Abstract.
Thermal block of unmyelinated axons may serve as a modality for control, suggesting a means for providing therapies for pain. Computational modeling predicted that potassium channels are necessary for mediating thermal block of propagating compound action potentials (CAPs) with infrared (IR) light. Our study tests that hypothesis. Results suggest that potassium channel blockers disrupt the ability of IR to block propagating CAPs in Aplysia californica nerves, whereas sodium channel blockers appear to have no significant effect. These observations validate the modeling results and suggest potential applications of thermal block to many other unmyelinated axons.
Keywords: infrared inhibition, potassium channels, sodium channels, tetraethylammonium chloride, tetrodotoxin
1. Introduction
Precise control of neural activity (neuromodulation) is a challenge that has major scientific and clinical applications for treating and managing symptoms and conditions that are neuropathic in origin.1 Electrical methods of neuromodulation have been used for some time but suffer from disadvantages such as lack of selectivity, surgical complications, lead migration, lead breakage, MRI incompatibility, and tolerance buildup.2,3 There is a need for an alternate modality of neuromodulation that can mitigate, if not completely eliminate, these disadvantages.4
The use of infrared (IR) irradiation on nerves could be one such method. It has been shown that IR light can be used for excitation5–9 and inhibition of nerves.10–14 The technique of IR inhibition of nerves is spatially precise10 and can be targeted to selectively inhibit axons of smaller diameters.12 The ability to target axons of small diameters helps motivate IR inhibition as a modality that can target finer sensory fibers carrying vital feedback information (e.g., pain, pressure, and temperature sensitivity). Understanding the mechanism of action of IR on nerves is critical to exploit the potential of IR inhibition as a clinical modality and optimize its parameter space. It has been shown that heating caused by IR absorption of nerves is responsible for inhibition.15–18 From simulations using Hodgkin–Huxley-based computational models,17,18 we hypothesize that the mechanism underlying IR inhibition of action potentials is a thermally driven accelerated activation of voltage-gated potassium ion channels. This paper tests this hypothesis by studying IR nerve inhibition in unmyelinated Aplysia nerves in the presence of voltage-gated ion channel blockers.
2. Methods
2.1. Animal Preparation
After anesthetizing Aplysia californica (250 to 350 g, Marinus Scientific, Long Beach, California) with magnesium chloride (333 mM, 50% body weight), the right pleural abdominal (PA) nerves were dissected out and suctioned into extracellular recording electrodes to record their electrophysiological response. The nerves were maintained in room temperature () Aplysia saline (460 mM NaCl, 10 mM KCl, 22 mM , 33 mM , 10 mM , 10 mM glucose, 10 mM HEPES, pH 7.6), which was modified depending on the type of experiment (see below). Measurements using a calibrated microscope done in the laboratory show that the diameter of the Aplysia PA nerve is in diameter (, for animals ranging from 250 to 300 g in weight).
2.2. Experimental Setup
Nerve-recording electrodes were made by hand-pulling polyethylene tubing (1.27-mm outer diameter, 0.86-mm inner diameter) over a flame and cutting them to the desired diameter. Recording electrodes were suction-filled with Aplysia saline prior to suctioning the nerve. Nerve signals were amplified () and bandpass filtered (300 to 500 Hz) using an AC-coupled differential amplifier (A-M Systems, Sequim, Washington), digitized using an Axon Digidata 1440A digitizer (Molecular Devices, San Jose, California), and recorded using Clampex computer software (Molecular Devices, San Jose, California). Monophasic stimulation current was supplied by a WPI A365 stimulus isolator (World Precision Instruments, Sarasota, Florida) for all experiments (stimulation parameters: current, , 1 Hz). The IR block was produced by a tunable diode laser (Capella Neurostimulator; Lockheed-Martin-Aculight, Bothell, Washington) with a wavelength of coupled to a -diameter multimode optical fiber (Ocean Optics, Dunedin, Florida). The optical fiber was secured in place using micromanipulators. The laser was triggered at 200 Hz with pulses for all experiments. Radiant exposures per pulse at the fiber output were calculated after measuring the power output using a power meter (Molectron EPM 2000, Coherent, Santa Clara, California). The optical fiber was maintained in contact with the nerve surface for all irradiation experiments [Fig. 1(a)]. The energy range used in the study was .
