Abstract
Objective
To compare the efficacy and safety of first line treatments for patients with advanced epidermal growth factor receptor (EGFR) mutated non-small cell lung cancer (NSCLC).
Design
Systematic review and network meta-analysis.
Data sources
PubMed, Embase, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, and several international conference databases, from inception to 20 May 2019.
Eligibility criteria for selecting studies
Published and unpublished randomised controlled trials comparing two or more treatments in the first line setting for patients with advanced EGFR mutated NSCLC were included in a bayesian network meta-analysis. Eligible studies reported at least one of the following clinical outcome measures: progression free survival, overall survival, objective response rate, and adverse events of grade 3 or higher.
Results
18 eligible trials involved 4628 patients and 12 treatments: EGFR tyrosine kinase inhibitors (TKIs; osimertinib, dacomitinib, afatinib, erlotinib, gefitinib, and icotinib), pemetrexed based chemotherapy, pemetrexed free chemotherapy, and combination treatments (afatinib plus cetuximab, erlotinib plus bevacizumab, gefitinib plus pemetrexed based chemotherapy, and gefitinib plus pemetrexed). Consistent with gefitinib plus pemetrexed based chemotherapy (hazard ratio 0.95, 95% credible interval 0.72 to 1.24), osimertinib showed the most favourable progression free survival, with significant differences versus dacomitinib (0.74, 0.55 to 1.00), afatinib (0.52, 0.40 to 0.68), erlotinib (0.48, 0.40 to 0.57), gefitinib (0.44, 0.37 to 0.52), icotinib (0.39, 0.24 to 0.62), pemetrexed based chemotherapy (0.24, 0.17 to 0.33), pemetrexed free chemotherapy (0.16, 0.13 to 0.20), afatinib plus cetuximab (0.44, 0.28 to 0.71), and gefitinib plus pemetrexed (0.65, 0.46 to 0.92). Osimertinib and gefitinib plus pemetrexed based chemotherapy were also consistent (0.94, 0.66 to 1.35) in providing the best overall survival benefit. Combination treatments caused more toxicity in general, especially erlotinib plus bevacizumab, which caused the most adverse events of grade 3 or higher. Different toxicity spectrums were revealed for individual EGFR-TKIs. Subgroup analyses by the two most common EGFR mutation types indicated that osimertinib was associated with the best progression free survival in patients with the exon 19 deletion, and gefitinib plus pemetrexed based chemotherapy was associated with the best progression free survival in patients with the Leu858Arg mutation.
Conclusions
These results indicate that osimertinib and gefitinib plus pemetrexed based chemotherapy were associated with the best progression free survival and overall survival benefits for patients with advanced EGFR mutated NSCLC, compared with other first line treatments. The treatments resulting in the best progression free survival for patients with the exon 19 deletion and Leu858Arg mutations were osimertinib and gefitinib plus pemetrexed based chemotherapy, respectively.
Systematic review registration
PROSPERO CRD42018111954.
Introduction
Lung cancer is the leading cause of cancer related deaths worldwide, and non-small cell lung cancer (NSCLC) accounts for about 85% of overall reported cases.1 A clinically significant proportion of patients with NSCLC have epidermal growth factor receptor (EGFR) mutations, especially those who are women, never smokers, east Asians, and adenocarcinoma.2 Over the past few decades, front treatments for these patients at advanced stage have evolved from the empirical use of cytotoxic treatments to target regimens that are known as EGFR tyrosine kinase inhibitors (TKIs), owing to their clinical benefits.3 So far, multiple generation EGFR-TKIs have been developed (including erlotinib, gefitinib, and icotinib (first generation); dacomitinib and afatinib (second generation); and osimertinib (third generation)), and most of these TKIs have been established as standard first line treatments.4 However, durable responses of EGFR-TKIs remain a perennial challenge for the inevitable development of acquired resistance.5 6 7 8 Biologically synergistic combinations of EGFR-TKIs with other treatments in different mechanisms of action, including chemotherapies, monoclonal antibodies, immunotherapies, and some pathway inhibitors have been investigated as first line options to overcome resistance and prolong survival.9 With these developments, questions regarding the relative efficacy and safety between any two of the multiple first line treatments have emerged.
Furthermore, previous studies have implied that the exon 19 deletion and Leu858Arg mutations accounting for about 90% of EGFR mutations,10 11 should be considered distinct biological and clinical entities.12 13 Therefore, the ideal treatment could differ in patients stratified by these two common EGFR mutations, although this hypothesis has not yet been investigated.
Several dozen randomised controlled trials and pairwise meta-analyses using only the direct comparison model have been conducted for conclusive evidence about the comparative efficacy and safety of first line treatments for patients with advanced EGFR mutated NSCLC. However, they have been unable to address the aforementioned problems. Network meta-analysis, which synthesises evidence from direct and indirect comparisons, is therefore needed to determine the best available treatments.14 Previous network meta-analyses have only partly compared treatments for patients with advanced EGFR mutated NSCLC but they have not incorporated recent alternative treatments or available trials and have not been specific enough in regards to accurate treatment profiles for tumours with different subtype mutations.15 16 17 18 With a well designed and comparative synthesis, we performed this network meta-analysis of randomised controlled trials to investigate the relative efficacy and safety of all first line treatments in patients with advanced EGFR mutated NSCLC, and then a subgroup analysis by EGFR mutation type (exon 19 deletion and Leu858Arg mutations) to identify the best clinical choice.
Methods
This network meta-analysis was performed following the PRISMA (preferred reporting items for systematic reviews and meta-analyses) extension statement for network meta-analysis (supplementary table S1).19 Frequentist and bayesian approaches are two typical models fitting network meta-analysis. We have applied bayesian network meta-analysis for its advantages of accommodating complex situations (such as its ability to account for the effect of study specific covariates, resulting in exact estimates in the presence of limited information), and it offers a more straightforward method for conducting probabilistic statements and predictions on the treatment effects.20 The protocol was registered in the Prospective Register of Systematic Reviews (PROSPERO CRD42018111954). Institutional review board exemption was granted for the innocuousness of the review study.
Data sources and searches
We searched PubMed, Embase, the Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov databases to find relevant articles up to 20 May 2019 in all languages using a combination of the main search terms “NSCLC” and “EGFR” within the restriction limit of “randomized controlled trial.” Then, to include complete and updated outcomes, abstracts and presentations of ongoing randomised controlled trials on lung cancer from several of the most important international conferences (American Society of Clinical Oncology, European Society of Medical Oncology, European Cancer Conference, and World Conference on Lung Cancer) from 2014 to 2018 were inspected. Finally, the reference lists of the relevant articles were checked for additional articles. The detailed search strategy is presented in supplementary table S2.
Study selection
We included published and unpublished phase II/III randomised controlled trials that met the following criteria:
Trials that enrolled patients with histologically or cytologically confirmed advanced (stage III/IV/recurrent) NSCLC with EGFR activating mutations
Trials that compared any two or more different arms of first line treatments for patients with EGFR mutated NSCLC
-
Trials that reported on at least one of the following clinical outcome measures:
Progression free survival, defined as the time from randomisation to first progression (locoregional or distant) or death
Overall survival, defined as the time from randomisation until death from any cause
Objective response rate, defined as the proportion of patients achieving an objective response
Toxicity regarding adverse events of grade 3 or higher, or specific adverse events defined and graded by the National Cancer Institute’s common terminology criteria for adverse events.
Studies not adhering to the inclusion criteria were excluded. Other exclusion criteria were:
Trials reporting results for patients with EGFR mutated NSCLC from a subgroup analysis that was a potential source of uncertain randomisation and therefore bias if patients failed to be originally randomised, owing to the heterogeneity of patient characteristics
Trials in which EGFR TKIs were used as maintenance or neoadjuvant treatments, or as sequential treatments with chemotherapy
Trials comparing treatments that have not been approved by any food and drug administration.
All study periods and durations of follow-up were eligible, and some updated data from mature or long term follow-up of an original article were used. Titles and abstracts were screened, and the full text of potentially eligible articles were sequentially assessed for final inclusion.
Data extraction and risk of bias assessment
Data on trial details (eg, study ID, first author, publication year, number of patients, and patient characteristics), treatments, and outcomes were extracted into a spreadsheet. Survival data assessed by the independent review facility were preferably extracted to avoid potential assessment bias by investigators. We preferred the use of treatment related adverse events, but if not specified as treatment related, we used all adverse events. ClinicalTrials.gov and other available sources were evaluated for the most recent and complete data. We also contacted study authors and pharmaceutical companies if important data were unclear or not reported.
The dominant histological type of EGFR mutated NSCLC was non-squamous carcinoma, in which pemetrexed yields better efficacy than other third generation chemotherapy drugs,21 22 so the pemetrexed based and pemetrexed free chemotherapies were considered separately in comparison arms, and described as monotherapies to optimise the network. Moreover, as the strategy of chemotherapy used in combination with gefitinib in the JMIT study23 was pemetrexed only, differing from the NEJ00924 and Han et al25 studies (which additionally used platinum), we regarded gefitinib plus pemetrexed in the JMIT study and gefitinib plus pemetrexed based chemotherapy in the other two studies as two single arms to eliminate discrepancy in estimation. In the FLAURA study,26 the control arm of standard EGFR TKIs grouped erlotinib and gefitinib together. We assumed that they showed the same outcomes when compared with osimertinib, respectively. If necessary, we used the reported ratio of erlotinib versus gefitinib (34%:66%) in the control arm to distribute patients taking osimertinib to create a sample match.
