Abstract
Patients with temporomandibular disorders (TMD) can become very complex. This article aims to highlight the importance of the multimodal and multidisciplinary approach in this type of patients to improve clinical outcomes. At present we have innumerable techniques and tools to approach this type of patients from a biopsychosocial model where active and adaptive type treatments are fundamental. There are various health professions that have competence in the treatment of TMD, however, although in the most complex cases should be treated simultaneously, still too many patients receive unique treatments and only from one point of view. This review exposes the treatments available from a clinical-scientific perspective and also emphasizes the importance of working in specialized units with those professionals who have competencies on the different conditions that may occur.
Keywords: temporomandibular disorders, physiotherapy, psychology, odontology, surgery
Introduction
Temporomandibular disorders (TMDs) present a challenge for health professionals, due to the great complexity of the condition. This complexity is evident in various aspects, including accurate diagnostic methods, treatment, associated comorbidities and the socioeconomic impact they entail. TMD cases are even more complex when the pathology becomes chronic or persistent.
By the mid-1970s, a new care concept was born: the multidisciplinary approach. This approach integrates a group of specialists dedicated jointly to the study, diagnosis and management of chronic pain conditions. The multidisciplinary approach had its origins at the University of Washington. Professor John J. Bonica led a novel project at the university’s multidisciplinary clinic that ranged from the systematic study and scientific dissemination of various painful syndromes to the clinical management of these syndromes. This project finally led to the creation of the International Association for the Study of Pain in 1985.
Thus, to approach TMD treatment with certain guarantees of success, it is necessary to possess all the available tools. The present manuscript thus aims to describe various ways of improving the results for patients with TMD of different types; all from a point of view based on current scientific evidence.
For better understanding, this paper will explain the available procedures independently and then explore some clinical implications that give meaning to multidisciplinary and multimodal treatment from a highly clinical approach. All the approaches explained below contain a detailed explanation preceded by a short introduction to put the reader in context.
Main evidence-based treatments
Psychological approach
Scientific evidence has accumulated suggesting that a variety of psychological characteristics, such as stress and anxiety, as well as social characteristics, such as the role of family and environment, play a relevant part in the progress and/or maintenance of TMD pain. Several psychological aspects have been implicated in the development of clinical manifestations1 and pain chronification.2 These aspects have also been associated with bruxism intensity.3,4 Alone, however, they have not yet been recognized as a risk for TMD progression. TMD pain has come to be accepted as the result of interactions between physical and psychological factors.5
During the first 6 months of pain, the discriminative system dominates the motivational/affective system; it is during this period that the patient’s brain can more easily locate the pain. Nevertheless, as time progresses, the system switches to greater dominance from the motivational/affective system. It is at this time that psychological symptoms begin to appear; if these are not considered during treatment, they can perpetuate and maintain the TMD.6,7 Biobehavioral factors can promote or prolong physical dysfunction, and thought processes and emotions can become distorted. These factors are as important to treat as the physical disease factors are, if the patient is to return to normal functioning, especially in the case of chronic pain.7
Researchers have proposed several psychological factors related to TMD development and maintenance, such as fear of pain, coping, catastrophizing, fear of movement, depression, stress, somatization and anxiety,8 which is why the psychological component should always be considered. Psychological therapy should be included in the classical biomedical treatment modalities of this group of patients to improve outcomes.9 Psychological therapies are mainly used to provide patients with the ability to comprehend and control pain.10
Biobehavioral treatment is noninvasive and reversible and can help control pain as well as improve the functional and affective impairment associated with TMD. This therapy includes several methods and procedures, such as relaxation, cognitive-behavioral techniques and self-management.11
Relaxation
Relaxation is based on a passive and tranquil manner of thinking achieved by focusing attention on a neutral object or objects; for example, regions of the body or the breathing, while distracting thoughts are ignored.12 This technique centers on achieving control over the physiological response to stressful experiences such as pain.11 Relaxation techniques, such as progressive muscular relaxation, trigger a neurophysiological response, causing muscle relaxation and decreasing the neuroendocrine reaction to an adverse event,11,13 offering patients a sensation of wellness and decreased anxiety and stress.14 This technique could be controlled externally using electromyography or a biofeedback system.15,16
This therapy can decrease sensory input and the affective aspects of pain and can reduce the need for medication in various patient groups with pain, such as those with chronic back pain, headache, TMD or fibromyalgia.17
Cognitive behavioral therapy and education
Cognitive behavioral therapy (CBT) has been shown to be a beneficial technique for individuals with chronic TMD.18 CBT consists of identifying and modifying maladaptive thought patterns linked to pain conditions or behaviors through use of coping skills (eg, avoiding thinking about the pain, directing the thoughts toward another topic, continuing with the usual activities).11 Pain neuroscience education is the basis from which to help and motivate patients to use these skills in coping with their pain,19 and is explained using simple and clear language.11,19 The purpose of this technique is to improve self-control of painful events.19
Self-management
Also known as “self-care” in the literature, self-management (SM) is considered one of the central parts of management of patients with TMD.20 Its purpose is to modify the patient’s behavior and can include the following multimodal care:18,21
Physiotherapy
Basic elements of CBT, including education
Relaxation techniques
Reinforcement of desired behaviors and withdrawal from unwanted behaviors
Medication
Dental treatment
It is a safe technique and no adverse factors have been described, suggesting a potentially favorable risk:benefit ratio for SM.21
In conclusion, biobehavioral techniques include therapeutic, safe, noninvasive and reversible interventions to improve coping abilities and self-control skills in patients with TMD13 and are a good complementary technique to other treatments including physical therapy and pharmacological and dental treatment.18,22,23
Brain training
Some patients with TMDs present limitation in mouth opening, as well as pain and/or fear of movement. In these cases, the patients cannot actively move their temporomandibular joint (TMJ). Brain training through motor imagery (MI) and action observation (AO) is possible for these patients. These techniques produce the activation of the same neurocognitive mechanisms (planning and execution) that develop during an actual action. In 1996, MI was defined as a dynamic mental process of a representation of an action, internally, without the real motor movement,24 which can be employed to improve motor performance and learn motor tasks, inducing the activation of various cortical areas, influencing the central nervous system and causing plastic changes in the brain.25 AO therapy is defined as a technique that evokes internal motor simulation in real time of the movements that the individual visually perceives.26 Mental rotation is an MI task that has been used in studies of patients with TMD; it consists of presenting rotated images of a body part to an individual, who evaluates whether the images are of a left or a right side.27 In 2015, Von Piekartz et al.28 had concluded that people with chronic facial pain were less accurate than controls at a left/right facial posture judgment task. Along these lines, in 2018, Uritani et al.29 used mental rotation for comparing individuals with and without painful TMD, observing that the reaction time in mental rotation was slower and the accuracy was lower in individuals with TMD than in those without TMD, concluding that TMD might influence MI in the orofacial region.27
Physical therapy approach
TMD is a term that pools several conditions that affect the various anatomical structures related to the temporomandibular joint.30 Of all the clinical manifestations, pain is the main reason why patients with TMD seek clinical assistance. Nevertheless, other signs and symptoms, such as impaired mobility, joint sounds and head and neck pain are usually also manifested, altering the patient’s function and quality of life.31 Hence, pain relief and restoration of motor function are the main goals of managing patients with TMD.
According to the World Confederation for Physical Therapy, physical therapy is a healthcare profession aimed at reducing pain and it is the most important discipline to restore and improve movement that has been threatened by injuries, disorders, aging, or environmental factors.32 Therefore, physical therapy is an important pillar in the management of patients with TMD through the following therapeutic options:33–35
Electrotherapy
Some of the following electrotherapy techniques are typically applied to reduce pain and improve function in patients with TMD: transcutaneous electrical nerve stimulation (TENS), pulsed radiofrequency energy, lower-level laser therapy (LLLT) and shock waves. However, the current literature does not recommend the use of TENS, pulsed radiofrequency energy or shock waves to reduce pain intensity, and indicates contradictory outcomes from LLLT.36,37 To establish more robust conclusions related to LLLT effectiveness, the literature suggests homogenizing the choice of frequency and intensity parameters.36 Nevertheless, LLLT has shown effectiveness in improving range of motion in patients with TMD, which could be explained by a decrease in inflammation due to the suppression of cyclooxygenase. This reduced inflammation would allow a greater range of joint motion; however, the mechanisms of LLLT remain unclear.38
Neuromusculoskeletal physical therapy
According to the International Federation of Orthopaedic Manual Physical Therapy, orthopedic manual therapy is responsible for managing neuromusculoskeletal dysfunctions using specific and therapeutic evidence-based alternatives, such as manual techniques and therapeutic exercises.39
Manual (“hands-on”) techniques include joint-nerve mobilization, joint manipulations and soft tissue techniques,35,40 whereas therapeutic exercise involves exercises to increase mobility, motor control and endurance of masticatory muscles. Both have demonstrated good results in pain relief pain and improving TMJ function when used separately, although the combination of both interventions has yielded better results.35
Manual therapy techniques work through mechanical inputs that trigger peripheral and central neurophysiological mechanisms that reduce pain intensity and muscle spasms.41,42 Meanwhile, exercise therapy includes, in addition to hypoallergenic neurophysiological mechanisms, a shift by the patient toward self-control of the situation by active coping, improving pain tolerance, function and locus of control.43–45
Moreover, the literature has shown that both therapies can be applied not only to the orofacial region but also to the cervical spine, particularly the upper cervical region, reducing pain and improving the function of patients with TMD.35,40 This improvement could be explained by the neuroanatomical connection between the nociceptive inputs that run from the first 3 spinal segments (C1–C3) to the trigeminal–cervical caudal nuclei, where they converge with the orofacial nociceptive afferents.46 The literature also suggests a biomechanical relationship between TMJ movement and the position and movement of the cervical spine.47,48
Therefore, neuromusculoskeletal physiotherapy is considered to play an important in patients with TMD, and we should no longer consider manual therapy and therapeutic exercise in isolation. The current proposal is to apply manual therapy to improve movement and modulate pain, creating a window of opportunity to begin performing various therapeutic exercises with the aim of increasing their effects and to engage patients in their own treatment. Furthermore, if pain dominates the patient condition, the therapist could mobilize further the TMJ; even when the neck has not shown adverse signs or symptoms, mobilization of the upper cervical spine could be used to modulate pain.
