Abstract
Background:
Despite lower socioeconomic status, Hispanics in the US paradoxically maintain equal or higher average survival rates compared to non-Hispanic Whites (NHW).
Methods:
We used multivariable Cox regression to assess whether this ‘Hispanic paradox’ applies to patients with liver cirrhosis using a retrospective cohort of 20,121 patients in a Chicago-wide electronic health record database.
Results:
Our study population included, 3,279 (16%) Hispanics, 9,150 (45%) NHW, 4,432 (22%) African Americans, 529 (3%) Asians and 2,731 (14%) comprised other races/ethnic groups. Compared to Hispanics, NHW (HR 1.26 95% CI 1.16–1.37), African American (HR 1.26 95%CI 1.15–1.39) and other races/ethnic groups (HR 1.55 95%CI 1.40–1.71) had an increased risk of death despite adjustment for age, sex, insurance status, etiology of cirrhosis, and co-morbidities. On stratified analyses, a mortality advantage for Hispanics compared to NHW was seen for alcohol cirrhosis (HR for NHW 1.35 95%CI 1.19–1.52), Hepatitis B (HR for NHW 1.35 95%CI 0.98–1.87), Hepatitis C (HR for NHW 1.21 95%CI 1.06–1.38), and NASH (HR for NHW 1.14 95%CI 0.94–1.39). There was no advantage associated with Hispanic race over NHW in cases of hepatocellular carcinoma or cholestatic liver disease.
Conclusions:
Hispanic patients with cirrhosis experience a survival advantage over many other racial groups despite adjustment for multiple covariates.
Introduction
Racial and ethnic disparities in healthcare outcomes in the United States (US) remain an important public health concern as the population becomes more diverse.1 Despite low socioeconomic status--a well-established risk factor for all-cause mortality--Hispanics in the US maintain similar or better age-adjusted all-cause mortality rates compared to non-Hispanic whites (NHW), a finding that has been termed the “Hispanic Paradox”.2–4 The extent to which this ‘paradox’ affects outcomes in liver disease has not been examined despite an increased burden of liver disease in the Hispanic population.5
Some researchers have argued that the Hispanic paradox can be explained by selection bias, confounding, or artifacts in data collection such as ascertainment of death.6 Despite these concerns, it is generally accepted that for some health conditions such as cardiovascular disease, there is strong evidence of a survival advantage for Hispanics compared to NHW independent of socioeconomic status.7,8 In a meta-analysis of 58 longitudinal studies, Ruiz et al found that Hispanic patients had a significant 17.5% mortality advantage for Hispanics over NHW in overall mortality, cardiovascular disease and renal disease.7
In contrast, Hispanics with liver cirrhosis have increased prevalence, higher disease severity, and worse outcomes compared to NHW with cirrhosis on unadjusted analyses.5 Based on national vital statistics data published by the Centers of Disease Control and Prevention (CDC), in 2010 the age-adjusted mortality rate from chronic liver disease and cirrhosis for Hispanics in the US was 13.7 per year per 100,000 Hispanics persons compared to 9.4 per year per 100,000 among NHW.9 Additionally, Hispanics have a higher prevalence of chronic alcoholic liver disease, incidence of hepatocellular carcinoma, and higher mortality from hepatitis B and C infection.10–12 Non alcoholic fatty liver disease NAFLD and NASH is more common in Hispanics as well.13,14 Despite the above, there have been no large studies to determine whether Hispanics with liver disease have a survival advantage compared to NHW largely due to lack of large data sources to address this question.
As an alternative to prospective cohorts or national vital statistics data, aggregated electronic health record data (EHR) data can be used to assemble retrospective cohorts of patients with liver disease and are increasingly being used successfully for clinical research.15,16 In this study we examine whether Hispanics with liver cirrhosis have a survival advantage compared to NHW and other racial/ethnic groups using the HealthLNK database, an aggregation of EHR data from 6 institutions serving the greater metropolitan Chicago area. Previous studies using HealthLNK data have been published addressing a wide range of research questions including this group’s previous work on a cohort of patients with liver cirrhosis.17–20
Materials and Methods
Data Sources
Data sources comprised of the HealthLNK database, Organ Procurement and Transplantation Network (OPTN) database and the Social Security Death Master File.20,21 Databases were merged together using patient identifiers (last name, first name, date of birth and social security number) then de-identified prior to analysis.
