Abstract
Background:
Elevated blood pressure (BP) is the leading global risk factor for mortality. Delay seeking hypertension care is associated with increased mortality.
Objective:
We investigated whether community health workers, equipped with behavioral communication strategies and smartphone technology, can increase linkage of individuals with elevated BP to a hypertension care program in western Kenya and significantly reduce BP.
Methods:
We conducted a cluster randomized trial with three arms: 1) usual care (standard training); 2) “paper-based” (tailored behavioral communication, using paper-based tools); and 3) “smartphone” (tailored behavioral communication, using smartphone technology). The co-primary outcomes were: 1) linkage to care, and 2) change in systolic BP (SBP). A covariate-adjusted mixed-effects model was used, adjusting for differential time to follow-up. Bootstrap and multiple imputation were used to handle missing data.
Results:
1460 individuals (58% women) were enrolled (491 usual care, 500 paper-based, 469 smartphone). Average baseline SBP was 159.4 mmHg. Follow-up measures of linkage were available for 1128 (77%) and BP for 1106 (76%). Linkage to care was 49% overall, with significantly greater linkage in the usual care and smartphone arms. Average overall follow-up SBP was 149.9 mmHg. Participants in the smartphone arm experienced a modestly greater reduction in SBP vs. usual care (−13.1 mmHg vs. −9.7), but this difference was not statistically significant. Mediation analysis revealed that linkage to care contributed to SBP change.
Conclusions:
A strategy combining tailored behavioral communication and mHealth for CHWs led to improved linkage to care, but not statistically significant improvement in SBP reduction. Further innovations to improve hypertension control are needed.
Trial Registration:
Registered as on www.clinicaltrials.gov.
Keywords: hypertension, linkage to care, community health workers, tailored behavioral communication, smartphone technology, Kenya
Condensed Abstract:
Elevated blood pressure (BP) is the leading global risk factor for mortality. We investigated whether community health workers, equipped with behavioral communication strategies and smartphone technology, can increase linkage of individuals with elevated BP to a hypertension care program and significantly reduce BP. We conducted a cluster randomized trial, enrolling 1460 individuals across three arms (491 usual care, 501 paper-based, 469 smartphone). Linkage to care was 49% overall, with significantly greater linkage in the usual care and smartphone arms. Average overall follow-up SBP was 149.9 mmHg. SBP reduction in the smartphone arm was not significantly greater than usual care.
Background
Hypertension, a major risk factor for ischemic heart disease, heart failure, and stroke (1), is the leading global risk for mortality (2). However, hypertension awareness, treatment, and control rates are low in Africa and worldwide (3). Given that hypertension may be asymptomatic, linkage and retention to care and medication adherence are particularly difficult challenges (4). Previous research in Kenya has indicated that linkage to hypertension care is very low, approximately 25% (5). Delays in seeking hypertension care have been shown to be associated with increased mortality (6). Thus, early linkage to hypertension care and successful retention to clinical services are critical components of hypertension management.
Recent studies have indicated that non-physician health workers (NPHWs) can improve hypertension management and blood pressure control (7,8). In particular, community health workers (CHWs)—members of a community who have received basic training to supply community members access to health and social services, to educate individuals about various health issues, and to support overall community development (9)—have been shown to have positive impact when integrated into hypertension management programs (10). However, the specific impact of CHWs on linkage to hypertension care in Africa is relatively unknown.
We report here the results of the LARK Hypertension Study, which aimed to evaluate the impact of CHWs, equipped with behavioral communication strategies and mobile health (mHealth) technology, on linkage to hypertension care and blood pressure reduction among individuals with elevated blood pressure in western Kenya.
Methods
Setting
Full details of the study design and methods have previously been described (11). Briefly, the Academic Model Providing Access to Healthcare Partnership (AMPATH) was initiated in Kenya in 2001 and has established an HIV care system in western Kenya that has served over 160,000 patients (12). Based on that foundation, and in partnership with the Government of Kenya, AMPATH has expanded its clinical scope of work to include hypertension (13). This study was conducted within the AMPATH infrastructure in western Kenya, in Kosirai and Turbo Divisions. The protocol was approved by the institutional review boards of all participating institutions, and the study is registered on www.clinicaltrials.gov (identifier ).
Study Design
After an initial formative phase of qualitative inquiry (14), we used a participatory, iterative design process to develop the interventions, involving stakeholders representing clinicians, patients, CHWs, administrators, and informatics personnel. We conducted a cluster randomized trial with three arms: 1) usual care (CHWs with standard training); 2) “paper-based” (CHWs trained in tailored behavioral communication, using paper-based tools); and 3) “smartphone” (CHWs with tailored behavioral communication, using smartphone technology). The unit of randomization was a geographically and administratively unique Community Unit (population approximately 5000), stratified by Division, and there were a total of 24 clusters (eight per arm). Each Community Unit is geographically nearby a rural health facility associated with the AMPATH hypertension program. The randomization process was conducted centrally by biostatisticians at Brown University. The participants and research staff were not blinded to intervention assignments. Study roll-out was conducted sequentially by arm: first the usual care community units, followed by paper-based and then smartphone intervention community units.