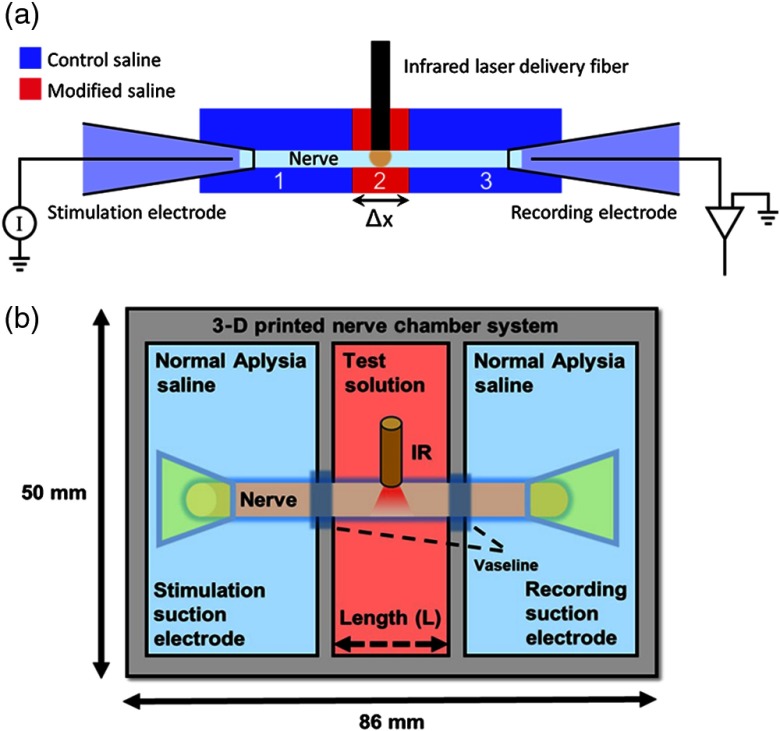
Fig. 1.
Experimental setup. (a) Schematic of experimental setup, which consists of an Aplysia PA connective nerve in a 3-D chamber that consists of three sections (1, 2, and 3). The sections at the ends (shown in blue) contain normal saline. The section in the middle (2, colored red) contains saline solution with or without ion channel blockers. The nerve is irradiated with IR laser radiation delivered via a fiber optic in the middle section. Suction electrodes at the ends of the nerve allow for stimulation and recording of CAPs ( to 3 mm). (b) A schematic showing the layout of the nerve chamber with dimensions.
A specially designed chamber was fabricated for our experiments. The chamber [Fig. 1(b)] consisted of three sections and was three-dimensional (3-D) printed on a Form 2 printer using black Formlabs Standard Resin (Formlabs Inc., Somerville, Massachusetts, layer height). The sections within the chamber were separated using 3-D printed partitions (made of Hewlett-Packard 3-D high reusability polycyclic aromatic 12 to provide finer detail). Resin was used for printing since it provided a good balance between quality and cost. For the experiments described in this paper, the width of the middle section (, Fig. 1) was maintained between 2.5 and 3 mm. This width is small enough to allow passive currents to propagate past the middle chamber and reinitiate action potentials, even in the presence of voltage-gated sodium ion channel blockers. The width was also large enough to allow reliable placement of the optical fiber in contact with the nerve. Leaking was minimized by brushing the edges of the partitions with biocompatible Vaseline (Unilever, London/Rotterdam) petroleum jelly to provide a good seal.