The HealthLNK Data Repository is an assembly of EHR data from six healthcare institutions comprising ≈42% of the total inpatient beds in Chicago, IL. These institutions include five major academic healthcare centers: Northwestern Medicine, University of Chicago Hospitals and Clinic, Rush University Medical Center, University of Illinois at Chicago Medical Center, and Loyola University Medical Center; and one large county health system, Cook County Health and Hospitals System.22 HealthLNK contains data from ≈2.95 million unique patients and spans healthcare encounters occurring between January 1, 2006 and December 31, 2012. For included patients, we abstracted demographics, procedure codes, medications, laboratory measurements, vital signs, and diagnostic codes from inpatient, outpatient, and emergency department encounters.22 The OPTN database comprises national registry data of all patients waitlisted for organ transplantation in the US as well as post transplant data.20 The Social Security Death Master File contains over 83 million records of deaths that have been reported to Social Security Administration in the US.21
Study Population and Study Variables.
After approval by the Northwestern University Institutional Review Board, cirrhosis patients were identified and included if they were ≥18 years of age and had one of three cirrhosis Ninth Revision of International Classification of Diseases and Health Related Problems (ICD-9) codes (571.2, 571.5, or 571.6) similar to previous studies.23–25
Race and ethnicity were abstracted from the medical record from the earliest encounter with a participating healthcare institution. They were combined into a single covariate “race” comprised of: Hispanic, NHW, African American, and Asian. Patients with missing data or who did not identify one of the above races (<2%) were added to an ‘other’ category.
Covariates related to the underlying cause of a patient’s cirrhosis were defined using ICD-9 codes as follows: Alcoholic cirrhosis (ICD-9 571.0, 571.1, 571.2 or 571.3); Hepatitis C (ICD9 070.41, 070.44, 070.51, 070.54, 070.70, 070.71, or V02.62); NASH (ICD-9 571.8 or 571.9) and Hepatitis B (ICD-9 070.20, 070.21, 070.22, 070.23, 070.30, 070.31, 070.32, 070.33, 070.42, or V02.61). Hepatocellular carcinoma was defined by ICD-9 code 155.00 or common procedural terminology codes 37204 or 37243 or 77778 or 79445 which correspond to chemoembolization or brachytherapy. Patients were allowed to have multiple codes relating to etiology, this was adjusted for in the multivariate models (see below).
Health insurance status was considered the measure for socioeconomic status. Non liver comorbidity was defined using the Elixhauser comorbidity index, a validated tool to assess severities of comorbidities using ICD codes.26
Statistical Methods
Demographic and clinical characteristics compared using the Chi-square test, ANOVA or Kruksal Wallis test. The primary endpoint of survival analyses was all-cause mortality with time at risk was defined as time from the first inclusion ICD-9 code until death, liver transplantation or the end of the study period. Patients with prevalent cirrhosis at the start of study were not allotted additional time at risk. Similarly, transplant was not treated as a competing risk due to the rarity of transplant in this population. A competing risk analysis was performed and can be found in supplemental materials. Multivariate Cox regression was adjusted for age, sex, race, health insurance status, Elixhauser comorbidity index and etiology of cirrhosis. Analyses stratified by underlying etiology was performed. A sensitivity analysis was performed to examine if the results were altered with inclusion of maximal Model for End Stage Liver Disease (MELD) score attained during followup. This was not included into the full model given known high rates of missingness in the dataset. Patients on Coumadin were excluded from this subanalysis. For all analyses, a p-value of <0.05 was considered statistically significant. Analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC) and RStudio version 1.1.419
Results
Study Population
A total of 20,121 patients were identified with an ICD-9 code for cirrhosis between January 1, 2006 and Dec 31, 2012. Baseline clinical and demographic characteristics are summarized in Table 1. Overall 11,122 (55%) were male with a mean age at diagnosis of cirrhosis of 57±12 years. Of the entire study population, 3,279 (16%) were Hispanics, 9,150 were NHW (45%), 4,432 (22%) were African Americans, 529 (3%) were Asian and 2,731 (14%) were listed as ‘other’. At the time of cirrhosis diagnosis Hispanics were younger (mean age of 55±12) and slightly more likely to be male compared to NHW and other races (61% vs 58%). Compared to NHW, Hispanics were less likely to have private health insurance (27% vs 41%).
