Abstract
Background
People who have chronic kidney disease (CKD) have important changes to bone structure, strength, and metabolism. Children experience bone deformity, pain, and delayed or impaired growth. Adults experience limb and vertebral fractures, avascular necrosis, and pain. The fracture risk after kidney transplantation is four times that of the general population and is related to Chronic Kidney Disease‐Mineral and Bone Disorder (CKD‐MBD) occurring with end‐stage kidney failure, steroid‐induced bone loss, and persistent hyperparathyroidism after transplantation. Fractures may reduce quality of life and lead to being unable to work or contribute to community roles and responsibilities. Earlier versions of this review have found low certainty evidence for effects of treatment. This is an update of a review first published in 2005 and updated in 2007.
Objectives
This review update evaluates the benefits and harms of interventions for preventing bone disease following kidney transplantation.
Search methods
We searched the Cochrane Kidney and Transplant Register of Studies up to 16 May 2019 through contact with the Information Specialist using search terms relevant to this review. Studies in the Register are identified through searches of CENTRAL, MEDLINE, and EMBASE, conference proceedings, the International Clinical Trials Register (ICTRP) Search Portal and ClinicalTrials.gov.
Selection criteria
RCTs and quasi‐RCTs evaluating treatments for bone disease among kidney transplant recipients of any age were eligible.
Data collection and analysis
Two authors independently assessed trial risks of bias and extracted data. Statistical analyses were performed using random effects meta‐analysis. The risk estimates were expressed as a risk ratio (RR) for dichotomous variables and mean difference (MD) for continuous outcomes together with the corresponding 95% confidence interval (CI). The primary efficacy outcome was bone fracture. The primary safety outcome was acute graft rejection. Secondary outcomes included death (all cause and cardiovascular), myocardial infarction, stroke, musculoskeletal disorders (e.g. skeletal deformity, bone pain), graft loss, nausea, hyper‐ or hypocalcaemia, kidney function, serum parathyroid hormone (PTH), and bone mineral density (BMD).
Main results
In this 2019 update, 65 studies (involving 3598 participants) were eligible; 45 studies contributed data to our meta‐analyses (2698 participants). Treatments included bisphosphonates, vitamin D compounds, teriparatide, denosumab, cinacalcet, parathyroidectomy, and calcitonin. Median duration of follow‐up was 12 months. Forty‐three studies evaluated bone density or bone‐related biomarkers, with more recent studies evaluating proteinuria and hyperparathyroidism. Bisphosphonate therapy was usually commenced in the perioperative transplantation period (within 3 weeks) and regardless of BMD. Risks of bias were generally high or unclear leading to lower certainty in the results. A single study reported outcomes among 60 children and adolescents. Studies were not designed to measure treatment effects on fracture, death or cardiovascular outcomes, or graft loss.
Compared to placebo, bisphosphonate therapy administered over 12 months in transplant recipients may prevent fracture (RR 0.62, 95% CI 0.38 to 1.01; low certainty evidence) although the 95% CI included the possibility that bisphosphonate therapy might make little or no difference. Fracture events were principally vertebral fractures identified during routine radiographic surveillance. It was uncertain whether any other drug class decreased fracture (low or very low certainty evidence). It was uncertain whether interventions for bone disease in kidney transplantation reduce all‐cause or cardiovascular death, myocardial infarction or stroke, or graft loss in very low certainty evidence. Bisphosphonate therapy may decrease acute graft rejection (RR 0.70, 95% CI 0.55 to 0.89; low certainty evidence), while it is uncertain whether any other treatment impacts graft rejection (very low certainty evidence). Bisphosphonate therapy may reduce bone pain (RR 0.20, 95% CI 0.04 to 0.93; very low certainty evidence), while it was very uncertain whether bisphosphonates prevent spinal deformity or avascular bone necrosis (very low certainty evidence). Bisphosphonates may increase to risk of hypocalcaemia (RR 5.59, 95% CI 1.00 to 31.06; low certainty evidence). It was uncertain whether vitamin D compounds had any effect on skeletal, cardiovascular, death, or transplant function outcomes (very low certainty or absence of evidence). Evidence for the benefits and harms of all other treatments was of very low certainty. Evidence for children and young adolescents was sparse.
Authors' conclusions
Bisphosphonate therapy may reduce fracture and bone pain after kidney transplantation, however low certainty in the evidence indicates it is possible that treatment may make little or no difference. It is uncertain whether bisphosphonate therapy or other bone treatments prevent other skeletal complications after kidney transplantation, including spinal deformity or avascular bone necrosis. The effects of bone treatment for children and adolescents after kidney transplantation are very uncertain.
Plain language summary
Interventions for preventing bone disease in kidney transplant recipients
What is the issue? People who have a kidney transplant can have more fragile bones because of changes to the ways bones are formed in kidney disease and because anti‐rejection medicines including prednisone can make their bones thinner. Bone fractures can cause difficulty with walking and carrying out the activities of everyday living such as work and family life. There are several treatment options for preventing fracture for people with thinner bones but whether these are helpful for kidney transplant patients is not clear. An earlier version of this Cochrane review in 2004 (and updated in 2007) did not find that any of these treatments prevented fractures.
What did we do?
We looked for new studies available since our last review published in 2007 to learn whether there is new information about available treatments for bone disease in people who have had a kidney transplant.
What did we find? In 2019, there are 65 research studies (involving 3598 people) that looked at whether medicines can prevent bone fractures after kidney transplant. The most common medicine in the studies was a bisphosphonate which slows bone breakdown. Bisphosphonates were given at around the time of kidney transplantation (generally just before or within a few weeks) and continued for about one year on average. Other treatment options in the studies were vitamin D, calcitonin, denosumab, teriparatide, or cinacalcet. Bisphosphonate treatment given after a transplant possibly prevents fractures and bone pain, however the range where the actual effect of treatment might be (the "margin of error") indicates that treatment might make little or no difference. Bisphosphonates possibly lower the chances of a rejection of the transplant kidney but because of problems with the research studies, we can't be very certain that this is true. Bisphosphonates caused low blood calcium levels for some people. There was low or very low confidence in the information about all the other possible treatments for bone fractures after a kidney transplant, as the studies were often too small. There was only one study for medicines in children so we don't know whether these drugs are useful and safe for younger people.
Conclusions It is still unclear whether bisphosphonate therapy makes any difference to bone fractures or are safe for both adults and children with a kidney transplant.
Summary of findings
Background
Description of the condition
Patient life expectancy after kidney transplantation has improved progressively (Hariharan 2001). Attention is increasingly focused on preventing the longer‐term complications of transplantation and improving quality of life by addressing factors that affect long‐term morbidity including cardiovascular risk, weight gain, post‐transplantation diabetes mellitus, cancer, and bone disease. The bone disease that develops after kidney transplantation is an important cause of complications including fracture, pain, deformity, and disability. The bone disease that accrues after transplantation is the pathological intersection of several processes including Chronic Kidney Disease Mineral and Bone Disorder (CKD‐MBD) due to long‐term kidney failure, bone metabolic changes related to transplant immunosuppression (particularly corticosteroids), and persistently impaired kidney function leading to ongoing raised parathyroid gland activity (Malluche 2010). The resulting pathobiology of the bone includes altered bone mineralization and bone turnover, reduced bone volume, and increased fragility related to altered bone tissue and architecture. Increased circulating levels of fibroblast growth factor 23 (FGF23) may persist after transplantation leading to hypophosphataemia and hypercalcaemia in the short term, and are associated with allograft dysfunction and mortality in the longer term (Wolff 2011).
Patients with chronic kidney disease (CKD) are at increased risk for fracture, with a vertebral fracture prevalence of 21% and relative risk (RR) for hip fracture increased up to 14‐fold (Sprague 2004). The fracture risk for kidney transplant recipients is four times that of the general population and is increased when compared with haemodialysis patients (Grotz 1994; Veenstra 1999). Studies report a fracture prevalence of 7% to 60% (Durieux 2002; Giannini 2001; Monier‐Faugere 2000; Nisbeth 1999; O'Shaunessy 2002; Vautour 2004) following successful kidney transplantation with an incidence of 2% per year (Abbott 2001; Grotz 1994). Women, patients with diabetes, those with an increased duration of dialysis therapy, older patients, and people who have experienced a longer time since transplantation have a higher risk (Sprague 2004). Recipients of a kidney transplant lose bone rapidly and early following transplantation (Almond 1994; Horber 1994; Julian 1991) from sites rich in trabecular bone. Bone mineral density (BMD) decreases in the lumbar spine by 5% in the first year after transplantation (Torregrosa 2003) and longitudinal studies in stable kidney transplant recipients demonstrate bone loss of 1.7% annually at the lumbar spine (Pichette 1996). Beyond three years after transplantation BMD does not change or may increase slightly but remains below values for the normal population (Grotz 1995). Fractures may occur early and affect patients with both low and normal BMD.
Immunosuppressive agents used in solid organ transplantation exert protean effects on bone metabolism (Torres 2002). Bone formation and mineralization lag times may be prolonged, suggesting an imbalance between bone formation and resorption because of osteoblastic dysfunction (Monier‐Faugere 2000). Glucocorticoids cause a substantial loss of trabecular bone in the initial months of treatment (Sambrook 1988), decrease calcium absorption and urinary calcium excretion, and exacerbate secondary hyperparathyroidism (Hahn 1981). Data regarding the effects of cyclosporin on bone function are conflicting although evidence suggests cyclosporin may contribute independently to lowered bone density following kidney transplantation (Heaf 2000). The roles of tacrolimus and sirolimus on bone metabolism do not extend beyond animal studies.
Description of the intervention
A number of agents are proven to treat and prevent osteoporosis in non‐transplant populations. Bisphosphonates, through their antiresorptive properties, are efficacious in the treatment steroid‐induced osteoporosis (Adachi 1997). Vitamin D metabolism is disturbed before and after kidney transplantation where half of patients show low blood levels of 1,25 dihydroxyvitamin D until six months after transplantation (De Sevaux 2002). Active vitamin D compound and calcium supplementation during this time reduces bone loss (Jeffery 2003). A meta‐analysis suggested 1,25 dihydroxyvitamin D (active vitamin D3, calcitriol) supplementation following kidney transplantation may be more efficacious in preventing vertebral fractures compared with no treatment, placebo or other vitamin D sterols with or without calcium supplementation (De Nijs 2004). Calcitonin has been proven to prevent recurrence of osteoporotic fractures in women with established osteoporosis (Chesnut 2000; Karachalios 2004) but data in patients receiving renal replacement therapy are absent. Following kidney transplantation female gender and post‐menopausal status are associated with an exaggerated risk of bone loss (Hung 1996). In non‐transplant populations, combined hormone replacement therapy has been shown to increase BMD in post‐menopausal osteoporosis (Grey 1994) and testosterone treatment reverses the deleterious effects of glucocorticoid drugs on bone mass in men (Reid 1996). The impact of gonadal hormone replacement following kidney transplantation is not characterised.
More recently denosumab, through inhibition of RANK ligand (RANKL)‐mediated osteoclast activation, has shown to be effective in the treatment of osteoporosis (Cummings 2009),with an equivalent efficacy to bisphosphonate (Brown 2009). Teriparatide, a recombinant parathyroid hormone (PTH), has proved to be efficacious in osteoporosis of both postmenopausal women (Neer 2001) and men (Orwoll 2003). Cinacalcet is a calcimimetic agent that has been shown to reduce intact PTH levels in patients with secondary hyperparathyroidism in the setting of CKD (Chonchol 2009), which may persist post‐kidney transplantation and contribute to osteoporosis. However, the efficacy of these agents in the treatment and prevention of osteoporosis in renal transplant recipients is largely unproven.
How the intervention might work
Bone loss occurs rapidly in the first 6 to 12 months after kidney transplantation. Contributing factors include pre‐existing bone disease related to kidney failure, immunosuppressive drugs, PTH activity, low serum phosphorus, and kidney transplant function (Weisinger 2006). In the absence of specific agents for the treatment and prevention of osteoporosis in the setting of CKD and post‐renal transplantation, treatments that have been proven in non‐transplant populations have been used to prevent and treat bone disease among kidney transplant recipients. The available drugs include bisphosphonate, vitamin D compounds, cinacalcet, calcitonin, testosterone, selective oestrogen receptor modulators, receptor activator of NF‐ĸB ligand (RANKL) inhibitors, synthetic human PTH, and treatments for acidosis such as potassium salts. Bone undergoes constant turnover; homeostasis is maintained through the balance of osteoblast activity (cells that generate bone matrix) and osteoclasts (cells that break down bone matrix). Each treatment acts on this complex bone remodelling process to either slow bone resorption or increase bone formation. Bisphosphonates inhibit osteoclast function by increasing programmed cell death (apoptosis); vitamin D compounds regulate circulating calcium and phosphorus concentrations and impacts on bone remodelling though increased bone resorption; RANKL inhibitors decrease RANKL‐induced osteoclast formation; synthetic human PTH increases the number and activity of osteoclasts; selective oestrogen receptor modulators (SERMs) act via the human transforming growth factor‐β3 gene, which regulates bone remodelling; cinacalcet mimics the action of calcium on tissues via activation of the calcium‐sensing receptors, increasing the sensitivity of calcium receptors on parathyroid cells to reduce PTH levels; calcitonin inhibits osteoclast activity and stimulates osteoblast activity; chronic acidosis changes the ionic composition of bone with reduced apatite, sodium and potassium and matrix gene expression with inhibition of osteoblast activity and increased osteoclastic function.
Why it is important to do this review
The wide variability in the causes of bone loss after kidney transplantation (low or high bone turnover, altered PTH function, steroid‐induced bone changes) suggests the possibility that treatments effective for osteoporosis in the wider population may not be directly applicable to the specific setting of kidney transplantation. In addition, treatments may exacerbate low bone turnover and increase complications of bone fragility and loss. Specialist guidelines regarding treatment of bone disease in kidney transplantation were previously based on uncontrolled data (Table 3 ‐ Published guidelines for bone disease in kidney transplant recipients) but randomised data is emerging specific to the treatment of bone disease in solid organ transplantation including among kidney transplant recipients. This Cochrane review update includes studies conducted during or before 2019 to determine the benefits and harms of treatments for bone disease in adults and children who have a kidney transplant and to identify areas requiring further study.
1. Published guidelines for bone disease in kidney transplant recipients.
| Guideline | Country | Year | Recommendation |
| Kidney Disease: Improving Global Outcomes (KDIGO) 2009 Clinical Practice Guideline for CKD Mineral and Bone Disorder (CKD‐MBD) (KDIGO CKD‐MBD Guideline 2009) |
International | 2009 | Serum concentrations of calcium, phosphorous and intact PTH should be monitored following transplantation. Serial 25(OH) vitamin D measurements should be considered. The lowest effective dose of glucocorticoids should be used. Recommend vitamin D deficiency and insufficiency be corrected. BMD measurement by DEXA scan is suggested within the first 3 months of transplantation if eGFR > 30 mL/min/1.73 m2 and patient is on corticosteroids or have risk factors for osteoporosis. In the first 12 months post transplantation, if eGFR > 30 mL/min/1.73 m2 and low BMD, suggest vitamin D, calcitriol/alpha calcidiol, or bisphosphonate be considered. Insufficient data to guide treatment after the first 12 months. Suggest BMD testing not performed routinely as BMD does not predict fracture risk or the type of transplant bone disease. |
| Kidney Disease: Improving Global Outcomes (KDIGO) 2009 Clinical Practice Guideline for the Care of Kidney Transplant (KDIGO Transplant Guideline 2009) |
International | 2009 | See Kidney Disease: Improving Global Outcomes (KDIGO) 2009 Clinical Practice Guidelines for CKD Mineral and Bone Disorder (CKD‐MBD) (KDIGO CKD‐MBD Guideline 2009) |
| Kidney Disease Outcome Quality Initiative (K‐DOQI) (KDOQI 2010) |
United States of America | 2010 |
Commentary on 2009 KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of CKD‐Mineral and Bone Disorder (CKD‐MBD) Serum concentrations of calcium, phosphorous and intact PTH should be monitored following transplantation. Serial 25(OH) vitamin D measurements should be considered. The lowest effective dose of glucocorticoids should be used. Recommend vitamin D deficiency and insufficiency be corrected. BMD measurement by DEXA scan is restricted to high risk populations including those receiving significant doses of corticosteroids or those with risk factors for osteoporosis in the general population. Bone density screening is suggested only for individuals with a well‐functioning transplant. Patients with more advanced CKD will more likely have abnormal bone quality from CKD mineral and bone disorder which is likely to compromise the ability of BMD to predict fracture. In the first 12 months post transplantation, if eGFR > 30 mL/min/1.73 m2 and low BMD, suggest vitamin D, calcitriol/alpha calcidiol, or bisphosphonate be considered, although due to the relative lack of evidence, treatment is discretionary. Insufficient data to guide treatment after the first 12 months. There is insufficient evidence to support treatment recommendations for bone disease in children. It is reasonable to consider bone biopsy to guide treatment, particularly before using bisphosphonate because these agents have better efficacy in high bone turnover and may lead to adynamic bone disease. |
| Caring for Australians with Renal Impairment (CARI) (Chadban 2009) |
Australia and New Zealand | 2009 | Kidney transplant recipients should be advised to take a vitamin D (or analogue) supplement at a low dose of at least 0.25 µg daily. Commentary on 2009 KDIGO Clinical Practice Guideline for the Care of Kidney Transplant Recipients No specific comment on 2009 KDIGO guidelines for care of kidney transplant recipients. |
| Canadian Society of Nephrology (CSN) (Knoll 2010) |
Canada | 2010 |
Commentary on 2009 KDIGO Clinical Practice Guideline for the Care of Kidney Transplant recipients No evidence for benefit resulting from supplementation to "sufficient" levels of serum 25 hydroxyvitamin D (> 75 nmol/L) and the clinical harm has not been defined. Bone biopsy is rarely available. In patients who have no biochemical evidence of CKD bone and mineral disorder, it is reasonable to assess and treat patients for their future fracture risk according to guidelines for the general population. management would include routine supplementation with vitamin D (800 to 2,000 U daily) and calcium (1000 to 15,000 mg daily) with specific pharmacotherapy based on overall risks of fracture, including bisphosphonate therapy when appropriate. Bone density should not be measured routinely to form the basis of diagnostic and therapeutic decisions. |
| European Best Practice Guidelines (EPBG) (ERBP 2011) |
Europe | 2011 |
Endorsement of the 2009 KDIGO Clinical Practice Guideline for Care of Kidney Transplant Recipients Endorsement of the 2009 KDIGO guidelines for care of kidney transplant recipients (KDIGO CKD‐MBD Guideline 2009) (no specific commentary on bone disease management). |
| British Renal Association (Baker 2010) |
United Kingdom | 2010, 2011 |
Post‐operative care of the kidney transplant recipient: bone and joint disease (Baker 2017) Recipients of kidney transplantation with osteoporosis or high risk should be considered for steroid‐avoiding immunosuppression. Recipients of a kidney transplant should undergo bone density measurement if eGFR > 30 mL/min/1.73 m2. Treatment should be according to the Royal College of Physicians guidelines for steroid induced osteoporosis. Commentary on 2009 KDIGO Clinical Practice Guideline for the Care of Kidney Transplant recipients The recommendations on transplant bone disease are derived from the KDIGO guideline on the diagnosis, evaluation, prevention and treatment of Chronic Kidney Disease‐Mineral and Bone Disorder (CKD‐MBD). The widespread use of DEXA scanning is not recommended since it predicts neither the occurrence of fractures nor the type of bone disease. |
Objectives
To evaluate the benefits and harms of interventions for preventing bone disease following kidney transplantation.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs) and quasi‐RCTs (RCTs in which allocation to treatment was obtained by alternation, use of alternate medical records, date of birth or other predictable methods) evaluating interventions for bone disease following kidney transplantation were included. The first period of randomised cross‐over studies was also included.
Types of participants
Inclusion criteria
Studies involving recipients of a kidney transplant were eligible. We included patients who received treatment at the time of transplantation (incident treatment) and those who received treatment at any time in the post‐transplantation period (prevalent treatment). Studies enrolling adults and children were included. Participants receiving any immunosuppression regimen following transplantation were included.
Exclusion criteria
Recipients of any transplant other than a kidney transplant were excluded (multi‐organ transplant recipients).
Types of interventions
Interventions for bone disease included bisphosphonate (parenteral and oral including alendronate, etidronate, ibandronate, pamidronate, risedronate, zolendronate), vitamin D compound, calcitonin, and gonadal hormone replacement, selective oestrogen receptor modulators, fluoride, anabolic steroids, RANK ligand antagonist (denosumab), recombinant PTH (teriparatide), calcimimetic (cinacalcet), and electrolyte supplements (including potassium citrate used in the context of metabolic acidosis). Study participants could also be taking any form of calcium supplementation and/or vitamin D compound in addition to active treatment or placebo. Studies comparing active treatment against placebo and studies where two or more active treatment modalities are compared were included. Interventions for bone disease given either prior to planned transplantation or in the post‐transplant period were eligible. Any duration of treatment and any mode of administration were included. Examination of the effect of modulation of immunosuppression regimens on bone disease was beyond the scope of this review.
Types of outcome measures
Primary outcomes
The primary efficacy outcome was fracture identified by radiographic examination
The primary safety outcome was acute graft rejection.
Secondary outcomes
Secondary efficacy outcomes
Death: all causes, cardiovascular
Cardiovascular events: myocardial infarction, stroke
Musculoskeletal disorders: bone pain, avascular necrosis, spinal deformity, height loss, arthralgia, myalgia, muscle cramps
BMD: measured by dual‐energy X‐ray absorptiometry using T‐scores or Z‐scores at the lumbar spine, femoral neck, hip bone and radius
Percentage changes in BMD by dual‐energy X‐ray absorptiometry using BMD score, T‐scores, or Z‐scores at the lumbar spine and femoral neck
Low bone turnover seen on bone histomorphometry (as defined by reduced bone formation rate as a function of either tissue volume or bone volume)
Serum PTH
Parathyroidectomy
Urine protein or albumin excretion
Vascular calcification score.
Secondary safety outcomes
Graft loss
Graft function: serum creatinine (SCr); estimated glomerular filtration rate (eGFR); measured GFR
Any gastro‐oesophageal disorder: oesophagitis, oesophageal ulcer, oesophageal stricture, oesophageal erosions, dysphagia, gastric bleeding, duodenitis or ulceration
Gastrointestinal symptoms: nausea, vomiting, diarrhoea
Hypersensitivity reactions
Hyper‐ or hypocalcaemia
Hyper‐ or hypophosphataemia
Fever
Mean haemoglobin
Leucopenia
Neuropsychiatric disorder
Venous thromboembolism
Oedema
Hot flushes.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Kidney and Transplant Specialised Register up to 16 May 2019 through contact with the Information Specialist using search terms relevant to this review. The Cochrane Kidney and Transplant Specialised Register contains studies identified from:
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL)
Weekly searches of MEDLINE OVID SP
Handsearching of kidney‐related journals and the proceedings of major kidney conferences
Searching of the current year of EMBASE OVID SP
Weekly current awareness alerts for selected kidney and transplant journals
Searches of the International Clinical Trials Register (ICTRP) Search Portal and ClinicalTrials.gov.
Studies contained in the Specialised register are identified through search strategies for CENTRAL, MEDLINE and EMBASE based on the scope of Cochrane Kidney and Transplant. Details of these strategies, as well as a list of handsearched journals, conference proceedings and current awareness alerts, are available in the Specialised Register section of information about Cochrane Kidney and Transplant.
See Appendix 1 for search terms used in strategies for this review.
Searching other resources
Reference lists of review articles, relevant studies and clinical practice guidelines
Contact experts/organisations in the field seeking information about unpublished or incomplete studies
Grey literature sources (e.g. abstracts, dissertations and theses), additional to those already included in the Cochrane Kidney and Transplant Register of Studies, were not be searched.
Data collection and analysis
Selection of studies
The original review in 2005 and the 2007 review update was conducted by three authors (SP, GS, DM). The 2019 review update has been undertaken by five authors (EC, SP, DM, FB, GS). In the 2019 update, the retrieved titles and abstracts were screened independently by two authors who discarded citations that were not applicable. Studies and reviews that included relevant data or information on trials were retained initially. Two authors independently assessed, retrieved abstracts and, where necessary, the full text of these articles to identify eligible studies.
Data extraction and management
Data extraction was carried out independently using standardised data extraction forms. Studies reported in a non‐English language journal were identified and translated versions were obtained through correspondence with the authors. When more than one publication of a study existed, reports were grouped together and the publication with the most complete data was included. Disagreements were resolved in consultation with the senior author who provided methodological assistance through the review process. Two authors were responsible for final data entry.
Assessment of risk of bias in included studies
The following items were independently assessed by two authors using the risk of bias assessment tool (Higgins 2011) (see Appendix 2).
Was there adequate sequence generation (selection bias)?
Was allocation adequately concealed (selection bias)?
-
Was knowledge of the allocated interventions adequately prevented during the study?
Participants and personnel (performance bias)
Outcome assessors (detection bias)
Were incomplete outcome data adequately addressed (attrition bias)?
Are reports of the study free of suggestion of selective outcome reporting (reporting bias)?
Measures of treatment effect
For dichotomous outcomes (e.g., fracture, graft loss, all‐cause mortality, acute graft rejection, adynamic bone disease, and adverse effects of treatment) results were expressed as risk ratio (RR) with 95% confidence intervals (CI). Where continuous scales of measurement were used to assess the effects of treatment (e.g. BMD by DEXA scanning, mean SCr at the end of treatment, mean haemoglobin at the end of treatment) the mean difference (MD) was used, or the standardised mean difference (SMD) if different scales of measurement were used.
Unit of analysis issues
Studies with non‐standard designs were analysed in this review including cross‐over RCTs, studies with more than two interventions, and cluster RCTs.
Cross‐over studies
Cross‐over studies were eligible for this meta‐analysis. However, as carry‐over of the dietary intervention given in the first period was likely to persist into subsequent treatment periods due to behaviour modification and extended treatment effects, we only included data for end points reported during the first period of study in which the order of receiving treatments was randomly allocated.
Studies with more than two interventions
Studies with multiple interventions were included. When a study was a 'multi‐arm' study, and all treatment arms provided data for eligible interventions, the study was included in this review. If there were adequate data from the study, then the treatment arms relevant to the treatment comparisons of interest were included in applicable meta‐analyses.
Cluster randomised studies
We planned to include information from cluster randomised studies. We planned to divide the effective sample size for each data point by a quantity called the design effect calculated as 1 + (M ‐ 1) ICC, where M was the average cluster size and ICC was the intra‐cluster correlation coefficient. In this calculation, a common design effect was assumed across all intervention groups. The intra‐cluster coefficient (ICC) is seldom available in published reports. We therefore planned to adopt a common approach to use external estimates obtained from similar studies. For dichotomous outcomes, we planned to divide the number of participants and the number experiencing the event by the design effect. For continuous endpoints only the sample size was planned to be divided by the design effect with means and standard deviations remaining unchanged. There were no cluster randomised studies that met the eligibility criteria for the review.
Dealing with missing data
Any further information required from the original authors of eligible studies was requested by written correspondence and any relevant information obtained in this manner was included in the review including clarification of possible secondary publication.
Assessment of heterogeneity
We will first assess the heterogeneity by visual inspection of the forest plot. We will quantify statistical heterogeneity using the I2 statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than sampling error (Higgins 2003). A guide to the interpretation of I2 values will be as follows:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity
The importance of the observed value of I2 depends on the magnitude and direction of treatment effects and the strength of evidence for heterogeneity (e.g. P‐value from the Chi2 test, or a confidence interval for I2) (Higgins 2011).
Assessment of reporting biases
If possible, funnel plots were used to assess for the potential existence of small study bias in meta‐analyses containing ten or more studies and in the absence of statistical heterogeneity (Higgins 2011).
Data synthesis
Treatment effects were summarised by random effects meta‐analysis.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was used to explore possible sources of heterogeneity. Subgroup analysis was carried out to explore treatment estimates for bisphosphonate versus placebo or no treatment based on the following.
Incident or prevalent transplant populations
Duration of treatment (6 months or less; > 6months)
Adults or children
Primary or secondary prevention of bone disease
Allocation concealment (low risk; high or unclear risk).
Sensitivity analysis
We planned sensitivity analyses repeating analyses taking account of risk of bias (allocation concealment), however there were either insufficient data observations or sufficient studies with low risks of bias to perform these analyses.
'Summary of findings' tables
We presented the main results of the review in a 'Summary of findings' tables for the comparisons of bisphosphonate or vitamin D therapy versus placebo or no treatment. These tables present key information concerning the quality of the evidence, the magnitude of the effects of the interventions examined, and the sum of the available data for the main outcomes (Schunemann 2011a). The 'Summary of findings' tables also included an overall grading of the evidence related to each of the main outcomes using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach (GRADE 2008). The GRADE approach defines the quality of a body of evidence as the extent to which one can have certainty that an estimate of effect or association is close to the true quantity of specific interest. The certainty one has in a body of evidence involves consideration of within‐trial risk of bias (methodological quality), directness of evidence, heterogeneity, precision of effect estimates and risk of publication bias (Schunemann 2011b). We presented the following outcomes in the 'Summary of findings' tables.
Primary efficacy outcome
Fracture
Primary safety outcome
Acute graft rejection
Secondary outcomes
Death (all causes)
Cardiovascular death
Bone pain
Spinal deformity
Hyper‐ or hypocalcaemia
Results
Description of studies
Results of the search
The flow of literature searching and identification of eligible studies in this review including the original published review in 2004 and in review updates published in 2007 and 2017 is shown in Figure 1.
1.
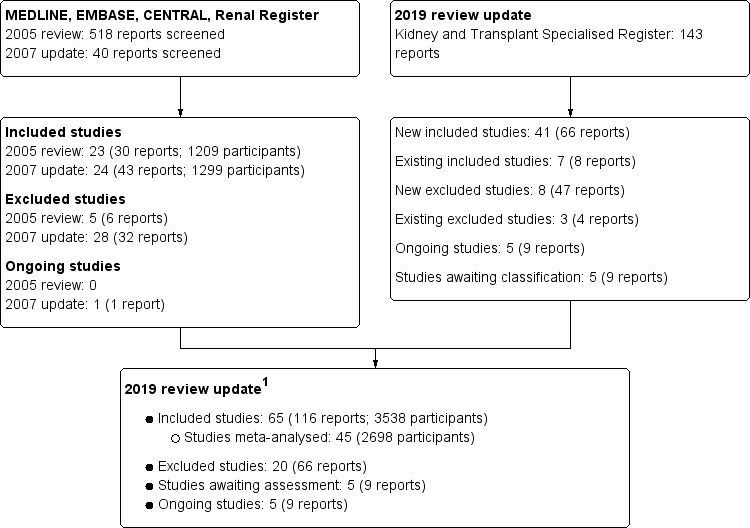
Flow chart of study identification and selection procedure (2019 update)
1Numbers of studies and participants differ slightly from previous versions of this review due to updated data in new publications, reclassification of studies as included/excluded and removal of non‐randomised studies.
Original review (2004)
In the original review, the search was conducted in 2004. Overall, 636 records were identified in the search (84 citations were retrieved from MEDLINE; 383 citations from EMBASE; and 169 from the Cochrane Renal Group Specialised Register). The number of potentially relevant citations identified after removal of overlapping records identified in more than one database was 518, of which 482 were excluded after screening based on review of the title and abstract. The major reasons for exclusions at this stage of screening were a non‐randomised design, non‐bone disease related interventions, duplicate publications, and a lack of empirical data.
Full‐text analysis of the remaining 36 publications identified 30 eligible records. Of the six records that were excluded, four were not randomised, one enrolled pancreas‐kidney transplant recipients and one was a duplicate publication. Following the exclusion of interim/early reports of main publications, 22 RCTs (30 publications involving 1209 participants), published as full articles or in abstract form, were identified and included in this review (Coco 2003; Cueto‐Manzano 2000; De Sevaux 2002; Eid 1996, El‐Agroudy 2003a; El‐Husseini 2004; Fan 2000; Giannini 2001; Grotz 1998; Grotz 2001; Haas 2003; Jeffrey 2003; Koc 2002; Nam 2000; Neubauer 1984; Nordal 1995; Psimenou 2002; Sharma 2002a; Tałałaj 1996; Torregrosa 2003; Torres 2004; Ugur 2000). Supplementary data were requested from authors of all trials. Authors of eight trials replied to our requests for unpublished data (Coco 2003; De Sevaux 2002; El‐Agroudy 2003a; Fan 2000; Jeffrey 2003; Koc 2002; Torregrosa 2003; Torres 2004).
Review update (2007)
A further search of the Cochrane Kidney and Transplant Specialised Register between 2004 and 2006 identified eight additional records. During full text analysis of these citations, one further RCT was included (Wissing 2005). Six publications provided additional information for studies that had been included in the 2004 review (Coco 2003; El‐Agroudy 2003a; El‐Husseini 2004) or were duplicate publications. One record was excluded as it concerned non‐transplant participants (Raggi 2004). There were 23 studies involving 1260 participants in the review update in 2007.
Review update (2019)
Searches of the Cochrane Kidney and Transplant specialised register were conducted in 2013, 2017 and 2019. These searches identified 143 new reports. Full text review of these reports identified 41 new studies (66 reports): eight reports of seven existing included studies; eight new excluded studies (47 reports); four reports of three existing excluded studies; five reports of five ongoing studies (NCT00748618; NCT00889629; NCT02224144; VITA‐D 2009; VITALE 2014); and, prior to publication, nine reports of five studies which will be assessed in a future update of this review (Jorge 2016; Marques 2019; NCT01675089; Oblak 2017; Tiryaki 2018).
A total of 65 studies involving 3538 randomised participants were included in this review update. Twenty studies could not be included in our meta‐analyses (did not report extractable data; did not report outcomes relevant to this review) (Chalopin 1987; Eid 1996; El‐Husseini 2005a; Fujii 2006; Lord 2001a; Marcen 2010; Montilla 2001; Nakamura 2009a; Nam 2000; Narasimhamurthy 2014; Oliden 2012; Omidvar 2011; Peeters 2001; Praditpornsilpa 2014; Sanchez‐Escuredo 2015; Shahidi 2011; Sirsat 2010; Thervet 2008; Tiryaki 2015; Ugur 2000). Therefore, the total number of studies that contributed to our analyses was 45 (2698 participants).
Authors of two studies replied to our requests for unpublished data or published data from studies reported in languages other than English (Cruzado 2015; Kharlamov 2012).
For this review update non‐RCTs have been deleted from excluded studies.
Included studies
Characteristics of included studies
The timing and duration of the evaluated treatments is described in Table 4. Studies were conducted in Europe (37 studies), the Americas (8 studies), the Middle East (9 studies), Asia (9 studies), was multinational (1 study), or was not stated (1 study). Follow up for clinical outcomes was 6 months or fewer in 17 studies, 12 months in 31 studies and between 13 and 36 months in five studies.
