Unknown until recently, the genus Emergomyces is composed of dimorphic fungi with human pathogenic potential. Five described species have been implicated as causes of disease in immunocompromised persons on at least 4 continents. In some regions, such as southern Africa, this disease, emergomycosis, is now the most commonly diagnosed dimorphic fungal infection. Herein, we review the history of these fungi, clinical features and pathogenesis of disease, what is known of their biology, and future research directions.
Origin story and current status
In 1994, an Italian woman with advanced HIV disease and widespread cutaneous lesions was diagnosed with an atypical disseminated mycosis. A biopsy of skin tissue demonstrated small budding yeasts, resembling those of Histoplasma capsulatum, in addition to larger pleomorphic cells. Moreover, the fungus that grew in culture had a dissimilar microscopic appearance [1, 2]. The conidia were arranged in complex “florets” on slightly swollen stalks reminiscent of Emmonsia crescens or Ea. parva, fungi for which the thermodependent phase is characterized by swollen, thick-walled, nonreplicating cells called adiaspores, usually observed in the lungs of small terrestrial mammals in a disease called adiaspiromycosis [3]. Genetic analysis suggested the clinical isolate was related to Ea. crescens, and the fungus was therefore described in 1998 as Ea. pasteuriana [2].
In 2013, following the introduction of molecular identification procedures in some South African laboratories, a dimorphic fungus most closely related to Ea. pasteuriana was found to be the cause of a disseminated mycosis in patients with advanced HIV disease [4]. Since then, infection with this fungus has been established to comprise the most frequently diagnosed dimorphic mycosis in South Africa [5–7]. In light of these reports, global collections were re-examined for dimorphic Emmonsia-like fungi. Archived isolates were examined phenotypically and with genetic analyses based on ribosomal DNA sequences, ultimately leading to a taxonomic revision within the family Ajellomycetaceae [8, 9]. In brief, Ea. parva, the type species of Emmonsia, was transferred to the genus Blastomyces (as B. parvus), and the genus Emmonsia was more narrowly defined to include Ea. crescens and Ea. soli, the latter currently known only from soil [8, 9]. A new genus, Emergomyces, was created to accommodate Emmonsia-like systemic dimorphic pathogens related to Es. pasteurianus (formerly Ea. pasteuriana) and characterized in the thermodependent phase by small yeast cells with narrow-based buds [8, 9].
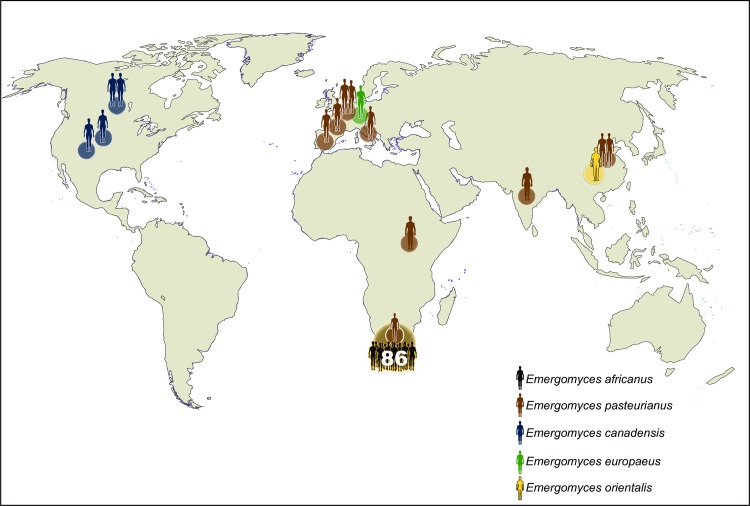
Five species are now described within Emergomyces [8, 9], and cases of disease have been reported globally (Fig 1). Es. pasteurianus, the type species, has been reported from Europe (including from Italy [1], Spain [10], France [ex-Georgia] [11], and the Netherlands [12]), Asia (China [13, 14] and India [ex-Nepal] [15]) and Africa (Uganda [ex-Rwanda] [16] and South Africa [9]). Es. africanus has been reported from South Africa and Lesotho [4, 9]. Es. canadensis has been reported from Canada (Saskatchewan) and the United States (Colorado and New Mexico) [17]. Es. orientalis has been reported from China [18], and Es. europaeus has been reported once from Germany [19].
