Abstract
Background
Cardiac arrest in hospitalized children is associated with poor outcomes, but no contemporary study has reported whether trends in survival have changed over time. In this study, we examined temporal trends in survival for pediatric patients with an in-hospital pulseless cardiac arrest and pediatric patients with a non-pulseless cardiopulmonary resuscitation event from 2000 to 2018.
Methods
This was an observational study of hospitalized pediatric patients (≤18 years of age) who received cardiopulmonary resuscitation from January 2000 to December 2018 and were included in the Get With The Guidelines®-Resuscitation registry, a US-based in-hospital cardiac arrest registry. The primary outcome was survival to hospital discharge and the secondary outcome was return of spontaneous circulation (binary outcomes). Generalized estimation equations were used to obtain unadjusted trends in outcomes over time. Separate analyses were performed for patients with a pulseless cardiac arrest and patients with a non-pulseless event (bradycardia with poor perfusion) requiring cardiopulmonary resuscitation. A subgroup analysis was conducted for shockable vs non-shockable initial rhythms in pulseless events.
Results
A total of 7433 patients with a pulseless cardiac arrest and 5751 patients with a non-pulseless event were included for the analyses. For pulseless cardiac arrests, survival was 19% (95%CI, 11%–29%) in 2000 and 38% (95%CI, 34%–43%) in 2018, with an absolute change of 0.67% (95%CI, 0.40%–0.95%; p <0.001) per year, although the increase in survival appeared to stagnate following 2010. Return of spontaneous circulation also increased over time, with an absolute change of 0.83% (95%CI, 0.53%–1.14%; p <0.001) per year. We found no interaction between survival to hospital discharge and the initial rhythm. For non-pulseless events, survival was 57% (95%CI, 39%–75%) in 2000 and 66% (95%CI, 61%–72%) in 2018, with an absolute change of 0.80% (95%CI, 0.32%–1.27%; p = 0.001) per year.
Conclusions
Survival has improved for pediatric events requiring cardiopulmonary resuscitation in the US, with a 19% absolute increase in survival for in-hospital pulseless cardiac arrests and a 9% absolute increase in survival for non-pulseless events between 2000 and 2018. However, survival from pulseless cardiac arrests appeared to have reached a plateau following 2010.
Keywords: Survival, Trends, Pediatric, Cardiac Arrest, Heart Arrest, Pediatrics, Mortality
Introduction
Cardiopulmonary resuscitation is performed in an estimated 15,000 hospitalized pediatric patients each year in the US.1 While the mortality associated with in-hospital pulseless cardiac arrest remains high, the most recent study to examine temporal trends in survival found an unadjusted increase in survival to hospital discharge from 14% in 2000 to 39% in 20092 and a recent update from the American Heart Association reported a survival of 37% in 20173.
In 2010, the American Heart Association announced a 10-year impact goal of increasing survival to 50% for pediatric in-hospital cardiac arrests.4 The Pediatric Advanced Life Support guidelines have subsequently been updated to improve survival from cardiac arrest, most recently in 2018.5 To our knowledge, no contemporary study has examined temporal survival trends in pediatric pulseless cardiac arrest patients and there is a need to assess the progress of ongoing quality-improvement efforts.3 Additionally, there have been no reports on survival trends in pediatric patients with non-pulseless events (bradycardia with poor perfusion), which is the presenting condition in up to 55% of hospitalized pediatric patients receiving cardiopulmonary resuscitation.6, 7
In this study, we examined temporal trends in survival to hospital discharge for pediatric patients with an in-hospital pulseless cardiac arrest and pediatric patients with a non-pulseless event requiring cardiopulmonary resuscitation from 2000 to 2018.
Methods
The data, analytical methods, and study materials will be made available to other researchers for purposes of reproducing the results or replicating the procedure once required permission is obtained from the Get With The Guidelines® – Resuscitation (GWTG-R) registry.
Study Design and Data Source
This was an analysis of prospectively collected data from the GWTG-R registry. The GWTG-R registry is a large, hospital-based, quality-improvement registry of in-hospital cardiac arrests in the US, sponsored by the American Heart Association. A detailed description of the registry has been provided elsewhere.8, 9 In brief, personnel at each participating site collect data on all in-hospital cardiac arrests without a do-not-resuscitate order. Pediatric cardiac arrest is defined as the loss of a palpable central pulse at any time during the event (initial or subsequent pulseless cardiac arrest) or the presence of a pulse with bradycardia and poor perfusion throughout the entire event (non-pulseless event), requiring chest compressions, defibrillation, or both, with a hospital-wide or unit-wide emergency response. Hospital-level data were obtained from the 2013 American Hospital Association Annual Survey10 and linked to the GWTG-R registry by the American Heart Association data management vendor.
IQVA is the data collection coordination center for the American Heart Association and American Stroke Association Get With The Guidelines® programs. Institutional Review Board (IRB) approval was obtained at Beth Israel Deaconess Medical Center (Boston, MA, USA) who determined that research involving the GWTG-R registry does not meet the federal definition of human subject research. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule.
Study Population and Outcomes
We included pediatric patients (≤18 years of age) with an index in-hospital cardiac arrest reported to the GWTG-R registry between January 1, 2000 and December 31, 2018. Hospital visitors and employees were excluded from the study, as were patients with missing data for the primary outcome and covariates (Table 1 and Table 2).
Table 1.