2.3. Channel Blockers and Inhibitors
To test hypotheses derived from computational modeling studies,18 we used a blocker of voltage-gated potassium ion channels [tetraethylammonium (TEA) chloride] and a blocker of voltage-gated sodium ion channels [tetrodotoxin (TTX)]. The formulation for TEA saline was 410 mM NaCl, 50 mM TEA, 10 mM KCl, 22 mM , 33 mM , 10 mM , 10 mM glucose, 10 mM HEPES, pH 7.6.19,20 Prior studies19,20 have shown that TEA blocks both voltage-dependent and -mediated potassium channels and disrupt potassium currents in Aplysia neurons. A solution of of TTX saline solution (TTX, Enzo Life Sciences Farmingdale, New York) was prepared by adding of 1 mM TTX normal Aplysia saline solution to make a final volume of 10 ml. The concentration of TTX in saline was chosen to be consistent with previously published experimental studies in Aplysia.21–23 In these studies,21–23 it has been observed that use of TTX blocks inward currents and decreases spiking activity in Aplysia pacemaking and buccal neurons. The effect of all ion channel blockers was reversible, which was confirmed by performing recordings after washing out the ion channel blocker solutions. The effect of TEA was reversed after 2 to 4 washouts over . The effect of TTX was reversed after 2 to 3 washouts over . The pH of all the saline solutions was adjusted to 7.6, which is the same as that of normal Aplysia saline. All solutions were brought to room temperature () prior to infusion into the chamber.
2.4. Experimental Protocol
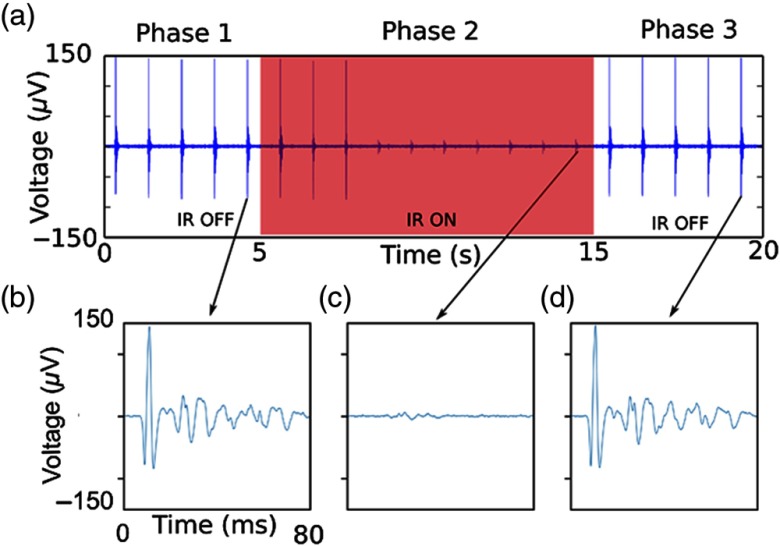
The nerve recording protocol consisted of multiple recordings of 20-s intervals. The nerve was electrically stimulated at a frequency of 1 Hz. Each recording consisted of three phases: (1) the time when the laser was off ( to 5 s), (2) the time when the laser was on ( to 15 s), and (3) the time when the laser was again off [ to 20 s; Fig. 2(a)]. Phase 3 of the recording allowed the nerve to recover from the thermal block induced by the IR laser irradiation during the second phase of the recording. In each study, the power of the laser was adjusted to obtain a complete block of the compound action potential (CAP) within the first 5 s after the laser turned on. Once the value of radiant exposure was determined, it was kept constant for the entire duration of a trial. Each trial consisted of three experimental conditions. The trials were conducted in a series of recordings in A-B-A-C-A format. Recording A refers to the observation of nerve activity in the control saline solution (with IR irradiation), before any ion channel blocker is introduced. Recording B refers to the observation of nerve activity in the presence of TEA (with IR irradiation), and recording C refers to the observation of nerve activity in the presence of TTX (with IR irradiation). Experiments were repeated in six different animals ().
Fig. 2.
Typical IR block. (a) Recording showing IR laser block obtained when the nerve is in normal Aplysia saline. The laser is switched on from to 15 s and switched off for the last 5 s in each recording. (b)–(d) Signals from each phase of the recording are shown in high temporal resolution [(b) preirradiation, (c) during irradiation, and (d) postirradiation]. In each of the high-resolution signals shown, the electrical recording artifacts are removed. (Laser parameters , , , , and .)
