Abstract
Pimavanserin is a first-in-class selective serotonin 5-HT2A receptor inverse agonist approved for the treatment of Parkinson disease psychosis. This article discusses pimavanserin’s mechanism of action, which patients are appropriate candidates for therapy, adverse reactions, and appropriate dosing.
Keywords: pimavanserin, Parkinson disease, psychosis, hallucinations, dysrhythmias, antipsychotic
A patient’s daughter visits the office, distressed and exasperated. Her mother has late-stage Parkinson disease presenting with hallucinations and delusions that are progressively worsening her quality of life. The patient failed gradual dose reduction of her carbidopalevodopa and apomorphine treatments because it aggravated her motor symptoms. Her only other medications are for constipation and hypertension, and she has been ruled out for concomitant infection.
This patient may be a candidate for pimavanserin, which offers a novel pharmacotherapeutic approach to treat the difficult symptomatology of Parkinson disease psychosis (PDP). Approved by the FDA in 2016, pimavanserin is the first drug specifically for treating PDP and the first-in-class selective serotonin 5-HT2A receptor inverse agonist.
A GROWING CONCERN
About 1% of the population over age 60 years in industrialized nations is diagnosed with Parkinson disease, making it the second most prevalent neurodegenerative disorder after Alzheimer disease (Figure 1).1 Parkinson disease affects the extrapyramidal motor system and is characterized by motor deficiencies such as rigidity, tremor, and bradykinesia. In addition to motor symptoms, up to 60% of patients develop PDP, a debilitating psychiatric condition characterized by hallucinations and/or delusions.2 Management of PDP often includes a reduction in dopaminergic Parkinson disease medications (such medicines can contribute to or cause psychosis) or the introduction of an atypical anti-psychotic medication, such as clozapine.3 Atypical antipsychotics have lower risk of causing extrapyramidal adverse reactions relative to typical antipsychotics, such as haloperidol, but can cause other serious adverse reactions such as metabolic syndrome, and in the case of clozapine, life-threatening agranulocytosis.
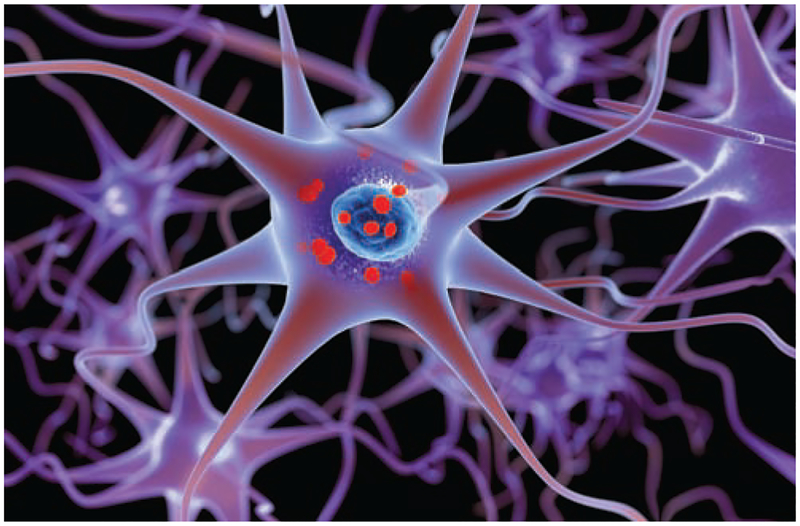
FIGURE 1.
Three-dimensional illustration of neurons containing Lewy bodies in a patient with Parkinson disease
Serotonin 5-HT2A receptor inverse agonism was found to be one of the common aspects of the polypharmacology of atypical antipsychotics, and correlation analyses suggested this contributes to their clinical efficacy and low incidence of extrapyramidal adverse reactions. These observations inspired the development of pimavanserin, a highly selective serotonin 5-HT2A (and to a lesser extent 5-HT2C) receptor inverse agonist, as a potentially safer medication for PDP.4 In a randomized, double-blind, placebo-controlled study, pimavanserin improved psychotic symptoms in patients with PDP, while also leading to improved sleep and decreased caregiver burden.5
The recommended dose of pimavanserin is 34 mg taken orally once daily. The recommended dose is 10 mg once daily if the patient also is taking a strong CYP3A4 inhibitor such as ketoconazole.
SAFETY CONCERNS
Pimavanserin was granted a breakthrough therapy designation by the FDA, which expedited its review and development. The definitive clinical trial that led to its approval was 6 weeks long, and no data exist on the drug’s long-term efficacy and safety in patients with Parkinson disease.5,6 Also, 91% of the patients in the clinical trial were white, so clinicians might want to take this into consideration when monitoring patients of other racial or ethnic backgrounds who are taking this drug.
Although pimavanserin effectively treats PDP and has high selectivity for its target, 5-HT2A receptors are important signaling proteins of the central and peripheral serotonin systems and inactivating them might cause problems. Reported adverse reactions to pimavanserin include confusional state, peripheral edema, and hallucinations (paradoxically); these reactions occurred in 5% or more of patients receiving pimavanserin (1 or more doses, N = 104) and did not also occur at or above this frequency with placebo (N = 94).
The warnings and precautions section of the prescribing information notes that pimavanserin prolongs the QT interval; this risk is increased if pimavanserin is taken with other drugs known to cause QT interval prolongation. Pimavanserin should not be prescribed to patients with a history of cardiac dysrhythmias.
Adverse reactions to pimavanserin reported postmarketing include rash, urticaria, tongue swelling, and other reactions consistent with angioedema, and somnolence. Because of the drug’s effects on sleep noted in the clinical trial, providers should monitor how this reaction affects patient quality of life.5
Patient and caregiver reports presented to the FDA suggested that pimavanserin may increase risk of death, though this could be confounded by the fact that patients with PDP often have advanced pathology that is associated with increased mortality. The FDA performed a postmarket review and did not discover any new or unexpected safety findings or findings inconsistent with the safety profile described in the prescribing information. Like other antipsychotics, pimavanserin carries a black box warning that it can increase mortality in older adults with dementia-related psychosis. The drug is not approved for treating psychosis unrelated to Parkinson disease.
CONCLUSION
Although more studies are needed to further investigate this drug’s potential benefit, potential risk, and long-term outcomes, pimavanserin may be an option for patients with PDP.
Footnotes
The authors have disclosed no potential conflicts of interest, financial or otherwise.
REFERENCES
- 1.Tysnes OB, Storstein A. Epidemiology of Parkinson’s disease. J Neural Transm (Vienna). 2017;124(8):901–905. [DOI] [PubMed] [Google Scholar]
- 2.Forsaa EB, Larsen JP, Wentzel-Larsen T, et al. A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol. 2010;67(8):996–1001. [DOI] [PubMed] [Google Scholar]
- 3.Chen JJ, Swope DM. Parkinson’s disease In: DiPiro JT, Talbert RL, Yee GC, et al. , eds. Pharmacotherapy: A Pathophysiologic Approach. 9th ed New York, NY: McGraw-Hill Co.; 2014. [Google Scholar]
- 4.Hacksell U, Burstein ES, McFarland K, et al. On the discovery and development of pimavanserin: a novel drug candidate for Parkinson’s psychosis. Neurochem Res. 2014;39(10):2008–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet. 2014;383(9916):533–540. [DOI] [PubMed] [Google Scholar]
- 6.US Food and Drug Administration. Fact sheet: breakthrough therapies. www.fda.gov/RegulatoryInformation/LawsEnforcedbyFDA/SignificantAmendmentstotheFDCAct/FDASIA/ucm329491.htm. Accessed December 4, 2018.