Abstract
The aim of this study was to investigate the association among the PlA1/A2 gene polymorphism, laboratory aspirin resistance and adverse clinical outcomes in coronary artery disease (CAD) patients who were on aspirin maintainance therapy. A comprehensive literature search was performed and 35 eligible clinical trials including 19025 CAD patients were recruited. Adverse clinical outcomes involving all-cause death, non-fatal myocardial infarction (MI), ischemic stroke and target vessel revascularization (TVR) were analyzed. The definition of aspirin resistance in each study was accepted. Meta-analysis was performed using the Review Manager 5.3.5 System. In CAD patients, the PlA2 gene carriers had similar incidence of laboratory aspirin resistance compared to those with PlA1/A1 genotype [29.7% vs 28.3%, OR = 0.94 (95% CI 0.63 to 1.40, P = 0.74)], and there were no significant differences in the adverse clinical outcomes between the PlA2 carriers and the PlA1/A1 genotype patients. However, the laboratory aspirin non-responders had higher risks of death [7.9% vs. 2.5%, OR = 2.42 (95% CI 1.86 to 3.15, P < 0.00001)] and TVR [4.5% vs. 1.7%, OR = 2.20 (95% CI 1.19 to 4.08, P = 0.01)] compared to the responders. In aspirin-treated CAD patients, the laboratory aspirin resistance predicts all-cause death and TVR. However, the PlA1/A2 gene polymorphism predicts neither the laboratory aspirin response nor the clinical outcomes.
Subject terms: Cardiovascular genetics, Platelets
Introduction
Aspirin (acetylsalicylic acid) is a well-known baseline anti-platelet agent for the treatment and prevention of coronary artery disease (CAD). It irreversibly acetylates a serine residue at position 529 in platelet prostaglandin synthase, and inhibits cyclooxygenase (COX) channel associated with platelet aggregation. However, up to 24% patients were reported to be resistant to aspirin1. This mechanism of resistance and its clinical impact are under investigation.
PlA1/A2 polymorphism, a single nucleotide substitution (T → C) at position 1565 in exon 2 of the GP IIIa (a component of the final platelet aggregation pathway GPIIb/IIIa) gene has been reported to be associated with the laboratory detected aspirin resistance2–5 and adverse clinical outcomes6–9. However, the results are inconsistent among different studies10–12. In addition, study results regarding whether aspirin resistance is associated with adverse cardiovascular events are also inconsistent13–17.
This meta-analysis aimed to include the latest studies and update the concept regarding whether the PlA1/A2 gene polymorphism predicts laboratory aspirin resistance and/or cardiovascular outcomes, and whether laboratory detected aspirin resistance predicts cardiovascular outcomes in CAD patients who are on aspirin treatment. The results of this study will provide evidence for the individualized anti-platelet treatment.
Materials and Methods
Eligibility and search strategy
We performed a comprehensive literature search to identify all the studies investigating the association among PlA1/A2 gene polymorphism, aspirin resistance and cardiovascular outcomes in patients with coronary artery disease treated with aspirin. The literature was scanned by computerized searches of Pubmed, Embase, Cochrane library and Chinese Medical Journal Network databases from establishment to September 2018. The search strategy included a combination of medical subject headings and text words as follows: A = (aspirin OR acetylsalicylic acid), B = (platelet aggregation OR platelet activity OR aspirin resistance OR aspirin non-responder OR aspirin low response), C = (gene OR polymorphism OR mutation OR genotype OR allele OR genetic), D = (death OR stroke OR myocardial infarction OR revascularization). The Medical Subject Headings terms and text words A, B, C were used for the search to investigate the association between PlA1/A2 gene polymorphism and aspirin resistance; The Medical Subject Headings terms and text words A, C, D were used for the search to assess the association between PlA1/A2 gene polymorphism and cardiovascular outcomes; The Medical Subject Headings terms and text words A, B, D were used for the search to investigate the association between aspirin resistance and cardiovascular outcomes. Reference literatures of the appropriate trials were hand searched. The search results were limited to human. No language restriction was enforced.
Study selection
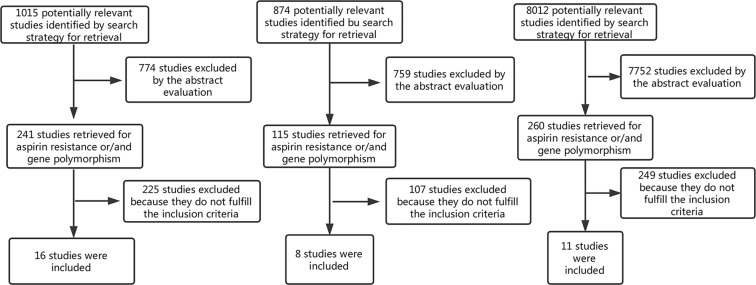
The inclusion criteria of this study include: (1) studies that include patients with confirmed CAD; (2) studies that include patients who were treated with aspirin for secondary prevention of cardiovascular events; (3) studies that contain a clear description of the method used to establish the effects of aspirin on platelet reactivity; (4) studies that contain a clear description of the PlA1/A2 polymorphism; (5) studies that report the incidence of either death, myocardial infarction (MI), ischemic stroke, or target vessel revascularization (TVR). Studies that meet the criteria (1), (2), (3), (4) were adopted to analyze the relationship between PlA1/A2 gene polymorphism and aspirin resistance. Studies that meet criteria (1), (2), (4), (5) were adopted to analyze the relationship between PlA1/A2 gene polymorphism and cardiovascular outcomes. Studies that meet criteria (1), (2), (3), (5) were adopted to analyze the relationship between aspirin resistance and cardiovascular outcomes (Fig. 1). We assessed the included observational studies according to the Newcastle-Ottawa Scale.
