Abstract
Objectives
This scoping review aims to give a comprehensive and systematic overview of published evaluations and the potential impact of patient education interventions for children, adolescents and young adults who are living with chronic illness and/or impairment loss.
Methods
Relevant literature published between 2008 and 2018 has been comprehensively reviewed, with attention paid to variations in study, intervention and patient characteristics. Arksey and O'Malley's framework for scoping studies guided the review process, and thematic analysis was undertaken to synthesize extracted data.
Results
Of the 7214 titles identified, 69 studies were included in this scoping review. Participant‐reported benefits of the interventions included less distress from symptoms, improved medical adherence and/or less use of medication, and improved knowledge. The majority of studies measuring physical activity and/or physiologic outcomes found beneficial effects. Interventions were also beneficial in terms of decreased use of urgent health care, hospitalization, visits to general practitioner and absence from school. By sharing experiences, participants had learned from each other and attained new insight on how they could manage illness‐related challenges.
Discussion
Study results corroborate previous research suggesting that different types of patient education interventions have a positive impact on children, adolescents and young adults, but research on this field is still in a starting phase. The results summed up in the current review supports the utility of patient education interventions that employ behavioural strategies tailored to the developmental needs of children, adolescents and young adults with different cultural backgrounds.
Keywords: adolescents, children, evaluation, patient education, patient engagement, scoping review
1. INTRODUCTION
Children living with chronic illness are less able to participate in social activities. The daily management of their illness often requires that the whole family adjust to a new way of life.1 Adolescents encounter difficulties due to experiences of physical and psychosocial changes, social pressure from their peers and adolescent health‐care transition. Moreover, adolescents tend to be afraid, anxious and shameful of their illness.2
Because chronic condition in childhood is one of the major health challenges of this century, gaining skills in self‐management becomes increasingly important.3 The challenges are particular worrisome in low‐ and middle‐income countries who experience an increase in the number of young people developing long‐term conditions.4
The process where patients are enabled to become actively involved in finding out what is important to them, in making decisions about factors that affect their lives and in taking action to achieve change, is often described as patient engagement.5 More recently, the concept of patient engagement has been envisaged as an crucial factor impacting on patients’ ability to self‐manage and as an important goal for medical communication and relationships.6 Patient education is a key patient engagement intervention for supporting and enabling children, adolescents and young adults to manage their lives with illness challenges.7, 8, 9 As others have argued,10, 11 children and adolescents who are living with long‐term health conditions want to gain more knowledge about their illness and its consequences for their everyday life. Many studies also report that young people do not have sufficient knowledge of the transition from child to adult health care.10, 12
There is a great variety in how patient education interventions are being offered to children, adolescents and young people, and they are often described as complex interventions.13 They can be given to groups or to individuals alone, and they can be led by health‐care providers or laypersons.14 Group‐based patient education programme, both disease‐specific and general approaches, has been considered an important part of health promotion politics in several Western countries and as being essential for chronic illness self‐management.15, 16, 17
Describing and evaluating the content and impact of how patient education interventions can help to pave the way towards more efficient interventions. A few reviews provide evidence that patient education interventions have been beneficial for children and adolescents with asthma,2, 18, 19 diabetes,9, 20 cancer,11 physical disabilities3 or across diagnoses (general paediatric care).10, 12 However, because of the great variety in type of intervention, setting, design and outcome measure of the included studies, it is not possible to conduct comparative analysis of the results that they present. To date, no review has addressed the full range of studies that have investigated the impact of patient education interventions targeting children, adolescents and young adults. This review aims to give a comprehensive and systematic overview of published evaluations and the potential impact of patient education interventions for children, adolescents and young adults who are living with chronic illness and/or impairment loss.
More specifically, the following questions are addressed:
What are the characteristics of the studies, participants and patient education interventions targeting children, adolescents and young people who are living with chronic illness and/or impairment loss as described in the literature?
How are patient education interventions designed specifically for children, adolescents and young people evaluated?
What impact is associated with patient education interventions targeting children, adolescents and young people, as reported in the literature?
2. METHODS
This scoping review is part of a larger research project with the objective to give a comprehensive and systematic overview of published evaluations and the potential impact of patient education interventions for the following:
Adults who are participating in group‐based patient education interventions14
Family members (both adults and children) who are participating in individual or group‐based patient education interventions (in progress)
Children, adolescents and young adults who are participating in individual and group‐based patient education interventions (this scoping review)
To capture the health economic aspects, one separate scoping review on the health economic impact of patient education interventions has been conducted and published in 2018.21 These four scoping reviews on impact of patient education interventions have followed the same methodological framework22, 23, 24 and are reporting on similar research questions regarding evaluation of patient education interventions targeting different kinds of participants.
As described earlier in the two published reviews14, 21 in this project, research on the effects of patient education interventions is a relatively new field. To gain a comprehensive overview of the published literature, the research questions were best answered by including different study designs. Thus, scoping review was considered appropriate, also for the current review. Scoping reviews “aim to rapidly identify the key concepts underpinning a research area and the main sources and types of evidence available, and can be undertaken as stand‐alone projects in their own right, especially where an area is complex or has not been reviewed comprehensively before.”25 This review followed the five‐stage framework proposed by Arksey and O`Malley22 and further refined by Levac et al23, 24
The following specifications were considered relevant for this scoping review:
Population: target population includes children, adolescents or young adults between the age of 0 and 25 who are living and coping with any type of chronic illness and/or impairment loss.
Intervention: any kind of face‐to‐face patient education intervention aimed at supporting self‐management, and optimizing health and well‐being, led by health‐care professionals and/or lay participants.
Comparisons: usual care/treatment, different types of interventions or no comparisons.
Outcomes: any of a range of different types of impacts and outcomes related to social, health, psychological, health economic or behavioural aspects.
We have conducted systematic searches in the following electronic databases from 01 January 2008 to 01 February 2018: MEDLINE, EMBASE, PsychINFO, AMED, CINAHL, SweMed+, ERIC and Cochrane Library Online. The literature searches have followed the PICO principles combined with and “OR” within group and subsequently combined with an “AND” between groups. We have used a wide variety of terms in the database thesaurus in addition to free text/key word method:
Participants: children, adolescent, youth, paediatric, young people, young adults.
Intervention: self‐management programme/education/group, group support programme, learning and mastery course, patient education, patient education course/programme/intervention, patient engagement, peer support, group intervention, group‐based education/programme.
Diagnosis/health: chronic disease, chronic illness, lung diseases, asthma, pain, fatigue syndrome, irritable bowel syndrome, gastrointestinal, osteoporosis, HIV infections, arthritis, diabetes mellitus, hypertension, myocardial ischaemia, heart failure, stroke, neoplasms, fibromyalgia, mental disorders, cardiovascular disease, obesity, COPD, lung illness, cancer.
We only included studies published in English, Norwegian, Swedish or Danish in peer‐reviewed journals. The studies were required to have investigated: the impact or effects over time (a) of individual‐ and/or group‐based patient education interventions (b) for children, adolescents and/or young adults living with any type of chronic illness challenges (c). Interventions based mainly on the use of technology were excluded. A different search strategy would have been required in order to capture the full scope of such studies.
All the members of the study group were involved in the discussions of the search strategy, and our discussions helped clarify the inclusion and exclusion criteria for this review. A broad search in all the relevant databases was conducted, with no restrictions. The search of the online databases yielded 7216 articles, and 7049 of these articles were excluded because they did not meet the inclusion criteria (Figure 1). The remaining 167 articles were obtained in full text and read by the first author and one co‐author. Of these, 98 articles were excluded, because inclusion criteria were not met. There were few disagreements about article inclusion, and these were resolved by discussion in the study group to reach consensus. As is frequently seen in research on patient education interventions tailored to adult patients,14 the interventions for children, adolescents and young people were often poorly described. In addition, interventions with similar‐sounding names could be very different in content. Therefore, every intervention was screened before inclusion, and 59 were excluded because the aim or content of the patient education intervention did not meet the criteria. A final total of 69 articles were included for analysis in this review.
Figure 1.
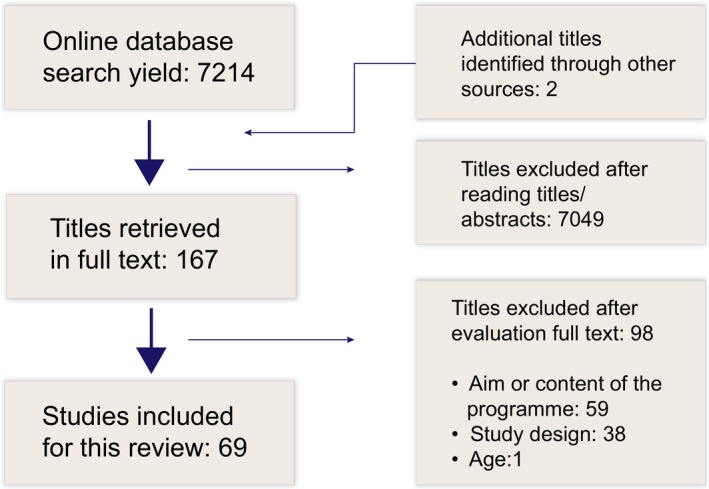
Included and excluded studies
Information about study characteristics, participant characteristics, descriptions of interventions, methods and results was collected on data extraction forms and reported separately for each study in an evidence summary Table S1 (Supporting Information).