Education and self-management in physical therapy
Various therapeutic educational alternatives to promote patient self-management are commonly applied by physiotherapists. Although, alone, they have not shown better outcomes than other physical therapy interventions, such as manual therapy or therapeutic exercise,47–52 results improve if combined with education and self-improvement interventions,51,52 as explained above.
The best education and self-management strategy for patients with TMD has not yet been determined. However, education based on a neuroscience approach, highlighting the differences between pain and nociception, emphasizing that the injured tissue is neither necessary nor sufficient to perceive pain, and providing a list of contributing factors that could perpetuate the symptomatology such as negative thoughts, emotions, anxiety or scant physical activity, has shown good results in pain relief, reducing psychosocial factors and disability in patients with chronic musculoskeletal pain.23 Thus, we propose to include this approach within the neuromusculoskeletal physiotherapy model.
Dry needling and acupuncture
Dry needling (DN) is defined as an
invasive procedure during which a thin filiform needle is inserted directly, without injection of any substance, into an active myofascial trigger point, with the condition of provoking a local contraction response.53
In relation to patients with TMD, evidence has shown that DN is useful for short-term reduction of pain and increasing function in those patients diagnosed with myofascial TMD.53–56
Acupuncture is often confused with DN; however, acupuncture is applied at specific body sites known as acupuncture points, and not just at myofascial trigger points, with the aim of influencing the physiological functions of the body.57 Although this therapeutic modality has shown short-term benefits in terms of pain reduction in patients with myogenic TMD, it has not shown good results for improving range of motion in TMJ.58,59
Better effects are obtained by applying acupuncture in the orofacial region itself than at standard acupuncture points far from this region.60 According to Goddard et al,60 these results might be explained by the implication of peripheral opioid receptors blocking the local nociceptive input during the therapeutic process. Likewise, when comparing DN results with those of acupuncture, there are no differences between them, even compared with placebo.58,59,61 In fact, it has been shown that the superficial application of a needle into the skin releases hypoalgesic substances such as serotonin and opioids.62–66
In conclusion, it is likely that these neurophysiological DN and acupuncture mechanisms are trigged by the skin perforation, with the physiotherapist being able to choose to prick deeply, superficially, near or far from the orofacial region depending on the hypersensitivity of the patient with TMD.
Odontology
The most common TMD treatments in dental practice after its clinical diagnosis are nonspecific in nature and can be prescribed and/or used by various professionals. Other treatments are purely dental, and it is to these professionals that this specific section is dedicated, particularly because there is controversy about their usefulness. However, they are not the only part of the TMD treatment performed by the dentist.
First, the diagnosis of the specific pathology is necessary to determine whether the problem requires a dental approach, as well as the objectives to aim for and which instrumentation or treatment to use.
These disorders include a wide range of pathologies that, even with some symptoms and signs in common, do not necessarily share the same etiology, pathophysiology or treatment.
Paraphrasing Fricton, “the most frequent cause of therapeutic failure is a bad diagnosis.” For most authors, it is a mistake to try to treat TMD as a single disease.67,68 No less important is the acute or chronic nature of the TTM, due to the implications of treatment that it entails.
Dental treatment is based mainly on the use of intraoral orthopedic devices, which are called orthoses or occlusal splints.
Intraoral orthopedic devices
In their various modalities, orthopedic intraoral devices are commonly used,67,69,70 both in the treatment of most TMD pathologies and for patients with bruxism.
Although many different devices are available, currently the most commonly used and those to which we will refer are those for stabilization and anterior replacement (full or partial coverage). However, we know little from the literature their mechanism of action, the most effective designs and materials, the indications for each type and their adverse effects.
Various systematic reviews and meta-analyses have shown no evidence of sufficient quality to answer any of these questions. Most studies have not had a large enough sample, have not proposed the same device design, have not been followed up, have been performed under the heading of general TMD (not for each specific pathology) and have not met the minimum criteria of quality required. Even the approaches used for the evaluation of the splints in the various systematic reviews have not been uniform.67,68 Thus, the main conclusion from all the literature is the need to perform further quality research.
Regarding stabilization splints, whose standard is the classic Michigan splint, the literature has not been able to provide solid evidence on its mechanism of action, nor on the characteristics of splint, indications or adverse effects. Zhang et al,69 in a 2016 meta-analysis, had recommended its use for the treatment and control of TMD in adults after finding reduced pain in patients with TMD. Michigan splints are effective for reducing limitations and moderating pain in patients with painful disc displacement with reduction (DDwR). In another recent meta-analysis, from 2017, Kuzmanovic et al.67 concluded that stabilization splints are effective in reducing pain in the short term, equaling other long-term therapeutic modalities. Alajbeg et al.71 also reported an increase in oral quality of life in relation to the use of these devices. It should be noted that in its guidelines, the American Academy of Orofacial Pain (AAOP)68 recognizes the success of these splints as a conservative treatment.
It is necessary to differentiate the role of stabilization splints as a key treatment in some TMD pathologies from their coadjuvant role in others,70,72 and as protection from masticatory structures in cases of bruxism or occlusal TMD sequelae.73 Generally, combined treatment with other therapies obtains better results.
Traditionally, it has been recommended that their effect is due to the ideal occlusion they provide (both in the distribution of the occlusal contacts and in guides). However, given that the TMD–occlusion relationship is uncertain, this argument is controversial. A distracting effect on TMJ has also been described, leading to a reduction in joint overload,72,74 as well as neuromuscular effects due to the alteration of proprioceptive stimuli,72,75,76 the placebo effect and central nervous system effects, as shown by studies that evaluate their effect on psychological aspects.70,76 In any case, the mechanism of action continues to be a question.
Indications
Although it is discussed, stabilization splints are used in joint pathology for the control of overload on structures generated mainly by sleep bruxism. Thus, splints will be indicated in cases of arthralgia, in cases of incipient symptomatic DDwR and to control overload on the retrodiscal tissue in cases of disc displacement without reduction (DDwoR), with and without limitation of mouth opening in patients with risk factors for degenerative processes (hypoplasic condyles, hypermobility, sleep bruxism).68,75
Stabilization splints are likewise usually indicated for patients with osteoarthritis associated or not with DDwoR, to favor positive remodeling of the joint, reductions in inflammation and condylar recorticalization, with its use being positively associated with other treatments.72,77
In cases of systemic arthritis, Michigan splints are used as co-adjuvants with typical medication to relieve arthralgia, to reduce overload and associated joint degeneration, and they are also used in children with juvenile idiopathic arthritis.78 The splints are also useful as adjuvants to control muscle pain associated with arthritis, as well as to provide occlusal stability, decreasing the load on dentoperiodontal structures when secondary malocclusions appear.
