Abstract
The Healthy Eating Index (HEI) is a measure of diet quality that can be used to examine alignment of dietary patterns with the Dietary Guidelines for Americans. The HEI is made up of multiple adequacy and moderation components, most of which are expressed relative to energy intake (ie, as densities) for the purpose of calculating scores. Due to these characteristics and the complexity of dietary intake data more broadly, calculating and using HEI scores can involve unique statistical considerations and, depending on the particular application, intensive computational methods. The objective of this article is to review potential applications of the HEI, including those relevant to surveillance, epidemiology, and intervention research, and to summarize available guidance for appropriate analysis and interpretation. Steps in calculating HEI scores are reviewed and statistical methods described. Consideration of salient issues in the calculation and interpretation of scores can help researchers avoid common pitfalls and reviewers ensure that articles reporting on the use of the HEI include sufficient details such that the work is comprehensible and replicable, with the overall goal of contributing to knowledge on dietary patterns and health among Americans.
Keywords: Healthy Eating Index, Dietary patterns, Diet quality, Diet indexes, Statistical modeling
ALTHOUGH MUCH NUTRITION RESEARCH HAS taken a reductionist approach with a focus on particular nutrients, food groups, or other dietary constituents, the complexity of the overall diet and its relations with health and disease outcomes are increasingly being recognized and embraced. For example, the 2015–2020 Dietary Guidelines for Americans (DGA) focused on eating patterns, noting that such patterns represent the totality of the foods and drinks habitually consumed by individuals and that these dietary components may act in synergistic and cumulative ways to predict health status and disease risk.1 The development of the DGA was informed by a review of the growing evidence on eating patterns and health outcomes, including cardiovascular disease, diabetes, cancer, and overweight and obesity.2,3
Various indexes have been developed to characterize dietary patterns and diet quality.4–6 Such measures use criteria established a priori according to recognized principles of a healthy diet.6 Commonly used indexes include those based on the Dietary Approaches to Stop Hypertension and Mediterranean diet patterns, as well as the Healthy Eating Index (HEI) and Alternate HEI.7–14 The HEI in particular is a tool that measures alignment with the DGA.7–10 The most recent iteration of the HEI15 measures alignment with the 2015–2020 DGA. Prior versions corresponding to the 2005 and 2010 DGA have been widely used in nutrition research.16 For example, an article published during spring 2017 reported that the 2005 version has been used in studies described in more than 185 scientific publications since its release in 2008, whereas the 2010 version, released in 2013, has been used in studies described in more than 100 articles.16 The HEI has been used for varying purposes, including documenting the diet quality of the US population and assessing differences in diet quality among population subgroups (eg, Guenther and colleagues8 and Wilson and colleagues17), elucidating influences on diet quality (eg, Savoca and colleagues18), evaluating associations between diet quality and disease risk and mortality (eg, Liese and colleagues,5 George and colleagues,19 Harmon and colleagues,20 and Reedy and colleagues21), and examining the effect of interventions on diet quality (eg, Nansel and colleagues22).
The HEI is made of up multiple adequacy and moderation components, most of which are expressed relative to energy intake (ie, as densities) and then scored according to standards.7,9,15 Due to the scoring of multiple components, as well as characteristics of dietary intake data more broadly, calculating and using HEI scores can involve unique statistical considerations and, depending on the particular purpose, intensive computational methods.10,23–25 The objectives of this article are to review potential applications of the HEI and to summarize available guidance for appropriate analysis and interpretation of scores. Both analytic methods for which code has been developed as well as potential approaches that require further development are described.
Although the HEI can be used to assess the food supply and menu offerings within various food environments (eg, fast-food restaurants),26–29 the focus of the current article is on the use of the HEI for assessing and analyzing diet quality in surveillance, epidemiologic, and intervention research (ie, cases in which dietary intake data for the purpose of characterizing diet quality are available for groups of individuals sampled from the population). The use of the HEI with individuals in clinical settings for the purpose of nutrition advising or counseling is also briefly described.
HEI
As noted, the HEI measures alignment with the DGA, allowing examination of overall diet quality in relation to federal dietary guidance, as well as patterns in terms of balance among multiple components.7,9,15 Since the 2005 iteration, the HEI has employed scoring that operates on a density basis (eg, amount per 1,000 kcal, ratio of fatty acids)7,9,15 (Table). As a result of this density feature, the HEI can be used to examine diet quality from the perspective of the relative mix of foods and drinks consumed and in terms of how calories are allocated; in other words, diet quality is assessed independent of quantity.9 This density-basis used in the 2005, 2010, and 2015 versions of the HEI represents a departure from the earlier HEI developed by the US Department of Agriculture (USDA) Center for Nutrition Policy and Promotion in 1995,30 which is not addressed in this article. The HEI addressed here is also distinct from similarly named indexes employed in other countries (eg, Woodruff and colleagues31). The abbreviation HEI as used in this article thus refers to the three density-based versions of the index developed in partnership by researchers from the Center for Nutrition Policy and Promotion and the National Cancer Institute (NCI) and known as the HEI-2005, HEI-2010, and HEI-2015.7–10,15 These versions share a common foundation, with nuances (Table) to reflect the evolution of dietary guidance, as expressed by the DGA, between 2005 and 2015.1,32,33
Table.
2005, 2010 and 2015 iterations of the Healthy Eating Index (HEI), along with their maximum scores and standards for maximum and minimum scoresabc
| Component | HEI-2005 | ||
|---|---|---|---|
| ADEQUACY COMPONENTS | |||
| Fruits and fruits subgroups | |||
| Total Fruits maximum score | 5 | ||
| Standard for maximum score | ≥0.8 c equivalents/1,000 kcal | ||
| Whole Fruits maximum score | 5 | ||
| Standard for maximum score | ≥0.4 c equivalents/1,000 kcal | ||
| Vegetables and vegetable subgroups | |||
| Total Vegetablesd maximum score | 5 | ||
| Standard for maximum score | ≥1.1 c equivalents/1,000 kcal | ||
| Dark Green and Orange Vegetables and Legumesd maximum score | 5 | ||
| Standard for maximum score | ≥0.4 c equivalents/1,000 kcal | ||
| Greens and Beansd maximum score | 5 | ||
| Standard for maximum score | ≥0.2 c equivalents/1,000 kcal | ||
| Grains and grains subgroups | |||
| Total Grains maximum score | 5 | ||
| Standard for maximum score | ≥3.0 oz equivalents/1,000 kcal | ||
| Whole Grains maximum score | 5 | 10 | |
| Standard for maximum score | ≥ 1.5 oz equivaents/1,000 kcal | ≥1.5 oz equivalents/1,000 kcal | |
| Milk/dairy | |||
| Milk/Dairye maximum score | 10 | ||
| Standard for maximum score | ≥1.3 c equivalents/1,000 kcal | ||
| Meat and beans/total protein foods and protein subgroups | |||
| Meat and Beans maximum score | 10 | ||
| Standard for maximum score | ≥2.5 oz equivalents/1,000 kcal | ||
| Total Protein Foodsd maximum score | 5 | ||
| Standard for maximum score | ≥2.5 oz equivalents/1,000 kcal | ||
| Seafood and Plant Proteinsd maximum score | 5 | ||
| Standard for maximum score | ≥0.8 oz equivalents/1,000 kcal | ||
| Oils and fatty acids | |||
| Oils maximum score | 10 | ||
| Standard for maximum score | ≥12 g/1,000 kcal | ||
| Fatty Acids maximum score | 10 | ||
| Standard for maximum score | (PUFAsf + MUFAsg) /SFAsh ≥2.5 | ||
| Standard for minimum score | (PUFAs+MUFAs)/SFAs ≤ 1.2 | ||
| MODERATION COMPONENTS | |||
| Saturated Fats maximum score | 10 | ||
| Standard for maximum score | ≤7% of energy | ||
| Standard for minimum score | ≥15% of energy | ||
| Refined Grains maximum score | 10 | ||
| Standard for maximum score | ≤1.8 oz equivalents/1,000 kcal | ||
| Standard for minimum score | ≥4.3 oz equivalents/1,000 kcal | ||
| Sodium maximum score | 10 | 10 | |
| Standard for maximum score | ≤0.7 g/1,000 kcal | ≤1.1 g/1,000 kcal | |
| Standard for minimum score | ≥2.0 g/1,000 kcal | ≥2.0 g/1,000 kcal | |
| Calories from Solid Fats, Alcohol, and Added Sugars/Empty Caloriesi maximum score | 20 | 20 | |
| Standard for maximum score | ≤20% of energy | ≤19% of energy | |
| Standard for minimum score | ≥50% of energy | ≥50% of energy | |
| Added Sugars maximum score | 10 | ||
| Standard for maximum score | ≤6.5% of energy | ||
| Standard for minimum score | ≥26% of energy | ||
| Maximum total | 100 | 100 | 100 |
For components for which the standard for the minimum score of zero is not specified, the standard is zero intake of the component (eg, zero total fruits).
