Abstract
Huntington’s disease (HD), an inherited neurodegenerative disorder that principally affects striatum and cerebral cortex, is generally thought to have an adult onset. However, a small percentage of cases develop symptoms before 20 years of age. This juvenile variant suggests that brain development may be altered in HD. Indeed, recent evidence supports an important role of normal huntingtin during embryonic brain development and mutations in this protein cause cortical abnormalities. Functional studies also demonstrated that the cerebral cortex becomes hyperexcitable with disease progression. In this review, we examine clinical and experimental evidence that cortical development is altered in HD. We also provide preliminary evidence that cortical pyramidal neurons from R6/2 mice, a model of juvenile HD, are hyperexcitable and display dysmorphic processes as early as postnatal day 7. Further, some symptomatic mice present with anatomical abnormalities reminiscent of human focal cortical dysplasia, which could explain the occurrence of epileptic seizures in this genetic mouse model and in children with juvenile HD. Finally, we discuss recent treatments aimed at correcting abnormal brain development.
Introduction
Huntington’s disease (HD) can be defined by a triad of motor, cognitive and psychiatric symptoms (Harper and Jones, 2002). The most characteristic and debilitating motor symptom is the occurrence of uncontrollable dance-like movements (chorea). Psychiatric symptoms include depression, mood swings and suicidal ideation. Cognitive symptoms typically precede chorea and include sensory and attention deficits (Lawrence et al., 1998; Bates et al., 2002). The cause of HD is a genetic mutation consisting of an expansion of CAG repeats in the huntingtin (HTT) gene, localized in the short arm of chromosome 4 (The Huntington’s Disease Collaborative Research Group, 1993). When the number of CAG repeats exceeds 39, the affected individual will invariably develop HD symptoms sooner or later. In addition, there is an inverse relationship between disease onset, severity of symptoms, and the number of CAG repeats, such that the longer the repeat length the sooner symptoms manifest (Andrew et al., 1993; Penney et al., 1997).
Histopathological studies have demonstrated that the brain regions more susceptible to degeneration in HD are the caudate nucleus/putamen and the cerebral cortex (Vonsattel and DiFiglia, 1998; Waldvogel et al., 2015). Striatal and cortical projection neurons are preferentially lost whereas diverse types of interneurons are spared, with the exception of GABAergic parvalbumin (PV)-expressing interneurons (Reiner et al., 2013). Interestingly, motor and psychiatric symptoms are tightly correlated with cell loss in the cerebral cortex (Thu et al., 2010; Waldvogel et al., 2015). Specifically, motor symptoms correlate with primary motor cortex cell loss whereas mood symptoms are associated with cell loss in the cingulate cortex (Thu et al., 2010).
Although neurodegenerative changes have long been recognized to underlie HD motor symptoms, several clinical and experimental studies have suggested that aberrant cortical development may also play an important role in the manifestation of HD symptoms (Paulsen et al., 2006; Godin et al., 2010; Tereshchenko et al., 2019). In this review, we discuss why we think that faulty cortical development is at the root of some HD functional alterations, in particular cortical hyperexcitability. Also, we provide preliminary morphological and electrophysiological evidence that in the R6/2 genetic mouse model of HD, cortical architecture, neurons, and circuits are altered very early in postnatal development.
Size matters; one mutation, two different forms of HD
HD is generally conceived as an adult-onset neurodegenerative disorder. However, another less common (5–10%) juvenile form (JHD, known as rigid or Westphal variant) of the disease also exists, typically when the CAG triplet repeat expansion is >65 (Hunnicutt et al., 2016). Studies have shown that the sex of the transmitting parent, usually the father, exerts a major influence on CAG repeat expansion leading to earlier symptom onset (Telenius et al., 1993). The symptoms of JHD differ from those typically seen in adult-onset HD. Children with HD display mental retardation, hyperactivity, and aggressive behavior. Some of these children also have microcephaly, suggesting that this form of HD may represent a developmental rather than a neurodegenerative disorder (Letort and Gonzalez-Alegre, 2013; Hunnicutt et al., 2016). With disease progression, dystonia, rigidity, and chorea also occur. A fundamental difference between JHD and adult-onset HD is the high prevalence of epileptic seizures in the juvenile form (Rasmussen et al., 2000; Gambardella et al., 2001; Seneca et al., 2004). The cause of epileptic seizures remains unknown (Cummings et al., 2009). However, we have hypothesized that seizures could be the result of faulty development of cortical circuits, similar to those observed in malformations of cortical development (MCD), specifically focal cortical dysplasia (FCD) of Taylor (Taylor et al., 1971; Estrada-Sánchez et al., 2016). This was based on evidence that in some animal models of HD, and presumably also in human cases, the cerebral cortex progressively becomes hyperexcitable (Cummings et al., 2009).
HTT is essential for normal brain development
The HTT protein has multiple functions that include, among many others, vesicle trafficking, spindle orientation during cell division, endocytosis, transcriptional regulation, maintenance of cell morphology and survival (Saudou and Humbert, 2016). It is also known that normal HTT plays a crucial role during development, as lack of this protein is lethal (Duyao et al., 1995; Nasir et al., 1995; Zeitlin et al., 1995; Saudou and Humbert, 2016). Other studies have shown that embryonic, conditional deletion of HTT from cortical pyramidal neurons (CPNs) reduced cortical volume and neuron abundance (Dragatsis et al., 2017). Similarly, loss of HTT function in subpallial lineages disrupted forebrain interneuron species early in life and also led to a number of neurological deficits reminiscent of HD (Mehler et al., 2019).
In the past few years, the idea that HD in general, and JHD in particular, is not solely a neurodegenerative but also a neurodevelopmental disease, has gained momentum (Godin et al., 2010; Durieux et al., 2011; Wiatr et al., 2017). Indeed, the HTT protein may alter different aspects of chromatin regulation and transcription during neural development (Durieux et al., 2011). For example, in vivo inactivation of HTT by RNA interference or deletion of the gene affects spindle orientation and cell fate of cortical progenitors in the ventricular zone of mouse embryos, altering the thickness of the developing cortex as well as the polarization and migration of newly generated neurons (Godin et al., 2010; Molina-Calavita et al., 2014). Furthermore, depletion of HTT in post-mitotic projection neurons leads to the mislocalization of layer-specific neuronal populations in the mouse neocortex, suggesting that HTT, via regulation of RAB11-dependent N-Cadherin trafficking, is critical for neuronal migration (Barnat et al., 2017). Importantly, the authors also evinced that mutant HTT (mHTT) loses its capacity to promote neuronal migration. Normal HTT also is required for the correct establishment of cortical and striatal excitatory circuits and this function is lost when the mHTT is present (McKinstry et al., 2014). When cortical HTT function is conditionally silenced from CPNs, cortical and striatal excitatory synapses form and mature at an accelerated rate through postnatal day (P)21 but exuberant synaptic connectivity is lost over time in the cortex, resulting in the deterioration of synapses by 5 weeks of age (McKinstry et al., 2014). It can thus be postulated that mHTT impairs neurodevelopmental pathways (Blockx et al., 2012; Consortium, 2017). Indeed, expression of mHTT during early development is sufficient to produce a permanent HD phenotype even if expression is terminated at P21. Furthermore, developmental deficits associated with HTT function render cells more susceptible to degeneration (Arteaga-Bracho et al., 2016; Molero et al., 2016).
Not only is cortical brain development compromised by the presence of mHTT, but CPN function itself is altered by the early formation of mHTT aggregates. In R6/2 transgenic mice (Mangiarini et al., 1996), intranuclear inclusions can be detected as early as 3 weeks of age (Morton et al., 2000; Meade et al., 2002; Cummings et al., 2012). At this age, intranuclear inclusions are most abundant in CA1 hippocampal region and cortical layers III-V whereas in striatum inclusions are rare (Morton et al., 2000). Using more sensitive immunohistochemical methods, diffuse proto-aggregates have been observed in developing axonal tracts during embryonic development and early postnatal brains in juvenile and adult-onset mouse models of HD (Osmand et al., 2016). These axonal aggregates could alter synaptic physiology during early postnatal development. In support, using a corticostriatal co-culture from YAC128 mice, a model of adult-onset HD (Slow et al., 2003), synaptic transmission was impaired as early as three weeks in vitro (Buren et al., 2016). In addition, in an in vitro model of HD based on the generation of induced pluripotent stem cells from HD patients and controls, it was observed that HD-derived cells displayed a greater number of neuronal progenitors compared with controls. This cell population showed enhanced vulnerability to brain-derived neurotropic factor (BDNF) withdrawal in the JHD lines (Mattis et al., 2015). Interestingly, increased vulnerability was due to N-methyl-D-aspartate (NMDA) glutamate receptor-mediated toxicity, suggesting that aberrant Ca2+ signaling could be involved.
