Abstract
The aim of the present study was to evaluate the protective effect and mechanism of Astragaloside IV (ASIV) on myocardial injury induced by type 2 diabetes, with a focus on energy metabolism. Blood glucose, the hemodynamic index, left ventricular weight/heart weight (LVW/HW), the left ventricular systolic pressure (LVSP), the left ventricular end diastolic pressure (LVEDP) and cell survival rate were measured in streptozotocin-induced diabetes model rats. Western blot analysis, PCR, hematoxylin-eosin and TUNEL staining, flow cytometry and ELISA were used to detect: i) Cardiomyocyte damage indicators such as atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), cytochrome c (Cyt C), caspase-3, cleaved caspase-3 and the apoptotic rate; ii) energy metabolism indicators such as ATP/AMP and ADP/AMP; and iii) energy metabolism associated pathway proteins such as peroxisome proliferator-activated receptor γ coactivator 1-α (PGC-1α) and nuclear respiratory factor 1 (NRF1). The present demonstrated increased blood glucose, LVW/HW, LVSP, LVEDP and the cardiomyocyte damage indicators (ANP, BNP, Cyt C and caspase-3), in the diabetic and high glucose-treated groups, which were decreased by ASIV. The expression of NRF-1 and PGC-1α significantly changed in the model group and was markedly improved following ASIV treatment. Furthermore, the abnormal energy metabolism in the model group was reversed by ASIV. According to the results, ASIV can regulate energy metabolism by regulating the release of PGC-1α and NRF1 to rescue the abnormal energy metabolism caused by diabetes mellitus, thus decreasing the myocardial damage caused by diabetic cardiomyopathy.
Keywords: diabetic cardiomyopathy, astragaloside IV, apoptosis, hypertrophy, mitochondrial energy metabolism, peroxisome proliferator-activated receptor γ coactivator 1-α, nuclear respiratory factor 1
Introduction
Diabetes is a metabolic disease, with the number of people with diabetes estimated to reach 700 million worldwide in 2040 (1). Cardiovascular complications are the main cause of mortality in diabetic patients, and ~80% of diabetic patients die from cardiovascular diseases (2). Diabetic cardiomyopathy (DCM) has the highest mortality rate associated with diabetic complications, and the methods for treatment are poor (3). In the early stage of the disease, patients exhibit symptoms such as ventricular diastolic dysfunction and myocardial remodeling; as the disease worsens, microvascular disease and the necrosis of myocardial tissue occurs, eventually leading to heart failure (4).
Although there are many unknown mechanisms of in diabetic cardiomyopathy, previous studies have shown that metabolic disorders have a significant role in the pathogenesis of diabetic cardiomyopathy. As the body does not normally use glucose to supply energy, the oxidation of fatty acids is exacerbated, causing toxicity from sugar and fat. This damages the mitochondria in myocardial cells (5), inducing mitochondrial dysfunction and deficits in ATP production, and the damage can eventually lead to the apoptosis of myocardial cells, hypertrophy and fibrosis, and, ultimately, cardiac dysfunction (6). Peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α), which is one of the members of the PGC-1α family, plays a vital role in the process of biosynthesis in mitochondria (7–9); it can stimulate nuclear transcription factor nuclear respiratory factor (NRF) and other downstream factors to promote the proliferation of mitochondria and the expression of proteins in mitochondria, regulate cellular energy metabolism and provides ATP to heart tissue (10). The increased expression of PGC-1α can improve myocardial metabolic disorders (11).
Following stimulation by adverse environmental factors, the apoptosis of cardiac cells is increased, and changes in cell function and structure lead to cardiac hypertrophy. Under conditions of high glucose, a series of metabolites generated by cardiac cells can stimulate the binding of extracellular apoptosis-associated ligands to specific receptors on the cell membrane, activating cysteine-containing aspartate-specific proteases (caspases), triggering a series of apoptosis pathways and accelerating the process of apoptosis (12). The abnormal structure or function of mitochondria can lead to abnormal energy metabolism, which not only damages myocardial function but also causes inflammation and oxidative stress to further aggravate the damage. Therefore, restoring mitochondrial function is key to the treatment of diabetic myocardium (13).
Astragaloside IV (ASIV) is a saponin compound isolated from Astragalus that has the anti-apoptotic, anti-oxidative and glucose-controlling effects; therefore it has a certain therapeutic effect on diabetic cardiomyopathy (14). However, the pharmacological action of ASIV on diabetic cardiomyopathy is still unclear and requires further investigation. Previous studies have found that ASIV can improve energy metabolism dysfunction induced by isoproterenol in rats by increasing the expression of PGC-1α by isoproterene in rats (15–20).
The aim of the present study was to investigate the pharmacological mechanism of ASIV in diabetic cardiomyopathy by focusing on the aspects of energy metabolism and PGC-1α.
Materials and methods
Reagents
ASIV was purchased from Nanjing Jingzhu Bio-Technology Co., Ltd. Streptozotocin (STZ) and carboxymethyl cellulose sodium (CMC-Na) were purchased from Sigma-Aldrich (Merck KGaA). A TUNEL kit (In Situ Cell Death Detection kit, AP) was purchased from Roche Molecular Diagnostics. ATP (kt39623), ADP (kt210319) and AMP (kt28319) ELISA kits were purchased from MSKBIO Co. Ltd. A BCA Protein Assay kit was purchased from Beyotime Institute of Biotechnology. TRIzol reagent and a reverse transcription-PCR (RT-PCR) kit were purchased from Dingguo Biological Co. Ltd. PGC-1α, NRF1, atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) were purchased from ABclonal. Cleaved caspase-3, caspase-3 and cytochrome c (Cyt C) were purchased from Biological Technology Co. Ltd.
Animals and experimental design
Healthy male Sprague-Dawley rats (6–8 weeks old, 180–200 g, n=50) were purchased from the Experimental Animal Center of Jinzhou Medical University (Jinzhou, China). All experiments and procedures were approved by the Medical Ethics Committee of Jinzhou Medical University (approval no. LNMU-2016-121). The rats were treated in accordance with the Guide for the Care and Use of Laboratory Animals (8th edition, National Academies Press) (21). The rats were adapted to their new environment (at a temperature of 20–23°C, humidity from 30–48%, and a 12-h light/dark cycle) for 1 week before the experiment. There were 5 groups in the in vivo experiments, and each group consisted of 10 rats. Healthy male SD rats (n=40) were injected with STZ through the tail vein at a dose of 35 mg/kg. The fasting blood glucose level was detected 1 week later. If an animal presented with a fasting blood glucose level >16.7 mM and symptoms of polydipsia, polyuria and polyphagia, it was considered a diabetic model rat. Diabetes was successfully established in 40 rats and 30 of them were randomly selected and randomly divided into three groups of 10 each. The ASIV-high (H), ASIV-mid (M) and ASIV-low (L) groups were established by the intraperitoneal injection of three different doses of ASIV (40, 20 and 10 mg/kg, respectively) once a day. ASIV was dissolved in 1% CMC. The remaining 10 rats were used for the diabetic model only group, and 10 SD rats were used as the control group. The same volume of 1% CMC was administered daily. Blood glucose was measured and recorded on day 1, and weeks 2, 4, 8, 12 and 16 following administration. After 16 weeks of ASIV treatment, rats were anesthetized [urethane, 1.5 g/kg, intraperitoneal injection (i.p.)] (22), and hemodynamic parameters were measured. Rats were euthanized by cervical dislocation under anesthesia (diazepam, 10 mg/kg and ketamine, 50 mg/kg) and myocardial tissue was collected. Some of the tissues were fixed with 4% paraformaldehyde solution at room temperature for 24 h, and the remaining tissue was stored at −86°C.
