Abstract
Background
Typical hospital lighting is rich in blue-wavelength emission, which can create unwanted circadian disruption in patients when exposed at night. Despite a growing body of evidence regarding the effects of poor sleep on health outcomes, physiologically neutral technologies have not been widely implemented in the US healthcare system.
Objective
The authors sought to determine if rechargeable, proximity-sensing, blue-depleted lighting pods that provide wireless task lighting can make overnight hospital care more efficient for providers and less disruptive to patients.
Design
Non-randomised, controlled interventional trial in an intermediate-acuity unit at a large urban medical centre.
Methods
Night-time healthcare providers abstained from turning on overhead patient room lighting in favour of a physiologically neutral lighting device. 33 nurses caring for patients on that unit were surveyed after each shift. 21 patients were evaluated after two nights with standard-of-care light and after two nights with lighting intervention.
Results
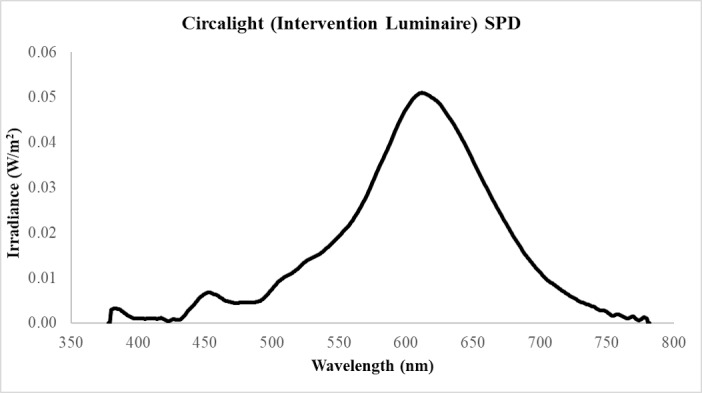
Providers reported a satisfaction score of 8 out of 10, with 82% responding that the lighting pods provided adequate lighting for overnight care tasks. Among patients, a median 2-point improvement on the Hospital Anxiety and Depression Scale was reported.
Conclusion and relevance
The authors noted improved caregiver satisfaction and decreased patient anxiety by using a blue-depleted automated task-lighting alternative to overhead room lights. Larger studies are needed to determine the impact of these lighting devices on sleep measures and patient health outcomes like delirium. With the shift to patient-centred financial incentives and emphasis on patient experience, this study points to the feasibility of a physiologically targeted solution for overnight task lighting in healthcare environments.
Keywords: patient-centered care, nurses, healthcare quality improvement, human factors, hospital medicine
INTRODUCTION
Circadian rhythms are mediated through a complex network of hormonal and environmental cues. The production of melatonin, a key hormone in sleep–wake regulation, is regulated through ‘doses’ of light—composed of wavelength, intensity and the angle at which light enters the eye.1 To better understand the way in which a light source affects the production of melatonin in humans, we must first define its spectral power distribution (SPD) curve (as in figures 1 and 2). From the Illuminating Engineering Society Handbook, SPD is “a pictorial representation of the radiant power emitted by a light source at each wavelength or band of wavelengths in the visible region of the electromagnetic spectrum (360 to 770 nanometers)”.2 Melatonin production is most affected through exposure to both high-intensity light as well as shorter light wavelengths that appear ‘blue’ to the naked eye,1 3 in other words, a light source with left-sided skew on the SPD curve. The authors will refer to these lights as inappropriate nocturnal photic stimuli. Disruption of melatonin production leads to sleep interruptions, unhinged sleep architecture, reduced sleep latency and lower subjective sleep satisfaction.4 5
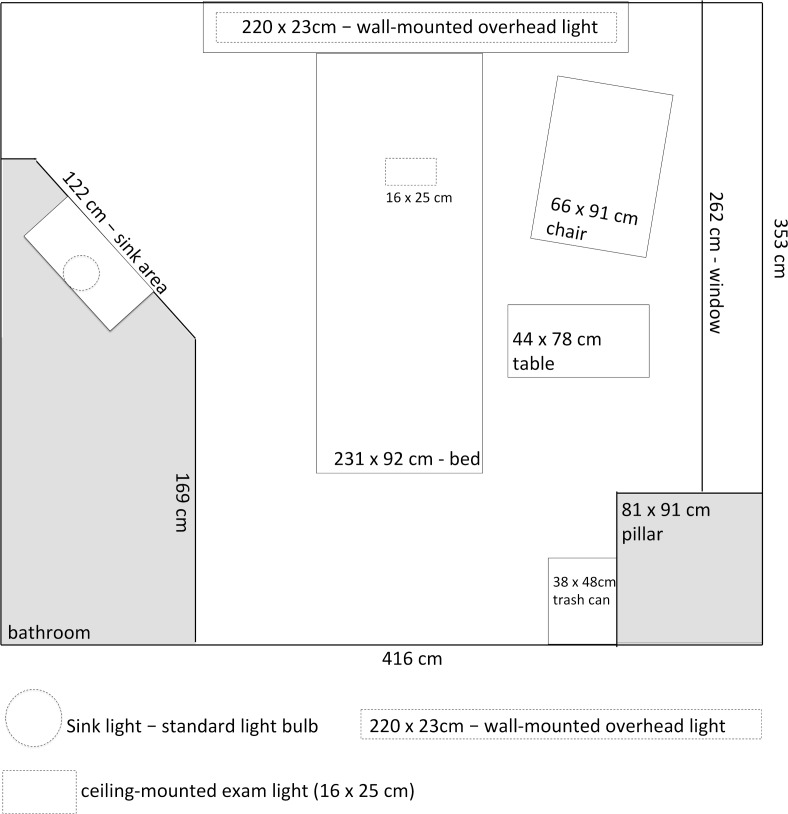
Figure 1.