Table 1:
Baseline clinical and demographic characteristics
| n=20,121 | ||||||
|---|---|---|---|---|---|---|
| Variable | Hispanic N=3279 |
White N=9150 |
Black N=4432 |
Asian N=529 |
Other N=2731 |
P Value |
| Age-years | 55±12 | 58±12 | 57±11 | 58±12 | 57±12 | <.0001a |
| Male- n (%) | 2002 (61) | 5292 (58) | 2357 (53) | 318 (60) | 1153 (57) | <.0001c |
| Diagnoses present†- n (%) | ||||||
| Alcohol | 1430 (44) | 3077 (34) | 1263 (29) | 80 (15) | 792 (29) | <.0001c |
| Hepatitis C | 1160 (35) | 3325 (36) | 2509 (57) | 193 (36) | 973 (36) | <.0001c |
| NASH | 810 (25) | 2066 (22) | 792 (18) | 84 (16) | 427 (16) | <.0001c |
| Hepatitis B | 189 (6) | 477 (5) | 545 (12) | 222 (42) | 223 (8) | <.0001c |
| Hepatocellular Carcinoma | 398 (12) | 1386 (15) | 538 (12) | 131 (25) | 372 (14) | <.0001 |
| Diagnoses per patient-mean (IQR) | 1.32 (1-2) | 1.26 (1-2) | 1.35 (1-2) | 1.43 (1-2) | 1.13 (1-2) | <.0001 |
| Median Elixhauser Score-(IQR) | 3 (2-6) | 3 (1-6) | 5 (2-8) | 2 (1-5) | 1 (0-4) | <.0001b |
| Insurance- n (%) | ||||||
| Medicare/Medicaid | 1383 (42) | 4591 (50) | 2581 (58) | 193 (36) | 1298 (48) | <.0001c |
| Private Insurance | 885 (27) | 3733 (41) | 992 (22) | 165 (31) | 1095 (40) | |
| Other | 1011 (31) | 826 (9) | 859 (19) | 171 (32) | 338 (12) | |
| Deaths (%) | 760 (23) | 2624 (29) | 1376 (31) | 112 (21) | 850 (31) | <.0001c |
| Transplant (%) | 107 (3) | 609 (7) | 81 (2) | 27 (5) | 95 (4) | <.0001c |
Categories are not mutually exclusive
ANOVA
Kruksal Wallis test
Chi-square
Alcoholic cirrhosis was the most common diagnosis among Hispanics (44%) while Hepatitis C was the most common diagnosis among NHW (36%), African Americans (57%), and ‘other’ races (37%). The most common diagnosis for Asians was Hepatitis B (42%). Slightly more than one third (33.5%) of all patients had more than one etiology of cirrhosis assigned based on ICD-9 coding with 9% of all patients having more than 2 etiologies assigned.
Hepatocellular carcinoma prevalence was the same when comparing Hispanics and African Americans (12%). However, compared to Hispanics, the prevalence of hepatocellular carcinoma was higher in NHW (15%) and Asians (25%). Rates of transplant were low in all populations (4.6%), ranging from 1.8% in African Americans to 6.5% in NHW.
Multivariable Modelling
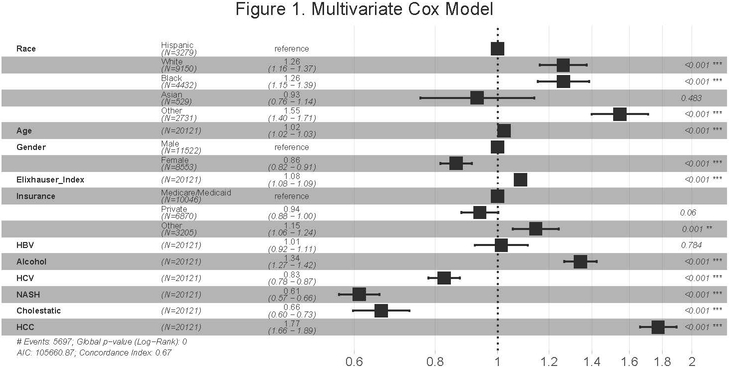
Adjusted odds ratios from the multivariable Cox model is shown in Figure 1. Hispanic race was associated with survival even after adjustment for age, sex, Elixhauser comorbidity index, insurance status, presence of HCC, and etiology of cirrhosis. Relative to Hispanics, patients who identified as NHW (aHR 1.26; 95% CI 1.16–1.37), African American (aHR 1.26; 95% CI 1.15–1.39), and ‘other’ (aHR 1.55; 95% CI 1.40–1.71) had an increased risk of death. Asians (aHR 0.93; 95% CI 0.76 – 1.14) were also noted to have a similar survival benefit as compared to NHW and ‘other’ with a trend in this direction compared to African Americans. After exclusion of patients on Coumadin, a sensitivity analysis which included maximal MELD score during the study period with the same variables above did not alter the direction or statistical significance of these relationships. Furthermore, incorporation of transplant as a competing risk did not alter these results (Figure S1-S2).