2. Treatment timing and duration.
| Study | Donor | Primary outcome | Intervention | Dose | Timing since transplantation | Duration of treatment or follow up | Risk factors for fracture in participant selection criteria (exclusions) |
| Bisphosphonates (in order of drug potency from low to high) | |||||||
|
Psimenou 2002 (adults) |
‐‐ | BMD | Etidronate | 200 mg/d for 15 days every 3 months | ‐‐ | 12 months | Low BMD; mean T‐scores < ‐2.7 at baseline (no exclusions specified) |
|
Grotz 1998 (adults) |
‐‐ | BMD | Clodronate | 800 mg/d | > 6 months | 12 months | BMD < 1.5 SD of normal; > 6 months after transplantation (no exclusions specified) |
|
Montilla 2001 (adults) |
‐‐ | BMD | Pamidronate | 200 mg twice/d | ‐‐ | 12 months | Long‐term kidney transplant recipients with severe osteopenia or osteoporosis (no exclusions specified) |
|
Fan 2000 (men) |
Deceased | BMD | Pamidronate | 0.5 mg/kg at time of transplantation and 1 month | Immediately pre‐transplant | 12 months | No risk factors specified. Incident population (women excluded) |
|
Nam 2000 (adults) |
‐‐ | BMD | Pamidronate | 30 mg every 4 weeks | 2 weeks | 6 months | No risk factors specified. Incident population (no exclusions specified) |
|
Coco 2003 (adults) |
Living and deceased | Bone histomorphometry and BMD | Pamidronate | 60 mg at transplantation and 30 mg at 1, 2, 3 and 6 months | 48 hours | 12 months | No risk factors specified. Incident population (excluded if unstable transplant function) |
|
Walsh 2009 (adults) |
‐‐ | BMD | Pamidronate | 1 mg/kg within 14 to 19 days of transplant, 1, 4, 8, 12 months after transplant | < 14 to 19 days | 12 months | Serum PTH level > 150 pg/mL (no exclusions specified) |
|
Torregrosa 2011 (adults) |
‐‐ | BMD | Pamidronate | 30 mg between day 7 to 10 and 3 months | 5 to 7 days | 12 months | T‐score < ‐1 at lumbar spine. (excluded if CrCl < 30 mL/min; corticosteroids > 3 months before transplantation) |
|
Sirsat 2010 (adults) |
‐‐ | BMD | Pamidronate | 60 mg at baseline and 6 months post transplant | ‐‐ | 1 year | Kidney transplant recipients (no exclusions reported) |
|
Shahidi 2015 (adults) |
Living | BMD | Pamidronate | 30 mg within 2 days and at 3 months | < 2 days | 12 months | No risk factors specified. Incident population (excluded if previous parathyroidectomy; corticosteroids > 3 months duration before transplantation) |
|
Omidvar 2011 (adults) |
‐‐ | BMD | Alendronate or pamidronate | 70 mg/week; 90 mg/month | 3 weeks | 6 months | T‐score < ‐2 (excluded if history of hyperparathyroidism, hypocalcaemia, hypercalcaemia; fracture within 2 years; CrCl < 35 mL/min) |
|
Giannini 2001 (adults) |
Deceased | BMD and bone biomarkers | Alendronate | 10 mg/d | > 6 months | 12 months | > 6 months after transplantation. Deceased donor kidney (excluded if antiresorptive drugs or bisphosphonate therapy) |
|
Koc 2002 (adults) |
‐‐ | BMD | Alendronate | 10 mg/d | 46.2 months on average | 12 months | Long‐term transplantation (46.2 months average) (excluded if diabetes; hyperparathyroidism; gonadal insufficiency; parathyroidectomy; other cause of osteoporosis) |
|
Sharma 2002a (adults) |
‐‐ | BMD | Alendronate | 10 mg/d | At time of transplantation | 6 months | No risk factors specified. Incident population (no exclusions specified) |
|
El‐Agroudy 2003a (men) |
Living | BMD | Alendronate | 5 mg/d | < 1 week | 12 months | No risk factors specified. Incident population (excluded if diabetes; steroids received before transplantation; HD > 2 years; SCr > 2 mg/dL; previous fractures; presence of other endocrine abnormalities) |
|
Jeffery 2003 (adults) |
Living and deceased | BMD | Alendronate | 10 mg/d | 8.5 to 9 years | 12 months | T‐score ≤ ‐1 (excluded if CrCl < 35 mL/min; unstable kidney function; hormonal replacement therapy; treated for symptomatic osteoporosis) |
|
Torregrosa 2003 (adults) |
‐‐ | BMD | Alendronate | 10 mg/d | 12 to 24 months | 12 months | T‐score < ‐2.5; SCr < 176.8 µmol/L; PTH < 240 pg/mL (excluded if diabetes) |
|
El‐Husseini 2004 (children and adolescents) |
Living | BMD | Alendronate | 5 mg/d | 48 months on average | 12 months | T‐score ≤ ‐1; SCr < 220 mmol/L (no exclusions specified) |
|
Nayak 2007 (adults) |
‐‐ | BMD | Alendronate | 35 mg/week | After stabilization of kidney function | 6 months | No risk factors specified. Incident population (excluded if bone disease or long‐term immunosuppressive therapy before onset of kidney failure) |
|
Lan 2008 (adults) |
‐‐ | BMD and bone biomarkers | Alendronate | 70 mg/week | > 12 months | 6 months | T‐score < ‐1; >1 year after transplantation (excluded if diabetes; liver disease; intake of vitamin D or analogues after transplantation) |
|
Sirsat 2010 (adults) |
‐‐ | BMD | Alendronate | 70 mg/week | ‐‐ | 1 year | Kidney transplant recipients (no exclusions specified) |
|
Trabulus 2008 (adults) |
Living and deceased | BMD | Alendronate or alendronate + alfacalcidol | 10 mg/d ± 0.5 µg/d | 37.3 to 49.7 months on average | 12 months | SCr < 124 µmol/L (excluded if post‐menopausal; oestrogen therapy; osteoporosis secondary to diabetes; hyperthyroidism; primary or tertiary hyperparathyroidism; hypogonadism; hyperprolactinaemia; Cushing's syndrome; acromegaly; diarrhoea; malabsorption syndromes) |
|
Dovas 2009 (adults) |
‐‐ | BMD | Alendronate + alfacalcidol | 70 mg weekly + 0.25 µg alternate daily | At transplantation | 24 months | Unselected patients (no exclusions specified) |
|
Okamoto 2014 (adults) |
‐‐ | BMD and vascular calcification score | Alendronate | 35 mg/week | > 12 months (mean 45.3 to 59.6 months) | 24 months | SCr < 176 µmol/L; stable graft function (no exclusions specified) |
|
Lord 2001a (adults) |
‐‐ | Fracture, BMD | Alendronate + Vitamin D + calcium | 5 mg/d | ‐‐ | 2 years | Kidney transplant recipients (excluded if aged 18 years (?); more than 1 kidney transplant; severe hyperparathyroidism or osteoporosis) |
|
Nakamura 2009a (adolescents and adults) |
‐‐ | BMD | Alendronate | ‐‐ | ‐‐ | 6 to 12 months | Kidney transplant recipients > 16 years with good kidney function (no exclusions specified) |
|
Grotz 2001 (adults) |
‐‐ | BMD | Ibandronate | 1 mg before transplantation and 2 mg at 3, 6, and 9 months | Immediately pre‐transplant | 12 months | No risk factors specified. Incident population (excluded combined kidney pancreas transplant recipients) |
|
Smerud 2012 (adults) |
Living or deceased | BMD | Ibandronate | 3 mg every 3 months | 18.5 days on average | 12 months | Stable kidney function (eGFR > 30 mL/min/1.73 m2; plasma calcium < 2.55 mmol/L). Incident population (excluded if adynamic bone disease; previous parathyroidectomy, use of bisphosphonate within previous 1 year; medications including sodium fluoride; calcitonin; strontium; PTH; selective oestrogen receptor modulators; growth hormone; anabolic steroids) |
|
Sanchez‐Escuredo 2015 (adults) |
‐‐ | BMD | Risedronate or ibandronate | 35 mg/week or 150 mg/month | > 12 months (mean 18 to 20 months) | 12 months | Minimum 12 months after transplantation. Serum PTH > 60 pg/mL; T‐score < 1; CrCl > 30 mL/min/1.73 m2 (excluded if diabetes; primary hyperthyroidism) |
|
Coco 2012 (adults) |
Living | BMD | Risedronate | 35 mg dose | Given when SCr < 2.0 mg/dL after transplantation | 12 months | Living donor transplantation. Incident population (no exclusions specified) |
|
Torregrosa 2007 (adults) |
‐‐ | Fracture, pain, and BMD | Risedronate | 35 mg/week | 12 to 36 months (21 to 23 months) | 12 months | T‐score < ‐1; SCr < 221 µmol/L; iPTH > 60 pg/mL (excluded if diabetes) |
|
Torregrosa 2010 (adults) |
‐‐ | BMD | Risedronate | 35 mg/week | At time of transplantation | 12 months | No risk factors specified. Incident population (excluded if insulin treatment; parathyroidectomy; fluorine, bisphosphonate, hormone therapy (oestrogen, selective modulator of oestrogen receptor), calcitonin therapy; PTH < 50 pg/mL) |
|
Fujii 2006 (adults) |
‐‐ | BMD | Risedronate | 2.5 mg/d | 11 ± 6 years | 2 years | Long‐term kidney transplant recipients; eGFR 64 ± 31 mL/min/1.73 m2; T‐score of ‐2.0 ± 0.9 at the lumbar spine (no exclusions specified) |
|
Haas 2003 (adults) |
Deceased | BMD | Zolendronate | 4 mg at 0 and 3 months | < 2 weeks | 6 months | Deceased donor transplantation. Incident population (excluded if treatment with calcitonin, bisphosphonate; hypocalcaemia) |
| Vitamin D | |||||||
|
Marcen 2010 (unknown) |
‐‐ | iPTH | Cholecalciferol + calcium supplements | 400 IU/d | ‐‐ | 6 to 12 months | Kidney transplant recipients with vitamin D insufficiency or deficiency (no exclusions reported) |
|
Thervet 2008 (unknown) |
‐‐ | PTH | Cholecalciferol | 100,000 U every 2 months initiated 4 months post transplant | 4 months | 12 months | Kidney transplant recipients; vitamin D < 30 ng/mL; calcium < 35 mmol/L (no exclusions specified) |
|
Thervet 2008 (unknown) |
‐‐ | PTH | Cholecalciferol | 100,000 U every 2 months initiated 6 months post transplant | 6 months | 12 months | Kidney transplant recipients; vitamin D < 30 ng/mL; calcium < 35 mmol/L (no exclusions specified) |
|
Wissing 2005 (adults) |
Living and deceased | BMD | Vitamin D3 | 25,000 IU/month | 1 week | 12 months | No risk factors specified. Incident population (excluded if serum calcium > 10.5 mg/dL; hypocalcaemia requiring treatment with active vitamin D compounds; multiorgan transplant) |
|
Tałałaj 1996 (adults) |
‐‐ | BMD | 25‐hydroxy vitamin D and calcium carbonate | 40 µg/d; 3000 mg/d | 25 to 26 months | 12 months | No risk factors specified (no exclusions specified) |
|
Praditpornsilpa 2014 (unknown) |
‐‐ | iPTH | Calcidiol | 20,000 IU/week | ‐‐ | ‐‐ | Kidney transplant recipients (no exclusions specified) |
|
De Sevaux 2002 (adults) |
Living and deceased | BMD | 1‐alpha‐hydroxy vitamin D + calcium | 0.25 µg/d 1000 mg/d |
< 1 month | 6 months | No risk factors specified. Incident population (excluded if corticosteroid treatment within 3 months of transplantation; total parathyroidectomy; treatment with bisphosphonates, fluoride, calcitonin, or anabolic steroids; serum calcium >2.80 mmol/L) |
|
El‐Agroudy 2003a (men) |
Living | BMD | Alfacalcidol | 0.5 µg/d | < 1 week | 12 months | No risk factors specified. Incident population (excluded if diabetes; steroids received before transplantation; HD > 2 years; SCr > 2 mg/dL; previous fractures; presence of other endocrine abnormalities) |
|
El‐Husseini 2004 (children and adolescents) |
Living | BMD | Alfacalcidol | 0.25 µg/d | 48 months on average | 12 months | T‐score ≤ ‐1 (excluded if anticonvulsant therapy or thiazide diuretic treatment) |
|
El‐Husseini 2005a (children and adolescents) |
‐‐ | BMD | Alfacalcidol | 0.25 µg/d | ‐‐ | 12 months | Kidney transplant recipients with low BMD (Z‐score ≤ ‐1) (no exclusions reports) |
|
Trabulus 2008 (adults) |
Living and deceased | BMD | Alfacalcidol | 0.5 µg/d | 37.3 to 49.7 months on average | 12 months | SCr < 1.4 mg/dL; stable graft function (excluded if post‐menopausal, oestrogen therapy; secondary osteoporosis due to type I or II diabetes; hyperthyroidism; hypogonadism; hyperprolactinaemia; Cushing's syndrome; acromegaly; chronic diarrhoea; malabsorption syndrome) |
|
Nakamura 2009a (adolescents and adults) |
‐‐ | BMD | Alfacalcidol | ‐‐ | ‐‐ | 6 to 12 months | Kidney transplant recipients > 16 years with good kidney function (no exclusions specified) |
|
Shahidi 2011 (adults) |
‐‐ | BMD | Calcitriol or vitamin D | ‐‐ | Immediately prior to transplantation | 12 months | Inclusion and exclusion criteria not reported in abstract |
|
Neubauer 1984 (adults) |
Deceased | Bone mineral content | Calcitriol | 0.25 µg/d | 8 weeks | 18 months | Deceased donor transplantation. Incident population (excluded if SCr > 1.8 mg/dL; hypercalcaemia; systemic disease) |
|
Eid 1996 (women) |
‐‐ | BMD | Calcitriol | 0.25 µg/d | Not described | 36 months | Post‐menopausal women (no exclusions specified) |
|
Messa 1999 (adults) |
‐‐ | Serum PTH | Calcitriol | 0.008 µg/kg/d | At transplantation | 6 months | Kidney transplantation (no exclusions specified) |
|
Tiryaki 2015 (adults) |
‐‐ | Albuminuria | Calcitriol | 0.25 mg/d | ‐‐ | 24 weeks | Hypertension; chronic allograft nephropathy; albuminuria (no exclusions specified) |
|
Cueto‐Manzano 2000 (adults) |
Living and deceased | BMD | Calcitriol + calcium carbonate | 0.25 µg/d 500 mg/d |
> 2 years | 12 months | Kidney transplantation > 2 years; stable graft function; SCr <2.0 mg/dL; normal dietary intake (excluded if previous vertebral or hip fracture; prolonged immobilisation; systemic illness; malignancy; oestrogen therapy; drugs affecting bone metabolism) |
|
Nam 2000 (adults) |
‐‐ | BMD | Calcitriol | 0.5 µg/d | 2 weeks | 6 months | Incident population (no exclusions specified) |
|
Ugur 2000 (adults) |
‐‐ | BMD | Calcitriol | 0.5 µg/d | > 12 months | 12 months | T‐score < ‐1; transplantation > 12 months (no exclusions specified) |
|
Giannini 2001 (adults) |
Deceased | BMD | Calcitriol | 0.25 µg/d | > 6 months | 12 months | Deceased donor transplantation; kidney transplantation > 6 months (excluded if previous treatment with bisphosphonates or other antiresorptive drugs) |
|
Koc 2002 (adults) |
‐‐ | BMD | Calcitriol | 0.5 µg/d | < 12 months | 12 months | Long‐term transplantation (46.2 months average) (excluded if diabetes; hyperparathyroidism; gonadal insufficiency; parathyroidectomy; other cause of osteoporosis) |
|
Torres 2004 (adults) |
‐‐ | BMD | Calcitriol | 0.5 µg/48 hours | At time of transplantation | 12 months | First or second kidney transplant (excluded is previous parathyroidectomy) |
|
Arnol 2011 (adults) |
‐‐ | Proteinuria | Paricalcitol | 2 µg/d | ≥ 3 months | 24 weeks | Kidney transplant > 3 months; UPCR ≥ 20 mg/mmol (no exclusions specified) |
|
Kharlamov 2012 (adults) |
Deceased | Chronic allograft nephropathy | Paricalcitol or calcitriol or vitamin D supplement | 2‐4 µg/d 1 to 6 µg/d 1200 to 1800 IU |
Day 5 after transplant | 6 months | Vitamin D deficiency (25(OH)D < 40 nmol/L) (excluded if acute illness; endocrinologic disease including diabetes; hyperparathyroidism; other thyroid disorders; need for dialysis) |
|
Oliden 2012 (adults) |
Living and deceased | PTH | Paricalcitol versus calcitriol | 2 µg/d 0.25 mg/d |
50 to 120 months | 24 weeks | GFR < 60 mL/min; secondary hyperparathyroidism (excluded if PTH < 110 pg/mL; corrected calcium > 10.5 mg/dL; serum phosphorus > 5.5 mg/dL) |
|
Amer 2013 (adults) |
Living and deceased | PTH | Paricalcitol | 2 µg/d | At transplantation | 12 months | First or second kidney transplant; eligible for steroid avoidance protocol (excluded if prior hypercalcaemia; total 25‐hydroxyvitamin D < 10 ng/mL; multiple organ transplant; receiving calcimimetic before transplant) |
|
Perez 2010 (adults) |
‐‐ | Bone mineral parameters, kidney function and inflammatory markers | Paricalcitol | 1 µg/d | ‐‐ | 12 months | Stable kidney transplant (no exclusions specified) |
|
Trillini 2015 (adults) |
‐‐ | PTH | Paricalcitol | 1 to 2 µg/d | 92.2 months on average | 6 months | Serum PTH > 80 pg/mL; 1‐month washout with previous vitamin D compounds; serum calcium ≤ 10.2 mg/dL; SCr < 2 mg/dL (excluded if vitamin D analogue therapy; changes in SCr > 30%; acute rejection episode over previous 6 months) |
|
Pihlstrom 2017 (adults) |
Living and deceased | Albuminuria | Paricalcitol | 2 µg/d | 7 to 8 weeks | 44 weeks | Kidney transplant or combined kidney‐pancreas transplant; eGFR > 30 mL/min; plasma calcium 2.0 to 2.6 mmol/L (excluded previous total parathyroidectomy; ongoing treatment with vitamin D, VDRA, or calcimimetic drugs; severe osteoporosis in axial skeleton; donor age > 75 years) |
|
Lord 2001a (adults) |
‐‐ | Fracture, BMD | Vitamin D + calcium | ‐‐ | ‐‐ | 2 years | Kidney transplant recipients (excluded if aged 18 years (?); more than 1 kidney transplant; severe hyperparathyroidism or osteoporosis) |
| RANKL inhibitor | |||||||
|
POSTOP 2014 (adults) |
Living and deceased | BMD | Denosumab | 60 mg at baseline and 6 months | 2 weeks | 12 months | Incident population (excluded if T‐score < ‐4; severe hypo‐ or hyperparathyroidism (iPTH > 800 or <10 mg/L; total calcium < 1.8 or > 2.7 mmol/L) |
| Recombinant PTH | |||||||
|
Cejka 2008 (adults) |
Deceased | BMD and histomorphometry | Teriparatide | 20 µg/d | 1 month | 6 months | Deceased donor transplantation; SCr < 2 mg/dL. Incident population (excluded if DGF; persistent severe hyperparathyroidism (reduction of < 50% in post‐transplant PTH levels with either biopsy‐proven high‐turnover renal bone disease or pre‐transplant concentration > 300 pg/mL); hypercalcaemia) |
| Calcimimetic | |||||||
|
Evenepoel 2014 (adults) |
‐‐ | Serum calcium | Cinacalcet | 30 to 180 mg/d | 9 weeks to 24 months | 12 months | First or second kidney transplant; stable kidney function (eGFR ≥ 30 mL/min/1.73 m2; corrected serum calcium > 10.5 mg/dL; iPTH > 100 pg/mL (excluded if continued use of bisphosphonates; vitamin D analogues; calcium supplements; phosphate binders or thiazide diuretics) |
|
Pasquali 2014 (adults) |
‐‐ | Serum calcium | Cinacalcet versus paricalcitol | Mean 41 ± 15 mg/d | 7 ± 5 years | 3 months | Kidney transplant recipient with secondary hyperparathyroidism, response to cinacalcet therapy (based on lowered serum calcium) (no exclusions specified) |
|
Cruzado 2015 (adults) |
‐‐ | Serum calcium | Cinacalcet | 30 mg/d titrated | ≥ 6 months | 12 months | eGFR ≥ 30 mL/min/1.73 m2; 6 months or longer since transplantation; serum PTH ≥ 15 pmol/L; total serum calcium ≥ 2.63 mmol/L; serum phosphorus ≤ 1.2 mmol/L (no exclusions specified) |
| Parathyroidectomy | |||||||
|
Cruzado 2015 (adults) |
‐‐ | Serum calcium | Parathyroidectomy | ‐‐ | ≥ 6 months | 12 months | eGFR ≥ 30 mL/min/1.73 m2; 6 months or longer since transplantation; serum PTH ≥ 15 pmol/L; total serum calcium ≥ 2.63 mmol/L; serum phosphorus ≤ 1.2 mmol/L (no exclusions specified) |
| Hormone replacement therapy | |||||||
|
Eid 1996 (women) |
‐‐ | BMD | β‐estradiol and medroxyprogesterone | 50 µg/d 10 mg/d |
Not described | 36 months | Post‐menopausal women (no exclusions specified) |
| Calcitonin | |||||||
|
Psimenou 2002 (adults) |
‐‐ | BMD | Calcitonin | 200 IU/d | ‐‐ | 12 months | Low BMD; mean T‐score < ‐2.7 at baseline (no exclusions specified) |
|
Nordal 1995 (adults) |
‐‐ | BMD | Calcitonin | 200 IU/d | At transplantation | 12 months | Inclusions and exclusions not specified. Incident population |
|
Ugur 2000 (adults) |
‐‐ | BMD | Calcitonin | 200 IU alternate days | > 12 months | 12 months | T‐score < ‐1; transplantation > 12 months (no exclusions specified) |
|
El‐Husseini 2004 (children and adolescents) |
Living | BMD | Calcitonin | 200 IU/d | 48 months on average | 12 months | T‐score ≤ ‐1 (excluded if anticonvulsant therapy or thiazide diuretic treatment) |
|
El‐Husseini 2005a (children and adolescents) |
‐‐ | BMD | Calcitonin | 200 IU/d | ‐‐ | 12 months | kidney transplant recipients with low BMD (Z‐score ≤ ‐1) (no exclusions specified) |
| Potassium | |||||||
|
Starke 2012 (adults) |
Living and deceased | BMD and bone histomorphometry | Potassium citrate or potassium chloride | Titrated to achieve bicarbonate > 24 mmol/L | 3 months to 8 years | 12 months | Transplantation > 3 months and < 8 years; venous serum bicarbonate concentration < 24 mmol/L; stable graft function; eGFR > 30 mL/min/1.73 m2 (excluded if acute rejection episodes; severe physical limitation; psychiatric disorder; malignancy; catabolic state due to systemic illness; acute systemic infection; pregnancy) |
| Ultraviolet light (UVB) | |||||||
|
Praditpornsilpa 2014 (unknown) |
‐‐ | iPTH | UVB treatment | Initiated at dose of 700 mJ/cm2 and the total accumulation dose was 6,952 mJ/cm2 in 7th weeks | ‐‐ | ‐‐ | Kidney transplant recipients (no exclusions specified) |
BMD ‐ bone mineral density; CrCl ‐ creatinine clearance; DGF ‐ delayed graft function; (e)GFR ‐ (estimated) glomerular filtration rate; HD ‐ haemodialysis; (i)PTH ‐ (intact) parathyroid hormone; SCr ‐ serum creatinine; SD ‐ standard deviation; UPCR ‐ urinary protein‐creatinine excretion ratio; UVB ‐ ultraviolet light B
Twenty‐two studies evaluated interventions commenced at the time of or within three weeks of kidney transplantation (Amer 2013; Cejka 2008, Coco 2003; Coco 2012; De Sevaux 2002; Dovas 2009; El‐Agroudy 2003a; Fan 2000; Grotz 2001; Haas 2003; Kharlamov 2012; Messa 1999; Nam 2000; Nayak 2007; Nordal 1995; Omidvar 2011; Shahidi 2015; Sharma 2002a; Sirsat 2010; Smerud 2012; Torregrosa 2011; Walsh 2009). Twenty studies randomised participants between 28 days and 179 months following transplantation (Arnol 2011; Cruzado 2015; Cueto‐Manzano 2000; Eid 1996; Evenepoel 2014; Giannini 2001; Grotz 1998; Jeffrey 2003; Koc 2002; Lan 2008; Okamoto 2014; Pasquali 2014; Perez 2010; Pihlstrom 2017; POSTOP 2014; Sanchez‐Escuredo 2015; Starke 2012; Trabulus 2008; Trillini 2015; Ugur 2000). One study evaluated therapy in children or adolescent recipients of a kidney transplant (El‐Husseini 2004).
In studies involving adults, the mean age was 47.9 years (range 27.7 to 64). Studies involved predominantly men (65% of participants on average) with three studies only including men (El‐Agroudy 2003a; Fan 2000; Kharlamov 2012) and one study only including women (Eid 1996). The proportion of post‐menopausal women to total participants was described in seven studies (106 of 371 participants) (Cueto‐Manzano 2000; De Sevaux 2002; Eid 1996; Fan 2000; Grotz 1998; Grotz 2001; Torres 2004) where one study enrolled only post‐menopausal women (Eid 1996), and in the four others post‐menopausal women were between 15% and 47% of enrolments. In the 20 studies reporting time on dialysis prior to transplantation, the average time spend on dialysis was 34.5 months (range 10.5 to 136). The mean eGFR at baseline ranged between 35.1 and 82 mL/min/1.73 m2. The mean or median baseline PTH level in contributing studies was variable; the mean PTH level was 156.6 pg/mL (16.6 pmol/L) and ranged between 6.3 and 465 pg/mL (0.67 to 49.3 pmol/L). The mean BMD T‐score at the lumbar spine ranged between ‐3.2 and 0.17 in the 17 studies reporting this information. Detailed information about potential risk factors for bone disease and related‐outcomes in each study populations is shown in Table 4.
Study comparisons
Interventions included bisphosphonates, vitamin D compounds and analogues, RANK inhibitors (denosumab), recombinant PTH (teriparatide), cinacalcet, hormone replacement therapy, calcitonin, parathyroidectomy, and potassium citrate, calcium supplementation, alone or in combination, and UVB (Table 4). Studies compared active treatment versus placebo or standard care, or two active treatments.
The active treatments versus placebo, no treatment or standard care included:
Bisphosphonate versus placebo/no treatment: 25 studies (1300 participants) (Coco 2003; Coco 2012; El‐Agroudy 2003a; El‐Husseini 2004; Fan 2000; Fujii 2006; Giannini 2001; Grotz 1998; Grotz 2001; Haas 2003; Koc 2002; Lan 2008; Montilla 2001; Nam 2000; Nayak 2007; Okamoto 2014; Shahidi 2015; Sharma 2002a; Smerud 2012; Torregrosa 2003; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Trabulus 2008Walsh 2009)
Vitamin D versus placebo/no treatment: 20 studies (1409 participants) (Amer 2013; Arnol 2011; Chalopin 1987; El‐Agroudy 2003a; El‐Husseini 2004; Kharlamov 2012; Koc 2002; Messa 1999; Nam 2000; Narasimhamurthy 2014; Neubauer 1984; Peeters 2001; Perez 2010; Pihlstrom 2017; Tiryaki 2015; Torres 2004; Trabulus 2008; Trillini 2015; Ugur 2000; Wissing 2005)
Calcitonin: 5 studies (273 participants) (El‐Agroudy 2003a; El‐Husseini 2004; Grotz 1998; Nordal 1995; Ugur 2000)
Denosumab (RANKL inhibitor) versus placebo/no treatment: 1 study (90 participants) (POSTOP 2014)
Teriparatide (synthetic PTH) versus placebo/no treatment: 1 study (36 participants) (Cejka 2008)
Cinacalcet versus placebo/no treatment: 1 study (114 participants) (Evenepoel 2014)
Bisphosphonate plus vitamin D: 2 studies (43 participants) (Dovas 2009; Trabulus 2008)
Vitamin D plus calcium: 5 studies (333 patients) (Cueto‐Manzano 2000; De Sevaux 2002; Marcen 2010Tałałaj 1996; Ugur 2000).
The two active treatments comparisons were:
Bisphosphonate versus vitamin D: 7 studies (384 participants) (El‐Agroudy 2003a; El‐Husseini 2004; Koc 2002; Jeffery 2003; Nakamura 2009a; Nam 2000; Trabulus 2008)
Bisphosphonate versus calcitonin: 4 studies (209 participants) (El‐Agroudy 2003a; El‐Husseini 2004; Grotz 1998; Psimenou 2002)
Bisphosphonate versus bisphosphonate: 3 studies (150 participants) (Omidvar 2011); Sanchez‐Escuredo 2015; Sirsat 2010)
Bisphosphonate plus vitamin D versus bisphosphonate: 2 arms of 1 study (29 participants) (Trabulus 2008)
Bisphosphonate plus vitamin D versus vitamin D: 2 arms of 1 study (38 participants) (Trabulus 2008)
Bisphosphonate plus calcium plus vitamin D versus calcium plus vitamin D: 1 study (45 participants (Lord 2001a)
Vitamin D versus calcimimetic: 1 study (16 participants) (Pasquali 2014)
Vitamin D versus calcitonin: 3 studies (150 participants) (El‐Agroudy 2003a; El‐Husseini 2004; El‐Husseini 2005a)
Vitamin D plus calcium versus calcium: 1 study (45 participants) (Ugur 2000)
Vitamin D versus vitamin D: 3 studies (180 participants) (Kharlamov 2012; Oliden 2012; Shahidi 2011)
Vitamin D versus 17b‐estradiol and medroxyprogesterone: 1 study (59 women) (Eid 1996)
Vitamin D started at 4 months post transplant versus 6 months: 1 study (49 participants) (Thervet 2008)
Vitamin D versus UVB: 1 study (40 participants) (Praditpornsilpa 2014)
Cinacalcet versus subtotal parathyroidectomy: 1 study (30 patients (Cruzado 2015)
Potassium citrate versus potassium chloride: 1 study (30 patients) (Starke 2012).
Co‐intervention with calcium and vitamin D compounds was reported in 16 studies (Amer 2013; Cejka 2008; Coco 2003; El‐Husseini 2005a; Lan 2008; Nayak 2007; Omidvar 2011; Peeters 2001; POSTOP 2014; Sanchez‐Escuredo 2015; Shahidi 2015; Sharma 2002a; Smerud 2012; Torregrosa 2003; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Walsh 2009), calcium alone in 12 studies (El‐Agroudy 2003a; El‐Husseini 2004; El‐Husseini 2005a; Grotz 1998; Grotz 2001; Haas 2003; Jeffrey 2003; Messa 1999; Nam 2000; Peeters 2001; Shahidi 2011; Trabulus 2008), and vitamin D compound alone in one study (Coco 2012).
Study outcomes
The primary clinical outcome for most studies related to BMD, bone histomorphometry, or biomarkers of bone activity (43 studies). Since 2012, there have been an increasing number of studies in which other outcomes have been specified as the primary outcome, including: protein or albumin excretion (Arnol 2011; Pihlstrom 2017; Tiryaki 2015), graft function (Kharlamov 2012), and treatment of hyperparathyroidism (Amer 2013; Cruzado 2015; Evenepoel 2014; Pasquali 2014; Trillini 2015). All studies evaluating bisphosphonate therapy included BMD and/or histomorphometry as the primary outcome. All studies assessing vitamin D compounds before 2011 (vitamin D3, 1‐alfa‐(OH)‐vitamin D3, 25(OH)‐vitamin D3 and calcitriol (1,25(OH)2‐vitamin D3 evaluated BMD as the primary outcome. All studies of paricalcitol reported primary outcomes of protein or albumin excretion or PTH levels. Studies of denosumab, teriparatide, hormone replacement therapy, calcitonin, and potassium citrate reported BMD as the primary outcome. Studies evaluating cinacalcet or parathyroidectomy reported serum calcium levels after transplantation as the primary study outcome.
Fracture outcomes were heterogeneously measured both in terms of timing and methodology. In eight studies (Grotz 2001; Shahidi 2015; Smerud 2012; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Trabulus 2008; Walsh 2009), fracture events were collected systematically by clinical questioning (Shahidi 2015) or spinal radiography (Grotz 2001; Smerud 2012; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Trabulus 2008; Walsh 2009). Of the fracture events reported, spinal or vertebral fractures were reported in 10 studies (Coco 2003; De Sevaux 2002; Grotz 2001; Smerud 2012; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Torres 2004; Trabulus 2008; Walsh 2009), peripheral fractures in six studies (Cruzado 2015; El‐Husseini 2004; Evenepoel 2014; Grotz 1998; Nordal 1995; POSTOP 2014), while the fracture site was not specified or zero fracture events were reported in seven studies (Amer 2013; Cueto‐Manzano 2000; El‐Agroudy 2003a; Giannini 2001; Haas 2003; Shahidi 2015; Trillini 2015). Overall, 85% of the 57 fracture events were identified through systematic radiographic surveillance during follow‐up.
The key outcomes for this review were included in meta‐analyses from the following studies.
Fracture: 25 studies (Amer 2013; Coco 2003; Cruzado 2015; Cueto‐Manzano 2000; De Sevaux 2002; El‐Agroudy 2003a; El‐Husseini 2004; Evenepoel 2014; Fan 2000; Giannini 2001; Grotz 1998; Grotz 2001; Haas 2003; Nordal 1995; Omidvar 2011; POSTOP 2014; Shahidi 2015; Smerud 2012; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Torres 2004; Trabulus 2008; Trillini 2015; Walsh 2009).
Death (all causes): 17 studies (Amer 2013; Coco 2003; Cruzado 2015; De Sevaux 2002; Evenepoel 2014; Fan 2000; Giannini 2001; Grotz 1998; Grotz 2001; Haas 2003; Jeffery 2003; Kharlamov 2012; Pihlstrom 2017; Shahidi 2015; Smerud 2012; Torregrosa 2007; Torregrosa 2010)
Cardiovascular death: 8 studies (Amer 2013; Evenepoel 2014; Grotz 1998; Grotz 2001; Jeffery 2003; Kharlamov 2012; Pihlstrom 2017; Shahidi 2015)
Myocardial infarction: 2 studies (Amer 2013; Trillini 2015)
Stroke: 1 study (Trillini 2015)
Acute graft rejection: 17 studies (Amer 2013; Cejka 2008; Cruzado 2015; De Sevaux 2002; Fan 2000; Grotz 2001; Haas 2003; Pihlstrom 2017; POSTOP 2014; Sanchez‐Escuredo 2015; Smerud 2012; Torregrosa 2010; Torregrosa 2011; Torres 2004; Trillini 2015; Walsh 2009; Wissing 2005).
Graft loss: 13 studies (Amer 2013; Coco 2003; Cueto‐Manzano 2000; De Sevaux 2002; El‐Husseini 2004; Fan 2000; Grotz 1998; Jeffery 2003; POSTOP 2014; Sanchez‐Escuredo 2015; Torregrosa 2007; Torregrosa 2010; Torres 2004).
Bone pain: 4 studies (Cueto‐Manzano 2000; El‐Agroudy 2003a; Torregrosa 2007; Torregrosa 2011)
Spinal deformity: 1 study (Grotz 2001)
Avascular necrosis: 2 studies (De Sevaux 2002; Nordal 1995
Hypercalcaemia and/or hypocalcaemia: 16 studies (Amer 2013; Coco 2003; Cruzado 2015; De Sevaux 2002; El‐Agroudy 2003a; El‐Husseini 2004; Fan 2000; Kharlamov 2012; Pihlstrom 2017; POSTOP 2014; Smerud 2012; Torres 2004; Trabulus 2008; Trillini 2015; Walsh 2009; Wissing 2005).
Parathyroidectomy: 1 study (Amer 2013)
Gastrointestinal events: 5 studies (Cueto‐Manzano 2000; Evenepoel 2014; Giannini 2001; Grotz 1998; POSTOP 2014)
BMD: 36 studies (Amer 2013; Coco 2003; Cejka 2008; Cruzado 2015; Cueto‐Manzano 2000; De Sevaux 2002; El‐Husseini 2004; Evenepoel 2014; Grotz 1998; Grotz 2001; Jeffery 2003; Koc 2002; Lan 2008; Messa 1999; Nam 2000; Nayak 2007; Neubauer 1984; Okamoto 2014; Omidvar 2011; Perez 2010; POSTOP 2014; Sanchez‐Escuredo 2015; Shahidi 2011; Shahidi 2015; Sharma 2002a; Smerud 2012; Starke 2012; Tałałaj 1996; Torregrosa 2003; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Trabulus 2008; Trillini 2015; Walsh 2009; Wissing 2005).
Presence of low bone turnover seen on bone histomorphometry: 4 studies (Cejka 2008; Coco 2003; Cueto‐Manzano 2000; Haas 2003).
