 | 7 | 4 | 5.24 | 9 |
| P = .038 | P = .005 | |||||
| SMMSE score (18) | ||||||
| Questionable dementia (26–29) | 7 | 7.22 | 13 | 3 | 3.38 | 10 |
| Mild dementia (21–25) | 7 | 6.6 | 27 | 4 | 3.9 | 27 |
| Moderate dementia (11–20) | 7 | 7.38 | 45 | 4 | 4.27 | 44 |
| Severe dementia (0–10) | 8.5 | 7.96 | 15 | 5.5 | 5.79 | 19 |
| P = .309 | P < .000 | |||||
| Assessment characteristics | ||||||
| Assessors | ||||||
| Health and social care professionals | 8 | 7.85 | 68 | 4 | 4.66 | 67 |
| ATT assessor | 5.5 | 6.51 | 29 | 3 | 3.86 | 29 |
| P = .051 | P = .028 | |||||
| Assessment method | ||||||
| In person at home | 10 | 9.14 | 85 | 5 | 5.06 | 82 |
| In person not at home | 5 | 6.43 | 8 | 3 | 3.38 | 8 |
| Telephone | 2 | 3.42 | 6 | 2 | 2.71 | 9 |
| Case notes | 3 | 3.33 | 1 | 2.5 | 3 | 1 |
| P < .000 | P < .000 | |||||
| Service structure | ||||||
| Public telecare provider | 7 | 7.59 | 73 | 4 | 4.41 | 70 |
| Not-for-profit telecare provider | 6 | 6.41 | 25 | 4 | 4.31 | 28 |
| P = .026 | P = 1.00 | |||||
| Mean fidelity with ATT assessment standard per participant | Mean number of responses per participant rated as an ATT need | |||||
| 7.2 assessment areas addressed (0–13) | 4.4 ATT needs (0–12) | |||||
Abbreviations: ATT, assistive technology and telecare; SMMSE, Standardized Mini–Mental State Examinations.
In total, 60% of assessment responses identified an ATT need, with 4.4 ATT needs (range 0–12) identified per participant (Table 2). The mean number of ATT needs identified varied, ranging from 2 to 6 per site (P < .000). Areas of concern most frequently identified as triggering the need for ATT were daily activities (93%), memory (89%), and problem-solving (83%). HSC professionals identified more ATT needs than did ATT assessors (P = .047). More ATT needs were identified by in-person-home than by telephone assessment methods (P < .000). There was no significant difference between ATT needs in men and women (P = .337). The number of ATT needs identified for each participant differed depending on the levels of wandering risk (P = .005), with medium risk of wandering associated with more ATT needs than in the case of low risk of wandering (P = .016). ATT needs varied by category of SMMSE score (P < .000): participants with severe dementia had more ATT needs than those with mild (P < .000), moderate (P = .002), and questionable dementia (P < .000).
A documented ATT recommendation was given for 413 participants with 1090 ATT devices recommended at the baseline, with a mean of three devices (range 1–14 devices). One or two ATT devices were recommended for 57% (235) of participants. The correlation between the ATT needs and ATT recommendations identified in local ATT assessments was weak (τ = 0.242; P < .000). Most recommendations were for safety-related devices (59%; 644/1090), followed by reminder/prompting devices (25%; 269/1090). Sixty-two percent (673/1090) of recommended ATT devices required monitoring; and 67% (353/526) of monitored devices with an identified responder required a formal (call center) response.
3.3. Recommendations and installations at follow-up (intervention arm only)
By 24 weeks, a mean of 3.5 devices were recommended for participants in the intervention arm. Of the ATT devices recommended, 53% (306/572) were not installed. However, 62% (438/704) of the ATT devices installed had not been recommended in the baseline assessment (Table 3). There was a moderate negative correlation between number of recommendations and number of installations per participant per ATT category (τ = −0.470; both P < .000).
Table 3.
