Abstract
This is a protocol for a Cochrane Review (Intervention). The objectives are as follows:
To assess the effects of decentralisation or centralisation of governance of health services on access to health care, utilisation of health services, population health and other outcomes of interest.
Background
Governance, particularly ‘good governance’ is an important determinant of economic growth, social advancement, and overall development, including the eight millennium development goals (MDGs) to be achieved in low‐and‐middle‐income countries (LMICs) (Akin 2001; Davoodi 1998; Siddiqi 2009). According to the United Nations Development Program (UNDP), governance is “the exercise of political, economic and administrative authority in the management of a country’s affairs at all levels” (United Nations Development Program 1997). In order to achieve development goals, public sector policy reforms are ongoing in both high‐income countries (HICs) and LMICs. Decentralisation is one such public sector policy reform, in which greater autonomy is provided to lower levels for one or more governmental services, including those levels responsible for health services. Thus decentralised governance of health services means transfer of authority in planning, management and decision making from national to sub‐national level (i.e. to the regional, state, district/municipal level), or in general from higher levels to lower levels in the hierarchy of governance (Robalino 2001). Decentralised governance of the health system may encompass some of the typical functions of higher level (central) government such as the allocation of central funds and recruitment of human resources for health. Authority for some functions may remain centralised while others are decentralised. Typically, decentralisation is a dynamic phenomenon with greater or less centralisation of governmental services at different times, depending on the political context.
In HICs such as the USA, UK, Spain and Italy, decentralisation of health services has been a part of broader fiscal decentralisation in which federal authority has been devolved to the sub‐national level by providing autonomy to regional and local authorities (Litvak 1998; Mills 1990; Saltman 2007). In contrast to this, decentralisation of the health services in many LMICs has mostly occurred as a response to the primary healthcare approach promoted by international agencies such as the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) (Akin 2001; WHO 1995). Health system decentralisation has been implemented in different forms and to different extents depending on the existing political and public administrative structure of the country and the organisation of the health system itself (Bossert 1995; WHO 1995). For instance, in Botswana, primary health care was decentralised to district and town councils and managed by a district health team while central government continued to fund the capital grants and recurrent expenses (Maganu 1990). In Chile, there are two levels of decentralisation: regional level and municipalities. The regional health secretariat and area health services have complete autonomy in all functions and in health services administration. Through an agreement with the director of health services, the municipalities own the primary healthcare system (which includes infrastructure, equipment and staff) but the costs of services, including staff salaries, are paid by national health funding (Montoya‐Aguilar 1990).
Several countries in south‐east Asia, including India, Nepal and Bangladesh, have also accepted decentralisation in principle through their respective constitutions and policy frameworks. However, the implementation of decentralisation has been very limited due to a lack of committees, boards or local governments (such as municipalities) in many settings; the unwillingness of central actors to take forward these policies; and resistance from health staff themselves (Pokharel 2000).
Description of the condition
Decentralisation of health services is not a simple health sector reform since it is not always clear which functions should be decentralised, who will initiate the process and at which levels decentralisation should take place. Furthermore, the enabling or constraining conditions for successful decentralisation are not well understood(Asfaw 2007; Jutting 2005).
Available studies on the effects of decentralised public governance (in general) report only outcomes such as government’s size and quality, and economic growth, and little on the effects of decentralisation on population health outcomes (Robalino 2001) and health systems performance, in terms of quality, access, utilisation, equity and efficiency. This literature is diverse in quality and content. It includes country case studies with descriptive analyses, qualitative studies and appraisals of decentralised health services governance. This literature provides theoretical frameworks and causal hypothesis about the possible effects of decentralised governance of health services on population health outcomes. However, there are a few quasi‐experimental and mixed methods studies which have assessed the effects of decentralised health services governance on health outcomes.
