Summary
Introduction
The increasing trend in the global prevalence of childhood overweight and obesity presents a major public health challenge. This study reports the results of a systematic review and meta‐analysis to estimate the prevalence of overweight and obesity among primary school learners residing in Africa according to the different body mass index criteria and population level characteristics.
Methods
A search of multiple databases was conducted to identify relevant research articles published between January 1980 and February 2017. Random effects models were used to pool prevalence data within and across population level characteristics after variance stabilization through arcsine transformation (PROSPERO registration number CRD42016035248).
Results
Data from 45 studies across 15 African countries, and comprising 92,379 and 89,468 participants for overweight and obesity estimates were included. Estimated overweight and obesity prevalence differed significantly across criteria: 10.5% [95% confidence interval, CI: 7.1–14.3] and 6.1% [3.4–9.7] by World Health Organization; 9.5% [6.5–13.0] and 4.0% [2.5–5.9] by International Obesity Task Force; and 11.5% [9.6–13.4] and 6.9% [5.0–9.0] by Centre for Diseases Control, respectively (p = 0.0027 for overweight; p < 0.0001 for obesity). Estimates were mostly higher in urban, and private schools, but generally similar by gender, major geographic regions, publication year and sample size. Substantial heterogeneity in the estimates across and within criteria were not always explained by major study characteristics.
Conclusion
Overweight and obesity are prevalent among African primary school learners, particularly those attending urban, and private schools. The results from this meta‐analysis could be helpful in making informed decisions on childhood obesity prevention efforts in African countries.
Keywords: Africa, Meta‐analysis, Overweight, learners
Introduction
Globally, the prevalence of childhood overweight/obesity is increasing 1, 2, 3, with public health implications in both developed and developing countries. According to the UNICEF, an estimated 41 million children under five were overweight or obese in 2016 with about 25% of this number living in Africa alone, while among children and adolescents aged 5–19 years, 340 million were overweight or obese 4. The prevalence may have stabilized in some industrialized countries; however, the trend seems to be on the increase particularly in some low‐to‐middle income countries 5.
Energy imbalance resulting from increased caloric intake and physical inactivity are the main drivers of obesity; however, biological, social and environmental factors also play crucial roles 6. Some documented risk factors for childhood obesity include family socioeconomic status (SES) 7, 8, maternal employment 9, parental obesity 10, school food and physical activity environments 11, 12 and community and neighbouring factors such as density of fast food restaurants, and living in close proximity to parks and playgrounds 13, 14.
Childhood obesity is associated with early onset of cardiovascular risk factors, including elevated blood pressure, and impaired fasting glucose as well as higher odds of remaining overweight or obese in the adulthood 15, 16, 17, 18. The growing obesity epidemic with its related health risks has the potential to significantly undermine improvements made in the healthcare delivery systems among populations living in low‐to‐middle income countries.
There is a growing interest in the epidemic of obesity across Africa, resulting in several in‐country studies to determine the prevalence 19. In a systematic review to investigate the trends of overweight and obesity among school‐aged children and youth in sub‐Saharan Africa, the body mass index (BMI) cut‐off points used in each study were not taken into consideration in estimating the prevalence rates 19. Using different BMI cut‐off references to estimate overweight and obesity prevalence in children poses a challenge in defining the extent of the problem at the population level. Although substantial heterogeneity was observed in the study methodology, this was not accounted for in the prevalence estimates.
To date, no comprehensive study has been conducted to examine the extent of the overweight and obesity problem among primary school learners overall and by region across Africa. It is important to assess and monitor the prevalence from a young age to provide relevant data that could inform decisions on appropriate interventions. Therefore, the objective of this review was to conduct a systematic review and meta‐analysis to estimate the prevalence of overweight and obesity among primary school learners residing in Africa according to different diagnostic criteria, the World Health Organization (WHO) 20, the Centers for Disease Control and Prevention (CDC) 21 and the International Obesity Task Force (IOTF) 22 criteria; and population level characteristics.
Methods
The methods for this systematic review and meta‐analysis have been previously described in details 23 and registered with PROSPERO, number CRD42016035248. The review is reported following the PRISMA guidelines (checklist available in Table S1). Included studies had to be school‐based surveys involving children aged between 6 and 12 years. Where the age covers a wider range but prevalence was reported by age categories to include the specified age range, the studies were retained. Studies had to be cross‐sectional or cross‐sectional evaluations in longitudinal surveys. Studies that used objective measures of body weight and height and were published between 1 January 1980 and February 2017 were included. No language restrictions were applied; however, included studies were published in either English or French. For articles reporting more than one study or defining overweight and obesity using different BMI criteria, each was considered as a separate study. Studies were excluded if they were conducted on school learners suffering from critical illness or known chronic health conditions such as diabetes, were conducted in African populations residing outside the continent and were not school‐based.
Identification and selection of relevant studies
A comprehensive search of the following electronic databases was conducted to identify eligible studies: MEDLINE (PubMed), MEDLINE (EBSCOHost), CINAHL (EBSCOHost), Academic Search Complete (EBSCOHost) and African Journals Online (AJOL). The complete search strategy comprised combinations of relevant Medical Subject Headings and keywords relating to obesity, overweight, BMI, school children, learners and the names of the 54 African countries and the five African subregions (Table S2). The searches were independently conducted by one reviewer and a research assistant. References were exported, and duplicates were removed and reviewed using EndNote software. The titles, abstracts and full text copies of potentially relevant articles were independently screened by the same reviewer and research assistant for eligibility. Any disagreement about the eligibility was resolved through a consensus and discussion with a third reviewer. The last search date was 20 February 2017.
Data extraction and quality assessment of included studies
The methodological quality of included studies was assessed using a modified version of Downs and Black checklist 24. Ten questions from the checklist were used to provide scores for the quality of reporting, internal validity (bias) and external validity. The following data were extracted: study details (author, year of publication, year of beginning of study and country of study), study characteristics (study design, mean/median age and range, sample size and diagnostic criteria), study setting/location (urban and rural and private and public school), type of sample (national and sub‐national and local), gender distribution, African region where the study country was located and prevalence of overweight and obesity (overall and by subgroups).
Data synthesis and analysis
Data analyses used the ‘meta’ package of the statistical software R (version 3.3.3 [2017‐03‐06], The R Foundation for Statistical Computing, Vienna, Austria). To minimize the influence of studies with extremely small or extremely large prevalence estimates on the overall estimate, the variance of the study‐specific prevalence was first stabilized using the Freeman–Tukey double arcsine transformation 25 before pooling using the random effects meta‐analysis model 26. Heterogeneity between studies was assessed using the Cochran's Q and I 2 statistics 27. The I 2 statistic estimates the percentage of total variation across studies due to true between‐study differences rather than chance. In general, I 2 values greater than 60–70% indicate the presence of substantial heterogeneity. The sources of heterogeneity were explored by comparing overweight/obesity prevalence between subgroups defined by several pre‐specified study‐level characteristics like gender for naturally occurring categories, and median values across studies for publication year and sample size. Subgroups comparisons were performed using the Q test based on ANOVA. The presence of publication bias was assessed using funnel plots and the Egger test of bias 28. Potential outliers were investigated in sensitivity analyses by dropping one study at a time. The Duval and Tweedie trim‐and‐fill method was used to adjust estimates for the effects of publication bias.
Role of the funding source
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Figure 1 shows the PRISMA flow chart of the study selection process. A total of 1,518 records were identified from searches. After removing duplicates, the titles and abstracts of 729 articles were screened for eligibility out of which 65 full text articles were accessed. A total of 40 articles composing of 45 studies met the inclusion criteria and were retained in the meta‐analysis.