Cells shaded in blue indicate components that are consistent across the HEI-2005 and HEI-2010. Cells shaded in green are consistent across the HEI-2010 and HEI-2015. Cells shaded in grey indicate components that are consistent across all three versions of the HEI.
Boldface type indicates changes in the standards for minimum and/or maximum scores for components that were included in multiple versions of the HEI.
The Total Vegetables, Greens and Beans, Total Protein Foods, and Seafood and Plant Proteins and their respective maximum scores and scoring standards are consistent between the 2010 and 2015 versions of the HEI. However, in the 2010 version, legumes were counted as protein foods—Total Protein Foods and Seafood and Plants Proteins—only if the standards for these components were otherwise not met, and they were counted toward vegetables only after the protein foods standards had been met. This is also true for the vegetable and protein components for 2005. However, for the HEI-2015, beans and peas count toward all of the vegetable and protein components.
Milk in the HEI-2005 was renamed Dairy for the HEI-2010 and HEI-2015.
PUFAs=polyunsaturated fatty acids.
MUFAs= monounsaturated fatty acids.
SFAs=saturated fatty acids.
The HEI-2005 included Calories from Solid Fats, Alcohol, and Added Sugars. In the HEI-2010, this component is known as Empty Calories.
NOTE: Information from this table is available at www.jandonline.org as part of a PowerPoint presentation.
The HEI-2005, HEI-2010, and HEI-2015 have each been shown to capture diet quality independently of energy intake and to distinguish among subgroups with known differences in diet quality.8,10,34 Further, associations have been observed between higher HEI scores and lower risk of death from all causes, cancer, and cardiovascular disease.5,19–21 The HEI is appropriate for the assessment of diet quality among populations to which the USDA Food Patterns35 apply. It is not applicable to children younger than age 2 years or those consuming breastmilk or infant formula.9
THE HEI SCORING ALGORITHM
The crux of each version of the HEI is a scoring algorithm that identifies the components along with their weights (ie, the maximum score allocated to a given component) and scoring standards (ie, the levels of intake used to assign scores to each component). For each version, both adequacy and moderation components are considered. The specifics of each iteration’s algorithm are summarized in the Table and detailed elsewhere.7,9,15 The most recent version, the HEI-2015, includes 13 components: nine adequacy components and four moderation components15 (Table). The prior two versions each included 12 components.7,9 Changes across the versions are briefly noted in the next section and described in detail elsewhere.9,15
Each component is typically scored to a maximum of 10 points; for components divided into two (eg, Total Fruits and Whole Fruits), each subcomponent is allocated 5 points. Standards for assigning maximum points for a component are based on the least-restrictive recommendations (ie, those that are easiest to achieve) among those varying by energy level, sex, and age.9 The standards utilized may be lower (for adequacy components) and higher (for moderation components) than the recommendation for any given individual due to the use of the least-restrictive recommendations. For the 2015 version of the HEI, only the 1,200 to 2,400 kcal patterns were used (compared with the range of 1,000 to 3,200 kcal, used for some components in prior versions),35 lending to a more consistent rationale for maximum standards across components and avoiding standards based on energy levels at the higher end of needs.15 Minimum scores for the adequacy components are based on zero consumption per 1,000 kcal.15 For sodium (a moderation component), the standard is based on the approach used for the Dietary Reference Intakes Tolerable Upper Intake Level,7,36 with zero points corresponding to ≥2.0 g/1,000 kcal. The standards allow for the application of points for each component such that the total HEI score can range from zero to 100. A score of zero on particular components is possible for a given individual, although a total score of zero is unlikely.
The application of the scoring algorithm allows the computation of scores for each HEI iteration at the level of an individual person (eg, based on data from 24-hour recalls [24HR], food records [or diaries], or a food frequency questionnaire [FFQ]). However, as discussed below, depending on the application, alternative computational methods may be preferred to better reflect true usual diet quality among groups of persons.
Evolution of the HEI
Here, consistency across the versions of the HEI and key differences are reviewed briefly to inform a subsequent illustration of how scores may be expected to change with the application of different versions due to nuances in the components and their scores and scoring standards. As can be seen in the Table, there are many common components across the three versions, with differences reflecting refinements in guidance from 2005 through 2015.
Beginning with the most recent iterations, changes between the 2010 and 2015 versions are modest and relate mainly to how sources of empty calories (for the purposes of the HEI, defined as calories from added sugars, solid fats, and alcohol) are captured. In each of the 2005 and 2010 versions, a moderation component capturing multiple sources of empty calories was allocated 20 points.7,9 In the HEI-2015, there are two separate components capturing sources of empty calories (Added Sugars and Saturated Fats, each scored to a maximum of 10 points), reflecting key recommendations of the DGA to limit intake of each of these dietary factors to <10% of total calorie intake.1 The HEI-2015 reintroduced Saturated Fats, which appears in the 2005 version (while also maintaining the Fatty Acids component introduced in the 2010 version). Furthermore, in the 2005 and 2010 versions, calories from alcohol consumed above a level considered moderate (ie, >2 drinks/day for men and 1 drink/day for women) were captured by the respective empty calories component. In contrast, a component that accounts for alcohol is not included in the HEI-2015. However, in all three versions of the HEI, the caloric energy in alcohol/alcoholic beverages is captured through its contribution to total calories, which is the denominator for most components. When alcohol is consumed, calories from alcohol in the denominator will result in lower component scores for those adequacy components expressed relative to energy and higher component scores for moderation components compared with diets with no calories from alcohol. Specific considerations related to alcohol are described in an article detailing the HEI-2015.15
An additional change pertinent to the HEI-2015 relates to the treatment of legumes (beans and peas) in the calculation of amounts of each relevant dietary constituent considered in arriving at HEI scores. The vegetable and protein groups and their corresponding maximum points and scoring standards are unchanged from 2010 to 2015. However, in the earlier versions of the HEI, legumes were counted as protein foods only in the case that the standard was otherwise not met (any legumes counted toward the Total Protein Foods standard were also counted toward the Seafood and Plant Proteins component), and counted toward the two vegetable subgroups only after the protein foods standard had been met. This was done to be consistent with the USDA Food Patterns,35 which note that legumes are considered both protein foods and vegetables but count them as only one or the other. For the HEI-2015, legumes are counted toward all four of the relevant vegetable and protein groups, for reasons described in detail elsewhere.15
Differences between the 2005 version and the more recent iterations of the index are more extensive. Four adequacy components (Total Fruits, Whole Fruits, Total Vegetables, and Whole Grains) appear in all three iterations, with one additional adequacy component remaining the same aside from a change in name (Milk vs Dairy). Of these, the maximum score has changed only for Whole Grains (from 5 points in the 2005 version to 10 points in 2010 and 2015). To round out grains, the 2005 version includes Total Grains (an adequacy component), whereas the 2010 and 2015 versions include Refined Grains (a moderation component). Vegetable subgroups changed from the 2005 (Dark Green and Orange Vegetables and Legumes) to the 2010 version, which introduced Greens and Beans, reflecting the two vegetable subgroups for which observed intakes were farthest from the recommendations.37 The 2005 version included Meat and Beans, whereas the 2010 and 2015 versions include Total Protein Foods as well as Seafood and Plant Proteins to capture specific choices from the protein foods group. Refined Grains (a moderation component) was new to the 2010 version, replacing the adequacy component Total Grains and addressing high levels of consumption of refined grains compared with recommended levels.37 The 2015 version carries forward the Refined Grains component, as well as Sodium, which is common to all three iterations, though the standard for maximum points changed from the HEI-2005 to HEI-2010. Finally, Fatty Acids (the ratio of unsaturated to saturated fats) was introduced in the 2010 version and replaced the Oils (adequacy) and Saturated Fats (moderation) components in the HEI-2005 version. This change reflected the recommendation in the 2010 DGA32 to replace saturated fatty acids with unsaturated fatty acids.
