Abstract
This study examined the differences in health spending within the World Health Organization (WHO) Europe region by comparing the EU15, the EU post-2004, CIS, EU Candidate and CARINFONET countries. The WHO European Region (53 countries) has been divided into the following sub-groups: EU15, EU post-2004, CIS, EU Candidate countries and CARINFONET countries. The study period, based on the availability of WHO Global Health expenditure data, was 1995 to 2014. EU15 countries have exhibited the strongest growth in total health spending both in nominal and purchasing power parity terms. The dynamics of CIS members’ private sector expenditure growth as a percentage of GDP change has exceeded that of other groups. Private sector expenditure on health as a percentage of total government expenditure, has steadily the highest percentage point share among CARINFONET countries. Furthermore, private households’ out-of-pocket payments on health as a percentage of total health expenditure, has been dominated by Central Asian republics for most of the period, although, for the period 2010 to 2014, the latter have tended to converge with those of CIS countries. Western EU15 nations have shown a serious growth of health expenditure far exceeding their pace of real economic growth in the long run. There is concerning growth of private health spending among the CIS and CARINFONET nations. It reflects growing citizen vulnerability in terms of questionable affordability of healthcare. Health care investment capability has grown most substantially in the Russian Federation, Turkey and Poland being the classical examples of emerging markets.
Keywords: health economics, WHO, Europe, public health expenditure, private health expenditure
1. Introduction
Healthcare spending became a matter of academic attention in the early works of the American economists Milton Friedman [1] and Selma Mushkin [2] ranging from the early 1920s until the early 1950s. These publications are counted among the historical beginnings of the interdisciplinary knowledge, which became known as the science of health economics [3]. Why did it all begin in the U.S., given the fact that early institutionalized national health systems had roots in Europe from the XIX (19th) century? In the U.S., since the 1840s up to the 1960s, according to available historical archives, there was a steady and parallel growth of the average industry worker’s net salary and the price of an ordinary physician examination [4]. After the 1950s, due to an array of socioeconomic changes and technology driven causes, these two trends became divergent leading to obvious disparity [5]. European nations, experiencing consecutive industrial revolutions were expanding their health care coverage within their nations very gradually. During the early years of Bismarck’s leadership, healthcare was provided only for industrial workers and their families from 1883 [6]. Beveridge evolved in the British mainland and its overseas colonies with some distinctive advantages being introduced around 1911 [7,8]. Surprisingly, the very first world’s healthcare system delivering universal health coverage for all its citizens including the poorest ones, at the level of medical technology of its time, was Soviet Semashko back in the early 1930s [9,10].
Today in Europe, North America and many other industrialized contemporary societies of Asia, real gross domestic product (GDP) growth is almost twice as slow as the long-term growth of total health expenditure [5]. The most commonly cited causes for health expenditure growth are advances in medical technology and pharmaceutical innovation [11], population aging [12], blossoming of non-communicable “prosperity” diseases [13] and growing citizen expectations [14]. A deeper understanding of long-term health expenditure patterns across geographies and jurisdictions might be essential for shaping responses to this challenge in the future [15].
This study aimed to reveal and explain the causes of underlying differences in health spending within the World Health Organization (WHO) Europe region by comparing the EU15, the EU post-2004, Commonwealth of Independent States (CIS) [16], EU Candidate and Central Asian Republics Information Network (CARINFONET) countries. This article contributes to the literature in several ways. Firstly, the studies on comparative research of healthcare systems have been rather limited to the Post-Soviet cultural space [15,17] outside the Russian language literature [18,19,20]. Secondly, it has added to the research on institutional change, which has been ongoing within the WHO Europe region since 1990 [21]. This concept of “transition” [22] from socialist centrally-planned economies, towards market-driven capitalist societies took place after the end of the Cold War era throughout the 1990s [23] and 2000s [24] alongside accelerated globalisation. This process had a profound impact on healthcare establishments [25], which is further explored alongside several distinctive development pathways.
Apparently, 45 years of the Cold War era [26] and consecutive accelerated globalisation [27] since 1991, has left a deep imprint on many spheres of life including healthcare systems [28]. Today, the major transnational associations on the continent are the European Union and the Commonwealth of Independent States as a legal successor authority of the Union of Soviet Socialist Republics (USSR) [29]. There are as well, other countries with various degrees of legislative proximity to one or another. The free-market or centrally-planned economic system establishment [30], prior to 1989 has had a profound impact on healthcare provision and financing patterns [25].
2. Materials and Methods
The geopolitical landscape within the WHO Europe Region comprising 53 countries and a total of 800+ million people was observed here by delineating specific groups of nations. Therefore, the WHO European Region was split into a total of five groups of nations (Table 1): EU15 (members of the European Union prior to 2004, having the established free-market economies since the Cold War era), the EU post-2004 (mostly former socialist, centrally-planned economies with the exceptions of Malta and Cyprus), the CIS (Commonwealth of Independent States with membership similar to 1991, due to the fact that all these countries shared the same Semashko healthcare systems), EU Candidate countries (consisting of former Yugoslavia republics/Western Balkans and Turkey) and CARINFONET countries (Central Asian nations, most of them members of the CIS, but represented a distinct subgroup of nations due to their shared socioeconomic characteristics.
Table 1.
List of country groups observed.
| EU15 | EU Post-2004 | CIS * | CARINFONET ** | EU Candidate Countries |
|---|---|---|---|---|
| Austria AUT | Bulgaria BGR | Armenia ARM | Kazakhstan KAZ | Albania ALB |
| Belgium BEL | Croatia HRV | Azerbaijan AZE | Kyrgyzstan KGZ | Montenegro MNE |
| Denmark DNK | Cyprus CYP | Belarus BLR | Tajikistan TJK | Serbia SRB |
| Finland FIN | Czech Republic CZE | Kazakhstan KAZ | Turkmenistan TKM | The former Yugoslav Republic of Macedonia MKD |
| France FRA | Estonia EST | Kyrgyzstan KGZ | Uzbekistan UZB | Turkey TUR |
| Germany DEU | Hungary HUN | Republic of Moldova MDA | Bosnia and Herzegovina BIH | |
| Greece GRC | Latvia LVA | Russian Federation RUS | ||
| Ireland IRL | Lithuania LTU | Tajikistan TJK | ||
| Italy ITA | Malta MLT | Turkmenistan TKM | ||
| Luxembourg LUX | Poland POL | Ukraine UKR | ||
| Netherlands NLD | Romania ROU | Uzbekistan UZB | ||
| Portugal PRT | Slovakia SVK | |||
| Spain ESP | Slovenia SVN | |||
| Sweden SWE | ||||
| United Kingdom GBR |
Note: * The Commonwealth of Independent States (CIS) formed when the former Soviet Union dissolved in 1991. ** CARINFONET (Central Asian Republics Information Network) Steering Group.