The observation of aberrant migration and polarization of cortical progenitors is reminiscent of the cortical maldevelopment observed in humans with FCD, a disorder characterized by dyslamination, CPN misorientation, and the presence of dysmorphic pyramidal neurons, all of which contribute to epileptogenesis (Taylor et al., 1971; Cepeda et al., 2003a; Dautan et al., 2016). Thus, we could hypothesize that the presence of mHTT in neuronal progenitors affects cortical organization and induces diffuse architectural and cellular abnormalities, similar to those observed in FCD, which results in cortical hyperexcitability (Cummings et al., 2009; Blumcke et al., 2011; Estrada-Sánchez et al., 2016).
The cerebral cortex is hyperexcitable in HD brains
The central role of the cerebral cortex in the genesis of the HD phenotype has long been recognized in clinical and experimental studies (Laforet et al., 2001; Paulsen et al., 2006; Estrada-Sanchez and Rebec, 2013; Virlogeux et al., 2018). In this section we review clinical and experimental evidence.
Evidence from human studies
The fact that cognitive and psychiatric disturbances appear long before overt motor symptoms (Lawrence et al., 1996; Lawrence et al., 1998) is an indication that the cortex is heavily involved in striatal neuron dysfunction. Functional abnormalities are evident as revealed by changes in cortical excitability and plasticity in preclinical and early HD (Schippling et al., 2009; Orth et al., 2010). Overall, studies indicate that at least certain cortical areas become hyperexcitable with disease progression (Agarwal et al., 2019). For example, transmagnetic stimulation (TMS) studies have demonstrated increased intracortical facilitation and reduced short interval intracortical inhibition in premanifest and early manifest HD patients (Abbruzzese et al., 1997; Nardone et al., 2007; Schippling et al., 2009; Berardelli and Suppa, 2013) indicating altered excitatory/inhibitory balance. As a consequence, motor cortex plasticity has been shown to be abnormal in HD gene carriers (Orth et al., 2010). Indeed, using paired-pulse TMS paradigms, it was suggested that GABA-mediated cortical inhibition is deficient in both presymptomatic and symptomatic patients (Philpott et al., 2016). Consistent with this idea, a study conducted on a small cohort of HD patients demonstrated that inhibitory TMS (1 Hz) of the supplementary motor area (SMA) significantly reduced choreic movements, leading the authors to conclude that overactivity of the SMA plays an essential role in the generation of abnormal movements (Brusa et al., 2005).
Evidence from animal studies
The excitotoxicity hypothesis of cell death in HD postulates that neurodegeneration is caused by excess glutamate release at striatal synapses and/or increased sensitivity of postsynaptic glutamate NMDA receptors (DiFiglia, 1990), in particular those located extrasynaptically (Okamoto et al., 2009; Milnerwood et al., 2010; Raymond et al., 2011). Thus, it is believed that sustained activation of extrasynaptic NMDA receptors triggers an apoptotic cascade that culminates in cell death of medium-sized spiny projection neurons (MSNs). While the traditional view considered the cerebral cortex as the main contributor of glutamate release, recent work has revealed a major contribution from the thalamo-striatal pathway (Huerta-Ocampo et al., 2014; Smith et al., 2014). This pathway is affected early and persistently in several HD mouse models (Deng et al., 2013; Kolodziejczyk and Raymond, 2016; Parievsky et al., 2017).
If glutamate release becomes excitotoxic to medium-sized spiny neurons (MSNs), it might be expected that reducing glutamate inputs could prevent cell loss in HD. Indeed, in animal models evidence indicates that removal of the cerebral cortex delays HD symptoms and extends life span (Stack et al., 2007). Furthermore, preventing the expression of mHTT in CPNs has been shown to ameliorate the HD phenotype (Wang et al., 2014; Estrada-Sanchez et al., 2015). There also is evidence of glutamate release dysregulation when overt symptoms emerge (Cepeda et al., 2003a), as well as biphasic changes in glutamate release, initially elevated and then progressively reduced (Joshi et al., 2009). The occurrence of large synaptic events in MSNs coinciding with the onset of overt symptoms in R6/2 mice suggested cortical hyperexcitability (Cepeda et al., 2003a). Consistent with this idea, electrophysiological studies in the BACHD mouse model (Gray et al., 2008) found decreased layer II/III PV-interneuron excitation and decreased CPN inhibition at 6 months, when behavioral symptoms become evident (Gu et al., 2005; Spampanato et al., 2008). Interestingly, it was recently shown that R6/2 mice have fewer perisomatic PV-positive terminals on CPNs than their wildtype (WT) counterparts, an observation that was also consistent in HD autopsy brains (Burgold et al., 2019). Importantly, this reduced inhibition was reflected by increased cortical activity measured with in vivo calcium imaging. Increased cortical excitability also was demonstrated electrophysiologically in vivo. For example, membrane fluctuations (Down to Up state) could be evoked with smaller currents in cortical neurons from symptomatic R6/2 compared with control mice (Stern, 2011). Furthermore, the amount of coherence in the state transitions of single neurons was less correlated with global activity compared with controls. This effect was proposed to affect the ability of CPNs to participate in coordinated activity within neuronal assemblies, which could explain the diminished synchrony of spikes found in behaving R6/2 mice (Walker et al., 2008).
As in humans, studies in HD animal models have shown impaired cortical synaptic plasticity, likely as a result of altered excitatory/inhibitory balance. For example, presymptomatic R6/1 mice show deficits in barrel cortex plasticity in a somatosensory whisker-deprivation paradigm (Cybulska-Klosowicz et al., 2004; Mazarakis et al., 2005). In the same mouse model, electrophysiological studies demonstrated progressive derailment of long-term depression (LTD) and long-term potentiation (LTP) at perirhinal and prefrontal synapses (Cummings et al., 2006; Cummings et al., 2007; Dallerac et al., 2011). Remarkably, alterations in LTD and LTP could be reversed by dopamine D2 and D1 receptor agonists respectively.
Definitive corroboration of cortical hyperexcitability and loss of the excitatory/inhibitory balance was provided by our group (Cummings et al., 2009). In three different genetic mouse models of HD, the frequency of spontaneous excitatory postsynaptic currents (EPSCs) was increased whereas that of spontaneous inhibitory postsynaptic currents (IPSCs) was decreased. In support of perturbations of the excitatory/inhibitory balance in the cerebral cortex of R6/2 mice, immunohistochemistry demonstrated increased VGLUT1 expression and reduced GAT1 expression. In addition, compared with WT mice, blockade of GABAA receptors in slices from R6/2 mice induced more frequent complex, ictal-like epileptiform discharges in CPNs. This phenomenon was observed in mice as young as P21. What is not known is why and how early the cerebral cortex becomes hyperexcitable.
New observations in developing R6/2 mice point to aberrant cortical neuron development and early hyperexcitability
Morphological and Electrophysiological findings
Recently we extended our studies on CPN excitability to developing R6/2 and control littermates (P7 and P14). Mice (n=13) of either sex were used at P7 (6 WT and 7 R6/2). Experimenters were blind to the genotype, which was only identified a posteriori from DNA tail samples, thus ensuring unbiased results. CPNs in layers II/III and V from the motor cortex were visualized with infrared differential interference contrast (IR-DIC) optics (see detailed methods in Supplementary Material). In order to increase cortical excitability, the GABAA receptor antagonist bicuculline (BIC, 10 μM), alone or in conjunction with the type “A” K+ channel blocker 4-aminopyridine (4-AP, 100 μM), were used. Both compounds are proconvulsant and we have used them in the past to examine cortical excitability and seizure susceptibility in HD mice (Cummings et al., 2009). The patch pipette also contained biocytin (0.2%) to label the recorded cells and, following histological processing, the fine morphology of CPNs was examined.