In determining the version of the HEI that is most suitable for a particular research initiative, in cross-sectional analyses it may be appropriate to use that which reflects the dietary guidance in place at the time the data were collected, depending on the research questions. In studies using prospectively collected data (eg, assessing associations between baseline dietary intake and subsequent health outcomes) or assessing trends in HEI scores over time, it may be prudent to use the most recent iteration to capture refinements related to the most recent dietary guidance, which is based on evolving evidence on diet and health. Using different versions within a given study is not recommended (unless a comparison of the versions is an explicit part of the study objectives) because changes to the index are likely to result in different scores, as described further below.
Features of the HEI Influencing Statistical Approaches
Regardless of the iteration, the HEI and the dietary data used to calculate component and total scores are characterized by several features that must be considered in scoring and integrating scores into statistical analyses. First, the HEI is multidimensional, requiring the simultaneous consideration of several dietary constituents. Second, the dietary constituents of interest include those consumed regularly (ie, on most days) by most persons (eg, added sugars) and others consumed on a more episodic basis by most persons (eg, whole grains) in the population.25,38 The need to account for both types of dietary components, as well as skewness in distributions of intake among a group, complicates the estimation of usual intake. Third, the density basis means that for each component, a ratio is invoked (eg, amount of fruits consumed relative to calories). Ratios expressing the amounts of one component relative to another (usually energy) can be derived at the level of individuals or groups, leading to different results.39 Further, the components within the HEI may be correlated with one another. Finally, as with any analysis of self-report dietary intake data whether applying the HEI or not, measurement error must be considered and addressed to the extent possible.40 Although measurement error is a complicated topic that is beyond the scope of this article, general concepts to consider here are that random error influences whether HEI scores calculated using a particular set of data can be used to represent usual diet quality, whereas systematic error or bias relates to how well HEI scores based on self-report data reflect true diet quality.40
Calculating HEI Scores
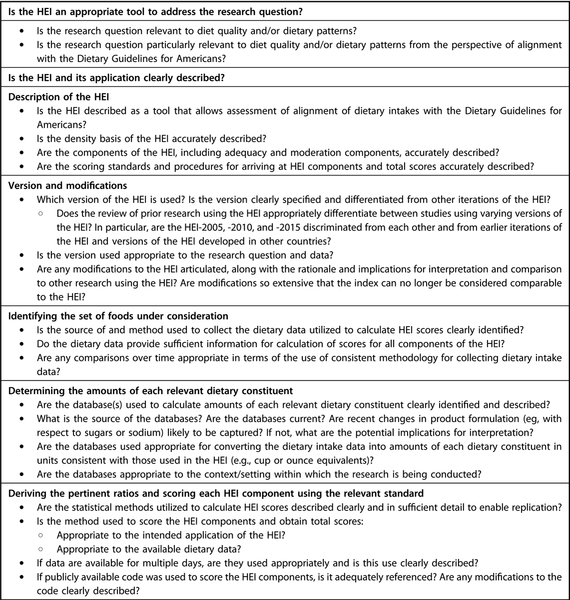
Below, basic steps in calculating HEI scores are described and the evidence on preferred methods for arriving at scores for different applications is summarized. Methods for some applications are quite well established, whereas other areas require development; thus, areas that could benefit from further methods evolution are highlighted. Also noted are considerations that should be borne in mind in interpreting HEI scores regardless of the particular application. An accompanying checklist (Figure 1) can be utilized by researchers using the HEI, as well as reviewers of relevant articles to help ensure that key issues and details are addressed and adequately reported. This checklist might be useful in combination with the Strengthening the Reporting of Observational Studies in Epidemiology-nutritional epidemiology guidelines,41 an extension to the Strengthening the Reporting of Observational Studies in Epidemiology statement intended to help authors improve quality and completeness of reporting of aspects of nutritional epidemiology research, including details of dietary assessment methods. Although targeted to nutritional epidemiology, the guidelines may have application to additional types of research considered here, such as surveillance and intervention studies.
Figure 1.
Considerations in the application of the Healthy Eating Index (HEI) for surveillance, epidemiology, and intervention research. NOTE: Information from this figure is available at www.jandonline.org as part of a PowerPoint presentation.
Steps in the Application of the HEI
For any application, the basic steps involved in calculating HEI scores include identifying the set of foods under consideration (in this case, the foods and beverages consumed by individuals), determining the amount of each relevant dietary constituent, and deriving the pertinent ratios and scoring each HEI component using the relevant standard.27,42
Identifying the Set of Foods under Consideration.
The calculation of HEI scores at the level of groups of persons requires the availability of intake data capturing the total diet. Such data are often collected using self-report tools, including 24HRs, food records, and FFQs. A full review of the characteristics of these methods and their advantages and disadvantages is beyond the scope of this article and available elsewhere.43,44 However, before calculating HEI scores, it is critical to consider the quality of the available data. This pertains to the extent to which the data reflect true intake (ie, requiring consideration of degree of bias) and also to which they represent usual, or long-term average, dietary intake (ie, consideration of degree of random error, which is driven primarily by day-to-day variation in intakes measured for a day or a few days). In most situations, the HEI should be calculated on the basis of usual dietary intake given that eating patterns and thus diet quality can vary from day to day and the DGA are intended to be met on average over time, not each and every day. An exception is alcohol, which is calculated on a per-day basis in the HEI-2005 and HEI-2010 (the two versions of the index that include a component capturing alcohol). An important distinction between diet assessment methods typically used to collect data amenable to the calculation of HEI scores is that 24HRs and food records capture short-term intake, whereas FFQs attempt to directly measure usual intake at the level of an individual person.44 Other salient points related to specific methods of collecting dietary data are noted below in the section on approaches for calculating HEI scores for different applications.
Determining the Amount of Each Relevant Dietary Constituent.
