Artemisinin-based combination therapies (ACTs) are the standard of care to treat uncomplicated falciparum malaria. However, resistance to artemisinins, defined as delayed parasite clearance after therapy, has emerged in Southeast Asia, and the spread of resistance to sub-Saharan Africa could have devastating consequences.
KEYWORDS: K13, Plasmodium falciparum, Uganda, artemisinin resistance
ABSTRACT
Artemisinin-based combination therapies (ACTs) are the standard of care to treat uncomplicated falciparum malaria. However, resistance to artemisinins, defined as delayed parasite clearance after therapy, has emerged in Southeast Asia, and the spread of resistance to sub-Saharan Africa could have devastating consequences. Artemisinin resistance has been associated in Southeast Asia with multiple nonsynonymous single nucleotide polymorphisms (NS-SNPs) in the propeller domain of the gene encoding the Plasmodium falciparum K13 protein (K13PD). Some K13PD NS-SNPs have been seen in Africa, but the relevance of these mutations is unclear. To assess whether ACT use has selected for specific K13PD mutations, we compared the K13PD genetic diversity in clinical isolates collected before and after the implementation of ACT use from seven sites across Uganda. We detected K13PD NS-SNPs in 16 of 683 (2.3%) clinical isolates collected between 1999 and 2004 and in 26 of 716 (3.6%) isolates collected between 2012 and 2016 (P = 0.16), representing a total of 29 different polymorphisms at 27 codons. Individual NS-SNPs were usually detected only once, and none were found in more than 0.7% of the isolates. Three SNPs (C469F, P574L, and A675V) associated with delayed clearance in Southeast Asia were seen in samples collected between 2012 and 2016, each in a single isolate. No differences in diversity following implementation of ACT use were found at any of the seven sites, nor was there evidence of selective pressures acting on the locus. Our results suggest that selection by ACTs is not impacting on K13PD diversity in Uganda.
INTRODUCTION
The World Health Organization recommends artemisinin-based combination therapies (ACTs) to treat uncomplicated Plasmodium falciparum malaria (1). These drugs combine potent, short-acting artemisinins that rapidly reduce parasite biomass and alleviate malaria symptoms with longer-acting partner drugs that eliminate remaining parasites and reduce the risk of selection for artemisinin resistance (2). ACTs have been adopted by most countries where malaria is endemic and have contributed to substantial decreases in malaria-related morbidity and mortality in recent years (3). However, resistance to artemisinins, defined as delayed parasite clearance following treatment (1), has emerged in Southeast Asia (4, 5), and the potential spread of resistance to sub-Saharan Africa, where over 90% of global malaria cases occur (6), could have devastating consequences.
Artemisinin resistance has been associated with multiple nonsynonymous single nucleotide polymorphisms (NS-SNPs) in the propeller domain of the K13 protein (K13PD) in Southeast Asia (7–9). At least 20 NS-SNPs have been associated with slow clearance in the region (1, 10). Of these, nine (F446I, N458Y, M476I, Y493H, R539T, I543T, P553L, R561H, and C580Y) have been validated in field isolates or genetically edited parasites by correlation with reduced ex vivo drug sensitivity in ring-stage survival assays (1, 10). However, the relevance of K13PD mutations in sub-Saharan Africa is unclear. More than 200 NS-SNPs, including some that have been associated with resistance in Southeast Asia, have been reported at low prevalence in clinical isolates from Africa, yet the delayed clearance phenotype is uncommon in the region, and ACTs continue to be highly efficacious (11). In addition, the most prevalent K13PD NS-SNP in Africa, A578S, was not associated with delayed clearance when introduced into a sensitive parasite (12). Nevertheless, history with other antimalarials suggests the likelihood for artemisinin resistance to emerge in Africa or to spread to the continent after originating elsewhere (13–15).
In Uganda, the standard therapy for uncomplicated malaria changed from chloroquine to chloroquine plus sulfadoxine-pyrimethamine (SP) in 2000 and then to the ACT artemether-lumefantrine (AL) in 2006 (16). In recent studies, K13PD mutations (17–21), delayed clearance after ACT therapy (22–24), and persistent parasitemia following DHA exposure in ring survival assays (25, 26) have all been uncommon in Uganda. However, it is unclear whether changes in the prevalence of K13PD mutations occurred after the institution of treatment with ACTs. Such a change might serve as an early indication of the evolution of artemisinin resistance in Uganda. To gain insight in this area, we compared the genetic diversity of the K13PD locus in clinical isolates collected before and after the implementation of ACT use from seven sites across the country.
RESULTS
K13 propeller domain polymorphisms before and after the introduction of ACTs.
