Abstract
Background
Children with developmental speech sound disorders have difficulties in producing the speech sounds of their native language. These speech difficulties could be due to structural, sensory or neurophysiological causes (e.g. hearing impairment), but more often the cause of the problem is unknown. One treatment approach used by speech‐language therapists/pathologists is non‐speech oral motor treatment (NSOMT). NSOMTs are non‐speech activities that aim to stimulate or improve speech production and treat specific speech errors. For example, using exercises such as smiling, pursing, blowing into horns, blowing bubbles, and lip massage to target lip mobility for the production of speech sounds involving the lips, such as /p/, /b/, and /m/. The efficacy of this treatment approach is controversial, and evidence regarding the efficacy of NSOMTs needs to be examined.
Objectives
To assess the efficacy of non‐speech oral motor treatment (NSOMT) in treating children with developmental speech sound disorders who have speech errors.
Search methods
In April 2014 we searched the Cochrane Central Register of Controlled Trials (CENTRAL), Ovid MEDLINE (R) and Ovid MEDLINE In‐Process & Other Non‐Indexed Citations, EMBASE, Education Resources Information Center (ERIC), PsycINFO and 11 other databases. We also searched five trial and research registers, checked the reference lists of relevant titles identified by the search and contacted researchers to identify other possible published and unpublished studies.
Selection criteria
Randomised and quasi‐randomised controlled trials that compared (1) NSOMT versus placebo or control; and (2) NSOMT as adjunctive treatment or speech intervention versus speech intervention alone, for children aged three to 16 years with developmental speech sound disorders, as judged by a speech and language therapist. Individuals with an intellectual disability (e.g. Down syndrome) or a physical disability were not excluded.
Data collection and analysis
The Trials Search Co‐ordinator of the Cochrane Developmental, Psychosocial and Learning Problems Group and one review author ran the searches. Two review authors independently screened titles and abstracts to eliminate irrelevant studies, extracted data from the included studies and assessed risk of bias in each of these studies. In cases of ambiguity or information missing from the paper, we contacted trial authors.
Main results
This review identified three studies (from four reports) involving a total of 22 children that investigated the efficacy of NSOMT as adjunctive treatment to conventional speech intervention versus conventional speech intervention for children with speech sound disorders. One study, a randomised controlled trial (RCT), included four boys aged seven years one month to nine years six months ‐ all had speech sound disorders, and two had additional conditions (one was diagnosed as "communication impaired" and the other as "multiply disabled"). Of the two quasi‐randomised controlled trials, one included 10 children (six boys and four girls), aged five years eight months to six years nine months, with speech sound disorders as a result of tongue thrust, and the other study included eight children (four boys and four girls), aged three to six years, with moderate to severe articulation disorder only. Two studies did not find NSOMT as adjunctive treatment to be more effective than conventional speech intervention alone, as both intervention and control groups made similar improvements in articulation after receiving treatments. One study reported a change in postintervention articulation test results but used an inappropriate statistical test and did not report the results clearly. None of the included studies examined the effects of NSOMTs on any other primary outcomes, such as speech intelligibility, speech physiology and adverse effects, or on any of the secondary outcomes such as listener acceptability.
The RCT was judged at low risk for selection bias. The two quasi‐randomised trials used randomisation but did not report the method for generating the random sequence and were judged as having unclear risk of selection bias. The three included studies were deemed to have high risk of performance bias as, given the nature of the intervention, blinding of participants was not possible. Only one study implemented blinding of outcome assessment and was at low risk for detection bias. One study showed high risk of other bias as the baseline characteristics of participants seemed to be unequal. The sample size of each of the included studies was very small, which means it is highly likely that participants in these studies were not representative of its target population. In the light of these serious limitations in methodology, the overall quality of the evidence provided by the included trials is judged to be low. Therefore, further research is very likely to have an important impact on our confidence in the estimate of treatment effect and is likely to change the estimate.
Authors' conclusions
The three included studies were small in scale and had a number of serious methodological limitations. In addition, they covered limited types of NSOMTs for treating children with speech sound disorders of unknown origin with the sounds /s/ and /z/. Hence, we judged the overall applicability of the evidence as limited and incomplete. Results of this review are consistent with those of previous reviews: Currently no strong evidence suggests that NSOMTs are an effective treatment or an effective adjunctive treatment for children with developmental speech sound disorders. Lack of strong evidence regarding the treatment efficacy of NSOMTs has implications for clinicians when they make decisions in relation to treatment plans. Well‐designed research is needed to carefully investigate NSOMT as a type of treatment for children with speech sound disorders.
Plain language summary
Non‐speech oral motor treatment for children with developmental speech sound disorders
Review question
We reviewed the evidence on the effects of non‐speech oral motor treatment (NSOMT) for treating children with developmental speech sound disorders who have speech errors.
Background
Children with developmental speech sound disorders have difficulties in producing the speech sounds of their own language. These speech difficulties could be due to structural, sensory or neurophysiological causes (e.g. hearing impairment), but more often the cause of the problem is unknown. One treatment approach used by speech and language therapists or pathologists consists of non‐speech oral motor treatments (NSOMTs). NSOMTs are activities that aim to stimulate or improve speech production and treat children with specific speech errors without requiring that the child produce a speech sound. This method of therapy uses exercises, such as smiling, pursing, blowing into horns and blowing bubbles and performing lip massage to target lip mobility for the production of speech sounds involving the lips, such as /p/, /b/ and /m/. Whether NSOMTs are effective for treating children with speech errors is controversial. Therefore, evidence regarding the effects of NSOMTs must be examined.
Study characteristics
The evidence is current to April 2014. We found three studies (from four reports) involving a total of 22 children aged three to nine years who received a combination of NSOMTs and articulation or phonological therapy (intervention group), or articulation or phonological therapy alone (control group). One study was a randomised controlled trial in which four boys with speech sound disorders were randomly assigned to one of the two groups. In this study, each participant received 16 × 30‐minute individual therapy sessions, twice per week over eight weeks, to treat the speech sound 's'. For the intervention group, NSOMT (oral placement therapy) was conducted in the first 10 minutes of each session, followed by 20‐minute articulation therapy. The other two studies used randomisation, but the method used to generate the random sequence was not reported. In one of these studies, six boys and four girls, all with speech sound disorders due to tongue thrust, were randomly assigned to one of the two groups. Each participant received 22 × 30‐minute individual sessions conducted weekly in the first six weeks, and twice a week in the following eight weeks, to treat 's' and 'z' sounds. The intervention group received NSOMT (Hanson's 1977 approach) in the first six weeks and alternating sessions of NSOMT and articulation therapy in the following eight weeks. The final study randomly assigned four boys and four girls with moderate to severe articulation disorder alone to either intervention group or control group. Each participant received 9 × 20‐minute group therapy sessions (two participants in each group), conducted twice a week over five weeks. For the intervention group, NSOMT (oral motor exercises for speech clarity) was conducted during the first 10 minutes of each session. Speech errors associated with the 's' sound were treated for the intervention group; however, the speech sound(s) treated for the control group were not detailed. None of the studies reported funding support.
Key results
Two studies (one that used oral placement therapy and one that used Hanson's 1977 approach) did not find NSOMT as an adjunctive treatment to be more effective than conventional speech intervention only, as both intervention and control groups had made similar improvements in articulation after treatment (i.e. fewer speech errors or increased percentage of correct articulation). The study that used oral motor exercises for speech clarity as the NSOMT reported a change in articulation test results after treatment, but used an inappropriate statistical test and did not report the results clearly.
Quality of the evidence
The three included studies were small in scale and had a number of serious methodological limitations. Moreover, these studies covered limited types of NSOMTs for treating just one class of speech sounds ‐ 's' with or without 'z' ‐ in children with speech sound disorders. Hence, the overall applicability of the evidence is limited, and the evidence is believed to be incomplete and of low quality. To conclude, currently no strong evidence indicates whether NSOMTs are effective as treatment or adjunctive treatment for children with developmental speech sound disorders.
Background
Description of the condition
'Developmental speech sound disorders' is a generic term that refers to "any combination of difficulties with perception, articulation/motor production, and/or phonological representation of speech segments (consonants and vowels), phonotactics (syllable and word shapes), and prosody (lexical and grammatical tones, rhythm, stress, and intonation) that may impact speech intelligibility and acceptability" in children (IEPMCS 2012, p 1). These speech difficulties can reflect a secondary impact of a structural deficit of the articulators (e.g. cleft palate), a sensory or motor disorder (e.g. hearing impairment) or a neuromuscular disorder (e.g. dysarthria, apraxia of speech). Alternatively, they may indicate a primary disorder for which the cause is unknown (Flipsen 2009; IEPMCS 2012; Ruscello 2008a; Shriberg 2010). Speech sound disorders can have damaging effects on many aspects of life. Speech problems can hamper daily communication, causing difficulties in socialisation. It has been reported that some forms of speech sound disorders are associated with difficulties in reading, writing, spelling and mathematics, and it has been estimated that about 50% to 70% of children with speech sound disorders show general academic difficulty throughout secondary education (see Williams 2010). Academic difficulties may affect employment later in adulthood. Thus, the impact of speech sound disorders can be manifold and long‐lasting for the affected individual.
Speech sound disorders are common in children. It has been estimated that around 7.5% of children between three and 11 years of age have clinically significant speech difficulties (Shriberg 1994). Children with developmental speech sound disorders account for a large proportion of the caseloads of speech and language therapists (SLTs) ‐ nearly half of a typical caseload for clinicians in the UK and Australia (see Joffe 2008). In the US, it has been estimated that about 80% of children with speech sound disorders require treatment services and about 92% of school‐based speech‐language pathologists provide treatment services to children with speech sound disorders (see Ruscello 2008a).
Description of the intervention
Phonetic and phonemic treatments
Different treatment approaches for managing speech sound disorders have been developed; they can be categorised broadly into phonetic (or sensory motor‐based) treatments, phonemic (or conceptual‐based) treatments and hybrid treatments that incorporate both phonetic and phonemic components (Ruscello 2008b). Phonetic treatments focus on improving the accuracy of articulatory movements for speech sounds through different levels of practice, from an isolated sound level to attain correct target sound production, to nonsense syllables, words, phrases and finally conversational speech (Ruscello 2008a; Ruscello 2008b). For phonemic treatments, the aim is to restructure or develop the child’s phonological knowledge through different types of contrastive practice (e.g. minimal pairs) or metalinguistic awareness tasks (e.g. metaphon), or both (Ruscello 2008a; Ruscello 2008b). Hybrid treatments consist of a combination of phonetic and phonemic treatments in which both phonetic practice and phonemic contrast are employed (Ruscello 2008a).
Clinical decisions about which treatment approach should be adopted for a particular child are based mainly on the cause of the speech disorder. For example, phonetic approaches, which focus on developing the child’s motor skills, are usually applied for those who have knowledge of phonological rules of the language but are unable to produce certain speech sounds correctly. Speech therapy using phonetic, phonemic or a combination of these approaches is regarded as standard speech intervention.
Non‐speech oral motor exercises
One alternate or adjunctive (i.e. additional to a phonetic or phonemic approach) approach for managing developmental speech sound disorder consists of non‐speech oral motor treatments (NSOMTs). An operational definition of NSOMTs is provided by the National Center for Evidence‐Based Practice in Communication Disorders of the American Speech‐Language‐Hearing Association (ASHA), which defines NSOMTs as "non‐speech activities that involve sensory stimulation to or actions of the lips, jaw, tongue, soft palate, larynx, and respiratory muscles that are intended to influence the physiological underpinnings of the oropharyngeal mechanism to improve its function. They may include activities described as active muscle exercise, muscle stretching, passive exercise, or sensory stimulation" (McCauley 2009, p 344).
NSOMTs are different from phonetic and phonemic treatments in that they do not involve the practice of speech sound articulation and auditory discrimination of the error sound and the target sound. Instead, they target non‐speech sensory or motor function, or both, and postures of articulators, with the aim of developing motor skills for correct speech sound production (Ruscello 2008a). For example, motor skills developed by exercising the lips in non‐speech activities, such as blowing horns, straws and bubbles, are thought to generalise to those required for production of bilabial speech sounds /p/, /b/ and /m/ (Marshalla 2000; Rosenfeld‐Johnson 2001). The paper by Ruscello 2008b provides a detailed overview of various types of NSOMTs.
NSOMTs are used in a variety of ways and for different client groups. A survey conducted in the US revealed that most clinicians ‐ 68% of 537 respondents ‐ used NSOMTs as an adjunctive 'warm‐up' technique followed by speech intervention (Lof 2008). About 25% of clinicians used NSOMTs in conjunction with speech intervention and 7% used NSOMTs exclusively to target speech production (Lof 2008). The survey also showed that clinicians often used NSOMTs with children who present with motor speech disorders, structural anomalies (e.g. cleft palate) or Down syndrome (Lof 2008). They used NSOMTs, albeit less frequently, with children identified as late talkers and those with phonological disorders, hearing impairment and speech sound disorders of unknown origin (Lof 2008). A survey conducted in Canada reported slightly different findings. There, clinicians are most likely to use NSOMTs with children exhibiting phonological disorders, apraxia of speech, dysarthria, Down syndrome or cerebral palsy (Hodge 2005b). In the UK, an unexpected finding was that NSOMTs are used more often by inexperienced therapists (one to three years) than by very experienced therapists (over 10 years) (Joffe 2008).
How the intervention might work
The use of NSOMTs for treating children with speech sound disorders is motivated by several assumptions (for details, see, for example, Bunton 2008; Clark 2010; and Ruscello 2008b). One assumption is that there is a common set of motor control principles and neural anatomical representation in the human nervous system for speech and non‐speech activities that involve the same structures. Hence, for example, movement characteristics and task demands for the production of bilabial speech sounds and those for blowing bubbles or horns are presumably similar, and the training effect caused by practising blowing bubbles or horns could be transferred to the production of bilabial sounds. Another assumption is based on the principles of motor learning, which suggest that learning could be facilitated by breaking down complex movements into subcomponents because this allows "the motor system to plan simpler movement patterns and gradually develop skilled control of more complex movement patterns" (Clark 2010, p 586). Hence, for example, to treat a child with a speech error for the sound /s/, exercises for establishing jaw stability, tongue stability, elevation of the lateral sides of the tongue, elevation of the tip of the tongue and so on are used (Marshalla 2000).