To enable the calculation of component and total scores, it is necessary to link intake data to databases that allow quantification of each of the dietary constituents of interest within the HEI. In addition to providing nutrient composition details, the databases must provide information on amounts of constituents such as fruits, vegetables, oils, and added sugars in units consistent with dietary guidance. Examples of databases used for these purposes are the USDA Food Patterns Equivalents Database (https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview/) and its predecessor, the MyPyramid Equivalents Database (https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/mped/mped2_doc.pdf#TitlePage), which disaggregate each food or beverage consumed into ingredients that are then sorted into groups relevant to dietary guidance. These databases can each be readily linked to National Health and Nutrition Examination Survey (NHANES) data and other sources of intake data coded using the Food and Nutrient Database for Dietary Surveys (https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds/), which provides information on nutrient composition. The Nutrition Data System for Research has also been used to quantify each of the dietary constituents included in the HEI based on 24HR data.45 The capacity to calculate HEI scores also exists for FFQ data that are linked to the requisite composition data. For example, in the Dietary Patterns Methods Project, HEI scores were calculated from frequency data collected in the National Institutes of Health-AARP (formerly known as the American Association of Retired Persons) Diet and Health Study, the Multiethnic Cohort, and the Women’s Health Initiative Observational Study.5,19–21
With any database, it is important to consider the quality of the available information, including its currency and completeness. This may be particularly salient for certain dietary constituents because changes are made to the food supply; for example, to reduce sodium or added sugars. Other issues related to databases may include the lack of information on branded items and reliance on composite nutrient and food group data. Such factors should be borne in mind in the interpretation of HEI scores, as with any analysis of self-report dietary intake data. Further, it should be considered that the use of different databases with varying sources of information on food composition to determine the amount of each relevant dietary constituent might influence results.
Deriving the Pertinent Ratios and Scoring Each HEI Component using the Relevant Standards.
The next step is to derive the pertinent ratios from the estimated quantities of each dietary constituent and apply the scoring standards to arrive at scores for each component. Component scores are summed to arrive at the total score. The intermediate outputs in this process are ratios (eg, cup equivalents of fruit per 1,000 kcal), referred to as densities. In some cases, researchers may be interested in these densities39 (eg, energy-adjusted fruit intake) in their own right; for example, for use in regression models. However, given that this article is focused on applications of the HEI, which involves the use of the standards to arrive at scores, the focus here is on applications making use of scores rather than the intermediate density variables.
Methods for Calculating HEI Scores Based on the Application and Available Data
The HEI can be used to describe diet quality among groups of persons, examine associations between diet quality and other factors such as health or disease outcomes, and assess the effects of interventions on diet quality. Thus, researchers are often interested in estimating HEI scores for describing diet quality for a group of persons, comparing diet quality among groups, or for use as dependent or independent variables within regression models. The key methods recommended for calculating scores for these varying purposes include the population ratio method (which involves calculating ratios and scores at the level of populations or subpopulations rather than individuals),25 the bivariate method (which allows simultaneous modeling of two dietary components),24 and the multivariate method (which allows simultaneous modeling of multiple dietary components).10,23 Code that can be used with SAS statistical software46 is available for each of the three highlighted methods, although to differing degrees for particular applications.42