Spectral power distribution (SPD) of Circalux luminaire (at maximum intensity) used in study.
Figure 2.
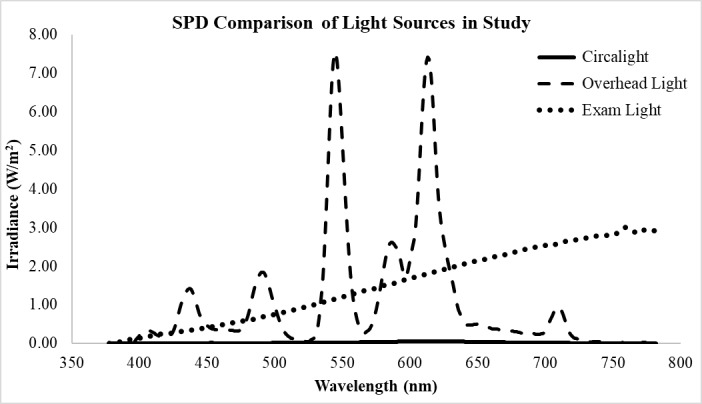
Spectral power distribution (SPD) of different light sources in the patient room studied in the authors’ hospital. Note: the circalight curve is almost not visible at this scale.
The effects of inappropriate nocturnal photic stimuli in humans is an area of increasing concern and may be linked to disease states.6 In the hospital setting, sleep-deprived patients have higher levels of stress hormones, and an increased risk for obesity, cardiovascular disease and diabetes.7–10 A recent study of healthy young adults showed that a single exposure to bright light (>500 lux) overnight increased non-esterified fatty acid, postprandial plasma glucose and insulin levels.11 The disruption of circadian rhythms has been implicated in hospital delirium (accounting for up to US$143 billion in healthcare expenditures annually), postoperative psychosis in surgical patients, and in the pathogenesis of neurodegenerative diseases like Parkinson’s disease and Alzheimer’s dementia.12–14
Sleep-promoting lighting is becoming more readily available in the commercial sector but has not been adopted in the US healthcare system. Many healthcare institutions still use fluorescent tube light sources in patient rooms, and even those that use LEDs will opt for (‘bright’ or ‘daylight’) short-wavelength irradiance that suppresses melatonin when switched on day or night.15 This is indeed the case in the institution discussed in this work (table 1). In the intensive care unit (ICU), where patient interactions occur up to eight times per hour, well-meaning providers often use flashlights and cellphone lights to complete tasks to avoid disturbing patients, not realising that most off-the-shelf torches or phone lights use disruptive bright-white (read: high-intensity, short-wavelength) LED chips.7 16–19 A 2016 survey found that 88% of over 1200 providers felt that poor sleep impacts the quality of patient healing, contributes to longer hospital stays and diminishes treatment responses.7 Of course, short-wavelength lighting is only part of the problem. Research in the area of patient sleep identifies different environmental factors that vary widely in their potential physiological impact and cost of implementation: from room temperature to the amount of natural daylight exposure.20–22 Physiologically neutral lighting systems exist and have been validated in the hospital—most notably the Philips HealWell suite (HealWell). Using LED lighting fixtures to attune correlated colour temperatures with circadian rhythms, HealWell improved patient sleep metrics after five nights in the hospital—including a 7.3% increase (29 min) in sleep duration.23 Despite promising results, many hospitals cannot afford to upgrade or retrofit all lighting systems, so it is not widely implemented.
Table 1.
Illuminance levels (lux) as a comparison of the various light sources in the patient room, including the Circalux luminaire at full, half and lowest intensities (as determined by the distance of the electronic tag)
| Light source | Illuminance at patient eye (lux) |
| Hospital room overhead light | 1520 |
| Hospital room examination light | 950 |
| Overhead light+examination light | 2470 |
| Circalight @ full (2 ft) | 6 |
| Circalight @ half (5 ft) | 3 |
| Circalight @ dimmest (8 ft) | 1 |
Accordingly, there is a need to study and address the problem of poor sleep architecture in the hospital with new, cost-effective lighting solutions. This feasibility study sought to determine if a novel lighting system developed by the authors to minimise circadian rhythm disruption could be incorporated into existing hospital workflows and settings. Secondarily, this study sought to gather preliminary data on the short-term effects of this lighting system on patient-reported quality, latency and duration of sleep, overall satisfaction with care, and Hospital Anxiety and Depression Scale (HADS) scores.