Figure 1.
Flowchart of the study selection.
Clinical outcomes
The adverse clinical outcomes involve all-cause death, non-fatal MI, ischemic stroke and TVR. The definition of each event in the original articles was accepted.
Statistical analysis
Statistical analysis was performed using Review Manager 5.3.5 (The Cochrane Collaboration, Oxford, England). The odds ratio (OR) or relative risk (RR), and 95% confidence interval (CI) for categorical variables were calculated using a fixed-effect model with the Mantel-Haenszel method. The DerSimonian and Laird random effect model was applied to the calculated OR and RR in case of significant heterogeneity across studies. Statistical heterogeneity was evaluated using the Q statistic with P < 0.1. Points were evaluated at the longest follow-up available. Statistical significance was considered as P < 0.05.
Results
PlA1/A2 gene polymorphism and aspirin resistance
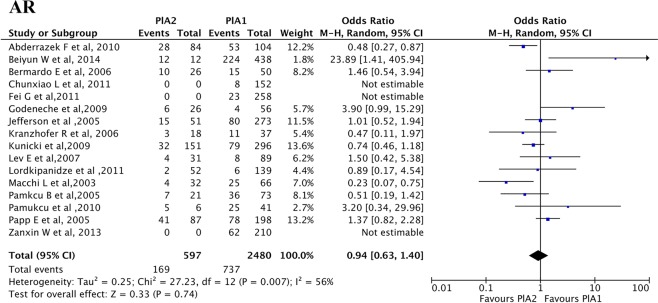
Sixteen studies18–33 including 3077 CAD patients were selected to assess the association between PlA1/A2 gene polymorphism and aspirin resistance. Details of included studies are summarized in Table 1. Heterogeneity testing showed considerable bias between different studies (P = 0.004), so a random effect model was adopted. An OR of 0.94 (95% CI 0.63 to 1.40, P = 0.74) was observed for aspirin resistance in patients carrying the PlA2 allele (PlA1/A2 + PlA2/A2) (Fig. 2).
Table 1.
Characteristics of eligible studies referring to the association between PlA1/A2 gene polymorphism and aspirin resistance.
| Source | Number of patients | Study design | Aspirin dosage (mg) | Method of assessment of lab AR | Definition of assessment of lab AR | PlA2 (AR/AS) | PlA1 (AR/AS) |
|---|---|---|---|---|---|---|---|
| Abderrazek F et al., 2010 | 188 | Cohort study | 250 | PFA-100 | CEPI-CT < 160 s | 28/56 | 53/51 |
| Beiyun W et al., 2014 | 450 | Cohort study | 100 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 12/0 | 224/214 |
| Bernardo E et al., 2006 | 76 | Cohort study | 100 | PFA-100 | CEPI-CT < 193s | 10/16 | 15/35 |
| Chunxiao L, et al., 2011 | 152 | Cohort study | 100 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 0/0 | 8/144 |
| Fei G et al., 2011 | 258 | Cohort study | 100 | 11-DH-TXB2 | 11-DH-TXB2 ≥ 20% | 0/0 | 23/235 |
| Kranzhofer R et al., 2006 | 55 | Cohort study | 100 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 3/15 | 11/26 |
| Lev EI et al., 2007 | 120 | Cohort study | 325 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 4/27 | 8/81 |
| Macchi L et al., 2003 | 98 | Cohort study | 160 | PFA-100 | CEPI-CT < 186 s | 4/28 | 25/41 |
| Pamukcu B et al., 2005 | 94 | Cohort study | 100–300 | PFA-100 | CEPI-CT < 186 s | 7/14 | 36/37 |
| Papp E et al., 2005 | 285 | Case-control study | 100–325 | LTA | UK | 41/46 | 78/120 |
| Zanxin W et al., 2013 | 210 | Cohort study | 100 | 11-DH-TXB2 | 11-DH-TXB2 ≥ 20% | 0/0 | 62/148 |
| Godeneche et al., 2009 | 82 | Cohort study | 160 | PFA-100 | CEPI-CT < 187 s | 6/26 | 4/56 |
| Jefferson et al., 2005 | 324 | Cohort study | 81 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 15/51 | 80/273 |
| Kunicki et al., 2009 | 447 | Cohort study | 75–150 | PFA-100 | CEPI-CT < 164 s/192 s | 32/151 | 79/296 |
| Lordkipanidze et al., 2011 | 191 | Cohort study | 85–325 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 2/52 | 6/139 |
| Pamukucu et al., 2010 | 47 | Cohort study | 193/207 | PFA-100 | CEPI-CT < 186 s | 5/6 | 25/41 |
AR, aspirin resistance; AS, aspirin sensitive; PFA-100, platelet function analyzer-100; ADP, adenosine diphosphate; AA, arachidonic acid; PLADP, ADP-induced platelet aggregation; PLAA, AA-induced platelet aggregation; UK, unknown;11-DH-TXB2, 11-dehydro-thromboxane B2; LTA, light transmittance aggregometry; CEPI-CT, collagen epinephrine-close time.
Figure 2.
Association between PlA1/A2 polymorphism and laboratory aspirin resistance. The position of the blue squares corresponds to the odds ratio (OR) per study and the horizontal black line to the 95% confidence intervals (CI). The size of the square is proportional to the relative weight of that study w(%) to compute the overall OR (black diamond). The width of the diamond represents the 95% CI of the overall OR. If a 95% CI spans one (indicated by the black vertical solid line), this study has found no significant difference in the incidence of aspirin resistance (AR) between patients carrying the PlA1 and PlA2 alleles. This meta-analysis shows no significant change in the incidence of AR of patients carrying the PlA2 allele over those carrying PlA1 allele. The overall OR is 0.94 (P = 0.74). Note that the p-value mentioned here is the p-value for Z test.
