Abstract
Background
In early breast cancer treatment, the preferred surgical regimen remains a topic of controversy, and conventional pairwise meta-analysis cannot provide a hierarchy based on clinical trial evidence. Therefore, a network meta-analysis was performed both for direct and indirect comparisons and to assess the survival outcomes of surgical regimens.
Methods
Randomized clinical trials comparing different surgical regimens for the treatment of early breast cancer were identified. Overall survival (OS) and disease-free-survival (DFS) were analyzed using random-effects network meta-analysis on the hazard ratio (HR) scale and calculated as combined HRs and 95% confidence intervals (CIs). All statistical tests were two-sided.
Results
The network meta-analysis compared 11 different surgical regimens that consisted of 13 and 17 direct comparisons between strategies for OS (34 trials; n = 23 587 patients) and DFS (32 trials; n = 22 552 patients), respectively. The values of surface under the cumulative ranking for OS and DFS after mastectomy (M)+radiotherapy (RT) were observed to be the largest. Breast-conserving surgery (BCS)+axillary node sampling+RT almost achieved the threshold for inferiority compared with the other surgical treatment arms and was statistically significantly associated with worse OS (HR = 0.51, 95% CI = 0.24 to 0.94; HR = 0.48, 95% CI = 0.22 to 0.92; HR = 0.51, 95% CI = 0.23 to 0.96). No statistically significant difference between BCS+sentinel lymph node biopsy (SLNB)+RT vs BCS+SLNB+intraoperative RT was observed in carrying out network meta-analysis (HR = 0.95, 95% CI = 0.64 to 1.36).
Conclusions
M+RT is safer than other surgical regimens for the treatment of early breast cancer patients because of the favorable balance between the survival outcomes. Early breast cancer patients who receive BCS should be given SLNB and not axillary node sampling. Intraoperative RT is no better than postoperative RT in patients who receive SLNB.
Breast cancer is one of the most common cancers among women in the world. Globally, about 2.4 million women are diagnosed with breast cancer and 523 000 die from it annually (1). The incidence of breast cancer has been on the rise, increasing by about 0.4% per year between 2004 and 2013, and approximately one in eight women is likely to be diagnosed with breast cancer during their lifetime (2). According to the seventh edition of the American Joint Committee on Cancer staging system, early-stage breast cancer refers to breast cancer stages I and II, T1‒2N0‒1M0 (3). Currently, about 30% of newly diagnosed cases of early breast cancer have a high cure rate of 96%‒98% (4–6); moreover, the detection rate of early-stage breast cancer is increasing because of early-detection tests, especially mammography screening.
It should be noted that in the absence of distant metastases, early breast cancer is curable. We reviewed the current strategies used for treatment of patients with early breast cancer. Currently, European Society for Medical Oncology guidelines recommend that almost all patients with early breast cancer receive chemotherapy after breast cancer surgery (7). The most recent publication of the Early Breast Cancer Trialists’ Collaborative Group overview states the relative benefit of chemotherapy is similar in all subgroups independent of age, stage, histopathological grade, and estrogen receptor status in early breast cancer (8). Owing to the similarity in treatment strategies, surgical treatment of early breast cancer is often regarded as the first choice for sensitive care (9). Surgery is the main treatment for early breast cancer, which includes partial or total mastectomy (M). During the past 20 years, a paradigm shift has been seen in the treatment of early-stage cancer when the treatment approach moved from Halsted radical mastectomy to breast-conserving surgery (BCS) (10).
The aim of surgery is to maximize local control with the least aggressive treatment. However, owing to the complexity of surgical approaches, surgeons differ greatly in the way they choose to operate. Topics of controversy in early breast cancer include not only the type of surgery performed (breast conservation with or without radiation vs M) and dissection of the axilla (sentinel lymph node biopsy [SLNB] vs none) but also the presence or absence of breast irradiation (11). Traditional meta-analyses refer to pairwise comparisons of two or three treatment options (12–14). As the number of possible head-to-head comparisons directly expands in quadratic proportions with the availability of effective agents, enough pairs of comparative data remain unavailable for available treatment options (15).
The network meta-analysis is a generalized version of a pairwise meta-analysis that includes multiple treatment options with more detailed inference from clinical trials. In network meta-analysis, direct and indirect evidence of multiple treatment arms across studies (provided there is at least one common arm between them) are compared, which helps in clinical decision making for clinicians and patients who may desire to know the overall “best treatment” (15–18).
There is a need for a complete, effective, and latest surgical treatment option for the diagnosis and treatment of patients with early breast cancer. Therefore, this study aims to summarize the evidence network supporting the surgical treatment method in patients with early breast cancer in terms of overall survival (OS) and disease-free survival (DFS) using the network meta-analysis study.
Materials and Methods
Protocol and Protocol Registration
This review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension statement for network meta-analysis for health care (19). A priori protocol was established for this review and registered with the international prospective register of systematic reviews, PROSPERO number: CRD42018094894 (access site: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=94894).
Search Strategy
Relevant published trials before July 2018 were identified after a thorough literature search of PubMed and EMBASE. Furthermore, prospective clinical trials that are ongoing and already published were identified after searching ClinicalTrials.gov. Populations, interventions, comparisons, and outcome strategies were identified with the following search terms: “surgical treatment,” “early breast cancer,” and “randomized clinical trial.” No restrictions were imposed regarding the sample size, population, language, publication year, publication type, or publication status. In addition, manual searches were conducted by reviewing the reference list of the relevant publications.
Selection Criteria
All the published and unpublished phase II or III randomized controlled trials (RCTs) that compared the type of surgery performed, dissection of the axilla, and breast irradiation in patients with early-stage breast cancer were included. The most recent and informative publication was included. Trials published only as abstracts (with no additional data available from other sources) and studies that included ductal carcinoma in situ and patients who received Halsted radical mastectomy were excluded. The characteristics of the included studies were assessed by two independent reviewers (Y.G. and X.L.), who used the Cochrane Collaboration risk of bias tool (20). A third reviewer (L.C.) adjudicated any discordance.
Data Extraction
Relevant data were extracted by the same two reviewers (Y.G. and X.L.) according to a prespecified protocol, and disagreements were resolved by discussion with a third reviewer (L.C.). The extracted data included characteristics of the study (year, country, number of arms, and period of follow-up), characteristics of the participants (age, number of patients included in analysis, and population analyzed), types of intervention, and control. Primary and secondary outcome measures were also recorded. In addition, we contacted the authors if any study had missing data. If no response was received, analysis was performed without these data.
Definition of Treatment Arms
To organize the existing treatment options tested in clinical trials into clinically meaningful arms, we used general prespecified criteria as shown in Box 1.
Box 1.
Abbreviations of all the surgical regimens
ARM 1. Breast-conserving surgery+axillary lymph node dissection (BCS+ALND)
ARM 2. Breast-conserving surgery+axillary lymph node dissection+radiotherapy (BCS+ALND+RT)
ARM 3. Breast-conserving surgery+axillary node sampling+radiotherapy (BCS+ANS+RT)
ARM 4. Breast-conserving surgery+sentinel lymph node biopsy (BCS+SLNB)
ARM 5. Breast-conserving surgery+sentinel lymph node biopsy+axillary radiotherapy+radiotherapy (BCS+SLNB+ART+RT)
ARM 6. Breast-conserving surgery+sentinel lymph node biopsy+intraoperative radiotherapy (BCS+SLNB+IORT)
ARM 7. Breast-conserving surgery+sentinel lymph node biopsy+radiotherapy (BCS+SLNB+RT)
ARM 8. Mastectomy (M)
ARM 9. Mastectomy+axillary lymph node dissection (M+ALND)
ARM 10. Mastectomy+axillary lymph node dissection+ radiotherapy (M+ALND+RT)
ARM 11. Mastectomy+radiotherapy (M+RT)
Statistical Analysis
The primary and secondary outcomes were OS and DFS. For OS and DFS, the hazard ratios and confidence intervals were directly extracted from the original enrolled studies or were calculated by the formula suggested by Tierney and colleagues (21). In addition, we also tried to contact the authors if the study provided only figures but not the exact data. In case the authors did not respond, the program Engauge Digitizer 4.1 (M. Mitchell, Engauge Digitizer, http://digitizer.sourceforge.net) was used to extract the exact data from the figures. This program can generate exact values by digitizing data points from an image file after the manual setting of the coordinate axis.
Standard pairwise meta-analysis using the DerSimonian and Laird random-effects model was performed to estimate pooled hazard ratios (HRs) and 95% confidence intervals (CIs) (22). A P value less than .05 was considered statistically significant. All statistical tests were two-sided. Chi-squared statistics used to assess the heterogeneity between two or more studies was expressed as the I2 value, which describes the percentage of total variation due to heterogeneity and also quantifies the effect of heterogeneity in the study results (23,24). Heterogeneity was considered low, moderate, or high for I2 values less than 25%, 25%, and 50% and greater, respectively (23).
A Bayesian network meta-analysis statistical model was used to compare the direct and indirect evidence for early-stage breast cancer by combining multiple surgical treatment arms across studies with all the information regarding OS and DFS. The Bayesian consistency model was used to analyze the data in which all the parameters were treated as random variables, and the Markov chain Monte Carlo method was used to estimate the posterior distribution of each parameter (25,26). A hierarchical Bayesian model synthesizes comparisons between the treatment pairs and simultaneously summarizes all outcomes of interest by assuming a common heterogeneity parameter (16). Each treatment comparison was presented along with 95% confidence intervals (27). The transitivity assumption was evaluated by comparing the distribution of clinical variables that could act as effect modifiers across treatment comparisons. In addition to allowing for indirect comparisons, network meta-analysis also provides a ranking probability curve of each treatment (rankogram) by calculating the probability of each arm to achieve the best rank. A simple numerical is used to estimate the surface under the cumulative ranking (SUCRA) for each treatment, and this value equals one when treatment is the best and zero when treatment is the worst (28).