We assessed risk of bias of individual studies using the Cochrane Risk of Bias Tool,27 which is based on the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias. Items were scored as low, high, or unclear risk of bias.
All investigators independently conducted study selection and data extraction. Two investigators (YZ and JL) independently assessed risk of bias of individual studies. Any discrepancies were resolved by consensus and arbitration by a panel of adjudicators (YZ, JL, XC, ZP, WL, and JH).
Data synthesis and statistical analysis
We synthesised all direct and indirect evidence to compare different treatments in terms of efficacy and safety, reported as hazard ratios for survival outcomes (progression free survival and overall survival) and odds ratios for binary outcomes (objective response rate and grade ≥3 adverse events) along with corresponding 95% credible intervals. The primary outcome was progression free survival. Secondary outcomes were overall survival, objective response rate, and adverse events of grade 3 or higher.
In Stata (version 14.0), we generated network plots for different outcomes of different targeted patients to illustrate the geometries, to clarify which treatments were compared directly or indirectly in the included studies.28 We did frequentist, fixed effects, pairwise meta-analysis on head-to-head comparisons based on two or more trials. We assessed heterogeneity between studies using the Q test and I2 statistic within a visual forest plot.29 Statistical significance was set at a P value of 0.05. Heterogeneity was considered low, moderate, or high for estimated I2 values under 25%, between 25% and 50%, and over 50%, respectively.29
Network meta-analyses in the analyses for patients with advanced EGFR mutated NSCLC (including subgroup analyses based on exon 19 deletion and Leu858Arg mutation subtypes) were performed in a bayesian framework using a Markov Chain Monte Carlo simulation technique in OpenBUGS (version 3.2.3). The fixed effects consistency model was used, as most direct evidence was from one trial.7 We used non-informative uniform and normal prior distributions30 and three different sets of initial values to fit the model. For progression free survival and overall survival effects, 150 000 sample iterations were generated with 100 000 burn-ins and a thinning interval of 1. For objective response rate and toxic effects, 100 000 was added in both sample iterations and burn-ins, and the thinning interval was increased to 10 to minimise autocorrelation.
We evaluated convergence of iterations by visual inspection of the three chains to establish homogenous parameter estimates and in accordance with the Brooks-Gelman-Rubin diagnostic (supplementary fig S1).31 Once convergence was established, the posterior distributions for the model parameters were obtained as the output of the network meta-analysis estimate (hazard/odds ratio and the corresponding 95% credible interval). In the presence of minimally informative priors, credible intervals can be interpreted like conventional confidence intervals.20 Within the bayesian framework, the network meta-analysis estimated the overall rankings of treatments by calculating the surface under the cumulative ranking curve for each, which equals 1 when a treatment is certain to be the best and 0 when a treatment is certain to be the worst.20
Two key assumptions underlying the network meta-analysis are transitivity (the exchangeability across studies to compare two treatments via a third one) and consistency (that the direct and indirect estimates are statistically similar).14 We minimised issues arising from potential lack of transitivity by only including randomised controlled trials with strict patient allocation, and optimised balance to address all treatments for the same condition. Transitivity was evaluated by use of descriptive statistics for study and population baselines, such as sample size, age, sex, and drug dose.32 Pairwise meta-analyses in a bayesian framework were also performed with results complemented by those in frequentist framework to contrast the corresponding pooled hazard or odds ratios from the network meta-analyses for the evaluation of local inconsistency; we evaluated global inconsistency by comparing the fit of consistency and inconsistency models.33 34 The node splitting approach was used to calculate the inconsistency of the model, where direct and indirect evidence were separately contrasted on a particular comparison (node).
To assess the robustness and reliability of results, we planned several sensitivity analyses. The first analysis restricted phase III randomised controlled trials. The second analysis excluded the FLAURA study26 in order to check the effect of the adjustments made for synthesis of unspecified data on the results. The third analysis stratified patients as Asian and non-Asian to observe the influence of patient ethnicity. Subgroup analyses by the two common EGFR mutation types were also conducted in the first and second sensitivity analyses.
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design and implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
Systematic review and characteristics
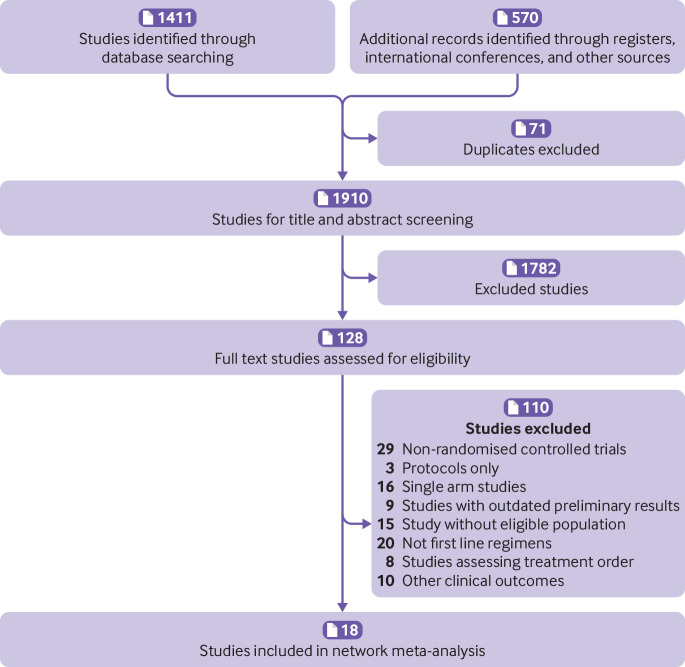
We identified 1981 records from the initial title and abstract screening, and retrieved and reviewed 128 reports in full text (fig 1). Finally, 18 randomised controlled trials12 13 23 24 25 26 35 36 37 38 39 40 41 42 43 44 45 46 47 were deemed eligible for inclusion with a total of 4628 patients enrolled to receive 12 different treatments including EGFR TKIs (osimertinib, dacomitinib, afatinib, erlotinib, gefitinib, and icotinib), pemetrexed based chemotherapy, pemetrexed free chemotherapy, and combination treatments (afatinib plus cetuximab, erlotinib plus bevacizumab, gefitinib plus pemetrexed based chemotherapy, and gefitinib plus pemetrexed). The networks are presented in figure 2. The main characteristics of all studies are reported in table 1. The assumption of transitivity was accepted because no variability was identified in the study and population baselines (supplementary fig S2). Supplementary figure S3 summarises the detailed risk of bias assessments.
Fig 1.
Study selection
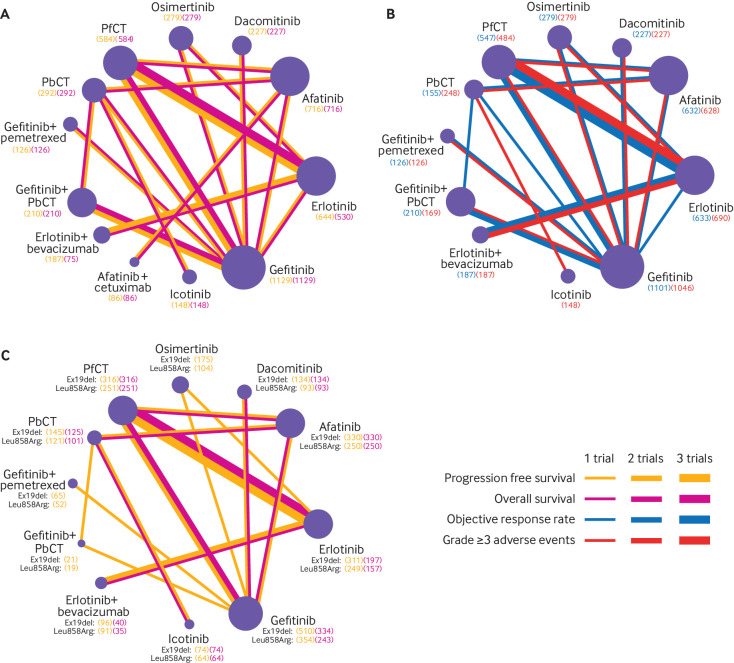
Fig 2.
Network diagrams of comparisons on different outcomes of treatments in different groups of patients with advanced epidermal growth factor receptor (EGFR) mutated non-small cell lung cancer (NSCLC). (A) Comparisons on progression free survival and overall survival in patients with advanced EGFR mutated NSCLC. (B) Comparisons on objective response rate and adverse events of grade 3 or higher in patients with advanced EGFR mutated NSCLC. (C) Comparisons on progression free survival and overall survival in subgroups of study patients with exon 19 deletion (Ex19del) and Leu858Arg mutation types. Each circular node represents a type of treatment. The node size is proportional to the total number of patients receiving a treatment (in brackets). Each line represents a type of head-to-head comparison. The width of lines is proportional to the number of trials comparing the connected treatments. PbCT=pemetrexed based chemotherapy; PfCT=pemetrexed free chemotherapy
Table 1.