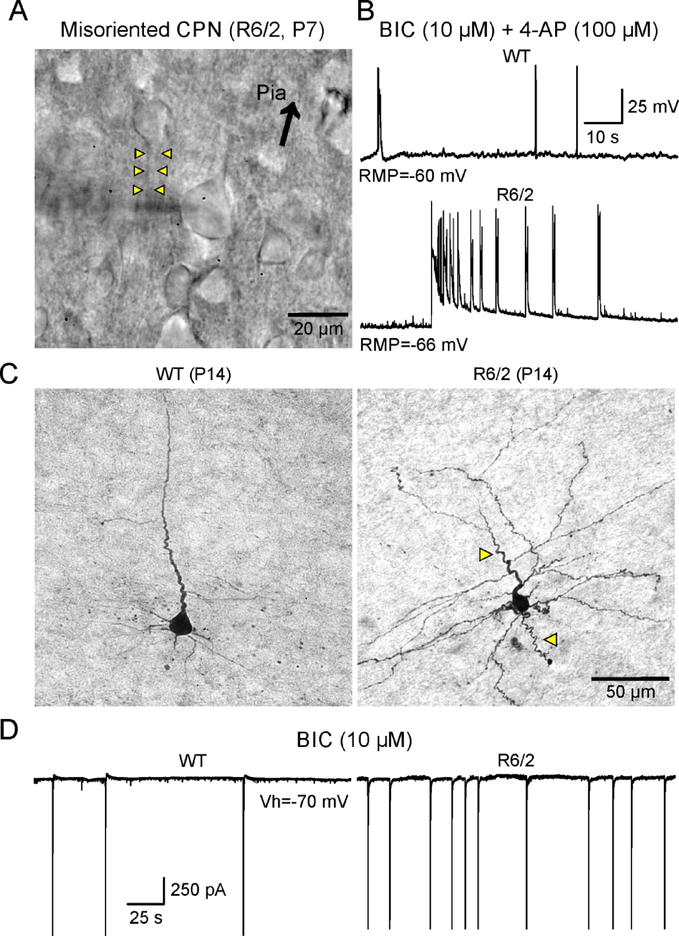
Preliminary observations indicate that CPN membrane excitability is increased in R6/2 mice as early as P7, the earliest age we examined. Indeed, blockade of GABAA receptors with BIC induced paroxysmal discharges more often in CPNs (4 out of 8) from HD mice but not in CPNs (1 out of 7) from age-matched WT littermates. Furthermore, concurrent application of BIC and 4-AP generated ictal-like activity in R6/2 CPNs, but not in WT CPNs (Fig. 1B). These observations are consistent with our previous study demonstrating the higher occurrence of complex paroxysmal discharges in R6/2 compared with WT mice at P21 (Cummings et al., 2009), and highlight the fact that changes in cortical excitability are present even earlier during postnatal life.
Fig. 1.
A. Infrared video image of CPNs in a slice from a R6/2 mouse at P7. A normally oriented CPN was patched and recorded. The shadow of the glass electrode can be seen in the center of the image. On the left and adjacent to this cell, a misoriented CPN can be seen. This cell had the apical dendrite completely inverted (yellow arrowheads) with respect to the pial surface (arrow). B. In two different slices, CPNs from WT and R6/2 mice (P7) were recorded in current clamp mode. Bath application of BIC and 4-AP induced paroxysmal activity in both. However, while only interictal activity was seen in the WT cell, in the R6/2 cell prolonged, complex discharges resembling ictal activity were observed. C. CPNs from WT and R6/2 mice (P14) were recorded and filled with biocytin. While the WT CPN showed normal morphology, albeit still immature, the CPN from the R6/2 mouse displayed overly tortuous apical dendrite and axon (yellow arrow heads). D. In the presence of BIC, WT and R6/2 CPNs recorded in voltage clamp mode displayed large-amplitude inward currents reflecting paroxysmal discharges. The R6/2 CPN showed more frequent paroxysmal discharges compared with the WT CPN.
Morphological evidence of CPN maldevelopment also was observed during early development. Under IR-DIC microscopy we observed that some CPNs displayed misorientation, e.g., apical dendrites pointing in the wrong direction, as well as the presence of dysmorphic dendritic and axonal processes (Fig. 1A, C). While these processes extend with smooth transitions in CPNs from WT mice, in R6/2 mice some CPNs exhibit curvy, meandering dendrites and axons, suggesting that pathfinding mechanisms during fetal development had been disturbed by the presence of mHTT. At P14, signs of hyperexcitability in CPNs from R6/2 mice also were found (Fig. 1D). In R6/2 CPNs, bath application of BIC induced more frequent epileptiform discharges compared with age-matched controls.
FCD-like abnormalities occur in the cerebral cortex of R6/2 mice
The cellular morphological abnormalities observed in young R6/2 mice are reminiscent of those we found in our studies of cortical tissue samples from pediatric epilepsy surgery patients with FCD histopathology (Cepeda et al., 2003b; Abdijadid et al., 2015), suggesting that cortical maldevelopment in HD could underlie cortical hyperexcitability and seizure proclivity. According to the International League Against Epilepsy (ILAE) classification of FCD, there are at least 3 different categories (Blumcke et al., 2011; Barkovich et al., 2015). FCD type 1 is characterized by cortical dyslamination with aberrant columnar and/or radial architecture. In addition, CPN misorientation and abnormal processes can be found. FCD type 2 is defined by additional features including the presence of dysmorphic, cytomegalic neurons and in some cases also balloon cells. FCD type 3 occurs only in association with other pathologies such as tumors or hippocampal sclerosis.
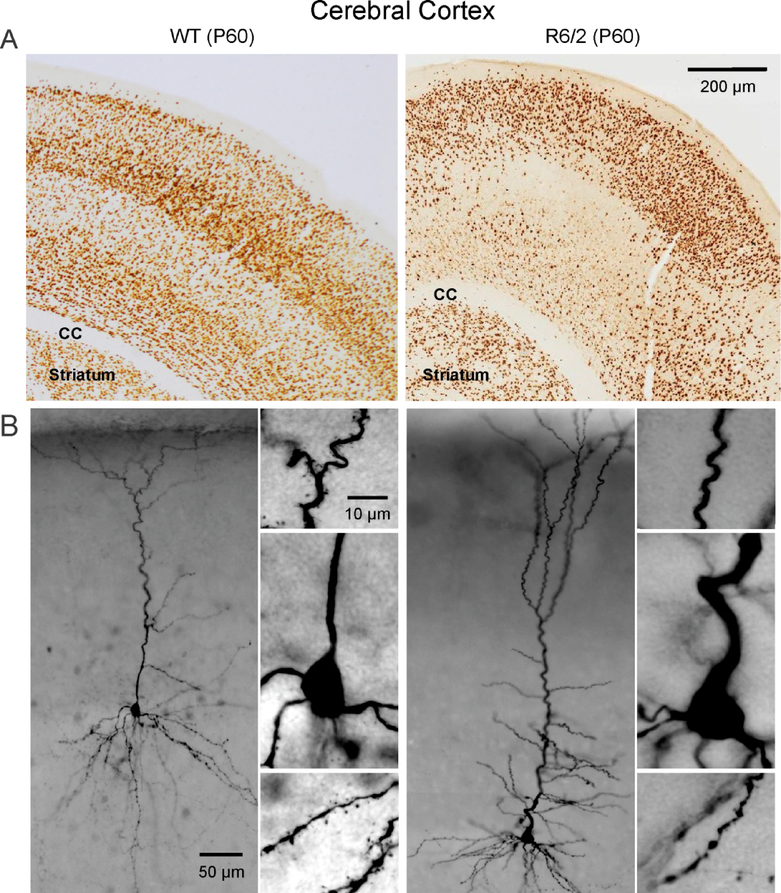
In a previous report, we speculated that one of the underlying mechanisms of cortical hyperexcitability and seizures in R6/2 mice could be a mild form of FCD, i.e., type 1 (Estrada-Sánchez et al., 2016). To test this hypothesis, we recently examined potential histopathological evidence of FCD in symptomatic R6/2 mice (age P60). We chose this age group in a first approximation because spontaneous or evoked convulsive seizures are only observed in fully symptomatic mice. Six pairs of R6/2 and control mice of either sex were perfused, sliced and stained for the specific neuronal marker, NeuN to examine cortical cytoarchitecture and CPN morphology (see Supplementary Material). Initial observations indicate that FCD-like abnormalities occur in the motor and somatosensory cortices of at least 50% of R6/2 mouse brains examined (Fig. 2A). Abnormalities include cortical dyslamination, neuronal crowding in some areas but others devoid of NeuN label, all suggesting cortical maldevelopment. In addition, biocytin staining of CPNs demonstrated the presence of abnormal processes similar to those observed in R6/2 mice at P7, including misoriented neurons, recurving dendrites and extreme meandering of axonal processes (Fig. 2B). Interestingly, in another model of HD with 100 CAG repeats we also documented the presence of misoriented CPNs as well as the common occurrence of dysmorphic dendrites (Laforet et al., 2001). These observations beg the question as to whether dysmorphic dendrites are the result of degenerative or abnormal neurodevelopmental processes.