Recommended ATT devices matched to ATT devices installed at 24 weeks (intervention arm only)
| ATT technology checklist | ATT recommended, N (%) | ATT recommended + installed at 24 wks. N (%) | ATT recommended + not installed, N (%)∗ | ATT installed at 24 wks. N (%) | ATT not recommended + installed N (%) |
|---|---|---|---|---|---|
| Control group technology | |||||
| Pendant alarm | 44/572 (8) | 22/44 (50) | 22/44 (50) | 89/704 (13) | 67/89 (75) |
| Non-monitored smoke detector | 0/572 (0) | 0 (0) | 0 (0) | 68/704 (10) | 68/68 (100) |
| Nonmonitored carbon monoxide | 1/572 (0) | 0/1 (0) | 1 (100) | 36/704 (5) | 36/36 (100) |
| Key safe | 18/572 (3) | 9/18 (50) | 9/18 (50) | 89/704 (13) | 80/89 (90) |
| Activity monitors assessment only | 8/572 (1) | 4/8 (50) | 4/8 (50) | 5/704 (1) | 1/5 (20) |
| Other devices | 1/572 (0) | 0/1 (0) | 1/1 (100) | 6/704 (1) | 6/6 (100) |
| Intervention group technology | |||||
| Reminder or prompting devices | |||||
| Date and time reminders | 31/572 (5) | 13/31 (42) | 18/31 (58) | 46/704 (7) | 33/46 (72) |
| Item locator devices | 9/572 (2) | 8/9 (89) | 1/9 (11) | 11/704 (2) | 3/11 (27) |
| Medication reminders/dispensers | 56/572 (10) | 25/56 (45) | 31/56 (55) | 33/704 (5) | 8/33 (24) |
| Voice recorders and memo minders | 46/572 (8) | 27/46 (59) | 19/46 (41) | 38/704 (5) | 11/38 (29) |
| Other reminder/prompting devices | 1/572 (0) | 0/1 (0) | 1/1 (100) | 6/704 (1) | 6/6 (100) |
| Devices to promote safety | |||||
| Activity monitors—on-going monitoring | 5/572 (1) | 1/5 (20) | 4/5 (80) | 6/704 (1) | 5/6 (83) |
| Fall detectors | 75/572 (13) | 31/75 (41) | 44/75 (59) | 53/704 (8) | 22/53 (42) |
| Continence management devices | 1/572 (0) | 1/1 (100) | 0/1 (0) | 1/704 (0) | 0/1 (0) |
| Alarm and pager units | 5/572 (1) | 2/5 (40) | 3/5 (60) | 5/704 (1) | 3/5 (60) |
| Flood detectors and water temperature monitor | 14/572 (2) | 9/14 (64) | 5/14 (36) | 11/704 (2) | 2/11 (18) |
| Gas detectors | 21/572 (4) | 8/21 (38) | 13/21 (62) | 19/704 (3) | 11/19 (58) |
| Monitored carbon monoxide detectors | 25/572 (4) | 8/25 (32) | 17/25 (68) | 22/704 (3) | 14/22 (64) |
| Monitored smoke detectors | 59/572 (10) | 39/59 (66) | 20/59 (34) | 47/704 (7) | 8/47 (17) |
| Monitored extreme temperature sensors | 26/572 (5) | 18/26 (42) | 15/26 (58) | 19/704 (3) | 8/19 (42) |
| Lighting devices | 2/572 (0) | 1/2 (50) | 1/2 (50) | 8/704 (1) | 7/8 (88) |
| Other safety and security devices | 15/572 (3) | 2/15 (13) | 13/15 (87) | 9/704 (1) | 7/9 (78) |
| Safer walking technologies | |||||
| To locate the user | 43/572 (8) | 20/43 (47) | 23/43 (53) | 28/704 (4) | 8/28 (29) |
| To alert the responder to movement | 59/572 (10) | 25/59 (42) | 34/59 (58) | 37/704 (5) | 12/37 (32) |
| Communication devices | |||||
| Intercoms | 2/572 (0) | 0/2 (0) | 2/2 (100) | 1/704 (0) | 1/1 (100) |
| Telephones | 3/572 (1) | 0/3 (0) | 3/3 (100) | 7/704 (1) | 7/7 (100) |
| Communication aids | 0/572 (0) | 0/0 (0) | 0/0 (0) | 1/704 (0) | 1/1 (100) |
| Other communication devices | 1/572 (0) | 0/1 (0) | 1/1 (100) | 0/704 (0) | 0/0 (0) |
| Devices that support meaningful use of leisure time | |||||
| Computer aids | 0/572 (0) | 0/0 (0) | 0/0 (0) | 0 (0) | 0 (0) |
| Dementia friendly TV/radio/music players | 0/572 (0) | 0/0 (0) | 0/0 (0) | 0 (0) | 0 (0) |
| Electronic photo albums/electronic reminiscence aids | 0/572 (0) | 0/0 (0) | 0/0 (0) | 0 (0) | 0 (0) |
| Electronic games | 0/5572 (0) | 0/0 (0) | 0/0 (0) | 1/551 (0) | 1/1 (100) |
| Other devices—support meaningful use of leisure time | 1/572 (0) | 0/1 (0) | 1/1 (100) | 2/551 (0) | 2/2 (100) |
| Total | 572 | 266/572 (47)∗ | 306/572 (53) | 704 | 438/704 (62) |
Abbreviation: ATT, assistive technology and telecare.