Plasma or SCr: 26 studies (Cejka 2008; Coco 2003; Coco 2012; Cueto‐Manzano 2000; De Sevaux 2002; El‐Agroudy 2003a; El‐Husseini 2004; Fan 2000; Grotz 1998; Grotz 2001; Haas 2003; Kharlamov 2012; Lan 2008; Neubauer 1984; Perez 2010; Pihlstrom 2017; Sanchez‐Escuredo 2015; Tałałaj 1996; Torregrosa 2003; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Torres 2004; Trabulus 2008; Trillini 2015; Walsh 2009).
eGFR: 16 studies (Amer 2013; Coco 2012; Cruzado 2015; De Sevaux 2002; Evenepoel 2014; Kharlamov 2012; Okamoto 2014; Omidvar 2011; Perez 2010; Pihlstrom 2017; POSTOP 2014; Shahidi 2015; Starke 2012; Torres 2004; Trabulus 2008; Wissing 2005)
Proteinuria: 4 studies (Arnol 2011; Coco 2012; Cruzado 2015; Pihlstrom 2017)
Vascular calcification score: 3 studies (Cruzado 2015; Okamoto 2014; Torregrosa 2010)
Serum PTH: 24 studies (Cruzado 2015; Dovas 2009; De Sevaux 2002; El‐Agroudy 2003a; El‐Husseini 2004; Evenepoel 2014; Fan 2000; Giannini 2001; Grotz 1998; Grotz 2001; Messa 1999; Pasquali 2014; Pihlstrom 2017; POSTOP 2014; Shahidi 2015; Smerud 2012; Starke 2012; Tałałaj 1996; Torregrosa 2003; Torregrosa 2011; Torres 2004; Trabulus 2008; Walsh 2009; Wissing 2005).
Excluded studies
Twenty studies were excluded as they did not enrol kidney transplant recipients (James 2003; Josephson 2004; Lippuner 1996; Reed 2004), did not include an eligible intervention (Campistol 1999; Campistol 2000; El‐Haggan 2002; Labib 1999; Lebranchu 1999; Lippuner 1998; Masse 2001; Ponticelli 1997; Rigotti 2003; ter Meulen 2003; THOMAS 2002; Vasquez 2004; Zaoui 2003), were not designed to measure outcomes of interest to this review (Ambuhl 1999; Ardalan 2007), or were terminated (NCT00646282).
Risk of bias in included studies
The risk of bias in included studies is summarised in Figure 2. The risk of bias for each adjudicated domain in individual studies is shown in Figure 3.
2.
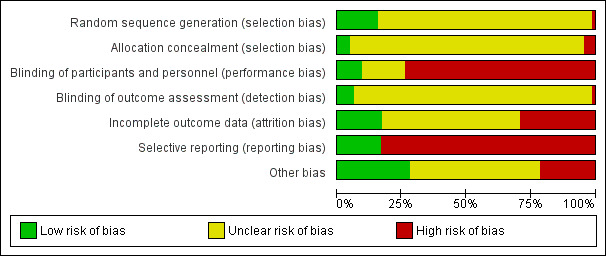
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
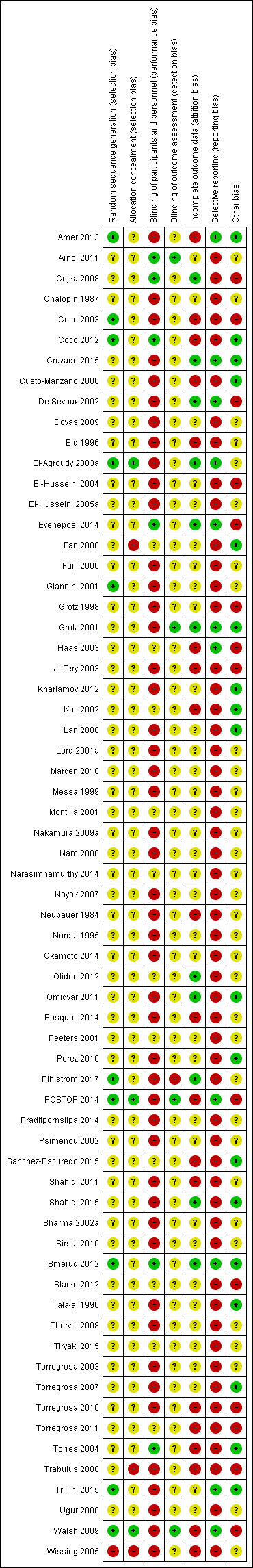
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
Methods used to generate the random sequence were at low risk of bias in 10 (15%) studies (Amer 2013; Coco 2003; Coco 2012; El‐Agroudy 2003a; Giannini 2001; Pihlstrom 2017; POSTOP 2014; Smerud 2012; Trillini 2015; Walsh 2009), at high risk of bias in one (2%) studies (Wissing 2005) and not sufficiently described in the remaining 54 studies to permit judgement.
Allocation concealment
Methods to conceal treatment allocation were at low risk of bias in three (6%) studies (El‐Agroudy 2003a; POSTOP 2014; Walsh 2009), at high risk of bias in three (6%) studies (Fan 2000; Trabulus 2008; Wissing 2005) and not sufficiently described in the remaining 59 studies to permit judgement.
Blinding
Blinding of participants and investigators
Participants and investigators were blinded to treatment allocation in six (9%) of studies (Arnol 2011; Cejka 2008; Coco 2012; Evenepoel 2014; Smerud 2012; Torres 2004); were not blinded to treatment allocation in 47 (72%) studies (Amer 2013; Chalopin 1987; Coco 2003; Cruzado 2015; Cueto‐Manzano 2000; De Sevaux 2002; Dovas 2009; Eid 1996; El‐Agroudy 2003a; El‐Husseini 2004; El‐Husseini 2005a; Fujii 2006; Giannini 2001; Grotz 1998; Grotz 2001; Jeffery 2003; Kharlamov 2012; Lan 2008; Lord 2001a; Marcen 2010; Messa 1999; Nakamura 2009a; Nam 2000; Nayak 2007; Neubauer 1984; Nordal 1995; Okamoto 2014; Omidvar 2011; Pasquali 2014; Perez 2010; Pihlstrom 2017; POSTOP 2014; Psimenou 2002; Shahidi 2011; Shahidi 2015; Sharma 2002a; Sirsat 2010; Tałałaj 1996; Thervet 2008; Torregrosa 2003; Torregrosa 2007; Torregrosa 2010; Trabulus 2008; Trillini 2015; Ugur 2000; Walsh 2009; Wissing 2005) and not sufficiently described in the remaining 12 studies to permit judgement.
Blinding of outcome assessment
Outcome assessment was blinded to treatment allocation in four (8%) studies (Arnol 2011; Grotz 2001; POSTOP 2014; Walsh 2009), not blinded in one study (Pihlstrom 2017), and not sufficiently described in the remaining 60 studies to permit judgement.
Incomplete outcome data
Outcome data reporting was judged to be at low risk of bias in 11 (17%) studies (Cejka 2008; Cruzado 2015; De Sevaux 2002; El‐Agroudy 2003a; Evenepoel 2014; Grotz 2001; Oliden 2012; Omidvar 2011; Pihlstrom 2017; Shahidi 2015; Smerud 2012); judged to be at high risk of bias as fewer than 90% of randomised participants and/or attrition from follow‐up was unequal between treatment groups in ways that might have been related to treatment in 19 (29%) studies (Amer 2013; Coco 2003; Coco 2012; Cueto‐Manzano 2000; Eid 1996; Haas 2003; Jeffery 2003; Koc 2002; Neubauer 1984; Pasquali 2014; POSTOP 2014; Sanchez‐Escuredo 2015; Shahidi 2011; Torregrosa 2010; Torregrosa 2011; Torres 2004; Trabulus 2008; Walsh 2009; Wissing 2005); and not sufficiently described in the remaining 25 studies to permit judgement.
Selective reporting
Selective reporting of outcomes was at low risk of bias in 11 (17%) studies (Amer 2013; Cruzado 2015; De Sevaux 2002; El‐Agroudy 2003a; Evenepoel 2014; Grotz 2001; Haas 2003; POSTOP 2014; Smerud 2012; Trillini 2015; Walsh 2009), and at high risk of bias in 54 (83%) studies (Arnol 2011; Cejka 2008; Chalopin 1987; Coco 2003; Coco 2012; Cueto‐Manzano 2000; Dovas 2009; Eid 1996; El‐Husseini 2004; El‐Husseini 2005a; Fan 2000; Fujii 2006; Giannini 2001; Grotz 1998; Jeffery 2003; Kharlamov 2012; Koc 2002; Lan 2008; Lord 2001a; Marcen 2010; Messa 1999; Montilla 2001; Nakamura 2009a; Nam 2000; Narasimhamurthy 2014; Nayak 2007; Neubauer 1984; Nordal 1995; Okamoto 2014; Oliden 2012; Omidvar 2011; Pasquali 2014; Peeters 2001; Perez 2010; Pihlstrom 2017; Praditpornsilpa 2014; Psimenou 2002; Sanchez‐Escuredo 2015; Shahidi 2011; Shahidi 2015; Sharma 2002a; Sirsat 2010; Starke 2012; Tałałaj 1996; Thervet 2008; Tiryaki 2015; Torregrosa 2003; Torregrosa 2007; Torregrosa 2010; Torregrosa 2011; Torres 2004; Trabulus 2008; Ugur 2000; Wissing 2005).
Other potential sources of bias
Other potential threats to validity were examined. Overall, 18 (28%) studies were at low risk of bias (Amer 2013; Coco 2012; Cruzado 2015; Cueto‐Manzano 2000; Fan 2000; Grotz 2001; Kharlamov 2012; Koc 2002; Lan 2008; Omidvar 2011; Perez 2010; Sanchez‐Escuredo 2015; Shahidi 2015; Smerud 2012; Tałałaj 1996; Torregrosa 2007; Torres 2004; Trillini 2015), 13 (20%) were at high risk of bias (Cejka 2008; Coco 2003; De Sevaux 2002; El‐Husseini 2004; Evenepoel 2014; Grotz 1998; Jeffery 2003; POSTOP 2014; Starke 2012; Torregrosa 2010; Torregrosa 2011; Trabulus 2008; Walsh 2009), and in the remaining 34 (52%) study reporting was not sufficient to permit judgement.
Effects of interventions
Summary of findings for the main comparison. Bisphosphonate compared to placebo or no treatment for preventing bone disease in kidney transplant recipients.
| Bisphosphonate compared to placebo or no treatment for preventing bone disease in kidney transplant recipients | |||||
| Patient or population: preventing bone disease in kidney transplant recipients Setting: Primary or secondary prevention (no bone disease or fracture/low bone density or previous fracture) Intervention: bisphosphonate Comparison: placebo or no treatment | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with placebo or no treatment | Risk with Bisphosphonate | ||||
| Fracture | 95 per 1,000 | 59 per 1,000 (36 to 96) | RR 0.62 (0.38 to 1.01) | 765 (13) | ⊕⊕⊝⊝ LOW 1 2 |
| Acute graft rejection | 404 per 1,000 | 282 per 1,000 (222 to 359) | RR 0.70 (0.55 to 0.89) | 470 (7) | ⊕⊕⊝⊝ LOW 1 3 |
| Death (all causes) | 33 per 1,000 | 33 per 1,000 (11 to 93) | RR 0.98 (0.34 to 2.80) | 597 (10) | ⊕⊝⊝⊝ VERY LOW 1 2 4 |
| Cardiovascular death | 13 per 1,000 | 4 per 1,000 (0 to 96) | RR 0.33 (0.01 to 7.58) | 150 (3) | ⊕⊝⊝⊝ VERY LOW 1 2 4 |
| Bone pain | 133 per 1,000 | 27 per 1,000 (5 to 124) | RR 0.20 (0.04 to 0.93) | 153 (3) | ⊕⊕⊝⊝ LOW 1 2 |
| Spinal deformity | 333 per 1,000 | 193 per 1,000 (87 to 437) | RR 0.58 (0.26 to 1.31) | 72 (1) | ⊕⊝⊝⊝ VERY LOW 1 5 |
| Hypocalcaemia | 0 per 1,000 | 0 per 1,000 (0 to 0) | RR 5.59 (1.00 to 31.06) | 207 (4) | ⊕⊝⊝⊝ VERY LOW 1 2 4 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Evidence certainty was downgraded one level grade because of study risks of bias
2 Evidence certainty was downgraded one level because of the reliance of the estimated effect on a small number of events
3 Evidence certainty was downgrade one level because of implausibly high event rate in the contributing studies ‐‐ higher than would be expected in clinical practice
4 Evidence certainty downgraded one level because of imprecise treatment estimate
5 Evidence certainty downgraded two levels for imprecision in a single small study
Summary of findings 2. Vitamin D compared to placebo or no treatment for preventing bone disease in kidney transplant recipients.
| Vitamin D compared to placebo or no treatment for preventing bone disease in kidney transplant recipients | |||||
| Patient or population: preventing bone disease in kidney transplant recipients Setting: Primary or secondary prevention (no bone disease or fracture/low bone density or previous fracture) Intervention: Vitamin D Comparison: placebo or no treatment | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with placebo or no treatment | Risk with Vitamin D | ||||
| Fracture | 7 per 1,000 | 7 per 1,000 (1 to 61) | RR 0.96 (0.10 to 8.94) | 299 (5) | ⊕⊝⊝⊝ VERY LOW 1 2 3 |
| Acute graft rejection | 89 per 1,000 | 87 per 1,000 (46 to 165) | RR 0.98 (0.52 to 1.86) | 385 (5) | ⊕⊝⊝⊝ VERY LOW 1 2 3 |
| Death (all causes) | 60 per 1,000 | 30 per 1,000 (2 to 556) | RR 0.49 (0.03 to 9.22) | 232 (3) | ⊕⊝⊝⊝ VERY LOW 1 2 3 |
| Cardiovascular death | 43 per 1,000 | 25 per 1,000 (2 to 326) | RR 0.57 (0.04 to 7.57) | 232 (3) | ⊕⊝⊝⊝ VERY LOW 1 2 3 |
| Bone pain | 0 per 1,000 | 0 per 1,000 (0 to 0) | not estimable | 40 (1) | ⊕⊝⊝⊝ VERY LOW 1 5 |
| Graft loss | 37 per 1,000 | 4 per 1,000 (0 to 74) | RR 0.11 (0.01 to 2.01) | 220 (3) | ⊕⊝⊝⊝ VERY LOW 1 2 3 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Evidence certainty was downgraded one level grade because of study risks of bias
2 Evidence certainty was downgraded one level because of the reliance of the estimated effect on a small number of events
3 Evidence certainty downgraded one level because of imprecise treatment estimate
4 Evidence certainty downgraded two levels because of imprecise treatment estimates with results based on two small studies with no events, and downgraded one level due to study limitations in one small study
5 Evidence certainty downgraded two levels for imprecision in a single small study
Bisphosphonate versus placebo or no treatment
Fracture
Bisphosphonate therapy may prevent fracture, although the 95% CI indicates that bisphosphonate treatment may make little or no difference (Analysis 1.1 (13 studies; 765 participants): RR 0.62, 95% CI 0.38 to 1.01; I2 = 0%; low certainty evidence) (Figure 4).
1.1. Analysis.
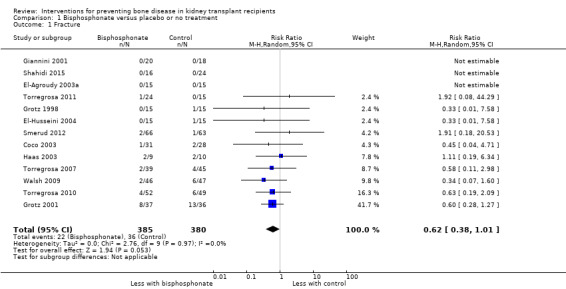
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 1 Fracture.
4.
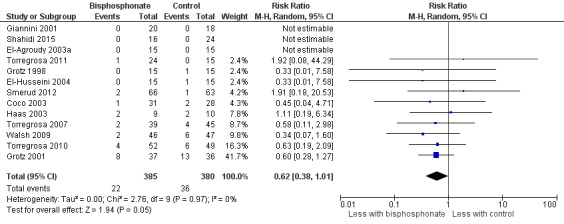
Effects of bisphosphonates versus placebo or no treatment, outcome on risks of fracture
Acute graft rejection
Bisphosphonate therapy may decrease acute graft rejection (Analysis 1.2 (7 studies, 470 participants): RR 0.70, 95% CI 0.55 to 0.89; I2 = 0%; low certainty evidence).
1.2. Analysis.
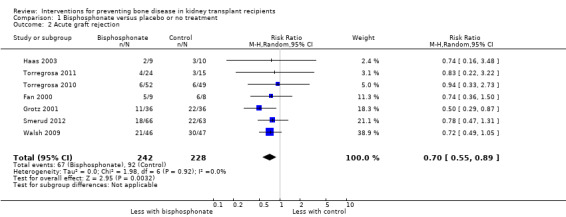
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 2 Acute graft rejection.
Death: all‐cause and cardiovascular
It is uncertain whether bisphosphonate therapy prevents death (all causes) (Analysis 1.3.1 (10 studies, 597 participants): RR 0.98, 95% CI 0.34 to 2.80; I2 = 16%; very low certainty evidence).
1.3. Analysis.
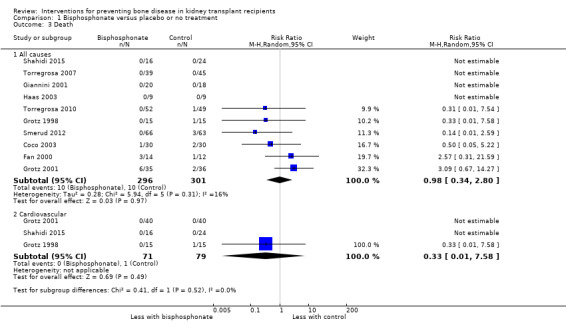
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 3 Death.
It is uncertain whether bisphosphonate therapy prevents cardiovascular death; three studies reported no cardiovascular deaths and one study (Grotz 1998) reported one death in the control group (Analysis 1.3.2).
Musculoskeletal disorders
Bone pain
Bisphosphonate treatment may reduce bone pain (Analysis 1.4.1 (3 studies, 153 participants): RR 0.20, 95% CI 0.04 to 0.93; I2 = 0%; very low certainty evidence).
1.4. Analysis.
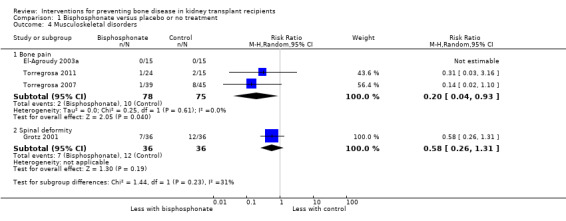
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 4 Musculoskeletal disorders.
Spinal deformity
Grotz 2001 reported little or no difference in spinal deformity with bisphosphonate treatment (Analysis 1.4.2).
Bone mineral density
Bisphosphonate therapy may make little or no difference to vertebral BMD (Analysis 1.5.1 (13 studies, 579 participants): MD 0.04 g calcium/cm2, 95% CI ‐0.01 to 0.08). There was evidence of substantial statistical heterogeneity in treatment effects between studies (I2 = 73%).
1.5. Analysis.
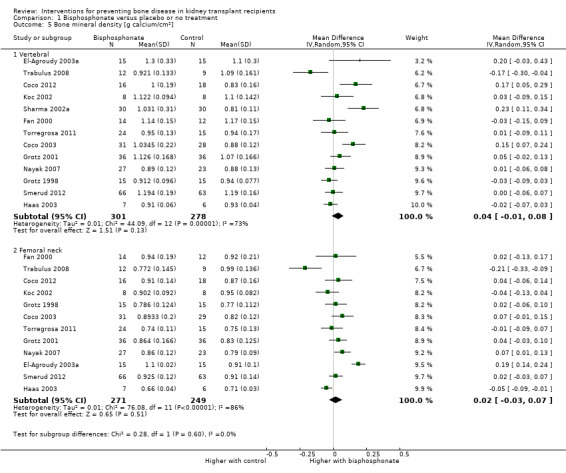
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 5 Bone mineral density [g calcium/cm2].
Bisphosphonate therapy may make little or no difference to femoral neck BMD (Analysis 1.5.2 (12 studies, 520 participants): MD 0.02 g calcium/cm2, 95% CI ‐0.03 to 0.07). There was evidence of high statistical heterogeneity (I2 = 86%).
Low bone turnover
It is uncertain whether bisphosphonate therapy decreases the presence of low bone turnover on bone histomorphometry (Analysis 1.6 (2 studies, 33 participants): RR 1.67, 95% CI 0.76 to 3.64).
1.6. Analysis.
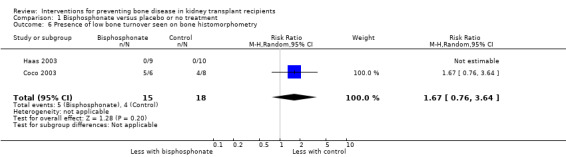
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 6 Presence of low bone turnover seen on bone histomorphometry.
Serum parathyroid hormone
Bisphosphonate therapy may make little or no difference to serum PTH levels (Analysis 1.7 (11 studies, 590 participants): MD 0.70 pmol/L, 95% CI ‐0.62 to 2.02). There was evidence of moderate statistical heterogeneity (I2 = 63%).
1.7. Analysis.
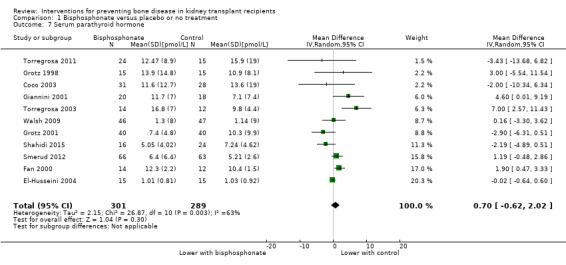
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 7 Serum parathyroid hormone.
Vascular calcification score
Bisphosphonate therapy may make little or no difference to the vascular calcification score (Analysis 1.8 (2 studies, 74 participants): SMD 0.00, 95% ‐0.46 to 0.4; I2 = 0%).
1.8. Analysis.
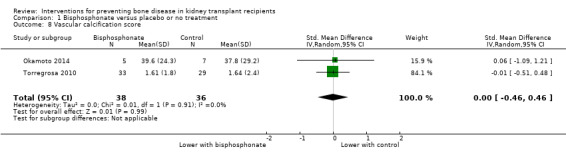
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 8 Vascular calcification score.
Proteinuria
Coco 2012 reported bisphosphonate therapy made little or no difference to proteinuria (Analysis 1.9).
1.9. Analysis.
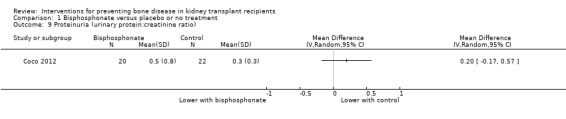
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 9 Proteinuria (urinary protein:creatinine ratio).
Graft loss
It is uncertain whether bisphosphonate treatment reduces graft loss (Analysis 1.10 (7 studies, 403 participants): RR 0.65, 95% CI 0.27 to 1.60; I2 = 22%; very low certainty evidence).
1.10. Analysis.
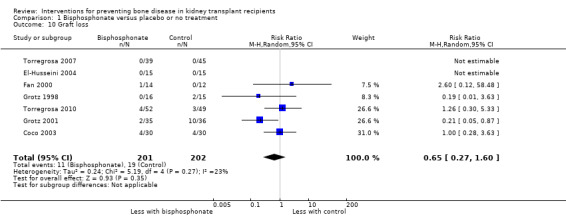
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 10 Graft loss.
Graft function
Bisphosphonate therapy may make little or no difference to SCr levels (Analysis 1.11 (12 studies, 504 participants): MD 2.18 μmol/L, 95% CI ‐7.78 to 12.15). There was evidence of moderate statistical heterogeneity (I2 = 39%).
1.11. Analysis.
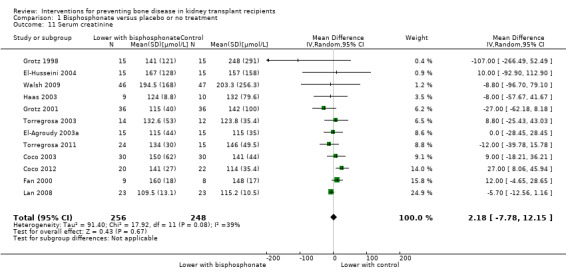
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 11 Serum creatinine.
Bisphosphonate therapy may make little or no difference to eGFR (Analysis 1.12 (2 studies, 82 participants): MD ‐0.97 mL/min/1.73 m2, 95% CI ‐17.62 to 15.67). There was evidence of high statistical heterogeneity (I2 = 79%).
1.12. Analysis.
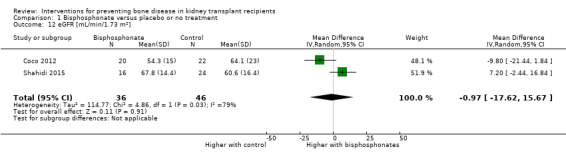
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 12 eGFR [mL/min/1.73 m2].
Gastro‐oesophageal disorder
Giannini 2001 reported little or no difference in the risk of gastro‐oesophageal disorder with bisphosphonate therapy (Analysis 1.13).
1.13. Analysis.
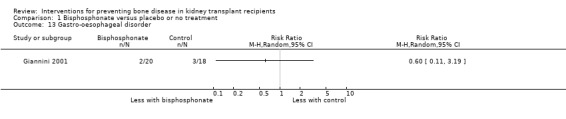
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 13 Gastro‐oesophageal disorder.
Gastrointestinal symptoms
Giannini 2001 reported little or no difference in nausea with bisphosphonate therapy) (Analysis 1.14), and Grotz 1998 (30 participants) reported little or no difference in vomiting (Analysis 1.14.2) or diarrhoea (Analysis 1.14.3).
1.14. Analysis.
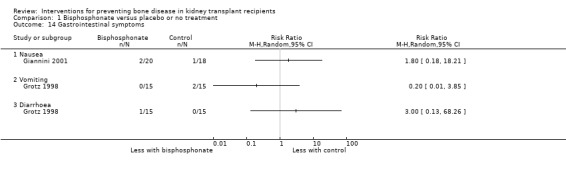
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 14 Gastrointestinal symptoms.
Hypercalcaemia
Smerud 2012 reported little or no difference in the risk of hypercalcaemia with bisphosphonate therapy (Analysis 1.15).
1.15. Analysis.
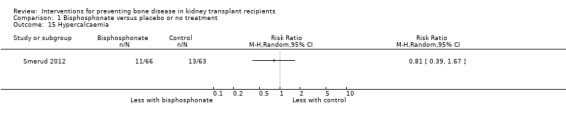
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 15 Hypercalcaemia.
Hypocalcaemia
Bisphosphonate treatment may increase the risk of hypocalcaemia (Analysis 1.16 (4 studies, 207 participants): RR 5.59, 95% CI 1.00 to 31.06; I2 = 0%; low certainty evidence).
1.16. Analysis.
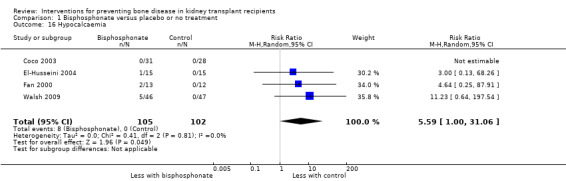
Comparison 1 Bisphosphonate versus placebo or no treatment, Outcome 16 Hypocalcaemia.
Other outcomes
The following outcomes were not reported: stroke, myocardial infarction, fever, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Vitamin D versus placebo or no treatment
Fracture
It is uncertain whether vitamin D treatment prevents fracture (Analysis 2.1 (5 studies, 299 participants): RR 0.96, 95% CI 0.10 to 8.94; I2 = 0%; very low certainty evidence).
2.1. Analysis.
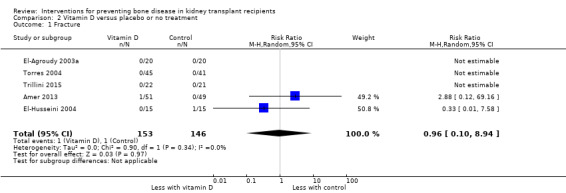
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 1 Fracture.
Acute graft rejection
It is uncertain whether vitamin D treatment makes any difference to acute graft rejection (Analysis 2.2 (5 studies, 385 participants); RR 0.98, 95% CI 0.52 to 1.86; I2 = 0%; very low certainty evidence).
2.2. Analysis.
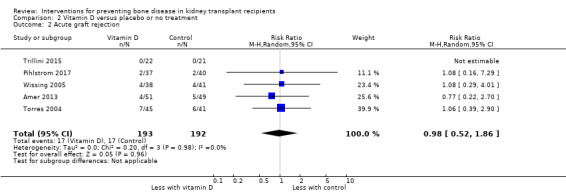
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 2 Acute graft rejection.
Death: all‐cause and cardiovascular
It is uncertain whether vitamin D treatment reduces death (all causes) (Analysis 2.3.1 (3 studies, 232 participants): RR 0.49, 95% CI 0.03 to 9.22; very low certainty evidence). There was evidence of moderate statistical heterogeneity (I2 = 60%).
2.3. Analysis.
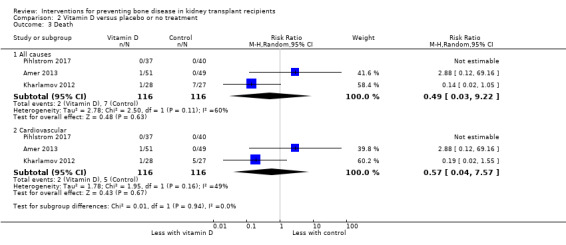
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 3 Death.
It is uncertain whether vitamin D treatment reduces cardiovascular death (Analysis 2.3.2 (3 studies 232 participants): RR 0.57, 95% CI 0.04 to 7.57; very low certainty evidence). There was evidence of moderate statistical heterogeneity (I2 = 49%).
Musculoskeletal disorders
Bone pain
El‐Agroudy 2003a reported no incidences of bone pain in either the vitamin D or control group (Analysis 2.4).
2.4. Analysis.
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 4 Musculoskeletal disorders.
Bone mineral density
It is uncertain whether vitamin D treatment makes any difference to BMD in the vertebrae (Analysis 2.5.1 (9 studies, 377 participants): MD 0.02 g calcium/cm2, 95% CI ‐0.03 to 0.07). There was evidence of moderate statistical heterogeneity (I2 = 46%).
2.5. Analysis.
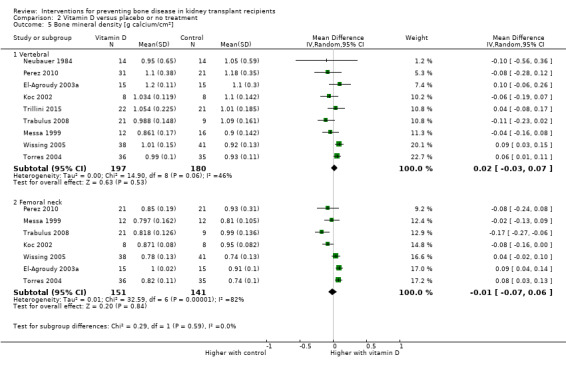
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 5 Bone mineral density [g calcium/cm2].
It is uncertain whether vitamin D treatment makes any difference to BMD at the femoral neck (Analysis 2.5.2 (7 studies, 292 participants): MD ‐0.01 g calcium/cm2, 95% CI ‐0.07 to 0.06). There was evidence of high statistical heterogeneity (I2 = 82%).
Serum parathyroid hormone
Vitamin D therapy may slightly decrease serum PTH (Analysis 2.6 (6 studies, 340 participants); MD ‐1.74 pmol/L, 95% CI ‐3.04 to ‐0.44). There was evidence of high statistical heterogeneity (I2 = 69%).
2.6. Analysis.
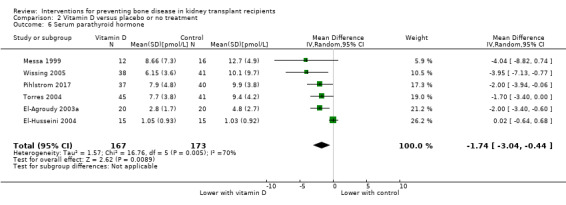
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 6 Serum parathyroid hormone.
Proteinuria
It is uncertain whether vitamin D treatment makes any difference to proteinuria (Analysis 2.7 (2 studies, 245 participants): SMD ‐0.43, ‐1.24 to 0.39). There was evidence of high statistical heterogeneity (I2 = 89%).
2.7. Analysis.
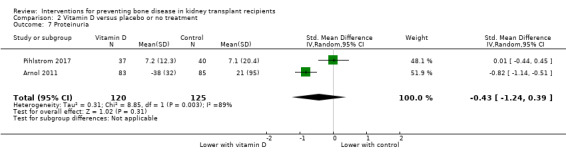
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 7 Proteinuria.
Graft loss
It is uncertain whether vitamin D treatment makes any difference to graft loss as two studies reported no events and Torres 2004 reported four events in the control group (Analysis 2.8 (3 studies, 220 participants): RR 0.11, 95% CI 0.01 to 2.01).
2.8. Analysis.
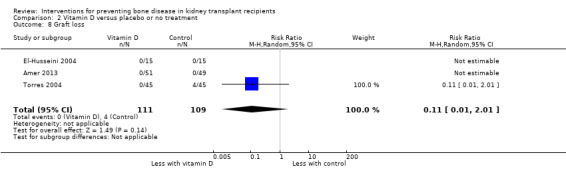
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 8 Graft loss.
Graft function
It is uncertain whether vitamin D treatment makes any difference to SCr levels (Analysis 2.9 (6 studies, 313 participants); MD 3.87 μmol/L, 95% CI ‐3.64 to 11.37; I2 = 0%).
2.9. Analysis.
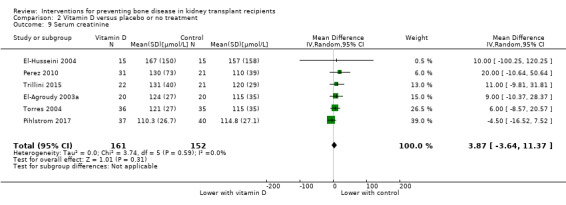
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 9 Serum creatinine.
It is uncertain whether vitamin D therapy makes any difference to eGFR (Analysis 2.10 (6 studies, 449 participants); MD 3.96 mL/min/1.73 m2, 95% CI ‐7.59 to 15.52). There was evidence of high statistical heterogeneity (I2 = 92%).
2.10. Analysis.
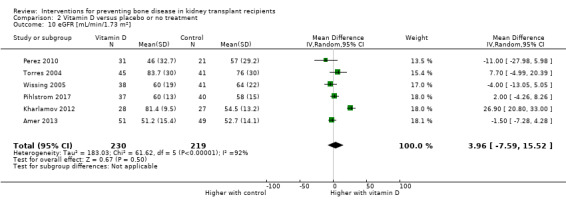
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 10 eGFR [mL/min/1.73 m2].
Hypercalcaemia
It is uncertain whether vitamin D treatment increases hypercalcaemia (Analysis 2.11 (7 studies, 465 participants); RR 2.09, 95% CI 0.84 to 5.22; very low certainty evidence). There was evidence of moderate statistical heterogeneity (I2 = 39%).
2.11. Analysis.
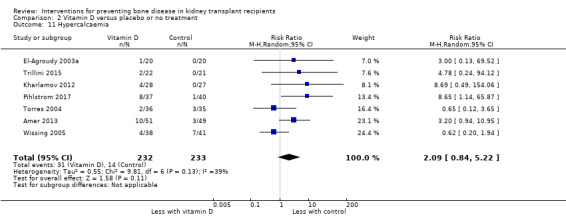
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 11 Hypercalcaemia.
Fever
Trillini 2015 reported no difference in fever between vitamin D and control (Analysis 2.12).
2.12. Analysis.
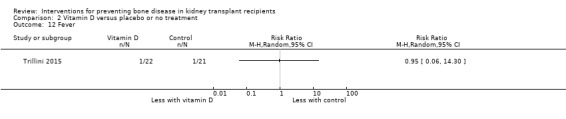
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 12 Fever.
Myocardial infarction and stroke
It is uncertain whether vitamin D treatment reduces myocardial infarction as one study reported no events and Amer 2013 reported one event in the control group (Analysis 2.13 (2 studies, 143 participants): RR 0.32, 95% CI 0.01 to 7.68).