Fig. 2.
A. WT and R6/2 mice (P60) were perfused and corticostriatal slices (30 μm thick) were processed for NeuN immunohistochemistry. The cortex of the WT mouse showed normal architecture and well delineated layers. In contrast, the cortex of the R6/2 mouse appeared dyslaminated and some areas were devoid of NeuN immunoreactivity while superficial areas showed neuronal crowding, suggestive of cortical dysplasia. B. Biocytin-filled CPNs from WT and symptomatic R6/2 mice (P80). Similar to observations in P14 R6/2 mice, some CPNs displayed overly tortuous processes. In particular, note the sharp bend of the initial segment of the apical dendrite in the R6/2 compared to the smooth, straight direction of the apical dendrite in the WT neuron. Also, fewer spines are seen in neurons from R6/2 mice compared to those from WTs.
Is HD a special case of malformations of cortical development (MCD)?
Cortical development is a delicate process that follows precise spatial and temporal rules. If, for any reason, these creodes (Waddington, 1962) are violated, the cytoarchitecture of the cortex crumbles. In particular, when CPNs terminate in ectopic positions FCD and other structural malformations ensue, leading to a growing number of neurological and psychiatric diseases (Rakic, 2006; Wu et al., 2014; Ayoub and Rakic, 2015). MCD represent a group of pathologies associated with aberrant development of the cerebral cortex and are a common etiology of epilepsy (Barkovich et al., 2015). The causes of MCD are multiple and diverse. Genetic as well as extrinsic factors play a role. As HD is a genetic disorder, we can surmise that mHTT is able to alter the rules that underlie cortical development. This is supported by experimental evidence that the presence of mHTT during embryonic development affects neuronal migration and final positioning and orientation (Osmand et al., 2016; Barnat et al., 2017).
Using Golgi impregnation of striatal neurons from HD patients, Graveland et al. described the abnormal presence of recurving terminal dendrites in MSNs (Graveland et al., 1985). Notably, the authors suggested that the high frequency of recurved dendrites may be a clue to the pathophysiology of HD. Degeneration and regeneration of CPNs from HD patients was also evinced by increases in the length of terminal branches and an overall greater branching complexity of the dendritic trees, somehow recapitulating normal brain development (Sotrel et al., 1993). Furthermore, an antibody used to detect the N-terminal region of mHTT was found in neuronal intranuclear inclusions and dystrophic neurites in the HD cortex and striatum (DiFiglia et al., 1997; Sapp et al., 1999). Dystrophic neurites, likely corresponding to distended axon terminals, were more prevalent in deep cortical layers and because they could be seen in a presymptomatic adult patient it was suggested that they precede clinical onset (DiFiglia et al., 1997). Morphological changes in the cerebral cortex include enlargement of gyral crowns and abnormally thin sulci (Paulsen et al., 2006; Nopoulos et al., 2007). Interestingly, enlargement of cortical gyri also is observed in some FCD types (Blumcke et al., 2011). Cortical thinning and white matter loss are common in pre-manifest HD subjects (Reading et al., 2005; Rosas et al., 2005; Rosas et al., 2006; Aylward, 2007; Waldvogel et al., 2015). Notably, smaller intracranial volumes in prodromal HD patients indicate that mHTT can cause abnormal brain development (Nopoulos et al., 2011). Interestingly, smaller intracranial volumes can be associated with cerebellar enlargement, which could explain hypokinesia in JHD (Tereshchenko et al., 2019). Thus, HD therapies have to take into account that the goal is not only to prevent neurodegeneration in a susceptible brain but also to correct aberrant development.
Targeting cortical maldevelopment as a new strategy for the treatment of HD
There is an almost universal consensus that, in order to treat HD symptoms, interventions should start early. The question is how early? Based on the previous review of the literature and recent morphological and electrophysiological data in very young R6/2 mice, it appears that only by targeting early brain development can any treatment be successful. So the question becomes, can cortical maldevelopment be rescued? Using human HD induced pluripotent stem cell cultures it was demonstrated that the presence of mHTT negatively affects striatal and cortical neuronal progenitor specification and commitment leading to abnormal cell organization and acquisition of mature neuronal identities in cerebral organoids (Conforti et al., 2018). Notably, these defects could be rescued by down-regulating mHTT with synthetic Zinc Finger Proteins or pharmacologically by inhibiting the metalloproteinase ADAM10, which is a mHTT effector. Another study showed that very early behavioral, cellular and molecular changes associated with the presence of mHTT can be reverted through administration of HDAC inhibitors (Siebzehnrubl et al., 2018). Finally, a recent study using a disease-on-a-chip microfluidic platform to examine the corticostriatal network in vitro, provided further evidence that cortical alterations are critical to the progression of the disease (Virlogeux et al., 2018). Further, substitution of HD cortical neurons with wildtype neurons was sufficient to rescue cellular alterations in mutant striatal neurons. Although we are still far from using these experimental approaches in human patients, these results offer a glimmer of hope.
Conclusions, future studies and some unanswered questions
Based on this review of the literature, as well as some preliminary data, we can conclude that brain development is altered in the most severe form of HD, i.e., JHD, where there is strong evidence of cortical maldevelopment, similar to FCD. However, more anatomical studies using neuron-specific markers in younger animals are warranted so as to determine when the first manifestations of cortical malformation occur. In that sense, studies using cortical layer-specific markers will help a better understanding of CPN malpositioning. Future studies should also consider potential sex differences of cortical development in genetic models of HD. For example, it has been shown that the pattern of structural brain changes associated with normal HTT is remarkably different between normal male and female school-age children. Thus, within the normal range of CAG repeats (<36), cortical thickness and cognitive function were directly correlated with higher number of repeats in females but not in males (Lee et al., 2017).
Another important question for future studies is how cortical maldevelopment and hyperexcitability in HD mice affect corticostriatal synapses and MSN function. Recent studies have shown that during a critical period of mouse brain development (P10–18) corticostriatal connectivity is extremely sensitive to changes in cortical activity, suggesting that early imbalances in cortical function can impair basal ganglia circuit development (Peixoto et al., 2016). Thus, we predict that altered excitatory/inhibitory balance in the cerebral cortex of HD mice will induce early changes in striatal neurons due to abnormal activity along the corticostriatal pathway. Initial support for this assumption was provided using a striatal and cortical co-culture system. As early as three weeks in vitro differences in striatal MSNs were observed, including reduced frequency of spontaneous EPSCs as well as reduced dendritic complexity (Buren et al., 2016).