To apply the population ratio method, which is applicable to 24HR and food record data, total intakes of the dietary constituents among the group of persons of interest are calculated (ie, intake of the relevant constituents, including energy, is summed for the total sample of interest). The relevant ratio of the totals for each HEI component is then derived and compared with the applicable standards for scoring. For example, total intakes of fruits and of energy for the group and the ratio of these two values are calculated, and the respective scoring standard applied. An alternate approach to the population ratio involves the application of the HEI scoring algorithm to data at the level of each individual person. The resulting person-level scores are then averaged to arrive at a mean score for the group.25 It is also possible to estimate scores of the mean ratio by deriving the pertinent ratios for each individual person, averaging these across individuals, and applying the scoring standards to arrive at scores for a group.25 Prior analyses have shown that the population ratio method provides a less biased estimate of mean HEI scores for a population compared with either the mean score or scores of the mean ratio.25 Although the population ratio method can theoretically be applied to a group as small as two individuals, the choice of the most appropriate approach to calculating HEI scores should be based on the research question. Approaches when interest is in a specific individual are described briefly below.
The bivariate and multivariate methods are extensions of the NCI Method for estimating usual intake distributions using 24HR (or record) data38,47 when at least a subset of the population have replicate 24HRs (or records). These methods, which are applicable to dietary components that are consumed most days by most persons as well as those that are consumed episodically, account for day-to-day or within-person variation in intakes, as well as skewness. They are unique from the methods discussed above in allowing estimation of percentiles of the distribution of usual HEI scores at the level of a group. Although the more complex methods for estimating distributions of HEI scores have primarily been applied to and tested with 24HR rather than food record data, they are amenable to use with replicates of food records completed on nonconsecutive days (eg, two 4-day food records 2 weeks apart). Approaches are needed to integrate FFQ data into methods developed for 24HR and record data, as elaborated upon below.
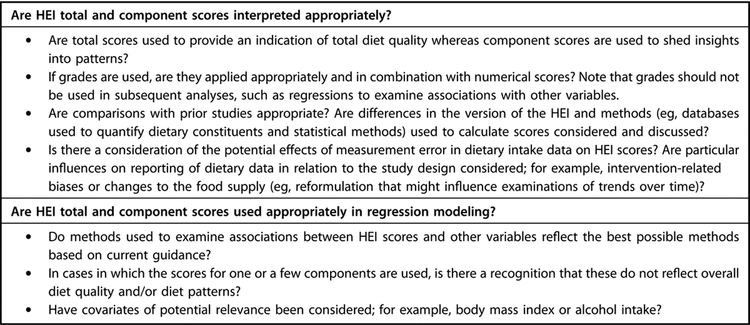
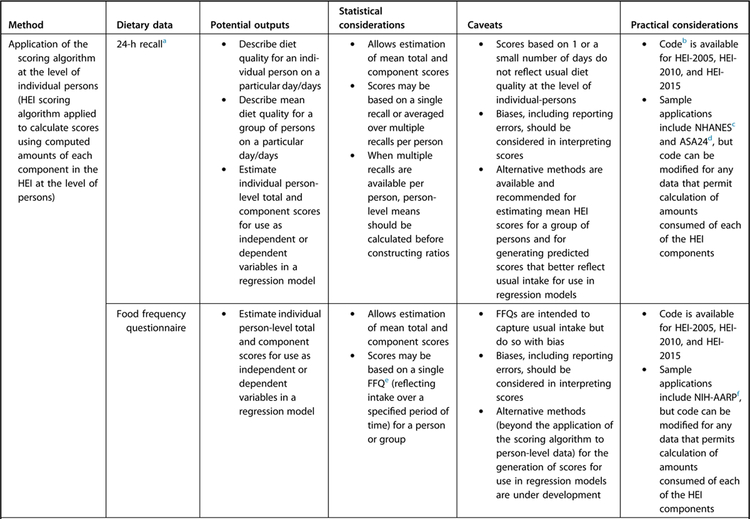
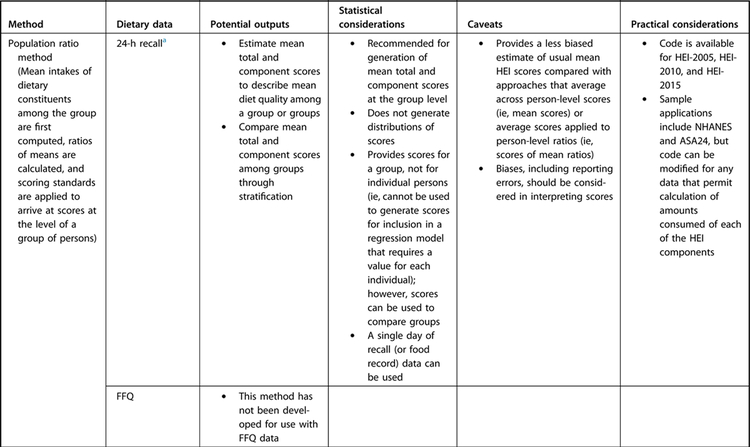
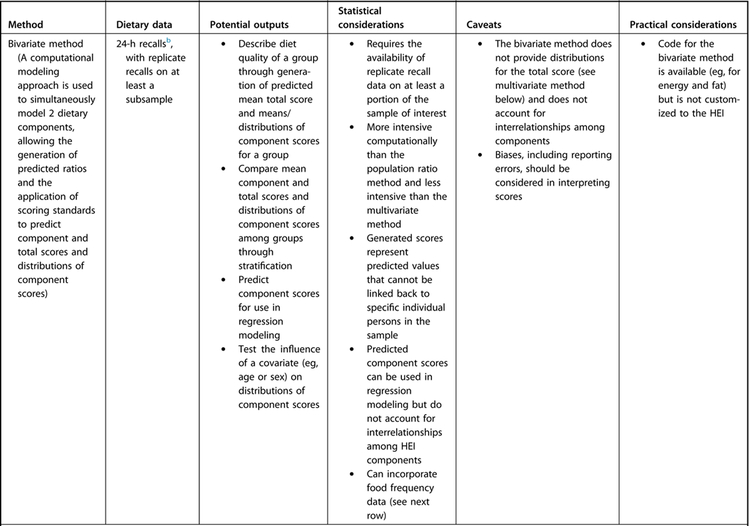
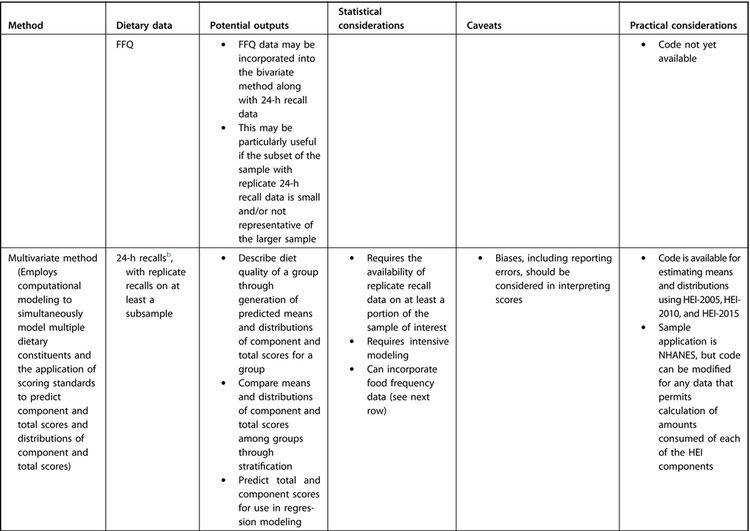
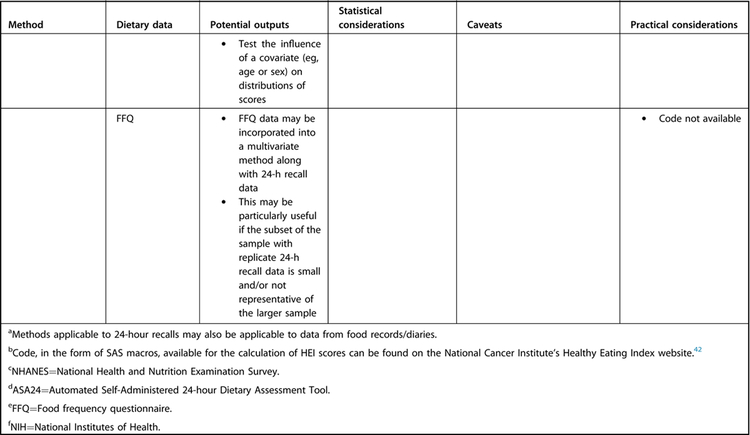
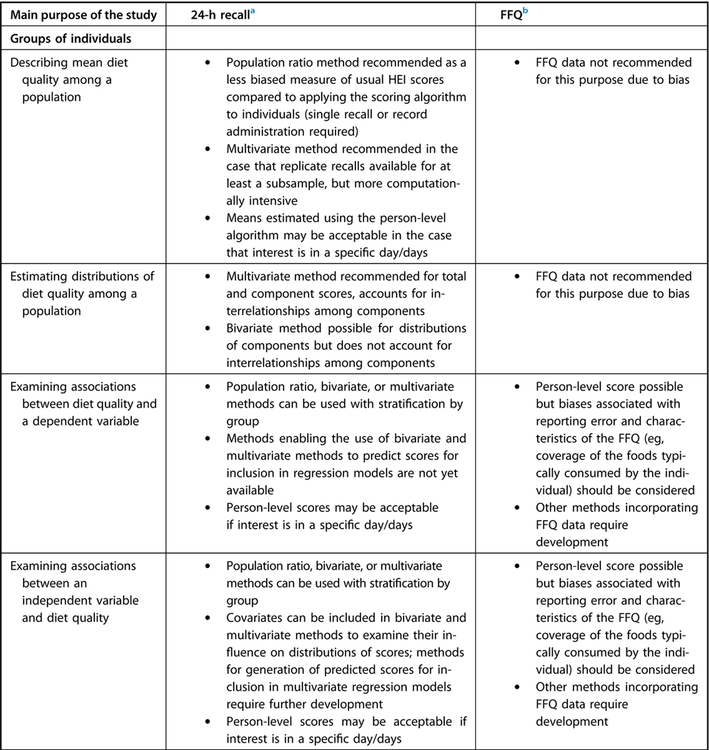
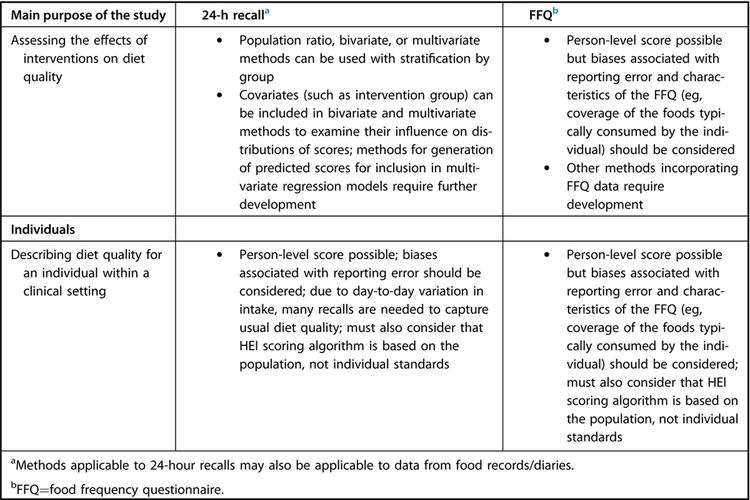
Drawing on these methods, recommended approaches for different research questions involving the HEI are described in the following sections. Figure 2 provides a summary of the possible statistical approaches, including outputs, considerations, and caveats for both 24HR/record and FFQ data. Figure 3 provides a complementary summary of potential research purposes with corresponding recommended methods.
Figure 2.
Summary of methods for the calculation of Healthy Eating Index (HEI) scores.
Figure 3.
Recommended methods to calculate Healthy Eating Index (HEI) scores depending on the main purpose of the study.
Describing Diet Quality among Groups or Subgroups of Persons
HEI component and total scores can be used to describe diet quality among a population group or subgroups differentiated by factors such as age, sex, or socioeconomic status. For such purposes, dietary intake data collected using 24HR or food records are recommended. Generally, the use of FFQs to describe diet quality is not recommended given that such data are known to be affected to a greater extent by systematic bias.48,49 The focus below is thus on 24HRs and records as the source of the dietary intake data.
