Abstract
Os subfibulare is an ossicle at the tip of the lateral malleolus. The ossicle is sometimes symptomatic and presents with local pain or lateral ankle instability. The purpose of this Technical Note is to describe the details of arthroscopic stabilization of the os subfibulare. It is indicated for symptomatic mechanical lateral ankle instability resulting from an unstable os subfibulare. The technique has the advantages of minimally invasive surgery, evaluation and treatment of concomitant ankle pathology, and preservation of integrity of the anterior talofibular ligament.
Os subfibulare is an ossicle at the tip of the lateral malleolus found in 1% of the human population.1 It is a result of an unfused accessory ossification center or an avulsion fracture of the anterior talofibular ligament.1, 2 Avulsion fracture may fail to unite because it is intra-articular and bathed in synovial fluid or because the tension on the anterior talofibular ligament attached to the ossicle causes a separation of the fragment from the bone.2
The ossicle is sometimes symptomatic and presents with local pain or lateral ankle instability.1 The pain can be a result of traction stress of the ossicle from the attached ligament, surrounding synovitis, hypertrophic soft tissue impingement, or impingement of the ossicle on the tip of the lateral malleolus during ankle dorsiflexion.1, 3, 4 In the presence of os subfibulare, the ankle is normally stable because of the tight binding between the talus and the fibular tip by the superficial fibers of the anterior talofibular ligament. However, the structure between the os subfibulare and the fibula is a mechanical weak point against inversion stress. Acute trauma or chronic inversion stress can lead to avulsion of the ossicle from the lateral malleolus, and the ankle may become symptomatic.2 Both size and location of the os subfibulare play a role in determining the clinical effect of the separated ossicle. An ossicle that is >10 mm or located at the anterior distal end of the lateral malleolus is more likely to be associated with disruption of the lateral ankle ligament complex.3
In general, nonoperative treatment (a period of rest with restricted weightbearing or immobilization) should be the first line of treatment.1 Surgical treatment is indicated if conservative treatment fails to relieve symptoms. Excision of the os subfibulare is indicated for a painful small ossicle without ankle instability.1 For symptomatic mechanical lateral ankle instability, surgical options include excision of the os subfibulare together with repair or reconstruction of the lateral ligament of the ankle or fusion of the ossicle.1, 5, 6, 7
A technique for arthroscopic resection of the os subfibulare has been reported.1 Arthroscopy has the advantages of minimally invasive surgery and allows evaluation and treatment of concomitant intra-articular pathology of the ankle.1, 2 This is important, as the prevalence of osteochondral lesions of the talus is significantly higher in cases of lateral ankle instability with the presence of os subfibulare than those without the ossicle,5 and poor clinical outcome will result if they are not addressed.8, 9, 10 An arthroscopic Broström procedure11, 12, 13, 14, 15, 16, 17 can also be done in the same setting of arthroscopic resection of the os subfibulare.
Currently, fusion of os subfibulare is performed as an open procedure. This report describes the technical details of arthroscopic stabilization of the unstable os subfibulare. It is indicated for symptomatic mechanical lateral ankle instability resulting from unstable os subfibulare that is recalcitrant to conservative treatment and an ossicle >10 mm.1, 3 This procedure is contraindicated if the lateral ankle instability results from anterior talofibular ligament insufficiency rather than the unstable ossicle or if there is concomitant subtalar instability. It is also contraindicated if the ossicle is too small or the bone quality is too poor to achieve stable internal fixation (Table 1).
Table 1.