Figure 1:
The multivariable Cox model. An increased risk of death was seen among NHW, African Americans and ‘other’ races compared to Hispanic patients. Private insurance was associated with a statistically significant reduced risk of death compared to Public insurance (Medicare/Medicaid). An increasing number of non liver comorbidities as measured by Elixhauser score was also associated with an increased risk of death.
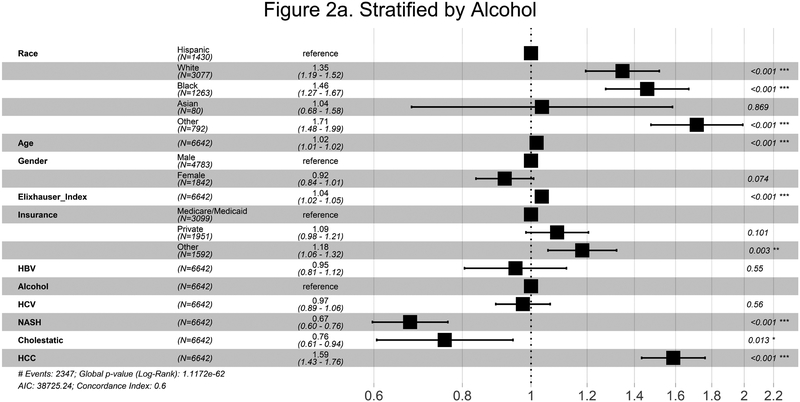
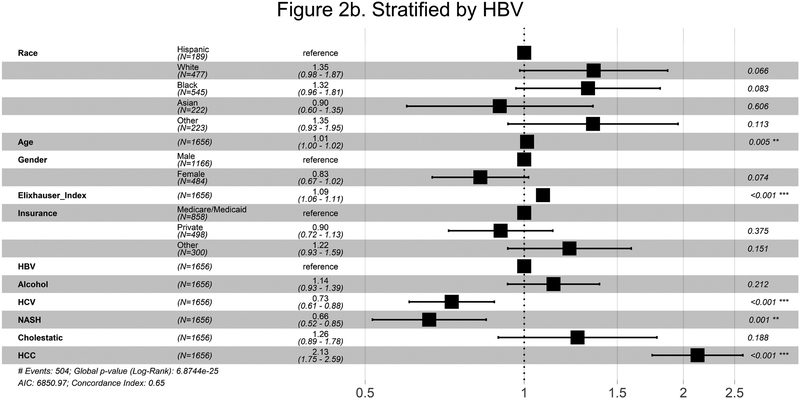
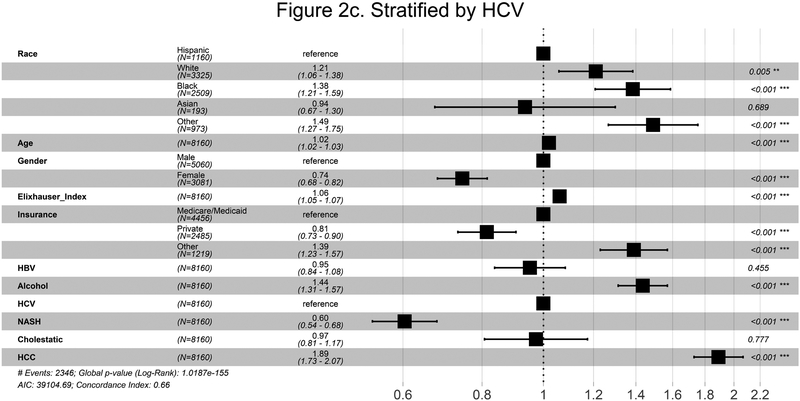
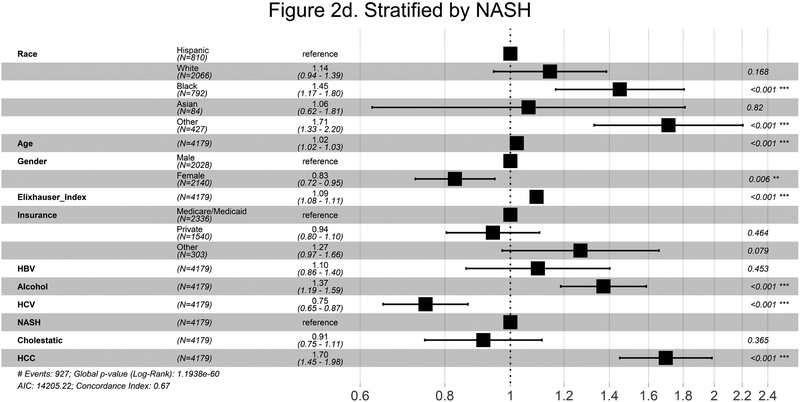
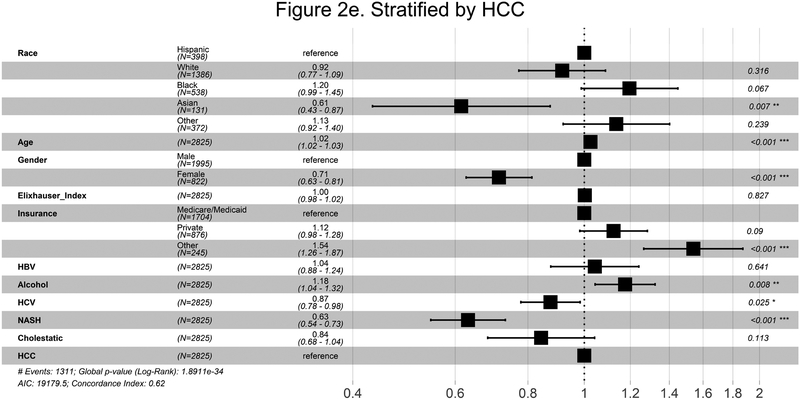
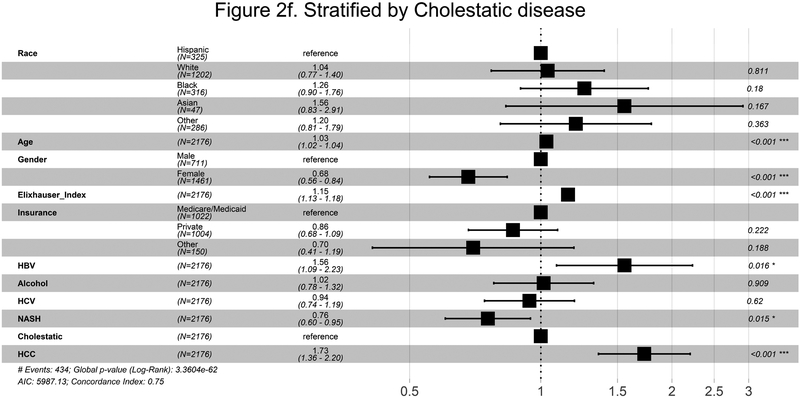
On stratified analyses, a mortality advantage for Hispanics compared to NHW was noted for multiple etiologies (Figure 2a-d). This was especially prominent in alcohol cirrhosis (HR for NHW 1.35 95%CI 1.19–1.52), and Hepatitis C (HR for NHW 1.21 95%CI 1.06–1.38). A trend towards a mortality advantage was seen in Hepatitis B (HR for NHW 1.35 95%CI 0.98–1.87) and NASH (HR for NHW 1.14 95%CI 0.94–1.39). There was no advantage associated with Hispanic race over NHW in cases of hepatocellular carcinoma or cholestatic liver disease (Figure 2e,f).
Figure 2a-f:
Summary survival of race stratified by underlying cause of liver cirrhosis or presence of hepatocellular carcinoma. Data were stratified by underlying cause of liver cirrhosis or presence of hepatocellular carcinoma and each model run adjusting for age, race, sex, insurance, Elixhauser score, and concurrent etiologies. Abbreviations: HBV Hepatitis B virus infection, HCV Hepatitis C virus Infection, NASH Non-Alcoholic Steatohepatitis, HCC hepatocellular carcinoma
Discussion
In this study of a large and diverse metropolitan population, we demonstrated that despite a lower socioeconomic status (as evidenced by public insurance status) Hispanic race appears to be associated with a survival advantage in cirrhosis even after adjustment for multiple confounders. This paradoxical advantage was observed in nearly all underlying etiologies except for hepatocellular carcinoma and cholestatic liver disease. These results are in contrast to national vital statistics data or longitudinal studies with a healthy study population at baseline which typically show worse unadjusted outcomes for Hispanic patients.
Several theories have been proposed to explain the paradoxical survival advantage Hispanics experience. These include: 1) the ‘Healthy migrant’ theory which proposes that migrants to the US constitute a population of healthier individuals27,28; 2) the ‘Salmon bias’ theory which posits that Hispanics with chronic disease may be more likely to migrate back to their origin country for familial support28; and 3) socio-cultural factors which result in different lifestyle choices or strong familial structure.28 None of the proposed justifications for the Hispanic paradox are entirely explanatory and it is currently thought that reasons for the paradox are likely multifactorial.6 In our study, patients who identified as Hispanic were more likely to have alcohol as a contributing factor to their liver disease. It is possible that more robust social support and the known hepatic recovery potential in the setting of alcohol abstinence may contribute to this associated benefit.