2.4.1. Data acquisition and analysis
CAPs were acquired at 50 kHz. Clampex (Molecular Devices, San Jose, California) was used to record acquired data in the computer. After acquisition, data analysis was performed using a combination of AxoGraph X (Axograph Scientific, Berkeley, California), Matlab (Mathworks, Natick, Massachusetts), Microsoft Excel (Microsoft, Redmond, Washington), and Mathematica (Wolfram Inc., Champaign, Illinois). Each recording was divided into three phases [laser off 0 to 5 s, laser on 5 to 15 s, and laser off 15 to 20 s, Fig. 2(a)]. The rectified area under the curve (rAUC) was evaluated for signals in each phase of the recording. The averages of the areas under “laser off” phase (phases 1 and 3) were plotted; since they were not significantly different (based on a paired -test), the ratio of the rAUC in phase 2 relative to phase 1 was computed. For the “laser on” phase (phase 2), rAUC for the signals observed between to 15 s of the recordings was measured. Prior studies had indicated that the effect of IR takes several seconds to occur,12 so focusing on the last 5 s of phase 2 ensured that the system had reached a stable state. The areas were normalized to the average area calculated for when the laser was off during the first phase of the recording. Tests for normality were performed using the Shapiro–Wilk test. The data also passed tests for heteroscedasticity so that analysis of variance (ANOVA) could be applied. Posthoc Tukey honest significant difference (HSD) tests were used to determine which changes were statistically significant at the level.
3. Results
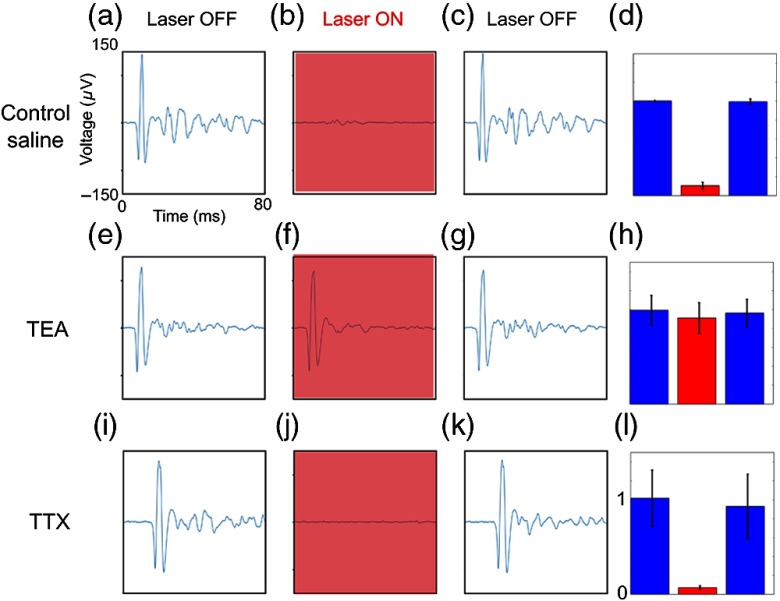
Control experiments using normal saline solutions (without any channel blockers) show a block when IR is used on the nerve [Figs. 2(a)–2(d); Figs. 3(a)–3(d)]. In the presence of TEA, the effect of IR in creating a propagation block is greatly reduced [Figs. 3(e)–3(h)]. Although TEA prevented laser-induced inhibition of the largest CAP units, it still appeared to inhibit smaller, slower units, which have a lower inhibition threshold, as predicted by modeling results.18 In the presence of TTX, IR block is again observed [Figs. 3(i)–3(l)].
Fig. 3.
Blocking potassium ion channels eliminates IR thermal inhibition. High temporal resolution views of representative signals from a nerve undergoing block in the presence of ion channel blockers. Signals prior to, during, and after laser irradiation in (a)–(c) control saline, (e)–(g) TEA, and (i)–(l) TTX are shown. IR-induced thermal inhibition is observed in (b) control (normal) saline and (j) TTX when the IR laser is switched on. (f) Thermal inhibition is reduced in the presence of a potassium channel blocker (TEA chloride). Normalized rAUCs summarizing results from observations in (d) control saline, (h) the presence of TEA, and (l) the presence of TTX. Lack of change in rAUC in TEA is highly significant (see text).