Figure 1.
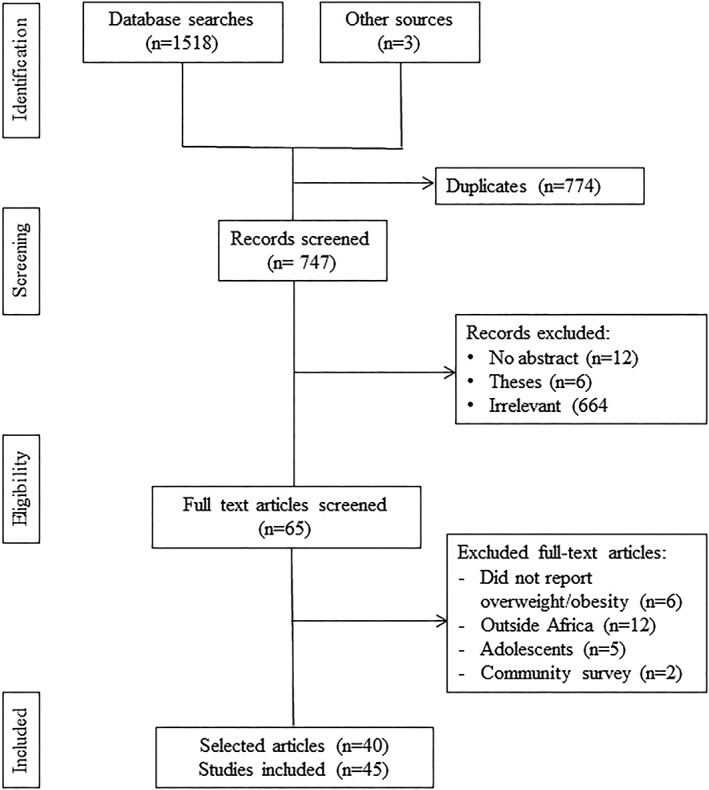
PRISMA flowchart for the study selection process.
Characteristics of included studies
Table 1 summarizes the characteristics of studies included in the meta‐analysis. The 45 included studies originated from 15 countries. With regard to regional representation, 22 studies were conducted in Southern Africa, six in Western, eight in Eastern, nine in Northern and one in Central Africa. Thirty‐seven studies presented data in both boys and girls, three studies reported on exclusively boys and five reported on exclusively girls. Of the studies that reported study settings, 18 were conducted exclusively in urban areas, six in rural areas and 11 in urban/rural areas. Out of the 26 studies that reported on school type, 16 were conducted in private/public schools, nine in public schools and one in exclusively private school. Year of beginning of study that reported in 26 studies ranged from 1994 to 2013. Majority of the included studies were conducted at the sub‐national level while only two were national in coverage. The mean/median age was 10.1 years, reported in 25 studies. All of the studies except two used the international BMI criteria to define overweight/obesity as WHO (22 studies, n = 36,981), IOTF (18 studies, n = 51,604) and the CDC (four studies, n = 2,433). The publication years varied from 2003 to 2016; 26 studies were published after year 2012.
Table 1.
Summary characteristics of included studies
| Reference | Publication year | Start year | Country | Region location | Data type | Study site | School type | Study design | Diagnostic criteria | Sample size | Quality score | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Boys/girls | Urban/rural | Private/public | |||||||||||
| Abrahams et al. 29 | 2011 | – | South Africa | Southern | Sub‐national | Urban–rural | – | – | WHO | 643 | NS | – | NS | 7 |
| Amidu et al. 30 | 2013 | 2012 | Ghana | Western | Sub‐national | Urban | Private–public | Cross‐sectional | CDC | 400 |
200 B 200 G |
400 U |
200 PR 200 PU |
8 |
| Armstrong et al. 31 | 2006 | 2001 | South Africa | Southern | National | Urban–rural | Private–public | Cross‐sectional | IOTF | 10195 |
5611 B 4584 G |
– | NS | 10 |
| Boukthir et al. 32 | 2011 | 2007 | Tunisia | Northern | Sub‐national | Urban | Public | Cross‐sectional | IOTF | 1335 |
637 B 698 G |
1335 U | 1335 PU | 8 |
| Caleyachetty et al. 33 | 2012 | 2006 | Mauritius | Southern | Sub‐national | Urban–rural | – | Cross‐sectional | IOTF | 841 |
412 B 429 G |
298 U 543 R | NS | 9 |
| Chebet et al. 34 | 2014 | – | Uganda | Eastern | Sub‐national | – | Private–public | Cross‐sectional | WHO | 958 |
435 B 523 G |
NS |
456 PR 502 PU |
5 |
| Daboné et al. 35 | 2011 | 2008 | Burkina Faso | Western | Sub‐national | Urban–rural | Private–public | Cross‐sectional | WHO | 649 |
309 B 340 G |
543 U 106 R |
192 PR 457 PU |
8 |
| Dekkaki et al. 36 | 2011 | 2010 | Morocco | Northern | Sub‐national | Urban | Public | Cross‐sectional | WHO | 1570 |
768 B 802 G |
1570 U | 1570 PU | 8 |
| El‐Sabely et al. 37 | 2013 | – | Egypt | Northern | Sub‐national | – | Private–public | Cross‐sectional | WHO | 288 | 288 G | – |
182 PR 106 PU |
7 |
| Fetuga et al. 38 | 2011 | – | Nigeria | Western | Sub‐national | Urban | Public | Cross‐sectional | WHO | 1016 |
479 B 537 G |
1016 U | 574 PU | 8 |
| Hassan et al. 39 | 2008 | 2002 | Egypt | Northern | Sub‐national | NS | Public | Cross‐sectional | CDC | 1283 |
681 B 602 G |
– | 1283 PU | 6 |
| Jinabhai et al. 40 | 2005 | 1995 | South Africa | Southern | Sub‐national | Rural | NS | Cross‐sectional | IOTF | 643 |
292 B 351 G |
643 R | – | 9 |
| Jinabhai et al. 41 | 2003 | 1994 | South Africa | Southern | National | Urban–rural | – | Secondary analysis | IOTF/WHO | 24391 | 14503 B 9888 G | – | – | 9 |
| Kirsten et al. 42 | 2013 | – | South Africa | Southern | Sub‐national | Urban | – | Cross‐sectional | IOTF | 638 | NS | 638 U | NS | 8 |
| Kyallo et al. 43 | 2013 | 2008 | Kenya | Eastern | Sub‐national | Urban | Private–public | Cross‐sectional | WHO | 321 |
153 B 168 G |
321 U |
138 PR 183 PU |
7 |
| Maruf et al. 44 | 2013 | 2009 | Nigeria | Western | – | – | Private–public | – | IOTF | 1775 |
873 B 902 G |
NS | NS | 9 |
| McKersie et al. 45 | 2014 | – | South Africa | Southern | Sub‐national | Urban | – | Cross‐sectional | IOTF | 713 |
372 B 341 G |
713 U | NS | 7 |
| Mogre et al. 46 | 2013 | 2010 | Ghana | Western | Sub‐national | Urban | – | Cross‐sectional | WHO | 218 |
91 B 127 G |
218 U | NS | 7 |
| Mohammed et al. 47 | 2012 | – | Ghana | Western | Sub‐National | Urban | Private | Cross‐sectional | WHO | 270 |
141 B 129 G |
270 U | 270 PR | 6 |
| Moselakgomo et al. 48 | 2015 | – | South Africa | Southern | Sub‐national | – | – | Cross‐sectional | NS | 1361 |
678 B 683 G |
NS | NS | 8 |
| Mosha et al. 49 | 2010 | 2008 | Tanzania | Eastern | Sub‐national | – | Private–public | Cross‐sectional | WHO | 428 |
150 B 278 G |
NS | NS | 6 |
| Mpembeni et al. 50 | 2014 | – | Tanzania | Eastern | Sub‐national | Urban–rural | Private–public | Cross‐sectional | CDC | 446 |