Our study also demonstrated a survival benefit associated with Hispanic race in certain subcategories of liver disease. In fact, the only two diagnosis groups that did not appear to be associated with a benefit were HCC and cholestatic liver disease. Although causality cannot be ascertained from our study design, given the high hazard of death associated with HCC and the low hazard of death associated with cholestatic liver disease in the full model (Figure 1), it is possible that the beneficial association noted with Hispanic race is insufficient to change the clinical course. With regard to hepatocellular carcinoma, previous studies have reported poorer outcomes for Hispanics compared to NHW. Alkhalili et al found that Hispanics with hepatocellular carcinoma had worse overall survival in a population of patients from New Mexico.29 In that study, Hispanics presented with more advanced liver disease and were less likely to receive less invasive, interventional radiology treatment. Our results also suggest that public health interventions and resources for Hispanics with liver disease could preferentially target hepatocellular carcinoma.30 For example Singhal and colleagues demonstrated in a randomized controlled trial that a dedicated outreach program increased ultrasound screening of patients with cirrhosis for hepatocellular carcinoma especially among Hispanics.31 Although the stratified analysis of patients with HBV did reveal a similar point estimate suggesting a benefit to Hispanic patients compared to NHW, the lack of significance in this case is likely due to the relatively low numbers of patients rather than a false result.
The notion than Hispanics are disproportionately affected by non alcoholic fatty liver disease and NASH is well documented.13,14,32,33 This finding is thought to be related to a high frequency of a unique polymorphism in the gene encoding the enzyme adiponutrin associated with fat deposition in the liver.34 Given rising levels of obesity and new anti-viral agents for hepatitis C, NASH cirrhosis is expected to emerge as a top cause of cirrhosis in the coming decades.5,14,35 In our cohort the proportionate difference between Hispanics and NHW with NASH was significant but not excessively large (25% vs 22%, p<0.05) however true prevalence estimation are not statistically appropriate given the administrative nature of HealthLNK. This predilection towards NASH may explain our lack of significant in the stratified analysis compared to other etiologies.
Besides our intended examination of Hispanic patients, we noted several other protective effects specifically among Asian patients and female patients. It can be argued that many Asian patients may benefit from the same sociocultural factors mentioned above. Additionally, in our population Asian patients had high rates of hepatitis B and hepatocellular carcinoma compared to the other groups. Although not statistically significant, Asians had a trend towards lower biologic MELD score during follow up. Lastly, our ‘HCC’ group was defined as not only an ICD code but also a procedure code. All of these facts may generate a bias in our ‘HCC’ group towards patients who have early disease and are undergoing treatment. In fact, the Asian group had the lowest rate of Medicare/Medicaid which may suggest more affluent socio-economic status. Furthermore, Asian patients one of the highest rates of transplant (Table 1, Figure S1b). Taken together, higher rates of hepatitis B and higher socio-economic status may lend itself to more frequent screening and earlier detection of hepatocellular carcinoma resulting in better outcomes or earlier transplantation.
An explanation for the survival benefit noted among female patients is less clear. This finding is surprising in that recent data has suggested that female patients have longer wait times for transplant and potentially higher mortality on the waitlist due to disproportionate MELD score reduction related to lower serum creatinine.36,37 We posit that divergence of our findings from other studies is due to our cohort representing the general population of patients with cirrhosis. This is in contrast to most studies that are done in a wait-list setting or using national transplant databases as these studies have some component of inherent referral and selection bias.
Unfortunately, the same traits that improve generalizability bring limitations to our study. For example, given that patients were not necessarily seen by specialists, lab testing that would allow for calculation of a MELD score were highly missing preventing routine adjustment in our analysis. We used maximal MELD score attained during followup to attempt to catch significant hepatic decompensation and did not see a difference in our results. Furthermore, to limit confounding we adjusted for non liver comorbidities using the Elixhauser score which has been well validated in other analyses.26
Given the retrospective nature of this cohort selection, information, and confounding bias cannot be completely eliminated.38 With regards to selection, patients were included based on the presence of ICD-9 codes for cirrhosis at one of six large academic hospitals in Chicago. Although these centers account for all the major liver referral centers and around 42% of all inpatient beds in the city, patients may not have been included due to geographic and socioeconomic factors limiting access.