Fig 1. Global geographic distribution of reported cases of emergomycosis [1, 4–7, 10–19, 28–30].
Each icon represents a single case except for Emergomyces africanus in South Africa, as indicated. Map created by Institute of Tropical Medicine, Antwerp.
The earliest known isolate among these Emergomyces species was from 1992 [17]. It remains unclear if these fungi have truly emerged or whether they are only now recognized because of an increase in the number of susceptible hosts, improved microbiology capacity, and/or the widespread adoption of molecular identification techniques in clinical and research laboratories.
Ecology
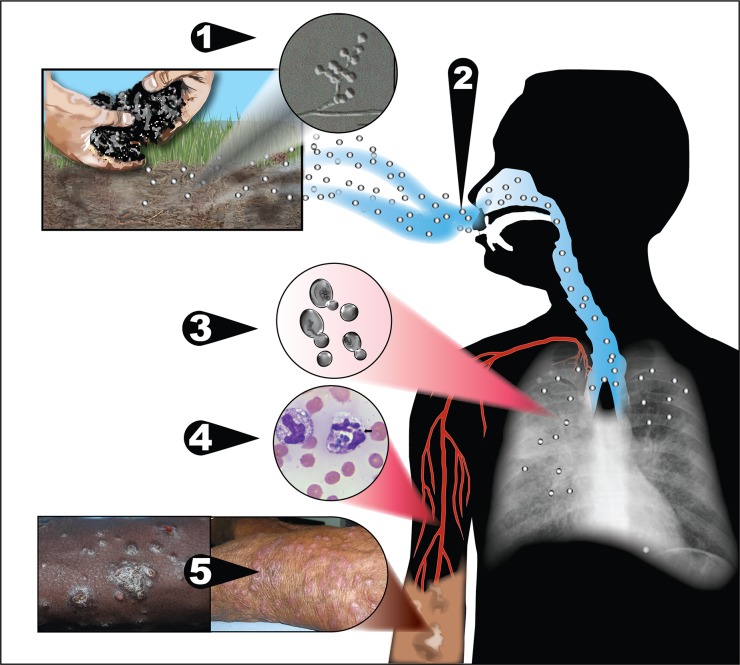
As with other systemic dimorphic fungi, infection is presumed to occur from inhalation of conidia, followed by a temperature-dependent transformation to a yeast-like phase that is capable of causing disease and of extrapulmonary dissemination (Fig 2).
Fig 2. Potential model for exposure and pathogenesis of Emergomyces.
1) Emergomyces species exist in soil in a mold phase, from where 2) conidia are released and aerosolized. 3) Upon inhalation by humans, the conidia undergo a temperature-dependent transformation in the lungs to yeast-like cells that replicate by budding and are capable of causing pulmonary disease in susceptible individuals. 4) Yeast-like cells disseminate hematogenously in macrophages throughout the body, causing extrapulmonary disease. 5) Cutaneous disease is most frequently reported, although virtually any body site can be affected.
Studies in search of an environmental reservoir for Emergomyces species have focused on Es. africanus in South Africa due to the large number of cases there [20–22]. Es. africanus DNA was detected in 30% of soil samples tested in the Western Cape Province, including from a wide range of soil habitats, such as soils associated with human activities like agriculture and horticulture and soils associated with plants endemic to the Cape Floral Kingdom. However, to date, the fungus has not been successfully isolated in culture from the environment, even with passage of soils through mice [20]. Es. africanus DNA was also detected in 10% of air samples collected in an urban location in the Cape Town metropole [21]. Naturally occurring infections of animals have not been demonstrated [22].