The research included in this study showed significant variation in type of intervention, design and outcome measures. The 69 study results comprising the research material under scrutiny were compared according to the type of patient education intervention, diagnosis and type of outcome measured in order to find patterns and similarities. The data summarization was mainly done by two of the authors (US and MH) and subsequently validated by all co‐authors.
3. RESULTS
In this scoping review, 69 research‐based studies have been included. The presentation of the results is organized according to the main questions addressed in this review.
3.1. Characteristics of the studies
The studies were published between 2008 and 2018. Most of the studies (47/69) were published in 2012 or later. The 69 published studies were conducted in 26 different countries (Table 1).
Table 1.
Country and number of studies
| Country | Number of studies |
|---|---|
| United States of America | 28 |
| Australia | 7 |
| Turkey | 4 |
| United Kingdom | 3 |
| Canada | 2 |
| Norway | 2 |
| Taiwan | 2 |
| Germany | 2 |
| China | 2 |
| Jordan | 1 |
| Sweden | 1 |
| Australia/Jordan | 1 |
| Chile | 1 |
| Netherlands | 1 |
| Poland | 1 |
| Switzerland | 1 |
| Iran | 1 |
| Italy | 1 |
| Belgium | 1 |
| France | 1 |
| Mexico | 1 |
| Pakistan | 1 |
| Denmark | 1 |
| Thailand | 1 |
| Serbia | 1 |
| Brazil | 1 |
| Total | 69 |
Among the 69 research‐based studies, three of them employed qualitative designs, and two made use of mixed‐method designs. Of the quantitative studies, 43 studies were randomized controlled trials with experimental design, and 21 had an observational analytical design (cohort or case‐control studies). Fifty of the quantitative studies (50/66; 76%) compared the outcomes of patients participating in patient education interventions with those of a control group of patients or compared outcomes of participation in different patient education interventions. In most of these studies, participants in control groups received usual care and treatment. All the quantitative studies reported changes over time, before and after participating in a patient education intervention:
Before and immediately after the intervention: 4 studies
Before and 12 months after intervention: 54 studies
Before and between 1 and 2 years after intervention: 6 studies
Before and more than two years after the intervention: 2 studies
3.2. Participant characteristics
A total of 15 124 participants were included in the studies for this scoping review (Table 2). The mean age of children and adolescents was 12.1 years (17 studies did not report mean age); 31/69 studies reported ethnicity, with the mean of 46.5% white participants.
Table 2.
Study participants: gender and age
| Number of participants (%) | |
|---|---|
| Total sample | 15.124 (100%) |
| Gender | |
| Women | 7.160 (47.34%) |
| Men | 6869 (45.42%) |
| Not reported | 975 (6.45%) |
| Age | |
| Mean age, y | 12.14 |
| Range, y | 3 to 29 |
3.3. Classification of chronic condition
A breakdown of the 69 studies by chronic condition is provided in Table 3. The largest number of studies included in this review focused on asthma (30/69), followed by diabetes (15/69).
Table 3.
Diagnosis and number of studies
| Diagnosis | Number of studies |
|---|---|
| Asthma | 30 |
| Diabetes | 15 |
| Obesity | 5 |
| Mental health disorders | 4 |
| Chronic illness (various) | 4 |
| Cancer | 3 |
| Chronic fatigue syndrome | 2 |
| Pain | 1 |
| Organ transplanted | 1 |
| Oesophageal atresia | 1 |
| Autism spectrum disorder | 1 |
| Migraine | 1 |
| Total | 69 |
3.4. Characteristics of the patient education interventions
The interventions had diverse origins, aims, target groups, settings and number of modules and were delivered by different health‐care personnel and/or peers. This is described in detail in Supporting Information Table S1. The interventions in these studies were face‐to‐face patient engagement interventions aimed at helping children, adolescents, young adults and families develop coping skills and gain knowledge to manage illness, health and everyday life.
In 13 of the studies, the interventions were tailored to the participants’ developmental phase, educational level or to ensure cultural comparability. Four (5.8%) of the studies were focused on the transition from child‐ to adult‐oriented health‐care services. A majority of the interventions concerned conventional self‐management education with pathophysiology and information, medication and action planning, lifestyle guidelines, self‐care, symptom management and adherence, but mostly in addition to other components such as problem‐solving (23/69; 333%), planning (51/69; 73.9%) and practising coping skills (37/69; 53.6%). Twenty‐one of the interventions were supplemented with written or multimedia material (21/69; 30.4%) and/or entertaining materials (8/69; 11.6%), phone calls (4/69; 5.8%) or website (3/69; 4.3%).
Commonly, interventions were led by trained facilitators (28/69; 40.6%) or multidisciplinary teams (19/69; 26%). Eight interventions (8/69) were led by nurses, and seven (7/69) were delivered by a nurse and a therapist in collaboration. Other personnel reported to be involved were family health coaches (3/69), community health‐care providers (3/69), physiotherapists (2/69), clinicians (1/69), a team of general practitioners and experts in physical activity (1/69), educators and dietitians (1/69) and study team counsellors (1/69). In two cases, a health‐care team, fellow peers and school personnel were responsible for implementing the intervention (2/69). Two of the interventions were peer‐led, and three studies provided no information on which personnel delivered the interventions.
The duration of the interventions ranged from one session (12/69; 17.4%), to two to eight sessions (33/69; 47.8%), to 10 sessions or more (5/69; 7.2%). Session lasted anywhere from 15 minutes to 2.5 hours in different studies. Seven interventions lasted between two and five whole days (7/69; 10.1%). One study compared 13 cognitive behavioural therapy sessions with four psychoeducational sessions. Four studies (4/69; 5.6%) reported no information on number of sessions, but a duration from 6 to 12 months. One study provided no information about the duration of the intervention.
Interventions for individual patients comprised 35/69 (50.7%), whereas 22 included family or support persons, and five combined joint and separate sessions. Among the group‐based interventions (28/69; 40.6%), nine included family, four had separate groups for the caretakers, and one included both family and teacher. Two of the studies (2/69; 2.9%) combined groups and individual sessions, and three studies (3/69; 4.3%) did not report the mode of the intervention.
The interventions were offered in hospitals (50/69; 72.5%), schools (10/69; 14.5%) or were home‐based (9/69;13%). Seven (7/24; 10.1%) interventions were offered in general practice, community centres, university training centres and primary care. Two (2.9%) studies lacked a description of the setting in which the intervention was delivered.
3.5. Characteristics of methods for evaluation
The studies included in this review have used a wide range of different outcome measures. Outcomes concerning disease management and coping, knowledge about conditions and treatments, symptom severity, self‐efficacy, self‐management behaviours, empowerment, self‐esteem and health economy were frequently measured. The health economic evaluations were measured in terms of hospitalization, use of urgent and preventive health services and number of days absent from school/college or work. Table 4 presents all the validated outcome measures and gives references to the primary source and/or validation studies. The table also shows whether the outcome measure is typically associated with a specific diagnose or is used across diagnoses.
Table 4.
