Abstract
Background:
Suicide is the second leading cause of death among adolescents. The purpose of this study was to test a family-focused outpatient cognitive-behavioral treatment (F-CBT) protocol for depressed adolescents following psychiatric hospitalization for a suicide attempt or suicidal ideation, and who had a co-occurring risk factor (suicidal behavior prior to the index admission, non-suicidal self-injury, and/or a substance use disorder), in a randomized Phase 2 efficacy trial.
Method:
One-hundred forty-seven adolescents (Mean age = 14.91 years; 76.2% female, 85.5% White) and their families, recruited primarily from an inpatient psychiatric hospitalization program, were randomly assigned to F-CBT or enhanced treatment-as-usual (E-TAU). A suicide attempt was the primary outcome variable. Depression, suicidal ideation and non-suicidal self-injury are also reported here. Assessments were completed at pre-treatment as well as 6, 12, and 18-months post-randomization. (Trial Registration ClinicalTrials.gov Identifier: )
Results:
In the sample as a whole, rates of attempts decreased from 20% at 6 months to 9% at 12-months to 7% at 18-months. There was no evidence of a significant difference between treatment arms in rates of suicide attempts, major depressive disorder, suicidal ideation, or non-suicidal self-injury at any of the post-randomization assessment points.
Conclusions:
Though F-CBT was associated with reductions in suicidality, depression, and non-suicidal self-injury, E-TAU showed an equally strong effect. Greater frequency of F-CBT treatment sessions, particularly at the start of care, and alternative approaches to transitioning to care at 12 months, may be necessary when using F-CBT with this population.
Keywords: Suicide, cognitive-behavioral therapy, adolescent, clinical trial
Introduction
Suicidal ideation (SI) and behavior increase markedly during adolescence. Suicide is the second leading cause of death among adolescents (Centers for Disease Control and Prevention, 2017). Over the past decade, suicide rates have tripled in this age group (Curtin, Hedegaard, Minino, and Warner, 2016). Hospitalizations for SI and behavior among youth have also doubled over the last 10 years (Plemmons et al., 2018) but clinical trials for adolescent suicidal behavior are limited (Ougrin, Tranah, Stahl, Moran, and Asarnow, 2015). Below we review randomized trials of in-person outpatient treatments for suicidal adolescents with or without non-suicidal self-injury (NSSI) that report these specific outcomes. References to self-harm below refer to suicide attempts (SAs) and/or NSSI.
There have been several therapeutic approaches tested for adolescent suicidal behavior. Developmental group therapy as an adjunct to treatment-as-usual (TAU) has been tested in three clinical trials with adolescents who self-harm. In the first trial with 63 adolescents, those who received group therapy (versus did not) were less likely to report repetitive self-harm at 6 to 7-month follow-up (Wood, Trainor, Rothwell, Moore, and Harrington, 2001). However, neither replication study showed efficacy for developmental group therapy as an adjunct to TAU on rates of self-harm or SAs (Greene et al., 2011; Hazell et al. 2009).
Rossouw and Fonagy (2011) randomized 80 adolescents with self-harm to mentalization based treatment (MBT-A) or TAU. MBT was associated with less self-harm at 12-month follow-up. However, slightly less than half of the participants completed treatment across both conditions. Dialectical behavioral therapy (DBT) has also been tested with adolescents. Mehlum et al. (2014) randomized 77 adolescents with self-harm to DBT or enhanced TAU (E-TAU). The DBT condition showed greater decreases in self-harm and SI compared to TAU at post-treatment (Mehlum et al, 2014). Differential effects on self-harm were retained at the one- and three-year follow-up (Mehlum et al., 2016; Mehlum et al., this issue). McCauley et al. (2018) randomized 173 adolescents with at least one lifetime SA, elevated SI, and repeated self-harm, to DBT or manualized individual and group supportive therapy (I-GST). DBT was associated with lower odds of SAs and NSSI than I-GST at the six, but not 12-, month follow-up; although DBT was associated with significantly higher rates of clinically significant change, defined as the absence of any self-harm at both the 6- and 12-month follow-up points.
Cognitive-behavioral therapy (CBT) has been tested in a number of trials. Asarnow et al. (2017) randomized 42 adolescents with a SA in the prior 3 months or NSSI and repeated self-harm to a DBT informed 12-week CBT protocol with a strong family focus (SAFETY) or E-TAU. SAFETY was associated with a higher probability of survival without a SA at 3-month follow-up than E-TAU. Donaldson, Spirito, and Esposito-Smythers (2005) randomized 35 adolescents who attempted suicide to brief individual CBT treatment or a supportive relationship treatment. No differences were found in SI or SAs (only 5% attempted) across conditions at three or six-month follow-up. This protocol was subsequently modified into a 12-month protocol, referred to as Integrated CBT (I-CBT). Esposito-Smythers, Spirito, Kahler, Hunt, and Monti (2011) randomized 40 adolescents with a SA or severe SI and a substance use disorder to I-CBT or E-TAU. Those in I-CBT made fewer SAs and had fewer re-hospitalizations and emergency department (ED) visits over the 18-month study period compared to E-TAU. They also showed greater reductions in heavy drinking and marijuana use days over time relative to E-TAU. No difference was found in SI.
In the current study, a parallel group randomized controlled trial was used to test whether F-CBT, a modified version of I-CBT, would be more efficacious than E-TAU on SAs, depression, SI, and NSSI, for psychiatrically hospitalized depressed suicidal adolescents, who also had a co-occurring risk factor, i.e. a SA prior to index admission, NSSI, and/or a substance use disorder.
Methods
Participants
Participants included 147 adolescents (aged 12–18 years) who were recruited from an inpatient unit (n = 131; 89.11%) or a partial hospitalization program (n = 16; 10.88%). Adolescents were eligible if they were: 1) English speaking; 2) met criteria for major depressive disorder, dysthymia, depression or mood disorder not otherwise specified; 3) were hospitalized for a SA or SI; and 4) had at least one of the following co-occurring risk factors: a SA prior to the index admission, NSSI, or a substance use disorder. Adolescents were ineligible if they had: 1) cognitive or developmental delays; 2) a diagnosis of autism spectrum disorder; 3) a primary diagnosis of a psychotic disorder, obsessive compulsive disorder, or an eating disorder; or 4) used “hard” illicit substances, such as opiates.
Procedures
All study procedures were approved by the hospital human subjects’ protection committee (Lifespan Corporation). This trial is registered with ClinicalTrials.gov Identifier: NCT01732601. Participants were identified through clinical team referrals or electronic health record (EHR) review and invited to participate in the study if they met the inclusion and exclusion criteria; 98.34% consented to a review of the EHR for SA and treatment-related data over the 18-month study period. After written informed consent and assent were obtained, a baseline assessment was administered while participants were psychiatrically hospitalized or during partial hospitalization (for those who were recruited directly from partial). After completion of the baseline assessment, families were assigned to their treatment condition by the study coordinator, on a 1:1 randomization schedule, using a computerized urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994). Urn randomization was used to retain random allocation while balancing the treatment conditions on two a priori variables (biological sex and history of a SA). The allocation sequence was concealed in the electronic program from the study coordinator. Research assistants who completed the follow-up assessments were masked to treatment condition, but did learn of condition on occasion, primarily due to spontaneous comments made by participants. Follow-up assessments, that included all study measures, were administered at 6, 12, and 18-months post-randomization. See Figure 1 for participant flow through the study.
Figure 1.
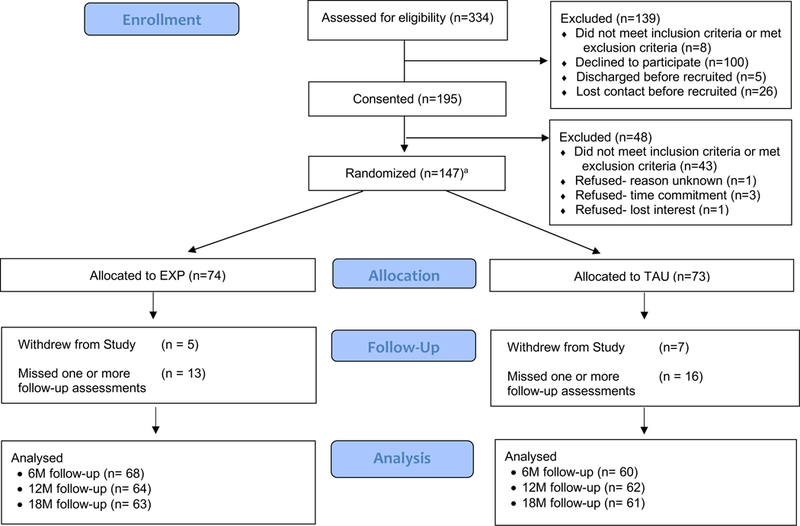
Participant flow through the study.
Note. aNumber analyzed in intent-to-treat analyses.
Treatment Conditions
Family-Focused Cognitive Behavioral Therapy (F-CBT).
The F-CBT protocol is a modified version of the I-CBT protocol that has been described in a previous trial (Esposito-Smythers et al., 2011). I-CBT integrates cognitive and behavioral techniques to address adolescent suicidality, substance abuse, and other common co-occurring conditions. It also employs motivational enhancement to improve motivation for change and treatment engagement. I-CBT is manualized and modular, and includes adolescent, parent training, and family modules. For each family, two therapists are assigned, one that works individually with the adolescent and one that works with the parents. Both therapists typically participate in family sessions. At the start of treatment, all families receive psychoeducation and safety planning. The manual includes four core skill sessions (problem-solving, cognitive restructuring, behavioral activation, and affect regulation) that all families receive as well as a menu of supplemental skills (e.g., enhancing social support, chain analysis). Sessions have common components, including a safety check-in, adherence to medication, homework review, agenda setting, new skill introduction/skill practice, agenda discussion, homework assignment, and parent-teen check-in. Treatment is flexible and skills can be repeated as necessary. Treatment was offered to families over a period of 12 months. Sessions decreased in frequency over time from 0 to 6 months (adolescents attend weekly and parents weekly to bi-weekly), 6 to 9 months (adolescents attended bi-weekly and parents bi-weekly to monthly), and 9–12 months (adolescents and parents attended monthly).
Based on the expansion our adolescent inclusion criteria in the present study and our prior experience, a number of changes were made to the I-CBT protocol resulting in the F-CBT protocol used here. To better accommodate a broader sample of suicidal youth, sessions were added to better address emotion regulation (distress tolerance), physical health (healthy lifestyle), trauma (trauma narrative), and anxiety (exposure). We also broadened the scope of prior substance specific sessions (e.g., the “Coping with Urges” module was used to address any high-risk behavior, such as NSSI, not just substance use urges). Parental “self-care” sessions were also added to the F-CBT manual. Therapists could teach parents seven skills only taught to adolescents (relaxation, behavioral activation, etc.) in I-CBT. We also added a parent training emotion coaching session to improve parent-child interactions. Table S1 contains the treatment modules in F-CBT.
Masters (n = 5) and doctoral level clinicians (n = 12) were trained using a combination of didactic instruction, review of videotaped sessions, and role-plays. Once trained, all intervention sessions were audio recorded. All recordings for the first two participant cases seen by each therapist, as well as a random selection of approximately 20% of subsequent recordings, were reviewed by the first, second, and last authors to rate fidelity and provide feedback and supervision. Weekly individual and group supervision included a review of weekly risk assessments (i.e., mood, suicidality, substance use), CBT strategies used in session, and ratings from tapes reviewed by supervisors. If therapist drift was evident, obstacles to adherence were processed, solutions generated, and role-plays conducted to enhance training.
Enhanced Treatment as Usual.
Those assigned to the E-TAU condition were referred for treatment by their inpatient or partial hospitalization treatment team. The frequency and type of outpatient care provided was at the discretion of the individual provider. To enhance this condition, parents/guardians were offered the study phone number so that they could contact study staff if they had trouble arranging services. They were also contacted twice between the baseline and 6-month follow-up to check on progress and whether study staff could help them problem-solve any issues related to their teen.
Adolescents across both conditions had their medication regimen reviewed and adjusted as needed during hospitalization by the attending psychiatrists who were supervised by the study psychiatrist. Adolescents in the F-CBT condition were given the option of having their medication managed by the study psychiatrist post-discharge. More than half of the study sample received intensive step-down care post-hospitalization prior to outpatient care. Partial hospitalization included 2–4 weeks of individual, group, and family therapy, as well as medication and case management.
Measures
Primary Outcome (SAs)
Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al., 2011).
The C-SSRS semi-structured interview defines SAs as any self-injurious act with at least some (non-zero) intent or desire to die. The C-SSRS has been found to be reliable for use with adolescent psychiatric samples (κ = .88) for SAs (Posner et al., 2011). A three to four-month training period was implemented by the third author before research assistants administered the C-SSRS independently. Each interview was reviewed by the third author, blind to participant condition and psychopathology, who made the final classification. A third rater was added to the process as needed for disagreements. This procedure provided some protection from potential bias in the rare event that a participant revealed his/her treatment condition.
Electronic health record (EHR) reviews were conducted for participants who provided consent. SAs found in the EHR were included in SA counts in study analyses. In instances where suicide data in the EHR revealed no suicidal intent present in indicated acts but the C-SSRS did capture intent, we prioritized the C-SSRS data and coded indicated acts as attempts. The EHR review resulted in inclusion of six attempts not reported on the C-SSRS (five among participants who withdrew and one for a participant who did not report accurately on the C-SSRS). SAs made over the prior six months were assessed at each post-randomization assessment.
Secondary Outcomes Related to Suicidal Behavior (Depression, SI, and NSSI)
Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS-PL; Kaufman et al, 1997).
The K-SADS-PL is semi-structured diagnostic interview that was used to assess the presence of DSM-IV-TR psychiatric disorders, including Major Depressive Disorder. Interviews were conducted by trained masters-level, post-doctoral, and licensed clinical psychologists. A supervising licensed clinical psychologist randomly selected 20% of audio-taped interviews to examine inter-rater reliability which was high (k=.90).
Suicidal Ideation Questionnaire - Junior (SIQ-Jr.).
The 15-item SIQ-Jr (SIQ-JR; Reynolds, 1985) was used to assess SI in the last 30 days. The SIQ uses a Likert scale ranging from 0 to 6 (‘I’ve never had this thought’ to ‘almost every day’). Scores range from 0–90 with those at 31 and above indicating clinical significance. The SIQ has excellent internal consistency and construct validity (Reynolds, 1987).
Self-Injurious Thoughts and Behavior Interview (SITBI; Nock, Holmberg, Photos, and Michel 2007).
The SITBI is a structured interview that was used to examine the presence, frequency, and characteristics of NSSI over the prior 30 days. The SITBI has strong interrater reliability and test-retest reliability (Nock et al., 2007). Interviewer training and supervision followed the same procedure as that done for the C-SSRS.
Children’s Depression Inventory 2 (CDI-2; Kovacs, 2011).
The 28-item CDI-2 was used to assess depressive symptoms over the prior two weeks. Scores range from 0 to 56 with higher scores representing more depressive symptoms. The CDI-2 has demonstrated good reliability and validity in clinical samples (Kovacs, 2011).
Treatment Contacts
Child and Adolescent Services Assessment (CASA; Burns, Angold, Magruder-Habib, Costello, and Patrick, 1997).
The CASA is a clinician administered interview used to assess adolescent service use for mental health problems. Adequate reliability has been demonstrated (ICCs=.74-.76) (Farmer, Angold, Burns, and Costello, 1994). EHRs were reviewed to gather additional data on inpatient and partial hospital admissions as well as ED visits.
Statistical Power
In a sample of 150 and expected 20% attrition, based on pilot I-CBT trial results for SAs (5.3% CBT vs. 35.3% TAU) and an alpha level of 0.01, power is 0.94 using a test of two independent proportions. A conservative alpha level was used due to the small sample size of the pilot RCT.
Analytic Plan
Logistic regression was used to assess predictors of study dropout, including treatment group assignment. To account for attrition, mixed effects models, including hierarchical linear and generalized linear mixed models to estimate differences in trial arm effects, were used. All study participants who provided data at pre-randomization were included in the intent-to-treat analyses. To account for variability in pre-randomization scores on tested outcomes, a random coefficient for the intercept was included. Mixed models included time, trial arm, the trial arm x time interaction, and were adjusted for randomization stratifiers (e.g., sex and lifetime history of a SA). Time was treated as a categorical variable with the pre-randomization period (baseline) as the reference point; this approach allowed for a direct test of treatment arm differences at the three post-randomization time points (6-, 12-, and 18-months). To test the hypotheses regarding trial arm differences for primary and secondary outcomes over the course of the trial, the parameter estimates of interest were the interaction terms between trial arm and measurement period. All treatment effect analyses were conducted in Mplus Version 8.2 with maximum likelihood estimation.
Results
F-CBT Treatment
Families randomized to F-CBT received an average of 26.97 individual adolescent sessions (SD = 14.86, Range = 1–53) and 19.94 parent/family sessions (SD = 11.57, Range = 0–40). Of the parent/family sessions, 75.4% were parent sessions (parent training and/or parent self-care) and 24.6% family sessions.
Therapist Competence/Fidelity
Approximately 26% of F-CBT therapy sessions (n=3,385) were rated for fidelity, including 24% of teen sessions and 29% of parent/family sessions. This included the first two cases seen by each therapist and a random selection of other tapes. The Cognitive Therapy Rating Scale (CTRS; Young & Beck, 1980) was used to measure therapist competence in the delivery of the I-CBT protocol. Scores ≥ 44 on the CTRS are considered acceptable. Approximately 92% of rated teen sessions (M = 49.49, SD = 5.34, range = 1 – 63) and 95% of parent/family sessions (M = 50.64, SD = 4.70, range = 31–61) met this criterion.
Adherence checklists, adapted slightly from those used in our prior work (Esposito-Smythers et al., 2011), were completed for each module. They included components common (e.g., set agenda) and unique (e.g., introduced the SOLVE method) to each session. The number of items on checklists ranged from 9 to 23 across sessions. Adherence to 80% of items in a session was deemed acceptable. Approximately 88% of teen sessions and 84% of parent/family sessions met the 80% criterion. The average adherence ratings for teens (M = 92.30%, SD =11.18%, range = 32% - 100%) and parent/family sessions (M = 91.43%, SD = 13.26%, range = 32% - 100%) was high.
Approximately 15% (n = 69) of rated tapes reviewed by a second rater to calculate inter-rater reliability. Interclass correlation coefficients (ICC) estimates and their 95% confidence intervals were calculated based on a mean-rating (k = 2), absolute-agreement, 2-way mixed-effects model. The ICC for adherence ratings was .93 (95% CI = .88-.96), indicating excellent reliability. The ICC for CTRS ratings was .83 (95% CI = .72-.89), indicating good reliability.
Outside Service Use
More than half of participants received intensive step-down services, partial hospitalization, following discharge from the psychiatric inpatient unit (F-CBT = 56.2%, E-TAU = 63.9%) before beginning outpatient F-CBT or E-TAU. After treatment assignment, about one-third were psychiatrically hospitalized (F-CBT = 37%, E-TAU = 36.6%), and about one-fifth were treated in an ED for a mental health related concern (F-CBT = 16.4%, E-TAU = 21.1%).
Attrition
Table 1 summarizes participants’ baseline demographic and clinical characteristics. Treatment arm did not predict missingness (p = .40). In separate logistic regression analyses, no sociodemographic, psychiatric diagnostic, or baseline indicators of suicidality (p’s > .05) predicted attrition.
Table 1.
Pre-randomization demographic, self-harm data, and psychiatric diagnosis by condition
| F-CBT Percent (N) |
E-TAU Percent (N) |
Total Percent (N) |
|
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) | 15.05 (1.44) | 14.75 (1.56) | 14.90 (1.51) |
| Sex (Female) | 77.03 (57) | 75.34 (55) | 76.19 (112) |
| Ethnicity (Non-Hispanic/Latino) | 85.14 (63) | 81.69 (58) | 83.45 (121) |
| Race | |||
| White | 86.49 (64) | 84.51 (60) | 85.52 (124) |
| Black/African American | 1.35 (1) | 2.82 (2) | 2.07 (3) |
| Asian/Pacific Islander | 4.05 (3) | 1.41 (1) | 2.76 (4) |
| Multiracial | 8.11 (6) | 11.27 (8) | 9.66 (14) |
| Suicide Attempt1 | |||
| Lifetime | 64.86 (48) | 66.20 (47) | 65.52 (95) |
| Number of attempts, mean (SD) | 1.97 (4.51) | 1.57 (2.87) | 1.78 (3.79) |
| Current DSM-IV-TR Diagnoses2 | |||
| Major Depressive Disorder | 93.24 (69) | 84.93 (62) | 89.12 (131) |
| Generalized Anxiety Disorder | 47.95 (35) | 30.99 (22) | 39.58 (57) |
| Post-Traumatic Stress Disorder | 18.31 (13) | 18.31 (13) | 18.31 (26) |
| ADHD | 22.54 (16) | 30.56 (22) | 26.57 (38) |
| Disruptive Behavior Disorder3 | 21.92 (16) | 15.49 (11) | 18.75 (27) |
| Alcohol/Substance Use Disorder | 18.06 (13) | 26.39 (19) | 22.22 (32) |
| Non-Suicidal Self-Injury4 | |||
| Lifetime | 79.73 (59) | 83.10 (59) | 81.38 (118) |
Note. Total N = 147 (F-CBT n = 74; E-TAU n = 73). Data are presented as observed number (percentage) endorsed unless otherwise indicated.
Columbia-Suicide Severity Rating Scale (C-SSRS).
Diagnoses derived from the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-PL). ADHD = attention/deficit-hyperactivity disorder;
Conduct Disorder or Oppositional Defiant Disorder;
Self-Injurious Thoughts and Behavior Interview (SITBI).
Primary Outcome: SAs
There was no evidence for a rate difference in SAs between the treatment arms at any point post-randomization (Table 2). Rates of attempts in the total sample decreased from 20% at 6-months to 9% at 12-months to 7% at 18-months.
Table 2.
Primary and Secondary Outcomes Related to Suicidal Behavior Between the I-CBT and E-TAU Arms At 6-, 12-, and 18-Months Post-randomization
| I-CBT Percent (N) |
E-TAU Percent (N) |
Model Coefficientsa [95% CI] |
p | |
|---|---|---|---|---|
| Primary Outcome: Suicide Attempt1 | ||||
| Pre-randomization | 52.7 (39) | 50.7 (36) | ||
| 6-months | 20.3 (14) | 20.3 (13) | −0.13 [−3.89 – 3.64] | .95 |
| 12-months | 12.1 (8) | 6.6 (4) | 0.83 [−1.26 – 2.92] | .44 |
| 18-months | 9.4 (6) | 3.3 (2) | 1.42 [−1.23 – 4.06] | .29 |
| Secondary Outcomes Related to Suicidal Behavior: Major Depression Diagnosis2 | ||||
| Pre-randomization | 93.2 (69) | 84.9 (62) | ||
| 6-months | 29.9 (20) | 29.8 (17) | −1.12 [−2.78 – 0.55] | .98 |
| 12-months | 21.0 (13) | 13.6 (8) | −0.44 [−2.26 – 0.55] | .64 |
| 18-months | 27.4 (17) | 12.5 (7) | 0.23 [−1.82 – 2.28] | .83 |
| Suicidal Ideation,3 mean (SD) | ||||
| Pre-randomization | 46.6 (22.7) | 48.9 (20.9) | ||
| 6-months | 20.2 (18.5) | 23.4 (18.1) | −2.70 [−10.34 – 4.94] | .49 |
| 12-months | 16.8 (14.2) | 16.4 (14.9) | 0.26 [−8.12 – 8.63] | .95 |
| 18-months | 18.6 (12.5) | 16.2 (8.1) | 3.26 [−3.96 – 10.48] | .38 |
| Depression Symptoms,4 mean (SD) | ||||
| Pre-randomization | 27.0 (8.7) | 26.3 (9.8) | ||
| 6-months | 17.2 (10.8) | 17.1 (10.6) | −0.49 [−4.67 – 3.70] | .82 |
| 12-months | 13.2 (9.3) | 13.8 (9.2) | −1.02 [−5.03 – 2.99] | .62 |
| 18-months | 16.0 (10.2) | 10.7 (8.8) | 4.80 [0.64 – 8.96] | .02 |
| Nonsuicidal Self-Injury5 | ||||
| Pre-randomization | 73.0 (54) | 74.7 (53) | ||
| 6-months | 52.9 (36) | 61.3 (38) | −0.79 [−2.35 – 0.78] | .33 |
| 12-months | 28.6 (18) | 38.3 (23) | −1.44 [−3.56 – 0.68] | .18 |
| 18-months | 22.2 (14) | 17.0 (10) | 1.09 [−2.66 – 4.84] | .57 |
Note. Total N = 147 (F-CBT n = 74; E-TAU n = 73). Data are presented as observed percentage (number) endorsed unless otherwise indicated. Models are adjusted for sex and lifetime history of suicide attempt.
Model coefficients represent odds ratios for binary outcomes and unstandardized regression coefficients for continuous outcomes.
Columbia-Suicide Severity Rating Scale (C-SSRS).
Diagnoses derived from the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADs).
Suicidal Ideation Questionnaire-Junior (SIQ-J).
Children’s Depression Inventory (CDI-2).
Self-Injurious Thoughts and Behavior Interview (SITBI).
When SAs were examined (n=67), most (73% total; 78.4% in F-CBT; 66.7% in E-TAU) were coded as “no to minor physical damage/not requiring medical care” using the C-SSRS Lethality/Medical Damage Scale. Exploratory analyses provided no evidence of a significant treatment effect on lethality/physical damage of SAs, although the rate of attempts coded as “moderate to severe physical damage” was somewhat lower in F-CBT than E-TAU youth (21.6% vs. 33.3%, χ2(1) =1.56, p=.28, d=0.27).
Secondary Outcome Related to Suicidal Behavior: SI and NSSI
There were no significant differences between the treatment arms in rates of major depressive disorder, severity of SI, or the occurrence of NSSI at any point post-randomization (Table 2). Although there were no differences in depressive symptoms between the arms at 6- or 12-months post-randomization, there was a significant difference at 18-months post-randomization; participants in the F-CBT arm (M = 15.95, SD = 10.16) reported higher scores on the CDI-2 than those in the E-TAU arm (M = 10.70, SD = 8.78).
Discussion
This trial did not provide evidence for the efficacy of the F-CBT intervention, compared to E-TAU, in a sample of psychiatrically hospitalized depressed suicidal adolescents, who also had a co-occurring risk factor, i.e. a SA prior to index admission, NSSI, and/or a substance use disorder. The lack of differential effects was surprising due to the strong results of the initial study (Esposito-Smythers et al., 2011). The most obvious clinical observation was the increased acuity and severity of psychopathology in this sample compared to the original sample. Despite the fact that most adolescents received step-down care, and F-CBT focused on managing acute suicidality, about one-third of the sample, in both conditions, were re-hospitalized within six months of enrollment. Cohort effects have been clearly evident in adolescent inpatient psychiatric samples over the last two decades and it was evident in the composition of this sample. Indeed, one multisite study examining site differences in CBT outcomes with treatment resistant depressed adolescents demonstrated that the level of psychopathology of the adolescents was the best predictor of CBT outcomes (Spirito et al., 2009). In addition, the I-CBT relative to the F-CBT sample, had notably higher rates of substance use (100% vs. 22%) and conduct (35% vs. 2%) disorders where an emphasis on parent training, such as that used in the I-CBT protocol, has been demonstrated to be critical to treatment success. The current sample had higher rates of generalized anxiety disorder (40% vs 16%) suggesting a more internalizing sample. Although the NSSI rates were comparable (71% vs. 87%), anecdotally, NSSI was more chronic and severe in the present study requiring much greater attention to NSSI as a treatment focus in the current sample.
F-CBT was delivered with comparable fidelity and competency as I-CBT, so the lack of differential findings would not appear to be related to therapist factors. However, it is possible that modifications made to the protocol, to account for differences in the sample composition in this study, played a role in the differential outcomes. For example, we may have reduced the potential efficacy of the parent component of our intervention by reducing the number of parent “training” sessions to accommodate parent “self-care” sessions.
SA measurement also differed across studies. Positive responses to any of three questions on the C-SSRS (Have you made a SA, done anything to harm yourself, or anything dangerous where you could have died?) could result in coding of a SA if the adolescent endorsed at least a 1% intent or desire to die. In the I-CBT study, questions from the K-SADS-PL were used to code SAs. Adolescents had to positively endorse the question, “Have you tried to kill yourself,” and thus beliefs about the act were considered in consensus coding. The McCauley et al. (2018) study used the Linehan Suicide Attempt Self-Injury Interview (SASII; Linehan, 2006), which requires that adolescents indicate that they believed that their acts “could have led to death” to be coded as a SA. Many attempts in our study would not have been coded if we used the latter definition. In fact, most SAs were coded as “no to mild” physical damage that did not require medical care in the present study.
There are several additional potential reasons for more positive findings in the DBT and the I-CBT studies. First, unlike the DBT studies, we recruited almost all participants from a psychiatric inpatient unit. Thus, the greater acuity of the sample could account for differential findings. Second, unlike the I-CBT study, the majority of adolescents (64%) in the E-TAU arm stepped down to intensive services before receiving outpatient services. The partial hospitalization treatment received in E-TAU may have led to greater stabilization post-hospitalization. Indeed, SA outcomes over 18 months for E-TAU in the present study appear somewhat better than E-TAU in the I-CBT study (26.2% vs. 35.3%, respectively). They were also comparable to the tightly controlled and monitored IGST condition used to mimic TAU in the McCauley et al. (2017) DBT study (21.5% in IGST vs. 20.3% in our E-TAU condition at 6 months, 10.3% in IGST vs. 6.6% in our E-TAU condition at 12 months). Although Mehlum et al. and Asarnow et al. (2017) used E-TAU as the comparator conditions and did see an advantage for DBT and DBT-informed family centered treatment, respectively.
Study assessors were required to breach confidentiality when clinically significant SI or a SA was reported during assessments. This procedure may have suppressed reporting in the E-TAU arm for fear of hospitalization and parental notification. In the F-CBT arm, SI and SAs were assessed at every therapy session. Adolescents learned that reporting SI or a SA was not necessarily a trigger for hospitalization but rather an opportunity to apply skills to manage suicidal thinking. Indeed, concern about being re-hospitalized is a well-documented barrier to youth willingness to disclose SI (Cigularov, Chen, Thurber, & Stallones, 2008). In addition, the repeated assessment of suicidality in therapy may have enhanced the recall of these events for those in the F-CBT condition at subsequent assessments. This procedure may also have desensitized adolescents in the F-CBT arm to reporting self-harm acts with little to no suicidal intent as SAs.
In the present study, data on type of outpatient therapeutic approach received was not obtained so we cannot rule out the possibility that adolescents in E-TAU received some form of CBT or DBT. Indeed, a survey of 86 mental health providers in the same local community found that 70% of psychiatrists, 86% of social workers, and 90% of psychologists reported CBT techniques as their most common treatment approach (Spirito et al, 2011). Further, the psychiatric inpatient unit, and to a lesser extent the step-down partial hospitalization program, that participants were recruited from taught CBT and DBT skills to patients, and did comprehensive safety planning with both adolescents and parents, prior to discharge. Exposure to CBT and/or DBT skills is likely weaker in other studies that used an active study-provided comparator treatment, such as IGST in McCauley et al. (2018).
Though all adolescents improved in depressive symptoms, there was an uptick in symptoms between 12 and 18 months in the F-CBT, but not the E-TAU arm. However, the mean for depressive symptoms across arms fell below the clinically elevated range on the CDI-2. Nonetheless, one potential reason for this increase was that after 12 months, the research protocol required that all F-CBT participants still in treatment terminate the trial and be transferred to a community therapist. This research procedure may make sense when single symptom, low acuity patients are the focus of treatment trials. However, with more severe psychiatrically impaired patients, this approach does not match the chronicity of the symptomatology or the potential iatrogenic effects of switching therapists at 12 months.
There are several limitations to this study. We did not analyze the contribution of psychotropic medication to outcomes due to the great heterogeneity of both medications prescribed and adherence to these medications. Second, we did not interview therapists in the E-TAU condition to accurately assess type of treatment received by adolescents in E-TAU and thus there may have been significant overlap in intervention content across conditions. Last, the adolescent sample included in this study was all primarily recruited from a psychiatric inpatient unit, most presenting with very high levels of psychopathology and complex family difficulties, and thus our results may not be generalizable to families who only require outpatient care.
Conclusion
Adolescents across conditions in this trial achieved reductions in rates of SAs, depression, SI, and NSSI over the course of 18 months. Although about 20% of the entire sample reported suicide attempts at the 6-month follow-up, over 70% of SAs caused no to minor physical damage and did not require medical care. In addition, there is some evidence that outcomes for E-TAU in the present study were stronger than that found in other studies. To better accommodate the current clinical severity and heterogeneity of adolescents discharged from inpatient care, a proportion of F-CBT patients may benefit from more frequent outpatient sessions, particularly at the start of the protocol. An alternative approach to transitioning to clinical care after discontinuation of the research protocol at 12 months may also be necessary to prevent potential iatrogenic effects of the research protocol on patient safety and outcomes.
Supplementary Material
Key Points.
Rates of psychiatric hospitalizations for adolescent suicidal behavior have increased dramatically over the past decade
Clinical trials for adolescent suicidal behavior are limited, in general, and in particular, for adolescents following discharge from psychiatric hospitalization
There was no evidence for efficacy of an intensive Family-Focused (F-CBT) protocol relative to enhanced care delivered by mental health providers in the community.
Adolescents across arms showed reductions in suicide attempts, depression, suicidal ideation, and NSSI over an 18-month period.
Acknowledgements
This research was supported by a grant from the National Institute of Mental Health (1R01MH097703) awarded to the first and last authors.
Footnotes
Supporting information
Additional Supporting Information may be found in the online version of this article:
Conflict of interest statement: No conflicts declared.
The authors have declared that they have no competing or potential conflicts of interest.
References
- Asarnow JR, Berk M, Hughes JL, & Anderson NL (2017). The SAFETY Program: A treatment-development trial of a cognitive-behavioral family treatment for adolescent suicide attempters. Journal of Clinical Child and Adolescent Psychology, 44, 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns B, Angold A, Magruder-Habib K, Costello E, Patrick M (1997). Child and Adolescent Services Assessment (version 4.2). Durham, NC: Duke University. [Google Scholar]
- Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System (WISQARS). Atlanta, GA: Centers for Disease Control and Prevention; 2017. http://www.cdc.gov/injury/wisqars/LeadingCauses.html [Google Scholar]
- Cigularov K, Chen PY, Thurber BW, & Stallones L (2008). What prevents adolescents from seeking help after a suicide education program? Suicide and Life-Threatening Behavior, 38, 74–86. [DOI] [PubMed] [Google Scholar]
- Curtin SC, Hedegaard H, Minino AM, Warner M QuickStats: Death rates for motor vehicle traffic injury, suicide, and homicide among children and adolescents aged 10–14 years — United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2016;65. [DOI] [PubMed] [Google Scholar]
- Donaldson D, Spirito A, & Esposito C (2005). Treatment for adolescents following a suicide attempt: Results of a pilot trial. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 113–20. [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, & Monti P (2011). Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized trial. Journal of Consulting and Clinical Psychology, 79, 728–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer EM, Angold A, Burns B, & Costello EJ (1994). Reliability of self-reported service use: test-retest consistency of children’s responses to the Child and Adolescent Services Assessment (CASA). Journal of Child and Family Studies, 3, 307–325. [Google Scholar]
- Greene JM, Wood AJ, Kerfoot MJ, Trainor G, Roberts C, Rothwell J, Woodham A, Ayodeji E, Barrett B, Byford S, & Harrington R (2011). Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ, 342: d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazell P, Martin G, McGill K, Kay T, Wood A, Trainor G, & Harrington R (2009). Group therapy for repeated deliberate self-harm in adolescents: Failure of replication of a randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 662–670. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Bormaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N (1997). Schedule for affective disorders and schizophrenia for school-aged children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kovacs M (2011). Children’s Depression Inventory 2 (CDI 2) (2nd ed.). North Tonawanda, NY: Multi-Health Systems Inc, 2010 [Google Scholar]
- McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, Avina C, Hughes J, Harned M, Gallop R, Linehand MM (2018). Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry, 75, 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Brown MZ, Heard HL, & Wagner A (2006). Suicide Attempt Self-Injury Interview (SASII): Development, reliability, and validity of a scale to assess suicide attempts and intentional self-Injury. Psychological Assessment, 18, 303–312. [DOI] [PubMed] [Google Scholar]
- Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, … Grøholt B (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: A randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53, 1082–1091. [DOI] [PubMed] [Google Scholar]
- Mehlum L, Ramberg M, Tørmoen AJ, Haga E, Diep LM, Stanley BH, … Grøholt B (2016). Dialectical behavior therapy compared with enhanced usual care for adolescents with repeated suicidal and self-harming behavior: Outcomes over a one-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 295–300. [DOI] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychological Assessment, 19, 309–317 [DOI] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 97–107e2. [DOI] [PubMed] [Google Scholar]
- Plemmons G, Hall M, Doupnik S, Gay J, Brown C, Browning W, Casey R, Freundlich K, Johnson DP, Lind C, Rehm K, Thomas S, Williams D (2018). Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics, 141, e20172426. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, & Mann JJ (2011). The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry, 168, 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds WM (1987). Suicidal Ideation Questionnaire. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Rossouw TI, & Fonagy P (2012). Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 51, 1304–1313. [DOI] [PubMed] [Google Scholar]
- Spirito A, Abebe K, Iyengar S, Brent D, Vitiello B, Clarke G, Wagner K Asarnow J, Emslie G, & Keller M (2009). Sources of site differences in the efficacy of a multi-site clinical trial: The Treatment of SSRI-Resistant Depression in Adolescents. Journal of Consulting and Clinical Psychology, 77, 439–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spirito A, Simon V, Cancilliere MK, Stein R, Norcott C, Loranger K, & Prinstein MJ (2011). Outpatient psychotherapy practice with adolescents following psychiatric hospitalization for suicide ideation or a suicide attempt. Clinical Child Psychology and Psychiatry, 16, 53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP & Del Boca FK (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Supplement No. 12, 70–75. [DOI] [PubMed] [Google Scholar]
- Wood A, Trainor G, Rothwell J, Moore A, & Harrington R (2001). Randomized trial of group therapy for repeated deliberate self-harm in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1246–1253. [DOI] [PubMed] [Google Scholar]
- Young J & Beck AT (1980). Cognitive Therapy Rating Scale manual. Unpublished manuscript, University of Pennsylvania, Philadelphia. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