Another still unresolved question is whether GABAergic interneuron fate and positioning in the cerebral cortex are affected by the HD mutation. In addition, as mHTT is also abundant in striatum, it would be important to know if striatal compartmental organization, i.e., striosome and matrix, is affected. For example, studies have shown that reduced expression of wildtype HTT during development can induce profound changes in striatal organization, including heterotopias that share striosome and matrix identities (Arteaga-Bracho et al., 2016). Finally, circuit organization in brain stem and thalamic regions, such as the inferior colliculus, should be examined to determine if abnormal development could explain the exquisite susceptibility of R6/2 mice to manifest audiogenic seizures.
A last point to consider is whether cortical maldeveloment is a general feature of HD or is only applicable to the more severe forms. At the present time it would be premature to generalize findings from JHD to adult-onset HD. However, recent morphological evidence obtained from a group of pre-manifest adult-onset HD patients, showed that the HTT mutation may indeed influence cortical neurodevelopment, although this seemed to be independent from processes leading to neurodegeneration (Kubera et al., 2019). In addition, based on the fact that in adult-onset HD the cortex also shows hyperexcitablity, we could speculate that cortical development could be altered and that its manifestations are delayed or mitigated by compensatory mechanisms. For example, in presymptomatic (P21) and early symptomatic (P40) R6/2 mice the frequency of spontaneous IPSCs is increased in CPNs compared with WTs (Cummings et al., 2009). In addition, at P21, some cells displayed a bursting pattern of large-amplitude IPSCs. This could suggest that the intrinsic firing properties of cortical GABAergic interneurons are altered in mouse models of HD, resulting in an increased inhibitory drive onto CPNs. This upregulation of GABA activity could prevent early manifestation of HD symptoms. However, with disease progression this compensatory mechanism is no longer sufficient to prevent cortical hyperexcitability and eventual cell loss. Thus, in addition to targeting cortical maldevelopment, reinforcing cortical inhibition represents another valid strategy for therapeutic intervention.
Supplementary Material
Acknowledgments
The authors would like to thank members of the Levine/Cepeda laboratory, in particular Dr. Sandra M. Holley, for fruitful discussions and suggestions. This work was funded by USPHS grant NS111316 (CC).
Footnotes
Conflict of Interest
The authors declare they do not have any conflicts of interest, financial or otherwise.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Abbruzzese G, Buccolieri A, Marchese R, Trompetto C, Mandich P, Schieppati M (1997) Intracortical inhibition and facilitation are abnormal in Huntington’s disease: a paired magnetic stimulation study. Neurosci Lett 228:87–90. [DOI] [PubMed] [Google Scholar]
- Abdijadid S, Mathern GW, Levine MS, Cepeda C (2015) Basic mechanisms of epileptogenesis in pediatric cortical dysplasia. CNS Neurosci Ther 21:92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal S, Koch G, Hillis AE, Huynh W, Ward NS, Vucic S, Kiernan MC (2019) Interrogating cortical function with transcranial magnetic stimulation: insights from neurodegenerative disease and stroke. J Neurol Neurosurg Psychiatry 90:47–57. [DOI] [PubMed] [Google Scholar]
- Andrew SE, Goldberg YP, Kremer B, Telenius H, Theilmann J, Adam S, Starr E, Squitieri F, Lin B, Kalchman MA, et al. (1993) The relationship between trinucleotide (CAG) repeat length and clinical features of Huntington’s disease. Nat Genet 4:398–403. [DOI] [PubMed] [Google Scholar]
- Arteaga-Bracho EE, Gulinello M, Winchester ML, Pichamoorthy N, Petronglo JR, Zambrano AD, Inocencio J, De Jesus CD, Louie JO, Gokhan S, Mehler MF, Molero AE (2016) Postnatal and adult consequences of loss of huntingtin during development: Implications for Huntington’s disease. Neurobiol Dis 96:144–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aylward EH (2007) Change in MRI striatal volumes as a biomarker in preclinical Huntington’s disease. Brain Res Bull 72:152–158. [DOI] [PubMed] [Google Scholar]
- Ayoub AE, Rakic P (2015) Neuronal misplacement in schizophrenia. Biol Psychiatry 77:925–926. [DOI] [PubMed] [Google Scholar]
- Barkovich AJ, Dobyns WB, Guerrini R (2015) Malformations of cortical development and epilepsy. Cold Spring Harb Perspect Med 5:a022392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnat M, Le Friec J, Benstaali C, Humbert S (2017) Huntingtin-Mediated Multipolar-Bipolar Transition of Newborn Cortical Neurons Is Critical for Their Postnatal Neuronal Morphology. Neuron 93:99–114. [DOI] [PubMed] [Google Scholar]
- Bates G, Harper PS, Jones L (2002) Huntington’s disease, 3rd Edition. Oxford; New York: Oxford University Press. [Google Scholar]
- Berardelli A, Suppa A (2013) Noninvasive brain stimulation in Huntington’s disease. Handbook of clinical neurology 116:555–560. [DOI] [PubMed] [Google Scholar]
- Blockx I, De Groof G, Verhoye M, Van Audekerke J, Raber K, Poot D, Sijbers J, Osmand AP, Von Horsten S, Van der Linden A (2012) Microstructural changes observed with DKI in a transgenic Huntington rat model: evidence for abnormal neurodevelopment. Neuroimage 59:957–967. [DOI] [PubMed] [Google Scholar]
- Blumcke I et al. (2011) The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia 52:158–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brusa L, Versace V, Koch G, Bernardi G, Iani C, Stanzione P, Centonze D (2005) Improvement of choreic movements by 1 Hz repetitive transcranial magnetic stimulation in Huntington’s disease patients. Ann Neurol 58:655–656. [DOI] [PubMed] [Google Scholar]
- Buren C, Parsons MP, Smith-Dijak A, Raymond LA (2016) Impaired development of corticostriatal synaptic connectivity in a cell culture model of Huntington’s disease. Neurobiol Dis 87:80–90. [DOI] [PubMed] [Google Scholar]
- Burgold J, Schulz-Trieglaff EK, Voelkl K, Gutierrez-Angel S, Bader JM, Hosp F, Mann M, Arzberger T, Klein R, Liebscher S, Dudanova I (2019) Cortical circuit alterations precede motor impairments in Huntington’s disease mice. Scientific reports 9:6634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda C, Hurst RS, Calvert CR, Hernandez-Echeagaray E, Nguyen OK, Jocoy E, Christian LJ, Ariano MA, Levine MS (2003a) Transient and progressive electrophysiological alterations in the corticostriatal pathway in a mouse model of Huntington’s disease. J Neurosci 23:961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda C, Hurst RS, Flores-Hernandez J, Hernandez-Echeagaray E, Klapstein GJ, Boylan MK, Calvert CR, Jocoy EL, Nguyen OK, Andre VM, Vinters HV, Ariano MA, Levine MS, Mathern GW (2003b) Morphological and electrophysiological characterization of abnormal cell types in pediatric cortical dysplasia. J Neurosci Res 72:472–486. [DOI] [PubMed] [Google Scholar]
- Conforti P, Besusso D, Bocchi VD, Faedo A, Cesana E, Rossetti G, Ranzani V, Svendsen CN, Thompson LM, Toselli M, Biella G, Pagani M, Cattaneo E (2018) Faulty neuronal determination and cell polarization are reverted by modulating HD early phenotypes. Proc Natl Acad Sci U S A 115:E762–E771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consortium THi(2017) Developmental alterations in Huntington’s disease neural cells and pharmacological rescue in cells and mice. Nat Neurosci 20:648–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings DM, Milnerwood AJ, Dallérac GM, Vatsavayai SC, Hirst MC, Murphy KPSJ(2007) Abnormal Cortical Synaptic Plasticity in Mice Transgenic for Exon 1 of the Human Huntington’s Disease Mutation. Brain Res Bul 72:103–107. [DOI] [PubMed] [Google Scholar]