A total of 1,408 P. falciparum isolates, 683 collected before implementation of ACTs (from 1999 to 2006) and 716 collected after implementation (from 2012 to 2016) from seven sites across Uganda (Fig. 1), were evaluated for the presence of K13PD NS-SNPs. K13PD NS-SNPs were seen in 42 of 1,408 isolates (3.0%). Twenty-nine different polymorphisms resulting in amino acid changes at 27 codons were identified (see Table S1 in the supplemental material). Of the 29 polymorphisms, 25 (86%) were observed as singletons, and 25 (86%) have been previously reported. The most prevalent NS-SNP, A578S, was present in 10 samples (0.71%) and seen in 0.44% of pre-ACT isolates and in 1.1% of post-ACT isolates. V555A, the next most prevalent polymorphism (five samples, 0.36%), was found in 0.58% of pre-ACT isolates and in 0.14% of post-ACT isolates. G533A and I540T were each seen in two post-ACT isolates (0.14% all samples, 0.28% post-ACT); other identified NS-SNPs were each seen in only a single isolate. There were no significant differences in the prevalences of any individual NS-SNP before or after the introduction of ACTs (Table S1). Among the 42 isolates in which NS-SNPs were detected, two polyclonal isolates contained two NS-SNPs. No difference in the prevalence of NS-SNPs in pre-ACT and post-ACT isolates was seen (2.3% pre-ACT versus 3.6% post-ACT, P = 0.16 [Fisher exact test]) (Table 1). Three polymorphisms that have been associated with artemisinin resistance in clinical studies from Southeast Asia (C469F, P574L, and A675V) were observed, each in a single isolate collected after the introduction of ACTs.
FIG 1.
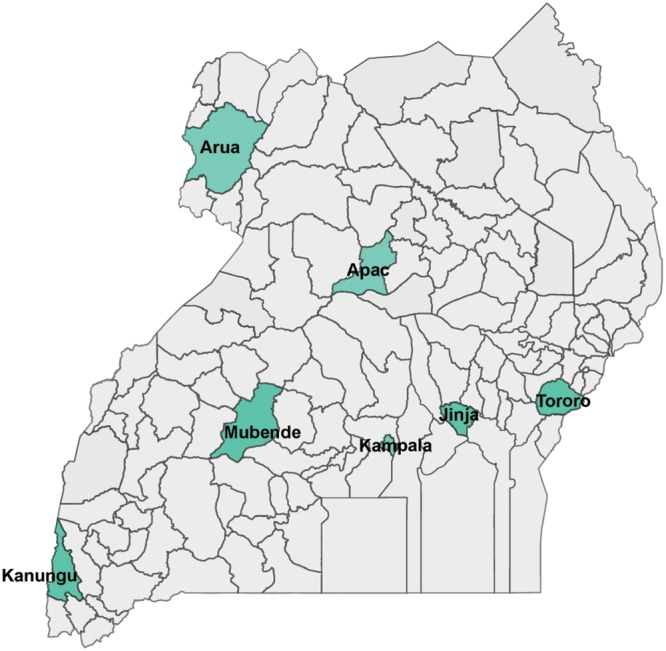
Map of Uganda. Sample districts are highlighted.
TABLE 1.
Prevalence of NS-SNPs in the K13 propeller domain before and after the introduction of ACTsa
| Site | Prevalence (%) |
P | Polymorphism(s) |
||
|---|---|---|---|---|---|
| Pre-ACTs (1999–2004) | Post-ACTs (2012–2016) | Pre-ACTs | Post-ACTs | ||
| Apac | 2/100 (2.0) | 0/19 (0.0) | 1.00 | K610E, P615N | |
| Arua | 4/86 (4.7) | 2/40 (5.0) | 1.00 | V555A, A578S, N594K, L618S | W470R, A675V, A578S |
| Jinja | 1/99 (1.0) | 3/99 (3.0) | 0.62 | V581I | K563E, A578S x2 |
| Kampala | 2/100 (2.0) | 2/65 (3.1) | 0.65 | V555A x2 | S522C, A578S |
| Kanungu | 0/100 (0.0) | 5/118 (4.2) | 0.06 | I540T x2, G533A x2, V555A | |
| Mubende | 5/99 (5.0) | 2/66 (3.0) | 0.70 | G496S, V555A, E567K, A578S x2 | C469Y, P574L |
| Tororo | 2/99 (2.0) | 12/303 (3.9) | 0.53 | L457I, W565R | I465T and L619S, C469F, M472V, Y558H, A569T, A569S, A578S x4, N594K, A617T |
| Total | 16/683 (2.3) | 26/716 (3.6) | 0.16 | ||
Isolates with mixed genotypes are considered mutant. Prevalences (i.e., the number of NS-SNPs/total SNPs) were compared using Fisher exact tests, and P values were considered significant if P < 0.05.
K13 propeller domain polymorphisms by site.
The proportion of isolates with an NS-SNP ranged from 0 to 5.0% at the seven study sites. There were no significant differences in the proportion of isolates with an NS-SNP or in the prevalence of any individual NS-SNP before and after ACT introduction at any site (Table 1 and see Table S1 in the supplemental material). Trends varied between sites, with four of seven showing an increase in the prevalence of NS-SNPs, two showing a decrease, and one remaining constant. Of the NS-SNPs seen in multiple isolates, G533A and I540T were only seen in Kanungu, while A578S and V555A were seen at multiple sites.
Nucleotide and haplotype diversity.
We used two population genetic indices for the assessment of nucleotide diversity: the average pairwise nucleotide difference (π) and the standardized number of segregating mutations per site (θS) (Table S2). In all studied sites, π was lower than θS, both before and after the introduction of ACTs, which reflects the observation that the polymorphisms were rare alleles. In all but two sites, Apac and Mubende, nucleotide diversity, the number of amino acid haplotypes, and the mean haplotype diversity increased following the introduction of ACTs (Table S2).
Population genetic analysis. (i) Frequency spectrum tests of neutrality.