209 B 237 G |
NS | NS | 9 |
| Muhihi et al. 51 | 2013 | 2011 | Tanzania | Eastern | Sub‐national | Urban–rural | Private–public | Cross‐sectional | IOTF | 446 |
209 B 237 G |
249 U 197 R | NS | 9 |
| Muthuri et al. 52 | 2014 | – | Kenya | Eastern | Sub‐national | Urban | Private–public | – | WHO | 563 |
262 B 301 G |
563 U |
268 PR 295 PU |
9 |
| Mwaikambo et al. 53 | 2015 | – | Tanzania | Eastern | Sub‐national | – | Private–public | Cross‐sectional | IOTF | 1722 |
779 B 943 G |
NS |
692 PR 1030 PU |
7 |
| Navti et al. 54 | 2014 | – | Cameroon | Central | Sub‐national | Urban–rural | Private–public | Cross‐sectional | WHO | 557 |
287 B 270 G |
384 U 173 R | NS | 7 |
| Oldewage‐Theron et al. 55 | 2010 | – | South Africa | Southern | Sub‐national | Rural | Public | – | WHO | 142 |
72 B 70 G |
142 R | NS | 6 |
| Pangani et al. 56 | 2016 | – | Tanzania | Eastern | Sub‐national | Urban | Private–public | Cross‐sectional | WHO | 1781 | 753 B 1028 G | 1781 U |
678 PR 1103 PU |
8 |
| Pedro et al. 57 | 2014 | 2009 | South Africa | Southern | Sub‐national | Rural | – | Cross‐sectional | WHO | 588 |
292 B 296 F |
588 R | NS | 8 |
| Pienaar, 2015 58 | 2015 | 2013 | South Africa | Southern | Sub‐national | – | – | Longitudinal | IOTF | 574 |
282 B 292 G |
NS | NS | 7 |
| Prista et al. 59 | 2003 | 1999 | Mozambique | Southern | Sub‐national | Urban–rural | Private–public | – | WHO | 1070 |
475 B 595 G |
NS | – | 7 |
| Puckree et al. 60 | 2011 | 2006 | South Africa | Southern | Sub‐national | Urban | Public | Cross‐sectional | WHO | 120 |
48 B 72 G |
120 U | 120 PU | 7 |
| Regaieg et al. 61 | 2014 | 2010 | Tunisia | Northern | Sub‐national | Urban | Public | Cross‐sectional | IOTF | 1529 |
782 B 747 G |
1529 U | 1529 PU | 7 |
| Salman et al. 62 | 2010 | – | Sudan | Northern | Sub‐national | Urban | – | Cross‐sectional | CDC | 304 |
68 B 236 G |
304 U | NS | 6 |
| Sebbani et al. 63 | 2013 | 2011 | Morocco | Northern | National | Urban | Public | Cross‐sectional | IOTF/WHO | 1418 |
709 B 709 G |
1418 U | 1418 PU | 6 |
| Taleb et al. 64 | 2010 | 1998 | Algeria | Northern | Sub‐national | Urban | – | NS | IOTF | 3396 | 1819 B 1577 G | 3396 U | – | 6 |
| Tathiah et al. 65 | 2013 | 2011 | South Africa | Southern | Sub‐national | Rural | – | Secondary analysis | IOTF | 952 | 952 G | 952 R | NS | 7 |
| Truter et al. 66 | 2010 | – | South Africa | Southern | Sub‐national | – | – | One way | IOTF | 280 |
128 B 152 G |
NS | NS | 7 |
| Van Den Ende et al. 67 | 2014 | 1999 | South Africa | Southern | Sub‐national | Rural | – | Cross‐sectional | IOTF | 825 |
421 B 404 G |
825 R | NS | 7 |
| Wiles et al. 68 | 2013 | – | South Africa | Southern | Sub‐national | Urban | – | Cross‐sectional | WHO | 311 |
138 B 173 G |
311 U | 311 PU | 6 |
B, boys; CDC, Centers for Disease Control and Prevention; G, girls; IOTF, International Obesity Task Force; NS, not specified; PR, private; PU, public; R, rural; U, urban; WHO, World Health Organization.
Quality scores of included studies
Majority of the included studies scored 7 or higher with a median of 7.4 (Table 1). Scores for reporting were moderate to adequate, and these ranged from 51.2% to 97.6%. However, the scores for external validity were low. Less than half of the studies (46.3%) reported that participants were representatives of the population from which they were recruited, and even fewer (14.6%) reported their recruited samples were representative of the population (Table S3).
Overall prevalence of overweight and obesity
The overall overweight prevalence estimates for WHO (21 studies, n = 36,981), IOTF (18 studies, n = 51,604) and CDC (four studies, n = 2,433) and unspecified criteria were 10.5% [95% confidence interval, CI: 7.1–14.3], 9.5% [6.5–13.0], 11.5% [9.6–13.4] and 0.5% [0.0–4.5], respectively, and differed significantly across the various criteria (p = 0.0027; Figure 2). Similarly, obesity prevalence for WHO (18 studies, n = 34,895), IOTF (16 studies, n = 50,779), CDC (four studies, n = 2,433) and unspecified criteria were 6.1% [3.4–9.7], 4.0% [2.5; 5.9], 6.9% [5.0–9.0] and 0.5% [0.0–1.7] with significance difference among the criteria (p < 0.0001; Figure 3, Tables S4 and S5).
Figure 2.

Forest plot of the prevalence of overweight by major diagnostic criteria. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Figure 3.
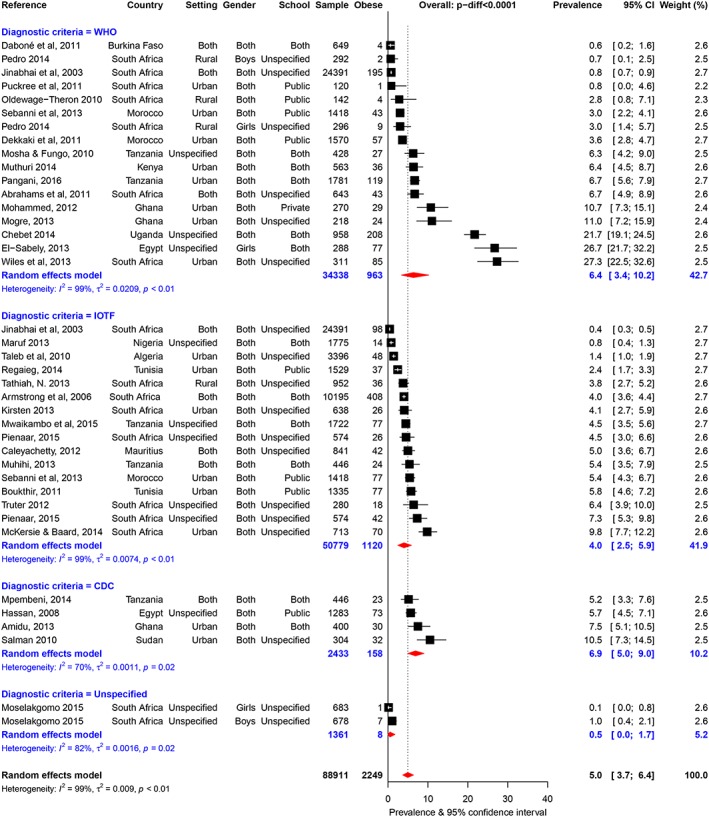
Forest plot of the prevalence of obesity by major diagnostic criteria. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Heterogeneity
There was substantial heterogeneity in estimates across included studies by diagnostic criteria for obesity prevalence (all heterogeneity p ≤ 0.019) and for overweight prevalence (all p < 0.0001) except across studies that used the CDC criteria to diagnose overweight (heterogeneity p = 0.124; see Tables S4 and Table S5 for more heterogeneity statistics). In sensitivity analyses using the leave‐one‐out approach, none of the studies had significant impact of the pooled prevalence estimates and measures of heterogeneity within diagnostic criteria (Figures S1 and S2).