Indications and Contraindications of Arthroscopic Stabilization of Unstable Os Subfibulare
| Indications | Contraindications |
|---|---|
| Symptomatic mechanical lateral ankle instability due to unstable os subfibulare that is recalcitrant to conservative treatment and an ossicle >10 mm | • Lateral ankle instability is anterior as a result of talofibular ligament insufficiency rather than the unstable ossicle |
| • There is concomitant subtalar instability | |
| • The ossicle is too small or the bone quality is too poor to achieve stable internal fixation |
Technique
Preoperative Planning and Patient Positioning
Careful history-taking and clinical examination are usually sufficient to establish the diagnosis of chronic lateral ankle instability. Clinical examination may show mobility of the os subfibulare if it is sizable: the ossicle will move distally or anteriorly during inversion stress test and anterior drawer test, respectively. A radiograph can confirm the presence of the os subfibulare and assess the size of the ossicle. Preoperative magnetic resonance imaging can be useful for detection of associated intra-articular lesions, such as osteochondral lesion.
The patient is put in supine position. A thigh tourniquet is applied to provide a bloodless operative field. A 2.7-mm 30° arthroscope (Henke Sass Wolf, Tuttlingen, Germany) is used for this procedure. Fluid inflow is by gravity, and no pump is used. No ankle distractor is used. The knee is flexed and supported by a triangular supporting frame (Innomed, Savannah, GA) during the arthroscopic procedure.
Examination Under Anesthesia
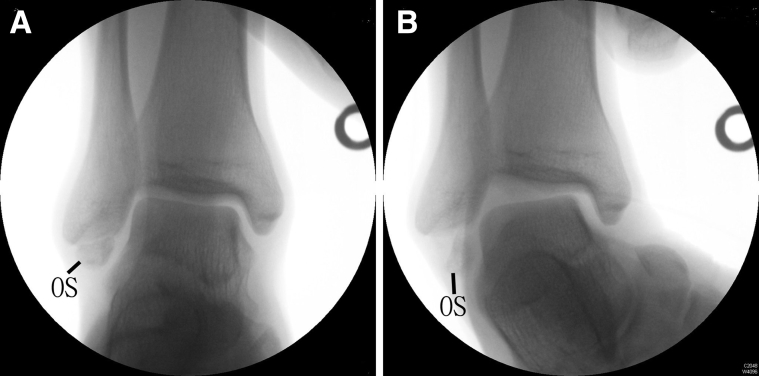
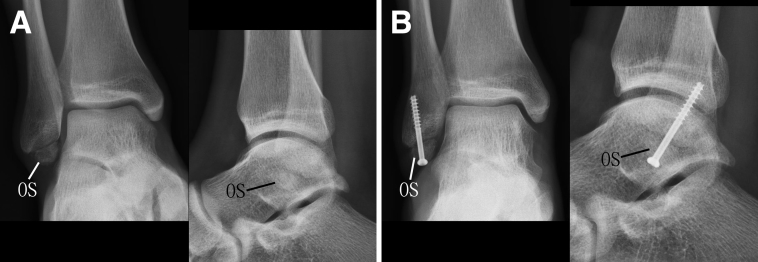
After application of general or spinal anesthesia, the ankle joint is examined under fluoroscopy. Displacement of the os subfibulare can be shown during an inversion stress test (Fig 1).
Fig 1.
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. After application of general or spinal anesthesia, the ankle joint is examined under fluoroscopy. Displacement of the os subfibulare can be shown during inversion stress test. (A) Ankle in neutral position. (B) Lateral ankle joint space opening up and plantar displacement of os subfibulare upon inversion stress. OS, os subfibulare.
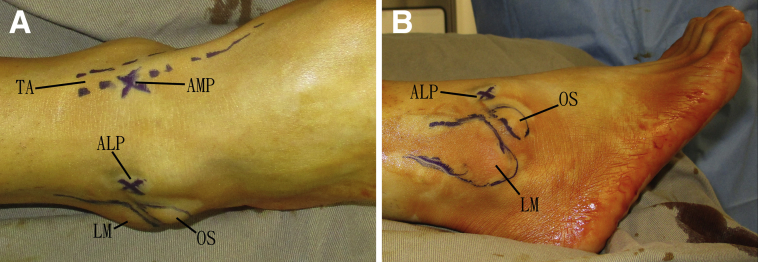
Portal Placement of Ankle Arthroscopy
Ankle arthroscopy is performed using anteromedial and anterolateral portals. The anteromedial portal locates lateral to the tibialis anterior tendon, and the anterolateral portal locates lateral to the peroneus tertius tendon (Fig 2). Lateral placement of the anteromedial portal enhances arthroscopic visualization of the lateral ankle gutter.