Description of the intervention
There is a lack of clear definitions for types and levels of decentralisation. Two approaches have been proposed for understanding decentralisation of health services. In the early 1990s, the WHO proposed a four‐fold typology (Mills 1990). Later, Bossert outlined a 'decision space approach' (Bossert 1998) which uses a ‘decision space map’ to help analyse the range of choices available. This approach focuses on how much choice is exercised by decentralised decision makers over ‘what functions'. The decision space approach defines health system functions (such as financing, service delivery, human resources, access rules, and governance) and their sub‐functions, and the range of choice exercised by officials at different levels of the health system for these functions (defined as ‘narrow’, ‘moderate’ or ‘wide’) (see Table 1) (Bossert 1998). The approach is therefore applicable to both decentralised and more centralised health system governance. Where governance is more centralised, the range of choice (authority) over various health system functions is greater for higher administrative levels, such as state/regional/provincial or national levels.
Table 1.
A ‘decision space map’ for analysing the range of choices exercised by decentralised decision makers
| Key functional areas |
| Financing‐ Sources of revenue ‐ Allocation of expenditures ‐ Income from fees and contracts |
| Service delivery and organisation‐ Hospital autonomy ‐ Insurance plans ‐ Payment mechanisms ‐ Contracts with private providers ‐ Required programs/norms |
| Health workforce‐ Salaries ‐ Contracts ‐ Civil service |
| Access rules‐ Targeting |
| Governance rules‐ Facility boards ‐ Health offices ‐ Community participation |
We will draw on elements of the 'decision space approach' for this review.
Based on this approach, we will include healthcare decisions made both at central and decentralised levels and covering a range of areas such as financing, service delivery and organisation over which the decision makers have authority. However, we will not attempt to classify the range of choice exercised by officials into ‘narrow’, ‘moderate’ and ‘wide’ since these categories are difficult to define clearly in the context of this review.
How the intervention might work
Governance forms one of the WHO's building blocks for health systems and influences the functions of the other building blocks within this framework (WHO 2007). It has been suggested that good governance may lead to improved health system performance (Bossert 1995). Indeed, the ultimate goal of health system reforms involving decentralised governance is often to improve access to and utilisation of healthcare services. Improved access may, in turn, lead to improvements in population health outcomes such as morbidity, disability and mortality (Collins 1995; Khaleghian 2004; Mills 1990).
In centralised governance, resources such as staffing and funding are managed from the centre and allocated to specific health programmes or functions. However, more decentralised models of governance, in which local decision makers have greater decision space, may help to ensure that the selection of priorities is more congruent with local needs as lower level authorities may have a better understanding of how best to use available resources. Decentralised governance may also be more accountable to local communities and stakeholders and may help to build local institutional capacity (Heywood 2010). One of the pathways through which decentralisation may improve access to health care and other social services may therefore be through enhancing the participation of the community in decision making (Collins 1994; Robalino 2001). However, it has been argued that institutional capacity and mechanisms of accountability are necessary for decentralised authority to translate into improvements in lower level health systems (Bossert 2011). In addition to the above benefits, decentralised health programs are said to be closer to their users, fulfil local health needs and allow for increased flexibility and transparency (Lieberman 2002; Litvack 1999). Figure 1 shows a logic model of pathways leading to improved health outcomes as a result of decentralised governance of health.
Figure 1.
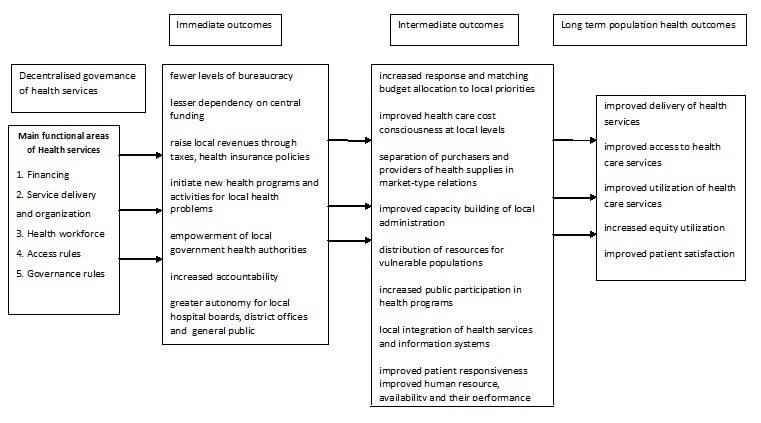
Logic model for pathways of decentralised governance of health services on health outcomes
Decentralised health systems governance may also have negative impacts. For example, poorer local governments may not be able to raise necessary revenues, resulting in the inadequate allocation of funds. For instance, local governments may provide inadequate funding for preventive services in the absence of centrally‐funded vertical health programs. Other unintended effects could include increased workloads of frontline health workers due to the integration of services at local level and expansion of the range of services provided by them. This, in turn, may lead to burnout and low morale (Lakshminarayanan 2003). Other potential negative consequences include the mismanagement of funds in the absence of control by higher authorities, and poor management of health services due to new roles and responsibilities, particularly if local managers do not have sufficient capacity and training to take on these roles (Tanzi 1996).
