Background:
Extensive evidence indicates that Collaborative Chronic Care Models (CCMs) improve outcome in chronic medical conditions and depression treated in primary care. Beginning with an evidence synthesis which indicated that CCMs are also effective for multiple mental health conditions, we describe a multistage process that translated this knowledge into evidence-based health system change in the US Department of Veterans Affairs (VA).
Evidence Synthesis:
In 2010, recognizing that there had been numerous CCM trials for a wide variety of mental health conditions, we conducted an evidence synthesis compiling randomized controlled trials of CCMs for any mental health condition. The systematic review demonstrated CCM effectiveness across mental health conditions and treatment venues. Cumulative meta-analysis and meta-regression further informed our approach to subsequent CCM implementation.
Policy Impact:
In 2015, based on the evidence synthesis, VA Office of Mental Health and Suicide Prevention (OMHSP) adopted the CCM as the model for their outpatient mental health teams.
Randomized Implementation Trial:
In 2015–2018 we partnered with OMHSP to conduct a 9-site stepped wedge implementation trial, guided by insights from the evidence synthesis.
Scale-Up and Spread:
In 2017 OMHSP launched an effort to scale-up and spread the CCM to additional VA medical centers. Seventeen facilitators were trained and 28 facilities engaged in facilitation.
Discussion:
Evidence synthesis provided leverage for evidence-based policy change. This formed the foundation for a health care leadership/researcher partnership, which conducted an implementation trial and subsequent scale-up and spread effort to enhance adoption of the CCM, as informed by the evidence synthesis.
Key Words: systematic review, meta-analysis, mental health, implementation, evidence-based care
BACKGROUND: THE CLINICAL CHALLENGE
Learning health care systems are those “in which science and informatics, patient-clinician partnerships, incentives, and culture are aligned to promote and enable continuous and real-time improvement in both the effectiveness and efficiency of care.”1 Atkins et al2 note that among the various pathways by which evidence leads to health system change, those that hold most promise for continuous system change are ones in which researchers and health care system leadership partner to develop systems, processes, research agendas, and infrastructure in an iterative process to improve care. This report describes one such partnership, which was established based on an evidence synthesis concerning a care model for treatment of individuals with mental health conditions. This partnership then launched a formal implementation trial, and subsequently initiated an effort to scale-up and spread the care model widely throughout the healthcare system (see Fig. 1 for time line).
FIGURE 1.
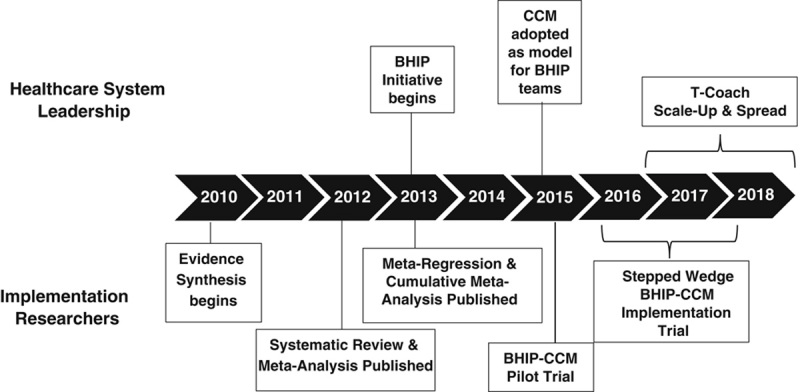
Time line from CCM evidence synthesis through scale-up and spread. BHIP indicates Behavioral Health Interdisciplinary Program Team; CCM, Collaborative Chronic Care Model; T-Coach, Transformational Coaching Program.