Characteristics of pulseless cardiac arrests
| 2000–2005 (n = 1403) | 2006–2010 (n = 2288) | 2011–2015 (n = 2212) | 2016–2018 (n = 1530) | |
|---|---|---|---|---|
| Demographics | ||||
| Sex | ||||
| Male | 784 (56) | 1277 (56) | 1234 (56) | 835 (55) |
| Female | 619 (44) | 1011 (44) | 978 (44) | 695 (45) |
| Age group | ||||
| Neonate (<1 month) | 223 (16) | 797 (35) | 673 (30) | 255 (17) |
| Infant (1 month to <1 year) | 367 (26) | 525 (23) | 394 (18) | 438 (29) |
| Child (1 year to <12 years) | 470 (33) | 618 (27) | 734 (33) | 567 (37) |
| Adolescent (≥12 years) | 343 (24) | 348 (15) | 411 (19) | 270 (18) |
| Illness category | ||||
| Medical | ||||
| Cardiac | 232 (17) | 319 (14) | 336 (15) | 289 (19) |
| Non-cardiac | 593 (42) | 782 (34) | 886 (40) | 712 (47) |
| Surgical | ||||
| Cardiac | 206 (15) | 392 (17) | 378 (17) | 261 (17) |
| Non-cardiac* | 275 (20) | 370 (16) | 342 (15) | 268 (18) |
| Newborn† | 97 (7) | 425 (19) | 270 (12) | 0 (0) |
| Pre-existing conditions‡ | ||||
| Acute non-stroke CNS event | 171 (12) | 149 (7) | 130 (6) | 100 (7) |
| Baseline depression in CNS | 276 (20) | 324 (14) | 260 (12) | 223 (15) |
| Heart failure prior admission | 216 (15) | 111 (5) | 96 (4) | 78 (5) |
| Heart failure this admission | 242 (17) | 141 (6) | 124 (6) | 104 (7) |
| Hepatic insufficiency | 79 (6) | 86 (4) | 97 (4) | 84 (5) |
| Hypotension | 594 (42) | 850 (37) | 607 (27) | 471 (31) |
| Metabolic abnormalities | 292 (21) | 402 (18) | 347 (16) | 392 (26) |
| Metastatic malignancy | 65 (5) | 95 (4) | 116 (5) | 87 (6) |
| Pneumonia | 143 (10) | 155 (7) | 141 (6) | 108 (7) |
| Respiratory insufficiency | 838 (60) | 1383 (60) | 1243 (56) | 1021 (67) |
| Renal insufficiency | 162 (12) | 206 (9) | 237 (11) | 201 (13) |
| Septicemia | 225 (16) | 353 (15) | 326 (15) | 190 (12) |
| Location and Time of Event | ||||
| Location of event | ||||
| Emergency department | 219 (16) | 274 (12) | 227 (10) | 137 (9) |
| Intensive care unit | 914 (65) | 1516 (66) | 1506 (68) | 1173 (77) |
| Floor | ||||
| Without telemetry | 107 (8) | 101 (4) | 98 (4) | 76 (5) |
| With telemetry | 19 (1) | 53 (2) | 29 (1) | 16 (1) |
| Other§ | 144 (10) | 344 (15) | 352 (16) | 128 (8) |
| Time of week | ||||
| Weekend∥ | 444 (32) | 676 (30) | 643 (29) | 433 (28) |
| Weekday | 959 (68) | 1612 (70) | 1569 (71) | 1097 (72) |
| Time of day | ||||
| Nighttime# | 443 (32) | 682 (30) | 633 (29) | 485 (32) |
| Daytime | 960 (68) | 1606 (70) | 1579 (71) | 1045 (68) |
| Event Characteristics | ||||
| Witnessed | ||||
| Yes | 1289 (92) | 2158 (94) | 2105 (95) | 1466 (96) |
| No | 114 (8) | 130 (6) | 107 (5) | 64 (4) |
| Monitored | ||||
| Yes | 186 (13) | 275 (12) | 244 (11) | 91 (6) |
| No | 1217 (87) | 2013 (88) | 1968 (89) | 1439 (94) |
| First pulseless rhythm | ||||
| Beginning of event | ||||
| Asystole | 540 (50) | 622 (38) | 593 (38) | 341 (33) |
| PEA | 367 (34) | 846 (51) | 750 (49) | 574 (55) |
| PVT | 64 (6) | 87 (5) | 109 (7) | 72 (7) |
| VF | 108 (10) | 100 (6) | 91 (6) | 55 (5) |
| During event** | ||||
| Asystole | 174 (54) | 369 (58) | 322 (48) | 206 (42) |
| PEA | 86 (27) | 213 (34) | 292 (44) | 239 (49) |
| PVT | 14 (4) | 23 (4) | 19 (3) | 21 (4) |
| VF | 50 (15) | 28 (4) | 36 (5) | 22 (5) |
| Hospital Characteristics | ||||
| Years of GWTG participation (years) | 9 (6, 15) | 14 (9, 15) | 13 (8, 15) | 11 (6, 15) |
| Geographic region | ||||
| North-East | 324 (23) | 262 (11) | 450 (20) | 298 (19) |
| South-East | 347 (25) | 541 (24) | 730 (33) | 423 (28) |
| North-Central | 191 (14) | 351 (15) | 361 (16) | 374 (24) |
| South-Central | 286 (20) | 763 (33) | 533 (24) | 288 (19) |
| West | 255 (18) | 371 (16) | 138 (6) | 147 (10) |
| Geographical area | ||||
| Rural | 64 (5) | 48 (2) | 20 (1) | 15 (1) |
| Urban | 1339 (95) | 2240 (98) | 2192 (99) | 1515 (99) |
| Ownership | ||||
| Government/Military | 213 (15) | 352 (15) | 278 (13) | 104 (7) |
| Non-profit | 1143 (81) | 1824 (80) | 1868 (84) | 1362 (89) |
| Private | 47 (3) | 112 (5) | 66 (3) | 64 (4) |
| Teaching status | ||||
| Major | 799 (57) | 1684 (74) | 1729 (78) | 1117 (73) |
| Minor | 441 (31) | 434 (19) | 391 (18) | 347 (23) |
| Non-teaching | 163 (12) | 170 (7) | 92 (4) | 66 (4) |
CNS denotes central nervous system; GWTG-R denotes Get With The Guidelines-Resuscitation; PEA denotes pulseless electrical activity; PVT denotes pulseless ventricular tachycardia; VF denotes ventricular fibrillation.