Why it is important to do this review
An abundance of commercial products and training workshops are available for NSOMTs; many clinicians use this approach for treating children with developmental speech sound disorders. For example, a survey conducted in the US in 2008 found that 85% of respondents reported using NSOMTs in their clinical practice (Lof 2008). However, use of this treatment approach in the US seems to be declining, as a recent survey reported that only 67% of respondents used NSOMTs with their clients (Brumbaugh 2013). (Similar surveys have been conducted in other countries; see Hodge 2005b; Joffe 2008; McLeod 2014.) Nevertheless, the use of NSOMTs for treating children with speech sound disorders is controversial. A number of research papers, book chapters and journal articles have discussed the theoretical reasons why NSOMTs might not be effective. See, for example, the clinical forum on NSOMTs published in the journal, Language, Speech, and Hearing Services in Schools (2008, volume 39, issue 3); a special issue, 'Controversies surrounding nonspeech oral motor exercises for childhood speech disorders', published in the journal Seminars in Speech and Language (2008, volume 29, issue 4); and other articles (e.g. Bowen 2005; Lof 2009; Lof 2010). Lof and Watson (Lof 2010) summarised the arguments about why NSOMTs do not work. First, isolated training of individual speech movements will not generalise to the whole articulatory gesture. Second, NSOMTs are not useful for improving muscle strength because it has been shown that high muscular strength is not required for producing speech. Moreover, reduced speech intelligibility and speech sound errors are not caused by reduced muscular strength of the articulators. Third, previous studies have demonstrated that neural organisation for speech and non‐speech tasks is different, even though the same oral structures are involved in those speech and non‐speech tasks. Fourth, NSOMTs for the purpose of warming up muscles or increasing children's awareness of their articulators are not useful or necessary because speaking does not tax the muscular system.
Although several research papers have discussed or reviewed the efficacy of NSOMTs (Forrest 2002; Lass 2008; Lof 2003; McCauley 2009; Ruscello 2008b; Ruscello 2008c; Ruscello 2010), the reviews were not conducted according to the standards set by The Cochrane Collaboration ‐ the types of studies reviewed were not limited to randomised clinical trials (RCTs) and quasi‐RCTs; only studies published in English were included for review; and the literature search was limited to databases that encompassed peer‐reviewed journals. Cochrane systematic reviews have examined the efficacy of speech intervention for speech problems related to childhood apraxia of speech (Morgan 2008a), dysarthria associated with acquired brain injury (Morgan 2008b) and primary speech and language delay or disorder (Law 2003). These reviews compared NSOMTs versus standard speech intervention and evaluated treatment efficacy for three levels of outcomes. However, it is uncertain whether factors such as frequency of therapy sessions and presence or absence of intellectual disability could affect the treatment efficacy of NSOMTs. Although some overlap may be seen with these systematic reviews, this review will cover a broader spectrum of developmental conditions and consequently will provide a more detailed evaluation of the treatment efficacy of NSOMTs.
Given the high incidence of speech sound disorders and the abundance of commercial products and training workshops developed for use with NSOMTs (Kamhi 2008), evidence regarding the efficacy of NSOMTs must be examined, so that clinicians can make informed decisions to ensure evidence‐based practice in their treatment plans. Moreover, patients and their families need to be made aware of the evidence related to efficacy, or lack thereof, for treatments that involve NSOMTs.
Objectives
To assess the efficacy of non‐speech oral motor treatment (NSOMT) in treating children with developmental speech sound disorders who have speech errors.
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised and quasi‐randomised controlled trials (e.g. studies in which participants were allocated to treatment by alternate allocation or allocation by date of birth). We excluded trials using a cross‐over design. This research design generally is not suitable for interventions that cause a permanent change in behaviour (e.g. reduced speech errors, improved articulation after speech intervention), as the effect of one treatment may carry over and alter the response to subsequent treatment (Sibbald 1998).
Types of participants
Children aged three to 16 years with developmental speech sound disorders, as judged by a speech‐language therapist. We did not exclude individuals with an intellectual disability (e.g. Down syndrome) or a physical disability.
Types of interventions
Non‐speech oral motor treatment (NSOMT) versus treatment with placebo or control; and NSOMT as adjunctive treatment, for example, speech intervention with NSOMT compared with speech intervention alone. We placed no restriction on the frequency, intensity or duration of the intervention.
Types of outcome measures
Primary outcomes
Although NSOMTs target non‐speech behaviours, this treatment approach is assumed to have a positive effect on speech. Hence, we included the following speech primary outcomes.
Correct articulation of speech sounds targeted by the treatment as measured by standardised tests (e.g. Goldman‐Fristoe Test of Articulation Second Edition (GFTA‐2) (Goldman 2000)) or non‐standardised articulation tests (e.g. percentage of correct speech sounds produced as determined by perceptual evaluation of articulation).
Speech intelligibility measured using a perceptual rating scale or percentage of words transcribed correctly by the investigator.
Speech physiology as measured by instrumental techniques such as acoustic analysis (e.g. measure of format frequencies for assessing vowel production), kinematic analysis and articulatory placement.
Adverse effect of an increase in articulation errors after treatment, which could be measured by the standardised and non‐standardised tests listed above. These articulation tests should be conducted by a speech‐language therapist (SLT).
We planned to include all primary outcomes in a 'Summary of findings' table.
Secondary outcomes
Listener acceptability, speech naturalness or bizarreness (e.g. as judged by a naive listener using a perceptual rating).
Self perception of change in articulation or speech intelligibility (e.g. as measured using a rating scale).
Time points for measuring outcomes
Immediately (within one month) after cessation of the intervention.
One to 12 months after cessation of the intervention.
One to two years after cessation of the intervention.
Search methods for identification of studies
The Trials Search Co‐ordinator for the Cochrane Developmental, Psychosocial and Learning Problems Group and one review author (AL) ran the searches in August 2012. The searches were updated in February 2013 and again in April 2014.
Electronic searches
We searched the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL) (2014 Issue 3).
Ovid MEDLINE (R), 1946 to April Week 1 2014.
Ovid MEDLINE In‐Process & Other Non‐index Citations, 14 April 2014.
EMBASE (Ovid), 1980 to Week 15 2014.
Education Resources Information Center (ERIC) (ProQuest), 1966 to current.
PsyINFO (Ovid), 1806 to April Week 2 2014.
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOhost), 1939 to current.
Science Citation Index‐Expanded (SCI‐EXPANDED) (Web of Knowledge), 1970 to 11 April 2014.
Social Science Citation Index (SSCI) (Web of Knowledge), 1970 to 11 April 2014.
Conference Proceedings Citation Index‐Sciences (CPCI‐S); Conference Proceedings Citation Index‐Social Sciences & Humanities (CPCI‐SSH), 1990 to 11 April 2014.
Latin American Caribbean Health Sciences Literature (LILACS), all available years.
Academic Search Complete (EBSCOhost), all available years.
ProQuest Dissertations and Theses: UK & Ireland, 1990 to current.
ProQuest Dissertations and Theses, Abstracts International (AI), 1970 to current.
Cochrane Database of Systematic Reviews (CDSR) (2014 Issue 4).
Database of Abstracts of Reviews of Effects (DARE) (2014 Issue 1).
speechBITE, www.speechbite.com/: all available years.
We also searched the following trials registers.
National Research Register Archive (last modified 27 October 2010 ) (nihr.ac.uk/Pages/NRRArchive.aspx).
UK Clinical Research Network (UKCRN) Portfolio Database (public.ukcrn.org.uk/search/).
ClinicalTrials.gov (clinicaltrials.gov/).
metaRegister of Controlled Trials (mRCT) (controlled‐trials.com).
World Health Organization International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/default.aspx).
We applied no restrictions to language, date or status of publication. We planned to seek translation when necessary; however, all included studies were written in English, so translation was not needed. The search strategies are detailed in Appendix 1.
Searching other resources
We checked the reference lists of relevant journal papers, book chapters and systematic reviews identified by the electronic searches. We emailed colleagues and researchers to identify other published and unpublished studies for possible inclusion such as technical or research reports, conference papers and dissertations.
Data collection and analysis
Selection of studies
We managed all references generated by the search strategy using Endnote (Endnote). We eliminated duplicates. Two review authors (AL and FG) independently conducted an initial screening of titles and abstracts to exclude references that did not meet the inclusion criteria. We obtained full papers for those that provided insufficient information in the abstract. These two review authors independently evaluated the papers and resolved disagreements by discussion.
Data extraction and management
A data extraction form was developed and piloted before data extraction was carried out. Two review authors (AL and FG) independently extracted the following information from each paper.
Participants: number, age, sex, inclusion and exclusion criteria, severity level of developmental speech sound disorders and other baseline characteristics reported (e.g. hearing ability, intellectual disability).
Methods: speech assessment(s), outcome measure(s) used and assessment results (e.g. numbers and types of articulation errors).
Interventions: types of interventions, number of therapy sessions given, duration of each therapy session, frequency of therapy and length of intervention, date and location and whether compliance was evaluated.
Intervention integrity: Using the coding categories proposed by Dane and Schneider (Dane 1998), we recorded, for example, whether a training manual outlining the intervention procedures was available to intervention provider(s), and whether the intervention provider(s) was given specific training regarding implementation of intervention procedures.
Assessment of risk of bias in included studies
Two review authors (AL and FG) independently assessed risk of bias in each included study across the following six domains according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This assessment consisted of two parts: (1) a succinct description, which included verbatim quotes from the paper or correspondence with the trial author(s), a comment from the review author about procedures used to avoid bias, or both; and (2) an assessment of risk of bias (resulting in assignment of a judgement of ‘low risk’, ‘high risk’ or ‘unclear risk’ of bias) for each of the domains described below. Studies that were judged as ‘high risk’ for each area of potential risk of bias were not included in subsequent analyses.
Sequence generation
Review authors described the method used to generate the allocation sequence using quotes when possible. They added a comment such as ‘probably done’ or ‘probably not done’ to supplement any ambiguous quote and assigned each included study to one of the following categories.
‘Low risk’ ‐ adequate method used for randomisation (e.g. computer generated, table of random numbers) or quasi‐randomisation.
‘High risk’ ‐ inadequate method of randomisation used (e.g. case file number, date of birth, alternate numbers).
‘Unclear risk’ ‐ uncertainty about whether an appropriate method of randomisation was used.
Allocation concealment
As regards the method used to conceal the allocation sequence, we assigned each included study to one of the following categories.
‘Low risk’ ‐ adequate concealment of allocation (e.g. pre‐numbered or coded identical containers administered serially to participants).
‘High risk’ ‐ allocation not adequately concealed (e.g. alternate assignment).
‘Unclear risk’ ‐ uncertainty about whether allocation was adequately concealed (e.g. study authors did not describe allocation methods).
Blinding
Blinding of participants and intervention providers (i.e. the SLTs) was not possible, but blinding of outcome assessor(s) and data analyst(s) from knowledge of which intervention a participant had received should have been ensured. Review authors evaluated and graded the method used to ensure blinding as ‘low risk’, ‘high risk’ or ‘unclear risk’ of bias. We performed assessment for each main outcome (e.g. outcome measured at six months post therapy, outcome measured at 12 months post therapy).
Incomplete outcome data
'Incomplete outcome data' refers to data that are missing as a result of attrition (dropout) during the study or exclusion from the analysis. We noted the numbers of, and reason(s) for, attrition or exclusions, and whether attrition was analysed appropriately (e.g. intention‐to‐treat (ITT) analysis). We graded this domain as having ‘low risk’, ‘high risk’ or ‘unclear risk’ of bias according to the criteria stated in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Selective reporting bias
This is also known as 'within‐study publication bias', which may arise in several ways (Higgins 2011).
Only some of the analysed outcomes were included in the study.
Outcomes were measured at different time points, or different instruments or assessors were employed to measure outcomes at the same time point.
Selective reporting of analysis was performed using the same data.
Results of subscales of a full measurement scale or a subset of events were selectively reported.
Some outcomes were reported but with inadequate detail for the data to be included in a meta‐analysis.
We assigned each included study to one of the following quality criteria.
‘Low risk’ indicating that studies have reported all prespecified outcomes.
‘High risk’ indicating that any of the above‐mentioned selective reporting is evident in the study.
‘Unclear risk’ indicating that it is uncertain whether selective reporting bias has been avoided.
Other sources of bias
Other sources of bias may include baseline imbalance, early stopping and co‐intervention. We described the nature of the bias and graded this domain as having ‘low risk’, ‘high risk’ or ‘unclear risk’ of bias.
Measures of treatment effect
We did not carry out further quantitative analysis of the data, as the three identified trials used different NSOMTs and outcome measures (see the 'Interventions' and 'Outcomes' subsections in the Results section below). Thus, methods planned in the protocol (Lee 2011) were not used in this review but will be used in updates of this review (see Table 1).