Publication bias
Figure 4 shows the funnel plots for publication bias across the different definition criteria. These plots were asymmetric for WHO (Egger test p = 0.0029 for overweight and p = 0.0019 for obesity) and IOTF (p = 0.020 for overweight and p = 0.003 for obesity) but not for CDC criteria (both p ≥ 0.320; Tables S4 and S5). The small number of studies available precluded similar analyses across studies that applied unspecified criteria to diagnose overweight or obesity.
Figure 4.
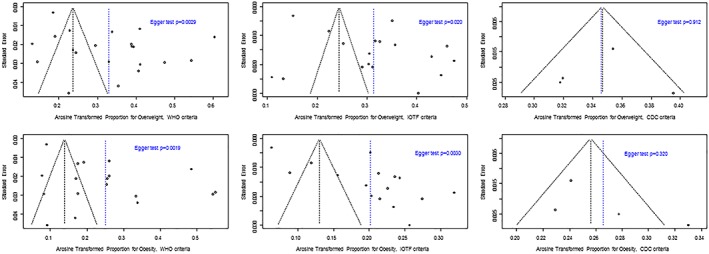
Funnel plots for the assessment of publication bias in studies of prevalent overweight (upper panels) and obesity (lower panels) by the World Health Organization (left column), International Obesity Task Force (middle column) and Centers for Diseases Control (right column) criteria, in African learners. For each figure panel, the dots are the arcsine transformed prevalence estimates of individual studies (horizontal axis) plotted against their standard error (vertical exist). The dotted vertical blue line is for the observed pooled prevalence estimates, while the dotted vertical black line bisector of the angle formed by the two upward converging lines, indicated where the pooled estimates should have been in the absence of publication bias. The p‐value from the egger test of bias is also shown.
For the CDC criteria as expected, no study was imputed through the trim‐and‐fill approach, and pooled estimates remained unchanged for both overweight and obesity. For the WHO criteria, nine studies were imputed for obesity and 10 for overweight, while equivalents for IOTF were eight and nine studies. Funnel plots became symmetrical and Egger test non‐significant when imputed studies were accounted for (Figure S3). However, for both criteria and outcomes, imputed studies had to be of large sample size, with a null prevalence of overweight or obesity (Figures S4 and S5). This is unrealistic in the context of the current epidemiology of overweight and obesity in children and adolescents. Therefore, the publication bias found in the main analysis was likely artefactual.
Prevalence of overweight and obesity within and across subgroups
Gender
In all, 29 studies (WHO), 28 studies (IOTF), six studies (CDC), two studies (unspecified criteria); and 18 studies (WHO), 16 studies (IOTF), four studies (CDC) and two studies (unspecified criteria) respectively provided overweight and obesity prevalence data by gender. The overall prevalence of overweight and obesity across these studies were 11.4% [8.4–14.9] and 7.0% [4.5–10.1], respectively, based on WHO criteria; 10.3% [8.4–12.3] and 4.3% [3.4–5.3] based on IOTF criteria and 11.5% [9.5–13.7] and 6.2% [4.7–8.0] based on CDC criteria, with always significant differences across criteria (overweight p ≤ 0.0028; obesity p < 0.0001; Tables S4 and S5).
By gender, point estimates of the pooled prevalence of overweight and obesity were always higher in girls compared to boys, but these did not result in significant gender differences within the major diagnostic criteria (all p ≥ 0.128 for gender comparisons). Within genders, pooled prevalence estimates always significantly differed across diagnostic criteria (all p < 0.0001; Figures S6–S9). There was substantial heterogeneity for WHO‐based and IOTF‐based studies (all p‐heterogeneity p < 0.0001) and for CDC‐based overweight prevalence in boys only (p = 0.029). Publication bias was apparent only for IOTF‐based obesity prevalence in boys (Egger p = 0.034; Tables S4 and Table S5).
Urban–rural settings
The estimates for overweight and obesity were 12.8% [8.7–17.5] and 9.8% [6.0–14.6] among children in urban compared to 6.9% [3.3–11.6] and 1.5% [0.6–2.9] in children in rural settings by WHO criterion. The respective estimates by the IOTF criteria were 9.4% [5.2–14.7] and 4.9% [3.0–7.2] among urban areas compared to 4.0% [1.3–8.2] and 1.8% [0.6–7.2] in rural areas. By CDC criterion, the prevalence were 12.0% [9.8–14.4] and 7.5% [5.1–10.5] overweight and obesity in only urban school children. The point estimates were consistently higher in children in urban, compared to those in rural schools, and significant with obesity estimates only within the major criteria (all p < 0.0001 for urban–rural comparison; Tables S4 and S5). Within urban–rural settings, the pooled estimates did not differ across diagnostic criteria (p ≥ 0.076; Figures S10–S14). There was substantial heterogeneity for WHO‐based and IOTF‐based prevalence (all p‐heterogeneity p ≤ 0.035) and for CDC‐based obesity prevalence estimate in urban areas (p = 0.015). Further, there was publication bias in IOTF‐based obesity prevalence in urban areas only (Egger p < 0.035; Tables S4 and S5).
Private–public schools
Across all criteria, the pooled overweight and obesity estimates were higher in private compared to public schools. Overweight prevalence were 22.6% [16.0–30.0] and 11.2% [7.4–15.7] by WHO criterion, 18.2% [15.4–21.2] and 7.6% [3.7–12.9] by IOTF criterion and 15.0% [10.4–20.3] and 8.0% [2.2–17.0] by CDC criterion in private and public schools, respectively. The corresponding estimates for obesity in private and public schools were 16.6% [10.4–23.8] and 6.2% [3.1–10.3] for WHO, 1.2% [0.5–2.1] and 4.9% [2.5–8.1] for IOTF and 12.5% [8.3–17.4] and 4.2% [1.6–7.9] for CDC. With the exception of overweight prevalence by CDC criterion, the pooled estimates differed by school type within the major criteria (p ≤ 0.018 for private–public comparisons). Within private–public schools, the point estimates did not differ significantly across the criteria (all p ≥ 0.209) except for obesity prevalence in private schools (p < 0.0001; Figures S15–S18). Heterogeneity was apparent across studies irrespective of criteria used (all p‐heterogeneity p ≤ 0.031). There was no evidence of publication bias for type of school (Egger p ≥ 0.241; Tables S4 and S5).