In cases of patients with myofascial muscle pain, splints can be used both as a pain treatment themselves or as co-adjuvants of other treatments. Kuzmanovic67 found in his meta-analysis that patients with myogenic TMD benefited significantly from treatment with occlusal splints. However, van Grootel argues that, if it is possible to control the clinical situation with other treatments, these other treatments would be desirable to improve outcomes in TMD patients.79
In patients with sleep bruxism, its etiology is fundamentally from central nervous system;80 therefore, the discharge splints do not cure it. Splints are effective in preventing the damage that overload generates on the structures of the system, especially in terms of dental protection.81
Contraindications
Splints should not be used in patients with morning intermittent locking or in small symptomatic DDwoR that can promote its progression or blockade. If their use is essential, it must be included in the consent document; however, it should be remembered that asymptomatic DDwoR cases (no pain, no blockage) do not require treatment. Splints are also not indicated in patients with short-term DDwR for whom recapturing is possible (an anterior replacement splint will be indicated).75
The use of these devices in patients with apnea-hypopnea syndrome is controversial, given the relationship between them (devices and apnea improvement) is not yet clear,82–84 and episodes of apnea could worsen in those patients for whom bruxism might act as a protective factor.80,85
In children, the controversy over whether the devices interfere with growth and the possibility of generating orthopedic changes is not yet resolved. It is necessary to weigh the treatment indications for rigid discharge splints and, most importantly, replacement splints for their orthopedic effect. Some authors, including the AAOP, defend the indication of soft splints for children.68,78
Undesirable effects
It is essential that splints are made, adjusted and supervised by a dentist. It is important to periodically review the splints to compensate for the changes that occur and to closely assess the evolution of the patient. The AAOP advises dentists to reevaluate the case if there has been no response in 3 or 4 weeks and to assess other factors involved.68
The most feared undesirable effect is occlusal change, such as an anterior or posterior open bite, depending on the device being used. The discharge plates must have full coverage of the arch in which they are located and present contacts of all opposing teeth to prevent the risk of dental extrusions and occlusal changes. These effects are minimized with periodic professional monitoring of the splint adjustment and avoiding its use 24 hrs per day. Generally, these adverse effects do not appear with only nocturnal use. However, cases of occlusal change have been reported in well-adjusted splints,73 related to a mandibular rotation mechanism. Other adverse effects are psychological dependence and, in terms of maintenance and oral habits of the patient, caries and gingivitis.68
Confection and adjustment characteristics
The lack of homogeneity in the criteria of what comprises a correct stabilization splint is a hindrance to obtaining quality scientific evidence. Although the requirements for a stabilization device are clear68 — rigid acrylic material, flat without traces, with canine or anterior guide, flat incisal shelf and in the most unstable arcade — most of these requirements are not met in studies that compare them with other treatments. This controversy arises in all fields of confection and adjustment. Thus, there is no agreement on whether occlusal traces should be missing or not, the location of the anterior guide, their thickness or whether they should be of rigid or soft material.86–88 Several studies that have compared the effectiveness of soft and hard splints have found a reduction in the signs and symptoms of TMD with both types of splints, giving greater credibility to the use of hard splints,89 especially in cases of bruxism;76 however, some authors argue that soft splints are faster and are as effective in relieving symptoms as hard splints.90
Time and duration
The use of a splint should be nocturnal or at most two-thirds of the day to avoid occlusal changes. It is logical to restrict its use to those periods in which there is greater overload, which usually coincides with the night period. In specific cases, such as recent DDwoR, its use can be indicated all day but for limited periods of time. Some studies report better results with 24 hr use, not considering the high risk of occlusal changes.67 Regarding the period during which extended use should be practiced, it would depend on the indication for the device. In cases of bruxism, discontinuous use has been shown to be more effective. In cases of degenerative processes, it is are recommended to confirm usage based on imaging, stability and favorable adaptation of the joint.
Anterior replacement devices
This type of device shows even less evidence than stabilization splints. Anterior replacement devices, such as anterior positioning appliance, are usually placed in the upper arch for simplicity and comfort. It presents a barrier that forces closure in an advanced position of the jaw such that a correct condyle:disc ratio68,78 is obtained for those joints in which the disc was previously displaced. Periodic revisions are fundamental to control for the possible appearance of later open bites.
Classically, use of anterior replacement devices was recommended in cases of disc displacements to return to its original position, using it during a period of 24 hrs and later relocating it to the patient’s usual position. However it was later reported that the disc replacement was not achieved91 or was not stable, and that there was a risk of significant posterior open bite. Really, on its capacity of disc replacement, only stayed the name of the device.
Currently, its main indication is for morning jaw locking due to DDwR and intermittent blockade, but always ensuring that the degree of displacement does not exceed 3–4 mm of protrusion. These devices reduce pain, prevent blockage and sometimes soften the associated click. Likewise, they are also used for short periods of time in patients with newly emerging DDwoR to reduce the pain generated in the retrodiscal tissue.68,75
Mandibular advancement devices, used for the treatment of mild-moderate apnea-hypopnea syndrome, are not the subject of this review.
Occlusion treatment: dental procedures
The relationship between TMD and occlusion continues to be a controversial issue in dentistry, although this relationship has been increasingly losing importance, especially since the appearance of the biopsychosocial model and the abandonment of the mechanistic model.92,93 Currently the literature agrees that, although dental treatments related to occlusion are necessary in patients with TMD, it is not a treatment per se in their management.68
Along these lines, several authors75,94,95 have shown that the prevalence of malocclusions is the same in populations with TMD and in the general population. No occlusal characteristics are associated with risk of developing a TMD; some characteristics could even be more consequences than causes.93,96 Asymmetry and mandibular retrognathia have also been associated with disc displacements in rabbits.78
The stomatognathic system has a great ability to adapt to changes, including occlusal changes. From the constant eruption/dental change, the dental losses and their rehabilitations, the system adapts.75,97
The ability of these contacts to develop or aggravate pathology is, therefore, related to a failure of the patient’s adaptive system and the multiple factors that can diminish this capacity, not only to the proprioceptive alteration itself.
In experimental studies, it has thus been observed that in healthy individuals, in the presence of experimental interference (like a sudden alteration of the occlusion or an iatrogenic alteration during a rehabilitation treatment) the electromyography activity of the masseter decreases to prevent dental contact and injury,98,99 whereas the population with myofascial TMD maintains its behavior and does not present an injury avoidance response.100 In addition, the impact of these interferences on muscle pain and headache is much greater in individuals with a high frequency of parafunctions.101 Thus, there might be a deregulation of the mechanisms underlying the masticatory system and central nervous system rather than a peripheral problem of occlusion.102 Patients with TMD are hypervigilant and have a decreased ability to adapt to change.
Currently, no evidence supports the treatment of TMD through occlusal methods.96 It is of vital importance to assess the possibility of TMD recurrence and its stability before starting a definitive and irreversible treatment of the occlusion for reasons not associated with the TMD.
Occlusal adjustment
If there is no proven causal relationship between malocclusion and the appearance of TMD, there is no justification for performing an irreversible occlusion procedure in patients under the guise of a therapeutic purpose.93,103
Another issue is whether, once stabilized, an adjustment is needed for the sake of greater masticatory efficacy and a prevention of possible dental damage for a patient with TMD who has had sequelae from the occlusion.68,103,104
Orthodontics
Regarding orthodontics, three possibilities can be proposed according to their objectives.105 First, considering the above-mentioned TMD-occlusion relationship, orthodontics as a treatment for patients with TMD is not justified.104
The second scenario contemplates that, once TMDs are stabilized, orthodontic treatment can be considered to improve masticatory efficacy or prevent dental or aesthetic damage, but not to cure or prevent relapses. According to Michelotti,94 it must be borne in mind that orthodontics in patients with TMD who have already been treated varies depending on the specific pathology within the TMD that has been experienced, and we should look for the position that provides greater stability.105 He also notes that orthodontic treatments should be avoided in patients with TMD who have severe pain until it is resolved. It is likely that patients with previous pain are more likely to develop a TMD or it is more likely to worsen.
Third, according to the AAOP, orthodontics in the normal population “neither produces nor cures.”68,104,106 According to the Orofacial Pain: Prospective Evaluation and Risk Assessment study, orthodontics was a slight risk factor (odds ratio 1.4) for chronic TMD.107 It is convenient to perform a TMD screening before beginning an orthodontic treatment to identify those patients most likely to develop painful TMDs (eg, high somatization scores, patients with tightly packed teeth, short-faced patients, patients with significant overbite, a history of other body areas with pain, high frequency of parafunctions). Given their capacity for adaptation is diminished, they are hypervigilant and less tolerant of changes.
Finally, if TMD complications arise during orthodontic treatment, it will be necessary to stop treatment and solve these complications. According to some authors, it does not appear that functional orthodontics, the use of elastics78,105,106 or of aligners can generate TMDs; however, this issue is still controversial.
Surgery
With an uncertain etiology and a lack of understanding of its pathophysiology, the surgical management of TMD is one of the most controversial approaches in the field of oral and maxillofacial surgery.