Outcome measures used in the research‐based studies included in this scoping review
| Outcome | Condition | Outcome measure |
|---|---|---|
| Disease | Asthma | Self‐Administered Nicotine Dependence Scale99 |
| management and | Asthma | Asthma Control Test (ACT)100, 101 |
| coping | Asthma | Childhood Asthma Control Questionnaire (ACQ)102 |
| Asthma | The Asthma Control Questionnaire103 | |
| Asthma | Child Asthma Control Test (CACT)104 | |
| Asthma | Asthma Inventory for Children (AIC)105 | |
| Asthma | The Asthma Belief Scale106 | |
| Cancer | Pediatric Cancer Coping Scale (PCCS)107 | |
| Diabetes | Summary of Diabetes Self‐Care Activities108 | |
| Diabetes | Issues in Coping with T1D‐Child Scale109 | |
| Across conditions | Kid Cope110 | |
| Knowledge | Asthma | Asthma Knowledge Consumer Questionnaire (CQ)111 |
| Asthma | Asthma Knowledge Test112, 113 | |
| Asthma | Questions About Asthma Questionnaire114 | |
| Autism | Autism Knowledge Quiz (AKQ)77 | |
| Diabetes | Diabetes Knowledge Test115 | |
| Self‐esteem | Across conditions | The Rosenberg Self‐Esteem Scale (RSES)116, 117 |
| Physiological | Asthma | Peak expiratory flow rate (PEF) |
| Across conditions | Waist circumference (WC) | |
| Across conditions | Hip circumference (HC) | |
| Across conditions | BMI score | |
| Health‐related quality of life | Asthma | Pediatric Asthma Quality of Life Questionnaire (PAQLQ)118 |
| Asthma | Mini Asthma Quality of Life Questionnaire (Mini‐AQLQ)119 | |
| Diabetes | Diabetes Quality of Life Scale (DQOLY‐SF)120 | |
| Across conditions | Medical Outcomes Survey‐Short form (SF‐36)121 | |
| Across conditions | EuroQol Questionnaire (EQ‐5D)122 | |
| Across conditions | Health‐related Quality of Life (DISABKIDS)123 | |
| Across conditions | Quality of Life Questionnaire (DUCATQOL/DUX‐25)124 | |
| Across conditions | The Pediatric Quality of Life Inventory (PedsQL)125 | |
| Across conditions | EUROHIS QOL‐8126 | |
| Psychosocial | Diabetes | Diabetes Family Responsibility Questionnaire (DFRQ)127 |
| Diabetes | Diabetes Family Conflict Scale (DFCS)128 | |
| Across conditions | Communal Family Mastery Scale129 | |
| Across conditions | Transition Readiness Assessment Questionnaire (TRAQ)130 | |
| Across conditions | Perceived Stress Scale131 | |
| Across conditions | Strengths and Difficulties Questionnaire (SDQ)132 | |
| Across conditions | University of California Los Angeles Loneliness Scale (UCLA)133 | |
| Health economics | Across conditions | Quality Adjusted Life‐Years (QALYs)134 |
| Across conditions | The Health Utilities Index Mark 2 (HUI‐2)135 | |
| Across conditions | The Child Health Utility 9D (CHU9D)136 | |
| Across conditions | Number of hospital days | |
| Across conditions | Number of re‐hospitalizations | |
| Across conditions | Number of Emergency Department visits | |
| Across conditions | Number of sick days | |
| Across conditions | Number of doctor visits | |
| Across conditions | Number of preventive visits | |
| Across conditions | Number of urgent care visits | |
| Across conditions | Number of missed schooldays | |
| Self‐efficacy/empowerment | Asthma | Asthmatic Child and Adolescent Self‐Efficacy Scale (ACASES)137 |
| Asthma | Child Asthma Self‐Efficacy Questionnaire138 | |
| Diabetes | Self‐Efficacy for Diabetes Scale139 | |
| Diabetes | Diabetes Empowerment Scale‐Short Form140 | |
| Across conditions | General Perceived Self‐Efficacy Scale (GSE)141 | |
| Impact of illness/symptom | Asthma | Number of asthma symptom free days |
| Diabetes | The Diabetes Behavior Rating Scale142 | |
| Across conditions | Hamilton Depression Rating Scale (HDRS)143 | |
| Across conditions | Children's Depression Inventory (CDI)144 | |
| Across conditions | Young Mania Rating Scale (YMRS)145 | |
| Across conditions | Chalder Fatigue Questionnaire82 | |
| Across conditions | Pittsburgh Sleep Quality Index (PSQI)146 | |
| Across conditions | Modified Yale Preoperative Anxiety Scale (m‐YPAS)147 | |
| Across conditions | Beck Depression Inventory (BDI)90 | |
| Across conditions | Depression Anxiety Stress Scale—short version (DASS‐21)148 | |
| Across conditions | Centers for Epidemiologic Studies Depression Scale (CES‐D)149, 150 | |
| Across conditions | Patient Health Questionnaire151 | |
| Self‐Management | Across conditions | Work and Social Adjustment Scale152 |
| Across conditions | Patient Activation Measure (PAM)153 | |
| Global improvement and satisfaction | Across conditions | Global Assessment of Functioning (GAF)154 |
| Across conditions | Health of Our Nation Outcome Scale (HoNOS)155 | |
| Across conditions | Number of sessions attended | |
| Across conditions | Satisfaction With Life Scale156 | |
| Across conditions | Arizona Integrative Outcomes Scale‐24 and Arizona Integrative Outcomes Scale‐30157 | |
| Physical activity/nutrition | Across conditions | Self‐reported physical activity levels (IPAQ‐SF)158 |
| Across conditions | Physical Activity Scale (PAS)159 | |
| Across conditions | Block Food Frequency Questionnaire (FFQ)160 | |
| Medication Adherence | Across conditions | Medication Adherence Rating Scale (MARS)161 |
| Mindfulness | Across conditions | Avoidance and Fusion Questionnaire for Youth (AFQ‐Y8 short version)162 |
| Children's Acceptance and Mindfulness Measure (CAMM short version)163 | ||
| Resiliency | Across conditions | Resiliency Scales for Children and Adolescents (RSCA)164 |
3.6. Psychosocial outcomes
One or several psychosocial outcomes had been investigated in most of the studies. Symptom management, medical adherence and/or medication use, health‐related quality of life and knowledge were frequently measured. Management or frequency of symptoms was examined in 44 studies. Four of the studies that had investigated symptom frequency found no differences,26, 27, 28, 29 and 25 studies reported reduction of symptoms and/or awareness of symptom triggers.30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54 Ten studies from interventions tailored to children and adolescents with asthma reported improved asthma control 51, 55, 56, 57, 58, 59, 60 and decreased number of asthma exacerbations. 38, 55, 56, 61, 62 One study found no changes in asthma control.57
All the studies that had investigated medical adherence and/or use of medication reported better adherence to medications31, 32, 38, 55, 63, 64, 65 and/or decreased need for use of medication.53, 55, 65, 66, 67, 68 Health‐related quality of life was measured in 23 studies. From these, eleven did not find any significant differences between the intervention group and the control group,26, 27, 29, 57, 63, 68, 69, 70, 71, 72, 73 while 12 studies found significant effects or improvements in intervention groups over time.40, 42, 52, 53, 55, 59, 60, 66, 74, 75, 76
Knowledge was investigated in 10 studies.41, 49, 52, 57, 58, 65, 69, 74, 77, 78, 79 All these studies reported significant improvements in knowledge scores after intervention. Eight studies had investigated changes in self‐efficacy. Three of these found significantly greater self‐efficacy in intervention participants38, 74, 75; in addition, two studies found improvements, albeit not significant,52, 58 and three studies found no effects on self‐efficacy.39, 76, 80 Whereas self‐efficacy describes persons’ belief in their capacity to arrange and carry out a course of action,81 empowerment is a consequence of achieving self‐efficacy. Only one study had empowerment as one of several outcome measures, and this study found no changes in empowerment.49
Four studies measured strengths and difficulties by using a behavioural screening tool for psychopathology and adaptation. One study found that, when compared to the control group, participants in the intervention group became more aware of their strengths as well as the difficulties connected to their diagnosis.77 One study was unfortunately underpowered and found no differences.73 One of the two studies that compared cognitive behavioural therapy‐based intervention with psycho‐education failed to find significant differences between the groups.82 The second study, however, found significant changes in the cognitive behavioural therapy group controlled for baseline scores.44
Self‐esteem was investigated in three studies. Two of these studies found increased self‐esteem after participation in group programmes for adolescents with type 1 diabetes78 or mental health challenges.83 However, the third study, investigating a one‐on‐one intervention for young people diagnosed with psychosis, did not detect statistically significant changes.35 Two studies had measured the level of patient engagement in their health. The interventions investigated in these studies did not affect activation over time.69, 72 One study had measured differences in social support and found that intervention participants gained significantly more social support when compared to participants receiving ordinary care.78 One study investigated mindfulness changes and found significant higher mindfulness scores among adolescents in the intervention group compared to those in the control group.83
3.7. Physical activity and physiologic outcomes
A variety of physical activity and physiologic outcomes were measured in 23 studies. Of these, 19 studies found improvements, 29, 30, 33, 35, 39, 41, 43, 49, 55, 71, 75, 78, 84, 85, 86, 87 and four studies found no changes.63, 70, 76, 88 Differences in blood glucose control were measured in 15 studies. Of these, four studies found no differences,63, 70, 76, 88 while 11 studies found improvements in glycaemic control.29, 39, 41, 43, 49, 50, 78, 84, 86, 87, 89 Improvements in physical activity or greater adherence to behavioural support were reported in all studies that had measured physical activity.33, 35, 44, 71, 75, 90 Nine studies had measured body mass index (BMI) scores. Of these, eight found greater reductions in BMI in the intervention group than controls.30, 35, 41, 43, 46, 50, 84, 85 One study found no impact on BMI.76
3.8. Health‐care utilization
Of the studies dealing with patient education interventions, 14/17 studies resulted in beneficial effects as measured by one or several health economic outcomes.31, 33, 38, 42, 45, 49, 53, 55, 56, 59, 61, 64, 66, 68 Three studies found no health economic impact or effects of the interventions.62, 91, 92 Use of urgent health care or the frequency of emergency visits, visits to the local doctor and hospitalization, and missed schooldays were frequently investigated in these studies. Use of urgent health care was investigated in 13 studies, and 11 of these found significantly decreased use of urgent health care or trends towards beneficial effects,31, 33, 38, 42, 45, 49, 55, 59, 64, 68 while two studies found no effects.91, 92 Of the six studies that had measured hospitalization, three found beneficial effects,31, 45, 61 while three found no effects.53, 56, 92 Six studies found beneficial effects: two in terms of fewer visits to general practitioners59, 66 and four in terms of less absence from school.38, 56, 66, 68 Apart from one study involving children with diabetes,49 all the patient education interventions in the studies that had investigated health‐care utilization were targeting children and adolescents with asthma.