Including non-cardiac surgical patients, trauma patients, and obstetric patients.
The newborn illness category was added to the GWTG-R registry in 2005 and removed in 2015.
Definitions have been provided elsewhere.11
Including ambulatory or outpatient clinics, diagnostic or interventional areas, operating room, post-anesthesia recovery room, rehabilitation unit, same-day surgical area, and delivery room.
Friday 11 PM to Monday 7 AM.
11:00 PM to 6:59 AM.
Patients with bradycardia and poor perfusion progressing into pulseless cardiac arrest during resuscitation
Table 2.
Characteristics of non-pulseless events
| 2000–2005 (n = 736) | 2006–2010 (n = 1914) | 2011–2015 (n = 2043) | 2016–2018 (n = 1058) | |
|---|---|---|---|---|
| Demographics | ||||
| Sex | ||||
| Male | 397 (54) | 1069 (56) | 1137 (56) | 598 (57) |
| Female | 339 (46) | 845 (44) | 906 (44) | 460 (43) |
| Age group | ||||
| Neonate (<1 month) | 225 (31) | 1111 (58) | 961 (47) | 260 (25) |
| Infant (1 month to <1 year) | 304 (41) | 481 (25) | 632 (31) | 548 (52) |
| Child (1 year to <12 years) | 162 (22) | 268 (14) | 368 (18) | 196 (19) |
| Adolescent (≥12 years) | 45 (6) | 54 (3) | 82 (4) | 54 (5) |
| Illness category | ||||
| Medical | ||||
| Cardiac | 113 (15) | 204 (11) | 249 (12) | 178 (17) |
| Non-cardiac | 315 (43) | 547 (29) | 742 (36) | 525 (50) |
| Surgical | ||||
| Cardiac | 101 (14) | 219 (11) | 320 (16) | 165 (16) |
| Non-cardiac* | 86 (12) | 170 (9) | 245 (12) | 190 (18) |
| Newborn† | 121 (16) | 774 (40) | 487 (24) | 0 (0) |
| Pre-existing conditions‡ | ||||
| Acute non-stroke CNS event | 38 (5) | 71 (4) | 77 (4) | 32 (3) |
| Baseline depression in CNS | 138 (19) | 183 (10) | 168 (8) | 97 (9) |
| Heart failure prior admission | 118 (16) | 57 (3) | 40 (2) | 31 (3) |
| Heart failure this admission | 131 (18) | 85 (4) | 55 (3) | 38 (4) |
| Hepatic insufficiency | 52 (7) | 71 (4) | 47 (2) | 27 (3) |
| Hypotension | 236 (32) | 434 (23) | 411 (20) | 232 (22) |
| Metabolic abnormalities | 125 (17) | 208 (11) | 214 (10) | 165 (16) |
| Metastatic malignancy | 18 (2) | 31 (2) | 29 (1) | 19 (2) |
| Pneumonia | 80 (11) | 116 (6) | 96 (5) | 45 (4) |
| Respiratory insufficiency | 543 (74) | 1274 (67) | 1370 (67) | 778 (74) |
| Renal insufficiency | 78 (11) | 122 (6) | 128 (6) | 63 (6) |
| Septicemia | 130 (18) | 273 (14) | 256 (13) | 66 (6) |
| Location and Time of Event | ||||
| Location of event | ||||
| Emergency department | 27 (4) | 45 (2) | 61 (3) | 28 (3) |
| Intensive care unit | 556 (76) | 1383 (72) | 1532 (75) | 855 (81) |
| Floor | ||||
| Without telemetry | 38 (5) | 55 (3) | 70 (3) | 37 (3) |
| With telemetry | 8 (1) | 22 (1) | 17 (1) | 9 (1) |
| Other§ | 107 (15) | 409 (21) | 363 (18) | 129 (12) |
| Time of week | ||||
| Weekend∥ | 239 (32) | 584 (31) | 578 (28) | 290 (27) |
| Weekday | 497 (68) | 1330 (69) | 1465 (72) | 768 (73) |
| Time of day | ||||
| Nighttime# | 208 (28) | 579 (30) | 570 (28) | 268 (25) |
| Daytime | 528 (72) | 1335 (70) | 1473 (72) | 790 (75) |
| Event Characteristics | ||||
| Witnessed | ||||
| Yes | 709 (96) | 1854 (97) | 1991 (97) | 1021 (97) |
| No | 27 (4) | 60 (3) | 52 (3) | 37 (3) |
| Monitored | ||||
| Yes | 72 (10) | 272 (14) | 190 (9) | 33 (3) |
| No | 664 (90) | 1642 (86) | 1853 (91) | 1025 (97) |
| Hospital Characteristics | ||||
| Years of GWTG participation (years) | 14 (7, 18) | 13 (7, 15) | 13 (10, 15) | 11 (7, 15) |
| Geographic region | ||||
| North-East | 234 (32) | 243 (13) | 490 (24) | 251 (24) |
| South-East | 138 (19) | 552 (29) | 647 (32) | 286 (27) |
| North-Central | 76 (10) | 161 (8) | 218 (11) | 210 (20) |
| South-Central | 172 (23) | 557 (29) | 521 (26) | 199 (19) |
| West | 116 (16) | 401 (21) | 167 (8) | 112 (11) |
| Geographical area | ||||
| Rural | 22 (3) | 31 (2) | 6 (<1) | 5 (<1) |
| Urban | 714 (97) | 1883 (98) | 2037 (>99) | 1053 (>99) |
| Ownership | ||||
| Government/Military | 58 (8) | 329 (17) | 276 (14) | 67 (6) |
| Non-profit | 649 (88) | 1477 (77) | 1713 (84) | 950 (90) |
| Private | 29 (4) | 108 (6) | 54 (3) | 41 (4) |
| Teaching status | ||||
| Major | 461 (63) | 1289 (67) | 1506 (74) | 754 (71) |
| Minor | 228 (31) | 491 (26) | 472 (23) | 261 (25) |