Analyses were performed in STATA 13.0 (pairwise meta-analysis, I² calculations, estimation of consistency and transitivity, rankograms, and SUCRA curves) and WinBUGS 1.4.3 (multiple-treatments meta-analysis models).
Results
Characteristics of the Identified Studies
Initially, a total of 3465 studies were identified on database search, of which 3291 studies were excluded based on the selection criteria. Subsequently, 174 potentially relevant full-text articles were reviewed further, and 36 studies met the eligibility criteria for the current study. Supplementary Figure 1 (available online) summarizes the overall literature search and selection criteria. A total of 24 702 women were included in the study and were randomly assigned to receive one of the following 11 different surgical treatment arms: BCS+ALND, BCS+ALND+RT, BCS+ANS+RT, BCS+SLNB, BCS+SLNB+ART+RT, BCS+SLNB+IORT, BCS+SLNB+RT, M, M+ALND, M+ALND+RT, and M+RT.
The main features of the participants from all included studies are presented in Table 1. Overall, 36 studies published from 1989 to 2017 were used for the network meta-analysis (29–64). All trials were carried out in North America and Europe except one trial that was conducted in Japan (53). The reported mean or median age ranged from 42.4 to 70.8 years across the eligible studies. A total of 23 587 participants were included in the OS analysis (34 studies), and 22 552 participants were included in the DFS analysis (32 studies). The mean duration of the studies was 9.7 years, and the mean sample size was 329 participants per group (range 42‒1857), with 31 trials having at least 100 participants per group. In total, 36 studies were included, of which 34 were two-arm trials, one was a three-arm trial, and one was a multi-arm trial and only 3 studies met the expected quality (Supplementary Figure 2, available online). Fifteen studies (comparing all included surgical treatment arms except BCS+ANS+RT and M+RT) had a follow-up longer than 10 years. Of the 36 included studies, there was high risk of bias masking of participants and personnel in 11 studies (34,36,44,47,49,51,56,57,62), masking of outcome assessment in three (49,51), selective outcome reporting areas in two (37,57), and other bias in six studies (37,45,47,54,62).
Table 1.
Baseline characteristics of studies included in the network meta-analysis*
| Study | Country | Participants’ median or mean age, y | Clinical stage | Sample size | Treatments | Median follow-up, y | Outcomes |
|---|---|---|---|---|---|---|---|
| Agresti et al., 2014 (29) | Italy | 52.6 | T1N0 | 1034 | BCS+SLNB+RT (517) | 5 | OS, DFS |
| vs BCS+ALND+RT (517) | |||||||
| Arriagada et al., 2003 (30) | France | — | T1N0–1M0 | 176 | BCS+ALND+RT (88) | 22.7 | OS, DFS |
| vs M+ALND+RT (88) | |||||||
| Blichert-Toft et al., 2008 (31) | Denmark | — | Stage I–II | 793 | BCS+ALND (381) | 19.6 | OS, DFS |
| vs M+ALND (350) | |||||||
| Cabanes et al., 1992 (32) | France | 50.6 | N0–1aM0 | 658 | BCS+ALND+RT (326) | 4.5 | OS |
| vs BCS+SLNB+RT (332) | |||||||
| Canavese et al., 2016 (33) | Italy | 59 in ALND | N0 | 225 | BCS+ALND+RT (115) | 14.3 | OS, DFS |
| 56 in SLNB | vs BCS+SLNB+RT (110) | ||||||
| Chetty et al., 2000 (34) | United Kingdom | 54 | T1N0–1M0 | 446 | BCS+ANS+RT (234) | 4.1 | OS, DFS |
| vs BCS+ALND+RT (232) | |||||||
| Clark et al., 1996 (35) | Canada | — | T1N0–1M0 | 837 | BCS+ALND (421) | 7.6 | OS, DFS |
| vs BCS+ALND+RT (416) | |||||||
| Fisher et al., 2002 (36) | United States | — | T1–2N0–1M0 | 1011 | M+RT (646) | 8 | OS, DFS |
| vs M (365) | |||||||
| Fisher et al., 1995 (37) | United States | — | T1–2N0–1M0 | 3628 | M (1775) | 12 | OS, DFS |
| vs BCS+SLNB (1853) | |||||||
| vs BCS+SLNB+RT (1857) | |||||||
| Galimberti et al., 2013 (38) | United States | 53 in ALND | T1–2N0–1M0 | 931 | M+ALND (44) vs M (42) | 5 | DFS |
| 54 in non–ALND | BCS+ALND (420) vs BCS+SLNB (425) | ||||||
| Giuliano et al., 2011 (39) | United States | 56 in ALND | T1–2 | 856 | BCS+SLNB+RT (436) | 6.3 | OS, DFS |
| 54 in SLNB | vs BCS+ALND+RT (420) | ||||||
| Holli et al., 2001 (40) | Finland | 54 in RT | T1–2N0M0 | 152 | BCS+ALND+RT (80) | 6.7 | OS, DFS |
| 56 in non–RT | vs BCS+ALND (72) | ||||||
| Fyles et al., 2004 (41) | Canada | — | T1–2N0M0 | 769 | BCS+SLNB+RT (386) | 5.6 | OS, DFS |
| vs BCS+SLNB (383) | |||||||
| Hughes et al., 2013 (42) | United States | — | T1N0M0 | 636 | BCS+SLNB+RT (317) | 12.6 | OS, DFS |
| vs BCS+SLNB (319) | |||||||
| Killander et al., 2016 (43) | Sweden | 60 | T1–2N0M0 | 1178 | BCS+ALND+RT (591) | 15.6 | OS, DFS |
| vs BCS+ALND (587) | |||||||
| Kunkler et al., 2015 (44) | United Kingdom | 70 | T1–2N0M0 | 1326 | BCS+SLNB+RT (658) | 5 | OS, DFS |
| vs BCS+SLNB (668) | |||||||
| Litiére et al., 2012 (45) | United Kingdom | 50 | T1–2N0 | 868 | BCS+ALND+RT (448) | 22.1 | OS, DFS |
| vs M+ALND+RT (420) | |||||||
| Louis–Sylvestre et al., 2004 (46) | France | 52 in ALND | T1–2N0M0 | 658 | BCS+ALND+RT (326) | 15 | OS, DFS |
| 50.6 in ART | vs BCS+SLNB+ART+RT (332) | ||||||
| Martelli et al., 2014 (47) | Italy | 70.8 | T1N0 | 219 | BCS+ALND+RT (109) | 12.5 | OS, DFS |
| vs BCS+SLNB+RT (110) | |||||||
| Newman et al., 1999 (48) | United States | 52 | T1–2N0M0 | 211 | BCS+SLNB+RT (42) | 5.6 | OS, DFS |
| vs M (168) | |||||||
| Poggi et al., 2003 (49) | United States | 50 | T1–2N0–1M0 | 237 | M+ALND (116) | 18.4 | OS, DFS |
| vs BCS+ALND+RT (121) | |||||||
| Polgár et al., 2013 (50) | Hungary | 59 in IORT | T1N0–1M0 | 258 | BCS+SLNB+IORT (128) | 10.2 | OS, DFS |
| 58 in RT | vs BCS+SLNB+RT (130) | ||||||
| Pötter et al., 2007 (51) | Austria | 66 | T1–2N0 | 869 | BCS+ALND+RT (414) | 4.5 | OS, DFS |
| vs BCS+ALND (417) | |||||||
| Sarrazin et al., 1989 (52) | France | — | T1N0–1M0 | 179 | M (91) | 10 | OS |
| vs BCS+SLNB+RT (88) | |||||||
| Sato et al., 2017 (53) | Japan | 44.0 in IORT | T1–2N0–1M0 | 184 | BCS+SLNB+IORT (99) | 3.8 | DFS |
| 42.4 in RT | vs BCS+SLNB+RT (85) | ||||||
| Sjöström et al., 2017 (54) | Sweden | 60 | T1–2N0M0 | 932 | BCS+ALND+RT (474) | 15.2 | OS |
| vs BCS+ALND (458) | |||||||
| Strnad et al., 2016 (55) | Germany | 62 | T1–2N0–1M0 | 1184 | BCS+SLNB+IORT (633) | 9 | OS, DFS |
| vs BCS+SLNB+RT (551) | |||||||
| Tinterri et al., 2014 (56) | Italy | — | T1–2N0–1M0 | 749 | BCS+SLNB+RT (376) | 9 | OS, DFS |
| vs BCS+SLNB (373) | |||||||
| van Dongen et al., 2000 (57) | Netherlands | — | T1–2N0M0 | 868 | BCS+SLNB+RT (448) | 13.4 | OS, DFS |
| vs M (420) | |||||||
| Veronesi et al., 2001 (58) | Italy | — | T1–2N0M0 | 579 | BCS+ALND+RT (294) | 9 | OS, DFS |
| vs BCS+ALND (273) | |||||||
| Veronesi et al., 2003 (59) | Italy | — | T1N0M0 | 516 | BCS+ALND+RT (257) | — | OS, DFS |
| vs BCS+SLNB+RT (259) | |||||||
| Veronesi et al., 2005 (60) | Italy | 57 | T1N0M0 | 435 | BCS+SLNB+ART+RT (221) | 5.2 | OS, DFS |
| vs BCS+SLNB+RT (214) | |||||||
| Veronesi et al., 2013 (61) | Italy | — | T1N0–1M0 | 1305 | BCS+SLNB+IORT (651) | 5.8 | OS, DFS |
| vs BCS+SLNB+RT (654) | |||||||
| Voogd et al., 1996 (62) | Netherlands | 51.6 in BCS | T1N0–1M0 | 921 | BCS+ALND (464) | 6.2 | OS, DFS |
| 58.3 in mastectomy | vs M+ALND (457) | ||||||
| Wickberg et al., 2014 (63) | Sweden | 59.0 in RT | T1N0M0 | 381 | BCS+ALND+RT (184) | 13 | OS |
| 60.9 in non–RT | vs BCS+ALND (197) | ||||||
| Winzer et al., 2004 (64) | Germany | — | T1N0M0 | 361 | BCS+ALND (159) | 5.9 | OS, DFS |
| vs BCS+ALND+RT (188) |
The number in parentheses under the column of Treatments is the number of patients included per group. BCS+ALND = breast–conserving surgery+axillary lymph node dissection; BCS+ALND+RT = breast–conserving surgery+axillary lymph node dissection+radiotherapy; BCS+ANS+RT = breast–conserving surgery+axillary node sample+radiotherapy; BCS+SLNB = breast–conserving surgery+sentinel lymph node biopsy; BCS+SLNB+ART+RT = breast–conserving surgery+sentinel lymph node biopsy+axillary radiotherapy+radiotherapy; BCS+SLNB+IORT = breast–conserving surgery+sentinel lymph node biopsy+intraoperative radiotherapy. BCS+SLNB+RT = breast–conserving surgery+sentinel lymph node biopsy+radiotherapy; DFS = disease-free survival; M = mastectomy; M+ALND = mastectomy+axillary lymph node dissection; M+ALND+RT = mastectomy+axillary lymph node dissection+radiotherapy; M+RT = mastectomy+radiotherapy; OS = overall survival.