Mental health conditions affect 46.6% of Americans during their lives and impact 26.6% in any given year.3 Outcome for mental health conditions is suboptimal, and care coordination is problematic, even in integrated health care systems like the US Department of Veterans Affairs (VA).4,5 Multicomponent care models which emphasize care coordination and evidence-based care have been shown to improve health outcomes for individuals across a variety of medical conditions. Specifically, the Chronic Care Model was developed for chronic medical illnesses treated in primary care. It was developed from the outset as multicomponent organizations of care, based on evidence that addressing single care processes did not improve outcome for chronic conditions.6,7 The model includes several or all of the following elements: work role redesign to support anticipatory, continuous care; patient self-management support; provider decision support; use of clinical information systems; linkage to community resources; and health care leadership support.6–8 These components represent elements that are flexibly implemented depending on local needs, capabilities, and priorities. An extensive evidence base supports effectiveness for chronic medical conditions,8–10 with additional evidence for effectiveness for depression treated in primary care.11,12
In this paper we describe a multistage effort that evolved over 8 years to move the Collaborative Chronic Care Model (CCM) into broad usage in the VA for mental health conditions. This experience illustrates the productive synergy possible when research, policy, and implementation efforts coalesce. Although not preplanned, the stages built sequentially, moving from research-based evidence synthesis to health care system policy change based on the evidence synthesis, to a formal implementation trial in partnership with VA mental health leadership, to scale-up and spread of the model beyond the facilities participating in the formal trial. Relevance to the learning health care system, limitations and challenges, and implications for future work are also discussed.
FROM EVIDENCE SYNTHESIS TO POLICY IMPACT
Evidence Synthesis
In 2010 we recognized that substantial work had been done applying the Chronic Care Model to individuals with a wide variety of mental health conditions, and that the model had been applied well beyond primary care clinics to treat populations cared for in mental health clinics. Therefore we conducted a systematic review and meta-analysis, compiling all the randomized controlled trials of the model for any mental health condition. We defined model-concordant interventions as those with at least 3 of the 6 Chronic Care Model elements above. Not surprisingly, not all interventions that referred to themselves as Chronic Care Models met these criteria, and a substantial number met the criteria without reference to the model—including one study that predated the original articulation of the model by Wagner, Von Korff, and colleagues.13 We also began—at the request of patients we treated in the model—to refer to the model as the CCM.
We included 163 analyses in the systematic review and meta-analysis,14 drawn from 78 articles across 57 trials (depression 41, bipolar disorder 5, anxiety disorders 10, multiple/other 10), with trial sample sizes ranging from 55 to 2796. Our meta-analyses indicated wide-ranging effectiveness of the CCM, typically compared with usual care, across mental health conditions treated in mental health clinics as well as primary care. The modest effect sizes seen (0.20–0.33) were consistent with effects seen in CCMs for medical conditions. Economic analyses indicated that total health care costs did not differ between the CCM and usual care. Systematic review, which also included those studies not amenable to meta-analysis, enlarged, and substantially confirmed meta-analytic findings.
In follow-up, we conducted a cumulative meta-analysis and meta-regression,15 which revealed stable CCM effect sizes over time throughout the literature reviewed. In addition we found, consistent with Wagner et al’s6 early insight, that no 1 of the 6 CCM elements was associated preferentially with therapeutic effects.
Thus this evidence synthesis14,15 indicated that CCMs can improve outcome across various mental health conditions treated in various treatment settings. Notably CCMs, as subjected to meta-analyses, were defined as a family of interventions with elements that were implemented heterogenously, rather than having a defined list of specified steps to institute.
These insights had several implications for future testing and implementation of the CCM. First, while this flexibility may make maintaining internal validity in controlled trials more challenging, it also provides a substantive advantage in terms of external validity and eventual implementation. Thus materials and trainings for implementation must be more adaptable than providing a prespecified step-by-step guide; rather, the process has to accommodate dynamic interplay between core CCM elements and local factors in order to achieve successful adoption of the CCM in diverse clinical locales. These insights aligned our efforts with the model of health care as a complex adaptive system16,17 rather than a highly deterministic machine. Specific to CCM implementation, this suggested that support should focus on creating conditions under which locally designed solutions for local challenges can be developed in accordance with CCM-based guidance, including both team-building and attention to specific health care processes.
