Abstract
Background:
Obesity is linked to hypercoagulability with an increased risk of venous thromboembolic events (VTE) in the uninjured population. Therefore, we hypothesize that obesity (Body Mass Index (BMI) ≥30 kg/m2) is associated with a hypercoagulable state postinjury characterized by increased clot strength and resistance to fibrinolysis.
Methods:
Our prospective Trauma Activation Protocol database includes all trauma activations patients for whom a rapid thrombelastography (TEG) is obtained within 60 minutes postinjury prior to any transfusions. The dataset was then stratified by BMI and subjects with BMI ≥ 30 kg/m2 were compared to those with BMI<30 kg/m2). The following TEG measurements were obtained: activated clotting time (ACT), clot formation rate (angle), maximum clot strength (MA), and % clot lysis 30 min after MA (LY30, %). Fibrinolysis shutdown (SD) was defined as LY30 < 0.6% and hyperfibrinolysis (HF) as LY30 > 7.6%. Continuous variables are expressed as median (IQR).
Results:
Overall, 687 patients were included of whom 161 (23%) had BMI ≥ 30kg/m2 (BMI30). The BMI30 group was older, had a lower proportion of males and of blunt trauma, and were less severely injured. After adjustment for confounders, BMI30 was independently associated with lower odds of MA<55mm (OR 0.28; 95% CI 0.130.60) and of HF (OR 0.31; 95% CI 0.10–0.97) and higher odds of SD (OR 1.82; 95% CI 1.09–3.05). No independent association was observed with angle<650 (OR 0.57 95% CI 0.30–1.05). While VTEs were more frequent among BMI30 patients (5.0 vs 3.3%), this did not reach significance after confounding adjustment (p=0.11).
Conclusion:
Obesity was protective against diminished clot strength and hyperfibrinolysis, and obesity was associated with an increased risk of fibrinolytic shutdown in severely injured patients. These findings suggest a relative hypercoagulability. Although no difference in VTEs was noted in this study, these findings may explain the higher rate of VTEs reported in other studies.
Level of Evidence: Level III, retrospective cohort study, prognostic
Keywords: Obesity, Trauma Induced Coagulopathy, Hypercoagulability, Thrombelastography, Fibrinolysis
Background:
The prevalence of obesity continues to increase worldwide and has reached epidemic levels in the United States with 40 percent of Americans now suffering from obesity.(1, 2) Several studies have shown that the presence of obesity increases the risk of morbidity and mortality following trauma; however, the underlying reason for this increased risk is not well known.(3–6) One possible explanation is the presence of a hypercoagulable state and consequent thrombotic morbidity associated with obesity.(7) With this hypercoagulable state, obesity has been linked to both arterial and venous thrombotic complications such as myocardial infarction and pulmonary emboli, respectively.(8–11) In trauma patients, obesity has been associated with a higher rate of venous thromboembolic (VTE) events, cardiovascular and pulmonary complications, and an increased risk of multiple organ failure (MOF). (12–15)
The mechanism of the obesity-related hypercoagulability involves a pro-thrombotic state secondary to chronic inflammation as well as decreased clot breakdown via inhibition of the fibrinolytic pathway.(16) Prior studies have shown that the obesity-induced hyperinflammatory state triggers upregulation of procoagulant factors in vascular endothelium and triggers increased platelet activity and thrombin generation.(17) Furthermore, levels of the antifibrinolytic protein plasminogen activator inhibitor-1 (PAI-1) are increased in subjects with obesity, especially those with high levels of visceral fat.(18) However, the interplay of these prothrombotic pathways in the setting of trauma-induced coagulopathy after severe injury in obese patients is poorly described.
Despite existing literature on obesity’s effects on coagulation, the effect of obesity on trauma-induced coagulopathy and fibrinolysis phenotypes after severe injury is not well known. Our group has previously shown that fibrinolysis shutdown is associated with an increase in mortality following trauma.(19) Kornblith et al. documented several effects of obesity on trauma-induced coagulation, yet they did not detect a correlation between BMI and thrombelastography-measured fibrinolysis as a continuous variable measured, and no comparison with specific fibrinolysis phenotypes (i.e., hyperfibrinolysis, physiologic fibrinolysis, and fibrinolysis shutdown) was done.(12)
Understanding the contribution of obesity to fibrinolysis phenotypes in trauma is of critical importance given the growing interest in early empiric therapies for coagulopathy in trauma and the increasing prevalence of obesity in trauma populations. Therefore, the aim of this study is to evaluate the effects of obesity on trauma-induced coagulation and fibrinolytic phenotypes in trauma using TEG. Given the hyperinflammatory and hypercoagulable state that occurs with obesity, we hypothesize that obesity is associated with a hypercoagulable state characterized by increased clot strength and resistance to clot lysis (fibrinolysis shutdown).