Participants and Procedures
Inclusion criteria for this study included adult individuals with elevated BP (SBP ≥ 140 or diastolic BP (DBP) ≥ 90) during community-based BP screening performed by trained research assistants, using a standard protocol with automated Omron blood pressure machines as described by WHO STEPS (15) and the Global Alliance for Chronic Diseases (16). Exclusion criteria were individuals without elevated BP, those who were acutely ill and required immediate medical attention at the time of testing, and individuals who did not provide informed consent. Individuals actively engaged in hypertension care were excluded from the study. Individuals who met inclusion criteria and no exclusion criteria were enrolled at the time of the community-based BP screening.
At the health facility, each individual had a repeat BP measured by the clinician, and those with repeat elevated BP were entered into the hypertension management program as “patients”. Patients were managed according to the AMPATH hypertension protocol derived from consensus guidelines for hypertension management, using drugs contained in the Kenyan national formulary (17-19). Once linked to care, patients were managed by a clinician (either a clinical officer or nurse) who had undergone hypertension care training and were equipped with the same care protocols. The clinicians had access to teleconsultation with a specialist whenever necessary.
An individual who did not present to the health facility within one month of BP testing was assigned to a CHW specific to the participant’s community unit, who was requested to visit that individual to encourage linkage to care. The CHW was equipped with the behavioral communication strategy +/− the mHealth tool, depending on which trial arm to which the CHW’s community unit was randomly allocated.
In the usual care arm, the CHW referred the individual to the health facility for further evaluation and management, as per the usual AMPATH clinical care protocol. In the paper-based arm, the CHW was instructed to engage in behavioral, clinical, and environmental assessments, followed by a tailored behavioral and motivational engagement, to help facilitate linkage to care. In the smartphone arm, the CHW conducted the same assessments described above; however, s/he was also equipped with a smartphone that had real-time decision support and data entry linked to the electronic health record. Thus, the smartphone provided the tailored messaging and specific recommendations based on inputs from the assessments. The smartphone technology also allowed for alternative messaging modalities, including images, audio-recordings, and video-recordings (Web Appendix). Follow-up assessment, including BP measurement, was conducted by trained research staff.
Statistical Analysis
The co-primary outcome measures were: 1) documented linkage to care and 2) change in SBP. The study was powered on the linkage to care outcome. With 24 clusters across three trial arms, our power calculations demonstrated > 80% power to detect a 20% difference in linkage, for a range of participants per cluster (down to average of 50 per cluster).
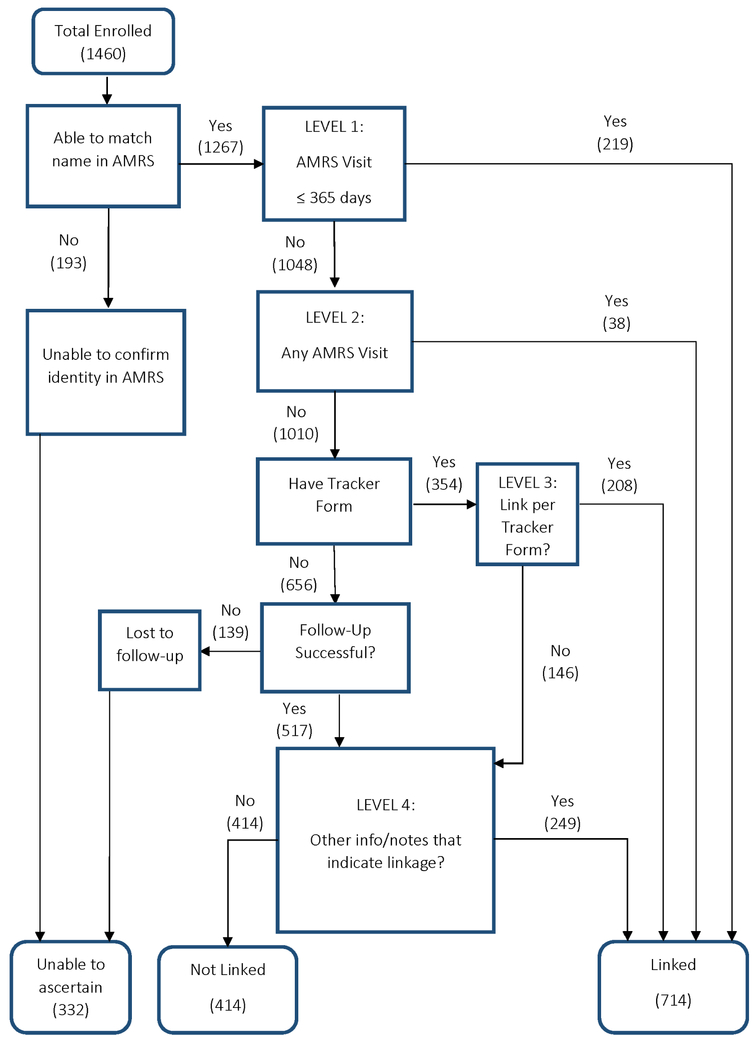
The binomial linkage measure included either a visit at a health facility documented in the electronic medical record or a self-reported visit. Linkage to care was originally assessed by relying on data entered into the AMPATH Medical Records System (AMRS), an electronic medical record and clinical database, to confirm attendance at a clinic visit. However, this proved problematic due to several reasons, including: 1) some individuals had multiple AMRS identification numbers, some of which did not match the AMRS number recorded on the research data collection form; 2) some individuals had demographic