Regional distribution
The pooled overweight prevalence ranged from 7.7% [2.4–15.7] in Western Africa to 16.1% [6.1–26.8] in Eastern Africa by WHO criteria (p = 0.155); 8.5% [4.6–13.5] in Southern Africa to 14.1% [6.8–23.5] in Eastern Africa by IOTF (p = 0.684); and 9.7% [7.0–12.8] in Western Africa to 12.1% [7.7–17.3] in Eastern Africa by CDC (p = 0.434). Obesity estimates ranged from 4.1% [0.7–9.9] in Southern Africa to 9.6% [3.8–17.6] in Eastern Africa by WHO (p < 0.0001); 0.8% [0.4–1.2] in Western Africa to 4.6% [2.2–7.8] in Southern Africa by IOTF (p < 0.0001); and 5.7% [4.5–7.0] in Northern Africa to 7.6% [3.2–13.6] in Eastern Africa by CDC criteria (p = 0.019). The point estimates across the regional subgroups were comparable within the major criteria and differed only for obesity prevalence by IOTF‐based criteria (p < 0.0001).
Within regional subgroups, the point estimates did not differ across the major criteria (all p ≥ 0.125) except for studies conducted in Southern Africa (p ≤ 0.014) and obesity for Western Africa (p < 0.0001). Substantial heterogeneity was observed in estimates across diagnostic criteria with regional subgroups (all p ≥ 0.042), with the exception of IOTF‐based obesity prevalence in Eastern Africa (p = 0.428). Publication bias was apparent in Southern African studies reporting overweight by WHO‐based criteria (Egger p = 0.032) and obesity by IOTF‐based criteria (Egger p = 0.043; Tables S4 and S5).
Publication year
By diagnostic criteria, the pooled estimates of overweight and obesity were always higher in recent studies (published in 2013 or after) compared to studies published earlier (published before 2013) by WHO criteria (p = 0.0007). Among studies that applied the IOTF and CDC criteria, overweight estimates were lower in recent compared to earlier studies, whereas obesity prevalence were higher in recent compared to earlier studies. Within publication year, pooled estimates of both overweight and obesity differed across all criteria except for studies published earlier (p = 0.154). Heterogeneity was observed for WHO and IOTF criteria (all p < 0.0001) and for CDC‐based obesity prevalence in studies published earlier only (p < 0.005). Publication bias was apparent in earlier studies (Egger p ≤ 0.028) using WHO criteria (Tables S4 and S5).
Sample size
Pooled estimates of overweight and obesity were not appreciably different between small (less than 638 participants) and large studies (638 or more participants), and regardless of criteria (all p ≥ 0.05). Pooled prevalence estimates of overweight and obesity were similar across criteria within small studies (both p ≥ 0.532) but differed significantly within large studies (both p < 0.0016), primarily driven by very low prevalence in studies based on unspecified diagnostic criteria. With the exception of small studies using CDC criteria for overweight (p = 0.074) and IOTF criteria for obesity (p = 0.221), there was substantial heterogeneity by diagnostic criteria within small and large studies (all p < 0.019). Publication bias was apparent only in large studies using IOTF‐based criteria (Egger p = 0.017; Tables S4 and S5).
Discussion
This study provides the first detailed contemporary meta‐analysis of overweight and obesity prevalence in African primary school learners. The results showed that by criteria, overall estimates ranged from 9.5% to 11.5% for overweight and 4.0% to 6.9% for obesity by IOTF and CDC, respectively, with significant variations across major diagnostic criteria. Prevalence estimates were mostly higher in urban compared with in rural schools, and in private compared with public schools, but mostly similar by gender, major geographic region, publication period and study size. There were substantial heterogeneities in the estimates across studies, which were not always explained by major study characteristics. Sensitivity analyses proved the few apparent publication biases to be artefactual.
These results highlight the increasing burden of overweight and obesity and are largely consistent with previous estimates suggesting an increasing overweight and obesity prevalence among children and adolescents globally 1. The estimates are notably higher than the prevalence estimates reported among children and adolescents in previous reviews 1, 19. By the major diagnostic criteria used, the highest overall estimated overweight and obesity prevalence was by the CDC‐based criterion and the lowest by IOTF definition. Notably, the CDC definition was used in four studies whereas 18 studies employed the IOTF definition. Together, CDC and IOTF criteria were used in over half of the studies. Given that the CDC and IOTF criteria underestimate the prevalence of overweight/obesity in children and adolescents compared with the WHO criterion 19, it is plausible that the overall prevalence reported in the present meta‐analysis have been underestimated. The lack of consensus on the BMI cut‐off references to use across studies presents a challenge for results comparability. The observed variations in the overall prevalence estimates by the major criteria thus underscores the relevance of the stratified meta‐analysis based on diagnostic criteria as performed in the present study.
Unlike other studies, gender differences were not observed in the prevalence estimates of overweight and obesity in the present meta‐analysis. The association between gender and overweight/obesity is inconsistent in the literature. A number of studies reported higher prevalence in girls 19, 69, some found higher estimates in boys 70, 71, 72, 73 and others reported similar prevalence estimates 74. In a study involving Australian school children, obesity prevalence did not differ between boys and girls in primary school children; however, substantial gender differences were observed among adolescents in high school 74 suggesting age–gender interactions 70, 73. While the prevalence tend to be similar in boys and girls in this study, among adults, the prevalence is consistently higher in women than in men 1, 75.
In addition to biology, this could be partially due to certain sociocultural practices that influence food choices and dietary intakes, overall energy expenditure and physical activity and perception of overweight/obesity. In some cultures in Africa for instance, overweight/obesity is perceived as an indicator of beauty, good health and wealth particularly among women 76, 77. Additionally, women tend to be more sedentary compared to men 78. Besides, adverse early life experiences such as abuse (physical, sexual and emotional) and child neglect have been linked with higher BMI, and development of overweight, or obesity in adulthood, especially among women, but not in childhood and adolescence 79, 80, 81. While some showed abuse‐specific effects, others reported more general effects across the spectrum of abuse.
Substantial variations in prevalence of overweight and obesity were observed across the rural–urban divide and also across private–public schools in the present study, broadly in line with previous studies 19, 72, 82, 83 that suggest significantly higher estimates in urban children attending private schools, compared to children living in rural areas, and in public schools. The results showed that studies conducted in private schools were mainly in urban areas as opposed to most of those studies in public schools, which were a mix of urban and rural.
African countries are undergoing increasingly rapid urbanization, globalization of the food markets and economic and human development. These are associated with lifestyle changes such as increased sedentary behaviours, physical inactivity and increased consumption of the ‘Westernized diets’ 84. Economic and human development may be linked to increased SES, which could reflect in higher disposable incomes for high‐calorie and ultra‐processed convenient foods, with low nutritional value. Working parents especially mothers who work longer hours may have limited time to prepare fresh nutritious meals and may depend on convenient foods for the family. For example, in the Millennium Cohort Study in the UK, a significant relationship of maternal employment and obesity was found only for children from households with higher annual incomes 9.
Access to technology like motorized transportation and varieties of gaming consoles for the children may be increased in the higher SES households. For instance, results from a study in Africa showed that increasing total annual income was inversely associated with meeting physical activity (PA) guidelines of children 78. Additionally, rapid urbanization may result in overcrowding and congestion, increased crime rates, limited space for neighbourhood playgrounds and parks for children, which may invariably lead to decreased physical activity. On the other hand, undernutrition 85 and PA like active transport and active play 19, 86 generally tend to be higher in rural children in sub‐Saharan Africa.