Two statistics were used to test for neutrality in the evolution of the K13PD gene sequence, Tajima’s D (27) and Fu and Li’s D (28). We used the K13PD gene sequence from P. praefalciparum, a gorilla malaria parasite and the closest known relative to P. falciparum (29), as the outgroup for calculating Fu and Li’s D. Both statistics resulted in negative values for D in all populations, although only a subset were statistically significant (Table S3). These negative values indicate an excess of singletons, suggesting that the gene has undergone nonrandom processes, such as a population size expansion or purifying selection. However, since these negative values were reported in samples collected before and after the implementation of ACTs, there is no evidence that these nonrandom processes are related to ACT pressure.
(ii) Tests for adaptive evolution.
To determine whether selection may have a played a role in the observed nucleotide diversity of the K13PD, we performed a McDonald and Kreitman (MK) test using the P. praefalciparum K13PD sequence for interspecies comparison. Considering 227 codons, we found no fixed nonsynonymous differences between P. falciparum and P. praefalciparum, suggesting that K13PD is highly conserved across Plasmodium species and that all mutations are recently derived. In addition, we did not find significant differences between the diversity within the P. falciparum samples and the divergence between P. falciparum and P. praefalciparum at synonymous and nonsynonymous sites, with the exception of the pre-ACT samples collected from Arua (P = 0.029) and Mubende (P =0.048) (Table S4). In both cases, the direction of selection statistic was negative, implying an excess of nonsynonymous polymorphisms, suggesting that slightly deleterious alleles were segregating in these populations (30). However, since these populations were sampled before the implementation of ACTs, this selection was not driven by artemisinin selection.
In addition, we explored evidence of natural selection acting on K13PD by estimating the average pairwise number of synonymous substitutions per synonymous site (dS) and nonsynonymous substitutions per nonsynonymous site (dN). This analysis similarly demonstrated no deviation from ratios expected under neutrality, except in the pre-ACT samples from Arua (dN − dS = 2.152, P = 0.033) (Table S4).
DISCUSSION
We evaluated the diversity of NS-SNPs in the K13PD in 1,399 P. falciparum isolates collected from seven sites across Uganda before and after the introduction of ACTs as the national standard treatment for malaria. In total, we found 29 NS-SNPs, present in 3.0% of samples, most of which appeared in only a single isolate. There was no difference in prevalence of NS-SNPs for samples collected before or after the introduction of ACTs. Three of the detected NS-SNPs, each seen only once and each in an isolate collected after introduction of ACTs, have been associated with delayed parasite clearance in Southeast Asia. Nucleotide diversity was low at all sites but increased modestly after the introduction of ACTs in five locations.
In addition to evaluating the diversity of polymorphism in K13PD, we performed population genetic analyses to detect the effects of selection and demographic processes on the sequences. First, we performed two neutrality tests based on the frequency distribution of nucleotide polymorphisms, Tajima’s D and Fu and Li’s D statistics. For both tests, we calculated negative values, indicative of an excess of rare variants, suggesting that purifying selection, selective sweeps, or population growth are impacting on the evolution of the gene. Identifying hallmarks of nonneutral evolution, we then performed tests to detect the effects of natural selection, using the MK test and performing a pairwise comparison of synonymous and nonsynonymous sites. These codon-based tests are insensitive to demographic processes because under most conditions, other than natural selection, synonymous and nonsynonymous mutations will behave the same; under natural selection, impacts will be different for the two types of mutations. In our analyses we did not detect significant deviation from expected ratios of synonymous and nonsynonymous mutations in any population sampled after the introduction of ACTs, indicating that the negative values from our D statistics are likely driven by demographic processes rather than adaptive evolution. Thus, we have detected no evidence that the use of ACTs has selected for K13PD mutations in Uganda.
The K13PD locus demonstrates remarkable conservation across the Plasmodium genus, with almost identical protein sequences among the closely related species in the subgenus Laverania, suggesting the gene evolved under strong purifying selection (31). However, a substantial number of K13PD polymorphisms were seen at low prevalence in our population and others from sub-Saharan Africa (11). This apparent contradiction is consistent with the expected consequences of the P. falciparum population expansion that has been hypothesized to have accompanied the expansion of humans out of Africa (31–33). Indeed, a large number of rare variants seems to be characteristic of the genomes of African, but not Asian, P. falciparum (34).
Additional studies comparing the genetic diversity in K13PD before and after the introduction of ACTs in Africa have generally been consistent with our findings from Uganda, with no significant difference in the proportion of parasites with a NS-SNP before and after the introduction of ACTs (35–38). However, a report from Kenya described a significant decrease, and one from Comoros described an increase in K13PD polymorphisms following the introduction ACTs (39, 40). The nucleotide diversity we report for the K13PD is in scale with that reported from other regions of Africa, as is the presence of an excess of rare alleles (41).
The bulk of available clinical, parasitological, molecular, and population genetic data suggest that artemisinin resistance is not yet a problem in Africa. However, the pressure of millions of doses of ACTs offers continued risk of resistance selection. Polymorphisms associated with resistance in Southeast Asia (1, 10) have already been reported at low frequencies in African P. falciparum populations (12, 18, 21, 34, 38, 42–48). It is likely only a matter of time before a favorable combination of variants allows resistant parasites to gain a foothold in Africa, and continued surveillance and work to improve tools to detect early indicators of resistance will be essential.