ATT installed at any time point up to 24 weeks; if all ATT recommended was installed percentage would be 100%.
3.4. Week 12-104, ATT installed (intervention arm only)
By week 104, there were 888 ATT devices installed for 209 participants in the intervention arm, a mean of 4.2 devices per participant (range 1–15). Of devices installed for intervention participants (Table 4), 42% (374/888) of those involved the types of technology provided to control arm participants (e.g., nonmonitored smoke detectors). Installations decreased over time (P < .031) with 79% (704/888) of ATT installed by week 24. Intervention participants' ATT devices were most frequently installed for safety reasons (38%) or for reminder/prompting (18%). ATT assessors were most frequently identified as having assessed for the installed devices (32%), followed by HSC professionals (20%) but 40% of assessors' backgrounds were unknown. While 41% of installations followed an in-person home visit (41%), in many cases the participants could not report the method of assessment (42%). Nearly half (47%) of the ATT devices installed required monitoring; 38% of monitored devices were networked to a call center (so that any alerts would receive an initial response from paid services).
Table 4.
ATT installations 12 wks–104 wks (for intervention arm only)
| Installation variables | 12 wks | 24 wks | 52 wks | 104 wks | Total (12wks–104 wks) |
|---|---|---|---|---|---|
| Control group technology installed | |||||
| Basic ATT | 235/580 (41%) | 58/124 (47%) | 45/87 (52%) | 36/97 (37%) | 374/888 (42%) |
| Intervention technology installed | |||||
| Reminder/prompting | 116/580 (20%) | 18/124 (15%) | 9/87 (10%) | 17/97 (18%) | 160/888 (18%) |
| Safety | 220/580 (38%) | 45/124 (36%) | 30/87 (35%) | 43/97 (44%) | 338/888 (38%) |
| Communication | 8/580 (1%) | 1/124 (0%) | 2/87 (2%) | 1/97 (1%) | 12/888 (2%) |
| Support leisure time | 1/580 (0%) | 2/124 (2%) | 1/87 (1%) | 0/97 (0%) | 4/888 (0%) |
| Any other devices | 0/580 (0%) | 0/124 (0%) | 0/87 (0%) | 0/97 (0%) | 0/888 (0%) |
| Total installed | 580 | 124 | 87 | 97 | 888 |
| Assessor | |||||
| Health/social care professionals | 126/580 (22%) | 20/124 (16%) | 13/87 (15%) | 17/97 (18%) | 176/888 (20%) |
| ATT assessor | 152/580 (26%) | 58/124 (47%) | 23/87 (26%) | 45/97 (46%) | 278/888 (32%) |
| Other | 68/580 (12%) | 0/124 (0%) | 3/87 (4%) | 4/97 (4%) | 75/888 (8%) |
| Unknown | 234/580 (40%) | 46/124 (37%) | 48/87 (55%) | 31/97 (32%) | 359/888 (40%) |
| Total installed | 580 | 124 | 87 | 97 | 888 |
| Assessment method | |||||
| In person at home | 216/580 (37%) | 70 (57%) | 30 (34%) | 55 (57%) | 371/888 (41%) |
| In person not at home | 7/580 (1%) | 3 (2%) | 1 (1%) | 4 (4%) | 15/888 (2%) |
| Telephone | 50/580 (9%) | 4 (3%) | 1 (1%) | 4 (4%) | 59/888 (7%) |
| Using case notes | 7/580 (1%) | 0 (0%) | 0 (0%) | 2 (2%) | 9/888 (1%) |
| Other | 56/580 (10%) | 1 (1%) | 2 (2%) | 0 (0%) | 59/888 (7%) |
| Unknown | 244/580 (42%) | 46 (37%) | 53 (61%) | 32 (33%) | 375/888 (42%) |
| Total installed | 580 | 124 | 87 | 97 | 888 |
| Monitoring | |||||
| Yes | 292/580 (51%) | 56/124 (45%) | 32/87 (37%) | 42/97 (43%) | 422/888 (47%) |
| No | 147/580 (25%) | 45/124 (36%) | 25/87 (29%) | 40/97 (41%) | 257/888 (29%) |
| Unknown | 141/580 (24%) | 23/124 (19%) | 30/87 (34%) | 15/97 (16%) | 209/888 (24%) |