Methods
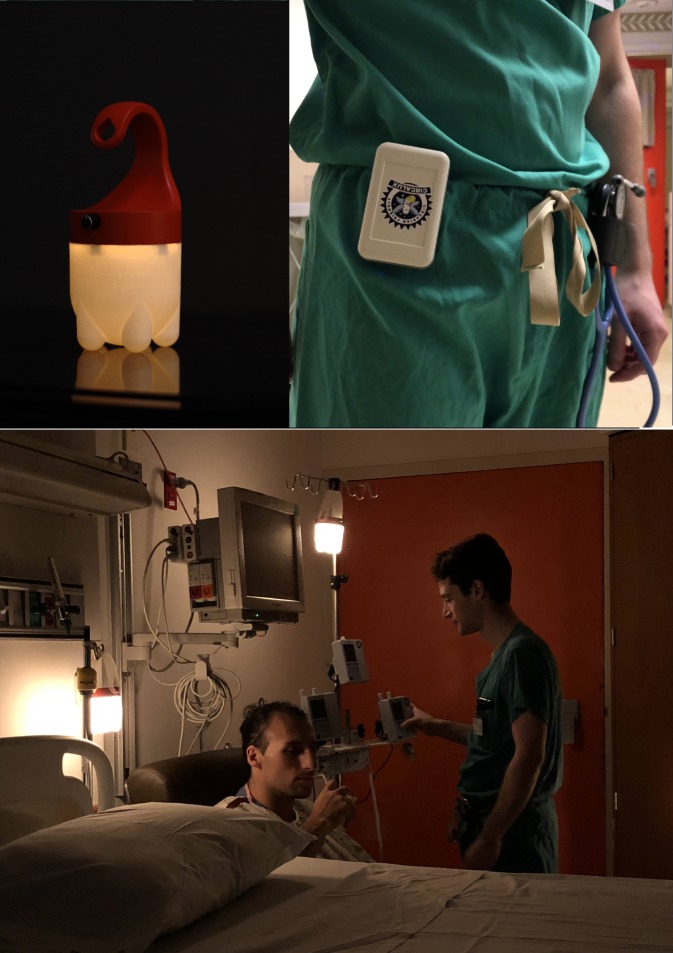
This research complied with the tenets of the Declaration of Helsinki. All participants were informed of the objectives, risks and benefits of the study. Two populations were evaluated in this feasibility study: patients and their nurses on an intermediate-care medical floor at a large medical centre in Philadelphia, PA. All patient rooms were single-occupancy, private rooms with matching layouts. When a healthcare provider enters a patient room, he can toggle the light switch for one or both of the room lights (overhead and/or examination light), as shown in figure 3.
Figure 3.
Schematic of hospital patient room at Thomas Jefferson University Hospital, with location of overhead fluorescent light source and examination light source.
Pre-investigation observation
To gain a better understanding of overnight light disruptions in the hospital, the authors mapped the frequency and duration of overhead lighting use in intermediate-care patient rooms for two nights. These were cardiac observation patients who were not ultimately enrolled in the study. Since observation did not require entering a patient room or eliciting information, no informed consent was pursued. During this observation period, it was noted that the overhead lights were turned on between 5 and 25 times overnight and stayed on for duration of 1–15 min at a time between 21:00 and 07:00. Staff used task lighting to complete vital sign checks, exchange intravenous fluids, administer medications, and record patient inputs and outputs. Nurses and aides were also observed to use flashlights and cell phones to complete their tasks as courteously as possible.
Pilot survey study
The authors also sought to evaluate the attitudes of hospital patients and their families regarding the current hospital night-time lighting environment. To this end, they conducted a small survey study of patients, families and nursing staff at Nemours Alfred I. DuPont Hospital for Children (Wilmington, DE). The authors chose this population so that a broad range of attitudes regarding sleep from minors (patients) and adults (parents) could be elicited. This pilot was approved by the DuPont Hospital Institutional Review Board, and informed consent was obtained from each participant. The surveys assessed attitudes about the impact of lighting on sleep, baseline sleep habits at home, sleep latency and quality at home and the hospital, night-time awakenings at home and in the hospital, the source of night-time disturbances at home and the hospital, impact of overnight lighting on views of hospital stay and interest in sleep-friendly lighting options in the hospital.