Baseline characteristics of studies included in the network meta-analysis of patients with advanced epidermal growth factor receptor (EGFR) mutated non-small cell lung cancer
| Study (phase, ethnicity) | Sample size (No); median age | Female (%) | EGFR mutation | Intervention arm | Control arm | Reported outcomes | |
|---|---|---|---|---|---|---|---|
| Exon 19 deletion | Leu858Arg | ||||||
| NEJ026 201935 (III, Asian) | 114/114; 67/68 | 63.4/65.2 | 50/48 | 50/50 | Erlotinib 150 mg once a day + bevacizumab 15 mg/kg every 3 weeks | Erlotinib 150 mg once a day | Progression free survival†, objective response rate, grade ≥3 AEs |
| SWOGS1403 201836 (II, NG) | 86/84; NG | NG | NG | NG | Afatinib 40 mg once a day + cetuximab 500 mg/m2 every 2 weeks | Afatinib 40 mg once a day | Progression free survival, overall survival |
| NEJ009 201824 (III, Asian) | 170/172; 64.1/64.8* | 62.8/67.1 | NG | NG | Gefitinib 250 mg once a day + PbCT (carboplatin AUC 5 + pemetrexed 500 mg/m2 every 3 weeks (4-6 cycles) + pemetrexed 500 mg/m2 every 3 weeks) | Gefitinib 250 mg once a day | Progression free survival, overall survival, objective response rate, grade ≥3 AEs |
| FLAURA 201826 (III, multiple) | 279/277; 64.0/64.0 | 64.0/62.0 | 63/63 | 37/37 | Osimertinib 80 mg once a day | Gefitinib 250 mg once a day | Progression free survival†, overall survival, objective response rate, grade ≥3 AEs |
| 63/63 | 37/37 | Osimertinib 80 mg once a day | Erlotinib 150 mg once a day | ||||
| ARCHER1050 201738 48 (III, multiple) | 227/225; 62.0/61.0 | 64.0/56.0 | 59/59 | 41/41 | Dacomitinib 45 mg once a day | Gefitinib 250 mg once a day | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| CONVINCE 201737 (III, Asian) | 148/137; 56.0/56.0 | 70.9/69.3 | 50/50 | 43/39 | Icotinib 125 mg three times a day | PbCT (cisplatin 75 mg/m2 + pemetrexed 500mg/m2 every 3 weeks (4 cycles) + pemetrexed 500 mg/m2 every 3 weeks) | Progression free survival†, overall survival†, grade ≥3 AEs |
| Han et al 201725 (II, Asian) | 40/40; NG | 62.5/57.5 | 53/50 | 48/50 | Gefitinib 250 mg once a day + PbCT (carboplatin AUC=5 + pemetrexed 500 mg/m2 every 4 weeks (6 cycles) + pemetrexed 500 mg/m2 every 4 weeks) | PbCT (carboplatin AUC=5 + pemetrexed 500 mg/m2 every 4 weeks (6 cycles) + pemetrexed 500 mg/m2 every 4 weeks) | Progression free survival†, overall survival, objective response rate |
| 40/41; NG | 62.5/56.1 | 53/51 | 48/49 | Gefitinib + PbCT | Gefitinib 250 mg once a day | ||
| 41/40; NG | 56.1/57.5 | 51/50 | 49/50 | Gefitinib | PbCT | ||
| CTONG0901 201739 (III, Asian) | 81/84; NG | 46.9/53.1 | 58/58 | 42/42 | Erlotinib 150 mg once a day | Gefitinib 250 mg once a day | Progression free survival, overall survival, objective response rate, grade ≥3 AEs |
| JMIT 201623 49 (II, Asian) | 126/65; 62.0/62.0 | 65.0/63.0 | 52/62 | 41/35 | Gefitinib 250 mg once a day + pemetrexed 500 mg/m2 every 3 weeks | Gefitinib 250 mg once a day | Progression free survival†, overall survival, objective response rate, grade ≥3 AEs |
| LUX-Lung7 201641 50 (IIB, multiple) | 160/159; 63.0/63.0 | 57.0/67.0 | 58/58 | 42/42 | Afatinib 40 mg once a day | Gefitinib 250 mg once a day | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| ENSURE 201513 (III, Asian) | 110/107; 57.5/56.0 | 61.8/60.7 | 52/57 | 48/43 | Erlotinib 150 mg once a day | PfCT (gemcitabine 1250 mg/m2 + cisplatin 75 mg/m2 every 3 weeks (≤4 cycles)) | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| JO25567 201442 51 (II, Asian) | 75/77; 67.0/67.0 | 60.0/66.0 | 53/52 | 47/48 | Erlotinib 150 mg once a day + bevacizumab 15 mg/kg every 3 weeks | Erlotinib 150 mg once a day | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| LUX-Lung6 201443 (III, Asian) | 242/122; 58.0/58.0 | 64.0/68.0 | 51/51 | 38/38 | Afatinib 40 mg once a day | PfCT (gemcitabine 1000 mg/m2 + cisplatin 75 mg/m2 every 3 weeks (≤6 cycles)) | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| LUX-Lung3 201312 (III, multiple) | 230/115; 61.5/61.0 | 63.9/67.0 | 49/50 | 40/41 | Afatinib 40 mg once a day | PbCT (cisplatin 75 mg/m2 + pemetrexed 500mg/m2 every 3 weeks (≤6 cycles)) | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| EURTAC 201244 (III, non-Asian) | 86/87; 65.0/65.0 | 67.0/78.0 | 66/67 | 34/33 | Erlotinib 150 mg once a day | PfCT (cisplatin 75 mg/m2 + docetaxel 75 mg/m2/gemcitabine 1250 mg/m2 every 3 weeks) | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| OPTIMAL 201145 52 (III, Asian) | 83/72; 57.0/59.0 | 59.0/60.0 | 52/54 | 48/46 | Erlotinib 150 mg once a day | PfCT (gemcitabine 1000 mg/m2 + cisplatin AUC=5 every 3 weeks (≤4 cycles)) | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| NEJ002 201046 53 (III, Asian) | 114/110; 63.9/62.6* | 63.2/64.0 | 51/54 | 43/44 | Gefitinib 250 mg once a day | PfCT (paclitaxel 200 mg/m2 + carboplatin AUC=6 every 3 weeks (≥3 cycles)) | Progression free survival†, overall survival†, objective response rate, grade ≥3 AEs |
| WJTOG3405 200947 54 (III, Asian) | 86/86; 64.0/64.0 | 68.6/69.8 | 58/43 | 42/47 | Gefitinib 250 mg once a day | PfCT (cisplatin 80 mg/m2 + docetaxel 60 mg/m2 every 3 weeks (3-6 cycles)) | Progression free survival†, overall survival†, objective response rate |
Data are expressed as intervention/control unless indicated otherwise. AE=adverse events; NG=not given; AUC=area under the concentration-time curve; PbCT=pemetrexed based chemotherapy; PfCT=pemetrexed free chemotherapy.
Mean age was given instead of median age.
Information of outcomes for exon 19 deletion and Leu858Arg mutation subgroups are also reported in trials.
Network meta-analysis in advanced EGFR mutated NSCLC
Network meta-analysis included all treatments for progression free survival and overall survival (fig 2A), 10 treatments for objective response rate, and 11 treatments for adverse events of grade 3 or higher (fig 2B). We used data from trials48 49 50 51 52 53 54 with longer follow-up than previously published.
In terms of progression free survival (fig 3A), osimertinib yielded not only the best benefit of all EGFR-TKIs monotherapies (versus dacomitinib (hazard ratio 0.74, 95% credible interval 0.55 to 1.00), afatinib (0.52, 0.40 to 0.68), erlotinib (0.48, 0.40 to 0.57), gefitinib (0.44, 0.37 to 0.52), and icotinib (0.39, 0.24 to 0.62)), but also significant benefits versus afatinib plus cetuximab (0.44, 0.28 to 0.71) and gefitinib plus pemetrexed (0.65, 0.46 to 0.92). Gefitinib plus pemetrexed based chemotherapy was shown to be consistent with osimertinib (0.95, 0.72 to 1.24) in providing the best progression free survival. Pemetrexed based chemotherapy significantly prolonged progression free survival compared with pemetrexed free chemotherapy (0.68, 0.50 to 0.91), although both were shown to have the worst progression free survival versus other treatments.
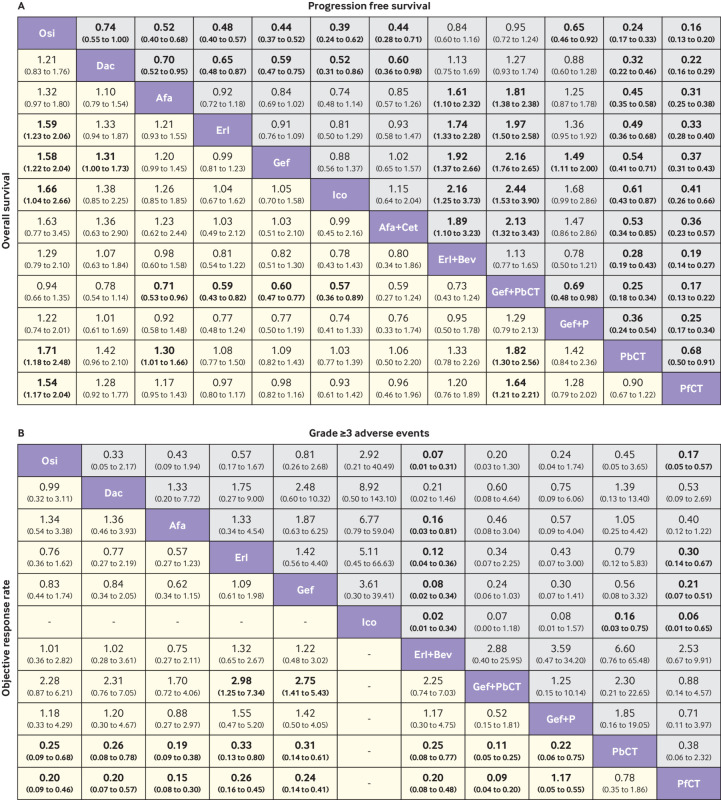
Fig 3.
