Abstract
Objectives:
The aims of this study were to identify the prevalence of molar–incisor hypomineralization (MIH) in a group of low-income schoolchildren and to evaluate the role of maternal education on MIH and dental caries in these children.
Materials and Methods:
This cross-sectional study enrolled 686 schoolchildren. To evaluate dental caries, the International Caries Dental Assessment System II (ICDAS) criteria were utilized. MIH was assessed by using the European Academy of Paediatric Dentistry criteria. Mixed-effects models were applied for the data analysis.
Results:
The prevalence of MIH was 35.4% (244). Most children exhibited moderate MIH (163, 67.1%), followed by mild MIH (45, 18.5%) and severe MIH (35, 14.4%). Caries presence in the first permanent molars, evaluated using ICDAS score, indicated that the mean number of noncavitated and cavitated lesions (ICDAS ≥2) was 0.90 (±0.30); the mean number of lesions with ICDAS ≥3 was 0.36 (±0.48). Odds ratio (OR) analysis of MIH severity revealed that the children of mothers with low education were more likely to exhibit MIH (OR 2.13; 95% confidence interval [CI]: 1.25–3.85). Modeling of dental caries (ICDAS ≥3) revealed that low maternal education (OR 2.27; 95% CI: 1.25–4.16) and the presence of MIH (OR 4.37; 95% CI: 3.05–6.25) were associated with dental caries.
Conclusions:
There were associations between low maternal education and both MIH and dental caries. The presence of both initial and cavitated caries lesions was associated with MIH. Dentists should offer adequate advice to mothers with children with MIH, based on their educational background.
KEYWORDS: dental caries, maternal education, molar–incisor hypomineralization, oral hygiene
INTRODUCTION
Molar–incisor hypomineralization (MIH) has a systemic origin. The causative insult appears during the stage of enamel hardening, thereby leading to reduced mineral deposition. MIH can occur in one or more first permanent molars (FPMs); permanent incisors can be affected simultaneously.[1] Clinically, MIH is characterized by clearly demarcated opacities, which vary in color from white to brown. In more severe cases, loss of enamel may occur, typically as a consequence of mastication forces.[2] In addition, patients experience hypersensitivity, pain, and appearance-related concerns.[3] Importantly, MIH is regarded as a cause of tooth loss.[4,5]
An association between MIH and dental caries has been identified in several population groups.[4] The presence of anomalies (such as MIH) in tooth formation limits the prevention of dental caries and increases the cost of dental treatment. Furthermore, the impact of MIH may be greater in groups with high risk of caries. The number of prevalent cases in 2015 was estimated at 878 million people.[6] There is a wide variation in the prevalence of this condition: from 2.4% in Bulgaria to 40.2% in Brazil.[7] With the exception of Brazil, there is little information regarding the prevalence of MIH in Latin American counties.[8,9]
The etiology of MIH is unclear. Both prenatal and postnatal factors have been associated with this developmental defect. These risk factors include the presence of respiratory infections, preterm birth, low birth weight, otitis media, fever, asthma, the use of antibiotics, and prior to birth maternal illness.[10,11] In addition, twin studies found that genetic factors are involved in the etiology of MIH. Despite the large number of studies regarding the prevalence and etiology of MIH, there are inconclusive data concerning the relationship between the socioeconomic status and prevalence of MIH.[11,12,13,14] A study in the UK found that children from high-income groups had a higher prevalence of MIH.[15] In contrast, a study in Brazil showed that children from rural areas had a higher prevalence of MIH than their urban counterparts.[16]
A systematic review of the literature indicated that low socioeconomic status was associated with high risk of caries.[17] Maternal education is frequently evaluated to determine socioeconomic status in epidemiological studies, because maternal education has been associated with significant health outcomes in children, including infant mortality.[18] In a similar manner, low maternal education has been associated with high dental caries index and high prevalence of gingivitis.[19,20] A longitudinal study in Australia revealed a higher dental caries risk in children whose mothers had fewer than 10 years of education, compared with those whose mothers had more than 12 years of education.[21] Information regarding the relationships among MIH, dental caries, and maternal education may facilitate the identification of strategies for the improvement of oral health in children.
Therefore, the aim of this study was to identify the prevalence of MIH in a group of low-income schoolchildren and to evaluate the association of maternal education with MIH and dental caries in these children.