3.9. Perceptions of participation—results from qualitative studies
The five studies with a qualitative approach had explored how children and adolescents who were living with diabetes, asthma, stress‐related problems or cancer experienced participating in patient education interventions.1, 40, 54, 93, 94 Overall, the studies showed that by sharing experiences, participants had learned from each other and attained new insight. They also learned through interaction with educational material and from health‐care personnel. Adolescents in one study described that the most challenging part was deciding to sign up for the course because it required them to admit to themselves that they needed the course.94 The studies showed that sharing experiences with peers spurred meaningful learning experiences and an empowering process. Children and adolescents found it easier to talk about their diseases and to share their thoughts and feelings about living with health challenges with family members and others after participating in patient education interventions.1, 54, 93, 94 In general, children and adolescents experienced alleviation, comfort and a feeling of hope when realizing that there are others struggling with the same issues.1, 94
And that’s what it’s about, meeting in a group: where everyone has the same problem, then everybody dares to raise issues. That’s really great. Nobody judges anybody, no way. 94 p. 8
Another important result from these five studies was that participants gained insight and concrete knowledge about the disease, its symptoms and potential causes, and how they could manage all the daily illness‐related challenges. For example, they learned how to manage symptoms and to be more aware of triggers and stress responses, how to take medication and cope with side‐effects, or other difficult situations and problems. Adolescents taking part in a stress management course found it useful to learn and understand how physical discomfort is highly related to stress in daily life.94 Participants in all five studies had learned concrete problem‐solving skills. How these skills and knowledge could be used in everyday life and activities was verbalized in the groups. Despite the perceived benefits of participating, after completing the courses some found it hard to remember what they learned, making it difficult to sustain a change in behaviour over a long period of time. These participants suggested including re‐education as an additional component in forthcoming courses, also because certain topics would become more significant when they got older.93
4. DISCUSSION
4.1. Summary of main findings
This scoping review is based on 69 studies published between 2008 and 2018. The major amount of the included studies was conducted in North America, Australia and Europe and had an experimental or observational analytical design and reported changes over the first year after intervention. Only eight studies had evaluated changes after more than one year after intervention. A total of 15 124 children, adolescents and young adults were included as participants in these studies, approximately equal numbers of males and females, with a mean age of 12.1 years. Most of the interventions were diagnosis‐specific (the main diagnoses are asthma, diabetes, obesity and cancer), and only four interventions included participants across different diagnoses.
As described by Lorig and Holman (2003),8 patient education aims to enable patients to understand the process of their illness, to acquire knowledge and skills to manage medical and disease challenges, to adjust treatment of their condition and to maintain quality of life. The patient education interventions in this review, both individual and group‐based, were aimed at helping children, adolescents, young adults and families develop coping skills and gain knowledge to manage illness, health and everyday life. The interventions were led by trained facilitators and multidisciplinary teams and were offered in hospitals and schools.
Participants considered the interventions beneficial, reporting less symptom distress, improved medical adherence and/or less use of medication, and improved knowledge. Several studies employed health‐related quality‐of‐life measurements, but only 12/23 studies found significant effects or improvements. The qualitative studies showed that by sharing experiences, children and young people learned from each other and created new insight, for example knowledge about disease, symptoms and potential causes, and how they could manage all the daily illness‐related challenges. Physical activity and physiologic outcomes were investigated in 24 studies, and 20 of these found beneficial effects on blood glucose control, physical activity and BMI scores.
In this review, 14/17 studies found that participation in patient education interventions was beneficial in terms of decreased use of urgent health care, hospitalization, visits to general practitioner and fewer missed days from school. No studies documented that participation in patient education interventions had any unintended negative effects on children, adolescents or young adults.
4.2. Strengths and limitations
This study shares the limitations that are inherent to scoping reviews in general.14, 21 Balancing breadth and depth of analysis is challenging, and a further complication lies in synthesizing studies with different designs and methods in the same review.95, 96 The motivation for doing this scoping review was to provide insight into systematic evaluations of patient education interventions in health care for children, adolescents and young adults who are coping with long‐term illness challenges. Our aim was to get an overview and capture the whole breadth of studies that had evaluated these types of interventions. Therefore, none of the studies have been excluded on the basis of methodological characteristics. In line with scoping review recommendations,97, 98 we have not performed assessments of methodological limitations of the studies. The purpose of scoping reviews is to give an overview of the literature on a certain topic and normally to not include evaluations of methodological weaknesses or risk of bias.
In this review, we have included studies on patient education interventions for children, adolescents and young adults with any type of long‐term illness challenges. We wanted to capture as many relevant studies as possible; therefore, we used a large number of synonyms in our searches in the databases. Nonetheless, the list of search terms was neither complete nor exhaustive. Since we had a broad definition of patient education interventions, we could include a wide range of interventions. Similar to our earlier reviews on patient education,13, 20 the interventions in this review also varied in terms of setting, theoretical basis, target groups, modules, duration and personnel/lay participants. In addition, the components of “ordinary care” or “waitlist controls” were often not described.
Chronic illness in children affects daily functioning in the whole family. Some of the interventions in the included studies involved parents, but parental outcomes are not included in this review. Another limitation we also found in our previous reviews on patient education14, 21 is the lack of information about the relationship between demographic characteristics and reported outcomes. Since the largest share of these studies has been conducted in USA and Australia, much of what we know is based on people with Western ethnicity. We are fully aware that the success of any patient education intervention in general is likely to be determined by local factors and situations, which are often difficult to model and replicate. Therefore, the general transferability of the results from the included studies in this scoping review and applicability to clinical practice has not been specifically analysed.
It is important to be aware of that the proportion of the included studies reporting significant effects of patient education interventions may be inflated due to publication bias. Finally, since this scoping review aimed to give breadth and comprehensiveness, it was necessary to compromise and reduce the depth of analysis and validity assessment.
4.3. How and why it agrees or disagrees with the existing literature
Results from earlier reviews are supported by the results from this study and indicate that patient education interventions have positive effects, reducing the frequency of hospitalizations and emergency visits,18 improving self‐management of chronic illness, the self‐efficacy of young people with long‐term conditions and the quality of life2, 19 of children with asthma. One review of the structured, more behaviourally focused programmes for youths with diabetes demonstrate beneficial results on young people's ability to manage their emotions, level of parent–adolescent conflict, adherence to medical treatment and sometimes metabolic control.9 Two reviews suggest that interventions facilitate a better transfer from paediatric to adult health care.10, 12 Nevertheless, due to the great variety in interventions and inclusion criteria, a comparison of the results presented in the reviews is not possible. To the best of our knowledge, no previous review has included and summed up such a broad scope of studies, including evaluations of benefits from patient education interventions for children, adolescents and young adults up to the age of 25 years, and of the challenges associated with these interventions.
4.4. Recommendations for future research
Although progress has been made in understanding the effects that can be achieved from patient education intervention for children, adolescents and young adults, much is yet to be learned. We need more knowledge on the effect of participation over time, how the need for knowledge and education changes at different phases of psychosocial development and illness trajectories, and how patient education interventions can best be tailored to children, adolescents and families with different learning styles and cultural backgrounds. To date, most of the research studies are from interventions for participants with asthma or diabetes. Future studies are recommended on interventions across diagnoses and from a wider range of diagnoses. The authors in several of the included studies highlight that the samples represent a relatively narrow range of socioeconomic status and cultural backgrounds. Thus, future research can benefit from exploring the sustained impact of patient education interventions for children, adolescents and young adults living in a different cultural, ethnic or socioeconomic environment. They should also include psychosocial adjustment and family functioning as intermediate variables.
This review highlights the need for a comprehensive approach in evaluating patient education interventions tailored to children, adolescents and young adults. As is evident from Table 4, the ways of measuring outcomes differ greatly. We need more knowledge about how we can evaluate impact, both for outcomes with standardized measurements, and on how we can evaluate process and subjective experiences from participating in patient education interventions. More consistent use of standardized measurements would also facilitate comparing interventions internationally.