data in the AMRS clinical dataset that did not match demographic data collected by the research team, thus challenging verification of the individual’s identity; 3) some participants who actually linked to care did not have clinical information entered into the AMRS clinical database. In an attempt to mitigate these issues, a data collection form to record self-reported linkage to care was specifically created and administered to LARK participants at the research follow-up visit. Since the above-described AMRS difficulties were detected after the trial had already started, not all participants were administered the “linkage tracker form.” The research assistants kept notes about participants in their research logs, which were also used to determine linkage status if the tracker form was not available. We therefore constructed different categories of linkage depending on the nature and quality of data available for each participant (Figure 1).
Figure 1. LARK linkage flow diagram.
Figure illustrates the different categories of linkage to hypertension care for participants in the study.
Mixed-effects models were used throughout to evaluate the outcome measures, using an intention-to-treat approach, taking into account geographical clustering. Bootstrap and multiple imputation were used to account for missing covariate and outcome data, and to nest the primary outcomes and mediation analyses under one analytic umbrella. First, 6000 bootstrapped samples of the data were generated, including missing values and using geographic community as the sampling unit (20). Next, multiple imputation was used to create one complete dataset from each bootstrapped sample (21). The main outcome analyses were adjusted for age, gender, enrollment SBP, and baseline covariates that were found to differ significantly across arms: enrollment in national health insurance, tobacco and/or alcohol use, employment status, physical activity, awareness of hypertension status, and geographic division. Due to differential time to follow-up assessment across trial arms, the effects of the interventions on SBP were estimated at 15 months after enrollment, a time point common to all trial arms. We used a non-parametric spline for time to follow-up and allowed a linear interaction between trial arm and follow-up time. We averaged the estimates for the mean effect and constructed bootstrap 95th percentile confidence intervals, removing the runs that did not converge. We also present a secondary analysis of the SBP outcome based on a partially adjusted model with only baseline SBP and follow-up time as covariates. All analyses were conducted in R version 3.5.1.
We hypothesized that the LARK intervention would impact follow-up SBP by changing linkage to hypertension care. In order to test that causal hypothesis, we conducted a causal mediation analysis dividing the total intervention effect into the direct and indirect (mediated by linkage to care) effects (22), using the mediation package in R (23).
Results
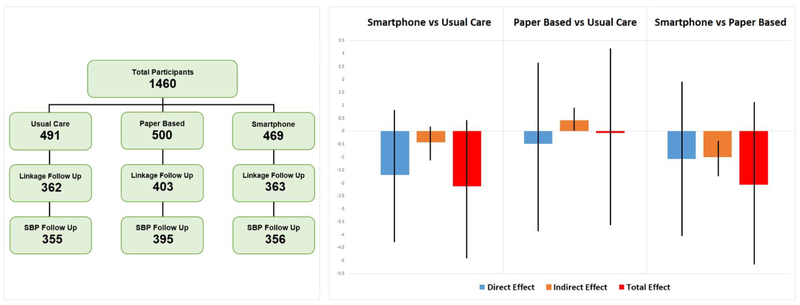
1460 individuals (58% women) were enrolled (491 usual care, 500 paper-based, 469 smartphone) (Central Illustration). Average baseline SBP was 159.4 mmHg and DBP was 89.7 mmHg. Full baseline characteristics are shown in Table 1. Notably, 21% of individuals reported no formal employment, and nearly 50% reported monthly earnings <5,000 Kenyan Shillings (approximately US $50) per month. While individuals in the smartphone arm were more likely to report no formal employment, the combined percentage of individuals either unemployed or earning <$50 per month was equivalent across all arms. Only 15% reported having enrolled in the Kenyan governmental national health insurance plan. Additional baseline characteristics are provided in Supplemental Table 1.