MATERIALS AND METHODS
Samples.
Samples were collected in clinical studies conducted at multiple sites across Uganda from 1999 to 2016 (17, 18, 22, 25, 26, 49–52). For this study, pre-ACT samples were randomly selected from available DNA samples with the goal of obtaining 100 K13PD sequences from each site, with the exception of Arua, where only 92 samples were available. We successfully obtained sequences from Apac (100 of 112 samples), Arua (86 of 92), Jinja (99 of 104), Kampala (100 of 101), Kanungu (100 of 106), Mubende (99 of 112), and Tororo (99 of 109) (total n = 683).(49, 50) Post-ACT samples (n = 716) were from previously published studies evaluating markers of antimalarial resistance conducted at the same sites (17, 18, 22, 25, 26, 51, 52). Accession numbers for previously published and newly generated sequences and information about the origin of samples can be found in Table S5 in the supplemental material.
K13 propeller domain genotyping.
DNA was extracted from stored filter paper samples as previously described (53). The K13PD (codons 440 to 726) was amplified as previously described (7). After confirmation of amplification by electrophoresis, amplicons were purified using Agencourt AMPureXP and dideoxy sequenced. Consensus sequences were aligned to the 3d7 reference and evaluated using CodonCode Aligner. Mixed alleles were considered mutant. Statistical analyses comparing prevalences were performed using StataSE 15.1.
Molecular evolutionary analysis.
The sequences used for these analyses had no gaps and were clipped to have a uniform length. Various approaches were used to assess whether the sequenced region of K13PD evolved neutrally after the introduction of ACTs in Uganda. Fisher exact tests were used to compare mutation prevalences between pre- and post-ACT populations and collection sites. Two standard measures of nucleotide diversity, the average number of pairwise nucleotide differences per site (π) (54) and the standardized number of segregating mutations per site (θs; Watterson’s estimator) (55), were calculated by DnaSP version 5.10 (56). To detect departures from neutrality, DnaSP was used to calculate Tajima’s D (27) and Fu and Li’s D (28). Two methods were used to detect evidence of adaptive selection, the McDonald-Kreitman (MK) test and a codon-based test of neutrality. The MK test was executed in DnaSNP, and a direction of selection statistic, defined as:
where DoS is direction of selection statistic, Da is the number of nonsynonymous interspecies fixed differences, Ds is the number of synonymous interspecies fixed differences, Pa is the number of nonsynonymous intraspecific differences, and Ps is the number of synonymous intraspecific differences (57), was calculated to correct for biases introduced by the small amount of divergence in our samples (30). The codon-based test of neutrality, in which the numbers of pairwise nonsynonymous (dN) and synonymous (dS) differences per site were estimated by the Nei and Gojobori (58) method with the Jukes and Cantor correction, was implemented in MEGA version 7 (59). The variance of the difference was computed using the bootstrap method (500 replicates). The probability of rejecting the null hypothesis of strict neutrality (dN = dS) is reported. The genomic sequence of the P. praefalciparum homolog of the Pfkelch13 gene (PPRFG01_1345600) was downloaded from PlasmdDB (60) and used as the outgroup to calculate the Fu and Li’s D value and for the MK test. For all tests, values of P < 0.05 are considered significant.
Data availability.
Accession numbers are reported in Table S5 in the supplemental material.
Supplementary Material
ACKNOWLEDGMENTS
We thank the clinical staff, physicians, laboratory technicians, study coordinators, and researchers who conducted the studies during which the samples utilized in this study were collected. In addition, we thank the authors of the published sequence data that were used in this analysis. In particular, we thank the study participants and their families for supporting our research.
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/AAC.01234-19.
REFERENCES
- 1.World Health Organization. 2018. Status report on artemisinin resistance and ACT efficacy (August 2018). World Health Organization, Geneva, Switzerland: https://www.who.int/malaria/publications/atoz/artemisinin-resistance-august2018/en/. [Google Scholar]
- 2.Nosten F, White NJ. 2007. Artemisinin-based combination treatment of falciparum malaria. Am J Trop Med Hyg 77:181–192. doi: 10.4269/ajtmh.2007.77.181. [DOI] [PubMed] [Google Scholar]
- 3.O’Meara WP, Mangeni JN, Steketee R, Greenwood B. 2010. Changes in the burden of malaria in sub-Saharan Africa. Lancet Infect Dis 10:545–555. doi: 10.1016/S1473-3099(10)70096-7. [DOI] [PubMed] [Google Scholar]