Estimating Mean HEI Total and Component Scores.
In studies in which data from at least one 24HR or administration of a food record are available, mean HEI and mean component scores can be calculated (Figure 2). As noted, one approach for estimating mean HEI total and component scores (and for which code is publicly available) is the population ratio method (Figure 2).25 This approach results in the generation of scores for a group of persons (not an individual person) that can be used to make inferences at the group level regarding alignment of diet quality with dietary guidance. With stratification, scores can be used to compare diet quality among subgroups; for example, based on age. In cases in which data from repeat administrations of 24HRs are available, it is possible to use either the first recall or to sum data from all recalls. The use of additional recalls can better reflect usual intake by accounting for variation across days. For food records, one can also calculate mean intakes and derive ratios across all days in the total sample (eg, mean intakes of fruit and energy are based on all days of data for all persons in the group). Decisions regarding the data to be used should consider whether there is any reason to believe that reporting quality might differ across days, for example, due to training effects or recording fatigue.
In situations in which repeat 24HRs are available for at least a subsample, mean component and total scores can be calculated using the NCI bivariate method to simultaneously model two food groups or nutrients, resulting in predicted ratios to which the scoring standards are applied (Figure 2). The bivariate method is more computationally intensive than the population ratio method and may not be necessary for applications in which only mean HEI scores (vs distributions of scores) are desired. However, it may offer greater precision than the population ratio method, as well as accounting for skewness in the dietary intake data. The multivariate method can also be used for arriving at mean scores, but this approach is computationally intensive and may not be the preferred approach for situations in which interest is only in means rather than distributions of HEI scores. Predicted scores yielded by the bivariate and multivariate modeling approaches do not represent the true usual HEI scores of individuals in the sample and they cannot be linked back to particular individual persons—this is because scores are based on prediction and do not reflect the variability of the population.
Estimating Distributions of HEI Total and Component Scores.
In situations in which data for a second recall or record are available for all or some persons in a sample, it is possible to estimate distributions of usual HEI scores,24 which can provide additional information to inform policies and programs or evaluate interventions. For example, the estimation of distributions of HEI scores undertaken as part of the evaluation of the HEI-201534 showed that the 99th percentile of total HEI scores for individuals aged 2 years and older from NHANES 2011–2012 was 81.2 (out of a maximum 100 points), suggesting that almost all of the population requires improvements to their eating patterns to align more closely with the DGA.
The bivariate method can be used to arrive at distributions of scores for the components (Figure 2). To estimate distributions of HEI component and total scores, the multivariate extension to the NCI Method, which employs a computational modeling method known as Markov Chain Monte Carlo, has been developed to simultaneously model the multiple dietary constituents in the HEI, including components consumed most days by most persons as well as those consumed more episodically by most persons in the population.23 The application of the multivariate method to estimate distributions of HEI scores has been illustrated through the evaluation of the HEI-2005 and HEI-2010,10 as well as the HEI-2015.34
Diet Quality per the HEI as an Independent Variable
Epidemiologic examinations of associations between diet quality and a dependent variable (eg, chronic disease mortality) have often relied upon data from FFQs because these are the tools traditionally used in prospective cohort studies.43 As it becomes possible with technology advances to collect 24HR and food record data in large prospective studies,43,50 it is increasingly feasible to use these data to characterize diet quality and assess associations with markers of health and disease. Such investigations require that assumptions regarding temporality are met; that is, in most cases, the measurement period to which the dietary exposure pertains should precede the development of the marker of health or disease, unless it is hypothesized that the dietary exposure and other variables of interest are related contemporaneously.
In analyses using 24HRs or records and that require person-level scores, such as regression modeling, the population ratio method is not applicable because it generates scores for a group of persons, not an individual person. It is possible to apply the HEI algorithm to 24HR or record data to arrive at person-level scores. These are unlikely to reflect usual intake but may be acceptable in situations in which interest is in a specific day or days. The bivariate method can be used to obtain predicted scores that can be included in regression models (eg, for studies examining dietary fat as a proportion of calories relative to a disease outcome), but the method has not yet been extended to applications of the HEI. Methods development is thus needed to expand the possibilities for examining associations between diet quality per the HEI based on 24HR and food record data and other variables using regression modeling because the most feasible approach at the current time relies on the calculation of person-level scores for a day or limited number of days. In such cases, there should be theoretical grounds that diet quality based on a single day (or small number of consecutive days in the case of a record) is related to the outcome of interest.
For FFQ data, the currently available method is the application of the HEI scoring algorithm at the person level. In using such scores, biases associated with reporting error and characteristics of the FFQ should be considered. Future methodologic research may identify approaches for mitigating measurement errors that may influence estimated HEI scores, for example, using 24HR data to reduce bias in the FFQ data, as well as incorporating FFQ data into the bivariate and multivariate methods making use of recall or record data.
In examining associations between diet quality per the HEI and health or disease outcomes, the total score can be used, or particular component scores can be used in cases in which specific aspects are of interest (although the overarching focus of the HEI is to enable examination of diet quality broadly). In addition, it is usually necessary to account for potential confounders. For example, prior analyses of associations with all-cause mortality have included adjustment for alcohol intake.5 Considering associations between alcohol and health or disease outcomes is complex.15 Thus, whether and how alcohol intake is accounted for in a model requires careful consideration, including taking into account how alcohol is treated in the version of the HEI used (eg, in contrast to the HEI-2005 and HEI-2010, the HEI-2015 does not include a component that captures alcohol, although calories from alcohol are considered in all versions of the HEI). It may be relevant to also consider markers of energy balance, such as anthropometric measures.9 Although energy balance is a focus of the respective DGA, it is not considered within the HEI given the index’s focus on diet quality rather than quantity. In addition, as discussed elsewhere,51,52 even when density variables are used in regression models, including self-reported energy can improve the estimation of diet-disease associations.
Diet Quality per the HEI as a Dependent Variable
For the purposes of examining how factors such as age, sex, and socioeconomic status are associated with diet quality, considerations for calculating HEI scores as dependent variables are similar to those outlined in the section on describing diet quality among groups or subgroups. These also pertain to studies to examine the influence of interventions on diet quality. To compare across groups (eg, differentiated by sex or intervention group), the population ratio method, bivariate, or multivariate methods can be used with stratification by group. In cases in which statistical tests, such as regression modeling, that draw on variability within the study sample are employed, person-level scores are needed. As noted previously, it is possible that the bivariate method can be used to generate predicted scores for inclusion in regression models, and this is also true of the multivariate method; however, these methods have not yet been extended to such applications specific to the HEI.
In studies in which diet quality is the dependent variable relative to an intervention, it is important to consider that those exposed to the intervention may misreport diet differently over time or in comparison to control groups,40 creating differential error among groups or across time points. In other words, those in a group that have been counseled or encouraged in other ways to follow a particular dietary pattern may be more likely to report dietary intakes that align with that pattern. Such differential error can lead to a loss of statistical power and spurious effects. In cases in which randomization has been employed and/or the intervention is targeted at the environment rather than individual behavior, this source of bias may be less of a concern. In the case that differential error is likely to be significant, it is recommended that self-report intake data not be used as the sole means of evaluating interventions.40
Describing Diet Quality for an Individual within a Clinical Setting
Approaches for describing diet quality at the group-level are generally not applicable to a given individual. For instance, the population ratio approach pools data across the population to reflect usual intake and results in component and total scores for a group of individuals, not a given individual. The bivariate and multivariate methods are also not applicable to clinical use with a specific individual.
