Abstract
This article reviews evaluation studies of interventions aimed at preventing and reducing incidents of suicide and self-harm among incarcerated individuals. Study design, sample characteristics, intervention procedures, study measures, and relevant results of each study are reviewed. The outcomes of interest include severity and frequency of self-harm episodes and suicidal ideation, scores on adaptive coping methods, scoring on the Beck Hopelessness scale and risk scores. The six evaluated studies are peer-reviewed, published between 1990 and 2015, and took place in the United States, the United Kingdom, and Pakistan. Treatment modalities widely vary across studies and include cognitive behavioral therapy, dialectical behavioral therapy, peer programming, staff intervention training, and uniquely-designed courses that incorporate various aspects from other treatment modalities. Due to the nature of the studies, only one multi-randomized controlled trial was identified. All identified studies had a pre- and post-treatment design either lacking a comparison group or containing 1–2 comparison groups and conduct follow-up of varying times. While Cognitive Behavioral Therapy (CBT) interventions and uniquely-tailored intervention programs suggest promising results, the general absence of comparison groups, the shortage of relevant evaluation studies and the inconsistency of behavioral outcome measurements compromise the capacity of this review. Further, definitional variances, particularly for self-injury (self-harm, non-suicidal self-injury [NSSI], deliberate self-harm, suicidal behavior, etc.) affect the ability to synthesize study results. This article aims to synthesize the literature results to identify the most effective interventions that would benefit from additional research.
Keywords: Public health, Psychiatry, Psychology, Sociology, Self-injury, Intervention, Self-harm, Suicidal behavior, NSSI, Prisons
1. Introduction
Within correctional facilities, staff and clinicians are tasked with managing self-injury and suicidal behavior among detainees. Research suggests that incarcerated individuals display higher rates of self-harm, estimating that between 7% and 48% of offenders have a history of self-injury in comparison to 4% of adults in the general population (Dixon-Gordon et al., 2012). From 2013 to 2014, suicide rates in prisons rose by 30% with suicide accounting for 7% of prison deaths by 2014 (Noonan, 2016). In comparison, research estimates that the risk of suicide has been estimated to be 5–8% for mental disorders. This increase has prompted the introduction of new prison suicide prevention programs and self-harm interventions that have elicited varied results. Dialectical Behavioral Therapy (DBT), CBT, peer training programming and staff training are among the most widely applied interventions for the treatment of self-harm in correctional facilities. The heightened rate of suicidal behavior and self-harm within prisons and jails has become a major public health issue, as well as a serious legal issue for the facilities. The government is responsible for the safety of those in its custody, and correctional officers have a duty to uphold this and the correctional institutions must consider liability and take reasonable preventative measures. However, there is a lack of guidance and limited research on this topic, particularly in the United States where the tremendous prison population size gives the problem a particularly high level of significance.
1.1. Self-harm and incarceration
The evaluated literature defines self-harm as “any act where a prisoner deliberately harms themselves irrespective of the method, intent or severity of any injury” (Horton et al., 2014). For the purposes of this review, this excludes self-harming substance use. It should be noted that the majority of research does not differentiate between self-injury and “suicidal behavior”.
Self-harming behavior is a pervasive problem in jails and prisons with research estimates indicating that about 30% of prisoners engage in the behavior (Appelbaum et al., 2011). In comparison, research estimates self-harm rates of 4% in the general population and 21% in the mental health population (Briere and Gil, 1998; Nock and Kessler, 2006). In an uncontrollable and stressful environment, self-harm may be used as a maladaptive coping tool that provides temporary relief from intense and distressing feelings. The lack of alternatives for an emotional outlet in the correctional setting makes self-harm a particularly appealing coping method for individuals experiencing distress. Studies indicate that self-harm is associated with reported feelings of hopelessness and helplessness, excessive guilt, self-punishment, desire to express needs and escape from isolation. Despite being short-term, the immediate gratification that self-injury provides serves as a strong behavioral reinforcement.
Research suggests that incarceration intensifies the risk of self-harm: Thornton (1990) found that his sample of juveniles in custody, one young person in 12 had self-injured during their incarceration. While self-injurious behavior is often non-suicidal, it perpetuates a cycle of maladaptive coping and puts an individual at risk for accidental death, given that it is difficult for individuals to judge the lethality of their self-harm. Demographic can put incarcerated individuals at an even higher risk for engaging in suicidal behavior, particularly young males with low education level and/or prior criminal history. A six-month study showed that 5% of male juveniles (aged 15/18) and 7% of male young offenders (aged 18/21) self-injured, compared to 1.5% of adult males (Muehlenkamp and Gutierrez, 2007,Welfare and Mitchell, 2005). Additional considerations in risk assessment include clinical factors (history of psychiatric problems and family issues), psychosocial factors (poor coping methods, stressful life events, past suicide attempts, receiving a new charge or conviction), and institutional factors (overcrowding, harassment, recent disciplinary action, lack of staff supervision, isolation) (Barker et al., 2014).
Multiple interventions have been implemented and evaluated in an attempt to prevent suicides, including staff training and DBT. A large proportion of suicide prevention interventions focus on training staff to identify suicide risk and provide direct supervision to those deemed susceptible to suicidal tendencies. However, limited staff and detainee reluctance to trust correctional officers has prompted the exploration of new intervention methods.