A subgroup analysis was conducted considering that the methodology used to assess aspirin resistance might influence the association. The data available allowed the comparison of two methods: light transmission aggregometry (LTA) and point-of-care assay PFA-100 (Supplemental Figs 1 and 2).
The LTA subgroup analysis showed significant homogeneity between studies (P = 0.22), but did not reveal a significant association between carriage of the PLA2 allele and aspirin resistance (OR 1.35, 95% CI 0.96, 1.91; P = 0.09). The PFA-100 subgroup analysis revealed a significant association between carriage of PLA2 allele and aspirin sensitivity (OR 0.7, 95% CI 0.52, 0.94; P = 0.02), but showed significant heterogeneity between studies (P = 0.02). This significance was lost when using the random effects model (OR 0.79, 95% CI 0.45, 1.38; P = 0.4).
PlA1/A2 gene polymorphism and adverse cardiovascular outcomes
Eight studies6–12,34 including 4091 CAD patients were selected to investigate the association between PlA1/A2 gene polymorphism and adverse cardiovascular events. Details of the included studies are summarized in Table 2. Among the recruited studies, data on death was available in eight studies6–12,34; data on non-fatal MI was available in seven studies6,8–12,34; and data on TVR was available in five studies6,8,10–12.
Table 2.
Characteristics of eligible studies referring to the association between PlA1/A2 gene polymorphism and adverse cardiovascular events.
| Source | Number of patients (PlA1/PlA2) | Study design | Aspirin dosage (mg) | Mean follow-up | Outcomes (PlA1/PlA2) | |
|---|---|---|---|---|---|---|
| Addad F et al., 2010 | 188(104/84) | Cohort study | 250 | 1 year | Death | (10/1) |
| Kastrati A et al., 2000 | 1759(1234/525) | Cohort study | 200 | 1 month | Death | (4/3) |
| MI | (51/24) | |||||
| TVR | (28/12) | |||||
| Laule M et al., 1999 | 653(470/183) | Case-control study | 100 | 1 month | MI | (8/4) |
| Death | (1/0) | |||||
| TVR | (18/10) | |||||
| Lopes NH et al., 2004 | 562(450/112) | Cohort study | UK | 3 years | Death | (41/2) |
| MI | (37/9) | |||||
| TVR | (44/2) | |||||
| Syros G et al., 2009 | 200(144/56) | Cohort study | UK | 1 year | Death | (2/2) |
| MI | (1/0) | |||||
| TVR | (8/1) | |||||
| Walter DH et al., 1997 | 318(255/63) | Cohort study | 100–500 | 1 month | Death | (0/0) |
| MI | (3/4) | |||||
| Walter DH et al., 2001 | 324(253/71) | Cohort study | 100 | 6 months | Death | (9/0) |
| MI | (9/2) | |||||
| TVR | (83/30) | |||||
| Wheeler GL et al., 2002 | 87(66/21) | Cohort study | UK | 24 h | Death | (0/0) |
| MI | (4/0) | |||||
MI, myocardial infarction; TVR, target vessel revascularization; UK, unknown.
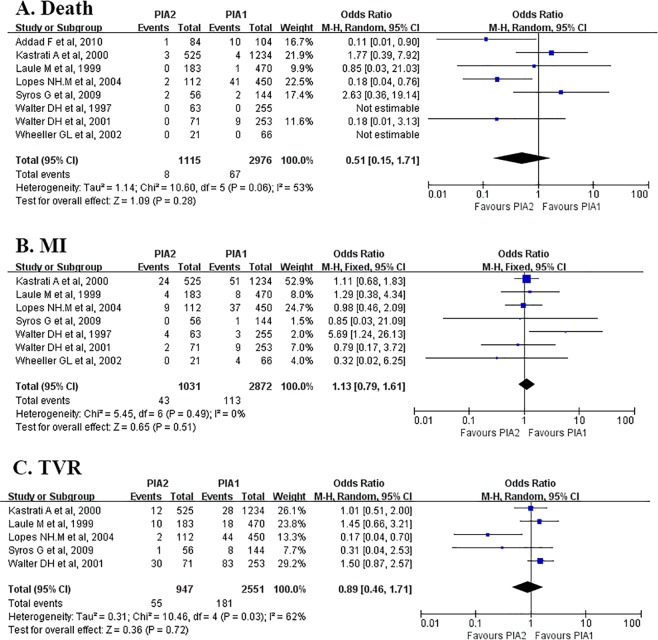
Meta-analysis showed that PlA2 gene carriers had similar risk of death compared with PlA1/A130. The incidences of MI and TVR in PlA2 gene carriers (PlA1/A2 or PlA2/A2) were also similar to those with the wild genotype (PlA1/A1) with ORs of 1.13 (95% CI 0.79 to 1.61, P = 0.51) and 0.89(95% CI 0.46 to 1.61, P = 0.71) respectively (Fig. 3).
Figure 3.
Association between PlA1/A2 polymorphism and clinical outcomes. Symbols and conventions are the same as in Fig. 2. This meta-analysis shows no significant change in the incidences of death, MI or TVR of patients carrying the PlA2 allele over those carrying PlA1 allele. The overall ORs of death, MI and TVR are 0.51(P = 0.28), 1.13 (P = 0.51) and 0.89 (P = 0.72) respectively. Note that the p-values mentioned here are the p-values for Z test. CI, confidence interval; MI, myocardial infarction; TVR, target vessel revascularization.