1. Methods planned in the protocol but not used in this review.
| Issue | Method |
| Measures of treatment effect |
Binary and categorical data Binary data (e.g. articulation improved vs no change) are likely. We will analyse the data by calculating the risk ratio (RR) Continuous data Most data from expected outcome measures, such as standardised articulation test results, articulation accuracy based on perceptual evaluation, judgement of speech intelligibility and listener acceptability, are likely to be continuous data. We will calculate the mean difference (MD, or the ‘difference in means’) when outcome measurements in all studies are made on the same scale. Otherwise, we will use standardised mean differences (SMDs) to combine studies that measured the same outcome using different methods |
| Unit of analysis issues |
Cluster‐randomised trials We may include cluster‐randomised trials in this review. In this case, appropriate statistical approaches should be used, for example, using a 2‐sample t‐test to compare the means of clusters in the intervention group vs those in the control group at cluster level, or a mixed effects linear regression approach at an individual level (Donner 2000). We will contact trial author(s) if it is unclear whether appropriate adjustments have been made (Donner 2000). When individual level data cannot be secured, we will control the data for the clustering effect by using the procedures described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For dichotomous data, we will divide the number of participants and the number experiencing the event by the design effect, 1 + (M‐1) * ICC, where M is the average cluster size and ICC is the intracluster correlation coefficient. For continuous data, we will divide the number of participants by the design effect, with means and standard deviations remaining unchanged. We will combine the results with those from individually randomised trials for meta‐analysis using the generic inverse‐variance method in RevMan when clinical heterogeneity between studies is small (Donner 2000; Higgins 2011) Multi‐arm studies For studies with more than 2 intervention groups (i.e. multi‐arm studies), we will combine groups to create a single pair‐wise comparison (Higgins 2011). We will combine all relevant experimental intervention groups to form a single group, and we will combine all relevant control groups and placebo groups to form a single control group. To avoid confusion over the nature of each study, we will mention all intervention groups of a multi‐arm study in the 'Notes' section of the Characteristics of included studies table. We will provide detailed descriptions of intervention groups relevant to the review in the 'Interventions' section of the table Cross‐over trials Cross‐over trials are not appropriate for an intervention that can have a lasting effect (Higgins 2011). Therefore, this design is not suitable for studying speech intervention, and we will not include in this review studies that applied this design |
| Dealing with missing data | We will assess missing data and dropouts for each included study and will report the reasons for and numbers and characteristics of dropouts. When possible, we will contact trial author(s) to supply the missing data and any relevant information. If the missing data appear to be missing at random (e.g. data lost because of computer problems), we will conduct an analysis on available data (Higgins 2011). However, if the data are not missing at random, we will conduct the analysis by imputing the missing data with replacement values. For dichotomous data, we will use a sensitivity analysis based on consideration of ‘best‐case’ and ‘worst‐case’ scenarios to assess the extent to which the results of the review could be altered by the missing data (Gamble 2005). The ‘best‐case’ scenario means that all participants with missing outcomes in the intervention group had good outcomes (e.g. improvement in articulation) and those with missing outcomes in the control group had poor outcomes (e.g. no improvement in articulation); the ‘worst‐case’ scenario is the reverse. For missing continuous data, we will conduct the analysis by imputing the missing data with replacement values (e.g. last observation carried forward (LOCF), mean of the treatment group) and treating these as if they were observed (Higgins 2011). We will address in the Discussion section the potential impact of missing data on the findings of the review |
| Assessment of heterogeneity | Variability in participants, interventions and outcomes between the different included studies is known as clinical heterogeneity, and variability in the intervention effects being evaluated in the included studies is known as statistical heterogeneity, or simply as heterogeneity (Higgins 2011). Clinical heterogeneity will lead to statistical heterogeneity if the intervention effect is influenced by factors such as participant characteristics (Higgins 2011). We will assess statistical heterogeneity by using the Chi2 test for heterogeneity, by visually inspecting forest plots and by using the I2 statistic (Higgins 2002; Higgins 2003). The Chi2 test assesses whether observed differences in results are compatible with chance alone (Higgins 2011). However, this test has low power if the meta‐analysis includes only a small number of studies, or if the included studies have small sample sizes. In this case, a P value of 0.10 (rather than the conventional level of 0.05) will be used to determine statistical significance (Higgins 2011). I2 is a statistic for assessing the impact of inconsistency across studies through the meta‐analysis. We will follow the rough guide to interpretation of the I2 statistic as stated in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). However, thresholds for interpretation of the I2 statistic may be misleading. We will take into account other issues, such as magnitude and direction of effects and strength of evidence for heterogeneity (e.g. the P value from the Chi2 test), when determining the importance of the observed value of the I2 statistic (Higgins 2011) |
| Assessment of reporting biases | Funnel plots (effect size vs error) will be drawn if sufficient studies are found. An asymmetrical funnel plot indicates a relationship between effect size and study size, which suggests the possibility of publication bias or a systematic difference between smaller and larger studies. If a relationship is identified, the clinical diversity of the studies will also be examined (Egger 1997) |
| Data synthesis | We will carry out a meta‐analysis using Review Manager version 5.1 (RevMan) if data are sufficient and if the interventions are similar in terms of characteristics of the participants, types of non‐speech oral motor treatments (NSOMTs) used, the schedule (e.g. frequency and duration) of the treatment and outcome measures. We will apply both a fixed‐effect model and a random‐effects model and will compare the results to assess the impact of statistical heterogeneity. We will present the results from the random‐effects model unless contraindicated (e.g. in cases of funnel plot asymmetry). In the case of serious funnel plot asymmetry, we will present both fixed‐effect and random‐effects analyses, under the assumption that asymmetry suggests that neither model is appropriate. When the same outcome is presented as dichotomous data in some studies and as continuous data in other studies, we will convert odds ratios (ORs) for the dichotomous data to standardised mean differences (SMDs) if it can be assumed that the underlying continuous measurements follow a normal or logistic distribution. Otherwise, we will conduct separate analyses Multiple time points For studies in which outcomes are measured at different time points, we will calculate the combined effect size across different time points (Borenstein 2009) |
| Subgroup analysis and investigation of heterogeneity | If sufficient homogenous studies are identified, we will conduct subgroup analyses to assess the impact of the cause of speech sound disorders (e.g. structural anomalies, neuromuscular impairment, unknown origin), intensity of therapy (to be determined by the frequency of therapy sessions), presence or absence of intellectual disability and use of NSOMTs as an adjunct to speech intervention |
| Sensitivity analysis | We will examine the impact of study quality on the robustness of conclusions by performing sensitivity analyses. Factors that are considered as important in judging study quality include randomisation, blinding to outcome assessment and attrition (Juni 2001). We will include studies that we categorised as having low or unclear risk of bias for these factors in the analysis |
| Evaluation of outcomes using the GRADE system | We will summarise the outcomes of included studies in a 'Summary of findings table'. We will grade each outcome using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (Guyatt 2008). The GRADE system classifies the quality of evidence in 1 of 4 categories: (1) high quality, when further research is very unlikely to change our confidence in the estimate of treatment effect; (2) moderate quality, when further research is likely to have an important impact on our confidence in the estimate of treatment effect and may change the estimate; (3) low quality, when further research is very likely to have an important impact on our confidence in the estimate of treatment effect and is likely to change the estimate; and (4) very low quality, when the estimate of treatment effect is very uncertain (Guyatt 2008). We will consider the following factors when grading the quality of evidence: research methodology, consistency of results, directness of evidence, precision of effect estimates and whether reporting bias is likely (Guyatt 2008). |
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies.
Results of the search
The searches identified a total of 7691 records. After removing duplicates, the two review authors (AL and FG) independently screened the titles and abstracts of 5853 records and identified 24 potentially relevant articles. We retrieved and assessed the full‐text reports for eligibility and determined that four reports met the inclusion criteria. See Figure 1 for the study flow diagram.
1.
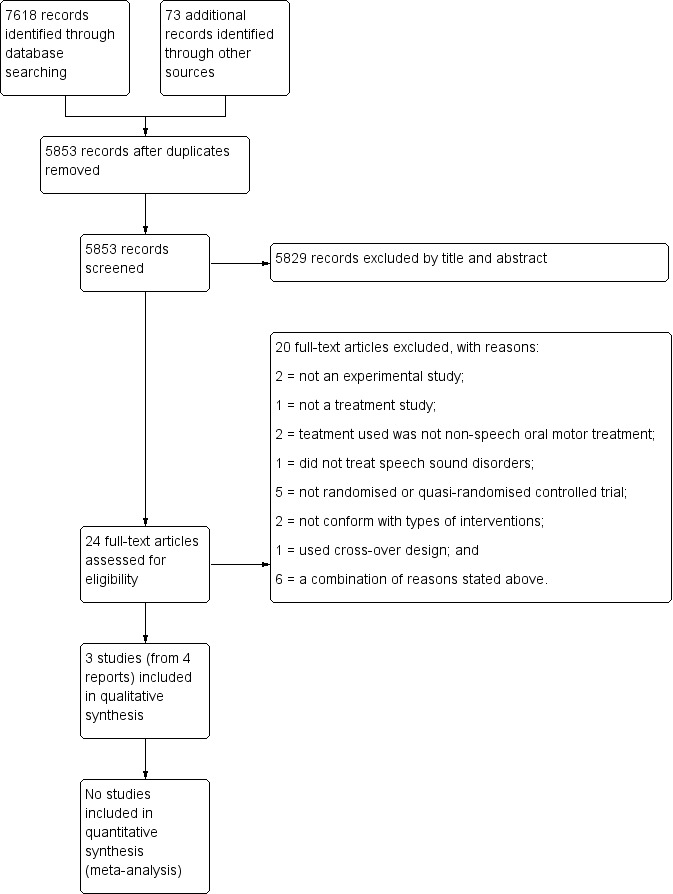
Study flow diagram.
One of the four reports is a conference paper (poster) authored by Fields and Polmanteer, which reported the same results as Fields' Master's thesis (Fields 2003). Data from Fields' study reported in this review were taken from Fields 2003, as this report included the full details of Fields' study. Hence, this review identified three relevant studies (from four reports) that investigated the efficacy of NSOMTs as adjunctive treatment to conventional speech intervention for children with speech sound disorders.
Included studies
The three included studies are Christensen 1981, Fields 2003 and Sargenti 2011. The study by Christensen and Hanson (Christensen 1981) was published in a peer‐reviewed journal. The studies by Fields (Fields 2003) and by Sargenti (Sargenti 2011) were undertaken and published as Master's theses.
Location of studies
The three included studies were conducted in the United States ‐ Salt Lake City School District, Utah, for Christensen 1981; rural eastern Kentucky for Fields 2003; and northern New Jersey for Sargenti 2011.
Participants
The study by Christensen 1981 included 10 children (six boys and four girls) aged between five years eight months and six years nine months; the study by Fields 2003 included eight children (four boys and four girls) aged between three and six years; and the study by Sargenti 2011 included four boys aged between seven years one month and nine years six months. Participants in all three studies were diagnosed as having speech sound disorders. In Christensen and Hanson's study, the 10 participants showed "visually and acoustically distorted /s/ and /z/, and two or more other dentally or interdentally produced tongue‐tip sounds" (Christensen 1981, p 162). In Fields' study, the eight participants had "moderate‐to‐severe articulation disorder" (Fields 2003, p 12). Three participants in the intervention group showed cluster reduction for /s/ clusters, and one showed stridency deletion; these errors were targeted in the NSOMTs. The study did not report other speech errors noted among participants in the intervention group, nor did it provide the details of speech errors demonstrated by participants in the control group. In Sargenti's study, the four participants showed "distorted production of /s/ and /z/ phonemes" and "an interdental (frontal) or lateral lisp" (Sargenti 2011, p 17). This study did not report other speech errors that the participants might have had or the severity level of these speech disorders.
Other participant baseline characteristics were slightly different among the three studies. In Christensen 1981 and Sargenti 2011, all participants had normal hearing, and participants in Sargenti's study also had delayed motor control (Sargenti 2011); however, participants' hearing ability and motor control ability were not reported in Fields 2003. The expressive and receptive language abilities of participants in all three studies were not fully tested; however, those in Fields 2003 were judged to be within normal limits for their receptive vocabulary. Whereas in the study by Sargenti 2011, one participant in the intervention group was diagnosed as "communication impaired" and one in the control group was classified as "multiply disabled (communication impaired, Attention Deficit Hyperactivity Disorder, Tourette Syndrome, and Obsessive‐Compulsive Disorder)" (p 17). The other two participants had "normal academic and language abilities" (p 17). For the Christensen 1981 study, "some unusual individual characteristics" were observed in four participants during the course of treatment (p 164). One participant in the intervention group did not complete the home practice because she was not compliant with it, and another participant in this group "was found to have a visual learning disability and had real difficulty using a mirror for tongue thrust exercises (the NSOMT)" (p 164). One participant in the control group showed "language disability involving syntax and semantics as well as phonology", and another participant in the same group had an anterior overjet which "made correct /s/ production difficult" (p 164).
Interventions
Christensen 1981 used "Hanson's 1977 approach" (Barrett 1978) to NSOMTs. Fields 2003 used "oral motor exercises for speech clarity" developed by Rosenfeld‐Johnson (Rosenfeld‐Johnson 2001), and Sargenti 2011 used "oral placement therapy" (OPT) for /s/ and /z/, which was also developed by Rosenfeld‐Johnson (Rosenfeld‐Johnson 2009).
Christensen 1981 provided little information on the "Hanson's 1977 approach", stating only that this programme "included the use of neuromuscular facilitation techniques" (p 162). Study authors provided no information on the activities or exercises used for treating target speech sounds.
Oral motor exercises for speech clarity (Rosenfeld‐Johnson 2001) include exercises for the jaw, lips and tongue. In the Fields' study, exercises used in the intervention were selected on the basis of the oral motor weakness identified in individual participants and the phoneme(s) that were misarticulated (Fields 2003). Hence, tongue exercises were administered to participants one and two; whereas jaw exercises were given to participants three and four. Participant one completed the four steps in the first exercise ‐ "tongue‐tip lateralisation midline to either side" ‐ and the first two steps (six steps altogether) in the second exercise ‐ "tongue‐tip lateralisation across midline". Participant two completed the four steps of the first tongue exercise and the first step of the second tongue exercise. Participants three and four completed the first two of the three steps of the "Bite Block #2" exercise.
Oral placement therapy (OPT) for /s/ and /z/ (Rosenfeld‐Johnson 2009) includes exercises for the jaw, lips and tongue, and use of the following tools: Talk Tools Jaw Grading Bite Blocks, Talk Tools Bubble Kit and Talk Tools Horn Kit, as well as a sensory programme that uses Talk Tools Vibrator/Toothettes (oral swab). In Sargenti 2011, exercises used in the intervention were selected on the basis of individual participant results on the Initial Speech System Evaluation (which comes with this treatment package). Hence, participant one went through the following exercises during the course of the intervention: bite block exercises level #2 to #7, blow bubble exercises level #3 to #5 and blow horn exercises level #2 to #12, whereas participant two went through bite block exercises level #4 to #7 and blow horn exercises level #9 to #12. Results of the Initial Speech System Evaluation revealed that both participants had "hypo‐sensitivity/responsivity" (p 22); thus, the sensory programme was administered to participants at the start of each therapy session "to increase awareness" before oral motor therapy was provided (p 26). The programme started with rubbing both sides of the buccal cavity, the upper and lower gum ridges, the surface and lateral margins of the tongue and the hard palate of the participant using a dampened Talk Tools Toothette; the procedure was repeated using a Talk Tools Vibrator. The sensory programme took about one to two minutes to complete.
In Christensen 1981, participants in both intervention and control groups initially received 1.5 to 2.5 30‐minute sessions of conventional articulation therapy targeting four sounds ‐ /t/, /d/, /l/ and /n/. After this, the intervention group received NSOMTs and conventional articulation therapy, whereas the control group received conventional articulation therapy only. In Fields 2003, the intervention group received NSOMTs as well as conventional articulation or phonological therapy, whereas the control group received conventional articulation or phonological therapy only. In Sargenti 2011, the intervention group received NSOMTs and conventional articulation therapy, whereas the control group received conventional articulation therapy only.
None of the included studies reported who delivered the intervention. In addition, two studies (Christensen 1981; Sargenti 2011) did not report whether investigators adhered to the intervention plan. As stated below, although Fields 2003 planned to conduct 10 therapy sessions, one session was not implemented for personal reasons of the trial author, who did not report whether investigators adhered to all other aspects of the intervention plan.
Duration and frequency of treatments
The frequency of treatment sessions was two sessions per week for two studies (Fields 2003; Sargenti 2011). In Christensen 1981, treatment was conducted once a week for the first six weeks and twice a week for the following eight weeks. The total number of treatment hours was different between the three studies ‐ 11 hours for Christensen and Hanson's study (22 × 30‐minute sessions), three hours for Fields' study (10 × 20‐minute sessions were planned, but one was not carried out for personal reasons of the trial author) and eight hours for Sargenti's study (16 × 30‐minute sessions) (Christensen 1981; Fields 2003; Sargenti 2011). In the studies by Fields 2003 and Sargenti 2011, the same length of time (the first 10 minutes) was allocated to NSOMTs in each therapy session. For Christensen 1981, the NSOMT was provided in the first six weeks and at every other session over the following eight weeks. The studies by Christensen 1981 and Sargenti 2011 used individual therapy, whereas the study by Fields 2003 used group therapy (two participants in each group).
Outcomes
Different tests were used as outcome measures. Christensen 1981 used the following tests for pre‐treatment and post‐treatment assessments of articulation: (1) a word repetition test for evaluating tongue‐tip placement during production of /t/, /d/, /l/, /n/, /s/ and /z/ ‐ one point for the error of dentalisation and two points for the error of interdentalisation; (2) a "clinician‐designed picture articulation test that elicited spontaneous production of 24 s‐words and 8 z‐words with the target phonemes occurring in all positions and of 7 initial s‐blends" (p 162) ‐ one point for each error (omission, substitution and distortion); and (3) GFTA First Edition (GTFA‐1) ‐ one point for each error (omission, substitution and distortion). Additional items were used for post‐treatment assessments of articulation: "(1) a sentence repetition series, including a sentence loaded with each of the tongue‐tip sounds and devoid of /ð/ and /Ɵ/ phonemes; (2) counting from 50 to 70 and describing zoo and playground pictures to elicit numerous /s/ and /z/ phonemes in conversation" (p 163), but the results were not reported.