Fig 2.
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. Ankle arthroscopy is performed using the anteromedial and anterolateral portals. The anteromedial portal locates lateral to the tibialis anterior tendon, and the anterolateral portal locates lateral to the peroneus tertius tendon. (A) Anterior view of the ankle. (B) Lateral view of the ankle. ALP, anterolateral portal; AMP, anteromedial portal; LM, lateral malleolus; OS, os subfibulare; TA, tibialis anterior tendon.
Arthroscopic Synovectomy of Lateral Gutter of the Ankle Joint
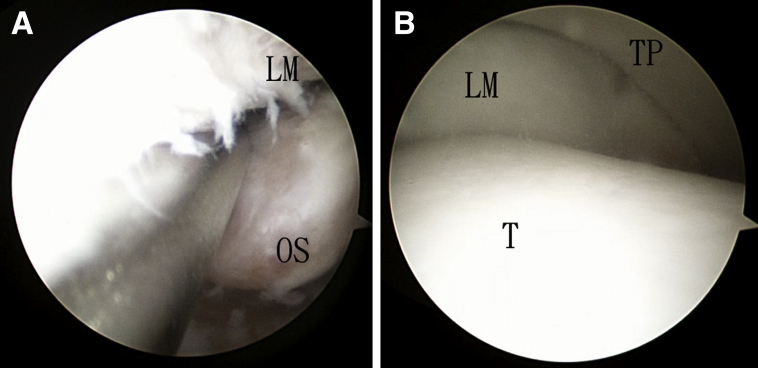
The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. The ankle joint is examined for any concomitant pathology (e.g., osteochondral lesion) and treated accordingly. Arthroscopic synovectomy of the lateral gutter of the ankle joint is performed with an arthroscopic shaver (Dyonics; Smith & Nephew, Andover, MA) (Fig 3).
Fig 3.
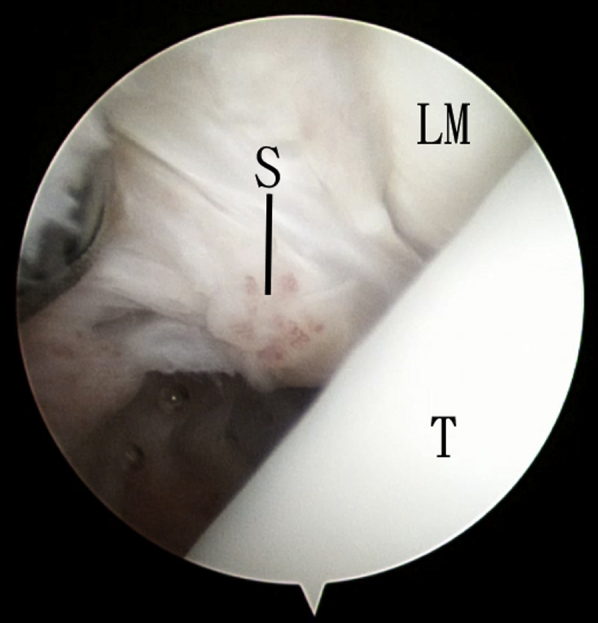
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the lateral ankle gutter is examined. LM, lateral malleolus; S, inflamed synovium; T, talus.
Arthroscopic Assessment of Instability of the Os Subfibulare and Ankle Joint
The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. After synovectomy, the mobility of the os subfibulare can be assessed. The lateral instability of the ankle joint can be confirmed arthroscopically by observing the lateral ankle opening up during inversion stress to the ankle (Figure 4).
Fig 4.
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. (A) The os subfibulare can be displaced distally. (B) The lateral ankle is opened up upon inversion stress. LM, lateral malleolus; S, inflamed synovium; T, talus; TP, tibial plafond.