2.13. Analysis.
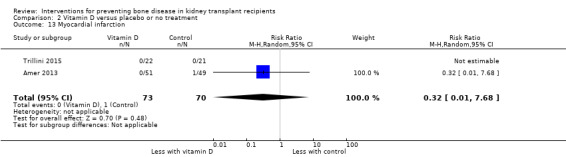
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 13 Myocardial infarction.
Trillini 2015 reported two stroke events in the vitamin D group (Analysis 2.14).
2.14. Analysis.
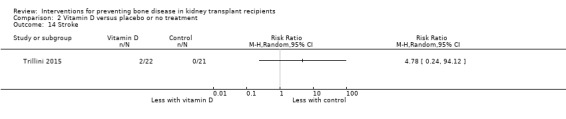
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 14 Stroke.
Parathyroidectomy
Amer 2013 reported two parathyroidectomies in the control group (Analysis 2.15).
2.15. Analysis.
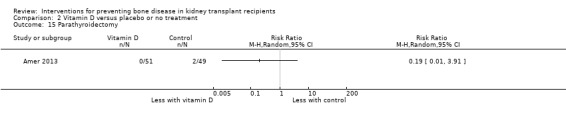
Comparison 2 Vitamin D versus placebo or no treatment, Outcome 15 Parathyroidectomy.
Other outcomes
The following outcomes were not reported: presence of low bone turnover, vascular calcification score, gastro‐oesophageal disorder; gastrointestinal symptoms, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Calcitonin versus placebo or no treatment
Fracture
It is uncertain whether calcitonin therapy decreases fracture (Analysis 3.1 (4 studies, 153 participants): RR 0.34, 95% CI 0.06 to 1.78; I2 = 0%; very low certainty evidence).
3.1. Analysis.
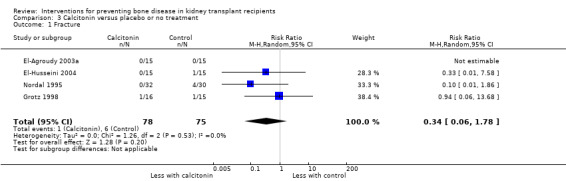
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 1 Fracture.
Death: all‐cause and cardiovascular
Grotz 1998 reported one cardiovascular death in the control group (Analysis 3.2)
3.2. Analysis.
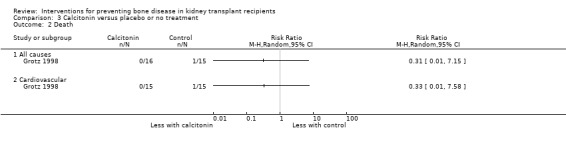
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 2 Death.
Musculoskeletal disorders
Avascular bone necrosis
Nordal 1995 reported four incidences of avascular bone necrosis in the control group (Analysis 3.3).
3.3. Analysis.
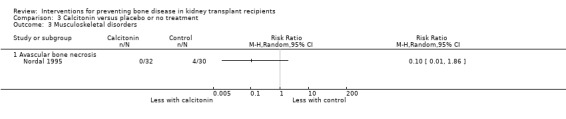
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 3 Musculoskeletal disorders.
Bone mineral density
It is uncertain whether calcitonin therapy makes any difference to BMD in the vertebrae (Analysis 3.4.1 (2 studies, 61 participants): MD ‐0.04 g calcium/cm2, 95% CI ‐0.10 to 0.02; I2 = 0%) or femoral neck (Analysis 3.4.2 (2 studies, 61 participants): MD 0.03 g calcium/cm2, 95% CI ‐0.08 to 0.15). There was evidence of high statistical heterogeneity in the latter analysis (I2 = 78%).
3.4. Analysis.
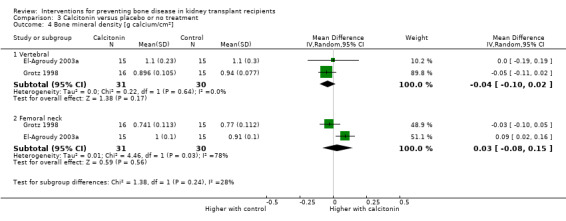
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 4 Bone mineral density [g calcium/cm2].
Serum parathyroid hormone
It is uncertain whether calcitonin therapy makes any difference to serum PTH (Analysis 3.5 (2 studies, 61 participants): MD 0.88 pmol/L, 95% CI ‐2.62 to 4.38). There was evidence of moderate statistical heterogeneity (I2 = 41%).
3.5. Analysis.
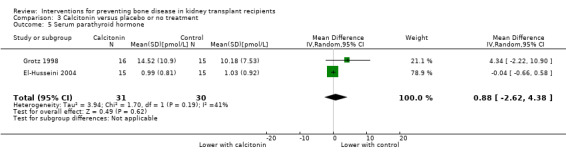
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 5 Serum parathyroid hormone.
Graft loss
It is uncertain whether calcitonin therapy prevents graft loss one study reported no graft losses and Grotz 1998 reported two events in the control group (Analysis 3.6 (2 studies, 61 participants): RR 0.19, 95% CI 0.01 to 3.63).
3.6. Analysis.
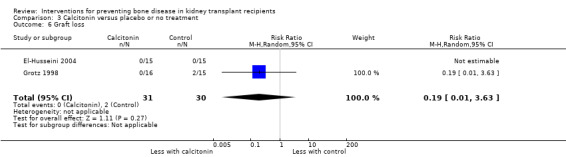
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 6 Graft loss.
Graft function
It is uncertain whether calcitonin therapy makes any difference to SCr levels (Analysis 3.7 (2 studies, 61 participants): MD ‐31.12 μmol/L, 95% CI ‐141.96 to 79.72; I2 = 33%).
3.7. Analysis.
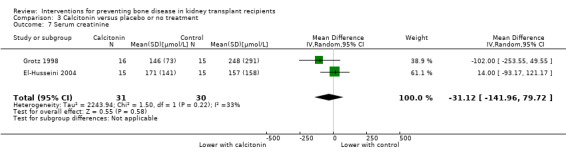
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 7 Serum creatinine.
Gastrointestinal symptoms
Vomiting
Grotz 1998 reported vomiting in two participants in the control group (Analysis 3.8).
3.8. Analysis.
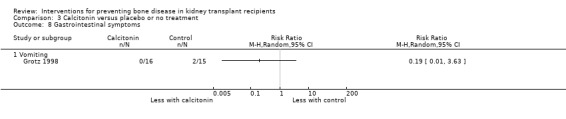
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 8 Gastrointestinal symptoms.
Hypocalcaemia
El‐Husseini 2004 reported one event of hypocalcaemia in the calcitonin group (Analysis 3.6).
Other outcomes
The following outcomes were not reported: acute graft rejection, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, gastro‐oesophageal disorder; haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
RANKL inhibitor versus placebo or no treatment
POSTOP 2014 reported no differences in fracture (Analysis 4.1), acute graft rejection (Analysis 4.2), serum PTH (Analysis 4.3), graft loss (Analysis 4.4), eGFR (Analysis 4.5), diarrhoea (Analysis 4.6), and hypocalcaemia (Analysis 4.7).
4.1. Analysis.
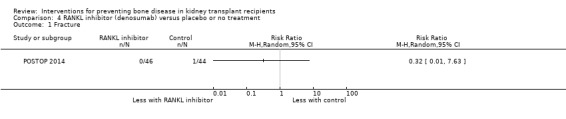
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 1 Fracture.
4.2. Analysis.
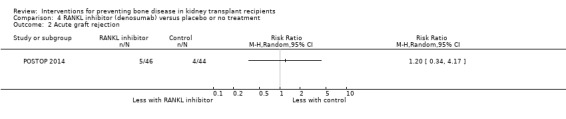
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 2 Acute graft rejection.
4.3. Analysis.
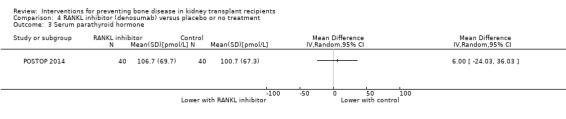
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 3 Serum parathyroid hormone.
4.4. Analysis.
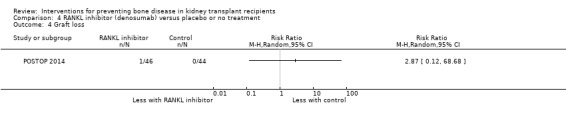
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 4 Graft loss.
4.5. Analysis.
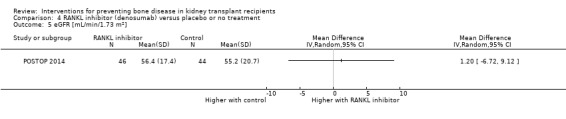
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 5 eGFR [mL/min/1.73 m2].
4.6. Analysis.
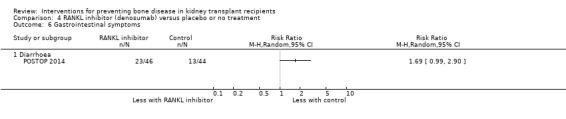
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 6 Gastrointestinal symptoms.
4.7. Analysis.
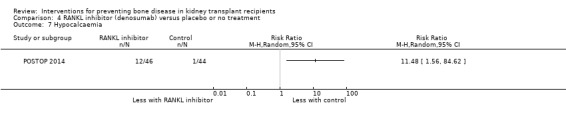
Comparison 4 RANKL inhibitor (denosumab) versus placebo or no treatment, Outcome 7 Hypocalcaemia.
The following outcomes were not reported: death, musculoskeletal disorders, BMD, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, gastro‐oesophageal disorder, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Synthetic parathyroid hormone versus placebo or no treatment
Cejka 2008 reported no differences in acute graft rejection (Analysis 5.1), BMD (Analysis 5.2), presence of low bone turnover (Analysis 5.3), or SCr (Analysis 5.4).
5.1. Analysis.
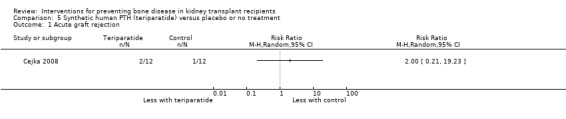
Comparison 5 Synthetic human PTH (teriparatide) versus placebo or no treatment, Outcome 1 Acute graft rejection.
5.2. Analysis.
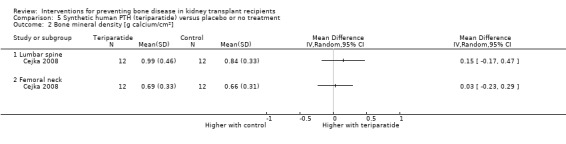
Comparison 5 Synthetic human PTH (teriparatide) versus placebo or no treatment, Outcome 2 Bone mineral density [g calcium/cm2].
5.3. Analysis.
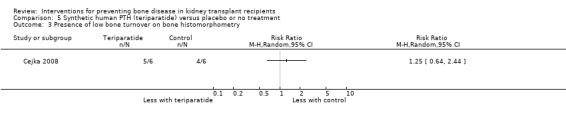
Comparison 5 Synthetic human PTH (teriparatide) versus placebo or no treatment, Outcome 3 Presence of low bone turnover on bone histomorphometry.
5.4. Analysis.
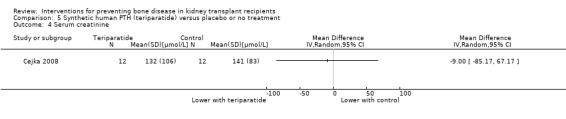
Comparison 5 Synthetic human PTH (teriparatide) versus placebo or no treatment, Outcome 4 Serum creatinine.
The following outcomes were not reported: fracture, death, BMD, stroke, myocardial infarction, serum PTH, vascular calcification score, proteinuria, graft loss, gastro‐oesophageal disorder; gastrointestinal symptoms, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Calcimimetic versus placebo or no treatment
Evenepoel 2014 reported no differences in fracture (Analysis 6.1), death (Analysis 6.2), BMD (Analysis 6.3), serum PTH (Analysis 6.4), eGFR (Analysis 6.5), or diarrhoea (Analysis 6.6).
6.1. Analysis.
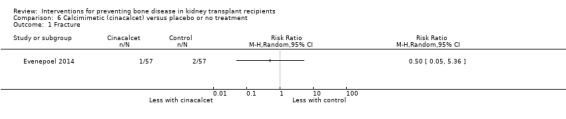
Comparison 6 Calcimimetic (cinacalcet) versus placebo or no treatment, Outcome 1 Fracture.
6.2. Analysis.
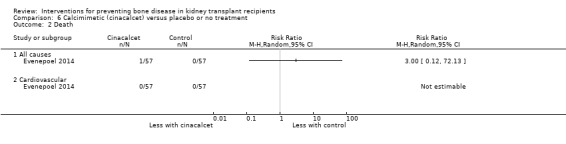
Comparison 6 Calcimimetic (cinacalcet) versus placebo or no treatment, Outcome 2 Death.
6.3. Analysis.
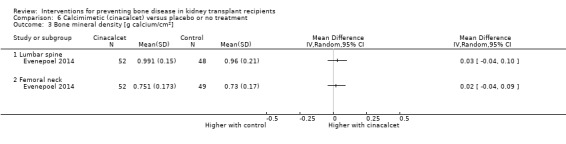
Comparison 6 Calcimimetic (cinacalcet) versus placebo or no treatment, Outcome 3 Bone mineral density [g calcium/cm2].
6.4. Analysis.
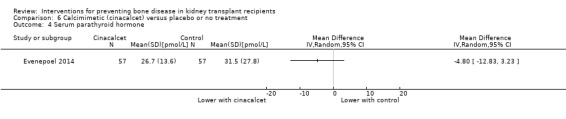
Comparison 6 Calcimimetic (cinacalcet) versus placebo or no treatment, Outcome 4 Serum parathyroid hormone.
6.5. Analysis.
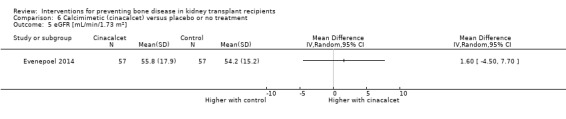
Comparison 6 Calcimimetic (cinacalcet) versus placebo or no treatment, Outcome 5 eGFR [mL/min/1.73 m2].
6.6. Analysis.
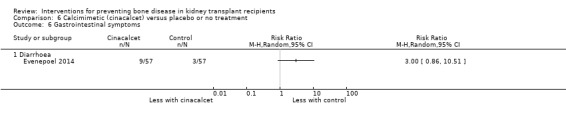
Comparison 6 Calcimimetic (cinacalcet) versus placebo or no treatment, Outcome 6 Gastrointestinal symptoms.
The following outcomes were not reported: acute graft rejection, musculoskeletal disorders, stroke, myocardial infarction, presence of low bone turnover, vascular calcification score, proteinuria, graft loss, gastro‐oesophageal disorder; hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Vitamin D plus calcium versus placebo or no treatment
Fracture
It is uncertain whether vitamin D plus calcium makes any difference to risks of fracture as one study reported no fractures occurred and De Sevaux 2002 reported two fractures in the control group (Analysis 7.1 (2 studies, 141 participants): RR 0.14, 95% CI 0.01 to 2.90).
7.1. Analysis.
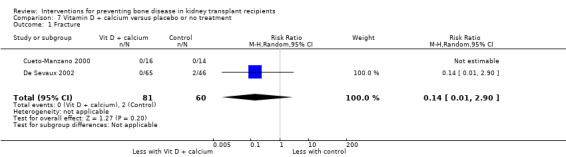
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 1 Fracture.
Acute graft rejection
De Sevaux 2002 reported no differences in acute graft rejection (Analysis 7.2).
7.2. Analysis.
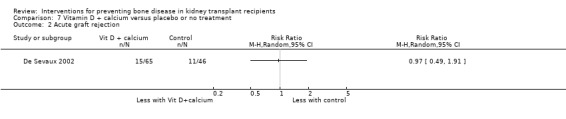
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 2 Acute graft rejection.
Death
De Sevaux 2002 reported no deaths in either group (Analysis 7.3).
7.3. Analysis.
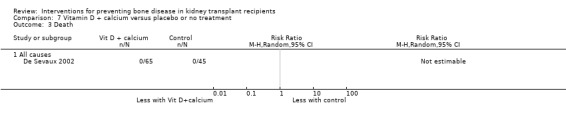
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 3 Death.
Musculoskeletal disorders
Cueto‐Manzano 2000 reported no pain (Analysis 7.4.1) or avascular bone necrosis in either group (Analysis 7.4.2).
7.4. Analysis.
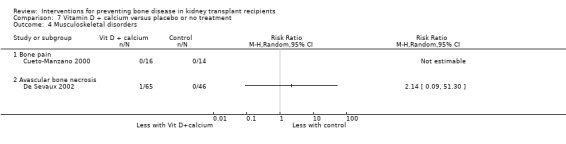
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 4 Musculoskeletal disorders.
Bone mineral density
Trabulus 2008 reported higher BMD for both vertebral (Analysis 7.5.1) and femoral neck (Analysis 7.5.2) in the control group.
7.5. Analysis.
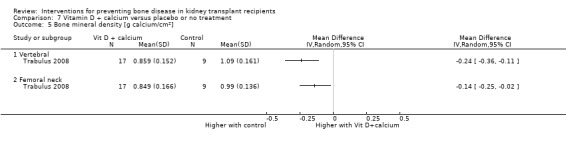
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 5 Bone mineral density [g calcium/cm2].
Presence of low bone turnover
Cueto‐Manzano 2000 reported no differences between the two groups (Analysis 7.6).
7.6. Analysis.
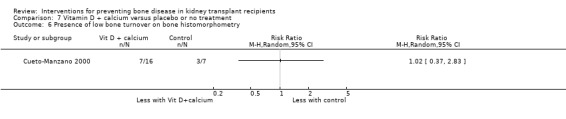
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 6 Presence of low bone turnover on bone histomorphometry.
Serum parathyroid hormone
It is uncertain whether vitamin D plus calcium makes any difference to serum PTH (Analysis 7.7 (2 studies, 188 participants); MD ‐0.32 pmol/L, 95% CI ‐2.94 to 2.31; I2 = 0%).
7.7. Analysis.
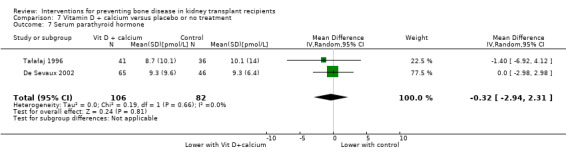
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 7 Serum parathyroid hormone.
Graft loss
It is uncertain whether vitamin D plus calcium makes any difference to the risk of graft loss (Analysis 7.8 (2 studies, 141 participants): RR 2.38, 95% CI 0.26‐22.12; I2 = 0%)
7.8. Analysis.
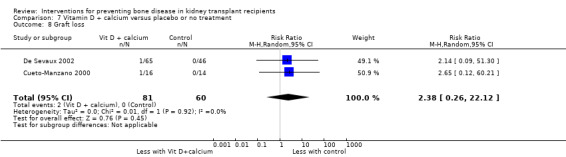
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 8 Graft loss.
Graft function
It is uncertain whether vitamin D plus calcium makes any difference to SCr levels (Analysis 7.9 (3 studies; 218 participants): MD 10.24 μmol/L, 95% CI ‐0.05 to 20.53; I2 = 0%).
7.9. Analysis.
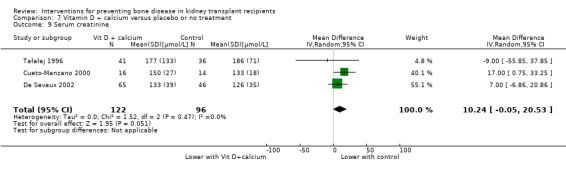
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 9 Serum creatinine.
De Sevaux 2002 reported no differences in eGFR (Analysis 7.10).
7.10. Analysis.
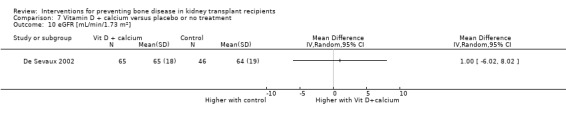
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 10 eGFR [mL/min/1.73 m2].
Gastro‐oesophageal disorders
Cueto‐Manzano 2000 reported no differences in gastro‐oesophageal disorders (Analysis 7.11).
7.11. Analysis.
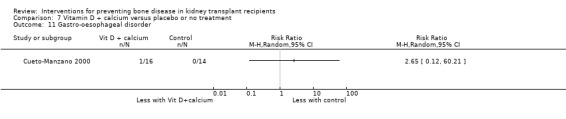
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 11 Gastro‐oesophageal disorder.
Hypercalcaemia
De Sevaux 2002 reported no differences in hypercalcaemia (Analysis 7.12).
7.12. Analysis.
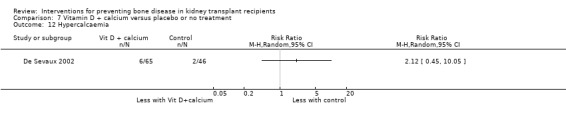
Comparison 7 Vitamin D + calcium versus placebo or no treatment, Outcome 12 Hypercalcaemia.
Other outcomes
The following outcomes were not reported: stroke, myocardial infarction, vascular calcification score, gastrointestinal symptoms, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Bisphosphonate versus vitamin D
Fracture
El‐Agroudy 2003a and Trabulus 2008 reported no fractures occurred in either group (Analysis 8.1).
8.1. Analysis.
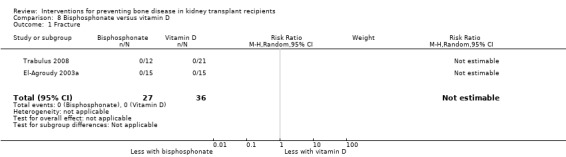
Comparison 8 Bisphosphonate versus vitamin D, Outcome 1 Fracture.
Death
Jeffery 2003 reported one patient died of sepsis in the bisphosphonate group (Analysis 8.2).
8.2. Analysis.
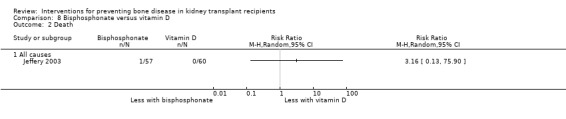
Comparison 8 Bisphosphonate versus vitamin D, Outcome 2 Death.
Musculoskeletal disorders
El‐Agroudy 2003a reported no incidences of bone pain in either group (Analysis 8.3).
8.3. Analysis.
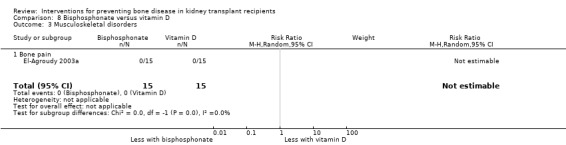
Comparison 8 Bisphosphonate versus vitamin D, Outcome 3 Musculoskeletal disorders.
Bone mineral density
It is uncertain whether bisphosphonate compared with vitamin D therapy makes any difference to BMD at the vertebrae compared with vitamin D therapy (Analysis 8.4.1 (4 studies, 176 participants): MD 0.02 g calcium/cm2, 95% CI ‐0.05 to 0.09). There was evidence of moderate statistical heterogeneity (I2 = 45%).
8.4. Analysis.
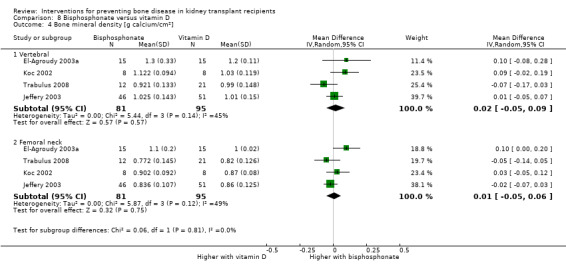
Comparison 8 Bisphosphonate versus vitamin D, Outcome 4 Bone mineral density [g calcium/cm2].
It is uncertain whether bisphosphonate and vitamin D therapy makes any difference to BMD at the femoral neck compared with vitamin D therapy (Analysis 8.4.2 (4 studies, 176 participants): MD 0.01 g calcium/cm2, 95% CI ‐0.05 to 0.06). There was evidence of moderate statistical heterogeneity (I2 = 49%).
Serum parathyroid hormone
It is uncertain whether bisphosphonate compared with vitamin D therapy makes any difference to serum PTH levels (Analysis 8.5 (2 studies, 63 participants): MD 3.14 pmol/L, 95% CI ‐3.55 to 9.82). There was evidence of high statistical heterogeneity (I2 = 92%).
8.5. Analysis.
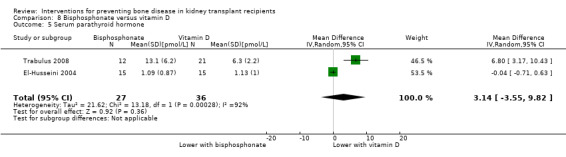
Comparison 8 Bisphosphonate versus vitamin D, Outcome 5 Serum parathyroid hormone.
Graft loss
El‐Husseini 2004 reported no incidence of graft loss in either group (Analysis 8.6).
8.6. Analysis.
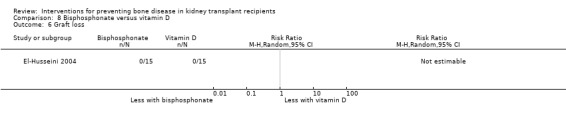
Comparison 8 Bisphosphonate versus vitamin D, Outcome 6 Graft loss.
Graft function
It is uncertain whether bisphosphonate makes any difference to SCr levels compared with vitamin D therapy (Analysis 8.7 (2 studies, 176 participants): MD ‐17.16 µmol/L, 95% CI ‐35.63 to 1.31; I2 = 0%).
8.7. Analysis.
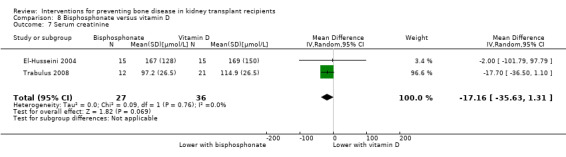
Comparison 8 Bisphosphonate versus vitamin D, Outcome 7 Serum creatinine.
Trabulus 2008 reported no difference in eGFR between the groups (Analysis 8.8).
8.8. Analysis.
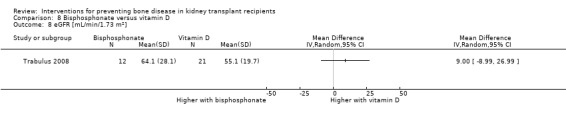
Comparison 8 Bisphosphonate versus vitamin D, Outcome 8 eGFR [mL/min/1.73 m2].
Hyper‐ and hypocalcaemia
Trabulus 2008 reported no difference in hypercalcaemia between the groups (Analysis 8.9).
8.9. Analysis.
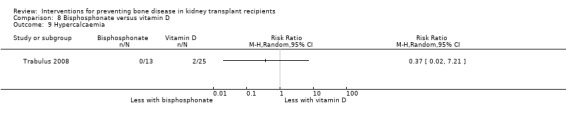
Comparison 8 Bisphosphonate versus vitamin D, Outcome 9 Hypercalcaemia.
El‐Husseini 2004 reported no difference in hypocalcaemia between the groups (Analysis 8.10).
8.10. Analysis.
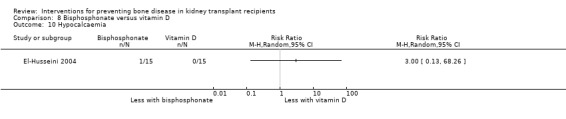
Comparison 8 Bisphosphonate versus vitamin D, Outcome 10 Hypocalcaemia.
Other outcomes
The following outcomes were not reported: acute graft rejection, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, gastro‐oesophageal disorder; gastrointestinal symptoms, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Bisphosphonate versus calcitonin
Fracture
It is uncertain whether bisphosphonate compared with calcitonin therapy makes any difference to the risk of fracture; Grotz 1998 reported one fracture in the control group (Analysis 9.1 (2 studies): RR 0.35, 95% CI 0.02 to 8.08).
9.1. Analysis.
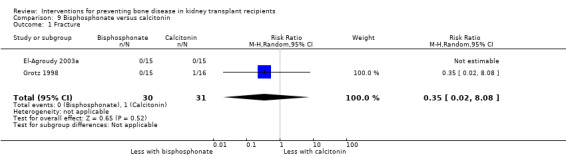
Comparison 9 Bisphosphonate versus calcitonin, Outcome 1 Fracture.
Musculoskeletal disorders
Bone pain
El‐Agroudy 2003a reported no bone pain in either group (Analysis 9.2.1).
9.2. Analysis.
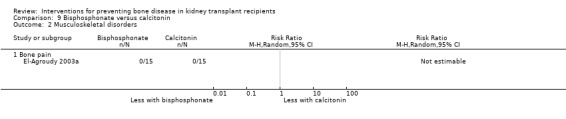
Comparison 9 Bisphosphonate versus calcitonin, Outcome 2 Musculoskeletal disorders.
Bone mineral density
It is uncertain whether bisphosphonate compared with calcitonin therapy makes any difference to BMD at the vertebrae (Analysis 9.3.1 (2 studies, 61 participants): MD 0.10 g calcium/cm2, 95% CI ‐0.10 to 0.31). There was evidence of high statistical heterogeneity (I2 = 74%).
9.3. Analysis.
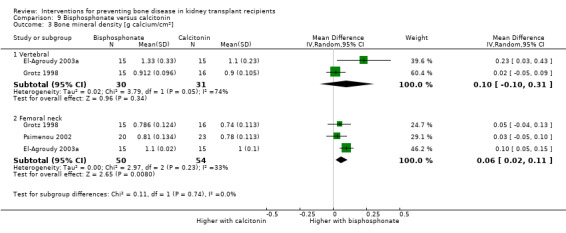
Comparison 9 Bisphosphonate versus calcitonin, Outcome 3 Bone mineral density [g calcium/cm2].
Bisphosphonate may slightly increase BMD at the femoral neck compared with calcitonin therapy (Analysis 9.3.2 (3 studies, 104 participants): MD 0.06 g calcium/cm2, 95% CI 0.02 to 0.11). There was evidence of low statistical heterogeneity (I2 = 33%).
Serum parathyroid hormone
It is uncertain whether bisphosphonate compared with calcitonin therapy makes any difference to serum PTH levels (Analysis 9.4 (2 studies, 61 participants): MD 0.01 pmol/L, 95% CI ‐0.61 to 0.63; I2 = 0%).
9.4. Analysis.
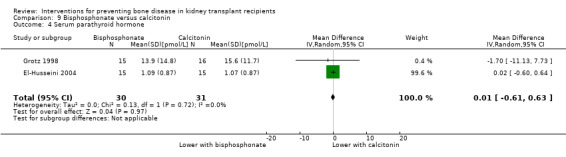
Comparison 9 Bisphosphonate versus calcitonin, Outcome 4 Serum parathyroid hormone.
Graft loss
El‐Husseini 2004 reported no graft losses in either group (Analysis 9.5).
9.5. Analysis.
Comparison 9 Bisphosphonate versus calcitonin, Outcome 5 Graft loss.
Graft function
El‐Husseini 2004 reported no difference in SCr between the two groups (Analysis 9.6).
9.6. Analysis.
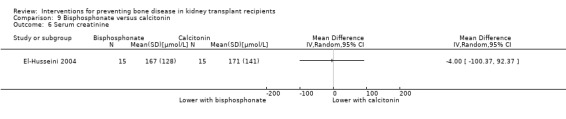
Comparison 9 Bisphosphonate versus calcitonin, Outcome 6 Serum creatinine.
Gastrointestinal symptoms
Diarrhoea
Grotz 1998 reported one event in the bisphosphonate group (Analysis 9.7).
9.7. Analysis.
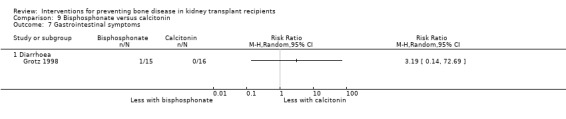
Comparison 9 Bisphosphonate versus calcitonin, Outcome 7 Gastrointestinal symptoms.
Other outcomes
The following outcomes were not reported: acute graft rejection, death, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, gastro‐oesophageal disorder, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Bisphosphonate plus vitamin D versus vitamin D
Trabulus 2008 reported no fractures in either group (Analysis 10.1); an increase in vertebral BMD with vitamin D alone (Analysis 10.2.1); no difference femoral neck BMD (Analysis 10.2.2); no differences in SCr (Analysis 10.3), or eGFR (Analysis 10.4); and no difference in hypercalcaemia (Analysis 10.5).
10.1. Analysis.
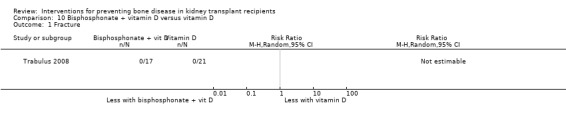
Comparison 10 Bisphosphonate + vitamin D versus vitamin D, Outcome 1 Fracture.
10.2. Analysis.
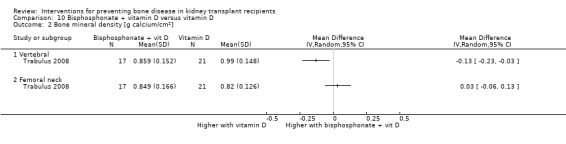
Comparison 10 Bisphosphonate + vitamin D versus vitamin D, Outcome 2 Bone mineral density [g calcium/cm2].
10.3. Analysis.
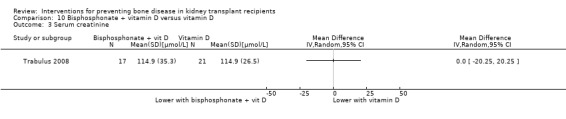
Comparison 10 Bisphosphonate + vitamin D versus vitamin D, Outcome 3 Serum creatinine.
10.4. Analysis.
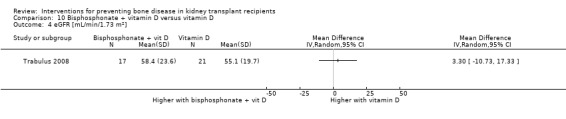
Comparison 10 Bisphosphonate + vitamin D versus vitamin D, Outcome 4 eGFR [mL/min/1.73 m2].
10.5. Analysis.
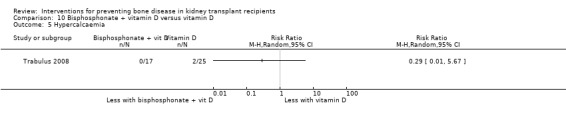
Comparison 10 Bisphosphonate + vitamin D versus vitamin D, Outcome 5 Hypercalcaemia.
The following outcomes were not reported: acute graft rejection, death, musculoskeletal disorders, stroke, myocardial infarction; presence of low bone turnover, serum PTH, vascular calcification score, proteinuria, graft loss, gastro‐oesophageal disorder; gastrointestinal symptoms, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Bisphosphonate plus vitamin D versus placebo or no treatment
Dovas 2009 reported no differences in PTH between the groups (Analysis 11.1).
11.1. Analysis.
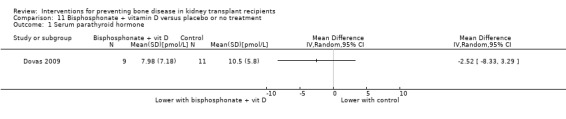
Comparison 11 Bisphosphonate + vitamin D versus placebo or no treatment, Outcome 1 Serum parathyroid hormone.
The following outcomes were not reported: fracture, acute graft rejection, death, musculoskeletal disorders, BMD, stroke, myocardial infarction; presence of low bone turnover, serum PTH, vascular calcification score, proteinuria, graft loss, graft function, gastro‐oesophageal disorder; gastrointestinal symptoms, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Vitamin D versus calcitonin
El‐Agroudy 2003a reported no fractures (Analysis 12.1), bone pain (Analysis 12.2.1), or graft loss (Analysis 12.5) in either group. There were no differences in vertebral or femoral BMD (Analysis 12.3), PTH (Analysis 12.4) or SCr (Analysis 12.6).
12.1. Analysis.
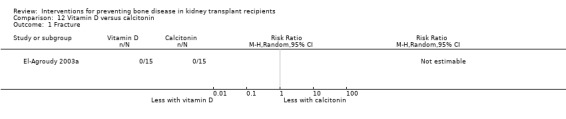
Comparison 12 Vitamin D versus calcitonin, Outcome 1 Fracture.