Direct Comparison Meta-Analysis
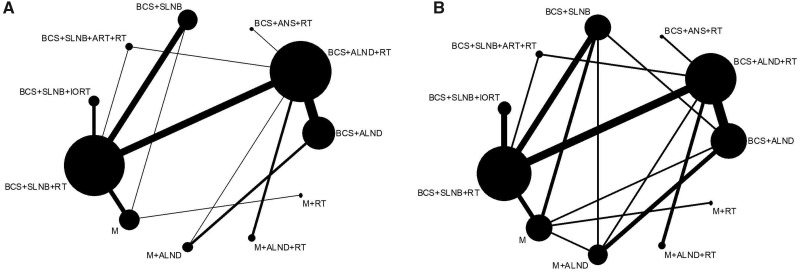
Eligible comparisons for the primary and secondary outcomes are presented in Figure 1. Of the 30 possible pairwise comparisons between the 11 surgical treatments, 13 were studied directly in one or more trials for OS and 17 for DFS.
Figure 1.
Networks for A) overall survival (OS) and B) disease-free survival (DFS). The width of the lines is proportional to the number of trials comparing each pair of treatments, and the size of each node is proportional to the number of randomly assigned participants (sample size). BCS+ALND = breast-conserving surgery+axillary lymph node dissection. BCS+ALND+RT = breast-conserving surgery+axillary lymph node dissection+radiotherapy. BCS+ANS+RT = breast-conserving surgery+axillary node sample+radiotherapy. BCS+SLNB = breast-conserving surgery+sentinel lymph node biopsy. BCS+SLNB+ART+RT = breast-conserving surgery+ sentinel lymph node biopsy+axillary radiotherapy +radiotherapy. BCS+SLNB+IORT = breast-conserving surgery+sentinel lymph node biopsy+Intraoperative radiotherapy. BCS+SLNB+RT = breast-conserving surgery+sentinel lymph node biopsy+radiotherapy. M = mastectomy. M+ALND = mastectomy+axillary lymph node dissection. M+ALND+RT = mastectomy+axillary lymph node dissection+radiotherapy. M+RT = mastectomy+radiotherapy.
We performed direct comparisons (Table 2), showing that DFS favors BCS+SLNB over M (HR = 1.09, 95% CI = 1.02 to 1.16, P = .009) and M+RT over M (HR = 1.26, 95% CI = 1.04 to 1.51, P = .02). These results were generated from 11 independent analyses without adjustment for multiple testing. Only one direct comparison showed that OS favors BCS+SLNB over BCS+SLNB+RT (HR = 1.10, 95% CI = 1.02 to 1.18, P = .01) (Table 2).
Table 2.
The HRs and heterogeneity for direct comparisons
| Outcome | No. of studies | Events | Total | Events | Total | HR (95% CI) | P* | I 2, % |
|---|---|---|---|---|---|---|---|---|
| BCS+SLNB | BCS+SLNB+RT | |||||||
| OS | 5 | 1012 | 3596 | 919 | 3594 | 1.10 (1.02 to 1.18) | .01 | 0 |
| DFS | 4 | 1071 | 2931 | 955 | 2933 | 1.17 (0.90 to 1.52) | .25 | 55.3 |
| BCS+ALND | M+ALND | |||||||
| OS | 2 | 246 | 845 | 279 | 807 | 0.83 (0.67 to 1.02) | .08 | 52.7 |
| DFS | 3 | 215 | 787 | 155 | 865 | 1.03 (0.63 to 1.66) | .92 | 78.0 |
| BCS+ALND | BCS+ALND+RT | |||||||
| OS | 8 | 739 | 2584 | 699 | 2641 | 1.06 (0.98 to 1.14) | .18 | 0 |
| DFS | 6 | 236 | 1929 | 222 | 1983 | 1.07 (0.70 to 1.62) | .76 | 72.8 |
| BCS+ALND+RT | M+ALND+RT | |||||||
| OS | 2 | 309 | 536 | 278 | 508 | 0.95 (0.66 to 1.36) | .77 | 78.2 |
| DFS | 2 | 231 | 536 | 207 | 508 | 0.97 (0.67 to 1.39) | .85 | 63.5 |
| BCS+ALND+RT | BCS+SLNB+RT | |||||||
| OS | 5 | 118 | 1629 | 119 | 1654 | 0.99 (0.68 to 1.45) | .96 | 51.8 |
| DFS | 5 | 121 | 1434 | 118 | 1416 | 0.99 (0.78 to 1.26) | .99 | 0 |
| BCS+ALND+RT | BCS+SLNB+ART+RT | |||||||
| OS | 1 | 80 | 326 | 87 | 332 | 0.94 (0.72 to 1.22) | .62 | — |
| DFS | 1 | 116 | 326 | 115 | 332 | 1.03 (0.84 to 1.26) | .80 | — |
| BCS+SLBN+ART+RT | BCS+SLNB+RT | |||||||
| OS | 1 | 2 | 221 | 8 | 214 | 0.24 (0.05 to 1.13) | .07 | — |
| DFS | 1 | 3 | 221 | 8 | 214 | 0.36 (0.10 to 1.35) | .13 | — |
| BCS+ANS+RT | BCS+ALND+RT | |||||||
| OS | 1 | 27 | 234 | 42 | 232 | 0.87 (0.65 to 1.18) | .37 | — |
| DFS | 1 | 49 | 234 | 56 | 232 | 0.87 (0.62 to 1.22) | .41 | — |
| BCS+SLNB+IORT | BCS+SLNB+RT | |||||||
| OS | 3 | 77 | 1412 | 79 | 1335 | 0.94 (0.64 to 1.39) | .76 | 38.8 |
| DFS | 4 | 73 | 1511 | 84 | 1420 | 0.83 (0.61 to 1.13) | .24 | 1.2 |
| BCS+SLNB+RT | M | |||||||
| OS | 4 | 854 | 2435 | 855 | 2454 | 1.01 (0.84 to 1.22) | .91 | 61.3 |
| DFS | 3 | 999 | 2347 | 1018 | 2363 | 0.94 (0.78 to 1.15) | .55 | 55.5 |
| BCS+SLNB | M | |||||||
| OS | 1 | 700 | 1853 | 642 | 1775 | 1.05 (0.96 to 1.14) | .32 | — |
| DFS | 2 | 1018 | 2278 | 853 | 1817 | 1.09 (1.02 to 1.16) | .01 | 0 |
| M+RT | M | |||||||
| OS | 1 | 159 | 646 | 86 | 365 | 1.05 (0.83 to 1.31) | .71 | — |
| DFS | 1 | 238 | 646 | 107 | 365 | 1.26 (1.04 to 1.52) | .02 | — |
| M+ALND | BCS+ALND+RT | |||||||
| OS | 1 | 46 | 116 | 52 | 121 | 0.92 (0.68 to 1.25) | .60 | — |
| DFS | 1 | 27 | 116 | 30 | 121 | 0.94 (0.60 to 1.48) | .79 | — |
| BCS+ALND | BCS+SLNB | |||||||
| DFS | 1 | 63 | 420 | 52 | 425 | 1.23 (0.87 to 1.73) | .24 | — |
| M | BCS+ALND | |||||||
| DFS | 1 | 3 | 42 | 63 | 420 | 0.48 (0.16 to 1.45) | .13 | — |
| M+ALND | M | |||||||
| DFS | 1 | 6 | 44 | 3 | 42 | 1.91 (0.51 to 7.15) | .34 | — |
| M+ALND | BCS+SLNB | |||||||
| DFS | 1 | 6 | 44 | 52 | 425 | 1.12 (0.51 to 2.45) | .79 | — |
The HRs and 95% CIs were used for pooling effect sizes using the DerSimonian-Laird random-effects model. I2 quantifies the effect of heterogeneity in the studies’ results with values greater than 50% indicative of large between-study heterogeneity, values of 25%–50% indicative of modest heterogeneity, and values less than 25% indicative of low heterogeneity. All statistical tests were two-sided. BCS+ALND = breast-conserving surgery+axillary lymph node dissection; BCS+ALND+RT = breast-conserving surgery+axillary lymph node dissection+radiotherapy; BCS+ANS+RT = breast-conserving surgery+axillary node sample+radiotherapy; BCS+SLNB = breast-conserving surgery+sentinel lymph node biopsy; BCS+SLNB+ART+RT = breast-conserving surgery+sentinel lymph node biopsy+axillary radiotherapy+radiotherapy; BCS+SLNB+IORT = breast-conserving surgery+sentinel lymph node biopsy+intraoperative radiotherapy. BCS+SLNB+RT = breast-conserving surgery+sentinel lymph node biopsy+radiotherapy; CI = confidence interval; DFS = disease-free survival; HR = hazard ratio; M = mastectomy; M+ALND = mastectomy+axillary lymph node dissection; M+ALND+RT = mastectomy+axillary lymph node dissection+radiotherapy; M+RT = mastectomy+radiotherapy; OS = overall survival.