- 4.Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, Sreng S, Anderson JM, Mao S, Sam B, Sopha C, Chuor CM, Nguon C, Sovannaroth S, Pukrittayakamee S, Jittamala P, Chotivanich K, Chutasmit K, Suchatsoonthorn C, Runcharoen R, Hien TT, Thuy-Nhien NT, Thanh NV, et al. 2014. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med 371:411–423. doi: 10.1056/NEJMoa1314981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fairhurst RM, Dondorp AM. 2016. Artemisinin-resistant Plasmodium falciparum malaria. Microbiol Spectr 4. doi: 10.1128/microbiolspec.EI10-0013-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. 2018. World malaria report 2018. World Health Organization, Geneva, Switzerland: https://www.who.int/malaria/publications/world-malaria-report-2018/en/. [Google Scholar]
- 7.Ariey F, Witkowski B, Amaratunga C, Beghain J, Langlois A-C, Khim N, Kim S, Duru V, Bouchier C, Ma L, Lim P, Leang R, Duong S, Sreng S, Suon S, Chuor CM, Bout DM, Ménard S, Rogers WO, Genton B, Fandeur T, Miotto O, Ringwald P, Le Bras J, Berry A, Barale J-C, Fairhurst RM, Benoit-Vical F, Mercereau-Puijalon O, Ménard D. 2014. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature 505:50–55. doi: 10.1038/nature12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Straimer J, Gnädig NF, Witkowski B, Amaratunga C, Duru V, Ramadani AP, Dacheux M, Khim N, Zhang L, Lam S, Gregory PD, Urnov FD, Mercereau-Puijalon O, Benoit-Vical F, Fairhurst RM, Ménard D, Fidock DA. 2015. Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science 347:428–431. doi: 10.1126/science.1260867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takala-Harrison S, Clark TG, Jacob CG, Cummings MP, Miotto O, Dondorp AM, Fukuda MM, Nosten F, Noedl H, Imwong M, Bethell D, Se Y, Lon C, Tyner SD, Saunders DL, Socheat D, Ariey F, Phyo AP, Starzengruber P, Fuehrer HP, Swoboda P, Stepniewska K, Flegg J, Arze C, Cerqueira GC, Silva JC, Ricklefs SM, Porcella SF, Stephens RM, Adams M, Kenefic LJ, Campino S, Auburn S, MacInnis B, Kwiatkowski DP, Su XZ, White NJ, Ringwald P, Plowe CV. 2013. Genetic loci associated with delayed clearance of Plasmodium falciparum following artemisinin treatment in Southeast Asia. Proc Natl Acad Sci U S A 110:240–245. doi: 10.1073/pnas.1211205110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WWARN K13 Genotype-Phenotype Study Group. 2019. Association of mutations in the Plasmodium falciparum Kelch13 gene (Pf3D7_1343700) with parasite clearance rates after artemisinin-based treatments-a WWARN individual patient data meta-analysis. BMC Med 17:1. doi: 10.1186/s12916-018-1207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conrad MD, Rosenthal PJ. 2019. Antimalarial drug resistance in Africa: the calm before the storm? Lancet Infect Dis. doi: 10.1016/S1473-3099(19)30261-0. [DOI] [PubMed] [Google Scholar]
- 12.Ménard D, Khim N, Beghain J, Adegnika AA, Shafiul-Alam M, Amodu O, Rahim-Awab G, Barnadas C, Berry A, Boum Y, Bustos MD, Cao J, Chen J-H, Collet L, Cui L, Thakur G-D, Dieye A, Djallé D, Dorkenoo MA, Eboumbou-Moukoko CE, Espino F-E-CJ, Fandeur T, Ferreira-da-Cruz M-F, et al. 2016. A worldwide map of Plasmodium falciparum K13-propeller polymorphisms. N Engl J Med 374:2453–2464. doi: 10.1056/NEJMoa1513137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roper C, Pearce R, Bredenkamp B, Gumede J, Drakeley C, Mosha F, Chandramohan D, Sharp B. 2003. Antifolate antimalarial resistance in southeast Africa: a population-based analysis. Lancet 361:1174–1181. doi: 10.1016/S0140-6736(03)12951-0. [DOI] [PubMed] [Google Scholar]
- 14.Mita T, Venkatesan M, Ohashi J, Culleton R, Takahashi N, Tsukahara T, Ndounga M, Dysoley L, Endo H, Hombhanje F, Ferreira MU, Plowe CV, Tanabe K. 2011. Limited geographical origin and global spread of sulfadoxine-resistant dhps alleles in Plasmodium falciparum populations. J Infect Dis 204:1980–1988. doi: 10.1093/infdis/jir664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wootton JC, Feng X, Ferdig MT, Cooper RA, Mu J, Baruch DI, Magill AJ, Su XZ. 2002. Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature 418:320–323. doi: 10.1038/nature00813. [DOI] [PubMed] [Google Scholar]