Methods:
Setting
This is a retrospective analysis of the Trauma Activation Protocol (TAP) dataset, a prospective study of risk factors for trauma-induced coagulopathy in consecutive trauma activation patients at the Ernest E Moore Shock Trauma Center at Denver Health (DH), an American College of Surgeons verified and Colorado State certified Level-1 trauma center. Inclusion criteria for this study were adults (age ≥ 18) meeting criteria for the highest trauma designation and who had a rapid thrombelastography (TEG) collected in the first hour after arrival and prior to any blood transfusions. All subjects were enrolled in this study after approval by the Colorado Multiple Institutional Review Board (COMIRB #13–3087) under waiver of consent due to minimal risk. To conform to the guidelines of minimal risk, only a single time point blood draw is obtained.
Participants:
Criteria for trauma activation at DH are: 1) any injury with systolic blood pressure (SBP) < 90 mm Hg, 2) respiratory compromise, obstruction and/or intubation with mechanism attributed to trauma, 3) Glasgow Coma Scale (GCS) <9 with mechanism attributed to trauma, 4) mechanically unstable pelvic injury, 5) gunshot wound penetrating the neck/torso or stab wounds to the neck, torso, or extremity proximal to elbow or knee, 6) amputation proximal to the ankle or wrist or 7) fall greater than or equal to 30 feet, 8) the emergency medicine attending or chief surgical resident suspects the patient is likely to require urgent operative intervention. Patients were excluded if they were transferred from an outside hospital, pregnant, prisoner, minor (<18 years old), with known chronic liver disease, an inherited coagulation dysfunction, or were taking anticoagulants prior to injury. Obesity was defined as body mass index (BMI) ≥ 30 kg/m2.(20)
Procedures:
Whole blood samples were collected in citrated vacuum tubes (3.5 mL, 3.2% sodium citrate, Greiner Bio-One, Monroe, North Carolina) either in the field by paramedics or upon arrival to the emergency department from May 2014 to April 2018. Citrated samples were recalcified and TEG was performed using the TEG 5000 Thrombelastography Hemostasis Analyzer (Haemonetics, Niles, IL) by trained professional research assistants. The TEG tracing provides the following measurements: activated clotting time (ACT [sec]), angle (°), maximum amplitude (MA [mm]), and percent lysis at 30 minutes after MA (LY30 [%]). ACT and angle represent clot formation while MA correlates with clot strength. Lastly, LY30 provides a measure of fibrinolysis (clot dissolution). Coagulopathy following trauma in this study was defined as ACT >128 seconds, MA <55 mm, and angle <65 degrees.(21) To determine fibrinolysis phenotypes, we used cutoffs derived for the trauma population as follows: fibrinolysis shutdown (SD) LY30 < 0.6% and hyperfibrinolysis (LY30 >7.7).(22) Functional Fibrinogen was performed as previously described.(23)
The TAP dataset prospectively collects transfusion data and clinical lab data including hemoglobin, platelet count, blood gas parameters, and conventional coagulation tests prothrombin time/International Normalized Ratio (PT/INR), and partial thromboplastin time (PTT). While research TEGs are completed prior to any transfusions received, clinical labs such as PT/INR and PTT may occur after the administration of transfusions or other interventions.
Outcomes and covariates
The primary outcome was the hemostatic profile by TEG (ACT, angle, MA, and LY30). Secondary outcomes included ventilator- and ICU-free days, clinical VTE, and mortality.(24) While guidance protocols exist for both, timing of extubation and ICU discharge was determined by the providing team. According to the guidelines by the American College of Chest Physicians our institution reserves routine VTE surveillance for high-risk trauma patients (e.g. pelvic factures and head injuries).(25)
Statistical analysis
Univariate analysis was conducted using t-tests, Wilcoxon tests, ANOVA or Kruskal-Wallis for numeric variables depending on whether the variable was normally distributed or skewed. Chi-square and Fisher exact tests were used for categorical variables. Multivariate analysis was conducted using logistic regression, with risk expressed with odds ratios (95% confidence intervals) for dichotomous outcomes and multinomial logistic regression for outcomes with greater than 2 categories (e.g. fibrinolysis). Model performance was assessed with AUROC (95%CI) for logistic regression models and with deviance and Pearson goodness of fit tests (for which higher p-values indicate better fit) for multinomial models. Effect modification by BMI30 on trauma-induced coagulopathy (TIC) indicators was tested by including interactions between TIC indicators and BMI30 into logistic regression models of death and VTE.