Laboratory aspirin resistance and adverse cardiovascular outcomes
Eleven studies13–17,35–40 with 11857 aspirin-treated CAD patients were included to analyze the association between laboratory aspirin resistance and adverse cardiovascular outcomes. Details of included studies are summarized in Table 3, where mortality was reported in 10 studies13–17,36–40, ischemic stroke was reported in 5 studies16,17,36–38, and revascularization was reported in 4 studies35,37–39.
Table 3.
Characteristics of eligible studies referring to the association between laboratory aspirin resistance and adverse cardiovascular outcomes.
| Source | Number of patients (AR/AS) | Study design | Aspirin dosage (mg) | Method of assessment of lab AR | Definition of assessment of lab AR | Mean follow-up | Outcomes (AR/AS) | |
|---|---|---|---|---|---|---|---|---|
| Salah A et al., 2015 | 50(24/26) | Cohort study | 150 | LTA | PLAA ≥ 20% | 6 months | Death | (0/0) |
| MI | (2/0) | |||||||
| Stone GW et al., 2013 | 8527(478/8049) | Cohort study | 300–324 | VerifyNow | >550ARU | 1 years | Death | (3/253) |
| MI | (7/143) | |||||||
| Li L et al., 1912 | 109(20/89) | Cohort study | 100 | CHRONO-LOG | >0Ω | 1years | UK | UK |
| Glulmez O et al., 2008 | 114(27/87) | Cohort study | 300 | PFA-100 | CEPI-CT < 165 s | 1 week | UK | UK |
| Christiaens L et al., 2008 | 97(29/ 68) | Cohort study | 160 | PFA-100 | CEPI-CT < 187 s | 2.5 years | Death | (3/5) |
| MI | (1/2) | |||||||
| Anderson K et al., 2002 | 71(25/46) | Cohort study | 75–160 | PFA-100 | CEPI-CT < 196 s | 4 years | MI | (3/4) |
| TVR | (9/9) | |||||||
| Gum PA et al., 2003 | 326(17/309) | Cohort study | 325 | LTA | PLADP ≥ 70% and PLAA ≥ 20% | 679 days | Death | (2/15) |
| MI | (1/12) | |||||||
| Kim HJ et al., 2002 | 220(39/181) | Cohort study | 100 | VerifyNow | ≥550ARU | 72 hours | Death | (0/1) |
| MI | (1/12) | |||||||
| TVR | (1/3) | |||||||
| Gori Am et al., 2016 | 1789(364/1425) | Cohort study | 100–325 | LTA | PLAA ≥ 20% | 2 years | Death | (35/54) |
| MI | (9/32) | |||||||
| TVR | (3/13) | |||||||
| Marcucci R et al., 2006 | 146(41/105) | Cohort study | 100 | PFA-100 | CEPI-CT < 203 s | 1 year | Death | (6/9) |
| MI | (4/13) | |||||||
| TVR | (8/4) | |||||||
| Foussas SG et al., 2009 | 496(121/375) | Cohort study | 100/160/280/325 | PFA-100 | CEPI-CT < 193 s | 1 year | Death | (28/36) |
AR, aspirin resistance; AS, aspirin sensitive; LTA, light transmittance aggregometry; PLAA, AA-induced platelet aggregation; MI, myocardial infarction; ARU, aspirin reaction units; UK, unknown; PFA-100, platelet function analyzer-100; CEPI-CT, collagen epinephrine-close time; TVR, target vessel revascularization; PLADP, ADP-induced platelet aggregation.
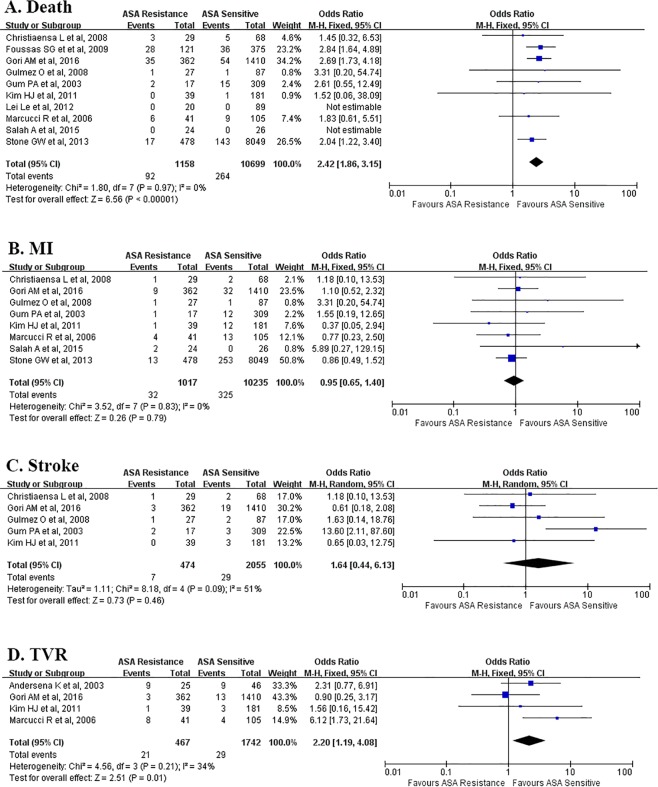
Meta-analysis showed that the laboratory aspirin resistance significantly increased the risk of all-cause death (OR = 2.42, 95% CI 1.86 to 3.15, I2 = 0%, P < 0.00001) and TVR (OR = 2.20, 95% CI 1.19 to 4.08, I2 = 13%, P = 0.01) (Fig. 4).