- 16.Nanyunja M, Nabyonga Orem J, Kato F, Kaggwa M, Katureebe C, Saweka J. 2011. Malaria treatment policy change and implementation: the case of Uganda. Malar Res Treat 2011:683167. doi: 10.4061/2011/683167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conrad MD, Bigira V, Kapisi J, Muhindo M, Kamya MR, Havlir DV, Dorsey G, Rosenthal PJ. 2014. Polymorphisms in K13 and falcipain-2 associated with artemisinin resistance are not prevalent in Plasmodium falciparum isolated from Ugandan children. PLoS One 9:e105690. doi: 10.1371/journal.pone.0105690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asua V, Vinden J, Conrad MD, Legac J, Kigozi SP, Kamya MR, Dorsey G, Nsobya SL, Rosenthal PJ. 2019. Changing molecular markers of antimalarial drug sensitivity across Uganda. Antimicrob Agents Chemother 63:e01818-18. doi: 10.1128/AAC.01818-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tumwebaze P, Conrad MD, Walakira A, LeClair N, Byaruhanga O, Nakazibwe C, Kozak B, Bloome J, Okiring J, Kakuru A, Bigira V, Kapisi J, Legac J, Gut J, Cooper RA, Kamya MR, Havlir DV, Dorsey G, Greenhouse B, Nsobya SL, Rosenthal PJ. 2015. Impact of antimalarial treatment and chemoprevention on the drug sensitivity of malaria parasites isolated from Ugandan children. Antimicrob Agents Chemother 59:3018–3030. doi: 10.1128/AAC.05141-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawkes M, Conroy AL, Opoka RO, Namasopo S, Zhong K, Liles WC, John CC, Kain KC. 2015. Slow clearance of Plasmodium falciparum in severe pediatric malaria, Uganda, 2011-2013. Emerg Infect Dis 21:1237–1239. doi: 10.3201/eid2107.150213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor SM, Parobek CM, DeConti DK, Kayentao K, Coulibaly SO, Greenwood BM, Tagbor H, Williams J, Bojang K, Njie F, Desai M, Kariuki S, Gutman J, Mathanga DP, Martensson A, Ngasala B, Conrad MD, Rosenthal PJ, Tshefu AK, Moormann AM, Vulule JM, Doumbo OK, Ter Kuile FO, Meshnick SR, Bailey JA, Juliano JJ. 2015. Absence of putative artemisinin resistance mutations among Plasmodium falciparum in Sub-Saharan Africa: a molecular epidemiologic study. J Infect Dis 211:680–688. doi: 10.1093/infdis/jiu467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yeka A, Kigozi R, Conrad MD, Lugemwa M, Okui P, Katureebe C, Belay K, Kapella BK, Chang MA, Kamya MR, Staedke SG, Dorsey G, Rosenthal PJ. 2016. Artesunate/amodiaquine versus artemether/lumefantrine for the treatment of uncomplicated malaria in Uganda: a randomized trial. J Infect Dis 213:1134–1142. doi: 10.1093/infdis/jiv551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yeka A, Wallender E, Mulebeke R, Kibuuka A, Kigozi R, Bosco A, Kyambadde P, Opigo J, Kalyesubula S, Senzoga J, Vinden J, Conrad M, Rosenthal PJ. 2019. Comparative efficacy of artemether-lumefantrine and dihydroartemisinin-piperaquine for the treatment of uncomplicated malaria in Ugandan children. J Infect Dis 219:1112–1120. doi: 10.1093/infdis/jiy637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muhindo MK, Kakuru A, Jagannathan P, Talisuna A, Osilo E, Orukan F, Arinaitwe E, Tappero JW, Kaharuza F, Kamya MR, Dorsey G. 2014. Early parasite clearance following artemisinin-based combination therapy among Ugandan children with uncomplicated Plasmodium falciparum malaria. Malar J 13:32. doi: 10.1186/1475-2875-13-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper RA, Conrad MD, Watson QD, Huezo SJ, Ninsiima H, Tumwebaze P, Nsobya SL, Rosenthal PJ. 2015. Lack of artemisinin resistance in Plasmodium falciparum in Uganda based on parasitological and molecular assays. Antimicrob Agents Chemother 59:5061–5064. doi: 10.1128/AAC.00921-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rasmussen SA, Ceja FG, Conrad MD, Tumwebaze PK, Byaruhanga O, Katairo T, Nsobya SL, Rosenthal PJ, Cooper RA. 2017. Changing antimalarial drug sensitivities in Uganda. Antimicrob Agents Chemother 61:e01516-17. doi: 10.1128/AAC.01516-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tajima F. 1989. Statistical method for testing the neutral mutation hypothesis by DNA polymorphism. Genetics 123:585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu YX, Li WH. 1993. Statistical tests of neutrality of mutations. Genetics 133:693–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Otto TD, Gilabert A, Crellen T, Bohme U, Arnathau C, Sanders M, Oyola SO, Okouga AP, Boundenga L, Willaume E, Ngoubangoye B, Moukodoum ND, Paupy C, Durand P, Rougeron V, Ollomo B, Renaud F, Newbold C, Berriman M, Prugnolle F. 2018. Genomes of all known members of a Plasmodium subgenus reveal paths to virulent human malaria. Nat Microbiol 3:687–697. doi: 10.1038/s41564-018-0162-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walsh B, Lynch M, Lynch M. 2018. Using molecular data to detect selection: signatures from multiple historical events, p xxix and 1459. In Evolution and selection of quantitative traits. Oxford University Press, New York, NY. [Google Scholar]