The selected indicators of health spending were: total health expenditure as a percentage of Gross Domestic Product (GDP); public sector expenditure on health as a percentage of GDP; private sector expenditure on health as a percentage of GDP; total health expenditure, purchasing power parity, USD per capita; public expenditure on health, purchasing power parity, USD per capita; public sector expenditure on health as a percentage of total government expenditure; private households’ out-of-pocket payments on health as a percentage of total health expenditure. While the WHO and The Organisation for Economic Co-operation and Development (OECD) estimates were used for the first indicator, the WHO estimates were only utilized for the others.
The data source selected, among OECD Health, EuroStat, World Bank Health Data and a few other similar sources, was the WHO Global Health Expenditure Database due to its broadest possible coverage of political entities and highly reliable methodology of data collection giving insight into the exact fiscal flows within various national health systems [31]. The time horizon observed was 1995–2014 for most of the indicators, due to data gaps in chronology for the earlier years. For total health expenditure, expressed as a percentage of GDP, and public health spending, the time horizon was 1990–2014. Coverage of all observed nations, with these aggregate data, was complete and no significant data gaps were present.
Whenever possible, the OECD definition of total health expenditure was applied in this study (for details see [32], p. 89). It consisted of: household health expenses, including goods and services purchased at the consumer’s own initiative and the cost sharing part of publicly financed or supplied care; government-supplied health services, including those in schools, prisons and armed forces and special public health programs such as vaccination; investment in clinics, laboratories, etc.; administration costs; research and development, excluding outlays by pharmaceutical firms; industrial medicine; outlays of voluntary and benevolent institutions. In the case of most central and eastern European countries, the following had to be included: direct state budget allocated to the health sector, state subsidies to the mandatory health insurance system; mandatory health insurance contributions by employers and employees; direct health expenditure of employers for running industrial medical facilities; direct health expenditures of ministries and governmental agencies; charity health expenditures; foreign assistance; outstanding debt at the end of the year; private health insurance and direct private health charges [33]. It is important to ensure that funding from the general budget revenues and health insurance contributions do not overlap [34].
3. Results
The first part of the analysis reported in this section was related to the GDP of the five groups of nations. This data presented was estimated by the WHO.
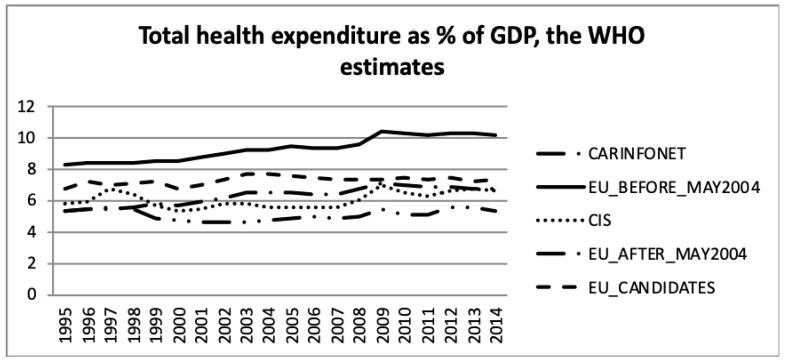
Figure 1 and Figure 2 present the total health expenditure as a percentage of GDP. Total health expenditures are the sum of general government expenditure on health and private expenditure on health.
Figure 1.
Total health expenditure as a percentage of Gross Domestic Product, the World Health Organization estimates.
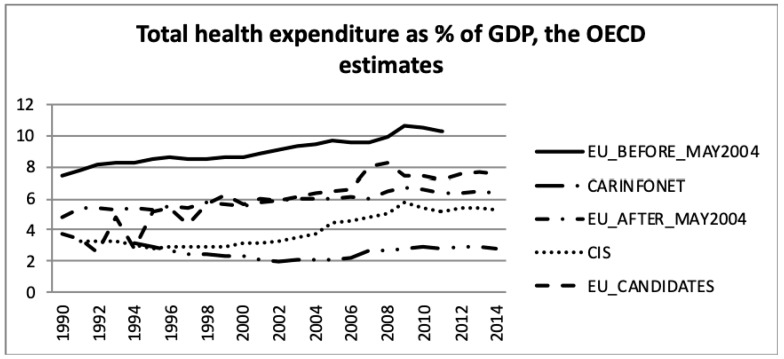
Figure 2.
Total health expenditure as a percentage of Gross Domestic Product (GDP), the Organisation for Economic Co-operation and Development (OECD) estimates.
The data of Figure 2, for OECD member states, was taken from the OECD Health Database [35]. For non-OECD countries, the data was as reported by the country in the European Health for All database (HFA-DB) [36] and may not have necessarily corresponded to the common WHO or OECD definition [37].
Comparing the health expenditure as a percentage of GDP, presented in Figure 1 and Figure 2, the data of EU_Candidates differed significantly between both sources. There was a gap in the data as shown in Figure 2 for the year 2011 and later for the EU_Before_May2004 group of nations. Nevertheless, both estimates showed that health expenditure was a greater share of GDP for the EU_Before_May2004 group of nations, and lower for the CARINFONET group. The EU_Before_May2004 group of nations had an increase in health expenditure as a percentage of GDP according to both data sources. Meanwhile, the EU_After_May2004, CIS and EU_Candidates also showed an increase in health expenditure as a proportion of GDP, but only in Figure 2, not confirmed by the WHO estimates (Figure 1).