Intervention lighting study
Materials
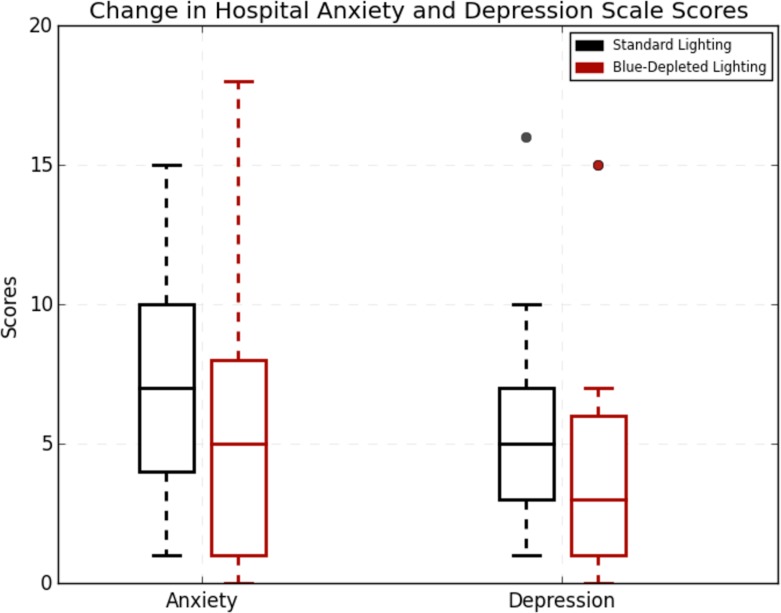
Twelve light source devices and wearable tags as pictured in figure 4 were provided for this study (Circalux, Philadelphia, USA). The devices, known as ‘circalights’, illuminate when in the presence of the tags, emitting predominantly long-wavelength white light through LEDs mounted to a printed circuit board. The authors constructed an SPD curve using a detector placed 50 cm from the circalights set to maximum intensity (figure 1). Maximum brightness emitted from the intervention luminaire used in the study was 6 lux at 50 cm. The devices contain a receiver that senses the distance to a wearable tag, and the maximum illuminance corresponds to the tag being within 2 feet of the light source. As the tag (ie, healthcare provider) moves further away, the luminaire is programmed to dim linearly and smoothly to zero lux at 8 feet (table 1). The dimensions of the device are 3 in.×3 in.×6 in. and the bottom half is 3 in. in height and the material is a prototype translucent nylon (Shapeways, New York, USA). The illuminance and SPD of these fully assembled prototype devices were measured.
Figure 4.
Device used (top left) and wearable transmitter that triggers light (top right). Actor depiction of usage at bottom.
The circalight exterior and printed circuit board was custom made. The pods could be cleaned with standard disinfection wipes used on hospital devices. The circalights are intended to provide healthcare providers a means to work by the illumination of a light with a flexible handle that can be placed or hung anywhere (powered by rechargeable battery) in the patient room and triggered by the proximity of the caregiver to the device (figure 4). Proximity sensing was enabled through an onboard ultrawide-band (UWB) radio transceiver, modulated by distance.
Light characteristics
Spectral irradiance and illuminance measures for this study were taken using a Sekonic C-7000 SpectroMaster Spectrometer (Sekonic, Tokyo, Japan) within a hospital room of the same layout as those used in the study. The shades were drawn and the door was closed to simulate a darkened/night-time scenario. The spectrometer was placed on the patient bed pillow facing upward towards the ceiling in order to replicate light exposure levels for the patient’s eye. The Circalux luminaire (circalight) was hung on a fixed pole that placed it at a distance of 50 cm from the patient’s eye, with the overhead fluorescent lighting at a distance of 60 cm and the overhead examination light at a distance of 1.4 m. As seen in figure 2, even at maximum, the intensity of the circalight is barely visible above the horizontal axis when compared with the other light sources in the room. The SPD in figure 1 provides increased magnification and more detail for the circalight spectral output. Table 1 provides illuminance levels (lux) as a comparison of the various light sources in the patient room, including the circalight at full, half and lowest intensities (as determined by the distance of the electronic tag).
The study luminaire (circalight) is 2–3 orders of magnitude less bright (by illuminance measurement), and it emits fewer short-wavelengths peaks than the hospital room overhead light. The authors believe that these characteristics make it an acceptable model for a physiologically neutral light source.
Study cohorts and testing
Patient population
Twenty patients were selected for this feasibility study. Inclusion criteria for the patient population were a Glasgow Coma Scale of 15 and the ability to communicate with the researchers. Exclusion criteria included altered mental status limiting awareness of the previous night’s sleep, disease acuity requiring ICU level of care or sleeping with the room lights on in the hospital. Participants experience two nights with standard hospital lighting and two nights with circalights. Patients completed surveys on sleep quality, sleep duration, sleep onset, sleep latency and overall satisfaction with their care experience—all ranked from 1 (lowest) to 10 (highest) on a Likert scale. Participants were made aware of the structure of the study including two nights with the standard lighting environment and two nights with circalights.