- 31.Pacheco MA, Kadakia ER, Chaudhary Z, Perkins DJ, Kelley J, Ravishankar S, Cranfield M, Talundzic E, Udhayakumar V, Escalante AA. 2019. Evolution and genetic diversity of the k13 gene associated with artemisinin delayed parasite clearance in Plasmodium falciparum. Antimicrob Agents Chemother 63:e02550-18. doi: 10.1128/AAC.02550-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joy DA, Feng X, Mu J, Furuya T, Chotivanich K, Krettli AU, Ho M, Wang A, White NJ, Suh E, Beerli P, Su XZ. 2003. Early origin and recent expansion of Plasmodium falciparum. Science 300:318–321. doi: 10.1126/science.1081449. [DOI] [PubMed] [Google Scholar]
- 33.Tanabe K, Mita T, Jombart T, Eriksson A, Horibe S, Palacpac N, Ranford-Cartwright L, Sawai H, Sakihama N, Ohmae H, Nakamura M, Ferreira MU, Escalante AA, Prugnolle F, Bjorkman A, Farnert A, Kaneko A, Horii T, Manica A, Kishino H, Balloux F. 2010. Plasmodium falciparum accompanied the human expansion out of Africa. Curr Biol 20:1283–1289. doi: 10.1016/j.cub.2010.05.053. [DOI] [PubMed] [Google Scholar]
- 34.MalariaGEN Plasmodium falciparum Community Project. 2016. Genomic epidemiology of artemisinin resistant malaria. Elife 5:e08747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Djaman JA, Olefongo D, Ako AB, Roman J, Ngane VF, Basco LK, Tahar R. 2017. Molecular epidemiology of malaria in Cameroon and Cote d’Ivoire. XXXI. Kelch 13 propeller sequences in Plasmodium falciparum isolates before and after implementation of artemisinin-based combination therapy. Am J Trop Med Hyg 97:222–224. doi: 10.4269/ajtmh.16-0889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Escobar C, Pateira S, Lobo E, Lobo L, Teodosio R, Dias F, Fernandes N, Arez AP, Varandas L, Nogueira F. 2015. Polymorphisms in Plasmodium falciparum K13-propeller in Angola and Mozambique after the introduction of the ACTs. PLoS One 10:e0119215. doi: 10.1371/journal.pone.0119215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guerra M, Neres R, Salgueiro P, Mendes C, Ndong-Mabale N, Berzosa P, de Sousa B, Arez AP. 2016. Plasmodium falciparum genetic diversity in continental equatorial Guinea before and after introduction of artemisinin-based combination therapy. Antimicrob Agents Chemother 61:e02556-15. doi: 10.1128/AAC.02556-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ouattara A, Kone A, Adams M, Fofana B, Maiga AW, Hampton S, Coulibaly D, Thera MA, Diallo N, Dara A, Sagara I, Gil JP, Bjorkman A, Takala-Harrison S, Doumbo OK, Plowe CV, Djimde AA. 2015. Polymorphisms in the K13-propeller gene in artemisinin-susceptible Plasmodium falciparum parasites from Bougoula-Hameau and Bandiagara, Mali. Am J Trop Med Hyg 92:1202–1206. doi: 10.4269/ajtmh.14-0605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Laurent ZR, Chebon LJ, Ingasia LA, Akala HM, Andagalu B, Ochola-Oyier LI, Kamau E. 2018. Polymorphisms in the K13 gene in Plasmodium falciparum from different malaria transmission areas of Kenya. Am J Trop Med Hyg 98:1360–1366. doi: 10.4269/ajtmh.17-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang B, Deng C, Yang T, Xue L, Wang Q, Huang S, Su XZ, Liu Y, Zheng S, Guan Y, Xu Q, Zhou J, Yuan J, Bacar A, Abdallah KS, Attoumane R, Mliva AM, Zhong Y, Lu F, Song J. 2015. Polymorphisms of the artemisinin resistant marker (K13) in Plasmodium falciparum parasite populations of Grande Comore Island 10 years after artemisinin combination therapy. Parasit Vectors 8:634. doi: 10.1186/s13071-015-1253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mita T, Culleton R, Takahashi N, Nakamura M, Tsukahara T, Hunja CW, Win ZZ, Htike WW, Marma AS, Dysoley L, Ndounga M, Dzodzomenyo M, Akhwale WS, Kobayashi J, Uemura H, Kaneko A, Hombhanje F, Ferreira MU, Bjorkman A, Endo H, Ohashi J. 2016. Little polymorphism at the K13 propeller locus in worldwide Plasmodium falciparum populations prior to the introduction of artemisinin combination therapies. Antimicrob Agents Chemother 60:3340–3347. doi: 10.1128/AAC.02370-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang C, Zhang H, Zhou R, Qian D, Liu Y, Zhao Y, Li S, Xu B. 2017. Polymorphisms of Plasmodium falciparum K13-propeller gene among migrant workers returning to Henan Province, China from Africa. BMC Infect Dis 17:560. doi: 10.1186/s12879-017-2634-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kakolwa MA, Mahende MK, Ishengoma DS, Mandara CI, Ngasala B, Kamugisha E, Kataraihya JB, Mandike R, Mkude S, Chacky F, Njau R, Premji Z, Lemnge MM, Warsame M, Menard D, Kabanywanyi AM. 2018. Efficacy and safety of artemisinin-based combination therapy, and molecular markers for artemisinin and piperaquine resistance in mainland Tanzania. Malar J 17:369. doi: 10.1186/s12936-018-2524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feng J, Li J, Yan H, Feng X, Xia Z. 2015. Evaluation of antimalarial resistance marker polymorphism in returned migrant workers in China. Antimicrob Agents Chemother 59:326–330. doi: 10.1128/AAC.04144-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu C, Wei Q, Yin K, Sun