Emergomycosis
Disease caused by Emergomyces infection has been called emergomycosis (formerly disseminated emmonsiosis), and similarities have been noted among cases caused by different species. In general, patients with reported emergomycosis have been immunocompromised, including with HIV infection, solid organ transplantation, hematological malignancies, and immunosuppressant use [23]. Most patients with Es. africanus infection have had cutaneous lesions, which most commonly appear as papules, plaques, nodules, or ulcers, typically with widespread distributions [4, 6]. Pulmonary disease is also common: 86% of patients had abnormal chest X-rays in a series from South Africa [6]. Chest radiograph abnormalities have included diffuse reticulonodular disease, consolidation, effusions, and/or lymphadenopathy [6]. Other sites of disease that have been reported include the gastrointestinal tract, liver, lymph nodes, and bone marrow [6]. Limited pulmonary disease has rarely been described, observed in the sole reported case of disease caused by Es. europaeus [19]. For other species, all reported cases have involved disseminated disease. This may reflect a diagnostic bias in clinical practice due to late disease presentation and limited access to more invasive (e.g., bronchoscopic) pulmonary sampling in resource limited settings or reporting bias in the medical literature.
The diagnosis of emergomycosis can be made by biopsy of affected tissue for histopathology and fungal culture. Histopathology findings include small (2–5-μm) yeasts with narrow-based budding, best seen with fungal stains [4]. The findings are insufficiently distinct from H. capsulatum to allow definitive identification from histopathological appearance alone [5]. The diagnosis can be confirmed by culture of Emergomyces species from clinical samples. Where fungal cultures are negative (or omitted), PCR of fresh, affected tissue using amplification and sequencing of the internal transcribed spacer (ITS) can establish the correct diagnosis [6, 9].
Emergomyces species grow readily on standard fungal media (e.g., Sabouraud agar, malt extract agar, or potato dextrose agar), incubated at 24–30°C. Colonies are yellowish white to tan, initially glabrous, becoming powdery, slightly raised, and furrowed, and reach diameters of 2.5 to 3.5 cm in 3 weeks. Microscopically, Emergomyces spp. are characterized in the mold phase by slender conidiophores that arise from hyphae at right angles and form “florets” of short secondary conidiophores bearing single small subspherical conidia (see Fig 2, step 1 [inset]). Conversion from the mold to the yeast phase occurs readily when colonies are streaked onto potato dextrose agar or malt extract agar and incubated at 35°C [8, 9, 17].
Clinical microbiologists should be aware that Emergomyces species can cross react with a commercial DNA probe for B. dermatitidis [17]. There are neither sensitive nor specific serological tests nor biomarkers for the diagnosis of emergomycosis, though cross-reactivity can be observed with tests for related fungal infections [5, 6]. Emergomyces species may cross react with Histoplasma urinary antigen tests [5, 6], but a negative test cannot exclude the diagnosis: in a series of 10 patients with culture-proven emergomycosis, only 3 tested positive by Histoplasma urinary antigen test [5].
Current treatment recommendations for emergomycosis are based on observational studies and expert opinion and are the same as those for patients with histoplasmosis [6, 23]. Initially, immunocompromised patients with emergomycosis should be treated with amphotericin B for 10–14 days; where available, liposomal formulations are preferred over deoxycholate because of a more favorable toxicity profile. Thereafter, patients should be treated with itraconazole or another newer azole for 12 months pending immune reconstitution. Fluconazole should be avoided because high minimum inhibitory concentrations have been observed [7, 17, 24]. Among HIV-infected persons with emergomycosis who are antiretroviral therapy (ART)–naive (or on a failing ART regimen), the optimal timing of ART initiation (or modification) has not been established.