2. Main text
This paper reviews the results of various interventions constructed to reduce or prevent self-harm and suicidal behavior in prisons and jails. The evaluated components include study design, participant characteristics, intervention procedures, applied measures, and analysis of treatment results. Potentially limiting factors were considered, including definitional variance, different measurements of behavioral outcomes, the inclusion or lack of follow-up procedures and comparison groups.
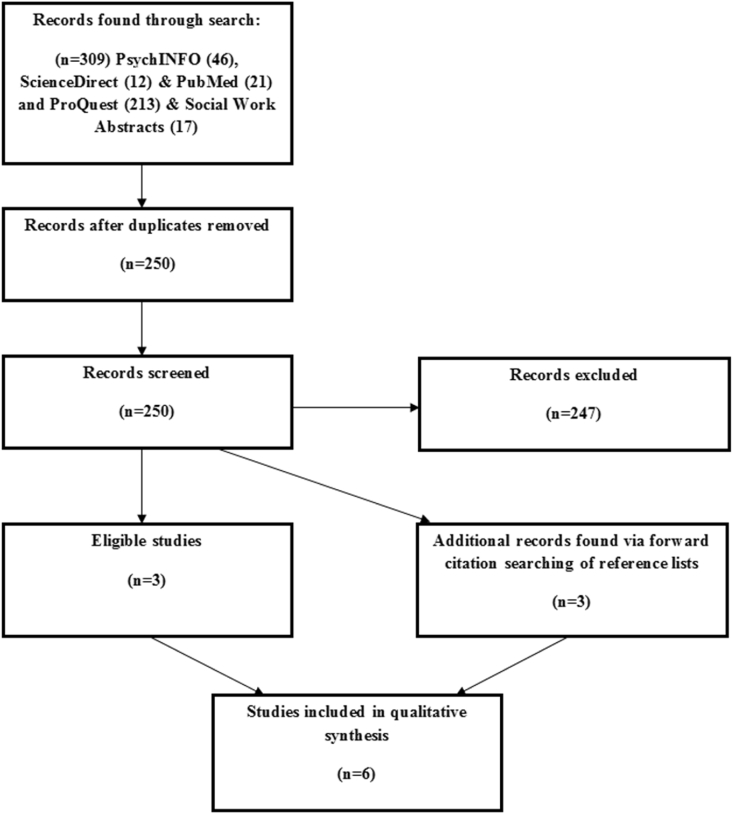
The PRISMA flow diagram (Fig. 1) illustrates the selection and elimination process for record inclusion in this analysis. Relevant studies were searched through five online databases: (a) PsychINFO, (b) ScienceDirect, (c) PubMed, (d) ProQuest, and (e) Social Work Abstracts (Ovid). The searches included keywords: "self-injury" "self-harm" "incarceration" "prison" "jail" "NSSI" "suicidal behavior". The search was restricted to the period between 1990 and 2016; this author did not locate relevant studies conducted prior to 1990. The initial review of the literature revealed 309 records that included the applied search terms- 79 records through PsychINFO, ScienceDirect, and PubMed and 230 records through ProQuest and Social Work Abstracts.
Fig. 1.
PRISMA flow diagram for study selection. PRISMA = Preferred Reporting of Items for Systematic Reviews and Meta-Analyses.
Initially, only articles containing the measurement of non-suicidal self-injury were considered for this systematic review, but after extensive searches for qualifying studies, inclusion criteria were expanded to incorporate studies measuring suicidal behavior and suicidal ideation. Due to the small number of available studies on the topic, the final parameters were: 1) study participants were either prison or jail (i.e. not a maximum security hospital), 2) there were more than 8 participants, 3) the study was conducted after 1990, 4) there was support of the intervention effectiveness rather than a summary, and 5) the article was published in a peer-reviewed journal. Studies were not limited by country or by gender or age of the participant.
After eliminating reviews, duplicates, and irrelevant content, a forward citation searching process was used by reviewing references for each study. Ultimately, 6 studies met inclusion criteria.
2.1. Results
2.1.1. Study characteristics
2.1.1.1. Study design
The designs of the six evaluated studies are displayed in Table 1. All included studies followed a pre-post methodology, and of the six, two of the studies contain a single treatment group with no comparison group (Riaz and Agha, 2012; Welfare and Mitchell, 2005). All of the studies conducted assessments of participants at baseline, post-treatment, and follow-up, with follow-up periods ranging from 30 days to 2 years post-treatment. Three studies implemented a multiple-case study design with one comparison group receiving treatment-as-usual (TAU) and an experimental group receiving the intervention (Rohde et al., 2004; Pratt et al., 2015; Mitchell et al., 2011). Pratt et al. (2015) and Mitchell et al. (2011) conducted randomized control trials with follow-up assessments within one year. Lastly, one study employed a pre-post treatment study design that included two comparison groups (Trupin et al., 2002). One of the included studies administered multiple follow-up assessments (Pratt et al., 2015).
Table 1.