There is a paucity of research on psychological and emotional experiences of children, adolescents and young adults becoming more actively involved in improving their own health. Based on the results from this review, we need more insight into the psychosocial and subjective experience for children, adolescents and young adults, and more knowledge about factors that may sustain or hinder engagement.
4.5. Implications for practice
The findings from the present scoping review give important input to political decision makers and health administrators. Most importantly, patient education interventions targeting children, adolescents and young adults can reduce the cost of care and improve the levels of physical activity, BMI and blood glucose control. Moreover, the participants experience beneficial effects owing to less symptom distress and improved knowledge.
This review supports the utility of patient education interventions that employ behavioural strategies tailored to the developmental needs of children, adolescents and young adults with different cultural backgrounds. Such interventions should be made available to a broader range of children, adolescents and young adults who are living with health challenges.
CONFLICT OF INTEREST
There are no financial or other ties involved in the present work that might lead to a conflict of interest.
Supporting information
ACKNOWLEDGEMENTS
Thanks to Camilla Lyngen for useful input in the planning of this study and to Janet Holmén for language editing. We would also like to thank all our colleagues for their support in this work, with special thanks to Siw‐Anita Bratli, Ann Britt Sandvin Olsson, Ann‐Helen Henriksen, Kari Hvinden, Cecilia Sønstebø, Siw Merete Paulsen and Hilde Blindheim Børve.
Stenberg U, Haaland‐Øverby M, Koricho AT, et al. How can we support children, adolescents and young adults in managing chronic health challenges? A scoping review on the effects of patient education interventions. Health Expect. 2019;22:849–862. 10.1111/hex.12906
Funding information
This work was funded by the Norwegian National Advisory Unit on Learning and Mastery in Health, Oslo University Hospital, Norway.
REFERENCES
- 1. Trollvik A, Ringsberg KC, Silen C. Children's experiences of a participation approach to asthma education. J Clin Nurs. 2013;22(7–8):996‐1004. [DOI] [PubMed] [Google Scholar]
- 2. Zhong SC, Melendez‐Torres GJ. The effect of peer‐led self‐management education programmes for adolescents: a systematic review and meta‐analysis. Health Educ J. 2017;76(6):676‐694. [Google Scholar]
- 3. Lindsay S, Kingsnorth S, McDougall C, Keating H. A systematic review of self‐management interventions for children and youth with physical disabilities. Disabil Rehabil. 2014;36(4):276‐288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. The L. Type 2 diabetes: the urgent need to protect young people. Lancet. 2018;392(10162):2325. [DOI] [PubMed] [Google Scholar]
- 5. Organization WHO . Patient Engagement: Technical Series on Safer Primary Care . 2016.
- 6. Graffigna G, Barello S. Spotlight on the Patient Health Engagement model (PHE model): a psychosocial theory to understand people's meaningful engagement in their own health care. Patient Prefer Adherence. 2018;12:1261‐1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Finset A. Patient participation, engagement and activation: increased emphasis on the role of patients in healthcare. Patient Educ Couns. 2017;100(7):1245‐1246. [DOI] [PubMed] [Google Scholar]
- 8. Lorig KR, Holman HR. Self‐management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1‐7. [DOI] [PubMed] [Google Scholar]
- 9. Plante AW, Lobato JD. Psychosocial group intervention for children and adolescents with type 1 diabetes: the state of the literature. Child Health Care. 2008;37(2):93‐111. [Google Scholar]
- 10. Morsa M, Gagnayre R, Deccache C, Lombrail P. Factors influencing the transition from pediatric to adult care: a scoping review of the literature to conceptualize a relevant education program. Patient Educ Couns. 2017;100(10):1796‐1806. [DOI] [PubMed] [Google Scholar]
- 11. Thompson AL, Young‐Saleme TK. Anticipatory guidance and psychoeducation as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62(Suppl 5):S684‐693. [DOI] [PubMed] [Google Scholar]
- 12. Campbell F, Biggs K, Aldiss SK, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev . 2016;4:CD009794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Steinsbekk A, Rygg LO, Lisulo M, Rise MB, Fretheim A. Group based diabetes self‐management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta‐analysis. BMC Health Serv Res. 2012;12:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stenberg U, Haaland‐Overby M, Fredriksen K, Westermann KF, Kvisvik T. A scoping review of the literature on benefits and challenges of participating in patient education programs aimed at promoting self‐management for people living with chronic illness. Patient Educ Couns. 2016;99:1759‐1771. [DOI] [PubMed] [Google Scholar]
- 15. Kristiansen TM, Antoft R. Patient education as a status passage in life – an ethnographic study exploring participation in a Danish group based patient education programme. Soc Sci Med. 2016;158:34‐42. [DOI] [PubMed] [Google Scholar]
- 16. Rogers A, Vassilev I, Sanders C, et al. Social networks, work and network‐based resources for the management of long‐term conditions: a framework and study protocol for developing self‐care support. Implement Sci. 2011;6:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taylor D, Bury M. Chronic illness, expert patients and care transition. Sociol Health Illn. 2007;29(1):27‐45. [DOI] [PubMed] [Google Scholar]
- 18. Coffman JM, Cabana MD, Halpin HA, Yelin EH. Effects of asthma education on children's use of acute care services: a meta‐analysis. Pediatrics. 2008;121(3):575‐586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Srof B, Taboas P, Velsor‐Friedrich B. Adolescent asthma education programs for teens: review and summary. J Pediatr Health Care. 2012;26(6):418‐426. [DOI] [PubMed] [Google Scholar]
- 20. Charalampopoulos D, Hesketh KR, Amin R, Paes VM, Viner RM, Stephenson T. Psycho‐educational interventions for children and young people with Type 1 Diabetes in the UK: How effective are they? A systematic review and meta‐analysis. PLoS ONE. 2017;12(6):e0179685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stenberg U, Vagan A, Flink M, et al. Health economic evaluations of patient education interventions a scoping review of the literature. Patient Educ Couns. 2018;101(6):1006‐1035. [DOI] [PubMed] [Google Scholar]
- 22. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:13. [Google Scholar]
- 23. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mays N, Roberts E, Popay J. Synthesising research evidence In: Fulop N, Allen P, Clarke A, Black N, eds. Studies the Organisation and Delivery of Health Services: Research Methods. London: Routledge; 2001:188‐220. [Google Scholar]
- 25. Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy‐making in the health field. J Health Serv Res Policy. 2005;10(Suppl 1):6‐20. [DOI] [PubMed] [Google Scholar]
- 26. Cardoso Tde A, Farias Cde A, Mondin TC, et al. Brief psychoeducation for bipolar disorder: impact on quality of life in young adults in a 6‐month follow‐up of a randomized controlled trial. Psychiatry Res. 2014;220(3):896‐902. [DOI] [PubMed] [Google Scholar]
- 27. Chalder T, Deary V, Husain K, Walwyn R. Family‐focused cognitive behaviour therapy versus psycho‐education for chronic fatigue syndrome in 11‐ to 18‐year‐olds: a randomized controlled treatment trial. Psychol Med. 2010;40(8):1269‐1279. [DOI] [PubMed] [Google Scholar]
- 28. Clark NM, Shah S, Dodge JA, Thomas LJ, Andridge RR, Little RJ. An evaluation of asthma interventions for preteen students. J Sch Health. 2010;80(2):80‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang YC, Stewart SM, Mackenzie M, Nakonezny PA, Edwards D, White PC. A randomized controlled trial comparing motivational interviewing in education to structured diabetes education in teens with type 1 diabetes. Diabetes Care. 2010;33(8):1741‐1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bean MK, Powell P, Quinoy A, Ingersoll K, Wickham EP 3rd, Mazzeo SE. Motivational interviewing targeting diet and physical activity improves adherence to paediatric obesity treatment: results from the MI Values randomized controlled trial. Pediatr Obes. 2015;10(2):118‐125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bryant‐Stephens T, Li Y. Outcomes of a home‐based environmental remediation for urban children with asthma. J Natl Med Assoc. 2008;100(3):306‐316. [DOI] [PubMed] [Google Scholar]