Cell culture
H9C2 cells were purchased from Wuhan Boster Biotech Company, Ltd. and the cells were propagated in DMEM (Gibco; Thermo Fisher Scientific, Inc.) supplemented with 10% FBS (HyClone; GE Healthcare Life Sciences) and 1% penicillin-streptomycin (Invitrogen; Thermo Fisher Scientific, Inc.). The H9C2 cells were divided into six groups: Con (control), mannitol (control + mannitol 7.5 mM), high glucose (HG; glucose 33.3 mmol·l−1), HG + ASIV-L (20 µmol·l−1), HG + ASIV-M (40 µmol·l−1) and HG + ASIV-H (80 µmol·l−1).
Detection of cardiac function indicators
After being anesthetized with 20% urethane (1.5 g/kg, i.p.), all rats were weighed before the beginning of the experiment. A physiological recorder was used to monitor the left ventricular systolic pressure (LVSP), the left ventricular end diastolic pressure (LVEDP) and the maximum left ventricular ascending/descending rate (± dp/dtmax), after the right common carotid artery was isolated and intubated into the left ventricle. The hearts of the rats were harvested and rinsed with precooled normal saline, and then dissected and weighed. The ratio of the left ventricle weight to the heart weight (LVW/HW) was separately calculated. Finally, the heart tissues retained for slicing were placed in 4% polyformaldehyde and the remaining heart tissues were stored at −86°C.
Hematoxylin and eosin (H&E) and TUNEL staining
After soaking in 4% formaldehyde at room temperature for 24 h, the heart tissues were embedded in paraffin and sectioned into 5-µm sections. The sections were stained using H&E (hematoxylin 2–3 min and eosin 1 min, both at room temperature) and TUNEL kits [50 µl TdT and dUTP (1:9) in a dark moist chamber at 37°C for 1 h], respectively. An inverted microscope (DMI3000B, Leica Microsystems GmbH) was used for observation (magnification, ×400), and the matching software LAS v4.3 was used to capture and analyze images. The apoptotic index (%) was calculated as the number of positive apoptotic cardiomyocytes/the total number of cardiomyocytes ×100.
Detection of the cell survival by MTT
H9C2 cells (Cell concentration ~5×104/ml) were seeded onto 96-well plates (8 wells per group) and cultured at 37°C and 5% CO2 for 24 h. After 48 h, 20 µl MTT (5 mg/ml) was added, and the cells were incubated for 4 h. Subsequently, 150 µl DMSO was added, and the plates were shaken for 10 min to dissolve the formazan crystals. The absorbance value (OD value) was measured at a wavelength of 490 nm using an enzyme-labeling instrument. Cell viability was calculated.
Apoptosis assays
Apoptosis was detected using an Annexin V-FITC apoptosis detection kit (Annexin V-FITC/PI Apoptosis Detection kit, Dalian Meilun Biology Technology Co., Ltd.) according to the manufacturer's instructions. The cells in each group (5×105-6 cells/ml) were extracted, 100 µl 1X binding buffer was added, and the cells were resuspended gently. After adding 5 µl Annexin V-FITC and 5 µl propidium iodide, the cells were mixed gently and incubated at room temperature without light for 10 min. Following the addition of 400 µl 1X binding buffer and suspending the cells gently, Annexin V-FITC staining was detected using a BD Accuri C6 Plus flow cytometer (BD Biosciences) and analyzed by FlowJo v10 (FlowJo LLC).
Detection of ATP/ADP and ATP/AMP
According to the ELISA kit instructions, the OD value was detected and recorded. First, standard curves were generated, and the related reagents were added to the myocardial tissues and H9C2 cells. Then, ATP, ADP and AMP were calculated by measuring the OD values and the standard curves of each group. Finally, the ATP/ADP and ATP/AMP ratio were obtained.
Preparation of protein extracts and western blot analysis
Nucleoproteins and mitochondrial proteins were extracted from the myocardial tissue and H9C2 cells with corresponding kits (Tissue or Cell Total Protein Extraction kit, Sangon Biotech Co. Ltd.; Nuclear Protein Extraction kit, Beijing Solarbio Science & Technology Co., Ltd.; Tissue Mitochondria Isolation kit, Novland Biopharma Co. Ltd.; www.novland.com.cn) The procedure was performed according to the manufacturer's instructions. The total protein, the cytoplasmic protein and the cytoplasmic protein after the removal of mitochondria were extracted. After the protein concentration was determined using the BCA method, the samples were prepared according to the required concentration and dosage (40 µg of total protein to each lane). SDS-PAGE (10–12% polyacrylamide gels) was used to separate protein samples. The isolated proteins were transferred to PVDF membranes (EMD Millipore) and blocked with 1% BSA at room temperature for 2 h. The membranes were incubated with primary antibodies against ANP (NPPA polyclonal antibody, ABclonal Biotech Co., Ltd. A14755, 1:1,000), BNP (BNP polyclonal antibody, ABclonal Biotech Co., Ltd. A2179, 1:1,000), Cyt C (anti-cytochrome c antibody, Boster Biological Technology, A03529, 1:1,000), caspase-3 (anti-caspase-3 antibody, Boster Biological Technology PB9188, 1:1,000), cleaved caspase-3 (anti-Caspase-3 p12 antibody, Boster Biological Technology BM4620, 1:1,000), NRF1 (NRF1 polyclonal antibody, ABclonal Biotech Co., Ltd. A5547, 1:1,000), PGC-1α (PGC1 α polyclonal antibody, ABclonal Biotech Co., Ltd. A12348, 1:1,000) and β-actin (β-actin Antibody, ProteinTech Group, Inc 66009-1-Ig, 1:20,000) at room temperature for 1.5 h. Then the PVDF membrane was placed in the corresponding antibody (HRP-conjugated Affinipure Goat Anti-Rabbit IgG(H+L), ProteinTech Group, Inc. SA00001-2, 1:20,000; HRP goat anti-mouse IgG (H+L), ABclonal Biotech Co., Ltd. AS003, 1:10,000) and incubated at room temperature for 2 h. All antibodies were diluted with 0.1% BSA. The results were detected with enhanced chemiluminescence reagents (Wanleibio Co., Ltd.) and analyzed using Results Quantity One software v6.0.1 (Bio-Rad Laboratories, Inc.).
Statistical analysis
All data are expressed as the mean ± SD and were analyzed using SPSS 19.0 software (IBM Corp.). Statistical analysis was performed using one-way ANOVA followed by Bonferroni's test. P<0.05 was considered to indicate a statistically significant difference.