Patients also completed the HADS questionnaire—a widely studied and validated point-based psychological screening tool that assesses the severity of anxiety/depression and quality of life in response to disease states and treatment.24–26 The Verran and Snyder-Halpern Sleep Scale assesses more acute changes in sleep patterns over 3 days, but this had not been used in similar pilot studies of hospital lighting systems like the HealWell study. Patients completed HADS surveys after two nights with standard hospital lighting and again after two nights using the pods.
Nurse population
Nurses were consented and enrolled in the study if they were taking care of patients who elected to participate. They were instructed on the use of the devices prior to each full night shift. Nurses who did not work a full night with an enrolled patient or who were unable to use the pods were excluded from the study. These providers completed surveys rating how helpful automatic lighting pods were in clinical care, where they were positioned, proportion of shift used and whether it was sufficient lights for tasks—each parameter of which was rated on a 10-point Likert scale (1 being least helpful, 10 being most helpful). Nurses were also asked to provide general short-answer feedback on the devices.
Statistical analysis
Likert Scale data on care experience and HADS scores were paired with ordinal data and were compared with the Wilcoxon signed-rank test where the null hypothesis was that there was no difference between the medians. Estimates of sleep duration were compared using a paired t-test where the null hypothesis was that there would be no difference in the means. Estimates of sleep latency were compared with the Wilcoxon signed-rank test with a correction for the continuous nature of the data due to a significantly non-normal distribution.
An α of 0.05 was selected a priori. Results were analysed in R V.3.1.1 (R Foundation for Statistical Computing).
Results
The DuPont survey results showed the following: 79% of patient survey respondents (n=122) believed that inappropriate nocturnal photic stimuli affects sleep, while 40% indicated that they got significantly less sleep in the hospital. Notably, estimated sleep duration was low for both the control and intervention periods. Inciting factors for sleep disruption included light alone (3%) as well as light and noise (42%). Forty-one per cent would like more sleep-friendly lighting, while 59% reported that a better lighting set-up would improve their opinion of their care at a hospital. Ninety-four per cent of nurses (n=16) agreed that poor sleep affects patient outcomes. The nurses entered patient rooms between four and eight times per night, administer care in almost complete darkness most of the time (44%) or half of the time (50%) to avoid bothering patients, and over 80% would be interested in an alternative solution.
Twenty-one patients were consented, enrolled in the study and completed two nights with lighting pods in addition to two nights with standard overhead lighting. Patients were admitted to a telemetry-monitoring floor in a large academic medical centre in an urban market and had been in the hospital for at least two nights at the time of enrolment. Patients were ages 42 to 84 with a female:male ratio of 1.4:1. As noted, anxiety and depression scores with standard hospital lighting did not meet thresholds for the HADS tool (8 points on a 21-point scale deemed positive). Three patients did not report an estimate of their sleep duration for either set of nights, and five patients failed to report estimates of sleep latency. These results are summarised in table 2.
Table 2.
Sleep quality, overnight care quality, anxiety, depression and sleep latency characteristics of the post-intervention with blue-depleted lights compared with pre-intervention
| Measure | N | Blue-depleted light | Standard lighting | Δ | P value | 95% CI |
| Medians | ||||||
| Sleep quality | 21 | 6 | 5 | 1 | 0.138 | (−3 to 1) |
| Overnight care quality | 21 | 7 | 8 | −1 | 0.895 | (−1.5 to 1.5) |
| HADS—Anxiety | 21 | 5 | 7 | −2 | 0.004 | (1.5 to 2.5) |
| HADS—Depression | 21 | 3 | 5 | −2 | 0.038 | (0 to 2.5) |
| Sleep latency (min) | 16 | 11.25 | 10 | 1.25 | 0.187 | (−32 to 9) |
| Means | ||||||
| Estimated sleep duration (h) | 18 | 4.47 | 4.5 | −0.29 | 0.3 | (−0.8 to 1.4) |
HADS, Hospital Anxiety and Depression Scale.
A total of 33 nurses participated in the study with all participants completing the survey. The median satisfaction with the blue-depleted lights was 8 out of 10, and 82% responded that the pods provided sufficient light for overnight tasks. Sixty-seven per cent responded that the lights were superior to an existing alternative.
A statistically significant difference in both anxiety and depression, as measured by the HADS, was observed in patients using the pods. These results are illustrated in figure 5. Use of lighting pods was associated with a median improvement of 2 points for both depression and anxiety ratings.
Figure 5.
Comparing anxiety and depression pre-intervention and post-intervention with blue-depleted light. n=21, significant median improvement of 2 points for both anxiety and depression (p<0.005, p<0.05, respectively).
Discussion
The DuPont study demonstrates that nurses have almost unanimous agreement on the effect of poor sleep on outcomes, likely credit to their experience as observer of countless patient experiences. It also exposes a disturbing statistic that is rarely discussed: nurses administer care in almost complete darkness most of the time (44%) or half of the time (50%) to avoid bothering patients. This does not inspire confidence, understandably, and providers are aware that this is indeed a problem, with the majority interested in an alternative.