| Non-teaching | 47 (6) | 134 (7) | 65 (3) | 43 (4) |
CNS denotes central nervous system; GWTG-R denotes Get With The Guidelines-Resuscitation.
Including non-cardiac surgical patients, trauma patients, and obstetric patients.
The newborn illness category was added to the GWTG-R registry in 2005 and removed in 2015.
Definitions have been provided elsewhere.11
Including ambulatory or outpatient clinics, diagnostic or interventional areas, operating room, post-anesthesia recovery room, rehabilitation unit, same-day surgical area, and delivery room.
Friday 11 PM to Monday 7 AM.
11:00 PM to 6:59 AM.
The primary outcome was survival to hospital discharge. The secondary outcome was sustained return of spontaneous circulation (ROSC), defined as the presence of a pulse and no further delivery of chest compressions for at least 20 minutes, or the initiation of cardiopulmonary bypass or extracorporeal membrane oxygenation. We initially planned to include survival to hospital discharge with favorable neurological status12 as a secondary outcome. However, due to a large proportion of missing data that varied with year (Figure S1), this was not a feasible outcome in our study.
Statistical Analysis
The goal of this study was to examine temporal survival trends for pediatric patients with an in-hospital pulseless cardiac arrest and pediatric patients with a non-pulseless event requiring cardiopulmonary resuscitation, separately. Descriptive statistics were used to summarize the study population over time, categorized by four time periods (2000 to 2005, 2006 to 2010, 2011 to 2015, and 2016 to 2018). Categorical data are presented as counts with frequencies and continuous data are presented as medians with 1st and 3rd quartiles.
To assess trends in survival over time, we used generalized estimation equations (GEE)13 with a Gaussian distribution (identity link function) to obtain absolute risk differences (RD) and a Poisson distribution (log link function)14, 15 to obtain relative risk (RR) estimates. An exchangeable variance-covariance structure was used to account for correlations between patients within hospitals.
We used a stepwise approach and developed three separate models, while adjusting for an incremental number of prespecified covariates. For the first model, we included survival to hospital discharge as the dependent variable and calendar year as an independent continuous variable to obtain unadjusted estimates for every unit increase in year between 2000 and 2018. For the second model, we added patient demographics and hospital characteristics (Table 1 and Table 2) to the model to obtain partly risk-adjusted estimates. For the third model, we added location, time of event, and event characteristics (all variables in Table 1 and Table 2) to the model to obtain fully risk-adjusted estimates. No absolute risk differences could be provided for the second and third model due to convergence issues. All three analyses were repeated for the secondary outcome.
As an additional analysis, we included calendar year as a categorical variable in the models, with 2009 as the reference year, to obtain relative risk ratios for each subsequent and preceding year between 2000 and 2018. Year 2009 was chosen as the reference category because of the larger number of events in this year.
As a prespecified subgroup analysis, we repeated the analyses for the primary outcome, after categorizing patients with an in-hospital pulseless cardiac arrest based on the first pulseless rhythm (shockable vs non-shockable). These analyses were performed by adding an interaction term between the subgroup variable and continuous calendar year into the models.
To account for missing data on covariates and the primary outcome (Table S1), multiple imputations were performed using the fully conditional specification method and assuming that the data were “missing at random”.16, 17 A total of 20 imputed datasets were created18 and multivariable regression was subsequently performed on each of the datasets, including calendar year as a continuous variable, survival to hospital discharge, and all characteristics listed in Table 1 and Table 2.