Results
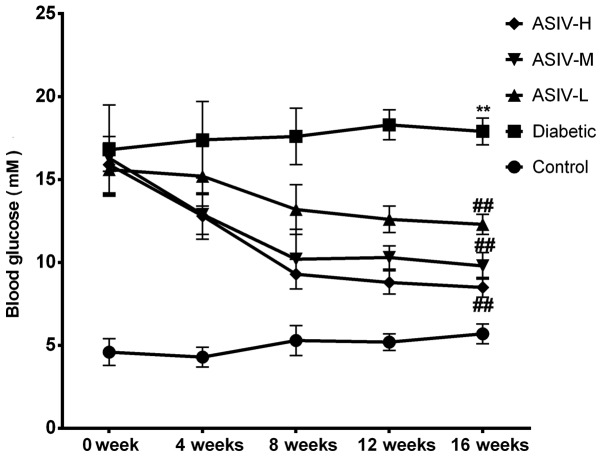
ASIV has a regulatory effect on blood glucose in diabetic rats
A broken line graph (Fig. 1) of the blood glucose levels was made to observe the effect of ASIV on blood glucose. No significant changes in blood glucose level in the control group and the diabetic group over the 16-week experimental period, indicating that the solvent did not regulate blood glucose. The blood glucose of the three groups administered ASIV decreased markedly as the duration of ASIV administration increased, and the degree of the decrease was associated with the administered dose, indicating that ASIV has an effect on hypoglycemia.
Figure 1.
ASIV inhibits the elevation of blood glucose in STZ-induced diabetic rats. Data are expressed as the means ± SD, n=10, **P<0.01 vs. control group. ##P<0.01 vs. diabetic group. ASIV, astragaloside IV.
ASIV improves the physiological indexes in STZ-induced diabetic rats and decreases the influence on tissue structure
Compared with the control group, the LVSP and +dp/dtmax in the diabetes model group were significantly decreased, indicating decreased myocardial systolic ability, whereas LVEDP was increased and -dp/dtmax decreased, reflecting decreased myocardial diastolic ability. Combined with the above signs of diabetic cardiomyopathy, myocardial diastolic function was abnormal and heart failure occurred. According to the results, the LVEDP gradually decreased as the dose increased, LVSP, +dp/dtmax and -dp/dtmax gradually increased, and myocardial function was significantly improved by ASIV intervention (Fig. 2A and B). As shown in Fig. 2C, the LVW/HW was significantly increased in the diabetic group compared with the control animals, indicating that diabetes caused the left heart to increase in weight. Following the administration of ASIV, the LVW/HW decreased compared with the diabetic model group, and the degree of the decrease dependent on the ASIV concentration, demonstrating the effect of ASIV on the degree of myocardial hypertrophy.
Figure 2.
ASIV improves the physiological indexes of STZ-induced diabetic rats and decreases the effects of diabetes on tissue structures. (A) LVEDP and LVSP, (B) ± dp/dtmax and (C) LVW/HW of rats in the different experimental groups. n=10. (D) Hematoxylin and eosin staining in cardiac tissue sections of each group. The black arrow indicates myocardial fibers. (E) Cell survival of H9C2 cells determined by MTT assay. n=8 Data are expressed as the mean ± SD. **P<0.01 vs. the control group. #P<0.05 and ##P<0.01 vs. diabetic group. LVEDP, left ventricular systolic pressure; LVSP, left ventricular end diastolic pressure; ASIV, astragaloside IV; L, low; M, mid; H, high; ± dp/dtmax, maximum left ventricular ascending/descending rate; LVW/HW, ratio of left ventricular weight to heart weight.
H&E staining showed that the myocardial fibers in the heart tissues of diabetic rats were disordered and transversely broken. This damage was improved in the ASIV-treated groups. The therapeutic effect depended on the dose (Fig. 2D). The results of the cell viability assay (Fig. 2E) showed that cells survival in the control and mannitol groups was >95%. The survival rate in the HG group was significantly decreased compared to the control group. Furthermore, the survival rate increased following ASIV intervention. This demonstrated that ASIV can protect cells and alleviate the damage under high-glucose conditions.
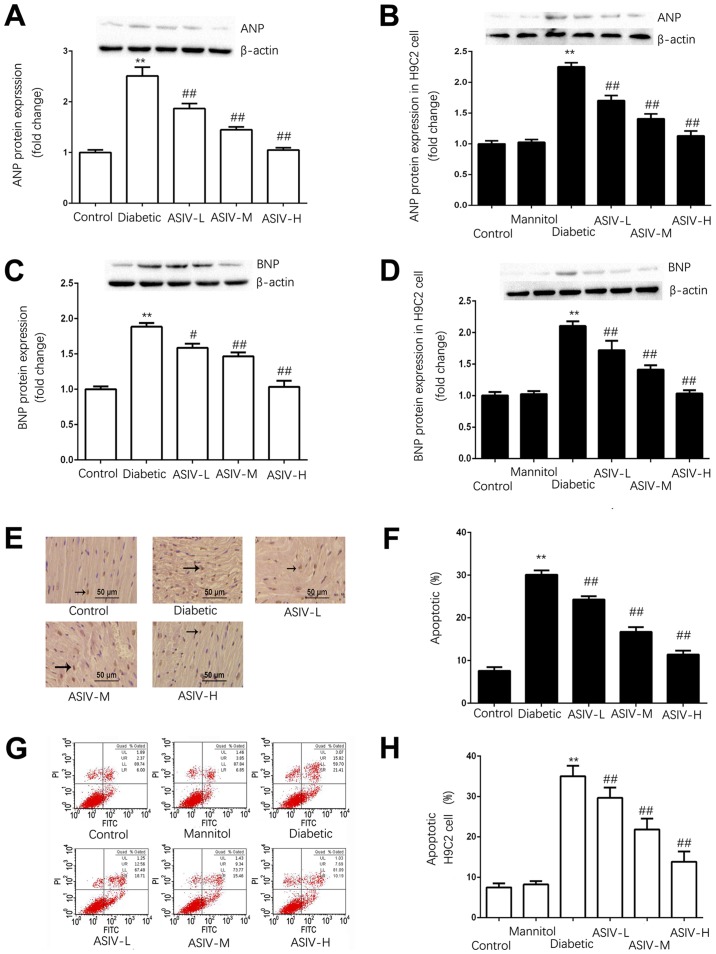
ASIV decreases the damage of myocardial tissue damage in diabetic rats and H9C2 cells in high-glucose conditions
As shown in Fig. 3A-D, the expression of ANP and BNP in the left ventricle of the diabetic group was significantly higher than that in the ventricles of the control group, indicating that the diabetic group exhibited myocardial hypertrophy. The expression of ANP and BNP decreased in the ASIV group.
Figure 3.