The DuPont data also show an interesting discordance within the patient answers: although 79% believed inappropriate nocturnal photic stimuli affects sleep, only 3% believed that light alone was an inciting factor for sleep disruption. The authors believe that patients indeed recognise that sleep disruption in the hospital is multifactorial (eg, light, noise, pain, anxiety, etc combined). The authors place a significant amount of weight on the investigation for improved lighting because of two main reasons: First, the authors are cognisant of the literature that supports light as the primordial driver of human circadian rhythm, and retinal light sensors have a direct phone line, per se, to the melatonin-producing cells of the brain (not the case for auditory circuits). Second, hospital lighting is a physical element of the environment that can be altered quite easily. Fluorescent overhead lighting is a remnant of the industrial warehouse-style hospital care of the mid-20th century, and it is most cost-effective. However, depending on the resources of the institution, lighting can be made as finely tuned to the circadian rhythm of patients as possible (see Philips HealWell Suite). The goal of the authors is to determine if the light element can be affected through a more cost-effective and easily deployable approach.
The aim of this study was to assess the feasibility of proximity-activated and blue-depleted night lights in the hospital. Patients showed significant improvement in HADS scores after two nights with circalights but major changes in sleep duration or sleep perceptions. Surveyed providers found the lights to be helpful in their overnight care and superior to existing alternatives like flashlights, cell phone lights and overhead lighting.
The median provider satisfaction score was 8 out of 10, supporting the hypothesis that circalights could be useful in clinical workflow. Eighty-two per cent of surveyed providers indicated that the lighting pods provided adequate lighting for overnight care tasks, while 67% found circalights to be superior to existing lighting alternatives. Nurses described the lights as soothing and less disruptive to patients. Negative nurse feedback included inadequate battery life for busy 12-hour shifts, not having enough tags for all the healthcare staff (eg, EKG technicians, phlebotomists) and not nearly enough light for comfortable venipuncture.
Patients with circalights in their rooms showed a median 2-point improvement in HADS ratings. Although statistically significant, it is unclear if the data are of clinical significance. However, data that point at non-inferiority inspire larger studies with blue-depleted lighting that explore clinical endpoints such as delirium and falls in patients. Mean estimated sleep duration was low for both the control and intervention arms. Clinical improvement with resolution of acute illness could impact improvements in anxiety and depression within a hospital stay. The authors were encouraged by the relatively low p-wave (p=0.138) observed in patient-reported sleep quality but acknowledge that this may reflect a placebo effect with circalights. There were no differences in patient-rated overnight care quality, sleep latency or estimated sleep duration. An unexpected use case: a deaf patient indicated that the proximity-sensing lights had the positive effect of alerting him to the presence of providers.
Inappropriate nocturnal photic stimuli may result in negative outcomes in patient care, increased healthcare costs and energy usage, and decreased staff efficiency.14 27–30 As value-based care and patient satisfaction metrics become increasingly incorporated into healthcare reimbursements, lighting alternatives that reinforce healthy sleep could represent an avenue to improve the hospital environment and overnight workflow. The cost to produce the device used in this study is approximately US$80 per device/tag combo and would likely drop to US$40–50 at scale. In addition, as a low-cost modality that does not interfere with other bandwidths, the UWB radio technology used in circalights could be used for real-time tracking, location of assets and ‘Internet-of-Hospital-Things’ applications.
Limitations of the study
Limitations of this feasibility study include use of non-validated custom surveys, inability to complete cross-over design, short duration of control and experimental periods, inability to factor in pre-existing sleep and psychiatric disorders, lack of objective sleep data, confounding mood improvement with clinical improvement and inability to effectively blind. In addition to inappropriate nocturnal photic stimuli, numerous factors affect sleep in the hospital including pain and noise. The authors were unable to provide tags to every member of the overnight care team (eg, EKG tech) so circalights could not be used for every single night-time care task. Since patient length of stay was so unpredictable on the observation unit, the organisers were not able to execute the planned cross-over design. While validated and used in the HealWell study, the HADS questionnaire does differentiate between anxiety or depression.
Future research
There are several interesting avenues of research for task lighting tuned to circadian rhythms in the hospital. The clinical significance of improved HADS scores with circalights needs to be correlated over longer periods, studied with a larger sample size, and stratified according to patient age and comorbid conditions like sleep apnoea. Sleep metrics should be correlated with objective measures like serum melatonin measurements, polysomnography and wrist actigraphy. The authors will prospectively study the impact of physiologically neutral lighting on costly outcomes like delirium and falls in the hospital. Future developments will include fluorescent placebo lights, improved battery life and replacement of the physical tag with a phone application. The organisers will also allow providers to add more lights to patient rooms to maximise utility. The authors also hope to study other patient populations—including people in long-term care facilities, individuals with pre-existing sleep disorders and hearing-impaired individuals. Finally, there are numerous opportunities to explore the applications of UWB technology in the hospital.