12.2. Analysis.
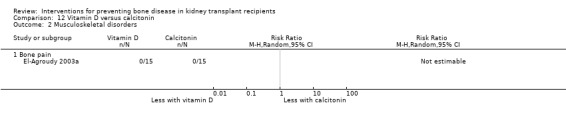
Comparison 12 Vitamin D versus calcitonin, Outcome 2 Musculoskeletal disorders.
12.5. Analysis.
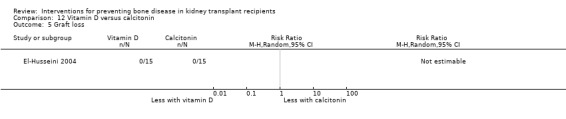
Comparison 12 Vitamin D versus calcitonin, Outcome 5 Graft loss.
12.3. Analysis.
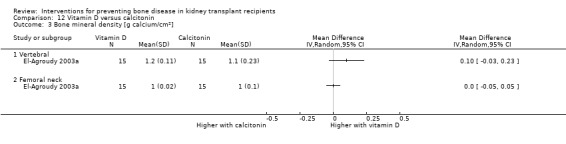
Comparison 12 Vitamin D versus calcitonin, Outcome 3 Bone mineral density [g calcium/cm2].
12.4. Analysis.
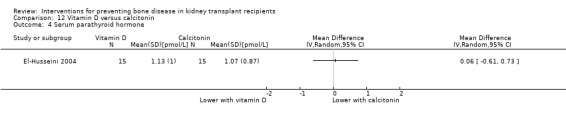
Comparison 12 Vitamin D versus calcitonin, Outcome 4 Serum parathyroid hormone.
12.6. Analysis.
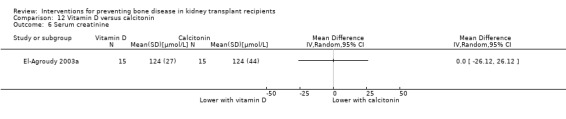
Comparison 12 Vitamin D versus calcitonin, Outcome 6 Serum creatinine.
The following outcomes were not reported: death, acute graft rejection, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, gastro‐oesophageal disorder; gastrointestinal symptoms, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Vitamin D versus vitamin D plus calcium
Kharlamov 2012 reported one death in the vitamin d plus calcium group (Analysis 13.1) and no difference in eGFR (Analysis 13.2).
13.1. Analysis.
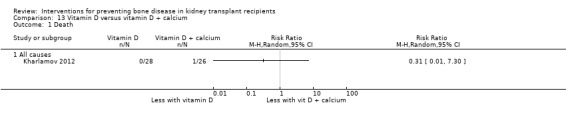
Comparison 13 Vitamin D versus vitamin D + calcium, Outcome 1 Death.
13.2. Analysis.
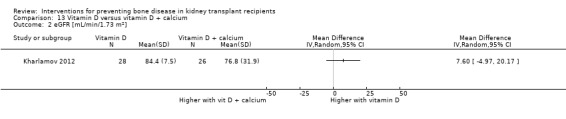
Comparison 13 Vitamin D versus vitamin D + calcium, Outcome 2 eGFR [mL/min/1.73 m2].
The following outcomes were not reported: fracture, acute graft rejection, musculoskeletal disorders, BMD, stroke, myocardial infarction; presence of low bone turnover, serum PTH, vascular calcification score, proteinuria, graft loss, gastro‐oesophageal disorder; gastrointestinal symptoms, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Vitamin D versus cinacalcet
Pasquali 2014 reported no difference in PTH between the groups (Analysis 14.1).
14.1. Analysis.
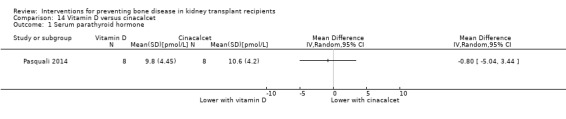
Comparison 14 Vitamin D versus cinacalcet, Outcome 1 Serum parathyroid hormone.
The following outcomes were not reported: fracture, death, acute graft rejection, musculoskeletal disorders, BMD, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, graft loss, graft function, gastro‐oesophageal disorder; gastrointestinal symptoms, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Cinacalcet versus subtotal parathyroidectomy
Cruzado 2015 reported one fracture in the cinacalcet group (Analysis 15.1) and no deaths (Analysis 15.2). There was no difference in vertebral BMD (Analysis 15.3.1), however femoral neck BMD was higher with parathyroidectomy (Analysis 15.3.2). PTH was lower with parathyroidectomy (Analysis 15.4). There were no differences in vascular calcification score (Analysis 15.5), proteinuria (Analysis 15.6), eGFR (Analysis 15.7), hypercalcaemia (Analysis 15.8) or hypocalcaemia (Analysis 15.9).
15.1. Analysis.
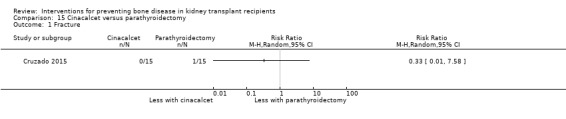
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 1 Fracture.
15.2. Analysis.
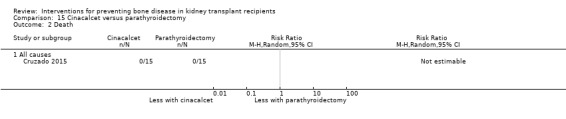
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 2 Death.
15.3. Analysis.
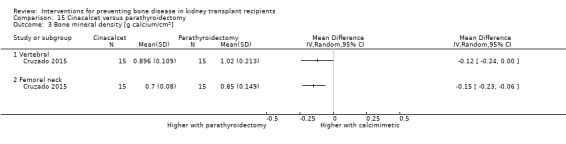
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 3 Bone mineral density [g calcium/cm2].
15.4. Analysis.
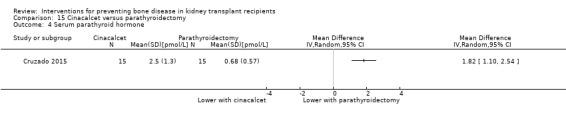
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 4 Serum parathyroid hormone.
15.5. Analysis.
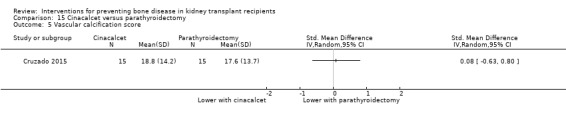
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 5 Vascular calcification score.
15.6. Analysis.
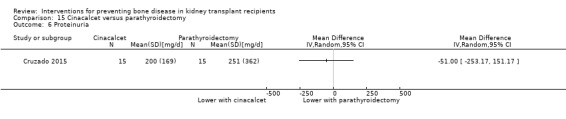
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 6 Proteinuria.
15.7. Analysis.
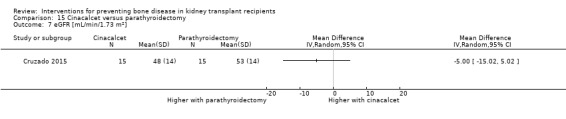
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 7 eGFR [mL/min/1.73 m2].
15.8. Analysis.
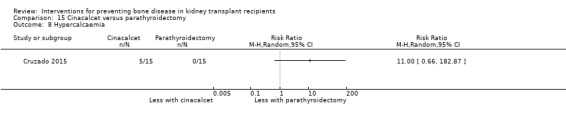
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 8 Hypercalcaemia.
15.9. Analysis.
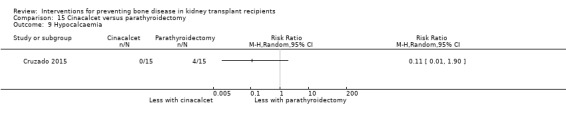
Comparison 15 Cinacalcet versus parathyroidectomy, Outcome 9 Hypocalcaemia.
The following outcomes were not reported: acute graft rejection, musculoskeletal disorders, stroke, myocardial infarction; presence of low bone turnover, graft loss, gastro‐oesophageal disorder; gastrointestinal symptoms, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Potassium citrate versus potassium chloride
Starke 2012 reported no differences in PTH (Analysis 16.1) or eGFR (Analysis 16.2).
16.1. Analysis.
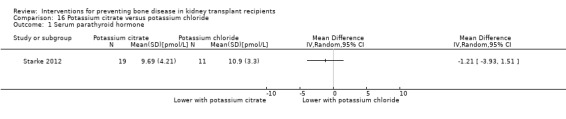
Comparison 16 Potassium citrate versus potassium chloride, Outcome 1 Serum parathyroid hormone.
16.2. Analysis.
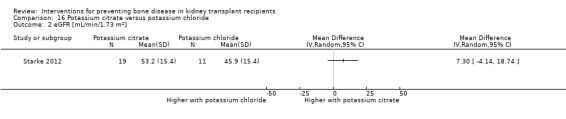
Comparison 16 Potassium citrate versus potassium chloride, Outcome 2 eGFR [mL/min/1.73 m2].
The following outcomes were not reported: fracture, acute graft rejection, death, musculoskeletal disorders, BMD, stroke, myocardial infarction; presence of low bone turnover, vascular calcification score, proteinuria, graft loss, gastro‐oesophageal disorder; gastrointestinal symptoms, hyper‐ or hypocalcaemia, haemoglobin, leucopenia, neuropsychiatric disorder, venous thromboembolism, oedema, or hot flushes.
Publication bias and subgroup analysis
Evidence of small study effects was examined for the outcome of fracture for all drug comparisons in which sufficient data observations were available (10 or more studies) and in which there was low or no statistical heterogeneity between studies. Overall, there were sufficient data for the outcome of fracture in studies comparing bisphosphonate treatment with placebo or no treatment. There was no evidence of small study effects in this analysis (Figure 5).
5.
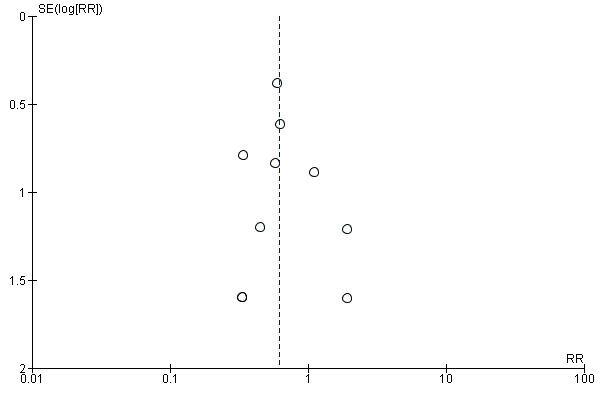
Funnel plot of comparison studies comparing bisphosphonate versus placebo or no treatment for the study endpoint of fracture
Subgroup analysis was carried out for the primary efficacy outcome (fracture) for the comparison of bisphosphonate versus placebo or no treatment. There was no evidence that treatment effects were modified by whether patients were incident (treatment at time of transplant) or prevalent (treatment after transplantation) (Analysis 17.1) (Figure 6), in adults or children (Analysis 17.2), with treatment duration (Analysis 17.3) or treatment for primary or secondary prevention (Analysis 17.4). In addition, there was no evidence of different effects of bisphosphonate therapy for systematically captured fracture events and clinical follow up (Analysis 17.5), baseline BMD (Analysis 17.6), peripheral or spinal fractures (Analysis 17.7), or drug potency (Analysis 17.8). There was no evidence of different effects of bisphosphonates on BMD based on drug potency (Analysis 17.9).
17.1. Analysis.
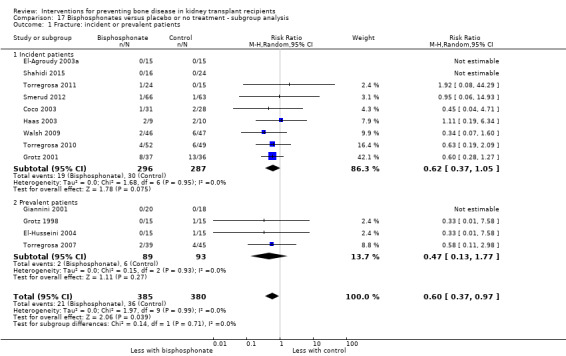
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 1 Fracture: incident or prevalent patients.
6.
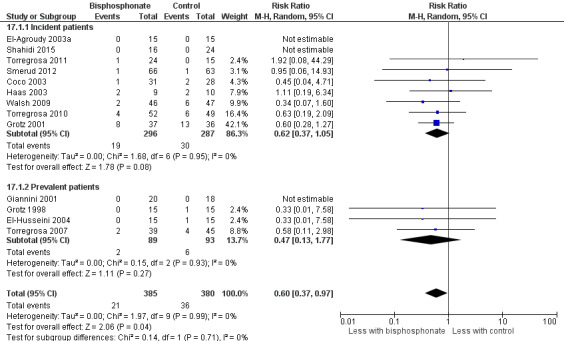
Subgroup analysis of bisphosphonate therapy versus placebo or no treatment on risk of fracture comparing effects in prevalent and incident kidney transplant recipients
17.2. Analysis.
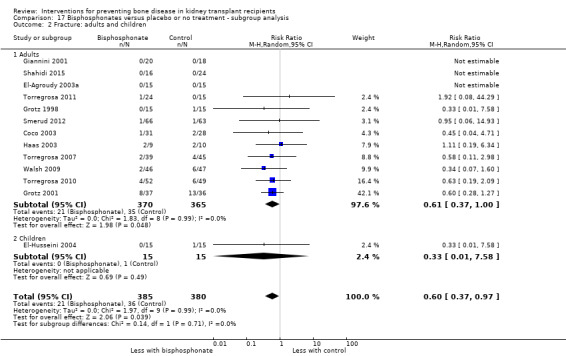
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 2 Fracture: adults and children.
17.3. Analysis.
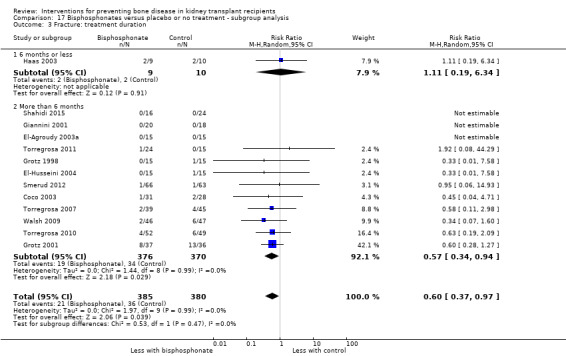
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 3 Fracture: treatment duration.
17.4. Analysis.
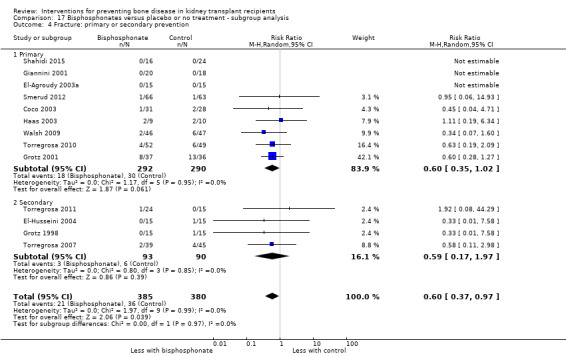
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 4 Fracture: primary or secondary prevention.
17.5. Analysis.
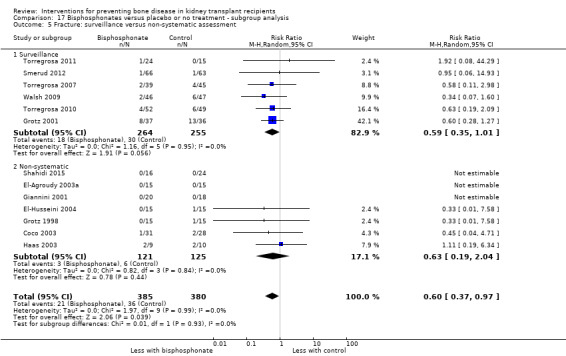
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 5 Fracture: surveillance versus non‐systematic assessment.
17.6. Analysis.
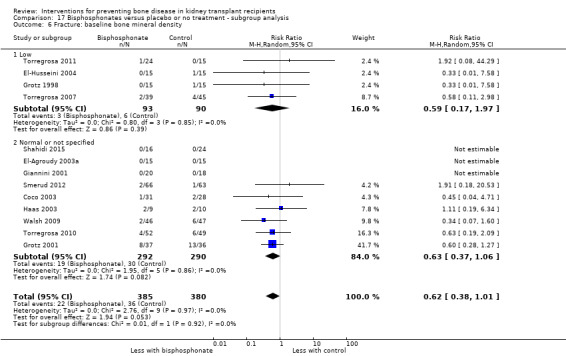
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 6 Fracture: baseline bone mineral density.
17.7. Analysis.
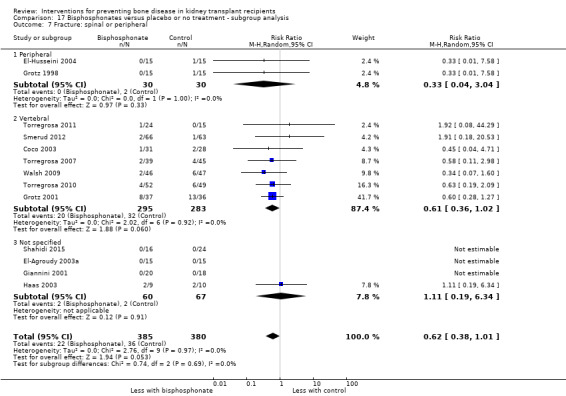
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 7 Fracture: spinal or peripheral.
17.8. Analysis.
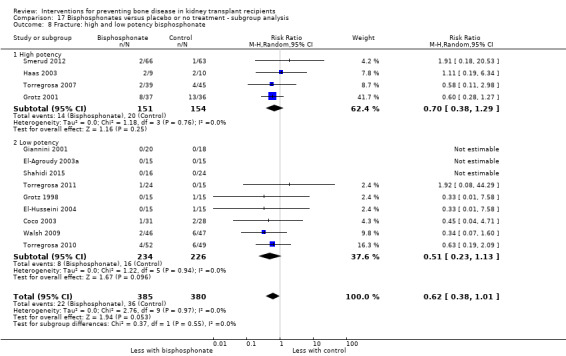
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 8 Fracture: high and low potency bisphosphonate.
17.9. Analysis.
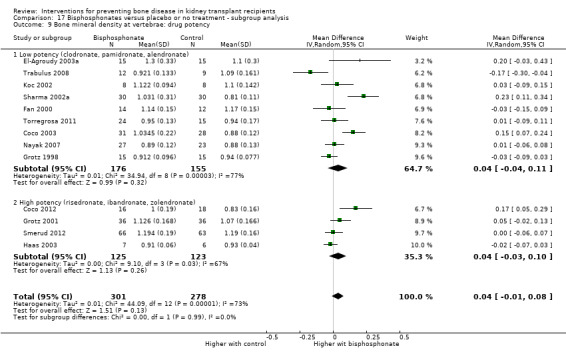
Comparison 17 Bisphosphonates versus placebo or no treatment ‐ subgroup analysis, Outcome 9 Bone mineral density at vertebrae: drug potency.
Discussion
Summary of main results
In this review update of the evidence for bone disease treatment after kidney transplantation, 65 studies involving 3538 participants were eligible; 45 studies (2698 participants) could be analysed. Studies generally included follow‐up for 12 months. Forty‐three studies were designed to evaluate the impact of treatment on BMD or histomorphometry. Studies were not designed to evaluate whether treatments made any difference to cardiovascular endpoints or vascular calcification, which are known to be associated with CKD‐MBD and which might be modified with bone‐targeted therapies. One study evaluated treatment in 60 children or young adults. The interventions included bisphosphonates, oral vitamin D compounds, synthetic PTH (teriparatide), RANKL inhibitor (denosumab), cinacalcet, parathyroidectomy, and calcium supplementation, alone or in combination. Bisphosphonate therapy was usually commenced within three weeks of transplantation and regardless of BMD.
Compared with placebo or standard care, bisphosphonate therapy given for 12 months at any time after kidney transplantation may reduce the risk of fracture, although the 95% CI included the possibility that bisphosphonate therapy might make little or no difference. Most fracture events were identified by routine surveillance radiographs of the spine, and may have not caused clinical symptoms. The clinical relevance of this outcome to patients and decision‐makers is unclear. It is uncertain whether any other therapy made any difference to fracture risk. Bisphosphonate therapy may decrease risk of acute graft rejection. It was uncertain whether any drug class decreased death or cardiovascular events. Bisphosphonate therapy may reduce bone pain, although data for this outcome were derived from a single centre. It is very uncertain whether bisphosphonates prevent spinal deformity or avascular bone necrosis. Bisphosphonates may lead to hypocalcaemia. It was uncertain whether vitamin D compounds had any effect on skeletal, cardiovascular, mortality, or transplant function outcomes. Evidence for the benefits and harms of all other treatments was of very low certainty. Evidence about treatment for children and young adolescents was sparse. Single recent studies evaluated newer therapies including RANKL inhibitors, synthetic PTH (denosumab), and calcimimetic therapy (cinacalcet). There was limited evidence that any treatment made any difference to BMD in analyses that were marked by often high statistical heterogeneity, leading to lower certainty in the results. Heterogeneity in analyses for BMD were likely due to marked differences in BMD between studies at baseline.
Overall completeness and applicability of evidence
This review aimed to be a comprehensive analysis of the benefits and harms of treatments for bone disease after kidney transplantation updated with evidence to 2019. This review principally examined the evidence of treatment benefits based on patient‐centred outcomes (fracture, death (all cause and cardiovascular), myocardial infarction, stroke, bone pain, skeletal deformity) and potential harms (including acute graft rejection and/or graft loss and adverse effects). As noted in previous versions of this review published in 2004 and updated in 2007, evidence for bone therapy in clinical trials in transplantation has been evaluated primarily using BMD and bone biomarkers and histomorphometry. The clinical relevance of these endpoints to predict subsequent risks of fracture or skeletal symptoms remains uncertain in the post‐transplant period as patients may have heterogeneous bone‐related changes including low bone turnover from pre‐existing kidney disease, elevated circulating PTH levels before and after transplantation, and glucocorticoid therapy in the post‐transplantation period (Weisinger 2006). Notably, none of the available studies reported fracture risk or skeletal symptoms as a primary outcome, with all but nine studies evaluating BMD, bone histology or bone‐related markers as the primary outcome for efficacy. Twenty‐five studies evaluated fracture risk, often not systematically and without blinding of outcome assessment. Fracture measurement in studies was principally based on skeletal radiographs. Bone pain was reported in four studies, spinal deformity was reported in one study, and avascular bone necrosis was reported in two studies. Death (all causes) was reported in 17 studies, although very few clinical events were observed.
Most studies had between six and 12 months of follow‐up after treatment was started, which limited the ability of the current evidence to measure longer term consequences of therapy on bone symptoms and transplant function, and importantly, any potential harms of therapy. Bisphosphonate treatment is associated with osteonecrosis of the jaw and may have different long‐term impact of bone health in the context of pre‐existing adynamic bone function accrued during treatment on dialysis and pre‐existing end‐stage kidney disease. Future long‐term post‐marketing surveillance and pragmatic trials of several years duration including those that capture data from within transplant registries could inform clinical practice about the longer term effects of such therapies to prevent bone disease. While this review did not identify evidence with high certainty for adverse effects of treatment, it should be noted that the systematic capture of treatment‐related harms was not included in most available studies.
The studies did not consistently include treatment administration commencing at the time of transplantation. In many studies, the time‐lag between transplantation and bone disease treatment was variable. While there was no evidence that the timing of treatment modified the effectiveness of bisphosphonate treatment, there were relatively few studies and data observations, such that the power of any analyses to detect a difference based on treatment timing was low. In addition, the inclusion criteria in studies varied from only patients with evidence of osteopenia identified by BMD scanning to patients unselected by existing bone density and including all patients at the time of transplantation. Therefore, it is unclear whether bisphosphonate treatment had different effectiveness based on BMD at the time treatment was commenced.
Only one study included children or young adults. Therefore, we were unable to determine the impact of bone treatment on children‐relevant outcomes including growth and height, bone pain and deformity and other outcomes of possible relevance to children and their families such as school attendance and educational attainment. Evidence overall for some therapies including RANKL inhibitors, synthetic PTH, and cinacalcet was limited to single studies. Additional evidence of efficacy is needed if these interventions are to be considered in routine clinical practice including adequate assessment of treatment‐related harms.
Quality of the evidence
In general, evidence identified in this systematic review for the primary efficacy and safety outcomes (fracture and acute rejection) was of low certainty meaning that the research provides only some indication of the likely effects of treatment. The evidence certainty for bisphosphonate therapy was principally downgraded due to the risk of bias in the included studies and reliance on few events leading to imprecision. The internal validity of the design, conduct, and analysis of the included studies was often difficult to assess due to omission of important methodologic details in the trial reports. Most studies failed to report the method of allocation concealment, whether outcome assessment was blinded, and selectively reported patient‐level outcomes. Of the 65 included studies, only six (9%) reporting blinding of participants and investigators to treatment allocation and four (8%) reported blinded outcome assessment including fractures. This was considered important as clinical decision making and interpretation of radiographs might have been influenced by knowledge of treatment allocation including withdrawal of steroids or interpretation of X‐ray findings for vertebral compression or limb fracture. The random sequence was at low risk of bias in eight studies and allocation to treatment was adequately concealed in only two studies. Knowledge of the treatment allocation might prompt investigators to selectively allocate treatment to specific patients (avoiding therapy in patient for whom treatment might be considered as less efficacious or more hazardous) and lower the certainty in the findings. It was not fully clear whether many studies were truly randomised and large differences in the BMD at baseline in different treatment groups precluded robust interpretations of the effects of many treatments on BMD.
Potential biases in the review process
While we sought evidence from the Cochrane Kidney and Transplant Specialised Register which includes hand‐searched study reports from the grey literature, it is possible that some studies were missed that were reported in the bone disease literature and that were not tagged for identification by our trials registry processes. There is a possibility that we did not include studies reported in conference proceedings or that were not reported in English. In some studies, information about some patient‐level outcomes were not reported in ways that could be extracted, which lowered certainty in the results.
Agreements and disagreements with other studies or reviews
The results of this review update are largely unchanged from our previous version of this Cochrane review that previously concluded that bisphosphonate therapy after kidney transplantation may make little or no difference to fracture or bone pain (Palmer 2007). Despite an additional 30 studies, evidence for whether bisphosphonates decrease fracture risk is still of low or very low certainty. The effects of treatment include the possibility of making little or no difference to fracture risk. Similarly, while there is evidence that bisphosphonates may decrease risks of acute graft rejection, this information has low certainty due to limitations in the available studies and reliance on an implausible rate of acute graft rejection in some studies, out of keeping with clinical practice. It is biologically possible that bisphosphonate therapy might influence graft rejection rates through the immunomodulatory and anti‐inflammatory properties of bisphosphonate drugs, which have been shown to suppress T‐cell function through suppression of cytokine release from activated macrophages/monocytes (Chambers 1980; de Vries 1982) and reduce graft rejection in animal studies (Fryer 1996).
This systematic review is consistent with a meta‐analysis reported in 2016 evaluating bisphosphonate to prevent bone complications in kidney transplant recipients that included four studies reporting fracture events in 296 participants (Versele 2016). In that review, the proportional reduction in risk of fracture with bisphosphonate (RR 0.58) was nearly identical to this Cochrane review (RR 0.62), and similarly the 95% CI included the possibility of no effect. As in the current Cochrane review, in that earlier review bisphosphonate therapy was associated with a reduced risk of acute graft rejection (RR 0.55, 95% CI 0.33 to 0.91) in two studies. In another systematic review of bisphosphonate therapy published in 2016 that included nine studies, the authors concluded that there was no evidence that bisphosphonate therapy reduced fracture risk in two studies and there were no reported bone pain or skeletal outcome or transplant function end‐points described by the reviewers (Wang 2016). The finding in this Cochrane review update of a relative lack of evidence to support clinical practice in children with a kidney transplant is similar to a 2015 Cochrane review of interventions for metabolic bone disease in children with CKD that identified a paucity of evidence for patient‐centred outcomes including growth rates, height, and bone pain and deformity (Hahn 2015).
Notably, it was uncertain whether bisphosphonate therapy made difference to BMD. In the setting of liver transplantation, BMD was not associated with prevalent vertebral fractures at screening before transplantation (Krol 2014a) or during the first 12 months after transplantation (Krol 2014b), suggesting BMD assessment may not correlate with vertebral fractures identified in surveillance radiographs in clinical trials.
Authors' conclusions
Implications for practice.
Bisphosphonates at the time or after kidney transplantation may decrease the risk of bone fracture pain during 12 months of follow‐up although there is the possibility that treatment makes little or no difference to skeletal complications. Most fracture events reported in studies may not have caused clinical symptoms.
It is unclear whether any treatment class other than bisphosphonates makes any difference to bone complications after kidney transplantation. There is little or no evidence to support the use of vitamin D, calcitonin, cinacalcet, RANKL inhibitors, or synthetic PTH to prevent skeletal complications after kidney transplantation.
Existing studies of bone disease therapies were not designed to measure mortality, cardiovascular events, or fracture.
Information about bisphosphonate treatment in children and young adults is very limited and does not allow any conclusions to be drawn on the effects of treatment on growth, height, or skeletal symptoms.
Follow‐up in existing studies is generally limited to 12 months. The longer term benefits and safety of therapy are unknown.
There is no evidence that bisphosphonate treatment is harmful and may prevent acute graft rejection, but the long term effects on graft survival or complications of immunosuppression such as infection or malignancy are unclear.
The effects of bisphosphonate treatment on BMD is uncertain due to the heterogeneous treatment effects across available studies.
Adverse effects of treatments are poorly quantified and very uncertain.
Implications for research.
Given the adverse consequences of skeletal fracture and pain after kidney transplantation, studies designed to measure these endpoints and safety outcomes are needed to determine if treatment should be recommended in clinical practice
Reliance on BMD as a primary outcome in clinical trials is unhelpful due to the relative lack of an association between bone density and risks of fracture and skeletal deformity and should not be a primary endpoint in future clinical studies.
Trials of bone therapies must prioritise bone fracture and other patient‐centred complications and adjudicate these endpoints blinded to treatment allocation.
Longer‐term studies are required in both adults and children, considering the endpoints that matter most to patients and their families including cardiovascular endpoints such as death, myocardial infarction, heart failure, and stroke.
Bone therapies require long‐term data for clinical endpoints in trials sufficiently powered to inform clinical care.
The benefit of bone therapy started in all patients at time of kidney transplantation is a specific population that requires a well‐conducted clinical trial. Pragmatic trial design including registry‐based follow‐up may facilitate recruitment and ensure efficient follow‐up for clinical events.
The benefits and harms of specific treatments among patients with impaired transplant function and among those with persistent hyperparathyroidism need to be determined.
What's new
| Date | Event | Description |
|---|---|---|
| 12 June 2019 | New citation required but conclusions have not changed | 42 new studies added |
| 12 June 2019 | New search has been performed | Updated search and review findings using search date 16 May 2019 |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 2, 2005
| Date | Event | Description |
|---|---|---|
| 13 August 2009 | Amended | Contact details updated. |
| 9 October 2008 | Amended | Converted to new review format. |
| 30 April 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The authors acknowledge the contribution of Drs Fan, El‐Agroudy, Torregrosa, Koc, De Sevaux, Jeffrey, Torres, Coco, Kharlamov, and Cruzado who responded to our queries about their studies. We also wish to thank the reviewers for their comments and feedback during the preparation of this review update. The funding and editorial support from Cochrane Kidney and Transplant to assist with the completion of the review is also gratefully acknowledged.
Appendices
Appendix 1. Electronic search strategies
| Database | Search strategy |
| CENTRAL |
|
| MEDLINE |
|
| EMBASE |
|
Appendix 2. Risk of bias assessment tool
| Potential source of bias | Assessment criteria |
|
Random sequence generation Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence |
Low risk of bias: Random number table; computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots; minimisation (minimisation may be implemented without a random element, and this is considered to be equivalent to being random). |
| High risk of bias: Sequence generated by odd or even date of birth; date (or day) of admission; sequence generated by hospital or clinic record number; allocation by judgement of the clinician; by preference of the participant; based on the results of a laboratory test or a series of tests; by availability of the intervention. | |
| Unclear: Insufficient information about the sequence generation process to permit judgement. | |
|
Allocation concealment Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment |
Low risk of bias: Randomisation method described that would not allow investigator/participant to know or influence intervention group before eligible participant entered in the study (e.g. central allocation, including telephone, web‐based, and pharmacy‐controlled, randomisation; sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes). |
| High risk of bias: Using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure. | |
| Unclear: Randomisation stated but no information on method used is available. | |
|
Blinding of participants and personnel Performance bias due to knowledge of the allocated interventions by participants and personnel during the study |
Low risk of bias: No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding; blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken. |
| High risk of bias: No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding. | |
| Unclear: Insufficient information to permit judgement | |
|
Blinding of outcome assessment Detection bias due to knowledge of the allocated interventions by outcome assessors. |
Low risk of bias: No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. |
| High risk of bias: No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding. | |
| Unclear: Insufficient information to permit judgement | |
|
Incomplete outcome data Attrition bias due to amount, nature or handling of incomplete outcome data. |
Low risk of bias: No missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data have been imputed using appropriate methods. |
| High risk of bias: Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; ‘as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation. | |
| Unclear: Insufficient information to permit judgement | |
|
Selective reporting Reporting bias due to selective outcome reporting |
Low risk of bias: The study protocol is available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way; the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon). |
| High risk of bias: Not all of the study’s pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. sub‐scales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study. | |
| Unclear: Insufficient information to permit judgement | |
|
Other bias Bias due to problems not covered elsewhere in the table |
Low risk of bias: The study appears to be free of other sources of bias. |
| High risk of bias: Had a potential source of bias related to the specific study design used; stopped early due to some data‐dependent process (including a formal‐stopping rule); had extreme baseline imbalance; has been claimed to have been fraudulent; had some other problem. | |
| Unclear: Insufficient information to assess whether an important risk of bias exists; insufficient rationale or evidence that an identified problem will introduce bias. |
Data and analyses
Comparison 1. Bisphosphonate versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| 2 Acute graft rejection | 7 | 470 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.55, 0.89] |
| 3 Death | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 All causes | 10 | 597 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.34, 2.80] |
| 3.2 Cardiovascular | 3 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.58] |
| 4 Musculoskeletal disorders | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Bone pain | 3 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.04, 0.93] |
| 4.2 Spinal deformity | 1 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.26, 1.31] |
| 5 Bone mineral density [g calcium/cm2] | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Vertebral | 13 | 579 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.01, 0.08] |
| 5.2 Femoral neck | 12 | 520 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.03, 0.07] |
| 6 Presence of low bone turnover seen on bone histomorphometry | 2 | 33 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.76, 3.64] |
| 7 Serum parathyroid hormone | 11 | 590 | Mean Difference (IV, Random, 95% CI) | 0.70 [‐0.62, 2.02] |
| 8 Vascular calcification score | 2 | 74 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.46, 0.46] |
| 9 Proteinuria (urinary protein:creatinine ratio) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10 Graft loss | 7 | 403 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.27, 1.60] |
| 11 Serum creatinine | 12 | 504 | Mean Difference (IV, Random, 95% CI) | 2.18 [‐7.78, 12.15] |
| 12 eGFR [mL/min/1.73 m2] | 2 | 82 | Mean Difference (IV, Random, 95% CI) | ‐0.97 [‐17.62, 15.67] |
| 13 Gastro‐oesophageal disorder | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14 Gastrointestinal symptoms | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14.1 Nausea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Hypercalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 16 Hypocalcaemia | 4 | 207 | Risk Ratio (M‐H, Random, 95% CI) | 5.59 [1.00, 31.06] |
Comparison 2. Vitamin D versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 5 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.10, 8.94] |
| 2 Acute graft rejection | 5 | 385 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.52, 1.86] |
| 3 Death | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 All causes | 3 | 232 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.03, 9.22] |
| 3.2 Cardiovascular | 3 | 232 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.04, 7.57] |
| 4 Musculoskeletal disorders | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Bone pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Bone mineral density [g calcium/cm2] | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Vertebral | 9 | 377 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.03, 0.07] |
| 5.2 Femoral neck | 7 | 292 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.07, 0.06] |
| 6 Serum parathyroid hormone | 6 | 340 | Mean Difference (IV, Random, 95% CI) | ‐1.74 [‐3.04, ‐0.44] |
| 7 Proteinuria | 2 | 245 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐1.24, 0.39] |
| 8 Graft loss | 3 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.11 [0.01, 2.01] |
| 9 Serum creatinine | 6 | 313 | Mean Difference (IV, Random, 95% CI) | 3.87 [‐3.64, 11.37] |
| 10 eGFR [mL/min/1.73 m2] | 6 | 449 | Mean Difference (IV, Random, 95% CI) | 3.96 [‐7.59, 15.52] |
| 11 Hypercalcaemia | 7 | 465 | Risk Ratio (M‐H, Random, 95% CI) | 2.09 [0.84, 5.22] |
| 12 Fever | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 13 Myocardial infarction | 2 | 143 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 7.68] |
| 14 Stroke | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 15 Parathyroidectomy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 3. Calcitonin versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 4 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.06, 1.78] |
| 2 Death | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 All causes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Cardiovascular | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Musculoskeletal disorders | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Avascular bone necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Bone mineral density [g calcium/cm2] | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Vertebral | 2 | 61 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.10, 0.02] |
| 4.2 Femoral neck | 2 | 61 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.08, 0.15] |
| 5 Serum parathyroid hormone | 2 | 61 | Mean Difference (IV, Random, 95% CI) | 0.88 [‐2.62, 4.38] |
| 6 Graft loss | 2 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.01, 3.63] |
| 7 Serum creatinine | 2 | 61 | Mean Difference (IV, Random, 95% CI) | ‐31.12 [‐141.96, 79.72] |
| 8 Gastrointestinal symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Hypocalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
3.9. Analysis.
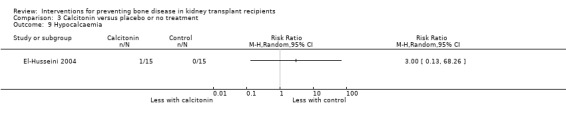
Comparison 3 Calcitonin versus placebo or no treatment, Outcome 9 Hypocalcaemia.