Central Illustration. LARK participant Flow and Systolic Blood Pressure Outcomes.
The figure illustrates both participant flow through enrollment and follow-up, as well as the fully adjusted SBP outcomes analysis including mediation. Vertical bars indicate 95% confidence intervals (Table 3). SBP = systolic blood pressure
Table 1.
LARK Baseline Demographic Characteristics stratified by arm. Values are mean (standard deviation) and N (%). * p<0.05 for a difference between any two study arms.
| Characteristic | Value | Total (n=1460) |
Usual Care (n=491) |
Paper Based (n=500) |
Smart Phone (n=469) |
|---|---|---|---|---|---|
| # Participants per Community Unit | 60.8 (14.2) | 61.3 (11.7) | 62.5 (9.6) | 58.6 (20.7) | |
| Age (years) | |||||
| 54.2 (16.4) | 54.6 (16.9) | 53.7 (15.6) | 54.3 (16.7) | ||
| Missing | 13 | 11 | 2 | 0 | |
| Gender | |||||
| Female | 849 (58) | 308 (63) | 278 (56) | 263 (56) | |
| Male | 611 (42) | 183 (37) | 222 (44) | 206 (44) | |
| Geographic Division | |||||
| Mosoriot | 482 (33) | 158 (32) | 205 (41) | 119 (25) | |
| Turbo | 978 (67) | 333 (68) | 295 (59) | 350 (75) | |
| Enrollment Diastolic BP | |||||
| 89.7 (12.0) | 89.0 (12.3) | 90.4 (12.1) | 89.7 (11.5) | ||
| Missing | 122 | 69 | 49 | 4 | |
| Enrollment Systolic BP* | |||||
| 159.4 (19.5) | 158.4 (19.6) | 158.3 (20.3) | 161.3 (18.5) | ||
| Missing | 122 | 69 | 49 | 4 | |
| Employment Status* | |||||
| No Job | 307 (21) | 84 (17) | 79 (16) | 144 (31) | |
| Farmer | 733 (50) | 284 (58) | 250 (50) | 199 (42) | |
| Business Person | 189 (13) | 64 (13) | 64 (13) | 61 (13) | |
| Public Sector Employee | 54 (4) | 13 (3) | 25 (5) | 16 (3) | |
| Student | 4 (0) | 1 (0) | 2 (0) | 1 (0) | |
| Other | 151 (10) | 34 (7) | 72 (14) | 45 (10) | |
| Missing | 22 (2) | 11 (2) | 8 (2) | 3 (1) | |
| Monthly Earnings (Kenyan Shillings per month) | |||||
| No Job | 307 (21) | 84 (17) | 79 (16) | 144 (31) | |
| <5000 | 720 (49) | 264 (54) | 259 (52) | 197 (42) | |
| >=5000 & <10,000 | 198 (14) | 55 (11) | 77 (15) | 66 (14) | |
| >=10,000 & <20,000 | 79 (5) | 28 (6) | 26 (5) | 25 (5) | |
| >=20,000 & <30,000 | 36 (2) | 7 (1) | 16 (3) | 13 (3) | |
| >=30,000 | 28 (2) | 10 (2) | 12 (2) | 6 (1) | |
| Missing | 92 (6) | 43 (9) | 31 (6) | 18 (4) | |
| Have National Health Insurance?* | |||||
| No | 1217 (83) | 427 (87) | 417 (83) | 373 (80) | |
| Yes | 214 (15) | 53 (11) | 70 (14) | 91 (19) | |
| Missing | 29 (2) | 11 (2) | 13 (3) | 5 (1) | |
| Physical Activity: > 150 moderate-equivalent minutes per week* | |||||
| No | 411 (28) | 123 (25) | 136 (27) | 152 (32) | |
| Yes | 986 (68) | 347 (71) | 344 (69) | 295 (63) | |
| Missing | 63 (4) | 21 (4) | 20 (4) | 22 (5) | |
| Current tobacco use* | |||||
| No | 1325 (91) | 458 (93) | 448 (90) | 419 (89) | |
| Yes | 113 (8) | 23 (5) | 43 (9) | 47 (10) | |
| Missing | 22 (2) | 10 (2) | 9 (2) | 3 (1) | |
| Current alcohol use* | |||||
| No | 1245 (85) | 441 (90) | 406 (81) | 398 (85) | |
| Yes | 193 (13) | 39 (8) | 86 (17) | 68 (14) | |
| Missing | 22 (2) | 11 (2) | 8 (2) | 3 (1) |
Follow-up measures of linkage were available for 1128 (77%). Our primary linkage outcome is “linkage overall” given the challenges described above about relying solely on the AMRS clinical data. Linkage to care was 49% overall (Table 2), with significantly greater linkage in the usual care and smartphone arms (Table 3). Linkage according to the AMRS clinical data was 15%.