We conducted three post-hoc analyses. First, we developed a separate model by including additional event characteristics (length of resuscitation, interventions in place at the time of event, and interventions during the event) as covariates in the model for pulseless cardiac arrests (Table S2) and non-pulseless events (Table S3). Second, we examined the unadjusted temporal trend in survival to hospital discharge for pediatric patients presenting with an initial non-pulseless event who deteriorated into pulseless cardiac arrest during resuscitation. Third, we repeated the unadjusted regression analyses after defining ROSC without considering cardiopulmonary bypass or extracorporeal membrane oxygenation.
All analyses were two-sided, with a significance level of p <0.05. SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for all analyses.
Results
Patient Characteristics
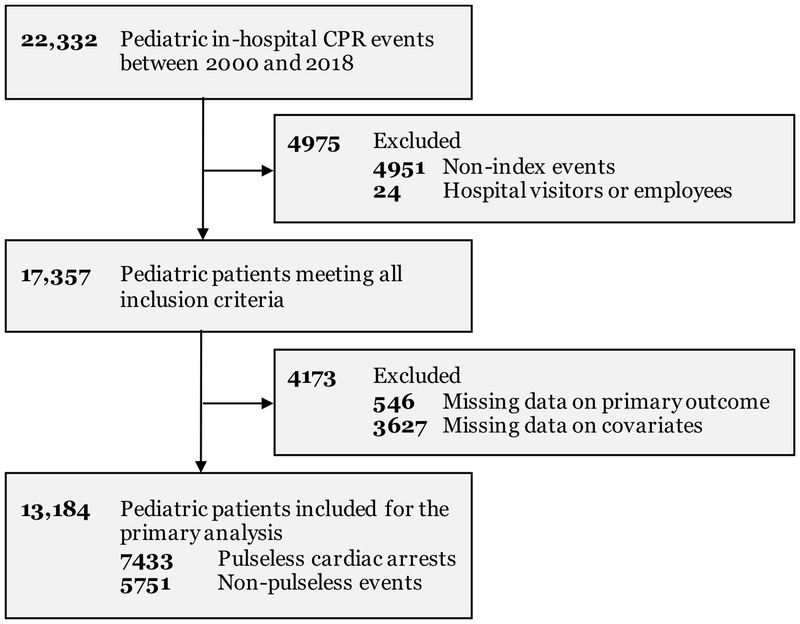
The study population included 13,184 pediatric patients, of which 7433 patients had a pulseless cardiac arrest and 5751 patients had a non-pulseless event requiring cardiopulmonary resuscitation (Figure 1). Baseline characteristics were comparable over time for both study populations (Table 1 and Table 2), although the number of patients with an event in the intensive care unit appeared to increase over time. Additional event characteristics are provided in the Supplementary Content (Table S2 and Table S3), including trends in the use of extracorporeal membrane oxygenation (Figure S2).
Figure 1. Inclusion and exclusion criteria for the primary analysis.
Between 2000 and 2018, 22,332 pediatric in-hospital events requiring CPR were registered in the Get With The Guidelines®-Resuscitation registry. A total of 13,184 patients were included for the final analysis, of which 7433 patients had a pulseless cardiac arrest and 5751 patients had a non-pulseless event requiring cardiopulmonary resuscitation. CPR denotes cardiopulmonary resuscitation.
Pulseless Cardiac Arrests
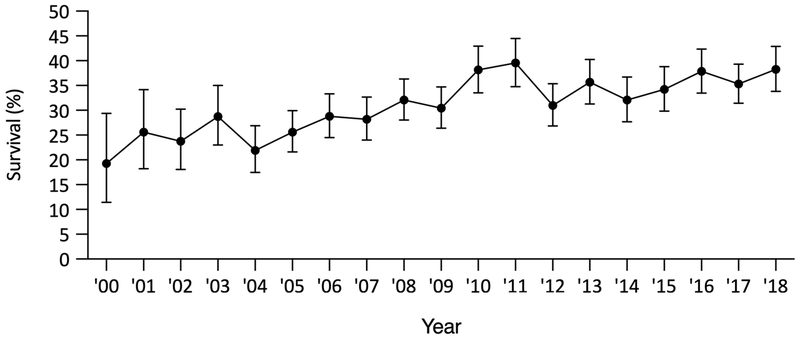
Out of the 7433 patients with a pulseless cardiac arrest between 2000 and 2018, 2394 (32%) patients survived to hospital discharge. Survival was 19% (95%CI, 11%–29%) in 2000 and 38% (95%CI, 34%–43%) in 2018, with a peak survival of 40% (95%CI, 35%–44%) in 2011.
In the unadjusted analysis, the absolute change in survival (RD) was 0.67% (95%CI, 0.40%–0.95%; p <0.001; Figure 2 and Table S4) and the relative change in survival (RR) was 1.02 (95%CI, 1.01–1.03; p <0.001; Figure S3 and Table S5) per year. In the partly risk-adjusted analysis and in the fully risk-adjusted analysis, the relative change in survival (RR) was 1.02 (95%CI, 1.00–1.03; p = 0.02; Figure S3 and Table S5) and 1.02 (95%CI, 1.00–1.03; p = 0.01; Figure S3 and Table S5) per year, respectively.
Figure 2. Survival trends for pulseless cardiac arrests.
The figure illustrates unadjusted trends in survival to hospital discharge from 2000 to 2018. Results are reported as absolute risks with 95% confidence intervals. The absolute change in survival to hospital discharge was 0.67% (95%CI, 0.40%–0.95%; p <0.001; Table S4) per unit increase in year.