Bayesian Network Meta-Analysis
Fifty-five indirect comparisons were made, and the results of all possible comparisons were expressed using hazard ratios and confidence intervals calculated with a Bayesian network meta-analysis (Table 3). This analysis showed that M+ALND almost achieved the threshold for superiority compared with the other surgical treatment arms and was statistically significantly associated with better OS compared with BCS+ANS+RT (HR = 0.48, 95% CI = 0.22 to 0.92) (even though less-clear benefits were noted with M+ALND compared with BCS+ALND, BCS+ALND+RT, BCS+SLNB, BCS+SLNB+ART+RT, BCS+SLNB+IORT, BCS+SLNB+RT, M, M+RT, and M+ALND+RT with a confidence interval for hazard ratio slightly more than 1.00). In addition, BCS+ANS+RT almost achieved the threshold for inferiority compared with the other surgical treatment arms and was statistically significantly associated with worse OS compared with BCS+SLNB, M+ALND, and M+RT. For DFS, M+RT almost achieved the threshold for superiority compared with the other surgical treatment arms (with a confidence interval for hazard ratio slightly more than 1.00). No statistically significant differences were observed in these results.
Table 3.
The HR and 95% CIs calculated by Bayesian network meta-analysis*
| Outcome | Treatment | DFS, HR (95% CI) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BCS+ALND | BCS+ALND+RT | BCS+ANS+RT | BCS+SLNB | BCS+SLNB+ART+RT | BCS+SLNB+IORT | BCS+SLNB+RT | M | M+ALND | M+ALND+RT | M+RT | ||
| OS, HR (95% CI) | BCS+ALND | — | 1.14 | 1.49 | 1.14 | 1.60 | 1.89 | 1.36 | 1.25 | 1.08 | 1.15 | 0.95 |
| (0.81 to 1.59) | (0.57 to 3.27) | (0.67 to 1.83) | (0.73 to 3.27) | (0.92 to 3.60) | (0.84 to 2.11) | (0.67 to 2.12) | (0.68 to 1.63) | (0.55 to 2.10) | (0.33 to 2.15) | |||
| BCS+ALND+RT | 1.09 | — | 1.31 | 1.01 | 1.40 | 1.67 | 1.20 | 1.11 | 0.97 | 1.01 | 0.84 | |
| (0.91 to 1.30) | (0.54 to 2.71) | (0.62 to 1.58) | (0.70 to 2.69) | (0.85 to 3.04) | (0.80 to 1.73) | (0.62 to 1.81) | (0.57 to 1.53) | (0.53 to 1.69) | (0.30 to 1.86) | |||
| BCS+ANS+RT | 1.93 | 1.77 | — | 0.91 | 1.27 | 1.51 | 1.09 | 1.00 | 0.87 | 0.91 | 0.76 | |
| (0.99 to 3.50) | (0.93 to 3.13) | (0.32 to 2.10) | (0.40 to 3.26) | (0.49 to 3.75) | (0.40 to 2.41) | (0.34 to 2.34) | (0.30 to 1.99) | (0.29 to 2.12) | (0.18 to 2.11) | |||
| BCS+SLNB | 0.89 | 0.82 | 0.51 | — | 1.46 | 1.69 | 1.22 | 1.12 | 1.00 | 1.06 | 0.84 | |
| (0.62 to 1.25) | (0.59 to 1.11) | (0.24 to 0.94) | (0.63 to 3.04) | (0.88 to 3.02) | (0.84 to 1.70) | (0.67 to 1.72 | (0.52 to 1.74) | (0.46 to 2.03) | (0.32 to 1.82) | |||
| BCS+SLNB+ART+RT | 1.18 | 1.08 | 0.67 | 1.35 | — | 1.33 | 0.96 | 0.88 | 0.77 | 0.81 | 0.67 | |
| (0.72 to 1.90) | (0.69 to 1.68) | (0.30 to 1.33) | (0.78 to 2.26) | (0.49 to 2.86) | (0.42 to 1.80) | (0.34 to 1.79) | (0.30 to 1.57) | (0.28 to 1.70) | (0.18 to 1.67) | |||
| BCS+SLNB+IORT | 1.06 | 0.98 | 0.61 | 1.21 | 0.95 | — | 0.77 | 0.71 | 0.64 | 0.67 | 0.54 | |
| (0.64 to 1.67) | (0.60 to 1.51) | (0.26 to 1.19) | (0.77 to 1.79) | (0.48 to 1.66) | (0.44 to 1.22) | (0.34 to 1.27) | (0.27 to 1.24) | (0.25 to 1.41) | (0.17 to 1.23) | |||
| BCS+SLNB+RT | 0.98 | 0.90 | 0.56 | 1.11 | 0.87 | 0.95 | — | 0.92 | 0.83 | 0.87 | 0.70 | |
| (0.72 to 1.31) | (0.69 to 1.154) | (0.27 to 1.01) | (0.90 to 1.34) | (0.51 to 1.37) | (0.64 to 1.36) | (0.59 to 1.37) | (0.45 to 1.41) | (0.40 to 1.62) | (0.70 to 1.48) | |||
| M | 0.98 | 0.90 | 0.56 | 1.11 | 0.88 | 0.96 | 1.00 | — | 0.93 | 0.98 | 0.76 | |
| (0.69 to 1.36) | (0.65 to 1.22) | (0.26 to 1.03) | (0.85 to 1.43) | (0.49 to 1.4) | (0.61 to 1.43) | (0.80 to 1.24) | (0.45 to 1.73) | (0.41 to 1.98) | (0.34 to 1.47) | |||
| M+ALND | 0.83 | 0.77 | 0.48 | 0.97 | 0.75 | 0.83 | 0.87 | 0.87 | — | 1.11 | 0.91 | |
| (0.57 to 1.20) | (0.52 to 1.11) | (0.22 to 0.92) | (0.58 to 1.54) | (0.40 to 1.27) | (0.45 to 1.43) | (0.54 to 1.35) | (0.53 to 1.40) | (0.48 to 2.17) | (0.30 to 2.16) | |||
| M+ALND+RT | 1.16 | 1.07 | 0.67 | 1.35 | 1.04 | 1.16 | 1.21 | 1.22 | 1.45 | — | 0.91 | |
| (0.75 to 1.66) | (0.72 to 1.47) | (0.30 to 1.24) | (0.79 to 2.06) | (0.53 to 1.73) | (0.61 to 1.94) | (0.74 to 1.80) | (0.71 to 1.86) | (0.79 to 2.30) | (0.27 to 2.31) | |||
| M+RT | 0.88 | 0.82 | 0.51 | 1.02 | 0.80 | 0.87 | 0.92 | 0.92 | 1.10 | 0.79 | — | |
| (0.61 to 1.23) | (0.56 to 1.15) | (0.23 to 0.96) | (0.66 to 1.50) | (0.42 to 1.36) | (0.50 to 1.41) | (0.62 to 1.32) | (0.63 to 1.31) | (0.63 to 1.74) | (0.47 to 1.30) | |||
BCS+ALND = breast-conserving surgery+axillary lymph node dissection; BCS+ALND+RT = breast-conserving surgery+axillary lymph node dissection+radiotherapy; BCS+ANS+RT = breast-conserving surgery+axillary node sample+radiotherapy; BCS+SLNB = breast-conserving surgery+sentinel lymph node biopsy; BCS+SLNB+ART+RT = breast-conserving surgery+sentinel lymph node biopsy+axillary radiotherapy+radiotherapy; BCS+SLNB+IORT = breast-conserving surgery+sentinel lymph node biopsy+intraoperative radiotherapy. BCS+SLNB+RT = breast-conserving surgery+sentinel lymph node biopsy+radiotherapy; CI = confidence interval; DFS = disease-free survival; HR = hazard ratio; M = mastectomy; M+ALND = mastectomy+axillary lymph node dissection; M+ALND+RT = mastectomy+axillary lymph node dissection+radiotherapy; M+RT = mastectomy+radiotherapy; OS = overall survival.
Our network meta-analysis and direct comparisons also showed no statistically significant difference between BCS+ALND and BCS+ALND+RT, BCS+SLNB+RT and BCS+SLNB+IORT, or BCS+SLNB+RT and BCS+SLNB+ART+RT (all 95% confidence intervals stride across 1.00). Additionally, our network meta-analysis demonstrated that there was no statistically significant difference between M+ALND and M+ALND+RT (all 95% confidence intervals stride across 1.00).
Transitivity, Inconsistency, and Heterogeneity
Assessment of transitivity by box plots indicated that the mean age and mean follow-up of early-stage breast cancer across treatment comparisons were relatively similar (Supplementary Figures 3 and 4, available online). The consistency assumption was generally supported by a better trade-off between model fit and complexity when consistency was assumed than when it was not. All loops were consistent because their 95% confidence intervals included 1 (ie, the direct estimate of the summary effect does not differentiate from the indirect estimate) according to the forest plots (Supplementary Figure 5, available online). In addition, heterogeneity was moderate, although for most comparisons the 95% confidence intervals included values that showed very high or no heterogeneity, reflecting the small number of included studies for each pairwise comparison. In the meta-analyses of direct comparisons for OS, I² values higher than 75% were recorded for the comparisons BCS+ALND+RT vs M+ALND+RT (I²=78.2%) for two studies. For DFS, I² values higher than 75% were recorded for the comparisons BCS+ALND vs M+ALND (I²=78.0%) for three studies in the meta-analysis (Table 2).