Fields 2003 used the Structured Photographic Articulation Test‐Dudsberry (SPAT‐D; Kresheck 1989), whereas Sargenti 2011 used the "assessment of oral‐motor functions during non‐speech tasks" (Mackie 1996, p 9) and GTFA Second Edition (GFTA‐2) (Goldman 2000). Three sets of probes (each of which includes four words that contain /s/ and four that contain /z/) were developed by the trial author for tracking treatment progress for /s/ and generalisation of treatment effect for /z/ (Sargenti 2011).
Excluded studies
We excluded 20 reports for various reasons.
Two were not experimental studies (Bathel 2006; Karch 2005).
One was not a treatment study but rather was a survey on the use of NSOMTs by speech‐language pathologists in Albert, Canada, for treating children with speech disorders (Hodge 2005a).
Two did not use NSOMT for treatment (Clark 1993; Helmick 1976).
One did not treat speech sound disorders (Bacha 1999).
Five were not randomised or quasi‐randomised controlled trials (Baskervill 1976; Forrest 2008; Gommerman 1995; Guisti 2002; Guisti Braislin 2005).
Two did not conform with the types of interventions stated in the protocol (Hayes 2006; Overstake 1976).
One used a cross‐over design (Roehrig 2004).
Six were excluded for a combination of reasons as stated above. Bäckman 2003 and Bäckman 2007 were not randomised or quasi‐randomised controlled trials; they did not treat speech sound disorders and did not use NSOMT for treatment. Carlstedt 2001 and Carlstedt 2003 did not treat speech sound disorders and did not use NSOMT for treatment. Powers 1974 was not a randomised or quasi‐randomised controlled trial and did not treat speech sound disorders. Robertson 2001 was not a randomised or quasi‐randomised controlled trial, and the participants were adults, not children.
Risk of bias in included studies
Results of the 'Risk of bias' assessment are detailed in the 'Risk of bias tables' beneath the Characteristics of included studies tables. These results are also presented as percentages in the 'Risk of bias graph' (Figure 2) and are summarised in the 'Risk of bias summary' (Figure 3).
2.
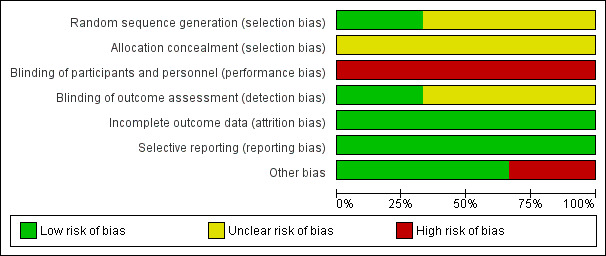
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
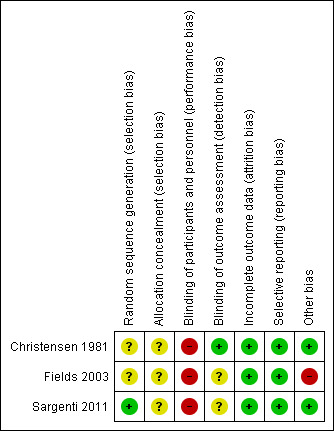
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The three included studies used randomisation in assigning participants to the intervention group and the control group; however, they used slightly different methods. In Christensen 1981, the 10 participants were randomly assigned to one of the two conditions; however, the study authors did not report how the random sequence was generated or who did it, and so we judged this study as having 'unclear' risk of selection bias. In Fields 2003, eight children were first placed into groups of two by their school‐based speech‐language pathologist (not the trial author), according to their age, disorder and individualised education plan (IEP) goals. The same school‐based speech‐language pathologist then randomly assigned groups to the intervention group or the control group (Fields 2014 [pers comm]). Study authors did not describe the person or the methods by which the random sequence was generated; therefore this study was judged as having 'unclear' risk of selection bias. Sargenti 2011 used a random number table to randomly assign the four participants to one of two groups, but did not specify who conducted the random allocation. For this reason, we judged this study as having 'low' risk of bias on random sequence generation and 'unclear' risk of bias on allocation concealment.
Blinding
Blinding of participants and of the intervention provider is not possible, given the nature of the intervention; therefore we judged all studies as having 'high' risk of performance bias. However, blinding of outcome assessors is possible and should be implemented. Only one study (Christensen 1981) employed two blinded outcome assessors; we rated this study as having 'low' risk of detection bias. The other two studies (Fields 2003; Sargenti 2011) did not identify the outcome assessor and did not report blinding of the outcome assessor; we rated these studies as having 'unclear' risk of detection bias.
Incomplete outcome data
No missing data or attrition was noted in any of the three included studies; consequently we judged all three studies as having 'low' risk of bias in this domain. Although Fields 2003 planned 10 therapy sessions, only nine were carried out because the trial author "did not implement therapy one day due to personal reasons" (p 23). All participants attended their nine therapy sessions. Participants in the other two studies (Christensen 1981; Sargenti 2011) attended all therapy sessions.
Selective reporting
All three included studies appear to be free of selective reporting bias and thus were judged as having 'low' risk of bias in this domain.
Other potential sources of bias
As regards Fields 2003, we identified the possibility of unequal baseline characteristics in the intervention group and the control group. Results of the Structured Photographic Articulation Test‐Dudsberry (SPAT‐D) before and after treatment for each participant were reported in the Master's thesis (on p 20). Scores for the four participants in the intervention group were 17, 38, 12 and 41, whereas scores for the four participants in the control group were 64, 50, 30 and 18. Although information on how to interpret these scores was not provided (e.g. it is unclear whether higher scores mean better articulation skills), the two groups seemed to show different SPAT‐D results before treatment. Therefore, we judged this study as being at 'high' risk of other bias. The other two studies (Christensen 1981; Sargenti 2011) appear to be free of other potential sources of bias; thus we judged them as having 'low' risk of bias in this domain.
Effects of interventions
All three included studies (Christensen 1981; Fields 2003; Sargenti 2011) measured the primary outcome ‐ correct articulation of speech sounds. None of the studies measured the other primary outcomes (speech intelligibility, speech physiology and adverse effects) or the secondary outcomes (listener acceptability, speech naturalness or bizarreness and self‐perception of change in articulation or speech intelligibility). We did not carry out a meta‐analysis on the primary outcome ‐ correct articulation of speech sounds ‐ because different standardised and non‐standardised tests of articulation were used in the three studies. Christensen 1981 used a standardised test of articulation (GFTA First Edition) and two non‐standardised tests of articulation; investigators compared (1) pre‐intervention and postintervention test scores for the intervention group and the control group (using the sign test), and (2) differences in pre‐intervention and postintervention test scores between the intervention group and the control group (using the Fisher exact probability test). Fields 2003 used a standardised test of articulation (SPAT‐D) and tested differences among four sets of data: (1) pre‐intervention test scores of the intervention group; (2) post‐intervention test scores of the intervention group; (3) pre‐intervention test scores of the control group and (4) postintervention test scores of the control group (using one‐way analysis of variance (ANOVA)). Sargenti 2011 used a standardised test of articulation (GFTA Second Edition) and a non‐standardised test of articulation, but researchers did not use inferential statistics to compare the intervention group against the control group, or pre‐intervention performance against postintervention performance. We describe below the results reported for each included study.
Primary outcomes
Correct articulation of speech sounds as measured by standardised and/or non‐standardised articulation test(s)
Different standardised tests were used in the three studies to assess treatment outcome. For Christensen 1981, the First Edition of the GFTA (total number of phoneme errors as assessed by the test) and two other non‐standardised tests of articulation (tongue‐tip sound placement, total number of /s/ and /z/ errors) were conducted before and after the intervention was provided. Study authors reported that results of the sign test (P value not reported) showed that "performance of both groups was significantly improved" post intervention, as measured by these three tests of articulation. In addition, results of the Fisher exact probability test (significance level at 0.05) showed "observed [pre‐ and post‐intervention test scores] differences [between the two groups] to be not significant" for each of those three outcomes (p 163).
In Fields 2003, the SPAT‐D (Kresheck 1989) was conducted before and after the intervention with participants in the intervention group and the control group. Study authors reported the following: "A one‐way Analysis of Variance revealed a significant difference between the groups, p < .05, p = .0001" (Fields 2003, p 20). In the Discussion section of the paper, study authors stated that "An ANOVA revealed a significant difference between the groups' pre‐test and post test scores..." (p 21). The report of statistical test results was ambiguous ‐ it remains unclear whether a difference between the two groups was evident in the postintervention assessment, or whether differences between pre‐intervention and postintervention performance could be seen for each group. Moreover, given the small sample size and the research design used (two‐arm pre/post study), one‐way ANOVA was not an appropriate test for assessing differences between groups and within participants.
In Sargenti 2011, investigators conducted two tests ‐ (1) "assessment of oral‐motor functions during non‐speech tasks" (Mackie 1996) and (2) GFTA‐2 (Goldman 2000) ‐ one week before and one week after the intervention was provided. In addition, they developed three sets of probes (each of which included four words that contain /s/ and four that contain /z/) for tracking treatment progress of /s/ and generalisation of treatment effect of /z/. They used probe one with all participants at the start of the first therapy session to determine the initial level of performance; they used probe two to record performance at the end of the first therapy session, and probe three to document performance at the end of the second therapy session. They assessed performance at the end of the remaining therapy sessions by alternating use of the three probes. Researchers calculated no inferential statistics to compare the intervention group against the control group, nor pre‐intervention performance against postintervention performance. The trial author reported that participants in both intervention groups and control groups "manifested more non‐speech oral tasks adequately" post intervention as judged by assessment of oral‐motor functions during non‐speech tasks (p 47). According to the results of GFTA‐2, one participant in the intervention group (C1) showed fewer articulation errors post intervention but no improvement in the treatment target /s/ and the non‐treatment target /z/. The other participant in the intervention group (C2) also showed fewer articulation errors post intervention and "achieved correct production of the targeted /s/ and the non‐targeted /z/ sounds in initial, medial and final word positions" (Sargenti 2011, p 44). One participant in the control group (T1) showed the same articulation errors post intervention, whereas the other participant (T2) showed fewer articulation errors post intervention and "achieved correct production of the targeted /s/ sound in initial, medial, and final word positions as well as the non‐targeted /z/ sound in initial and medial word positions" (Sargenti 2011, p 43). Results of the s/z probes showed that C1 in the intervention group scored zero for both /s/ and /z/ during the course of the intervention and C2 reached 100% in session 11 for /s/ and made "steady progress" for /z/ (Sargenti 2011, p 46). In the control group, T1 scored zero for both /s/ and /z/, whereas T2 reached 100% in session six for /s/ and showed "steady progress" for /z/" (Sargenti 2011, p 46).
None of the included studies provided information on effect sizes and 95% confidence intervals.
None of the included studies examined the impact of NSOMTs on the remaining primary outcomes ‐ speech intelligibility, speech physiology and adverse effects.
Secondary outcomes
None of the included studies examined the impact of NSOMTs on any of the secondary outcomes: listener acceptability, speech naturalness or bizarreness and self perception of change in articulation or speech intelligibility.
Discussion
Summary of main results
The search of the literature yielded several intervention studies that investigated the effectiveness of non‐speech oral motor treatments (NSOMTs), but only three studies (from four reports), involving 22 children, met the inclusion criteria (Christensen 1981; Fields 2003; Sargenti 2011). Sargenti 2011, a randomised controlled trial (RCT), randomly assigned participants to one of the two intervention conditions using a random number table. The other two studies (Christensen 1981; Fields 2003) stated that random allocation of participants was conducted but did not report the details of sequence generation. Hence, we judged them to be quasi‐randomised controlled trials. None of the included studies reported the method used for concealing allocation of participants; hence, we judged risk of allocation concealment as unclear for all three included studies.
We did not conduct a meta‐analysis, as the included studies used different outcome measures. The three studies showed different findings as regards the efficacy of NSOMTs for treating developmental speech sound disorders. Christensen 1981 reported differences between pre‐intervention and postintervention assessments of articulation for both intervention and control groups using the sign test (significance level not reported). However, researchers noted no differences between the two groups in terms of pre‐intervention and postintervention test scores as assessed by the Fisher exact probability test at a significance level of 0.05. Hence, the study authors concluded that participants "in both groups made essentially the same progress in correcting tongue‐tip sound placement, remediating /s/ and /z/ misarticulations and remediating general articulation errors" (p 163).
Fields 2003 (p 20) reported that "A one‐way Analysis of Variance revealed a significant difference between the groups, p < .05, p = .0001". Also, in the Discussion section of the paper, study authors stated that "An ANOVA revealed a significant difference between the groups' pre‐test and post test scores indicating the possibility that the implementation of ten minutes of oral motor therapy prior to ten minutes of articulation of phonology therapy appeared to increase correct productions of phonemes for the four participants in Group A (the intervention group)" (Fields 2003, p 21). Statistical test results were not clearly presented and one‐way ANOVA was not an appropriate test for a study of this research design ‐ two‐arm pre/post study.
Sargenti 2011 found that "similar improvements were made by the subjects who received OMT in conjunction with articulation therapy as compared to those who received articulation alone" (p 62). Thus, trial authors concluded that "OMT used in conjunction with articulation therapy is not more effective than articulation therapy alone in the treatment of speech sounds disorders for children who exhibit delayed oral motor control" (p 62).
Overall completeness and applicability of evidence
The overall applicability of evidence is limited and incomplete. This review identified three small‐scale randomised or quasi‐randomised controlled trials that investigated the efficacy of NSOMT as adjunctive treatment to conventional speech intervention for children between three and nine years of age with speech sound disorders (Christensen 1981; Fields 2003; Sargenti 2011). Speech problems of children in the three studies seemed to be unrelated to any obvious structural, neuromuscular, sensory or intellectual impairment. Therefore, it is uncertain whether the evidence could be generalised to individuals who have speech sound disorders with organic causes. Furthermore, the speech sound targeted in therapy in the three studies was limited to one or two speech sounds ‐ both /s/ and /z/ were treated in one study (Christensen 1981), whereas only /s/ was treated in the other studies (Fields 2003; Sargenti 2011). These sounds ‐ /s/ and /z/ ‐ are often targeted for treatment in speech therapy, as they are a common source of speech errors (Gibbon 2006). However, the limited range of NSOMTs targeted means that, even though the three studies used different treatment packages as NSOMTs, we are uncertain whether current evidence could be generalised to other speech sounds and other treatment exercises (e.g. sensory stimulation using massage).