TMJ surgery is reserved for patients whose TMJ pain and dysfunction are refractory to nonsurgical modalities and when symptoms result in significant impairment.108
Arthrocentesis
Arthrocentesis is a safe and rapid procedure used to treat a multitude of TMDs.109
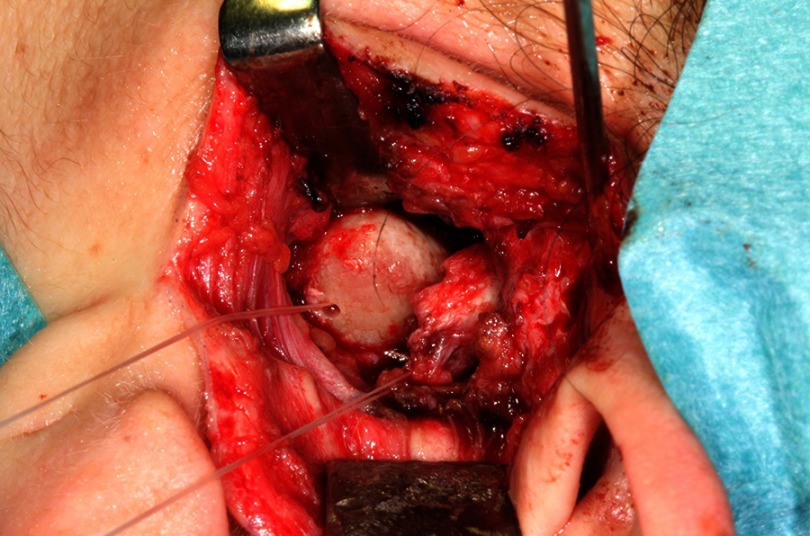
An auriculotemporal block and infiltration to the areas for joint penetration are completed using a local anesthetic. This technique includes the insertion of 2 needles into the TMJ along the canthal-tragal line; the first is placed into the upper joint compartment, and the second anterior to the first to allow correct TMJ lavage.110 Once the joint space is entered, it can be insufflated with Ringer’s lactate solution. The lavage is performed by the surgeon, using approximately 100 mL of fluid. At the completion of the procedure, sodium hyaluronate has been proposed as a therapeutic agent for the treatment of TMJ disorders (Figure 1).111
Figure 1.
Arthrocentesis of Temporomandibular Joint.
Arthroscopy
In the late 1980s and 1990s, many studies on TMJ arthroscopy were published. This surgical technique consisted of an arthroscopic sweep of the adhesions in the upper joint compartment by a blunt trocar and lavage of the joint space.112 The main advantage was that this procedure could be performed in approximately 30 mins using a single, safe puncture technique.
The TMJ is a synovial joint with two joint cavities (upper and lower), with an intervening articular disc. The volume of fluid in the upper and lower compartments is important to understand. The volume of the normal upper joint space is approximately 2 mL: however, it can increase to as much as 6 mL with pathology. The lower space volume is approximately 1 mL and can increase to 2 mL.
Arthroscopy can be undertaken, with the patient receiving a local (usually in a single-puncture observation of the joint) or general (most often in an operating room) anesthetic. Lidocaine with epinephrine can be injected subcutaneously for hemostasis at the puncture site. Ringer’s lactate solution is then injected into the upper cavity of the joint, and a puncture using the sharp trocar of a 1.9–2.3 mm arthroscope should be made along the tragacanthal line, approximately 1 cm anterior to the midtragus.113
The blunt obturator is placed in the 2.7-mm cannula and introduced anteriorly and superiorly along the path of the 2 previously made needle punctures. When the blunt obturator meets some resistance at the capsule, it is removed, and the sharp obturator is used to penetrate the superior joint space. After a pop into the intra-articular space is felt, the obturator is then immediately removed to prevent scuffing of the articular surfaces. By use of the locked connections, Ringer’s lactate solution is introduced into the joint space to confirm the position of the cannula. When correctly placed, back pressure or pistoning should be felt, along with forward movement of the mandible.
Once the capsule is changed, an 18-gauge needle is used as a temporary outflow port while the arthroscope is inserted and a careful examination around the superior space is conducted. The diagnostic arthroscopic examination begins with confirmation of proper entry into the joint, by identifying landmarks in the posterior-superior joint space (Figure 2).
Figure 2.
TMJ arthroscopy, superior space.
When the examination of the glenoid fossa is complete, the arthroscope should be directed to explore the joint disc. Disc mobility is observed by maintaining the arthroscope in a lateral position. For anterior recess examination, the condyle should be situated within the temporal fossa.
By measuring the length of the first trocar, the second puncture point can be established. The second puncture is performed at 90 degrees to the first. The surgeon should be able to see the entrance of the second trocar in his field in the anterior recess.
Lysis and lavage consist of the breakdown of adhesions between articular surfaces rinsed with abundant serum and then allowing the patients’ sleeping mandibular movements to do the rest. The ability to suture the temporomandibular joint disc to stabilize it in a more posterior and/or lateral position is a valuable TMJ arthroscopic technique.
Open surgical procedures
Multiple open surgical procedures have been described in the literature for the management of TMJ disc derangements.114 These include the following:
Disc repositioning
Discectomy
Disc replacement
TMJ prosthesis
A modified short endaural incision is made with an extension of 3 cm. The incision is placed within a preauricular skin crease, which is located posterior to the superficial temporal vessels and the auriculotemporal nerve. A sharp dissection is then made with scissors from the tragal cartilage downward, approximately 12–15 mm to the subcutaneous tissue. Digital manipulation is performed in order to identify the zygomatic arch and the condyle into the fossa when the mandible is moved laterally.
At this level, on top of the zygomatic arch, 8 mm in front of the tragal cartilage, a blunt dissection is made with Dean scissors, perpendicular to the arch, carried to the temporal muscle fascia, below the fat tissue. The dissection is continued anteriorly to expose the articular eminence. When the lateral capsule is identified, the superior joint space is insufflated with 2 mL of 1% lidocaine 1:100,000 epinephrine to hydraulically offset the disc inferiorly. The lateral capsular attachments are incised superficially with a #15 blade 45 degrees from an inferior to a superior aspect. A freer elevator is used to enter the superior joint space superficially. Care must be taken not to damage the posterior attachment of the disc while dissecting the capsule.
The capsule can be reapproximated and closed with interrupted 4/0 sutures. The deeper tissues that lie over the capsule are also closed with interrupted 4/0 sutures. Closure of an endaural incision begins by suturing the corners of the tragal portion of the incision with interrupted 5/0 sutures.
Disc repositioning
The disc is then inspected for deformities or perforations. Disc mobility is evaluated by applying traction with forceps. Disc repositioning is performed following wedge resection of the pathologic posterior attachment by posterior and lateral sutures.115
Some authors have had success with the use of mini anchors (titanium condylar implants) for better stabilization of the disc in a more physiologic position.116 The mini anchor, which is a metal insert with a suture attached to it, is placed in the posterolateral portion of condylar head. The suture is then used to secure the lateral and posterior of the disc to the condylar head (Figure 3).
Figure 3.
Temporomandibular joint disk repositioning with Mitek anchor.
Discectomy
If a deformed disc is determined to be unsalvageable, a discectomy is considered. Discectomy is indicated in several situations:
Irreparable disc perforation
Severe displacement
Complete loss of elasticity and deformation of the disc
Persistent pain and TMJ dysfunction even after disc repositioning
Partial and total discectomy have been described in the literature.117 The condyle can be conservatively recontoured to remove any irregularities or osteophytes. After a discectomy, some masticatory muscle and joint tenderness can be expected for a variable period from several weeks to months. Postdiscectomy physical therapy is essential because the therapy helps the patient reestablish an adequate range of motion, among other benefits.
Disc replacement
Many arthroplasty procedures were developed to reshape and reposition the displaced or deformed disc or to remove and replace the disc with some type of disc substitute material as a temporary (Silastic, Michigan Medical Corporation, Santa Barbara, CA, USA) or permanent (dermis, cartilage, fascia, temporalis) replacement (Figure 4).
Figure 4.
Intraoperative view of the temporomandibular joint showing a dermis interposition graft after diskectomy.
Over the years, numerous alloplastic implants and autogenous materials have been used for disc replacement; however, foreign body reactions have been reported, and no ideal material has yet been identified.118
The exact advantages of autogenous tissues for disc replacement are not clear, and donor site morbidity and difficulties in anchoring any graft material to remaining tissues (retrodiscal tissue remnants, lateral pterygoid muscle attachments or the lateral pole of the condylar head) continue to be problematic technical concerns for surgeons.
Animal studies have suggested that autogenous graft placement alter discectomy is beneficial.
TMJ prosthesis
The primary goal of alloplastic total TMJ replacement (Figure 5) is the long-term restoration of mandibular function and form.119 The TMJ is essential to the functions of mastication, speech, airway support and deglutition.
Figure 5.
Intraoperative view of TMJ prothesis.
TMJ reconstruction is indicated as management of the following conditions:119
Inflammatory arthritis involving the TMJ not responsive to other modalities of treatment.
Fibrosis/ankyloses not responsive to other modalities of treatment.
Failed tissue grafts or alloplastic joint reconstruction.
Loss of vertical mandibular height and/or occlusal relationship attributable to bony resorption, trauma, developmental abnormalities or pathologic lesions.