Arthroscopic Preparation of Fusion Surfaces
The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. The opposing surfaces of lateral malleolus and os subfibulare are debrided with an arthroscopic shaver, arthroscopic burr (Dyonics; Smith & Nephew), and arthroscopic curette (Acufex; Smith & Nephew) (Fig 5). This is followed by microfracture of the fusion surface of the lateral malleolus with an arthroscopic awl (Acufex; Smith & Nephew). Microfracture of the fusion surface of the os subfibulare is not effective because of the mobility of the ossicle. Instead, the os subfibulare is drilled with a Kirschner wire (K wire) (Zimmer, Warsaw, IN).
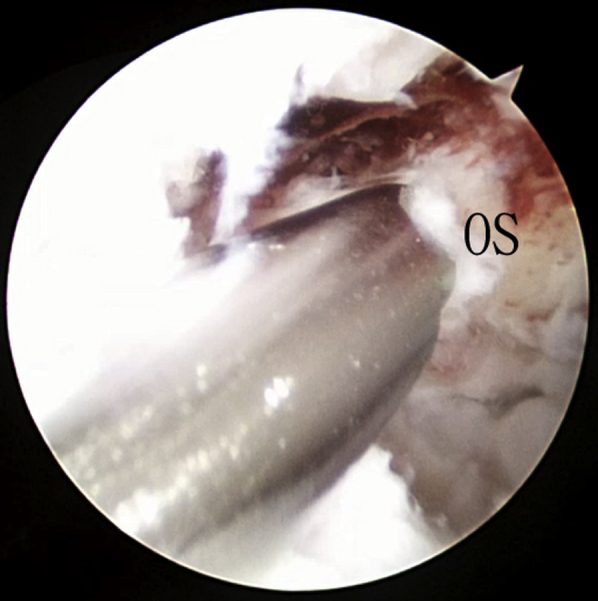
Fig 5.
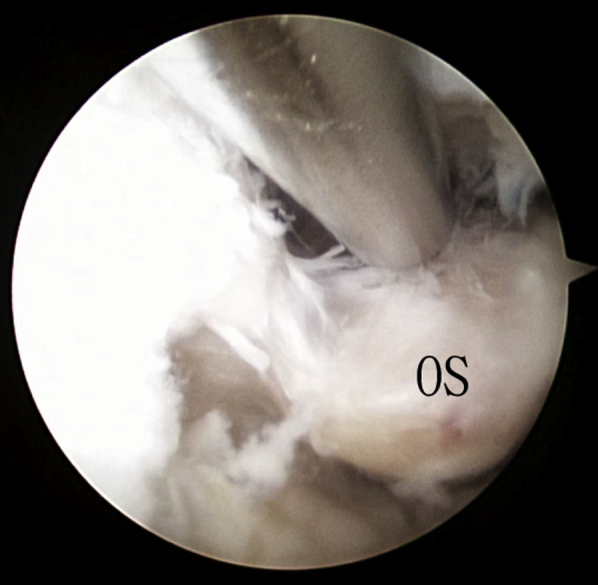
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. The opposing surfaces of lateral malleolus and os subfibulare are debrided with an arthroscopic shaver. OS, os subfibulare.
Arthroscopically Assisted Fixation of Os Subfibulare
The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. The ossicle is reduced and temporarily fixed with a K wire. The articular surface of the lateral malleolus is examined to confirm anatomic reduction of the ossicle.