Results
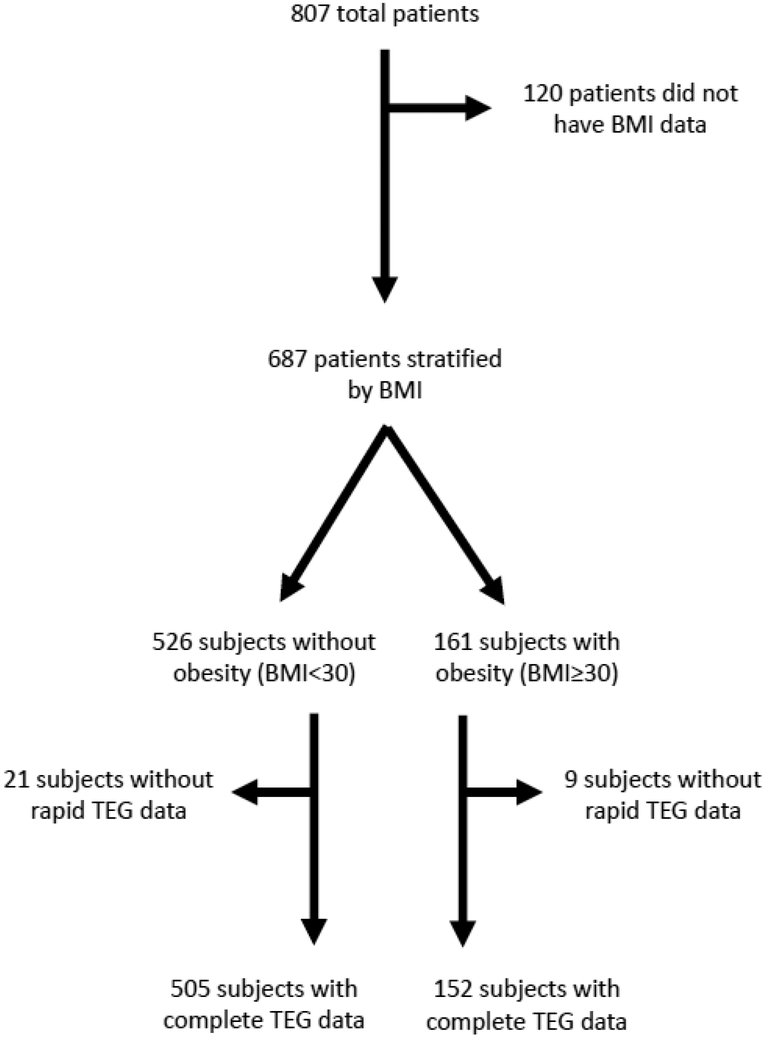
A total of 687 (85%) patients out of 807 consecutive patients had available data on BMI and were included, of whom 161 (23%) had BMI ≥30 kg/m2 (BMI30). Patients with and without BMI data did not differ regarding the outcomes or variables of interest suggesting data were missing at random. A consort diagram detailing patient exclusions can be found in Figure 1. The characteristics and outcomes of the study sample for subjects with and without BMI≥ 30 kg/m2 are shown in Table 1. The BMI30 group had a lower proportion of men and of blunt trauma, was less severely injured (lower new injury severity score, NISS) and had a higher Glasgow Coma Scale (GCS). There were no significant differences in hospital arrival systolic blood pressure (SBP), base deficit, hemoglobin, or platelet count. The BMI30 group had shorter, albeit not statistically different, prothrombin time/International Normalized Ratio (INR) and partial thromboplastin time (PTT) (Table 2). However, no difference was seen with the proportion of patients with INR > 1.3 or PTT > 35sec.
Figure 1:
CONSORT Diagram
Table 1:
Study sample characteristics stratified by BMI. Data presented as median (25–75 interquartile range) or sample size (%) as appropriate.