Policy Impact of the CCM Evidence Synthesis for Mental Health Conditions
In 2013 the US Department of Veterans Affairs’ Office of Mental Health and Suicide Prevention (OMHSP) began a high priority effort to enhance care coordination in general mental health clinics by establishing interdisciplinary teams (called Behavioral Health Interdisciplinary Program, or BHIP, teams) in each VA medical center nationally. OMHSP had disseminated centralized guidance18 via multiple communication and educational methods, though facilities were given broad latitude to develop team processes locally.
OMHSP became aware of our evidence synthesis,14,15 and in 2015 adopted the CCM as the foundational model for BHIP teams. OMHSP then began collaboration with study investigators to develop CCM training materials and implementation support methods to augment preexisting BHIP guidance, informed by the evidence synthesis.
HEALTH SYSTEM/RESEARCHER PARTNERSHIP TO DEVELOP AND TEST CCM IMPLEMENTATION IMPACT
Forming the Partnership and Laying the Groundwork
Notably, despite strong evidence for CCMs from clinical trials, data on their implementation in clinical practice was quite limited at the time the partnership began. By 2015 only 2 observational studies of CCM implementation for depression in primary care had been published,19,20 with one randomized controlled trial on bipolar disorder in community clinics which showed that the CCM could be implemented21 but did not improve clinical outcome.22 Therefore in 2015, in partnership with OMHSP and the New England VA region (VISN 1), we designed and conducted a pilot implementation trial funded by the VA Quality Enhancement Research Initiative (QUERI) to develop a CCM implementation strategy within the context of a research/policy partnership. As part of this partnership, OMHSP provided the motivation to move the system toward evidence-based team care through the BHIP Initiative, and supplied in-kind resources such as infrastructure to engage sites, publicize activities, and motivate and educate staff about the CCM. Researchers brought to the partnership expertise in implementation science, assessment, and study design.
For this pilot, we adapted the evidence-based blended facilitation implementation strategy developed by Kirchner et al,23 which consisted of an external facilitator partnering with an internal facilitator to support team function and to review and revise specific clinical processes to bring them into alignment with the 6 elements of the CCM. In this implementation strategy, the external facilitator (study-funded) provided guidance and quality improvement expertise to teams while the internal facilitator (facility-funded) worked on-site to direct the redesign process. Pilot work with 1 medical center allowed us to hone the strategy and develop a step-by-step workbook, The BHIP-CCM Enhancement Guide (available on request), to guide implementation.
Designing the Formal Implementation Trial
In 2016–2018 in partnership with OMHSP we conducted a quasi-experimental randomized stepped wedge24,25 trial to implement the CCM for a mixed-diagnosis population treated in general mental health clinics. We designed the trial26 to investigate 2 questions of importance to both VA health care leadership and to the fields of implementation science and mental health services research: (1) Can blended facilitation, utilizing minimal external research support, enhance alignment of BHIP teams with the evidence-based CCM?; and (2) Will alignment with the CCM improve veteran health status and perceptions of care? This dual focus was addressed by a hybrid type II implementation-intervention design, that is, specifying and testing intervention and implementation outcomes of co-equal importance.27
In an ideal research-driven world we would have explored these questions in a randomized controlled trial with a concurrent parallel control group design. However, policy considerations and practicalities led us to a randomized stepped wedge design,24,25 in which all sites received the same implementation support, but the timing of support was randomly assigned. In terms of policy, it was essential that all participating facilities to receive implementation support. Practically, facilitation resources were too limited to intervene at many facilities simultaneously.
Several other considerations shaped trial methodology. Intriguingly, these design decisions, which appeared to be limitations, also conferred benefits:
All sites needed to receive support; this provided motivational benefit in recruiting and retaining sites.
The trial was “piggy-backed” onto the ongoing BHIP Initiative; this allowed us to capitalize on momentum to recruit sites, and enhanced the potential for subsequent sustainability and spread.