MATERIALS AND METHODS
The study group was gathered from an area Southeast of Mexico City. Based on data from the Mexican National Council for the Evaluation of Social Development Policy (CONEVAL), the area selected for the study was located among three municipalities with the highest poverty index in Mexico City. According to CONEVAL, a person is in a situation of poverty when they have at least a social deficiency (in terms of education, access to health services, access to social security, quality of housing spaces, and home utilities, such as gas and electricity) and if their income is insufficient to acquire goods and services to satisfy their basic food and nonfood needs.[22]
A single-stage cluster sampling plan was applied. Each of the public primary schools in the area was defined as a cluster. The three schools included in the study were randomly selected from among the eight public schools located in the study area. This area was defined based on information from the National Institute of Statistics and Informatics of Mexico. This Institution divides Mexico City into basic geographical areas, which are extensions that correspond to a geostatistical subdivision of the municipalities; these areas serve as the basic units of the National Geostatistical Framework. The sample size was calculated for an odds ratio (OR) of 2, considering that the proportion of children affected by dental caries in the FPMs in the group without MIH was 30%, (1−β) = 0.80, and α = 0.05. The resulting sample size was 540 children. In accordance with the guidance of the school authorities who advised invitations of entire classes, a total of 762 children, 7–12-years, were invited. The inclusion criteria required that the parents signed a consent form for the participation of their children in the study and that the child assented to an oral examination; the children were also required to be present during the days of the oral examination, in order to be included in the study. Informed consent was obtained from the parents of 713 students (93.6% response rate). Children in whom no FPMs were erupted or who had no more than one-third of the anatomical crown visible in any FPM were excluded from the present report (10, 1.4%). In addition, 17 (2.4%) children were excluded because they had not attended school during the days of the study. Therefore, the total number of participants was 686. In addition, upon signing the informed consent, the parents were requested to provide sociodemographic information. The study protocol was approved by the Ethics Committee of the Division of Graduate Studies and Research, Faculty of Dentistry, National Autonomous University of Mexico (CIE/02/10/06/2016/06-2).
CLINICAL ORAL EXAMINATION
Oral examinations were performed under an artificial white light, using a World Health Organization type probe with a 2-mm ball end. The evaluation of MIH was performed in accordance with criteria established by the European Academy of Paediatric Dentistry MIH/HSPM on wet teeth, after the children had brushed their teeth with a dentist’s supervision.[23] Two calibrated dentists examined the children’s oral cavities. To standardize the criteria for assessment of dental caries (International Caries Dental Assessment System II [ICDAS]) and MIH, the first stage comprised a discussion session to review the criteria for dental caries and MIH. This session included comments on the visual material provided to learn ICDAS II and MIH.[24,25] Differential diagnoses with other types of enamel defects were examined (dental fluorosis, amelogenesis imperfecta, enamel hypoplasia, and other types of tooth malformations). The second stage comprised two field sessions, working with the schoolchildren. The aim of these sessions was to review the criteria applied in the observed lesions and to improve consistency in the diagnosis of oral conditions included in the study. Twenty children participated in this exercise (they were not included in the study sample). Cases involving difficult diagnoses were discussed until an agreement was reached with the senior examiner (MI-C). The inter- and intra-examiner kappa values were ≥0.85 for ICDAS (cutoff value code ≥3), ≥0.80 for MIH (present/absent), ≥0.77 for MIH severity (mild/moderate-to-severe cutoff value code ≥2), and ≥0.85 for Simplified-Oral Hygiene Index (S-OHI) (cutoff value code ≥2). During the survey, 10% of the oral examinations were repeated to ascertain the reliability of the examiners during data collection.
A child was diagnosed with MIH if at least one of the FPMs was affected. After determining the presence of MIH, the severity of this condition was assessed using the following criteria: a surface was considered to exhibit mild MIH when demarcated opacities affected less than one-third of the tooth surface, without posteruptive enamel breakdown; moderate MIH involved demarcated opacities that affected at least one-third but less than two-thirds of the surface, without posteruptive enamel breakdown; atypical caries lesions could affect less than two-thirds of the surface. Severe MIH involved demarcated opacities that affected more than two-thirds of the tooth surface, or the presence of posteruptive enamel breakdown, atypical caries lesions larger than two-thirds of the surface, or large restaurations with unusual shape, extended to smooth surfaces, or extraction of the tooth because of MIH.
The ICDAS II criteria include initial lesions that are clinically detectable due to changes in the enamel tooth color and opacity (Codes 1 and 2).[26] Compressed air drying was unavailable; therefore, Code 1 was not recorded in the study. To assess caries prevalence, each child was classified based on the tooth reflecting the highest ICDAS score. The decayed, missing, and filled teeth (dmft and DMFT) indices were obtained based on the ICDAS II score; the cutoff value for the decayed component of the index was code 3. The S-OHI criterion for classifying debris was applied for the evaluation of biofilm deposits.[27]
The variables included in the analysis were sex, age, maternal education, frequency of toothbrushing (cutoff point ≤1, times/day), S-OHI (cutoff point >2), MIH (presence/absence), MIH severity (mild/moderate-to-severe cutoff value code ≥2), and dental caries ICDAS (cutoff point code ≥2 and code ≥3).
STATISTICAL ANALYSIS
Bivariate analysis for categorical variables was performed using the Chi-square test. For continuous variables, the Kruskal–Wallis test was applied. Mixed logistic regression models were calculated for dental caries using two different cutoff values (cutoff value ≥2 and cutoff value ≥3). In addition, this type of models were used to analyze the prevalence and severity of MIH. Random intercept models were performed because the children were clustered in schools. ORs and 95% confidence intervals (CIs) were obtained. The statistical significance level was P < 0.05. STATA V14 (StataCorp LLC, College Station, Texas, USA) was used for data analysis.