With regard to the study of race itself, several issues are raised. First, patients were categorized into race based on self-report. Those who identify as ‘Hispanic’ constitute a heterogeneous group of people from many cultures and traditions. The Hispanic population in the Chicago is similar to other major US cities in that it is 80% Mexican which is also the largest Hispanic subgroup in the US in general.39 Thus although we feel that our Hispanic cohort is relatively uniform our dataset is not granular enough to verify our cohort’s heritage to this level. Furthermore, there were a significant amount of patients who identified as ‘other’. Although this simulates our ever mixing diverse population, it is difficult to interpret the associated finding of increased adjusted mortality in this group. Second, racial disparity in access to liver transplantation has been reported which may affect our endpoint of survival.40 We did not perform a competing risk analysis as the very low rate of transplantation our cohort would suggest that this effect is minimal. Third, our study included all patients treated at our Chicago centers regardless of citizenship status, however ascertainment of death from Social Security records relies on citizenship. Although Hispanic patients may be more likely to be undocumented, when this was studied race related ascertainment bias was not found in Social Security death records.41
In conclusion, contrary to previous reports, Hispanics with liver cirrhosis do experience a survival advantage relative to NHW however, this advantage was not seen in cholestatic cirrhosis or HCC. Further research is needed to unveil the mechanism of this positive association so that it might potentially benefit other patients with the same disease.
Supplementary Material
Acknowledgments
Funding: Dr. Atiemo and Mazumder were supported by NIH grant T32DK077662 PI MM Abecassis. Dr VanWagner is supported by NIH grant K23 HL136891.
Abbreviations
- CDC
Centers of Disease Control and Prevention
- EHR
Electronic health record
- ICD-9
International Classification of Diseases and Health Related Problems
- NHW
Non-Hispanic Whites
- OPTN
Organ Procurement and Transplantation Network
- US
United States
Footnotes
Disclosures: The authors declare no conflicts of interest
References
- 1.U.S. Department of Health and Human Services. Healthy People 2020. Available at https://www.healthypeople.gov. Published 2014. Accessed March 1, 2019.
- 2.Rawshani A, Svensson AM, Zethelius B, et al. Association Between Socioeconomic Status and Mortality, Cardiovascular Disease, and Cancer in Patients With Type 2 Diabetes. JAMA Intern Med. 2016;176(8):1146–1154. [DOI] [PubMed] [Google Scholar]
- 3.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- 4.Patel KV, Eschbach K, Ray LA, et al. Evaluation of mortality data for older Mexican Americans: implications for the Hispanic paradox. Am J Epidemiol. 2004;159(7):707–715. [DOI] [PubMed] [Google Scholar]
- 5.Carrion AF, Ghanta R, Carrasquillo O, et al. Chronic liver disease in the Hispanic population of the United States. Clin Gastroenterol Hepatol. 2011;9(10):834–e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- 7.Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health. 2013;103(3):e52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cortes-Bergoderi M, Goel K, Murad MH, et al. Cardiovascular mortality in Hispanics compared to non-Hispanic whites: a systematic review and meta-analysis of the Hispanic paradox. Eur J Intern Med. 2013;24(8):791–799. [DOI] [PubMed] [Google Scholar]
- 9.Murphy S, Xu J, Kochanek KD. Deaths Final Data 2010. Natl Vital Stat Rep. 2013;61(4):80. [PubMed] [Google Scholar]
- 10.Yang AL, Vadhavkar S, Singh G, et al. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med. 2008;168(6):649–656. [DOI] [PubMed] [Google Scholar]
- 11.Division of Viral Hepatitis C. Viral Hepatitis Surveillance United States, 2012. Available at https://www.cdc.gov/hepatitis/statistics/2012surveillance/commentary.htm#hepC. Published 2012. Accessed March 1, 2019.