Ranking of Treatment Arms
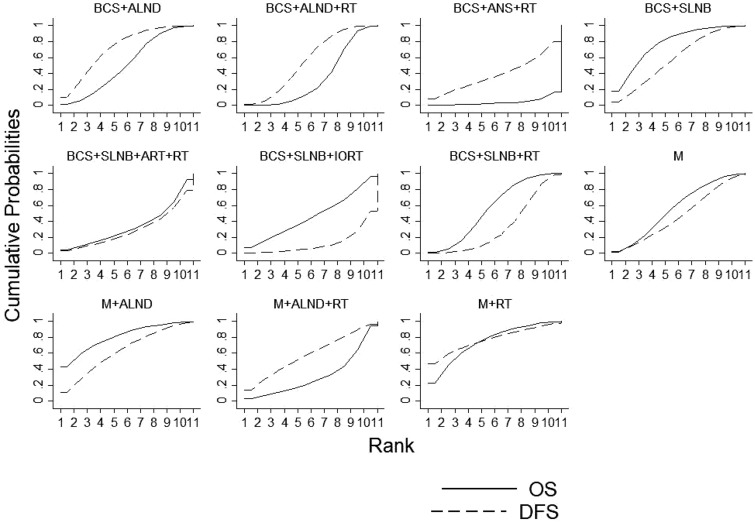
The total values of SUCRA in terms of OS and DFS indicated that M+RT had the highest probability of being the best treatment arm (SUCRA = 152.5%), followed by M+ALND (SUCRA =144.5), BCS+SLNB (SUCRA = 136.7%), BCS+ALND (SUCRA = 124.4%), M (SUCRA = 103.9%), BCS+ALND+RT (SUCRA = 91.4%), M+ALND+RT (SUCRA = 90.3%), BCS+SLNB+RT (SUCRA = 90%), BCS+SLNB+ART+RT (SUCRA = 64%), BCS+SLNB+IORT (SUCRA = 59.2%), and BCS+ANS+RT (SUCRA = 43.2%). The M+RT and BCS+ANS+RT arms had the highest and lowest probability of being the best in terms of OS and DFS, respectively (Figure 2; Supplementary Figure 6, available online). The highest cumulative probabilities of being the best and worst regimen among all surgical treatments in terms of OS and DFS were M+RT (64.7%) and BCS+ANS+RT (104.5%) (Table 4).
Figure 2.
Surface under the cumulative ranking (SUCRA) ranking curve for overall survival (OS) and disease-free survival (DFS). Rankograms display the cumulative probabilities of ranking first to 13th based on the findings of the network meta-analysis; these are used to calculate SUCRA values. BCS+ALND = breast-conserving surgery+axillary lymph node dissection. BCS+ALND+RT = breast-conserving surgery+axillary lymph node dissection+radiotherapy. BCS+ANS+RT = breast-conserving surgery+axillary node sample+radiotherapy. BCS+SLNB = breast-conserving surgery+sentinel lymph node biopsy. BCS+SLNB+ART+RT = breast-conserving surgery+ sentinel lymph node biopsy+axillary radiotherapy +radiotherapy. BCS+SLNB+IORT = breast-conserving surgery+sentinel lymph node biopsy+Intraoperative radiotherapy. BCS+SLNB+RT = breast-conserving surgery+sentinel lymph node biopsy+radiotherapy. M = mastectomy. M+ALND = mastectomy+axillary lymph node dissection. M+ALND+RT = mastectomy+axillary lymph node dissection+radiotherapy. M+RT = mastectomy+radiotherapy.
Table 4.
Ranking for OS and DFS*
| Treatment | Rank 1 |
Rank 2 |
Rank 3 |
Rank 4 |
Rank 5 |
Rank 6 |
Rank 7 |
Rank 8 |
Rank 9 |
Rank 10 |
Rank 11 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | OS | DFS | |
| BCS+ALND | 0.6 | 9.3 | 11.1† | 21.2‡ | 15.7† | 19.8‡ | 14.8† | 18.2‡ | 12.1† | 12.4‡ | 14† | 9.7 | 14.4† | 5.3 | 10† | 2.6 | 5.5 | 1.2 | 1.5 | 0.3 | 0.3 | 0 |
| BCS+ALND+RT | 0.1 | 0.5 | 0.6 | 6.1 | 2.1 | 11.9‡ | 6.8 | 5.2 | 10.9† | 21.2‡ | 12.2† | 19.2‡ | 18.6† | 14.5‡ | 25.5† | 7.7 | 17.2† | 3.1 | 5.8 | 0.6 | 0.2 | 0 |
| BCS+ANS+RT | 0.1 | 8.8 | 0.2 | 5.8 | 0.5 | 5.4 | 0.7 | 5.1 | 0.6 | 5.5 | 0.8 | 6.5 | 1.1 | 5.8 | 2 | 8.2 | 2.7 | 13.4‡ | 7.6 | 14.7‡ | 83.7† | 20.8‡ |
| BCS+SLNB | 15.5† | 5.3 | 24.8† | 11.2‡ | 21.5† | 16‡ | 13.8† | 13 | 8.4 | 13.7‡ | 6.1 | 15‡ | 4.6 | 11.3‡ | 3.5 | 8.4 | 1.5 | 4.4 | 0.3 | 1.5 | 0 | 0.2 |
| BCS+SLNB+ART+RT | 7.5 | 4.8 | 8 | 5.6 | 7.9 | 4.3 | 6.1 | 4.3 | 5.3 | 5.5 | 7.2 | 5.4 | 8.5 | 6.4 | 8.4 | 9.5 | 15.5† | 12.9‡ | 21.9† | 20.3‡ | 3.7 | 21 |
| BCS+SLNB+IORT | 6.8 | 0.4 | 8.3 | 0.9 | 7.6 | 1 | 7.9 | 2.2 | 8.1 | 2 | 9.8 | 1 | 6.6 | 4.2 | 10.5† | 6.1 | 13.9† | 10.6‡ | 16.6† | 25.6‡ | 3.9 | 46‡ |
| BCS+SLNB+RT | 0.3 | 0 | 3.9 | 0.1 | 9.7 | 1.8 | 18.3† | 3.9 | 21.3† | 4.7 | 18.5† | 9.7 | 13.6† | 18.2‡ | 8.4 | 23.6‡ | 4.8 | 21.7‡ | 1.1 | 14.6‡ | 0.1 | 1.7 |
| M | 1.2 | 0.7 | 6 | 6.8 | 9.5 | 8.3 | 13.8† | 9.5 | 14.5† | 11.1‡ | 14.9† | 9.8 | 13.6† | 12.3‡ | 9.7 | 16.8‡ | 10.8† | 13.2‡ | 5.4 | 8.6 | 0.6 | 2.9 |
| M+ALND | 48.1† | 10.3‡ | 18.7† | 16.5‡ | 11.3† | 12.8‡ | 7.4 | 12.9‡ | 5.1 | 10.5‡ | 4.5 | 9.5 | 2.8 | 7.9 | 1.3 | 6.6 | 0.8 | 7.8 | 0 | 3.7 | 0 | 1.5 |
| M+ALND+RT | 1.3 | 13.7‡ | 3.6 | 13.3‡ | 4 | 9.6 | 4 | 9.3 | 6.7 | 8.2 | 5.1 | 9.6 | 9.1 | 9.1 | 14† | 7.4 | 17.4† | 7.9 | 29.9† | 7.9 | 4.9 | 4 |
| M+RT | 18.5† | 46.2‡ | 14.8† | 12.5‡ | 10.2† | 9.1 | 6.4 | 6.4 | 7 | 5.2 | 6.9 | 4.6 | 7.1 | 5 | 6.7 | 3.1 | 9.9 | 3.8 | 9.9 | 2.2 | 2.6 | 1.9 |
Ranks indicate the probability to be the best treatment, the second best, the third best, and so on, among the 11 surgical treatments. BCS+ALND = breast-conserving surgery+axillary lymph node dissection; BCS+ALND+RT = breast-conserving surgery+axillary lymph node dissection+radiotherapy; BCS+ANS+RT = breast-conserving surgery+axillary node sample+radiotherapy; BCS+SLNB = breast-conserving surgery+sentinel lymph node biopsy; BCS+SLNB+ART+RT = breast-conserving surgery+sentinel lymph node biopsy+axillary radiotherapy+radiotherapy; BCS+SLNB+IORT = breast-conserving surgery+sentinel lymph node biopsy+intraoperative radiotherapy. BCS+SLNB+RT = breast-conserving surgery+sentinel lymph node biopsy+radiotherapy; DFS = disease-free survival; M = mastectomy; M+ALND = mastectomy+axillary lymph node dissection; M+ALND+RT = mastectomy+axillary lymph node dissection+radiotherapy; M+RT = mastectomy+radiotherapy; OS = overall survival.
The possibility of being the best treatment, the second best, the third best, and so on, among the 11 surgical treatments was more than 10% for OS.
The possibility of being the best treatment, the second best, the third best, and so on, among the 11 surgical treatments was more than 10% for DFS.
Discussion
To the best of our knowledge, this is the first time network meta-analysis has been used in the field of primary surgical treatment of early breast cancer. Current national and international guidelines are based on the results of single RCTs as well as standard meta-analyses dedicated to pairwise comparisons of two or three surgical treatment options. In the present systematic review, we gathered evidence from RCTs assessing the role of 11 surgical treatment options in more than 30 000 women. This study shows both statistically and clinically significant differences between surgical treatments in early breast cancer. In terms of OS, M+ALND and M+RT outperformed other surgical treatments, and BCS+ANS+RT was inferior to other surgical treatments. In terms of DFS, M+RT was better than M+ALND. Our meta-analysis also showed that patients receiving M+ALND and M+RT achieved statistically significantly better OS and DFS than patients receiving other surgical treatments from the best available evidence. In addition, the OS for M+ALND and M+RT was indistinguishable when compared indirectly in this study, but the overall effect on OS and DFS was inferior in the M+ALND group. Therefore, patients treated with M+RT are expected to benefit from the overall effect on OS and DFS. These results have potential clinical implications that should be considered while developing the clinical practice guidelines.