Reflections and conclusions
We have a wide range of tools to treat patients with TMD. However, there are still too many failures with the evolution of more complex patients. Perhaps one of the reasons for these failures is a lack of awareness on the part of patients and the professionals themselves of all the therapeutic possibilities currently available. Following this assumption, we must consider that patient access to the therapies is not being allowed; thus, many patients could be underevaluated and undertreated.
On the other hand, even when patients and professionals know of the treatments available, as well as their effects and their correct application, the clinical reality suggests that, in the clear majority of cases, these treatments were being applied in a very unstructured and independent way. Along these lines, true units specialized in the approach to these patients would be ideal. To date, however, the clinical research on multidisciplinary interventions for patients with TMJ is limited, which makes it difficult for them to be translated to clinical practice, although there have been hopeful results.120 In the few cases in which these specialized units exist, the treatments are applied independently in time; that is, each professional applies their own techniques, often without considering the other treatment professionals, and also without performing the treatment simultaneously.
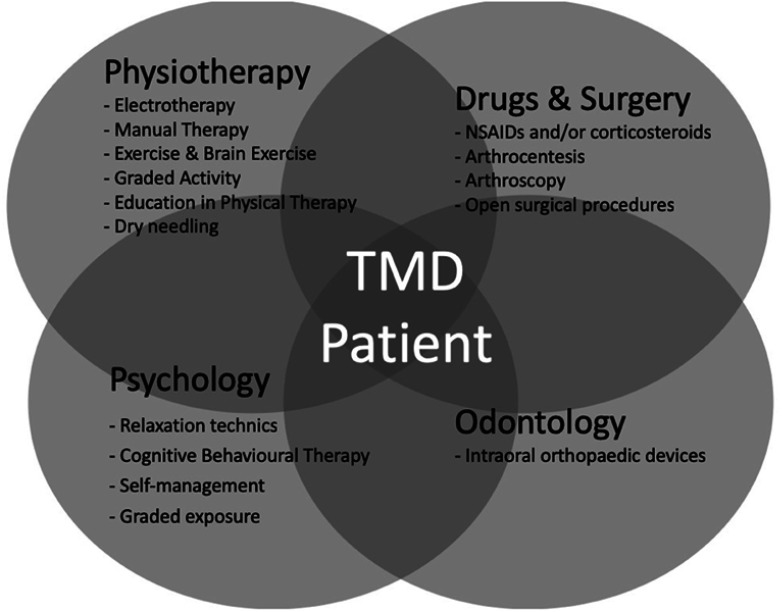
Meanwhile, the multimodal and multidisciplinary approach refers to the simultaneous and coordinated application of these approaches, which has been shown to be more effective than their use separately in other patients with musculoskeletal disorders.121–124 To achieve a multidisciplinary approach, 2 aspects are necessary: First, the lack of literature means further pragmatic clinical trials are required in which the benefits of multimodal management of these patients can be shown, as has already been done for other patients with chronic disorders (references). Only then will it be possible to address the second aspect, which is to develop clinics in which multiple professions are involved in a coordinated and effective way, considering together the various approaches as fundamental to improving the outcomes of these patients (Figure 6).
Figure 6.
Multidisciplinary approach for TMD. Patient-centered care.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Fillingim RB, Ohrbach R, Greenspan JD, et al. Potential psychosocial risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain. 2011;12(11 Suppl):T46–T60. doi: 10.1016/j.jpain.2011.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galli U, Ettlin DA, Palla S, Ehlert U, Gaab J. Do illness perceptions predict pain-related disability and mood in chronic orofacial pain patients? A 6-month follow-up study. Eur J Pain. 2010;14(5):550–558. doi: 10.1016/j.ejpain.2009.08.011 [DOI] [PubMed] [Google Scholar]
- 3.Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9(6):613–633. doi: 10.1016/j.ejpain.2005.01.012 [DOI] [PubMed] [Google Scholar]
- 4.van Selms MK, Muzalev K, Visscher CM, Koutris M, Bulut M, Lobbezoo F. Are pain-related temporomandibular disorders the product of an interaction between psychological factors and self-reported Bruxism? J Oral Facial Pain Headache. 2017;31(4):331–338. doi: 10.11607/ofph.1909 [DOI] [PubMed] [Google Scholar]
- 5.Manfredini D, Landi N, Bandettini Di Poggio A, Dell’Osso L, Bosco M. A critical review on the importance of psychological factors in temporomandibular disorders. Minerva Stomatol. 2003;52(6):321–326, 327–330. [PubMed] [Google Scholar]
- 6.Auvenshine RC. Temporomandibular disorders: associated features. Dent Clin North Am. 2007;51(1):105–27, vi. doi: 10.1016/j.cden.2006.10.005 [DOI] [PubMed] [Google Scholar]
- 7.Alrashdan M, Alkhader M. Psychological factors in oral mucosal and orofacial pain conditions. Eur J Dent. 2017;11(4):548. doi: 10.4103/ejd.ejd_11_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maísa Soares G, Rizzatti-Barbosa CM. Chronicity factors of temporomandibular disorders: a critical review of the literature. Braz Oral Res. 2015;29(1):1–6. doi: 10.1590/1807-3107BOR-2015.vol29.0018 [DOI] [PubMed] [Google Scholar]
- 9.Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res. 2018;11:571–587. doi: 10.2147/JPR.S127950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson CR. Psychological considerations for chronic orofacial pain. Oral Maxillofac Surg Clin North Am. 2008;20(2):185–95, vi. doi: 10.1016/j.coms.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 11.Scrivani SJ, Khawaja SN, Bavia PF. Nonsurgical management of pediatric temporomandibular joint dysfunction. Oral Maxillofac Surg Clin North Am. 2018;30(1):35–45. doi: 10.1016/j.coms.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y, Montoya L, Ebrahim S, et al. Hypnosis/relaxation therapy for temporomandibular disorders: a systematic review and meta-analysis of randomized controlled trials. J Oral Facial Pain Headache. 2015;29(2):115–125. doi: 10.11607/ofph.1330 [DOI] [PubMed] [Google Scholar]
- 13.Dworkin SF. Behavioral and educational modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83(1):128–133. [DOI] [PubMed] [Google Scholar]
- 14.Orlando B, Manfredini D, Salvetti G, Bosco M. Evaluation of the effectiveness of biobehavioral therapy in the treatment of temporomandibular disorders: a literature review. Behav Med. 2007;33(3):101–118. doi: 10.3200/BMED.33.3.101-118 [DOI] [PubMed] [Google Scholar]
- 15.Gardea MA, Gatchel RJ, Mishra KD. Long-term efficacy of biobehavioral treatment of temporomandibular disorders. J Behav Med. 2001;24(4):341–359. [DOI] [PubMed] [Google Scholar]
- 16.Crider A, Glaros AG, Gevirtz RN. Efficacy of biofeedback-based treatments for temporomandibular disorders. Appl Psychophysiol Biofeedback. 2005;30(4):333–345. doi: 10.1007/s10484-005-8420-5 [DOI] [PubMed] [Google Scholar]
- 17.Kröner-Herwig B. Chronic pain syndromes and their treatment by psychological interventions. Curr Opin Psychiatry. 2009;22(2):200–204. doi: 10.1097/YCO.0b013e3283252d5a [DOI] [PubMed] [Google Scholar]
- 18.Randhawa K, Bohay R, Côté P, et al. The effectiveness of noninvasive interventions for temporomandibular disorders: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) collaboration. Clin J Pain. 2016;32(3):260–278. doi: 10.1097/AJP.0000000000000247 [DOI] [PubMed] [Google Scholar]
- 19.Nijs J, Malfliet A, Ickmans K, Baert I, Meeus M. Treatment of central sensitization in patients with “unexplained” chronic pain: an update. Expert Opin Pharmacother. 2014;15(12):1671–1683. doi: 10.1517/14656566.2014.925446 [DOI] [PubMed] [Google Scholar]
- 20.Greene CS. Managing the care of patients with temporomandibular disorders: a new guideline for care. J Am Dent Assoc. 2010;141(9):1086–1088. doi: 10.14219/jada.archive.2010.0337 [DOI] [PubMed] [Google Scholar]
- 21.Story WP, Durham J, Al-Baghdadi M, Steele J, Araujo-Soares V. Self-management in temporomandibular disorders: a systematic review of behavioural components. J Oral Rehabil. 2016;43(10):759–770. doi: 10.1111/joor.12422 [DOI] [PubMed] [Google Scholar]
- 22.Kotiranta U, Suvinen T, Forssell H. Tailored treatments in temporomandibular disorders: where are we now? A systematic qualitative literature review. J Oral Facial Pain Headache. 2014;28(1):28–37. doi: 10.11607/jop.1121 [DOI] [PubMed] [Google Scholar]
- 23.Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2016;32(5):332–355. doi: 10.1080/09593985.2016.1194646 [DOI] [PubMed] [Google Scholar]
- 24.Decety J. The neurophysiological basis of motor imagery. Behav Brain Res. 1996;77(1–2):45–52. [DOI] [PubMed] [Google Scholar]
- 25.Dickstein R, Deutsch JE. Motor imagery in physical therapist practice. Phys Ther. 2007;87(7):942–953. doi: 10.2522/ptj.20060331 [DOI] [PubMed] [Google Scholar]
- 26.Rizzolatti G, Sinigaglia C. The functional role of the parieto-frontal mirror circuit: interpretations and misinterpretations. Nat Rev Neurosci. 2010;11(4):264–274. doi: 10.1038/nrn2805 [DOI] [PubMed] [Google Scholar]
- 27.Navarro-Fernández G, de-la-Puente-Ranea L, Gandía-González M, Gil-Martínez A. Endogenous neurostimulation and physiotherapy in cluster headache: a clinical case. Brain Sci. 2019;9(3):60. doi: 10.3390/brainsci9030060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Piekartz H, Wallwork SB, Mohr G, Butler DS, Moseley GL. People with chronic facial pain perform worse than controls at a facial emotion recognition task, but it is not all about the emotion. J Oral Rehabil. 2015;42(4):243–250. doi: 10.1111/joor.12249 [DOI] [PubMed] [Google Scholar]
- 29.Uritani D, Nishida T, Sakaguchi N, Kawakami T, Jones LE, Kirita T. Difference in response to a motor imagery task: a comparison between individuals with and without painful temporomandibular disorders. Pain Res Manag. 2018;2018:6810412. doi: 10.1155/2018/6810412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrison AL, Thorp JN, Ritzline PD. A proposed diagnostic classification of patients with temporomandibular disorders: implications for physical therapists. J Orthop Sports Phys Ther. 2014;44(3):182–197. doi: 10.2519/jospt.2014.4847 [DOI] [PubMed] [Google Scholar]
- 31.Isong U, Gansky SA, Plesh O. Temporomandibular joint and muscle disorder-type pain in U.S. adults: the national health interview survey. J Orofac Pain. 2008;22(4):317–322. [PMC free article] [PubMed] [Google Scholar]
- 32.World Confederation for Physical Therapy.What is physical therapy | world confederation for physical therapy. Available from: https://www.wcpt.org/what-is-physical-therapy. Accessed March18, 2018.