Comparison 4. RANKL inhibitor (denosumab) versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Acute graft rejection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Graft loss | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Gastrointestinal symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Hypocalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 5. Synthetic human PTH (teriparatide) versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Acute graft rejection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Bone mineral density [g calcium/cm2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Lumbar spine | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Femoral neck | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Presence of low bone turnover on bone histomorphometry | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Serum creatinine | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 6. Calcimimetic (cinacalcet) versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Death | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 All causes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Cardiovascular | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Bone mineral density [g calcium/cm2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Lumbar spine | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Femoral neck | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Gastrointestinal symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 7. Vitamin D + calcium versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.90] |
| 2 Acute graft rejection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Death | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 All causes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Musculoskeletal disorders | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Bone pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Avascular bone necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Bone mineral density [g calcium/cm2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Vertebral | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Femoral neck | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Presence of low bone turnover on bone histomorphometry | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Serum parathyroid hormone | 2 | 188 | Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐2.94, 2.31] |
| 8 Graft loss | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 2.38 [0.26, 22.12] |
| 9 Serum creatinine | 3 | 218 | Mean Difference (IV, Random, 95% CI) | 10.24 [‐0.05, 20.53] |
| 10 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11 Gastro‐oesophageal disorder | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12 Hypercalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 8. Bisphosphonate versus vitamin D.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 2 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Death | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 All causes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Musculoskeletal disorders | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Bone pain | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Bone mineral density [g calcium/cm2] | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Vertebral | 4 | 176 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.05, 0.09] |
| 4.2 Femoral neck | 4 | 176 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.05, 0.06] |
| 5 Serum parathyroid hormone | 2 | 63 | Mean Difference (IV, Random, 95% CI) | 3.14 [‐3.55, 9.82] |
| 6 Graft loss | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Serum creatinine | 2 | 63 | Mean Difference (IV, Random, 95% CI) | ‐17.16 [‐35.63, 1.31] |
| 8 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Hypercalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10 Hypocalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 9. Bisphosphonate versus calcitonin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 2 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.02, 8.08] |
| 2 Musculoskeletal disorders | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Bone pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Bone mineral density [g calcium/cm2] | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Vertebral | 2 | 61 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.10, 0.31] |
| 3.2 Femoral neck | 3 | 104 | Mean Difference (IV, Random, 95% CI) | 0.06 [0.02, 0.11] |
| 4 Serum parathyroid hormone | 2 | 61 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.61, 0.63] |
| 5 Graft loss | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Serum creatinine | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Gastrointestinal symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 10. Bisphosphonate + vitamin D versus vitamin D.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Bone mineral density [g calcium/cm2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Vertebral | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Femoral neck | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Serum creatinine | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Hypercalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 11. Bisphosphonate + vitamin D versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 12. Vitamin D versus calcitonin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Musculoskeletal disorders | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Bone pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Bone mineral density [g calcium/cm2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Vertebral | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Femoral neck | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Graft loss | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Serum creatinine | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 13. Vitamin D versus vitamin D + calcium.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Death | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 All causes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 14. Vitamin D versus cinacalcet.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 15. Cinacalcet versus parathyroidectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Death | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 All causes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Bone mineral density [g calcium/cm2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Vertebral | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Femoral neck | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Vascular calcification score | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Proteinuria | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Hypercalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Hypocalcaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 16. Potassium citrate versus potassium chloride.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serum parathyroid hormone | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 eGFR [mL/min/1.73 m2] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 17. Bisphosphonates versus placebo or no treatment ‐ subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture: incident or prevalent patients | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.37, 0.97] |
| 1.1 Incident patients | 9 | 583 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.37, 1.05] |
| 1.2 Prevalent patients | 4 | 182 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.13, 1.77] |
| 2 Fracture: adults and children | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.37, 0.97] |
| 2.1 Adults | 12 | 735 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.37, 1.00] |
| 2.2 Children | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.58] |
| 3 Fracture: treatment duration | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.37, 0.97] |
| 3.1 6 months or less | 1 | 19 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.19, 6.34] |
| 3.2 More than 6 months | 12 | 746 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.34, 0.94] |
| 4 Fracture: primary or secondary prevention | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.37, 0.97] |
| 4.1 Primary | 9 | 582 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.35, 1.02] |
| 4.2 Secondary | 4 | 183 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.17, 1.97] |
| 5 Fracture: surveillance versus non‐systematic assessment | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.37, 0.97] |
| 5.1 Surveillance | 6 | 519 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.35, 1.01] |
| 5.2 Non‐systematic | 7 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.19, 2.04] |
| 6 Fracture: baseline bone mineral density | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| 6.1 Low | 4 | 183 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.17, 1.97] |
| 6.2 Normal or not specified | 9 | 582 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.37, 1.06] |
| 7 Fracture: spinal or peripheral | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| 7.1 Peripheral | 2 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.04] |
| 7.2 Vertebral | 7 | 578 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.36, 1.02] |
| 7.3 Not specified | 4 | 127 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.19, 6.34] |
| 8 Fracture: high and low potency bisphosphonate | 13 | 765 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| 8.1 High potency | 4 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.38, 1.29] |
| 8.2 Low potency | 9 | 460 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.23, 1.13] |
| 9 Bone mineral density at vertebrae: drug potency | 13 | 579 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.01, 0.08] |
| 9.1 Low potency (clodronate, pamidronate, alendronate) | 9 | 331 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.04, 0.11] |
| 9.2 High potency (risedronate, ibandronate, zolendronate) | 4 | 248 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.03, 0.10] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Amer 2013.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation tables generated by statistician |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement for primary study endpoint (hyperparathyroidism) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13/100 participants were not included in full follow‐up. Although the proportion were similar in each arm, the overall proportion indicated high risk of bias |
| Selective reporting (reporting bias) | Low risk | The study reported patient‐level outcomes including death, graft function, and adverse events |
| Other bias | Low risk | Study appears free of other biases |
Arnol 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐level outcomes including adverse events were not systematically reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Cejka 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were assigned randomisation numbers immediately prior to kidney transplantation by the physician who drew numbers from an envelope for this purpose." Unclear if the envelopes were opaque |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Medication was blinded at a different institution not affiliated with our department" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two patients decided that the daily subcutaneous injections were too laborious and withdrew their consent"; one from each group |
| Selective reporting (reporting bias) | High risk | Patient‐level outcomes including adverse events were not systematically reported |
| Other bias | High risk | Imbalance between groups in the proportion of patients with previous rejection at baseline (and therefore possible steroid exposure) |
Chalopin 1987.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Coco 2003.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number system |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | IV versus oral therapy. Unlikely to be blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13 out of 72 patients did not complete the study and their data were excluded from analysis |
| Selective reporting (reporting bias) | High risk | Did not report patient‐level outcomes including graft function or fracture. No protocol published before published trial was completed |
| Other bias | High risk | Imbalance in gender and time on dialysis between treatment groups |
Coco 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Unclear risk | Randomisation was done by pharmacist using computer‐generated randomisation. Reported in insufficient detail to perform adjudication |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical placebo achieved by over encapsulation of the risedronate capsules to appear similar to the placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13/42 participants were not included in entire follow up for reasons that may have been related to outcome |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes were not systematically evaluated or reported |
| Other bias | Low risk | Study appears free of other biases |
Cruzado 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study between medical and surgical treatments |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Low risk | Reporting of all anticipated patient‐level outcomes including adverse events |
| Other bias | Low risk | Study appears free of other biases |
Cueto‐Manzano 2000.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 15/45 patients were not included in full study follow up |
| Selective reporting (reporting bias) | High risk | Patient‐level outcomes were not systematically captured |
| Other bias | Low risk | Study appears free of other biases |
De Sevaux 2002.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Active treatment compared with no treatment; not possible to administer in blinded fashion |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Patient‐level outcomes reported for all participants during follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected patient level outcomes reported |
| Other bias | High risk | Imbalanced gender and comorbidity between groups at baseline |
Dovas 2009.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Treatment interventions sufficiently different that blinding was unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not captured or reported systematically |
| Other bias | Unclear risk | Insufficient data to perform adjudication |
Eid 1996.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Treatments were sufficiently different that blinding was unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 21/58 participants did not complete follow‐up |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not captured or reported systematically |
| Other bias | Unclear risk | Insufficient data to perform adjudication |
El‐Agroudy 2003a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated sequence |
| Allocation concealment (selection bias) | Low risk | Randomised treatment allocation was concealed in sequentially numbered and sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Single‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed 1 year of the study |
| Selective reporting (reporting bias) | Low risk | Patient‐centred outcomes captured and reported systematically |
| Other bias | Unclear risk | No additional threats to validity identified |
El‐Husseini 2004.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Treatment group 3
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded. Different interventions indicate that blinding was unlikely. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Not all patient‐centred outcomes reported systematically |
| Other bias | High risk | Imbalanced duration of renal replacement therapy among treatment groups at baseline |
El‐Husseini 2005a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Evenepoel 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded placebo‐controlled trial |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10/114 discontinued study with equal attrition in both groups |
| Selective reporting (reporting bias) | Low risk | Patient‐level outcomes reported as expected |
| Other bias | High risk | Funded by Amgen; 3 authors are employees of Amgen |
Fan 2000.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | High risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported in sufficient detail. Intervention and comparison were different and not described as identical. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 patient in the treatment group did not complete study (3rd transplant) |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes including adverse events were not reported systematically |
| Other bias | Low risk | No additional threats to validity identified. |
Fujii 2006.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Giannini 2001.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2/20 patients in control group did not complete study follow up and were not included in analyses |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not captured or reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Grotz 1998.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Allocation using sealed envelopes. Not described as sequentially numbered. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1/46 patients did not complete the study |
| Selective reporting (reporting bias) | High risk | Kidney transplant outcomes not reported systematically |
| Other bias | High risk | Imbalanced gender and menopausal status between groups at baseline |
Grotz 2001.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All X‐rays were evaluated by a radiologist who was blinded to the randomisation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8/80 patients did not complete the study with equal numbers in each group |
| Selective reporting (reporting bias) | Low risk | Patient‐centred outcomes including graft function were reported |
| Other bias | Low risk | No additional threats to validity identified |
Haas 2003.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Patients treated with intervention or placebo, but nature of placebo not fully described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Bone biopsy histological analysis conducted by pathologist who was unaware of treatment allocation. Assessment of fracture not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data reported for 13/28 participants |
| Selective reporting (reporting bias) | Low risk | Patient‐centred outcomes reported |
| Other bias | High risk | Funded by Novartis |
Jeffery 2003.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 20/117 participants did not complete study |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported systematically |
| Other bias | High risk | Imbalanced time since transplantation between groups at baseline |
Kharlamov 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Treatment group 3
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐important outcomes not reported |
| Other bias | Low risk | No additional threats to validity identified |
Koc 2002.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 11/24 participants were not included in final analysis |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported systematically |
| Other bias | Low risk | No additional threats to validity identified |
Lan 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported. Unlikely to be blinded due to differences in medication regimens |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not reported systematically |
| Other bias | Low risk | No additional threats to validity identified |
Lord 2001a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Marcen 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Messa 1999.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported ‐ unlikely to be blinded as different interventions |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Montilla 2001.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Nakamura 2009a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Nam 2000.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported ‐ unlikely to be blinded as different routes of interventions |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Narasimhamurthy 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Nayak 2007.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not described. Unlikely to be blinded due to differences between intervention and control (no therapy) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported in sufficient detail to per from adjudication |
| Selective reporting (reporting bias) | High risk | Patient important outcomes such as death and graft survival not captured and reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Neubauer 1984.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10/38 participants did not complete study |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported in sufficient detail to include in meta‐analysis |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Nordal 1995.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and investigators not blinded as treatment was intranasal and control treatment not used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Death, fracture, and graft outcomes not reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Okamoto 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely to be blinded due to differences in treatments (oral treatment versus no treatment) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not captured or reported systematically |
| Other bias | Unclear risk | Partially funded by Merck Sharpe Dohme K.K. |
Oliden 2012.
| Methods | judgementCountry: Study design: Prospective randomised uncontrolled parallel‐group randomised trial Duration of study: not reported Duration of follow‐up: 24 weeks |
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients included in outcome assessment at 24 weeks |
| Selective reporting (reporting bias) | High risk | Patient important outcomes were not all reported in systematic way |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Omidvar 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comparing intravenous with oral medication. Although stated that investigators were blinded to treatment allocation, patients were unblinded and nature of interventions meant that blinding was unlikely. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 40 patients completed study |
| Selective reporting (reporting bias) | High risk | Patient important outcomes were not all reported in systematic way |
| Other bias | Low risk | No additional threats to validity identified |
Pasquali 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported. Differences in treatments indicate blinding did not occur |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3/19 patients did not complete study and were not included in analyses |
| Selective reporting (reporting bias) | High risk | Key clinical and adverse outcomes were not reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Peeters 2001.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Perez 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded. Patients allocated to oral treatment or no treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not captured or reported systematically |
| Other bias | Low risk | No additional threats to validity identified |
Pihlstrom 2017.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated by independent statistician using computer‐generated block‐randomisation with non‐fixed block size |
| Allocation concealment (selection bias) | Unclear risk | Principal investigator performed opening of sealed envelopes. Not reported whether envelopes were opaque or sequentially numbered |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant was lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Patient‐level outcomes including adverse events were not systematically reported |
| Other bias | Unclear risk | No additional threats to validity identified |
POSTOP 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated by hospital pharmacist with computer algorithm |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was ensured by the use of sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study physicians and nurses and participants were aware of the treatment allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The persons who performed DEXA and CT scanning and biomarker measurements were masked to allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All randomised patients were included in analysis. Loss to follow up was uneven between groups (7 lost from denosumab group and 1 lost from control group) |
| Selective reporting (reporting bias) | Low risk | All patient important outcomes were reported systematically |
| Other bias | High risk | Imbalanced gender at baseline |
Praditpornsilpa 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Psimenou 2002.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Treatment group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study. Interventions given by different routes |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred fracture, death and graft outcomes not systematically captured or reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Sanchez‐Escuredo 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 8/69 patients did not complete the study due to treatment‐related side effects |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not captured or reported systematically |
| Other bias | Low risk | Study appears free of other biases |
Shahidi 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded comparing different drug regimens without control |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 11/48 participants did not complete study |
| Selective reporting (reporting bias) | High risk | Patient reported outcomes not captured or reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Shahidi 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study comparing intravenous therapy with no treatment control |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reported as all patients included in follow up |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not captured or reported systematically |
| Other bias | Low risk | No additional threats to validity identified |
Sharma 2002a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Sirsat 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data cannot be meta‐analysed, numbers per group not reported, no SD |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Smerud 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated list of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Sequentially allocated a randomisation number. Not sufficient information to perform adjudication |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Comparing treatment with matching placebo. All study personnel were blinded to allocation for the duration of the study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16 patients did not receive all infusions, 10 stopped medication early but were included in analysis. 2 patients were lost to follow‐up and single patient withdrew due to early fractures |
| Selective reporting (reporting bias) | Low risk | Patient‐relevant outcomes captured and reported systematically |
| Other bias | Low risk | No additional threats to validity identified |
Starke 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not captured or reported systematically |
| Other bias | High risk | Imbalances in gender and duration of transplantation between treatment groups at baseline |
Tałałaj 1996.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Adverse events not systematically captured |
| Other bias | Low risk | No additional threats to validity identified |
Thervet 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data unable to be meta‐analysed |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Tiryaki 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Adverse events not systematically captured |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Torregrosa 2003.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Torregrosa 2007.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Adverse events not reported systematically |
| Other bias | Low risk | No additional threats to validity identified |
Torregrosa 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Done using sealed envelopes. Unclear whether the envelopes were sequentially numbered and opaque |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessment of radiographs Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 15/101 patients did not complete study |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not fully reported |
| Other bias | High risk | Funded by Astellas Pharma |
Torregrosa 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Stated as double‐blind but unclear whether placebo actually used and whether patients and/or investigators unaware of treatment allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10/39 patients discontinued study |
| Selective reporting (reporting bias) | High risk | Patient important outcomes not captured or reported systematically |
| Other bias | High risk | Imbalances in previous treatments between groups at baseline; funded by Novartis |
Torres 2004.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Randomisation was performed by open a sealed envelope with the lowest available study number. Not clear whether sequentially number and whether envelopes were opaque. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded. Placebo pills were undistinguishable from calcitriol |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4/90 patients (all in placebo group) were excluded from analysis initially and 19 patients excluded at one year |
| Selective reporting (reporting bias) | High risk | Not reporting all patient‐centred outcomes |
| Other bias | Low risk | No other threats to validity identified |
Trabulus 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Treatment group 3
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | High risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded allocation to different medication strategies |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 14/64 patients did not complete treatment for reasons that related to medication adverse effects |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not captured or reported systematically |
| Other bias | High risk | Imbalanced duration of kidney disease among treatment groups at baseline |
Trillini 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | Randomised to two treatments by an independent investigator at the coordinating centre. Not sufficient detail to perform adjudication |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Allocated to two different treatments (oral drug versus no treatment) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2/43 patients did not complete study (intervention group) |
| Selective reporting (reporting bias) | Low risk | Patient‐centred outcomes systematically captured and reported |
| Other bias | Low risk | No additional threats to validity identified |
Ugur 2000.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Treatment group 3
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported systematically |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Walsh 2009.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Statistical Analysis System (SAS Institute, Cary, NC)–based randomization macro; randomization was stratified for sex and baseline PTH level" |
| Allocation concealment (selection bias) | Low risk | Quote: "Four‐digit randomization numbers were allocated to patients through a telephone randomization process" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded comparing intravenous therapy with no treatment control |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Observers blinded to treatment allocation assessed radiographs individually then conferred with 2nd observed |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 125 randomly assigned to treatment; 32 randomised participants were excluded (19 in treatment group and 13 in control group) |
| Selective reporting (reporting bias) | Low risk | Patient‐centred outcomes captured and reported |
| Other bias | High risk | Funded by Novartis; one author employee of Novartis |
Wissing 2005.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Co‐interventions
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate allocation |
| Allocation concealment (selection bias) | High risk | Alternate allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 11/90 participants lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Patient‐centred outcomes not reported systematically |
| Other bias | Unclear risk | No additional threats to validity identified |
ACR ‐ albumin‐creatinine ratio; BMD ‐ bone mineral density; CNI ‐ calcineurin inhibitor/s; CrCl ‐ creatinine clearance; DEXA ‐ dual energy X‐ray absorptiometry; DGF ‐ delayed graft function; DM ‐ diabetes mellitus; (e)GFR ‐ (estimated) glomerular filtration rate; GI ‐ gastrointestinal; HD ‐ haemodialysis; HIV ‐ human immunodeficiency virus; M/F ‐ male/female; MMF ‐ mycophenolate mofetil; PRA ‐ panel reactive antibody; (i)PTH ‐ (intact) parathyroid hormone; RAAS ‐ renin‐angiotensin‐aldosterone system; RAS ‐ renin‐angiotensin system; RCT ‐ randomised controlled trial; SC ‐ subcutaneous; SCr ‐ SCr; SD ‐ standard deviation; UACR ‐ urinary albumin:creatinine ratio; UPCR ‐ urinary protein:creatinine ratio
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ambuhl 1999 | Outcomes of interest not investigated: effect of phosphate replacement on calcium, phosphate and acid/base balance in kidney transplant recipients |
| Ardalan 2007 | Outcomes of interest not investigated: effect of vitamin D on T‐cell populations in kidney transplant recipients |
| Campistol 1999 | Wrong intervention: a study on the influence of immunosuppressive treatment on markers of bone remodelling in kidney transplantation (comparison between cyclosporine and sirolimus). The effect of immunosuppression regimens on bone disease is beyond the scope of this systematic review |
| Campistol 2000 | Wrong intervention: a study of the effect of sirolimus on bone disease in kidney transplant patients. Beyond the scope of this systematic review |
| El‐Haggan 2002 | Wrong intervention: study evaluating one‐year evolution of BMD in kidney transplantation comparing tacrolimus with cyclosporin. Interventions are not eligible for inclusion in this review |
| James 2003 | Wrong population: 2‐year follow‐up report of RCT in non‐kidney transplant patients |
| Josephson 2004 | Wrong population: included kidney‐pancreas transplant recipients |
| Labib 1999 | Wrong intervention: calculation therapy |
| Lebranchu 1999 | Wrong intervention: effect of steroid withdrawal on bone disease in kidney transplant recipients |
| Lippuner 1996 | Wrong population: effect of disodium monofluorophosphate, calcium and vitamin D supplementation on BMD in patients with chronic steroid treatment (not related to kidney transplantation) |
| Lippuner 1998 | Wrong intervention: effect of deflazacort versus prednisone on bone disease early after kidney transplantation |
| Masse 2001 | Wrong intervention: non‐bone modulating treatment |
| NCT00646282 | Study terminated: doxercalciferol versus no treatment in adult kidney transplant recipients. Only information about trial is available on ClinicalTrials.gov; no results posted in registry |
| Ponticelli 1997 | Wrong intervention: effect of 3 different immunosuppressive regimens on BMD in kidney transplant recipients |
| Reed 2004 | Wrong population: cinacalcet in dialysis patients |
| Rigotti 2003 | Wrong intervention: effect of steroid‐free regimen on change in BMD after kidney transplantation |
| ter Meulen 2003 | Wrong intervention: effect of steroid‐free regimen with a regimen with limited steroid exposure on changes in bone mass after kidney transplantation |
| THOMAS 2002 | Wrong intervention: effects of different steroid doses on BMD in kidney transplant recipients |
| Vasquez 2004 | Wrong intervention: effect of simvastatin on bone disease following kidney transplantation |
| Zaoui 2003 | Wrong intervention: effect of steroid‐free immunosuppressive regimen |
BMD ‐ bone mineral density; RCT ‐ randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Jorge 2016.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Notes |
|
Marques 2019.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Notes |
|
NCT01675089.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Notes |
|
Oblak 2017.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Notes |
|
Tiryaki 2018.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Notes |
|
ABD ‐ adynamic bone disease; ALP ‐ alkaline phosphatase; BMD ‐ bone mineral density; CRP ‐ C‐reactive protein; (e)GFR ‐ (estimated) glomerular filtration rate; (i)PTH ‐ (intact) parathyroid hormone; MI ‐ myocardial infarction; RAS ‐ renin‐angiotensin system; SCr ‐ serum creatinine; UACR ‐ urinary albumin‐creatinine ratio; UPCR ‐ urinary protein‐creatinine ratio
Characteristics of ongoing studies [ordered by study ID]
NCT00748618.
| Trial name or title | Vitamin D replacement after kidney transplant |
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Starting date | September 2008 |
| Contact information | Jillian M Witte: jmwitte@unmc.edu Terica L Hudson: thudson@unmc.edu |
| Notes | Recruitment status of the study is unknown because the information has not been verified recently. The Principal investigator, Professor Larsen (jlarsen@unmc.edu) has been contacted to request an update on the status of this study. No reply has been received. The contact information for other investigators described on the clinicaltrials.gov registry are no longer valid |
NCT00889629.
| Trial name or title | Pilot study evaluating doxercalciferol replacement therapy in kidney transplant recipients |
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Starting date | November 2008 |
| Contact information | Mariana Markell ‐ State University of New York ‐ Downstate Medical Center |
| Notes | Recruitment status of the study is unknown because the information has not been verified recently. We could not find any contact details for the contact person on the clinicaltrials.gov website |
NCT02224144.
| Trial name or title | Bone mass and strength after kidney transplantation |
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Starting date | August 2014 |
| Contact information | Thomas Nickolas: tln2001@cumc.columbia.edu Daniel Velez: dav2125@cumc.columbia.edu |
| Notes | Study currently recruiting patients |
VITA‐D 2009.
| Trial name or title | Vitamin D for improving the outcome after kidney transplantation: Rationale, design, and baseline characteristics of the participants of the vita‐D randomised controlled trial |
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Starting date | January 2009 |
| Contact information | Georg Heinze: georg.heinze@meduniwien.ac.at |
| Notes | Data analysis is ongoing. We have contacted Professor Borchhardt to request an update on the status of this trial as the status could not be verified in the clinicaltrials.gov registry (kyra.borchhardt@gmail.com). We have not received any reply. |
VITALE 2014.
| Trial name or title | VITamin D supplementation in renAL transplant recipients (VITALE): a prospective, multicentre, double‐blind, randomised trial of vitamin D estimating the benefit and safety of vitamin D3 treatment at a dose of 100,000 UI compared with a dose of 12,000 UI in renal transplant recipients: study protocol for a double‐blind, randomised, controlled trial |
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
Co‐interventions
|
| Outcomes |
|
| Starting date | Not reported |
| Contact information | Marie Courbebaisse: marie.courbebaisse@egp.aphp.fr |
| Notes | No published data available and no response from authors upon correspondence |
ACEi ‐ angiotensin‐converting enzyme inhibitor; ARB ‐ angiotensin receptor blocker; BMD ‐ bone mineral density; BSL ‐ blood sugar level; DM ‐ diabetes mellitus; FGF‐23 ‐ fibroblast growth factor 23; (e)GFR ‐ (estimated) glomerular filtration rate; GI ‐ gastrointestinal; HRpQCT‐ high resolution peripheral quantitative computed tomography; MDRD ‐ modified diet in renal disease; (i)PTH ‐ (intact) parathyroid hormone; RCT ‐ randomised controlled trial; SCr ‐ serum creatinine
Differences between protocol and review
2019: for this update we have included the outcomes myocardial infarction, stroke and parathyroidectomy; GRADE has been used to assess the quality/certainty of the evidence
Contributions of authors
EC: developed the search strategy with the help of the Cochrane Kidney and Transplant Information Specialist, identified studies for inclusion and exclusion, assessed quality, data extraction, data analysis, writing of review
SP: conceived of and designed the review, developed the search strategy with the help of the Cochrane Kidney and Transplant Information Specialist, identified studies for inclusion and exclusion, assessed quality, data extraction, data analysis, writing of review
FB: interpretation of data analysis, writing of review
DM: identified studies for inclusion and exclusion, assessed quality, data extraction, data analysis, writing of review
GS: data extraction, data entry, data analysis, writing of review
Declarations of interest
Suetonia C Palmer: none known
Edmund YM Chung: none known
David O McGregor: none known
Friederike Bachmann: none known
Giovanni FM Strippoli: none known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Amer 2013 {published data only}
- Amer H, Griffin M, Cosio F, Park W, Kremers W, Mazur M, et al. Oral paricalcitol in kidney transplant recipients receiving a corticosteroid‐free immunosuppressive regimen: an open label randomized trial [abstract no: LB33]. American Journal of Transplantation 2012;12(Suppl S3):452. [EMBASE: 70747416] [Google Scholar]
- Amer H, Griffin M, Park W, Kremers W, Stegall M, Cosio F, et al. Effects of paricalcitol on bone turnover in kidney transplant recipients [abstract no: A39]. Transplantation 2014;98(Suppl 1):882. [EMBASE: 71546547] [Google Scholar]
- Amer H, Griffin MD, Stegall MD, Cosio FG, Park WD, Kremers WK, et al. Oral paricalcitol reduces the prevalence of posttransplant hyperparathyroidism: results of an open label randomized trial. American Journal of Transplantation 2013;13(6):1576‐85. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Arnol 2011 {published data only}
- Arnol M, Oblak M, Mlinsek G, Bren AF, Buturovic‐Ponikvar J, Kandus A. Proteinuria in kidney transplant recipients: prevalence in a national cohort and study design of the effect of paricalcitol for reduction of proteinuria [abstract no: RO‐204]. Transplant International 2011;24(Suppl 2):185. [EMBASE: 70527733] [Google Scholar]
- Arnol M, Oblak M, Mlinsek G, Buturovic‐Ponikvar J, Kandus A. Paricalcitol versus placebo for reduction of proteinuria in kidney transplant recipients: a double‐blind, randomized controlled trial [abstract no: 426.4]. Transplantation 2016;100(7 Suppl 1):S214‐5. [EMBASE: 613005120] [DOI] [PubMed] [Google Scholar]
Cejka 2008 {published data only}
- Cejka D, Benesch T, Krestan C, Roschger P, Klaushofer K, Pietschmann P, et al. Effect of teriparatide on early bone loss after kidney transplantation. American Journal of Transplantation 2008;8(9):1864‐70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chalopin 1987 {published data only}
- Chalopin JM, Garnier PC, D'Athis P, Cabanne JF, Perceau C, Tanter Y, et al. Vitamin D3 metabolites and mineral metabolism parameters after renal transplantation: prospective randomized study with 250H vitamin D3 therapy [abstract]. 10th International Congress of Nephrology; 1987 Jul 26‐31; London, UK. 1987:418. [CENTRAL: CN‐00784682]
Coco 2003 {published data only}
- Coco M, Glicklich D, Bognar I, Burris L, Durkin P, Tellis V, et al. Randomized trial of IV pamidronate to ameliorate bone loss in renal transplant (RT) recipients [abstract]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):927A. [CENTRAL: CN‐00550697] [DOI] [PubMed] [Google Scholar]
- Coco M, Glicklich D, Burris L, Bognar I, Tellis V, Greenstein S, et al. Prospective randomised trial of IV pamidronate in renal transplant recipients: 6 and 12 month follow‐up [abstract no: F‐FC044]. Journal of the American Society of Nephrology 2002;13(Program & Abstracts):10A. [CENTRAL: CN‐00444866] [DOI] [PubMed] [Google Scholar]
- Coco M, Glicklich D, Burris L, Durkin P, Tellis V, Greenstein S, et al. Effect of IV pamidronate on bone biochemical parameters in renal transplant recipients [abstract]. Journal of the American Society of Nephrology 2000;11(Sept):561A. [CENTRAL: CN‐00550699] [Google Scholar]
- Coco M, Glicklich D, Faugere MC, Burris L, Bognar I, Durkin P, et al. Prevention of bone loss in renal transplant recipients: a prospective, randomized trial of intravenous pamidronate. Journal of the American Society of Nephrology 2003;14(10):2669‐76. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lee S, Glicklich D, Coco M. Pamidronate used to ameliorate post renal transplant bone loss is not associated with increased renal dysfunction [abstract no: SU‐PO729]. Journal of the American Society of Nephrology 2003;14(Nov):695A. [CENTRAL: CN‐00615885] [Google Scholar]
- Lee S, Glicklich D, Coco M. Pamidronate used to attenuate post‐renal transplant bone loss is not associated with renal dysfunction. Nephrology Dialysis Transplantation 2004;19(11):2870‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Coco 2012 {published data only}
- Coco M, Glicklich D, Pullman J. Prophylactic risedronate in new renal transplant recipients: effects on serial bone mineral density and bone histology [abstract no: F‐PO909]. Journal of the American Society of Nephrology 2007;18(Abstracts):302A. [CENTRAL: CN‐00783952] [Google Scholar]
- Coco M, Glicklich D, Pullman J. Randomized controlled trial of risedronate in renal transplant recipients: histomorphometry shows lowered bone turnover but not adynamic bone [Abstract no: SA‐PO2830]. Journal of the American Society of Nephrology 2009;20(Abstract Suppl):759A. [Google Scholar]
- Coco M, Pullman J, Cohen HW, Lee S, Shapiro C, Solorzano C, et al. Effect of risedronate on bone in renal transplant recipients. Journal of the American Society of Nephrology 2012;23(8):1426‐37. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cruzado 2015 {published data only}
- Cruzado J, Torregrosa V, Mast R, Garcia‐Barrasa A, Bestard O, Melilli E, et al. A randomized study comparing parathyroidectomy versus cinacalcet to treat hypercalcemia in kidney allograft recipients with persistent hyperparathyroidism [abstract no: 756]. American Journal of Transplantation 2015;15(Suppl 3). [EMBASE: 71952932] [Google Scholar]
- Cruzado JM, Moreno P, Torregrosa JV, Taco O, Mast R, Gomez‐Vaquero C, et al. A randomized study comparing parathyroidectomy with cinacalcet for treating hypercalcemia in kidney allograft recipients with hyperparathyroidism. Journal of the American Society of Nephrology 2015;27(8):2487‐94. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruzado JM, Taco O, Vicens T, Mast R, Polo C, Bestard O, et al. A randomized study comparing parathyroidectomy versus cinacalcet to treat hypercalcemia in kidney allograft recipients with persistent hyperparathyroidism [abstract]. Nephrology Dialysis Transplantation 2015;30(Suppl 3):iii36. [EMBASE: 72206357] [Google Scholar]
Cueto‐Manzano 2000 {published data only}
- Cueto‐Manzano AM, Konel S, Freemont AJ, Adams JE, Mawer B, Gokal R, et al. Effect of 1,25‐dihydroxyvitamin D3 and calcium carbonate on bone loss associated with long‐term renal transplantation. American Journal of Kidney Diseases 2000;35(2):227‐36. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
De Sevaux 2002 {published data only}
- Sevaux R, Hoitsma A, Corstens F, Wetzels J. Prophylaxis of bone loss after renal transplantation with calcium and vitamin D [abstract no: A4855]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):929A. [CENTRAL: CN‐00550384] [Google Scholar]
- Sevaux RG, Hoitsma AJ, Corstens FHM, Wetzels JF. Treatment with vitamin D and calcium reduces bone loss after renal transplantation: a randomized study. Journal of the American Society of Nephrology 2002;13(6):1608‐14. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dovas 2009 {published data only}
- Dovas S, Economidou D, Papagianni A, Kazantzidou E, Pateinakis P, Efstratiadis G, et al. A prospective study for prevention of post transplantation bone loss in renal transplant recipients [abstract no: P‐662]. Transplant International 2009;22(Suppl 2):259. [Google Scholar]
Eid 1996 {published data only}
- Eid P, Scuderi G, Aroldi A, Ciammella M, Nencioni T. Bone loss after renal transplantation: HRT versus calcitriol in postmenopausal recipients [abstract no: PTu844]. Osteoporosis International 1996;6(Suppl 1):294. [CENTRAL: CN‐00260191] [Google Scholar]
El‐Agroudy 2003a {published data only}
- El‐Agroudy A, El‐Husseini A, El‐Sayed M, Ghoneim MA. Prevention of osteoporosis after kidney transplantation: a prospective randomized study [abstract no: M777]. Nephrology Dialysis Transplantation 2003;18(Suppl 4):249. [Google Scholar]
- El‐Agroudy AE, El‐Husseini AA, El‐Sayed M, Ghoneim MA. Preventing bone loss in renal transplant recipients with vitamin D. Journal of the American Society of Nephrology 2003;14(11):2975‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- El‐Agroudy AE, El‐Husseini AA, El‐Sayed M, Mohsen T, Ghoneim MA. A prospective randomized study for prevention of postrenal transplantation bone loss. Kidney International 2005;67(5):2039‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
El‐Husseini 2004 {published data only}
- Husseini A, Elagroudy A, Elsayed M, Sobh M, Ghoneim M. Treatment of bone loss with vitamin D in live related kidney transplant children and adolescents: a prospective randomized study [abstract no: SP231]. 41st Congress European Renal Association European Dialysis and Transplantation Association; 2004 May 15‐18; Lisbon, Portugal. 2004:93. [CENTRAL: CN‐00509176]
- El‐Husseini A, El‐Agroudy A, El‐Sayed M, Sobh M, Ghoneim M. Treatment of bone loss in renal transplant children and adolescents [abstract no: T818]. Nephrology Dialysis Transplantation 2003;18(Suppl 4):544. [CENTRAL: CN‐00445216] [Google Scholar]
- El‐Husseini AA, El‐Agroudy AE, El‐Sayed M, Sobh MA, Ghoneim MA. A prospective randomized study for the treatment of bone loss with vitamin D during kidney transplantation in children and adolescents. American Journal of Transplantation 2004;4(12):2052‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- El‐Husseini AA, El‐Agroudy AE, El‐Sayed MF, Sobh MA, Ghoneim MA. A prospective randomized study for the treatment of bone loss with alendronate in kidney transplant children and adolescents [abstract no: SP181]. Nephrology Dialysis Transplantation 2005;20(Suppl 5):v80. [CENTRAL: CN‐00782294] [Google Scholar]
- El‐Husseini AA, El‐Agroudy AE, El‐Sayed MF, Sobh MA, Ghoneim MA. Treatment of osteopenia and osteoporosis in renal transplant children and adolescents. Pediatric Transplantation 2004;8(4):357‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
El‐Husseini 2005a {published data only}
- El‐Husseini AA, El‐Agroudy A, El‐Sayed MF, Sobh MA, Ghoneim MA. Alfacalcidol versus calcitonin for the treatment of bone loss after renal transplantation in children and adolescents [abstract no: MP482]. Nephrology Dialysis Transplantation 2005;20(Suppl 5):v361. [CENTRAL: CN‐00782136] [Google Scholar]
Evenepoel 2014 {published data only}
- Evenepoel P, Cooper K, Holdaas H, Messa P, Mourad G, Olgaard K, et al. A randomized study evaluating cinacalcet to treat hypercalcemia in renal transplant recipients with persistent hyperparathyroidism. American Journal of Transplantation 2014;14(11):2545‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fan 2000 {published data only}
- Fan S, Almond MK, Ball E, Evans K, Cunningham J. Randomized prospective study demonstrating prevention of bone loss by pamidronate during the first year after renal transplantation [abstract no: A2714]. Journal of the American Society of Nephrology 1996;7(Program & Abstracts):1789. [CENTRAL: CN‐00445275] [Google Scholar]
- Fan SL, Almond MK, Ball E, Evans K, Cunningham J. Pamidronate therapy as prevention of bone loss following renal transplantation. Kidney International 2000;57(2):684‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Fan SL, Kumar S, Cunningham J. Long‐term effects on bone mineral density of pamidronate given at the time of renal transplantation. Kidney International 2003;63(6):2275‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fujii 2006 {published data only}
- Fujii N, Hamano T, Mikami S, Ito T, Kokado Y, Kojima Y, et al. Oral risedronate is a successful treatment for bone loss in the long‐term kidney transplant patients [abstract no: TH‐PO123]. Journal of the American Society of Nephrology 2006;17(Abstracts):132A. [CENTRAL: CN‐00783786] [Google Scholar]
Giannini 2001 {published data only}
- Carraro G, Perin N, Giannini S, Naso A, Legnaro A, D'Angelo A, et al. Alendronate prevents further bone loss in renal transplant recipients [abstract no: 448]. 10th ESOT & 12th ETCO Congress. Bridging the Future; 2001 Oct 6‐11; Lisbon, Portugal. 2001.