The values of SUCRA for OS and DFS were the highest for M+RT among all surgical treatments (Figure 2). Interventions with high SUCRA values are ranked higher (28). Therefore, network meta-analysis in this study demonstrated that M+RT may be safer than other surgical regimens as a first-line regimen for treatment in patients with early-stage breast cancer because it has a better overall effect on OS and DFS. Although BCS and M are both well-established local therapies for early breast cancer, a few trials have reported higher rates of locoregional recurrence for BCS than for M (10%–22%) (49,57,65). Fear of cancer recurrence was the major reason for choosing M in a study by Tate et al. (66). The results of quality-of-life surveys have shown that women who underwent BCS experience little change in quality of life over time and those who underwent M experienced a marginally better quality of life over time. This result gave a sense of security and decreased fear of recurrence (67). However, an appreciable risk of local recurrence (eg, in the chest wall or lymph nodes) can remain. Post-M RT can statistically significantly reduce the risk of local recurrence. Previous trials (68–71) and meta-analyses (72,73) have shown that post-M RT can produce a moderate but definitive long-term reduction in breast cancer mortality. Although the likelihood of undergoing radiation following M is changing based on improved understanding of the disease, this is still a decision that is controversial and variable depending on the individual institutions and patient preference. Hence, we strongly considered RT after M for the treatment of patients with early breast cancer.
Our role as health-care professionals is to practice beneficence, present evidence-based information to our patients, and respect and support our patients in their decision making, thereby maximizing long-term patient satisfaction (74). BCS is the main choice of treatment for patients with early breast cancer who are unwilling to undergo M. BCS facilitates the removal of large volumes of breast tissue with statistically significantly improved cosmetic outcomes and patient satisfaction while maintaining good oncological principles and potentially reducing reexcision rates (75) and M rates. A major concern regarding breast-conserving therapy is related primarily to whether local tumor control can be obtained equivalent to that in M. After BCS, a particularly common site of local recurrence is the conserved breast itself (or the axilla, if this has not been treated effectively). Therefore, the most commonly used axillary treatments for breast cancer patients after BCS are SLNB, ALND, and ANS.
Our network meta-analysis proved that ANS is not to be recommended because, in terms of OS and DFS, the combined treatment of BCS+ANS+RT almost achieved the threshold for inferiority compared with the other surgical treatment arms, especially BCS+SLNB. To obtain at least four palpable lymph nodes from the axilla and work upward from the axillary tail, ANS is used. During the pre-SLNB era, the most popular conservative treatment approach to the axilla was undirected four-node sampling. Earlier studies have reported that ANS even acts as a useful alternative to SLNB. Many studies have reported similar node positivity rates with ANS and SLNB, showing they are equally accurate in predicting the axillary nodal status in cases of early breast cancer (76–78). Although palpation of the axilla is an important part of ANS, the technique, if performed without mapping, has been criticized because random selection of the sample nodes is performed solely on the basis of the surgeon’s judgment and expertise (79). Some of the earlier research reports also described ANS as an anatomically imprecise, ill-defined procedure ranging from blind biopsy in the vicinity of the axillary tail to a formal level I dissection (80). Kjaergaard et al. reported that the sampled material contained insufficient or no lymph node tissue at all when their method of ANS was adopted in 40% of cases (81). Thus, in view of the perceived haphazard technique of node identification during surgery, the surgical community has not been enthusiastic to pursue nontargeted approaches to the axilla. Our network meta-analysis also revealed that early breast cancer patients who underwent the combinational therapy of BCS+ANS+RT had poorer survival than those treated with BCS+SLNB. SLNB with blue dye or radiolabeled colloid, either individually (82,83) or in combination (84), is considered to be an effective minimally invasive procedure with low morbidity, high sensitivity (>90%), and a low false-negative rate (81–83,85). Therefore, from our findings it is clear that SLNB is irreplaceable by ANS for axillary treatment in patients with early breast cancer who underwent BCS treatment.
In early breast cancer patients who underwent SLNB following BCS treatment, no statistically significant difference was found in the survival rates between patients who received IORT and RT therapies. IORT is a set of clinical techniques involving administration of a uniform absorbed dose in a single fraction to the tumor or tumor bed during a surgical procedure while the patient is under anesthesia. It is an attractive treatment strategy that not only shortens the course of RT from 3–7 weeks to 2–5 days but also very effectively reduces the radiation dose to the breasts, skin, lungs, and, in particular, heart (86,87). IORT has been a boon especially for elderly patients, working women, and women who live far away from RT facilities because it is devoid of some of the drawbacks of prolonged treatment. Earlier studies have reported appreciable cosmetic outcomes and a lower risk of late side effects on the skin and acute toxicity with the use of IORT than with RT (50,55). Vaidya et al. claimed in their study that the use of IORT instead of RT results in a lower 5-year non-breast cancer and overall mortality rate (88). However, no differences were observed between IORT and RT in either in-breast recurrence or OS in the current study. Patients in the IORT group exhibited an increase in the locoregional recurrence as reported by the TARGeted Intraoperative Radiotherapy Alone trial (89) and the European Institute of Oncology Trial using Electron Intraoperative Radiotherapy (61), but the OS was not found to differ between the treatment groups. Although IORT is advantageous because of a shorter irradiation time, higher quality of life, fewer complications, and better cosmetic effects, its cost is more than 20% more than the cost of RT with no difference in OS between the two groups (90). Socioeconomic factors do influence the patient’s decision to undergo BCS therapy, and no difference in survival results between the two RT methods has been observed; thus, women with limited financial means have been found to opt for RT (91). IORT has not been found to be better than postoperative RT in early breast cancer patients in this study. In addition, whether ART can improve survival rates in early breast cancer patients undergoing the combinational BCS+SLNB+RT therapy remains controversial. Veronesi et al. reported that 5-year DFS was not statistically significantly different between early breast cancer patients who received BCS+SLNB+RT with ART and those who received it without ART (60). ART does not improve survival rates after BCS+SLNB+RT therapy in early breast cancer patients, and thus we found ART to be unnecessary in these patients.
Survival outcomes between BCS+ALND and BCS+ALND+RT therapies were not found to differ in early breast cancer patients in this network meta-analysis study, which means that for patients undergoing ALND post-BCS therapy, RT shows improvement in survival rates. Earlier research has shown ALND is beneficial for patients with early breast cancer because it controls regional nodal disease and may improve OS, and approximately 36% of women diagnosed with early breast cancer undergo ALND surgery (92). Several randomized trials performed before the last decade found ALND is associated with lower rates of axillary recurrence than observed for clinically negative axillary lymph nodes in patients with early breast cancer (46,47). It is yet to be studied clinically whether RT is necessary post–BCS+ALND in early breast cancer patients. Clinical trials have yet to demonstrate an impact of breast irradiation on survival; thus, it is imperative that serious long-term morbidity of treatment be eliminated. Several studies have reported that BCS+ALND followed by RT can reduce the incidence of recurrence of ipsilateral breast tumor and OS at 15 years of follow-up (43,51). A meta-analysis by the Early Breast Cancer Trialists Collaborative Group showed that postoperative RT resulted in a 5.4% reduction in breast cancer mortality at 15 years, but this benefit was found to be partly counteracted by increased deaths due to cardiovascular and lung disease (93,94). In the trial by Wärnberg et al., the omission of RT was not found to statistically significantly affect the overall mortality or indicate an increased risk of cardiovascular deaths after RT (95). The omission of RT was found to be affected neither by breast cancer death nor the overall mortality in our network meta-analysis. Therefore, RT has been found to be unnecessary for early breast cancer after BCS+ALND therapy. Moreover, survival outcome was also not found to be different between patients who received M+ALND and those who received M+ALND+RT in the current study, indicating that RT is not to be recommended for early breast cancer patients after M+ALND therapy.
There are some limitations of this work. First, despite our efforts to be fully systematic in the literature search, some relevant articles might have been overlooked. The findings of these missing reports might change the estimates of the treatment effects calculated in this study, although our conclusions are mainly based on very robust data (as supported by the narrow confidence intervals of most estimates generated by the network meta-analysis). Second, the network meta-analysis was based on the summary data extracted from article reports and not on individual patient data. Although the overall results were found to remain relatively robust with respect to study quality and important baseline characteristics as per the sensitivity analysis (ie, performance status and disease extent), unknown prognostic factors could not be accounted for. For example, there was a difference recorded in the follow-up time, and this might have hampered the interpretation of DFS. Therefore, we also reported OS in our study, because OS is less prone to the influence of the follow-up time. Third, meta-analyses are inherently observational, and despite best efforts to investigate inconsistencies and to assess the impact of effect modifiers using sensitivity analysis, our results may possibly be affected by unmeasured confounding factors. Estimates that substantially rely on indirect evidence should be interpreted carefully. For example, this was the case in many comparisons with BCS+SLNB+IORT, M+ALND+RT, or BCS+ANS+RT therapy.
In conclusion, this is the first study to our knowledge that involved network meta-analysis to examine the survival outcomes of patients with early-stage breast cancer after commonly used surgical treatments and combine available evidence to aid evidence-informed clinical decisions in the management of these patients. Our study, with clinical trial data regarding different surgical treatments (ie, BCS, M+RT), provides evidence that M+ALND and M+RT show the most promising survival outcomes as a first-line regimen for the treatment of patients with early-stage breast cancer but that M+ALND is associated with a poorer DFS. The total values of SUCRA in terms of OS and DFS for M+RT were the highest among all surgical treatments. Therefore, M+RT might be safer than other surgical regimens as a first-line regimen for early-stage breast cancer patients. In addition, our results showed SLNB cannot be replaced by ANS for axillary treatment in patients with early breast cancer who received BCS. For early breast cancer patients who received BCS+SLNB, IORT is no better than postoperative RT and ART is not recommended for patients who choose postoperative RT. Furthermore, postoperative RT cannot be performed in early breast cancer patients receiving BCS+ALND or M+ALND.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (no. 81372813).
Notes
Affiliations of authors: Breast Disease Center (YG, XL, XC, XY, SL, QP, LC) and Burn Research Institute (XL), Southwest Hospital, Army Medical University, Chongqing, China; National Key Laboratory of Trauma and Burns, Chongqing Key Lab of Disease Proteomics, Chongqing, China (XL, LC).