| BMI< 30 kg/m2 | BMI ≥ 30 kg/m2 | P value * | |
|---|---|---|---|
| Demographics | |||
| Age (Years) | 33.4 (25.5 – 48.6) | 38.0 (27.2 – 50.1) | 0.08 |
| Male (%) | 432 (82) | 121 (75) | 0.04 |
| Blunt mechanism (%) | 306 (58) | 82 (50) | 0.01 |
| NISS | 22.0 (11 – 34.0) | 18.0 (9.0 – 32.0) | 0.1 |
| Arrival GCS | 14.0 (6.5 – 15.0) | 15.0 (9.0 – 15.0) | < 0.01 |
| Severe TBI** | 146 (28%) | 26 (16%) | < 0.01 |
| Physiology upon hospital arrival | |||
| SBP (mmHg) | 117 (91 – 140) | 116 (90 – 140) | 0.52 |
| Base Deficit (mEq/L) | 6.8 (4 – 10) | 6.9 (3.6 – 10) | 0.99 |
| Hemoglobin (g/dL) | 13.9 (12.4 – 15.2) | 13.8 (12.6 – 15.5) | 0.50 |
| Platelet count (1,000/dL) | 250 (201 – 305) | 258 (217 – 305) | 0.13 |
| Transfusions within 24 hours postinjury | |||
| Required RBC (%) | 204 (39%) | 69 (43%) | 0.37 |
| Required plasma (%) | 199 (38) | 67 (42) | 0.41 |
| Required platelet transfusion (%) | 108 (21) | 29 (18) | 0.47 |
| Required cryoprecipitate (%) | 53 (10) | 17 (11) | 0.87 |
| Outcomes | |||
| Venous Thromboembolic Events | 17 (3.2) | 8 (5.0) | 0.31 |
| Deep Venous Thrombosis (%) | 11 (2.1) | 3 (1.9) | 0.85 |
| Pulmonary Embolus (%) | 6 (1.2%) | 5 (3.1%) | 0.08 |
| Deaths (%) | 45 (8.6) | 13 (8.1) | 0.84 |
| ICU Days | 3 (1 – 7) | 3 (1.5 – 6) | 0.98 |
| Ventilator Days | 1 (0 – 4) | 1 (0 – 3) | 0.98 |
| ICU free days | 23 (4.5 – 26) | 23 (13 – 25) | 0.84 |
| Ventilator free days | 26 (11 – 28) | 26 (18 – 28) | 0.88 |
TBI – traumatic brain injury, BMI – body mass index, NISS – New Injury Severity Score, GCS – Glasgow Coma Scale, SBP – Systolic Blood pressure, RBC – red blood cell units, ICU – intensive care unit.
Wilcoxon test
Severe TBI defined as AIS head > 2
Table 2:
Differences in coagulation measurements between subjects with BMI ≥ 30 kg/m2 and BMI < 30 kg/m2 following injury. Data presented as median (25–75 interquartile range) or sample size (%) as appropriate.
| BMI< 30 kg/m2 | BMI ≥ 30 kg/m2 | P value * | |
|---|---|---|---|
| INR | 1.12 (1.03 – 1.25) | 1.08 (1.01 – 1.21) | 0.08 |
| INR>1.3 (%) | 99 (19) | 25 (16) | 0.91 |
| PTT | 27.2 (24.4 – 31.0) | 26.3 (24.0 – 30.0) | 0.13 |
| PTT > 35 | 76 (15) | 24 (15) | 0.92 |
| ACT (seconds) | 121 (113 – 128) | 121 (113 – 128) | 0.60 |
| ACT <128 seconds | 197 (39) | 51 (34) | 0.22 |
| MA (mm) | 62.5 (56.8 – 66.3) | 66.0 (61.0 – 69.4) | <0.01 |
| MA<55 mm (%) | 92 (18) | 9 (6) | <0.01 |
| Angle (degrees) | 72.2 (66.7 – 75.7) | 74.3 (67.8 – 77.7) | <0.01 |
| Angle<65 degrees (%) | 94 (19) | 15 (10) | 0.01 |
| LY30 (%) | 1.8 (0.9 – 3.0) | 1.7 (0.5 – 2.9) | 0.17 |
| Fibrinolysis shutdown (LY30<0.6%) (%) | 63 (14) | 31 (23) | 0.01 |
| Physiologic fibrinolysis | 344 (77) | 99 (74) | 0.44 |
| (LY30 0.6–7.6%) (%) | |||
| Hyperfibrinolysis (LY30>7.7%) (%) | 39 (9) | 4 (3) | 0.03 |
| Functional fibrinogen (mg/dL) | 410(347–475) | 452 (383 – 502) | <0.01 |
| Functional fibrinogen <356mg/dL (%) | 141 (29) | 27 (18) | <0.01 |
BMI- Body Mass Index - INR – International Normalized Ratio, PTT – Partial Thromboplastin Time, ACT – Activated clotting time, MA – Maximal Amplitude, LY30 – lysis 30 minutes after MA
Thrombelastography (TEG)
The TEG phenotypes of the two groups differed in several ways, with the BMI30 group having a higher median angle and MA and a lower proportion with a diminished angle (< 65°) and MA (< 55 mm) (Table 2). The two groups did not differ in ACT, and this lack of difference persisted after adjustment for confounders (age, sex, blunt mechanism, NISS, SBP and GCS, Table 3). Similarly, after adjustment for confounders, there was no association between BMI30 and angle< 65°; however, the BMI30 group was significantly less likely to have a low MA. The BMI30 group also had a higher median functional fibrinogen and a lower proportion with hypofibrinogenemia; although, this difference did not persist after adjustment for confounders.