Why it is important to do this review
There is conflicting evidence regarding the desirable and undesirable effects of decentralisation and centralisation (Anokbonggo 2004; Atkinson 2004; Bossert 2002; Bossert 2003; Bossert 2007; Gupta 2004; Heywood 2010; Jimenez 2005; Lakshminarayanan 2003; Robalino 2001; Rubio 2011; Soto 2012). To date, no systematic review has been undertaken to assess the available evidence of the effects of decentralisation or centralisation on access to health care, utilisation of health services, population health and other outcomes of interest.
Objectives
To assess the effects of decentralisation or centralisation of governance of health services on access to health care, utilisation of health services, population health and other outcomes of interest.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs)
Non‐randomised controlled trials (NRCTs)
Controlled before‐after (CBA) studies
Interrupted time series (ITS) studies
CBA studies with at least two intervention sites and at least two control sites and ITS studies with at least three time points before and after the implementation of the intervention will be considered. We will include cluster randomised and non‐randomised studies, provided that they meet our other inclusion criteria.
Types of participants
Decision makers, including policy makers, public officials and health facility managers; health service providers; and health service users in any country.
Types of interventions
Centralisation of governance of health services where the authority for policy making, planning or management is transferred to a higher (more central) level of government from a lower (more decentralised) level of government; e.g. from district to state or from state to national authorities.
Decentralisation of governance of health services, where the authority for policy making, planning or management is transferred to a lower (more decentralised) level of government, from a higher (more central) level of government; e.g. from national to state or from state to district authorities.
Interventions to decentralise or centralise health service governance may include components intended to change the degree to which officials and others making decisions regarding health care make use of their decision‐making powers (i.e. their decision space (Bossert 1998)).
‘Authorities’ include governments and government agencies with responsibility for policy making, planning or management of health services. Government agencies can have varying degrees of autonomy, independence and accountability.
Exclusions
We will exclude interventions that transfer authority from the government to a government agency, or from a government agency to the government at the same level of government. This is because such changes do not constitute either centralisation or decentralisation of health service governance.
We will exclude interventions that do not transfer authority for policy making, planning or management of health services. This includes transfer of authority over educational institutions that train health professionals and transfer of authority over other sectors that affect health (e.g. food or housing), unless it is part of a broader reform that also includes transfer of authority over health services.
We will exclude interventions that expand the authority of the government or government agencies by transferring authority from the private sector to the government or a government agency. Interventions that transfer authority from the government or a government agency to the private sector (privatisation) also will be excluded. This includes transfer of authority to or from professional organisations, non‐governmental organisations, and international development agencies. This is because such changes do not necessarily constitute either centralisation or decentralisation of health service governance.
Types of outcome measures
Primary outcomes
To be included, studies must report at least one of the following types of outcomes:
Utilisation, coverage or access to health services or health insurance
Quality of care
Patient outcomes
Resource use
Productivity or efficiency
Any adverse (undesirable) effects
Secondary outcomes
In addition we will record any of the following outcomes that are reported in included studies:
Impacts on equity (i.e. differential effects across advantaged and disadvantaged populations, such as low‐income or rural populations)
Health provider outcomes, including workload, work morale, stress, burnout, sick leave
Satisfaction of patients, providers, decision makers or other stakeholders
Changes in revenue sources
Search methods for identification of studies
We will search for and include both published and unpublished studies and studies reported in any language without any time limits.