Pooled estimates of the network meta-analysis. (A) Pooled hazard ratios (95% credible intervals) for progression free survival (upper triangle) and overall survival (lower triangle). (B) Pooled odds ratios (95% credible intervals) for adverse events of grade 3 or higher (upper triangle) and objective response rate (lower triangle). Data in each cell are hazard or odds ratios (95% credible intervals) for the comparison of row-defining treatment versus column-defining treatment. Hazard ratios less than 1 and odds ratios more than 1 favour row-defining treatment. Significant results are in bold. Osi=osimertinib; Dac=dacomitinib; Afa=afatinib; Erl=erlotinib; Gef=gefitinib; Ico=icotinib; Cet=cetuximab; Bev=bevacizumab; Gef+P=gefitinib plus pemetrexed; PbCT=pemetrexed based chemotherapy; PfCT=pemetrexed free chemotherapy
In terms of overall survival (fig 3A), osimertinib and gefitinib plus pemetrexed based chemotherapy were also consistent (hazard ratio 0.94, 95% credible interval 0.66 to 1.35) in providing the best overall survival benefit; significant differences were also observed when compared with most other monotherapies. Similar efficacy was found between dacomitinib and afatinib, and among erlotinib, gefitinib, icotinib, pemetrexed based chemotherapy, pemetrexed free chemotherapy, and afatinib plus cetuximab, because the hazard ratios were close to 1.
In terms of objective response rate (fig 3B), no significant difference was observed in any comparable EGFR-TKI monotherapies, however, EGFR-TKIs produced significant objective response rate benefits over chemotherapy. For multiple comparisons, the addition of pemetrexed based chemotherapy to gefitinib significantly increased objective response rate over gefitinib alone (odds ratio 2.75, 95% credible interval 1.41 to 5.43). Furthermore, gefitinib plus pemetrexed based chemotherapy was likely to be the best treatment in achieving an objective response.
We saw less toxicity related to EGFR-TKIs among the comparable treatments, particularly icotinib and osimertinib, which had the fewest and second fewest adverse events of grade 3 or higher, respectively (fig 3B). Afatinib was noted with the most adverse events of grade 3 or higher, compared with other EGFR-TKIs. More than 120 different types of specific adverse events were reported, of which 16 were selected as a representation of the most clinically relevant in current practice. Commonly reported adverse events for EGFR-TKIs included rash, diarrhoea, stomatitis, paronychia, dry skin, liver dysfunction, and interstitial lung disease, which were different from those of conventional chemotherapy (supplementary fig S4).
We also saw differences regarding the probability of these specific adverse events among TKIs (supplementary fig S5). Afatinib had the greatest probability to cause rash, diarrhoea, and stomatitis, followed by dacomitinib. Dacomitinib was associated with the highest risk of paronychia and dry skin. Osimertinib, erlotinib, and gefitinib had relatively mild toxicity spectrums; nevertheless, liver dysfunction was predominant for gefitinib, and gefitinib and dacomitinib caused more interstitial lung disease. Icotinib had the narrowest and safest toxicity spectrum.
The addition of other treatments to an EGFR-TKI, such as erlotinib plus bevacizumab versus erlotinib (odds ratio 8.33, 95% credible interval 2.78 to 25.00) and gefitinib plus pemetrexed based chemotherapy versus gefitinib (4.17, 0.97 to 16.67), was associated with an increase in the risk of adverse events of grade 3 or higher. Furthermore, in the multiple comparisons, erlotinib plus bevacizumab was likely to produce the most adverse events of grade 3 or higher (fig 3B).
Subgroup analysis by EGFR mutation type (exon 19 deletion and Leu858Arg mutations)
Regarding the outcomes in patients with the exon 19 deletion or Leu858Arg mutations, only progression free survival and overall survival network meta-analyses could be conducted while 11 treatments and eight treatments were available for comparison, respectively (fig 2C). Treatments providing the best benefit differed in the two subgroups.
In terms of progression free survival (fig 4A), osimertinib showed superiority in the exon 19 deletion subgroup, while gefitinib plus pemetrexed based chemotherapy showed superiority in the Leu858Arg subgroup. The comparison between the exon 19 deletion and Leu858Arg subgroups showed more pronounced differences among EGFR-TKIs for the exon 19 deletion subgroup, and between pemetrexed based chemotherapy and pemetrexed free chemotherapy for the Leu858Arg subgroup.
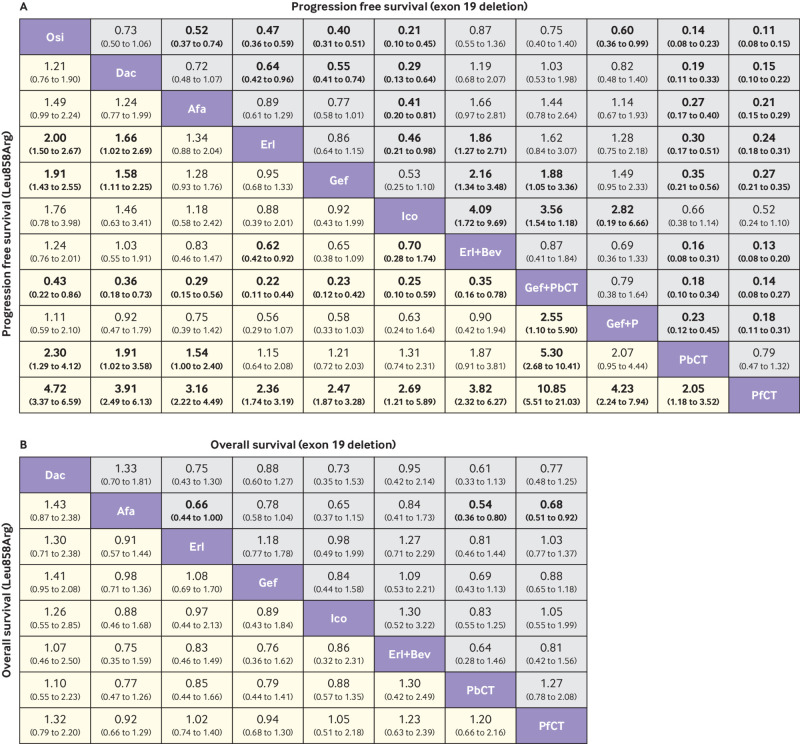
Fig 4.
Pooled estimates of subgroup analyses (patients stratified into exon 19 deletion and Leu858Arg subgroups). (A) Pooled hazard ratios (95% credible intervals) for progression free survival of exon 19 deletion (upper triangle) and Leu858Arg (lower triangle) subgroups. (B) Pooled hazard ratios (95% credible intervals) for overall survival of exon 19 deletion (upper triangle) and Leu858Arg (lower triangle) subgroups. Data in each cell are hazard ratios (95% credible interval) for the comparison of row-defining treatment versus column-defining treatment. Hazard ratios less than 1 favours row-defining treatment. Significant results are in bold. Osi=osimertinib; Dac=dacomitinib; Afa=afatinib; Erl=erlotinib; Gef=gefitinib; Ico=icotinib; Bev=bevacizumab; Gef+P=gefitinib plus pemetrexed; PbCT=pemetrexed based chemotherapy; PfCT=pemetrexed free chemotherapy
In terms of the overall survival (fig 4B), for exon 19 deletion subgroup, the significant differences in afatinib versus erlotinib (hazard ratio 0.66, 95% credible interval 0.44 to 1.00), pemetrexed based chemotherapy (0.54, 0.36 to 0.80), and pemetrexed free chemotherapy (0.68, 0.51 to 0.92), and the marginal difference in afatinib versus gefitinib (0.78, 0.58 to 1.04) were in favour of afatinib as the best option among the comparable treatments. For the Leu858Arg subgroup, we saw no significant difference in any two comparisons, with most hazard ratios close to 1. Dacomitinib showed possible increased efficacy.