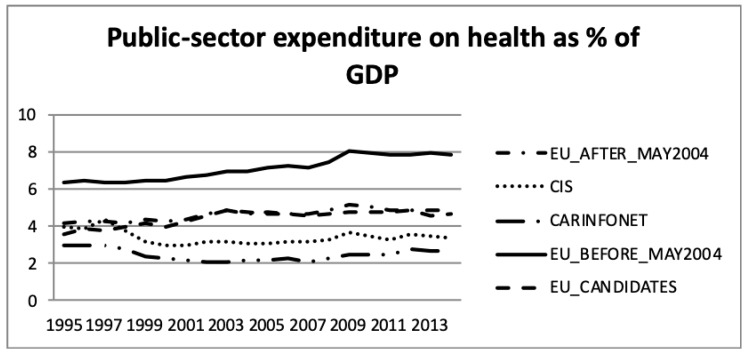
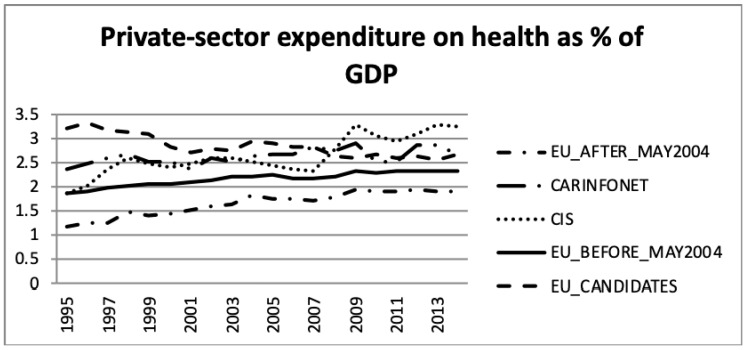
Concerning the comparison between public- and private sector expenditure on health as a percentage of GDP, Figure 3 and Figure 4 present the WHO estimates.
Figure 3.
Public and private sector expenditure on health as a percentage of Gross Domestic Product (GDP), the World Health Organization estimates.
Figure 4.
Public and private sector expenditure on health as a percentage of Gross Domestic Product (GDP), the World Health Organization estimates.
For the EU_Before_May2004 group of nations both public- and private sector expenditure on health, as a percentage of GDP increased by two and 0.5 percentage points, respectively. This was in accordance with the increase of the total health expenditure presented in Figure 1 and Figure 2. This group had the highest public sector expenditure and the second lowest private sector expenditure among the five groups of nations. However, this group of nations had an increase in investment until 2009, which stabilised after 2009.
The EU_After_May2004 group showed a similar tendency in public- and private sector expenditure on health, as a percentage of GDP, as the other EU nations. Health expenditure, however, accounted for a lower proportion of GDP for this group of countries.
These data show that the EU member nations—both those who were members before and after May 2004—experienced increasing health expenditure GDP shares until 2009, but thereafter health expenditure accounted for a stable share of the economy. A comparison of Figure 1 and Figure 2 shows that the public sector health expenditure of each group was three to four times larger than the respective private expenditure share.
Concerning the CIS and CARINFONET groups of nations, they presented a similar pattern in the total health expenditure, as a percentage of GDP, both in public and private sectors. Nevertheless, the CARINFONET had a generally lower investment in healthcare, and in public spending, of about one point in percentage point share terms. Concerning the private investment, they presented a similar level of investment (by the percentage of GDP). However, the CIS group significantly increased their private investment in 1995–1998 and 2008–2009. The CIS group of nations (which included the CARINFONET group) had a stabilised level of total investment (about 6% of GDP). The public sector expenditure remained stabilised between 3% and 4% of GDP, meanwhile the private sector expenditure increased from 2% to more than 3% of GDP. The public and private expenditure appeared to be balanced under the CIS group of nations.
Concerning the EU_Candidate countries, the public sector expenditure on health remained stable, but the private sector suffered a decrease of almost one percentage point from 3.2% to 2.5% of GDP. This trend of lower expenditure in the private sector, among the EU Candidate economies, was opposite as a tendency with regard to the other groups of nations. The EU_Candidates private expenditure seemed to follow an approximation to the level of private expenditure of the EU nations.
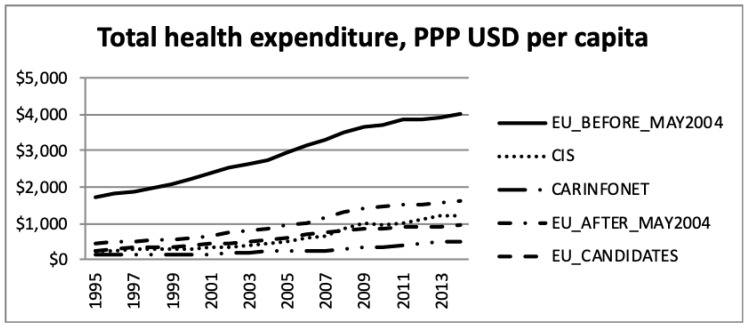
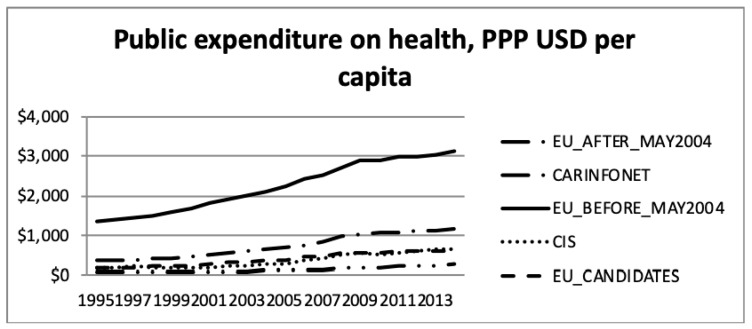
The total health expenditure, purchasing power parity (PPP), in USD per capita, and the public sector expenditure on health, purchasing power parity, in USD per capita, according to the WHO estimates, is presented in Figure 5 and Figure 6.
Figure 5.
Total health expenditure, purchasing power parity (USD) per capita, the World Health Organisation estimates. Note:
Figure 6.
Public health expenditure, purchasing power parity (USD) per capita, the World Health Organisation estimates.
The data presented in Figure 5 and Figure 6 are net values, not considering the GDP and inflation, during the period. Therefore, this increase should be read under this consideration. Thus, the increase in total and public sector expenditure on health during the period 1995 to 2013, should be regarded considering the inflation. The different level of expenditure among groups of nations showed a significantly higher expenditure for EU Members prior to May 2004. However, this difference should be regarded in the face of different levels of costs, among the groups of nations, for the same type of operation/product. In this group the price of medical care was generally higher than in the other groups of nations.
In absolute nominal monetary terms, Western European EU15 countries have exhibited the strongest upward growth in total health spending. Observing the purchasing power parity landscape [38], the EU15 nations were mostly outperforming their counterparts in Eastern Europe, the Balkans and Central Asia, not only in the public sector, but also in total.