The application of the HEI scoring algorithm occurs at the level of individual persons and results in component and total scores for each person. Alternately, a ratio of means can be employed to calculate scores for a single person using multiple days of data. However, an individual’s HEI score based on intake on a given day or even over several nonconsecutive days is unlikely to reflect usual diet quality relative to the DGA. This is noteworthy because the HEI standards and the underlying USDA Food Patterns,35 as well as nutrient requirements where they are used (eg, sodium), are meant to be met over time, not necessarily every day. In cases in which data are collected for the individual using an FFQ, the HEI scoring algorithm could be applied, with recognition of likely biases in the intake data. In addition, any interpretation of HEI scores for a given individual should account for the fact that the scoring standards do not reflect a given person’s individual requirements, but rather are based on population-level recommendations and the least-restrictive standards, as noted previously.
Considerations in Interpreting HEI Scores
In interpreting HEI scores, it is important to bear in mind several factors, including leveraging the multivariate nature of the index to gain a full understanding of diet quality and patterns, as well as issues related to comparing scores between HEI versions and over time, and limitations due to measurement error (Figure 1). Appropriate interpretation of HEI scores includes assessment of total scores indicative of overall diet quality, as well as component scores to examine the quality of the mix of foods consumed. Particularly for scores in the midrange, total scores may be based on middling scores on all components or high scores on some and low scores on others. Examining scores for the individual components in addition to total scores10 is recommended to maximize one’s understanding of diet quality and patterns.
It is possible to use a graded approach to describe diet quality, as outlined in an article describing the HEI-2015.15 The grades provide an indication of the degree to which diets conform with guidance as operationalized by the HEI. Briefly, grades range from A (90 points or above) to F (0 to 59 points), with points in between graded accordingly. Grades do not reflect the degree to which nutrient requirements are met nor the appropriateness of energy intake, but rather the quality of the mix of foods. Further, it is emphasized that grades should be used in combination with numerical scores, not alone. As well, numerical scores rather than grades should be used in further analyses making use of the HEI (eg, regression modeling to examine associations with other variables) because categorizing results in a loss of information and may result in misclassification of scores at or near cut points used for differentiating grade levels.15
In utilizing the HEI to monitor trends in diet quality over time or assess the effects of interventions, it is necessary to consider what constitutes meaningful differences between groups or change over time. This may also be salient to epidemiologic analyses in interpreting the magnitude of differences in HEI scores that are associated with differences in risk of disease. Previous analyses of HEI scores have shown that the standard deviation of the usual distribution of HEI scores is approximately 10 among children and 11 to 12 among adults (data not shown). Applying an effect size of 0.5 (which may denote a moderate effect), a difference between independent groups of 5 to 6 points might be considered meaningful. However, it is possible that the standard deviation may differ by population and assessment tool, suggesting that researchers need to carefully evaluate differences over time or across groups in the context of the range of scores observed in the study and/or similar studies. Other factors that might have contributed to changes in scores over time, such as intervention-related biases or changes to the food supply, should also be considered. Further, depending on the assessment tool used, the degree of within-person or day-to-day variation,43 and the scoring method used, scores based on data for a given day may be different than those computed using data for another day. Analyses of repeat measures may also need to account for correlation across time points.
Due to changes across the iterations of the HEI described previously, changes in scores may be observed when different versions of the HEI are applied to the same dataset. For the most part, the shifts in scores represent desired refinements of HEI scores to better reflect evolving dietary guidance, but these nonetheless need to be addressed when comparing research findings based on different HEI iterations. Based on internal analyses of NHANES data from 1999–2000 through 2011–2012, the application of the HEI-2010 vs the HEI-2005 using the population ratio method tends to result in lower total scores of a magnitude of about 6 points on average (data not shown). In the 2005 version, Meat and Beans was weighted at 10 points (the mean score in all years from 1999–2000 through 2011–2012 was 10), whereas in the 2010 version, that component was subdivided into two subgroups. Total Protein Foods is akin to Meat and Beans conceptually and receives the maximum points across all years. Seafood and Plant Proteins is also scored to a maximum of 5 points; however, scores are below 5 across the years, resulting in lower scores overall for the 2010 index. As well, comparing the 2010 to the 2005 index, mean scores for Fatty Acids (vs Oils); Greens and Beans (vs Dark Green and Orange Vegetables); Sodium; and Solid Fats, Alcohol, and Added Sugars (vs Empty Calories) tend to be lower.
Analysis using NHANES 2011–2012 and the population ratio approach results in total scores for the HEI-2015 that are higher by ~1 point compared with the HEI-2010.34 Contributors to this difference include higher component scores due to counting legumes toward all vegetable and protein components in the HEI-2015, the influence of which is attenuated by slightly lower points for components capturing empty calories in the 2015 vs the 2010 index.
In comparing the effect of changes between versions of the index on scores, it is possible that particular dietary patterns may be more or less affected. For example, large shifts in scores may be seen for some diets, particularly when a large proportion of the calories comes from dietary components captured differentially across different versions of the HEI. For example, the change in counting of legumes from 2010 to 2015 will have a larger effect on scores when examining diets in which intake of these is high.
In addition to considering changes across versions of the HEI, researchers may find it desirable to make modifications to the index for their own purposes. In the event of adapted versions of the index, the resulting scores do not represent those yielded by the standardized metric known as the HEI. Such changes should be carefully documented, along with a discussion of potential implications for comparing the results with other studies making use of the HEI.
Finally, as noted above, in applications of self-report dietary intake data, it is important to consider the influence of measurement error in the interpretation of HEI scores. Different dietary components appear to be misreported to different degrees.48,49 To the extent that less healthy foods may be underreported and more healthy foods may be overreported, HEI scores based on self-report intake data may be overly optimistic.
CONCLUSIONS
The HEI is a diet quality index measuring alignment with federal dietary guidance that can be used to address various research questions, with techniques for different applications continuing to evolve. The statistical methods required for some applications can be complex and computationally intensive. Researchers are encouraged to consult a statistician early in the planning stages of projects making use of the HEI to ensure that the appropriate data are collected and analytic techniques are well matched to the research question. Researchers are also encouraged to use the checklist (Figure 1) to ensure that salient considerations are attended to and scientific articles include the necessary details so that research making use of the HEI can be interpreted appropriately and replicated, helping to build a cohesive body of evidence pertaining to dietary quality in accordance with federal dietary guidance.
Supplementary Material
FUNDING/SUPPORT
S. I. Kirkpatrick is supported by the National Cancer Institute (NCI) (grant no. HHSN261201500365P) and in part by a Canadian Cancer Society Research Institute Capacity Development Award (grant no. 702855). J. A. Tooze is supported by NCI grant no. HHSN261201500411P and in part by NCI Cancer Center Support grant no. P30 CA012097 to the Comprehensive Cancer Center of Wake Forest Baptist Medical Center.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
Supplementary materials:
PowerPoint presentation available at www.jandonline.org
References
- 1.US Department of Health and Human Services and US Department of Agriculture 2015–2020 Dietary Guidelines for Americans, 8th Edition 2015. https://health.gov/dietaryguidelines/2015/guidelines/. Accessed July 11, 2018. [Google Scholar]
- 2.2015 Dietary Guidelines Advisory Committee Scientific Report of the 2015 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. Washington, DC: US Department of Agriculture, Agricultural Research Service; 2015. https://health.gov/dietaryguidelines/2015-scientific-report/pdfs/scientific-report-of-the-2015-dietary-guidelines-advisory-committee.pdf. Accessed July 11, 2018. [Google Scholar]
- 3.US Department of Agriculture Nutrition Evidence Library. 2015 Dietary Guidelines Advisory Committee Nutrition Evidence Library (NEL) Systematic Reviews. 2015. http://www.nel.gov/category.cfm?cid=50. Accessed September 12, 2017.