Study design, characteristics of sample, and treatment procedures.
| Authors | Design | Sample characteristics (age & gender) | Intervention Setting | Intervention Procedure | Measures | Results |
|---|---|---|---|---|---|---|
| Cox and Morschauser (1997) | Pre-post with no comparison group, 3 years with 9-year regular follow ups | Gender not specified General inmate population & personnel from all county jails and most Police Department lockups in the 57 counties |
Adult jail facilities- New York, United States | “Local Forensic Suicide Prevention Crisis Service Program”- an 8-hour basic suicide prevention curriculum and procedure guide-lines for jail officer trainers and clinicians, with a 4-hour suicide prevention refresher train-ing and a 14-hour criminal justice system/suicide prevention training for mental health providers |
pre- and post-implementation rates of suicide in jails; survey of 46 jails (conducted by the Bureau of Forensic Services) | Suicides in local jails diminished from 26 in 1984 to 9 in 1996; 78% of the respondents reported improved mental health services following implementation of the program |
| Hall and Gabor (2004) | Pre-post with no comparison group with one-year and two-year follow-up | Gender not specified N = 260; general inmate population n = 242, SAM volunteers n = 18 |
Adult prison facility- Alberta, Canada | SAM volunteers (also incarcerated) undergo are trained on topics including effective and active listening, suicide prevention and intervention, non-verbal communications, the nature of mental illness, and the concept of befriending. Requests could be made by inmates at any time to meet with a SAM volunteer | Contact sheets completed by SAM volunteers that summarize information relating to the contact; in-depth interviews conducted with volunteers; surveys completed by general inmate population; questionnaire completed by correctional officers; interviews conducted with professional staff. | SAM volunteers exceeded target number of contacts by 27% During 5-year period, four completed suicides were recorded; effect of intervention is inconclusive given the low absolute frequency of suicide in this facility “The general inmate population viewed the service as accessible and helpful” |
| Junker et al. (2005) | Pre-post with no comparison group, two 12-week time periods | Gender not specified N = 37; mean age 34.38 |
Federal Bureau of Prisons Medical Referral Center within Federal penal system- United States | Suicidal individuals were placed under constant observation- in the first 12-week interval, prison staff conducted the observation, and in the second 12-week interval, trained inmate observers conducted the observation. Inmate observers participated in 4-hour training sessions provided by a psychologist. | Recorded log entries by observers at 15-minute intervals; inmate medical records; email notification system which tracked suicide watches and watch discontinuation | There was a significant decrease in the number of hours on watch after trained inmate observers were applied, particularly for inmates with a psychotic diagnosis. There was a 52% decrease in the number of individuals on watch after peer-observer program implementation among the personality disorder group. |
| Mitchell et al. (2011) | Pre-post with one comparison group Multi-RCT design with 11-month follow-up |
Gender not specified N = 40 CBT n = 19, TAU n = 21; mean age 15 |
Youth correctional facilities- United Kingdom | CBT group received intervention that emphasized flexibility, accessibility and inclusiveness and motivation (to maximize engagement and retention) on a weekly basis. TAU group received any individualized interventions for emotional or mental health problems routinely offered at that specific trial site | SAVRY assessment; WASI; Youth Self Report (YSR); DCP; SNASA | There were reductions over time in problem severity for self-harm and suicidal ideation (F [1,36] ¼ 7.66, p < 0.01) |
| Pratt et al. (2015) | Pre-post with one comparison group RCT with four-month and six-month follow-up |
N = 62 (all men) CBT + TAU n = 31 TAU alone n = 31 mean age 35.2 |
Adult male prison facility- England | CBT participants received up to 20 1-h sessions, twice weekly during the initial phases of therapy and once-weekly sessions when therapeutic engagement had been established. Intervention included five components: 1) Attention broadening, 2) Cognitive restructuring, 3) Mood management and behavioural activation 4) Problem-solving training, 5) Improving self-esteem and positive schema Participants randomized to the TAU group received the usual care |
number of episodes of suicidal or SIB in the past 6 months (assessed by examination of participants' prison records); Beck Scale for Suicidal Ideation (BSSI); Suicide Probability Scale; Beck Hopelessness, Depression and Anxiety Inventory; Robson Self-Concept Questionnaire; Brief Psychiatric Rating Scale; Standardised Assessment of Personality – Abbreviated Scale | At 6-month assessment the mean number of SIBs for the CBSP group had decreased by almost 50% to 0.58, compared to only 1.48 for the TAU group; CBSP group engaged in fewer SIBs compared with the TAU group; no participants within the CBSP group were found to have increased numbers of SIBs relative to baseline, whereas within the TAU group six participants had increased numbers of SIB. |
| Riaz and Agha (2012) | Pre-post with no comparison group with one-month follow-up | N = 9 (all Pakistani women); mean age 30.9 | Adult female prison- Pakistan | 12 sessions of CBT administered to group of 9 women for four months, in 45–60 min sessions, once per week (12 sessions total). Intervention included psychoeducation, cognitive restructuring, problem-solving, and relaxation procedures. | Deliberate Self-harm inventory and Brief COPE; type and number of episodes reported by incarcerated women | Mean scores of some adaptive coping methods showed improvement post-therapy. Therapy had delayed time of average attempt. The number of DSH episodes was minimal during therapy and did not occur between end of intervention and follow-up. |
| Rohde et al. (2004) | Pre-post with one comparison group | N = 76 (male adolescents) in 2 groups; one group assigned to the Coping Course n = 46, One group assigned to usual care n = 30; mean age 16 Not randomly selected |