Table 3:
Independent Effect of BMI>30 kg/m2 on thrombelastography (TEG) values
| Dependent variable | Adjusted Odds Ratios (95% confidence interval) | Model performance *** |
|---|---|---|
| ACT>128 (seconds) | 0.95 (0.60 – 1.51) | 0.62 (0.57 – 0.68) |
| MA<55 (mm) | 0.28 (0.13 – 0.60) | 0.74 (0.69 – 0.79) |
| Angle<65 (degrees) | 0.57 (0.30 – 1.05) | 0.73 (0.68 – 0.78) |
| FLEV<365 (mg/dL) | 0.63 (0.39 – 1.02) | 0.74 (0.70 – 0.78) |
| Hyperfibrinolysis (LY30>7.7%) ** | 0.31 (0.10 – 0.97) | Pearson Goodness of fit = 0.72 * |
| Fibrinolysis shutdown (LY30<0.6%) ** | 1.82 (1.09 – 3.05) |
All models adjusted for age, sex, blunt mechanism, New Injury Severity Score, arrival systolic blood pressure and Glasgow Coma Scale.
higher p-values indicate better fit;
Compared to physiologic fibrinolysis;
Area under the receiver-operating characteristics curve (AUROC) with 95% CI unless otherwise indicated ACT – Activated Clotting Time, MA – Maximal Amplitude, LY30- lysis 30 minutes after MA FLEV – Functional Fibrinogen Level.
The BMI30 group had a significantly higher proportion with fibrinolysis shutdown and lower proportion with hyperfibrinolysis (Table 2). After adjustment for the aforementioned confounders, BMI30 remained significantly associated with a higher likelihood of fibrinolysis shutdown and was protective against hyperfibrinolysis (Table 3).
Outcomes
There were no significant differences between groups in the rate of VTE, length of stay, ventilator free days, or ICU free days (Table 1). After adjustment for confounders, BMI30 was not associated with VTE or death (p=0.10 and p=0.71 respectively, both AUROCs>0.70). Interactions between BMI and TEG abnormal values in logistic regression models for death and VTE (adjusted for the confounders) were all non-significant (p>0.05), suggesting no effect modification, although a type 2 error could not be ruled out.
Discussion
Our study aimed to evaluate the contribution of obesity to the frequency of trauma-induced coagulopathy and fibrinolysis phenotypes following injury. There is limited data describing how fibrinolysis phenotypes are altered by the presence of obesity. Similar to prior studies by Kornblith et al., we found that BMI30 provided a protective effect against trauma-induced coagulopathy with less frequent diminished clot formation and low clot strength. Furthermore, BMI30 was significantly associated with a higher risk of fibrinolysis shutdown and with a lower risk of hyperfibrinolysis. This, however, did not translate to significant differences in thrombotic events such as VTEs or to worse outcomes such as decreased ICU free days or increased mortality.
The association of obesity with increased incidence of fibrinolytic shutdown and decreased incidence of hyperfibrinolysis following trauma is congruent with the mechanistic studies evaluating obesity’s effects on fibrinolysis. Obesity has been linked to an increased rate of VTE events in several studies.(8, 26–28) This risk has been attributed to an increased circulating level of PAI-1. PAI-1, a potent inhibitor of fibrinolysis, is increased in visceral adipose tissue, and subsequently subjects with obesity have higher levels of plasma-based PAI-1.(18, 29, 30). In contrast, hemorrhagic shock triggers a release of tissue plasminogen activator (tPA) stimulating a fibrinolytic response.(31, 32) However, it is likely that trauma patients with obesity have a higher capacity to counteract this hyperfibrinolytic response to hemorrhagic shock. While Kornblith et al. did not identify a correlation with BMI and fibrinolysis, by stratifying by fibrinolytic phenotypes (e.g. fibrinolytic shutdown or hyperfibrinolysis), we found that obesity alters a patient’s propensity for fibrinolytic shutdown.(12)
Our work further supports the findings of prior studies that obesity invokes a protective effect against trauma-induced coagulopathy. Previous work has shown that in animal models of trauma and human cohorts, obesity prevents prolongation of clot initiation, enhances fibrin cross-linking, and promotes clot strength following hemorrhagic shock. (12, 33) Several studies have also shown an interaction with obesity and platelet activity due to alterations in several pathways that invoke platelet activation.(34) Leptin, a signaling hormone produced by adipocytes has been shown to enhance platelet aggregation, promoting thrombosis.(35, 36) Similarly, tumor necrosis factor α (TNFα), which circulates at increased concentrations in obesity, has been shown to stimulate platelet activity as well.(37, 38) Preserved clot strength may also be due to increases in fibrin formation and cross-linking, since obesity has been associated with an increase in fibrinogen concentration and factor XII (which cross-links fibrin and enhances clot strength).(39, 40) Our finding of a protective effect of obesity against a diminished MA is consistent with previous studies. However, we failed to demonstrate an association with obesity and decreased risk of hypofibrinogenemia or altered fibrin cross-linking as demonstrated by a diminished TEG angle.