Table 2.
Summary of outcome measures overall and by arm. Values are mean (standard deviation) and N (%).
| Outcome Variable | value | Total (n=1460) |
Usual Care (n=491) |
Paper Based (n=500) |
Smart Phone (n=469) |
|---|---|---|---|---|---|
| Link in 1 year, captured in AMRS | |||||
| No | 1048 (72) | 312 (64) | 385 (77) | 351 (75) | |
| Yes | 219 (15) | 100 (20) | 63 (13) | 56 (12) | |
| Unable to capture in AMRS | 193 (13) | 79 (16) | 52 (10) | 62 (13) | |
| Linkage Overall | |||||
| No | 414 (28) | 117 (24) | 186 (37) | 111 (24) | |
| Yes | 714 (49) | 245 (50) | 217 (43) | 252 (54) | |
| Unable to Ascertain | 332 (23) | 129 (26) | 97 (19) | 106 (23) | |
| Follow up systolic BP | |||||
| 149.9 (21.8) | 150.0 (22.9) | 150.2 (21.6) | 149.4 (20.8) | ||
| Missing | 354 | 136 | 105 | 113 | |
| Follow up diastolic BP | |||||
| 90.8 (13.5) | 90.1 (13.7) | 91.0 (14.1) | 91.3 (12.7) | ||
| Missing | 354 | 136 | 105 | 113 | |
| Change in Systolic BP | |||||
| −10.4 (23.3) | −9.7 (25.1) | −8.4 (24.0) | −13.1 (20.5) | ||
| Missing | 451 | 188 | 147 | 116 | |
| Change in Diastolic BP | |||||
| 0.7 (14.2) | 0.1 (14.7) | 0.4 (15.2) | 1.5 (12.7) | ||
| Missing | 451 | 188 | 147 | 116 | |
| Controlled BP at follow up | |||||
| No | 817 (56) | 256 (52) | 289 (58) | 272 (58) | |
| Yes | 289 (20) | 99 (20) | 106 (21) | 84 (18) | |
| Missing | 354 | 136 | 105 | 113 | |
| Days between enrollment and follow up | |||||
| 552.8 (181.4) | 615.6 (197.2) | 580.2 (184.9) | 459.8 (111.0) | ||
| Missing | 354 | 136 | 105 | 113 |
Table 3.
Summary of effects of intervention on linkage to care, SBP, and BP control. Mediation analysis presented, including direct, indirect, and total effect. *Incorporates multiple imputation and the bootstrap, and partially adjusted for baseline SBP and follow-up time. **Incorporates multiple imputation and the bootstrap, and fully adjusted for: baseline SBP, follow-up time, age, gender, enrollment in national health insurance, tobacco and/or alcohol use, employment status, physical activity, awareness of hypertension status, and geographic division.
| Paper Based vs Usual Care |
Smartphone vs Usual Care |
Smartphone vs Paper Based |
|
|---|---|---|---|
| Linkage to Care (OR, 95% CI) | |||
| Unadjusted | 0.65 (0.44, 0.94) | 1.28 (0.75, 2.10) | 1.99 (1.28, 3.03) |
| Fully adjusted | 0.63 (0.43, 0.91) | 1.21 (0.70, 2.01) | 1.95 (1.23, 3.01) |
| SBP (Difference, 95% CI) | |||
| Partially adjusted* | −0.49 (−4.06, 2.81) | −2.08 (−4.84, 0.53) | −1.59 (−4.67, 1.70) |
| Total Effect (Fully adjusted)** | −0.06 (−3.61, 3.20) | −2.13 (−4.89, 0.42) | −2.07 (−5.14, 1.12) |
| Direct Effect | −0.48 (−3.85, 2.64) | −1.70 (−4.27, 0.81) | −1.07 (−4.03, 1.91) |
| Indirect (mediated) Effect | 0.43 (0.05, 0.89) | −0.43 (−1.11, 0.16) | −1.00 (−1.71, −0.39) |
| BP control (OR, 95% CI) (Fully adjusted) | 0.97 (0.63, 1.42) | 0.95 (0.61, 1.38) | 1.00 (0.69, 1.40) |
Follow-up information for BP was available for 1106 individuals (76%). Average overall follow-up SBP and DBP were 149.9 and 90.8 mmHg, respectively. The intraclass correlation coefficient of SBP was estimated to be 0.01 in an unadjusted, complete-case model. The participants in the smartphone arm experienced a slightly greater reduction in SBP than usual care (−13.1 mmHg vs. −9.7), but this difference was not statistically significant in the fully adjusted model (difference −2.13 mmHg (95% confidence interval (CI) −4.89, 0.42)). BP control (<140/90) was achieved in 26% of participants with follow-up BP data, and there was no statistically significant difference across the study arms.