- 12.Altekruse SF, Henley SJ, Cucinelli JE, et al. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol. 2014;109(4):542–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Argo CK, Caldwell SH. Epidemiology and natural history of non-alcoholic steatohepatitis. Clin Liver Dis. 2009;13(4):511–531. [DOI] [PubMed] [Google Scholar]
- 14.Lazo M, Bilal U, Perez-Escamilla R. Epidemiology of NAFLD and Type 2 Diabetes: Health Disparities Among Persons of Hispanic Origin. Curr Diab Rep. 2015;15(12):116. [DOI] [PubMed] [Google Scholar]
- 15.Prokosch HU, Ganslandt T. Perspectives for medical informatics. Reusing the electronic medical record for clinical research. Methods Inf Med. 2009;48(1):38–44. [PubMed] [Google Scholar]
- 16.Jensen PB, Jensen LJ, Brunak S. Mining electronic health records: towards better research applications and clinical care. Nat Rev Genet. 2012;13(6):395–405. [DOI] [PubMed] [Google Scholar]
- 17.Jackson KL, Goel S, Kho AN, et al. Distance from hospital impacts adverse event detection after outpatient endoscopy. Gastrointest Endos. 2017;85(2):380–386. [DOI] [PubMed] [Google Scholar]
- 18.Fishman J, McLafferty S, Galanter W. Does Spatial Access to Primary Care Affect Emergency Department Utilization for Nonemergent Conditions? Health Serv Res. 2018;53(1):489–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mays JA, Jackson KL, Derby TA, et al. An Evaluation of Recurrent Diabetic Ketoacidosis, Fragmentation of Care, and Mortality Across Chicago, Illinois. Diabetes Care. 2016;39(10):1671–1676. [DOI] [PubMed] [Google Scholar]
- 20.Atiemo K, Skaro A, Maddur H, et al. Mortality Risk Factors Among Patients With Cirrhosis and a Low Model for End-Stage Liver Disease Sodium Score (≤15): An Analysis of Liver Transplant Allocation Policy Using Aggregated Electronic Health Record Data. Am J Transplant. 2017;17(9):2410–2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National technical Information Service. Social Security Death Index. Available at http://www.ntis.gov/products/ssa-dmf.aspx.
- 22.Kho AN, Cashy JP, Jackson KL, et al. Design and implementation of a privacy preserving electronic health record linkage tool in Chicago. J Am Med Inform Assoc. 2015;22(5):1072–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nehra MS, Ma Y, Clark C, et al. Use of administrative claims data for identifying patients with cirrhosis. J Clin Gastroenterol. 2013;47(5):e50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lo Re V 3rd, Lim JK, Goetz MB, et al. Validity of diagnostic codes and liver-related laboratory abnormalities to identify hepatic decompensation events in the Veterans Aging Cohort Study. Pharmacoepidemiol Drug Saf. 2011;20(7):689–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldberg DS, Lewis JD, Halpern SD, et al. Validation of a coding algorithm to identify patients with hepatocellular carcinoma in an administrative database. Pharmacoepidemiol Drug Saf. 2013;22(1):103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. [DOI] [PubMed] [Google Scholar]
- 27.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. [DOI] [PubMed] [Google Scholar]
- 28.Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, et al. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alkhalili E, Greenbaum A, Luo L, et al. Racial disparities in treatment and survival of hepatocellular carcinoma in native Americans and Hispanics. Am J Surg. 2017;214(1):100–104. [DOI] [PubMed] [Google Scholar]
- 30.Guy J, Yee HF Jr. Health disparities in liver disease: Time to take notice and take action. Hepatology. 2009;50(1):309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singal AG, Tiro JA, Marrero JA, et al. Mailed Outreach Program Increases Ultrasound Screening of Patients With Cirrhosis for Hepatocellular Carcinoma. Gastroenterology. 2017;152(3):608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol. 2006;40 Suppl 1:S5–10. [DOI] [PubMed] [Google Scholar]
- 33.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40(6):1387–1395. [DOI] [PubMed] [Google Scholar]
- 34.Rotman Y, Koh C, Zmuda JM, et al. The association of genetic variability in patatin-like phospholipase domain-containing protein 3 (PNPLA3) with histological severity of nonalcoholic fatty liver disease. Hepatology. 2010;52(3):894–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fox AN, Jacobson IM. Recent successes and noteworthy future prospects in the treatment of chronic hepatitis C. Clin Infect Dis. 2012;55 Suppl 1:S16–24. [DOI] [PubMed] [Google Scholar]
- 36.Mindikoglu AL, Regev A, Seliger SL, et al. Gender disparity in liver transplant waiting-list mortality: the importance of kidney function. Liver Transpl. 2010;16(10):1147–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cullaro G, Sarkar M, Lai JC. Sex-based disparities in delisting for being “too sick” for liver transplantation. Am J Transplant. 2018;18(5):1214–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet. 2002;359(9302):248–252. [DOI] [PubMed] [Google Scholar]
- 39.Pew Research Center. Hispanic Population and Origin in Select U.S. Metropolitan Areas, 2014. Available at http://www.pewhispanic.org/interactives/hispanic-population-in-select-u-s-metropolitan-areas. Published September 6, 2016. Accessed March 8, 2018.
- 40.Nguyen GC, Thuluvath PJ. Racial disparity in liver disease: Biological, cultural, or socioeconomic factors. Hepatology. 2008;47(3):1058–1066. [DOI] [PubMed] [Google Scholar]
- 41.Schisterman EF, Whitcomb BW. Use of the Social Security Administration Death Master File for ascertainment of mortality status. Popul Health Metr. 2004;2(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.