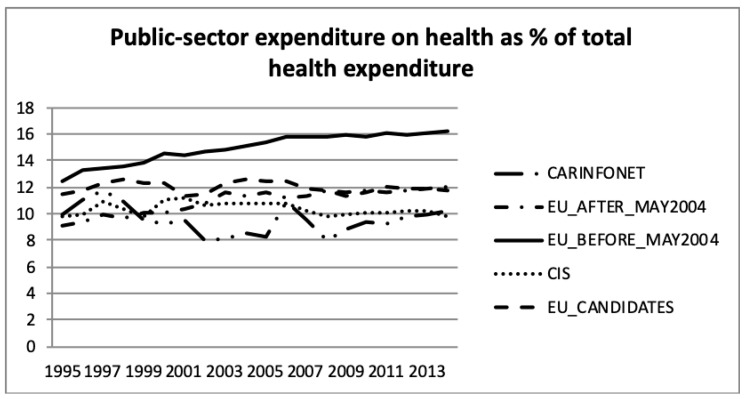
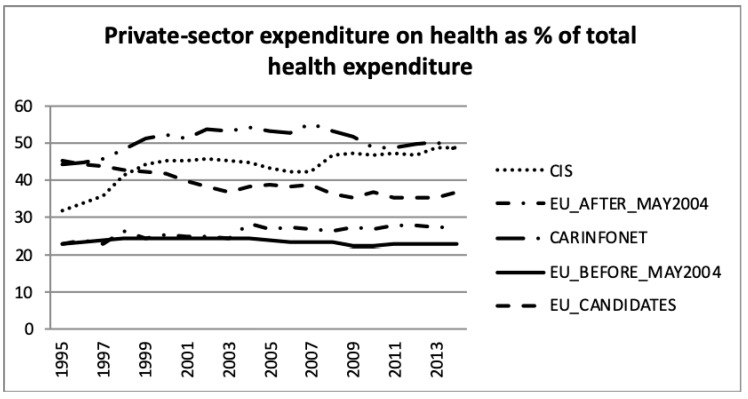
Figure 7 and Figure 8 present the public- and private sector expenditure on health, as a percentage of total health expenditure, according to the WHO estimates. This information was in accordance with public sector expenditure on health, as a percentage of GDP, presented in Figure 2, but showed the government expenditure in public sector health. It can be seen that the EU_Before_May2004 group of nations had a higher investment in health than the other groups. The EU_Before and After_May2004 had an increase until 2009, but after that it remained stable until 2013, about 16% for EU_Before_May2004 and 12% for EU_After_May2004. The EU_Candidates aligned the public sector expenditure on health with EU_After_May2004 since 2008. The CIS group of nations had a stabilised effort on expenditure in the public health sector of around 10% of total government expenditure. The CARINFONET group of nations had several fluctuations of public sector expenditure between 1995 and 2013.
Figure 7.
Public sector expenditure on health as a percentage of total health expenditure, the World Health Organisation estimates.
Figure 8.
Private sector expenditure on health as a percentage of total health expenditure, the World Health Organisation estimates.
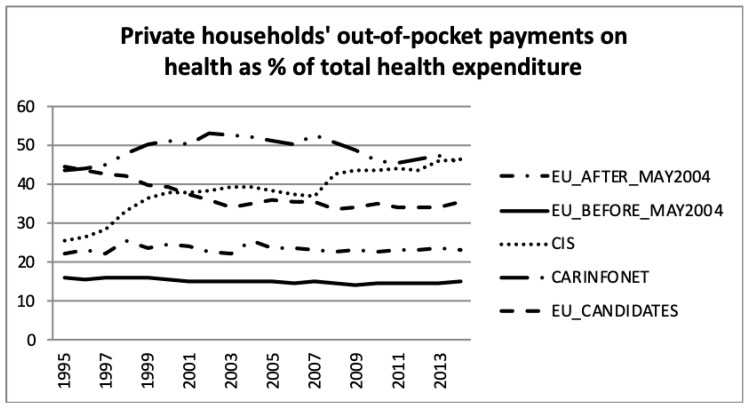
Figure 9 presents the private households’ out-of-pocket payments on health as a percentage of total health expenditure for the five groups of nations. This feature was dominated by the Central Asian republics (CARINFONET) for most of the period, shared with CIS values in latter years. The EU_Before_May2004 and EU After_May2004 presented a lower and stable level of private households’ out-of-pocket spending on health, which was around 15% and 23% of total health expenditure, respectively. These results were in accordance with previous analysis of Figure 4, Figure 5 and Figure 6. The EU_Candidates’ group of nations made an effort to reduce its expenditure in this category and stabilised after 2003, to around 33% to 36% of total health expenditure.
Figure 9.
Private households’ out-of-pocket payments on health as a percentage of total health expenditure, the World Health Organisation estimates.
4. Study Limitations
One of the possible methodological weaknesses of this study is the fact that reported annual values of health spending by the major multilateral agencies such as the World Bank (WB) and OECD Health may differ to a minor extent (up to +/− few percentage point shares). Geoeconomic division of WHO European region into the five observed regions might be questioned to some extent, alongside other major division lines separating diverse health financing and provision traditions across Europe. One such possible division that might be objected to as an alternative core criterion is the separation of the European health systems to Bismarck, Beveridge and Semashko route models, following their historical order of appearance. Estimates for total expenditure on health produced by the WHO were reliable to the greatest extent possible, based on the National Health Accounts [39] classification [40]. The sources included both nationally reported data and estimates from international organisations namely: WHO, the United Nations (UN), the International Monetary Fund (IMF), WB and OECD. Therefore, they may differ somewhat from official national statistics reported by countries [41]. The WHO estimates for this indicator are generally more accurate [42]. Therefore, the authors worked with the best publicly accessible data for international comparisons of inherently different economic systems. However, the core findings of the study should not be questioned based on these minor differences in accounting practices across jurisdictions.
5. Discussion
The historical legacy of the Cold War era and accelerated globalisation in the post-1989 period, has shaped economic systems throughout the European continent. During this process, several distinctive geopolitical [43] and economic zones have emerged [44,45]. This research has explored the best publicly accessible international data sources on the long-term evolution of healthcare-related spending. Comparison of these five groups of nations, sharing significant internal similarities, reveals surprising findings which so far, remain unpublished in literature [46].