| Total installed | 580 | 124 | 87 | 97 | 888 |
| Response | |||||
| Formal services | 104/292 (36%) | 29/56 (52%) | 15/32 (47%) | 14/42 (33%) | 162/422 (38%) |
| Informal services | 79/292 (27%) | 11/56 (20%) | 8/32 (25%) | 16/42 (38%) | 114/422 (27%) |
| Mixed services | 106/292 (36%) | 14/56 (25%) | 8/32 (25%) | 12/42 (29%) | 140/422 (33%) |
| Unknown | 3/292 (1%) | 2/56 (3%) | 1/32 (3%) | 0/42 (0%) | 6/422 (2%) |
| Total installed | 292 | 56 | 32 | 42 | 422 |
Abbreviations: ATT, assistive technology and telecare.
Results have been summarized using the TIDieR framework in Table 5.
Table 5.
Current ATT practice with people with dementia using TIDieR format
| TIDieR format [11] | Current ATT practice for people with dementia | ||
|---|---|---|---|
| When?∗ | When did assessments, recommendation and installations happen? | Baseline (week 0), assessment and recommendations Week 12, 24, 52, 104, assessment and installation |
|
| What? | What areas of assessment, within local ATT assessments, had higher fidelity to the ATT assessment standard? | Daily activity, memory, mobility, and social support | |
| What areas of assessment more frequently triggered the need for ATT? | Daily activities, memory, problem-solving | ||
| What ATT was recommended more frequently within local ATT assessments? | Devices for safety issues and to remind/prompt with monitoring/formal response | ||
| What ATT was installed more frequently? | Devices for safety issues and to remind/prompt with monitoring/formal response and control arm devices (e.g., nonmonitored smoke detectors) | ||
| How much? | How much of the ATT assessment was completed? | 52% of ATT assessment areas were completed 7.2 ATT assessment areas addressed on average (range 0–13) |
|
| How many ATT needs were present? | 4.4 ATT needs on average (range 0–12 ATT risks) | ||
| How many ATT recommendations were identified? | 3 ATT devices on average (range 1–14 ATT devices) 57% of participants had 1 or 2 ATT device recommended |
||
| How many installations happened? | 4.2 ATT devices on average (range 1–15 ATT devices) (incl. control arm devices) 79% installed by week 24, with reduction of installation over time |
||
| How much monitoring and response happened? | 47% of installed ATT required monitoring, of which 38% required formal response |
||
| Who? | Who were the participants? | >80 years old, female, widowed, white British, not living alone, and had moderate dementia. | |
| Who were the assessors of installed devices? | Baseline 57% health and social care professionals 33% ATT assessors 10% of assessors not known |
Week 12–104 32% ATT assessors 20% health and social care professionals 40% of assessors not known 8% other |
|
| Where? | Where did the ATT assessment take place? | 41% of installed devices were assessed by in-person home visits | |
| Where did the installations take place? | Participant's home | ||
| Tailoring | Was the devices tailored to the participants? | There was an expectation that ATT installations would be tailored to participants by the baseline ATT assessment, however, there was weak to moderate tailoring between.
|
|
Abbreviations: TIDieR, Template for Intervention Description and Replication; ATT, assistive technology and telecare.