The findings in this study have several implications. First, the finding of increased clot strength in severely injured subjects with obesity suggests a more conservative platelet transfusion strategy may be appropriate in this population. Following the PROPPR trial, many trauma centers have adopted a 1:1 red blood cell to platelet transfusion strategy.(41) However, the PROPPR trial did not account for or report BMI or body weight, leaving unanswered how BMI may alter outcomes in the setting of a ratio-based platelet transfusion strategy. Furthermore, the association with obesity and clot strength may enhance the risk of VTEs. Although we did not identify differences in VTE rates, other studies have found an association with increased clot strength an VTE formation in trauma and non-trauma cohorts.(42, 43)
Interestingly, we did not identify an association with obesity and increased clot formation or functional fibrinogen. Several studies examining coagulation changes due to obesity in a non-trauma population have found an association with obesity and a higher fibrinogen level.(16, 40, 44) Similarly, our group recently published a prospective study comparing a healthy control group to an un-injured cohort with severe obesity, and we found the cohort with obesity had a significantly higher TEG angle and MA compared to controls, and this persisted six months after bariatric surgery.(45) One possible explanation is that we controlled for the presence of TBI. Our group previously published an association with severe TBI and a diminished angle and decreased fibrinogen.(46) By adjusting for TBI, we likely lost any association between obesity and alterations in these two variables.
This study has several limitations. First, as obesity frequently increases the risk of several comorbidities including hypertension, hypercholesterolemia, and type 2 diabetes mellitus, it is possible that a related disease process that accompanies obesity is the true underlying cause for these findings. However, several studies, including work by this group have shown that obesity, independent of other comorbidities is associated with a hypercoagulable state. (47–49) Also, we may be underestimating the effect of obesity on fibrinolysis in treating obesity as a categorical variable, instead of evaluating BMI as a continuous variable. It is possible that changes in fibrinolysis in response to weight gain occur in linear fashion with diminished fibrinolysis with any increase in BMI. Lastly, at our center, routine surveillance for venous thrombosis is only done for high risk patients and at the discretion of the attending physician. As a result, the true incidence of VTEs may be underreported. This resulted in a lack of power for assessing differences in VTEs and could account for the lack of a difference seen between the two groups.
Conclusion
This study further supports obesity’s protective effect against trauma-induced coagulopathy. Importantly, we found that obesity is associated with an increased risk of fibrinolytic shutdown and decreased risk of hyperfibrinolysis.
Acknowledgments:
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health (T32 GM008315 and P50 GM049222), The National Heart, Lung, and Blood Institute (UM 1HL 120877) and the Department of Defense (USAMRAA, W81XWH-12-2-0028). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (or other sponsors of the project).
Financial Disclosures: The authors appreciate research support from Haemonetics with shared intellectual property.
Footnotes
Presentation history: portions of this manuscript will be presented at the 20th European Congress of Trauma and Emergency Surgery in Prague, Czech Republic, May 7th – 9th
References:
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England). 2014;384(9945):766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief. 2017(288):1–8. [PubMed] [Google Scholar]
- 3.Joseph B, Hadeed S, Haider AA, Ditillo M, Joseph A, Pandit V, Kulvatunyou N, Tang A, Latifi R, Rhee P. Obesity and trauma mortality: Sizing up the risks in motor vehicle crashes. Obes Res Clin Pract. 2017;11(1):72–8. [DOI] [PubMed] [Google Scholar]
- 4.Glance LG, Li Y, Osler TM, Mukamel DB, Dick AW. Impact of obesity on mortality and complications in trauma patients. Ann Surg. 2014;259(3):576–81. [DOI] [PubMed] [Google Scholar]
- 5.Liu T, Chen JJ, Bai XJ, Zheng GS, Gao W. The effect of obesity on outcomes in trauma patients: a meta-analysis. Injury. 2013;44(9):1145–52. [DOI] [PubMed] [Google Scholar]
- 6.Ditillo M, Pandit V, Rhee P, Aziz H, Hadeed S, Bhattacharya B, Friese RS, Davis K, Joseph B. Morbid obesity predisposes trauma patients to worse outcomes: a National Trauma Data Bank analysis. J Trauma Acute Care Surg. 2014;76(1):176–9. [DOI] [PubMed] [Google Scholar]
