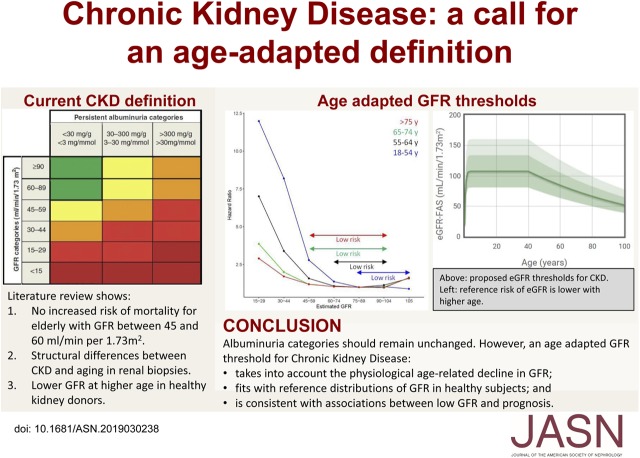
Visual Abstract
Keywords: chronic kidney disease, epidemiology and outcomes, glomerular filtration rate
Abstract
Current criteria for the diagnosis of CKD in adults include persistent signs of kidney damage, such as increased urine albumin-to-creatinine ratio or a GFR below the threshold of 60 ml/min per 1.73 m2. This threshold has important caveats because it does not separate kidney disease from kidney aging, and therefore does not hold for all ages. In an extensive review of the literature, we found that GFR declines with healthy aging without any overt signs of compensation (such as elevated single-nephron GFR) or kidney damage. Older living kidney donors, who are carefully selected based on good health, have a lower predonation GFR compared with younger donors. Furthermore, the results from the large meta-analyses conducted by the CKD Prognosis Consortium and from numerous other studies indicate that the GFR threshold above which the risk of mortality is increased is not consistent across all ages. Among younger persons, mortality is increased at GFR <75 ml/min per 1.73 m2, whereas in elderly people it is increased at levels <45 ml/min per 1.73 m2. Therefore, we suggest that amending the CKD definition to include age-specific thresholds for GFR. The implications of an updated definition are far reaching. Having fewer healthy elderly individuals diagnosed with CKD could help reduce inappropriate care and its associated adverse effects. Global prevalence estimates for CKD would be substantially reduced. Also, using an age-specific threshold for younger persons might lead to earlier identification of CKD onset for such individuals, at a point when progressive kidney damage may still be preventable.
The current criteria used for the definition of CKD in adults are: (1) signs of kidney damage, most often determined by an elevated urine albumin (or protein)-to-creatinine ratio (ACR); or (2) reduced kidney function, indicated by GFR <60 ml/min per 1.73 m2. GFR is considered the best determinant of kidney function,1 and CKD is staged according to six GFR categories (G1, G2, G3a, G3b, G4, and G5) and three categories for urine ACR levels (A1, A2 and A3) (Table 1). There is a broad agreement that abnormal urine ACR should trigger a diagnosis of CKD, but controversy remains regarding the most appropriate diagnostic criteria regarding GFR.
Table 1.
Current CKD staging according to GFR and urine ACR
| CDK Stage | Measurement |
|---|---|
| GFR category | GFR (ml/min per 1.73 m2) |
| G1 | ≥90 |
| G2 | 60–89 |
| G3a | 45–59 |
| G3b | 30–44 |
| G4 | 15–29 |
| G5 | <15 |
| ACR category | Urine ACR (mg/g) |
| A1 | <30 |
| A2 | 30–300 |
| A3 | >300 |
In this article, we will focus on the role of GFR in the definition of CKD. Laboratory thresholds for disease identification are commonly determined in two ways.2–4 First, the distribution of the laboratory results in a representative population of healthy persons is obtained and thresholds for defining disease are calculated according to extreme values based on this distribution (typically 95th or 97.5th percentile for “too high” and 2.5th or fifth percentile for “too low”). Second, a threshold associated with an adverse outcome is identified through epidemiologic studies. We will discuss these two strategies (reference distribution and prognosis) in the specific case of using GFR for CKD definition.
Current CKD Definition and Related Caveats
The current and widely adopted definition of CKD in adults is based on the 2013 Kidney Disease Improving Global Outcomes (KDIGO) guidelines.1 Although not entirely undisputed, we do recognize the merit of these guidelines, as they standardized the definition of CKD.5–11 Not only is GFR one of the two main criteria for diagnosis of CKD, an isolated GFR <60 ml/min per 1.73 m2 (confirmed with a second value after at least 90 days) suffices for the diagnosis of CKD. In other words, anyone with a GFR <60 ml/min per 1.73 m2 persisting for at least 3 months, by definition, has CKD, even if the urine ACR and structure or kidney morphology (ascertained by imaging or biopsy) are normal (e.g., category G3a GFR/stage A1 level of albuminuria), and irrespective of an individual’s age.
The considerations in favor of a fixed threshold at 60 ml/min per 1.73 m2 in the current CKD definition proposed by KDIGO are as follows:1
Simplicity. Only one number needs to be kept in mind. This argument is understandably relevant for non-nephrologists and patients, but carries the risk of oversimplification of the complexities of kidney pathophysiology.
Biology. A GFR <60 ml/min per 1.73 m2 is believed to represent <50% of the kidney function measured in healthy young adults.1 The choice of 50% of normal function is, however, arbitrary, and whether GFR in healthy young adults is actually about 120 ml/min per 1.73 m2 is debatable. This value was originally based on measured GFR (mGFR) values compiled and published in 1969 by Wesson.12 More recent studies have shown that median GFR values in healthy young adults are <120 ml/min per 1.73 m2.13–15 Indeed, one meta-analysis of mGFR data in 5482 living kidney donors found normal mean GFR values of 106.7 ml/min per 1.73 m2 at ages 20–30 years.14 Such values were also observed in a large cohort of 2007 French living kidney donors <40 years of age, with a mean mGFR of 107.2 ml/min per 1.73 m2.15
Prognosis. The third argument for a threshold at 60 ml/min per 1.73 m2 was based on the association of lower GFR values with increased morbidity and mortality. Many large epidemiologic studies, especially from the CKD Prognosis Consortium, have seemingly supported the choice of the 60 ml/min per 1.73 m2 threshold for CKD. We will discuss this argument in depth below.
The Prognostic Argument for an Age-Adapted Definition of CKD
Absolute risks of mortality are typically higher in older patients simply because of the limited human life span. Regarding relative risk, several studies from the CKD Prognosis Consortium have demonstrated that GFR <60 ml/min per 1.73 m2 was independently associated with adverse outcomes, particularly cardiovascular events and all-cause mortality,16–28 thereby confirming findings from the seminal study published by Go et al.29 in 2004. Of note, most of the Consortium analyses of GFR and risk of adverse events in both high-risk and general populations use as the reference group participants with only a single eGFR available (hence, no confirmation of chronicity) of ≥95 ml/min per 1.73 m2.16–28 However, the Consortium’s 2012 meta-analysis, which was dedicated to age and included more than 2-million individuals from 46 different cohorts (33 from the general population and 13 CKD cohorts), used 80 ml/min per 1.73 m2 as the reference group eGFR rather than 95 ml/min per 1.73 m2.17 The associations with mortality and ESKD remained significant when eGFR was <60 ml/min per 1.73 m2 in all age categories, although hazard ratios were much lower in older people.17 Although the risk of ESKD was increased, the progression to ESKD in elderly patients with an eGFR of 45–59 ml/min per 1.73 m2 and no abnormal urine ACR is very rare (<1% risk in 5 years using the Kidney Failure Risk Equation).30
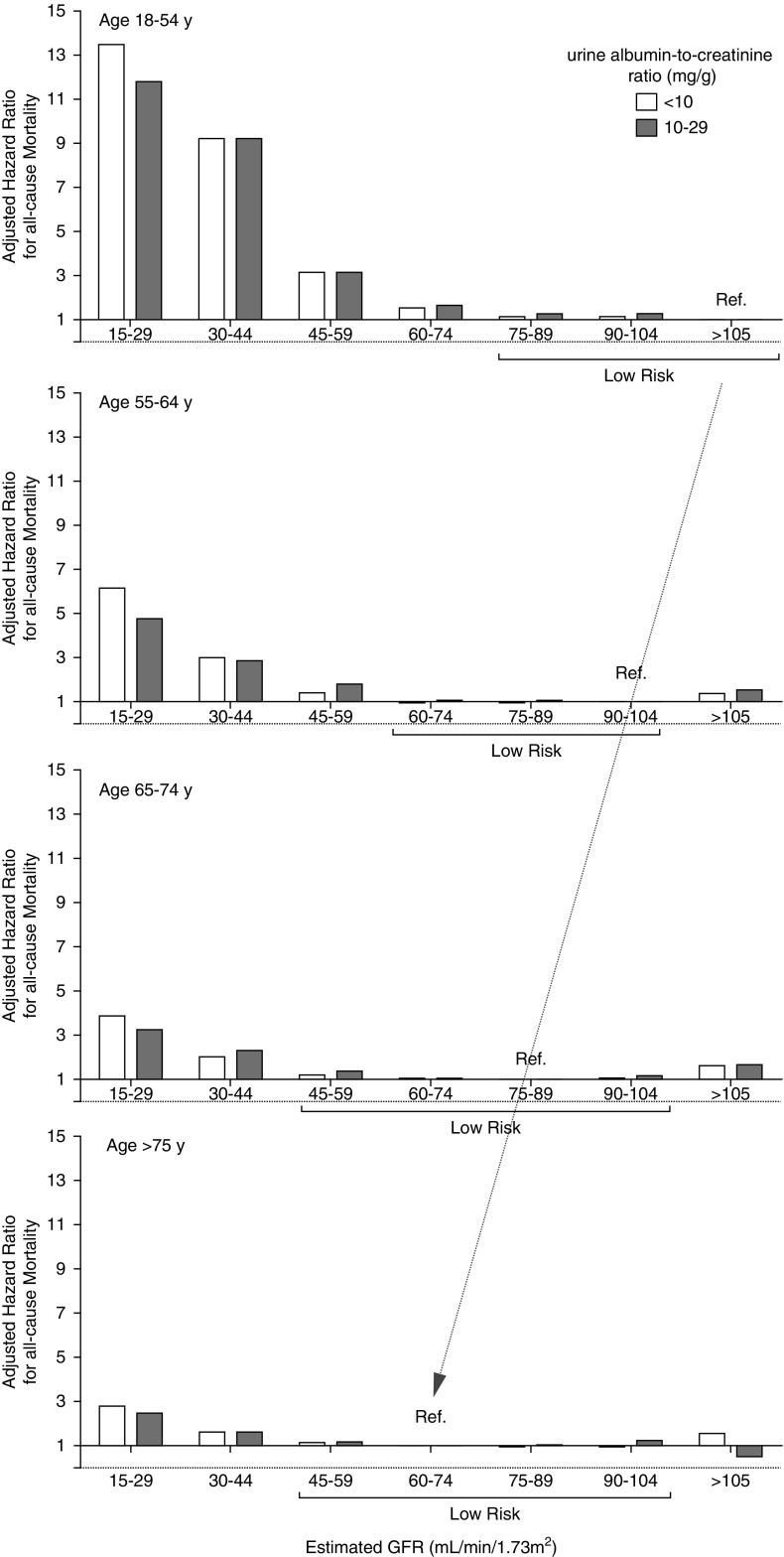
Given the critical importance of the choice of the reference group in such analyses, others have reanalyzed the data from the CKD Prognosis Consortium for mortality using different reference groups based on age (Figure 1).31–34 In these analyses,31,34 the reference eGFR group in each age category was defined as the one with the lowest mortality risk (in subsets with urine ACR <10 or 10–29 mg/g). The results revealed that, in the 55–64 years age category (reference eGFR 90–104 ml/min per 1.73 m2), the mortality risk began to increase when GFR fell below 60 ml/min per 1.73 m2. However, for people older than 65 years (reference eGFR 75–89 ml/min per 1.73 m2), the risk was trivial until the eGFR had fallen below 45 ml/min per 1.73 m2. In the youngest age category of 18–54 years (reference eGFR >105 ml/min per 1.73 m2), the risk of mortality started to increase when eGFR was <75 ml/min per 1.73 m2.31–34 Therefore, an age-specific analysis of the data used by the CKD Prognosis Consortium provides a strong argument for an age-adapted definition of CKD using appropriate prognostic strata for age.
Figure 1.
The association between eGFR and all-cause mortality depends on the age group. Hazard ratio for mortality when the reference group is the one with the lowest risk. eGFR ranges are within the brackets (low risk) and are not significantly different from the reference group (from Denic et al.34).
Tables 2 and 3 summarize the studies on associations between eGFR and risk of adverse events outside of the CKD Prognosis Consortium. The analysis considered only published full-length articles. We included studies that used creatinine-based equations (Modification of Diet in Renal Disease study or CKD Epidemiology Collaboration [CKD-EPI] equations) and reported adjusted risks of cardiovascular or all-cause mortality.29,35–55 We excluded studies that had only participants with eGFR categories G3–G5 and those without older individuals. Instead, we focused on studies that were performed in elderly individuals or reported results in separate age categories. Our main hypothesis was that the increased risk of mortality associated with lower eGFR differs across age categories and, notably, that an eGFR of 45–60 ml/min per 1.73 m2 in older age groups is not associated with excess mortality.
Table 2.
Characteristics of studies that investigated outcomes in relation to GFR in general populations
| Author (reference) | Study Name | Country | Time Period of Data Collection | Number of Subjects (N) | Age in years (mean±SD/median and IQR) and Other Potentially Relevant Characteristics | Follow-Up Time (years) | Clinical Cohort/General Population |
|---|---|---|---|---|---|---|---|
| Manjunath et al.35 | Cardiovascular Health Study | United States | 1989–1990 | 4893 | 73.4 (mean) | 5.05 (maximum) | GP |
| Go et al.29 | Kaiser Permanente Renal Registry | United States | 1996–2000 | 1,120,295 | 52.2±16.3 (mean±SD) | 2.84 (median) 1.65–4.01 (IQR) | GP (health insurer) |
| O’Hare et al.36 | Department of Veterans Affairs | United States | 2001–2002 | 2,583,911 | 63.6±14 (mean±SD) 95% men | 3.17±0.62 (mean±SD) | GP (health care provider) |
| Maaravi et al.37 | Jerusalem Seventy-Year-Old Longitudinal Study | Israel | 1990–1991 | 441 | 70 (all) | 12 (maximum) | GP |
| Hallan et al.38 | HUNT II | Norway | 1995–1997 | 9709 | All with DM or treated HT plus 5% random sample. DM/HT age 65.9±11.9 (mean±SD); random non-DM/HT age 49.6±16.0 (mean±SD) | 8.3 (median) | GP (health survey); population based, but in fact a “high-risk” study population |
| Raymond et al.56 | NA | United Kingdom | 2000–2003 | 106,366 | 57.7±19.1 (mean±SD) | 3 (maximum) | GP |
| Brantsma et al.39 | PREVEND | Netherlands | 1997–1998 | 8495 | 49.2±12.7 (mean±SD) | 7.5 (median) 6.9–7.8 (IQR) | GP (oversampling of individuals with elevated ACR levels) |
| Hwang et al.40 | Elderly Health Examination Program | Taiwan | 2002–2004 | 35,529 | 75.7±5.3 (mean±SD) | From 2.6±0.3 (mean±SD) for eGFR ≥60 ml/min to 2.3±0.7 (mean±SD) for stage 5 | GP |
| Roderick et al.41 | MRC General Practice Research Framework | United Kingdom | 1994–1999 | 13,177 | 80.2 (median) IQR 6.9 | 7.3 (median) IQR 5 | GP (primary care) |
| Van der Velde et al.42 | PREVEND | Netherlands | 1997–1998 | 8047 | 49±13 (mean±SD) | 7.0±1.6 (mean±SD) | GP (oversampling of individuals with elevated ACR levels) |
| Muntner et al.43 | REGARDS | United States | 2003–2007 | 24,350 | ≥45 | 4.5 (median) | GP (oversampling of black people) |
| Stengel et al.44 | Three-City | France | 1999–2001 | 8705 | 74.3±5.5 (mean±SD) | 6 (maximum) | GP |
| Van Pottelbergh et al.45 | BELFRAIL | Belgium | 2008–2009 | 539 | 84.7±3.6 (mean±SD) | 2.9±0.3 | GP (primary care) |
| Oh et al.46 | KloSHA | Korea | 2005–2006 | 949 | 75.8±9.0 (mean±SD) | 5.3±1.4 (mean±SD) | GP |
| Minutolo et al.47 | Health Search/Cegedim Strategic Data Longitudinal Patient Database | Italy | 2003–2005 | 30,326 | 71.0±11.0 (mean±SD) | 7.2 (median) 4.7–7.7 (IQR) | GP (primary care); population without nephrology consultation at baseline |
| Malmgren et al.48 | OPRA | Sweden | NA | 1011 | 75.2±0.2 (mean±SD) 100% women | 10 (all) | GP |
| Chowdhury et al.49 | ANBP2 | Australia | NA | 6083 | 71.9±4.9 (mean±SD) | 10.8 (median) 9.6–11.4 (IQR) | RCT participants; hypertensive population |
| Nagai et al.50 | Ibaraki Prefecture | Japan | 1993 | 89,547 | Men 60.2 (mean) Women 57.8 (mean) | 17.1 (mean) | GP (exclusion of those with history of CVD) |
| Corsonello et al.51 | InChianti | Italy | 1998–2000 | 828 | 74.4±6.9 (mean±SD) | 9 (maximum) | GP |
| Wu et al.52 | Kailuan Study | China | 2006–2007 | 95,391 | 52.0±12.6 (mean±SD) | 8 (maximum) | GP |
GP, general population; IQR, interquartile range; DM, diabetes mellitus; HT, hypertension; NA, not available; HUNT, Nord-Trøndelag Health Study; PREVEND, Prevention of Renal and Vascular Endstage Disease; MRC, Medical Research Council; REGARDS, Reasons for Geographic and Racial Differences in Stroke; KloSHA, Korean Longitudinal Study on Health and Aging; OPRA, Osteoporosis Risk Assessment; ANBP2, Second Australian National Blood Pressure Study; RCT, randomized controlled trial; CVD, cardiovascular disease.
Table 3.
Findings of studies that investigated outcomes in relation to GFR in general populations
| Author (reference) | Study Name | eGFR/ACR (GFR equation) | Outcome Studied (ACM or CVM) | Comparison Made and Reference Category | Adjusted Hazard Ratios in Exposure Categories | Comments |
|---|---|---|---|---|---|---|
| Manjunath et al.35 | Cardiovascular Health Study | MDRD | ACM | 90–130 ml/min per 1.73 m2 | 60–89 ml/min 1.05 (0.78–1.41) 15–59 ml/min 1.47 (1.05–2.06) | |
| Go et al.29 | Kaiser Permanente Renal Registry | MDRD | ACM CV events | ≥60 ml/min per 1.73 m2 | ACM: | In a subgroup where chronicity was confirmed (repeated serum creatinine measurements) (n=172,144), eGFR at 45–59 ml/min was not associated with ACM 1.0 (1.0–1.1) |
| 45–59 ml/min 1.2 (1.1–1.2) | ||||||
| 30–44 ml/min 1.8 (1.7–1.9) | ||||||
| 15–29 ml/min 3.2 (3.1–3.4) | ||||||
| <15 ml/min 5.9 (5.4–6.5) | ||||||
| CV events: | ||||||
| 45–59 ml/min 1.4 (1.4–1.5) | ||||||
| 30–44 ml/min 2.0 (1.9–2.1) | ||||||
| 15–29 ml/min 2.8 (2.6–2.9) | ||||||
| <15 ml/min 3.4 (3.1–3.8) | ||||||
| O’Hare et al.36 | Department of Veterans Affairs | MDRD | ACM | ≥60 ml/min per 1.73 m2 | 18–44 yr: | In younger age categories, adjusted HRs were higher and statistically significant already from 50 to 59 ml/min. In younger people and elderly with stable eGFR adjusted HRs were lower in all eGFR categories, 50–59 ml/min was not associated with ACM. Findings suggest that mortality risk stratification in younger and elderly people should not be based on the same eGFR cut-off points |
| 50–59 ml/min 1.56 (1.30–1.88) | ||||||
| 40–49 ml/min 1.90 (1.35–2.67) | ||||||
| 30–39 ml/min 3.58 (2.54–5.05) | ||||||
| 45–54 yr: | ||||||
| 50–59 ml/min 1.27 (1.19–1.36) | ||||||
| 40–49 ml/min 1.89 (1.74–2.06) | ||||||
| 30–39 ml/min 2.89 (2.63–3.18) | ||||||
| 55–64 yr: | ||||||
| 50–59 ml/min 1.18 (1.13–1.23) | ||||||
| 40–49 ml/min 1.75 (1.65–1.85) | ||||||
| 30–39 ml/min 2.43 (2.27–2.59) | ||||||
| 65–74 yr: | ||||||
| 50–59 ml/min 1.02 (0.99–1.05) | ||||||
| 40–49 ml/min 1.35 (1.32–1.39) | ||||||
| 30–39 ml/min 1.81 (1.75–1.87) | ||||||
| 75–84 yr: | ||||||
| 50–59 ml/min 1.02 (0.99–1.04) | ||||||
| 40–49 ml/min 1.21 (1.18–1.23) | ||||||
| 30–39 ml/min 1.55 (1.51–1.58) | ||||||
| 85+ yr: | ||||||
| 50–59 ml/min 1.02 (0.97–1.06) | ||||||
| 40–49 ml/min 1.10 (1.05–1.15) | ||||||
| 30–39 ml/min 1.36 (1.29–1.44) | ||||||
| Maaravi et al.37 | Jerusalem Seventy-Year-Old Longitudinal Study | MDRD CG Mayo Clinic | ACM | ≥60 ml/min per 1.73 m2 Results presented for MDRD | <60 ml/min 1.19 (0.83–1.71) | |
| Hallan et al.38 | HUNT II | MDRD | CVM | ≥75 ml/min per 1.73 m2 and optimal ACR; ACR below sex-specific median (<5 and 7 mg/g in men and women) | <70 yr: | |
| Optimal ACR: | ||||||
| 60–74 ml/min 1.17 (0.35–3.91) | ||||||
| 45–59 ml/min 0.73 (0.26–2.02) | ||||||
| <45 ml/min 1.08 (0.19–6.10) | ||||||
| High normal ACR: | ||||||
| 60–74 ml/min 1.53 (0.55–4.26) | ||||||
| 45–59 ml/min 3.29 (1.02–10.6) | ||||||
| <45 ml/min 2.57 (0.88–7.51) | ||||||
| Micro-albuminuria: | ||||||
| 60–74 ml/min 1.92 (0.71–5.16) | ||||||
| 45–59 ml/min 2.22 (0.87–5.70) | ||||||
| <45 ml/min 5.94 (2.06–17.2) | ||||||
| ≥70 yr: | ||||||
| Optimal ACR: | ||||||
| 60–74 ml/min 0.79 (0.30–2.10) | ||||||
| 45–59 ml/min 2.48 (0.76–8.13) | ||||||
| <45 ml/min 1.49 (0.46–4.86) | ||||||
| High normal ACR: | ||||||
| 60–74 ml/min 1.68 (0.61–4.69) | ||||||
| 45–59 ml/min 1.93 (0.63–5.92) | ||||||
| <45 ml/min 4.70 (1.57–14.1) | ||||||
| Micro-albuminuria: | ||||||
| 60–74 ml/min 3.80 (1.33–10.80) | ||||||
| 45–59 ml/min 4.09 (1.52–10.90) | ||||||
| <45 ml/min 8.38 (2.83–24.9) | ||||||
| Raymond et al.56 | NA | MDRD | ACM | ≥60 ml/min per 1.73 m2 | 20–44 yr: | |
| Stage 3a 13.6 (6.2–29.8) | ||||||
| Stage 3b 12.1 (4.0–36.5) | ||||||
| Stage 4 17.4 (5.9–51.4) | ||||||
| Stage 5 26.1 (9.1–74.8) | ||||||
| 45–54 yr: | ||||||
| Stage 3a 7.5 (4.4–12.6) | ||||||
| Stage 3b 13.6 (7.5–24.7) | ||||||
| Stage 4 4.6 (1.2–17.4) | ||||||
| Stage 5 28.6 (17.4–47.2) | ||||||
| 55–64 yr: | ||||||
| Stage 3a 3.0 (2.2–4.1) | ||||||
| Stage 3b 5.9 (3.9–8.9) | ||||||
| Stage 4 9.3 (6.1–14.2) | ||||||
| Stage 5 18.2 (13.9–23.9) | ||||||
| 65–74 yr: | ||||||
| Stage 3a 1.8 (1.5–2.1) | ||||||
| Stage 3b 3.2 (2.6–3.9) | ||||||
| Stage 4 5.2 (4.1–6.5) | ||||||
| Stage 5 7.6 (5.7–10.1) | ||||||
| 75–84 yr: | ||||||
| Stage 3a 1.2 (1.0–1.3) | ||||||
| Stage 3b 1.9 (1.7–2.1) | ||||||
| Stage 4 3.3 (2.9–3.8) | ||||||
| Stage 5 4.4 (3.7–5.3) | ||||||
| 85+ yr: | ||||||
| Stage 3a 0.9 (0.8–1.0) | ||||||
| Stage 3b 1.3 (1.2–1.5) | ||||||
| Stage 4 1.8 (1.7–2.0) | ||||||
| Stage 5 2.5 (2.3–2.8) | ||||||
| Brantsma et al.39 | PREVEND | MDRD ACR | CVM and CV hospitalization combined | No CKD | Stage 1 2.2 (1.5–3.3) | |
| Stage 2 1.6 (1.3–2.0) | ||||||
| Stage 3 1.3 (1.0–1.7) | ||||||
| Stage 3 with UAE <30 mg/24 h 1.0 (0.7–1.4) | ||||||
| Stage 3 with UAE >30 mg/24 h 1.6 (1.1–2.3) | ||||||
| Hwang et al.40 | Elderly Health Examination Program | MDRD | ACM CVM | ≥60 ml/min per 1.73 m2 | ACM: | |
| 45–59 ml/min 1.10 (1.0–1.2) | ||||||
| 30–44 ml/min 1.52 (1.3–1.8) | ||||||
| 15–29 ml/min 2.1 (1.7–2.6) | ||||||
| <15 ml/min 2.55 (1.8–3.6) | ||||||
| CVM: | ||||||
| 45–59 ml/min 1.30 (1.0–1.7) | ||||||
| 30–44 ml/min 2.42 (1.7–3.4) | ||||||
| 15–29 ml/min 3.62 (2.3–5.8) | ||||||
| <15 ml/min 3.22 (1.3–8.3) | ||||||
| Roderick et al.41 | MRC General Practice Research Framework | MDRD Dipstick proteinuria | ACM CVM in those without CVD at baseline | ≥60 ml/min per 1.73 m2; proteinuria negative | ACM after 0–2 yr: | Short-term (0–2 yr) eGFR-related risk is higher than long term (>2 yr) risk (not shown) |
| Men: | ||||||
| 45–59 ml/min 1.13 (0.93–1.37) | ||||||
| 30–44 ml/min 1.69 (1.26–2.28) | ||||||
| <30 ml/min 3.87 (2.78–5.38) | ||||||
| Women: | ||||||
| 45–59 ml/min 1.14 (0.93–1.40) | ||||||
| 30–44 ml/min 1.33 (1.06–1.68) | ||||||
| <30 ml/min 2.44 (1.68–3.56) | ||||||
| CVM after 0–2 yr: | ||||||
| Men: | ||||||
| 45–59 ml/min 1.67 (1.15–2.43) | ||||||
| 30–44 ml/min 1.60 (0.94–2.73) | ||||||
| <30 ml/min 2.89 (1.22–6.84) | ||||||
| Women: | ||||||
| 45–59 ml/min 1.59 (1.01–2.50) | ||||||
| 30–44 ml/min 1.45 (0.93–2.28) | ||||||
| <30 ml/min 3.80 (1.87–7.75) | ||||||
| ACM: | ||||||
| Men: | ||||||
| Proteinuria positive | ||||||
| >60 ml/min 1.29 (1.07–1.56) | ||||||
| 45–59 ml/min 1.25 (1.02–1.52) | ||||||
| 30–44 ml/min 1.08 (0.82–1.42) | ||||||
| <30 ml/min 0.95 (0.56–1.59) | ||||||
| Women: | ||||||
| Proteinuria positive | ||||||
| >60 ml/min 1.19 (0.96–1.47) | ||||||
| 45–59 ml/min 0.94 (0.77–1.15) | ||||||
| 30–44 ml/min 1.39 (1.10–1.77) | ||||||
| <30 ml/min 1.70 (1.15–2.52) | ||||||
| CVM: | ||||||
| Men: | ||||||
| Proteinuria positive | ||||||
| >60 ml/min 1.05 (0.70–1.57) | ||||||
| 45–59 ml/min 1.31 (0.91–1.89) | ||||||
| 30–44 ml/min 0.83 (0.47–1.46) | ||||||
| <30 ml/min 0.97 (0.35–2.68) | ||||||
| Women: | ||||||
| Proteinuria positive | ||||||
| >60 ml/min 1.18 (0.80–1.74) | ||||||
| 45–59 ml/min 0.93 (0.65–1.32) | ||||||
| 30–44 ml/min 1.34 (0.88–2.03) | ||||||
| <30 ml/min 2.79 (1.40–5.54) | ||||||
| Van der Velde et al.42 | PREVEND | MDRD CKD-EPI SCr CysC SCr-CysC Creatinine clearance | Fatal and nonfatal CV events | +10 ml/min per 1.73 m2 increase in eGFR. Results presented for CKD-EPI | <60 yr: | The association between eGFR and risk of CV events is weaker in elderly subjects than in younger subjects |
| 0.70 (0.62–0.79) | ||||||
| ≥60 yr: | ||||||
| 1.02 (0.92–1.13) | ||||||
| Muntner et al.43 | REGARDS | CKD-EPI ACR | ACM | ≥60 ml/min per 1.73 m2 | 45–59 yr: | If ACR is <10 mg/g, the results are similar: |
| 45–59 yr: | ||||||
| 45–60 ml/min 2.5 (1.3–4.6) | 45–60 ml/min 4.5 (1.8–11.1) | |||||
| <45 ml/min 3.5 (1.8–6.8) | <45 ml/min 4.7 (0.7–34.2) | |||||
| 60–69 yr: | 60–69 yr: | |||||
| 45–60 ml/min 1.7 (1.3–2.3) | 45–60 ml/min 1.9 (1.2–3.1) | |||||
| <45 ml/min 2.2 (1.6–3.0) | <45 ml/min 2.5 (1.0–6.1) | |||||
| 70–79 yr: | 70–79 yr: | |||||
| 45–60 ml/min 1.1 (0.9–1.3) | 45–60 ml/min 1.1 (0.8–1.6) | |||||
| <45 ml/min 1.9 (1.5–2.4) | <45 ml/min 2.1 (1.2–3.6) | |||||
| ≥80 yr: | ≥80 yr: | |||||
| 45–60 ml/min 1.3 (1.0–1.7) | 45–60 ml/min 1.4 (0.9–2.2) | |||||
| <45 ml/min 1.5 (1.1–2.0) | <45 ml/min 1.6 (0.9–2.8) | |||||
| Stengel et al.44 | Three-City | CKD-EPI MDRD | ACM CVM | ≥75–89 ml/min per 1.73 m2; results presented for CKD-EPI | ACM: | |
| 60–74 ml/min 0.9 (0.8–1.1) | ||||||
| 45–59 ml/min 1.1 (0.9–1.3) | ||||||
| 30–44 ml/min 2.0 (1.5–2.7) | ||||||
| <30 ml/min 3.3 (2.0–5.5) | ||||||
| CVM: | ||||||
| 60–74 ml/min 0.9 (0.6–1.3) | ||||||
| 45–59 ml/min 1.6 (1.1–2.3) | ||||||
| 30–44 ml/min 3.1 (1.8–5.0) | ||||||
| <30 ml/min 4.3 (1.8–10.2) | ||||||
| Van Pottelbergh et al.45 | BELFRAIL | MDRD CKD-EPI SCr CKD-EPI CysC CKD-EPI SCr-CysC BIS-2 SCr-CysC | ACM and RRT combined | 60–90 ml/min per 1.73 m2; results presented for CKD-EPI SCr | 45–60 ml/min 1.65 (1.05–2.61) | |
| 30–45 ml/min 1.72 (1.03–2.88) | ||||||
| <30 ml/min 5.04 (2.95–8.60) | ||||||
| Oh et al.46 | KLoSHA | CKD-EPI Disptick proteinuria | ACM | ≥90 ml/min per 1.73 m2; proteinuria negative | 60–89 ml/min 1.37 (0.75–2.52) | If proteinuria: Trace 1.24 (0.78–1.96) ≥1+1.73 (1.13–2.63) |
| 45–59 ml/min 1.65 (0.84–3.25) | ||||||
| <45 ml/min 2.36 (1.17–4.75) | ||||||
| Minutolo et al.47 | Health Search/Cegedim Strategic Data Longitudinal Patient Database | MDRD | ACM | ≥60 ml/min per 1.73 m2 | ACM: | |
| Stage 3a 1.11 (0.99–1.23) | ||||||
| Stage 3b 1.66 (1.49–1.86) | ||||||
| Stage 4 2.75 (2.41–3.13) | ||||||
| Stage 5 2.54 (2.01–3.22) | ||||||
| Malmgren et al.48 | OPRA | CKD-EPI MDRD Revised Lund-Malmö BIS-1 CG | ACM | ≥60 ml/min per 1.73 m2; results presented for CKD-EPI | 75–80 yr: | |
| 45–60 ml/min 1.1 (0.6–2.0) | ||||||
| 0–45 ml/min 4.5 (2.2–9.2) | ||||||
| 75–85 yr: | ||||||
| 45–60 ml/min 1.4 (1.0–1.9) | ||||||
| 0–45 ml/min 3.5 (2.1–5.8) | ||||||
| 80–85 yr: | ||||||
| 45–60 ml/min 1.7 (1.1–2.6) | ||||||
| 0–45 ml/min 2.6 (1.4–5.0) | ||||||
| Chowdhury et al.49 | ANBP2 | MDRD CKD-EPI | ACM CVM | ≥60 ml/min per 1.73 m2; results presented for CKD-EPI | ACM: | |
| 45–59 ml/min 1.13 (1.01–1.27) | ||||||
| 30–44 ml/min 1.65 (1.37–1.99) | ||||||
| <30 ml/min 5.16 (3.17–8.42) | ||||||
| CVM: | ||||||
| 45–59 ml/min 1.05 (0.89–1.23) | ||||||
| 30–44 ml/min 1.64 (1.27–2.13) | ||||||
| <30 ml/min 5.60 (2.32–13.51) | ||||||
| Nagai et al.50 | Ibaraki Prefecture | MDRD | ACM CVM | ≥60 ml/min per 1.73 m2 | ACM: | |
| Men: | ||||||
| 40–69 yr: | ||||||
| 45–49 ml/min 1.33 (1.06–1.67) | ||||||
| 30–44 ml/min 1.53 (1.20–1.96) | ||||||
| 70–80 yr: | ||||||
| 45–49 ml/min 1.02 (0.82–1.25) | ||||||
| 30–44 ml/min 1.63 (1.33–2.00) | ||||||
| Women: | ||||||
| 40–69 yr: | ||||||
| 45–49 ml/min 1.50 (1.27–1.78) | ||||||
| 30–44 ml/min 2.21 (1.81–2.71) | ||||||
| 70–80 yr: | ||||||
| 45–49 ml/min 1.19 (1.02–1.38) | ||||||
| 30–44 ml/min 1.53 (1.31–1.79) | ||||||
| CVM: | ||||||
| Men: | ||||||
| 40–69 yr: | ||||||
| 45–49 ml/min 1.82 (1.23–2.69) | ||||||
| 30–44 ml/min 1.65 (1.04–2.62) | ||||||
| 70–80 yr: | ||||||
| 45–49 ml/min 1.03 (0.72–1.48) | ||||||
| 30–44 ml/min 1.37 (0.93–2.02) | ||||||
| Women: | ||||||
| 40–69 yr: | ||||||
| 45–49 ml/min 1.34 (0.98–1.82) | ||||||
| 30–44 ml/min 2.24 (1.58–3.17) | ||||||
| 70–80 yr: | ||||||
| 45–49 ml/min 1.43 (1.14–1.79) | ||||||
| 30–44 ml/min 1.57 (1.23–2.00) | ||||||
| Corsonello et al.51 | InChianti | CKD-EPI SCr BIS-1 SCr FAS CKD-EPI SCr-CysC BIS-2 SCr-CysC | ACM | ≥90 ml/min per 1.73 m2; results presented for CKD-EPI SCr | 60–89.9 ml/min 1.63 (0.84–3.17) | |
| 45–59.9 ml/min 2.50 (1.21–5.15) | ||||||
| 30–44.9 ml/min 5.44 (1.10–27.7) | ||||||
| <30 ml/min 7.42 (1.79–30.6) | ||||||
| Wu et al.52 | Kailuan Study | CKD-EPI Dipstick proteinuria | ACM | ≥ 90 ml/min per 1.73 m2 | All: | |
| 60–89 ml/min 1.01 (0.93–1.09) | ||||||
| 45–59 ml/min 1.11 (0.99–1.24) | ||||||
| <45 ml/min 1.51 (1.30–1.74) | ||||||
| Men: | ||||||
| 60–89 ml/min 1.01 (0.94–1.10) | ||||||
| 45–59 ml/min 1.11 (0.99–1.23) | ||||||
| <45 ml/min 1.35 (1.17–1.57) | ||||||
| Women: | ||||||
| 60–89 ml/min 1.65 (1.16–2.34) | ||||||
| 45–59 ml/min 1.92 (1.25–2.96) | ||||||
| <45 ml/min 4.11 (2.50–6.76) |
ACM, all-cause mortality; CVM, cardiovascular mortality; MDRD, Modified Diet in Renal Disease Study equation; CV, cardiovascular; HR, hazard ratio; CG, Cockcroft and Gault formula; MRC, Medical Research Council; CVD, cardiovascular disease; HUNT, Nord-Trøndelag Health Study; PREVEND, Prevention of Renal and Vascular Endstage Disease; CysC, cystatin C; REGARDS, Reasons for Geographic and Racial Differences in Stroke; KLoSHA, Korean Longitudinal Study on Health and Aging; NA, not available; OPRA, Osteoporosis Risk Assessment; ANBP2, Second Australian National Blood Pressure Study; SCr, serum creatinine; BIS1, Berlin Initiative Study; FAS, full age spectrum.
When looking at studies that presented a separate eGFR category of 45–60 ml/min per 1.73 m2 and used eGFR >60 ml/min per 1.73 m2 as a reference category, only a few studies demonstrated an increased risk,43,45,49,56 whereas others did not.40,41,47,48 The largest study to date included a separate analysis of individuals with an eGFR of 50–60 ml/min per 1.73 m2 in the older age categories. The results showed that, in this eGFR category, the risk of death was not higher than in the category eGFR>60 ml/min per 1.73 m2.36 In addition, the Renal Risk in Derby study deserves particular attention, as it included follow-up data on eGFR.55 A total of 1741 participants, most with confirmed CKD, were prospectively followed for 5 years. The mean age of the cohort was 72.9±9 years, the mean eGFR using the CKD-EPI equation was 54±12 ml/min per 1.73 m2, and most participants had normal urine ACR. After 5 years, 34.1% of the cohort was considered to be stable and 19.3% had even improved their GFR category. Nearly all of the participants who improved their CKD status had been classified as category G3a/A1 at baseline.55 Interestingly, the age- and sex-standardized mortality rates of those with category G3a GFR were similar to those in the general population, whereas those with category G3b or G4 at baseline had higher mortality rates.55,57
Regarding the prognosis argument, we acknowledge that our proposal of an age-adapted definition for CKD is mainly based on mortality risk. We did not consider other outcomes, even though other publications have reported the risk of lower GFR with classic metabolic complications of CKD (anemia, hyperparathyroidism, acidosis, hyperphosphoremia)58,59 and other clinical complications (such as frailty, impaired quality of life, and fracture).60,61 These studies, unfortunately, are of little utility in informing our proposal of an age-adapted threshold. Although higher risk of these complications is frequently observed when eGFR is <45 ml/min per 1.73 m2,58 results are much more variable at higher eGFRs (unlike mortality, the definitions of specific complications or of clinical status are not uniform).
In summary, most studies showed no or a trivial additional mortality risk for older adult participants with an eGFR of 45–59 ml/min per 1.73 m2 and normal urine ACR. Prognostic arguments thus favor an age-adapted threshold for eGFR in the CKD definition.
Kidney Senescence as an Argument for an Age-Adapted Definition of CKD
Another concern with a GFR threshold fixed at 60 ml/min per 1.73 m2 is that it fails to account for the distinct microstructural and macrostructural differences between the aging kidney and kidneys affected by CKD. It also does not take into account the fact that a substantial proportion of healthy older people have an mGFR of <60 ml/min per 1.73 m2.
Structural Differences Between Aging Kidney and CKD
Among healthy kidney donors, aging is reflected by an indolent nephrosclerosis, characterized by arteriosclerosis, ischemic globally (but not segmentally) sclerotic glomeruli, and interstitial fibrosis and tubular atrophy.62 Although the interstitial fibrosis and tubular atrophy that occur with aging are fairly minimal,62 there is a substantial nephron loss and dropout (from about 1,000,000 nephrons per kidney in healthy adults aged 18–29 years to 500,000 per kidney in healthy individuals aged 70–75 years).63 Despite this substantial nephron loss with age, there is no compensation by the remaining nephrons because glomerular volume, single-nephron GFR, and single-nephron glomerular filtration capacity remain stable.63–65
CKD, on the other hand, is often characterized by disease-specific pathology that differs from age-induced nephrosclerosis. CKD can include unique microstructural findings (such as specific immunofluorescence staining patterns) or macrostructural findings (such as polycystic kidney or renal artery stenosis) that are not seen with aging alone. Although risk factors for CKD such as obesity, diabetes, and hypertension are associated with nephrosclerosis, they are also associated with glomerular enlargement, segmental glomerulosclerosis, and higher single-nephron GFR in intact nonsclerotic glomeruli.63,64 Only when the degree of global glomerulosclerosis exceeds that expected for age or when there is increased metabolic demand (e.g., obesity and hyperglycemia) is there an increase in single-nephron GFR. Therefore, application of age-adapted thresholds for glomerulosclerosis is also useful with kidney biopsies performed in clinical care, as only glomerulosclerosis exceeding that expected for age is a risk factor for CKD progression.66,67
Decline of GFR with Aging
As already stated, the definition of normality for laboratory results can also be obtained by the distribution of the results in healthy populations. Establishing reference interval values with a fixed threshold, as per the KDIGO guidelines, would mean that the GFR reference values are constant across all age categories.13,14,68–81 However, more reliable studies, using mGFR and living kidney donors or healthy individuals selected from the general population, indicate a clear decrease in GFR with age13–15,64,68–90 and show that the rate of mGFR decline becomes significant after age 40 years.2,12–15,73,76,80,85,88,91,92 Importantly, such a decline in mGFR with aging has been established on different continents and in different ethnic groups.68,77,79–81,87,89 From these data, it is obvious that a substantial proportion of healthy older people have an mGFR of <60 ml/min per 1.73 m2, despite the paucity of studies focusing on the elderly and using mGFR.
Regarding eGFR,93–95 available cross-sectional studies from different parts of the world confirmed that many people older than 65 years of age have an eGFR value <60 ml/min per 1.73 m2, suggesting a rather ubiquitous decline of eGFR with age.13,68,96–101 Unfortunately, the few published longitudinal studies have shown discrepancies in the rate of kidney function decline or suffered from methodological limitations, such as use of eGFR or 24-hour creatinine clearance, inclusion of nonhealthy individuals, limited follow-up duration, and study attrition, making it difficult to draw a definitive conclusion about the magnitude of the average rate of GFR decline with aging.
Despite these limitations, all studies have shown a significant decline in GFR with aging in the majority of healthy participants.48,96,102–114 The only longitudinal study using mGFR in a healthy general population is the Renal Iohexol Clearance Survey in Tromsø 6, which included a representative sample of 1594 white people aged 50–62 years from the general population without CKD, diabetes, or cardiovascular disease. The iohexol clearance measurement was repeated in 1299 (81%) patients after a median period of 5.6 years. The authors showed a mean GFR decline rate of 0.84±2.00 ml/min per year (or 0.95±2.23 ml/min per 1.73 m2 per year). Although this may be the most valid study to date, it nevertheless was limited by its inclusion of only middle-aged white people and by its relatively short follow-up, with only two measurements in the majority of participants.114
Proposals for an Age-Adapted CKD Definition
The concept of an age-adapted definition of CKD is not new and has been proposed by a number of authors.2,3,8,10,31,33,34,36,64,98,99,115–124 Such adaptation could be achieved in different ways. We emphasize that the suggested change in CKD definition should pertain only to people without other evidence of kidney damage (notably those with normal urine ACR).
Age-Related Percentiles of GFR
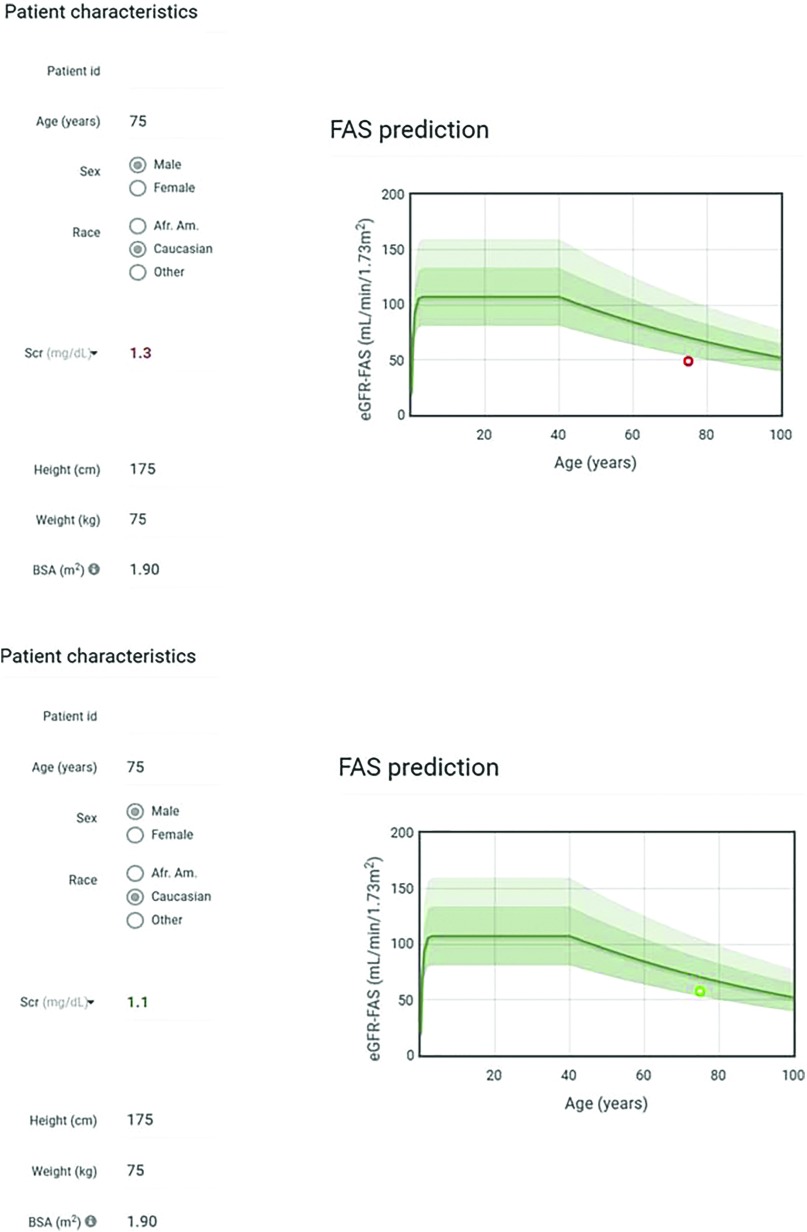
One way to achieve an age-adapted definition of CKD is to refer to percentiles of GFR in the healthy population, which are available in the literature for mGFR or eGFR in different ethnic groups.13,68,96–99 In practice, this would mean interpreting a GFR result in light of age-specific GFR percentiles, and defining CKD as a value below a given percentile in healthy persons (Figure 2). By relating measurements to percentiles using different mGFR or eGFR methods, this approach may overcome differences in mGFR measurement techniques125,126 or eGFR equations.93,94,127 Using percentiles for each year of age minimizes the “birthday paradox,” in which healthy people can become classified as having a disease or individuals with a disease can “recover” simply by becoming 1 year older; this problem is inherent to a single -threshold approach or an age-based approach with only a few thresholds.
Figure 2.
The interpretation of GFR results depends on age. Examples of interpretation of GFR (here GFR estimated using the FAS equation but the same can be applied to measured GFR or eGFR using other estimating equations) according to age and normal percentiles: abnormal (bottom) and normal (below) GFR result. The red circle corresponds to FAS=48 ml/min per 1.73 m2 (serum creatinine [SCr]=1.3 mg/dl corresponds to SCr/Q=1.3/0.9=1.44>1.33) and the green circle corresponds to FAS=58 ml/min per 1.73 m2 (SCr=1.1 mg/dl corresponds to SCr/Q=1.22<1.33). These results are abnormally low and normal predicted eGFR-FAS results with the age-adapted staging, respectively. Dark green shaded area corresponds to reference intervals for mGFR±SD and symmetrical limits for FAS based on SCr/Q=1 (middle line) and SCr/Q=1.33 (lower limit) (14). Light green area corresponds to the upper limit for FAS, based on SCr/Q=0.67. The interval (0.67 to 1.33) is considered the reference interval for SCr/Q. FAS, full age spectrum. Q, median SCr from healthy populations to account for age and sex.
By employing age-specific means and SDs, the individual patient levels can be transformed into a SD score (SDS), a metric commonly used in pediatrics (or even in adults for diagnosing diseases like osteoporosis, using bone mass density). An SDS value of ≤−2 corresponds to an mGFR/eGFR at the 2.5th percentile or lower. Calculation of an SDS requires well characterized reference values across the entire age spectrum. Using these data, GFR SDS can be reported directly by the laboratory, analogous to reporting the eGFR results. The SDS is independent of age and method and is therefore ideal for follow-up. Furthermore, reference values may be included in the laboratory report (Figure 2).
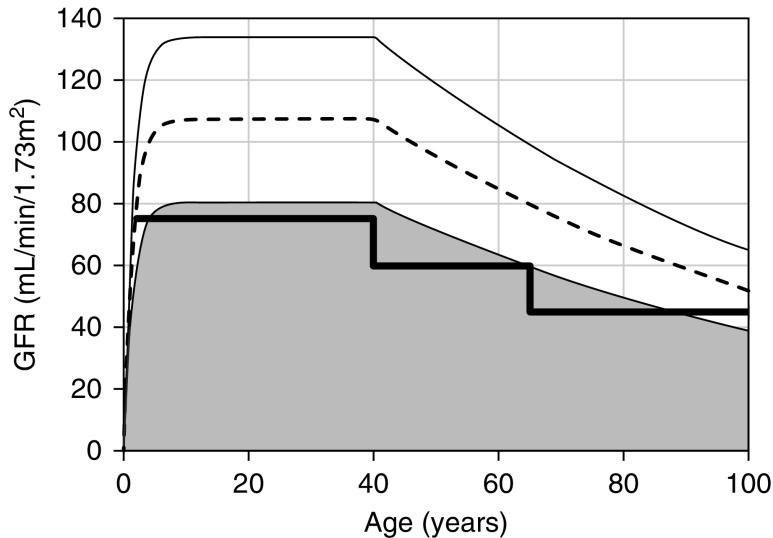
A Limited Set of Age-Specific Thresholds
One can consider the CKD staging based on three pivotal age categories (Figure 3): <40 years, 40–65 years, and >65 years. We suggest GFR cut-offs of 75 ml/min per 1.73 m2 for the youngest group, 60 ml/min per 1.73 m2 for individuals aged 40–65 years, and 45 ml/min per 1.73 m2 for those older than 65 years. In other words, in individuals older than 65 years, the current CKD category G3a/A1 (GFR 45–60 ml/min per 1.73 m2) would not be considered to have CKD. Moreover, younger adults with a GFR <75 ml/min per 1.73 m2 would be considered to have CKD, as their kidney function is below what would be expected for their age.31,34,97,120,123,128,129 The choice of the different GFR thresholds can be justified by associations of these thresholds with prognosis (Figure 1).
Figure 3.
Age-specific thresholds in relation to age-specific GFR percentiles. GFR cut-off values and percentiles according to age (here percentiles of eGFR are calculated using the FAS equation). The bold line represents an age-adapted threshold for CKD: 75 ml/min per 1.73 m2 for age below 40 years, 60 ml/min per 1.73 m2 for age between 40 and 65 years, and 45 ml/min per 1.73 m2 for age above 65 years. The dashed line represents the median (50th percentile) and the thin solid lines represent the 97.5th and 2.5th percentiles. The shaded zone is considered as below the normal reference intervals for GFR (<2.5th percentile).
Potential Effect of an Updated Definition of CKD
A modification of the CKD definition would have a substantial effect on the estimation of CKD prevalence. The KDIGO guidelines used the data from the National Health and Nutrition Examination Survey (NHANES) study (1999–2006) and estimated the CKD prevalence in the US adult general population at 11.5%. Individuals with a GFR of 45–59 ml/min per 1.73 m2 and normal urine ACR represented 3.6% of the general population, and 75% of patients that are classified with CKD solely by the GFR criterion. Individuals with category G3a/A1 represented >30% of all people with CKD.1 CKD categories 3 or 3a are unequivocally the largest or second largest group in terms of CKD prevalence in other studies as well.47,48,55,56,97,123,130–139 The epidemiologic literature clearly shows that CKD prevalence increases with age when using the fixed-threshold CKD definition of 60 ml/min per 1.73 m2.1,48,56,97,101,123,130–134,138–143 Most older subjects defined as having CKD have a GFR of 45–59 ml/min per 1.73 m2 and normal urine ACR, whereas the younger individuals more frequently have elevated urine ACR and GFR >60 ml/min per 1.73 m2.53,97,134,144 Thus, among the 3.6% of the general population with normal urine ACR and a GFR of between 45–59 ml/min per 1.73 m2 in the NHANES (1999–2006) cohort, a large proportion are adults older than 65 years, without any other signs of kidney damage. These individuals would be considered free of disease with the age-adapted definition proposed above. Likewise, results from the MAREMAR (Maladies Rénales Chroniques au Maroc) study crucially illustrate the important effect of an age-adapted definition on the CKD prevalence. Among the 10,524 individuals screened, 2.7% had a confirmed eGFR <60 ml/min per 1.73 m2. However, almost half of those with eGFR <60 ml/min per 1.73 m2 had an eGFR above the third percentile of the population. These people, all older than 55 years and with normal dipstick analysis, would not be considered to have CKD with the age-adapted definition (using age-related percentiles) and the estimated CKD prevalence based on GFR would decrease from 2.7% to 1.8%, a 33% decrease.97
The current fixed GFR threshold of 60 ml/min per 1.73 m2 not only results in overdiagnosis of CKD in the older adults, it may also lead to missed diagnoses of CKD in younger individuals who lack overt signs of kidney damage and have a GFR above the fixed threshold of 60 ml/min per 1.73 m2 but below the lowest percentile for their age. This group may include young people with low-nephron endowment, such as individuals born with a single kidney,145 those born preterm146 or at a low birth weight, patients with Down syndrome,147 or young people with a past history of treatment with nephrotoxic drugs.148 Such individuals are at risk for developing progressive CKD over their remaining lifetime, and may experience associated comorbidities and adverse events, including an increase in mortality.33,97,123,129
Because the availability of curative therapies is limited, treatment of CKD rests on the prevention of progressive kidney damage. The sooner younger people with CKD are identified, the greater the likelihood that poor health outcomes may be prevented. In the MAREMAR study, young individuals with a low-for-age GFR represented 1.3% of the population.97 These persons remain unrecognized in most epidemiologic studies that use a fixed GFR threshold of 60 ml/min per 1.73 m2.97,123 Using SDS, percentiles, or age-adapted staging in the definition of CKD would result in classifying these patients as having a disease. Further research, with a focus on long-term follow-up data, is warranted to elucidate whether such patients should be considered at risk for adverse renal or other disease-related outcomes.
Moving from a CKD definition with a fixed GFR threshold to a definition based on GFR adapted to age has several advantages. These include:
taking into account the physiologic age-related decline in GFR.
fitting with reference distributions of mGFR and eGFR in healthy individuals.
consistency with the observed associations between low GFR and prognosis.
reconciling the two ways to define a disease—namely, the distribution of laboratory findings and the prognostic approach.
facilitating the identification, evaluation, and treatment of younger patients with a GFR that is too low for their age.
avoiding overdiagnosis of CKD in elderly patients.
Use of an age-adapted definition of CKD will also result in a much lower global CKD prevalence (perhaps by as much as 50%), particularly for elderly individuals. However, given that older adults without increased urine ACR or other signs of kidney damage usually have slightly decreased GFR that is physiologic and will on average remain stable (or could even improve) during follow-up, and have a mortality risk similar to those with higher GFR, there is no reason to consider such older individuals as living with a disease that requires investigations, referrals, and even therapeutic interventions with potential side effects.149 At an individual level, applying a CKD status to older people (“D” meaning “disease”) can sometimes be a source of unjustified stress. In some countries, this diagnosis can also lead to adverse consequences in terms of insurance. Using the age-adapted CKD definition could eventually result in more appropriate attention and directing resources to those who are at higher risk of adverse outcomes associated with CKD.
Disclosures
Dr. Jager declared speaker honoraria from Fresenius and received grant support from European Renal Association – European Dialysis and Transplant Association. Dr. Schaeffner declared speaker honoraria from Fresenius Medical Care, Fresenius Kabi, and Siemens Health Care. Dr. White received grant support from Academic Health Science Center Alternate Funding Plan Innovation Fund. Dr. Melsom declared speaker honoraria from Astellas, Norwegian evening summit, American Society of Nephrology, 2018, and grants from Boehringer Ingelheim AS, outside the submitted work. Dr. van Londen declared speaker honoraria from Fresenius Medical Care. Dr. Rule declared royalties as “UpToDate” author on “The Aging Kidney.” Dr. van der Giet reports personal fees from Novartis, personal fees from Bayer, personal fees and “other” from IEM, personal fees and other from Charité Research Organization, grants from Deutsche Forschungsgemeinschaft, grants from Else Kröner Freseniusstiftung, personal fees from Berlin Chemie, personal fees from Otsuka, personal fees from Servier, and personal fees from CVRX, outside the submitted work. Dr. Glassock reports other from Wolters-Kluwer, outside the submitted work. Dr. Rule reports grants from National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, during the conduct of the study. All authors are members of the ERA-EDTA European Kidney Function Consortium.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Kidney Disease: Improving Global Outcomes (KDIGO) Chronic Kidney Disease Work Group : KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3: 1–150, 2013 [DOI] [PubMed] [Google Scholar]
- 2.Delanaye P, Schaeffner E, Ebert N, Cavalier E, Mariat C, Krzesinski JM, et al.: Normal reference values for glomerular filtration rate: What do we really know? Nephrol Dial Transplant 27: 2664–2672, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Poggio ED, Rule AD: Can we do better than a single estimated GFR threshold when screening for chronic kidney disease? Kidney Int 72: 534–536, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Poggio ED, Rule AD: A critical evaluation of chronic kidney disease--should isolated reduced estimated glomerular filtration rate be considered a ‘disease’? Nephrol Dial Transplant 24: 698–700, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tonna SJ: Invited commentary: Defining incident chronic kidney disease in epidemiologic study settings. Am J Epidemiol 170: 425–427, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Bash LD, Coresh J, Köttgen A, Parekh RS, Fulop T, Wang Y, et al.: Defining incident chronic kidney disease in the research setting: The ARIC Study. Am J Epidemiol 170: 414–424, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu CY, Chertow GM: Chronic renal confusion: Insufficiency, failure, dysfunction, or disease. Am J Kidney Dis 36: 415–418, 2000 [DOI] [PubMed] [Google Scholar]
- 8.Hall YN, Himmelfarb J: The CKD classification system in the precision medicine era. Clin J Am Soc Nephrol 12: 346–348, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Black C, van der Veer SN: Unlocking the value of variation in CKD prevalence. J Am Soc Nephrol 27: 1874–1877, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauer C, Melamed ML, Hostetter TH: Staging of chronic kidney disease: Time for a course correction. J Am Soc Nephrol 19: 844–846, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Eknoyan G: Chronic kidney disease definition and classification: The quest for refinements. Kidney Int 72: 1183–1185, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Wesson LG: Renal hemodynamics in physiologic states. In: Physiology of the Human Kidney, edited by Wesson LG, New York, Grune and Stratton, 1969, pp 96–108 [Google Scholar]
- 13.Poggio ED, Rule AD, Tanchanco R, Arrigain S, Butler RS, Srinivas T, et al.: Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney Int 75: 1079–1087, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pottel H, Hoste L, Yayo E, Delanaye P: Glomerular filtration rate in healthy living potential kidney donors: A meta-analysis. Nephron 135: 105–119, 2017 [DOI] [PubMed] [Google Scholar]
- 15.Gaillard F, Courbebaisse M, Kamar N, Rostaing L, Del Bello A, Girerd S, et al.: The age-calibrated measured glomerular filtration rate improves living kidney donation selection process. Kidney Int 94: 616–624, 2018 [DOI] [PubMed] [Google Scholar]
- 16.Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, et al.: Chronic Kidney Disease Prognosis Consortium : Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet 375: 2073–2081, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hallan SI, Matsushita K, Sang Y, Mahmoodi BK, Black C, Ishani A, et al.: Chronic Kidney Disease Prognosis Consortium : Age and association of kidney measures with mortality and end-stage renal disease. JAMA 308: 2349–2360, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsushita K, Ballew SH, Coresh J, Arima H, Ärnlöv J, Cirillo M, et al.: Chronic Kidney Disease Prognosis Consortium : Measures of chronic kidney disease and risk of incident peripheral artery disease: A collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol 5: 718–728, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fox CS, Matsushita K, Woodward M, Bilo HJ, Chalmers J, Heerspink HJ, et al.: Chronic Kidney Disease Prognosis Consortium : Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: A meta-analysis. Lancet 380: 1662–1673, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nitsch D, Grams M, Sang Y, Black C, Cirillo M, Djurdjev O, et al.: Chronic Kidney Disease Prognosis Consortium : Associations of estimated glomerular filtration rate and albuminuria with mortality and renal failure by sex: A meta-analysis. BMJ 346: f324, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahmoodi BK, Matsushita K, Woodward M, Blankestijn PJ, Cirillo M, Ohkubo T, et al.: Chronic Kidney Disease Prognosis Consortium : Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: A meta-analysis. Lancet 380: 1649–1661, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matsushita K, Coresh J, Sang Y, Chalmers J, Fox C, Guallar E, et al.: CKD Prognosis Consortium : Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: A collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol 3: 514–525, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas B, Matsushita K, Abate KH, Al-Aly Z, Ärnlöv J, Asayama K, et al.: Global Burden of Disease 2013 GFR Collaborators; CKD Prognosis Consortium; Global Burden of Disease Genitourinary Expert Group : Global cardiovascular and renal outcomes of reduced GFR. J Am Soc Nephrol 28: 2167–2179, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wen CP, Matsushita K, Coresh J, Iseki K, Islam M, Katz R, et al. : Relative risks of chronic kidney disease for mortality and end-stage renal disease across races are similar. Kidney Int 86: 819–827, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey A, et al.: Chronic Kidney Disease Prognosis Consortium : Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int 79: 1341–1352, 2011 [DOI] [PubMed] [Google Scholar]
- 26.Astor BC, Matsushita K, Gansevoort RT, van der Velde M, Woodward M, Levey AS, et al.: Chronic Kidney Disease Prognosis Consortium : Lower estimated glomerular filtration rate and higher albuminuria are associated with mortality and end-stage renal disease. A collaborative meta-analysis of kidney disease population cohorts. Kidney Int 79: 1331–1340, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gansevoort RT, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al.: Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int 80: 93–104, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hui X, Matsushita K, Sang Y, Ballew SH, Fülöp T, Coresh J: CKD and cardiovascular disease in the atherosclerosis risk in communities (ARIC) study: Interactions with age, sex, and race. Am J Kidney Dis 62: 691–702, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Tangri N, Stevens LA, Griffith J, Tighiouart H, Djurdjev O, Naimark D, et al.: A predictive model for progression of chronic kidney disease to kidney failure. JAMA 305: 1553–1559, 2011 [DOI] [PubMed] [Google Scholar]
- 31.Delanaye P, Glassock RJ, Pottel H, Rule AD: An age-calibrated definition of chronic kidney disease: Rationale and benefits. Clin Biochem Rev 37: 17–26, 2016 [PMC free article] [PubMed] [Google Scholar]
- 32.Glassock R, Denic A, Rule AD: When kidneys get old: An essay on nephro-geriatrics. J Bras Nefrol 39: 59–64, 2017 [DOI] [PubMed] [Google Scholar]
- 33.Glassock RJ: Con: Thresholds to define chronic kidney disease should not be age dependent. Nephrol Dial Transplant 29: 774–779, discussion 779–782, 2014 [DOI] [PubMed] [Google Scholar]
- 34.Denic A, Glassock RJ, Rule AD: Structural and functional changes with the aging kidney. Adv Chronic Kidney Dis 23: 19–28, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manjunath G, Tighiouart H, Coresh J, Macleod B, Salem DN, Griffith JL, et al.: Level of kidney function as a risk factor for cardiovascular outcomes in the elderly. Kidney Int 63: 1121–1129, 2003 [DOI] [PubMed] [Google Scholar]
- 36.O’Hare AM, Bertenthal D, Covinsky KE, Landefeld CS, Sen S, Mehta K, et al.: Mortality risk stratification in chronic kidney disease: One size for all ages? J Am Soc Nephrol 17: 846–853, 2006 [DOI] [PubMed] [Google Scholar]
- 37.Maaravi Y, Bursztyn M, Hammerman-Rozenberg R, Stessman J: Glomerular filtration rate estimation and mortality in an elderly population. QJM 100: 441–449, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Hallan S, Astor B, Romundstad S, Aasarød K, Kvenild K, Coresh J: Association of kidney function and albuminuria with cardiovascular mortality in older vs younger individuals: The HUNT II Study. Arch Intern Med 167: 2490–2496, 2007 [DOI] [PubMed] [Google Scholar]
- 39.Brantsma AH, Bakker SJL, Hillege HL, de Zeeuw D, de Jong PE, Gansevoort RT; PREVEND Study Group : Cardiovascular and renal outcome in subjects with K/DOQI stage 1-3 chronic kidney disease: The importance of urinary albumin excretion. Nephrol Dial Transplant 23: 3851–3858, 2008 [DOI] [PubMed] [Google Scholar]
- 40.Hwang SJ, Lin MY, Chen HC, Hwang SC, Yang WC, Hsu CC, et al.: Increased risk of mortality in the elderly population with late-stage chronic kidney disease: A cohort study in Taiwan. Nephrol Dial Transplant 23: 3192–3198, 2008 [DOI] [PubMed] [Google Scholar]
- 41.Roderick PJ, Atkins RJ, Smeeth L, Mylne A, Nitsch DD, Hubbard RB, et al.: CKD and mortality risk in older people: A community-based population study in the United Kingdom. Am J Kidney Dis 53: 950–960, 2009 [DOI] [PubMed] [Google Scholar]
- 42.van der Velde M, Bakker SJL, de Jong PE, Gansevoort RT: Influence of age and measure of eGFR on the association between renal function and cardiovascular events. Clin J Am Soc Nephrol 5: 2053–2059, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muntner P, Bowling CB, Gao L, Rizk D, Judd S, Tanner RM, et al.: Age-specific association of reduced estimated glomerular filtration rate and albuminuria with all-cause mortality. Clin J Am Soc Nephrol 6: 2200–2207, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stengel B, Metzger M, Froissart M, Rainfray M, Berr C, Tzourio C, et al.: Epidemiology and prognostic significance of chronic kidney disease in the elderly--the Three-City prospective cohort study. Nephrol Dial Transplant 26: 3286–3295, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Pottelbergh G, Vaes B, Adriaensen W, Matheï C, Legrand D, Wallemacq P, et al.: The glomerular filtration rate estimated by new and old equations as a predictor of important outcomes in elderly patients. BMC Med 12: 27, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oh SW, Kim S, Na KY, Kim KW, Chae DW, Chin HJ: Glomerular filtration rate and proteinuria: Association with mortality and renal progression in a prospective cohort of a community-based elderly population. PLoS One 9: e94120, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Minutolo R, Lapi F, Chiodini P, Simonetti M, Bianchini E, Pecchioli S, et al.: Risk of ESRD and death in patients with CKD not referred to a nephrologist: A 7-year prospective study. Clin J Am Soc Nephrol 9: 1586–1593, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malmgren L, McGuigan FE, Berglundh S, Westman K, Christensson A, Åkesson K: Declining estimated glomerular filtration rate and its association with mortality and comorbidity over 10 years in elderly women. Nephron 130: 245–255, 2015 [DOI] [PubMed] [Google Scholar]
- 49.Chowdhury EK, Langham RG, Owen A, Krum H, Wing LM, Nelson MR, et al.: Second Australian National Blood Pressure Study Management Committeem : Comparison of predictive performance of renal function estimation equations for all-cause and cardiovascular mortality in an elderly hypertensive population. Am J Hypertens 28: 380–386, 2015 [DOI] [PubMed] [Google Scholar]
- 50.Nagai K, Sairenchi T, Irie F, Watanabe H, Ota H, Yamagata K: Relationship between estimated glomerular filtration rate and cardiovascular mortality in a Japanese cohort with long-term follow-up. PLoS One 11: e0156792, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Corsonello A, Pedone C, Bandinelli S, Ferrucci L, Antonelli Incalzi R: Predicting survival of older community-dwelling individuals according to five estimated glomerular filtration rate equations: The InChianti study. Geriatr Gerontol Int 18: 607–614, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wu J, Jia J, Li Z, Pan H, Wang A, Guo X, et al.: Association of estimated glomerular filtration rate and proteinuria with all-cause mortality in community-based population in China: A result from Kailuan study. Sci Rep 8: 2157, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O’Hare AM, Hailpern SM, Pavkov ME, Rios-Burrows N, Gupta I, Maynard C, et al.: Prognostic implications of the urinary albumin to creatinine ratio in veterans of different ages with diabetes. Arch Intern Med 170: 930–936, 2010 [DOI] [PubMed] [Google Scholar]
- 54.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, et al.: Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 382: 339–352, 2013 [DOI] [PubMed] [Google Scholar]
- 55.Shardlow A, McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW: Chronic kidney disease in primary care: Outcomes after five years in a prospective cohort study. PLoS Med 13: e1002128, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Raymond NT, Zehnder D, Smith SC, Stinson JA, Lehnert H, Higgins RM: Elevated relative mortality risk with mild-to-moderate chronic kidney disease decreases with age. Nephrol Dial Transplant 22: 3214–3220, 2007 [DOI] [PubMed] [Google Scholar]
- 57.Wyatt CM: A rose by any other name: Is stage 3a chronic kidney disease really a disease? Kidney Int 91: 6–8, 2017 [DOI] [PubMed] [Google Scholar]
- 58.Moranne O, Froissart M, Rossert J, Gauci C, Boffa JJ, Haymann JP, et al.: NephroTest Study Group : Timing of onset of CKD-related metabolic complications. J Am Soc Nephrol 20: 164–171, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Drawz PE, Babineau DC, Rahman M: Metabolic complications in elderly adults with chronic kidney disease. J Am Geriatr Soc 60: 310–315, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bowling CB, Muntner P, Sawyer P, Sanders PW, Kutner N, Kennedy R, et al.: Community mobility among older adults with reduced kidney function: A study of life-space. Am J Kidney Dis 63: 429–436, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fried LF, Lee JS, Shlipak M, Chertow GM, Green C, Ding J, et al.: Chronic kidney disease and functional limitation in older people: Health, aging and body composition study. J Am Geriatr Soc 54: 750–756, 2006 [DOI] [PubMed] [Google Scholar]
- 62.Rule AD, Amer H, Cornell LD, Taler SJ, Cosio FG, Kremers WK, et al.: The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med 152: 561–567, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Denic A, Lieske JC, Chakkera HA, Poggio ED, Alexander MP, Singh P, et al.: The substantial loss of nephrons in healthy human kidneys with aging. J Am Soc Nephrol 28: 313–320, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Denic A, Mathew J, Lerman LO, Lieske JC, Larson JJ, Alexander MP, et al.: Single-nephron glomerular filtration rate in healthy adults. N Engl J Med 376: 2349–2357, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tan JC, Busque S, Workeneh B, Ho B, Derby G, Blouch KL, et al.: Effects of aging on glomerular function and number in living kidney donors. Kidney Int 78: 686–692, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hommos MS, Zeng C, Liu Z, Troost JP, Rosenberg AZ, Palmer M, et al.: Global glomerulosclerosis with nephrotic syndrome; the clinical importance of age adjustment. Kidney Int 93: 1175–1182, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Srivastava A, Palsson R, Kaze AD, Chen ME, Palacios P, Sabbisetti V, et al.: The prognostic value of histopathologic lesions in native kidney biopsy specimens: Results from the boston kidney biopsy cohort study. J Am Soc Nephrol 29: 2213–2224, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yayo E, Ayé M, Yao C, Gnionsahé A, Attoungbré M-L, Cavalier E, et al.: Measured (and estimated) glomerular filtration rate: Reference values in West Africa. Nephrol Dial Transplant 33: 1176–1180, 2018 [DOI] [PubMed] [Google Scholar]
- 69.Hogeman O: Normal individuals. Acta Med Scand Suppl 131: 99–108, 1948 [Google Scholar]
- 70.Bucht H: Studies on renal function in man; with special reference to glomerular filtration and renal plasma flow in pregnancy. Scand J Clin Lab Invest 3[Suppl 3]: 1–64, 1951 [PubMed] [Google Scholar]
- 71.Slack TK, Wilson DM: Normal renal function: CIN and CPAH in healthy donors before and after nephrectomy. Mayo Clin Proc 51: 296–300, 1976 [PubMed] [Google Scholar]
- 72.Landahl S, Aurell M, Jagenburg R: Glomerular filtration rate at the age of 70 and 75. J Clin Exp Gerontol 3: 29–45, 1981 [Google Scholar]
- 73.Granerus G, Aurell M: Reference values for 51Cr-EDTA clearance as a measure of glomerular filtration rate. Scand J Clin Lab Invest 41: 611–616, 1981 [DOI] [PubMed] [Google Scholar]
- 74.Hamilton D, Riley P, Miola U, Mousa D, Popovich W, al Khader A: Total plasma clearance of 51Cr-EDTA: Variation with age and sex in normal adults. Nucl Med Commun 21: 187–192, 2000 [DOI] [PubMed] [Google Scholar]
- 75.Rule AD, Gussak HM, Pond GR, Bergstralh EJ, Stegall MD, Cosio FG, et al.: Measured and estimated GFR in healthy potential kidney donors. Am J Kidney Dis 43: 112–119, 2004 [DOI] [PubMed] [Google Scholar]
- 76.Grewal GS, Blake GM: Reference data for 51Cr-EDTA measurements of the glomerular filtration rate derived from live kidney donors. Nucl Med Commun 26: 61–65, 2005 [DOI] [PubMed] [Google Scholar]
- 77.Barai S, Bandopadhayaya GP, Patel CD, Rathi M, Kumar R, Bhowmik D, et al.: Do healthy potential kidney donors in India have an average glomerular filtration rate of 81.4 ml/min? Nephron, Physiol 101: 21–26, 2005 [DOI] [PubMed] [Google Scholar]
- 78.Berg UB: Differences in decline in GFR with age between males and females. Reference data on clearances of inulin and PAH in potential kidney donors. Nephrol Dial Transplant 21: 2577–2582, 2006 [DOI] [PubMed] [Google Scholar]
- 79.Jafar TH, Islam M, Jessani S, Bux R, Inker LA, Mariat C, et al.: Level and determinants of kidney function in a South Asian population in Pakistan. Am J Kidney Dis 58: 764–772, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ma YC, Zuo L, Chen L, Su ZM, Meng S, Li JJ, et al.: Distribution of measured GFR in apparently healthy Chinese adults. Am J Kidney Dis 56: 420–421, 2010 [DOI] [PubMed] [Google Scholar]
- 81.Soares AA, Prates AB, Weinert LS, Veronese FV, de Azevedo MJ, Silveiro SP: Reference values for glomerular filtration rate in healthy Brazilian adults. BMC Nephrol 14: 54, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Peters AM, Perry L, Hooker CA, Howard B, Neilly MD, Seshadri N, et al.: Extracellular fluid volume and glomerular filtration rate in 1878 healthy potential renal transplant donors: Effects of age, gender, obesity and scaling. Nephrol Dial Transplant 27: 1429–1437, 2012 [DOI] [PubMed] [Google Scholar]
- 83.Holness JL, Fleming JS, Malaroda AL, Warwick JM: (99m)Tc-DTPA volume of distribution, half-life and glomerular filtration rate in normal adults. Nucl Med Commun 34: 1005–1014, 2013 [DOI] [PubMed] [Google Scholar]
- 84.De Santo NG, Capasso G, Anastasio P, Coppola S, Policastro M, Bellini L, et al.: Renal functional reserve. Child Nephrol Urol 11: 140–145, 1991 [PubMed] [Google Scholar]
- 85.Davies DF, Shock NW: Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest 29: 496–507, 1950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shock NW: Kidney function tests in aged males. Geriatrics 1: 232–239, 1946 [PubMed] [Google Scholar]
- 87.Horio M, Yasuda Y, Kaimori J, Ichimaru N, Isaka Y, Takahara S, et al.: Performance of the Japanese GFR equation in potential kidney donors. Clin Exp Nephrol 16: 415–420, 2012 [DOI] [PubMed] [Google Scholar]
- 88.Hoang K, Tan JC, Derby G, Blouch KL, Masek M, Ma I, et al.: Determinants of glomerular hypofiltration in aging humans. Kidney Int 64: 1417–1424, 2003 [DOI] [PubMed] [Google Scholar]
- 89.Teo BW, Xu H, Koh YY, Li J, Subramanian S, Sinha AK, et al.: Glomerular filtration rates in healthy Asians without kidney disease. Nephrology (Carlton) 19: 72–79, 2014 [DOI] [PubMed] [Google Scholar]
- 90.den Bakker E, Gemke RJBJ, Bökenkamp A: Endogenous markers for kidney function in children: A review. Crit Rev Clin Lab Sci 55: 163–183, 2018 [DOI] [PubMed] [Google Scholar]
- 91.Pottel H, Delanaye P, Weekers L, Selistre L, Goffin K, Gheysens O, et al.: Age-dependent reference intervals for estimated and measured glomerular filtration rate. Clin Kidney J 10: 545–551, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bäck SE, Ljungberg B, Nilsson-Ehle I, Borgå O, Nilsson-Ehle P: Age dependence of renal function: Clearance of iohexol and p-amino hippurate in healthy males. Scand J Clin Lab Invest 49: 641–646, 1989 [DOI] [PubMed] [Google Scholar]
- 93.Pottel H, Hoste L, Dubourg L, Ebert N, Schaeffner E, Eriksen BO, et al.: An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant 31: 798–806, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al.: CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schaeffner ES, Ebert N, Delanaye P, Frei U, Gaedeke J, Jakob O, et al.: Two novel equations to estimate kidney function in persons aged 70 years or older. Ann Intern Med 157: 471–481, 2012 [DOI] [PubMed] [Google Scholar]
- 96.Baba M, Shimbo T, Horio M, Ando M, Yasuda Y, Komatsu Y, et al.: Longitudinal study of the decline in renal function in healthy subjects. PLoS One 10: e0129036, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Benghanem Gharbi M, Elseviers M, Zamd M, Belghiti Alaoui A, Benahadi N, Trabelssi H, et al.: Chronic kidney disease, hypertension, diabetes, and obesity in the adult population of Morocco: How to avoid “over”- and “under”-diagnosis of CKD. Kidney Int 89: 1363–1371, 2016 [DOI] [PubMed] [Google Scholar]