Female youth correctional facility- Oregon, United States | Adolescents were randomly assigned to either Coping Course or usual care. Coping Course involved 16 treatment sessions over the course of 8 weeks with a group leader teaching emotion regulation skills. Control group received TAU, which varied but generally included drug/alcohol groups, critical thinking-skills intervention, and sex offender groups. Incentive of $10 was offered | Questionnaires were completed by participants twice over the 8-week period. Questionnaire included LAS-SF (assesses suicide proneness), Coping skills, Self-Esteem Scale, Loneliness Scale, Social Adjustment Scale, and Suicidal Ideation/Attempts. | Comparing pre and post-intervention, there was a statistically significant decrease in LAS total score and LAS death-related scores among those in the intervention group |
| Trupin et al. (2002) | Pre–post with two comparison groups and 90 day follow-up | N = 60 (all adolescent females) in 3 groups; one treatment condition applied in Mental Health Cottage (MHC) n = 22, one treatment condition applied in General Population Cottage (GPCD) n = 23, one TAU condition applied in General Population Comparison Cottage (GPCC) n = 15; mean age 15.2 | Female youth correctional facility- Washington, United States | DBT administered to MHC and GPCD for four weeks, in 60–90 min sessions, once or twice per week. Treatment was delivered in a group format with eight residents per group.Five categories of skills were taught: Core Mindfulness, Interpersonal Effectiveness, Emotion Regulation, Distress Tolerance and Self-Management. Staff was trained in DBT for 80 h prior to study. GPCC received TAU (behavioral modification program) | Initial interviews included DISC, CAFAS, and rating of functional impairment; Daily Behavior logs done by staff Massachusetts Youth Screening Instrument (MAYSI) and Community Risk Assessment Scores (CRA) done at intake and 90-day follow-up Daily Diary Card done by participants recording the frequency of coping skill usage |
No significant risk score change by DBT condition, but overall decrease in risk score across all groups. MHC participants demonstrated significant decrease in serious behavior problems during 10-month period of the study, including a decrease in suicidal acts. *lack of suicidal self-mutilating and para-suicidal behavior primary targets of DBT |
| Welfare and Mitchell (2005) | Pre-post with no comparison and 6-week follow-up | Gender not specified N = 16 (all adolescents) |
Youth correctional facility- United Kingdom | Access program was delivered over 12 sessions, each session involving an hour of classroom work and an hour in the gymnasium.Psychologist and PE Officer delivered the course.Program is designed to increase self-esteem and decrease hopeless and incidents of self-harm. | Beck Hopelessness Scale, Rosenberg Self-Esteem Scale, Social Problem-Solving Inventory, Locus of Control Scale; Personal Officers completed Staff Assessment Checklists | According to participant's self-report data, there was an improvement in the Beck Hopelessness scale and self-esteem.Staff reports indicate a decrease in participant actual and threatened self-injury that was maintained at 6-week follow-up. Records of self-harm incidents show that the outcomes for participants were significantly better than for those in the wait-list group who did not receive the intervention. |
2.1.1.2. Sample characteristics
Among the reviewed studies, the mean sample size was 62, ranging from 9 (Riaz and Agha, 2012) to 76 (Rohde et al., 2004). While the majority of the studies did not specify participant gender, two studies included only females (Trupin et al., 2002; Riaz and Agha, 2012), and two studies included only males (Rohde et al., 2004; Pratt et al., 2015). The age of participants varied, but four studies exclusively studied adolescents (Trupin et al., 2002; Mitchell et al., 2011; Rohde et al., 2004; Welfare and Mitchell, 2005). The remaining studies that specified the age of participants had an average age of 33.9. Studies were conducted in the United States, United Kingdom, and Pakistan -two in the United States (Rohde et al., 2004; Trupin et al., 2002), three in the United Kingdom (Pratt et al., 2015; Welfare and Mitchell, 2005; Mitchell et al., 2011) and one in Pakistan (Riaz and Agha, 2012). All interventions were applied in either jails, prisons or youth correctional facilities.
2.2. Treatment procedures
2.2.1. Cognitive-behavioral therapy
Among the studies included in this review, three implemented a CBT intervention to reduce frequency and severity of self-harm and suicidal behavior (Mitchell et al., 2011; Riaz and Agha, 2012; Pratt et al., 2015). Treatment was delivered in a manualized format in hourly sessions on a weekly basis, continuing for between 12-20 hourly sessions. Topics typically covered identifying triggers, recognizing the consequent thoughts and feelings, identifying thought distortions, changing distorted thinking, adopting new, more rational thoughts and coping skills. The treatments involved a combination of psychoeducation, cognitive restructuring, problem-solving, and relaxation techniques. Pratt et al. (2015) implemented a CBT intervention that is known as Cognitive–Behavioural Suicide Prevention (CBSP) therapy, specifically designed to address suicidal ideation/behavior. The model incorporates three aspects: "(i) information-processing biases, (ii) appraisals and (iii) a suicide schema to be the main components contributing to an individual's experience of suicidality" (Pratt et al., 2015). Pratt's CBSP study is promising - at the 6-month assessment, results indicate a decrease in the mean number of self-injury behaviors of almost 50% for the CBSP treatment group, while the group receiving TAU showed negligible change in the mean number of SIBS. Further, no CBSP participants reported increased rates of SIBs relative to baseline, while six TAU participants reported an increase. At the end-point of treatment, 56% of CBSP participants achieved a "clinically significant recovery" in comparison to the 23% of TAU group participants, although this improvement was not maintained at the 6-month follow-up.