- 32. Burkhart PV, Rayens MK, Oakley MG, Abshire DA, Zhang M. Testing an intervention to promote children's adherence to asthma self‐management. J Nurs Scholarsh. 2007;39(2):133‐140. [DOI] [PubMed] [Google Scholar]
- 33. Campbell JD, Brooks M, Hosokawa P, Robinson J, Song L, Krieger J. Community health worker home visits for medicaid‐enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105(11):2366‐2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chiang LC, Ma WF, Huang JL, Tseng LF, Hsueh KC. Effect of relaxation‐breathing training on anxiety and asthma signs/symptoms of children with moderate‐to‐severe asthma: a randomized controlled trial. Int J Nurs Stud. 2009;46(8):1061‐1070. [DOI] [PubMed] [Google Scholar]
- 35. Curtis J, Watkins A, Rosenbaum S, et al. Evaluating an individualized lifestyle and life skills intervention to prevent antipsychotic‐induced weight gain in first‐episode psychosis. Early Interv Psychiatry. 2016;10(3):267‐276. [DOI] [PubMed] [Google Scholar]
- 36. Fincher W, Shaw J, Ramelet AS. The effectiveness of a standardised preoperative preparation in reducing child and parent anxiety: a single‐blind randomised controlled trial. J Clin Nurs. 2012;21(7–8):946‐955. [DOI] [PubMed] [Google Scholar]
- 37. Garvik M, Idsoe T, Bru E. Effectiveness study of a CBT‐based adolescent coping with depression course. Emot Behav Diffic. 2014;19(2):195‐209. [Google Scholar]
- 38. Guner UC, Celebioglu A. Impact of symptom management training among asthmatic children and adolescents of self‐efficacy and disease course. J Asthma. 2015;52(8):858‐865. [DOI] [PubMed] [Google Scholar]
- 39. Holmes CS, Chen R, Mackey E, Grey M, Streisand R. Randomized clinical trial of clinic‐integrated, low‐intensity treatment to prevent deterioration of disease care in adolescents with type 1 diabetes. Diabetes Care. 2014;37(6):1535‐1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Janssens T, Harver A. Effects of symptom perception interventions on trigger identification and quality of life in children with asthma. Pulm Med. 2015;2015:825137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kenney A, Chambers RA, Rosenstock S, et al. The impact of a home‐based diabetes prevention and management program on high‐risk American Indian youth. Diabetes Educ. 2016;42(5):585‐595. [DOI] [PubMed] [Google Scholar]
- 42. Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self‐management support comparing clinic‐based nurses and in‐home community health workers: the Seattle‐King County Healthy Homes II Project. Arch Pediatr Adolesc Med. 2009;163(2):141‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Laguna‐Alcaraz AD, Mejia‐Rodriguez O, Rendon‐Paredes AL, Villa‐Barajas R, Paniagua R. Impact of a comprehensive intervention to families with teenage sons with overweight and obesity in a primary care setting: a case report. Diabetes Metab Syndr. 2017;11(Suppl 1):S195‐S200. [DOI] [PubMed] [Google Scholar]
- 44. Lloyd S, Chalder T, Rimes KA. Family‐focused cognitive behaviour therapy versus psycho‐education for adolescents with chronic fatigue syndrome: long‐term follow‐up of an RCT. Behav Res Ther. 2012;50(11):719‐725. [DOI] [PubMed] [Google Scholar]
- 45. Magzamen S, Patel B, Davis A, Edelstein J, Tager IB. Kickin' Asthma: school‐based asthma education in an urban community. J Sch Health. 2008;78(12):655‐665. [DOI] [PubMed] [Google Scholar]
- 46. Melnyk BM, Jacobson D, Kelly SA, et al. Twelve‐Month Effects of the COPE Healthy Lifestyles TEEN Program on overweight and depressive symptoms in high school adolescents. J Sch Health. 2015;85(12):861‐870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ng SM, Li AM, Lou VW, Tso IF, Wan PY, Chan DF. Incorporating family therapy into asthma group intervention: a randomized waitlist‐controlled trial. Fam Process. 2008;47(1):115‐130. [DOI] [PubMed] [Google Scholar]
- 48. Powers SW, Kashikar‐Zuck SM, Allen JR, et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents: a randomized clinical trial. JAMA. 2013;310(24):2622‐2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pyatak EA, Sequeira PA, Vigen CL, et al. Clinical and psychosocial outcomes of a structured transition program among young adults with type 1 diabetes. J Adolesc Health. 2017;60(2):212‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Santiprabhob J, Leewanun C, Limprayoon K, et al. Outcomes of group‐based treatment program with parental involvement for the management of childhood and adolescent obesity. Patient Educ Couns. 2014;97(1):67‐74. [DOI] [PubMed] [Google Scholar]
- 51. Turkeli A, Yilmaz O, Yuksel H. Metered dose inhaler‐spacer use education effects on achieve asthma control in children. Tuberk Toraks. 2016;64(2):105‐111. [DOI] [PubMed] [Google Scholar]
- 52. Velsor‐Friedrich B, Militello LK, Richards MH, et al. Effects of coping‐skills training in low‐income urban African‐American adolescents with asthma. J Asthma. 2012;49(4):372‐379. [DOI] [PubMed] [Google Scholar]
- 53. Watson WT, Gillespie C, Thomas N, et al. Small‐group, interactive education and the effect on asthma control by children and their families. CMAJ. 2009;181(5):257‐263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wu LM, Chiou SS, Sheen JM, et al. Evaluating the acceptability and efficacy of a psycho‐educational intervention for coping and symptom management by children with cancer: a randomized controlled study. J Adv Nurs. 2014;70(7):1653‐1662. [DOI] [PubMed] [Google Scholar]
- 55. Almomani BA, Mayyas RK, Ekteish FA, Ayoub AM, Ababneh MA, Alzoubi SA. The effectiveness of clinical pharmacist's intervention in improving asthma care in children and adolescents: randomized controlled study in Jordan. Patient Educ Couns. 2017;100(4):728‐735. [DOI] [PubMed] [Google Scholar]
- 56. Arikan‐Ayyildiz Z, Isik S, Caglayan‐Sozmen S, Anal O, Karaman O, Uzuner N. Efficacy of asthma education program on asthma control in children with uncontrolled asthma. Turk J Pediatr. 2016;58(4):383‐388. [DOI] [PubMed] [Google Scholar]
- 57. Bowen F. Asthma education and health outcomes of children aged 8 to 12 years. Clin Nurs Res. 2013;22(2):172‐185. [DOI] [PubMed] [Google Scholar]
- 58. Horner SD, Fouladi RT. Improvement of rural children's asthma self‐management by lay health educators. J Sch Health. 2008;78(9):506‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Larson A, Ward J, Ross L, Whyatt D, Weatherston M, Landau L. Impact of structured education and self management on rural asthma outcomes. Aust Fam Physician. 2010;39(3):141‐144. [PubMed] [Google Scholar]
- 60. McGhan SL, Wong E, Sharpe HM, et al. A children's asthma education program: Roaring Adventures of Puff (RAP), improves quality of life. Can Respir J. 2010;17(2):67‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Espinoza‐Palma T, Zamorano A, Arancibia F, et al. Effectiveness of asthma education with and without a self‐management plan in hospitalized children. J Asthma. 2009;46(9):906‐910. [DOI] [PubMed] [Google Scholar]
- 62. Indinnimeo L, Bonci E, Capra L, et al. Clinical effects of a Long‐term Educational Program for children with asthma – Aironet. A 1‐yr randomized controlled trial. Pediatr Allergy Immunol. 2009;20(7):654‐659. [DOI] [PubMed] [Google Scholar]
- 63. Murphy HR, Wadham C, Hassler‐Hurst J, et al. Randomized trial of a diabetes self‐management education and family teamwork intervention in adolescents with Type 1 diabetes. Diabet Med. 2012;29(8):e249‐254. [DOI] [PubMed] [Google Scholar]
- 64. Otsuki M, Eakin MN, Rand CS, et al. Adherence feedback to improve asthma outcomes among inner‐city children: a randomized trial. Pediatrics. 2009;124(6):1513‐1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zivkovic Z, Radic S, Cerovic S, Vukasinovic Z. Asthma School Program in children and their parents. World J Pediatr. 2008;4(4):267‐273. [DOI] [PubMed] [Google Scholar]
- 66. Flapper BC, Duiverman EJ, Gerritsen J, Postema K, van der Schans CP. Happiness to be gained in paediatric asthma care. Eur Respir J. 2008;32(6):1555‐1562. [DOI] [PubMed] [Google Scholar]
- 67. Haeberli S, Grotzer MA, Niggli FK, et al. A psychoeducational intervention reduces the need for anesthesia during radiotherapy for young childhood cancer patients. Radiat Oncol. 2008;3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Julian V, Amat F, Petit I, et al. Impact of a short early therapeutic education program on the quality of life of asthmatic children and their families. Pediatr Pulmonol. 2014;50:213‐221. [DOI] [PubMed] [Google Scholar]
- 69. Dingemann J, Szczepanski R, Ernst G, et al. Transition of patients with esophageal atresia to adult care: results of a transition‐specific education program. Eur J Pediatr Surg. 2017;27(1):61‐67. [DOI] [PubMed] [Google Scholar]