Pathogenesis
There remains much to learn about the virulence factors of these fungi and pathogenesis involved in infection. Known virulence factor genes of dimorphic fungi are conserved in Es. africanus and Es. pasteurianus [25]. The role of these in Emergomyces pathogenesis still needs to be evaluated. Strains of Es. africanus, Es. europaeus, and Es. pasteurianus (but not Es. canadensis or Es. orientalis) express urease [8, 26], a known virulence factor for some pathogenic fungi like Cryptococcus neoformans and C. gattii. Experimental infections have demonstrated susceptibility of golden hamsters and mice [20, 27]. Schwartz and colleagues found that intraperitoneal inoculations with Es. africanus were fatal to wild-type mice at doses of 106 conidia, whereas lower doses did not cause disease (although the organism could still be cultured from their livers and spleens with inoculae as low as 102 conidia) [20]. Moreover, C57BL/6 mice were more susceptible to disease than BALB/c mice [20]. Further work is underway to understand the pathogenesis of disease and the immunology of infection.
Future directions
There are many unresolved questions about Emergomyces. The true geographic range of Emergomyces species remains speculative, given the sporadic reports of disease from areas with limited mycological diagnostic capacity. For example, a case of emergomycosis caused by Es. pasteurianus in Uganda was diagnosed after a visiting doctor returned to Germany with a skin biopsy specimen that was collected from a Ugandan patient with a disseminated mycosis [16]. There, the diagnosis was made by nucleic acid amplification and sequencing, technology lacking in most African settings. It is presumed that this case and those diagnosed in South Africa represent the “ears of the hippo” on the African continent and that many other cases there and possibly on other continents go unrecognized. The development of an affordable, accessible, and feasible diagnostic test for emergomycosis should be prioritized to enable the diagnosis in places where the disease is widespread and to detect the presence of it elsewhere for epidemiological surveillance.
Funding Statement
This research was funded by the Fonds Wetenschappelijk Onderzoek – Vlaanderen (G.0514.14N). ISS received salary support from the Association of Medical Microbiology and Infectious Disease Canada–Astellas post-residency fellowship (2014), a Marie Curie Actions International Research Staff Exchange Scheme (2015), the R. Samuel McLaughlin – Manitoba Medical Services Foundation and University of Manitoba Dean's Fellowship Fund (2015/2016), a Detweiler Travelling Fellowship from the Royal College of Physicians and Surgeons of Canada (2017-2018), and the University of Alberta Faculty of Medicine and Dentistry, Department of Medicine. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gori S, Drouhet E, Gueho E, Huerre M, Lofaro A, Parenti M, et al. Cutaneous disseminated mycosis in a patient with AIDS due to a new dimorphic fungus. J Mycol Med. 1998;8(2):57–63. [Google Scholar]
- 2.Drouhet E, Gueho E, Gori S, Huerre M, Provost F, Borgers M, et al. Mycological, ultrastructural and experimental aspects of a new dimorphic fungus, Emmonsia pasteuriana sp. nov. isolated from a cutaneous disseminated mycosis in AIDS. J Mycol Med. 1998;8(2):64–77. [Google Scholar]
- 3.Sigler L. Adiaspiromycosis and other infections caused by Emmonsia species In: Hay RJ, Merz WG, editors. Topley and Wilson's Microbiology and Microbial Infections. 10th ed London, U.K: Arnold Hodder; 2005. p. 809–24. [Google Scholar]