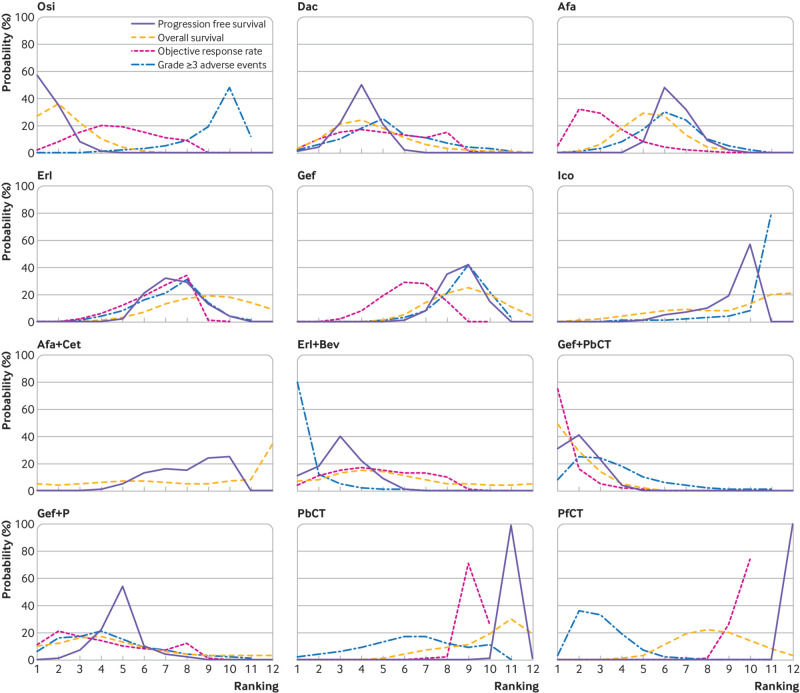
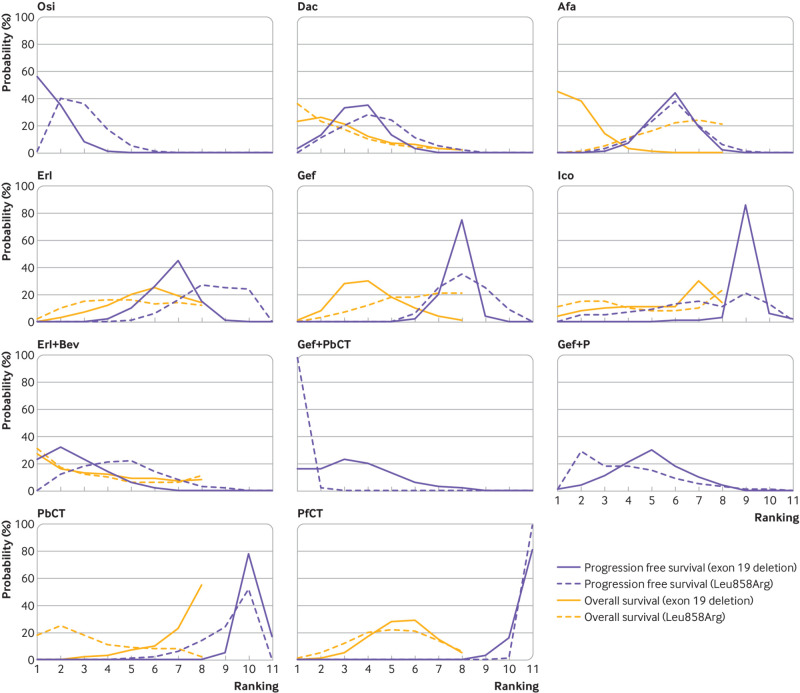
Rank probabilities
Figure 5 and figure 6 show the bayesian ranking profiles of comparable treatments in different populations (with detail ranking results summarised in supplementary table S3). The bayesian ranking results were almost in line with the pooled analyses using hazard and odds ratios. For patients with advanced EGFR mutated NSCLC, osimertinib was most likely to be ranked first for progression free survival (cumulative probability 57%), gefitinib plus pemetrexed based chemotherapy for both overall survival (49%) and objective response rate (75%), and erlotinib plus bevacizumab for adverse events of grade 3 or higher (80%; fig 5). Icotinib had the highest probability (80%) of ranking last in causing adverse events of grade 3 or higher followed by osimertinib. When EGFR mutation types were considered (fig 6), treatments with the greatest probability of being ranked first were different: osimertinib for the exon 19 deletion subgroup (56%) and gefitinib plus pemetrexed based chemotherapy for the Leu858Arg subgroup (98%) in terms of progression free survival; and afatinib for the exon 19 deletion (45%) subgroup and dacomitinib for the Leu858Arg subgroup (36%) in terms of overall survival.
Fig 5.
Bayesian ranking profiles of comparable treatments on efficacy for patients with advanced epidermal growth factor receptor mutated, non-small cell lung cancer. Profiles indicate the probability of each comparable treatment being ranked from first to last on progression free survival, overall survival, objective response rate, and grade ≥3 adverse events. Ranking curves are described according to the bayesian ranking results presented in supplementary table S3. Osi=osimertinib; Dac=dacomitinib; Afa=afatinib; Erl=erlotinib; Gef=gefitinib; Ico=icotinib; Cet=cetuximab; Bev=bevacizumab; Gef+P=gefitinib plus pemetrexed; PbCT=pemetrexed based chemotherapy; PfCT=pemetrexed free chemotherapy
Fig 6.
Bayesian ranking profiles of comparable treatments on safety for patients with advanced epidermal growth factor receptor mutated, non-small cell lung cancer, stratified into exon 19 deletion and Leu858Arg subgroups. Profiles indicate the probability of each comparable treatment being ranked from first to last on progression free survival and overall survival. Ranking curves are described according to the bayesian ranking results presented in supplementary table S3. Osi=osimertinib; Dac=dacomitinib; Afa=afatinib; Erl=erlotinib; Gef=gefitinib; Ico=icotinib; Bev=bevacizumab; Gef+P=gefitinib plus pemetrexed; PbCT=pemetrexed based chemotherapy; PfCT=pemetrexed free chemotherapy
Heterogeneity and inconsistency assessment
Forest plots of four feasible pairwise comparisons with heterogeneity estimates were generated in supplementary figure S6. Our assessment suggested minimal (I2=0%) or low heterogeneity in half of all comparisons regarding different outcomes in overall and subgroup populations. However, moderate to high heterogeneity was detected in comparisons of:
Erlotinib versus pemetrexed free chemotherapy for progression free survival (80.3%), objective response rate (83.9%), and adverse events of grade 3 or higher (82.0%)
Gefitinib versus pemetrexed free chemotherapy for progression free survival (74.7%), overall survival (40.6%), and objective response rate (35.5%)
Gefitinib plus pemetrexed based chemotherapy versus gefitinib for overall survival (77.6%) in patients with advanced EGFR mutated NSCLC
Erlotinib versus pemetrexed free chemotherapy (41.8%), gefitinib versus pemetrexed free chemotherapy (56.6%), and erlotinib plus bevacizumab versus erlotinib (34.2%) for progression free survival in the exon 19 deletion subgroup
Erlotinib versus pemetrexed free chemotherapy (43.3%) for progression free survival in the Leu858Arg subgroup.
The fit of the consistency model was similar or better than that of inconsistency model (supplementary table S4). We observed consistency between direct and indirect evidence after comparing results from pairwise meta-analyses (either bayesian or frequentist) and network meta-analyses (supplementary figs S6 and S7). Inconsistency between direct and indirect estimates from the node splitting analysis did not show significant differences in comparisons except for afatinib versus pemetrexed based chemotherapy (P=0.002) for progression free survival (supplementary table S5).
Sensitivity analysis
With a total of 3994 patients, 13 phase III trials12 13 24 26 35 37 38 39 43 44 45 46 47 and one phase IIB trial41 (for its high quality with multinational exploration, considerable sample size, and detailed outcomes) were included into the first sensitivity analysis (supplementary fig S8). Results did not show relevant deviations compared with the original network meta-analysis, but showed a higher probability of ranking best overall survival for osimertinib over gefitinib plus pemetrexed based chemotherapy (supplementary figs S9 and S10 and table S6). The robustness of results was also detected in the comparisons of the remaining treatments after the removal of the FLAURA study26 in the second sensitivity analysis (supplementary figs S11-S13).
Overall, 11 treatments for 3738 Asian patients (98% were east Asians) from 16 studies, and seven treatments for 722 non-Asian patients from six studies were included in the third sensitivity analysis by patient ethnicity. Owing to the low number of involved studies, only comparisons among monotherapies for progression free survival were accessible in the non-Asian subgroup (supplementary fig S14). For Asian patients, osimertinib, dacomitinib, and erlotinib plus bevacizumab seemed to show the same progression free survival benefit, and gefitinib plus pemetrexed based chemotherapy had the greatest probability to provide the best progression free survival, overall survival, and objective response rate (supplementary fig S15). For non-Asian patients, osimertinib showed the best progression free survival.
Discussion
Principal findings
In this systematic review and network meta-analysis, we comprehensively summarise the comparative efficacy and safety of multiple first line treatments including all available EGFR-TKIs and combination strategies for patients with advanced EGFR mutated NSCLC. The results suggest that:
Osimertinib and gefitinib plus pemetrexed based chemotherapy were consistent in providing the best progression free survival and overall survival for advanced EGFR mutated patients
The most promising treatments differed in patients stratified by the two common EGFR mutation types—that is, osimertinib for the exon 19 deletion subgroup and gefitinib plus pemetrexed based chemotherapy for the Leu858Arg subgroup
Combination treatments caused more toxicity in general and EGFR-TKIs were associated with different toxicity spectrums.