The results of Riaz and Agha's (2012) and Mitchell et al. (2011) studies suggest that a suicide prevention-specific cognitive behavioral treatment may not be necessary to reduce incidents of self-harm. Riaz and Agha (2012) applied a group-based CBT intervention to nine incarcerated, Pakistani women for four months and observed a reduction in the number of deliberate self-harm episodes and even an absence of these events between the end of intervention and follow-up. Participants demonstrated improved use of adaptive coping methods post-therapy, for example, the increased involvement in religion. However, some participants displayed an increase in avoidant behaviors, such as cigarette use or self-distraction upon the reduction of self-harm behaviors. This may be partially attributed to the limited coping methods that a restrictive prison environment affords. Notably, the sample size was very small and only one follow-up was conducted at one-month post-treatment due to institutional constraints.
Mitchell et al. (2011) administered cognitive behavioral therapy on a weekly basis to adolescents living in either a Secure Children's Home (SCH) or a Young Offender Institution (YOI). Scores on the Difficulties and Coping Profiles Questionnaire (DCP) indicated a decrease in self-harm and suicidal ideation among the adolescents receiving CBT, while a minimal change was seen within the TAU treatment group. The CBT group also achieved significant increases in the coping ability for depression and anxiety, although there was no change reported in self-harm coping abilities. Although participant retention was high in this study, researchers found no statistically significant outcomes for key measures at the 12-month follow-up.
Rohde et al. (2004) developed unique program interventions for adolescents in institutions for young offenders. Rohde et al. (2004) intervention, “Coping Course”, involved 16 treatment sessions provided over the course of eight weeks in which a group leader taught emotional regulation skills. The intervention aimed to enhance participants' coping skills and included social skills training, relaxation techniques, cognitive restructuring, communication improvement and problem-solving. In a comparison of pre and post-intervention scores on the Life Attitudes Schedule death-related (LAS death-related), study participants demonstrated a statistically significant decrease in scores, and this change was exclusively associated with the study group.
Welfare and Mitchell (2005) implemented the "Access Program", an intervention for adolescents that was uniquely designed to reduce the incidence of self-injury and improve participant hopelessness, self-esteem, locus of control and assertiveness. The program combines physical activity and cognitive behavioral techniques, incorporating an hour of emotional skills work and an hour of gymnasium activity for twelve sessions. The gym exercises intended to facilitate teamwork and confidence building, while the class work covered problem-solving and emotion management. Records of self-harm incidents suggest that the outcomes for participants were significantly better than for those in the wait-list group who did not receive the intervention. Staff reports indicate a decrease in participant actual and threatened self-injury that was maintained at the 6-week follow-up. Further, according to participant's self-report data, there was an improvement in adolescents' scores on the Beck Hopelessness scale and self-esteem measures (Welfare and Mitchell, 2005).
2.2.2. Dialectical behavioral therapy
While the original intent of DBT was to treat patients with suicidal behavior, only one study was found that employed DBT within correctional facilities and did not specifically target individuals diagnosed with borderline personality disorder. Trupin et al. (2002) administered a DBT intervention in a Juvenile Rehabilitation Administration facility for adolescent females and included two control groups: One control group was living in the General Population Cottage (GPCD) and received DBT, while the other control group was living in the General Population Cottage (GPCC) but received treatment-as-usual. Additionally, the records of thirty other females in the facility were used as a baseline comparison and mental health comparison. The experimental group consisted of juveniles females being housed in the "Mental Health Cottage" (MHC). At baseline, 58% of the MHC participants reported moderate to severe impairment on the self-harm subset of Child and Adolescent Functional Assessment Scale (CAFAS), compared to 21% of the GPCD participants.
DBT was only administered to the MHC and GPCD groups, on a weekly basis for four weeks in 60–90 min sessions. Treatment was delivered in a group format with eight residents per group; MHT staff received 80 h of DBT training prior to the study while GPCD staff received 14 h. The authors described the treatment approach as being "focused on validation of patients' current emotional, cognitive and behavioural responses as understandable in the context of the patient's skill level" which includes training in five skill categories: Core Mindfulness, Interpersonal Effectiveness, Emotion Regulation, Distress Tolerance and Self-Management (Trupin et al., 2002). GPCC's TAU consisted of the standard behavioral modification program provided in the facility.
The results of this study demonstrated a significant reduction in “serious” behavior problems among MHC participants during the length of study while this was not demonstrated among youth in the GPCD group. However, MHC staff received 80 h of DBT training while the GPCD staff received only 16 h. Additionally, the observed reduction in suicidal behavior, specifically, was not significantly greater “compared to the prior year on the same unit” (Trupin et al., 2002), which the authors partially attribute the mixed results to frequent transfers between the MHC and the GPC. The effectiveness of this intervention may improve if the DBT program was geared towards a target problem (i.e. self-harm), rather than all “serious behavioral problems”.