- 4.Kenyon C, Bonorchis K, Corcoran C, Meintjes G, Locketz M, Lehloenya R, et al. A dimorphic fungus causing disseminated infection in South Africa. N Engl J Med. 2013;369(15):1416–24. 10.1056/NEJMoa1215460 [DOI] [PubMed] [Google Scholar]
- 5.Schwartz IS, Kenyon C, Lehloenya R, Claasens S, Spengane Z, Prozesky H, et al. AIDS-related endemic mycoses in Western Cape, South Africa, and clinical mimics: a cross-sectional study of adults with advanced HIV and recent-onset, widespread skin lesions. Open Forum Infect Dis. 2017;4(4):ofx186. 10.1093/ofid/ofx186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz IS, Govender NP, Corcoran C, Dlamini S, Prozesky H, Burton R, et al. Clinical characteristics, diagnosis, management and outcomes of disseminated emmonsiosis: a retrospective case series. Clin Infect Dis. 2015;61(6):1004–12. 10.1093/cid/civ439 [DOI] [PubMed] [Google Scholar]
- 7.Maphanga TG, Britz E, Zulu TG, Mpembe RS, Naicker SD, Schwartz IS, et al. In vitro antifungal susceptibility of yeast and mold phases of isolates of dimorphic fungal pathogen Emergomyces africanus (formerly Emmonsia sp.) from HIV-infected South African patients. J Clin Microbiol. 2017;55(6). 10.1128/JCM.02524-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang Y, Dukik K, Munoz J, Sigler L, Schwartz IS, Govender NP, et al. Phylogeny, ecology and taxonomy of systemic pathogens and their relatives in Ajellomycetaceae (Onygenales): Blastomyces, Emergomyces, Emmonsia, Emmonsiellopsis. Fungal Divers. 2018;90(1):245–91. 10.1007/s13225-018-0403-y. [DOI] [Google Scholar]
- 9.Dukik K, Muñoz JF, Jiang Y, Feng P, Sigler L, Stielow JB, et al. Novel taxa of thermally dimorphic systemic pathogens in the Ajellomycetaceae (Onygenales). Mycoses. 2017;60(5):296–309. 10.1111/myc.12601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pelegrín I, Alastruey-Izquierdo A, Ayats J, Cuenca-Estrella M, Cabellos C. A second look at Emmonsia infection can make the difference. Transpl Infect Dis. 2014;16(3):519–20. 10.1111/tid.12214 [DOI] [PubMed] [Google Scholar]
- 11.Lavergne R-A, Kandel-Aznar C, Khatchatourian L, Garcia-Hermoso D, Jeddi F, Boutoille D, et al. Emmonsia pasteuriana: une cause rare d'infection fongique chez l'immunodéprimé. J Mycol Med. 2017;27(3):e7–e8. 10.1016/j.mycmed.2017.04.025 [DOI] [Google Scholar]
- 12.Gast KB, van der Hoeven A, de Boer MGJ, van Esser JWJ, Kuijper EJ, Verweij JJ, et al. Two cases of Emergomyces pasteurianus infection in immunocompromised patients in the Netherlands. Med Mycol Case Rep. 2019. 10.1016/j.mmcr.2019.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feng P, Yin S, Zhu G, Li M, Wu B, Xie Y, et al. Disseminated infection caused by Emmonsia pasteuriana in a renal transplant recipient. J Dermatol. 2015;42(12):1179–82. 10.1111/1346-8138.12975 [DOI] [PubMed] [Google Scholar]
- 14.Tang XH, Zhou H, Zhang XQ, Han JD, Gao Q. Cutaneous disseminated emmonsiosis due to Emmonsia pasteuriana in a patient with cytomegalovirus enteritis. JAMA Dermatol. 2015;151(11):1263–4. 10.1001/jamadermatol.2015.1792 [DOI] [PubMed] [Google Scholar]
- 15.Malik R, Capoor MR, Vanidassane I, Gogna A, Singh A, Sen B, et al. Disseminated Emmonsia pasteuriana infection in India: a case report and a review. Mycoses. 2016;59(2):127–32. 10.1111/myc.12437 [DOI] [PubMed] [Google Scholar]
- 16.Wilmes D, Rooms I, Heidemarie L, McCormick Smith I, Haase G, Rickerts V. Emergomycosis: Case report of a disseminated Emergomyces pasteurianus infection and review of an emerging fungal infection. 52nd Scientific Conference of the German speaking Mycological Society (DMykG) together with the Austrian Society for Medical Mycology (ÖGMM), 6 September– 8 September 2018; 6–8 September, 2018; Innsbruck, Austria: Mycoses; 2018.