ASIV decreases the damage of myocardial tissue of diabetic rats and H9C2 cells in high-glucose environment. Protein expression of ANP in (A) the myocardium and (B) H9C2 cells. The protein expression of BNP in (C) the myocardium and (D) H9C2 cells. (E) Myocardial apoptosis assayed by TUNEL staining. TUNEL-positive cells were manifested as a marked appearance of dark brown apoptotic cell nuclei, and (F) the percentage of apoptotic cells in myocardial tissue. (G) The detection of apoptosis in H9C2 cells by AnnexinV-FITC and PI double staining, and (H) the percentage of apoptotic H9C2 cells. The protein expression of (I) caspase-3, (J) cleaved caspase-3 and (K) cytoplasmic Cyt C in the myocardium, and (L) caspase-3, (M) cleaved caspase-3 and (N) cytoplasmic Cyt C in H9C2 cells. The data are expressed as the means ± SD. n=4. **P<0.01 vs. control group. #P<0.05 and ##P<0.01 vs. diabetic group. The black arrows indicate the nucleus of apoptotic cardiomyocytes. ANP, atrial natriuretic peptide; ASIV, astragaloside IV; L, low; M, mid; H, high; BNP, brain natriuretic peptide; PI, propidium iodide; Cyt C, cytochrome c.
TUNEL staining and FITC/PI double staining were used to detect the apoptosis of the myocardial tissue and H9C2 cells, respectively (Fig. 3E-H). In the myocardial tissue and H9C2 cells, the apoptotic rate of the control group was <10%. Apoptosis was significantly increased in the diabetic group and HG group compared with the control in tissue and cells. The apoptotic rate was dose-dependently decreased by ASIV compared with the diabetic model groups.
The expression of caspase-3, cleaved caspase-3 and cytoplasmic Cyt C (Fig. 3I-N), revealed that the expression of Cyt C in the cytoplasm and cleaved caspase-3 was significantly increased and that caspase-3 was decreased in the model group, whereas the expression of Cyt C and cleaved caspase-3 in the control group was not significantly different from that in the mannitol group; this excluded the influence of osmotic pressure on the results. Following ASIV administration, the protein expression of Cyt C and cleaved caspase-3 were decreased both in heart tissues and H9C2 cells, whereas caspase-3 was significantly increased. The results demonstrated that ASIV can downregulate the increased expression of Cyt C and cleaved caspase-3 induced by the diabetes model.
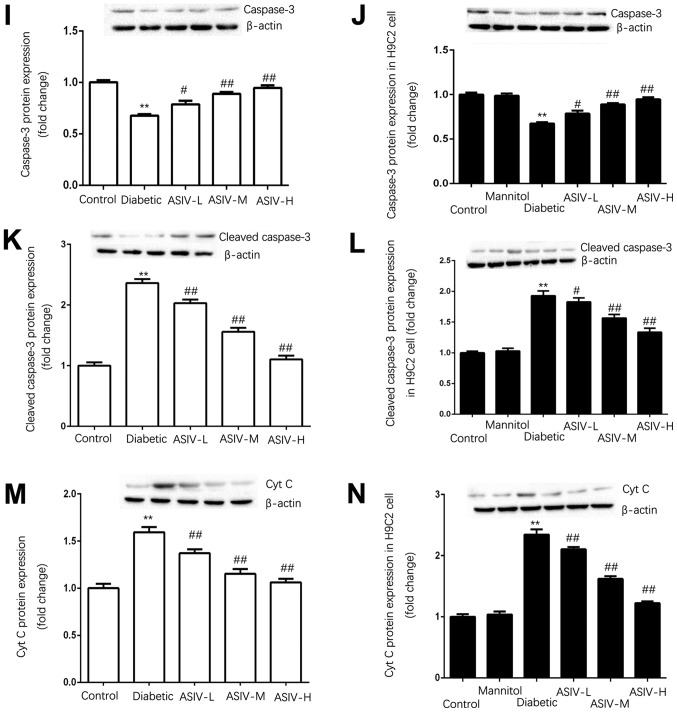
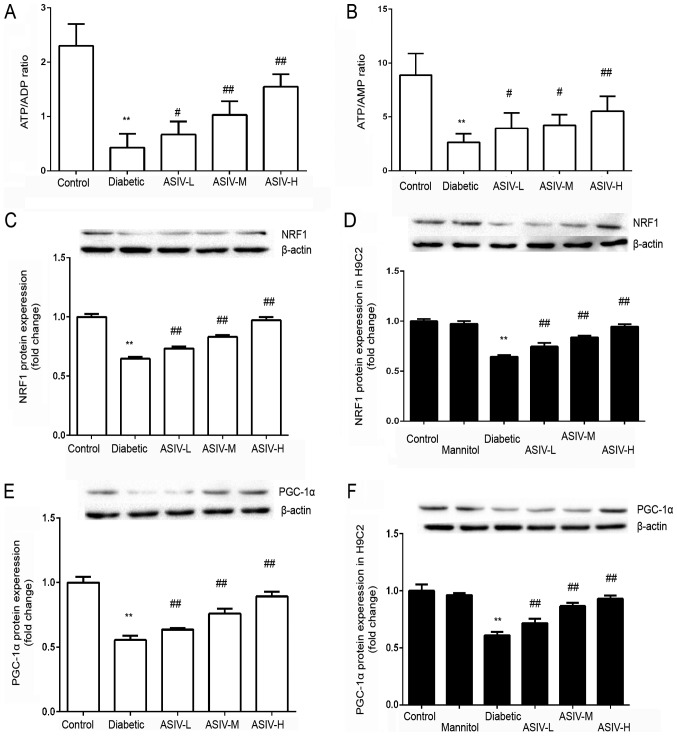
ASIV can regulate the expression of energy metabolism-associated signals and the level of energy metabolism in myocardial tissue and H9C2 cells
The ATP/ADP and ATP/AMP ratios of each group were calculated. The results show that, compared with that of the control group, the ratios were significantly decreased in the diabetic group. These ratios were increased by the different doses of ASIV (Fig. 4A and B).
Figure 4.
ASIV regulates the expression of energy metabolism associated signals and the level of energy metabolism in myocardial tissue and H9C2 cells. Ratio of (A) ATP/ADP and (B) ATP/AMP in H9C2 cells. n=8. The protein expression of NRF1 in (C) the myocardium and (D) H9C2 cells. n=4. The protein expression of PGC-1α in (E) the myocardium and (F) H9C2 cells. n=4. The data are expressed as the mean ± SD. **P<0.01 vs. control group. #P<0.05 and ##P<0.01 vs. diabetic group. ASIV, astragaloside IV; L, low; M, mid; H, high; NRF-1, nuclear respiratory factor 1; PGC-1, peroxisome proliferator-activated receptor λ coactivator 1-α.
Compared with that in the control group and the model (diabetic and HG) groups, the expression of PGC-1α and NRF1 was significantly decreased in the model group (Fig. 4C-F). Following ASIV administration, the expression of PGC-1α and NRF1 was increased, and the expression increased with increasing ASIV concentration. This indicated that ASIV may improve myocardial energy metabolism abnormalities caused by diabetes. By detecting the mRNA expression of PGC-1α and NRF1 in the H9C2 cells, under high-glucose conditions, the influence of osmotic pressure was determined and obtained the same result as that of histone expression, fully demonstrating the function of ASIV in improving myocardial energy metabolism.