The authors find several key implications of this work. A 2-day trial of blue-depleted overnight task lighting improves patient and provider satisfaction and possibly clinical measures. Notably, these aims can be accomplished in a cost-effective manner without an infrastructural overhaul. The authors recommend healthcare workflows that prioritise an 8-hour patient sleep window and minimising illumination in patient rooms during sleep hours by optimising care task timing. For task lighting in overnight care, the authors recommend lighting sources that minimise brightness and ‘blue’ wavelengths or alternative changes in workflow that shield patients from light altogether. Ultimately, the implementation of internal lighting that embraces its effect on circadian rhythms and healing requires validation and understanding by caregivers and also by patients, hospital administrators, financiers and designers.
Conclusion
Night-specific lighting pods are an efficient, cost-effective night-time lighting option for use in hospitals. This feasibility study provides information regarding the acceptability of the pods, and their ability to improve patient hospital experience via reduction in patient’s ratings of anxiety and depression while hospitalised. Lighting pods were well liked by care providers and helpful to complete their overnight care tasks. This study provided valuable information to guide lighting improvements and can stimulate development of more extensive studies on the use of these solutions in the hospital environment.
Key points.
Healthcare lighting design should mimic daylight–night to reinforce circadian physiology and optimise patient safety and outcomes.
The vast majority of hospitals do not have illumination or workflow designed to reinforce circadian rhythms or to minimise visual circadian disruptions despite reports of poor sleep in hospitals.
The authors implemented a standalone lighting device that helped providers to be more efficient in their care tasks and were less disruptive to patient sleep. They demonstrated feasible use in an intermediate-acuity hospital ward.
Acknowledgments
The authors would like to thank George Brainard, Ph.D. of the Light Research Program of Thomas Jefferson University for expertise and advising. The authors would also like to thank Lisa Wus and the nurses on 5W and 5NW who helped with and participated in this study. Publication made possible in part by support from the Thomas Jefferson University + Philadelphia University Open Access Fund. This project would not be possible without the support of Dr. Bon Ku, Jeffsolves, Jefferson Health Design Lab, and the Jefferson Innovation Pillar.
Footnotes
Contributors: LA planned the study, wrote the introduction, final editing, submission. TB created IRB protocol, wrote discussion and conclusion. ZM performed data analysis. MLC, ES and SN administered surveys and wrote materials section, maintained records. GH wrote results. YL organised nursing. BW provided illuminance and SPD data. JH worked with TB editing IRB protocol and manuscript editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: Thomas Jefferson University (Jefferson) and Circalux Inc. (Circalux) have a license agreement whereas Jefferson has intellectual property pending and is licensing to Circalux. Some of the authors (TB, LA and GH) hold equity in Circalux, and are inventors of the intellectual property, and as such did not participate in data collection or analysis. These same individuals were enrolled as students at Jefferson during the study duration. There was no financial exchange between any of the authors, Circalux and Jefferson for the purposes of this study. YL and JH are employees of Jefferson.
Patient consent for publication: Obtained.
Ethics approval: Thomas Jefferson University IRB Control no. 17C.566 JeffTrial no. 11814.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request, for a period of 24 months after data collection.
References
- 1.Brainard GC, Hanifin JP, Greeson JM, et al. . Action spectrum for melatonin regulation in humans: evidence for a novel circadian photoreceptor. J Neurosci 2001;21:6405–12. 10.1523/JNEUROSCI.21-16-06405.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DiLaura D, Houser KW, Misrtrick RG, et al. . The lighting handbook: reference and application. Illuminating Engineering Society of North America. 120 10th edn, 2011. [Google Scholar]
- 3.Lockley SW, Brainard GC, Czeisler CA. High sensitivity of the human circadian melatonin rhythm to resetting by short wavelength light. J Clin Endocrinol Metab 2003;88:4502–5. 10.1210/jc.2003-030570 [DOI] [PubMed] [Google Scholar]
- 4.Chellappa SL, Steiner R, Oelhafen P, et al. . Acute exposure to evening blue-enriched light impacts on human sleep. J Sleep Res 2013;22:573–80. 10.1111/jsr.12050 [DOI] [PubMed] [Google Scholar]
- 5.Bedrosian TA, Nelson RJ. Influence of the modern light environment on mood. Mol Psychiatry 2013;18:751–7. 10.1038/mp.2013.70 [DOI] [PubMed] [Google Scholar]