RESULTS
Among the 686 children studied, the mean age was 9.0 (±1.4) years; 365 (53.2%) were girls. The mothers of 67 children (9.8%) had no formal education or had some years of elementary school; mothers of 269 children (39.2%) finished elementary school or had some middle-school education; and mothers of 350 children (51.0%) finished middle school or had higher educational attainment (≥9 years).
Most children brushed their teeth twice or more per day (531, 77.4%); 155 (22.6%) brushed once per day or less often. Fluoride toothpaste was used by 98.8% of the children, and 82.4% used the same brand, which contained 1450 ppmF. The S-OHI demonstrated that 176 (25.7%) of the participants had poor oral hygiene (S-OHI ≥2). Older age was associated with higher frequency of toothbrushing, (P < 0.001). Accordingly, older children showed better oral hygiene (S-OHI <2) than younger children (P < 0.001). Children whose mothers had higher educational attainment brushed more frequently (P = 0.002). Low brushing frequency (once per day or less) was observed in 37.3% of children whose mothers had no formal education or had some years of elementary school. About one-quarter (24.2%) of the children in the group with mothers who finished elementary school or some middle-school education had low brushing frequency; 18.2% of children whose mothers finished middle school or had higher educational attainment had low brushing frequency (P = 0.002).
MOLAR INCISOR HYPOMINERALIZATION
The prevalence of MIH was 243/686 (35.4%). Figure 1 depicts the percentage of FPMs and incisors affected by MIH; molars were more frequently affected than incisors. Among the affected children, the distribution of molars with MIH was as follows: 16 (6.6%) had one FPM, 53 (21.7%) had two FPMs, 69 (28.3%) had three FPMs, and 106 (43.4%) had four FPMs. In the children with MIH, the mean number of affected FPMs was 3.1 (±0.94). A child was assigned to a severity category based on the most severely affected FPM. Most of the children with MIH were in the moderate category (163, 67.1%), followed by the mild category (45, 18.5%) and the severe category (35, 14.4%).
Figure 1.
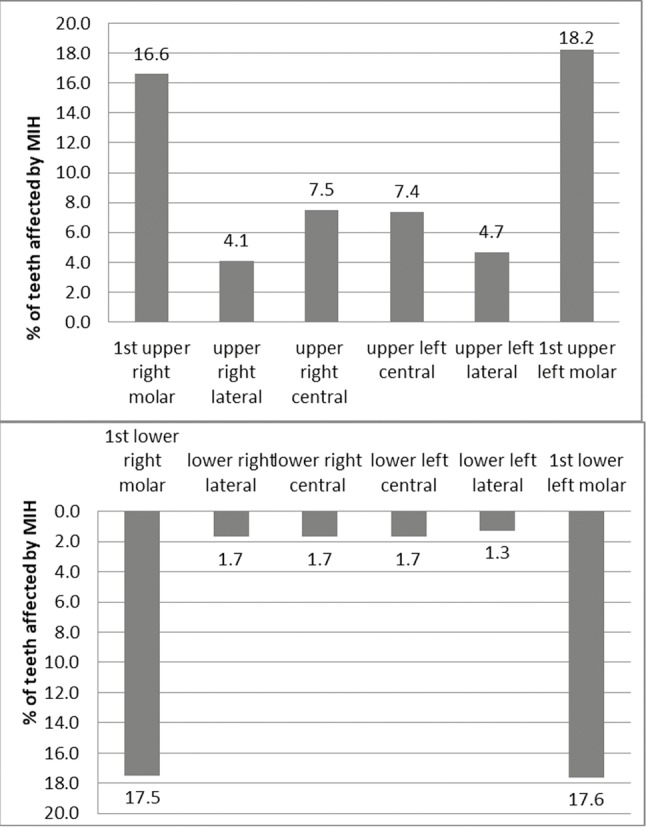
Percentage distribution of molar–incisor hypomineralization of the upper and lower central and lateral incisors and first permanent molars
Table 1 presents the results of bivariate analysis regarding the MIH prevalence, MIH severity, age, sex, maternal education, S-OHI, and toothbrushing frequency. Older children showed a higher prevalence of MIH (P = 0.032). No significant sex-based difference was found in MIH prevalence (P = 0.137). Lower brushing frequency was identified in children with MIH (P = 0.034), compared with children without this defect. MIH severity was similar, and there were significant associations with age (P = 0.002) and toothbrushing frequency (P = 0.039).
Table 1.