- 33.Paço M, Peleteiro B, Duarte J, Pinho T. The effectiveness of physiotherapy in the management of temporomandibular disorders: a systematic review and meta-analysis. J Oral Facial Pain Headache. 2016;30(3):210–220. doi: 10.11607/ofph.1661 [DOI] [PubMed] [Google Scholar]
- 34.Dickerson SM, Weaver JM, Boyson AN, et al. The effectiveness of exercise therapy for temporomandibular dysfunction: a systematic review and meta-analysis. Clin Rehabil. 2017;31(8):1039–1048. doi: 10.1177/0269215516672275 [DOI] [PubMed] [Google Scholar]
- 35.Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: systematic review and meta-analysis. Phys Ther. 2016;96(1):9–25. doi: 10.2522/ptj.20140548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McNeely ML, Armijo Olivo S, Magee DJ. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86(5):710–725. [PubMed] [Google Scholar]
- 37.List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010;37(6):430–451. doi: 10.1111/j.1365-2842.2010.02089.x [DOI] [PubMed] [Google Scholar]
- 38.Sakurai Y, Yamaguchi M, Abiko Y. Inhibitory effect of low-level laser irradiation on LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur J Oral Sci. 2000;108(1):29–34. [DOI] [PubMed] [Google Scholar]
- 39.Rushton A, Beeton K, Ronel D, et al. International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) INC.
- 40.Calixtre LB, Moreira RFC, Franchini GH, Alburquerque-Sendín F, Oliveira AB. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: a systematic review of randomised controlled trials. J Oral Rehabil. 2015;42(11):847–861. doi: 10.1111/joor.12321 [DOI] [PubMed] [Google Scholar]
- 41.Vigotsky AD, Bruhns RP. The role of descending modulation in manual therapy and its analgesic implications: a narrative review. Pain Res Treat. 2015;2015:1–11. doi: 10.1155/2015/292805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bishop MD, Torres-Cueco R, Gay CW, Lluch-Girbés E, Beneciuk JM, Bialosky JE. What effect can manual therapy have on a patient’s pain experience? Pain Manag. 2015;5(6):455–464. doi: 10.2217/pmt.15.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Takai Y, Yamamoto-Mitani N, Abe Y, Suzuki M. Literature review of pain management for people with chronic pain. Japan J Nurs Sci. 2015;12(3):167–183. doi: 10.1111/jjns.12065 [DOI] [PubMed] [Google Scholar]
- 44.Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of cochrane reviews In: Geneen LJ, editor. Cochrane Database of Systematic Reviews. Vol. 4 Chichester, UK: John Wiley & Sons, Ltd; 2017: CD011279. doi: 10.1002/14651858.CD011279.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O’Riordan C, Clifford A, Van De Ven P, Nelson J. Chronic neck pain and exercise interventions: frequency, intensity, time, and type principle. Arch Phys Med Rehabil. 2014;95(4):770–783. doi: 10.1016/j.apmr.2013.11.015 [DOI] [PubMed] [Google Scholar]
- 46.Bartsch T, Goadsby PJ. Increased responses in trigeminocervical nociceptive neurons to cervical input after stimulation of the dura mater. Brain. 2003;126(8):1801–1813. doi: 10.1093/brain/awg190 [DOI] [PubMed] [Google Scholar]
- 47.Zafar H, Nordh E, Eriksson PO. Temporal coordination between mandibular and head-neck movements during jaw opening-closing tasks in man. Arch Oral Biol. 2000;45(8):675–682. doi: 10.1016/s0003-9969(00)00032-7 [DOI] [PubMed] [Google Scholar]
- 48.Eriksson PO, Zafar H, Nordh E. Concomitant mandibular and head-neck movements during jaw opening-closing in man. J Oral Rehabil. 1998;25(11):859–870. [DOI] [PubMed] [Google Scholar]
- 49.Craane B, Dijkstra PU, Stappaerts K, De Laat A. One-year evaluation of the effect of physical therapy for masticatory muscle pain: a randomized controlled trial. Eur J Pain. 2012;16(5):737–747. doi: 10.1002/j.1532-2149.2011.00038.x [DOI] [PubMed] [Google Scholar]
- 50.Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R. The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. J Orofac Pain. 2004;18(2):114–125. [PubMed] [Google Scholar]
- 51.Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012;143(1):47–53. doi: 10.14219/jada.archive.2012.0018 [DOI] [PubMed] [Google Scholar]
- 52.Wright EF, Domenech MA, Fischer JR. Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000;131(2):202–210. doi: 10.14219/jada.archive.2000.0148 [DOI] [PubMed] [Google Scholar]
- 53.Mahmoudzadeh A, Rezaeian Z, Karimi A, Dommerholt J. The effect of dry needling on the radiating pain in subjects with discogenic low-back pain: a randomized control trial. J Res Med Sci. 2016;21(1):86. doi: 10.4103/1735-1995.192502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fernández-Carnero J, La Touche R, Ortega-Santiago R, et al. Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. J Orofac Pain. 2010;24(1):106–112. [PubMed] [Google Scholar]
- 55.González-Iglesias J, Cleland JA, Neto F, Hall T, Fernández-de-las-Peñas C. Mobilization with movement, thoracic spine manipulation, and dry needling for the management of temporomandibular disorder: a prospective case series. Physiother Theory Pract. 2013;29(8):586–595. doi: 10.3109/09593985.2013.783895 [DOI] [PubMed] [Google Scholar]
- 56.Gonzalez-Perez L-M, Infante-Cossio P, Granados-Nunez M, F-J U-L, Lopez-Martos R, Ruiz-Canela-Mendez P. Deep dry needling of trigger points located in the lateral pterygoid muscle: efficacy and safety of treatment for management of myofascial pain and temporomandibular dysfunction. Med Oral Patol Oral Cir Bucal. 2015;20(3):e326–e333. doi: 10.4317/medoral.20384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136(5):374. doi: 10.7326/0003-4819-136-5-200203050-00010 [DOI] [PubMed] [Google Scholar]
- 58.Jung A, Shin B-C, Lee MS, Sim H, Ernst E. Acupuncture for treating temporomandibular joint disorders: a systematic review and meta-analysis of randomized, sham-controlled trials. J Dent. 2011;39(5):341–350. doi: 10.1016/j.jdent.2011.02.006 [DOI] [PubMed] [Google Scholar]
- 59.Wu J-Y, Zhang C, Xu Y-P, et al. Acupuncture therapy in the management of the clinical outcomes for temporomandibular disorders. Medicine (Baltimore). 2017;96(9):e6064. doi: 10.1097/MD.0000000000006064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goddard G, Karibe H, McNeill C, Villafuerte E. Acupuncture and sham acupuncture reduce muscle pain in myofascial pain patients. J Orofac Pain. 2002;16(1):71–76. [PubMed] [Google Scholar]
- 61.Dıraçoğlu D, Vural M, Karan A, Aksoy C. Effectiveness of dry needling for the treatment of temporomandibular myofascial pain: a double-blind, randomized, placebo controlled study. J Back Musculoskelet Rehabil. 2012;25(4):285–290. doi: 10.3233/BMR-2012-0338 [DOI] [PubMed] [Google Scholar]
- 62.Cheng RSS, Pomeranz B. Electroacupuncture analgesia could be mediated by at least two pain-relieving mechanisms; endorphin and non-endorphin systems. Life Sci. 1979;25(23):1957–1962. doi: 10.1016/0024-3205(79)90598-8 [DOI] [PubMed] [Google Scholar]
- 63.H-Y TSAI, J-G LIN, INOKI R. Further evidence for possible analgesic mechanism of electroacupuncture: effects on neuropeptides and serotonergic neurons in rat spinal cord. Jpn J Pharmacol. 1989;49(2):181–185. doi: 10.1254/jjp.49.181 [DOI] [PubMed] [Google Scholar]