The sensitivity analyses showed that the overall results remained relatively robust. The loss of ranking superiority over osimertinib for gefitinib plus pemetrexed based chemotherapy regarding overall survival in the first sensitivity analysis only including phase III trials, and the potential difference of EGFR-TKI preference for Asian and non-Asians in the second sensitivity analysis should be considered.
The translation of the progression free survival benefit of osimertinib to the improvement in overall survival activity might account for its additional inhibition of the T790M mutation, which accounts for about 50-60% acquired resistance.5 55 Gefitinib plus pemetrexed based chemotherapy was associated with the most rapid and persistent response based on objective response rate and overall survival priority. Possible explanations include that simultaneous treatment with gefitinib and pemetrexed was previously reported to prevent the appearance of gefitinib resistance mediated by the T790M mutation or epithelial-to-mesenchymal transition, respectively, in cell lines with the exon 19 deletion mutation.56 Furthermore, patients might receive multiple lines of treatment at disease progression as crossover is common, thus efficacy of the possible salvage treatments received must be taken into account. In addition, the comparison of erlotinib versus erlotinib plus bevacizumab (hazard ratio 1.74, 95% credible interval 1.33 to 2.28; fig 3A) favoured the combination treatment for extension of progression free survival duration. These results suggest a hypothesis that patients with advanced EGFR mutated NSCLC might obtain overall clinical benefits from the addition of chemotherapy (especially pemetrexed based chemotherapy) or bevacizumab to osimertinib, compared with the current standard of care.
Some existing evidence implies that different types of EGFR mutations vary in their clinical and pathological correlations, downstream signalling, and responsiveness to EGFR-TKIs, which suggests that the benefit of EGFR-TKIs is greater in exon 19 deletion mutated tumours than in Leu858Arg mutated tumours.57 58 One hypothesis is that Leu858Arg mutated tumours might be associated with more frequent T790M mutations.59 60 Alternatively, previous studies have shown that concomitant mutation (comutation) including other oncogenic driver alterations in several other genes (TP53, PIK3CA, BRAF, MET, MYC, CDK6, and CTNNB1)61 might be associated with higher rates of primary resistance to EGFR-TKIs62 63 and also limited response to EGFR-TKIs.64 65 A significantly higher incidence of comutations was found with Leu858Arg mutation than with exon 19 deletion mutation.65 This recent concept might explain why the addition of chemotherapy was associated with a benefit for the Leu858Arg subgroup, and should be more thoroughly investigated in future studies.
EGFR-TKIs were associated with less toxicity, while combination strategies caused more, reflecting the expected additional adverse events for either combined drug. For instance, higher incidences of hypertension, haemorrhagic events, and proteinuria were observed with the addition of bevacizumab to erlotinib; and anorexia, vomiting, neutropenia, and anaemia were observed with the addition of chemotherapy to gefitinib (supplementary fig S4). Clinicians should keep in mind the possibility of increased toxicity when prescribing combination therapy. From this multiple comparison, erlotinib plus bevacizumab and icotinib had the worst and best safety profiles, respectively. The relatively more frequent and severe toxicity of the erlotinib plus bevacizumab group was reported in both NEJ026 and JMIT studies23 35 and was well tolerated and clinically manageable.
Previous studies have characterised icotinib with favourable safety,66 67 which was deemed to be attributed to its broad therapeutic window and high selectivity towards the target EGFR.68 Moreover, we found differences in toxicity spectrums among EGFR-TKIs. For a better management and treatment selection, knowledge of the predominant adverse events related to each EGFR-TKI during long term use is critical because toxicity is part of the same aspect of the evaluation. A well performed systemic review with a mass sample size and a thorough assessment is warranted to generate a complete and potent toxicity spectrum of EGFR-TKIs.
Strengths and comparison with other studies
Compared with the reported network meta-analyses investigating treatments for patients with advanced EGFR mutated NSCLC,15 16 17 18 our present network meta-analysis had several strengths. The study ensured the homogeneity of study population by consisting exclusively of patients with advanced EGFR mutated NSCLC. The present study also established comparisons among all monotherapies including osimertinib and dacomitinib, and combination treatments in a first line setting for this population, and comprehensively analysed all major efficacy and toxicity outcomes with the most extensive data including the previously unpublished or recently updated results. In particular, we separately established multiple comparisons to investigate the relative effectiveness of treatments in exon 19 deletion or Leu858Arg subgroups. Moreover, network transitivity, heterogeneity, and inconsistency were thoroughly investigated. No differences in drug dose or the assessible key baseline characteristics within the studies were found to explain the high heterogeneity in erlotinib and gefitinib versus pemetrexed free chemotherapy in particular, and the significant inconsistency in afatinib versus pemetrexed based chemotherapy. However, chemotherapy drugs differed in trials but were grouped as single pemetrexed based chemotherapy and pemetrexed free chemotherapy network nodes in our study, which could be a potential source of heterogeneity and inconsistency, and also possible weak transitivity.
Implications
By synthesising all randomised controlled trials evidence, this review provides clinicians a reference source to evaluate strengths and weaknesses for practice choice among multiple promising options. Osimertinib and gefitinib plus pemetrexed based chemotherapy were shown to be comparable as the optimal treatments for patients with advanced EGFR mutated NSCLC, and were preferentially recommended to exon 19 deletion or Leu858Arg subgroups, respectively. Complementing recent guidelines, these findings can help answer questions of whether combination treatments had a role in the standard care of patients with advanced EGFR mutated NSCLC, and which treatments might be most suitable for patients with the two most common mutations (which are often used as stratification and prognostic factors in many EGFR-TKI trials). Such investigation, studying combination treatments, and potentially different management for subgroups, should also be applied to other kinds of cancers. Future trials highlighting head-to-head comparisons such as osimertinib versus gefitinib plus pemetrexed based chemotherapy, potentially more effective strategies such as osimertinib plus pemetrexed based chemotherapy or bevacizumab, or the heterogeneity of EGFR mutated tumours should be conducted, especially with the ongoing challenge of emerging drug resistance.
Limitations
The present study had several limitations. Firstly, unavoidable confounding factors remain in this inherently observational network meta-analysis based on data entirely from clinical trials. For example, because most treatments were compared indirectly and most direct evidence was from one trial in the present network, estimates should be interpreted with care for their reliance on previous distributions and assumptions of transitivity and consistency, even though only randomised controlled trials were included and assumptions were investigated. For another example, methodological heterogeneity across studies was anticipated in this network meta-analysis, thus the same model selection (fixed effects model) was applied in both pairwise meta-analysis and network meta-analysis obtaining the highest generalisability in the pooled estimates. Secondly, the present study also had potential publication and selection bias, for example, phase II clinical trials commonly present unclear randomisation sequence generations in small sample sizes. We did not use funnel plots to assess the publication bias and small study effects given the small number of trials included in each comparison. Therefore, sensitivity analysis including only phase III trials was conducted, and relatively robust results were ensured.
Thirdly, data on overall survival might cause heterogeneity when taken as an endpoint to evaluate each individual treatment’s realistic effect. This heterogeneity could be possible for two reasons. Although we initially searched for the most updated overall survival hazard ratios, data on overall survival had only 25% maturity at the interim analysis in the FLAURA trial26; thus, it is still tempting for clinicians to consider a substantial improvement in overall survival activity for first line osimertinib. Furthermore, these patients often received second or later line treatments, which was not commonly reported and might hamper the interpretation of overall survival. As a result, we reported progression free survival as the primary outcome measure because progression free survival represents the survival until first disease progression beyond the influence of later line treatment.
A fourth limitation was that patients were not stratified according to factors such as smoking status or sex, which might modify treatment benefits.57 Future studies should investigate the relative treatment efficacy according to these clinical characteristics using the network meta-analysis statistical method, although this was not possible in the present study because of data sparseness across trials. Finally, questions regarding the efficacy of treatments in sequential or maintenance use was not investigated and therefore, remains a subject for further studies. Other imprecise estimates were likely:
Due to the limitation of the FLAURA study design,26 we had to consider the gefitinib and erlotinib in the control arm as having the same efficacy and toxicity, but the main results of remaining comparisons did not change based on the sensitivity analysis that removed the FLAURA study
Some trials were not included in all analyses because they did not have some specific endpoints; for example, only six treatments were compared in terms of overall survival in the exon 19 deletion and Leu858Arg subgroups
Patients stratified by exon 19 deletion and Leu858Arg mutations were not originally randomly studied in trials, and thus the risk of imprecision in the comparison is probable in these subgroup analyses.
Conclusions
In this network meta-analysis, osimertinib and gefitinib plus pemetrexed based chemotherapy appears to be superior first line treatment choices for patients with advanced EGFR mutated NSCLC, and were preferentially recommended to patients with exon 19 deletion or Leu858Arg mutations, respectively. We also found EGFR-TKIs, especially icotinib, were associated with less toxicity, although toxicity risk generally rose when they were combined with other treatments—in particular, erlotinib plus bevacizumab caused the most adverse events of grade 3 or higher. These findings could complement current standard of care and enhance future trial design for advanced EGFR mutated NSCLC.