- Cummings DM, Andre VM, Uzgil BO, Gee SM, Fisher YE, Cepeda C, Levine MS (2009) Alterations in cortical excitation and inhibition in genetic mouse models of Huntington’s disease. J Neurosci 29:10371–10386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings DM, Milnerwood AJ, Dallerac GM, Waights V, Brown JY, Vatsavayai SC, Hirst MC, Murphy KP (2006) Aberrant cortical synaptic plasticity and dopaminergic dysfunction in a mouse model of huntington’s disease. Hum Mol Genet 15:2856–2868. [DOI] [PubMed] [Google Scholar]
- Cummings DM, Alaghband Y, Hickey MA, Joshi PR, Hong SC, Zhu C, Ando TK, Andre VM, Cepeda C, Watson JB, Levine MS (2012) A critical window of CAG repeat-length correlates with phenotype severity in the R6/2 mouse model of Huntington’s disease. J Neurophysiol 107:677–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cybulska-Klosowicz A, Mazarakis NK, Van Dellen A, Blakemore C, Hannan AJ, Kossut M (2004) Impaired learning-dependent cortical plasticity in Huntington’s disease transgenic mice. Neurobiol Dis 17:427–434. [DOI] [PubMed] [Google Scholar]
- Dallerac GM, Vatsavayai SC, Cummings DM, Milnerwood AJ, Peddie CJ, Evans KA, Walters SW, Rezaie P, Hirst MC, Murphy KP (2011) Impaired long-term potentiation in the prefrontal cortex of Huntington’s disease mouse models: rescue by D1 dopamine receptor activation. Neurodegener Dis 8:230–239. [DOI] [PubMed] [Google Scholar]
- Dautan D, Souza AS, Huerta-Ocampo I, Valencia M, Assous M, Witten IB, Deisseroth K, Tepper JM, Bolam JP, Gerdjikov TV, Mena-Segovia J (2016) Segregated cholinergic transmission modulates dopamine neurons integrated in distinct functional circuits. Nat Neurosci 19:1025–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng YP, Wong T, Bricker-Anthony C, Deng B, Reiner A (2013) Loss of corticostriatal and thalamostriatal synaptic terminals precedes striatal projection neuron pathology in heterozygous Q140 Huntington’s disease mice. Neurobiol Dis 60:89–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFiglia M (1990) Excitotoxic injury of the neostriatum: a model for Huntington’s disease. Trends Neurosci 13:286–289. [DOI] [PubMed] [Google Scholar]
- DiFiglia M, Sapp E, Chase KO, Davies SW, Bates GP, Vonsattel JP, Aronin N (1997) Aggregation of huntingtin in neuronal intranuclear inclusions and dystrophic neurites in brain. Science 277:1990–1993. [DOI] [PubMed] [Google Scholar]
- Dragatsis I, Dietrich P, Ren H, Deng YP, Del Mar N, Wang HB, Johnson IM, Jones KR, Reiner A (2017) Effect of early embryonic deletion of huntingtin from pyramidal neurons on the development and long-term survival of neurons in cerebral cortex and striatum. Neurobiol Dis 111:102–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durieux PF, Schiffmann SN, de Kerchove d’Exaerde A (2011) Targeting neuronal populations of the striatum. Front Neuroanat 5:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duyao MP, Auerbach AB, Ryan A, Persichetti F, Barnes GT, McNeil SM, Ge P, Vonsattel JP, Gusella JF, Joyner AL, et al. (1995) Inactivation of the mouse Huntington’s disease gene homolog Hdh. Science 269:407–410. [DOI] [PubMed] [Google Scholar]
- Estrada-Sanchez AM, Rebec GV (2013) Role of cerebral cortex in the neuropathology of Huntington’s disease. Frontiers in neural circuits 7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada-Sanchez AM, Burroughs CL, Cavaliere S, Barton SJ, Chen S, Yang XW, Rebec GV (2015) Cortical efferents lacking mutant huntingtin improve striatal neuronal activity and behavior in a conditional mouse model of Huntington’s disease. J Neurosci 35:4440–4451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada-Sánchez AM, Levine MS, Cepeda C (2016) Epilepsy in other neurodegenerative disorders: Huntington’s and Parkinson’s diseases In: Models of seizures and epilepsy 2nd Edition (Pitkänen ABP, Galanopoulou AS, Moshé SLed), pp 1043–1058: Elsevier Inc. [Google Scholar]
- Gambardella A, Muglia M, Labate A, Magariello A, Gabriele AL, Mazzei R, Pirritano D, Conforti FL, Patitucci A, Valentino P, Zappia M, Quattrone A (2001) Juvenile Huntington’s disease presenting as progressive myoclonic epilepsy. Neurology 57:708–711. [DOI] [PubMed] [Google Scholar]
- Godin JD, Colombo K, Molina-Calavita M, Keryer G, Zala D, Charrin BC, Dietrich P, Volvert ML, Guillemot F, Dragatsis I, Bellaiche Y, Saudou F, Nguyen L, Humbert S (2010) Huntingtin is required for mitotic spindle orientation and mammalian neurogenesis. Neuron 67:392–406. [DOI] [PubMed] [Google Scholar]
- Graveland GA, Williams RS, DiFiglia M (1985) Evidence for degenerative and regenerative changes in neostriatal spiny neurons in Huntington’s disease. Science 227:770–773. [DOI] [PubMed] [Google Scholar]
- Gray M, Shirasaki DI, Cepeda C, Andre VM, Wilburn B, Lu XH, Tao J, Yamazaki I, Li SH, Sun YE, Li XJ, Levine MS, Yang XW (2008) Full-length human mutant huntingtin with a stable polyglutamine repeat can elicit progressive and selective neuropathogenesis in BACHD mice. J Neurosci 28:6182–6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu X, Li C, Wei W, Lo V, Gong S, Li SH, Iwasato T, Itohara S, Li XJ, Mody I, Heintz N, Yang XW (2005) Pathological cell-cell interactions elicited by a neuropathogenic form of mutant Huntingtin contribute to cortical pathogenesis in HD mice. Neuron 46:433–444. [DOI] [PubMed] [Google Scholar]
- Harper PS, Jones L (2002) Huntington’s disease: Genetic and molecular studies In: Huntington’s Disease, Third Edition (Bates GP, Harper PS, Jones L, eds), pp 113–158. Oxford: Oxford University Press. [Google Scholar]
- Huerta-Ocampo I, Mena-Segovia J, Bolam JP (2014) Convergence of cortical and thalamic input to direct and indirect pathway medium spiny neurons in the striatum. Brain structure & function 219:1787–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunnicutt BJ, Jongbloets BC, Birdsong WT, Gertz KJ, Zhong H, Mao T (2016) A comprehensive excitatory input map of the striatum reveals novel functional organization. eLife 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi PR, Wu NP, Andre VM, Cummings DM, Cepeda C, Joyce JA, Carroll JB, Leavitt BR, Hayden MR, Levine MS, Bamford NS (2009) Age-dependent alterations of corticostriatal activity in the YAC128 mouse model of Huntington disease. J Neurosci 29:2414–2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodziejczyk K, Raymond LA (2016) Differential changes in thalamic and cortical excitatory synapses onto striatal spiny projection neurons in a Huntington disease mouse model. Neurobiol Dis 86:62–74. [DOI] [PubMed] [Google Scholar]
- Kubera KM, Schmitgen MM, Hirjak D, Wolf RC, Orth M (2019) Cortical neurodevelopment in pre-manifest Huntington’s disease. NeuroImage: Clinical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laforet GA, Sapp E, Chase K, McIntyre C, Boyce FM, Campbell M, Cadigan BA, Warzecki L, Tagle DA, Reddy PH, Cepeda C, Calvert CR, Jokel ES, Klapstein GJ, Ariano MA, Levine MS, DiFiglia M, Aronin N (2001) Changes in cortical and striatal neurons predict behavioral and electrophysiological abnormalities in a transgenic murine model of Huntington’s disease. J Neurosci 21:9112–9123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence AD, Sahakian BJ, Hodges JR, Rosser AE, Lange KW, Robbins TW (1996) Executive and mnemonic functions in early Huntington’s disease. Brain 119 (Pt 5):1633–1645. [DOI] [PubMed] [Google Scholar]