Figure 4.
Association between laboratory aspirin resistance and clinical outcomes. Symbols and conventions are the same as in Fig. 2. This meta-analysis shows significant overall increase in the incidences of death and TVR of patients with AR over those without AR, while no significant change in the incidences of MI or stroke. The overall ORs in death, MI, stroke and TVR are 2.42 (P < 0.00001), 0.95 (P = 0.79), 1.64 (P = 0.46) and 2.2 (P = 0.01) respectively. Note that the p-values mentioned here are the p-values for Z test. CI, confidence interval; ASA, aspirin; MI, myocardial infarction; TVR, target vessel revascularization.
Discussion
In this systematic review and meta-analysis we have found that: (1) there is no significant association between the PlA1/A2 polymorphism and aspirin resistance, or the PlA1/A2 polymorphism and worse clinical outcomes. (2) Laboratory aspirin resistance predicts all-cause death and TVR.
The PlA1/A2 gene polymorphism generated great interest since Weiss et al.41 first reported that PlA2 gene carriers presented a two-fold increase in risk of acute coronary syndromes. It has been clarified that PlA1/A2 encodes the platelet membrane glycoprotein IIIa which is integrated with glycoprotein IIb to form a complex. People with wild-type PlA1 have leucine at position 33 of mature glycoprotein IIIa, while those with point mutation PlA2 have proline at this position as a consequence of the substitution of cytosine for thymidine at position 1565 in exon 2 of the glycoprotein IIIa gene42. However, whether this mutation affects the anti-platelet effect of aspirin remains controversial.
By this meta-analysis, we found that PlA1/A2 polymorphism does not predict laboratory aspirin resistance. In fact, aspirin reduces the activation of platelets by irreversibly acetylating serine at position 529 of cyclooxygenase-1 (COX-1), and thereby reduces thromboxane A2 (TXA2) formation from the platelets43. So when aspirin effectively blocks the COX-1 channel, platelet aggregation would be effectively inhibited as a consequence of less TXA2 formation even in PlA2 carriers who have an increased activity of the GpIIb/IIIa receptor44. We suggest that PlA1/A2 polymorphism does not affect the anti-platelet effect of aspirin as aspirin has an upstream inhibitory effect on platelet aggregation, which may also account for its inability to predict the clinical outcomes.
Goodman et al.45 reported their meta-analysis which showed a genetic association between the PlA1/A2 molecular variant and aspirin resistance in healthy subjects who took aspirin alone. However, they failed to find significant association between carriage of the PlA2 allele and aspirin resistance in subjects with cardiovascular disease, which was consistent with our findings. In fact, in our study 51.1% of the CAD patients are on dual anti-platelet treatment with aspirin and a P2Y12 receptor antagonist, and it has been demonstrated that P2Y12 antagonists potentiate the inhibitory actions of PGI2, which would be converted to TXA2 46. So it is possible that P2Y12 antagonists cause certain degree of platelet inhibition through blockage of TXA2 formation, and thereby obscuring the presence of aspirin resistance, as well as bias our study results. However, we believe that the efficacy of PlA1/A2 on aspirin resistance as well as the clinical outcomes would be too weak to be significant, should it exist.
Our study found that laboratory aspirin resistance predicted all-cause death and TVR, though the following studies reported negative results. Kim et al.37 included 220 patients who were planned to receive off-pump coronary artery bypass surgery (OPCAB), but it only recorded in-hospital clinical outcomes during the same admission period with relatively small sample size and very short follow-up intervals. This could lead to a study bias. The study conducted by Gulmez et al.16 was similar in this aspect.
Floyd et al. investigated the association between PlA1/A2 polymorphism of glycoprotein IIIa and the efficacy of aspirin by meta-analysis in 201447, in which they included 14 papers18,19,21,22,24–26,29–33,48,49 published before 1 April 2013, and 1463 subjects who were homozygous for the PlA1 allele and 622 who carried the PlA2 allele were enrolled in their meta-analysis. In our study, however, we only included papers studying on patients with coronary artery disease, so we excluded 2 papers48,49 included in Floyd’s study, but recruited another 4 papers20,23,27,28 in the analysis. As a result, sixteen studies18–33 including 3077 CAD patients were enrolled to assess the association between PlA1/A2 gene polymorphism and aspirin resistance. To the best of our knowledge, this meta-analysis is the first to simultaneously investigate the relationship among PlA1/A2, aspirin resistance and clinical outcomes, which included the latest studies and recruited the largest study population, and would come out with the most updated, accurate and realistic results on this topic.
Although we adopted a random effect model in the process of this meta-analysis, the following limitations could not be avoided: (1) The recruited studies differed in genders and the duration of follow-up time, which might cause heterogeneities. If more data were available in the future, it would be preferable to perform a refined stratification analysis with data being adjusted for these factors. (2) The recruited studies differed in geographical areas, of which 4 were performed in Asia, 8 in America, and 12 in Europe. It was reported that the prevalence of the PlA2 allele is dependent on ethnicity, with a frequency of approximately 15 per 100 in Caucasian populations falling to 1 per 100 in Oriental populations50,51. If we have a detailed data on the ethnicity of each included patient, a stratification analysis on different ethnicity would be valuable to elucidate whether the results would be differ by ethnicity. (3) As pointed out by Floyd et al., mortality bias may attenuate or entirely obscure any true association52. Almost a third of individuals with a first major coronary event die out-of-hospital, and are not accounted for in the predominantly retrospective data presented in this meta- analysis52.