What is already known on this topic
The current standard of first line care for patients with advanced epidermal growth factor receptor (EGFR) mutated non-small cell lung cancer (NSCLC) is treatment with EGFR tyrosine kinase inhibitors (TKIs; eg, osimertinib, dacomitinib, afatinib, erlotinib, and gefitinib); however, acquired drug resistance inevitably develops
For further improved outcomes, biologically synergistic combinations building on the foundation treatment of EGFR-TKIs were investigated as first line options
Previous studies have implied that the EGFR exon 19 deletion and Leu858Arg mutations should be considered as distinct biological and clinical entities
What this study adds
Osimertinib and gefitinib plus pemetrexed based chemotherapy were shown to be similar to the optimal treatments for patients with EGFR mutated NSCLC, and were preferentially recommended to patients with exon 19 deletion or Leu858Arg, respectively
Combination treatments caused more toxicity in general, especially erlotinib plus bevacizumab caused the most adverse events of grade 3 or higher; EGFR-TKIs were associated with different toxicity spectrums
The current findings might help the decision making process between patients and clinicians, regarding combination treatments for patients with advanced EGFR mutated NSCLC, and the most suitable treatments for patients with the two most common EGFR mutations
Acknowledgments
We thank Caichen Li, Bo Cheng, Jianfu Li, Shan Xiong, and Lei Jin, from the First Affiliated Hospital of Guangzhou Medical University, for their assistance in analysing data and formatting the manuscript.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary material
Contributors: JH and WL contributed equally to this paper and are joint corresponding authors. YZ, JL, XC, and ZP are joint first authors. All corresponding and first authors contributed to study concept and design. All authors selected the articles and extracted the data. JL, WY, HC, and HL contacted study investigators and pharmaceutical companies to request additional information. YZ, JL, and WL analysed and interpreted the data. YZ, JL, and ZX wrote the first draft of the report with input from WL and JH. All authors approved the final version of the report. YZ was responsible for the integrity and accuracy of the data and is the guarantor. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: There was no funding source for this study.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required.
Data sharing: No additional data available.
The manuscript’s guarantor affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned and registered have been explained.
References
- 1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2. Rosell R, Moran T, Queralt C, et al. Spanish Lung Cancer Group Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med 2009;361:958-67. 10.1056/NEJMoa0904554. [DOI] [PubMed] [Google Scholar]
- 3. Greenhalgh J, Dwan K, Boland A, et al. First-line treatment of advanced epidermal growth factor receptor (EGFR) mutation positive non-squamous non-small cell lung cancer. Cochrane Database Syst Rev 2016;(5):CD010383. 10.1002/14651858.CD010383.pub2. [DOI] [PubMed] [Google Scholar]
- 4.NCCN clinical practice guidelines in oncology for non-small cell lung cancer. Version 2. 2019. https://www.nccn.org/patients. Accessed 21 November 2018.
- 5. Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res 2013;19:2240-7. 10.1158/1078-0432.CCR-12-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jänne PA, Yang JC, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med 2015;372:1689-99. 10.1056/NEJMoa1411817. [DOI] [PubMed] [Google Scholar]
- 7. Thress KS, Paweletz CP, Felip E, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med 2015;21:560-2. 10.1038/nm.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barlesi F, Mazieres J, Merlio J-P, et al. Biomarkers France contributors Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT). Lancet 2016;387:1415-26. 10.1016/S0140-6736(16)00004-0. [DOI] [PubMed] [Google Scholar]
- 9. Wu SG, Shih JY. Management of acquired resistance to EGFR TKI-targeted therapy in advanced non-small cell lung cancer. Mol Cancer 2018;17:38. 10.1186/s12943-018-0777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pan Q, Pao W, Ladanyi M. Rapid polymerase chain reaction-based detection of epidermal growth factor receptor gene mutations in lung adenocarcinomas. J Mol Diagn 2005;7:396-403. 10.1016/S1525-1578(10)60569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Murray S, Dahabreh IJ, Linardou H, Manoloukos M, Bafaloukos D, Kosmidis P. Somatic mutations of the tyrosine kinase domain of epidermal growth factor receptor and tyrosine kinase inhibitor response to TKIs in non-small cell lung cancer: an analytical database. J Thorac Oncol 2008;3:832-9. 10.1097/JTO.0b013e31818071f3. [DOI] [PubMed] [Google Scholar]
- 12. Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. 10.1200/JCO.2012.44.2806. [DOI] [PubMed] [Google Scholar]
- 13. Wu YL, Zhou C, Liam CK, et al. First-line erlotinib versus gemcitabine/cisplatin in patients with advanced EGFR mutation-positive non-small-cell lung cancer: analyses from the phase III, randomized, open-label, ENSURE study. Ann Oncol 2015;26:1883-9. 10.1093/annonc/mdv270. [DOI] [PubMed] [Google Scholar]
- 14. Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med 2013;159:130-7. 10.7326/0003-4819-159-2-201307160-00008. [DOI] [PubMed] [Google Scholar]
- 15. Zhang Y, Zhang Z, Huang X, et al. Therapeutic efficacy comparison of 5 major EGFR-TKIs in advanced EGFR-positive Non-small-cell lung cancer: a network meta-analysis based on head-to-head trials. Clin Lung Cancer 2017;18:e333-40. 10.1016/j.cllc.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 16. Liang W, Wu X, Fang W, et al. Network meta-analysis of erlotinib, gefitinib, afatinib and icotinib in patients with advanced non-small-cell lung cancer harboring EGFR mutations. PLoS One 2014;9:e85245. 10.1371/journal.pone.0085245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Popat S, Mok T, Yang JC, et al. Afatinib in the treatment of EGFR mutation-positive NSCLC--a network meta-analysis. Lung Cancer 2014;85:230-8. 10.1016/j.lungcan.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 18. Popat S, Lungershausen J, Griebsch I, Marten A, Wu YL. Treatments for EGFR mutation-positive (M+) NSCLC patients - a network meta-analysis (NMA) by mutation type. Value Health 2014;17:A615. 10.1016/j.jval.2014.08.2166. [DOI] [PubMed] [Google Scholar]
- 19. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777-84. 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 20. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011;64:163-71. 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 21. Scagliotti G, Hanna N, Fossella F, et al. The differential efficacy of pemetrexed according to NSCLC histology: a review of two Phase III studies. Oncologist 2009;14:253-63. 10.1634/theoncologist.2008-0232. [DOI] [PubMed] [Google Scholar]
- 22. Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 2008;26:3543-51. 10.1200/JCO.2007.15.0375. [DOI] [PubMed] [Google Scholar]
- 23. Cheng Y, Murakami H, Yang P-C, et al. Randomized phase II trial of gefitinib with and without pemetrexed as first-line therapy in patients with advanced nonsquamous non-small-cell lung cancer with activating epidermal growth factor receptor mutations. J Clin Oncol 2016;34:3258-66. 10.1200/JCO.2016.66.9218. [DOI] [PubMed] [Google Scholar]
- 24.Abstract 9005. Phase III study comparing gefitinib monotherapy (G) to combination therapy with gefitinib, carboplatin, and pemetrexed (GCP) for untreated patients (pts) with advanced non-small cell lung cancer (NSCLC) with EGFR mutations (NEJ009). ASCO 54th Annual Meeting; 2018; Chicago, United States.
- 25. Han B, Jin B, Chu T, et al. Combination of chemotherapy and gefitinib as first-line treatment for patients with advanced lung adenocarcinoma and sensitive EGFR mutations: A randomized controlled trial. Int J Cancer 2017;141:1249-56. 10.1002/ijc.30806. [DOI] [PubMed] [Google Scholar]
- 26. Soria JC, Ohe Y, Vansteenkiste J, et al. FLAURA Investigators Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med 2018;378:113-25. 10.1056/NEJMoa1713137. [DOI] [PubMed] [Google Scholar]
- 27. Higgins J, Green S. Cochrane handbook of systematic reviews of interventions . Cochrane Collaboration, Wiley, 2008. 10.1002/9780470712184. [DOI] [Google Scholar]
- 28. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One 2013;8:e76654. 10.1371/journal.pone.0076654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sutton A, Ades AE, Cooper N, Abrams K. Use of indirect and mixed treatment comparisons for technology assessment. Pharmacoeconomics 2008;26:753-67. 10.2165/00019053-200826090-00006 [DOI] [PubMed] [Google Scholar]
- 31. Stephen P, Brooks AG. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat 1998;7:434-55. [Google Scholar]
- 32. Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods 2012;3:80-97. 10.1002/jrsm.1037. [DOI] [PubMed] [Google Scholar]
- 33. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med 2010;29:932-44. 10.1002/sim.3767. [DOI] [PubMed] [Google Scholar]
- 34.Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. NICE DSU technical support document 4: inconsistency in networks of evidence based on randomised controlled trials. 2011; updated April 2014. NICE Decision Support Unit, 2014. http://nicedsu.org.uk/ (accessed 22 August 2017). [PubMed]
- 35. Saito H, Fukuhara T, Furuya N, et al. Erlotinib plus bevacizumab versus erlotinib alone in patients with EGFR-positive advanced non-squamous non-small-cell lung cancer (NEJ026): interim analysis of an open-label, randomised, multicentre, phase 3 trial. Lancet Oncol 2019;20:625-35. 10.1016/S1470-2045(19)30035-X [DOI] [PubMed] [Google Scholar]
- 36.OA10. 04. Afatinib with or without cetuximab for EGFR-mutant non-small cell lung cancer: safety and efficacy results from SWOG S1403. IASLC 19th WCLC; 2018; Toronto, Canada.