- 7.Samad F, Ruf W. Inflammation, obesity, and thrombosis. Blood. 2013;122(20):3415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Epidemiology Cushman M. and risk factors for venous thrombosis. Semin Hematol. 2007;44(2):62–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B, Derazne E, Tzur D, Shamis A, Vinker S, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011;364(14):1315–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stein PD, Beemath A, Olson RE. Obesity as a risk factor in venous thromboembolism. Am J Med. 2005;118(9):978–80. [DOI] [PubMed] [Google Scholar]
- 12.Kornblith LZ, Howard B, Kunitake R, Redick B, Nelson M, Cohen MJ, Callcut R. Obesity and clotting: Body mass index independently contributes to hypercoagulability after injury. J Trauma Acute Care Surg. 2015;78(1):30–6; discussion 7–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shibuya N, Frost CH, Campbell JD, Davis ML, Jupiter DC. Incidence of acute deep vein thrombosis and pulmonary embolism in foot and ankle trauma: analysis of the National Trauma Data Bank. J Foot Ankle Surg. 2012;51(1):63–8. [DOI] [PubMed] [Google Scholar]
- 14.Bell T, Stokes S, Jenkins PC, Hatcher L, Fecher AM. Prevalence of cardiovascular and respiratory complications following trauma in patients with obesity. Heart Lung. 2017;46(5):347–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. Obesity Increases Risk of Organ Failure after Severe Trauma. J Am Coll Surg. 2006;203(4):539–45. [DOI] [PubMed] [Google Scholar]
- 16.Blokhin IO, Lentz SR. Mechanisms of thrombosis in obesity. Curr Opin Hematol. 2013;20(5):437–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levi M, van der Poll T, Schultz M. Infection and inflammation as risk factors for thrombosis and atherosclerosis. Semin Thromb Hemost. 2012;38(5):506–14. [DOI] [PubMed] [Google Scholar]
- 18.Shimomura I, Funahashi T, Takahashi M, Maeda K, Kotani K, Nakamura T, Yamashita S, Miura M, Fukuda Y, Takemura K, et al. Enhanced expression of PAI-1 in visceral fat: possible contributor to vascular disease in obesity. Nat Med. 1996;2(7):800–3. [DOI] [PubMed] [Google Scholar]
- 19.Moore HB, Moore EE, Liras IN, Gonzalez E, Harvin JA, Holcomb JB, Sauaia A, Cotton BA. Acute Fibrinolysis Shutdown after Injury Occurs Frequently and Increases Mortality: A Multicenter Evaluation of 2,540 Severely Injured Patients. J Am Coll Surg. 2016;222(4):347–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6 Suppl 2:51S–209S. [PubMed] [Google Scholar]
- 21.Einersen PM, Moore EE, Chapman MP, Moore HB, Gonzalez E, Silliman CC, Banerjee A, Sauaia A. Rapid-thrombelastography (r-TEG) thresholds for goal-directed resuscitation of patients at risk for massive transfusion. J Trauma Acute Care Surg. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stettler GR, Moore EE, Moore HB, Nunns GR, Silliman CC, Banerjee A, Sauaia A. Redefining Post Injury Fibrinolysis Phenotypes Using Two Viscoelastic Assays. J Trauma Acute Care Surg. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harr JN, Moore EE, Ghasabyan A, Chin TL, Sauaia A, Banerjee A, Silliman CC. Functional fibrinogen assay indicates that fibrinogen is critical in correcting abnormal clot strength following trauma. Shock. 2013;39(1):45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schoenfeld DA, Bernard GR, Network A. Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit Care Med. 2002;30(8):1772–7. [DOI] [PubMed] [Google Scholar]
- 25.Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, Samama CM. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e227S–e77S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hagan KA, Harrington LB, Kim J, Lindstrom S, Camargo CA Jr., Grodstein F, Kabrhel C. Adiposity throughout the life course and risk of venous thromboembolism. Thromb Res. 2018;172:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stein PD, Goldman J. Obesity and thromboembolic disease. Clin Chest Med. 2009;30(3):489–93, viii. [DOI] [PubMed] [Google Scholar]
- 28.Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation. 2008;117(1):93–102. [DOI] [PubMed] [Google Scholar]
- 29.Alessi MC, Nicaud V, Scroyen I, Lange C, Saut N, Fumeron F, Marre M, Lantieri O, Fontaine-Bisson B, Juhan-Vague I, et al. Association of vitronectin and plasminogen activator inhibitor-1 levels with the risk of metabolic syndrome and type 2 diabetes mellitus. Results from the D.E.S.I.R. prospective cohort. Thromb Haemost. 2011;106(3):416–22. [DOI] [PubMed] [Google Scholar]