Electronic searches
We will search the following electronic databases:
The Cochrane Central Register of Controlled Trials (including The Cochrane Effective Practice and Organisation of Care (EPOC) Group Specialised Register) (The Cochrane Library)
MEDLINE (Ovid)
EMBASE (Athens)
PubMed
International political science abstracts (Ebsco)
PAIS
Worldwide Political Science Abstracts
Health Management
Global Health (CAB Direct)
World Health Organization (WHO) Global Health Library
The Database of Abstracts of Reviews of Effects (DARE, The Cochrane Library)
LILACS
We will develop strategies that incorporate the methodological component of the EPOC search strategy combined with selected index terms and free text terms. The MEDLINE search strategy will be translated into the other databases using the appropriate controlled vocabulary as applicable (See Appendix 1 for our MEDLINE search strategy).
We will search for ongoing trials in the following two trial registries:
International Clinical Trials Registry Platform (ICTRP), World Health Organization (WHO): http://www.who.int/ictrp/en/
ClinicalTrials.gov, US National Institutes of Health (NIH): http://clinicaltrials.gov/
Searching other resources
We will search the websites and online resources of the following organisations: United Nations Development Program, World Bank, European Observatory on Health Systems and Policies, the Society for Health Systems Research.
We will also handsearch the journals Health Policy and Planning and Health Services Research.
We will check the reference lists of all the identified primary studies to identify additional studies. The authors of relevant studies will also be contacted to identify any further published or unpublished studies. In addition, we will search the Science Citation Index and the Social Sciences Citation Index for studies which cite studies included in the review.
We will contact experts in the field of health systems research or authors of other relevant reviews to check if they are aware of any relevant studies.
Data collection and analysis
Selection of studies
The search results from the various sources will be uploaded into EROS (Early Review Organising Software) (see: http://www.eros‐systematic‐review.org/). We will use EROS for managing and screening references. We will delete duplicate records of the same references. Titles, abstract and full text articles for potentially‐relevant studies will be screened independently by two review authors (CTS and TNS).
Any disagreements between the authors will be resolved through discussion or by consultation with a potential third review author. If a potentially‐eligible study or included study has incomplete information, we will attempt to contact the authors to obtain further details.
Data extraction and management
Each of the two review authors will independently extract data from the eligible studies, including the following elements:
1) Study details
Name of the first author
Year when the study was conducted
Date of publication
Country and region within the country where study was conducted
World Bank classification of the country (low‐income country, middle‐income country or high‐income country)
2) Types of interventions
Level of government or government agencies to which authority is transferred
Level of government or government from which authority is transferred
Types of areas for which authority is transferred (e.g. decisions about financing, service organisation, human resources)
How decentralisation/centralisation was undertaken (i.e. the process used to implement this change)
Intervention group participants
Control group participants
We will also extract information about key functional areas for which authority was transferred. For example, these may include the formation of local governing bodies (e.g., at district hospitals or at community level) who have autonomy to levy user fees and to use the funds generated for hospital development, procuring essential drugs and equipment, recruiting doctors, nurses, technicians, etc.
3) Study characteristics
Study design
Risk of bias (see Assessment of risk of bias in included studies below)
4) Outcome measures assessed in the study
Primary outcomes
Secondary outcomes
Assessment of risk of bias in included studies
Two independent authors (CTS and TNS) will assess the risk of bias for studies that are included in the review. For this purpose we will use the 'Risk of bias' criteria suggested by the Cochrane Effective Practice and Organisation of Care (EPOC) group (EPOC 2013). These include nine criteria which provide guidance to assess sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome and reporting and other potential sources of bias for randomised trials, non‐randomised trials and controlled before‐after studies, and seven criteria for interrupted time series studies. The studies will be divided into three categories based on the 'Risk of bias' approach suggested in the Cochrane Handbook (Higgins 2011): low risk of bias, moderate risk of bias, high risk of bias. Disagreements about risk of bias will be resolved either through discussion or by consulting the third author.