Preventing excess weight gain in childhood is a major preventive strategy with lasting benefits, and the school provides opportunities and challenges for implementation of behavioural change programmes in children and adolescents. Restricting or limiting of marketing of unhealthy foods and beverages to children and provision of PA facilities are some of the recommended strategies 87, and the schools could provide children with the supportive environments to improve the PA and healthy eating habits by strengthening the school health promotion programmes.
A strength of this study is the stratified meta‐analysis based on the diagnostic criteria used. The PRISMA checklist guided the study from selection of studies to synthesis. This meta‐analysis pooled and compared results from different studies that employed various diagnostic criteria to define overweight and obesity. Although there were substantial heterogeneity across studies, the sources of heterogeneity were thoroughly investigated on pre‐specified population level characteristics. Likewise, an exhaustive search of multiple databases was conducted to identify relevant studies originating from Africa. The study has highlighted the extent of the problem of overweight/obesity and provided valuable data for consideration by policymakers and public health practitioners on the prevention and control strategies among primary school learners in Africa.
There are a number of limitations that might influence the interpretation of the results. Some of the studies were not originally designed to assess prevalence of overweight and obesity. Results were pooled from studies conducted at different geographical locations, among different ethnic groups and with methodological differences, but attempts were made to adjust for these differences through robust methodology. It is possible that some studies that were published in local and unindexed journals were missed. Also, all the geographical locations were not evenly represented. Finally, the predictors of childhood overweight and obesity were not explored in this study because this was an aggregated data meta‐analysis.
Conclusions
In conclusion, the high prevalence of overweight and obesity reported in this review is of great concern considering the negative health impact across the life cycle. Results from the present study demonstrate that while overweight and obesity are more prevalent in urban children, rural residence does not protect against the epidemic. The similar prevalence estimates observed between genders also suggest that among African learners, boys and girls are equally affected. Private school attendance, an indicator of SES of families and urban residence are thus major driving forces of overweight and obesity among African school children. If this prevalence persists, it may lead to increased healthcare cost and burden on healthcare facilities. Results from this meta‐analysis could be helpful in making informed decisions on childhood obesity prevention efforts in African countries.
Conflicts of interest statement
No conflict of interest was declared.
Funding
There was no external funding for this study.
Author contributions
T. A. contributed to study conception, study design, literature search, data collection, data analysis and interpretation and drafted the first manuscript. A. P. K. contributed to study conception, study design and data analysis and critically reviewed the first draft manuscript. A. D. V. and T. P. contributed to study design and critically reviewed the manuscript. All the authors read and approved the final version of the manuscript.
Supporting information
Table S1. Search strategy for PubMed
Table S2. PRISMA checklist
Table S3. Summary of the quality scores of the included studies
Table S4. Summary statistics from meta‐analyses of prevalence studies of overweight in African school going children using random effects model and arcsine transformations
Table S5. Summary statistics from meta‐analyses of prevalence studies of obesity in African school going children using random effects model and arcsine transformations
Fig S1. Forest plot showing the effect of omitting one study at a time on pooled prevalence and heterogeneity statistics from studies that used World Health Organisation (WHO) criteria to diagnose prevalent obesity (first panel) and overweight (second panel) in African school learners
Fig S2. Forest plot showing the effect of omitting one study at a time on pooled prevalence and heterogeneity statistics from studies that used International Obesity Task Force (IOTF, upper panels) and Centre for Diseases Control (CDC, lower panels) criteria to diagnose prevalent obesity (left panels) and overweight (right panels) in African school learners
Fig S3. Funnel plots for the assessment of publication bias in studies of prevalent overweight (upper panels) and obesity (lower panels) by the World Health organisation (left column), International Obesity Task Force (middle column) and Centre for Diseases Control (right column) criteria, in African school going children, after implementation of the trim & fill methods to correct for publication bias.
Fig. S4. Forest plots showing the effect of studies imputations on pooled prevalence estimates from trim and fill methods, for studies that used the World Health Organisation (WHO) criteria to diagnose obesity (first panel) or overweight (second panel) in African school going children
Fig. S5. Forest plots showing the effect of studies imputations on pooled prevalence estimates from trim and fill methods, for studies that used the International Obesity Task Force (IOTF, upper panels) or Centre for Diseases Control (CDC, lower panels) criteria to diagnose obesity (left panels) or overweight (right panels) in African school going children
Fig. S6. Prevalence of overweight by major diagnostic criteria in boys. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig.S7. Prevalence of overweight by major diagnostic criteria in girls. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig S8. Prevalence of obesity by major diagnostic criteria in boys. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S9. Prevalence of obesity by major diagnostic criteria in girls. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S10. Prevalence of overweight by major diagnostic criteria in urban studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S11. Prevalence of overweight by major diagnostic criteria in rural studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S12. Prevalence of overweight by major diagnostic criteria in urban and rural studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S13. Prevalence of obesity by major diagnostic criteria in urban studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S14. Prevalence of obesity by major diagnostic criteria in rural studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S15. Prevalence of overweight by major diagnostic criteria in public schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S16. Prevalence of overweight by major diagnostic criteria in private schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S17. Prevalence of obesity by major diagnostic criteria in public schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S18. Prevalence of obesity by major diagnostic criteria in private schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Acknowledgement
The authors are grateful to Ms Yaa Pokuaa Akomea for her contributions towards the literature search and selection of relevant articles.
Adom T., Kengne A. P., De Villiers A., and Puoane T. (2019) Prevalence of overweight and obesity among African primary school learners: a systematic review and meta‐analysis, Obesity Science & Practice. 5:487–502.doi: 10.1002/osp4.355.