Frequency distribution of age, sex, maternal education, oral hygiene by presence, and severity of molar–incisor hypomineralization
| Variables | MIH presence | MIH severitya | ||||
|---|---|---|---|---|---|---|
| No (n = 443), n (%) | Yes (n = 243), n (%) | P | Codes 0–1 (n = 488), n (%) | Codes 2–3 (n = 198), n (%) | P | |
| Age, mean±SD | 8.9±1.51 | 9.2±1.40 | 0.032 | 8.9±1.50 | 9.3±1.41 | 0.002 |
| Sex | ||||||
| Females | 245 (67.1) | 120 (32.9) | 0.137 | 265 (72.6) | 100 (27.4) | 0.366 |
| Male | 198 (61.7) | 123 (38.3) | 223 (69.5) | 98 (30.5) | ||
| Maternal education | ||||||
| No formal education or elementary school | 39 (10.5) | 28 (89.5) | 0.500b | 40 (59.7) | 27 (40.3) | 0.076 |
| Elementary school or some middle school | 24 (58.2) | 245 (41.8) | 191 (71.0) | 78 (29.0) | ||
| Middle school or higher educational attainment | 230 (65.7) | 120 (34.3) | 257 (73.4) | 93 (27.6) | ||
| Toothbrushing frequency (/day) | ||||||
| ≤1 | 89 (57.4) | 66 (42.6) | 0.034 | 100 (64.5) | 55 (35.5) | 0.039 |
| >1 | 354 (66.7) | 177 (33.3) | 388 (73.0) | 143 (26.9) | ||
| Dental biofilm | ||||||
| OHI <2 | 328 (64.3) | 182 (35.7) | 0.806 | 356 (69.8) | 154 (30.2) | 0.190 |
| OHI ≥2 | 115 (65.3) | 61 (34.7) | 132 (75.0) | 44 (25.0) | ||
aMIH severity code: 0 = No MIH, 1 = Mild, 2 = Moderate, 3 = severe, bChi-square test P value of maternal education categories. MIH = Molar–incisor hypomineralization, SD = Standard deviation, OHI = Oral Hygiene Index
DENTAL CARIES
In the primary dentition, the mean dmf score was 2.81 (± 2.9) including children of 7–10 years. In the permanent dentition, the mean DMFT score was 0.77 (±1.31) in children of 7–12 years. Restorations in permanent teeth were detected in 67 (9.8%) of the children and one child showed missing permanent teeth due to the extraction of two FPMs. Caries experience in FPMs, evaluated using ICDAS score, indicated that the mean number of no-cavitated and cavitated lesions (ICDAS ≥2) was 0.90 (±0.30); considering ICDAS ≥3, the mean was 0.36 (±0.48). Figure 2 depicts the distribution of children by dental caries status in FPMs according to the ICDAS criterion. In FPMs, ICDAS codes ≥2 were observed in 618 (90.1%); the number of children with ICDAS ≥3 was 249 (36.3%).
Figure 2.
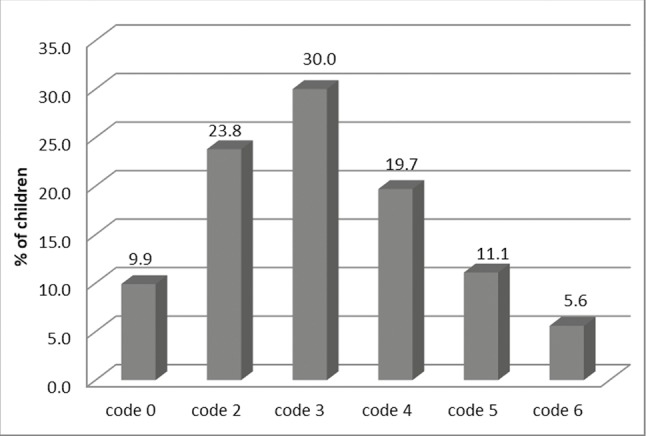
Percentage distribution of children by the International Caries Dental Assessment System codes
Table 2 presents the distribution of children by age, sex, maternal education, and oral hygiene score, brushing frequency, and MIH across the dental caries index using two cutoff points (ICDAS ≥2 and ICDAS ≥3) in FPMs. The results of bivariate analysis showed an association with age (P < 0.001) using both cutoff points of ICDAS score. Higher frequency of tooth brushing, once per day or more, was associated with lower prevalence of cavitated caries lesions (ICDAS ≥3) (P < 0.001). In addition, the presence of MIH was associated with higher ICDAS score for both of the two cutoff values applied (P < 0.001).
Table 2.