OMHSP prioritized working with facilities that were early in the process of improving BHIP care; this policy priority minimized ceiling effects and supported external validity.
Site recruitment utilized preexisting OMHSP national communication structures; this enhanced identification of facilities, particularly sites beyond “usual suspects” and “friends of friends” that often result from word-of-mouth recruiting.
We utilized a community of practice as wait-time control (monthly teleconferences through which sites were introduced to the CCM elements and could share experiences with one another); this provided support to facilities as early as possible while still providing a credible control condition.
One year of implementation support was based on OMHSP experience; this was feasible given available external facilitation resources.
We used a predominantly virtual facilitation strategy via teleconference and telephone, as neither the operational nor the research budget would support frequent facility visits; this subsequently allowed greater spread than intensive on-site facilitation process would.
We utilized existing facility clinicians without research support beyond external facilitation; this made sustainability more likely and also represented a distinct scientific contribution by testing whether limited study-funded implementation support could have impact.
The Randomized Implementation Trial
The final protocol enrolled 9 BHIP teams in 9 VA medical center general mental health outpatient clinics. All facilities received 1 year of facilitation, but start-time was randomized, consistent with a stepped wedge design.24,25 Details are available in the protocol26 and main outcomes28 papers.
Briefly, trial results were promising. As a hybrid type II design,27 outcomes studied included both implementation and clinical outcomes (summarized in Tables 1, 2). Among implementation outcomes, facilitation was associated with improvement in team function. Specifically, while team clinician ratings of communication and cohesion were high at baseline and did not change, significant improvements were seen in team clinician ratings of role clarity and primacy of team goals over individual goals. Concordance with CCM processes was heterogenous, with teams aligning 44%–89% of their clinical processes with CCM principles.
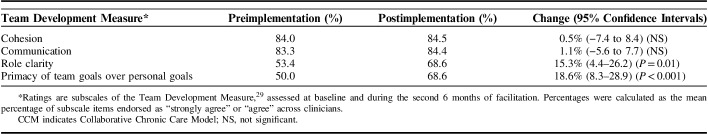
TABLE 1.
Summary of Implementation Outcomes for the CCM Randomized Implementation Trial28
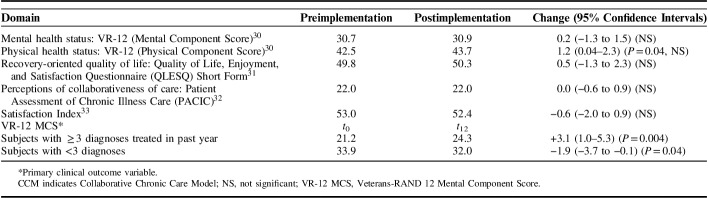
TABLE 2.
Summary of Clinical Outcomes for the CCM Randomized Implementation Trial28
Among intervention outcomes (CCM impact on health status), there was no effect in the interview sample on self-reported mental or physical health status, quality of life, or perceptions of care. However secondary analyses indicated improved mental health status among patients treated for 3 or more mental health conditions in the prior year, compared with others; effects were of similar magnitude to those seen in randomized controlled trials.14,15 In addition, facilitation was associated with a significant and sustained reduction in hospitalization rates, a finding which could not be explained by seasonality, facility-level effects, selective loss to follow-up, or regression to the mean.
In summary, facilitation supported team function while impact on CCM processes was heterogenous. However, benefits were demonstrated in terms of hospitalization rate and, for multimorbidity individuals, mental health status. Thus facilitating CCM-based teams, even with the “light touch” of virtual facilitation using minimal research support, was associated with improvements in outcome at least for complex individuals. Notably, although the study design appeared to be constrained by policy exigencies and practicalities, these factors supported external validity and positioned the partnership to scale-up and spread this practical, efficient implementation support strategy.