Predefined by trial protocol.
4. Discussion
Providing ATT for people with dementia is a complex intervention [10] which includes ATT assessment, recommendations, installation, monitoring, and response. Above all, a comprehensive assessment is critical to tailoring ATT to individual users' needs [6], [7]. Limiting the amount of assessment information available may reduce a provider's ability to personalize the technology to individual circumstances. Effective tailoring is needed if the technology is to be used and integrated into the person's life [7], [8]. Examining the ATTILA sites' local ATT assessment documentation, we found 14 common assessment areas. An ATT assessment covering all 14 areas would provide a range of information on the person's values, insight, interests, routines, communication, cognitive and physical skills, and physical and social environment. However, we found that only half (52%) of these assessment areas were documented by assessors, with 60% of responses indicating an ATT need. One explanation for limited coverage of the 14 assessment areas in many assessments could be that assessors did address all the assessment areas but only documented the areas of greatest concern. On the other hand, confidence that assessment processes were comprehensive will be tempered by the finding that 22% of participants' assessments consisted of 0–2 assessment areas addressed (typically in the form of one-line emails). Local authorities facing severe budgetary pressures may be tempted to take short cuts and allow ATT to be installed without a full assessment [7]; our research provides some evidence that this did occur. Furthermore, local ATT assessments tended to be narrowly focused on certain areas of the assessment, particularly the area of safety.
HSC professionals carried out the bulk of baseline assessments for ATTILA participants. However, more installations were at the request of ATT assessors than HSC professionals across the 12-to-104 week follow-ups. The title “ATT assessor” suggests a worker with specialist skills; however, ATT assessors within our study were from a variety of backgrounds, with and without professional qualifications, including personnel with wider job remits than ATT and personnel working solely in ATT teams. ATT assessors demonstrated lower fidelity to the ATT assessment standard than HSC professionals. A recent study [20] suggested that ATT training within CASSRs for people holding responsibility for ATT deployment was brief, “product based” and seen as a marketing opportunity by telecare suppliers. This in turn may limit the scope of the ATT assessment to only those devices available from a particular telecare supplier. Value network mapping yielded two groupings of ATTILA sites, based on the sector of telecare provider offering value to ATTILA participants. The scope of assessors' roles (e.g., their remit to assess for a narrower or broader range of ATT) appeared to differ between network types. It seemed that the organizational resources available to assessors to deliver value to users of ATT differed between sectors. The contractual arrangements existing between CASSRs and other network actors and the extent to which they had contracted out ATT services may also have influenced the resources available to assessors, and thereby the scope of their roles. These must remain tentative findings, given the limitations in information available from a relatively small number of key informants.
The number of ATT needs identified were similar to the number of ATT installations (4.4 and 4.2 per participant, respectively), which on the surface might suggest that assessment recommendations generally translated into installations. Yet there were mismatches: devices were installed for needs that had not been identified in the assessment process, whereas half of the devices recommended as a result of assessment were not installed. Other ATT research suggests some reasons for these results: that difficulties identifying the resources to progress installation may have delayed or deterred installation [21], [22], that individuals may decline in cognitive capacity while awaiting installation so that the ATT is no longer appropriate [23], and that technology may be heavily promoted by suppliers, leading to overprescribing of ATT [24].
Local authorities have identified the most important goals of ATT as being to delay the need for care and support and to enhance quality of life for people with care and support needs [20]. This study found that ATT was most often recommended and installed for safety reasons. Indeed, it has been argued that the use of ATT for safety reasons could delay care by managing identified risks. ATT designed to increase quality of life through meaningful use of leisure time [9], [25], [26], [27], [28] was rarely recommended or installed during the trial.