Since a lengthy time period was explored, there were roughly two different stages of historical evolution particularly prominent on the eastern side of the former Iron Curtain frontier. For most of the 1990s the entire Eastern Europe, being mutually interdependent with the former USSR, was dragged into the new Russian recession, bottoming out in 1998. This heavily reflected on demographic trends of the time, healthcare investment and its outcomes in most of the former socialist countries. This early transitional period was marked with difficulties, even with quite successful health reforms, such as the Polish [47], Hungarian [48] or Czech ones [49]. In the civil wars of the former Yugoslavia, sanctions and waves of refugee migration devastated economies and led to a decade-long delay in significant health reforms and spending growth [50]. This was most prominent in the largest country of the region, Serbia [51], acting as the historical core for Yugoslavia after World War I and World War II [12]. Turkey had a rather slower pace of essential health system progress back in the 1990s [52].
The second, far more prosperous period, roughly began in the early 2000s, for most of the Eastern European [53,54] and Balkan nations [55]. Since the beginning of the XXI (19th) century, just like the Russian Federation’s [9], Turkey’s overall development and ability to increase health expenditure was growing much faster in comparison to the high-income OECD economies [56]. The contemporary Turkish health system delivered surprisingly well-balanced, and, to a large degree, cost-effective spending mechanisms, leading to limited inequalities and medical care affordability [57].
The high-income Western European EU15 nations had rather steady and satisfactory, overall economic growth spanning from 1989 to 2007 [58]. However, between 1990 and 2014, these rich countries exhibited an exceptionally alarming rate of health spending growth, even when their real GDP growth was taken into account [59]. This means that public cost containment policies, conducted over the past thirty years, have been largely ineffective in dealing with this challenge [60]. Accelerated and advanced stage population aging [61] remains particularly prominent in Western, Northern and Central Europe [62]. One should emphasize here that this core driver of health-spending remains slightly less influential in Eastern European societies compared to EU15. This is due to the fact that population-aging evolution, in Eastern Europe, is at an earlier stage, as was recently documented in UN datasets, comprising data from the previous century [63]. Furthermore, the Russian Federation’s early 2000s fertility-supportive policies gained momentum with a recent RANEPA report [64] claiming total fertility growth rate [65], on average, from 1.3 to 1.7 children per woman, over a decade long perspective [64]. Another fact is that life expectancies remain significantly lower across the CIS nations [66] with men living shorter lives than women [67]. However, exploring the core investment–output ration between health spending and longevity, throughout the vast Eastern EU-post-2004, the Balkans and CIS region provide another surprising perspective. Life expectancy gains in South-East Europe [68] were quite similar to EU-post-2004 members at a far lower healthcare investment increase [69]. Furthermore, the CIS relationship curve, between current total health expenditure and longevity growth margin, although positioned in the lower quadrant, in comparison to the other two regions, has the steepest upward pathway, promising improvement in the future [70].
Therefore, it seems that the EU nations (before and after May 2004), had an increase of expenditures as a percentage of GDP until 2009, but stopped the further growth after this year [71]. This is clearly attributable to the fiscal austerity policies triggered by the Global Recession, following the bankruptcy of the Lehman Brothers in 2007 [72]. Such strategies were centrally designated by the European Commission among EU members [73] and EU Candidate countries to a lesser extent [74]. The lasting macroeconomic crisis effects, between 2007 and 2016, contributed significantly to the worsening of health financing sustainability. A recent Brookings Institute report, based on World Bank data, claims the beginnings of sustainable global economic growth in 2017 and 2018 [75]. Their estimates are that one half of this real GDP growth, worldwide, remains to be driven by seven major Emerging Markets or EM7 (BRICS + Mexico, Indonesia and Turkey), while only a quarter by G7 nations on the time horizon 2017–2020 [76]. These promising signs give hope for a European-wide ability to invest more in health, which should be recovered in the near future. This refers to not only nominal and purchasing power parity spending, but also percentage point share of real disposable GDP.
6. Conclusions
Regardless of some grounds for optimism, there is a prevailing consensus among health policy authorities in the EU and Eurasian Union, CIS and WHO Europe alike, that health financing efficiency will have to be substantially improved. The core underlying assumption of all European health system establishments, since their late XIX century creation, was a demographic growth model. This postulate has now changed in Europe and worldwide, with the advent and acceleration of global population aging. A shrinking workforce and contracted tax base in the labor market are constraining the supply-side of modern-day societies’ ability to invest in medical care. The demand-side is burdened by the spreading of non-communicable diseases, demand for long-term, home-based care, family caregiving and prohibitively expensive last-year-of-life, amounting to the entire lifetime medical consumption of a citizen. Given these core drivers in the equation, technological innovation in medicine, and consecutive public demand for cutting-edge technologies remain far less containable areas by cost-effective resource allocation policies. These challenges, alongside fiscal constraints, are shared across the East and West of the European continent in the long run. Hopefully, these vast regions will be able to learn from each other’s distinctive historical experiences and create more adaptive system responses in the future.
Author Contributions
M.J., P.O.F., and J.P.T., were responsible for the study design and research questions definition; N.R., acquired the data; M.J., N.R., Y.T. and V.R. provided administrative, technical, or logistic support; M.J., P.O.F., J.P.T.,Y.T. and V.R. provided interpretation of analysis; M.J., P.O.F., J.P.T., N.R., Y.T. and V.R., did the drafting and critical drafting of the manuscript, respectively; M.J. and P.O.F., obtained funding; M.J., was responsible for supervision and coordination of the joint efforts. All authors participated sufficiently in the work to take public responsibility for the appropriate portions of the content. All authors have read and approved the final manuscript.