- 37. Shi YK, Wang L, Han BH, et al. First-line icotinib versus cisplatin/pemetrexed plus pemetrexed maintenance therapy for patients with advanced EGFR mutation-positive lung adenocarcinoma (CONVINCE): a phase 3, open-label, randomized study. Ann Oncol 2017;28:2443-50. 10.1093/annonc/mdx359. [DOI] [PubMed] [Google Scholar]
- 38. Wu Y-L, Cheng Y, Zhou X, et al. Dacomitinib versus gefitinib as first-line treatment for patients with EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): a randomised, open-label, phase 3 trial. Lancet Oncol 2017;18:1454-66. 10.1016/S1470-2045(17)30608-3. [DOI] [PubMed] [Google Scholar]
- 39. Yang JJ, Zhou Q, Yan HH, et al. A phase III randomised controlled trial of erlotinib vs gefitinib in advanced non-small cell lung cancer with EGFR mutations. Br J Cancer 2017;116:568-74. 10.1038/bjc.2016.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Leighl NB, Rizvi NA, de Lima LG, Jr, et al. Phase 2 study of erlotinib in combination with linsitinib (OSI-906) or placebo in chemotherapy-naive patients with non-small-cell lung cancer and activating epidermal growth factor receptor mutations. Clin Lung Cancer 2017;18:34-42 e2. 10.1016/j.cllc.2016.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Park K, Tan E-H, O’Byrne K, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol 2016;17:577-89. 10.1016/S1470-2045(16)30033-X. [DOI] [PubMed] [Google Scholar]
- 42. Seto T, Kato T, Nishio M, et al. Erlotinib alone or with bevacizumab as first-line therapy in patients with advanced non-squamous non-small-cell lung cancer harbouring EGFR mutations (JO25567): an open-label, randomised, multicentre, phase 2 study. Lancet Oncol 2014;15:1236-44. 10.1016/S1470-2045(14)70381-X. [DOI] [PubMed] [Google Scholar]
- 43. Wu Y-L, Zhou C, Hu C-P, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:213-22. 10.1016/S1470-2045(13)70604-1. [DOI] [PubMed] [Google Scholar]
- 44. Rosell R, Carcereny E, Gervais R, et al. Spanish Lung Cancer Group in collaboration with Groupe Français de Pneumo-Cancérologie and Associazione Italiana Oncologia Toracica Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- 45. Zhou C, Wu Y-L, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. 10.1016/S1470-2045(11)70184-X. [DOI] [PubMed] [Google Scholar]
- 46. Maemondo M, Inoue A, Kobayashi K, et al. North-East Japan Study Group Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- 47. Mitsudomi T, Morita S, Yatabe Y, et al. West Japan Oncology Group Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 2010;11:121-8. 10.1016/S1470-2045(09)70364-X. [DOI] [PubMed] [Google Scholar]
- 48. Tony S, Mok YC, Zhou X, et al. Improvement in overall survival in a randomized study that compared dacomitinib with gefitinib in patients with advanced non-small-cell lung cancer and EGFR-activating mutations. J Clin Oncol 2018;36:2244-50. 10.1200/JCO.2018.78.7994. [DOI] [PubMed] [Google Scholar]
- 49.1381PD. Gefitinib with or without pemetrexed in nonsquamous non–small cell lung cancer with EGFR mutation: final overall survival results from a randomized phase II study. 43rd ESMO Congress; 2018; Munich, Germany.
- 50. Paz-Ares L, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: overall survival data from the phase IIb LUX-Lung 7 trial. Ann Oncol 2017;28:270-7. 10.1093/annonc/mdw611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abstract 9007. Erlotinib plus bevacizumab (EB) versus erlotinib alone (E) as first-line treatment for advanced EGFR mutation-positive non-squamous non-small-cell lung cancer (NSCLC): Survival follow-up results of JO25567. ASCO 54th Annual Meeting; 2018; Chicago, United States.
- 52. Zhou C, Wu YL, Chen G, et al. Final overall survival results from a randomised, phase III study of erlotinib versus chemotherapy as first-line treatment of EGFR mutation-positive advanced non-small-cell lung cancer (OPTIMAL, CTONG-0802). Ann Oncol 2015;26:1877-83. 10.1093/annonc/mdv276 [DOI] [PubMed] [Google Scholar]
- 53. Inoue A, Kobayashi K, Maemondo M, et al. North-East Japan Study Group Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naïve non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol 2013;24:54-9. 10.1093/annonc/mds214. [DOI] [PubMed] [Google Scholar]
- 54. Yoshioka H, Mitsudomi T, Morita S, et al. Final overall survival results of WJTOG 3405, a randomized phase 3 trial comparing gefitinib (G) with cisplatin plus docetaxel (CD) as the first-line treatment for patients with non-small cell lung cancer (NSCLC) harboring mutations of the epidermal growth factor receptor (EGFR). J Clin Oncol 2014;32:8117-17. 10.1200/jco.2014.32.15_suppl.8117. [DOI] [Google Scholar]
- 55. Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26. 10.1126/scitranslmed.3002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. La Monica S, Madeddu D, Tiseo M, et al. Combination of gefitinib and pemetrexed prevents the acquisition of TKI resistance in NSCLC cell lines carrying EGFR-activating mutation. J Thorac Oncol 2016;11:1051-63. 10.1016/j.jtho.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 57. Lee CK, Wu YL, Ding PN, et al. Impact of specific epidermal growth factor receptor (EGFR) mutations and clinical characteristics on outcomes after treatment with EGFR tyrosine kinase inhibitors versus chemotherapy in EGFR-mutant lung cancer: a meta-analysis. J Clin Oncol 2015;33:1958-65. 10.1200/JCO.2014.58.1736. [DOI] [PubMed] [Google Scholar]
- 58. Riely GJ, Pao W, Pham D, et al. Clinical course of patients with non-small cell lung cancer and epidermal growth factor receptor exon 19 and exon 21 mutations treated with gefitinib or erlotinib. Clin Cancer Res 2006;12:839-44. 10.1158/1078-0432.CCR-05-1846. [DOI] [PubMed] [Google Scholar]
- 59. Jackman DM, Yeap BY, Sequist LV, et al. Exon 19 deletion mutations of epidermal growth factor receptor are associated with prolonged survival in non-small cell lung cancer patients treated with gefitinib or erlotinib. Clin Cancer Res 2006;12:3908-14. [DOI] [PubMed] [Google Scholar]
- 60. Zhu JQ, Zhong WZ, Zhang GC, et al. Better survival with EGFR exon 19 than exon 21 mutations in gefitinib-treated non-small cell lung cancer patients is due to differential inhibition of downstream signals. Cancer Lett 2008;265:307-17. 10.1016/j.canlet.2008.02.064. [DOI] [PubMed] [Google Scholar]
- 61. Blakely CM, Watkins TBK, Wu W, et al. Evolution and clinical impact of co-occurring genetic alterations in advanced-stage EGFR-mutant lung cancers. Nat Genet 2017;49:1693-704. 10.1038/ng.3990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. De Pas T, Toffalorio F, Manzotti M, et al. Activity of epidermal growth factor receptor-tyrosine kinase inhibitors in patients with non-small cell lung cancer harboring rare epidermal growth factor receptor mutations. J Thorac Oncol 2011;6:1895-901. 10.1097/JTO.0b013e318227e8c6. [DOI] [PubMed] [Google Scholar]
- 63. Massarelli E, Johnson FM, Erickson HS, Wistuba II, Papadimitrakopoulou V. Uncommon epidermal growth factor receptor mutations in non-small cell lung cancer and their mechanisms of EGFR tyrosine kinase inhibitors sensitivity and resistance. Lung Cancer 2013;80:235-41. 10.1016/j.lungcan.2013.01.018. [DOI] [PubMed] [Google Scholar]
- 64. Barnet MB, O’Toole S, Horvath LG, et al. EGFR-co-mutated advanced NSCLC and response to EGFR tyrosine kinase inhibitors. J Thorac Oncol 2017;12:585-90. 10.1016/j.jtho.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 65. Hong S, Gao F, Fu S, et al. Concomitant genetic alterations with response to treatment and epidermal growth factor receptor tyrosine kinase inhibitors in patients with EGFR-mutant advanced non-small cell lung cancer. JAMA Oncol 2018;4:739-42. 10.1001/jamaoncol.2018.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hu X, Han B, Gu A, et al. A single-arm, multicenter, safety-monitoring, phase IV study of icotinib in treating advanced non-small cell lung cancer (NSCLC). Lung Cancer 2014;86:207-12. 10.1016/j.lungcan.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 67. Shi Y, Zhang L, Liu X, et al. Icotinib versus gefitinib in previously treated advanced non-small-cell lung cancer (ICOGEN): a randomised, double-blind phase 3 non-inferiority trial. Lancet Oncol 2013;14:953-61. 10.1016/S1470-2045(13)70355-3. [DOI] [PubMed] [Google Scholar]
- 68. Tan F, Shen X, Wang D, et al. Icotinib (BPI-2009H), a novel EGFR tyrosine kinase inhibitor, displays potent efficacy in preclinical studies. Lung Cancer 2012;76:177-82. 10.1016/j.lungcan.2011.10.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary material