Abstract
Background
Gender equity has historically been a challenge within gastroenterology.
Aims
The Canadian Association of Gastroenterology (CAG) developed a survey to identify issues pertaining to equity and gender faced by its membership and to determine areas of action.
Methods
In 2014, the survey was emailed to all 1155 CAG members, and the data were analyzed using statistical methods.
Results
One hundred eleven CAG members responded to the survey. Of those, 52% were male, 75% were between 26 and 45 years of age, and 55% were in their first decade of practice. More males held the status of full professor (21% versus 0%; P=0.022). Male CAG members reported working more hours per week than their female counterparts (58.3 ± 15.4 versus 52.3 ± 11.8, P=0.025). Regarding commitments outside the workplace, 81% of respondents had a spouse/partner, and 52% had children under 18 years of age, both of which did not significantly differ based on gender. Overall, 70% were satisfied or very satisfied with their career path. However, significantly more females felt their age/ethnicity/gender/marital status hindered career advancement (36% versus 14%; P=0.008). Furthermore, more females reported difficulties attaining work-life balance (45% versus 22%; P=0.015).
Conclusions
This survey highlights that gender and equity challenges continue to exist within gastroenterology. The needs assessment highlights that work-life balance, physician well-being, negotiation skills and mentorship are areas of importance to many CAG members.
Keywords: Diversity, Equity, Gastroenterology, Gender, Women in medicine
Over the past several decades, the number of women in medicine has steadily increased to the point that women now account for approximately half of all medical students. In 2014, 56% of all students enrolled in Canadian faculties of medicine were female (1), and in 2015, 55% of all medical graduates (excluding visa trainees) entering Canadian residency programs were female (2). Between 2005 and 2014, the percentage of women in Canadian internal medicine programs has remained relatively stable increasing from 47% to 48%, while adult gastroenterology has seen an increase from 30% to 38% (1). Despite this, data from the Canadian Medical Association shows that females accounted for only 29% of all practicing gastroenterologists in 2015 (3).
Previous studies have demonstrated that female gastroenterologists perceive that gender has affected their career advancement and report lower overall career satisfaction than their male counterparts (4). In 1997, the Canadian Association of Gastroenterology (CAG) carried out a survey that demonstrated that female gastroenterologists achieved equal career opportunity by compromise (5). This study showed that although female gastroenterologists achieved similar levels of career advancement, they were less likely to marry and have families. It also illustrated that female gastroenterologists were more likely to have a lower personal income than their male colleagues. No further studies have since addressed whether such gender disparities continue to exist in Canada.
The CAG established the Equity and Gender (now Diversity & Equity) committee in 1999 with a mandate to identify and address concerns from CAG members regarding issues related to gender and minority groups for discussion and action. In 2014, this survey was undertaken by the CAG to identify issues of relevance and to determine potential areas of action that would be of most benefit to CAG members.
MATERIALS AND METHODS
Survey Development and Distribution
The survey instrument was compiled by the CAG Diversity and Equity Committee (supplementary material). It was piloted at the annual meeting of the CAG (i.e., Canadian Digestive Diseases Week) in 2014. The survey instrument was modified based on pilot feedback and was then distributed by the CAG via email to all members in May 2014 and redistributed in June 2014. The survey was anonymously administered using SurveyMonkey software. No identifying details of the respondents were collected.
Statistical Analysis
Data analysis was based on the original questions contained in the survey. Specific a priori analyses were not planned. Categorical variables were compared using Fisher exact tests using the Graph Pad Software Inc. online calculator (http://graphpad.com/quickcalcs/contingency2/). Continuous variables were compared using Student t tests using Microsoft Excel. A P value of less than 0.05 was considered statistically significant.
RESULTS
Demographics of Respondents
Of the 1155 CAG members, 111 responded to the survey, which accounted for a response rate of approximately 10%. Of the respondents, 48% were female; this is slightly higher than the overall proportion of female CAG members (39%). The majority (75%) of respondents were between 26 to 45 years of age. There were significantly more female respondents between the ages of 36 and 45 (P=0.015, Table 1) and more male respondents between 56 and 65 (P=0.031). Field of practice varied, with 51% being adult or pediatric gastroenterologists, 20% basic scientists and 20% residents or fellows. Among clinical scientists, there were significantly more female respondents (9.4% versus 0%; P=0.022). There were no significant differences with regards to education and practice location.
Table 1.
Demographic characteristics
| Variable | Total (%) (N=111) | Male (N=58) | Female (N=53) | P value |
|---|---|---|---|---|
| Age | ||||
| <25 | 1 (0.9%) | 0 | 1 | 0.478 |
| 26–35 | 43 (38.7%) | 23 | 20 | 0.848 |
| 36–45 | 37 (33.3%) | 13 | 24 | *0.015 |
| 46–55 | 16 (14.4%) | 10 | 6 | 0.427 |
| 56–65 | 12 (10.8%) | 10 | 2 | *0.031 |
| 66> | 2 (1.8%) | 2 | 0 | 0.497 |
| Education§ | ||||
| MD or equivalent | 78 (70.3%) | 43 | 35 | 0.408 |
| PhD | 32 (28.8%) | 17 | 15 | 1.000 |
| MSc | 25 (22.5%) | 12 | 13 | 0.656 |
| Other | 12 (10.8%) | 4 | 8 | 0.224 |
| Practice location | ||||
| Alberta | 23 (20.7%) | 9 | 14 | 0.169 |
| British Columbia | 12 (10.8%) | 8 | 4 | 0.367 |
| Manitoba | 7 (6.3%) | 6 | 1 | 0.116 |
| New Brunswick | 2 (1.8%) | 0 | 2 | 0.226 |
| Newfoundland and Labrador | 1 (0.9%) | 1 | 0 | 1.000 |
| Northwest Territories | 0 (0. 0%) | 0 | 0 | 1.000 |
| Nova Scotia | 4 (3.6%) | 3 | 1 | 0.620 |
| Nunavut | 0 (0.0%) | 0 | 0 | 1.000 |
| Ontario | 45 (40.5%) | 22 | 23 | 0.369 |
| Prince Edward Island | 0 (0. 0%) | 0 | 0 | 1.000 |
| Quebec | 17 (15.3%) | 9 | 8 | 1.000 |
| Saskatchewan | 0 (0.0%) | 0 | 0 | 1.000 |
| Yukon | 0 (0.0%) | 0 | 0 | 1.000 |
| Field of practice | ||||
| Gastroenterologist (adult) | 44 (39.6%) | 26 | 18 | 0.252 |
| Gastroenterologist (pediatric) | 8 (7.2%) | 5 | 3 | 0.719 |
| Hepatologist | 4 (3.6%) | 2 | 2 | 1.000 |
| Surgeon | 0 (0.0%) | 0 | 0 | 1.000 |
| Clinical Scientist | 5 (4.5%) | 0 | 5 | *0.022 |
| Basic Scientist | 22 (19.8%) | 13 | 9 | 0.634 |
| Resident/Fellow | 20 (18.0%) | 10 | 10 | 1.000 |
| Graduate student | 3 (2.7%) | 1 | 2 | 0.605 |
| RN | 3 (2.7%) | 1 | 2 | 0.605 |
| Other | 2 (1.8%) | 0 | 2 | 0.226 |
*A statistically significant difference
§Respondents were allowed to select more than one option.
Details of Practice and Appointments
Fifty-six percent of respondents were in their first 10 years of practice, with 31% in their first five years (Table 2). More females were within their first five to 10 years of practice, (36% versus 15.5%; P=0. 017), whereas significantly more men had been in practice for 21 to 30 years (21% versus 0%; P < 0.001). With regard to practice setting, 65% worked in academic settings, with no significant differences between males and females. While 21% of males in academic settings had attained the status of full professor, no females reported having achieved this academic rank (P=0.022). Two males held the position of departmental chair or chief compared with no females, while four males held the position of division chair or chief compared with no females. However, these differences did not reach statistical significance.
Table 2.
Years of practice, practice setting, academic and other responsibilities
| Variable | Total (%) (N=111) | Male (N=58) | Female (N=53) | P value |
|---|---|---|---|---|
| Years in practice | ||||
| 1–4 years | 34 (30.6%) | 16 | 18 | 0.539 |
| 5–10 years | 28 (25.2%) | 9 | 19 | *0.017 |
| 11–20 years | 19 (17.1%) | 10 | 9 | 1.000 |
| 21–30 years | 12 (10.8%) | 12 | 0 | *0.0003 |
| 31 or more years | 5 (4.5%) | 3 | 2 | 1.000 |
| Not applicable | 13 (11.7%) | 8 | 5 | 0.562 |
| Practice setting | ||||
| Teaching hospital | 72 (64.9%) | 36 | 36 | 0.555 |
| Community-based with hospital privileges | 13 (11.7%) | 8 | 5 | 0.562 |
| Community-based w/o hospital privileges | 1 (0.9%) | 1 | 0 | 1.000 |
| None of the above/not applicable | 25 (22.5%) | 13 | 12 | 1.000 |
| Academic appointments | ||||
| Full Professor | 2 (1.8%) | 10 | 1 | *0.022 |
| Associate Professor | 32 (28.8%) | 6 | 7 | 0.770 |
| Assistant Professor | 13 (11.7%) | 17 | 15 | 1.000 |
| Adjunct Professor | 11 (9.9%) | 2 | 0 | 0.497 |
| Professor Emeritus | 1 (0.9%) | 0 | 1 | 0.478 |
| Not applicable | 41 (36.9%) | 19 | 22 | 0.431 |
| Other | 11 (9.9%) | 4 | 7 | 0.346 |
| Administrative positions | ||||
| Department Chair/Chief | 2 (1.8%) | 2 | 0 | 0.497 |
| Division Chair/Chief | 4 (3.6%) | 4 | 0 | 0.120 |
| University/Hospital/PA Committee Chair | 10 (9.0%) | 4 | 6 | 0.515 |
| University/Hospital/PA Committee Member | 17 (15.3%) | 7 | 10 | 0.430 |
| None of the above | 78 (70.3%) | 41 | 37 | 1.000 |
*A statistically significant difference
PA: Professional association
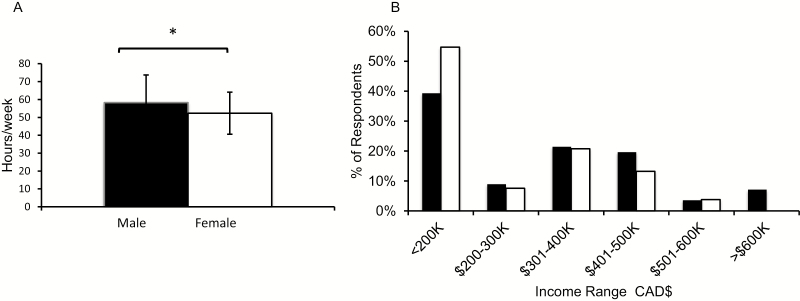
With regards to hours of work per week, male CAG members reported working a mean of 58.3 (±15.4) hours per week, while females worked 52.3 (±11.8) hours (Figure 1A). This difference in workweek was statistically significant (P=0.025). With regards to self-reported gross annual income, the majority of respondents reported earning less than $200,000 (Figure 1B), with no significant difference between male and female respondents.
Figure 1.
A) Average number of hours worked per week. Error bars depict standard deviation from mean. B) Self-reported annual income range of respondents. Black bars depict responses of male respondents, and white bars depict responses of female respondents. *A statistically significant difference, K=1000.
Nonwork-Related commitments
Eighty one percent of respondents had a spouse, with no significant differences between male and female respondents (Table 3). Of the respondents who had a spouse, 29% were married to physicians, which again was similar between genders. Fourteen men and four women were married to spouses who were homemakers (P=0.06). Fifty two percent had children under the age of 18, with no significant difference observed between male and female respondents. Fourteen percent of respondents were responsible for caring for aging relatives, and 31% reported having other significant nonwork-related responsibilities, both of which were equally distributed between the two genders.
Table 3.
Nonwork-related commitments
| Variable | Total (%) (N=111) | Males | Females | P value |
|---|---|---|---|---|
| Spouse/partner | ||||
| Yes | 90 (81.1%) | 51 | 39 | 0.088 |
| No | 21 (18.9%) | 7 | 14 | |
| Children under 18 years | ||||
| Yes | 58 (52.3%) | 26 | 32 | 0.129 |
| No | 53 (47.7%) | 32 | 21 | |
| Number of children (mean±standard deviation) | 2.15 (±0.95) | 1.88 (±0.75) | 0.287 | |
| Care for aging relative(s) | ||||
| Yes | 16 (14.4%) | 9 | 7 | 0.792 |
| No | 95 (85.6%) | 49 | 46 | |
| Other significant non-work related responsibility | ||||
| Yes | 34 (30.6%) | 17 | 17 | 0.838 |
| No | 77 (69.4%) | 41 | 36 | |
Career Satisfaction, Work-Life Balance and Gender and Equity Issues
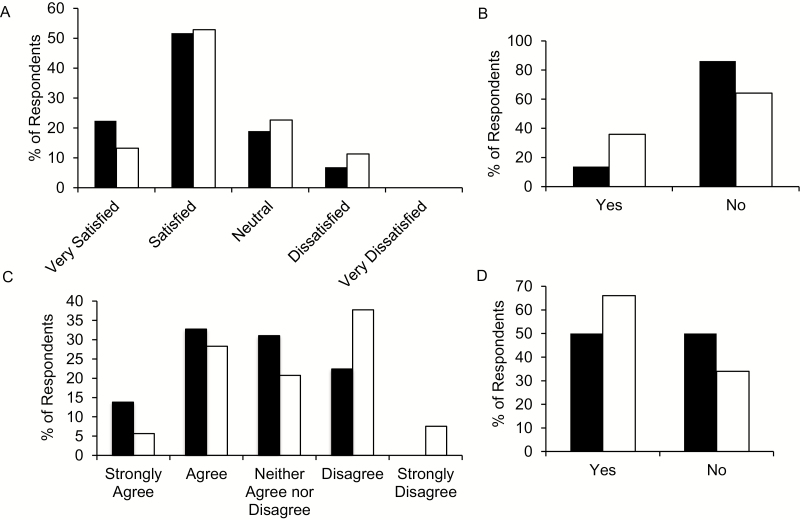
When asked about satisfaction with their current or evolving career path, approximately 70% (74% males compared with 66% of females; P=0.408) reported being either satisfied or very satisfied, and none reported being very dissatisfied (Figure 2A). When asked about perceived barriers, more females than males (36% versus 14%; P=0.008) felt that their age, ethnicity, gender or marital status had hindered their career advancement (Figure 2B). Respondents were asked to what extent they agreed or disagreed with the following statement: “I have been able to balance my home/personal life and work life without hindering my career progression” (Figure 2C). Forty percent of all respondents agreed or strongly agreed with this statement, with no significant differences between the genders (data not shown). However, significantly more females strongly disagreed with this statement (7.5% versus 0%; P=0.008). Furthermore, significantly more females either disagreed or strongly disagreed with this statement (45% versus 22%; P=0.015), indicating that work-life balance was an issue. Both men and women (50% and 66%, respectively) felt that equity and gender issues exist within gastroenterology (Figure 2D).
Figure 2.
A) Career satisfaction of respondents. B) Perception of age/ethnicity/gender/marital status on hindering career advancement. C) Ability to balance home/personal and work life without hindering career progression. D) Perception of the existence of equity & gender issues within gastroenterology? Black bars depict responses of male respondents and white bars depict responses of female respondents.
Needs Assessment of CAG Membership
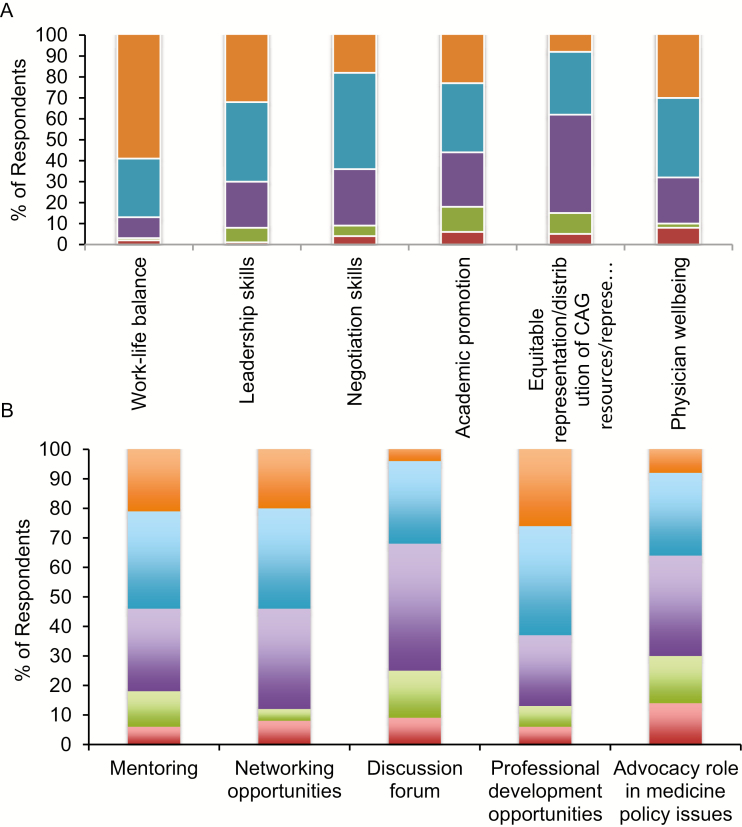
To ascertain which areas may benefit from CAG involvement, members were asked to use a five-point Likert scale to rate the importance of several topics. Of those surveyed, 87% ranked work-life balance as important or very important, while 70% felt physician well-being and leadership skills were important or very important (Figure 3A). Both males and females (58% and 64%, respectively) rated work-life balance as a very important topic (data not shown). Other areas identified included negotiation skills and academic promotion. Regarding potential areas for CAG involvement, mentoring and networking were ranked as important or very important by 55% and 56%, respectively (Figure 3B).
Figure 3.
A) Topics of interest to CAG membership. B) Needs assessment of CAG membership. Responses were on a five-point Likert scale with one being not important and five being very important (orange = five, blue = four, purple = three, green = two, red = one.
Discussion
Despite increasing numbers of women entering the specialty, gastroenterology still remains a male-dominated medical field. It is likely that the demand for female gastroenterologists will increase over time as female patients have been shown to be more likely to have a preference for a female gastroenterologist/endoscopist (6–8).
There have only been a few studies that have addressed gender equity in gastroenterology and only one prior study in Canada, which was reported in 1997 (5). The current study is important because it reports the results of a nationwide survey distributed by the CAG addressing equity and gender issues and represents a more current picture of the gender roles of Canadian gastroenterologists.
Data from our survey demonstrate that more men than women have attained the status of full professor. In our study, there were more male respondents over the age of 55 and more males that had been in practice for a longer duration, both of which increase the likelihood of promotion to full professorship. Nevertheless, this finding is similar to studies done in the United States, where more male gastroenterologists achieved the rank of full professor, with no difference in the proportion of men and women that had attained assistant/associate professorships (4). This does not appear to be limited to the field of gastroenterology, as is evident by a recent study of physicians with faculty appointments at American medical schools demonstrating that women were less likely than men to be full professors even after correcting for age, experience, specialty and research productivity (9). None of the women in our study held the position of department or division chair. Although this may also be related to stage of career, this finding is in keeping with a study that found that women only accounted for 13% (137/1018) of department leaders at the top 50 National Institute of Health (NIH)–funded medical schools in the United States (10). Another possibility is that the differences in academic ranking relate at least in part to research productivity or recognition. We did not specifically ask respondents about their publication track record, grant success, awards and keynote presentations. However, this information may provide insight regarding factors contributing to academic accomplishment and should be considered in any future studies. Mentorship has been shown to affect research productivity, including publication and grant success (11). Thus, targeted mentorship programs can be used as one facet of a multipronged approach to promote the academic success of women in the field of gastroenterology. Universities, professional organizations and hospitals should all work collaboratively to help create tailored policies and programs that encourage faculty to maximize their potential by navigating common personal and institutional barriers.
In the present study, male respondents reported working significantly more hours per week. However, we did not specifically assess the number of faculty that worked full-time versus those that work part-time, and it is possible that this may have contributed to the differences seen in our study. A recent survey of faculty at several US medical schools found that more females (62%) work part-time compared with their male counterparts (12). This was also documented in the American Gastroenterology Association–sponsored survey of US gastroenterologists that found that women were more likely to choose private practice over an academic career because of the availability of part-time options (4). Furthermore, the reasons for choosing part-time work differed, with women choosing part-time work to care for dependent children, while men chose part-time work due to another professional position or to accommodate work at another site (12).
We also found no significant differences in nonwork-related commitments among male and female respondents. This is in contrast to the prior CAG study that demonstrated that female gastroenterologists were less likely to marry (5). A more recent survey by the American Association of Gastroenterology in 2007 also showed no difference in marital status or number of children among male and female respondents (4). Therefore, it is possible that since the initial Canadian study, there have been changes at the institutional and societal levels that removed some of the barriers that prevented female gastroenterologists from taking on family responsibilities. Additionally, in our study, significantly more females strongly felt that they were not able to maintain work-life balance without hindering career progression. Furthermore, significantly more females felt that age, gender, ethnicity or marital status had affected the advancement of their careers. This is in keeping with a previous study where nearly half of all the women surveyed felt that gender had negatively affected their career advancement (4). Additionally, results from the 2014 to 2015 Physician Burnout Survey of the American College of Gastroenterology demonstrated that female sex, younger age, childlessness or having younger children, as well as time spent on domestic and childcare work, were personal factors associated with burnout (13).
In our needs assessment, mentorship was highlighted as an area of importance. A systematic review demonstrated that mentorship impacted career guidance/choice and personal development (11). This study also found that females perceived greater difficulty finding a mentor. It has been suggested that the dearth of female role models may discourage female residents from choosing a career in gastroenterology (4), thereby creating a self-perpetuating cycle that acts to limit the number of women in the subspecialty. Therefore, supporting mentorship is likely to promote the personal and professional success of both men and women, while helping mitigate some of the disadvantages experienced by females. The CAG can play an important role in helping improve both opportunities for mentorship and the quality of mentorship experiences of trainees and junior faculty in gastroenterology.
An overwhelming majority of those surveyed felt that work-life balance and physician well-being were areas that would benefit from CAG involvement. Difficulties maintaining work-life balance have been cited as one of the primary reasons fewer women go into the field of gastroenterology (14). This is timely in the context that a recent study of almost 7000 US physicians found that more physicians reported at least one symptom of burnout in 2014 compared with 2011 (15). The authors also found that satisfaction with work-life balance declined in physicians between 2011 and 2014 (48.5% versus 40.9%). While the prevalence varied among specialties, both internal medicine and pediatric subspecialties demonstrated an increase in physician burnout over this period. Given that burnout and work-life balance can impact the quality of patient care (16–18), it is important that organizations such as CAG develop thoughtful strategies to combat these issues.
There are several limitations to our study. The first limitation is that only 10% of the CAG membership responded to this survey, which increases the possibility of introducing a response bias. Moreover, given the small number of respondents, we were unable to perform subgroup analyses. While low, this response rate is comparable to that of similar studies, including the member survey sponsored by the American Gastroenterology Association (4). Importantly, it is possible that those who perceived gender or equity issues as concerning were more likely to respond to this survey. Low response rates to physician surveys have been an ongoing issue that has previously been explored by studies of research methodology (19, 20). Data from the Canadian National Physician Survey in 2007 do not show a significant increase in response rates with shorter questionnaires, e-mail follow up, marketing strategies or monetary lottery incentives (the latter provided only to trainees) (19). However, given the focus on the field of gastroenterology, promoting future surveys at the annual meeting during Canadian Digestive Diseases Week (CDDW) would likely be of benefit. Additionally, nonmonetary incentives such as the opportunity to win free registration to the CDDW meeting may increase response rates to future surveys of the CAG Diversity and Equity Committee. In addition, while we did send one reminder e-mail, multiple reminders that are strategically timed may also increase response rates in the future. Overall, in spite of the low response rate, we believe this survey has the ability to underscore current issues in the practice of gastroenterology in Canada.
Only 20% of all respondents were trainees (students/residents/fellows), although they comprise 48% of overall CAG membership. While the reason for the low response rate is unclear, it is possible that this could be secondary to many trainees feeling that the survey and its contents were not relevant at their stage of training. In addition, 3% of the respondents were registered nurses or nurse practitioners. Furthermore, about 20% were basic scientists, although it was not clear if they were also involved in clinical work. Given that most of the questions included in this survey were aimed at physicians, it is possible that the inclusion of these groups affected some of the results of this study. For instance, the self-reported income in our survey is below $200,000 and did not significantly vary between males and females, likely reflecting in part the inclusion of trainees and nonphysician members in our study. This is in contrast to the previous CAG survey in 1997, which found the income of females was significantly lower (5). Additionally, another study that followed gastroenterologists for 10 years after graduating from fellowship programs in the United States found that female gastroenterologists earned 22% less per year than their male colleagues after adjusting for practice setting, work hours, practice-ownership, free endoscopy centre practice and vacation time (21). In future assessments, we plan to explore this topic more carefully to determine if such gender-based differences still continues to exist in Canada.
Moreover, while neither the likelihood of having a child nor the mean number of children significantly differed between males and females, this study only collected information on children under the age if 18 because we sought to determine the number of dependents per respondent. It is possible that inclusion of children regardless of age may have affected our results.
Despite these limitations, this study addresses an important gap in our understanding of the current landscape of gastroenterology in Canada. While it is encouraging that female gastroenterologists no longer have to compromise their personal life to the extent that was noted in the previous CAG study, our results demonstrate that barriers remain which prevent females from achieving career success equivalent to their male colleagues. Nonetheless, issues of work-life balance previously thought to affect primarily women appear to be becoming more universal, a phenomenon that has been described before (22). If the field of gastroenterology is to maintain an environment that stimulates and nurtures all its practitioners, then these concerns need to be systematically addressed.
Conclusions
This survey highlights that gender and equity challenges continue to exist within gastroenterology, albeit not to the level reported in previous studies. Our study demonstrates no difference in personal commitments or overall career satisfaction among males and females. However, females were more likely to perceive that their career advancement was affected by gender, ethnicity, age or marital status. In addition, more women reported difficulties maintaining work-life balance. Women were also less likely than men to attain the status of full professor. Furthermore, this study revealed that work-life balance, physician well-being and negotiation skills are areas of importance to many CAG members regardless of gender. The results of this survey also underscore the importance of creating mentoring and networking opportunities as two potential areas that would be of benefit to the CAG membership.
Supplementary Material
Acknowledgements
We would like to thank Palma Colacino for her assistance with this study.
References
- 1. Canadian Medical Education Statistics 2015. The Association of Faculties of Medicine Canada. <https://www.afmc.ca/sites/default/files/documents/en/Publications/CMES/Archives/CMES2015-reduced.pdf> (Accessed July 12, 2016). [Google Scholar]
- 2. 2015–2016 Annual Census of Post-M.D. Trainees. Canadian Post-MD Education Registry (CAPER). <http://caper.ca/~assets/documents/pdf_2015_16CAPER_Census.pdf> (Accessed July 12, 2016). [Google Scholar]
- 3. Canadian Medical Association Gastroenterology Profile 2015. [https://www.cma.ca/Assets/assets-library/document/en/advocacy/Gastronenterology-e.pdf> (Accessed July 12, 2016).
- 4. Gerson LB, Twomey K, Hecht G, et al. Does gender affect career satisfaction and advancement in gastroenterology? Results of an AGA institute-sponsored survey. Gastroenterology 2007;132(4):1598–606. [DOI] [PubMed] [Google Scholar]
- 5. Heathcote J, Cauch-Dudek K, Rhyne D. The professional lives of women in gastroenterology: A Canadian comparison study with men. Gastroenterology 1997;113(2):669–74. [DOI] [PubMed] [Google Scholar]
- 6. Chong VH. Gender preference and implications for screening colonoscopy: Impact of endoscopy nurses. World J Gastroenterol 2012;18(27):3590–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Varadarajulu S, Petruff C, Ramsey WH. Patient preferences for gender of endoscopists. Gastrointest Endosc 2002;56(2):170–3. [DOI] [PubMed] [Google Scholar]
- 8. Shah DK, Karasek V, Gerkin RD, et al. Sex preferences for colonoscopists and GI physicians among patients and health care professionals. Gastrointest Endosc 2011;74(1):122–7.e122. [DOI] [PubMed] [Google Scholar]
- 9. Jena AB, Khullar D, Ho O, et al. Sex differences in academic rank in US Medical Schools in 2014. JAMA 2015;314(11):1149–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wehner MR, Nead KT, Linos K, et al. Plenty of moustaches but not enough women: Cross sectional study of medical leaders. BMJ 2015;351:h6311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: A systematic review. JAMA 2006;296(9):1103–15. [DOI] [PubMed] [Google Scholar]
- 12. Pollart SM, Dandar V, Brubaker L, et al. Characteristics, satisfaction, and engagement of part-time faculty at U.S. medical schools. Acad Med 2015;90(3):355–64. [DOI] [PubMed] [Google Scholar]
- 13. Burke C, Surawicz CM, Oxentenko AS, et al. A National Survey of Burnout in Gastroenterologists. In: World Congress of Gastroenterology at ACG2017. Orlando, Florida: American College of Gastroenterology, 2017. [Google Scholar]
- 14. Shukla R. Current challenges facing women in gastroenterology: How do we move forward?ACG Case Rep J 2016;3(3):144–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015;90(12):1600–13. [DOI] [PubMed] [Google Scholar]
- 16. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg 2010;251(6):995–1000. [DOI] [PubMed] [Google Scholar]
- 17. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction?J Gen Intern Med 2000;15(2):122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grol R, Mokkink H, Smits A, et al. Work satisfaction of general practitioners and the quality of patient care. Fam Pract 1985;2(3):128–35. [DOI] [PubMed] [Google Scholar]
- 19. Grava-Gubins I, Scott S. Effects of various methodologic strategies: Survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician 2008;54(10):1424–30. [PMC free article] [PubMed] [Google Scholar]
- 20. Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med 2001;20(1):61–7. [DOI] [PubMed] [Google Scholar]
- 21. Singh A, Burke CA, Larive B, et al. Women in gastroenterology committee of American college of G: Do gender disparities persist in gastroenterology after 10 years of practice?Am J Gastroenterol 2008;103(7):1589–95. [DOI] [PubMed] [Google Scholar]
- 22. Achkar E. Will women ever break the glass ceiling in medicine?Am J Gastroenterol 2008;103(7):1587–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.