Distribution of age, sex, maternal education, oral hygiene, and molar–incisor hypomineralization by the International Caries Dental Assessment System II score, using two cutoff points International Caries Dental Assessment System II codes ≥2 and International Caries Dental Assessment System II codes ≥3 in first permanent molars
| Variables | ICDAS 0 (n = 68), n (%) | ICDAS ≥2 (n = 618), n (%) | P | ICDAS (0–2) (n = 437), n (%) | ICDAS ≥3 (n = 249), n (%) | P |
|---|---|---|---|---|---|---|
| Age, mean±SD | 8.5±1.51 | 9.1±1.52 | <0.001 | 8.7±1.50 | 9.5±1.29 | <0.001 |
| Sex | ||||||
| Females | 35 (10.9) | 286 (89.1) | 0.415 | 230 (63.0) | 135 (37.0) | 0.689 |
| Male | 33 (9.0) | 332 (91.0) | 207 (64.5) | 114 (35.5) | ||
| Maternal education | ||||||
| No formal education or elementary school | 7 (10.5) | 60 (89.5) | 0.784a | 36 (53.7) | 31 (46.3) | 0.077a |
| Elementary school or some middle school | 24 (8.9) | 245 (91.1) | 166 (61.7) | 103 (38.3) | ||
| Middle school or higher educational attainment | 37 (10.6) | 313 (89.4) | 235 (67.1) | 115 (32.9) | ||
| Toothbrushing frequency (/day) | ||||||
| ≤1 | 58 (10.9) | 473 (89.1) | 0.101 | 356 (67.0) | 175 (33.0) | <0.001 |
| >1 | 354 (66.7) | 177 (33.3) | 388 (73.0) | 143 (26.9) | ||
| Dental biofilm | ||||||
| OHI <2 | 50 (9.8) | 460 (90.2) | 0.871 | 334 (65.5) | 176 (34.5) | 0.190 |
| OHI ≥2 | 18 (10.2) | 158 (89.9) | 103 (58.5) | 73 (41.5) | ||
| MIH | ||||||
| No | 57 (12.9) | 386 (87.1) | <0.001 | 103 (42.4) | 140 (57.6) | <0.001 |
| Yes | 11 (4.5) | 232 (95.5) | 334 (75.4) | 109 (24.6) |
aChi-square test P value of maternal education categories. ICDAS = International Caries Dental Assessment System II, MIH = Molar–incisor hypomineralization, SD = Standard deviation, OHI = Oral Hygiene Index
MIXED-EFFECTS MODELS
The ORs from the logistic regression mixed model for the MIH prevalence and severity are shown in Table 3. The association between age and MIH indicated that older children were more likely to have MIH, or to have moderate or severe levels of MIH, compared with younger children, adjusted by sex, and maternal education. The severity of MIH was associated with maternal education. Children whose mothers did not have any formal education or only had some elementary school showed a higher probability of severe forms of MIH than children whose mothers had higher educational attainment (OR 2.13, P = 0.006), adjusted by age and sex.
Table 3.
Odds ratios of the mixed-effects models for molar–incisor hypomineralization prevalence and severity for age, sex, and maternal educationa,b
| Variables | MIH presencea | MIH severityb | ||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age | 1.14 (1.02–1.27) | 0.018 | 1.22 (1.09–1.37) | <0.001 |
| Sexc | ||||
| Female | 0.77 (0.56–1.05) | 0.103 | 0.82 (0.59–1.15) | 0.254 |
| Maternal educationd | ||||
| Elementary school or some middle school | 1.39 (0.79–2.38) | 0.251 | 1.79 (1.02–3.13) | 0.042 |
| No formal education or elementary school | 1.51 (0.88–2.63) | 0.127 | 2.13 (1.25–3.85) | 0.006 |
aMIH present in any first permanent molar, bMIH severity = No MIH or mild MIH versus moderate and severe levels. Reference category: cSex = Males, dMaternal education = Middle school or higher level of education. MIH = Molar–incisor hypomineralization, OR = Odds ratio, CI = Confidence interval
Table 4 presents the mixed model ORs for dental caries, using two cutoff points (ICDAS ≥2 and ICDAS ≥3). The model for ICDAS ≥2 indicated that the presence of MIH was associated with higher probability of dental caries, including noncavitated lesions (OR = 2.91, P = 0.002). The model for ICDAS ≥3 showed an association with biofilm accumulation (OR = 1.84, P = 0.003). In addition, children whose mothers had no formal education or had some elementary school had a higher probability of caries lesions (ICDAS ≥2), compared with children whose mothers completed middle school or higher education (OR 2.27, P = 0.008). The results of the model indicated that children with MIH were more likely to show cavitated caries lesions (ICDAS ≥3) (OR 4.37, P < 0.001), compared to children without MIH.
Table 4.