Overall ANOVA for independent experiments shows that the overall changes due to the presence of the blockers is highly significant (). Posthoc Tukey HSD tests showed that normalized changes in areas of CAPs in saline and TTX (when IR was on, phase 2) relative to control (IR laser off, phase 1) were not statistically significant, whereas normalized changes in the CAPs in TEA (laser on, phase 2) relative to control (laser off, phase 1) showed no reductions during IR irradiation and are highly significantly different from the saline and TTX results ().
4. Discussion
The results presented in this paper support the hypothesis that the primary mechanism by which thermal block occurs is due to voltage-dependent potassium ion channels. As shown in previous modeling studies,17,18 in response to heating, voltage-dependent potassium channels in unmyelinated axons respond more rapidly than they do in unheated axons, generating a hyperpolarizing current in response to depolarizing currents. Results also suggest that sodium channels do not appear to play a significant role in establishing a thermal block. Increase in activity of potassium channels in mammalian models caused by accelerated kinetics and increased conductance at elevated temperatures have been reported in the literature.24–26 Potassium channel blockers have been reported to affect conduction block at elevated temperatures,27–29 but the underlying mechanism has remained elusive. While all studies mentioned above examined mammalian systems, to the best of our knowledge, the study presented here is the first to highlight the key role of potassium channels during thermal block induced by IR laser radiation in an unmyelinated axon system. These results may lead to targeted therapies for unmyelinated axons, which carry sensory information such as pain and temperature in a wide range of species, including humans.
Acknowledgments
This research was supported by the U.S. Air Force Office of Sponsored Research (AFOSR) Grant No. FA 9550-17-1-0374 and the U.S. National Institutes of Health (NIH) Grant Nos. SPARC OT2 OD025307 and R01 HL126747.
Disclosures
No conflicts of interest, financial or otherwise, are declared by the authors.
Contributor Information
Mohit Ganguly, Email: mohit.ganguly@vanderbilt.edu.
Jeremy B. Ford, Email: jeremy.ford@vanderbilt.edu.
Junqi Zhuo, Email: jxz624@case.edu.
Matthew T. McPheeters, Email: mtm44@case.edu.
Michael W. Jenkins, Email: mwj5@case.edu.
Hillel J. Chiel, Email: hjc@case.edu.
References
- 1.Mekhail N. A., et al. , “Clinical applications of neurostimulation: forty years later,” Pain Pract. 10, 103–112 (2010). 10.1111/papr.2010.10.issue-2 [DOI] [PubMed] [Google Scholar]
- 2.Shim J. H., “Limitations of spinal cord stimulation for pain management,” Korean J. Anesthesiol. 68, 321–322 (2015). 10.4097/kjae.2015.68.4.321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bendersky D., et al. , “Is spinal cord stimulation safe? A review of its complications,” World Neurosurg. 82, 1359–1368 (2014). 10.1016/j.wneu.2013.06.012 [DOI] [PubMed] [Google Scholar]
- 4.Chernov M. M., et al. , “Material considerations for optical interfacing to the nervous system,” MRS Bull. 37, 599–605 (2012). 10.1557/mrs.2012.121 [DOI] [Google Scholar]
- 5.Wells J., et al. , “Optical stimulation of neural tissue in vivo,” Opt. Lett. 30, 504–506 (2005). 10.1364/OL.30.000504 [DOI] [PubMed] [Google Scholar]
- 6.Wells J., et al. , “Biophysical mechanisms of transient optical stimulation of peripheral nerve,” Biophys. J. 93, 2567–2580 (2007). 10.1529/biophysj.107.104786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duke A. R., et al. , “Combined optical and electrical stimulation of neural tissue in vivo,” J. Biomed. Opt. 14, 060501 (2009). 10.1117/1.3257230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson A. C., et al. , “Optical stimulation of neurons,” Curr. Mol. Imaging 3, 162–177 (2014). 10.2174/2211555203666141117220611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ford S. M., et al. , “A review of optical pacing with infrared light,” J. Neural Eng. 15, 011001 (2018). 10.1088/1741-2552/aa795f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duke A. R., et al. , “Transient and selective suppression of neural activity with infrared light,” Sci. Rep. 3, 2600 (2013). 