5. Summary
The literature has argued for the importance of assessment in enabling assistive technology to maximize good outcomes; however, this trial identified assessment recommendations were routinely disregarded at the point of installation. It is, therefore, unlikely that assistive technology is being deployed in a way that will result in benefits for recipients. There is a subsequent need, therefore, to understand how to more effectively translate ATT needs into ATT recommendations and effective ATT installations. Two different delivery systems for deploying ATT were also identified which seemed to have different organizational resources available to assessors and clarity should be sought as to how this impacts on outcomes. Finally, ATT was not deployed to support meaningful use of leisure time which is inconsistent with local authority goals of enhancing quality of life and a review of barriers to deployment is needed.
Research in context.
-
1.
Systematic review: The authors reviewed the literature using traditional (e.g., PubMed) sources and meeting abstracts and presentations. Although assistive technology with people with dementia has not been described, there have been several studies, which advocate for assessment to drive installation. These relevant citations are appropriately cited.
-
2.
Interpretation: Our findings are the first to describe assistive technology for people with dementia. It provides unique evidence that (A) assistive technology practice is not consistent with best practice as promoted within the literature, (B) assistive technology is deployed through at least two service delivery systems, namely, public and not-for-profit telecare provider.
-
3.
Future directions: The article proposes a framework for the generation of new hypotheses and the conduct of additional studies. Examples include (A) understanding how to translate recommendations into effective installations and (B) understanding how different delivery systems for deploying assistive technology impacts on outcomes for people with dementia.
Acknowledgments
Funding for the trial came from the NIHR Health Technology Assessment program (HTA 10/50/02). Neither the funders nor the sponsor have been involved in the preparation or publication of this article. P.B. received financial support from TauRx Therapeutics. J.O.B. received financial support from TauRx, GE Healthcare, Avid/Lilly, and Eisai.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.trci.2019.07.010.
Supplementary Data
References
- 1.Prince M., Wimo A., Guerchet M., Ali G., Wu Y., Prina M. Alzheimer's Disease International; London: 2015. World Alzheimer Report 2015: The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Costs and Trends. [Google Scholar]
- 2.Luppa M., Luck T., Brahler E., Konig H., Riedel-Heller S. Prediction of Institutionalisation in Dementia: a Systematic Review. Dement Geriatr Cogn Disord. 2008;26:65–78. doi: 10.1159/000144027. [DOI] [PubMed] [Google Scholar]
- 3.Marshall M., editor. Astrid: a social and technological response to meeting the needs of individuals with dementia and their carers; a guide to using technology within dementia care. Hawker; UK, London: 2000. [Google Scholar]
- 4.Department of Health . Department of Health, UK Government; Leeds, UK: 2009. Living Well with Dementia: A National Dementia Strategy. [Google Scholar]
- 5.Department of Health . Department of Health; UK, London: 2005. Older People and Disability Division. Building Telecare in England. [Google Scholar]
- 6.Bjorneby S., Topo P., Holthe T. Norwegian Centre for Dementia Care; 1999. Technology, Ethics and Dementia: a Guidebook on How to Apply Technology in Dementia Care. [Google Scholar]
- 7.Sugarhood P., Wherton J., Procter R., Hinder S., Greenhalgh T. Technology as system innovation: A key informant interview study of the application of the diffusion of innovation model to telecare. Disabil Rehabil Assistive Technology. 2014;9:79–87. doi: 10.3109/17483107.2013.823573. [DOI] [PubMed] [Google Scholar]