Mixed-effects model odds ratios of age, maternal education, and oral hygiene and molar–incisor hypomineralization by International Caries Dental Assessment System II score, using two cutoff points International Caries Dental Assessment System II codes ≥2 and International Caries Dental Assessment System II codes ≥3
| Variables | ICDAS ≥2 | ICDAS ≥3 | ||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age | 1.33 (1.10–1.60) | 0.003 | 1.62 (1.42–1.86) | <0.001 |
| Maternal educationa | ||||
| Elementary school or some middle school | 0.85 (0.34–2.08) | 0.715 | 0.68 (0.37–1.25) | 0.212 |
| No formal education or elementary school | 1.10 (0.46–2.63) | 0.833 | 0.44 (0.24–0.80) | 0.008 |
| Dental biofilmb | ||||
| OHI ≥2 | 1.08 (0.61–1.94) | 0.788 | 1.84 (1.23–2.76) | 0.003 |
| MIHc | ||||
| Yes | 2.91 (1.49–5.69) | 0.002 | 4.37 (3.05–6.25) | <0.001 |
Reference category: aMaternal education = Middle school or higher level of education, bDental biofilm = S-OHI <2, cMIH = No MIH. MIH = Molar–incisor hypomineralization, OR = Odds ratio, CI = Confidence interval, ICDAS = International Caries Dental Assessment System II, OHI = Oral Hygiene Index, S-OHI = Simplified-OHI
DISCUSSION
In the present study, maternal education, poor oral hygiene, and the presence of MIH increased the likelihood of cavitated caries lesions. The association between MIH and dental caries was present for both cutoff points analyzed (ICDAS ≥2 and ICDAS ≥3). MIH enamel has lower Ca and P content, reduced hardness, higher porosity, and protein content, compared to unaffected enamel. These characteristics may explain the association between MIH and dental caries.[28]
Accordingly, a literature review by Americano et al.,[4] regarding the relationship between caries and MIH, found an association between these conditions. In that review, most studies used DMFT to assess dental caries, and only one study performed in Germany included precavitated lesions; the number of permanent molars with MIH was not associated with the presence of this type of caries lesion. Those authors argued that it is more likely that the low caries prevalence and high number of sealed teeth in the study group did not allow the identification of an association between dental caries and MIH.[29] Moreover, a study in Iraqi children with precavitated caries lesions found an association between the severity of MIH and the level of caries destruction in FPMs. Teeth with MIH that exhibited posteruptive enamel breakdown were ten-fold more likely to exhibit large lesions (ICDAS ≥5) than teeth with ICDAS codes 0–4.[30] However, there was not a clear pattern in terms of the relationship between the severity of MIH and the severity of dental caries. Furthermore, a study in Spain did not find an association between the prevalence of MIH and dental caries; however, caries was significantly higher in children with severe MIH than in children without MIH.[31] Further studies are needed to identify the impact of MIH in each stage of dental caries lesion development.
The global prevalence of MIH varies considerably and shows variation within respective countries.[6] Approximately one-third of the Mexican children examined presented MIH. A previous study in Mexico showed a lower prevalence (15.8%) than that identified in the present study.[8] Studies in other countries also demonstrated variations in the MIH prevalence among different groups.[9] Methodological differences may limit comparisons among studies.
In the present study, MIH was associated with age. It has been suggested that the severity of teeth with MIH increases in an age-related manner, due to increased exposure to the oral environment.[16] It has been observed that proper oral hygiene in teeth with MIH is difficult because of the increased sensitivity of the affected teeth to thermal and mechanical stimuli.[3] Accordingly, the results of this study indicated that children with MIH had a lower brushing frequency than children without MIH.
In the present study, lower maternal schooling was associated with the higher prevalence of dental caries. This is consistent with the results of a meta-analysis that showed that low socioeconomic status was associated with the increased prevalence of caries.[17] Maternal education may be associated with higher income, and therefore, greater access to preventive methods, such as toothpaste, toothbrush, oral rinses, as well as improved access to preventive professional care. Further, it is possible that more educated mothers have better knowledge regarding children’s health.[32] It is likely that mothers with low educational background consumed unhealthy diets, including more fermentable carbohydrates.[33] However, maternal education has shown a direct effect on dental caries that was not mediated by sweet food intake.[20]
In the present study, an association was identified between maternal education and severity of MIH. Some of the pre- and post-natal presumed causes of MIH have been associated with low maternal educational background; for instance, preterm birth and low birth weight.[34] In a large national birth cohort study in the United States, more advantageous health investment behaviors at each phase of early development during the 1st years of life were associated with higher levels of maternal education.[35] However, some studies did not find an association between the presence of MIH and maternal education.[12] In the present study, an association was identified between MIH severity and maternal education, but not between the MIH prevalence and maternal education. It is possible that the assessment of MIH severity has greater sensitivity for associated factors than the assessment of MIH prevalence.
A limitation of this study was its cross-sectional design; nevertheless, MIH is a condition that occurs during tooth formation and therefore precedes the development of dental caries. The presence of restorations limits the identification of MIH defects. In the present study, approximately 10% of the children had restorations; and consequently, this was not a major factor for underdiagnosis of MIH. Information regarding other risk factors of dental caries (e.g., sugar consumption and use of dental services) was unavailable. In addition, a convenience sample was utilized, which included low Socioeconomic position (SEP) children of Mexico City. Thus, the results cannot be extrapolated to high-income children. However, in Mexico, a large proportion of the population is in a low SEP. A notable strength of the study was the high participation rate of the families in the included schools. In addition, the examiners were carefully calibrated to obtain reliable information with respect to the oral health assessment. The use of ICDAS criteria for dental caries provided detailed information regarding dental caries within the children, thus allowing analysis of additional elements with respect to the association of dental caries with MIH.
CONCLUSIONS
More than one-third of the children in this study had MIH. A strong association was found between MIH and cavitated caries lesions. Both dental caries and MIH severity were associated with low maternal education. Adequate preventive and treatment programs are required to control dental caries and provide timely treatment of teeth affected by MIH. Close attention is needed to ensure adequate counseling of mothers regarding this developmental condition, particularly those with low educational background, in order to reduce inequalities and improve children’s quality of life.