References
- 1. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980‐2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781. 10.1016/s0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. de Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr 2010; 92: 1257–1264. 10.3945/ajcn.2010.29786.1. [DOI] [PubMed] [Google Scholar]
- 3. Wang Y, Lim H. The global childhood obesity epidemic and the association between socio‐economic status and childhood obesity. Int Rev Psychiatry 2012; 24: 176–188. 10.3109/09540261.2012.688195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. UNICEF , World Health Organization , World Bank Group . Levels and trends in child malnutrition. 2016:1‐8. 10.1016/S0266-6138(96)90067-4. [DOI]
- 5. Wabitsch M, Moss A, Kromeyer‐hauschild K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med 2014; 12: 17 http://www.biomedcentral.com/1741‐7015/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McLeroy K, Bibeau D, Steckler A, Glanz K. An Ecological Perspective on Health Promotion Programs. Health Educ Q 1988; 15: 351–377. [DOI] [PubMed] [Google Scholar]
- 7. Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005‐2008. NCHS Data Brief 2010; 127: 1–8. 10.1001/archsurg.138.4.354. [DOI] [PubMed] [Google Scholar]
- 8. Gupta N, Goel K, Shah P, Misra A. Childhood obesity in developing countries: Epidemiology, determinants, and prevention. Endocr Rev 2012; 33: 48–70. 10.1210/er.2010-0028. [DOI] [PubMed] [Google Scholar]
- 9. Hawkins S, Cole TJ, Law C. The Millennium Cohort Study Child Health Group. Maternal employment and early childhood overweight: findings from the UK Millennium Cohort Study. Int J Obes (Lond) 2008; 32: 30–38. 10.1038/sj.ijo.0803682.Maternal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Keane E, Layte R, Harrington J, Kearney PM, Perry IJ. Measured parental weight status and familial socio‐economic status correlates with childhood overweight and obesity at age 9. PLoS ONE 2012; 7: e43503 10.1371/journal.pone.0043503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mâsse LC, de Niet‐Fitzgerald J, Watts AW, Naylor P‐J, Saewyc EM. Associations between the school food environment, student consumption and body mass index of Canadian adolescents. Int J Behav Nutr Phys Act 2014; 11: 29 10.1186/1479-5868-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Morton KL, Atkin AJ, Corder K, Suhrcke M, van Sluijs EMF. The school environment and adolescent physical activity and sedentary behaviour: A mixed‐studies systematic review. Obes Rev 2016; 17: 142–158. 10.1111/obr.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev 2007; 29: 129–143. [DOI] [PubMed] [Google Scholar]
- 14. Cummins S, Macintyre S. Food environments and obesity ‐ Neighbourhood or nation? Int J Epidemiol 2006; 35: 100–104. 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 15. Reilly JJ, Kelly J. Long‐term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int J Obes (Lond) 2011; 35: 891–898. 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 16. Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev 2008; 9: 474–488. 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 17. Noubiap JJ, Essouma M, Bigna JJ, Jingi AM, Aminde LN, Nansseu JR. Prevalence of elevated blood pressure in children and adolescents in Africa: a systematic review and meta‐analysis. Lancet Public Health 2017; 2: e375–e386. 10.1016/S2468-2667(17)30123-8. [DOI] [PubMed] [Google Scholar]
- 18. Agyemang C, Redekop WK, Owusu‐Dabo E, Bruijnzeels M. a. Blood pressure patterns in rural, semi‐urban and urban children in the Ashanti region of Ghana, West Africa. BMC Public Health 2005; 5: 114 10.1186/1471-2458-5-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Muthuri SK, Francis CE, Wachira L‐JM, et al. Evidence of an Overweight/Obesity Transition among School‐Aged Children and Youth in Sub‐Saharan Africa: A Systematic Review. PLoS ONE 2014; 9: 1–26. 10.1371/journal.pone.0092846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school‐aged children and adolescents. Bull World Health Organ 2007; 85: 812–819. 10.2471/BLT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kuczmarski R, Ogden CL, Guo S, Grummer‐Strawn L, Flegal K, Al E. CDC Growth Charts for the United States: methods and development. Vital Health Stat 2000: 1–190. https://www.cdc.gov/growthcharts/2000growthchart‐us.pdf. [PubMed] [Google Scholar]
- 22. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1–6. 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adom T, Puoane T, De Villiers A, Kengne AP. Prevalence of obesity and overweight in African learners: a protocol for systematic review and meta‐analysis. BMJ Open 2017; 7: e013538 10.1136/bmjopen-2016-013538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non‐randomized studies of health care interventions. J Epidemiol Community Health 1998; 52: 377–384. 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta‐analysis of prevalence. J Epidemiol Community Health 2013; 67: 974–978. 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 26. Dersimonian R, Laird N. Meta‐Analysis in Clinical Trials*. Stat Med 1986; 188: 177–188. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 27. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ Br Med J 2003; 327: 557–560. 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Egger M, Smith GD, Schneider M, Minder C. Bias in meta analysis detected by a simple , graphical test. BMJ 1997; 14: 1–16. 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Abrahams Z, de Villiers A, Steyn NP, et al. What's in the lunchbox? Dietary behaviour of learners from disadvantaged schools in the Western Cape, South Africa. Public Health Nutr 2011; 14: 1752–1758. 10.1017/s1368980011001108. [DOI] [PubMed] [Google Scholar]
- 30. Amidu N, Owiredu WKBA, Saaka M, et al. Determinants of childhood obesity among basic school children aged 6 – 12 years in Tamale Metropolis. J Med Biomed Sci 2013; 2: 26–34. [Google Scholar]
- 31. Armstrong ME, Lambert MI, Sharwood KA, Lambert EV. Obesity and overweight in South African primary school children ‐ the Health of the Nation Study. S Afr Med J 2006; 96: 439–444. [PubMed] [Google Scholar]
- 32. Boukthir S, Essaddam L, Mazigh Mrad S, et al. Prevalence and risk factors of overweight and obesity in elementary schoolchildren in the metropolitan region of Tunis, Tunisia. Tunis Med 2011; 89: 50–54. [PubMed] [Google Scholar]
- 33. Caleyachetty R, Rudnicka AR, Echouffo‐Tcheugui JB, Siegel KR, Richards N, Whincup PH. Prevalence of overweight, obesity and thinness in 9‐10 year old children in Mauritius. Glob Heal 2012; 8: 28 10.1186/1744-8603-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chebet M, Goon DT, Nsibambi C, Otala J. Prevalence of overweight and obesity among primary school children in Kampala central, Uganda. AJPHERD 2014; 20: 1365–1378. [Google Scholar]
- 35. Daboné C, Delisle HF, Receveur O. Poor nutritional status of schoolchildren in urban and peri‐urban areas of Ouagadougou (Burkina Faso). Nutr J 2011; 10: 34 10.1186/1475-2891-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dekkaki IC, Mouane N, Ettair S, Meskini T, Bouklouze A, Barkat A. Prevalence of obesity and overweight in children: A study in government primary schools in rabat, Morocco. Arch Med Res 2011; 42: 703–708. 10.1016/j.arcmed.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 37. El‐Sabely AA, Tork HMM, Hussien YE. Comparative Study of Nutritional Status and Dietary Habits of Children from Public and Private Primary Schools in Zagazig City, Egypt. IOSR J Nurs Heal Sci 2013; 3: 47–52. [Google Scholar]
- 38. Fetuga MB, Ogunlesi TA, Adekanmbi AF, Alabi AD. Nutritional Status of Semi‐Urban Nigerian School Children using the 2007 WHO Reference Population. West Afr J Med 2011; 30: 331–336. http://www.ncbi.nlm.nih.gov/pubmed/22752820. [PubMed] [Google Scholar]
- 39. Hassan NE, El‐Masry SA, El‐Sawaf AE. Waist circumference and central fatness of Egyptian primary‐school children. East Mediterr Health J 2008; 14: 916–925. [PubMed] [Google Scholar]