SCALE-UP AND SPREAD OF THE EVIDENCE-BASED CCM
On the basis of early experience with the trial, in 2017 OMHSP decided to scale-up and spread the CCM to general mental health BHIP teams in additional VA medical centers. The limited external facilitation resources of the QUERI implementation trial staff would not spread far, so OMHSP engaged the Office of VA Access to Care to provide effort from senior facilitators from their Transformational Coach (T-Coach) program. These T-Coaches came from various disciplines, ranging from clinicians to administrators to chaplains, and had previously received extensive training and certification in a variety of system redesign and team-building modalities. However, few had mental health backgrounds and none was familiar with the BHIP Initiative or the CCM.
The scale-up and spread effort was launched with a 2-day face-to-face training for the T-Coaches in September 2016. The 3 original trial external facilitators and health system leadership served as subject matter experts and conducted the training, which oriented the T-Coaches to VA mental health services, the BHIP Initiative, the CCM, and the implementation strategy that was used in the QUERI-funded trial. After brief content-oriented didactics, the training emphasized role-playing and trouble-shooting. Seventeen T-Coaches were oriented through this training or subsequent cyber-seminar.
Blended facilitation was conducted virtually for 12 months, as in the QUERI-funded trial; however, in this scale-up and spread effort, due to limitations in travel dollars, site visits for several facilities were virtual rather than on-site. Each of the T-Coaches partnered with a BHIP-CCM subject matter expert for the effort, and they conferred on a regular basis throughout the year.
Sites were again recruited via OMHSP, initially working through regional mental health leads who identified sites that had shown an interest in enhancing their BHIP teams and were thought to have at least some available mental health staff who were familiar with system redesign efforts. Thirty-nine sites were approached, with the same requirements as for the QUERI-funded study: willingness to assign 10% effort of a staff member as internal facilitator and willingness to allocate 1 hour per week for the target BHIP team to attend process redesign meetings.
Participation in the scale-up and spread effort is summarized in Figure 2. Of 39 facilities that showed initial interest, 35 (89.7%) signed a letter of agreement. Each T-Coach worked with one to 3 facilities simultaneously. Of those facilities that signed the letter of agreement and began the facilitation process, 28 facilities (80.0%) completed a site visit and entered the ongoing virtual facilitation process. Facilities were widely spread geographically (Fig. 3) and diverse in terms of size, complexity, and rural/urban location.
FIGURE 2.
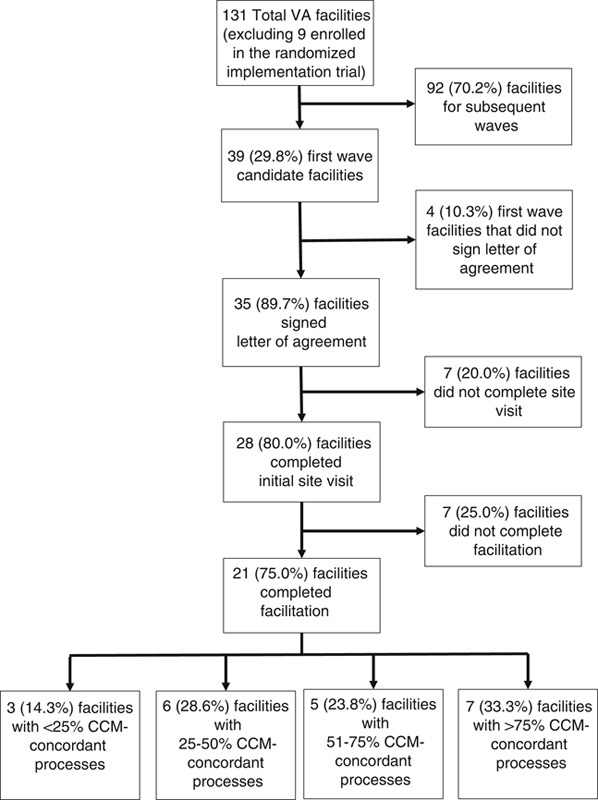
Participation in the CCM scale-up and spread led by Transformational Coaches. CCM indicates Collaborative Chronic Care Model; VA, Veterans Affairs.