Mediation analysis revealed that linkage to care contributed to SBP change (Central Illustration; Table 3). For the smartphone vs. usual care comparison, the direct effect was estimated at −1.70 mmHg and the indirect (mediated) effect was −0.43. For the smartphone vs. paper-based comparison, the direct and indirect effects were −1.07 and −1.00, respectively. Additional outcome measures are provided in Supplemental Table 2.
Discussion
In this cluster randomized trial in western Kenya, CHWs equipped with a tailored behavioral communication strategy and a smartphone-based mHealth tool led to improved linkage to hypertension care but not statistically significant improvement in SBP reduction among hypertensive individuals, compared to usual care. Some of the SBP effect was mediated by linkage to care. Participants in all three arms of the trial experienced substantial reductions in SBP. While not statistically significant, the smartphone-based intervention tended towards modestly greater improvement in SBP reduction. It is quite plausible that, with a larger sample size, a statistically significant improvement would have resulted. Given the substantive absolute declines in SBP observed in our study, substantial cardiovascular and mortality benefit would be expected from a clinical and population perspective.(24)
Other studies using CHWs for hypertension and other non-communicable disease care have demonstrated a positive impact from CHW-based interventions. For instance, trained NPHWs can accurately perform cardiovascular risk screening to identify high-risk patients and counsel them on behavior change (25-27). NPHWs can also screen for oral and cervical cancers (28,29); screen and treat depression (30,31), prescribe and dispense medications for conditions including epilepsy, diabetes, hypertension, and asthma (32-34), and track and improve patients’ adherence to these therapies. In our study, the usual care arm outperformed historical comparisons and our expectations.(35) It is quite possible that the context of the trial contributed to better-than-expected performance of the usual care CHWs, thus challenging comparisons between intervention arms and usual care. While we note that all arms generated a substantive decline in SBP among trial participants, the lack of a statistically significant comparison across arms also indicates a need to consider other innovative ways to deliver hypertension care while incorporating CHWs into the management team.
Our smartphone-based intervention did improve linkage to hypertension care compared to both the usual care and paper-based arms, which did contribute to SBP reduction. Other interventions to improve linkage to care include facilitating transportation and reducing transport costs (36), portable care delivered outside the health facility in community and group settings (5), and improved health insurance coverage (37). Future interventions to improve linkage and retention to hypertension care should therefore consider a multi-component approach that incorporates several of these strategies. Indeed, linkage and retention to hypertension care remain substantial problems for hypertension management in many parts of the world (38).
One of the key baseline factors in our study population was the notable poverty and lack of health insurance. More than half of our participants were either unemployed or earned less than $1.50 per day. Over 80% had no health insurance. In the face of that economic adversity and lack of financial protection, it is not surprising that our intervention had limited additional impact compared to usual care. Neither the tailored behavioral communication strategy nor the smartphone-based tool intervened directly upon the economic reality of our study participants, which has been shown to impact health-seeking behavior and linkage to care (39). In response to this adverse economic context, we have subsequently developed other interventions that combine economic and health components (e.g., the BIGPIC trial), in order to more directly intervene upon those structural factors (40). The results of the BIGPIC trial will help to illuminate the impact of interventions that tackle the economic reality of individuals residing in low-resource settings worldwide.
The global burden of hypertension and other non-communicable diseases is substantial and increasing, especially in low- and middle-income countries. Each step in the clinical cascade, including linkage and retention to care, can benefit from improved implementation. The LARK Hypertension Study demonstrates that CHWs have the potential to improve linkage to care, which can contribute to improved blood pressure. Our study adds to the growing literature demonstrating that the infrastructure and strategies that have been established for the control of communicable diseases—including community-based screening, task redistribution within teams, partnerships with local providers, and medical informatics—can serve as a foundation for an integrated delivery system approach to the control of non-communicable chronic conditions (41). Our results also highlight the need for further innovations to improve hypertension management and control in low-resource settings worldwide (42).
Admittedly, there were several limitations to our study. One significant challenge was the initial reliance on clinical data stored in the AMRS, a strategy that ultimately was deemed to have several shortcomings. While we rectified the situation and created a fully stand-alone research database that assessed self-reported linkage, there remain limitations to self-reported data, as is well known. Second, there were missing data, both at baseline and at follow-up, which impacted our analytic approach and influenced the imputation methods utilized. Third, there were some significant baseline differences across trial arms, likely due to the cluster randomized nature of the trial, which necessitated an analytic approach that accounted for those baseline differences. Fourth, there was differential time to follow-up across the arms that required analytic rectification. Fifth, due to the same limitations we have described for the linkage determination via AMRS, we unfortunately do not have access to medication prescribing data for the participants derived from the clinical records. While we do have data on self-reported medication usage, we do not feel confident in the reliability of those self-reported data, and therefore did not include medication prescription information in this manuscript. Finally, individuals who participated in the community-based BP screening activities may not be fully representative of the general population. .