There was an increase in ROSC over time, with an absolute change (RD) of 0.83% (95%CI, 0.53%–1.14%; p <0.001; Figure S4 and Table S4) and a relative change (RR) of 1.01 (95%CI, 1.01–1.02; p <0.001; Figure S5 and Table S6) per year in the unadjusted analysis, a relative change (RR) of 1.01 (95%CI, 1.01–1.02; p <0.001; Figure S5 and Table S6) per year in the partly risk-adjusted analysis, and a relative change (RR) of 1.01 (95%CI, 1.01–1.02; p <0.001; Figure S5 and Table S6) per year in the fully risk-adjusted analysis.
Non-Pulseless Events
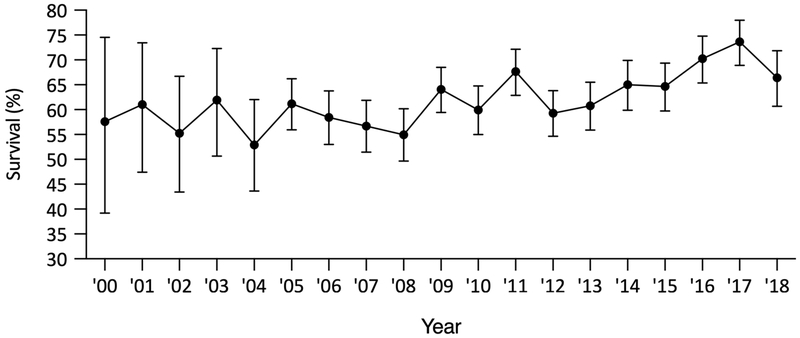
Out of the 5751 patients with a non-pulseless event requiring cardiopulmonary resuscitation, 3605 (63%) patients survived to hospital discharge, with a survival of 57% (95%CI, 39%–75%) in 2000 and 66% (95%CI, 61%–72%) in 2018.
In the unadjusted analysis, the absolute change in survival (RD) was 0.80% (95%CI, 0.32%–1.27%; p = 0.001; Figure 3 and Table S7) and the relative change in survival (RR) was 1.01 (95%CI, 1.01–1.02; p = 0.001; Figure S6 and Table S8) per year. In the partly and fully risk-adjusted analyses, the relative change in survival (RR) was 1.01 (95%CI, 0.99–1.02; p = 0.32; Figure S6 and Table S8) and 1.01 (95%CI, 1.00–1.02; p = 0.26; Figure S6 and Table S8) per year, respectively.
Figure 3. Survival trends for non-pulseless events.
The figure illustrates unadjusted trends in survival to hospital discharge from 2000 to 2018. Results are reported as absolute risks with 95% confidence intervals. The absolute change in survival to hospital discharge was 0.80% (95%CI, 0.32%–1.27%; p = 0.001; Table S7) per unit increase in year. Non-pulseless events refer to events requiring cardiopulmonary resuscitation for bradycardia and poor perfusion.
Subgroup and Sensitivity Analyses
For pulseless cardiac arrests, there was no significant interaction between survival to hospital discharge and the initial rhythm in either model (unadjusted analysis: p = 0.41, partly risk-adjusted analysis: p = 0.39, fully risk-adjusted analysis: p = 0.51).
A total of 17,357 pediatric patients were included in the sensitivity analysis to account for missing data. Data were missing or inconsistent for 4173 (24%) patients with a median number of missing variables of 2 (quartiles: 2–6; mean: 5.3, SD: 5.6). The combined estimate from the 20 imputed datasets was similar to the primary analysis, with a relative change in survival (RR) of 1.02 (95%CI, 1.01–1.03; p = 0.002) per year for pulseless cardiac arrests and 1.01 (95%CI, 0.99–1.02; p = 0.32) per year for non-pulseless events.
Post-Hoc Analyses
A total of 7257 patients with a pulseless cardiac arrest and 5570 patients with a non-pulseless event were available for the analysis adjusting for additional event characteristics (length of resuscitation, interventions in place at time of event, and interventions during resuscitation). The relative change (RR) in survival was 1.01 (95%CI, 1.00–1.02; p = 0.05) per year and 1.00 (95%CI, 1.00–1.01; p = 0.35) per year for pulseless cardiac arrests and non-pulseless events, respectively.
Out of the 5751 patients with an initial non-pulseless event, 2114 (37%) patients deteriorated into pulseless cardiac arrest during resuscitation, with a survival to hospital discharge of 10% (95%CI, 1%–31%) in 2000 and 32% (95%CI, 24%–40%) in 2018. In this cohort, the unadjusted absolute change (RD) in survival was 0.88% (95%CI, 0.42%–1.35%; p <0.001; Figure S7) and the relative change (RR) in survival was 1.04 (95%CI, 1.02–1.07; p <0.001) per year.
Extracorporeal cardiopulmonary bypass was used in 630 (9%) patients in the pulseless cohort. When defining ROSC without including cardiopulmonary bypass or extracorporeal membrane oxygenation, the unadjusted trend in ROSC was similar to the primary analysis, with an absolute change (RD) of 0.81% (95%CI, 0.52%–1.10%; p <0.001) and a relative change (RR) of 1.01 (95%CI, 1.01–1.02; p <0.001) per year.