H, Li J, Xiao T, Kong X, Wang Y, Zhao G, Zhu S, Kou J, Yan G, Huang B. 2018. Surveillance of antimalarial resistance Pfcrt, Pfmdr1, and Pfkelch13 polymorphisms in African Plasmodium falciparum imported to Shandong Province, China. Sci Rep 8:12951. doi: 10.1038/s41598-018-31207-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tacoli C, Gai PP, Bayingana C, Sifft K, Geus D, Ndoli J, Sendegeya A, Gahutu JB, Mockenhaupt FP. 2016. Artemisinin resistance-associated K13 polymorphisms of Plasmodium falciparum in southern Rwanda, 2010-2015. Am J Trop Med Hyg 95:1090–1093. doi: 10.4269/ajtmh.16-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yao Y, Wu K, Xu M, Yang Y, Zhang Y, Yang W, Shang R, Du W, Tan H, Chen J, Lin M, Li J. 2018. Surveillance of genetic variations associated with antimalarial resistance of Plasmodium falciparum isolates from returned migrant workers in Wuhan, central China. Antimicrob Agents Chemother 62. doi: 10.1128/AAC.02387-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ikeda M, Kaneko M, Tachibana SI, Balikagala B, Sakurai-Yatsushiro M, Yatsushiro S, Takahashi N, Yamauchi M, Sekihara M, Hashimoto M, Katuro OT, Olia A, Obwoya PS, Auma MA, Anywar DA, Odongo-Aginya EI, Okello-Onen J, Hirai M, Ohashi J, Palacpac NMQ, Kataoka M, Tsuboi T, Kimura E, Horii T, Mita T. 2018. Artemisinin-resistant Plasmodium falciparum with high survival rates, Uganda, 2014-2016. Emerg Infect Dis 24:718–726. doi: 10.3201/eid2404.170141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dorsey G, Kamya MR, Singh A, Rosenthal PJ. 2001. Polymorphisms in the Plasmodium falciparum pfcrt and pfmdr-1 genes and clinical response to chloroquine in Kampala, Uganda. J Infect Dis 183:1417–1420. doi: 10.1086/319865. [DOI] [PubMed] [Google Scholar]
- 50.Francis D, Nsobya SL, Talisuna A, Yeka A, Kamya MR, Machekano R, Dokomajilar C, Rosenthal PJ, Dorsey G. 2006. Geographic differences in antimalarial drug efficacy in Uganda are explained by differences in endemicity and not by known molecular markers of drug resistance. J Infect Dis 193:978–986. doi: 10.1086/500951. [DOI] [PubMed] [Google Scholar]
- 51.Tumwebaze P, Tukwasibwe S, Taylor A, Conrad M, Ruhamyankaka E, Asua V, Walakira A, Nankabirwa J, Yeka A, Staedke SG, Greenhouse B, Nsobya SL, Kamya MR, Dorsey G, Rosenthal PJ. 2017. Changing antimalarial drug resistance patterns identified by surveillance at three sites in Uganda. J Infect Dis 215:631–635. doi: 10.1093/infdis/jiw614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Conrad MD, Mota D, Foster M, Tukwasibwe S, Legac J, Tumwebaze P, Whalen M, Kakuru A, Nayebare P, Wallender E, Havlir DV, Jagannathan P, Huang L, Aweeka F, Kamya MR, Dorsey G, Rosenthal PJ. 2017. Impact of intermittent preventive treatment during pregnancy on Plasmodium falciparum drug resistance-mediating polymorphisms in Uganda. J Infect Dis 216:1008–1017. doi: 10.1093/infdis/jix421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE. 1995. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg 52:565–568. doi: 10.4269/ajtmh.1995.52.565. [DOI] [PubMed] [Google Scholar]
- 54.Nei M. 1987. Molecular evolutionary genetics. Columbia University Press, New York, NY. [Google Scholar]
- 55.Watterson GA. 1975. On the number of segregating sites in genetic models without recombination. Theor Popul Biol 7:256–276. doi: 10.1016/0040-5809(75)90020-9. [DOI] [PubMed] [Google Scholar]
- 56.Librado P, Rozas J. 2009. DnaSP v5: a software for comprehensive analysis of DNA polymorphism data. Bioinformatics 25:1451–1452. doi: 10.1093/bioinformatics/btp187. [DOI] [PubMed] [Google Scholar]
- 57.Stoletzki N, Eyre-Walker A. 2011. Estimation of the neutrality index. Mol Biol Evol 28:63–70. doi: 10.1093/molbev/msq249. [DOI] [PubMed] [Google Scholar]
- 58.Nei M, Gojobori T. 1986. Simple methods for estimating the numbers of synonymous and nonsynonymous nucleotide substitutions. Mol Biol Evol 3:418–426. doi: 10.1093/oxfordjournals.molbev.a040410. [DOI] [PubMed] [Google Scholar]
- 59.Kumar S, Stecher G, Tamura K. 2016. MEGA7: molecular evolutionary genetics analysis version 7.0 for bigger datasets. Mol Biol Evol 33:1870–1874. doi: 10.1093/molbev/msw054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aurrecoechea C, Brestelli J, Brunk BP, Dommer J, Fischer S, Gajria B, Gao X, Gingle A, Grant G, Harb OS, Heiges M, Innamorato F, Iodice J, Kissinger JC, Kraemer E, Li W, Miller JA, Nayak V, Pennington C, Pinney DF, Roos DS, Ross C, Stoeckert CJ Jr, Treatman C, Wang H. 2009. PlasmoDB: a functional genomic database for malaria parasites. Nucleic Acids Res 37:D539–D543. doi: 10.1093/nar/gkn814. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Accession numbers are reported in Table S5 in the supplemental material.