FIGURE 3.

Sites engaged in Collaborative Chronic Care Model (CCM) implementation. Triangles represent randomized stepped wedge implementation trial sites (n=9). Circles represent sites that engaged in CCM implementation as part of Transformational Coach scale-up and spread effort (n=28).
Of these 28 facilities, 21 (75.0%) completed the 1-year facilitation process and submitted CCM-concordance process summaries as in the QUERI-funded study. The proportion of CCM-concordant processes ranged widely across facilities, with the more concordant sites equaling rates seen in the QUERI-funded trial along with a broader low-end distribution (trial: 44%–89%, T-Coach scale-up: 13%–93%).
In summary there was, not surprisingly, a broader range of CCM-concordance among these scale-up and spread sites compared with the QUERI-funded trial, and the modest amount of funding support did not allow collection of clinical impact data as in the formal trial. Nonetheless, taken together, the 2 CCM implementation efforts reached 30 VA medical centers, of which 17 (56.7%) aligned over half of designated care processes with the evidence-based CCM.
DISCUSSION
From Evidence Synthesis to Scale-Up and Spread
This report describes the multiyear process by which a comprehensive evidence synthesis provided leverage for evidence-based change for VA mental health services, and stimulated a partnership between health system leadership and implementation researchers. The partnership then collaborated to design and conduct a formal implementation trial funded by QUERI and guided by the evidence synthesis. Subsequently, with strong buy-in from the health system leadership of two VA offices, a scale-up and spread effort supported by the evidence synthesis was conducted.
This experience highlights the synergy possible among research, policymaking, program development, and implementation. The foundational research work of the evidence synthesis both impacted policy (Section 2.2) and informed the design of the implementation strategy for the randomized trial (Section 3.2). The policy exigencies and priorities also influenced the design of the randomized trial (Section 3.2 and Bauer et al26). The implementation trial then contributed to the CCM research literature, not least by virtue of those design features shaped by policy exigencies. The implementation trial also guided the development of the scale-up and spread effort (Section 4), which in turn points the way toward additional research questions (Section 5.3).
Relevance to the Learning Health Care System
This experience also illustrates the relevance of implementation science to the development of a learning healthcare system. Chambers et al34 articulate 4 such contributions.
First, context matters and is multi-level. This effort engaged all levels of the health care system, including top OMHSP leadership, and a facilitation process that engaged stakeholders across all levels of the facility from leadership to front-line staff and the veterans they treat.
Second, the focus must be not just on whether a practice is effective, but whether it can be delivered in many real-world settings. The effort to align BHIP teams with the evidence-based CCM began with a pilot site, then engaged a cohort of trial sites, and then a broad and diverse group of scale-up and spread sites. Moreover, this spread effort entailed working with heterogenous sites rather than those that had already achieved high performance, and working with T-Coaches who, while experienced facilitators, did not have CCM or mental health subject matter expertise.
Third, evidence-based practices should be implemented with evidence-based implementation strategies. This effort utilized blended facilitation, which has a developing evidence base,23 and it contributed to that evidence base by careful attention to measuring both implementation and, in the formal implementation trial, intervention outcomes.
Finally, Chambers and colleagues note that implementation science is a “team sport,” requiring the engagement of a broad array of stakeholders. Consistent with a complex adaptive systems approach,16,17 the BHIP-CCM Enhancement Guide focuses attention on working within a multifaceted health care system, with one of the first tasks for the BHIP team being to identify stakeholders across multiple services and organizational levels, and then to fashion a plan to engage them. Without attention to this issue, no amount of process redesign would have been successful in changing clinical processes.
Limitations and Challenges
This experience also illustrates not only the potential, but also the challenges, of moving from a comprehensive evidence-based synthesis to a formal implementation trial to a broader scale-up and spread effort. First, this process, while relatively fast by research standards, still unfolded over 8 years from beginning the evidence synthesis to finishing the first scale-up and spread wave (Fig. 1). Second, the research effort required adaptation of traditional scientific methods to real-world conditions; nonetheless, design choices that maximized external validity made for the trial actually supported the eventual scale-up and spread process. Third, the success of the effort was highly dependent on organizational commitment from health care system leadership; the scale-up and spread was done on a shoestring budget, but was able to be launched because of the enduring commitment from 2 VA offices.