Discussion
In this study, using a large, multicenter, in-hospital cardiac arrest registry in the US, we found an increase in survival to hospital discharge and ROSC from 2000 to 2018 for children with a pulseless cardiac arrest. Survival to hospital discharge also increased for children receiving cardiopulmonary resuscitation for non-pulseless events in the unadjusted analysis, but not in any of the adjusted analyses. The results remained consistent when accounting for missing data.
Few previous studies have reported national trends in survival for pediatric in-hospital pulseless cardiac arrests.3 One of the more recent studies was published by Girotra et al. in 2013 who used the same nationwide in-hospital cardiac arrest registry as this study to describe trends in survival between 2000 and 2009.2 The authors found an unadjusted increase in survival from 14% in 2000 to 39% in 2009, compared to survival of 19% in 2000, 31% in 2009, and 38% in 2018 in our study. There are several potential reasons for the different trend in survival between the studies. First, the previous study was restricted to hospitals with more than three years of consecutive data and high case volumes, yielding a study sample of 1031 patients from 12 hospitals between 2000 and 2009. In comparison, we included 7433 patients from 351 hospitals over a longer time period, which may provide more generalizable results, although survival could have been affected by changes in GWTG-R participating hospitals over time. Second, the previous study population was limited to cardiac arrests in inpatient locations, not including events in the emergency department, operating suites, and procedural suites, where survival may differ from other locations. Despite the above differences, the increase in survival across both studies is reassuring and can perhaps provide some evidence for the progress of quality-improvement efforts, although the reason for this improvement is speculative and could be related to other unmeasured factors.
Both the unadjusted (model 1) and adjusted (model 2 and model 3) analyses showed an increase in survival for pulseless cardiac arrests when including calendar year as a continuous variable in the models. The consistent results across all models suggest that survival has increased independently from trends in specific patient, hospital, and event characteristics (all variables in Table 1). However, we were not able to distinguish whether the increase in survival was related to unmeasured baseline factors and/or resuscitation practices (such as cardiopulmonary resuscitation quality), which could not be controlled for in our analyses. In addition, whether survival was driven by improvements in specific hospitals providing data to the GWTG-R registry, similar to what has been suggested for the adult population19, remains unknown. End-of-life policies may also have changed during the study period, although the incidence of pediatric cardiac arrests without a do-not-resuscitate order was recently reported to remain stable over time.1
Compared to pulseless cardiac arrests, survival for non-pulseless events increased significantly in the unadjusted model, but not in any of the adjusted models, which may be explained by changes in baseline characteristics over time (Table 2). For example, the number of events occurring in intensive care units were higher in more recent years, which may allow for earlier detection and rapid resuscitation efforts, similar to what has been described in previous studies.20 Additionally, for patients with a non-pulseless event who deteriorated into pulseless cardiac arrest during resuscitation, survival was overall lower compared to patients with an initial pulseless cardiac arrest (23% vs 38% in 2018).
When including calendar year as a categorical variable in the models for pulseless cardiac arrests, survival to hospital discharge (Figure 2 and Figure S3) and ROSC (Figure S4 and Figure S5) appeared to increase steadily from 2000 to 2010 but remained largely unchanged from 2011 to 2018. One explanation for the stagnating trend in survival, although speculative, could be that we have reached a plateau in our current understanding of causes, diagnosis, and treatment of pediatric in-hospital cardiac arrest. Given that ROSC and survival to hospital discharge has been changing in parallel over time, it is possible that survival has primarily been driven by changes in the number of patients who are successfully resuscitated. The introduction of the 2010 Advanced Life Support guidelines (including a new sequence of cardiopulmonary resuscitation and updates to post-resuscitation care) may also have affected outcomes, although our study was not designed to identify the specific reasons for changes in survival.
Based on a recent estimate of the national pediatric in-hospital cardiac arrest incidence in the US, we can extrapolate our findings to the national level.1 For example, with a reported incidence of 6900 pulseless cardiac arrest cases and 8400 non-pulseless events in 2017, we estimate that about 4485 (65%) and 2184 (26%) children died from pulseless cardiac arrests and non-pulseless events in the US, respectively. These numbers highlight the persistent public health burden of cardiac arrest in the US, regardless of the improvement in survival over the past decade, and additional efforts are needed to improve outcomes following cardiac arrest in children.
The results should be interpreted in the context of the following limitations. First, we were limited by the available data in the GWTG-R registry and the trends in survival could potentially be explained by other variables, such as quality of care and post-resuscitation care. Second, we were unable to provide results for favorable neurological outcome due to a large amount of missing data. Third, hospitals providing data to the GWTG-R registry may not be representative of the remaining hospitals in the US, which could limit the generalizability of our results.1
In conclusion, survival has improved significantly for pediatric events requiring cardiopulmonary resuscitation in the US, with a 19% absolute increase in survival for in-hospital pulseless cardiac arrests and a 9% absolute increase in survival for non-pulseless events between 2000 and 2018.
Supplementary Material
Clinical Perspective.
What is New?
-
-
Survival has improved significantly for hospitalized children receiving cardiopulmonary resuscitation, with a 19% absolute increase in survival for pulseless cardiac arrests and a 9% absolute increase in survival for non-pulseless events (bradycardia and poor perfusion) between 2000 and 2018
-
-
Survival for pulseless cardiac arrests appeared to have reached a plateau following 2010
What are the Clinical Implications?