- Lawrence AD, Hodges JR, Rosser AE, Kershaw A, ffrench-Constant C, Rubinsztein DC, Robbins TW, Sahakian BJ (1998) Evidence for specific cognitive deficits in preclinical Huntington’s disease. Brain 121 (Pt 7):1329–1341. [DOI] [PubMed] [Google Scholar]
- Lee JK, Ding Y, Conrad AL, Cattaneo E, Epping E, Mathews K, Gonzalez-Alegre P, Cahill L, Magnotta V, Schlaggar BL, Perlmutter JS, Kim RE, Dawson JD, Nopoulos P (2017) Sex-specific effects of the Huntington gene on normal neurodevelopment. J Neurosci Res 95:398–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letort D, Gonzalez-Alegre P (2013) Huntington’s disease in children. Handb Clin Neurol 113:1913–1917. [DOI] [PubMed] [Google Scholar]
- Mangiarini L, Sathasivam K, Seller M, Cozens B, Harper A, Hetherington C, Lawton M, Trottier Y, Lehrach H, Davies SW, Bates GP (1996) Exon 1 of the HD gene with an expanded CAG repeat is sufficient to cause a progressive neurological phenotype in transgenic mice. Cell 87:493–506. [DOI] [PubMed] [Google Scholar]
- Mattis VB, Tom C, Akimov S, Saeedian J, Ostergaard ME, Southwell AL, Doty CN, Ornelas L, Sahabian A, Lenaeus L, Mandefro B, Sareen D, Arjomand J, Hayden MR, Ross CA, Svendsen CN (2015) HD iPSC-derived neural progenitors accumulate in culture and are susceptible to BDNF withdrawal due to glutamate toxicity. Hum Mol Genet 24:3257–3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazarakis NK, Cybulska-Klosowicz A, Grote H, Pang T, Van Dellen A, Kossut M, Blakemore C, Hannan AJ (2005) Deficits in experience-dependent cortical plasticity and sensory-discrimination learning in presymptomatic Huntington’s disease mice. J Neurosci 25:3059–3066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinstry SU, Karadeniz YB, Worthington AK, Hayrapetyan VY, Ozlu MI, Serafin-Molina K, Risher WC, Ustunkaya T, Dragatsis I, Zeitlin S, Yin HH, Eroglu C (2014) Huntingtin is required for normal excitatory synapse development in cortical and striatal circuits. J Neurosci 34:9455–9472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CA, Deng YP, Fusco FR, Del Mar N, Hersch S, Goldowitz D, Reiner A (2002) Cellular localization and development of neuronal intranuclear inclusions in striatal and cortical neurons in R6/2 transgenic mice. J Comp Neurol 449:241–269. [DOI] [PubMed] [Google Scholar]
- Mehler MF, Petronglo JR, Arteaga-Bracho EE, Gulinello ME, Winchester ML, Pichamoorthy N, Young SK, DeJesus CD, Ishtiaq H, Gokhan S, Molero AE (2019) Loss-of-Huntingtin in Medial and Lateral Ganglionic Lineages Differentially Disrupts Regional Interneuron and Projection Neuron Subtypes and Promotes Huntington’s Disease-Associated Behavioral, Cellular, and Pathological Hallmarks. J Neurosci 39:1892–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milnerwood AJ, Gladding CM, Pouladi MA, Kaufman AM, Hines RM, Boyd JD, Ko RW, Vasuta OC, Graham RK, Hayden MR, Murphy TH, Raymond LA (2010) Early increase in extrasynaptic NMDA receptor signaling and expression contributes to phenotype onset in Huntington’s disease mice. Neuron 65:178–190. [DOI] [PubMed] [Google Scholar]
- Molero AE, Arteaga-Bracho EE, Chen CH, Gulinello M, Winchester ML, Pichamoorthy N, Gokhan S, Khodakhah K, Mehler MF (2016) Selective expression of mutant huntingtin during development recapitulates characteristic features of Huntington’s disease. Proc Natl Acad Sci U S A 113:5736–5741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina-Calavita M, Barnat M, Elias S, Aparicio E, Piel M, Humbert S (2014) Mutant huntingtin affects cortical progenitor cell division and development of the mouse neocortex. J Neurosci 34:10034–10040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton AJ, Lagan MA, Skepper JN, Dunnett SB (2000) Progressive formation of inclusions in the striatum and hippocampus of mice transgenic for the human Huntington’s disease mutation. J Neurocytol 29:679–702. [DOI] [PubMed] [Google Scholar]
- Nardone R, Lochner P, Marth R, Ausserer H, Bratti A, Tezzon F (2007) Abnormal intracortical facilitation in early-stage Huntington’s disease. Clin Neurophysiol 118:1149–1154. [DOI] [PubMed] [Google Scholar]
- Nasir J, Floresco SB, O’Kusky JR, Diewert VM, Richman JM, Zeisler J, Borowski A, Marth JD, Phillips AG, Hayden MR (1995) Targeted disruption of the Huntington’s disease gene results in embryonic lethality and behavioral and morphological changes in heterozygotes. Cell 81:811–823. [DOI] [PubMed] [Google Scholar]
- Nopoulos P, Magnotta VA, Mikos A, Paulson H, Andreasen NC, Paulsen JS (2007) Morphology of the cerebral cortex in preclinical Huntington’s disease. The American journal of psychiatry 164:1428–1434. [DOI] [PubMed] [Google Scholar]
- Nopoulos PC, Aylward EH, Ross CA, Mills JA, Langbehn DR, Johnson HJ, Magnotta VA, Pierson RK, Beglinger LJ, Nance MA, Barker RA, Paulsen JS, Investigators P-H, Coordinators of the Huntington Study G (2011) Smaller intracranial volume in prodromal Huntington’s disease: evidence for abnormal neurodevelopment. Brain 134:137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto S, Pouladi MA, Talantova M, Yao D, Xia P, Ehrnhoefer DE, Zaidi R, Clemente A, Kaul M, Graham RK, Zhang D, Vincent Chen HS, Tong G, Hayden MR, Lipton SA (2009) Balance between synaptic versus extrasynaptic NMDA receptor activity influences inclusions and neurotoxicity of mutant huntingtin. Nat Med 15:1407–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orth M, Schippling S, Schneider SA, Bhatia KP, Talelli P, Tabrizi SJ, Rothwell JC (2010) Abnormal motor cortex plasticity in premanifest and very early manifest Huntington disease. J Neurol Neurosurg Psychiatry 81:267–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osmand AP, Bichell TJ, Bowman AB, Bates GP (2016) Embryonic Mutant Huntingtin Aggregate Formation in Mouse Models of Huntington’s Disease. J Huntingtons Dis 5:343–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parievsky A, Moore C, Kamdjou T, Cepeda C, Meshul CK, Levine MS (2017) Differential electrophysiological and morphological alterations of thalamostriatal and corticostriatal projections in the R6/2 mouse model of Huntington’s disease. Neurobiol Dis 108:29–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulsen JS, Magnotta VA, Mikos AE, Paulson HL, Penziner E, Andreasen NC, Nopoulos PC (2006) Brain structure in preclinical Huntington’s disease. Biol Psychiatry 59:57–63. [DOI] [PubMed] [Google Scholar]
- Peixoto RT, Wang W, Croney DM, Kozorovitskiy Y, Sabatini BL (2016) Early hyperactivity and precocious maturation of corticostriatal circuits in Shank3B(−/−) mice. Nat Neurosci 19:716–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penney JB Jr., Vonsattel JP, MacDonald ME, Gusella JF, Myers RH(1997) CAG repeat number governs the development rate of pathology in Huntington’s disease. Ann Neurol 41:689–692. [DOI] [PubMed] [Google Scholar]
- Philpott AL, Cummins TDR, Bailey NW, Churchyard A, Fitzgerald PB, Georgiou-Karistianis N (2016) Cortical inhibitory deficits in premanifest and early Huntington’s disease. Behav Brain Res 296:311–317. [DOI] [PubMed] [Google Scholar]