Finally, we saw greater variability in CCM concordance with T-Coach scale-up and spread than in the implementation trial. This was not surprising, and may have been due to 1 or several factors. The sites may have differed in motivation or capabilities. T-Coaches, though senior facilitators, had less CCM, BHIP, and mental health subject matter expertise than did trial external facilitators. Although the formal implementation trial deployed very little in the way of research-supported resources (only the external facilitator was study-funded), the scale-up and spread process could afford even less tracking and assessment infrastructure.
CONCLUSIONS
Evidence synthesis provided the basis for implementation of the CCM for mental health conditions in VA mental health clinics. It also provided the foundation on which to form a productive health system leadership/implementation researcher partnership. Further, it helped to guide the development of the implementation strategy. These insights led us to take an approach informed by complex adaptive systems theory16,17 and, as our healthcare system leadership partners were often fond of saying, “meeting the sites where they’re at,” while at the same time guiding them with a solid evidence base.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the support of the VA Quality Enhancement Research Initiative (RRP-12-237 and QUE-15-289). The authors also wish to acknowledge the support of the VA Health Services Research and Development Center for Organization, Leadership, & Management Research (COLMR) and its successor the Center for Healthcare Organization & Implementation Research (CHOIR; CIN-13-403), which sponsored the original evidence synthesis project.
Footnotes
M.S.B.: receives royalties from Springer Publishing and New Harbinger Publishing for books related to the Collaborative Chronic Care Model for individuals with bipolar disorder. The remaining authors declare no conflict of interest.
REFERENCES
- 1.Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academy Press; 2012. Available at: www.nap.edu/read/13444/chapter/3. Accessed December 27, 2018. [PubMed] [Google Scholar]
- 2.Atkins D, Kilbourne AM, Shulkin D. Moving from discovery to system-wide change: the role of research in a learning health care system: experience from three decades of health systems research in the Veterans Health Administration. Ann Rev Public Health. 2017;38:467–487. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Ann Rev Public Health. 2008;29:115–129. [DOI] [PubMed] [Google Scholar]
- 4.Hogan MF. New freedom commission report: The President’s New Freedom Commission: recommendations to transform mental health care in America. Psychiatr Serv. 2003;54:1467–1474. [DOI] [PubMed] [Google Scholar]
- 5.Watkins KE, Pincus HA, Paddock S, et al. Care for veterans with mental and substance use disorders: good performance, but room to improve on many measures. Health Aff. 2011;30:2194–2203. [DOI] [PubMed] [Google Scholar]
- 6.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Millbank Q. 1996;74:511–545. [PubMed] [Google Scholar]
- 7.Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–1102. [DOI] [PubMed] [Google Scholar]
- 8.Coleman K, Austin BT, Brach C, et al. Evidence on the Chronic Care Model in the new millennium. Health Aff. 2009;28:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness Part I. J Am Med Assoc. 2002;288:1775–1779. [DOI] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness Part 2. J Am Med Assoc. 2002;288:1909–1914. [DOI] [PubMed] [Google Scholar]
- 11.Badamgarav E, Weingarten SR, Henning JM, et al. Effectiveness of disease management programs in depression: a systematic review. Am J Psychiatr. 2003;160:2080–2090. [DOI] [PubMed] [Google Scholar]
- 12.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166:2314–2321. [DOI] [PubMed] [Google Scholar]
- 13.Callahan CM, Hendrie HC, Dittus RS, et al. Improving treatment of late life depression in primary care: a randomized clinical trial. J Am Geriatr Soc. 1994;42:839–846. [DOI] [PubMed] [Google Scholar]
- 14.Woltmann E, Grogan-Kaylor A, Perron B, et al. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatr. 2012;169:790–804. [DOI] [PubMed] [Google Scholar]
- 15.Miller CJ, Grogan-Kaylor A, Perron BE, et al. Collaborative chronic care models for mental health conditions: cumulative meta-analysis and metaregression to guide future research and implementation. Medical Care. 2013;51:922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plesk P.Committee on Quality of Health Care in America, Institute of Medicine Redesigning health care with insights from the science of complex adaptive systems. Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001:309–322. [Google Scholar]
- 17.Jordan ME, Lanha HJ, Crabtree BF, et al. The role of conversation in health care interventions: enabling sensemaking and learning. Implement Sci. 2009;4:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Department of Veterans Affairs Office of Mental Health and Suicide Prevention. BHIP Technical Assistance SharePoint. 2013. Available at: https://vawwportalvagov/sites/OMHS/BHIP/defaultaspx. Accessed December 5, 2018.