Funding
This research was financially supported by the Bilateral Intergovernmental Grant Serbia–Portugal Grant number 451-03-1924/2016-09/13 and Serbian Ministry of Education Science and Technological Development Grant OI 175 014.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Kuznets S., Friedman M. Incomes from Independent Professional Practice. NBER; Berkshire, UK: 1939. Incomes from Independent Professional Practice, 1929–1936. [Google Scholar]
- 2.Mushkin S.J. Toward a definition of health economics. Public Health Rep. 1958;73:785–794. doi: 10.2307/4590242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jakovljevic M.B., Ogura S. Health economics at the crossroads of centuries—From the past to the future. Front. Public Health. 2016;4:115. doi: 10.3389/fpubh.2016.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Getzen T.E. Medical care price indexes: Theory, construction & empirical analysis of the US series 1927–1990. Adv. Health Econ. Health Serv. Res. 1992;13:83–128. [PubMed] [Google Scholar]
- 5.Smith S., Newhouse J.P., Freeland M.S. Income, insurance, and technology: Why does health spending outpace economic growth? Health Aff. 2009;28:1276–1284. doi: 10.1377/hlthaff.28.5.1276. [DOI] [PubMed] [Google Scholar]
- 6.Bärnighausen T., Sauerborn R. One hundred and eighteen years of the German health insurance system: Are there any lessons for middle-and low-income countries? Soc. Sci. Med. 2002;54:1559–1587. doi: 10.1016/S0277-9536(01)00137-X. [DOI] [PubMed] [Google Scholar]
- 7.Grimes S.S. The British National Health Service: State Intervention in the Medical Marketplace, 1911–1948. Routledge; London, UK: 2016. [Google Scholar]
- 8.Kutzin J., Ibraimova A., Jakab M., O’Dougherty S. Bismarck meets Beveridge on the Silk Road: Coordinating funding sources to create a universal health financing system in Kyrgyzstan. Bull. World Health Organ. 2009;87:549–554. doi: 10.2471/BLT.07.049544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jakovljevic M., Potapchik E., Popovich L., Barik D., Getzen T.E. Evolving health expenditure landscape of the BRICS nations and projections to 2025. Health Econ. 2017;26:844–852. doi: 10.1002/hec.3406. [DOI] [PubMed] [Google Scholar]
- 10.Arsentyev E.V., Reshetnikov V.A. To the biography of N.A. Semashko: The activities of the first Commissar of Health in 1920–1925. Soc. Hist. Med. 2018;3:183–192. [Google Scholar]
- 11.Cutler D.M., McClellan M. Is technological change in medicine worth it? Health Aff. 2001;20:11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- 12.Ogura S., Jakovljevic M.B. Health financing constrained by population aging—An opportunity to learn from Japanese experience. Serb. J. Exp. Clin. Res. 2014;15:175–181. doi: 10.2478/sjecr-2014-0022. [DOI] [Google Scholar]
- 13.Jakovljevic M.B., Milovanovic O. Growing burden of non-communicable diseases in the emerging health markets: The case of BRICS. Front. Public Health. 2015;3:65. doi: 10.3389/fpubh.2015.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parente S.T., Feldman R., Christianson J.B. Evaluation of the effect of a consumer-driven health plan on medical care expenditures and utilization. Health Serv. Res. 2004;39:1189–1210. doi: 10.1111/j.1475-6773.2004.00282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Footman K., Roberts B., Mills A., Richardson E., McKee M. Public satisfaction as a measure of health system performance: A study of nine countries in the former Soviet Union. Health Policy. 2013;112:62–69. doi: 10.1016/j.healthpol.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Bonilla-Chacin M.E., Murrugarra E., Temourov M. Health care during transition and health systems reform: Evidence from the poorest CIS countries. Soc. Policy Adm. 2005;39:381–408. doi: 10.1111/j.1467-9515.2005.00446.x. [DOI] [Google Scholar]
- 17.Groenewegen P.P., Dourgnon P., Greß S., Jurgutis A., Willems S. Strengthening weak primary care systems: Steps towards stronger primary care in selected Western and Eastern European countries. Health Policy. 2013;113:170–179. doi: 10.1016/j.healthpol.2013.05.024. [DOI] [PubMed] [Google Scholar]
- 18.Mechanick A. Пирамида Семашко [The Pyramid of Semashko] Expert. 2011;30/31:68–72. (In Russian) [Google Scholar]
- 19.Ulumbekova G.E. Здравоохранение России. Что надо делать: научное обоснование «Стратегии развития здравоохранения РФ до 2020 года» [Healthcare of Russia. What to do: The Scientific Rationale of the “Strategy for the development of healthcare in the Russian Federation until 2020”] Mosc. Geotar-Media. 2010:1–96. (In Russian) [Google Scholar]
- 20.Manerova O.A., Drygin D.M., Davydov P.K. Актуальные Вопросы Подготовки Медицинских Кадров: к 140-Летию со Дня Рождения Н.А. Семашко [Topical Issues Concerning Medical Training: Devoted the 140th Anniversary of the Birth N.A. Semashko] [(accessed on 20 July 2014)]; Available online: https://historymedjournal.com/volume/number_3/3-2014__Manerova_Dpigin_Davidov_aktual%20voprosi.pdf.
- 21.Fleck F. Rocky road from the Semashko to a new health model. World Health Organization. Bull. World Health Organ. 2013;91:320–321. doi: 10.2471/BLT.13.030513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borisova L.V. Health care systems as determinants of health outcomes in transition countries: Developing classification. Soc. Theory Health. 2011;9:326–354. doi: 10.1057/sth.2011.14. [DOI] [Google Scholar]
- 23.Habibov N.N., Afandi E.N. Self-rated health and social capital in transitional countries: Multilevel analysis of comparative surveys in Armenia, Azerbaijan, and Georgia. Soc. Sci. Med. 2011;72:1193–1204. doi: 10.1016/j.socscimed.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 24.Borowitz M., Atun R. The unfinished journey from Semashko to Bismarck: Health reform in Central Asia from 1991 to 2006. Central Asian Surv. 2006;25:419–440. doi: 10.1080/02634930701210633. [DOI] [Google Scholar]
- 25.Jakovljevic M.B., Arsenijevic J., Pavlova M., Verhaeghe N., Laaser U., Groot W. Within the triangle of healthcare legacies: Comparing the performance of South-Eastern European health systems. J. Med. Econ. 2017;20:483–492. doi: 10.1080/13696998.2016.1277228. [DOI] [PubMed] [Google Scholar]
- 26.Rapkin D.P., Thompson W.R., Christopherson J.A. Bipolarity and bipolarization in the Cold War era: Conceptualization, measurement, and validation. J. Confl. Resolut. 1979;23:261–295. doi: 10.1177/002200277902300203. [DOI] [Google Scholar]
- 27.Farazmand A. Public organizations in the age of accelerated globalization. Public Organ. Rev. 2001;1:5–11. doi: 10.1023/A:1011592426725. [DOI] [Google Scholar]
- 28.Cueto M. The origins of primary health care and selective primary health care. Am. J. Public Health. 2004;94:1864–1874. doi: 10.2105/AJPH.94.11.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rowland D., Telyukov A.V. Soviet health care from two perspectives. Health Aff. 1991;10:71–86. doi: 10.1377/hlthaff.10.3.71. [DOI] [PubMed] [Google Scholar]
- 30.Rhodes M., Van Apeldoorn B. Developments in West European Politics. Palgrave; London, UK: 1997. Capitalism versus capitalism in Western Europe; pp. 171–189. [Google Scholar]
- 31.WHO Global Health Expenditure Database. [(accessed on 5 August 2019)]; Available online: http://apps.who.int/nha/database.