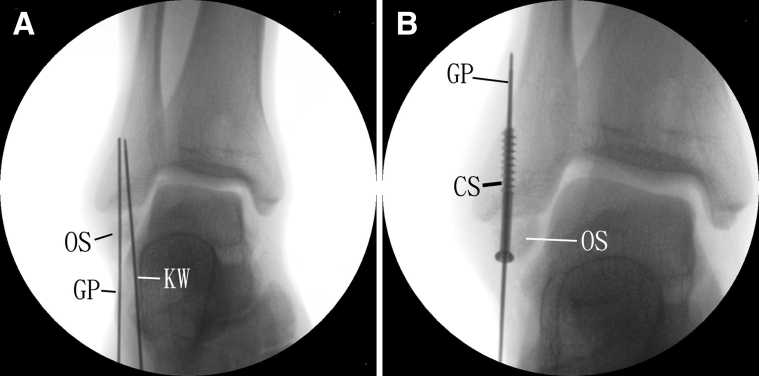
Screw Fixation of the Os Subfibulare
After confirmation of anatomic reduction of the os subfibulare, a guide pin is inserted percutaneously across the ossicle to the lateral malleolus (Fig 6). The correct positioning of the guide pin is confirmed fluoroscopically, and a 4-mm cannulated screw is inserted (Fig 7). The K wire and guide pin are then removed.
Fig 6.
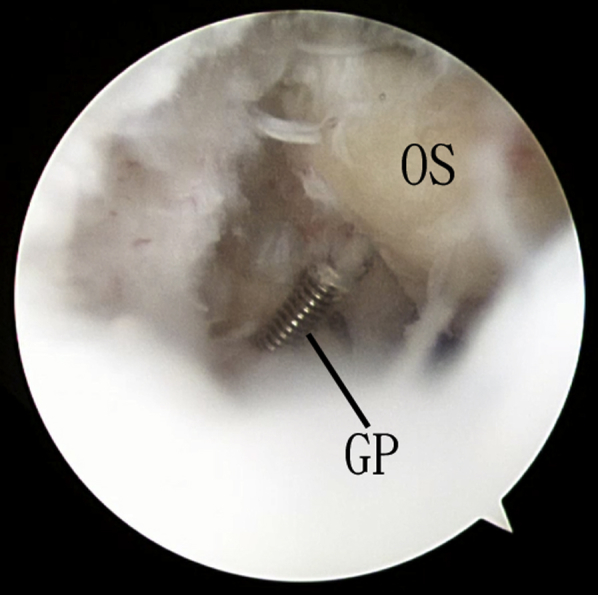
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. After temporary fixation of the os subfibulare with a Kirschner wire, a guide pin is inserted. GP, guide pin; OS, os subfibulare.
Fig 7.
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. (A) The correct position of the guide pin is confirmed by fluoroscopy. (B) A 4-mm cannulated screw is inserted along the guide pin. CS, cannulated screw; GP, guide pin; KW, Kirschner wire; OS, os subfibulare.
Arthroscopic Assessment of Stability of Os Subfibulare and the Ankle Joint After Screw Fixation
The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. The stability of the os subfibulare and ankle joint is confirmed arthroscopically (Fig 8, Table 2, Video). The integrity of the anterior talofibular ligament is also confirmed with an arthroscopic probe (Acufex; Smith & Nephew).
Fig 8.
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. The stability of the os subfibulare after screw fixation is tested. OS, os subfibulare.
Table 2.
Pearls and Pitfalls of Arthroscopic Stabilization of Unstable Os Subfibulare
| Pearls | Pitfalls |
|---|---|
| • The anteromedial portal is placed lateral to the tibialis anterior tendon to enhance visualization of the lateral ankle gutter. | • Subtalar instability, if present, cannot be detected during ankle arthroscopy. Screening of the subtalar stability under fluoroscopy after fixation of the os subfibulare is essential. |
| • The subcutaneous tissue at the anteromedial portal is bluntly dissected down to the joint capsule, to minimize the risk of injury to the deep peroneal nerve. | • For those ossicles located anteromedially to the lateral malleolus and not at its tip, the interface between the ossicle and lateral malleolus is oblique.2 It is difficult to put in a screw perpendicular to the interface. Kirschner wire fixation of the ossicle or resection of the ossicle is a better choice. |
| • Drilling of the mobile os subfibulare is easier than microfracture of the ossicle with an arthroscopic awl. |
Postoperative Care
The ankle is immobilized in a short leg cast for 2 weeks, and the patient is non-weightbearing during this period. After that, the patient is allowed weightbearing walking in an Aircast Air-Stirrup ankle support brace (DJO, Dallas, TX) for another 4 weeks (Fig 9).