In conclusion, in aspirin-treated CAD patients, the laboratory aspirin resistance predicts all-cause death and TVR. However, the PlA1/A2 gene polymorphism predicts neither the laboratory aspirin response nor the clinical outcomes. Given this result, individualized anti-platelet treatment with the guidance of PlA1/A2 genetic testing may not be meaningful. This is in accordance with the 2018 ESC/EACTS guidelines on myocardial revascularization which recommended that genetic testing can not be recommended on a routine basis for tailoring and escalating dual anti-platelet treatment after stent implantation in all percutaneous coronary intervention (PCI)-treated patients53. However, as the results of laboratory platelet function test on individual aspirin response predict clinical outcomes, patients with aspirin resistance would benefit from intensified anti-platelet treatment.
Supplementary information
Acknowledgements
This work was supported by a grant from the National Natural Science Funding of China (81170181), a grant from the Jiangsu Province’s Key Provincial Talents Program (ZDRCA2016013), and a Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutes (PAPD).
Author Contributions
All the authors have made substantial contributions to the intellectual content of the manuscript. C.L., J.W. & J.L. - Designed the study; J.W., J.L., Y.Z. & F.W. - Collected the data. J.W., J.L., F.W. & K.X. - Prepared the manuscript. D.K., J.B., J.C., X.G. & H.M. - Analyzed the data. C.L. - Revised and edited the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jing Wang, Jie Liu, Yaqing Zhou and Fei Wang contributed equally.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-49123-y.
References
- 1.Hovens MM, et al. Prevalence of persistent platelet reactivity despite use of aspirin: a systematic review. American heart journal. 2007;153:175–181. doi: 10.1016/j.ahj.2006.10.040. [DOI] [PubMed] [Google Scholar]
- 2.Newman PJ, Derbes RS, Aster RH. The human platelet alloantigens, PlA1 and PlA2, are associated with a leucine33/proline33 amino acid polymorphism in membrane glycoprotein IIIa, and are distinguishable by DNA typing. Journal of Clinical Investigation. 1989;83:1778. doi: 10.1172/JCI114082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooke GE, Bray PF, Hamlington JD, Pham DM, Goldschmidt-Clermont PJ. PlA2 polymorphism and efficacy of aspirin. The Lancet. 1998;351:1253–1253. doi: 10.1016/S0140-6736(05)79320-X. [DOI] [PubMed] [Google Scholar]
- 4.Michelson AD, et al. Platelet GP IIIa PlA polymorphisms display different sensitivities to agonists. Circulation. 2000;101:1013–1018. doi: 10.1161/01.CIR.101.9.1013. [DOI] [PubMed] [Google Scholar]
- 5.Gum PA, et al. Profile and prevalence of aspirin resistance in patients with cardiovascular disease. The American journal of cardiology. 2001;88:230–235. doi: 10.1016/S0002-9149(01)01631-9. [DOI] [PubMed] [Google Scholar]
- 6.Lopes NH, et al. Effect of glycoprotein IIIa PlA2 polymorphism on outcome of patients with stable coronary artery disease and effect of smoking. Am J Cardiol. 2004;93:1469–1472. doi: 10.1016/j.amjcard.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Addad F, et al. Platelet glycoprotein IIIa (platelet antigen 1/platelet antigen 2) polymorphism and 1-year outcome in patients with stable coronary artery disease. Blood Coagul Fibrinolysis. 2010;21:674–678. doi: 10.1097/MBC.0b013e32833e47c1. [DOI] [PubMed] [Google Scholar]
- 8.Walter DH, Schachinger V, Elsner M, Dimmeler S, Zeiher AM. Platelet glycoprotein IIIa polymorphisms and risk of coronary stent thrombosis. Lancet (London, England) 1997;350:1217–1219. doi: 10.1016/S0140-6736(97)05399-3. [DOI] [PubMed] [Google Scholar]
- 9.Wheeler GL, et al. Reduced inhibition by abciximab in platelets with the PlA2 polymorphism. Am Heart J. 2002;143:76–82. doi: 10.1067/mhj.2002.119763. [DOI] [PubMed] [Google Scholar]
- 10.Laule M, et al. A1/A2 polymorphism of glycoprotein IIIa and association with excess procedural risk for coronary catheter interventions: a case-controlled study. Lancet (London, England) 1999;353:708–712. doi: 10.1016/s0140-6736(98)07257-2. [DOI] [PubMed] [Google Scholar]
- 11.Kastrati A, et al. PlA polymorphism of glycoprotein IIIa and risk of adverse events after coronary stent placement. Journal of the American College of Cardiology. 2000;36:84–89. doi: 10.1016/S0735-1097(00)00709-9. [DOI] [PubMed] [Google Scholar]
- 12.Syros G, et al. Role of PLA2 polymorphism on clinical events after percutaneous coronary intervention. Acute cardiac care. 2009;11:88–91. doi: 10.1080/17482940902785474. [DOI] [PubMed] [Google Scholar]
- 13.Salah A, El-Desuky M, Rizk A, El-Hadidy A. Aspirin resistance: Prevalence and clinical outcome in Egypt. The Egyptian Journal of Critical Care Medicine. 2015;3:23–27. doi: 10.1016/j.ejccm.2014.12.001. [DOI] [Google Scholar]
- 14.Stone GW, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet (London, England) 2013;382:614–623. doi: 10.1016/s0140-6736(13)61170-8. [DOI] [PubMed] [Google Scholar]