- 32.OECD Reviews of Health Systems: A Series of Country Reports. [(accessed on 5 August 2019)]; Available online: https://www.oecd.org/els/health-systems/reviews-health-systems.htm.
- 33.OECD Improving Estimates of Spending on Administration. [(accessed on 5 August 2019)]; Available online: https://www.oecd.org/els/health-systems/Improving-Estimates-of-Spending-on-Administration.pdf.
- 34.OECD Classification of Health Care Financing Schemes (ICHA-HF) [(accessed on 5 August 2019)]; Available online: https://www.oecd-ilibrary.org/docserver/9789264270985-9-en.pdf?expires=1555511574&id=id&accname=guest&checksum=6D1A3B7F7058293A58BD2831DA3845B2.
- 35.OECD Health Statistics 2018. [(accessed on 5 August 2019)]; Available online: http://www.oecd.org/els/health-systems/health-data.htm.
- 36.WHO European Health for All Database (HFA-DB) Data Source. [(accessed on 5 August 2019)]; Available online: http://www.euro.who.int/en/data-and-evidence/databases/european-health-for-all-family-of-databases-hfa-db.
- 37.WHO European Health for All Database (HFA-DB) [(accessed on 5 August 2019)]; Available online: https://gateway.euro.who.int/en/datasets/european-health-for-all-database/
- 38.Pedroni P. Purchasing power parity tests in cointegrated panels. Rev. Econ. Stat. 2001;83:727–731. doi: 10.1162/003465301753237803. [DOI] [Google Scholar]
- 39.Poullier J.P., Hernandez P., Kawabata K., Savedoff D.W. National Health Accounts: Concepts, Data Sources and Methodology. [(accessed on 5 August 2019)]; Available online: https://books.google.rs/books?hl=en&lr=&id=Ut_xcxWHobYC&oi=fnd&pg=PA182&dq=41.39.%09Poullier,+J.P.%3B+Hernandez,+P.%3B+Kawabata,+K.%3B+Savedoff,+D.W.+National+health+accounts:+Concepts,+data+sources+and+methodology.+World+Health+Organ&ots=ji1I980VTv&sig=g_37Y2ci0WEdklTrfR4nK0sSAKk&redir_esc=y#v=onepage&q&f=false.
- 40.Berman P.A. National health accounts in developing countries: Appropriate methods and recent applications. Health Econ. 1997;6:11–30. doi: 10.1002/(SICI)1099-1050(199701)6:1<11::AID-HEC238>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 41.Bui A.L., Lavado R.F., Johnson E.K., Brooks B.P., Freeman M.K., Graves C.M., Haakenstad A., Shoemaker B., Hanlon M., Dieleman J.L., et al. National health accounts data from 1996 to 2010: A systematic review. Bull. World Health Organ. 2015;93:566–576. doi: 10.2471/BLT.14.145235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WHO . WHO Methods and Data Sources for Global Burden of Disease Estimates 2000–2011. Department of Health Statistics and Information Systems; Geneva, Switzerland: 2013. [Google Scholar]
- 43.Cowen D., Smith N. After geopolitics? From the geopolitical social to geoeconomics. Antipode. 2009;41:22–48. doi: 10.1111/j.1467-8330.2008.00654.x. [DOI] [Google Scholar]
- 44.Sparke M. From geopolitics to geoeconomics: Transnational state effects in the borderlands. Geopolitics. 1998;3:62–98. doi: 10.1080/14650049808407619. [DOI] [Google Scholar]
- 45.Wigell M., Vihma A. Geopolitics versus geoeconomics: The case of Russia’s geostrategy and its effects on the EU. Int. Aff. 2016;92:605–627. doi: 10.1111/1468-2346.12600. [DOI] [Google Scholar]
- 46.Saltman R.B., Figueras J., Sakellarides C. Critical Challenges for Health Care Reform in Europe. McGraw-Hill Education; Berkshire, UK: 1998. [Google Scholar]
- 47.Krajewski-Siuda K., Romaniuk P. Poland—An “experimental range” for health care system changes. Two reforms: Decentralization and centralization and their consequences. J. Public Health. 2008;16:61–70. doi: 10.1007/s10389-007-0118-0. [DOI] [Google Scholar]
- 48.Széles G., Vokó Z., Jenei T., Kardos L., Pocsai Z., Bajtay A., Papp E., Pásti G., Kósa Z., Molnár I., et al. A preliminary evaluation of a health monitoring programme in Hungary. Eur. J. Public Health. 2005;15:26–32. doi: 10.1093/eurpub/cki107. [DOI] [PubMed] [Google Scholar]
- 49.Bryndová L., Pavloková K., Roubal T., Rokosová M., Gaskins M., van Ginneken E. Czech Republic. Health system review. Health Syst. Transit. (Eur. Obs. Health Syst. Policies) 2009;11 [Google Scholar]
- 50.Jakovljevic M.B. Resource allocation strategies in Southeastern European Health Policy. Res. Alloc. Strategy. Southeast. Eur. Health Policy. 2013;14:153–159. doi: 10.1007/s10198-012-0439-y. [DOI] [PubMed] [Google Scholar]
- 51.Jakovljevic M., Vukovic M., Chen C.C., Antunovic M., Dragojevic-Simic V., Velickovic-Radovanovic R., Djendji M.S., Jankovic N., Rankovic A., Kovacevic A., et al. Do health reforms impact cost consciousness of Health care professionals? Results from a nation-wide survey in the Balkans. Balkan Med. J. 2016;3:8–17. doi: 10.5152/balkanmedj.2015.15869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baris E., Mollahaliloglu S., Aydin S. Healthcare in Turkey: From laggard to leader. BMJ. 2011;342:c7456. doi: 10.1136/bmj.c7456. [DOI] [PubMed] [Google Scholar]
- 53.Akaeev A.A., Anufriev I.E., Popov G.N. Технологическая модернизация- промышленности и инновационное развитие – ключ к экономическому возрождению России в XXI веке [Technological modernization of industry and innovative development is the key to the economic revival of Russia in the XXI century] Инновации [Innovations] 2010:15–28. (In Russian) [Google Scholar]
- 54.Yegorychev A.M., Dubinin S.N. Россия на пороге XXI века: инновационные тенденции и национальные приоритеты [Russia on the edge of the XXI century: Innovation trends and national priorities] Ученые Записки Российского Государственного Социального Университета [Sci. Notes Rus. State Soc. Univ.] 2010:10–15. (In Russian) [Google Scholar]
- 55.Kotz D.M. Lessons from economic transition in Russia and China. Political Econ. Contemp. Capital. Radic. Perspect. Econ. Theory Policy. 2000:210–217. [Google Scholar]
- 56.Rancic N., Jakovljevic M.B. Long term health spending alongside population aging in N-11 emerging nations. East Eur. Bus. Econ. J. 2016;2:2–26. [Google Scholar]
- 57.Caliskan Z. The relationship between pharmaceutical expenditure and life expectancy: Evidence from 21 OECD countries. Appl. Econ. Lett. 2009;16:1651–1655. doi: 10.1080/13504850701604136. [DOI] [Google Scholar]
- 58.Mourre G. What Explains the Differences in Income and Labour Utilisation and Drives Labour and Economic Growth in Europe? European Commission; Brussels, Belgium: 2009. A GDP Accounting Perspective (No. 354). Directorate General Economic and Financial Affairs (DG ECFIN) [Google Scholar]
- 59.Kaitila V. Convergence of Real GDP Per Capita in the EU15. How do the Accession Countries Fit in? (No. 025) [(accessed on 21 August 2019)];2004 Available online: https://ideas.repec.org/p/epr/enepwp/025.html.