- 70. Katz ML, Volkening LK, Butler DA, Anderson BJ, Laffel LM. Family‐based psychoeducation and Care Ambassador intervention to improve glycemic control in youth with type 1 diabetes: a randomized trial. Pediatr Diabetes. 2014;15(2):142‐150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Rathleff MS, Roos EM, Olesen JL, Rasmussen S. Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med. 2015;49(6):406‐412. [DOI] [PubMed] [Google Scholar]
- 72. Schmidt S, Herrmann‐Garitz C, Bomba F, Thyen U. A multicenter prospective quasi‐experimental study on the impact of a transition‐oriented generic patient education program on health service participation and quality of life in adolescents and young adults. Patient Educ Couns. 2016;99(3):421‐428. [DOI] [PubMed] [Google Scholar]
- 73. van Bragt S, van den Bemt L, Kievits R, Merkus P, van Weel C, Schermer T. PELICAN: a cluster‐randomized controlled trial in Dutch general practices to assess a self‐management support intervention based on individual goals for children with asthma. J Asthma. 2015;52(2):211‐219. [DOI] [PubMed] [Google Scholar]
- 74. Al‐sheyab N, Gallagher R, Crisp J, Shah S. Peer‐led education for adolescents with asthma in Jordan: a cluster‐randomized controlled trial. Pediatrics. 2012;129(1):e106‐112. [DOI] [PubMed] [Google Scholar]
- 75. Li HC, Chung OK, Ho KY, Chiu SY, Lopez V. Effectiveness of an integrated adventure‐based training and health education program in promoting regular physical activity among childhood cancer survivors. Psychooncology. 2013;22(11):2601‐2610. [DOI] [PubMed] [Google Scholar]
- 76. Price KJ, Knowles JA, Fox M, et al. Effectiveness of the Kids in Control of Food (KICk‐OFF) structured education course for 11–16 year olds with type 1 diabetes. Diabet Med. 2016;33(2):192‐203. [DOI] [PubMed] [Google Scholar]
- 77. Gordon K, Murin M, Baykaner O, et al. A randomised controlled trial of PEGASUS, a psychoeducational programme for young people with high‐functioning autism spectrum disorder. J Child Psychol Psychiatry. 2015;56(4):468‐476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Altundag S, Bayat M. Peer interaction and group education for adaptation to disease in adolescents with type 1 diabetes mellitus. Pak J Med Sci. 2016;32(4):1010‐1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Coughlin CC, Perez M, Kumar MG, Jeffe DB, Bayliss SJ, Sternhell‐Blackwell K. Skin cancer risk education in pediatric solid organ transplant patients: an evaluation of knowledge, behavior, and perceptions over time. Pediatr Transplant. 2017;21(2):e12817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Grey M, Whittemore R, Jaser S, et al. Effects of coping skills training in school‐age children with type 1 diabetes. Res Nurs Health. 2009;32(4):405‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Bandura A. Self‐efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191‐215. [DOI] [PubMed] [Google Scholar]
- 82. Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147‐153. [DOI] [PubMed] [Google Scholar]
- 83. Tan L, Martin G. Taming the adolescent mind: preliminary report of a mindfulness‐based psychological intervention for adolescents with clinical heterogeneous mental health diagnoses. Clin Child Psychol Psychiatry. 2013;18(2):300‐312. [DOI] [PubMed] [Google Scholar]
- 84. Garanty‐Bogacka B, Syrenicz M, Goral J, et al. Changes in inflammatory biomarkers after successful lifestyle intervention in obese children. Endokrynol Pol. 2011;62(6):499‐505. [PubMed] [Google Scholar]
- 85. Hashemipour M, Kelishadi R, Tavalaee Zavvareh SA, Ghatreh‐Samani S. Effect of education on anthropometric indices in obese parents and children after one year of follow‐up. ARYA Atheroscler. 2012;8(1):21‐26. [PMC free article] [PubMed] [Google Scholar]
- 86. Kelsey MM, Geffner ME, Guandalini C, et al. Presentation and effectiveness of early treatment of type 2 diabetes in youth: lessons from the TODAY study. Pediatr Diabetes. 2016;17(3):212‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Sequeira PA, Pyatak EA, Weigensberg MJ, et al. Let's Empower and Prepare (LEAP): evaluation of a structured transition program for young adults with type 1 diabetes. Diabetes Care. 2015;38(8):1412‐1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Cabrera SM, Srivastava NT, Behzadi JM, Pottorff TM, Dimeglio LA, Walvoord EC. Long‐term glycemic control as a result of initial education for children with new onset type 1 diabetes: does the setting matter? Diabetes Educ. 2013;39(2):187‐194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Qayyum AA, Lone SW, Ibrahim MN, Atta I, Raza J. Effects of diabetes self‐management education on glycaemic control in children with insulin‐dependent diabetes mellitus. J Coll Physicians Surg Pak. 2010;20(12):802‐805. [PubMed] [Google Scholar]
- 90. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561‐571. [DOI] [PubMed] [Google Scholar]
- 91. Butz AM, Halterman J, Bellin M, et al. Improving preventive care in high risk children with asthma: lessons learned. J Asthma. 2014;51(5):498‐507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Davis AM, Benson M, Cooney D, Spruell B, Orelian J. A matched‐cohort evaluation of a bedside asthma intervention for patients hospitalized at a large urban children's hospital. J Urban Health. 2011;88(Suppl 1):49‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Herbert LJ, Sweenie R, Kelly KP, Holmes C, Streisand R. Using qualitative methods to evaluate a family behavioral intervention for type 1 diabetes. J Pediatr Health Care. 2014;28(5):376‐385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Stromback M, Malmgren‐Olsson EB, Wiklund M. 'Girls need to strengthen each other as a group': experiences from a gender‐sensitive stress management intervention by youth‐friendly Swedish health services–a qualitative study. BMC Public Health. 2013;13:907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Goldsmith MR, Bankhead CR, Austoker J. Synthesising quantitative and qualitative research in evidence‐based patient information. J Epidemiol Community Health. 2007;61(3):262‐270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Pham MT, Rajic A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371‐385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Munn Z, Peters M, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141‐146. [DOI] [PubMed] [Google Scholar]
- 99. Davis LJ Jr, Hurt RD, Offord KP, Lauger GG, Morse RM, Bruce BK. Self‐administered Nicotine‐Dependence Scale (SANDS): item selection, reliability estimation, and initial validation. J Clin Psychol. 1994;50(6):918‐930. [DOI] [PubMed] [Google Scholar]
- 100. Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59‐65. [DOI] [PubMed] [Google Scholar]
- 101. Schatz M, Sorkness CA, Li JT, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549‐556. [DOI] [PubMed] [Google Scholar]
- 102. Juniper EF, Gruffydd‐Jones K, Ward S, Svensson K. Asthma Control Questionnaire in children: validation, measurement properties, interpretation. Eur Respir J. 2010;36(6):1410‐1416. [DOI] [PubMed] [Google Scholar]
- 103. Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902‐907. [DOI] [PubMed] [Google Scholar]
- 104. Liu AH, Zeiger R, Sorkness C, et al. Development and cross‐sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119(4):817‐825. [DOI] [PubMed] [Google Scholar]
- 105. Kieckhefer GM. Testing self‐perception of health theory to predict health promotion and illness management behavior in children with asthma. J Pediatr Nurs. 1987;2(6):381‐391. [PubMed] [Google Scholar]
- 106. Velsor‐Friedrich B, Pigott TD, Srof B, Froman R. The asthma belief survey: development and testing. J Nurs Meas. 2004;12(1):7‐19. [PubMed] [Google Scholar]
- 107. Wu LM, Chin CC, Chen CH, Lai FC, Tseng YY. Development and validation of the paediatric cancer coping scale. J Adv Nurs. 2011;67(5):1142‐1151. [DOI] [PubMed] [Google Scholar]
- 108. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self‐care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943‐950. [DOI] [PubMed] [Google Scholar]
- 109. Kovacs M, Brent D, Steinberg TF, Paulauskas S, Reid J. Children's self‐reports of psychologic adjustment and coping strategies during first year of insulin‐dependent diabetes mellitus. Diabetes Care. 1986;9(5):472‐479. [DOI] [PubMed] [Google Scholar]
- 110. Spirito A, Stark LJ, Williams C. Development of a brief coping checklist for use with pediatric populations. J Pediatr Psychol. 1988;13(4):555‐574. [DOI] [PubMed] [Google Scholar]
- 111. Kritikos V, Krass I, Chan HS, Bosnic‐Anticevich SZ. The validity and reliability of two asthma knowledge questionnaires. J Asthma. 2005;42(9):795‐801. [DOI] [PubMed] [Google Scholar]