- 15.Li L, et al. Correlation between antiplatelet resistance and recurrent cardiac ischemic events of patients with acute myocardial infarction. Zhonghua yi xue za zhi. 2012;92:2677–2680. [PubMed] [Google Scholar]
- 16.Gulmez O, et al. Effects of persistent platelet reactivity despite aspirin therapy on cardiac troponin I and creatine kinase-MB levels after elective percutaneous coronary interventions. Journal of thrombosis and thrombolysis. 2008;25:239–246. doi: 10.1007/s11239-007-0067-z. [DOI] [PubMed] [Google Scholar]
- 17.Christiaens L, Ragot S, Mergy J, Allal J, Macchi L. Major clinical vascular events and aspirin-resistance status as determined by the PFA-100 method among patients with stable coronary artery disease: a prospective study. Blood Coagul Fibrinolysis. 2008;19:235–239. doi: 10.1097/MBC.0b013e3282f9ade8. [DOI] [PubMed] [Google Scholar]
- 18.Abderrazek F, et al. The GPIIIa PlA polymorphism and the platelet hyperactivity in Tunisian patients with stable coronary artery disease treated with aspirin. Thromb Res. 2010;125:e265–268. doi: 10.1016/j.thromres.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Bernardo E, et al. Lack of association between gene sequence variations of platelet membrane receptors and aspirin responsiveness detected by the PFA-100 system in patients with coronary artery disease. Platelets. 2006;17:586–590. doi: 10.1080/09537100600881412. [DOI] [PubMed] [Google Scholar]
- 20.Gao F, Wang ZX, Men JL, Ren J, Wei MX. Effect of polymorphism and type II diabetes on aspirin resistance in patients with unstable coronary artery disease. Chinese medical journal. 2011;124:1731–1734. [PubMed] [Google Scholar]
- 21.Kranzhofer R, Ruef J. Aspirin resistance in coronary artery disease is correlated to elevated markers for oxidative stress but not to the expression of cyclooxygenase (COX) 1/2, a novel COX-1 polymorphism or the PlA(1/2) polymorphism. Platelets. 2006;17:163–169. doi: 10.1080/09537100500441101. [DOI] [PubMed] [Google Scholar]
- 22.Lev EI, et al. Genetic polymorphisms of the platelet receptors P2Y(12), P2Y(1) and GP IIIa and response to aspirin and clopidogrel. Thromb Res. 2007;119:355–360. doi: 10.1016/j.thromres.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Li C-X, Wei L, Yang Z-H, Liu Z-T, Hou L-L. Relationship Between the Gene Polymorphisms of Platelet Glycoprotein III aPLA and I a 807 C/T with Aspirin Resistance. Progress in Modern Biomedicine. 2011;11:2324–2327. [Google Scholar]
- 24.Macchi L, et al. Resistance in vitro to low-dose aspirin is associated with platelet PlA1 (GP IIIa) polymorphism but not with C807T(GP Ia/IIa) and C-5T Kozak (GP Ibalpha) polymorphisms. Journal of the American College of Cardiology. 2003;42:1115–1119. doi: 10.1016/S0735-1097(03)00921-5. [DOI] [PubMed] [Google Scholar]
- 25.Pamukcu B, Oflaz H, Nisanci Y. The role of platelet glycoprotein IIIa polymorphism in the high prevalence of in vitro aspirin resistance in patients with intracoronary stent restenosis. Am Heart J. 2005;149:675–680. doi: 10.1016/j.ahj.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 26.Papp E, et al. Glycoprotein IIIA gene (PlA) polymorphism and aspirin resistance: is there any correlation? The Annals of pharmacotherapy. 2005;39:1013–1018. doi: 10.1345/aph.1E227. [DOI] [PubMed] [Google Scholar]
- 27.Wang B-Y, Tan S-J. Platelet glycoprotein IIIa gene polymorphism (Leu33Pro) and aspirin resistance in a very elderly Chinese population. Genetic testing and molecular biomarkers. 2014;18:389–393. doi: 10.1089/gtmb.2013.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Z, et al. Polymorphisms and high on-aspirin platelet reactivity after off-pump coronary artery bypass grafting. Scandinavian cardiovascular journal: SCJ. 2013;47:194–199. doi: 10.3109/14017431.2013.800640. [DOI] [PubMed] [Google Scholar]
- 29.Godeneche G, et al. Stroke and aspirin non-responder patients: Relation with hypertension and platelet response to adenosine diphosphate. Platelets. 2009;20:471–477. doi: 10.3109/09537100903171404. [DOI] [PubMed] [Google Scholar]
- 30.Jefferson BK, et al. <em>Aspirin</em> resistance and a single gene. American Journal of Cardiology. 2005;95:805–808. doi: 10.1016/j.amjcard.2004.11.045. [DOI] [PubMed] [Google Scholar]
- 31.Kunicki R, et al. Lack of association between aspirin responsiveness and seven candidate gene haplotypes in patients with symptomatic vascular disease. Thrombosis and Haemostasis. 2017;101:123–133. doi: 10.1160/th08-05-0287. [DOI] [PubMed] [Google Scholar]
- 32.Lordkipanidzé M, et al. Genetic determinants of response to aspirin: Appraisal of 4 candidate genes. Thrombosis Research. 2011;128:47–53. doi: 10.1016/j.thromres.2011.02.019. [DOI] [PubMed] [Google Scholar]
- 33.Pamukcu B, et al. Impact of genetic polymorphisms on platelet function and aspirin resistance. Blood Coagul Fibrinolysis. 2010;21:53–56. doi: 10.1097/MBC.0b013e328332ef66. [DOI] [PubMed] [Google Scholar]