10.1038/srep02600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lothet E. H., et al. , “Alternating current and infrared produce an onset-free reversible nerve block,” Neurophotonics 1, 011010 (2014). 10.1117/1.NPh.1.1.011010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lothet E. H., et al. , “Selective inhibition of small-diameter axons using infrared light,” Sci. Rep. 7, 3275 (2017). 10.1038/s41598-017-03374-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y. T., et al. , “Infrared inhibition of embryonic hearts,” J. Biomed. Opt. 21, 060505 (2016). 10.1117/1.JBO.21.6.060505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walsh A. J., et al. , “Action potential block in neurons by infrared light,” Neurophotonics 3, 040501 (2016). 10.1117/1.NPh.3.4.040501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huxley A. F., “Ion movements during nerve activity,” Ann. N. Y. Acad. Sci. 81, 221–246 (1959). 10.1111/j.1749-6632.1959.tb49311.x [DOI] [PubMed] [Google Scholar]
- 16.Mou Z., et al. , “A simulation study of the combined thermoelectric extracellular stimulation of the sciatic nerve of the Xenopus laevis: the localized transient heat block,” IEEE Trans. Biomed. Eng. 59, 1758–1769 (2012). 10.1109/TBME.2012.2194146 [DOI] [PubMed] [Google Scholar]
- 17.Ganguly M., et al. , “Modeling the effects of elevated temperatures on action potential propagation in unmyelinated axons,” Proc. SPIE 9690, 96901O (2016). 10.1117/12.2211048 [DOI] [Google Scholar]
- 18.Ganguly M., et al. , “Thermal block of action potentials is primarily due to voltage-dependent potassium currents: a modeling study,” J. Neural Eng. 16(3), 036020 (2019). 10.1088/1741-2552/ab131b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hermann A., et al. , “External and internal effects of tetraethylammonium on voltage-dependent and Ca-dependent currents components in molluscan pacemaker neurons,” Neurosci. Lett. 12, 87–92 (1979). 10.1016/0304-3940(79)91485-X [DOI] [PubMed] [Google Scholar]
- 20.Hermann A., et al. , “Effects of tetraethylammonium on potassium currents in a molluscan neurons,” J. Gen. Physiol. 78, 87–110 (1981). 10.1085/jgp.78.1.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller N., et al. , “Neurons controlling Aplysia feeding inhibit themselves by continuous NO production,” PLoS One 6, e17779 (2011). 10.1371/journal.pone.0017779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geduldig D., et al. , “Voltage clamp of the Aplysia giant neurone: early sodium and calcium currents,” J. Physiol. 211, 217–244 (1970). 10.1113/jphysiol.1970.sp009276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Futamachi K., et al. , “Action of tetrodotoxin on pacemaker conductances in Aplysia neurons,” Brain Res. 233, 424–430 (1982). 10.1016/0006-8993(82)91218-5 [DOI] [PubMed] [Google Scholar]
- 24.Fleischmann B. K., et al. , “Control of resting membrane potential by delayed rectifier potassium currents in ferret airway smooth muscle cells,” J. Physiol. 469, 625–638 (1993). 10.1113/jphysiol.1993.sp019834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pahapill P. A., et al. , “Modulation of potassium channels in human T lymphocytes: effects of temperature,” J. Physiol. 422, 103–126 (1990). 10.1113/jphysiol.1990.sp017975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beam K. G., et al. , “A quantitative study of potassium channel kinetics in rat skeletal muscle from 1 to 37°C,” J. Gen. Physiol. 81, 485–512 (1983). 10.1085/jgp.81.4.485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eliasson S. G., et al. , “Potassium ion channel blockade restores conduction in heat-injured nerve and spinal nerve roots,” Exp. Neurol. 93, 128–137 (1986). 10.1016/0014-4886(86)90152-4 [DOI] [PubMed] [Google Scholar]
- 28.Bostock H., et al. , “After-effects of near-threshold stimulation in single human motor axons,” J. Physiol. 564, 931–940 (2005). 10.1113/jphysiol.2005.083394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu B. S., et al. , “Heat shock-induced thermoprotection of action potentials in the locust flight system,” J. Neurobiol. 49, 188–199 (2001). 10.1002/(ISSN)1097-4695 [DOI] [PubMed] [Google Scholar]