- 60.Kerem K., Puss T., Viies M., Maldre R. Health and convergence of health care expenditure in EU. Int. Bus. Econ. Res. J. 2008;7:29–44. doi: 10.19030/iber.v7i3.3232. [DOI] [Google Scholar]
- 61.Bech M., Christiansen T., Khoman E., Lauridsen J., Weale M. Ageing and health care expenditure in EU-15. Eur. J. Health Econ. 2011;12:469–478. doi: 10.1007/s10198-010-0260-4. [DOI] [PubMed] [Google Scholar]
- 62.Jakovljevic M. The aging of Europe. The unexplored potential. Farmecon. Health Econ. Ther. Pathw. 2015;16:89–92. doi: 10.7175/fe.v16i4.1220. [DOI] [Google Scholar]
- 63.Jakovljevic M.B., Netz Y., Buttigieg S.C., Asany R., Laaser U., Varjacic M. Population aging and migration—History and UN forecasts in the EU-28 and its east and south near neighborhood—One century perspective 1950–2050. Glob. Health. 2018;14:30. doi: 10.1186/s12992-018-0348-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Korotayev A., Arkhangelsky V., Bogevolnov J., Goldstone J., Khaltourina G.A., Malkov A., Novikov A., Riazantsev S., Rybalchenko S., Rybalchenko S., et al. Critical 10 Years. Demographic Policies of the Russian Federation: Successes and Challenges. “Delo” Publishing House (RANEPA); Moscow, Russia: Apr, 2015. [Google Scholar]
- 65.Khasanova R.R. Самосохранительное поведение населения как фактор продолжительности жизни [Self-preservation behavior of the population as a factor in life expectancy] Здоровье населения и среда обитания [Public Health Habitat] 2013;5:43–46. (In Russian) [Google Scholar]
- 66.Denisenko M., Varshavskaya E. Продолжительность трудовой жизни в России [Working life expectancy in Russia] HSE Econ. J. 2017;21:592–622. (In Russian) [Google Scholar]
- 67.Belov V.B., Rogovina A.G. Основные медико-демографические показатели здоровья населения России к 2013 г [The basic medical demographic indicators of population health of Russia up to 2013] Проблемы социальной гигиены, здравоохранения и истории медицины [Probl. Soc. Hyg. Public Health Hist. Med.] 2014;6:18–22. (In Russian) [PubMed] [Google Scholar]
- 68.Jakovljevic M.B., Laaser U. Population aging from 1950 to 2010 in seventeen transitional countries in the wider region of South Eastern Europe. SEEJPH. 2015;3:1–12. [Google Scholar]
- 69.Jakovljevic M.B. Starenje stanovništva i rast izdvajanja za zdravstvenu zaštitu [Aging of the population and growth of appropriations for health care] Srpski Arhiv za Celokupno Lekarstvo. 2017;145:534–539. doi: 10.2298/SARH160906113J. (In Serbian) [DOI] [Google Scholar]
- 70.Jakovljevic M., Vukovic M., Fontanesi J. Life expectancy and health expenditure evolution in Eastern Europe—DiD and DEA analysis. Expert Rev. Pharm. Outcomes Res. 2016;16:537–546. doi: 10.1586/14737167.2016.1125293. [DOI] [PubMed] [Google Scholar]
- 71.Morgan D., Astolfi R. Financial impact of the GFC: Health care spending across the OECD. Health Econ. Policy Law. 2015;10:7–19. doi: 10.1017/S1744133114000218. [DOI] [PubMed] [Google Scholar]
- 72.Rivlin A.M., Antos J.R. Restoring Fiscal Sanity 2007: The Health Spending Challenge. Brookings Institution Press; Washington, DC, USA: 2007. [Google Scholar]
- 73.Jakovljevic M., Souliotis K. Pharmaceutical expenditure changes in Serbia and Greece during the global economic recession. South East. Eur. J. Public Health. 2016;5:1–17. [Google Scholar]
- 74.Sotiropoulos D.A. The EU’s impact on the Greek welfare state: Europeanization on paper? J. Eur. Soc. Policy. 2004;14:267–284. doi: 10.1177/0958928704044627. [DOI] [Google Scholar]
- 75.Huidrom R., Kose A., Ohnsorge F.L. How Important Are Spillovers from Major Emerging Markets? Policy Research Working Paper, no. WPS 8093. World Bank Group; Washington, DC, USA: 2017. [Google Scholar]
- 76.Kose A. Big Emerging Market Economies Versus the G7: Which Group Will Drive the Upswing in Global Growth? [(accessed on 5 August 2019)]; Available online: https://www.brookings.edu/blog/up-front/2017/07/14/big-emerging-market-economies-versus-the-g-7-which-group-will-drive-the-upswing-in-global-growth/