- 34.Walter DH, et al. Statin therapy is associated with reduced restenosis rates after coronary stent implantation in carriers of the Pl(A2)allele of the platelet glycoprotein IIIa gene. European heart journal. 2001;22:587–595. doi: 10.1053/euhj.2000.2313. [DOI] [PubMed] [Google Scholar]
- 35.Andersen K, Hurlen M, Arnesen H, Seljeflot I. Aspirin non-responsiveness as measured by PFA-100 in patients with coronary artery disease. Thromb Res. 2002;108:37–42. doi: 10.1016/S0049-3848(02)00405-X. [DOI] [PubMed] [Google Scholar]
- 36.Gum PA, Kottke-Marchant K, Welsh PA, White J, Topol EJ. A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. Journal of the American College of Cardiology. 2003;41:961–965. doi: 10.1016/S0735-1097(02)03014-0. [DOI] [PubMed] [Google Scholar]
- 37.Kim HJ, et al. Preoperative aspirin resistance does not increase myocardial injury during off-pump coronary artery bypass surgery. Journal of Korean medical science. 2011;26:1041–1046. doi: 10.3346/jkms.2011.26.8.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gori AM, et al. High on-aspirin platelet reactivity predicts cardiac death in acute coronary syndrome patients undergoing PCI. European journal of internal medicine. 2016;30:49–54. doi: 10.1016/j.ejim.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Marcucci R, et al. Usefulness of aspirin resistance after percutaneous coronary intervention for acute myocardial infarction in predicting one-year major adverse coronary events. Am J Cardiol. 2006;98:1156–1159. doi: 10.1016/j.amjcard.2006.05.041. [DOI] [PubMed] [Google Scholar]
- 40.Foussas SG, et al. The Impact of Aspirin Resistance on the Long‐term Cardiovascular Mortality in Patients with Non‐ST Segment Elevation Acute Coronary Syndromes. Clinical cardiology. 2009;32:142–147. doi: 10.1002/clc.20293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weiss EJ, et al. A polymorphism of a platelet glycoprotein receptor as an inherited risk factor for coronary thrombosis. New England Journal of Medicine. 1996;334:1090–1094. doi: 10.1056/NEJM199604253341703. [DOI] [PubMed] [Google Scholar]
- 42.Kunicki TJ, Aster RH. Isolation and immunologic characterization of the human platelet alloantigen, P1 A1. Molecular immunology. 1979;16:353–360. doi: 10.1016/0161-5890(79)90100-7. [DOI] [PubMed] [Google Scholar]
- 43.Hankey GJ, Eikelboom JW. Aspirin resistance. The Lancet. 2006;367:606–617. doi: 10.1016/S0140-6736(06)68040-9. [DOI] [PubMed] [Google Scholar]
- 44.Frey UH, Aral N, Muller N, Siffert W. Cooperative effect of GNB3 825C>T and GPIIIa PI(A) polymorphisms in enhanced platelet aggregation. Thromb Res. 2003;109:279–286. doi: 10.1016/S0049-3848(03)00253-6. [DOI] [PubMed] [Google Scholar]
- 45.Goodman T, Ferro A, Sharma P. Pharmacogenetics of aspirin resistance: a comprehensive systematic review. British journal of clinical pharmacology. 2008;66:222–232. doi: 10.1111/j.1365-2125.2008.03183.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan Melissa V., Knowles Rebecca B. M., Lundberg Martina H., Tucker Arthur T., Mohamed Nura A., Kirkby Nicholas S., Armstrong Paul C. J., Mitchell Jane A., Warner Timothy D. P2Y12receptor blockade synergizes strongly with nitric oxide and prostacyclin to inhibit platelet activation. British Journal of Clinical Pharmacology. 2016;81(4):621–633. doi: 10.1111/bcp.12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Floyd CN, Ferro A. The PlA1/A2 polymorphism of glycoprotein IIIa in relation to efficacy of antiplatelet drugs: a systematic review and meta-analysis. British journal of clinical pharmacology. 2014;77:446–457. doi: 10.1111/bcp.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.FONTANA P., NOLLI S., REBER G., DE MOERLOOSE P. Biological effects of aspirin and clopidogrel in a randomized cross-over study in 96 healthy volunteers. Journal of Thrombosis and Haemostasis. 2006;4(4):813–819. doi: 10.1111/j.1538-7836.2006.01867.x. [DOI] [PubMed] [Google Scholar]
- 49.Gonzalez-Conejero Rocio, Rivera Jose, Corral Javier, Acuña Carmen, Guerrero Jose A., Vicente Vincente. Biological Assessment of Aspirin Efficacy on Healthy Individuals. Stroke. 2005;36(2):276–280. doi: 10.1161/01.STR.0000151362.65339.f9. [DOI] [PubMed] [Google Scholar]
- 50.Simsek S, et al. Determination of human platelet antigen frequencies in the Dutch population by immunophenotyping and DNA (allele-specific restriction enzyme) analysis. Blood. 1993;81:835–840. [PubMed] [Google Scholar]
- 51.Lim J, et al. Variation of the platelet glycoprotein IIIa PI(A1/A2) allele frequencies in the three ethnic groups of Singapore. Int J Cardiol. 2003;90:269–273. doi: 10.1016/S0167-5273(02)00567-3. [DOI] [PubMed] [Google Scholar]
- 52.Floyd CN, Mustafa A, Ferro A. The PlA1/A2 polymorphism of glycoprotein IIIa as a risk factor for myocardial infarction: a meta-analysis. PLoS One. 2014;9:e101518. doi: 10.1371/journal.pone.0101518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Neumann FJ, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. doi: 10.1093/eurheartj/ehy394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.