- Rakic P (2006) A century of progress in corticoneurogenesis: from silver impregnation to genetic engineering. Cereb Cortex 16 Suppl 1:i3–17. [DOI] [PubMed] [Google Scholar]
- Rasmussen A, Macias R, Yescas P, Ochoa A, Davila G, Alonso E (2000) Huntington disease in children: genotype-phenotype correlation. Neuropediatrics 31:190–194. [DOI] [PubMed] [Google Scholar]
- Raymond LA, André VM, Cepeda C, Gladding CM, Milnerwood AJ, Levine MS (2011) Pathophysiology of Huntington’s disease: time-dependent alterations in synaptic and receptor function. Neuroscience. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reading SA, Yassa MA, Bakker A, Dziorny AC, Gourley LM, Yallapragada V, Rosenblatt A, Margolis RL, Aylward EH, Brandt J, Mori S, van Zijl P, Bassett SS, Ross CA (2005) Regional white matter change in pre-symptomatic Huntington’s disease: a diffusion tensor imaging study. Psychiatry Res 140:55–62. [DOI] [PubMed] [Google Scholar]
- Reiner A, Shelby E, Wang H, Demarch Z, Deng Y, Guley NH, Hogg V, Roxburgh R, Tippett LJ, Waldvogel HJ, Faull RL (2013) Striatal parvalbuminergic neurons are lost in Huntington’s disease: implications for dystonia. Mov Disord 28:1691–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosas HD, Hevelone ND, Zaleta AK, Greve DN, Salat DH, Fischl B (2005) Regional cortical thinning in preclinical Huntington disease and its relationship to cognition. Neurology 65:745–747. [DOI] [PubMed] [Google Scholar]
- Rosas HD, Tuch DS, Hevelone ND, Zaleta AK, Vangel M, Hersch SM, Salat DH (2006) Diffusion tensor imaging in presymptomatic and early Huntington’s disease: Selective white matter pathology and its relationship to clinical measures. Mov Disord 21:1317–1325. [DOI] [PubMed] [Google Scholar]
- Sapp E, Penney J, Young A, Aronin N, Vonsattel JP, DiFiglia M (1999) Axonal transport of Nterminal huntingtin suggests early pathology of corticostriatal projections in Huntington disease. J Neuropathol Exp Neurol 58:165–173. [DOI] [PubMed] [Google Scholar]
- Saudou F, Humbert S (2016) The Biology of Huntingtin. Neuron 89:910–926. [DOI] [PubMed] [Google Scholar]
- Schippling S, Schneider SA, Bhatia KP, Munchau A, Rothwell JC, Tabrizi SJ, Orth M (2009) Abnormal motor cortex excitability in preclinical and very early Huntington’s disease. Biol Psychiatry 65:959–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seneca S, Fagnart D, Keymolen K, Lissens W, Hasaerts D, Debulpaep S, Desprechins B, Liebaers I, De Meirleir L (2004) Early onset Huntington disease: a neuronal degeneration syndrome. Eur J Pediatr 163:717–721. [DOI] [PubMed] [Google Scholar]
- Siebzehnrubl FA et al. (2018) Early postnatal behavioral, cellular, and molecular changes in models of Huntington disease are reversible by HDAC inhibition. Proc Natl Acad Sci U S A 115:E8765–E8774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slow EJ, van Raamsdonk J, Rogers D, Coleman SH, Graham RK, Deng Y, Oh R, Bissada N, Hossain SM, Yang YZ, Li XJ, Simpson EM, Gutekunst CA, Leavitt BR, Hayden MR (2003) Selective striatal neuronal loss in a YAC128 mouse model of Huntington disease. Hum Mol Genet 12:1555–1567. [DOI] [PubMed] [Google Scholar]
- Smith Y, Galvan A, Ellender TJ, Doig N, Villalba RM, Huerta-Ocampo I, Wichmann T, Bolam JP (2014) The thalamostriatal system in normal and diseased states. Front Syst Neurosci 8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotrel A, Williams RS, Kaufmann WE, Myers RH (1993) Evidence for neuronal degeneration and dendritic plasticity in cortical pyramidal neurons of Huntington’s disease: a quantitative Golgi study. Neurology 43:2088–2096. [DOI] [PubMed] [Google Scholar]
- Spampanato J, Gu X, Yang XW, Mody I (2008) Progressive synaptic pathology of motor cortical neurons in a BAC transgenic mouse model of Huntington’s disease. Neuroscience 157:606–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack EC, Dedeoglu A, Smith KM, Cormier K, Kubilus JK, Bogdanov M, Matson WR, Yang L, Jenkins BG, Luthi-Carter R, Kowall NW, Hersch SM, Beal MF, Ferrante RJ (2007) Neuroprotective effects of synaptic modulation in Huntington’s disease R6/2 mice. J Neurosci 27:12908–12915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern EA (2011) Functional Changes in Neocortical Activity in Huntington’s Disease Model Mice: An in vivo Intracellular Study. Front Syst Neurosci 5:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DC, Falconer MA, Bruton CJ, Corsellis JA (1971) Focal dysplasia of the cerebral cortex in epilepsy. J Neurol Neurosurg Psychiatry 34:369–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telenius H, Kremer HP, Theilmann J, Andrew SE, Almqvist E, Anvret M, Greenberg C, Greenberg J, Lucotte G, Squitieri F, et al. (1993) Molecular analysis of juvenile Huntington disease: the major influence on (CAG)n repeat length is the sex of the affected parent. Hum Mol Genet 2:1535–1540. [DOI] [PubMed] [Google Scholar]
- Tereshchenko A, Magnotta V, Epping E, Mathews K, Espe-Pfeifer P, Martin E, Dawson J, Duan W, Nopoulos P (2019) Brain structure in juvenile-onset Huntington disease. Neurology 92:e1939–e1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Huntington’s Disease Collaborative Research Group (1993) A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell 72:971–983. [DOI] [PubMed] [Google Scholar]
- Thu DC, Oorschot DE, Tippett LJ, Nana AL, Hogg VM, Synek BJ, Luthi-Carter R, Waldvogel HJ, Faull RL (2010) Cell loss in the motor and cingulate cortex correlates with symptomatology in Huntington’s disease. Brain 133:1094–1110. [DOI] [PubMed] [Google Scholar]
- Virlogeux A, Moutaux E, Christaller W, Genoux A, Bruyere J, Fino E, Charlot B, Cazorla M, Saudou F (2018) Reconstituting Corticostriatal Network on-a-Chip Reveals the Contribution of the Presynaptic Compartment to Huntington’s Disease. Cell reports 22:110–122. [DOI] [PubMed] [Google Scholar]
- Vonsattel JP, DiFiglia M (1998) Huntington disease. J Neuropathol Exp Neurol 57:369–384. [DOI] [PubMed] [Google Scholar]
- Waddington CH (1962) The Nature of Life. New York: Athenum. [Google Scholar]
- Waldvogel HJ, Kim EH, Tippett LJ, Vonsattel JP, Faull RL (2015) The Neuropathology of Huntington’s Disease. Current topics in behavioral neurosciences 22:33–80. [DOI] [PubMed] [Google Scholar]
- Walker AG, Miller BR, Fritsch JN, Barton SJ, Rebec GV (2008) Altered information processing in the prefrontal cortex of Huntington’s disease mouse models. J Neurosci 28:8973–8982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang N, Gray M, Lu XH, Cantle JP, Holley SM, Greiner E, Gu X, Shirasaki D, Cepeda C, Li Y, Dong H, Levine MS, Yang XW (2014) Neuronal targets for reducing mutant huntingtin expression to ameliorate disease in a mouse model of Huntington’s disease. Nat Med 20:536–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiatr K, Szlachcic WJ, Trzeciak M, Figlerowicz M, Figiel M (2017) Huntington Disease as a Neurodevelopmental Disorder and Early Signs of the Disease in Stem Cells. Mol Neurobiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Q, Liu J, Fang A, Li R, Bai Y, Kriegstein AR, Wang X (2014) The dynamics of neuronal migration. Advances in experimental medicine and biology 800:25–36. [DOI] [PubMed] [Google Scholar]
- Zeitlin S, Liu JP, Chapman DL, Papaioannou VE, Efstratiadis A (1995) Increased apoptosis and early embryonic lethality in mice nullizygous for the Huntington’s disease gene homologue. Nat Genet 11:155–163. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.