- 8.Greenhalgh T., Procter R., Wherton J., Sugarhood P., Hinder S., Rouncefield M. What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med. 2015;13:91. doi: 10.1186/s12916-015-0279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leroi I., Woolham J., Gathercole R., Howard R., Dunk B., Fox C. Does telecare prolong community living in dementia? A study protocol for a pragmatic randomised controlled trial. Trials. 2013;14:349. doi: 10.1186/1745-6215-14-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M., on behalf of the Medical Research Council . Medical Research Council; UK: 2008. Developing and Evaluating Complex Interventions: Following Considerable Development in the Field Since 2006, MRS and NIHR Have Jointly Commissoned an Update of this Guidance to be Published in 2019. [Google Scholar]
- 11.Hoffman T., Glasziou P., Boutron I., Milne R., Perera R., Moher D. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:1–12. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 12.Ritchie J., Lewis J., editors. Qualitative Research Practice: A Guide for Social Science Students and Researchers. Sage Publications; London: 2003. [Google Scholar]
- 13.Ehrenhard M., Kijl B., Nieuwenhuis L. Market adoption barriers of multi-stakeholder technology: smart homes for the aging population. Technol Forecast Soc Change. 2014;89:306–315. [Google Scholar]
- 14.Kijl B., Nieuwenhuis L., Veld H., Vollenbroek-Hutten M., Hermens H. Deployment of e-health services - a business model engineering strategy. J Telemed Telecare. 2010;16:344–353. doi: 10.1258/jtt.2010.006009. [DOI] [PubMed] [Google Scholar]
- 15.Molloy D., Standish T. A guide to the standardized mini-mental state examination. Int Psychogeriatr. 1997;9:143–150. doi: 10.1017/s1041610297004754. [DOI] [PubMed] [Google Scholar]
- 16.Parkinson S., Forsyth K., Kielhofner G. University of Illinois; Chicago: 2002. User's Manual for the Model of Human Occupation Screening Tool (MOHOST) [Google Scholar]
- 17.Siegel S. Google Scholar; New York: 1956. Nonparametric Statistics for the Behavioral Sciences. [Google Scholar]
- 18.Perneczky R., Wagenpfeil S., Komossa K., Grimmer T., Diehl J., Kurz A. Regular research articles: mapping scores onto stages: mini-mental state examination and clinical dementia rating. Am J Geriatr Psychiatry. 2006;14:139–144. doi: 10.1097/01.JGP.0000192478.82189.a8. [DOI] [PubMed] [Google Scholar]
- 19.Schober P., Boer C., Schwarte L.A. Correlation coefficients: appropriate use and interpretation. Anesth Analgesia. 2018;126:1763–1768. doi: 10.1213/ANE.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 20.Woolham J.G., Steils N., Fisk M., Porteus J., Forsyth K. Social Care Workforce Research Unit, Kings College, London; London, UK: 2018. The Utopia Project. Using Telecare for older people in adult social care: The findings of a 2016-2017 National Survey of Local Authority Telecare Provision for Older People in England. [Google Scholar]
- 21.Gibson G., Dickinson C., Brittain K., Robinson L. The everyday use of assistive technology by people with dementia and their family carers: a qualitative study. BMC Geriatr. 2015;15:89. doi: 10.1186/s12877-015-0091-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gibson G., Newton L., Pritchard G., Finch T., Brittain K., Robinson L. The provision of assistive technology products and services for people with dementia in the United Kingdom. Dementia (London) 2016;15:681–701. doi: 10.1177/1471301214532643. [DOI] [PubMed] [Google Scholar]
- 23.Canevelli M., Kelaiditi E., del Campo N., Bruno G., Vellas B., Cesari M. Predicting the rate of cognitive decline in Alzheimer's disease: data from the ICTUS study. Alz Dis Assoc Disord. 2016;30:237–242. doi: 10.1097/WAD.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 24.Milligan C., Roberts C., Mort M. Telecare and older people: who cares where? Soc Sci Med. 2011;72:347–354. doi: 10.1016/j.socscimed.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 25.Lund M., Christiensen H., Caltenco H., Lontis E., Bentsen B., Struijk L. 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology; 31 Aug - 4 Sept 2010. IEEE; Buenos Aires, Argentina: 2010. Inductive tongue-control of powered wheelchairs. [DOI] [PubMed] [Google Scholar]
- 26.Windle K., Francis J., Coomber C. Social Care Institute for Excellence; UK; London: 2011. Preventing Loneliness and Social Isolation: Interventions and Outcomes. Research Briefing. [Google Scholar]
- 27.Steptoe A., Shankar A., Demakakos P., Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. PNAS [Internet] 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pols J. The heart of the matter: about good nursing and telecare. Health Care Anal. 2010;18:374–388. doi: 10.1007/s10728-009-0140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.