- 112. Evans D, Clark NM, Levison MJ, Levin B, Mellins RB. Can children teach their parents about asthma? Health Educ Behav. 2001;28(4):500‐511. [DOI] [PubMed] [Google Scholar]
- 113. Kaplan DL, Rips JL, Clark NM, Evans D, Wasilewski Y, Feldman CH. Transferring a clinic‐based health education program for children with asthma to a school setting. J Sch Health. 1986;56(7):267‐271. [DOI] [PubMed] [Google Scholar]
- 114. Parcel GS, Nader PR, Tiernan K. A health education program for children with asthma. J Dev Behav Pediatr. 1980;1(3):128‐132. [PubMed] [Google Scholar]
- 115. Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21(5):706‐710. [DOI] [PubMed] [Google Scholar]
- 116. Rosenberg M. Society and the Adolescent Self‐Image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 117. Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self‐ esteem and specific self‐esteem: different concepts, different outcomes. Am Sociol Rev. 1995;60(1):141‐157. [Google Scholar]
- 118. Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Qual Life Res. 1996;5(1):35‐46. [DOI] [PubMed] [Google Scholar]
- 119. Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J. 1999;14(1):32‐38. [DOI] [PubMed] [Google Scholar]
- 120. Ingersoll GM, Marrero DG. A modified quality‐of‐life measure for youths: psychometric properties. Diabetes Educ. 1991;17(2):114‐118. [DOI] [PubMed] [Google Scholar]
- 121. Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ‐C30: a quality‐of‐life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365‐376. [DOI] [PubMed] [Google Scholar]
- 122. Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53‐72. [DOI] [PubMed] [Google Scholar]
- 123. Bullinger M, Schmidt S, Petersen C, DISABKIDS Group . Assessing quality of life of children with chronic health conditions and disabilities: a European approach. Int J Rehabil Res. 2002;25(3):197‐206. [DOI] [PubMed] [Google Scholar]
- 124. Kolsteren MM, Koopman HM, Schalekamp G, Mearin ML. Health‐related quality of life in children with celiac disease. J Pediatr. 2001;138(4):593‐595. [DOI] [PubMed] [Google Scholar]
- 125. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800‐812. [DOI] [PubMed] [Google Scholar]
- 126. Schmidt S, Muhlan H, Power M. The EUROHIS‐QOL 8‐item index: psychometric results of a cross‐cultural field study. Eur J Public Health. 2006;16(4):420‐428. [DOI] [PubMed] [Google Scholar]
- 127. Anderson BJ, Auslander WF, Jung KC, Miller JP, Santiago JV. Assessing family sharing of diabetes responsibilities. J Pediatr Psychol. 1990;15(4):477‐492. [DOI] [PubMed] [Google Scholar]
- 128. Hood KK, Butler DA, Anderson BJ, Laffel LM. Updated and revised Diabetes Family Conflict Scale. Diabetes Care. 2007;30(7):1764‐1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Fok CC, Allen J, Henry D, Mohatt GV, People Awakening Team . Multicultural Mastery Scale for youth: multidimensional assessment of culturally mediated coping strategies. Psychol Assess. 2012;24(2):313‐327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Sawicki GS, Lukens‐Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ–Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36(2):160‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385‐396. [PubMed] [Google Scholar]
- 132. Muris P, Meesters C, van den Berg F. The Strengths and Difficulties Questionnaire (SDQ)–further evidence for its reliability and validity in a community sample of Dutch children and adolescents. Eur Child Adolesc Psychiatry. 2003;12(1):1‐8. [DOI] [PubMed] [Google Scholar]
- 133. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20‐40. [DOI] [PubMed] [Google Scholar]
- 134. Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96:5‐21. [DOI] [PubMed] [Google Scholar]
- 135. McCabe C, Stevens K, Roberts J, Brazier J. Health state values for the HUI 2 descriptive system: results from a UK survey. Health Econ. 2005;14(3):231‐244. [DOI] [PubMed] [Google Scholar]
- 136. Stevens K. Valuation of the Child Health Utility 9D Index. Pharmacoeconomics. 2012;30(8):729‐747. [DOI] [PubMed] [Google Scholar]
- 137. Schlosser M, Havermans G. A self‐efficacy scale for children and adolescents with asthma: construction and validation. J Asthma. 1992;29(2):99‐108. [DOI] [PubMed] [Google Scholar]
- 138. Bursch B, Schwankovsky L, Gilbert J, Zeiger R. Construction and validation of four childhood asthma self‐management scales: parent barriers, child and parent self‐efficacy, and parent belief in treatment efficacy. J Asthma. 1999;36(1):115‐128. [DOI] [PubMed] [Google Scholar]
- 139. Grossman HY, Brink S, Hauser ST. Self‐efficacy in adolescent girls and boys with insulin‐dependent diabetes mellitus. Diabetes Care. 1987;10(3):324‐329. [DOI] [PubMed] [Google Scholar]
- 140. Anderson RM, Fitzgerald JT, Gruppen LD, Funnell MM, Oh MS. The Diabetes Empowerment Scale‐Short Form (DES‐SF). Diabetes Care. 2003;26(5):1641‐1642. [DOI] [PubMed] [Google Scholar]
- 141. Johnston M, Wright S, Weinman I. Measures in Health Psychology: A User's Portfolio. Windsor, ON: NFER Nelson; 1995. [Google Scholar]
- 142. Iannotti RJ, Nansel TR, Schneider S, et al. Assessing regimen adherence of adolescents with type 1 diabetes. Diabetes Care. 2006;29(10):2263‐2267. [DOI] [PubMed] [Google Scholar]
- 143. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278‐296. [DOI] [PubMed] [Google Scholar]
- 144. Kovacs M. The Children's Depression, Inventory (CDI). Psychopharmacol Bull. 1985;21(4):995‐998. [PubMed] [Google Scholar]
- 145. Vilela JA, Crippa JA, Del‐Ben CM, Loureiro SR. Reliability and validity of a Portuguese version of the Young Mania Rating Scale. Braz J Med Biol Res. 2005;38(9):1429‐1439. [DOI] [PubMed] [Google Scholar]
- 146. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193‐213. [DOI] [PubMed] [Google Scholar]
- 147. Kain ZN, Mayes LC, Cicchetti DV, Bagnall AL, Finley JD, Hofstadter MB. The Yale Preoperative Anxiety Scale: how does it compare with a "gold standard"? Anest Analg. 1997;85(4):783‐788. [DOI] [PubMed] [Google Scholar]
- 148. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales (2nd ed.). Sydney, NSW: Psychology Foundation; 1995. [Google Scholar]
- 149. Radloff LS. The CES‐D Scale: a self‐report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385‐401. [Google Scholar]
- 150. Radloff LS, Locke BZ. The community mental health assessment survey and the CES‐D Scale In: Weissman MM, Myers JK, Ross CE, eds. Community surveys of psychiatric disorders. New Brunswick, NJ: Rutgers University Press; 1986:177‐189. [Google Scholar]
- 151. Kroenke K, Spitzer RL, Williams JB. The PHQ‐15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258‐266. [DOI] [PubMed] [Google Scholar]
- 152. Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180:461‐464. [DOI] [PubMed] [Google Scholar]
- 153. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918‐1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Hall RC. Global assessment of functioning. A modified scale. Psychosomatics. 1995;36(3):267‐275. [DOI] [PubMed] [Google Scholar]
- 155. Wing JK, Beevor AS, Curtis RH, Park SB, Hadden S, Burns A. Health of the Nation Outcome Scales (HoNOS). Research and development. Br J Psychiatry. 1998;172:11‐18. [DOI] [PubMed] [Google Scholar]
- 156. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71‐75. [DOI] [PubMed] [Google Scholar]
- 157. Bell IR, Cunningham V, Caspi O, Meek P, Ferro L. Development and validation of a new global well‐being outcomes rating scale for integrative medicine research. BMC Complement Altern Med. 2004;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12‐country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381‐1395. [DOI] [PubMed] [Google Scholar]
- 159. Aadahl M, Jorgensen T. Validation of a new self‐report instrument for measuring physical activity. Med Sci Sports Exerc. 2003;35(7):1196‐1202. [DOI] [PubMed] [Google Scholar]
- 160. Ireland P, Jolley D, Giles G, et al. Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac J Clin Nutr. 1994;3(1):19‐31. [PubMed] [Google Scholar]
- 161. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241‐247. [DOI] [PubMed] [Google Scholar]
- 162. Greco LA, Lambert W, Baer RA. Psychological inflexibility in childhood and adolescence: development and evaluation of the Avoidance and Fusion Questionnaire for Youth. Psychol Assess. 2008;20(2):93‐102. [DOI] [PubMed] [Google Scholar]
- 163. Greco LA, Baer RA, Smith GT. Assessing mindfulness in children and adolescents: development and validation of the Child and Adolescent Mindfulness Measure (CAMM). Psychol Assess. 2011;23(3):606‐614. [DOI] [PubMed] [Google Scholar]
- 164. Prince‐Embury S. Resiliency Scales for Children and Adolescents: A Profile of Personal Strengths. San Antonio, TX: Harcourt Assessment, Inc; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