- 4.Krebs-Smith SM, Subar AF, Reedy J. Examining dietary patterns in relation to chronic disease: Matching measures and methods to questions of interest. Circulation. 2015;132(9):790–793. [DOI] [PubMed] [Google Scholar]
- 5.Liese AD, Krebs-Smith SM, Subar AF, et al. The Dietary Patterns Methods Project: Synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145(3):393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ocké MC. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc Nutr Soc. 2013;72(2):191–199. [DOI] [PubMed] [Google Scholar]
- 7.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11): 1896–1901. [DOI] [PubMed] [Google Scholar]
- 8.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB. Evaluation of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11): 1854–1864. [DOI] [PubMed] [Google Scholar]
- 9.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113(4):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144(3):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6): 1009–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fung TT, McCullough ML, Newby PK, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–173. [DOI] [PubMed] [Google Scholar]
- 13.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7): 713–720. [DOI] [PubMed] [Google Scholar]
- 14.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8): 1093–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krebs-Smith SM, Pannucci TR, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schap T, Kuczynski K, Hiza H. Healthy Eating Index-beyond the score. J Acad Nutr Diet. 2017;117(4):519–521. [DOI] [PubMed] [Google Scholar]
- 17.Wilson MM, Reedy J, Krebs-Smith SM. American diet quality: Where it is, where it is heading, and what it could be. J Acad Nutr Diet. 2016;116(2):302–310.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savoca MR, Arcury TA, Leng X, Bell RA, Chen H, Anderson A, et al. The diet quality of rural older adults in the south as measured by Healthy Eating Index-2005 varies by ethnicity. J Am Diet Assoc. 2009;109(12): 2063–2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George SM, Ballard-Barbash R, Manson JE, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: Evidence to inform national dietary guidance. Am J Epidemiol. 2014;180(6):616–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harmon BE, Boushey CJ, Shvetsov YB, et al. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: The Dietary Patterns Methods Project. Am J Clin Nutr. 2015;101(3): 587–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality Is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144(6): 881–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nansel TR, Laffel LM, Haynie DL, et al. Improving dietary quality in youth with type 1 diabetes: Randomized clinical trial of a family-based behavioral intervention. Int J Behav Nutr Phys Act. 2015;12(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang S, Midthune D, Guenther PM, et al. A new multivariate measurement error model with zero-inflated dietary data, and its application to dietary assessment. Ann Appl Stat. 2011;5(2B): 1456–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freedman LS, Guenther PM, Krebs-Smith SM, Dodd KW, Midthune D. A population’s distribution of Healthy Eating Index-2005 component scores can be estimated when more than one 24-hour recall is available. J Nutr. 2010;140(8): 1529–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freedman LS, Guenther PM, Krebs-Smith SM, Kott PS. A population’s mean Healthy Eating Index-2005 scores are best estimated by the score of the population ratio when one 24-hour recall is available. J Nutr. 2008;138(9):1725–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krebs-Smith SM, Reedy J, Bosire C. Healthfulness of the US food supply. Am J Prev Med. 2010;38(5):472–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reedy J, Krebs-Smith SM, Bosire C. Evaluating the food environment: Application of the Healthy Eating Index-2005. Am J Prev Med. 2010;38(5):465–471. [DOI] [PubMed] [Google Scholar]
- 28.Miller PE, Reedy J, Kirkpatrick SI, Krebs-Smith SM. The United States food supply is not consistent with dietary guidance: Evidence from an evaluation using the Healthy Eating Index-2010. J Acad Nutr Diet. 2015;115(1):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirkpatrick SI, Reedy J, Kahle LL, Harris JL, Ohri-Vachaspati P, Krebs-Smith SM. Fast-food menu offerings vary in dietary quality, but are consistently poor. Public Health Nutr. 2014;17(4): 924–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: Design and applications. J Am Diet Assoc. 1995;95(10): 1103–1108. [DOI] [PubMed] [Google Scholar]
- 31.Woodruff SJ, Hanning RM. Development and implications of a revised Canadian Healthy Eating Index (HEIC-2009). Public Health Nutr. 2010;13(6):820–825. [DOI] [PubMed] [Google Scholar]
- 32.US Department of Agriculture and US Department of Health and Human Services Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: US Government Printing Office; https://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf. Accessed July 11, 2018. [Google Scholar]
- 33.US Department of Health and Human Services and US Department of Agriculture Dietary Guidelines for Americans, 2005. 6th Edition Washington, DC: US Government Printing Office; https://health.gov/dietaryguidelines/dga2005/document/pdf/DGA2005.pdf. Accessed July 11, 2018. [Google Scholar]
- 34.Reedy J, Lerman J, Tooze JA, et al. Evaluation of the Healthy Eating Index-2015. J Acad Nutr Diet. 2018;118(9):1622–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Center for Nutrition Policy and Promotion. USDA food patterns. https://www.cnpp.usda.gov/USDAFoodPatterns. Accessed February 13, 2018.
- 36.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 37.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140(10):1832–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tooze JA, Midthune D, Dodd KW, et al. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106(10): 1575–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freedman LS, Guenther PM, Dodd KW, Krebs-Smith SM, Midthune D. The population distribution of ratios of usual in-takes of dietary components that are consumed every day can be estimated from repeated 24-hour recalls. J Nutr. 2010;140(1): 111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Cancer Institute. Dietary assessment primer. 2015. https://dietassessmentprimer.cancer.gov/. Accessed September 12, 2017. [DOI] [PMC free article] [PubMed]
- 41.Lachat C, Hawwash D, Ocké MC, et al. Strengthening the Reporting of Observational Studies in Epidemiology—Nutritional Epidemiology (STROBE-nut): An extension of the STROBE statement. PLOS Med. 2016;13(6):e1002036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Cancer Institute. HEI tools for researchers. 2016. https://epi.grants.cancer.gov/hei/tools.html. Accessed September 12, 2017.
- 43.Thompson FE, Kirkpatrick SI, Subar AF, et al. The National Cancer Institute’s Dietary Assessment Primer: A resource for diet research. J Acad Nutr Diet. 2015;115(12):1986–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thompson FE, Subar AF. Dietary assessment methodology In: Coulston A, Boushey C, Ferruzzi M, eds. Nutrition in the Prevention and Treatment of Disease. 3rd edition New York, NY: Academic Press; 2013:5–46. [Google Scholar]
- 45.Miller PE, Mitchell DC, Harala PL, Pettit JM, Smiciklas-Wright H, Hartman TJ. Development and evaluation of a method for calculating the Healthy Eating Index-2005 using the Nutrition Data System for Research. Public Health Nutr. 2011;14(2):306–313. [DOI] [PubMed] [Google Scholar]
- 46.SAS [computer program]. Version 9.4 Cary, NC: SAS Institute Inc; 2017. [Google Scholar]
- 47.Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: The NCI method. Stat Med. 2010;29(27): 2857–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freedman LS, Commins JM, Moler JE, et al. Pooled resultsfrom 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am J Epidemiol. 2015;181(7):473–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Freedman LS, Commins JM, Moler JE, et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for energy and protein intake. Am J Epidemiol. 2014;180(2):172–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Subar AF, Kirkpatrick SI, Mittl B, et al. The Automated Self-Administered 24-hour dietary recall (ASA24): A resource for researchers, clinicians, and educators from the National Cancer Institute. J Acad Nutr Diet. 2012;112(8):1134–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Willett WC. Nutritional Epidemiology. 3rd edition Oxford, UK: Oxford University Press; 2013. [Google Scholar]
- 52.Subar AF, Freedman LS, Tooze JA, et al. Addressing current criticism regarding the value of self-report dietary data. J Nutr. 2015;145(12): 2639–2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.