Fig 9.
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. (A) Preoperative anteroposterior and lateral radiographs of the ankle. (B) Postoperative anteroposterior and lateral radiographs of the ankle showed screw fixation of the os subfibulare.
Discussion
The best surgical option for lateral ankle instability associated with an unstable os subfibulare is still undetermined. Excision of the ossicle has been proposed; however, the anterior talofibular ligament connected to the ossicle will be damaged during dissection of the ossicle.1, 2 Resection of large ossicles may raise additional risks of ligament defects that can affect joint stability, and ligament repair or reconstruction should also be performed.3 However, when the ossicle is large, excision and a modified Broström technique can achieve varus stability but not sagittal stability of the ankle.5 Moreover, removal of a large articular fragment will markedly reduce the articular surface of the lateral malleolus. To minimize potential disruption to the ankle joint related to the removal of a large os subfibulare (>10 mm), fusion of the unstable os subfibulare is indicated.5
Special consideration should be given to patients whose distal fibular growth plate has not yet closed. They have good bone healing potential, but there is risk of injury to the growth plate by the guide pin and screw. The size, length, and placement of the screw should be carefully planned to avoid damage to the growth plate, or an alternative fixation modality such as a K wire should be considered.1, 3
Conclusions
Arthroscopic stabilization of unstable os subfibulare has the advantages of better cosmetic results, less pain, and less surgical trauma. It allows evaluation and treatment of concomitant ankle pathology. The working space of the reported technique is at the interface, and the anterior talofibular ligament would not be disrupted. The potential risks of this technique include iatrogenic fracture of the ossicle and injury to the the branches of the deep or superficial portal nerve (Table 3). This technique is not technically demanding and can be attempted by the average foot and ankle arthroscopist.
Table 3.
Advantages and Risks of Arthroscopic Stabilization of Unstable Os Subfibulare
| Advantages | Risks |
|---|---|
| • Better cosmetic result | • Iatrogenic fracture of the os subfibulare |
| • Less pain | • Injury to the the branches of the deep or superficial portal nerve |
| • Less surgical trauma | |
| • Allows evaluation and treatment of concomitant ankle pathology | |
| • The anterior talofibular ligament is not disrupted |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. Hypertrophied synovium of the lateral ankle gutter is resected to expose the os subfibulare. The stability of the ossicle and lateral ankle is evaluated. The opposing surfaces of the ossicle and lateral malleolus are debrided and microfractured. The ossicle is reduced and temporarily fixed with a Kirschner wire. The articular surfaces of the lateral malleolus and os subfibulare are examined to confirm anatomic reduction of the ossicle. After that, a guide pin is inserted, and correct positioning is confirmed fluoroscopically. A 4-mm cannulated screw is then inserted along the guide pin.