Discussion
The main cause of morbidity and mortality in diabetic patients is cardiovascular complications, which accounts for 80% of mortalities in diabetic patients (23). The most notable cardiovascular complication is diabetic cardiomyopathy, which increases the risk of future heart failure 5-fold (24–28). Diabetes has adverse effects on the different cell types of the heart, including endothelial cells (29,30), fibroblasts and myocardial cells (31), and the damage to myocardial cells may be the main cause of heart failure (31–35). With the development of diabetes mellitus, the heart experiences cardiac hypertrophy, decreased compliance, decreased contractility and cell stability damage, leading to cardiac dysfunction (36). The number of apoptotic and necrotic cardiomyocytes began to increase. When the normal physiological structure was destroyed to a certain extent, compensatory adjustment can no longer compensate for myocardial damage, ultimately leading to heart failure (37).
Damage to the myocardium was mainly manifested by myocardial hypertrophy and apoptosis. ASIV, as one of the main active components in Astragalus, is a purified small-molecule saponin. According to existing studies, ASIV has anti-inflammatory and antioxidant effects. In previous studies, ASIV demonstrated efficacious inhibitory effect on apoptosis in vascular endothelial cells and to regulate the energy metabolism of vascular endothelial cells (15–20,38,39). Additionally, in other experiments, it was found that its anti-inflammatory and antioxidant effects can improve the hypertrophy and apoptosis of the myocardium due to inflammation. Therefore, a diabetes model and the administration of ASIV was conducted, in order to study the effect and mechanism of ASIV in diabetic cardiomyopathy.
For the choice of index of hypertrophy, ANP and BNP were measured. Of course, there are other subtypes of natriuretic peptide, especially C-type natriuretic peptide (CNP) and N-terminal-proBNP (NT-proBNP) (40). CNP is involved in the regulation of myocardial changes in myocardial infarction, ischemia-reperfusion and heart failure, but its expression level was also affected by blood pressure and vascular endothelial cells, which cannot specifically respond to myocardial changes. Although NT-proBNP has no biological activity, it has a longer half-life and is more stable than BNP, and has been proposed as a biomarker of heart failure by the American Society of Clinical Chemistry (40–42). However, NT-proBNP could not reflect the changes in cardiac myocytes. ANP and BNP, as important biological signals of myocardial hypertrophy, are mainly synthesized in the atrium and left ventricle respectively, and in addition to indexes such as heart weight index (HWI) and left ventricular weight index (LVWI), ANP and BNP correspond to increased wall tension (43–46). The plasma level of polypeptides was shown to be positively correlated with the pressure caused by the filling of the heart, making it a good marker of LV dysfunction and LV wall stress abnormalities. There was a 23- to 85-fold increase in BNP, particularly in tissues with hypertrophy, compared with that in the control group. Apoptosis is regulated by a series of enzyme-linked reactions, mainly including two signal transduction pathways. One is the extrinsic pathway, that is, the death receptor pathway, which is under the stimulation of external factors; extracellular signal are transmitted to the intracellular caspase-protease promoter enzyme (47). The other is the intrinsic pathway, that is, the mitochondrial pathway (48). Caspase-3, the core protease in the apoptosis signal transduction pathway and an important executive enzyme for apoptosis, acts downstream in both the external pathway and the internal pathway (48,49). The protein expression of caspase-3, as a downstream regulator in the death receptor pathway and mitochondrial apoptosis pathway, directly affects the apoptosis of myocardial cells. After Cyt C is transported from the mitochondria to the cytoplasm, it regulates the activity of the downstream caspase-3 enzyme and promotes the apoptosis of myocardial cells (50,51).
In the present study, STZ was used to establish a diabetes model, and gradient ASIV was used to treat diabetes model animals. The myocardial injury indicators were examined, including myocardial hypertrophy and myocardial apoptosis. HWI, LVWI, ANP and BNP increased, and myocardial hypertrophy occurred in the model group. The expression of cytoplasmic Cyt C and cleaved caspase-3 was increased, and these data combined with the flow cytometry results and TUNEL staining results suggest that apoptosis was increased in the model group. Following ASIV treatment, the indexes of myocardial hypertrophy and myocardial apoptosis recovered to varying degrees. The same results were obtained in H9C2 cells, indicating that ASIV has a therapeutic effect on diabetic myocardial injury.
How does ASIV improve myocardial injury in diabetes? Thus far, previous studies have established the correlation between diabetic complications and mitochondrial dysfunction in multiple tissues (52–54), but the potential mechanism of mitochondrial dysfunction in DCM was not clarified. Normally, the heart relies on persistent aerobic metabolism to maintain the ATP supply and redox balance for optimal systolic function. More than 90% of heart metabolism is aerobic (55,56). Hyperglycemia is a major driver of mitochondrial dysfunction in diabetic myocardium (57–59). Due to the high-energy demand of the heart and the relief of myocardial injury in diabetic cardiomyopathy following abnormal energy metabolism is corrected, mitochondrial dysfunction was considered to be the cause of DCM (60–62). Studies using noninvasive 31p nuclear magnetic resonance imaging found that left ventricular hypertrophy and contractile inhibition are associated with decreased ATP levels, indicating that mitochondrial function was impaired under high-glucose conditions (63,64). PGC-1α is the most important coactivator in mitochondrial synthesis and energy metabolism and has a crucial role in regulating mitochondrial biosynthesis. PGC-1α regulates mitochondrial biosynthesis by activating downstream transcription factors, such as nuclear respiration factor (NRF). NRF is the most important transcription factor in the regulation of mitochondrial biosynthesis (65). The nuclear transcription factor NRF1 regulates the transcription, translation and replication of mitochondrial DNA and the expression of various proteins, including enzymes in the respiratory chain that promote oxidative energy supply, in the mitochondria.
ASIV was postulated to affect mitochondrial synthesis by regulating PGC-1α and NRF1, thereby improving mitochondrial energy metabolism and decreasing the myocardial damage caused by diabetic cardiomyopathy. The expression of PGC-1α and NRF1 protein in myocardial tissues, and the mRNA expression of PGC-1α and NRF1 in H9C2 cells were detected in each group. ASIV upregulated the expression of PGC-1α and NRF1, and the levels of ATP and ADP in H9C2 cells were also detected. The results showed that ASIV improved the energy metabolism level.
Based on the findings of the present study, it can be concluded that ASIV can decrease the damage of myocardial hypertrophy and apoptosis by improving mitochondrial energy metabolism via regulating PGC-1α and NRF1 in diabetic cardiomyopathy. Moreover, the experimental results showed that ASIV had a hypoglycemic effect, but the underlying mechanism was still unclear. In addition, based on previous studies, ASIV also has a protective and therapeutic role in ischemia-reperfusion and oxidative stress on the heart; therefore, the protective effect of ASIV on diabetes mellitus on cardiomyopathy is not specific. Thus, ASIV has a broad protective effect on the heart.
In conclusion, ASIV can ameliorate myocardial mitochondrial energy metabolism abnormalities induced by diabetes mellitus via regulating the expression of PGC-1α and NRF1. Improving abnormal energy metabolism in mitochondria can inhibit apoptosis and myocardial hypertrophy, thereby reducing myocardial injury. Thus, ASIV has the potential to alleviate myocardial damage induced by diabetes, by improving energy metabolism.
Acknowledgements
The authors would like to thank the laboratory teachers Dr Meili Lu, Dr Yang Liu, Dr Tairan Sun, Mr. Cong Li, Mr. Kun Zhao, Miss Tong Zhang, Miss Xiaoyao Zhang and Miss Yang Sun (Key Laboratory of Cardiovascular and Cerebrovascular Drug Researh of Liaoning Province, Junzhou Medical University) for providing technical support in the course of the experiment.