- 98.van den Brand JA, van Boekel GA, Willems HL, Kiemeney LA, den Heijer M, Wetzels JF: Introduction of the CKD-EPI equation to estimate glomerular filtration rate in a Caucasian population. Nephrol Dial Transplant 26: 3176–3181, 2011 [DOI] [PubMed] [Google Scholar]
- 99.Wetzels JF, Kiemeney LA, Swinkels DW, Willems HL, den Heijer M: Age- and gender-specific reference values of estimated GFR in Caucasians: The Nijmegen Biomedical study. Kidney Int 72: 632–637, 2007 [DOI] [PubMed] [Google Scholar]
- 100.Elseviers MM, Verpooten GA, De Broe ME, De Backer GG: Interpretation of creatinine clearance. Lancet 1: 457, 1987 [DOI] [PubMed] [Google Scholar]
- 101.Ebert N, Jakob O, Gaedeke J, van der Giet M, Kuhlmann MK, Martus P, et al.: Prevalence of reduced kidney function and albuminuria in older adults: The Berlin initiative study. Nephrol Dial Transplant 32: 997–1005, 2017 [DOI] [PubMed] [Google Scholar]
- 102.Lindeman RD, Tobin J, Shock NW: Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc 33: 278–285, 1985 [DOI] [PubMed] [Google Scholar]
- 103.Kasiske BL, Anderson-Haag T, Israni AK, Kalil RS, Kimmel PL, Kraus ES, et al.: A prospective controlled study of living kidney donors: Three-year follow-up. Am J Kidney Dis 66: 114–124, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rowe JW, Andres R, Tobin JD, Norris AH, Shock NW: The effect of age on creatinine clearance in men: A cross-sectional and longitudinal study. J Gerontol 31: 155–163, 1976 [DOI] [PubMed] [Google Scholar]
- 105.Cohen E, Nardi Y, Krause I, Goldberg E, Milo G, Garty M, et al.: A longitudinal assessment of the natural rate of decline in renal function with age. J Nephrol 27: 635–641, 2014 [DOI] [PubMed] [Google Scholar]
- 106.Hollenberg NK, Rivera A, Meinking T, Martinez G, McCullough M, Passan D, et al.: Age, renal perfusion and function in island-dwelling indigenous Kuna Amerinds of Panama. Nephron 82: 131–138, 1999 [DOI] [PubMed] [Google Scholar]
- 107.O’Sullivan ED, Hughes J, Ferenbach DA: Renal aging: Causes and consequences. J Am Soc Nephrol 28: 407–420, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, et al.: Slower decline of glomerular filtration rate in the Japanese general population: A longitudinal 10-year follow-up study. Hypertens Res 31: 433–441, 2008 [DOI] [PubMed] [Google Scholar]
- 109.Lauretani F, Semba RD, Bandinelli S, Miller ER 3rd, Ruggiero C, Cherubini A, et al.: Plasma polyunsaturated fatty acids and the decline of renal function. Clin Chem 54: 475–481, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bolignano D, Mattace-Raso F, Sijbrands EJG, Zoccali C: The aging kidney revisited: A systematic review. Ageing Res Rev 14: 65–80, 2014 [DOI] [PubMed] [Google Scholar]
- 111.Jiang S, Sun X, Gu H, Chen Y, Xi C, Qiao X, et al.: Age-related change in kidney function, its influencing factors, and association with asymptomatic carotid atherosclerosis in healthy individuals--a 5-year follow-up study. Maturitas 73: 230–238, 2012 [DOI] [PubMed] [Google Scholar]
- 112.Delanaye P, Glassock RJ: Glomerular filtration rate and aging: Another longitudinal study--A long time coming! Nephron 131: 1–4, 2015 [DOI] [PubMed] [Google Scholar]
- 113.Eriksen BO, Ingebretsen OC: The progression of chronic kidney disease: A 10-year population-based study of the effects of gender and age. Kidney Int 69: 375–382, 2006 [DOI] [PubMed] [Google Scholar]
- 114.Eriksen BO, Stefansson VTN, Jenssen TG, Mathisen UD, Schei J, Solbu MD, et al.: Elevated blood pressure is not associated with accelerated glomerular filtration rate decline in the general non-diabetic middle-aged population. Kidney Int 90: 404–410, 2016 [DOI] [PubMed] [Google Scholar]
- 115.Rule AD, Glassock RJ: Chronic kidney disease: Classification of CKD should be about more than prognosis. Nat Rev Nephrol 9: 697–698, 2013 [DOI] [PubMed] [Google Scholar]
- 116.Glassock RJ, Winearls C: An epidemic of chronic kidney disease: Fact or fiction? Nephrol Dial Transplant 23: 1117–1121, 2008 [DOI] [PubMed] [Google Scholar]
- 117.Delanaye P, Cavalier E: Staging chronic kidney disease and estimating glomerular filtration rate: An opinion paper about the new international recommendations. Clin Chem Lab Med 51: 1911–1917, 2013 [DOI] [PubMed] [Google Scholar]
- 118.Glassock RJ, Rule AD: The implications of anatomical and functional changes of the aging kidney: With an emphasis on the glomeruli. Kidney Int 82: 270–277, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wetzels JF, Willems HL, den Heijer M: Age- and gender-specific reference values of estimated glomerular filtration rate in a Caucasian population: Results of the Nijmegen Biomedical study. Kidney Int 73: 657–658, 2008 [DOI] [PubMed] [Google Scholar]
- 120.Ellam T, Twohig H, Khwaja A: Chronic kidney disease in elderly people: Disease or disease label? BMJ 352: h6559, 2016 [DOI] [PubMed] [Google Scholar]
- 121.Moynihan R, Glassock R, Doust J: Chronic kidney disease controversy: How expanding definitions are unnecessarily labelling many people as diseased. BMJ 347: f4298, 2013 [DOI] [PubMed] [Google Scholar]
- 122.Botev R, Mallié JP, Wetzels JF, Couchoud C, Schück O: The clinician and estimation of glomerular filtration rate by creatinine-based formulas: Current limitations and quo vadis. Clin J Am Soc Nephrol 6: 937–950, 2011 [DOI] [PubMed] [Google Scholar]
- 123.De Broe ME, Gharbi MB, Zamd M, Elseviers M: Why overestimate or underestimate chronic kidney disease when correct estimation is possible? Nephrol Dial Transplant 32[suppl_2]: ii136–ii141, 2017 [DOI] [PubMed] [Google Scholar]
- 124.Roderick PJ, Atkins RJ, Smeeth L, Nitsch DM, Hubbard RB, Fletcher AE, et al.: Detecting chronic kidney disease in older people; what are the implications? [published correction appears in Age Ageing 2009; 38: 638]. Age Ageing 37: 179–186, 2008 [DOI] [PubMed] [Google Scholar]
- 125.Boele-Schutte E, Gansevoort RT: Measured GFR: Not a gold, but a gold-plated standard. Nephrol Dial Transplant 32 [suppl 2]: ii180–ii184, 2017 [DOI] [PubMed] [Google Scholar]
- 126.Soveri I, Berg UB, Björk J, Elinder CG, Grubb A, Mejare I, et al. ; SBU GFR Review Group : Measuring GFR: A systematic review. Am J Kidney Dis 64: 411–424, 2014 [DOI] [PubMed] [Google Scholar]
- 127.Björk J, Bäck SE, Ebert N, Evans M, Grubb A, Hansson M, et al.: GFR estimation based on standardized creatinine and cystatin C: A european multicenter analysis in older adults. Clin Chem Lab Med 56: 422–435, 2018 [DOI] [PubMed] [Google Scholar]
- 128.Glassock R, Delanaye P, El Nahas M: An age-calibrated classification of chronic kidney disease. JAMA 314: 559–560, 2015 [DOI] [PubMed] [Google Scholar]
- 129.Pottel H, Hoste L, Delanaye P: Abnormal glomerular filtration rate in children, adolescents and young adults starts below 75 mL/min/1.73 m(2). Pediatr Nephrol 30: 821–828, 2015 [DOI] [PubMed] [Google Scholar]
- 130.Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, et al. : A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int 88: 950–957, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al.: Global prevalence of chronic kidney disease - a systematic review and meta-analysis. PLoS One 11: e0158765, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gambaro G, Yabarek T, Graziani MS, Gemelli A, Abaterusso C, Frigo AC, et al.: INCIPE Study Group : Prevalence of CKD in northeastern Italy: Results of the INCIPE study and comparison with NHANES. Clin J Am Soc Nephrol 5: 1946–1953, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.De Nicola L, Donfrancesco C, Minutolo R, Lo Noce C, Palmieri L, De Curtis A, et al.: ANMCO-SIN Research Group : Prevalence and cardiovascular risk profile of chronic kidney disease in Italy: Results of the 2008-12 National Health Examination Survey. Nephrol Dial Transplant 30: 806–814, 2015 [DOI] [PubMed] [Google Scholar]
- 134.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al.: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 135.Zdrojewski Ł, Zdrojewski T, Rutkowski M, Bandosz P, Król E, Wyrzykowski B, et al.: Prevalence of chronic kidney disease in a representative sample of the polish population: Results of the NATPOL 2011 survey. Nephrol Dial Transplant 31: 433–439, 2016 [DOI] [PubMed] [Google Scholar]
- 136.Zdrojewski Ł, Król E, Rutkowski B, Piotrowski W, Pająk A, Drygas W, et al.: Chronic kidney disease in polish elderly population aged 75+: Results of the WOBASZ Senior Survey. Int Urol Nephrol 49: 669–676, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wen CP, Cheng TYD, Tsai MK, Chang YC, Chan HT, Tsai SP, et al.: All-cause mortality attributable to chronic kidney disease: A prospective cohort study based on 462 293 adults in Taiwan. Lancet 371: 2173–2182, 2008 [DOI] [PubMed] [Google Scholar]
- 138.Hallan SI, Øvrehus MA, Romundstad S, Rifkin D, Langhammer A, Stevens PE, et al. : Long-term trends in the prevalence of chronic kidney disease and the influence of cardiovascular risk factors in Norway. Kidney Int 90: 665–673, 2016 [DOI] [PubMed] [Google Scholar]
- 139.Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, et al.: Analysis of the Global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int 94: 567–581, 2018 [DOI] [PubMed] [Google Scholar]
- 140.Brück K, Stel VS, Gambaro G, Hallan S, Völzke H, Ärnlöv J, et al.: European CKD Burden Consortium : CKD prevalence varies across the european general population. J Am Soc Nephrol 27: 2135–2147, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pottel H, Delanaye P, Schaeffner E, Dubourg L, Eriksen BOBO, Melsom T, et al.: Estimating glomerular filtration rate for the full age spectrum from serum creatinine and cystatin C. Nephrol Dial Transplant 32: 497–507, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Delanaye P, Cavalier E, Krzesinski JM: Chronic kidney disease in Taiwan. Lancet 372: 1950, author reply 1950–1951, 2008 [DOI] [PubMed] [Google Scholar]
- 143.McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW: Risk profile in chronic kidney disease stage 3: Older versus younger patients. Nephron Clin Pract 119: c269–c276, 2011 [DOI] [PubMed] [Google Scholar]
- 144.James MT, Hemmelgarn BR, Wiebe N, Pannu N, Manns BJ, Klarenbach SW, et al.: Alberta Kidney Disease Network : Glomerular filtration rate, proteinuria, and the incidence and consequences of acute kidney injury: A cohort study. Lancet 376: 2096–2103, 2010 [DOI] [PubMed] [Google Scholar]
- 145.Schreuder MF: Life with one kidney. Pediatr Nephrol 33: 595–604, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Abitbol CL, DeFreitas MJ, Strauss J: Assessment of kidney function in preterm infants: Lifelong implications. Pediatr Nephrol 31: 2213–2222, 2016 [DOI] [PubMed] [Google Scholar]
- 147.Yamakawa S, Nagai T, Uemura O: Down syndrome and mild kidney dysfunction. Pediatr Int (Roma) 60: 391–393, 2018 [DOI] [PubMed] [Google Scholar]
- 148.Ellis MJ, Parikh CR, Inrig JK, Kanbay M, Patel UD: Chronic kidney disease after hematopoietic cell transplantation: A systematic review [published correction appears in Am J Transplant 2009; 9: 865]. Am J Transplant 8: 2378–2390, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.O’Hare AM, Hotchkiss JR, Kurella Tamura M, Larson EB, Hemmelgarn BR, Batten A, et al.: Interpreting treatment effects from clinical trials in the context of real-world risk information: End-stage renal disease prevention in older adults. JAMA Intern Med 174: 391–397, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]