Quality of the evidence
We noted several limitations in the methodology of the included studies (Christensen 1981; Fields 2003; Sargenti 2011). First, the sample size of each of the included studies was very small ‐ 10 participants in Christensen 1981, eight in Fields 2003 and four in Sargenti 2011 ‐ and none of the studies attempted to calculate the sample size required before recruiting participants. Small sample sizes are highly unlikely to be representative of the study population, and this affects the validity of conclusions that can be drawn regarding treatment efficacy (Nelson 2009). Second, studies were at unclear risk for selection bias given that methods used to generate the random sequence were not reported in two of the included studies (Christensen 1981; Fields 2003), and none of the studies provided details of allocation concealment. In addition, two studies were at unclear risk of detection bias, as they did not report the use of blinded outcome assessors (Fields 2003; Sargenti 2011). Another matter of concern involved unequal baseline characteristics of participants in the intervention group and in the control group in one of the included studies (Fields 2003), as suggested by results of the articulation test (SPAT‐D). Third, no inferential statistics were calculated to compare the intervention group against the control group, or pre‐intervention performance against postintervention performance, in one study (Sargenti 2011). What is more, another study used an inappropriate statistical test and did not clearly report results of the statistical test (Fields 2003), and in the two studies that conducted inferential statistics (Christensen 1981; Fields 2003), reporting of statistical test results was incomplete (e.g. effect sizes were not reported, significance level was not reported for one test). Finally, the fact that two studies (Fields 2003; Sargenti 2011) were research projects written as Master's theses, which have not been subsequently published in peer‐reviewed journals, further compromises the quality of evidence provided by these studies. In the light of serious limitations in methodology, we judged the overall quality of the evidence provided by the included trials to be low. Therefore, further research is very likely to have an important impact on our confidence in the estimate of treatment effect and is likely to change the estimate (Guyatt 2008).
Potential biases in the review process
To identify all relevant studies, we conducted comprehensive searches, contacted colleagues and researchers for grey literature and checked the reference lists of related articles. We searched five additional relevant electronic databases that were not listed in the protocol, as recommended by the Trials Search Co‐ordinator of the Cochrane Developmental, Psychological and Learning Problems Group. We adhered to our published protocol (Lee 2011) as much as possible throughout the review process ‐ two review authors independently screened titles and abstracts to eliminate irrelevant titles, judged whether remaining titles met the inclusion criteria and resolved differences of opinion by discussion. Therefore, it seems unlikely that an important trial was omitted. Another strength of the present research is that we conducted the risk of bias assessment of all included studies using full‐text versions of the titles. Furthermore, the review authors declared that no direct funding was received for conducting this review and noted no potential of conflicts of interest.
One limitation of this review is that we were not able to contact the authors of two studies regarding issues of random sequence generation and allocation concealment (Christensen 1981), and whether allocation concealment was ensured (Sargenti 2011). We were able to contact the author of the Fields 2003 study; however, information regarding random sequence generation method and allocation concealment was not provided. Hence, we were unable to classify the studies by Christensen 1981 and Fields 2003 as RCTs. Another limitation is that we were unable to conduct a meta‐analysis, as different outcome measures were used in the three included studies. Therefore, the conclusions of this review are based on a qualitative analysis of the included studies.
Agreements and disagreements with other studies or reviews
Three previous systematic reviews examined the efficacy of NSOMTs. The first was conducted in 2008 by Lass and Pannbacker (Lass 2008), who searched for NSOMT studies on treating phonological disorders using two databases (MEDLINE and Cumulative Index to Nursing and Allied Health Literature (CINAHL)). Their search strategies yielded nine articles, and review authors evaluated the level of evidence for each of these nine treatment studies. The second review was conducted by McCauley and colleagues (McCauley 2009), who searched 19 electronic databases and other literature sources to identify studies written in English and published in peer‐reviewed journals between 1960 and 2007 that addressed at least one of the following questions: (1) What is the influence of oral motor exercises on speech physiology? (2) What is the influence of oral motor exercises on sound production? and (3) What is the influence of oral motor exercises on functional speech outcomes? Review authors identified and reviewed a total of 15 titles. The third review, which was conducted in 2010, used similar procedures to the second review (Ruscello 2010). The review author searched 21 electronic databases and other relevant literature sources to identify peer‐reviewed English literature published during the same period (1960 to 2007) that addressed one of the following questions: (1) Does oral motor exercise have a positive effect on speech physiology? (2) Does oral motor exercise have a positive effect on speech production? or (3) Is oral motor exercise effective when examined through functional speech outcomes such as measures of intelligibility? This review also identified 15 titles.
The present review identified one randomised controlled trial (Sargenti 2011) and two quasi‐randomised controlled trials (Christensen 1981; Fields 2003). The study by Christensen and Hanson (Christensen 1981) was included in the three previous reviews, whereas the other two studies (Fields 2003; Sargenti 2011) were not. Studies included in previous reviews were excluded from the present review (except one) because most were case studies, participants were not children or treatment did not target speech sound disorders (e.g. voice disorder was treated). The discrepancy in search results between previous reviews and the present review was probably due to the greater number of electronic databases searched in this review and the different inclusion criteria used. Despite different search results, the findings of this review are consistent with those of the three previous reviews in that methodological limitations are evident in the included studies, including small sample size; unclear randomisation method; insufficient description of protocols, interventions and participant characteristics; different baseline characteristics between treatment group and control group; and lack of blinding of outcome assessor(s) (Lass 2008; McCauley 2009; Ruscello 2010). In addition, and consistent with previous findings, this review did not identify a study that compared NSOMT only versus conventional speech intervention only. This type of comparison is important for evaluating the absolute efficacy of NSOMTs (McCauley 2009). Overall, the present review concurs with previous reviews that no strong evidence is available to support the efficacy of NSOMTs for treating children with speech sound disorders.
Authors' conclusions
Implications for practice.
This review identified three small‐scale studies that investigated the efficacy of NSOMT as adjunctive treatment to conventional speech intervention for children with speech sound disorders (Christensen 1981, Fields 2003; Sargenti 2011). Two studies (Christensen 1981; Sargenti 2011) did not find NSOMT as adjunctive treatment to be more effective than conventional speech intervention, as intervention and control groups showed similar improvements in articulation after treatment. One study (Fields 2003) reported a change in postintervention articulation test results, but an inappropriate statistical test was used and study results were not reported clearly.
Reports of the three studies suggest that each had methodological limitations. As well as small sample sizes, the participant group was limited to children with speech sound disorders of unknown origin, and the target for treatment was limited to /s/ and /z/. In addition, reports often provided little or no information about important risks of bias such as allocation concealment and random sequence generation. Masking of outcome assessors was not reported in two of the studies; two used inferential statistics but did not include full details of statistical test results; and one study used an inappropriate statistical test. Overall, the evidence is limited and incomplete. Thus, findings of the present review are consistent with those of previous research, which currently provide no strong evidence suggesting that NSOMTs are effective as treatment or adjunctive treatment for children with developmental speech sound disorders.
Implications for research.
A five‐phase model has been proposed to test the efficacy and effectiveness of intervention approaches for managing communication disorders (Robey 2004). Results of this review show that NSOMTs are in the first phase of this clinical outcome research model, that is, the stage of investigating whether a therapeutic effect is present and subsequently estimating the magnitude of this therapeutic effect if present (Robey 2004). As several methodological limitations have been associated with previous treatment studies of NSOMTs, further well‐designed research is needed to answer the question of whether NSOMTs have a therapeutic effect in children with developmental speech sound disorders at this pretrial phase. The following methodological issues identified in this review should be addressed in future research: sample size; the need for a clear description of the method used to generate the randomisation sequence and allocation concealment; blinding of outcome assessor(s); comparable baseline characteristics between treatment groups and control groups; a detailed description of baseline characteristics of all participants; a detailed description of interventions used and reports on whether the intervention plan was adhered to; appropriate statistical analysis and complete reporting of statistical test results; and inclusion of both primary and secondary outcome measures. It is recommended that future research teams should include expert(s) in randomised controlled trial design and statistics to ensure the quality of research methodology. Research designs such as well‐controlled single case studies and small‐group pre/post studies would be useful for pretrial research (McCauley 2009; Robey 2004).
What's new
| Date | Event | Description |
|---|---|---|
| 13 September 2019 | Amended | Correcting typo in plain language summary. |
Acknowledgements
The review authors would like to thank colleagues in the field for providing information, articles and support for this review: Ms Laura MacDonald, Dr Joanne Wilson and Professor Geraldine MacDonald of Queen's University, Belfast (UK), for support and guidance throughout the protocol development and review process; Ms Margaret Anderson, also of Queen's University Belfast, for advice on search strategies and work in conducting most of the electronic searches; anonymous reviewers and the statistician for useful comments on previous drafts of the protocol and the review; and Ms Doris Murphy for a preliminary study of this review.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL), 2014 Issue 3, part of The Cochrane Library. Last searched 15 April 2014
#1MeSH descriptor: [Speech] this term only #2MeSH descriptor: [Speech Intelligibility] this term only #3MeSH descriptor: [Speech Disorders] explode all trees #4MeSH descriptor: [Apraxias] this term only #5(speech near/3 apraxia*) #6dysarthri* #7(mute or mutism) #8((speech or speak* or articulat* or phonetic* or phonologic* or phonemic*) near/5 (difficult* or disorder* or delay* or dysfunction* or impair* or problem*)) #9speech next sound #10#1 or #2 or #3 or #4 or #5 or#6 or #7 or #8 or #9 #11MeSH descriptor: [Speech Disorders] explode all trees and with qualifiers:[Rehabilitation ‐ RH, Therapy ‐ TH] #12non next speech or nonspeech #13MeSH descriptor: [Speech Therapy] this term only #14MeSH descriptor: [Myofunctional Therapy] this term only #15(myofunctional next (therap* or treat*)) #16(orofacial or oro next facial or oral next facial or oralfacial) #17((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) near/5 (action* or exercise* or motion* or movement* or physio* or stimulat* or stimulus or stretch* or treatment* or therapy)) #18(NSOM* or OME or OMEs) #19(oral next motor or oromotor or oro next motor) #20#11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 #21#10 and #20
Ovid MEDLINE (R), 1946 to April Week 1 2014. Last searched 15 April 2014
1 Speech/ 2 exp Speech Disorders/ 3 Speech intelligibility/ 4 Apraxias/ 5 (speech adj3 apraxia$).tw. 6 dysarthri$.tw. 7 (mute or mutism).tw. 8 ((speech or speak$ or articulat$ or phonetic$ or phonologic$ or phonemic$) adj5 (difficult$ or disorder$ or delay$ or dysfunction$ or impair$ or problem$)).tw. 9 speech sound.tw. 10 or/1‐9 11 oral motor.tw. 12 oromotor.tw. 13 oro‐motor.tw. 14 (NSOM$ or OME or OMEs).tw. 15 Speech Disorders/rh, th [Rehabilitation, Therapy] 16 (non‐speech or nonspeech$).tw. 17 Speech Therapy/ 18 Myofunctional Therapy/ 19 (myofunctional adj (therap$ or treatment$)).tw. 20 (orofacial or oro‐facial or oral facial or oralfacial).tw. 21 ((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) adj5 (action$ or exercise$ or motion or movement$ or physio$ or sensory or stimulat$ or stimulus or stretching or treatment$ or therapy)).tw. 22 or/11‐21 23 randomized controlled trial.pt. 24 controlled clinical trial.pt. 25 randomi#ed.ab. 26 placebo$.ab. 27 drug therapy.fs. 28 randomly.ab. 29 trial.ab. 30 groups.ab. 31 or/23‐30 32 exp animals/ not humans.sh. 33 31 not 32 34 10 and 22 and 33
Ovid MEDLINE (R) In‐Process & Other Non‐index Citations, updated 14 April 2014. Last searched 15 April 2014
1 ((speech or speak$ or articulat$ or phonetic$ or phonologic$ or phonemic$) adj5 (difficult$ or disorder$ or delay$ or dysfunction$ or impair$ or problem$)).tw. 2 (speech adj3 apraxia$).tw. 3 dysarthri$.tw. 4 (mute or mutism).tw. 5 speech sound.tw. 6 1 or 2 or 3 or 4 or 5 7 ((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) adj5 (action$ or exercise$ or motion$ or movement$ or physio$ or stimulat$ or stimulus or stretch$ or treatment$ or therapy)).tw. 8 oral motor.tw. 9 oromotor.tw. 10 oro‐motor.tw. 11 (NSOM$ or OME or OMEs).tw. 12 (myofunctional adj (therap$ or treatment$)).tw. 13 (orofacial or oro‐facial or oral facial or oralfacial).tw. 14 (speech adj3 (therap$ or rehabilit$)).tw. 15 or/7‐14 16 6 and 15
EMBASE (Ovid), 1980 to 2014 Week 15. Last searched 16 April 2014
1 exp speech/ 2 exp Speech Disorder/ 3 speech intelligibility/ 4 apraxia/ 5 (speech adj3 apraxia$).tw. 6 dysarthria/ 7 dysarthri$.tw. 8 mutism/ 9 (mute or mutism).tw. 10 ((speech or speak$ or articulat$ or phonetic$ or phonologic$ or phonemic$) adj5 (difficult$ or disorder$ or delay$ or dysfunction$ or impair$ or problem$)).tw. 11 speech sound.tw. 12 or/1‐11 13 exp speech disorder/rh, th [Rehabilitation, Therapy] 14 speech therapy/ 15 speech rehabilitation/ 16 muscle training/ 17 (myofunctional adj (therap$ or treatment$)).tw. 18 (orofacial or oro‐facial or oral facial or oralfacial).tw. 19 ((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) adj5 (action$ or exercise$ or motion$ or movement$ or physio$ or stimulat$ or stimulus or stretch$ or treatment$ or therapy)).tw. 20 oral motor.tw. 21 oromotor.tw. 22 oro‐motor.tw. 23 (non‐speech or nonspeech$).tw. 24 (NSOM$ or OME or OMEs).tw. 25 or/13‐24 26 12 and 25 27 exp Clinical trial/ 28 Randomized controlled trial/ 29 Randomization/ 30 Single blind procedure/ 31 Double blind procedure/ 32 triple blind procedure/ 33 Crossover procedure/ 34 Placebo/ 35 Randomi#ed.tw. 36 RCT.tw. 37 (random$ adj3 (allocat$ or assign$)).tw. 38 randomly.ab. 39 groups.ab. 40 trial.ab. 41 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 42 Placebo$.tw. 43 Prospective study/ 44 (crossover or cross‐over).tw. 45 prospective.tw. 46 or/27‐45 47 26 and 46
ERIC (ProQuest), 1966 to current. Last searched 16 April 2014
Searched for:(SU.EXACT("Longitudinal Studies") OR SU.EXACT("Control Groups") OR SU.EXACT("Program Effectiveness") OR SU.EXACT("Experimental Groups") OR SU.EXACT("Followup Studies") OR SU.EXACT("Comparative Analysis") OR prospective OR "follow up" OR ((evaluat* OR compar* OR blind*) NEAR/5 (study OR studies OR research)) OR ((compar* OR control*) NEAR/5 group*) OR random* OR intervention* OR experiment* OR trial*) AND ((SU.EXACT("Speech") OR SU.EXACT("Articulation (Speech)") OR SU.EXACT("Articulation Impairments") OR ((speech NEAR/1 sound) OR (speech OR speak[*3] OR articulat[*3] OR phonetic[*1] OR phonologic[*4] OR phonemic[*4]) NEAR/5 (difficult[*3] OR disorder[*2] OR delay[*3] OR dysfunction[*2])) OR (dysarthri[*1]) OR (mute OR mutism) OR (speech NEAR/1 apraxi[*1])) AND ("oral motor" OR oromotor OR "oro motor" OR NSOM[*2] OR OME OR OMEs OR nonspeech OR "non speech" OR orofacial OR "oro facial" OR "oral facial" OR oralfacial OR (myofunctional NEAR/1 (therap[*5] OR treat[*5])) OR ((oral OR face OR facial OR jaw OR larynx OR lips OR mouth OR palate OR tongue) NEAR/5 (action[*1] OR exercise[*1] OR motion[*1] OR movement[*1] OR physio[*7] OR stimulat[*3] OR stimulus OR stretch[*3] OR treatment[*1] OR therapy)) OR SU.EXACT.EXPLODE("Speech Therapy") OR SU.EXACT.EXPLODE("Speech Improvement")))
PsycINFO (Ovid), 1806 to April Week 2 2014. Last searched 16 April 2014
1 speech/ 2 exp speech characteristics/ 3 exp speech disorders/ 4 apraxia/ 5 (speech adj3 apraxia$).tw. 6 dysarthri$.tw. 7 Mutism/ 8 (mute or mutism).tw. 9 ((speech or speak$ or articulat$ or phonetic$ or phonologic$ or phonemic$) adj5 (difficult$ or disorder$ or delay$ or dysfunction$ or impair$ or problem$)).tw. 10 speech sound.tw. 11 or/1‐10 12 speech therapy/ 13 rehabilitation/ 14 oral motor.tw. 15 oromotor.tw. 16 oro‐motor.tw. 17 (NSOM$ or OME or OMEs).tw. 18 (non‐speech or nonspeech$).tw. 19 (myofunctional adj (therap$ or treatment$)).tw. 20 (orofacial or oro‐facial or oral facial or oralfacial).tw. 21 ((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) adj5 (action$ or exercise$ or motion$ or movement$ or physio$ or stimulat$ or stimulus or stretch$ or treatment$ or therapy)).tw. 22 or/12‐21 23 11 and 22 24 clinical trials/ 25 (randomis$ or randomiz$).tw. 26 (random$ adj3 (allocat$ or assign$)).tw. 27 ((clinic$ or control$) adj trial$).tw. 28 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 29 (crossover$ or "cross over$").tw. 30 random sampling/ 31 Experiment Controls/ 32 Placebo/ 33 placebo$.tw. 34 exp program evaluation/ 35 treatment effectiveness evaluation/ 36 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 37 or/24‐36 38 23 and 37
CINAHL (EBSCOhost), 1939 to current. Last searched 16 April 2014
S38 S22 and S37 S37 S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 S36 TI (evaluat* study or evaluat* research) or AB (evaluate* study or evaluat* research) or TI (effectiv* study or effectiv* research) or AB (effectiv* study or effectiv* research) OR TI (prospectiv* study or prospectiv* research) or AB (prospectiv* study or prospectiv* research) or TI (follow‐up study or follow‐up research) or AB (follow‐up study or follow‐up research) S35 placebo* S34 crossover* or "cross over*" S33 (MH "Crossover Design") S32 (tripl* N3 mask*) or (tripl* N3 blind*) S31 (trebl* N3 mask*) or (trebl* N3 blind*) S30 (doubl* N3 mask*) or (doubl* N3 blind*) S29 (singl* N3 mask*) or (singl* N3 blind*) S28 (clinic* N3 trial*) or (control* N3 trial*) S27 (random* N3 allocat* ) or (random* N3 assign*) S26 randomis* or randomiz* S25 (MH "Meta Analysis") S24 (MH "Clinical Trials+") S23 MH random assignment S22 S10 and S21 S21 S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 S20 ((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) N5 (action* or exercise* or motion* or movement* or physio* or stimulat* or stimulus or stretch* or treatment* or therapy)) S19 orofacial OR oro‐facial or (oro facial) OR (oral facial) S18 (myofunctional N1 (therap* or treatment*)) S17 (MH "Speech Therapy") S16 (MH "Speech Disorders/RH/TH") S15 non‐speech* or nonspeech* or (non speech) S14 NSOM* or OME or OMEs S13 oro‐motor or (oro motor) S12 oromotor S11 oral motor S10 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 S9 (speech sound) S8 ((speech or speak* or articulat* or phonetic* or phonologic* or phonemic*) N5 (difficult* or disorder* or delay* or dysfunction* or impair* or problem*)) S7 mute or mutism S6 dysarthri* S5 (speech N3 apraxia*) S4 (MH "Apraxia") S3 (MH "Speech Intelligibility") S2 (MH "Speech Disorders+") S1 (MH "Speech")
Science Citation Index‐Expanded (SCI‐EXPANDED) and Social Sciences Citation Index (SSCI) (Web of Knowledge), 1970 to 16 April 2014. Last searched 16 April 2014 Conference Proceedings Citation Index‐Science (CPCI‐S) and Conference Proceedings Citation Index‐Social Sciences & Humanities (CPCI‐SSH) (Web of Knowledge), 1990 to 11 April 2014. Last searched 16 April 2014
#16#15 AND #14 DocType=All document types; Language=All languages; #15TS=(random* or control* or trial* or groups* or effectiv* or intervention* or evaluation or placebo*) DocType=All document types; Language=All languages; #14#13 AND #7 DocType=All document types; Language=All languages; #13#12 OR #11 OR #10 OR #9 OR #8 DocType=All document types; Language=All languages; #12TS=(NSOM* or OME or OMEs) DocType=All document types; Language=All languages; #11Ts=("oral motor" OR oromotor OR "oro‐motor") DocType=All document types; Language=All languages; #10TS=(orofacial or "oro‐facial" or "oral facial" or oralfacial) DocType=All document types; Language=All languages; #9TS=( myofunctional NEAR/1 (therap* or treatment*)) DocType=All document types; Language=All languages; #8TS=((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) NEAR/5 (action* or exercise* or motion* or movement* or physio* or stimulat* or stimulus or stretch* or treatment* or therapy)) DocType=All document types; Language=All languages; #7#6 OR #5 OR #4 OR #3 OR #2 OR #1 DocType=All document types; Language=All languages; #6TS=(mute or mutism) DocType=All document types; Language=All languages; #5TS=(dysarthri*) DocType=All document types; Language=All languages; #4TS=(dysarthri*) DocType=All document types; Language=All languages; #3TS=(speech NEAR/3 apraxi*) DocType=All document types; Language=All languages; #2TS=("speech sound") DocType=All document types; Language=All languages; #1TS=((speech or speak* or articulat* or phonetic* or phonologic* or phonemic*) NEAR/5 (difficult* or disorder* or delay* or dysfunction* or impair* or problem*)) DocType=All document types; Language=All languages;
LILACS,http://bases.bireme.br/cgi‐bin/wxislind.exe/iah/online/, all available years. Last searched 16 April 2014
(Mh SPEECH DISORDERS or Mh APRAXIAS or Mh SPEECH INTELLIGIBILITY or ( SPEECH or SPEAK OR ARTICULAT$ OR APRAXIA OR DYSARTHI$ or PHONETIC$ or PHONEMIC$ or PHONOLOGIC$)) [Words] and (Mh Myofunctional Therapy OR Mh Speech therapy OR OROFACIAL or "ORO FACIAL" OR "ORAL FACIAL" OR orofacial OR "oral motor" OR oromotor or "oro motor" or NSOME$ or ome OR omes ) [Words] and ((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animal AND NOT (Ct human and Ct animal))) [Words]
Academic Search Complete (EBSCOhost), all available years. Last searched 14 April 2014
S37 S21 and S36 S36 S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 S35 TI (evaluat* study or evaluat* research) or AB (evaluate* study or evaluat* research) or TI (effectiv* study or effectiv* research) or AB (effectiv* study or effectiv* research) OR TI (prospectiv* study or prospectiv* research) or AB (prospectiv* study or prospectiv* research) or TI (follow‐up study or follow‐up research) or AB (follow‐up study or follow‐up research) S34 placebo* S33 crossover* or "cross over*" S32 Crossover Design S31 (tripl* N3 mask*) or (tripl* N3 blind*) S30 (trebl* N3 mask*) or (trebl* N3 blind*) S29 (doubl* N3 mask*) or (doubl* N3 blind*) S28 (singl* N3 mask*) or (singl* N3 blind*) S27 (clinic* N3 trial*) or (control* N3 trial*) S26 (random* N3 allocat* ) or (random* N3 assign*) S25 randomis* or randomiz* S24 SU Meta Analysis S23 SU Clinical Trials S22 random assignment S21 S10 AND S20 S20 S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 S19 ((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) N5 (action* or exercise* or motion* or movement* or physio* or stimulat* or stimulus or stretch* or treatment* or therapy)) S18 orofacial or oro‐facial or (oro facial) or (oral facial) S17 myofunctional N1 (therap* or treatment*) S16 SU Speech Therapy S15 non‐speech* or nonspeech* or (non speech) S14 NSOM* or OME or OMEs S13 oro‐motor or (oro motor) S12 oromotor S11 oral motor S10 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 S9 (speech sound) S8 ((speech or speak* or articulat* or phonetic* or phonologic* or phonemic*) N5 (difficult* or disorder* or delay* or dysfunction* or impair* or problem*)) S7 mute or mutism S6 dysarthri* S5 (speech N3 apraxia*) S4 SU Apraxia S3 SU Speech Intelligibility S2 SU Speech Disorders S1 SU Speech
ProQuest Dissertations and Theses: UK & Ireland, 1990 to current. Last searched 14 April 2014
Searched for:(SU.EXACT("Longitudinal Studies") OR SU.EXACT("Control Groups") OR SU.EXACT("Program Effectiveness") OR SU.EXACT("Experimental Groups") OR SU.EXACT("Followup Studies") OR SU.EXACT("Comparative Analysis") OR prospective OR "follow up" OR ((evaluat* OR compar* OR blind*) NEAR/5 (study OR studies OR research)) OR ((compar* OR control*) NEAR/5 group*) OR random* OR intervention* OR experiment* OR trial*) AND ((SU.EXACT("Speech") OR SU.EXACT("Articulation (Speech)") OR SU.EXACT("Articulation Impairments") OR ((speech NEAR/1 sound) OR (speech OR speak[*3] OR articulat[*3] OR phonetic[*1] OR phonologic[*4] OR phonemic[*4]) NEAR/5 (difficult[*3] OR disorder[*2] OR delay[*3] OR dysfunction[*2])) OR (dysarthri[*1]) OR (mute OR mutism) OR (speech NEAR/1 apraxi[*1])) AND ("oral motor" OR oromotor OR "oro motor" OR NSOM[*2] OR OME OR OMEs OR nonspeech OR "non speech" OR orofacial OR "oro facial" OR "oral facial" OR oralfacial OR (myofunctional NEAR/1 (therap[*5] OR treat[*5])) OR ((oral OR face OR facial OR jaw OR larynx OR lips OR mouth OR palate OR tongue) NEAR/5 (action[*1] OR exercise[*1] OR motion[*1] OR movement[*1] OR physio[*7] OR stimulat[*3] OR stimulus OR stretch[*3] OR treatment[*1] OR therapy)) OR SU.EXACT.EXPLODE("Speech Therapy") OR SU.EXACT.EXPLODE("Speech Improvement")))
ProQuest Dissertations and Theses A&I, 1970 to current. Last searched 14 April 2014
(("oral motor" OR oromotor OR "oro motor" OR "NSOM[*2]" OR OME OR OMEs OR orofacial OR "oro facial" OR "oral facial" OR oralfacial OR myofunctional) NEAR/5 (action* OR exercise* OR motion* OR movement* OR physio* OR stimulat* OR stimulus OR stretch* OR treatment* OR therap* OR intervention)) AND (speech OR speak* OR articulat* OR phonetic* OR phonologic* OR phonemic*) AND child*
Cochrane Database of Systematic Reviews (CDSR), 2014 Issue 4 of 12. Last searched 15 April 2014
#1MeSH descriptor: [Speech] this term only #2MeSH descriptor: [Speech Intelligibility] this term only #3MeSH descriptor: [Speech Disorders] explode all trees #4MeSH descriptor: [Apraxias] this term only #5(speech near/3 apraxia*) #6dysarthri* #7(mute or mutism) #8((speech or speak* or articulat* or phonetic* or phonologic* or phonemic*) near/5 (difficult* or disorder* or delay* or dysfunction* or impair* or problem*)) #9speech next sound #10#1 or #2 or #3 or #4 or #5 or#6 or #7 or #8 or #9 #11MeSH descriptor: [Speech Disorders] explode all trees and with qualifiers: [Rehabilitation ‐ RH, Therapy ‐ TH] #12non next speech or nonspeech #13MeSH descriptor: [Speech Therapy] this term only #14MeSH descriptor: [Myofunctional Therapy] this term only #15(myofunctional next (therap* or treat*)) #16(orofacial or oro next facial or oral next facial or oralfacial) #17((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) near/5 (action* or exercise* or motion* or movement* or physio* or stimulat* or stimulus or stretch* or treatment* or therapy)) #18(NSOM* or OME or OMEs) #19(oral next motor or oromotor or oro next motor) #20#11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 #21#10 and #20
Database of Abtracts of Reviews of Effects (DARE), 2014 Issue 1 of 4. Last searched 15 April 2014
#1MeSH descriptor: [Speech] this term only #2MeSH descriptor: [Speech Intelligibility] this term only #3MeSH descriptor: [Speech Disorders] explode all trees #4MeSH descriptor: [Apraxias] this term only #5(speech near/3 apraxia*) #6dysarthri* #7(mute or mutism) #8((speech or speak* or articulat* or phonetic* or phonologic* or phonemic*) near/5 (difficult* or disorder* or delay* or dysfunction* or impair* or problem*)) #9speech next sound #10#1 or #2 or #3 or #4 or #5 or#6 or #7 or #8 or #9 #11MeSH descriptor: [Speech Disorders] explode all trees and with qualifiers: [Rehabilitation ‐ RH, Therapy ‐ TH] #12non next speech or nonspeech #13MeSH descriptor: [Speech Therapy] this term only #14MeSH descriptor: [Myofunctional Therapy] this term only #15(myofunctional next (therap* or treat*)) #16(orofacial or oro next facial or oral next facial or oralfacial) #17((oral or face or facial or jaw or larynx or lips or mouth or palate or tongue) near/5 (action* or exercise* or motion* or movement* or physio* or stimulat* or stimulus or stretch* or treatment* or therapy)) #18(NSOM* or OME or OMEs) #19(oral next motor or oromotor or oro next motor) #20#11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 #21#10 and #20
speechBITE,www.speechbite.com/, all available years. Last searched 17 April 2014
"speech sound" filtered by publication type= RCTs
The National Research Register (NRR) Archive,www.nihr.ac.uk/Pages/NRRArchiveSearch.aspx. Last searched 6 February 2013, as archive was last modified in October 2010
speech OR articulation in All Fields Search results for “non speech” OR “oral motor” OR nsom* in methodology
UK Clinical Research Network Portal (UKCRN),http://public.ukcrn.org.uk/search/. Last searched 17 April 2014
Topics: all Research summary: speech articulation Searching with "Any" term selected
ClinicalTrials.gov,http://clinicaltrials. gov/. Last searched 16 April 2014
Advanced Search speech sound OR articulation | Child
metaRegister of Current Controlled Trials (mRCT),www.controlled‐trials.com/mrct/. Last searched 17 April 2014. This service is currently under review (19 December 2014)
non motor OR nonmotor OR NSOME*
World Health Organization International Clinical Trials Registry Platform (ICTRP),http://apps.who.int/trialsearch/. Last searched 17 April 2014
non speech OR NSOME* OR oral motor OR oromotor
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Christensen 1981.