FINANCIAL SUPPORT AND SPONSORSHIP
Metropolitan Autonomous University-Xochimilco (UAM-X) and The Master and Doctoral Dental Medical Sciences and Health Program, National Autonomous University of Mexico (UNAM), and the National Council for Science and Technology (CONACYT).
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENTS
The authors acknowledge the support of the Metropolitan Autonomous University-Xochimilco (UAM-X) and The Master and Doctoral Dental Medical Sciences and Health Program, National Autonomous University of Mexico (UNAM), and the National Council for Science and Technology (CONACYT), Mexico.
REFERENCES
- 1.Weerheijm KL, Jälevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35:390–1. doi: 10.1159/000047479. [DOI] [PubMed] [Google Scholar]
- 2.Jälevik B, Norén JG. Enamel hypomineralization of permanent first molars: a morphological study and survey of possible aetiological factors. Int J Paediatr Dent. 2000;10:278–89. doi: 10.1046/j.1365-263x.2000.00210.x. [DOI] [PubMed] [Google Scholar]
- 3.Raposo F, de Carvalho Rodrigues AC, Lia ÉN, Leal SC. Prevalence of hypersensitivity in teeth affected by molar-incisor hypomineralization (MIH) Caries Res. 2019;53:424–30. doi: 10.1159/000495848. [DOI] [PubMed] [Google Scholar]
- 4.Americano GC, Jacobsen PE, Soviero VM, Haubek D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int J Paediatr Dent. 2017;27:11–21. doi: 10.1111/ipd.12233. [DOI] [PubMed] [Google Scholar]
- 5.Albadri S, Zaitoun H, McDonnell ST, Davidson LE. Extraction of first permanent molar teeth: results from three dental hospitals. Br Dent J. 2007;203:E14. doi: 10.1038/bdj.2007.679. discussion 408-9. [DOI] [PubMed] [Google Scholar]
- 6.Schneider PM, Silva M. Endemic molar incisor hypomineralization: a pandemic problem that requires monitoring by the entire health care community. Curr Osteoporos Rep. 2018;16:283–8. doi: 10.1007/s11914-018-0444-x. [DOI] [PubMed] [Google Scholar]
- 7.Jälevik B. Prevalence and diagnosis of molar-incisor- hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent. 2010;11:59–64. doi: 10.1007/BF03262714. [DOI] [PubMed] [Google Scholar]
- 8.Gurrusquieta BJ, Núñez VM, López ML. Prevalence of molar incisor hypomineralization in Mexican children. J Clin Pediatr Dent. 2017;41:18–21. doi: 10.17796/1053-4628-41.1.18. [DOI] [PubMed] [Google Scholar]
- 9.Zhao D, Dong B, Yu D, Ren Q, Sun Y. The prevalence of molar incisor hypomineralization: evidence from 70 studies. Int J Paediatr Dent. 2018;28:170–9. doi: 10.1111/ipd.12323. [DOI] [PubMed] [Google Scholar]
- 10.Silva MJ, Scurrah KJ, Craig JM, Manton DJ, Kilpatrick N. Etiology of molar incisor hypomineralization - A systematic review. Community Dent Oral Epidemiol. 2016;44:342–53. doi: 10.1111/cdoe.12229. [DOI] [PubMed] [Google Scholar]
- 11.Brogårdh-Roth S, Matsson L, Klingberg G. Molar-incisor hypomineralization and oral hygiene in 10- to-12-yr-old Swedish children born preterm. Eur J Oral Sci. 2011;119:33–9. doi: 10.1111/j.1600-0722.2011.00792.x. [DOI] [PubMed] [Google Scholar]
- 12.Allazzam SM, Alaki SM, El Meligy OA. Molar incisor hypomineralization, prevalence, and etiology. Int J Dent. 2014;2014:234508. doi: 10.1155/2014/234508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teixeira RJPB, Andrade NS, Queiroz LCC, Mendes FM, Moura MS, Moura LFAD, et al. Exploring the association between genetic and environmental factors and molar incisor hypomineralization: evidence from a win study. Int J Paediatr Dent. 2018;28:198–206. doi: 10.1111/ipd.12327. [DOI] [PubMed] [Google Scholar]
- 14.Wuollet E, Laisi S, Alaluusua S, Waltimo-Sirén J. The association between molar-incisor hypomineralization and dental caries with socioeconomic status as an explanatory variable in a group of Finnish children. Int J Environ Res Public Health. 2018:15. doi: 10.3390/ijerph15071324. pii: E1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balmer R, Toumba J, Godson J, Duggal M. The prevalence of molar incisor hypomineralisation in Northern England and its relationship to socioeconomic status and water fluoridation. Int J Paediatr Dent. 2012;22:250–7. doi: 10.1111/j.1365-263X.2011.01189.x. [DOI] [PubMed] [Google Scholar]
- 16.da Costa-Silva CM, Jeremias F, de Souza JF, Cordeiro Rde C, Santos-Pinto L, Zuanon AC. Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent. 2010;20:426–34. doi: 10.1111/j.1365-263X.2010.01097.x. [DOI] [PubMed] [Google Scholar]