Measures of treatment effect
Continuous and categorical data extracted from eligible studies will be analysed separately. For dichotomous outcome variables we will calculate risk ratios and their 95% CIs. For continuous data we will calculate mean differences and their 95% CIs. If similar outcomes are measured on different scales, we will calculate standardised mean differences. For continuous outcomes, we will preferably extract post‐intervention values if the required means and standard deviations are available, since all studies may not report change from baseline (change score) (Higgins 2008).
For ITS studies, we will perform re‐analysis if sufficient data are available from the eligible studies or authors provide the data (if sufficient data are not available). For each outcome measure we will undertake re‐analyses to calculate standardised short‐ and long‐term effects as the changes in level and in trends (respectively) before and after the intervention (Aaserud 2006).
Unit of analysis issues
If cluster randomised trials or controlled before‐after studies are included in the review, we will use the reported cluster adjusted risk ratios or mean differences and their 95% CIs. If the analysis was not adjusted for clustering we will use the intracluster correlation coefficient (ICC), if available, to adjust the confidence interval. If the ICC is not available, we will attempt to impute it from other studies included in the review.
Dealing with missing data
We will try to contact the authors of included studies to obtain missing data where possible. If it is not possible to obtain missing data, we will attempt to impute missing values. All the assumptions made for any imputations will be documented.
We will use intention‐to‐treat analyses if the authors have reported this or contact the authors to perform such re‐analyses. In case of unavailability of intention‐to‐treat analyses, and indications that the data are not missing at random, we will consider whether this constitutes a risk of bias.
If aggregate data such as the standard deviation for change‐from‐baseline are missing, we will use the standard deviation for the same outcome from another study, if available, or we will impute the standard deviations using recommended methods (Abrams 2005).
Assessment of heterogeneity
Studies meeting the inclusion criteria will be assessed for heterogeneity on the basis of the context (including the income level of the country), differences in the participants, differences in the interventions with respect to the levels from and to which authority is transferred and the decision space (types of authority that are transferred), and differences in study designs.
For studies that evaluate similar interventions and report similar outcomes and might therefore be included in a meta‐analysis, statistical heterogeneity will be measured according to recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (section 9.5.2). We will measure heterogeneity using the I2 statistic. This statistic describes the percentage of total variation across studies that is due to heterogeneity (Higgins 2011).
Assessment of reporting biases
If there is a sufficient number of included studies (at least 10) reporting similar comparisons and outcomes, we will examine asymmetry in funnel plots as an indication of the need to explore the risk of publication bias or other causes of asymmetry (Sterne 2001). For continuous outcomes with intervention effects measured as mean differences, the test proposed by Egger 1997 will be used to test for funnel plot asymmetry. For dichotomous outcomes with intervention effects measured as risk ratios, and continuous outcomes with intervention effects measured as standardised mean differences, we will not undertake funnel plot calculations as the methods for this are not well developed.
We will interpret the results of tests for funnel plot asymmetry in the light of visual inspection of the funnel plot, as the statistical results may not be representative if there are small‐study effects.
Data synthesis
Studies that evaluate similar interventions will be grouped together and the results for those studies will be summarised in tables, including key characteristics of each study (explanatory factors), outcomes reported in natural units and, when relevant, standardised outcome measures to facilitate comparisons across studies. If there are two or more studies that evaluate similar interventions and report similar outcomes, we will calculate pooled risk ratios, mean differences or standardised mean differences using a random‐effects model. Otherwise, we will report the median and range of effects, if relevant, or measures of effect from individual studies when there are not other studies evaluating a similar intervention and reporting a similar outcome.
For each group of studies we will prepare a 'Summary of findings' table, including an assessment of the quality of evidence for each of the main outcomes or types of outcomes (as listed under Types of outcome measures above). Quality of evidence will be assessed using the GRADE approach (Guyatt 2008).