- Giannini S, D'Angelo A, Carraro G, Nobile M, Rigotti P, Bonfante L, et al. Alendronate prevents further bone loss in renal transplant recipients. Journal of Bone & Mineral Research 2001;16(11):2111‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Grotz 1998 {published data only}
- Grotz WH, Rump LC, Niessen A, Schmidt‐Gayk H, Reichelt A, Gunter K, et al. Treatment of osteopenia and osteoporosis after kidney transplantation. Transplantation 1998;66(8):1004‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Grotz 2001 {published data only}
- Gerke P, Olschewski M, Grotz W. Early ibandronate administration improves long‐term renal allograft function [abstract no: SA‐PO2533]. Journal of the American Society of Nephrology 2008;19(Abstracts Issue):679A. [CENTRAL: CN‐00782904] [Google Scholar]
- Grotz W, Nagel C, Poeschel D, Cybulla M, Petersen KG, Uhl M, et al. Effect of ibandronate on bone loss and renal function after kidney transplantation. Journal of the American Society of Nephrology 2001;12(7):1530‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Haas 2003 {published data only}
- Haas M, Leko‐Mohr Z, Roschger P, Kletzmayr J, Schwarz C, Mitterbauer C, et al. Zoledronic acid to prevent bone loss in the first 6 months after renal transplantation. Kidney International 2003;63(3):1130‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Schwarz C, Mitterbauer C, Heinze G, Woloszczuk W, Haas M, Oberbauer R. Nonsustained effect of short‐term bisphosphonate therapy on bone turnover three years after renal transplantation. Kidney International 2004;65(1):304‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Schwarz C, Mitterbauer C, Heinze G, Wolusczcuk W, Haas M, Oberbauer R. Non‐sustained effect of short term bisphsophonate therapy on bone turnover three years after renal transplantation [abstract no: SU‐PO736]. Journal of the American Society of Nephrology 2003;14(Nov):697A. [CENTRAL: CN‐00783721] [Google Scholar]
Jeffery 2003 {published data only}
- Jeffery JR, Leslie WD, Karpinski ME, Nickerson PW, Rush DN. A randomized prospective trial of calcitriol versus alendronate for the treatment of osteopenia in renal transplant recipients [abstract]. American Journal of Transplantation 2003;3(Suppl 5):353. [CENTRAL: CN‐00445907] [DOI] [PubMed] [Google Scholar]
- Jeffery JR, Leslie WD, Karpinski ME, Nickerson PW, Rush DN. Prevalence and treatment of decreased bone density in renal transplant recipients: a randomized prospective trial of calcitriol versus alendronate. Transplantation 2003;76(10):1498‐502. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kharlamov 2012 {published data only}
- Kharlamov AN, Parrish AN, Ivanova EJ, Gabinsky JL, Veselova VS, Novoselova OS. Cholecalciferol for prevention of chronic allograft nephropathy, kidney repair, and management of cardiorenal syndrome in vitamin D insufficient kidney transplant recipients [abstract]. European Journal of Medical Research 2010;15(Suppl 1):124. [EMBASE: 71295070] [Google Scholar]
- Kharlamov AN, Perrish AN, Gabiskii I, Ronne K, Ivanova EI. Vitamin D in the treatment of cardiorenal syndrome in patients with chronic nephropathy. Kardiologiia 2012;52(3):33‐44. [MEDLINE: ] [PubMed] [Google Scholar]
Koc 2002 {published data only}
- Koc M, Tuglular H, Arikan H, Ozener C, Akoglu E. Alendronate increases bone mineral density in long‐term renal transplant recipients. Transplantation Proceedings 2002;34(6):2111‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Koc M, Tuglular S, Arikan H, Ozener C, Akoglu E. Alendronate increases bone mineral density in renal transplant recipients [abstract]. Nephrology Dialysis Transplantation 2001;16(6):A227. [CENTRAL: CN‐00446130] [DOI] [PubMed] [Google Scholar]
Lan 2008 {published data only}
- Lan G, Peng L, Xie X, Peng F, Wang Y, Yu S. Alendronate is effective to treat bone loss in renal transplantation recipients. Transplantation Proceedings 2008;40(10):3496‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lord 2001a {published data only}
- Lord H, Cailhier J, Leblanc M, Boucher A, Dandavino R, Ouimet D, et al. Prevention of bone loss following kidney transplantation with alendronate: a randomized controlled study [abstract no: A4897]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):937‐8A. [CENTRAL: CN‐00783925] [Google Scholar]
Marcen 2010 {published data only}
- Marcén R, Fernández‐Rodriguez A, Galeano C, Villacorta FJ, Villafruela JJ, Teruel JL, et al. Cholecalciferol supplements in renal transplant recipients with vitamin D deficiency [abstract no: 1688]. American Journal of Transplantation 2010;10(Suppl 4):518. [EMBASE: 70465063] [DOI] [PubMed] [Google Scholar]
Messa 1999 {published data only}
- Messa P, Sindici C, Miotti V, Gropuzzo M, Cattaruzzi E, Englaro E, et al. Calcitriol and VDR genotype influences on bone mineral density after renal transplantation [abstract no: A3149]. Journal of the American Society of Nephrology 1999;10(Program & Abstracts):622A. [CENTRAL: CN‐00782465] [Google Scholar]
Montilla 2001 {published data only}
- Montilla C, Carlini RG, Martinis R, Hernandez E, Arminio A, Clesca P, et al. One year controlled trial of pamidronate in the treatment of severe osteopenia after long term renal transplantation (TX) [abstract no: A4914]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):941A. [CENTRAL: CN‐00783760] [Google Scholar]
Nakamura 2009a {published data only}
- Nakamura N, Ogahara S, Mikami H, Matsubara T, Higuchi K, Furuya R, et al. The effects of bisphosphonates to prevent GIOP in kidney transplantation recipients. The tentative report of single‐blind randomized prospective clinical study [abstract no: P‐568]. Transplant International 2009;22(Suppl 2):235‐6. [Google Scholar]
Nam 2000 {published data only}
- Nam JH, Moon JI, Chung SS, Kim SI, Park KI, Song YD, et al. Pamidronate and calcitriol trial for the prevention of early bone loss after renal transplantation. Transplantation Proceedings 2000;32(7):1876. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Narasimhamurthy 2014 {published data only}
- Narasimhamurthy M, Kamal F, Igari M, Natraj S, Gohh R. Reduction of proteinuria with selective vitamin D receptor activation using paricalcitol in renal transplant patients [abstract no: 2244]. Transplantation 2014;98(Suppl 1):127. [EMBASE: 71543930] [Google Scholar]
Nayak 2007 {published data only}
- Nayak B, Guleria S, Varma M, Tandon N, Aggarwal S, Bhowmick D, et al. Effect of bisphosphonates on bone mineral density after renal transplantation as assessed by bone mineral densitometry. Transplantation Proceedings 2007;39(3):750‐2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Neubauer 1984 {published data only}
- Neubauer E, Neubauer N, Ritz E, Dreikorn K, Krause KH. Bone mineral content after renal transplantation. Placebo‐controlled prospective study with 1,25‐dihydroxy vitamin D3. Klinische Wochenschrift 1984;62(2):93‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nordal 1995 {published data only}
- Nordal KP, Halse J, Dahl E. The effect of nasal calcitonin on bone mineral density in renal transplant recipients [abstract]. Nephrology Dialysis Transplantation 1996;11(6):1212. [CENTRAL: CN‐00261230] [Google Scholar]
- Nordal KP, Halse J, Kronborg J, Dahl E, Hartmann A. Nasal calcitonin reduces bone loss in renal transplant recipients [abstract]. Journal of the American Society of Nephrology 1995;6(3):1109. [CENTRAL: CN‐00485256] [Google Scholar]
Okamoto 2014 {published data only}
- Okamoto M, Yamanaka S, Yoshimoto W, Shigematsu T. Alendronate as an effective treatment for bone loss and vascular calcification in kidney transplant recipients. Journal of Transplantation 2014:269613. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oliden 2012 {published data only}
- Oliden C, Leon L, Tavera M, Minue E, Anzieta N, Colom P, et al. Oral paricalcitol versus oral calcitriol for the treatment of secondary hyperparathyroidism in renal transplantation [abstract no: 1707]. Transplantation 2012;94(10 Suppl):898. [EMBASE: 71251572] [Google Scholar]
Omidvar 2011 {published data only}
- Omidvar B, Ghorbani A, Shahbazian H, Beladi Mousavi SS, Shariat Nabavi SJ, Alasti M. Comparison of alendronate and pamidronate on bone loss in kidney transplant patients for the first 6 months of transplantation. [Erratum appears in Iran J Kidney Dis. 2012 Jul;6(4):321]. Iranian Journal of Kidney Diseases 2011;5(6):420‐4. [MEDLINE: ] [PubMed] [Google Scholar]
- Omidvar B, Ghorbani A, Shahbazian H, Mousavi SS, Hayati F, Nabavi SJ. Comparison the effect of alendronate and pamidronate on early BMD changes in kidney transplant patients in the first 6 months of transplantation [abstract no: 0740]. International Journal of Rheumatic Diseases 2010;13(Suppl 1):170. [EMBASE: 70198173] [Google Scholar]
Pasquali 2014 {published data only}
- Pasquali M, Tartaglione L, Rotondi S, Luisa MM, Mandanici G, Leonangeli C, et al. Cinacalcet (CM) vs paricalcitol (PC) in renal transplant (TX) patients with hypercalcemic persisting secondary hyperparathyroidism (HPSH) a pilot study (EudraCT 2010‐021041‐42) [abstract no: MP219]. Nephrology Dialysis Transplantation 2014;29(Suppl 3):iii400. [EMBASE: 71492622] [Google Scholar]
Peeters 2001 {published data only}
- Peeters J, Maes B, Vanwalleghem J, Boonen S, Vanrenterghem Y. Alfa‐calcidol protects against spinal bone loss after cadaveric renal transplantation: a randomised placebo‐controlled trial [abstract no: O14]. Nephrology Dialysis Transplantation 2002;17(Suppl 12):6‐7. [CENTRAL: CN‐00782134] [Google Scholar]
- Peeters JC, Maes BD, Herelixka AS, Vanwalleghem JF, Boonen S, Vanrenterghem YF. Alfa‐calcidol protects against spinal bone loss after renal transplantation: a randomised placebo controlled trial [abstract no: A4925]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):943A. [CENTRAL: CN‐00782135] [Google Scholar]
Perez 2010 {published data only}
- Perez V, Sanchez A, Bayes B, Navarro‐Munoz M, Lauzurica R, Pastor MC, et al. Effect of paricalcitol on the urinary peptidome of kidney transplant patients. Transplantation Proceedings 2010;42(8):2924‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Perez V, Sanchez‐Escuredo A, Lauzurica R, Bayes B, Navarro‐Munoz M, Pastor MC, et al. Magnetic bead‐based proteomic technology to study paricalcitol effect in kidney transplant recipients. European Journal of Pharmacology 2013;709(1‐3):72‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pihlstrom 2017 {published data only}
- Pihlstrom HK, Gatti F, Hammarstrom C, Eide IA, Kasprzycka M, Wang J, et al. Early introduction of oral paricalcitol in renal transplant recipients. An open‐label randomized study. Transplant International 2017;30(8):827‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Pihlstrøm H, Eide IA, Midtvedt K, Hartmann A, Bollerslev J, Svensson MHS. Paricalcitol for prevention and reduction of albuminuria in the general renal transplant recipient [abstract no: P767]. Transplant International 2015;28(Suppl 4):815. [EMBASE: 72112694] [Google Scholar]
- Pihlstrøm H, Gatti F, Hammarstrom C, Eide I, Kasprzycka M, Wang J, et al. Early introduction of oral paricalcitol in renal transplant recipients. an open‐label randomized study [abstract no: D149]. American Journal of Transplantation 2017;17(Suppl 3):760. [EMBASE: 615705633] [DOI] [PubMed] [Google Scholar]
POSTOP 2014 {published data only}
- Bonani M, Brockmann J, Cohen CD, Fehr T, Nocito A, Schiesser M, et al. A randomized open‐label clinical trial examining the effect of denosumab on the prevention of 1st‐year bone mineral density loss after renal transplantation (POSTOP study; NCT01377467) [abstract]. Nephrology Dialysis Transplantation 2012;27(Suppl 2):ii304. [EMBASE: 70766189] [Google Scholar]
- Bonani M, Fehr T, Mueller T, Blum M, Brockmann J, Frey D, et al. Prevention of bone mineral density (BMD) loss after kidney transplantation with the rank ligand inhibitor denosumab (POSTOP study): Baseline data, biomarker response and initial safety [abstract no: P47]. Swiss Medical Weekly 2014;144(Suppl 208):24S. [EMBASE: 71713909] [Google Scholar]
- Bonani M, Frey D, Brockmann J, Fehr T, Mueller TF, Saleh L, et al. Effect of twice‐yearly denosumab on prevention of bone mineral density loss in de novo kidney transplant recipients: a randomized controlled trial. American Journal of Transplantation 2016;16(6):1882‐91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bonani M, Frey D, Brockmann J, Fehr T, Muller T, Graf N, et al. Denosumab prevents bone mineral density loss in de novo kidney transplant recipients: results from a randomized controlled trial [abstract]. American Journal of Transplantation 2016;16(Suppl 3):323. [EMBASE: 611700418] [DOI] [PubMed] [Google Scholar]
- Bonani M, Frey D, Brockmann J, Fehr T, Muller T, Graf N, et al. Infections in de novo kidney transplant recipients treated with the RANKL inhibitor denosumab: a post‐hoc analysis of the POSTOP clinical trial (NCT01377467) [abstract]. American Journal of Transplantation 2016;16(Suppl 3):580. [EMBASE: 611699497] [Google Scholar]
- Bonani M, Frey D, Rrougemont O, Mueller NJ, Mueller TF, Graf N, et al. Infections in de novo kidney transplant recipients treated with the RANKL inhibitor denosumab. Transplantation 2016;101(9):2139‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bonani M, Meyer U, Frey D, Graf N, Bischoff‐Ferrari HA, Wuthrich RP. Effect of denosumab on peripheral compartmental bone density, microarchitecture and estimated bone strength in de novo kidney transplant recipients. Kidney & Blood Pressure Research 2016;41(5):614‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bonani M, Rodriguez D, Fehr T, Mohebbi N, Brockmann J, Blum M, et al. Sclerostin blood levels before and after kidney transplantation. Kidney & Blood Pressure Research 2014;39(4):230‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bonani M, Serra AL, Fehr T, Brockmann J, Schiesser M, Frey DP, et al. A randomized open‐label clinical trial examining the effect of denosumab on the prevention of first‐year bone mineral density loss after renal transplantation (postop study; NCT01377467) [abstract]. Transplantation 2012;94(Suppl 105):887. [EMNBASE: 71251549] [Google Scholar]
- Wuthrich R, Frey D, Mueller T, Graf N, Bonani M. Effect of the RANKL inhibitor denosumab on early loss of bone mineral density and skeletal microstructure in first‐year kidney transplant recipients [abstract]. Transplantation 2016;100(7 Suppl 1):S215. [EMBASE: 613005138] [Google Scholar]
- Wuthrich RP, Frey DP, Blum M, Rodriguez D, Bonani M. Effect of RANK ligand inhibition with denosumab on CKD‐MBD parameters in de novo renal transplant recipients [abstract no: TH‐PO613]. Journal of the American Society of Nephrology 2014;25(Abstract Suppl):247A. [Google Scholar]
- Wuthrich RP, Frey DP, Brockmann JG, Fehr T, Mueller TF, Saleh L, et al. Prevention of bone mineral density loss in de novo kidney transplant recipients with twice‐yearly denosumab: a randomized controlled trial (clinicaltrials.gov number NCT01377467 [abstract no: HI‐OR06]. Journal of the American Society of Nephrology 2015;26(Abstract Suppl):B2. [DOI] [PubMed] [Google Scholar]
- Wuthrich RP, Graf N, Bonani M. Effect of denosumab on trabecular bone score (TBS) in de novo kidney transplant recipients (KTR) [abstract no: SA‐PO654]. Journal of the American Society of Nephrology 2018;29(Abstract Suppl):905. [Google Scholar]
Praditpornsilpa 2014 {published data only}
- Praditpornsilpa K, Auswinporn S, Asawanonda P, Townamchai N, Avihingsanon Y, Eiam‐Ong S. UVB exposure increases serum calcidiol level in vitamin D deficiency kidney transplantation recipients [abstract no: B931]. Transplantation 2014;98(Suppl 1):528. [EMBASE: 71545313] [Google Scholar]
Psimenou 2002 {published data only}
- Psimenou E, Konstantinidou E, Giapraka N, Marinaki S, Kostakis A, Stathakis CP, et al. Randomised controlled study of calcitonin and etidronate in the treatment of osteoporosis in renal transplant patients [abstract no: 2316]. XIXth International Congress of the Transplantation Society; 2002 Aug 25‐30; Miami, USA. 2002. [CENTRAL: CN‐00416499]
Sanchez‐Escuredo 2015 {published data only}
- Sanchez‐Escuredo A, Fuster D, Rubello D, Muxi A, Ramos A, Campos F, et al. Monthly ibandronate versus weekly risedronate treatment for low bone mineral density in stable renal transplant patients. Nuclear Medicine Communications 2015;36(8):815‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Shahidi 2011 {published data only}
- Shahidi S, Kolahdooz S, Mortazavi M. Comparison between the effects of calcitriol and cholecalciferol on bone mineral density of renal transplant patients [abstract]. Journal of Isfahan Medical School 2012;30(197). [EMBASE: 373961649] [Google Scholar]
- Shahidi S, Kolahdose S, Mortazavi M. Comparison between the effects of calcitriol and cholecalciferol on bone mineral density of renal transplant patients [abstract]. Iranian Journal of Kidney Diseases 2011;5(Suppl 2):4. [EMBASE: 70673814] [Google Scholar]
Shahidi 2015 {published data only}
- Shahidi S, Ashrafi F, Mohammadi M, Moeinzadeh F, Atapour A. Low‐dose pamidronate for treatment of early bone loss following kidney transplantation: a randomized controlled trial. Iranian Journal of Kidney Diseases 2015;9(1):50‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Sharma 2002a {published data only}
- Sharma RK, Jeloka T, Gupta A, Gupta S, Gulati S, Kapoor R. Effect of alendronate on post renal transplant osteoporosis: a randomised study [abstract no: M‐PO50059]. Nephrology 2005;10(Suppl 1):A96. [CENTRAL: CN‐00782943] [Google Scholar]
- Sharma RK, Jeloka T, Gupta A, Gupta S, Gulati S, Kapoor R, et al. Effect of alendronate of post renal transplant osteoporosis: a randomised study [abstract no: O153]. Transplantation 2004;78(2 Suppl):60. [CENTRAL: CN‐00509474] [Google Scholar]
- Sharma RK, Jeloka T, Gupta A, Gupta S, Gulati S, Sharma AP. Effect of alendronate on post renal transplant osteoporosis: a randomized study [abstract no: SU‐PO544]. Journal of the American Society of Nephrology 2003;14(Nov):652A. [CENTRAL: CN‐00583910] [Google Scholar]
- Sharma RK, Jeloka T, Gupta A, Gupta S, Gulati S, Sharma AP, et al. Role of alendronate in post renal transplant osteoporosis: a randomised study [abstract]. Indian Journal of Nephrology 2002;12(4):236‐7. [CENTRAL: CN‐00461717] [Google Scholar]
- Sharma RK, Jeloka T, Gupta S, Gupta S, Gulati S, Sharma AP, et al. Role of alendronate on post renal transplant osteoporosis: a randomised study [abstract no: M775]. Nephrology Dialysis Transplantation 2003;18(Suppl 4):249. [CENTRAL: CN‐00447697] [Google Scholar]
Sirsat 2010 {published data only}
- Sirsat RA, Puri VS, Holkar SD, Almeida AF, Langote AC, Kothari JP, et al. Is pamidronate more effective than alendronate in adult patients for the prevention of bone loss after kidney transplantation? [abstract no: PUB116]. Journal of the American Society of Nephrology 2010;21(Abstract Suppl):836A. [Google Scholar]
Smerud 2012 {published data only}
- Smerud KT, Asberg A, Kile H, Pasch A, Dahle DO, Bollerslev J, et al. A rapid and sustained improvement of calcification propensity score (serum T50) after successful kidney transplantation: reanalysis of a randomized controlled trial of ibandronate. Clinical Transplantation 2017;31(12):e13131. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Smerud KT, Dolgos S, Olsen IC, Asberg A, Sagedal S, Reisaeter AV, et al. A 1‐year randomized, double‐blind, placebo‐controlled study of intravenous ibandronate on bone loss following renal transplantation. American Journal of Transplantation 2012;12(12):3316‐25. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Smerud KT, Dolgos S, Olsen IC, Asberg A, Sagedal S, Reisaeter AV, et al. A one year prospective, randomised, double‐blind, placebo‐controlled study of intravenous ibandronate on bone loss following renal transplantation [abstract no: O‐144]. Transplant International 2011;24(Suppl 2):40. [EMBASE: 70527221] [Google Scholar]
Starke 2012 {published data only}
- Starke A, Corsenca A, Kohler T, Knubben J, Kraenzlin M, Uebelhart D, et al. Correction of metabolic acidosis with potassium citrate in renal transplant patients and its effect on bone quality. Clinical Journal of the American Society of Nephrology: CJASN 2012;7(9):1461‐72. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tałałaj 1996 {published data only}
- Talalaj M, Gradowska L, Marcinowska‐Suchowierska E, Durlik M, Gaciong Z, Lao M. Efficiency of preventive treatment of glucocorticoid‐induced osteoporosis with 25‐hydroxyvitamin D3 and calcium in kidney transplant patients. Transplantation Proceedings 1996;28(6):3485‐7. [MEDLINE: ] [PubMed] [Google Scholar]
Thervet 2008 {published data only}
- Thervet E, Courbebaisse M, Couberbielle JC, Zuber J, Martinez F, Mamzer MF, et al. Prospective evaluation of the risk benefit ratio of a vitamin D treatment during the early period after renal transplantation [abstract no: 697]. Transplantation 2008;86(Suppl 2):244. [CENTRAL: CN‐00783956] [Google Scholar]
Tiryaki 2015 {published data only}
- Tiryaki O, Usalan C, Coban S, Yildiz F. Vitamin D receptor activation with calcitriol reduce urinary angiotensinogen A marker of intrarenal renin angiotensin system correlates with albuminuria in patients with hypertensive chronic renal allograft nephropathy [abstract no: P275]. Transplant International 2015;28(Suppl 4):462. [EMBASE: 72112261] [Google Scholar]
Torregrosa 2003 {published and unpublished data}
- Torregrosa JV, Moreno A, Gutierrez A, Vidal S, Oppenheimer F. Alendronate for treatment of renal transplant patients with osteoporosis. Transplantation Proceedings 2003;35(4):1393‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Torregrosa 2007 {published data only}
- Torregrosa JV, Fuster D, Pedroso S, Diekmann F, Campistol JM, Rubi S, et al. Weekly risedronate in kidney transplant patients with osteopenia. Transplant International 2007;20(8):708‐11. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Torregrosa 2010 {published data only}
- Torregrosa JV, Fuster D, Gentil MA, Marcen R, Guirado L, Zarraga S, et al. Open‐label trial: effect of weekly risedronate immediately after transplantation in kidney recipients. Transplantation 2010;89(12):1476‐81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Torregrosa JV, Gentil MA, Marcen R, Zarraga S, Bravo J, Guirado L, et al. Open‐label trial: weekly risedronate immediately after transplantation in kidney recipients with osteopenia and vascular calcification [abstract no: M728]. World Congress of Nephrology; 2009 May 22‐26; Milan, Italy. 2009.
Torregrosa 2011 {published data only}
- Torregrosa JV, Fuster D, Monegal A, Gentil MA, Bravo J, Guirado L, et al. Efficacy of low doses of pamidronate in osteopenic patients administered in the early post‐renal transplant. Osteoporosis International 2011;22(1):281‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Torres 2004 {published data only}
- Garcia S, Barrios Y, Gonzalez A, Concepcion MT, Checa MD, Lorenzo V, et al. Oral calcitriol prevents early bone loss after renal transplantation (RT): double blind placebo controlled study [abstract no: 3036]. Journal of the American Society of Nephrology 2000;11(Sept):575A. [CENTRAL: CN‐00601909] [Google Scholar]
- Torres A, Garcia S, Gomez A, Gonzalez A, Barrios Y, Concepcion MT, et al. Treatment with intermittent calcitriol and calcium reduces bone loss after renal transplantation. Kidney International 2004;65(2):705‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Trabulus 2008 {published data only}
- Trabulus S, Altiparmak MR, Apaydin S, Serdengecti K, Sariyar M. Treatment of renal transplant recipients with low bone mineral density: a randomized prospective trial of alendronate, alfacalcidol, and alendronate combined with alfacalcidol. Transplantation Proceedings 2008;40(1):160‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Trillini 2015 {published data only}
- Trillini M, Cortinovis M, Ruggenenti P, Reyes Loaeza J, Courville K, Ferrer‐Siles C, et al. Paricalcitol for secondary hyperparathyroidism in renal transplantation. Journal of the American Society of Nephrology 2015;26(5):1205‐14. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trillini M, Reyes Loaeza J, Courville K, Ferrer‐Siles C, Prandini S, Gaspari F, et al. Oral paricalcitol ameliorates post‐transplant hyperparathyroidism and proteinuria in kidney transplantation [abstract no: SA‐PO975]. Journal of the American Society of Nephrology 2013;24(Abstracts):850A. [Google Scholar]
Ugur 2000 {published data only}
- Uğur A, Guvener N, Isiklar I, Karakayali H, Erdal R. Efficiency of preventive treatment for osteoporosis after renal transplantation. Transplantation Proceedings 2000;32(3):556‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Walsh 2009 {published data only}
- Cunningham J, Altmann P, Pattison J, Wilkie M, Dudley C, Cockwell P, et al. Effect of pamidronate (aredia) on bone loss and fracture after renal transplantation [abstract no: TH‐PO121]. Journal of the American Society of Nephrology 2006;17(Abstracts):131A. [CENTRAL: CN‐00783004] [Google Scholar]
- Walsh SB, Altmann P, Pattison J, Wilkie M, Yaqoob MM, Dudley C, et al. Effect of pamidronate on bone loss after kidney transplantation: a randomized trial. American Journal of Kidney Diseases 2009;53(5):856‐65. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wissing 2005 {published data only}
- Wissing KM, Broeders N, Moreno‐Reyes R, Gervy C, Stallenberg B, Abramowicz D. A controlled study of vitamin D3 to prevent bone loss in renal‐transplant patients receiving low doses of steroids. Transplantation 2005;79(1):108‐15. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Wissing M, Broeders N, Schoutens A, Abramowicz D. A prospective and randomized study of calcium and cholecalciferol treatment to prevent bone loss after renal transplantation [abstract]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):952A. [CENTRAL: CN‐00550566] [Google Scholar]
References to studies excluded from this review
Ambuhl 1999 {published data only}
- Ambuhl PM, Meier D, Wolf B, Dydak U, Boesiger P, Binswanger U. Metabolic aspects of phosphate replacement therapy for hypophosphatemia after renal transplantation: impact on muscular phosphate content, mineral metabolism, and acid/base homeostasis. American Journal of Kidney Diseases 1999;34(5):875‐83. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ardalan 2007 {published data only}
- Ardalan MR, Maljaei H, Shoja MM, Piri AR, Khosroshahi HT, Noshad H, et al. Calcitriol started in the donor, expands the population of CD4+CD25+ T cells in renal transplant recipients. Transplantation Proceedings 2007;39(4):951‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Campistol 1999 {published data only}
- Campistol JM, Backman L, Brattstrom C, Kreis H, Morales JM, Sirolimus European Renal Transplant Study Group. Influence of immunosuppressive treatment on markers of bone remodeling in renal transplantation: comparison between cyclosporine and sirolimus [abstract]. Journal of the American Society of Nephrology 1999;10(Program & Abstracts):754A. [CENTRAL: CN–00550450] [Google Scholar]
Campistol 2000 {published data only}
- Campistol JM, Cole E, Gioud‐Paquet M, US European and Global Renal Transplant Study Groups. Sirolimus (rapamune): effects on bone in renal transplant patients [abstract]. Transplantation 2000;69(8 Suppl):S289. [CENTRAL: CN–00444659] [Google Scholar]
El‐Haggan 2002 {published data only}
- El‐Haggan W, Barthe N, Berger F, Castaing F, Chauveau P, Vendrely B, et al. Changes in bone mineral density (BMD) in kidney transplant recipients receiving tacrolimus (FK506) versus cyclosporine (Cy‐A) [abstract no: A4637]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):886A‐887A. [CENTRAL: CN‐00433625] [Google Scholar]
- El‐Haggan W, Barthe N, Vendrely B, Chauveau P, Berger F, Aparicio M, et al. One year evolution of bone mineral density in kidney transplant recipients receiving tacrolimus versus cyclosporine. Transplantation Proceedings 2002;34(5):1817‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
James 2003 {published data only}
- James G, Raggi P, Boulay A, Burke S, Chasan‐Taber S, Chertow G, et al. Thoracic vertebral bone density increases with Renagel and decreases with calcium‐based phosphate binder therapy ‐ a two year study [abstract no: W423]. Nephrology Dialysis Transplantation 2003;18(Suppl 4):681. [CENTRAL: CN‐00445894] [Google Scholar]
Josephson 2004 {published data only}
- Josephson MA, Schum LP, Chiu MY, Marshall C, Sprague SM. Post‐transplant osteopenia [abstract]. Journal of the American Society of Nephrology 1999;10(Program & Abstracts):759A. [CENTRAL: CN‐00583636] [Google Scholar]
- Josephson MA, Schumm LP, Chiu MY, Marshall C, Sprague SM. Calcium and calcitriol prophylaxis against post‐transplant bone loss [abstract]. Journal of the American Society of Nephrology 2000;11(Program & Abstracts):720A. [CENTRAL: CN‐00583638] [Google Scholar]
- Josephson MA, Schumm LP, Chiu MY, Marshall C, Thistlethwaite JR, Sprague SM. Calcium and calcitriol prophylaxis attenuates posttransplant bone loss. Transplantation 2004;78(8):1233‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Labib 1999 {published data only}
- Labib B, Ibrahim MA, Shawarby M, Abudl Rahman A, Abdel Wahab M, Elagroudy A. Effect of calculation therapy on renal osteodystrophy [abstract]. XXXVI Congress of the European Renal Association European Dialysis & Transplant Association; 1999 Sep 5‐8; Madrid, Spain. 1999:42. [CENTRAL: CN‐00484726]
Lebranchu 1999 {published data only}
- Hene RJ, M55002 Study Group. A randomized, double‐blind, multi‐center trial comparing two corticosteroid regimens in combination with mycophenolate mofetil (MMF) and cyslosporine (CYA) in renal transplant recipients [abstract no: 420]. Transplantation 1998;65(12):S107. [CENTRAL: CN‐00763818] [Google Scholar]
- Lebranchu Y. Comparison of two corticosteroid regimens in combination with CellCept and cyclosporine A for prevention of acute allograft rejection: 12 month results of a double‐blind, randomized, multi‐center study. M 55002 Study Group. Transplantation Proceedings 1999;31(1‐2):249‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lebranchu Y, Aubert P, Bayle F, Bedrossian J, Berthoux F, Bourbigot B, et al. Could steroids be withdrawn in renal transplant patients sequentially treated with ATG, cyclosporine, and cellcept? One‐year results of a double‐blind, randomized, multicenter study comparing normal dose versus low‐dose and withdrawal of steroids. M 55002 French Study Group. Transplantation Proceedings 2000;32(2):396‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lebranchu Y, M55002 Study Group. A comparison of two corticosteroid regimens in kidney transplanted patients treated with ATG/OKT3 induction, mycophenolate mofetil (MMF) and cyclosporine A (CyA) for prevention of acute allograft rejection. 12 months results of a double‐blind, randomized, multi‐center study [abstract no: 932]. Transplantation 1999;67(7):S239. [CENTRAL: CN‐00763351] [DOI] [PubMed] [Google Scholar]
- Nowacka‐Cieciura E, Durlik M, Cieciura T, Kukula K, Lewandowska D, Baczkowska T, et al. Elevated serum immunoglobulins after steroid withdrawal in renal allograft recipients. Transplantation Proceedings 2002;34(2):564‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nowacka‐Cieciura E, Durlik M, Cieciura T, Lewandowska D, Baczkowska T, Kukula K, et al. Steroid withdrawal after renal transplantation‐‐risks and benefits. Transplantation Proceedings 2002;34(2):560‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nowacka‐Cieciura E, Durlik M, Cieciura T, TaLaLaj M, KukuLa K, Lewadowska D, et al. Positive effect of steroid withdrawal on bone mineral density in renal allograft recipients [abstract no: P0568W]. XVIII International Congress of the Transplantation Society; 2000 Aug 27‐Sep 1; Rome, Italy. 2000. [CENTRAL: CN‐00446978] [DOI] [PubMed]
- Nowacka‐Cieciura E, Durlik M, Cieciura T, Talalaj M, KukuLa K, Lewandowska D, et al. Positive effect of steroid withdrawal on bone mineral density in renal allograft recipients. Transplantation Proceedings 2001;33(1‐2):1273‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nowacka‐Cieciura E, Durlik M, Cieciura T, Talalaj M, Kukula K, Lewadowska D, et al. Positive effect of steroid withdrawal on bone mineral density in renal allograft recipients [abstract]. XVIII International Congress of the Transplantation Society; 2000 Aug 27 Sep 1; Rome, Italy. 2000. [CENTRAL: CN‐00446978] [DOI] [PubMed]
- Nowacka‐Cieciura E, Durlik M, Cieciura T, Talalaj M, Kukula K, Lewandowska D, et al. Positive effect of steroid withdrawal on bone mineral density in renal allograft recipients. Transplantation Proceedings 2001;33(1‐2):1273‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nowacka‐Cieciura E, Soluch L, Cieciura T, Lewandowska D, Durlik M, Shaibani B, et al. Effect of glucocorticoid‐free immunosuppressive protocol on serum lipids in renal transplant patients. Transplantation Proceedings 2000;32(6):1339‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Puig i Mari JM. Induction treatment with mycophenolate mofetil, cyclosporine, and low‐dose steroids with subsequent early withdrawal in renal transplant patients: results of the Spanish Group. Spanish Group of the CellCept Study. Transplantation Proceedings 1999;31(6):2256‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Vanrenterghem Y, Lebranchu Y, Hene R, Oppenheimer F, Ekberg H. Double‐blind comparison of two corticosteroid regimens plus mycophenolate mofetil and cyclosporine for prevention of acute renal allograft rejection. Transplantation 2000;70(9):1352‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lippuner 1996 {published data only}
- Lippuner K, Haller B, Casez JP, Montandon A, Jaeger P. Effect of disodium monofluorophosphate, calcium and vitamin D supplementation on bone mineral density in patients chronically treated with glucocorticosteroids: a prospective, randomized, double‐blind study. Mineral & Electrolyte Metabolism 1996;22(4):207‐13. [MEDLINE: ] [PubMed] [Google Scholar]
Lippuner 1998 {published data only}
- Lippuner K, Casez JP, Horber F, Dijkhuis E, Jaeger P. Glucocorticosteroids (GC) early after kidney transplantation (KT): beneficial effect of deflazacort (DFZ) versus prednisone (PRED) on bone and body composition in a double blind study [abstract no: A3223]. Journal of the American Society of Nephrology 1997;8(Program & Abstracts):692A. [CENTRAL: CN‐00446424] [Google Scholar]
- Lippuner K, Casez JP, Horber FF, Jaeger P. Effects of deflazacort versus prednisone on bone mass, body composition, and lipid profile: a randomized, double blind study in kidney transplant patients. Journal of Clinical Endocrinology & Metabolism 1998;83(11):3795‐802. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Masse 2001 {published data only}
- Masse M, Girardin C, Ouimet D, Dandavino R, Boucher A, Madore F, et al. Initial bone loss in kidney transplant recipients: a prospective study. Transplantation Proceedings 2001;33(1‐2):1211. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
NCT00646282 {published data only}
- Raggi P, Guasch A. Mineral metabolism and vascular effects of Vitamin D therapy in kidney. www.clinicaltrials.gov/ct2/show/NCT00646282 (first received 25 March 2008).