The funder had no role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
The authors have no conflicts of interest to disclose directly related to this work.
Supplementary Material
References
- 1. Fitzmaurice C, Allen C, Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2016;34:524–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Siege RL, Miller KD, Jemal A.. Cancer statistics, 2017. CA Cancer J Clin. 2017;671:7–30. [DOI] [PubMed] [Google Scholar]
- 3. American Joint Committee on Cancer. AJCC Cancer Staging Manual New York, NY: Springer; 2012. [Google Scholar]
- 4. Allegra CJ, Aberle DR, Ganschow P,. et al. National Institutes of Health State-of-the-Science Conference statement: Diagnosis and Management of Ductal Carcinoma In Situ September 22–24, 2009. J Natl Cancer Inst. 2010;1023:161–169. [DOI] [PubMed] [Google Scholar]
- 5. Ernster VL, Ballard-Barbash R, Barlow WE, et al. Detection of ductal carcinoma in situ in women undergoing screening mammography. J Natl Cancer Inst. 2002;9420:1546–1554. [DOI] [PubMed] [Google Scholar]
- 6. Smigal C, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin. 2006;563:168–183. [DOI] [PubMed] [Google Scholar]
- 7. Senkus E, Kyriakides S, Ohno S, et al. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(suppl 5):v8–v30. [DOI] [PubMed] [Google Scholar]
- 8. Peto R, Davies C, Godwin J, et al. ; Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100, 000 women in 123 randomised trials. Lancet. 2012;3799814:432–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wennberg JE, Fisher ES, Skinner JS.. Geography and the debate over Medicare reform. Health Aff (Millwood). 2002;Suppl Web Exclusives:W96–W114. [DOI] [PubMed] [Google Scholar]
- 10. Cody HS. Current surgical management of breast cancer. Curr Opin Obstet Gynecol. 2002;141:45–52. [DOI] [PubMed] [Google Scholar]
- 11. Kumar S, Sacchini V.. The surgical management of ductal carcinoma in situ. Breast J. 2010;16(suppl 1):S49–S52. [DOI] [PubMed] [Google Scholar]
- 12. Vila J, Gandini S, Gentilini O.. Overall survival according to type of surgery in young (≤40 years) early breast cancer patients: a systematic meta-analysis comparing breast-conserving surgery versus mastectomy. Breast. 2015;243:175–181. [DOI] [PubMed] [Google Scholar]
- 13. El Hage Chehade H, Headon H, Wazir U, Abtar H, Kasem A, Mokbel K.. Is sentinel lymph node biopsy indicated in patients with a diagnosis of ductal carcinoma in situ? A systematic literature review and meta-analysis. Am J Surg. 2017;2131:171–180. [DOI] [PubMed] [Google Scholar]
- 14. Zhang L, Zhou Z, Mei X, et al. Intraoperative radiotherapy versus whole-breast external beam radiotherapy in early-stage breast cancer: a systematic review and meta-analysis. Medicine (Baltimore). 2015;9427:e1143.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med. 2002;2116:2313–2324. [DOI] [PubMed] [Google Scholar]
- 16. Lu G, Ades AE.. Combination of direct and indirect evidence in mixed treatment comparisons. Sta Med. 2004;2320:3105–3124. [DOI] [PubMed] [Google Scholar]
- 17. Hoaglin DC, Hawkins N, Jansen JP, et al. Conducting indirect-treatment-comparison and network-meta-analysis studies: report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: part 2. Value Health. 2011;144:429–437. [DOI] [PubMed] [Google Scholar]
- 18. Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Syn Meth. 2012;32:80–97. [DOI] [PubMed] [Google Scholar]
- 19. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;16211:777–784. [DOI] [PubMed] [Google Scholar]
- 20. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR.. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DerSimonian R, Laird N.. Meta-analysis in clinical trials. Control Clin Trials. 1986;73:177–188. [DOI] [PubMed] [Google Scholar]
- 23. Higgins JP, Thompson SG, Deeks JJ, Altman DG.. Measuring inconsistency in meta-analyses. BMJ. 2003;3277414:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Higgins JP, Thompson SG.. Quantifying heterogeneity in a meta-analysis. StaMed. 2002;2111:1539–1558. [DOI] [PubMed] [Google Scholar]
- 25. Caldwell DM, Ades AE, Higgins JP.. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;3317521:897–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mavridis D, Salanti G.. A practical introduction to multivariate meta-analysis. Stat Methods Med Res. 2013;222:133–158. [DOI] [PubMed] [Google Scholar]
- 27. Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G.. Evaluation of inconsistency in networks of interventions. Int J Epidemiol. 2013;421:332–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Salanti G, Ades AE, Ioannidis JP.. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;642:163–171. [DOI] [PubMed] [Google Scholar]
- 29. Agresti R, Martelli G, Sandri M, et al. Axillary lymph node dissection versus no dissection in patients with T1N0 breast cancer: a randomized clinical trial (INT09/98). Cancer. 2014;1206:885–893. [DOI] [PubMed] [Google Scholar]
- 30. Arriagada R, Lê MG, Guinebretière JM, Dunant A, Rochard F, Tursz T.. Late local recurrences in a randomised trial comparing conservative treatment with total mastectomy in early breast cancer patients. Ann Oncol. 2003;1411:1617–1622. [DOI] [PubMed] [Google Scholar]
- 31. Blichert-Toft M, Nielsen M, Düring M, et al. Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol. 2008;474:672–681. [DOI] [PubMed] [Google Scholar]
- 32. Cabanes PA, Salmon RJ, Vilcoq JR, et al. Value of axillary dissection in addition to lumpectomy and radiotherapy in early breast cancer. The Breast Carcinoma Collaborative Group of the Institut Curie. Lancet. 1992;3398804:1245–1248. [DOI] [PubMed] [Google Scholar]
- 33. Canavese G, Bruzzi P, Catturich A, et al. Sentinel lymph node biopsy versus axillary dissection in node-negative early-stage breast cancer: 15-year follow-up update of a randomized clinical trial. Ann Surg Oncol. 2016;238:2494–2500. [DOI] [PubMed] [Google Scholar]
- 34. Chetty U, Jack W, Prescott RJ, Tyler C, Rodger A.. Management of the axilla in operable breast cancer treated by breast conservation: a randomized clinical trial. Edinburgh Breast Unit. Br J Surg. 2000;872:163–169. [DOI] [PubMed] [Google Scholar]
- 35. Clark RM, Whelan T, Levine M, et al. ; Ontario Clinical Oncology Group. Randomized clinical trial of breast irradiation following lumpectomy and axillary dissection for node-negative breast cancer: an update. J Natl Cancer Inst. 1996;8822:1659–1664. [DOI] [PubMed] [Google Scholar]
- 36. Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N.. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;3478:567–575. [DOI] [PubMed] [Google Scholar]
- 37. Fisher B, Anderson S, Redmond CK, Wolmark N, Wickerham DL, Cronin WM.. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995;33322:1456–1461. [DOI] [PubMed] [Google Scholar]
- 38. Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;144:297–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;3056:569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Holli K, Saaristo R, Isola J, Joensuu H, Hakama M.. Lumpectomy with or without postoperative radiotherapy for breast cancer with favourable prognostic features: results of a randomized study. Br J Cancer. 2001;842:164–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fyles AW, McCready DR, Manchul LA, et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N Engl J Med. 2004;35110:963–970. [DOI] [PubMed] [Google Scholar]
- 42. Hughes KS, Schnaper LA, Bellon JR, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol. 2013;3119:2382–2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Killander F, Karlsson P, Anderson H, et al. No breast cancer subgroup can be spared postoperative radiotherapy after breast-conserving surgery. Fifteen-year results from the Swedish Breast Cancer Group randomised trial, SweBCG 91 RT. Eur J Cancer. 2016;67:57–65. [DOI] [PubMed] [Google Scholar]
- 44. Kunkler IH, Williams LJ, Jack WJ, Cameron DA, Dixon JM, PRIME II investigators. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol. 2015;163:266–273. [DOI] [PubMed] [Google Scholar]
- 45. Litière S, Werutsky G, Fentiman IS, et al. Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol. 2012;134:412–419. [DOI] [PubMed] [Google Scholar]
- 46. Louis-Sylvestre C, Clough K, Asselain B, et al. Axillary treatment in conservative management of operable breast cancer: dissection or radiotherapy? Results of a randomized study with 15 years of follow-up. J Clin Oncol. 2004;221:97–101. [DOI] [PubMed] [Google Scholar]
- 47. Martelli G, Boracchi P, Orenti A, et al. Axillary dissection versus no axillary dissection in older T1N0 breast cancer patients: 15-year results of trial and out-trial patients. Eur J Surg Oncol. 2014;407:805–812. [DOI] [PubMed] [Google Scholar]
- 48. Newman LA, Kuerer HM, Hunt KK, et al. Local recurrence and survival among black women with early-stage breast cancer treated with breast-conservation therapy or mastectomy. Ann Surg Oncol. 1999;63:241–248. [DOI] [PubMed] [Google Scholar]
- 49. Poggi MM, Danforth DN, Sciuto LC, et al. Eighteen-year results in the treatment of early breast carcinoma with mastectomy versus breast conservation therapy: The National Cancer Institute Randomized Trial. Cancer. 2003;984:697–702. [DOI] [PubMed] [Google Scholar]
- 50. Polgár C, Fodor J, Major T, Sulyok Z, Kásler M.. Breast-conserving therapy with partial or whole breast irradiation: ten-year results of the Budapest randomized trial. Radiother Oncol. 2013;1082:197–202. [DOI] [PubMed] [Google Scholar]