Subgroup analysis and investigation of heterogeneity
We expect that there could be variations in the findings of the different studies included in the review due to various sources of heterogeneity. These include the level to and from which authority was transferred, the areas of health service governance for which authority was transferred, economic status of the countries (HICs or LMICs according to the World Bank classification), political structure (i.e. the system of government of the country) and the outcomes measured (e.g. utilisation, coverage or access for different types of health services) (see Table 2). We will use graphical ways to report the results (e.g. bubble plots or box‐plots displaying medians and quartiles) to visually explore heterogeneity due to the factors outlined above. If this approach suggests important heterogeneity, and there are sufficient numbers of studies, meta‐regression will be used to examine the listed variables as predictors of heterogeneity. We will use 'metareg' command in STATA (version 10) with the restricted maximum likelihood option (Sharp 1998). We will also consider equity analysis for selected outcomes. Equity analysis will explore if subgroups of the included populations, such as the poorest and richest or lowest educated and highest educated groups, benefited equally from the intervention. We will classify the populations according to whatever relevant social determinants of health are reported in each study.
Table 2.
Subgroup analyses for differences in the effects of decentralised or centralised authority
| Explanatory factors | Categories that will be considered for each factor | Predicted interaction and its direction |
| Functional areas of health services governance for which authority was transferred |
|
|
| Economic status of the country (World Bank definition) |
|
The effects of decentralised governance of health services may be less in LMICs compared to HICs. This is because the infrastructure and resources to support decentralisation are inadequate or less developed in LMICs. |
If sufficient studies reporting similar interventions and similar outcomes are available we will perform subgroup analyses to explore the differences in main outcome measures according to the categories outlined in Table 2.
Sensitivity analysis
We will test the robustness of our findings by modifying any assumptions that are made about missing data within a plausible range of values and by removing studies at a high risk of bias, if there are studies with different risks of bias evaluating the similar interventions and reporting similar outcomes.
Acknowledgements
The authors acknowledge the help provided by Marit Johansen in developing the search strategies and additional support from the Cochane EPOC Review Group.
Appendices
Appendix 1. MEDLINE search strategy
| # | Searches |
| 1 | (decentraliz* or decentralis* or de centraliz* or de centralis*).ti,ab. |
| 2 | (((transfer* or transition? or hand* over or handover or pass* over or passover or shift* or delegat* or devolv* or devolution) adj6 (authority* or responsibilit* or resources or funds or funding or autonomy or autonomous)) and (district* or region* or local or municipal* or community or communities or town?)).ti,ab. |
| 3 | (governance adj3 (district* or region* or local or municipal* or community or communities or town? or centralized or centralised)).ti,ab. |
| 4 | or/1‐3 |
| 5 | randomized controlled trial.pt. |
| 6 | controlled clinical trial.pt. |
| 7 | multicenter study.pt. |
| 8 | (randomis* or randomiz* or randomly).ti,ab. |
| 9 | groups.ab. |
| 10 | (trial or multicenter or multi center or multicentre or multi centre).ti. |
| 11 | (intervention? or controlled or control group? or (before adj5 after) or (pre adj5 post) or ((pretest or pre test) and (posttest or post test)) or quasiexperiment* or quasi experiment* or evaluat* or effect? or impact? or time series or time point? or repeated measur*).ti,ab. |
| 12 | or/5‐11 |
| 13 | exp Animals/ |
| 14 | Humans/ |
| 15 | 13 not (13 and 14) |
| 16 | review.pt. |
| 17 | meta analysis.pt. |
| 18 | news.pt. |
| 19 | comment.pt. |
| 20 | editorial.pt. |
| 21 | cochrane database of systematic reviews.jn. |
| 22 | comment on.cm. |
| 23 | (systematic review or literature review).ti. |
| 24 | or/15‐23 |
| 25 | 12 not 24 |
| 26 | 4 and 25 |
What's new
| Date | Event | Description |
|---|---|---|
| 19 September 2019 | Amended | Protocol withdrawn from publication |
Contributions of authors
CTS: drafted the protocol, will obtain copies of the studies and select studies to be included, extract data and enter data into RevMan, perform the analysis and interpret the results, and draft and update the final review.
TNS: will obtain copies of the studies and select which studies to include, extract the data and carry out duplicate data entry, interpret the analysis, and co‐draft the final review.
Declarations of interest
No conflict/s of interests to declare.
Notes
This protocol has not been successfully converted into a full Cochrane Review within established timelines due to lack of resources to complete the review. For this reason, the protocol has been withdrawn from the CDSR.