-
-
The increase in survival over time is reassuring and can perhaps provide some evidence for the progress of quality-improvement efforts
-
-
Given the plateau in survival following 2010, there is a continued need for clinical focus and new interventions to improve outcomes of pediatric in-hospital cardiac arrest
Acknowledgements
Mathias J. Holmberg and Lars W. Andersen were responsible for the data acquisition, performed the statistical analyses, and drafted the manuscript. All authors contributed to the design of the study, interpreted the results, and critically revised the manuscript. All authors approved the final manuscript as submitted and agrees to be accountable for all aspects of the submitted work.
Sources of Funding
There was no specific funding for this study. Dr. Andersen serves as a statistical reviewer for JAMA. Dr. Donnino is supported by grant 5K24HL127101-04 and 5R01HL136705-03 from the National Heart, Lung, and Blood Institute. The remaining authors have no conflicts of interest to disclose.
Non-standard Abbreviations and Acronyms
- US
United States
- GWTG-R
Get With The Guidelines – Resuscitation
- IRB
Institutional Review Board
- ROSC
Return of spontaneous circulation
- GEE
Generalized estimation equations
- RD
Risk differences
- RR
Relative risk
- CPR
Cardiopulmonary resuscitation
Appendix
Besides the author Monica Kleinman, M.D., members of the Get With The Guidelines®-Resuscitation Pediatric Research Task Force include: Anne-Marie Guerguerian, M.D., Ph.D., F.R.C.P.C., Dianne Atkins, M.D., Elizabeth Foglia, M.D., M.S.C.E., Jordan Duval-Arnould, M.P.H., Dr.P.H. Ericka Fink, M.D., Javier J. Lasa, M.D., F.A.A.P., Joan Roberts, M.D., Melanie Bembea, M.D., M.P.H., Michael Gaies, M.D., M.P.H., M.Sc., Punkaj Gupta, M.B.B.S., Robert Sutton, M.D., M.S.C.E., Taylor Sawyer, D.O.Med.
Footnotes
Disclosures
None.
References
- 1.Holmberg MJ, Ross CE, Chan PS, Duval-Arnould J, Grossestreuer AV, Yankama T, Donnino MW, and Andersen LW. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12:e005580. [PMC free article] [PubMed] [Google Scholar]
- 2.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, and Chan PS. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6:42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019:CIR0000000000000659. [DOI] [PubMed] [Google Scholar]
- 4.Neumar RW. Doubling Cardiac Arrest Survival by 2020: Achieving the American Heart Association Impact Goal. Circulation. 2016;134:2037–2039. [DOI] [PubMed] [Google Scholar]
- 5.Duff JP, Topjian A, Berg MD, Chan M, Haskell SE, Joyner BL, Lasa JJ, Ley SJ, Raymond TT, Sutton RM et al. 2018 American Heart Association Focused Update on Pediatric Advanced Life Support: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2018;138:e731–e739. [DOI] [PubMed] [Google Scholar]
- 6.Donoghue A, Berg RA, Hazinski MF, Praestgaard AH, Roberts K, and Nadkarni VM. Cardiopulmonary resuscitation for bradycardia with poor perfusion versus pulseless cardiac arrest. Pediatrics. 2009;124:1541–1548. [DOI] [PubMed] [Google Scholar]
- 7.Khera R, Tang Y, Girotra S, Nadkarni VM, Link MS, Raymond TT, Guerguerian AM, Berg RA, and Chan PS. Pulselessness After Initiation of Cardiopulmonary Resuscitation for Bradycardia in Hospitalized Children: Prevalence, Predictors of Survival, and Implications for Hospital Profiling. Circulation. 2019;140:370–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, and Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. [DOI] [PubMed] [Google Scholar]
- 9.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. [DOI] [PubMed] [Google Scholar]
- 10.American Hospital Association (AHA). AHA Annual Survey Database Fiscal Year 2013. https://www.ahdataviewer.com/book-cd-products/aha-survey. Accessed March 8, 2018.
- 11.Holmberg MJ, Moskowitz A, Raymond TT, Berg RA, Nadkarni VM, Topjian AA, Grossestreuer AV, Donnino MW, and Andersen LW. Derivation and Internal Validation of a Mortality Prediction Tool for Initial Survivors of Pediatric In-Hospital Cardiac Arrest. Pediatr Crit Care Med. 2018;19:186–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74. [DOI] [PubMed] [Google Scholar]
- 13.Zeger SL, Liang KY, and Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 14.Zou GY and Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22:661–670. [DOI] [PubMed] [Google Scholar]
- 15.Zou G A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 16.van Buuren S Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–242. [DOI] [PubMed] [Google Scholar]
- 17.Lee KJ and Carlin JB. Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol. 2010;171:624–632. [DOI] [PubMed] [Google Scholar]
- 18.Graham JW, Olchowski AE, and Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev Sci. 2007;8:206–213. [DOI] [PubMed] [Google Scholar]
- 19.Girotra S, Cram P, Spertus JA, Nallamothu BK, Li Y, Jones PG, and Chan PS. Hospital variation in survival trends for in-hospital cardiac arrest. J Am Heart Assoc. 2014;3:e000871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berg RA, Sutton RM, Holubkov R, Nicholson CE, Dean JM, Harrison R, Heidemann S, Meert K, Newth C, Moler F et al. Ratio of PICU versus ward cardiopulmonary resuscitation events is increasing. Crit Care Med. 2013;41:2292–2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.