Conclusions
A strategy combining tailored behavioral communication and mHealth for CHWs led to improved linkage to care, with modest, but not statistically significant, improvement in SBP reduction among individuals with elevated BP in western Kenya. Further innovations to improve engagement in the hypertension care cascade and hypertension control are needed.
Supplementary Material
Perspectives.
Competency in Systems-Based Practice: Community health workers in rural Africa equipped with behavioral and communication strategies and can improve linkage to hypertension care.
Translational Outlook: More implementation research is needed to develop strategies that translate linkage to hypertension care into better long-term clinical outcomes.
Acknowledgments:
The authors would like to thank the LARK research team members for their assistance with all aspects of the project. We would like to thank all study participants for their involvement with this project.
Funding: Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number 1U01HL114200.
Abbreviations
- AMRS
AMPATH Medical Records System
- AMPATH
Academic Model Providing Access to Healthcare Partnership
- BP
blood pressure
- CHW
community health worker
- DBP
diastolic blood pressure
- NPHW
non-physician health worker
- SBP
systolic blood pressure
Footnotes
Competing Interests: The authors declare that they have no competing interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–13. [DOI] [PubMed] [Google Scholar]
- 2.Stanaway JD, Afshin A, Gakidou E et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2018;392:1923–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chow CK, Teo KK, Rangarajan S et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Rural and Urban Communities in High-, Middle-, and Low-Income Countries Global Prevalence and Control of Hypertension Global Prevalence and Control of Hypertension. JAMA 2013;310:959–968. [DOI] [PubMed] [Google Scholar]
- 4.Khatib R, Schwalm J-D, Yusuf S et al. Patient and Healthcare Provider Barriers to Hypertension Awareness, Treatment and Follow Up: A Systematic Review and Meta-Analysis of Qualitative and Quantitative Studies. PLOS ONE 2014;9:e84238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pastakia S, Manyara S, Vedanthan R et al. Impact of Bridging Income Generation with GrouP Integrated Care (BIGPIC) on Hypertension and Diabetes in Rural Western Kenya. Journal of General Internal Medicine 2017;32:540–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moodley J Maternal deaths associated with hypertension in South Africa: lessons to learn from the Saving Mothers report, 2005-2007. Cardiovasc J Afr 2011;22:31–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogedegbe G, Plange-Rhule J, Gyamfi J et al. Health insurance coverage with or without a nurse-led task shifting strategy for hypertension control: A pragmatic cluster randomized trial in Ghana. PLoS Med 2018;15:e1002561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joshi R, Alim M, Kengne AP et al. Task Shifting for Non-Communicable Disease Management in Low and Middle Income Countries – A Systematic Review. PLOS ONE 2014;9:e103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prasad B, Muraleedharan V. Community Health Workers: a Review of Concepts, Practice and Policy Concerns. HRH Global Resource Center, 2007. [Google Scholar]
- 10.He J, Irazola V, Mills KT, et al. Effect of a community health worker–led multicomponent intervention on blood pressure control in low-income patients in argentina: A randomized clinical trial. JAMA 2017;318:1016–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vedanthan R, Kamano JH, Naanyu V et al. Optimizing linkage and retention to hypertension care in rural Kenya (LARK hypertension study): study protocol for a randomized controlled trial. Trials 2014;15:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Einterz RM, Kimaiyo S, Mengech HN et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med 2007;82:812–8. [DOI] [PubMed] [Google Scholar]
- 13.Bloomfield GS, Kimaiyo S, Carter EJ et al. Chronic noncommunicable cardiovascular and pulmonary disease in sub-Saharan Africa: an academic model for countering the epidemic. Am Heart J 2011;161:842–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naanyu V, Vedanthan R, Kamano JH et al. Barriers influencing linkage to hypertension care in Kenya: qualitative analysis from the lark hypertension study. Journal of general internal medicine 2016;31:304–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO STEPS Surveillance Manual: The WHO STEPwise approach to chronic disease risk factor surveillance. Geneva, 2005. [Google Scholar]
- 16.Riddell MA, Edwards N, Thompson SR et al. Developing consensus measures for global programs: lessons from the Global Alliance for Chronic Diseases Hypertension research program. Global Health 2017;13:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003;21:1983–92. [DOI] [PubMed] [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Jama 2003;289:2560–72. [DOI] [PubMed] [Google Scholar]