Withdrawn from publication for reasons stated in the review
References
Additional references
- Aaserud M, Dahlgren AT, Sturm H, Kosters JP, Hill S, Furbert CD, et al. Pharmaceutical policies: effects on rational drug use, an overview of 13 reviews. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD004397.pub2] [DOI] [Google Scholar]
- Abrams KR, Gillies CL, Lambert PC. Meta‐analysis of heterogeneously reported trials assessing change from baseline. Statistics in Medicine 2005;24:3823‐44. [DOI] [PubMed] [Google Scholar]
- Akin J, Hutchinson P, Strumpf K. Decentralization and Government Provision of Public Goods: The Public Health Sector in Uganda. Carolina Population Center University of North Carolina at Chapel Hill, Working Paper 01‐352001.
- Anokbonggo WW, Ogwal‐Okeng JW, Obua C, Aupont O, Ross‐Degnan D. Impact of decentralization on health services in Uganda: a look at facility utilization, prescribing and availability of essential drugs. East African Medical Journal 2004;Suppl: S2‐7. [PubMed] [Google Scholar]
- Asfaw A, Frohberg K, James KS, Jütting J. Fiscal decentralization and health outcomes: empirical evidence from rural India. Journal of Developing Areas 2007;41:17‐35. [Google Scholar]
- Atkinson S, Haran D. Back to basics: does decentralization improve health system performance? Evidence from Ceara in north‐east Brazil. Bulletin of the World Health Organization 2004;82(11):822‐7. [PMC free article] [PubMed] [Google Scholar]
- Bossert T. Analyzing the decentralization of health systems in developing countries: decision space, innovation and performance. Social Science and Medicine 1998;47(10):1513‐27. [DOI] [PubMed] [Google Scholar]
- Bossert T, Larrañaga O, Giedion U, Arbelaez J, Bowser D. Decentralization and equity of resource allocation: evidence from Colombia and Chile. Bulletin of the World Health Organization 2003;81(2):95‐100. [PMC free article] [PubMed] [Google Scholar]
- Bossert T, Bowser D, Amenyah J. Is decentralization good for logistics systems? Evidence on essential medicine logistics from Ghana and Guatemala. Health Policy and Planning 2007;22:73‐82. [DOI] [PubMed] [Google Scholar]
- Bossert T, Mitchell A. Health sector decentralization and local decision‐making: decision space, institutional capacities and accountability in Pakistan. Social Science and Medicine 2011;72:39‐48. [DOI] [PubMed] [Google Scholar]
- Bossert TJ. Decentralization. In: Janovsky K editor(s). Health Policy and Systems Development. Geneva: World Health Organization, 1995. [Google Scholar]
- Bossert TJ, Beauvais JC. Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space. Health Policy and Planning 2002;1:14‐31. [DOI] [PubMed] [Google Scholar]
- Collins C, Green A. Decentralization and primary health care: some negative implications in developing countries. International Journal of Health Services 1994;24:459‐75. [DOI] [PubMed] [Google Scholar]
- Collins C. Decentralization. In: Janovsky K editor(s). Health policy and systems development, WHO document WHO/SHS/NHP/96.1. Geneva: World Health Organization, 1995:161‐78. [Google Scholar]
- Davoodi H, Zou H. Fiscal decentralization and economic growth: a cross‐country study. Journal of Urban Economics 1998 ;43:244‐57. [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effective Practice and Organisation of Care (EPOC) Group. EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services2013. [Available at: http://epocoslo.cochrane.org/epoc‐specific‐resources‐review‐authors]
- Gupta MD, Gauri V, Khemani S. Decentralized delivery of primary health services in Nigeria: survey evidence from the states of Lagos and Kogi. Africa Region Human Development Working Paper Series. Development Sector, Africa Region: World Bank, 2004. [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, Schünemann HJ. Rating quality of evidence and strength of recommendations: GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heywood P, Choi Y. Health system performance at the district level in Indonesia after decentralization. BMC International Health and Human Rights 2010;10(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated September 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org. Wiley Online Library.