- 51. Pötter R, Gnant M, Kwasny W, et al. Lumpectomy plus tamoxifen or anastrozole with or without whole breast irradiation in women with favorable early breast cancer. Int J Radiat Oncol Biol Phys. 2007;682:334–340. [DOI] [PubMed] [Google Scholar]
- 52. Sarrazin D, Lê MG, Arriagada R, et al. Ten-year results of a randomized trial comparing a conservative treatment to mastectomy in early breast cancer. Radiother Oncol. 1989;143:177–184. [DOI] [PubMed] [Google Scholar]
- 53. Sato K, Mizuno Y, Fuchikami H, et al. Impact of young age on local control after partial breast irradiation in Japanese patients with early stage breast cancer. Breast Cancer. 2017;241:79–85. [DOI] [PubMed] [Google Scholar]
- 54. Sjöström M, Lundstedt D, Hartman L, et al. Response to radiotherapy after breast-conserving surgery in different breast cancer subtypes in the Swedish Breast Cancer Group 91 radiotherapy randomized clinical trial. J Clin Oncol. 2017;3528:3222–3229. [DOI] [PubMed] [Google Scholar]
- 55. Strnad V, Ott OJ, Hildebrandt G, et al. 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet. 2016;38710015:229–238. [DOI] [PubMed] [Google Scholar]
- 56. Tinterri C, Gatzemeier W, Costa A, et al. Breast-conservative surgery with and without radiotherapy in patients aged 55-75 years with early-stage breast cancer: a prospective, randomized, multicenter trial analysis after 108 months of median follow-up. Ann Surg Oncol. 2014;212:408–415. [DOI] [PubMed] [Google Scholar]
- 57. van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;9214:1143–1150. [DOI] [PubMed] [Google Scholar]
- 58. Veronesi U, Marubini E, Mariani L, et al. Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol. 2001;127:997–1003. [DOI] [PubMed] [Google Scholar]
- 59. Veronesi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;3496:546–553. [DOI] [PubMed] [Google Scholar]
- 60. Veronesi U, Orecchia R, Zurrida S, et al. Avoiding axillary dissection in breast cancer surgery: a randomized trial to assess the role of axillary radiotherapy. Ann Oncol. 2005;163:383–388. [DOI] [PubMed] [Google Scholar]
- 61. Veronesi U, Orecchia R, Maisonneuve P, et al. Intraoperative radiotherapy versus external radiotherapy for early breast cancer (ELIOT): a randomised controlled equivalence trial. Lancet Oncol. 2013;1413:1269–1277. [DOI] [PubMed] [Google Scholar]
- 62. Voogd AC, Nab HW, Crommelin MA, van der Heijden LH, Kluck HM, Coebergh JW.. Comparison of breast-conserving therapy with mastectomy for treatment of early breast cancer in community hospitals. Eur J Surg Oncol. 1996;221:13–16. [DOI] [PubMed] [Google Scholar]
- 63. Wickberg A, Holmberg L, Adami HO, Magnuson A, Villman K, Liljegren G.. Sector resection with or without postoperative radiotherapy for stage I breast cancer: 20-year results of a randomized trial. J Clin Oncol. 2014;328:791–797. [DOI] [PubMed] [Google Scholar]
- 64. Winzer KJ, Sauer R, Sauerbrei W, et al. Radiation therapy after breast-conserving surgery; first results of a randomised clinical trial in patients with low risk of recurrence. Eur J Cancer. 2004;407:998–1005. [DOI] [PubMed] [Google Scholar]
- 65. Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;34716:1233–1241. [DOI] [PubMed] [Google Scholar]
- 66. Tate PS, McGee EM, Hopkins SF, Rogers EL, Page GV.. Breast conservation versus mastectomy: patient preferences in a community practice in Kentucky. J Surg Oncol. 1993;524:213–216. [DOI] [PubMed] [Google Scholar]
- 67. Cohen L, Hack TF, de Moor C, Katz J, Goss PE.. The effects of type of surgery and time on psychological adjustment in women after breast cancer treatment. Ann Surg Oncol. 2000;76:427–434. [DOI] [PubMed] [Google Scholar]
- 68. Arriagada R, Rutqvist LE, Mattsson A, Kramar A, Ratstein S.. Adequate locoregional treatment for early breast cancer may prevent secondary dissemination. J Clin Oncol. 1995;1312:2869–2878. [DOI] [PubMed] [Google Scholar]
- 69. Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. N Engl J Med. 1997;33714:949–955. [DOI] [PubMed] [Google Scholar]
- 70. Overgaard M, Jensen M-B, Overgaard J, et al. Postoperative radiotherapy in high-risk postmenopausal breast cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999;3539165:1641–1648. [DOI] [PubMed] [Google Scholar]
- 71. Ragaz J, Olivotto IA, Spinelli JJ, et al. Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst. 2005;972:116–126. [DOI] [PubMed] [Google Scholar]
- 72. Cuzick J, Stewart H, Rutqvist L, et al. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol. 1994;123:447–453. [DOI] [PubMed] [Google Scholar]
- 73. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of radiotherapy and surgery in early breast cancer: an overview of the randomized trials. N Engl J Med. 1995;33322:1444–1455. [DOI] [PubMed] [Google Scholar]
- 74. Mac Bride MB, Neal L, Dilaveri CA, et al. Factors associated with surgical decision making in women with early-stage breast cancer: a literature review. J Womens Health (Larchmt). 2013;223:236–242. [DOI] [PubMed] [Google Scholar]
- 75. Schaverien MV, Raine C, Majdak-Paredes E, Dixon JM.. Therapeutic mammaplasty--extending indications and achieving low incomplete excision rates. Eur J Surg Oncol. 2013;394:329–333. [DOI] [PubMed] [Google Scholar]
- 76. Parmar V, Hawaldar R, Nair NS, et al. RA Sentinel node biopsy versus low axillary sampling in women with clinically node negative operable breast cancer. Breast. 2013;226:1081–1086. [DOI] [PubMed] [Google Scholar]
- 77. Adwani A, Ebbs SR, Burton S, et al. Sentinel node biopsy should be supplemented by axillary sampling in patients with small breast cancers. Int Sem Surg Oncol. 2005;21:27.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Macmillan RD, Barbera D, Hadjiminas DJ, et al. Sentinel node biopsy for breast cancer may have little to offer four-node-samplers: results of a prospective comparison study. Eur J Cancer. 2001;379:1076–1080. [DOI] [PubMed] [Google Scholar]
- 79. Gui GPH, Joubert DJ, Reichert R, et al. Continued axillary sampling is unnecessary and provides no further information to sentinel node biopsy in staging breast cancer. Eur J Surg Oncol. 2005;317:707–714. [DOI] [PubMed] [Google Scholar]
- 80. Spillane AJ, Sacks NP.. Role of axillary surgery in early breast cancer: review of the current evidence. Aust N Z J Surg. 2000;707:515–524. [DOI] [PubMed] [Google Scholar]
- 81. Kjaergaard J, Blichert-Toft M, Andersen JA, Rank F, Pedersen BV; (Danish Breast Cancer Cooperative Group). Probability of false negative nodal staging in conjunction with partial axillary dissection in breast cancer. Br J Surg. 1985;725:365–367. [DOI] [PubMed] [Google Scholar]
- 82. Giuliano AE, Jones RC, Brennan M, Statman R.. Sentinel lymphadenectomy in breast cancer. J Clin Oncol. 1997;156:2345–2350. [DOI] [PubMed] [Google Scholar]
- 83. Veronesi U, Paganelli G, Galimberti V, et al. Sentinel node biopsy to avoid axillary dissection in breast cancer with clinically negative nodes. Lancet. 1997;3499069:1864–1867. [DOI] [PubMed] [Google Scholar]
- 84. Albertini JJ, Lyman GH, Cox C, et al. Lymphatic mapping and sentinel node biopsy in patient with breast cancer. JAMA. 1996;27622:1818–1822. [PubMed] [Google Scholar]
- 85. McIntosh SA, Purushotham AD.. Lymphatic mapping and sentinel node biopsy in breast cancer. Br J Surg. 1998;8510:1347–1356. [DOI] [PubMed] [Google Scholar]
- 86. García-Cases F, Perez-Calatayud J, Ballester F, Vijande J, Granero D.. Peripheral dose around a mobile linac for intraoperative radiotherapy: radiation protection aspects. J Radiol Prot. 2018;384:1393–1411. [DOI] [PubMed] [Google Scholar]
- 87. Lettmaier S, Kreppner S, Lotter M, et al. Radiation exposure of the heart, lung and skin by radiation therapy for breast cancer: a dosimetric comparison between partial breast irradiation using multicatheter brachytherapy and whole breast teletherapy. Radiother Oncol. 2011;1002:189–194. [DOI] [PubMed] [Google Scholar]
- 88. Vaidya JS, Bulsara M, Wenz F, et al. Reduced mortality with partial-breast irradiation for early breast cancer: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys. 2016;962:259–265. [DOI] [PubMed] [Google Scholar]
- 89. Vaidya JS, Wenz F, Bulsara M, et al. Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet. 2014;3839917:603–613. [DOI] [PubMed] [Google Scholar]
- 90. Grobmyer SR, Lightsey JL, Bryant CM, et al. Low-kilovoltage, single-dose intraoperative radiation therapy for breast cancer: results and impact on a multidisciplinary breast cancer program. J Am Coll Surg. 2013;2164:617–623. [DOI] [PubMed] [Google Scholar]
- 91. Nattinger AB, Kneusel RT, Hoffmann RG, Gilligan MA.. Relationship of distance from a radiotherapy facility and initial breast cancer treatment. J Natl Cancer Inst. 2001;9317:1344–1346. [DOI] [PubMed] [Google Scholar]
- 92. Moore MP, Kinne DW.. Axillary lymphadenectomy: a diagnostic and therapeutic procedure. J Surg Oncol. 1997;661:2–6. [DOI] [PubMed] [Google Scholar]
- 93. Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;3669503:2087–2106. [DOI] [PubMed] [Google Scholar]
- 94. Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;36811:987–998. [DOI] [PubMed] [Google Scholar]
- 95. Wärnberg F, Garmo H, Emdin S, et al. Effect of radiotherapy after breast-conserving surgery for ductal carcinoma in situ: 20 years follow-up in the randomized SweDCIS Trial. J Clin Oncol. 2014;3232:3613–3618. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.