Funding
This work was supported by the National Nature Science Foundation of China (grant nos. 81673632 and 81703793) and LiaoNing Revitalization Talents Program (grant no. XLYC1802017).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
HW and ZZ designed the whole experiment, and contributed to the writing and modification of the article. ZZ, HZ, YZ and JW were responsible for the collection of data. ZZ and HZ performed the analysis and interpretaion of the data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All experiments and procedures were approved by the Medical Ethics Committee of Jinzhou Medical University (approval No. LNMU-2016-121). The raising of animals and the use of drugs are in accordance with the guidelines for the Care and use of Experimental Animals (8th Edition, Press of the National Academy of Sciences).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Lee CD, Folsom AR, Pankow JS, Brancati FL, Atherosclerosis Risk in Communities (ARIC) Study Investigators Cardiovascular events in diabetic and nondiabetic adults with or without history of myocardial infarction. Circulation. 2004;109:855–860. doi: 10.1161/01.CIR.0000116389.61864.DE. [DOI] [PubMed] [Google Scholar]
- 3.Knapp M, Tu X, Wu R. Vascular endothelial dysfunction, a major mediator in diabetic cardiomyopathy. Acta Pharmacol Sin. 2019;40:1–8. doi: 10.1038/s41401-018-0042-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Escaned J, Colmenárez H, Ferrer MC, Gutiérrez M, Jiménez-Quevedo P, Hernández R, Alfonso F, Bañuelos C, Deisla LP, Zamorano JL, Macaya C. Diastolic dysfunction in diabetic patients assessed with Doppler echocardiography: Relationship with coronary atherosclerotic burden and microcirculatory impairment. Rev Esp Cardiol. 2009;62:1395–1403. doi: 10.1016/S0300-8932(09)73125-2. [DOI] [PubMed] [Google Scholar]
- 5.Zheng X, Sun T, Wang X. Activation of type 2 cannabinoid receptors (CB2R) promotes fatty acid oxidation through the SIRT1/PGC-1α pathway. Biochem Biophys Res Commun. 2013;436:377–381. doi: 10.1016/j.bbrc.2013.05.108. [DOI] [PubMed] [Google Scholar]
- 6.Sun X, Chen RC, Yang ZH, Sun GB, Wang M, Ma XJ, Yang LJ, Sun XB. Taxifolin prevents diabetic cardiomyopathy in vivo and in vitro by inhibition of oxidative stress and cell apoptosis. Food Chem Toxicol. 2014;63:221–232. doi: 10.1016/j.fct.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Rowe GC, Jiang A, Arany Z. PGC-1 coactivators in cardiac development and disease. Circ Res. 2010;107:825–838. doi: 10.1161/CIRCRESAHA.110.223818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arany Z, He H, Lin J, Hoyer K, Handschin C, Toka O, Ahmad F, Matsui T, Chin S, Wu PH, et al. Transcriptional coactivator PGC-1 alpha controls the energy state and contractile function of cardiac muscle. Cell Metab. 2005;1:259–271. doi: 10.1016/j.cmet.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Sebastiani M, Giordano C, Nediani C, Travaglini C, Borchi E, Zani M, Feccia M, Mancini M, Petrozza V, Cossarizza A, et al. Induction of mitochondrial biogenesis is a maladaptive mechanism in mitochondrial cardiomyopathies. J Am Coll Cardiol. 2007;50:1362–1369. doi: 10.1016/j.jacc.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 10.Koh JH, Hancock CR, Terada S, Higashida K, Holloszy JO, Han DH. PPARβ is essential for maintaining normal levels of PGC-1α and mitochondria and for the increase in muscle mitochondria induced by exercise. Cell Metab. 2017;25:1176–1185.e5. doi: 10.1016/j.cmet.2017.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell. 1999;98:115–124. doi: 10.1016/S0092-8674(00)80611-X. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura H, Matoba S, Iwai-Kanai E, Kimata M, Hoshino A, Nakaoka M, Katamura M, Okawa Y, Ariyoshi M, Mita Y, et al. p53 promotes cardiac dysfunction in diabetic mellitus caused by excessive mitochondrial respiration-mediated reactive oxygen species generation and lipid accumulation. Circ Heart Fail. 2012;5:106–115. doi: 10.1161/CIRCHEARTFAILURE.111.961565. [DOI] [PubMed] [Google Scholar]
- 13.Anderson EJ, Rodriguez E, Anderson CA, Thayne K, Chitwood WR, Kypson AP. Increased propensity for cell death in diabetic human heart is mediated by mitochondrial-dependent pathways. Am J Physiol Heart Circ Physiol. 2011;300:H118–H124. doi: 10.1152/ajpheart.00932.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mei M, Tang F, Lu M, He X, Wang H, Hou X, Hu J, Xu C, Han R. Astragaloside IV attenuates apoptosis of hypertrophic cardiomyocyte through inhibiting oxidative stress and calpain-1 activation. Environ Toxicol Pharmacol. 2015;40:764–773. doi: 10.1016/j.etap.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Zhang S, Tang F, Yang Y, Lu M, Luan A, Zhang J, Yang J, Wang H. Astragaloside IV protects against isoproterenol-induced cardiac hypertrophy by regulating NF-κB/PGC-1α signaling mediated energy biosynthesis. PLoS One. 2015;10:e0118759. doi: 10.1371/journal.pone.0118759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jia G, Leng B, Wang H, Dai H. Inhibition of cardiotrophin-1 overexpression is involved in the anti-fibrotic effect of Astrogaloside IV. Mol Med Rep. 2017;16:8365–8370. doi: 10.3892/mmr.2017.7676. [DOI] [PubMed] [Google Scholar]
- 17.Dai H, Jia G, Lu M, Liang C, Wang Y, Wang H. Astragaloside IV inhibits isoprenaline-induced cardiac fibrosis by targeting the reactive oxygen species/mitogen-activated protein kinase signaling axis. Mol Med Rep. 2017;15:1765–1770. doi: 10.3892/mmr.2017.6220. [DOI] [PubMed] [Google Scholar]
- 18.Xu C, Tang F, Lu M, Yang J, Han R, Mei M, Hu J, Wang H. Pretreatment with Astragaloside IV protects human umbilical vein endothelial cells from hydrogen peroxide induced oxidative stress and cell dysfunction via inhibiting eNOS uncoupling and NADPH oxidase-ROS-NF-κB pathway. Can J Physiol Pharmacol. 2016;94:1132–1140. doi: 10.1139/cjpp-2015-0572. [DOI] [PubMed] [Google Scholar]
- 19.Xu C, Tang F, Lu M, Yang J, Han R, Mei M, Hu J, Zhou M, Wang H. Astragaloside IV improves the isoproterenol-induced vascular dysfunction via attenuating eNOS uncoupling-mediated oxidative stress and inhibiting ROS-NF-κB pathways. Int Immunopharmacol. 2016;33:119–127. doi: 10.1016/j.intimp.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Lu M, Tang F, Zhang J, Luan A, Mei M, Xu C, Zhang S, Wang H, Maslov LN. Astragaloside IV attenuates injury caused by myocardial ischemia/reperfusion in rats via regulation of toll-like receptor 4/nuclear factor-κB signaling pathway. Phytother Res. 2015;29:599–606. doi: 10.1002/ptr.5297. [DOI] [PubMed] [Google Scholar]