- 17.Schwendicke F, Dörfer CE, Schlattmann P, Foster Page L, Thomson WM, Paris S. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 2015;94:10–8. doi: 10.1177/0022034514557546. [DOI] [PubMed] [Google Scholar]
- 18.Li Q, Tsui AO. Maternal risk exposure and adult daughters’ health, schooling, and employment: A constructed cohort analysis of 50 developing countries. Demography. 2016;53:835–63. doi: 10.1007/s13524-016-0472-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oliveira LB, Sheiham A, Bönecker M. Exploring the association of dental caries with social factors and nutritional status in brazilian preschool children. Eur J Oral Sci. 2008;116:37–43. doi: 10.1111/j.1600-0722.2007.00507.x. [DOI] [PubMed] [Google Scholar]
- 20.Peres MA, Nascimento GG, Peres KG, Demarco FF, Menezes AB. Oral health-related behaviours do not mediate the effect of maternal education on adolescents’ gingival bleeding: A birth cohort study. Community Dent Oral Epidemiol. 2018;46:169–77. doi: 10.1111/cdoe.12350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ju X, Jamieson LM, Mejia GC. Estimating the effects of maternal education on child dental caries using marginal structural models: the longitudinal study of indigenous Australian children. Community Dent Oral Epidemiol. 2016;44:602–10. doi: 10.1111/cdoe.12259. [DOI] [PubMed] [Google Scholar]
- 22.National Council for the Evaluation of Social Development Policy (CONEVAL). Poverty Statistics in Mexico City. [Last accessed on 2019, June 12]. Available from: https://www.coneval.org.mx/coordinacion/entidades/DistritoFederal/PublishingImages/municipal_2015/CDMX.JPG .
- 23.Weerheijm KL. Molar incisor hypomineralisation (MIH) Eur J Paediatr Dent. 2003;4:114–20. [PubMed] [Google Scholar]
- 24.International Caries Detection and Assessment System. [Last accessed on 2018 November 21]. Available from: https://www.iccms-web.com/
- 25.Ghanim A, Silva MJ, Elfrink MEC, Lygidakis NA, Mariño RJ, Weerheijm KL, et al. Molar incisor hypomineralisation (MIH) training manual for clinical field surveys and practice. Eur Arch Paediatr Dent. 2017;18:225–42. doi: 10.1007/s40368-017-0293-9. [DOI] [PubMed] [Google Scholar]
- 26.Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007;35:170–8. doi: 10.1111/j.1600-0528.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 27.Greene JC, Vermillion JR. The Simplified Oral Hygiene Index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 28.Elhennawy K, Manton DJ, Crombie F, Zaslansky P, Radlanski RJ, Jost-Brinkmann PG, et al. Structural, mechanical and chemical evaluation of molar-incisor hypomineralization-affected enamel: A systematic review. Arch Oral Biol. 2017;83:272–81. doi: 10.1016/j.archoralbio.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Heitmüller D, Thiering E, Hoffmann U, Heinrich J, Manton D, Kühnisch J, et al. GINIplus Study Group. Is there a positive relationship between molar incisor hypomineralisations and the presence of dental caries? Int J Paediatr Dent. 2013;23:116–24. doi: 10.1111/j.1365-263X.2012.01233.x. [DOI] [PubMed] [Google Scholar]
- 30.Ghanim A, Mariño R, Morgan M, Bailey D, Manton D. An in vivo investigation of salivary properties, enamel hypomineralisation, and carious lesion severity in a group of Iraqi schoolchildren. Int J Paediatr Dent. 2013;23:2–12. doi: 10.1111/j.1365-263X.2011.01215.x. [DOI] [PubMed] [Google Scholar]
- 31.Negre-Barber A, Montiel-Company JM, Catalá-Pizarro M, Almerich-Silla JM. Degree of severity of molar incisor hypomineralization and its relation to dental caries. Sci Rep. 2018;8:1248. doi: 10.1038/s41598-018-19821-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vann WF, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. 2010;89:1395–400. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cribb VL, Jones LR, Rogers IS, Ness AR, Emmett PM. Is maternal education level associated with diet in 10-year-old children? Public Health Nutr. 2011;14:2037–48. doi: 10.1017/S136898001100036X. [DOI] [PubMed] [Google Scholar]
- 34.Silvestrin S, Silva CH, Hirakata VN, Goldani AA, Silveira PP, Goldani MZ. Maternal education level and low birth weight: A meta-analysis. J Pediatr (Rio J) 2013;89:339–45. doi: 10.1016/j.jped.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Prickett KC, Augustine JM. Maternal education and investments in children’s health. J Marriage Fam. 2016;78:7–25. doi: 10.1111/jomf.12253. [DOI] [PMC free article] [PubMed] [Google Scholar]