- 6.Zielinska-Dabkowska KM. Make lighting healthier. Nature 2018;553:274–6. 10.1038/d41586-018-00568-7 [DOI] [PubMed] [Google Scholar]
- 7.Kamdar BB, Knauert MP, Jones SF, et al. . Perceptions and practices regarding sleep in the intensive care unit. A survey of 1,223 critical care providers. Ann Am Thorac Soc 2016;13:1370–7. 10.1513/AnnalsATS.201601-087OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch - Eur J Physiol 2012;463:121–37. 10.1007/s00424-011-1044-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haus EL, Smolensky MH. Shift work and cancer risk: potential mechanistic roles of circadian disruption, light at night, and sleep deprivation. Sleep Med Rev 2013;17:273–84. 10.1016/j.smrv.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 10.Miller MA, Cappuccio FP. Inflammation, sleep, obesity and cardiovascular disease. Curr Vasc Pharmacol 2007;5:93–102. 10.2174/157016107780368280 [DOI] [PubMed] [Google Scholar]
- 11.Albreiki MS, Middleton B, Hampton SM. A single night light exposure acutely alters hormonal and metabolic responses in healthy participants. Endocr Connect 2017;6:100–10. 10.1530/EC-16-0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leslie DL, Inouye SK. The importance of delirium: economic and societal costs. J Am Geriatr Soc 2011;59 Suppl 2:S241–S243. 10.1111/j.1532-5415.2011.03671.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bourne RS, Mills GH. Melatonin: possible implications for the postoperative and critically ill patient. Intensive Care Med 2006;32:371–9. 10.1007/s00134-005-0061-x [DOI] [PubMed] [Google Scholar]
- 14.Wennberg AMV, Wu MN, Rosenberg PB, et al. . Sleep disturbance, cognitive decline, and dementia: a review. Semin Neurol 2017;37:395–406. 10.1055/s-0037-1604351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cajochen C, Münch M, Kobialka S, et al. . High sensitivity of human melatonin, alertness, thermoregulation, and heart rate to short wavelength light. J Clin Endocrinol Metab 2005;90:1311–6. 10.1210/jc.2004-0957 [DOI] [PubMed] [Google Scholar]
- 16.Nelson RJ, DeVries AC. Medical hypothesis: light at night is a factor worth considering in critical care units. Adv Integr Med 2017;4:115–20. 10.1016/j.aimed.2017.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunn H, Anderson MA, Hill PD. Nighttime lighting in intensive care units. Crit Care Nurse 2010;30:31–7. 10.4037/ccn2010342 [DOI] [PubMed] [Google Scholar]
- 18.Freedman NS, Kotzer N, Schwab RJ. Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Respir Crit Care Med 1999;159:1155–62. 10.1164/ajrccm.159.4.9806141 [DOI] [PubMed] [Google Scholar]
- 19.Bernhofer EI, Higgins PA, Daly BJ, et al. . Hospital lighting and its association with sleep, mood and pain in medical inpatients. J Adv Nurs 2014;70:1164–73. 10.1111/jan.12282 [DOI] [PubMed] [Google Scholar]
- 20.Beauchemin KM, Hays P. Sunny hospital rooms expedite recovery from severe and refractory depressions. J Affect Disord 1996;40:49–51. 10.1016/0165-0327(96)00040-7 [DOI] [PubMed] [Google Scholar]
- 21.Park MY, Chai C-G, Lee H-K, et al. . The effects of natural daylight on length of hospital stay. Environ Health Insights 2018;12:117863021881281 10.1177/1178630218812817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huisman ERCM, Morales E, van Hoof J, et al. . Healing environment: a review of the impact of physical environmental factors on users. Build Environ 2012;58:70–80. 10.1016/j.buildenv.2012.06.016 [DOI] [Google Scholar]
- 23.Giménez MC, Geerdinck LM, Versteylen M, et al. . Patient room lighting influences on sleep, appraisal and mood in hospitalized people. J Sleep Res 2017;26:236–46. 10.1111/jsr.12470 [DOI] [PubMed] [Google Scholar]
- 24.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 25.Bjelland I, Dahl AA, Haug TT, et al. . The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002;52:69–77. 10.1016/s0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 26.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical results. J Psychosom Res 1997;42:17–41. 10.1016/S0022-3999(96)00216-4 [DOI] [PubMed] [Google Scholar]
- 27.Dalke H, Little J, Niemann E, et al. . Colour and lighting in hospital design. Opt Laser Technol 2006;38:343–65. 10.1016/j.optlastec.2005.06.040 [DOI] [Google Scholar]
- 28.Martin J, Marler M, Shochat T, et al. . Circadian rhythms of agitation in institutionalized patients with Alzheimer’s disease. Chronobiol Int 2000;17:405–18. 10.1081/CBI-100101054 [DOI] [PubMed] [Google Scholar]
- 29.Saidur R, Hasanuzzaman M, Yogeswaran S, et al. . An end-use energy analysis in a Malaysian public hospital. Energy 2010;35:4780–5. 10.1016/j.energy.2010.09.012 [DOI] [Google Scholar]
- 30.Stevens RG, Brainard GC, Blask DE, et al. . Adverse health effects of nighttime lighting: comments on American Medical Association policy statement. Am J Prev Med 2013;45:343–6. 10.1016/j.amepre.2013.04.011 [DOI] [PubMed] [Google Scholar]