- 21.Holly EN, Shimamoto A, Debold JF, Miczek KA. Sex differences in behavioral and neural cross-sensitization and escalated cocaine taking as a result of episodic social defeat stress in rats. Pyschopharmacology (Berl) 2012;224:179–188. doi: 10.1007/s00213-012-2846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walczak M, Błasiak T. Midbrain dopaminergic neuron activity across alternating brain states of urethane anaesthetized rat. Eur J Neurosci. 2017;45:1068–1077. doi: 10.1111/ejn.13533. [DOI] [PubMed] [Google Scholar]
- 23.Seferović PM, Petrie MC, Filippatos GS, Anker SD, Rosano G, Bauersachs J, Paulus WJ, Komajda M, Cosentino F, de Boer RA, et al. Type 2 diabetes mellitus and heart failure: A position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20:853–872. doi: 10.1002/ejhf.1170. [DOI] [PubMed] [Google Scholar]
- 24.Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: Estimates and projections to the year 2010. Diabet Med. 1997;14(Suppl 5):S1–S85. doi: 10.1002/(SICI)1096-9136(199712)14:5+<S7::AID-DIA522>3.3.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 25.Dries DL, Sweitzer NK, Drazner MH, Stevenson LW, Gersh BJ. Prognostic impact of diabetes mellitus in patients with heart failure according to the etiology of left ventricular systolic dysfunction. J Am Coll Cardiol. 2001;38:421–428. doi: 10.1016/S0735-1097(01)01408-5. [DOI] [PubMed] [Google Scholar]
- 26.Kannel WB, Hjortland M, Castelli WP. Role of diabetes in congestive heart failure: The framingham study. Am J Cardiol. 1974;34:29–34. doi: 10.1016/0002-9149(74)90089-7. [DOI] [PubMed] [Google Scholar]
- 27.Alaei Faradonbeh N, Nikaeen F, Akbari M, Almasi N, Vakhshoori M. Cardiovascular disease risk prediction among Iranian patients with diabetes mellitus in Isfahan Province, Iran, in 2014, by using Framingham risk score, atherosclerotic cardiovascular disease risk score, and high-sensitive C-reactive protein. ARYA Atheroscler. 2018;14:163–168. doi: 10.22122/arya.v14i4.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tadic M, Cuspidi C. Obesity and heart failure with preserved ejection fraction: A paradox or something else? Heart Fail Rev. 2019;24:379–385. doi: 10.1007/s10741-018-09766-x. [DOI] [PubMed] [Google Scholar]
- 29.Icks A, Claessen H, Kirchberger I, Heier M, Peters A, Trentinaglia I, Giani G, von Scheidt W, Meisinger C. Mortality after first myocardial infarction in diabetic and non-diabetic people between 1985 and 2009. The MONICA/KORA registry. Eur J Epidemiol. 2014;29:899–909. doi: 10.1007/s10654-014-9964-6. [DOI] [PubMed] [Google Scholar]
- 30.Feuvray D. Diabetic cardiomyopathy. Arch Mal Coeur Vaiss. 2004;97:261–265. [PubMed] [Google Scholar]
- 31.Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115:3213–3223. doi: 10.1161/CIRCULATIONAHA.106.679597. [DOI] [PubMed] [Google Scholar]
- 32.Fiordaliso F, Li B, Latini R, Sonnenblick EH, Anversa P, Leri A, Kajstura J. Myocyte death in streptozotocin-induced diabetes in rats in angiotensin II-dependent. Lab Invest. 2000;80:513–527. doi: 10.1038/labinvest.3780057. [DOI] [PubMed] [Google Scholar]
- 33.Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol. 2003;41:1387–1393. doi: 10.1016/S0735-1097(03)00166-9. [DOI] [PubMed] [Google Scholar]
- 34.Riehle C, Bauersachs J. Of mice and men: Models and mechanisms of diabetic cardiomyopathy. Basic Res Cardiol. 2018;114:2. doi: 10.1007/s00395-018-0711-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilca GE, Stefanescu G, Badulescu O, Tanase DM, Bararu I, Ciocoiu M. Diabetic cardiomyopathy: Current approach and potential diagnostic and therapeutic targets. J Diabetes Res. 2017;2017:1310265. doi: 10.1155/2017/1310265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Voulgari C, Papadogiannis D, Tentolouris N. Diabetic cardiomyopathy: From the pathophysiology of the cardiac myocytes to current diagnosis and management strategies. Vasc Health Risk Manag. 2010;6:883–903. doi: 10.2147/VHRM.S11681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lu M, Leng B, He X, Zhang Z, Wang H, Tang F. Calcium sensing receptor-related pathway contributes to cardiac injury and the mechanism of Astragaloside IV on cardioprotection. Front Pharmacol. 2018;9:1163. doi: 10.3389/fphar.2018.01163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guan FY, Yang SJ, Liu J, Yang SR. Effect of astragaloside IV against rat myocardial cell apoptosis induced by oxidative stress via mitochondrial ATP-sensitive potassium channels. Mol Med Rep. 2015;12:371–376. doi: 10.3892/mmr.2015.3400. [DOI] [PubMed] [Google Scholar]
- 39.Kakoullis L, Giannopoulou E, Papachristodoulou E, Pantzaris ND, Karamouzos V, Kounis NG, Koniari I, Velissaris D. The utility of brain natriuretic peptides in septic shock as markers for mortality and cardiac dysfunction: A systematic review. Int J Clin Pract. 2019;73:e13374. doi: 10.1111/ijcp.13374. [DOI] [PubMed] [Google Scholar]
- 40.Pemberton CJ, Johnson ML, Yandle TG, Espiner EA. Deconvolution analysis of cardiac natriuretic peptides during acute volume overload. Hypertension. 2000;36:355–359. doi: 10.1161/01.HYP.36.3.355. [DOI] [PubMed] [Google Scholar]
- 41.Tang WH, Francis GS, Morrow DA, Newby LK, Cannon CP, Jesse RL, Storrow AB, Christenson RH, NACB Committee National academy of clinical biochemistry laboratory medicine practice guidelines: Clinical utilization of cardiac biomarker testing in heart failure. Clin Biochem. 2008;41:210–221. doi: 10.1016/j.clinbiochem.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Li S, Xiao Z, Li L, Hu B, Zhou Z, Yi S, Luo J, Xie L, Nie B, Mo L, Wang S. Establishment of normal reference values of NT-proBNP and its application in diagnosing acute heart failure in children with severe hand food and mouth disease. Medicine. 2018;97:e12218. doi: 10.1097/MD.0000000000012218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Candido R, Forbes JM, Thomas MC, Thallas V, Dean RG, Burns WC, Tikellis C, Ritchie RH, Twigg SM, Cooper ME, Burrell LM. A breaker of advanced glycation end products attenuates diabetes-induced myocardial structural changes. Circ Res. 2003;92:785–792. doi: 10.1161/01.RES.0000065620.39919.20. [DOI] [PubMed] [Google Scholar]