References
- 1.Monden S., Hasegawa A., Hio N., Taki M., Noguchi H. Arthroscopic excision of separated ossicles of the lateral malleolus. J Orthop Sci. 2013;18:733–739. doi: 10.1007/s00776-013-0412-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasegawa A., Kimura M., Tomizawa S., Shirakura K. Separated ossicles of the lateral malleolus. Clin Orthop Relat Res. 1996;330:157–165. doi: 10.1097/00003086-199609000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Zhang C., Wang X., Ma X., Huang J., Jiang J. A novel 9-region systematic assessment tool for separated ossicle at the fibular tip effects on lateral ankle ligament complex integrity: A cadaveric study. Surg Radiol Anat. 2014;36:281–288. doi: 10.1007/s00276-013-1165-6. [DOI] [PubMed] [Google Scholar]
- 4.Vega J., Marimón J., Golanó P., Pérez-Carro L., Salmerón J., Aguilera J.M. True submalleolar accessory ossicles causing impingement of the ankle. Knee Surg Sports Traumatol Arthrosc. 2010;18:254–257. doi: 10.1007/s00167-009-0913-y. [DOI] [PubMed] [Google Scholar]
- 5.Kim B.S., Choi W.J., Kim Y.S., Lee J.W. The effect of an ossicle of the lateral malleolus on ligament reconstruction of chronic lateral ankle instability. Foot Ankle Int. 2010;31:191–196. doi: 10.3113/FAI.2010.0191. [DOI] [PubMed] [Google Scholar]
- 6.Chun T.H., Park Y.S., Sung K.S. The effect of ossicle resection in the lateral ligament repair for treatment of chronic lateral ankle instability. Foot Ankle Int. 2013;34:1128–1133. doi: 10.1177/1071100713481457. [DOI] [PubMed] [Google Scholar]
- 7.Ahn H.W., Lee K.B. Comparison of the modified Brostrom procedure for chronic lateral ankle instability with and without subfibular ossicle. Am J Sports Med. 2016;44:3158–3164. doi: 10.1177/0363546516660069. [DOI] [PubMed] [Google Scholar]
- 8.Cha S.D., Kim H.S., Chung S.T. Intra-articular lesions in chronic lateral ankle instability: Comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg. 2012;4:293–299. doi: 10.4055/cios.2012.4.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guillo S., Bauer T., Lee J.W. Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99S:S411–S419. doi: 10.1016/j.otsr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Hua Y., Chen S., Li Y., Chen J., Li H. Combination of modified broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy. 2010;26:524–528. doi: 10.1016/j.arthro.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Cottom J.M., Rigby R.B. The “all inside” arthroscopic Brostrom procedure: A prospective study of 40 consecutive patients. J Foot Ankle Surg. 2013;52:568–574. doi: 10.1053/j.jfas.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 12.Corte-Real N.M., Moreira R.M. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2009;30:213–217. doi: 10.3113/FAI.2009.0213. [DOI] [PubMed] [Google Scholar]
- 13.Lui T.H. Modified arthroscopic Brostrom procedure. Foot Ankle Surg. 2015;21:216–219. doi: 10.1016/j.fas.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Lui T.H. Modified arthroscopic Brostrom procedure with bone tunnels. Arthrosc Tech. 2016;5:e775–e780. doi: 10.1016/j.eats.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nery C., Raduan F., Del Buono A., Asaumi I.D., Cohen M., Maffulli N. Arthroscopic-assisted Brostrom-Gould for chronic ankle instability: A long-term follow-up. Am J Sports Med. 2011;39:2381–2388. doi: 10.1177/0363546511416069. [DOI] [PubMed] [Google Scholar]
- 16.Kim E.S., Lee K.T., Park J.S., Lee Y.K. Arthroscopic anterior talofibular ligament repair for chronic ankle instability with a suture anchor technique. Orthopedics. 2011;34 doi: 10.3928/01477447-20110228-03. [DOI] [PubMed] [Google Scholar]
- 17.Wang J., Hua Y., Chen S., Li H., Zhang J., Li Y. Arthroscopic repair of lateral ankle ligament complex by suture anchor. Arthroscopy. 2014;30:766–773. doi: 10.1016/j.arthro.2014.02.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic stabilization of unstable os subfibulare of the right ankle. The patient is in supine position. The anteromedial portal is the viewing portal, and the anterolateral portal is the working portal. Hypertrophied synovium of the lateral ankle gutter is resected to expose the os subfibulare. The stability of the ossicle and lateral ankle is evaluated. The opposing surfaces of the ossicle and lateral malleolus are debrided and microfractured. The ossicle is reduced and temporarily fixed with a Kirschner wire. The articular surfaces of the lateral malleolus and os subfibulare are examined to confirm anatomic reduction of the ossicle. After that, a guide pin is inserted, and correct positioning is confirmed fluoroscopically. A 4-mm cannulated screw is then inserted along the guide pin.