Ponticelli 1997 {published data only}
- Aroldi A, Tarantino A, Montagnino G, Cesana B, Cocucci C, Ponticelli C. Effects of three immunosuppressive regimens on vertebral bone density in renal transplant recipients: a prospective study. Transplantation 1997;63(3):380‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Goffin E, Devogelaer JP, Depresseux G, Squifflet JP, Pirson Y. Osteoporosis after organ transplantation. Lancet 2001;357(9268):1623. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Montagnino G, Tarantino A, Maccario M, Elli A, Cesana B, Ponticelli C. Long‐term results with cyclosporine monotherapy in renal transplant patients: a multivariate analysis of risk factors. American Journal of Kidney Diseases 2000;35(6):1135‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Montagnino G, Tarantino A, Segoloni GP, Cambi V, Rizzo G, Altieri P, et al. Long‐term results of a randomized study comparing three immunosuppressive schedules with cyclosporine in cadaveric kidney transplantation. Journal of the American Society of Nephrology 2001;12(10):2163‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Ponticelli C. Steroid withdrawal in organ transplant recipients [abstract no: 0351]. XVIII International Congress of the Transplantation Society; 2000 Aug 27‐Sep 1; Rome, Italy. 2000. [CENTRAL: CN‐00583616]
- Ponticelli C, Aroldi A. Osteoporosis after organ transplantation. Lancet 2001;357(9268):1623. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Ponticelli C, Tarantino A, Montagnino G. Steroid withdrawal in renal transplant recipients. Transplantation Proceedings 2001;33(1‐2):987‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Ponticelli C, Tarantino A, Segoloni GP, Cambi V, Rizzo G, Altieri P, et al. A randomized study comparing cyclosporine alone vs double and triple therapy in renal transplants. The Italian Multicentre Study Group for Renal Transplantation (SIMTRe). Transplantation Proceedings 1997;29(1‐2):290‐1. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Ponticelli C, Tarantino A, Segoloni GP, Cambi V, Rizzo G, Altieri P, et al. A randomized study comparing three cyclosporine‐based regimens in cadaveric renal transplantation. Italian Multicentre Study Group for Renal Transplantation (SIMTRe). Journal of the American Society of Nephrology 1997;8(4):638‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Tarantino A, Italian Multicentre Study Group for Renal Transplantation (SIMTRe). Is cylosporine (CsA, Sandimmun) monotherapy an effective and safe immunosuppressant in renal transplant recipients? [abstract]. 16th Annual Meeting. American Society of Transplant Physicians (ASTP); 1997 May 10‐14; Chicago (IL). 1997:128. [CENTRAL: CN‐00509501]
- Tarantino A, Segoloni GP, Cambi V, Rizzo G, Altieri P, Mastrangelo F, et al. A randomized study comparing three cyclosporine‐based regimens in cadaveric renal transplantation: results at 7 years. Transplantation Proceedings 1998;30(5):1729‐31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Tarantino A, per il Gruppo SIMTRE. Long‐term results of a randomized trial of 3 cyclosporine (CSA) regimens in cadaveric kidney allografts (TXC) [abstract]. Nephrology Dialysis Transplantation 2000;15(9):A250. [CENTRAL: CN‐00461836] [Google Scholar]
Reed 2004 {published data only}
- Reed J, Keightley G, Blumenthal S, Bradley C, LaBrecque J, Turner S, et al. The CONTROL STUDY: enhanced achievement of NKF‐K/DOQITM bone metabolism and disease targets using cinacalcet HCI (SensiparTM) [abstract no: F‐PO986]. Journal of the American Society of Nephrology 2004;15(Program & Abstracts):280–1A. [CENTRAL: CN–00550527] [Google Scholar]
Rigotti 2003 {published data only}
- Rigotti P, Vialtel P, Pascual J, Sanchez‐Fructuoso A, Escuin F, the Bone Mineral Density Study Group. Immunosuppression without maintenance steroids prevents decline of bone mineral density following renal transplantation [abstract]. American Journal of Transplantation 2003;3(Suppl 5):199. [CENTRAL: CN–00447406] [Google Scholar]
ter Meulen 2003 {published data only}
- Hendrikx TK, Klepper M, Ijzermans J, Weimar W, Baan CC. Clinical rejection and persistent immune regulation in kidney transplant patients. Transplant Immunology 2009;21(3):129‐35. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Hesselink DA, Ngyuen H, Wabbijn M, Gregoor PJ, Steyerberg EW, Riemsdijk IC, et al. Tacrolimus dose requirement in renal transplant recipients is significantly higher when used in combination with corticosteroids. British Journal of Clinical Pharmacology 2003;56(3):327‐30. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselink DA, Ngyuen H, Wabbijn M, Smak Gregoor PJ, Steyerberg EW, Riemsdijk IC, et al. Tacrolimus dose requirement in renal transplant recipients is significantly higher when used in combination with corticosteroids [abstract no: 1290]. American Journal of Transplantation 2003;3(Suppl 5):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Meulen CG, Riemsdijk IC, Hene RJ, Christiaans MHL, Gelder T, Hilbrands LB, et al. A prospective randomized trial comparing steroid‐free immunosuppresion with limited steroid exposure on bone mineral density in the first year after renal transplantation [abstract no: 0344]. XIXth International Congress of the Transplantation Society; 2002 Aug 25‐30; Miami (FL). 2002. [CENTRAL: CN‐00402832]
- ter Meulen CG, Goertz JH, Klasen IS, Verweij CM, Hilbrands LB, Wetzels JF, et al. Decreased renal excretion of soluble interleukin‐2 receptor alpha after treatment with daclizumab. Kidney International 2003;64(2):697‐703. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- ter Meulen CG, Hilbrands LB, Bergh JP, Hermus AR, Hoitsma AJ. The influence of corticosteroids on quantitative ultrasound parameters of the calcaneus in the 1st year after renal transplantation. Osteoporosis International 2005;16(3):255‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- ter Meulen CG, Riemsdijk I, Hene RJ, Christiaans MH, Borm GF, Corstens FH, et al. No important influence of limited steroid exposure on bone mass during the first year after renal transplantation: a prospective, randomized, multicenter study. Transplantation 2004;78(1):101‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- ter Meulen CG, Riemsdijk IC, Hene RJ, Christiaans MHL, Gelder T, Hilbrands LB, et al. A prospective randomized trial comparing steroid‐free immunosuppression with limited steroid exposure on bone mineral density in the first year after renal transplantation [abstract no: 0344]. XIXth International Congress of the Transplantation Society; 2002 Aug 25‐30; Miami (FL). 2002. [CENTRAL: CN‐00402832]
- Gelder T, ter Meulen CG, Hene RJ, Christiaans MhL, Borm GF, Riemsdijk IC, et al. Steroid withdrawal at three days after renal transplantation with anti IL‐2 receptor therapy: a prospective randomized multicenter trial [abstract no: 1529]. American Journal of Transplantation 2004;4(Suppl 8):578. [CENTRAL: CN‐00509529] [DOI] [PubMed] [Google Scholar]
- Riemsdijk IC, Termeulen RG, Christiaans MH, Hene RJ, Hoitsma AJ, Hooff JP, et al. Anti‐CD25 prophylaxis allows steroid‐free renal transplantation in tacrolimus‐based immunosuppression [abstract no: 133]. American Journal of Transplantation 2002;2(Suppl 3):171. [CENTRAL: CN‐00402963] [Google Scholar]
THOMAS 2002 {published data only}
- Boots JM, Ham EC, Christiaans MH, Hooff JP. Risk of adrenal insufficiency with steroid maintenance therapy in renal transplantation. Transplantation Proceedings 2002;34(5):1696‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Budde K, Salmela K, Pascual J, Rigotti P, THOMAS Study Group. Steroid‐withdrawal in tacrolimus‐treated renal transplant recipients: results of a 3‐year follow‐up study [abstract no: 221]. 3rd International Congress on Immunosuppression; 2004 Dec 8‐11; San Diego (CA). 2004. [CENTRAL: CN‐00550470]
- Jindal RM, Salmela K, Vanrentergheim Y, Hooff JP, Squifflet JP. Reduction of high cholesterol levels by early withdrawal of steroids from a tacrolimus‐based triple regimen [abstract no: 206]. American Journal of Transplantation 2002;2(Suppl 3):190. [CENTRAL: CN‐00520347] [Google Scholar]
- Pascual J, Hooff JP, Salmela K, Budde K, Rigotti P, Lang P. Long‐term efficacy and safety of steroid‐withdrawal in tacrolimus treated renal transplant recipients: results of a 3 year follow‐up [abstract no: 1524]. American Journal of Transplantation 2004;4(Suppl 8):576‐7. [CENTRAL: CN‐00615852] [Google Scholar]
- Pascual J, Hooff JP, Salmela K, Lang P, Rigotti P, Budde K. Three‐year observational follow‐up of a multicenter, randomized trial on tacrolimus‐based therapy with withdrawal of steroids or mycophenolate mofetil after renal transplant. Transplantation 2006;82(1):55‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Rigotti P, European Tacrolimus/MMF Transplantation Study Group. Patients with high cholesterol levels benefit most from early withdrawal of corticosteroids. Transplantation Proceedings 2002;34(5):1797‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Squifflet JP, Vanrenterghem Y, Hooff JP, Salmela K, Rigotti P, European Tacrolimus/MMF Transplantation Study Group. Safe withdrawal of corticosteroids or mycophenolate mofetil: results of a large, prospective, multicenter, randomized study. Transplantation Proceedings 2002;34(5):1584‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Hoof JP, Salmela K, Budde K, Pascual J, Rigotti P, Lang P, et al. Long‐term efficacy and safety of steroid‐withdrawal in tacrolimus‐treated patients: results of a long‐term follow‐up study in renal transplant recipients [abstract no: 99]. 11th Congress of the European Society for Transplantation (ESOT); 2003 Sep 20‐24; Venice, Italy. 2003. [CENTRAL: CN‐00653800]
- Vanrenterghem Y, Hooff JP, Squifflet JP, Salmela K, Rigotti P, Jindal RM, et al. Minimization of immunosuppressive therapy after renal transplantation: results of a randomized controlled trial. American Journal of Transplantation 2005;5(1):87‐95. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Hooff JP, Vanrenterghem Y, Squifflet JP, Salmela K, Ancona E, European Tacrolimus/MMF Transplantation Study Group. First, large, prospective study of a controlled withdrawal of steroids or MMF following three months of tacrolimus/MMF/steroid therapy [abstract no: A4809]. Journal of the American Society of Nephrology 2001;12(Program & Abstracts):920A‐1A. [CENTRAL: CN‐00550422] [Google Scholar]
- Hooff JP, European Tacrolimus/MMF Transplantation Study Group. Effect of controlled steroid withdrawal on glucose levels in a tacrolimus‐based immunosuppression regimen [abstract no: P‐69]. 3rd International Congress on Immunosuppression; 2004 Dec 8‐11; San Diego (CA). 2004. [CENTRAL: CN‐00550420]
- Ham EC, Christiaans MH, Heidendal GA, van‐Hooff JP. Effects of different steroid dosages on bone mineral density and body composition in renal transplant patients [abstract]. Clinical Nutrition 1998;17(Suppl 1):44. [CENTRAL: CN‐00285279] [Google Scholar]
- Ham EC, Kooman JP, Christiaans MH, Hooff JP. The influence of early steroid withdrawal on body composition in renal transplant patients [abstract]. Journal of the American Society of Nephrology 2000;11(Sept):711A. [CENTRAL: CN‐00550623] [Google Scholar]
- Ham EC, Kooman JP, Christiaans ML, Hooff JP. The influence of early steroid withdrawal on body composition and bone mineral density in renal transplantation patients. Transplant International 2003;16(2):82‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vasquez 2004 {published data only}
- Vasquez EM, Sifontis N, Jacobssen V, Testa G, Sankary H, Benedetti E. Simvastatin for prevention of bone loss following renal transplantation [abstract no: P284]. Transplantation 2004;78(2 Suppl):293. [CENTRAL: CN‐00509537] [Google Scholar]
Zaoui 2003 {published data only}
- Zaoui P, Vialtel P, Rigotti P, Pascual J, Sanchez‐Fructuoso A, Escuin F, et al. A steroid‐free immunosuppressive regimen of daclizumab, tacrolimus and MMF prevents loss of bone mass following renal transplantation [abstract]. Nephrology Dialysis Transplantation 2003;18(Suppl 4):495. [CENTRAL: CN–00448519] [Google Scholar]
References to studies awaiting assessment
Jorge 2016 {published data only}
- Jorge C, Adragao T, Matias P, Bruges M, Birne R, Laranjinha I, et al. A prospective randomized controlled study of cholecalciferol supplementation in kidney transplant recipients‐ preliminary results at 30 months [abstract no: TH‐PO766]. Journal of the American Society of Nephrology 2016;27(Abstract Suppl):271A. [Google Scholar]
Marques 2019 {published data only}
- Marques I, Araujo MJC, Graciolli F, dos Reis L, Pereira RM, Custodio M, et al. A prospective and randomized trial of zoledronic acid to prevent bone loss in the first year after kidney transplantation. [abstract no: TH‐PO923]. Journal of the American Society of Nephrology 2017;28(Abstract Suppl):339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques IDB, Araujo MJCL, Graciolli FG, dos Reis LM, Pereira RMR, Alvarenga JC, et al. A randomized trial of zoledronic acid to prevent bone loss in the first year after kidney transplantation. Journal of the American Society of Nephrology 2019;30(2):355‐65. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01675089 {published data only}
- David‐Neto E. Zoledronic acid to prevent bone loss after kidney transplantation. www.clinicaltrials.gov/ct2/show/NCT01675089 (first received 23 August 2012).
Oblak 2017 {published data only}
- Arnol M, Oblak M, Mlinsek G, Bren AF, Buturovic‐Ponikvar J, Kandus A. Proteinuria in kidney transplant recipients: Prevalence in a national cohort and study design of the effect of paricalcitol for reduction of proteinuria [abstract no: RO‐204]. Transplant International 2011;24(Suppl 2):185. [EMBASE: 70527733] [Google Scholar]
- Arnol M, Oblak M, Mlinsek G, Buturovic‐Ponikvar J, Kandus A. Paricalcitol versus placebo for reduction of proteinuria in kidney transplant recipients: a double‐blind, randomized controlled trial [abstract]. Transplantation 2016;100(7 Suppl 1):S214‐5. [EMBASE: 613005120] [DOI] [PubMed] [Google Scholar]
- Oblak M, Mlinsek G, Kandus A, Buturovic‐Ponikvar J, Arnol M. Effects of paricalcitol on biomarkers of inflammation and fibrosis in kidney transplant recipients: results of a randomized controlled trial. Clinical Nephrology 2017;88(13):119‐25. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Oblak M, Mlinsek G, Kandus A, Buturovic‐Ponikvar J, Arnol M. Paricalcitol versus placebo for reduction of proteinuria in kidney transplant recipients: a double‐blind, randomized controlled trial. Transplant International 2018;31(12):1391‐404. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Tiryaki 2018 {published data only}
- Tiryaki O, Usalan C, Tarakcioglu M, Coban S. Calcitriol reduces albuminuria and urinary angiotensinogen level in renal transplant recipients. Transplantation Proceedings 2018;50(5):1342‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT00748618 {published data only}
- Larsen J. Vitamin D replacement after kidney transplant. www.clinicaltrials.gov/ct2/show/NCT00748618 (first received 4 September 2008).
NCT00889629 {published data only}
- Markell M. Pilot study: Effects of hectorol (doxercalciferol) vitamin D replacement on proteinuria, PTH level and bone turnover in stable kidney transplant recipients: a single‐blind, placebo‐controlled study in patients receiving 25‐oh vitamin D3. www.clinicaltrials.gov/ct2/show/NCT00889629 (first received 23 April 2009).
NCT02224144 {published data only}
- Nickolas T. A comparative trial of calcitriol versus placebo for the preservation of bone mass and strength after kidney transplantation. www.clinicaltrials.gov/ct2/show/NCT02224144 (first received 22 August 2014).
VITA‐D 2009 {published data only}
- Thiem U, Gessl A, Heinze G, Gossler U, Perkmann T, Kainberger F, et al. Influence of high‐dose vitamin D3 therapy on calcitriol levels in vitamin‐D‐deficient kidney transplant recipients: preliminary results of a randomized controlled trial [abstract]. Austrian Journal of Clinical Endocrinology & Metabolism 2011;4:19. [EMBASE: 70805209] [Google Scholar]
- Thiem U, Gessl A, Heinze G, Gossler U, Perkmann T, Kainberger F, et al. Treatment of vitamin D deficiency and its impact on albumin excretion in kidney transplant recipients: preliminary results of a randomized controlled trial [abstract no: P‐303]. Transplant International 2011;24(Suppl 2):303. [EMBASE: 70528199] [Google Scholar]
- Thiem U, Heinze G, Gossler U, Perkmann T, Winkler S, Marculescu R, et al. Vitamin D for improving the outcome after kidney transplantation: rationale, design, and baseline characteristics of the participants of the VITA‐D randomized controlled trial [abstract no: P520]. Transplant International 2013;26(Suppl 2):289. [EMBASE: 71360130] [Google Scholar]
- Thiem U, Heinze G, Segel R, Perkmann T, Kainberger F, Muhlbacher F, et al. VITA‐D: cholecalciferol substitution in vitamin D deficient kidney transplant recipients: a randomized, placebo‐controlled study to evaluate the post‐transplant outcome. Trials [Electronic Resource] 2009;10:36. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiem U, Heinze G, Segel R, Perkmann T, Kainberger F, Muhlbacher F, et al. Vita‐D: cholecalciferol substitution in vitamin D deficient kidney transplant recipients: preliminary report of a RCT to evaluate the post‐transplant outcome [abstract no: Sa673]. NDT Plus 2010;3(Suppl 3):iii269. [EMBASE: 70484139] [DOI] [PMC free article] [PubMed] [Google Scholar]
VITALE 2014 {published data only}
- Courbebaisse M, Alberti C, Colas S, Prie D, Souberbielle JC, Treluyer JM, et al. VITamin D supplementation in renAL transplant recipients (VITALE): a prospective, multicentre, double‐blind, randomized trial of vitamin D estimating the benefit and safety of vitamin D3 treatment at a dose of 100,000 UI compared with a dose of 12,000 UI in renal transplant recipients: study protocol for a double‐blind, randomized, controlled trial. Trials [Electronic Resource] 2014;15(1):430. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abbott 2001
- Abbott KC, Oglesby RJ, Hypolite IO, Kirk AD, Ko CW, Welch PG, et al. Hospitalizations for fractures after renal transplantation in the United States. Annals of Epidemiology 2001;11(7):450‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Adachi 1997
- Adachi JD, Bensen WG, Brown J, Hanley D, Hodsman A, Josse R, et al. Intermittent etidronate therapy to prevent corticosteroid induced osteoporosis. New England Journal of Medicine 1997;337(6):382‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Almond 1994
- Almond MK, Kwan JT, Evans K, Cunningham J. Loss of regional bone mineral density in the first 12 months following renal transplantation. Nephron 1994;66(1):52‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Baker 2010
- Baker R, Jardine A, MacTier R. How do the KDIGO Clinical Practice Guidelines on the care of kidney transplant recipients apply to the UK?. www.renal.org/wp‐content/uploads/2017/06/management‐of‐the‐kidney‐transplant‐recipient‐in‐the‐uk.pdf (accessed 12 June 2019).
Baker 2017
- Baker RJ, Mark PB, Patel RK, Stevens KK, Palmer N. Renal Association Clinical Practice Guideline. Post‐operative care in the kidney transplant recipient. www.renal.org/wp‐content/uploads/2017/06/final‐post‐operative‐care‐guideline.pdf (accessed 12 June 2019). [DOI] [PMC free article] [PubMed]
Brown 2009
- Brown JP, Prince RL, Deal C, Recker RR, Kiel DP, Gregorio LH, et al. Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. Journal of Bone & Mineral Research 2009;24(1):153‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chadban 2009
- Chadban S, Chan M, Fry K, Patwardhan A, Ryan C, Trevillian P, et al. Nutritional interventions for the prevention of bone disease in kidney transplant recipients. Nephrology 2010;15 Suppl 1:S43‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chambers 1980
- Chambers TJ. Diphosphonates inhibit bone resorption by macrophages in vitro. Journal of Pathology 1980;132(3):255‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chesnut 2000
- Chesnut CH 3rd, Silverman S, Andriano K, Genant H, Gimona A, Harris S, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the prevent recurrence of osteoporotic fractures study. PROOF Study Group. American Journal of Medicine 2000;109(4):267‐76. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chonchol 2009
- Chonchol M, Locatelli F, Abboud HE, Charytan C, Francisco AL, Jolly S, et al. A randomized, double‐blind, placebo‐controlled study to assess the efficacy and safety of cinacalcet HCl in participants with CKD not receiving dialysis. American Journal of Kidney Diseases 2009;53(2):197‐207. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cummings 2009
- Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. New England Journal of Medicine 2009;361(8):756‐65. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
De Nijs 2004
- Nijs RN, Jacobs JW, Algra A, Lems WF, Bijlsma JW. Prevention and treatment of glucocorticoid‐induced osteoporosis with active vitamin D3 analogues: a review with meta‐analysis of randomized controlled trials including organ transplantation studies. Osteoporosis International 2004;15(8):589‐602. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
de Vries 1982
- Vries E, Weij JP, Veen CJ, Paassen HC, Jager MJ, Sleeboom HP, et al. In vitro effect of (3‐amino‐1‐hydroxypropylidene)‐1,1‐bisphosphonic acid (APD) on the function of mononuclear phagocytes in lymphocyte proliferation. Immunology 1982;47(1):157‐63. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Durieux 2002
- Durieux S, Mercadal L, Orcel, P, Dao H, Rioux C, Bernard M, et al. Bone mineral density and fracture prevalence in long‐term kidney graft recipients. Transplantation 2002;74(4):496‐500. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
ERBP 2011
- Heemann U, Abramowicz D, Spasovski G, VanHolder R, European Renal Best Practice (ERBP) Work Group on Kidney Transplantation. Endorsement of the Kidney Disease Improving Global Outcomes (KDIGO) guidelines on kidney transplantation: a European Renal Best Practice (ERBP) position statement. Nephrology Dialysis and Transplantation 2011;26(7):2099‐106. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fryer 1996
- Fryer J, Grant D, Jiang J, Metrakos P, Ozcay N, Ford C, et al. Influence of macrophage depletion on bacterial translocation and rejection in small bowel transplantation. Transplantation 1996;62(5):553‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
GRADE 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grey 1994
- Grey AB, Cundy TF, Reid IR. Continuous combined oestrogen/progestin therapy is well tolerated and increases bone density at the hip and spine in post‐menopausal osteoporosis. Clinical Endocrinology 1994;40(5):671‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Grotz 1994
- Grotz WH, Mundinger FA, Gugel B, Exner V, Kirste G, Schollmeyer PJ. Bone fracture and osteodensitometry with dual energy X‐ray absorptiometry in kidney transplant recipients. Transplantation 1994;58(8):912‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Grotz 1995
- Grotz WH, Mundinger FA, Rasenack J, Speidel L, Olschewski M, Exner VM, et al. Bone loss after kidney transplantation: a longitudinal study in 115 graft recipients. Nephrology Dialysis Transplantation 1995;10(11):2096‐100. [MEDLINE: ] [PubMed] [Google Scholar]
Hahn 1981
- Hahn TJ, Halstead LR, Baran DT. Effects of short term glucocorticoid administration on intestinal calcium absorption and circulating vitamin D metabolite concentrations in man. Journal of Clinical Endocrinology & Metabolism 1981;52(1):111‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hahn 2015
- Hahn D, Hodson EM, Craig JC. Interventions for metabolic bone disease in children with chronic kidney disease. Cochrane Database of Systematic Reviews 2015, Issue 11. [DOI: 10.1002/14651858.CD008327.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hariharan 2001
- Hariharan S. Long‐term kidney transplant survival. American Journal of Kidney Diseases 2001;38(6 Suppl 6):S44‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Heaf 2000
- Heaf J, Tvedegaard E, Kanstrup IL, Fogh‐Andersen N. Bone loss after renal transplantation: role of hyperparathyroidism, acidosis, cyclosporine and systemic disease. Clinical Transplantation 2000;14(5):457‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Horber 1994
- Horber FF, Casez JP, Steiger U, Czerniak A, Montandon A, Jaeger P. Changes in bone mass early after kidney transplantation. Journal of Bone & Mineral Research 1994;9(1):1‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hung 1996
- Hung CJ, Lee PC, Song CM, Chang YT, Tsai MT, Dai YS, et al. Clinical implication of hormone treatment in postmenopausal kidney transplants. Transplantation Proceedings 1996;28(3):1548‐50. [MEDLINE: ] [PubMed] [Google Scholar]
Jeffrey 2003
- Jeffrey JR, Leslie WD, Karpinski ME, Nickerson PW, Rush DN. Prevalence and treatment of decreased bone density in renal transplant recipients: a randomized prospective trial of calcitriol versus alendronate. Transplantation 2003;76(10):1498‐502. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Julian 1991
- Julian BA, Laskow DA, Dubovsky J, Dubovsky EV, Curtis JJ, Quarles LD. Rapid loss of vertebral mineral density after renal transplantation. New England Journal of Medicine 1991;325(8):544‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Karachalios 2004
- Karachalios T, Lyritis GP, Kaloudis J, Roidis N, Katsiri M. The effects of calcitonin on acute bone loss after pertrochanteric fractures. Journal of Bone & Joint Surgery ‐ British Volume 2004;86(3):350‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
KDIGO CKD‐MBD Guideline 2009
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD‐MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease‐Mineral and Bone Disorder (CKD‐MBD). Kidney International ‐ Supplement 2009, (113):S1‐130. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
KDIGO Transplant Guideline 2009
- Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. American Journal of Transplantation 2009;9 Suppl 3:S1‐155. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
KDOQI 2010
- Uhlig K, Berns JS, Kestenbaum B, Kumar R, Leonard MB, Martin KJ, et al. KDOQI US Commentary on the 2009 KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of CKD‐Mineral and Bone Disorder (CKD‐MBD). American Journal of Kidney Diseases 2010;55(5):773‐99. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Knoll 2010
- Knoll GA, Blydt‐Hansen TD, Campbell P, Cantarovich M, Cole E, Fairhead T, et al. Canadian Society of Transplantation and Canadian Society of Nephrology commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. American Journal of Kidney Diseases 2010;56(2):219‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Krol 2014a
- Krol CG, Dekkers OM, Kroon HM, Rabelink TJ, Koek B, Hamdy NA. No association between BMD and prevalent vertebral fractures in liver transplant recipients at time of screening for transplantation. Journal of Clinical Endocrinology & Metabolism 2014;99(10):3677‐85. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Krol 2014b
- Krol CG, Dekkers OM, Kroon HM, Rabelink TJ, Hoek B, Hamdy NA. Longitudinal changes in BMD and fracture risk in orthotopic liver transplant recipients not using bone‐modifying treatment. Journal of Bone & Mineral Research 2014;29(8):1763‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Malluche 2010
- Malluche HH, Monier‐Faugere M‐C, Herberth J. Bone disease after renal transplantation. Nature Reviews Nephrology 2010;6(1):32‐40. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Monier‐Faugere 2000
- Monier‐Faugere MC, Mawad H, Qi Q, Friedler RM, Malluche HH. High prevalence of low bone turnover and occurrence of osteomalacia after kidney transplantation. Journal of the American Society of Nephrology 2000;11(6):1093‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Neer 2001
- Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1‐34) on fractures and bone mineral density in postmenopausal women with osteoporosis. New England Journal of Medicine 2001;344(19):1434‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nisbeth 1999
- Nisbeth U, Lindh E, Ljunghall S, Backman U, Fellstrom B. Increased fracture rate in diabetes mellitus and females after renal transplantation. Transplantation 1999;67(9):1218‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
O'Shaunessy 2002
- O'Shaughnessy EA, Dahl DC, Smith CL, Kasiske BL. Risk factors for fractures in kidney transplantation. Transplantation 2002;74(3):362‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Orwoll 2003
- Orwoll ES, Scheele WH, Paul S, Adami S, Syversen U, Diez‐Perez A, et al. The effect of teriparatide [human parathyroid hormone (1‐34)] therapy on bone density in men with osteoporosis. Journal of Bone & Mineral Research 2003;18(1):9‐17. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pichette 1996
- Pichette V, Bonnardeaux A, Prudhomme L, Gagne M, Cardinal J, Ouimet D. Long‐term bone loss in kidney transplant recipients: a cross‐sectional and longitudinal study. American Journal of Kidney Diseases 1996;28(1):105‐14. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Raggi 2004
- Raggi P, Burke S, Chasen‐Taber S, Chertow G, Holzer H, Bommer J. Sevelamer preserves trabecular bone mineral density [abstract]. 41st Congress. European Renal Association. European Dialysis and Transplantation Association; 2004 May 15‐18; Lisbon, Portugal. 2004:103‐4. [CENTRAL: CN‐00509430]
Reid 1996
- Reid IR, Wattie DJ, Evans MC, Stapleton JP. Testosterone therapy in glucocorticoid‐treated men. Archives of Internal Medicine 1996;156(11):1173‐7. [MEDLINE: ] [PubMed] [Google Scholar]
Sambrook 1988
- Sambrook PN, Eisman JA, Champion GD, Pocock NA. Sex hormone status and osteoporosis in postmenopausal women with rheumatoid arthritis. Arthritis & Rheumatism 1988;31(8):973‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schunemann 2011a
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Schunemann 2011b
- Schünemann HJ, Oxman AD, Higgins JP, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Sprague 2004
- Sprague SM, Josephson MA. Bone disease after kidney transplantation. Seminars in Nephrology 2004;24(1):82‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Torres 2002
- Torres A, Lorenzo V, Salido E. Calcium metabolism and skeletal problems after transplantation. Journal of the American Society of Nephrology 2002;13(2):551‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vautour 2004
- Vautour LM, Melton LJ 3rd, Clarke BL, Achenbach SJ, Oberg AL, McCarthy JT. Long‐term fracture risk following renal transplantation: a population based study. Osteoporosis International 2004;15(2):160‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Veenstra 1999
- Veenstra DL, Best JH, Hornberger J, Sullivan SD, Hricik DE. Incidence and long‐term cost of steroid‐related side effects after renal transplantation. American Journal of Kidney Diseases 1999;33(5):829‐39. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Versele 2016
- Versele EB, Laecke S, Dhondt AW, Verbeke F, Vanholder R, Biesen W, et al. Bisphosphonates for preventing bone disease in kidney transplant recipients: a meta‐analysis of randomized controlled trials. Transplant International 2016;29(2):153‐64. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wang 2016
- Wang J, Yao M, Xu JH, Shu B, Wang YJ, Cui XJ. Bisphosphonates for prevention of osteopenia in kidney‐transplant recipients: a systematic review of randomized controlled trials. Osteoporosis International 2016;27(5):1683‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Weisinger 2006
- Weisinger JR, Carlini RG, Rojas E, Bellorin‐Font E. Bone disease after renal transplantation. Clinical Journal of The American Society of Nephrology: CJASN 2006;1(6):1300‐13. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wolff 2011
- Wolff M, Molnar MZ, Amaral AP, Czira ME, Rudas A, Ujszaszi A, et al. Elevated fibroblast growth factor 23 is a risk factor for kidney transplant loss and mortality. Journal of the American Society of Nephrology 2011;22(5):956‐66. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Palmer 2004
- Palmer SC, McGregor DO, Strippoli GF. Interventions for preventing bone disease in kidney transplant recipients. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD005015] [DOI] [PubMed] [Google Scholar]
Palmer 2005a
- Palmer SC, McGregor DO, Strippoli GF. Interventions for preventing bone disease in kidney transplant recipients. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD005015.pub2] [DOI] [PubMed] [Google Scholar]
Palmer 2005b
- Palmer SC, Strippoli GF, McGregor DO. Interventions for preventing bone disease in kidney transplant recipients: a systematic review of randomized controlled trials. American Journal of Kidney Diseases 2005;45(4):638‐49. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Palmer 2007
- Palmer SC, McGregor DO, Strippoli GF. Interventions for preventing bone disease in kidney transplant recipients. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD005015.pub3] [DOI] [PubMed] [Google Scholar]