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration, 2011. [Google Scholar]
- Jimenez D, Smith PC. Discussion Papers in Economics, Department of Economics and Related Studies. York: University of York, 2005. [Google Scholar]
- Jutting J, Corsi E, Kauffmann C, McDonnell I, Osterreider H, Pinaud N, et al. What makes decentralization in developing countries pro‐poor?. The European Journal of Development Research 2005;17(4):626‐48. [Google Scholar]
- Khaleghian P. Decentralization and public services: the case of immunization. Social Science & Medicine 2004;59(1):163‐83. [DOI] [PubMed] [Google Scholar]
- Lakshminarayanan R. Decentralisation and its implications for reproductive health: the Philippines experience. Reproductive Health Matters 2003;21:96‐107. [DOI] [PubMed] [Google Scholar]
- Lieberman SS. Decentralization and health in the Philippines and Indonesia. An Interim Report, East Asia Human Development2002.
- Litvack J, Seddon J. Decentralization Briefing Notes. Washington, DC: World Bank Institute, 1999. [Google Scholar]
- Litvak J, Ahmad J, Bird R. Rethinking decentralization in developing countries. Sector Studies Series. Washington, DC: The World Bank, 1998. [Google Scholar]
- Maganu ET. Decentralisation of health services in Botswana. Health System Decentralization: Concepts, Issues and Country Experience. Geneva: World Health Organization, 1990:45‐54. [Google Scholar]
- Mills A, Vaughan JP, Smith DL, Tabibzadeh I. Health System Decentralization: Concepts, Issues and Country Experience. Geneva: World Health Organization, 1990. [Google Scholar]
- Montoya‐Aguilar C, Vaughan P. Decentralisation and local management of health system in Chile. Health System Decentralization: Concepts, Issues and Country Experience. Geneva: World Health Organization, 1990. [Google Scholar]
- Pokharel B. Decentralization of Health Services. World Health Organization, Regional Office for South‐East Asia. New Delhi. SEA‐HSD‐2452000.
- Robalino DA, Picazo OF, Voetberg A. Does Fiscal Decentralization Improve Health Outcomes? Evidence from a Cross‐country Analysis. Policy Research Working Paper 2565. Washington DC: World Bank, 2001. [Google Scholar]
- Rubio DJ. The impact of decentralization of health services on health outcomes: evidence from Canada. Applied Economics 2011;43(26):3907‐17. [Google Scholar]
- Saltman R, Bankauskaite V, Vrangbaek K (editors). Decentralization in Health Care. McGraw‐Hill International, 2007. [Google Scholar]
- Sharp S. Meta‐analysis regression. Stata Technical Bulletin 1998;42:16‐22. [Google Scholar]
- Siddiqi S, Masud TI, Nishtar S, Peters DH, Sabri B, Bile KM, et al. Framework for assessing governance of the health system in developing countries: gateway to good governance. Health Policy 2009;9(1):13‐25. [DOI] [PubMed] [Google Scholar]
- Soto VE, Farfan MI, Lorant V. Fiscal decentralization and infant mortality rate: the Colombian case. Social Science and Medicine 2012;74(9):1426‐34. [DOI] [PubMed] [Google Scholar]
- Sterne JAC, Egger M, Smith GD. Investigating and dealing with publication and other biases. In: Egger M, Smith GD, Altman DG editor(s). Systematic Reviews in Health Care: Meta‐analysis in Context. London: BMJ Books, 2001:189‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanzi V. Fiscal federalism and decentralization: a review of some efficiency and macroeconomic aspects. Annual World Bank Conference on Development Economics. Washington, DC: World Bank, 1996. [Google Scholar]
- United Nations Development Program (UNDP). Governance for Sustainable Human Development: A UNDP Policy Document. New York: UNDP, 1997. [Google Scholar]
- World Health Organization. Decentralization and Health Systems Change: A Framework for Analysis. WHO document WHO/SHS/ NHP/95.2. Geneva: World Health Organization, 1995. [Google Scholar]
- World Health Organization. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes ‐ WHO’s Framework for Action. Geneva: WHO, 2007. [Google Scholar]