- 64.Han Z, Jiang Y-H, Wan Y, Wang Y, Chang J-K, Han J-S. Endomorphin-1 mediates 2 Hz but not 100 Hz electroacupuncture analgesia in the rat. Neurosci Lett. 1999;274(2):75–78. doi: 10.1016/S0304-3940(99)00670-9 [DOI] [PubMed] [Google Scholar]
- 65.Mendelson G. The possible role of enkephalin in the mechanism of acupuncture analgesia in man. Med Hypotheses. 1977;3(4):144–145. doi: 10.1016/0306-9877(77)90062-7 [DOI] [PubMed] [Google Scholar]
- 66.Pomeranz B, Chiu D. Naloxone blockade of acupuncture analgesia: endorphin implicated. Life Sci. 1976;19(11):1757–1762. doi: 10.1016/0024-3205(76)90084-9 [DOI] [PubMed] [Google Scholar]
- 67.Pficer JK, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: meta-analysis of short and long term effects. milgrom PM, ed. PLoS One. 2017;12(2):e0171296. doi: 10.1371/journal.pone.0171296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.de Leeuw R, Klasser GD; American Academy of Orofacial Pain. Orofacial Pain : Guidelines for Assessment, Diagnosis, and Management. Fifth. (Leeuw D, Reny, Klasser, D. G, eds.).Quintessence Publishing Co, Inc. ; 2018. [Google Scholar]
- 69.Zhang C, Wu J-Y, Deng D-L, et al. Efficacy of splint therapy for the management of temporomandibular disorders: a meta-analysis. Oncotarget. 2016;7(51):84043–84053. doi: 10.18632/oncotarget.13059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Costa YM, Porporatti AL, Stuginski-Barbosa J, Bonjardim LR, Conti PCR. Additional effect of occlusal splints on the improvement of psychological aspects in temporomandibular disorder subjects: a randomized controlled trial. Arch Oral Biol. 2015;60(5):738–744. doi: 10.1016/j.archoralbio.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 71.Alajbeg IZ, Gikić M, Valentić-Peruzović M. Changes in pain intensity and oral health-related quality of life in patients with temporomandibular disorders during stabilization splint therapy–a pilot study. Acta Clin Croat. 2014;53(1):7–16. [PubMed] [Google Scholar]
- 72.Tvrdy P, Heinz P, Zapletalova J, Pink R, Michl P. Effect of combination therapy of arthrocentesis and occlusal splint on nonreducing temporomandibular joint disk displacement. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015;159(4):677–680. doi: 10.5507/bp.2014.044 [DOI] [PubMed] [Google Scholar]
- 73.Magdaleno F, Ginestal E. Side effects of stabilization occlusal splints: a report of three cases and literature review. CRANIO®. 2010;28(2):128–135. doi: 10.1179/crn.2010.018 [DOI] [PubMed] [Google Scholar]
- 74.Hasegawa Y, Kakimoto N, Tomita S, et al. Movement of the mandibular condyle and articular disc on placement of an occlusal splint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(5):640–647. doi: 10.1016/j.tripleo.2011.06.013 [DOI] [PubMed] [Google Scholar]
- 75.Greene CS, Obrez A. Treating temporomandibular disorders with permanent mandibular repositioning: is it medically necessary? Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(5):489–498. doi: 10.1016/j.oooo.2015.01.020 [DOI] [PubMed] [Google Scholar]
- 76.Cruz-Reyes RA, Martínez-Aragón I, Guerrero-Arias RE, García-Zura DA, González-Sánchez LE. Influence of occlusal stabilization splints and soft occlusal splints on the electromyographic pattern, in basal state and at the end of six weeks treatment in patients with bruxism. Acta Odontol Latinoam. 2011;24(1):66–74. [PubMed] [Google Scholar]
- 77.Yang J-W, Huang Y-C, Wu S-L, Ko S-Y, Tsai -C-C. Clinical efficacy of a centric relation occlusal splint and intra-articular liquid phase concentrated growth factor injection for the treatment of temporomandibular disorders. Medicine (Baltimore). 2017;96(11):e6302. doi: 10.1097/MD.0000000000006302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Michelotti A. An interview with ambrosina michelotti. Dental Press J Orthod. 2018;23(2):22–29. doi: 10.1590/2177-6709.23.2.022-029.int [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.van Grootel RJ, Buchner R, Wismeijer D, van der Glas HW. Towards an optimal therapy strategy for myogenous TMD, physiotherapy compared with occlusal splint therapy in an RCT with therapy-and-patient-specific treatment durations. BMC Musculoskelet Disord. 2017;18(1):76. doi: 10.1186/s12891-017-1404-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lobbezoo F, Ahlberg J, Raphael KG, et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018;45(11):837–844. doi: 10.1111/joor.12663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Macedo CR, Silva AB, Machado MAC, Saconato H, Prado GF. Occlusal splints for treating sleep bruxism (tooth grinding). Cochrane Database Syst Rev. 2007;4:CD005514. doi: 10.1002/14651858.CD005514.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jokubauskas L, Baltrušaitytė A. Relationship between obstructive sleep apnoea syndrome and sleep bruxism: a systematic review. J Oral Rehabil. 2017;44(2):144–153. doi: 10.1111/joor.12468 [DOI] [PubMed] [Google Scholar]
- 83.Saito M, Yamaguchi T, Mikami S, et al. Weak association between sleep bruxism and obstructive sleep apnea. A sleep laboratory study. Sleep Breath. 2016;20(2):703–709. doi: 10.1007/s11325-015-1284-x [DOI] [PubMed] [Google Scholar]
- 84.Winck M, Drummond M, Viana P, Pinho JC, Winck JC. Sleep bruxism associated with obstructive sleep apnoea syndrome – a pilot study using a new portable device. Rev Port Pneumol. 2017;23(1):22–26. doi: 10.1016/j.rppnen.2016.07.001 [DOI] [PubMed] [Google Scholar]
- 85.Mayer P, Heinzer R, Lavigne G. Sleep bruxism in respiratory medicine practice. Chest. 2016;149(1):262–271. doi: 10.1378/chest.15-0822 [DOI] [PubMed] [Google Scholar]
- 86.Hegab AF, Youssef AH, Al Hameed HIA, Karam KS. MRI-based determination of occlusal splint thickness for temporomandibular joint disk derangement: a randomized controlled clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(1):74–87. doi: 10.1016/j.oooo.2017.09.017 [DOI] [PubMed] [Google Scholar]
- 87.Pita MS, Ribeiro AB, Garcia AR, Pedrazzi V, Zuim PRJ. Effect of occlusal splint thickness on electrical masticatory muscle activity during rest and clenching. Braz Oral Res. 2011;25(6):506–511. [DOI] [PubMed] [Google Scholar]
- 88.Akbulut N, Altan A, Akbulut S, Atakan C. Evaluation of the 3 mm thickness splint therapy on Temporomandibular Joint Disorders (TMDs). Pain Res Manag. 2018;2018:1–7. doi: 10.1155/2018/3756587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dylina TJ. A common-sense approach to splint therapy. J Prosthet Dent. 2001;86(5):539–545. doi: 10.1067/mpr.2001.118878 [DOI] [PubMed] [Google Scholar]
- 90.Seifeldin SA, Elhayes KA. Soft versus hard occlusal splint therapy in the management of temporomandibular disorders (TMDs). Saudi Dent J. 2015;27(4):208–214. doi: 10.1016/j.sdentj.2014.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen H-M, Liu M-Q, Yap AU-J, Fu K-Y. Physiological effects of anterior repositioning splint on temporomandibular joint disc displacement: a quantitative analysis. J Oral Rehabil. 2017;44(9):664–672. doi: 10.1111/joor.12532 [DOI] [PubMed] [Google Scholar]
- 92.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301–355. [PubMed] [Google Scholar]
- 93.Manfredini D, Lombardo L, Siciliani G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? J Oral Rehabil. 2017;44(11):908–923. doi: 10.1111/joor.12531 [DOI] [PubMed] [Google Scholar]