- 17.Schwartz IS, Sanche S, Wiederhold NP, Patterson TF, Sigler L. Emergomyces canadensis, a dimorphic fungus causing fatal systemic human disease in North America. Emerg Infect Dis. 2018;24(4). 10.3201/eid2404.171765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang P, Kenyon C, de Hoog S, Guo L, Fan H, Liu H, et al. A novel dimorphic pathogen, Emergomyces orientalis (Onygenales), agent of disseminated infection. Mycoses. 2017;60(5):310–9. 10.1111/myc.12583 [DOI] [PubMed] [Google Scholar]
- 19.Wellinghausen N, Kern WV, Haase G, Rozdzinski E, Kern P, Marre R, et al. Chronic granulomatous lung infection caused by the dimorphic fungus Emmonsia sp. Int J Med Microbiol. 2003;293(6):441–5. 10.1078/1438-4221-00281 [DOI] [PubMed] [Google Scholar]
- 20.Schwartz IS, Lerm B, Hoving JC, Kenyon C, Horsnell WG, Basson WJ, et al. Emergomyces africanus in soil, South Africa. Emerg Infect Dis. 2018;24(2). 10.3201/eid2402.171351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz IS, McLoud JD, Berman D, Botha A, Lerm B, Colebunders R, et al. Molecular detection of airborne Emergomyces africanus, a thermally dimorphic fungal pathogen, in Cape Town, South Africa. PLoS Negl Trop Dis. 2018;12(1). 10.1371/journal.pntd.0006174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cronjé N, Schwartz IS, Retief L, Bastos ADS, Matthee S, Preiser W, et al. Attempted molecular detection of the thermally dimorphic human fungal pathogen Emergomyces africanus in terrestrial small mammals in South Africa. Med Mycol. 2018;56(4):510–3. 10.1093/mmy/myx065 [DOI] [PubMed] [Google Scholar]
- 23.Schwartz IS, Maphanga TG, Govender NP. Emergomyces: a new genus of dimorphic fungal pathogens causing disseminated disease among immunocompromised persons globally. Curr Fungal Infect Rep. 2018. 10.1007/s12281-018-0308-y [DOI] [Google Scholar]
- 24.Dukik K, Al-Hatmi AMS, Curfs-Breuker I, Faro D, De Hoog S, Meis JF. Antifungal susceptibility of emerging dimorphic pathogens in the family Ajellomycetaceae. Antimicrob Agents Chemother. 2018;62(1):e01886–17. 10.1128/AAC.01886-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munoz JF, McEwen JG, Clay OK, Cuomo CA. Genome analysis reveals evolutionary mechanisms of adaptation in systemic dimorphic fungi. Sci Rep. 2018;8(1):4473 Epub 2018/03/16. 10.1038/s41598-018-22816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lerm B, Kenyon C, Schwartz IS, Kroukamp H, de Witt R, Govender NP, et al. First report of urease activity in the novel systemic fungal pathogen Emergomyces africanus: A comparison with the neurotrope Cryptococcus neoformans. FEMS Yeast Research. 2017;17(7). 10.1093/femsyr/fox069 [DOI] [PubMed] [Google Scholar]
- 27.Drouhet E, Huerre M. Yeast tissue phase of Emmonsia pasteuriana inoculated in golden hamster by intratesticular way. Mycoses. 1999;42 Suppl 2:11–8. 10.1111/j.1439-0507.1999.tb00006.x [DOI] [PubMed] [Google Scholar]
- 28.Crombie K, Spengane Z, Locketz M, Dlamini S, Lehloenya R, Wasserman S, et al. Paradoxical worsening of Emergomyces africanus infection in an HIV-infected male on itraconazole and antiretroviral therapy. PLoS Negl Trop Dis. 2018;12(3):e0006173 10.1371/journal.pntd.0006173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lochan H, Naicker P, Maphanga T, Ryan A, Pillay K, Govender NP, et al. A case of emmonsiosis in an HIV-infected child. South Afr J HIV Med 2015;16(1). 10.4102/sajhivmed.v16i1.352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhagoobhai L, Seetharam S, Wadula J, editors. Dimorphic fungus (Emmonsia species) isolated from sterile sites between March 2014 to April 2015. 6th FIDSSA Congress 2015. Drakensberg, KwaZulu-Natal, South Africa: South Afr J of Infect Dis.