2.2.3. Peer prevention program
Junker et al. (2005) and Hall and Gabor (2004) implemented and reviewed peer prevention programs in which fellow inmates undergo training on topics such as effective and active listening, suicide prevention and intervention, non-verbal communications, the nature of mental illness, and the concept of befriending. These trainees were made available to incarcerated individuals in distress to serve as a “peer listener”. Following the application of the Inmate Observer Program, Junker et al. (2005) study demonstrated a decrease in the mean number of hours that individuals were on “suicide watch”. The study also indicated that when inmate observers were employed, individuals with personality disorder diagnoses had significantly fewer watches.
Hall and Gabor (2004) examined a peer program in a Canadian correctional facility that involved volunteers, correctional staff, the inmate population, and clinicians. However, the authors could not draw reasonable conclusions from the small sample size.
2.3. Limitations
This paper reviewed six studies that report promising results for the prevention of self-injury and suicide in correctional facilities. Nevertheless, in many cases, the integrity of the studies is compromised by definitional variances, missing comparison groups, and inconsistency of behavioral outcome measures. Moreover, it would be unfair to make direct comparisons between interventions given the wide variance in sample sizes (the minimum sample size was nine women; the largest sample included all of the general inmate population and personnel from 46 New York county jails). These studies provide important groundwork for further intervention design, with results suggesting that peer support networks and CBT components could be impactful in the prevention of suicidal behaviors. Pratt et al. (2015) pilot study yielded results that could justify further, more robust studies that include a larger sample size, yearly follow-ups, and clearer differentiation between self-injurious behavior and suicidal behavior. The application of DBT interventions-teaching mindfulness, interpersonal effectiveness, emotion regulation, distress tolerance and self-management- indicated a reduction in self-harm. However, the validity of further studies could be augmented by implementation longer-term, more intensive treatments with larger sample sizes.
2.3.1. Definitional variances
The literature on suicide and self-injury employ a variety of terms to describe the target behavior, including self-harm, non-suicidal self-injury (NSSI), self-injury, suicidal behavior and deliberate self-harm (DSH). Some studies condense all forms of self-injury, both suicidal and nonsuicidal, under one blanket term, such as "suicidal behavior" or "problem behavior" (Trupin et al., 2002; Mitchell et al., 2011), and one study only observed death-related thoughts (Rohde et al., 2004) rather than actual suicidal behavior. This is a significant need for a more clear-cut differentiation between “suicidal behavior” and “self-injury” in the literature. Pattison and Kahan (1983) define self-injury by its repetitive, time-limited nature with low lethality, and distinguish self-harm from suicide attempts by emphasizing the absence of the intent to die. Hooley and Franklin (2017) emphasize the need for a clearer distinction between suicidal behavior and NSSI. Their theory proposes that individuals engage in NSSI to 1) regulate or improve affect, 2) satisfy urges to self-punish, 3) identify with other self-injuring peers and 4) convey experienced pain or strength. Although NSSI serves as a risk factor for suicidal behavior and is strongly associated with suicidal behavior, NSSI is distinctive in its lack of suicidal intent (Hooley and Franklin, 2017).
2.3.2. Differences in behavioral outcome measures
For those studies that explicitly measure the same target behavior, there are still inconsistencies in the applied measurement tools. Mitchell et al. (2011), for example, used the SAVRY assessment, the Youth Self-Report and the Difficulties and Coping Profile. These tools place more emphasis on the risk of violence and rely on participant self-report, which provide a greater opportunity for bias. Conversely, Trupin et al. (2002) measured overall problem behavior through Community Risk Assessment Scores and assessed self-harm incidents via qualitative information from Daily Behavior Logs and staff reports.
Pratt et al. (2015) perhaps gathered the most comprehensive outcome measures by applying a wide range of tests. Researchers reviewed prison medical records to track the number of episodes of suicidal or self-injurious behaviors and in conjunction, participants completed the Beck Scale for Suicidal Ideation (BSSI), Suicide Probability Scale, Beck Hopelessness, Depression and Anxiety Inventories, Robson Self-Concept Questionnaire, Brief Psychiatric Rating Scale, and the Standardised Assessment of Personality– Abbreviated Scale. Not only did this study assess both suicidal behavior and self-harming behavior, but it collected information on contributing factors. It would be to the benefit of the other studies in this review to utilize a more exhaustive list of measurement tools to more accurately compare study-to-study results.
The results of each study certainly have clinical significance and implications for practice, but this discrepancy affects the ability to truly synthesize study results and accurately compare interventions.
2.3.3. Nature of self harm
It is challenging to assess an intervention for a behavior that serves so many functions, particularly in a correctional facility. According to Jeglic et al. (2005), the four main functions of self-harm in forensic populations include “1) depression and suicidal intent, 2) manipulation of the environment, 3) emotion regulation, and 4) a response to psychotic delusions or hallucinations”. To address self-harm related to depression and suicidal intent, research suggests the use of psychotherapy, CBT and/or pharmacotherapy. In the case of self-harm as a way of having needs met, Jeglic et al. (2005) recommend a behavioral plan, such as minimizing opportunity for secondary gain through self-harm i.e. reducing emotional responses to the behavior, altering the environment, etc. However, it is risky to assume manipulative intent and correctional staff should not discount the dangerousness of this behavior. Research suggests that 66% of male prisoners who reported to engage in self-injury for manipulative or gain-seeking reasons had demonstrated moderately severe or lethal behaviors (Dear et al., 2000).