- 94.Michelotti A, Iodice G. The role of orthodontics in temporomandibular disorders. J Oral Rehabil. 2010;37(6):411–429. doi: 10.1111/j.1365-2842.2010.02087.x [DOI] [PubMed] [Google Scholar]
- 95.Manfredini D, Perinetti G, Stellini E, Di Leonardo B, Guarda-Nardini L. Prevalence of static and dynamic dental malocclusion features in subgroups of temporomandibular disorder patients: implications for the epidemiology of the TMD-occlusion association. Quintessence Int. 2015;46(4):341–349. doi: 10.3290/j.qi.a32986 [DOI] [PubMed] [Google Scholar]
- 96.Manfredini D. Occlusal equilibration for the management of temporomandibular disorders. Oral Maxillofac Surg Clin North Am. 2018;30(3):257–264. doi: 10.1016/j.coms.2018.04.002 [DOI] [PubMed] [Google Scholar]
- 97.de Kanter RJAM, Battistuzzi PGFCM, Truin G-J. Temporomandibular disorders: “occlusion” matters! Pain Res Manag. 2018;2018:1–13. doi: 10.1155/2018/8746858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Michelotti A, Farella M, Gallo LM, Veltri A, Palla S, Martina R. Effect of occlusal interference on habitual activity of human masseter. J Dent Res. 2005;84(7):644–648. doi: 10.1177/154405910508400712 [DOI] [PubMed] [Google Scholar]
- 99.Michelotti A, Farella M, Steenks MH, Gallo LM, Palla S. No effect of experimental occlusal interferences on pressure pain thresholds of the masseter and temporalis muscles in healthy women. Eur J Oral Sci. 2006;114(2):167–170. doi: 10.1111/j.1600-0722.2006.00298.x [DOI] [PubMed] [Google Scholar]
- 100.Cioffi I, Farella M, Festa P, Martina R, Palla S, Michelotti A. Short-term sensorimotor effects of experimental occlusal interferences on the wake-time masseter muscle activity of females with masticatory muscle pain. J Oral Facial Pain Headache. 2015;29(4):331–339. doi: 10.11607/ofph.1478 [DOI] [PubMed] [Google Scholar]
- 101.Michelotti A, Cioffi I, Landino D, Galeone C, Farella M. Effects of experimental occlusal interferences in individuals reporting different levels of wake-time parafunctions. J Orofac Pain. 2012;26(3):168–175. [PubMed] [Google Scholar]
- 102.Ohrbach R, Bair E, Fillingim RB, et al. Clinical orofacial characteristics associated with risk of first-onset TMD: the OPPERA prospective cohort study. J Pain. 2013;14(12 Suppl):T33–T50. doi: 10.1016/j.jpain.2013.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. J Oral Rehabil. 2004;31(4):287–292. doi: 10.1046/j.1365-2842.2003.01257.x [DOI] [PubMed] [Google Scholar]
- 104.Shroff B. Malocclusion as a cause for temporomandibular disorders and orthodontics as a treatment. Oral Maxillofac Surg Clin North Am. 2018;30(3):299–302. doi: 10.1016/j.coms.2018.04.006 [DOI] [PubMed] [Google Scholar]
- 105.Hernandez de Felipe M, de la Hoz Aizpurúa J, Gutierrez JS. Oclusión, ortodoncia y disfunción craneomandibular. Rev Cons Odontoestomatol España. 2013;18(3):167–171. [Google Scholar]
- 106.Leite RA, Rodrigues JF, Sakima MT, Sakima T. Relationship between temporomandibular disorders and orthodontic treatment: a literature review. Dental Press J Orthod. 2013;18(1):150–157. doi: 10.1590/S2176-94512013000100027 [DOI] [PubMed] [Google Scholar]
- 107.Ohrbach R, Fillingim RB, Mulkey F, et al. Clinical findings and pain symptoms as potential risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain. 2011;12(11):T27–T45. doi: 10.1016/j.jpain.2011.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Dolwick MF, Dimitroulis G. Is there a role for temporomandibular joint surgery? Br J Oral Maxillofac Surg. 1994;32(5):307–313. [DOI] [PubMed] [Google Scholar]
- 109.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49(11):1163–1167. discussion 1168–70. doi: 10.1016/0278-2391(91)90409-f [DOI] [PubMed] [Google Scholar]
- 110.Nitzan DW, Samson B, Better H. Long-term outcome of arthrocentesis for sudden-onset, persistent, severe closed lock of the temporomandibular joint. J Oral Maxillofac Surg. 1997;55(2):151–157. discussion 157–8. doi: 10.1016/s0278-2391(97)90233-0 [DOI] [PubMed] [Google Scholar]
- 111.Patel P, Idrees F, Newaskar V, Agrawal D. Sodium hyaluronate: an effective adjunct in temporomandibular joint arthrocentesis. Oral Maxillofac Surg. 2016;20(4):405–410. doi: 10.1007/s10006-016-0581-2 [DOI] [PubMed] [Google Scholar]
- 112.Sanders B, Buoncristiani R. Diagnostic and surgical arthroscopy of the temporomandibular joint: clinical experience with 137 procedures over a 2-year period. J Craniomandib Disord. 1987;1(3):202–213. [PubMed] [Google Scholar]
- 113.Greene MW, Hackney FL, Van Sickels JE. Arthroscopy of the temporomandibular joint: an anatomic perspective. J Oral Maxillofac Surg. 1989;47(4):386–389. doi: 10.1016/0278-2391(89)90341-8 [DOI] [PubMed] [Google Scholar]
- 114.Trumpy IG, Lyberg T. Surgical treatment of internal derangement of the temporomandibular joint: long-term evaluation of three techniques. J Oral Maxillofac Surg. 1995;53(7):740–746. discussion 746–7. doi: 10.1016/0278-2391(95)90321-6 [DOI] [PubMed] [Google Scholar]
- 115.Zhang S, Liu X, Yang X, et al. Temporomandibular joint disc repositioning using bone anchors: an immediate post surgical evaluation by magnetic resonance imaging. BMC Musculoskelet Disord. 2010;11(1):262. doi: 10.1186/1471-2474-11-262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mehra P, Wolford LM. The mitek mini anchor for TMJ disc repositioning: surgical technique and results. Int J Oral Maxillofac Surg. 2001;30(6):497–503. doi: 10.1054/ijom.2001.0163 [DOI] [PubMed] [Google Scholar]
- 117.Holmlund AB, Gynther G, Axelsson S. Discectomy in treatment of internal derangement of the temporomandibular joint. Follow-up at 1, 3, and 5 years. Oral Surg Oral Med Oral Pathol. 1993;76(3):266–271. doi: 10.1016/0030-4220(93)90250-8 [DOI] [PubMed] [Google Scholar]
- 118.MacIntosh RB. The use of autogenous tissues for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58(1):63–69. doi: 10.1016/s0278-2391(00)80019-1 [DOI] [PubMed] [Google Scholar]
- 119.Mercuri LG. The use of alloplastic prostheses for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58(1):70–75. doi: 10.1016/s0278-2391(00)80020-8 [DOI] [PubMed] [Google Scholar]
- 120.Ahmed N, Poate T, Nacher-Garcia C, et al. Temporomandibular joint multidisciplinary team clinic. Br J Oral Maxillofac Surg. 2014;52(9):827–830. doi: 10.1016/j.bjoms.2014.07.254 [DOI] [PubMed] [Google Scholar]
- 121.Karjalainen KA, Malmivaara A, van Tulder MW, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev. 2003;3:CD002194. doi: 10.1002/14651858.CD002194 [DOI] [PubMed] [Google Scholar]
- 122.Karjalainen KA, Malmivaara A, van Tulder MW, et al. Multidisciplinary rehabilitation for fibromyalgia and musculoskeletal pain in working age adults. Cochrane Database Syst Rev. 1999;2:CD001984. doi: 10.1002/14651858.CD001984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Khan F, Ng L, Gonzalez S, Hale T, Turner-Stokes L. Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database Syst Rev. 2008;2:CD004957. doi: 10.1002/14651858.CD004957.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ. 2015;350(feb185):h444. doi: 10.1136/bmj.h444 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- World Confederation for Physical Therapy.What is physical therapy | world confederation for physical therapy. Available from: https://www.wcpt.org/what-is-physical-therapy. Accessed March18, 2018.