- 44.Connelly KA, Kelly DJ, Zhang Y, Prior DL, Martin J, Cox AJ, Thai K, Feneley MP, Tsoporis J, White KE, et al. Functional, structural and molecular aspects of diastolic heart failure in the diabetic (mRen-2)27 rat. Cardiovasc Res. 2007;76:280–291. doi: 10.1016/j.cardiores.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 45.Ritchie RH, Quinn JM, Cao AH, Drummond GR, Kaye DM, Favaloro JM, Proietto J, Delbridge LM. The antioxidant tempol inhibits cardiac hypertrophy in the insulin-resistant GLUT4-deficient mouse in vivo. J Mol Cell Cardiol. 2007;42:1119–1128. doi: 10.1016/j.yjmcc.2007.03.900. [DOI] [PubMed] [Google Scholar]
- 46.Huynh K, McMullen JR, Julius TL, Tan JW, Love JE, Cemerlang N, Kiriazis H, Du XJ, Ritchie RH. Cardiac-specific IGF-1 receptor transgenic expression protects against cardiac fibrosis and diastolic dysfunction in a mouse model of diabetic cardiomyopathy. Diabetes. 2010;59:1512–1520. doi: 10.2337/db09-1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Das DK. Redox regulation of cardiomyocyte survival and death. Antioxid Redox Signal. 2001;3:23–37. doi: 10.1089/152308601750100461. [DOI] [PubMed] [Google Scholar]
- 48.Webster KA, Graham RM, Bishopric NH. BNip3 and signal-specific programmed death in the heart. J Mol Cell Cardiol. 2005;38:35–45. doi: 10.1016/j.yjmcc.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Das S, Khan N, Mukherjee S, Bagchi D, Gurusamy N, Swartz H, Das DK. Redox regulation of resveratrol-mediated switching of death signal into survival signal. Free Radic Biol Med. 2008;44:82–90. doi: 10.1016/j.freeradbiomed.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 50.Lax NZ, Turnbull DM, Reeve AK. Mitochondrial mutations: Newly discovered players in neuronal degeneration. Neuroscientist. 2011;17:645–658. doi: 10.1177/1073858410385469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li XD, Li XM, Gu JW, Sun XC. MiR-155 regulates lymphoma cell proliferation and apoptosis through targeting SOCS3/JAK-STAT3 signaling pathway. Eur Rev Med Pharmacol Sci. 2017;21:5153–5159. doi: 10.26355/eurrev_201711_13832. [DOI] [PubMed] [Google Scholar]
- 52.Fetterman JL, Holbrook M, Westbrook DG, Brown JA, Feeley KP, Bretón-Romero R, Linder EA, Berk BD, Weisbrod RM, Widlansky ME, et al. Mitochondrial DNA damage and vascular function in patients with diabetes mellitus and atherosclerotic cardiovascular disease. Cardiovasc Diabetol. 2016;15:53. doi: 10.1186/s12933-016-0372-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kalvala AK, Khan I, Gundu C, Kumar A. An overview on ATP dependent and independent proteases including an anterograde to retrograde control on mitochondrial function; Focus on diabetes and diabetic complications. Curr Pharm Des. 2019 Jul 18; doi: 10.2174/1381612825666190718153901. (Epub ahead of print). doi: 10.2174/1381612825666190718153901. [DOI] [PubMed] [Google Scholar]
- 54.Jin H, Zhu B, Liu X, Jin J, Zou H. Metabolic characterization of diabetic retinopathy: An 1H-NMR-based metabolomic approach using human aqueous humor. J Pharm Biomed Anal. 2019;174:414–421. doi: 10.1016/j.jpba.2019.06.013. [DOI] [PubMed] [Google Scholar]
- 55.Rolfe DF, Brown GC. Cellular energy utilization and molecular origin of standard metabolic rate in mammals. Physiol Rev. 1997;77:731–758. doi: 10.1152/physrev.1997.77.3.731. [DOI] [PubMed] [Google Scholar]
- 56.Trost SU, Belke DD, Bluhm WF, Meyer M, Swanson E, Dillmann WH. Overexpression of the sarcoplasmic reticulum Ca(2+)-ATPase improves myocardial contractility in diabetic cardiomyopathy. Diabetes. 2002;51:1166–1171. doi: 10.2337/diabetes.51.4.1166. [DOI] [PubMed] [Google Scholar]
- 57.Camara AK, Bienengraeber M, Stowe DF. Mitochondrial approaches to protect against cardiac ischemia and reperfusion injury. Front Physiol. 2011;2:13. doi: 10.3389/fphys.2011.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chatham JC, Seymour AM. Cardiac carbohydrate metabolism in Zucker diabetic fatty rats. Cardiovasc Res. 2002;55:104–112. doi: 10.1016/S0008-6363(02)00399-1. [DOI] [PubMed] [Google Scholar]
- 59.Dey S, DeMazumder D, Sidor A, Foster DB, O'Rourke B. Mitochondrial ROS drive sudden cardiac death and chronic proteome remodeling in heart failure. Circ Res. 2018;123:356–371. doi: 10.1161/res.123.suppl_1.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang Y, Gao P, Wei C, Li H, Zhang L, Zhao Y, Wu B, Tian Y, Zhang W, Wu L, et al. Calcium sensing receptor protects high glucose-induced energy metabolism disorder via blocking gp78-ubiquitin proteasome pathway. Cell Death Dis. 2017;8:e2799. doi: 10.1038/cddis.2017.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ares-Carrasco S, Picatoste B, Camafeita E, Carrasco-Navarro S, Zubiri I, Ortiz A, Egido J, López JA, Tuñón J, Lorenzo O. Proteome changes in the myocardium of experimental chronic diabetes and hypertension: Role of PPARα in the associated hypertrophy. J Proteomics. 2012;75:1816–1829. doi: 10.1016/j.jprot.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 62.Tsushima K, Bugger H, Wende AR, Soto J, Jenson GA, Tor AR, McGlauflin R, Kenny HC, Zhang Y, Souvenir R, et al. Mitochondrial reactive oxygen species in lipotoxic hearts induce Post-translational modifications of AKAP121, DRP1, and OPA1 that promote mitochondrial fission. Circ Res. 2018;122:58–73. doi: 10.1161/CIRCRESAHA.117.311307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Knowlton AA, Chen L, Malik ZA. Heart failure and mitochondrial dysfunction: The role of mitochondrial fission/fusion abnormalities and new therapeutic strategies. J Cardiovasc Pharmacol. 2014;63:196–206. doi: 10.1097/01.fjc.0000432861.55968.a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Song M, Mihara K, Chen Y, Scorrano L, Dorn GW., II Mitochondrial fission and fusion factors reciprocally orchestrate mitophagic culling in mouse hearts and cultured fibroblasts. Cell Metab. 2015;21:273–286. doi: 10.1016/j.cmet.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Recchia FA, McConnell PI, Bernstein RD, Vogel TR, Xu X, Hintze TH. Reduced nitric oxide production and altered myocardial metabolism during the decompensation of pacing-induced heart failure in the conscious dog. Circ Res. 1998;83:969–979. doi: 10.1161/01.RES.83.10.969. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.