Given the nature of some self-injury in the prison environment, correctional system clinicians tend to view self-harm as a symptom of Borderline Personality Disorder. However, research on self-harm in clinical populations find occurrences of NSSI across all psychiatric diagnosis and even among non-clinical populations (Hooley and Franklin, 2017).
Self-injury that is associated with emotional regulation may call for a DBT approach, involving behavioral chain analysis for incidents of self-injury and working to build emotional regulation and distress tolerance skills. Clinicians will likely approach psychosis-related self-harm through psychotherapy, antipsychotic medications and group therapy (Jeglic et al., 2005).
Taking this research into account, it seems impractical to treat self-injury as one, uniform problem and subsequently apply one, blanket treatment. Although it can be difficult to assess and identify the intent behind one's self-harming behaviors, researchers ought to study interventions that target specific subcategories of intent for a more customized, effective approach and possibly improved results.
2.3.4. Study design
The comparison of interventions was compounded by significant differences in sample size and study design. Two out of the six studies reviewed in this paper did not include a comparison group. This brings into question both the external and internal validity of the study results. Another limitation was the non-specification of gender in five studies, which disregards the possibility that a particular intervention may be more effective for females than males, or vice versa, or special considerations for suicidal behavior and self-injury among transgender population. The potential for significant baseline differences (i.e. higher lethality rates, higher rates of externalizing or internalizing behaviors, culture-related gender norms) harms the validity of a direct comparison.
A crucial point: it is extremely difficult to assess the effectiveness of suicide prevention. While unfortunately, suicide occurs at a higher rate in jails compared to the general population, it is not an everyday occurrence. The authors caution against drawing conclusions from data with such low absolute frequency.
Lastly, there was a wide variation between studies in follow-up times. Follow-ups occurred from one-month post-intervention (Riaz and Agha, 2012) to 11 months post-intervention (Mitchell et al., 2011). Short follow-up times allow more opportunity for bias and do not convey whether the initial improvements made post-intervention are lasting are enduring or short-lived. The inconsistency of follow-up periods among studies also affects the ability to make direct comparisons between results, given that some measures were taken while the intervention was recent and others were obtained long after treatment termination.
2.3.5. Logistical barriers
Given that all of the reviewed studies were conducted in correctional facilities, researchers were faced with a gamut of systemic obstacles that may have compromised treatment delivery or data collection. Firstly, attrition rates were moderately high in most of the studies due to frequent facility transfers or treatment refusal. Pratt et al. (2015) reported a refusal rate of 64% among eligible prisoners. This attrition or refusal rate threatens the internal and external validity of results, considering that completers may differ in study-based characteristics from those who drop-out or refuse to participate.
Second, researchers may have had limited access to prison facilities that impeded their ability to conduct treatment sessions. In the study performed by Riaz and Agha (2012), for example, the researchers were given access to the prison for only six months. One month of this period was used for recruitment, leaving limited time for the therapeutic intervention and a follow-up at one-month post-intervention- "a very short time period to assess the impact of CBT on a complex behavior like DSH" (Riaz and Agha, 2012). To exacerbate the issue, the therapist in this study was prohibited from conducting the sessions in the same room as participants, and the spaces made available for treatment offered very limited privacy. Correctional staff would occasionally attend sessions resulting in reserved behavior from participants, unable to express staff-related complaints or share incidents of rule-breaking.
Treatment sessions may be further impeded by frequent lockdowns on the prison block or throughout the entire facility, requiring participants to return to their cells. This common occurrence causes a loss of treatment time and a disruption of flow during therapeutic sessions.
The validity of self-reports in correctional facilities also comes into question. Incarcerated participants are often reluctant to disclose potentially damning information such as self-harm or possession of a sharp implement, considering the potential consequences. Therefore, there was an increased chance of inaccurate information in studies that relied on self-reports (Mitchell et al., 2011).
3. Conclusion
This systematic review highlights several areas for improvement within the research on suicide and self-injury in correctional facilities. Research would benefit from more consistent outcome measures and follow-up periods, and studies should clarify the target behavior and make the distinction between suicide, suicide attempts, suicidal self-injury and non-suicidal self-injury. Given that young adults are at a higher risk of self-injury than the general population (Welfare and Mitchell, 2005), more studies should be devoted to adolescent self-harm in correctional facilities (Mitchell et al., 2011; Rohde et al., 2004). This issue warrants greater attention, given that 1) there were approximately 34,000 incarcerated youth in the U.S. in 2016 (Rabuy, 2016) and 2) incarceration tends to increase the risk of self-injury (Welfare and Mitchell, 2005). Finally, while the many institutional regulations pose as a major barrier for research, researchers should make every attempt to conduct follow-up for as long as possible post-intervention for more accurate information on the durability of treatment effects.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Footnotes
References with * are the studies being included; all others are supporting documents.