| Methods | Quasi‐randomised controlled trial comparing 1 intervention group (a combination of articulation and oral myofunctional (tongue thrust) therapy) and 1 control group (articulation therapy only). (The date of the study was not reported.) | |
| Participants | 10 children (6 boys and 4 girls) aged 5 years 8 months to 6 years 9 months. All participants had "normal hearing as measured by puretone screening tests, normal development as reported by parents, no other known physical or psychological abnormalities, no previous speech or tongue thrust services, willingness of the parents to cooperate and carry out daily home practice sessions, and white middle‐class home environment" (p 161). In addition, "all children...were observed by the investigator to have visually and acoustically distorted /s/ and /z/, 2 or more other dentally or interdentally produced tongue‐tip sounds (although acoustically correct) and interdental tongue positioning on swallows of all 3 swallowing media (liquid, solids and saliva)" (p 162) | |
| Interventions | The 10 participants were randomly assigned to 1 of 2 groups Intervention group (n = 5)
Control group (n = 5)
At the start of the intervention, about 1.5 to 2.5 therapy sessions were devoted to articulation therapy targeting the placement of speech sounds /t/, /d/, /l/ and /n/ for all participants. As stated above, the frequency of therapy sessions was the same for both intervention and control groups. Total therapy time was 11 hours for each participant. All participants "were given weekly home assignments to be completed with the mother's help in brief, daily home practices" (p 162). "Articulation home assignments" and home assignments for oral myofunctional therapy were mentioned, but it was not clear whether the intervention group was given both home assignments and the control group was given only articulation home assignments (p 162) |
|
| Outcomes | The following tests were used for pretreatment and post‐treatment assessments of articulation
Additional items were used for post‐treatment assessments of articulation
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method used to generate the random sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | The method used to conceal allocation was not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of the outcome assessor was ensured ‐ "pre‐ and post‐treatment test responses were evaluated by two independent observers... Neither judge knew which children were receiving tongue‐thrust services" (p 162) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the 22 therapy sessions |
| Selective reporting (reporting bias) | Low risk | The study appears to be free of selective reporting bias |
| Other bias | Low risk | The study appears to be free of other bias |
Fields 2003.
| Methods | Quasi‐randomised controlled trial comparing 1 intervention group (oral motor therapy and articulation or phonological therapy) and 1 control group (articulation or phonological therapy only). Conducted in 2002 | |
| Participants | 8 children (4 boys and 4 girls) aged between 3 and 6 years; mean age was 4.63 years. All participants had not received oral motor therapy before the study. All had a current IEP with speech and language assessment no more than 1 year old, and all had been receiving articulation therapy for at least 3 months. Receptive vocabulary score on the PPVT‐III was within normal limits, and the standard score on SPAT‐D fell within 1.5 and 2 standard deviations below the mean. All participants were diagnosed as having moderate to severe articulation disorder. In the intervention group, participants 1, 2 and 3 showed "cluster reduction /s/ errors" and participant 4 had "stridency deletion" (p 18); it was not reported whether additional speech errors were observed in these participants. Investigators did not report speech errors shown by participants in the control group | |
| Interventions | 8 children were placed first into 4 groups (2 in each group) according to age, disorder and IEP goals by the speech‐language pathologist at the school the children were attending. Groups were then randomly assigned to 1 of 2 conditions Intervention group (n = 4)
Control group (n = 4)
10 therapy sessions were planned; however, only 9 were administered because the "researcher did not implement therapy one day due to personal reasons" (p 23). The frequency of therapy sessions was the same for both intervention and control groups: 2 therapy sessions per week, over 5 weeks. Total therapy time was 3 hours for each participant. All therapy sessions, for both conditions, were carried out in groups of 2 children |
|
| Outcomes | SPAT‐D was conducted pre‐intervention and post intervention to measure treatment effect | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method used to generate the random sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | The method used to conceal allocation was not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor was not identified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the 9 therapy sessions |
| Selective reporting (reporting bias) | Low risk | The study appears to be free of selective reporting bias |
| Other bias | High risk | Query the possibility of unequal baseline characteristics of the 2 groups ‐ the intervention group had a mean score of 27 and an SD of 14.6 for SPAT‐D pre‐treatment, whereas the control group had a mean score of 40.5 and an SD of 20.5 for SPAT‐D. The intervention group appeared to have fewer speech errors than the control group at the start of the study |
Sargenti 2011.
| Methods | Randomised controlled trial comparing 1 intervention group (oral motor therapy and articulation therapy) and 1 control group (articulation therapy only). Conducted from January to March 2011 | |
| Participants | 4 children (all boys) aged 7.01 to 9.06 years; mean age was 8.02 years. All participants had normal hearing and showed delayed motor control. 1 participant in the intervention group was diagnosed as "communication impaired", and 1 participant in the control group was classified as "multiply disabled (communication impaired, Attention Deficit Hyperactivity Disorder, Tourette Syndrome, and Obsessive‐Compulsive Disorder)". The other 2 participants had "normal academic and language abilities" (p 17). All participants showed "distorted production of the phonemes /s/ and /z/ and exhibited an interdental (frontal) or lateral lisp" (p 17) | |
| Interventions | The 4 participants were randomly assigned to 1 of the 2 groups by means of a random number table Intervention group (n = 2)
Control group (n = 2)
The frequency of therapy sessions was the same for both intervention and control groups ‐ 2 therapy sessions per week over 8 weeks. Total therapy time was 8 hours for each participant. All therapy sessions were conducted as individual therapy. All participants were "given specific articulation homework assignments biweekly" (p 38) and "specific (oral motor therapy) homework assignments were given biweekly" to participants in the Intervention group (p 30) |
|
| Outcomes | Assessment of Oral‐Motor Functions During Non‐Speech Tasks (Mackie 1996) and Goldman‐Fristoe Test of Articulation Second Edition (Goldman 2000) were conducted on all participants 1 week before the intervention and 1 week after the final therapy session. 3 sets of probes (each of which includes 4 words that contain /s/ and 4 words that contain /z/) were developed for tracking treatment progress of /s/ and generalisation of treatment effect to /z/. Probe 1 was conducted on all participants at the start of the first therapy session to determine the initial level of performance; probe 2 was used to record performance at the end of the first therapy session; and probe 3 was used to document performance at the end of the second therapy session. Performance at the end of the remaining therapy sessions was assessed by alternating use of the 3 probes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A random number table was used to randomly assign subjects to one of two groups" (p 18) |
| Allocation concealment (selection bias) | Unclear risk | The method used to conceal allocation was not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor was not identified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the 16 therapy sessions |
| Selective reporting (reporting bias) | Low risk | The study appears to be free of selective reporting bias |
| Other bias | Low risk | The study appears to be free of other bias |
IEP = individualised education plan; PPVT‐III = Peabody Picture Vocabulary Test Third Edition; SPAT‐D = Structured Photographic Articulation Test ‐ Dudsberry.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bacha 1999 | Investigators did not treat speech sound disorders. Breathing, feeding, oral‐facial habits, buccal hygiene and corporal posture or physical activity were treatment targets |
| Baskervill 1976 | Not a randomised or quasi‐randomised controlled trial. The study used a pretest/post‐test design with no control group |
| Bathel 2006 | Not an experimental study. This article described current research in the field of oral‐motor muscle‐based therapies |
| Bäckman 2003 | Not a randomised or quasi‐randomised controlled trial; investigators did not treat speech sound disorders, and treatment used was not NSOMT. This case‐control study included 42 children with Down syndrome in the experimental group (age‐matched to 31 typically developing children (control group 1)) and 33 children with Down syndrome (control group 2). Researchers investigated the effects of a palatal plate on several dental outcomes (e.g. eruption of teeth, sucking habits, tongue morphology, overjet and overbite), oral motor function and speech production |
| Bäckman 2007 | Not a randomised or quasi‐randomised controlled trial; investigators did not treat speech sound disorders, and treatment used was not NSOMT. This was a case‐control study. Participants in the experimental group (n = 38) also took part in the Bäckman 2003 study. Researchers investigated the effects of palatal plate on several dental outcomes (e.g. eruption of teeth, sucking habits, tongue morphology, overjet and overbite), oral motor function and speech production |
| Carlstedt 2001 | Investigators did not treat speech sound disorders, and treatment used was not NSOMT. Researchers investigated the effects of palatal plate on facial expression and oral motor function during silence and speech |
| Carlstedt 2003 | Investigators did not treat speech sound disorders, and treatment used was not NSOMT. Researchers investigated the effects of palatal plate on oral facial structure appearance, oral motor function, speech sound articulation and communication preferences |
| Clark 1993 | Treatment used was not NSOMT. Researchers investigated the effects of a removable prosthetic appliance for treating distortion or substitution errors for /r/, or both |
| Forrest 2008 | Not a randomised or quasi‐randomised controlled trial. Investigators used a pretest/post‐test "alternating treatment design" whereby all participants received (1) NSOMT for treating 1 speech sound, (2) speech intervention ("traditional production treatment") for treating a second, linguistically unrelated sound and (3) no treatment for a third sound, which served as a control for non‐experiment effects (p 307) |
| Gommerman 1995 | Not a randomised or quasi‐randomised controlled trial. This was a single case study |
| Guisti 2002 | Not a randomised or quasi‐randomised controlled trial. Investigators used a pretest/post‐test design with no control group |
| Guisti Braislin 2005 | Not a randomised or quasi‐randomised controlled trial. Investigators used a pretest/post‐test design with no control group. Note that this study (a Master's thesis) was identical to Guisti 2002 |
| Hayes 2006 | Trial did not conform with the types of interventions stated in the protocol. Although participants were randomly assigned to 1 of the 2 intervention conditions, NSOMT was used in both interventions ‐ 1 group received baseline, followed by traditional articulation treatment only, combined traditional articulation treatment and NSOMT and traditional articulation treatment only. The other group received baseline, followed by NSOMT only, combined traditional articulation treatment and NSOMT and NSOMT only |
| Helmick 1976 | Treatment used was not NSOMT. Researchers investigated the effects of conventional speech intervention in remediating articulation errors in children with speech sound disorders |
| Hodge 2005a | Not a treatment study. This study is a survey on the use of NSOMTs by speech‐language pathologies in Alberta, Canada, for the treatment of speech disorders in children |
| Karch 2005 | Not an experimental study. The article describes orofacial regulation therapy |
| Overstake 1976 | Trial did not conform with the types of interventions stated in the protocol. Investigators compared "swallow therapy only" vs "swallow and speech therapy" |
| Powers 1974 | Not a randomised or quasi‐randomised controlled trial; investigators did not treat speech sound disorders. Researchers used a pretest/post‐test design for investigating the effects of muscle exercises in treating hypernasality |
| Robertson 2001 | Not a randomised or quasi‐randomised controlled trial; participants were adults, not children. Researchers used a pretest/post‐test design |
| Roehrig 2004 | Cross‐over design was used |
NSOMT = non‐speech oral motor treatment.
Differences between protocol and review
Parts of the Background section have been rewritten. It now contains an updated and detailed definition of developmental speech sound disorders and additional information regarding the debate on efficacy of non‐speech oral motor treatments (NSOMTs).
As recommended by the Trials Search Co‐ordinator for the Cochrane Developmental, Psychological and Learing Problems Group, we searched five additional electronic databases that were not listed in the protocol: (1) Ovid MEDLINE In‐Process & Other Non‐index Citations; (2) Cochrane Database of Systematic Reviews (CDSR); (3) Database of Abstracts of Reviews of Effects (DARE); (4) Conference Proceedings Citation Index‐Science (CPCI‐S) and Conference Proceedings Citation Index‐Social Sciences & Humanities (CPCI‐SSH); and (5) speechBITE (http://www.speechbite.com/).
We had hoped to assess the quality of all primary outcomes using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (Guyatt 2008) and to report these ratings in a 'Summary of findings table', but we did not, as the studies were too heterogeneous to be combined in a meta‐analysis. We have added this intention to our additional methods, which have been archived for future updates of this review (see Table 1).
Contributions of authors
AL and FG planned the review. AL was the primary author of the protocol. AL developed and conducted the search strategies with help from Ms Margaret Anderson. AL and FG independently assessed titles. AL is the primary author of the review.
Sources of support
Internal sources
No sources of support supplied, Other.
External sources
No sources of support supplied, Other.
Declarations of interest
Alice S‐Y Lee: none known.
Fiona E Gibbon: receives royalties as Co‐Editor of The Handbook of Clinical Phonetics. The Japan Cleft Palate Association paid travel and accommodation costs for Professor Gibbon to give a keynote lecture in May 2012. Professor Gibbon is principal investigator on the project titled "The effect of speaker accent on sentence comprehension in children with language delay". The Health Research Board is paying funds to the University College Cork for this project from 2012 to 2015. Professor Gibbon was paid honorarium in 2013 for advice on research strategy for the Research Assessment Exercise at the University of Hong Kong.
Edited (no change to conclusions)
References
References to studies included in this review
Christensen 1981 {published data only}
- Christensen M, Hanson M. An investigation of the efficacy of oral myofunctional therapy as a precursor to articulation therapy for pre‐first grade children. Journal of Speech and Hearing Disorders 1981;46(2):160‐5. [DOI] [PubMed] [Google Scholar]
Fields 2003 {unpublished data only}
- Fields D, Polmanteer K. Effectiveness of oral motor techniques in articulation and phonology therapy. Paper presented at the 2002 American Speech‐Language‐Hearing Association (ASHA) Convention; 2002 November. Atlanta (GA), 2002.
- Fields DC. The Effectiveness of Oral Motor Techniques in Articulation and Phonology Therapy [unpublished Master's thesis]. Richmond, Kentucky, US: Eastern Kentucky University, 2003. [Google Scholar]
Sargenti 2011 {unpublished data only}
- Sargenti T. The Effects of Oral‐Motor Treatment in Remediating Speech Sound Disorders for Children Who Exhibit a Lack of Sufficient Oral‐Motor Control [unpublished Master's thesis]. Wayne, New Jersey, US: The William Paterson University of New Jersey, 2011. [Google Scholar]
References to studies excluded from this review
Bacha 1999 {published data only}
- Bacha SM, Rìspoli CF. Myofunctional therapy: brief intervention. International Journal of Orofacial Myology 1999;25:37‐47. [PubMed] [Google Scholar]
Bäckman 2003 {published data only}
- Bäckman B, Grevér‐Sjölander AC, Holm AK, Johansson I. Children with Down syndrome: oral development and morphology after use of palatal plates between 6 and 18 months of age. International Journal of Paediatric Dentistry 2003;13(5):327‐35. [DOI] [PubMed] [Google Scholar]
Bäckman 2007 {published data only}
- Bäckman B, Grevér‐Sjölander AC, Bengtsson K, Persson J, Johansson I. Children with Down syndrome: oral development and morphology after use of palatal plates between 6 and 48 months of age. International Journal of Paediatric Dentistry 2007;17(1):19‐28. [DOI] [PubMed] [Google Scholar]
Baskervill 1976 {published data only}
- Baskervill RD. The effects of special speech therapeutic procedures involving individuals with sibilant distortions: a pilot study. International Journal of Oral Myology 1976;2(4):86‐92. [PubMed] [Google Scholar]
Bathel 2006 {published data only}
- Bathel JA. Current research in the field of oral‐motor, muscled‐based therapies: response to: logic, theory and evidence against the use of non‐speech oral motor exercises to change speech sound productions by Gregory Lof. http://bit.ly/17avafN (accessed 10 February 2014).
Carlstedt 2001 {published data only}
- Carlstedt K, Henningsson G, McAllister A, Dahllöf G. Long‐term effects of palatal plate therapy on oral motor function in children with Down syndrome evaluated by video registration. Acta Odontologica Scandinavica 2001;59(2):63‐8. [DOI] [PubMed] [Google Scholar]
Carlstedt 2003 {published data only}
- Carlstedt K, Henningsson G, Dahllöf G. A four‐year longitudinal study of palatal plate therapy in children with Down syndrome: effects on oral motor function, articulation and communication preferences. Acta Odontologica Scandinavica 2003;61(1):39‐46. [DOI] [PubMed] [Google Scholar]
Clark 1993 {published data only}
- Clark CE, Schwarz IE, Blakeley RW. The removable r‐appliance as a practice device to facilitate correct production of /r/. American Journal of Speech‐Language Pathology 1993;2(1):84‐92. [Google Scholar]
Forrest 2008 {published data only}
- Forrest K, Iuzzini J. A comparison of oral motor and production training for children with speech sound disorders. Seminars in Speech and Language 2008;29(4):304‐11. [DOI] [PubMed] [Google Scholar]
Gommerman 1995 {published data only}
- Gommerman SL, Hodge MM. Effects of oral myofunctional therapy on swallowing and sibilant production. International Journal of Orofacial Myology 1995;21:9‐22. [PubMed] [Google Scholar]
Guisti 2002 {published data only}
- Guisti MA. The Efficacy of Oral Motor Therapy for Children with Mild Articulation Disorders [unpublished Master's thesis]. New Haven, Connecticut, US: Southern Connecticut State University, 2002. [Google Scholar]
Guisti Braislin 2005 {published data only}
- Guisti Braislin MA, Cascella PW. A preliminary investigation of the efficacy of oral motor exercises for children with mild articulation disorders. International Journal of Rehabilitation Research 2005;28(3):263‐6. [DOI] [PubMed] [Google Scholar]
Hayes 2006 {published data only}
- Hayes S. Comparison of an Oral Motor Treatment and Traditional Articulation Treatment in Children [unpublished PhD thesis]. Fort Lauderdale, Florida, US: Nova Southeastern University, 2006. [Google Scholar]
Helmick 1976 {published data only}
- Helmick JW. Effects of therapy on articulation skills in elementary‐school children. Language, Speech, and Hearing Services in Schools 1976;7:169‐72. [Google Scholar]
Hodge 2005a {published data only}
- Hodge M, Salonka R, Kollias S. Use of nonspeech oral‐motor exercises in children's speech therapy. Paper presented at the 2005 American Speech‐Language‐Hearing Association (ASHA) Convention; 2005 November; San Diego (CA). 2005.
Karch 2005 {published data only}
- Karch D, Groß‐Selbeck G, Pietz J, Schlack HG. Orofacial regulation therapy after Castillo Morales: position of the Society for Neuropediatrics, abridged version ‐ Kommission zu Behandlungsverfahren bei Entwicklungsstorungen and zerebralen Bewegungsstorungen. Monatsschrift Kinderheilkunde 2005;153(8):782‐5. [Google Scholar]
Overstake 1976 {published data only}
- Overstake C. Investigation of the efficacy of a treatment program for deviant swallowing and allied problems. II. International Journal of Oral Myology 1976;2(1):1‐6. [PubMed] [Google Scholar]
Powers 1974 {published data only}
- Powers GL, Starr CD. The effects of muscle exercises on velopharyngeal gap and nasality. Cleft Palate Journal 1974;11:28‐35. [Google Scholar]
Robertson 2001 {published data only}
- Robertson S. The efficacy of oro‐facial and articulation exercises in dysarthria following stroke. International Journal of Language and Communication Disorders 2001;36(Suppl 1):292‐7. [DOI] [PubMed] [Google Scholar]
Roehrig 2004 {published data only}
- Roehrig S, Suiter D, Pierce T. An examination of the effectiveness of passive oral‐motor exercises. Paper presented at the 2004 American Speech‐Language‐Hearing Association (ASHA) Convention; 2004 November; Philadelphia, PA. 2004.
Additional references
Barrett 1978
- Barrett RH, Hanson ML. Oral Myofunctional Disorders. St. Louis: Mosby, 1978. [Google Scholar]
Borenstein 2009
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta‐Analysis. Chichester, UK: John Wiley & Sons, 2009. [Google Scholar]
Bowen 2005
- Bowen C. What is the evidence for oral motor therapy?. Acquiring Knowledge in Speech, Language and Hearing 2005;7(3):144‐7. [Google Scholar]
Brumbaugh 2013
- Brumbaugh KM, Smit AB. Treating children ages 3‐6 who have speech sound disorder: a survey. Language, Speech, and Hearing Services in Schools 2013;44:306‐19. [DOI] [PubMed] [Google Scholar]
Bunton 2008
- Bunton K. Speech versus nonspeech: different tasks, different neural organization. Seminars in Speech and Language 2008;29(4):267‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2010
- Clark HM. Nonspeech oral motor intervention. In: Williams AL, McLeod S, McCauley RJ editor(s). Interventions for Speech Sound Disorders in Children. Baltimore, MD: Paul H. Brookes Publishing, 2010:579‐99. [Google Scholar]
Dane 1998
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clinical Psychology Review 1998;18(1):23‐45. [DOI] [PubMed] [Google Scholar]
Donner 2000
- Donner A, Klar N. Design and Analysis of Cluster Randomization Trials in Health Research. London: Arnold, 2000. [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Endnote [Computer program]
- Thomson Reuters. Endnote. Version X7. New York, US: Thomson Reuters, 1988‐2013.
Fields 2014 [pers comm]
- Fields DC. (Shannon Johnson Elementary, Foley Middle School, Madison Southern High School, Kentucky, US). [personal communication]. Conversation with: A Lee (University College Cork, Cork, Ireland) 28 April 2014.
Flipsen 2009
- Flipsen P Jr, Bankson NW, Bernthal JE. Classication and factors related to speech sound disorders. In: Bernthal JE, Bankson NW, Flipsen P Jr editor(s). Articulation and Phonological Disorders: Speech Sound Disorders in Children. 6th Edition. Boston: Pearson Education, 2009:121‐86. [Google Scholar]
Forrest 2002
- Forrest K. Are oral‐motor exercises useful in the treatment of phonological/articulatory disorders?. Seminars in Speech and Language 2002;23(1):15‐26. [DOI] [PubMed] [Google Scholar]
Gamble 2005
- Gamble C, Hollis S. Uncertainty method improved on best‐worst case analysis in a binary meta‐analysis. Journal of Clinical Epidemiology 2005;58(6):579‐88. [DOI] [PubMed] [Google Scholar]
Gibbon 2006
- Gibbon FE, Paterson L. A survey of speech and language therapists' views on electropalatography therapy outcomes in Scotland. Child Language Teaching and Therapy 2006;22(3):275‐92. [Google Scholar]
Goldman 2000
- Goldman R, Fristoe M. Goldman‐Fristoe Test of Articulation. 2nd Edition. Circle Pines, MN: American Guidance Service, Inc, 2000. [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Hodge 2005b
- Hodge MM, Salonka R, Kollias S. Use of nonspeech oral‐motor exercises in children’s speech therapy. Paper presented at: Annual Meeting of the American Speech‐Language‐Hearing Association, 2005, San Diego (CA).
IEPMCS 2012
- International Expert Panel on Multilingual Children’s Speech (IEPMCS). Multilingual Children with Speech Sound Disorders: Position Paper. Bathurst, NSW, Australia: Research Institute for Professional Practice, Learning and Education (RIPPLE), Charles Sturt University, 2012. [Google Scholar]
Joffe 2008
- Joffe V, Pring T. Children with phonological problems: a survey of clinical practice. International Journal of Language and Communication Disorders 2008;43(2):154‐64. [DOI] [PubMed] [Google Scholar]
Juni 2001
- Juni P, Altman DG, Egger M. Assessing the quality of randomized controlled trials. In: Egger M, Smith GD, Altman DG editor(s). Systematic Reviews in Health Care: Meta‐Analysis in Context. London: BMJ Books, 2001:87‐108. [Google Scholar]
Kamhi 2008
- Kamhi AG. A meme's‐eye view of nonspeech oral‐motor exercises. Seminars in Speech and Language 2008;29(4):331‐8. [DOI] [PubMed] [Google Scholar]
Kresheck 1989
- Kresheck JD. Structured Photographic Articulation Test‐Dudsberry. Sandwich, IL: Janelle Publications, Inc, 1989. [Google Scholar]
Lass 2008
- Lass NJ, Pannbacker M. The application of evidence‐based practice to nonspeech oral motor treatments. Language, Speech, and Hearing Services in Schools 2008;39:408‐21. [DOI] [PubMed] [Google Scholar]
Law 2003
- Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD004110] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lof 2003
- Lof GL. Oral motor exercises and treatment outcomes. Perspectives on Language, Learning, and Education 2003;10(1):7‐11. [Google Scholar]
Lof 2008
- Lof GL. Controversies surrounding nonspeech oral motor exercises for childhood speech disorders. Seminars in Speech and Language 2008;29(4):253‐5. [DOI] [PubMed] [Google Scholar]
Lof 2009
- Lof GL. The nonspeech‐oral motor exercise phenomenon in speech pathology practice. In: Bowen C editor(s). Children's Speech Sound Disorders. West Sussex: Wiley‐Blackwell, 2009:180‐4. [Google Scholar]
Lof 2010
- Lof GL, Watson M. Five reasons why nonspeech oral motor exercises (NSOME) do not work. Perspectives on School‐Based Issues 2010;11:109‐17. [Google Scholar]
Mackie 1996
- Mackie E. Oral Motor Activities for School‐Aged Children. East Moline, IL: LinguiSystems, 1996. [Google Scholar]
Marshalla 2000
- Marshalla P. Oral‐Motor Techniques in Articulation and Phonological Therapy. Kirkland, WA: Marshall Speech and Language, 2000. [Google Scholar]
McCauley 2009
- McCauley RJ, Strand E, Lof GL, Schooling T, Frymark T. Evidence‐based systematic review: effects of nonspeech oral motor exercises on speech. American Journal of Speech‐Language Pathology 2009;18(4):343‐60. [DOI] [PubMed] [Google Scholar]
McLeod 2014
- McLeod S, Baker E. Speech‐language pathologists' practices regarding assessment, analysis, target selection, intervention, and service delivery for children with speech sound disorders. Clinical Linguistics and Phonetics 2014;28(7‐8):508‐31. [DOI] [PubMed] [Google Scholar]
Morgan 2008a
- Morgan AT, Vogel AP. Intervention for childhood apraxia of speech. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD006278.pub2] [DOI] [PubMed] [Google Scholar]
Morgan 2008b
- Morgan AT, Vogel AP. Intervention for dysarthria associated with acquired brain injury in children and adolescents. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD006279.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2009
- Nelson LK. Research in Communication Sciences and Disorders. San Diego: Plural Publishing Inc, 2009. [Google Scholar]
Review Manager [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Robey 2004
- Robey RR. A five‐phase model for clinical‐outcome research. Journal of Communication Disorders 2004;37(5):401‐11. [DOI] [PubMed] [Google Scholar]
Rosenfeld‐Johnson 2001
- Rosenfeld‐Johnson S. Oral‐Motor Exercises for Speech Clarity. Tucson, AZ: Innovative Therapists, 2001. [Google Scholar]
Rosenfeld‐Johnson 2009
- Rosenfeld‐Johnson S. Oral Placement Therapy for /S/ and /Z/. Tucson, AZ: Talk Tools, 2009. [Google Scholar]
Ruscello 2008a
- Ruscello DM. Treating Articulation and Phonological Disorders in Children. St. Louis: Elsevier, 2008. [Google Scholar]
Ruscello 2008b
- Ruscello DM. Nonspeech oral motor treatment issues related to children with developmental speech sound disorders. Language, Speech, and Hearing Services in Schools 2008;39(3):380‐91. [DOI] [PubMed] [Google Scholar]
Ruscello 2008c
- Ruscello DM. An examination of nonspeech oral motor exercises for children with velopharyngeal inadequacy. Seminars in Speech and Language 2008;29(4):294‐303. [DOI] [PubMed] [Google Scholar]
Ruscello 2010
- Ruscello DM. Collective findings neither support nor refute the use of oral motor exercises as a treatment for speech sound disorders. Evidence‐Based Communication Assessment and Intervention 2010;4(2):65‐72. [Google Scholar]
Shriberg 1994
- Shriberg LD, Kwiatkowski J. Developmental phonological disorders. I: a clinical profile. Journal of Speech and Hearing Research 1994;37(5):1100‐26. [DOI] [PubMed] [Google Scholar]
Shriberg 2010
- Shriberg LD, Fourakis M, Hall SD, Karlsson HB, Lohmeier HL, McSweeny JL, et al. Extensions to the Speech Disorders Classification System (SDCS). Clinical Linguistics and Phonetics 2010;24(10):795‐824. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sibbald 1998
- Sibbald B, Roberts C. Understanding controlled trials. Crossover trials. BMJ 1998;316(7146):1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2010
- Williams AL, McLeod S, McCauley RJ. Introduction to interventions for speech sound disorders in children. In: Williams AL, McLeod S, McCauley RJ editor(s). Interventions for Speech Sound Disorders in Children. Baltimore, MD: Paul H. Brookes Publishing, 2010:1‐26. [Google Scholar]
References to other published versions of this review
Lee 2011
- Lee AS‐Y, Gibbon FE. Non‐speech oral motor treatment for developmental speech sound disorders in children. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD009383] [DOI] [PMC free article] [PubMed] [Google Scholar]