- 19.Clinical Management and Referral Guidelines, Volume III Nairobi, Kenya: Ministry of Medical Services and Ministry of Public Health and Sanitation, 2010. [Google Scholar]
- 20.Schomaker M, Heumann C. Bootstrap inference when using multiple imputation. Statistics in Medicine 2018;37:2252–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Multivariate Imputation by Chained Equations. https://cran.r-project.org/web/packages/mice/index.html. Accessed July 12, 2019
- 22.Imai K, Keele L, Yamamoto T. Identification, Inference and Sensitivity Analysis for Causal Mediation Effects, 2010. [Google Scholar]
- 23.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. mediation: R Package for Causal Mediation Analysis. 2014 2014;59:38. [Google Scholar]
- 24.Ettehad D, Emdin CA, Kiran A et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet (London, England) 2016;387:957–967. [DOI] [PubMed] [Google Scholar]
- 25.Abegunde DO, Shengelia B, Luyten A et al. Can non-physician health-care workers assess and manage cardiovascular risk in primary care? Bulletin of the World Health Organization 2007;85:432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaziano TA, Abrahams-Gessel S, Denman CA et al. An assessment of community health workers' ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: an observational study. The Lancet Global Health 2015;3:e556–e563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan M, Lamelas P, Musa H et al. Development, Testing, and Implementation of a Training Curriculum for Nonphysician Health Workers to Reduce Cardiovascular Disease. Global heart 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gajalakshmi CK, Krishnamurthi S, Ananth R, Shanta V. Cervical cancer screening in Tamilnadu, India: a feasibility study of training the village health nurse. Cancer Causes & Control 1996;7:520–524. [DOI] [PubMed] [Google Scholar]
- 29.Warnakulasuriya K, Ekanayake A, Sivayoham S et al. Utilization of primary health care workers for early detection of oral cancer and precancer cases in Sri Lanka. Bulletin of the World Health Organization 1984;62:243. [PMC free article] [PubMed] [Google Scholar]
- 30.Patel V, Weiss HA, Chowdhary N et al. Lay health worker led intervention for depressive and anxiety disorders in India: impact on clinical and disability outcomes over 12 months. The British Journal of Psychiatry 2011;199:459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weobong B, Weiss HA, McDaid D et al. Sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial. PLoS medicine 2017;14:e1002385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kengne AP, Fezeu L, Awah PK, Sobngwi E, Mbanya JC. Task shifting in the management of epilepsy in resource-poor settings. Epilepsia 2010;51:931–932. [DOI] [PubMed] [Google Scholar]
- 33.Kengne AP, Sobngwi E, Fezeu LL et al. Nurse-led care for asthma at primary level in rural sub-Saharan Africa: the experience of Bafut in Cameroon. Journal of Asthma 2008;45:437–443. [DOI] [PubMed] [Google Scholar]
- 34.Labhardt ND, Balo JR, Ndam M, Grimm JJ, Manga E. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Serv Res 2010;10:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pastakia SD, Manyara SM, Vedanthan R et al. Impact of Bridging Income Generation with Group Integrated Care (BIGPIC) on Hypertension and Diabetes in Rural Western Kenya. Journal of General Internal Medicine 2017;32:540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kotwani P, Balzer L, Kwarisiima D et al. Evaluating linkage to care for hypertension after community-based screening in rural Uganda. Trop Med Int Health 2014;19:459–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fang J, Zhao G, Wang G, Ayala C, Loustalot F. Insurance Status Among Adults With Hypertension-The Impact of Underinsurance. J Am Heart Assoc 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geldsetzer P, Manne-Goehler J, Marcus M-E et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. The Lancet. [DOI] [PubMed] [Google Scholar]
- 39.Musinguzi G, Anthierens S, Nuwaha F, Van Geertruyden JP, Wanyenze RK, Bastiaens H. Factors Influencing Compliance and Health Seeking Behaviour for Hypertension in Mukono and Buikwe in Uganda: A Qualitative Study. Int J Hypertens 2018;2018:8307591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vedanthan R, Kamano JH, Lee H et al. Bridging Income Generation with Group Integrated Care for cardiovascular risk reduction: Rationale and design of the BIGPIC study. Am Heart J 2017;188:175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rabkin M, El-Sadr WM. Why reinvent the wheel? Leveraging the lessons of HIV scale-up to confront non-communicable diseases. Glob Public Hlth 2011;6:247–56. [DOI] [PubMed] [Google Scholar]
- 42.Vedanthan R, Bernabe-Ortiz A, Herasme OI et al. Innovative Approaches to Hypertension Control in Low- and Middle-Income Countries. Cardiology Clinics 2017;35:99–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.