References1
- Appelbaum K., Savageau J., Trestman R., Metzner J., Baillargeon J. A national survey of self-injurious behavior in American prisons. Psychiatr. Serv. 2011;62(3):285–290. doi: 10.1176/ps.62.3.pss6203_0285. [DOI] [PubMed] [Google Scholar]
- Barker E., Kõlves K., Leo D.D. Management of suicide and self-harming behaviors in prisons: systematic literature review of evidence based activities. Arch. Suicide Res. 2014;18(3):227–240. doi: 10.1080/13811118.2013.824830. [DOI] [PubMed] [Google Scholar]
- Briere J., Gil E. Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. Am. J. Orthopsychiatry. 1998;68(4):609–620. doi: 10.1037/h0080369. [DOI] [PubMed] [Google Scholar]
- Cox J.F., Morschauser P.C. A solution to the problem of jail suicide. Crisis. 1997;18:178–184. doi: 10.1027/0227-5910.18.4.178. [DOI] [PubMed] [Google Scholar]
- Dear G.E., Thomson D.M., Hills A.M. Self-harm in prisons: manipulators can also be suicide attempters. Crim. Justice Behav. 2000;27(2):160–175. [Google Scholar]
- Dixon-Gordon K., Harrison N., Roesch R. Non-suicidal self-injury within offender populations: a systematic review. Int. J. Forensic Ment. Health. 2012;11(1):33–50. [Google Scholar]
- Hall B., Gabor P. Peer suicide prevention in a prison. Crisis. 2004;25:19–26. doi: 10.1027/0227-5910.25.1.19. [DOI] [PubMed] [Google Scholar]
- Hooley J.M., Franklin J.C. Why do people hurt themselves? A new conceptual model of nonsuicidal self-injury. Clin. Psychol. Sci. 2017;6(3):428–451. 2018. [Google Scholar]
- Horton M., Wright N., Dyer W., Wright-Hughes A., Farrin A., Mohammed Z. Assessing the risk of self-harm in an adult offender population: an incidence cohort study. Health Technol. Assess. 2014;18(64) doi: 10.3310/hta18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeglic E., Vanderhoff H., Donovick P. The function of self-harm behavior in a forensic population. Int. J. Offender Ther. Comp. Criminol. 2005;49(2):131–142. doi: 10.1177/0306624X04271130. [DOI] [PubMed] [Google Scholar]
- Junker G., Beeler A., Bates J. Using trained offender observers for suicide watch in a federal correctional setting: a win-win solution. Psychol. Serv. 2005;2(1):20–27. [Google Scholar]
- Mitchell P., Smedley K., Kenning C., Mckee A., Woods D., Rennie C.E., Dolan M. Cognitive behaviour therapy for adolescent offenders with mental health problems in custody. J. Adolesc. 2011;34(3):433–443. doi: 10.1016/j.adolescence.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp J.J., Gutierrez P.M. Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Arch. Suicide Res. 2007;11(1):69–82. doi: 10.1080/13811110600992902. [DOI] [PubMed] [Google Scholar]
- Nock M.K., Kessler R.C. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J. Abnorm. Psychol. 2006;115:616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- Noonan . Bureau of Justice Statistics; 2016. Mortality in State Prison, 2001-2014 Statistical Tables.https://www.bjs.gov/content/pub/pdf/msp0114st.pdf Retrieved from. [Google Scholar]
- Pattison E.M., Kahan J. The deliberate self-harm syndrome. Am. J. Psychiatry. 1983;140:867–872. doi: 10.1176/ajp.140.7.867. [DOI] [PubMed] [Google Scholar]
- Pratt D., Tarrier N., Dunn G., Awenat Y., Shaw J., Ulph F., Gooding P. Cognitive–behavioural suicide prevention for male prisoners: a pilot randomized controlled trial. Psychol. Med. 2015;45(16):3441–3451. doi: 10.1017/S0033291715001348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabuy P.W. 2016. Mass Incarceration: the Whole Pie 2016.https://www.prisonpolicy.org/reports/pie2016.html Retrieved. from. [Google Scholar]
- Riaz R., Agha S. Efficacy of cognitive behavior therapy with deliberate self-harm in incarcerated women. Pakistan J. Psychol. Res. 2012;27(1):21–35. [Google Scholar]
- Rohde P., Jorgensen J.S., Seeley J.R., Mace D.,E. Pilot evaluation of the coping course: a cognitive-behavioral intervention to enhance coping skills in incarcerated youth. J. Am. Acad. Child Adolesc. Psychiatry. 2004;43(6):669–678. doi: 10.1097/01.chi.0000121068.29744.a5. [DOI] [PubMed] [Google Scholar]
- Thornton D. Depression, self-injury and attempted suicide amongst the YOI population. In: Fludger N.L., Simmons I.P., editors. Vol. 34. 1990. pp. 47–55. (Proceedings of the Prison Psychologists’ Conference, Division of Psychological Services Report Series 1). [Google Scholar]
- Trupin E.W., Stewart D.G., Beach B., Boesky L. Effectiveness of a dialectical behaviour therapy program for incarcerated female juvenile offenders. Child Adolesc. Ment. Health. 2002;7(3):121–127. [Google Scholar]
- Welfare H., Mitchell J. Addressing vulnerability amongst imprisoned juvenile offenders: an evaluation of the Access course. Int. J. Prison. Health. 2005;1:171–181. [Google Scholar]