- 19.Solberg LI, Crain AL, Jaeckels N, et al. The DIAMOND initiative: implementing collaborative care for depression in 75 primary care clinics. Implement Sci. 2013;8:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bauer AM, Azzone V, Goldman HH, et al. Implementation of collaborative depression management at community-based primary care clinics: an evaluation. Psychiatr Serv. 2011;62:1047–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waxmonsky J, Kilbourne AM, Goodrich DE, et al. Enhanced fidelity to treatment for bipolar disorder: results from a randomized controlled implementation trial. Psychiatr Serv. 2014;65:81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kilbourne AM, Goodrich DE, Nord KM, et al. Long-term clinical outcomes from a randomized controlled trial of two implementation strategies to promote collaborative care attendance in community practices. Admin Policy Ment Health. 2015;42:642–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirchner JE, Ritchie MJ, Pitcock JA, et al. Outcomes of a partnered facilitation strategy to implement primary care-mental health. J Gen Intl Med. 2014;29(suppl 4):904–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hargreaves JR, Prost A, Fielding KL, et al. How important is randomisation in a stepped wedge trial. Trials. 2015;16:359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prost A, Binik A, Abubakar I, et al. Logistic, ethical, and political dimensions of stepped wedge trials: critical review and case studies. Trials. 2015;16:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bauer MS, Miller C, Kim B, et al. Partnering with health system operations leadership to develop a controlled implementation trial. Implement Sci. 2016;11:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Curran GM, Bauer M, Mittman B, et al. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care. 2012;50:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bauer MS, Miller C, Kim B, et al. Effectiveness of implementing a collaborative chronic care model on mental health clinician teams and the mental health of patients receiving care: a randomized trial. JAMA Network Open. 2019;2:e190230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stock R, Mahoney E, Carney P. Measuring team development in clinical settings. Fam Med. 2013;45:691–700. [PubMed] [Google Scholar]
- 30.Selim AJ, Rogers W, Fleishman JA, et al. Updated US population standard for the Veterans RAND 12-item Health Survey (VR-12). Qual Life Res. 2009;18:43–52. [DOI] [PubMed] [Google Scholar]
- 31.Riendeau RP, Sullivan JL, Meterko M, et al. Factor structure of the Q-LES-Q Short Form in an enrolled mental health clinic population. Qual Life Res. 2018;27:2953–2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gugiu PC, Coryn C, Clark R, et al. Development and evaluation of the shrot version of the Patient Assessment of Chronic Illness Care instrument. Chronic Illn. 2009;5:268–276. [DOI] [PubMed] [Google Scholar]
- 33.Nabati L, Shea N, McBride L, et al. Adaptation of a simple patient satisfaction instrument to mental health: psychometric properties. Psychiatry Res. 1998;77:51–56. [DOI] [PubMed] [Google Scholar]
- 34.Chambers DA, Feero WG, Khoury MJ. Convergence of implementation science, precision medicine, and the learning health care system: a new model for biomedical research. J Amer Med Assoc. 2016;315:1941–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]