- 30.Singh A, Foster GD, Gunawardana J, McCoy TA, Nguyen T, Vander Veur S, Komaroff E, Rao AK. Elevated circulating tissue factor procoagulant activity, factor VII, and plasminogen activator inhibitor-1 in childhood obesity: evidence of a procoagulant state. Br J Haematol. 2012;158(4):523–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cardenas JC, Matijevic N, Baer LA, Holcomb JB, Cotton BA, Wade CE. Elevated tissue plasminogen activator and reduced plasminogen activator inhibitor promote hyperfibrinolysis in trauma patients. Shock. 2014;41(6):514–21. [DOI] [PubMed] [Google Scholar]
- 32.Chapman MP, Moore EE, Moore HB, Gonzalez E, Gamboni F, Chandler JG, Mitra S, Ghasabyan A, Chin TL, Sauaia A, et al. Overwhelming tPA release, not PAI-1 degradation, is responsible for hyperfibrinolysis in severely injured trauma patients. J Trauma Acute Care Surg. 2016;80(1):16–23; discussion −5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCully BH, Dean RK, McCully SP, Schreiber MA. Diet-induced obesity prevents the development of acute traumatic coagulopathy. J Trauma Acute Care Surg. 2014;77(6):873–7; discussion 8. [DOI] [PubMed] [Google Scholar]
- 34.Santilli F, Vazzana N, Liani R, Guagnano MT, Davi G. Platelet activation in obesity and metabolic syndrome. Obes Rev. 2012;13(1):27–42. [DOI] [PubMed] [Google Scholar]
- 35.Nakata M, Yada T, Soejima N, Maruyama I. Leptin promotes aggregation of human platelets via the long form of its receptor. Diabetes. 1999;48(2):426–9. [DOI] [PubMed] [Google Scholar]
- 36.Bodary PF, Westrick RJ, Wickenheiser KJ, Shen Y, Eitzman DT. Effect of leptin on arterial thrombosis following vascular injury in mice. JAMA. 2002;287(13):1706–9. [DOI] [PubMed] [Google Scholar]
- 37.Pignatelli P, De Biase L, Lenti L, Tocci G, Brunelli A, Cangemi R, Riondino S, Grego S, Volpe M, Violi F. Tumor necrosis factor-alpha as trigger of platelet activation in patients with heart failure. Blood. 2005;106(6):1992–4. [DOI] [PubMed] [Google Scholar]
- 38.Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259(5091):87–91. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen XM, Lane J, Smith BR, Nguyen NT. Changes in inflammatory biomarkers across weight classes in a representative US population: a link between obesity and inflammation. J Gastrointest Surg. 2009;13(7):1205–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaye SM, Pietilainen KH, Kotronen A, Joutsi-Korhonen L, Kaprio J, Yki-Jarvinen H, Silveira A, Hamsten A, Lassila R, Rissanen A. Obesity-related derangements of coagulation and fibrinolysis: a study of obesity-discordant monozygotic twin pairs. Obesity (Silver Spring). 2012;20(1):88–94. [DOI] [PubMed] [Google Scholar]
- 41.Holcomb JB, del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, Alarcon LH, Bai Y, Brasel KJ, Bulger EM, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148(2):127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allen CJ, Murray CR, Meizoso JP, Ray JJ, Teisch LF, Ruiz XD, Hanna MM, Guarch GA, Manning RJ, Livingstone AS, et al. Coagulation Profile Changes Due to Thromboprophylaxis and Platelets in Trauma Patients at High-Risk for Venous Thromboembolism. Am Surg 2015;81(7):663–8. [PubMed] [Google Scholar]
- 43.Hincker A, Feit J, Sladen RN, Wagener G. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014;18(5):549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ditschuneit HH, Flechtner-Mors M, Adler G. Fibrinogen in obesity before and after weight reduction. Obes Res. 1995;3(1):43–8. [DOI] [PubMed] [Google Scholar]
- 45.Samuels J, Lawson PJ, Morton AP, Moore HB, Hansen KC, Sauaia A, Schoen JA. Prospective Assessment of Fibrinolysis in Morbid Obesity: Tissue Plasminogen Activator Resistance Improves Following Bariatric Surgery. Surg Obes Relat Dis. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Samuels JM, Moore EE, Silliman CC, Banerjee A, Cohen MJ, Ghasabyan A, Chandler J, Coleman JR, Sauaia A. Severe traumatic brain injury is associated with a unique coagulopathy phenotype. J Trauma Acute Care Surg. 2019;86(4):686–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kupcinskiene K, Trepenaitis D, Petereit R, Kupcinskas J, Gudaityte R, Maleckas A, Macas A. Monitoring of Hypercoagulability by Thromboelastography in Bariatric Surgery. Med Sci Monit. 2017;23:1819–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tuovila M, Erkinaro T, Koivukangas V, Savolainen ER, Laurila P, Ohtonen P, Ala-Kokko T. Thromboelastography Values Remain Hypercoagulative 6 Months After Obesity Surgery: a Pilot Study. Obes Surg. 2018;28(12):3943–9. [DOI] [PubMed] [Google Scholar]
- 49.Pivalizza EG, Pivalizza PJ, Weavind LM. Perioperative thromboelastography and sonoclot analysis in morbidly obese patients. Can J Anaesth. 1997;44(9):942–5. [DOI] [PubMed] [Google Scholar]