- 40. Jinabhai CC, Taylor M, Sullivan KR. Changing patterns of under‐ and over‐nutrition in South African children ‐ future risks of non‐communicable diseases. Ann Trop Paediatr 2005; 25: 3–15. 10.1179/146532805X23290. [DOI] [PubMed] [Google Scholar]
- 41. Jinabhai CC, Taylor M, Sullivan KR. Implications of the prevalence of stunting, overweight and obesity amongst South African primary school children: a possible nutritional transition? Eur J Clin Nutr 2003; 57: 358–365. 10.1038/sj.ejcn.1601534. [DOI] [PubMed] [Google Scholar]
- 42. Kirsten AP, Marais D, Schübl C. The influence of socio‐demographic factors on the nutritional status of children in the Stellenbosch area , Western Cape. S Afr J Clin Nutr 2013; 26: 124–131. [Google Scholar]
- 43. Kyallo F, Makokha A, Mwangi AM. Overweight and obesity among public and private primary school children in Nairobi, Kenya. Health (Irvine Calif) 2013; 5: 85–90. 10.4236/health.2013.58A3012. [DOI] [Google Scholar]
- 44. Maruf FA, Aronu U, Chukwuegbu K, Aronu AE. Influence of gender on prevalence of overweight and obesity in Nigerian schoolchildren and adolescents. Tanzan J Health Res 2013; 15: 247–251. [DOI] [PubMed] [Google Scholar]
- 45. McKersie JM, Baard ML. Body mass index and associated physical activity levels in 7 ‐ 10‐year‐old children in primary schools in Port Elizabeth. South African J Sport Med 2014; 26: 115–118. 10.7196/SAJSM.551. [DOI] [Google Scholar]
- 46. Mogre V, Gaa PK, Nagumsi R, Abukari S. Overweight , Obesity and Thinness and Associated Factors Among School‐ Aged Children (5‐14 Years) in Tamale. Eur Sci J 2013; 9: 160–175. [Google Scholar]
- 47. Mohammed H, Vuvor F. Prevalence of childhood overweight/obesity in basic school in Accra. Ghana Med J 2013/05/11 2012; 46: 124–127. [PMC free article] [PubMed] [Google Scholar]
- 48. Moselakgomo VK, Monyeki MA, Toriola AL. Relationship between physical activity and risk factors of body weight disorders among south African primary school children. Biomed Res 2015; 26: 730–738. [Google Scholar]
- 49. Mosha TC, Fungo S. Prevalence of overweight and obesity among children aged 6‐12 years in Dodoma and Kinondoni municipalities, Tanzania. Tanzan J Health Res 2010; 12: 6–16. [DOI] [PubMed] [Google Scholar]
- 50. Mpembeni RN, Muhihi AJ, Maghembe M, et al. Overweight, obesity and perceptions about body weight among primary schoolchildren in Dar es Salaam. Tanzania Tanzan J Heal Res 2014; 16: 304–311. [DOI] [PubMed] [Google Scholar]
- 51. Muhihi AJ, Mpembeni RNM, Njelekela MA, et al. Prevalence and determinants of obesity among primary school children in Dar es Salaam, Tanzania. Arch Public Heal 2013; 71: 26 10.1186/0778-7367-71-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Muthuri SK, Wachira LM, Onywera VO, Tremblay MS. Correlates of objectively measured overweight/obesity and physical activity in Kenyan school children: results from ISCOLE‐Kenya. BMC Public Health 2014; 14: 1–11. 10.1186/1471-2458-14-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mwaikambo SA, Leyna GH, Killewo J, Simba A, Puoane T. Why are primary school children overweight and obese? A cross sectional study undertaken in Kinondoni district, Dar‐es‐salaam. BMC Public Health 2015; 15: 1269 10.1186/s12889-015-2598-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Navti LK, Ferrari U, Tange E, Bechtold‐Dalla Pozza S, Parhofer KG. Contribution of socioeconomic status, stature and birth weight to obesity in Sub‐Saharan Africa: cross‐sectional data from primary school‐age children in Cameroon. BMC Public Health 2014; 14: 320 10.1186/1471-2458-14-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Oldewage‐Theron WH, Egal AA. Nutrition knowledge and nutritional status of primary school children in QwaQwa. South African J Clin Nutr 2010; 23: 149–154. [Google Scholar]
- 56. Pangani IN, Kiplamai FK, Kamau JW, Onywera VO. Prevalence of Overweight and Obesity among Primary School Children Aged 8–13 Years in Dar es Salaam City, Tanzania. Adv Prev Med 2016; 2016: 1–5. 10.1155/2016/1345017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pedro T, Kahn K. Under‐ and overnutrition and evidence of metabolic disease risk in rural black South African children and adolescents. S Afr J Clin Nutr 2014; 27: 194–200. [Google Scholar]
- 58. Pienaar AE. Prevalence of overweight and obesity among primary school children in a developing country: NW‐CHILD longitudinal data of 6–9‐yr‐old children in South Africa. BMC Obes 2015; 2: 2 10.1186/s40608-014-0030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Prista A, Maia JAR. Damasceno A and BG. Anthropometric indicators of nutritional status : implications for fitness, activity, and health in school‐age children and adolescents. Am J Clin Nutr 2003; 77: 952–959. [DOI] [PubMed] [Google Scholar]
- 60. Puckree T, Naidoo P, Pillay P, Naidoo T. Underweight and overweight in primary school children in eThekwini district in kwazulu‐Natal, South Africa. African J Prim Heal Care Fam Med 2011; 3: 1–6. 10.4102/phcfm.v3i1.203. [DOI] [Google Scholar]
- 61. Regaieg S, Charfi N, Trabelsi L, et al. Prevalence and risk factors of overweight and obesity in a population of school children in urban areas Sfax, Tunisia. Pan Afr Med J 2014; 17: 57 10.11604/pamj.2014.17.57.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Salman Z, Kirk GD, DeBoer MD. High Rate of Obesity‐Associated Hypertension among Primary Schoolchildren in Sudan. Int J Hypertens 2011; 2011: 1–5. 10.4061/2011/629492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sebbani M, Elbouchti I, Adarmouch L, Amine M. Prevalence of obesity and overweight among children in primary schools in Marrakech, Morocco. Rev Epidemiol Sante Publique 2013; 61: 545–549. 10.1016/j.respe.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 64. Taleb S, Oulamara H, Agli AN. Prevalence of overweight and obesity in schoolchildren in Tebessa (Algeria) between 1998 and 2005. East Mediterr Health J 2010; 16: 746–751. [PubMed] [Google Scholar]
- 65. Tathiah N, Moodley I, Mubaiwa V, Denny L, Taylor M. South Africa's nutritional transition: overweight, obesity, underweight and stunting in female primary school learners in rural KwaZulu‐Natal, South Africa. S Afr Med J 2013; 103: 718–723. 10.7196/samj.6922. [DOI] [PubMed] [Google Scholar]
- 66. Truter L, Pienaar AE, Du Toit D. The relationship of overweight and obesity to the motor performance of children living in South Africa. S Afr Fam Pract 2012; 54: 429–435. 10.1080/20786204.2012.10874266. [DOI] [Google Scholar]
- 67. van den Ende C, Twisk JW, Monyeki KD. The relationship between BMI and dietary intake of primary school children from a rural area of South Africa: The Ellisras longitudinal study. Am J Hum Biol 2014; 26: 701–706. 10.1002/ajhb.22585. [DOI] [PubMed] [Google Scholar]
- 68. Wiles NL, Green JMVF. Tuck‐shop purchasing practices of Grade 4 learners in Pietermaritzburg and childhood overweight and obesity. S Afr J Clin Nutr 2013; 26: 37–42. [Google Scholar]
- 69. Negash S, Agyemang C, Matsha TE, Peer N, Erasmus RT, Kengne AP. Differential prevalence and associations of overweight and obesity by gender and population group among school learners in South Africa: a cross‐sectional study. BMC Obes 2017; 4: 29 10.1186/s40608-017-0165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in Obesity Prevalence by Demographics and Urbanization in US Children and Adolescents, 2013‐2016. JAMA 2018; 319: 2410–2418. 10.1001/jama.2018.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Song Y, Wang H‐J, Dong B, Ma J, Wang Z, Agardh A. 25‐year trends in gender disparity for obesity and overweight by using WHO and IOTF definitions among Chinese school‐aged children: a multiple cross‐sectional study. BMJ Open 2016; 6: e011904 10.1136/bmjopen-2016-011904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Chirita‐Emandi A, Barbu CG, Cinteza EE, Chesaru BI, Gafencu M, Mocanu V. Overweight and Underweight Prevalence Trends in Children from Romania – Pooled Analysis of Cross‐Sectional Studies between 2006 and 2015. Obes Facts 2016; 9: 206–220. 10.1159/000444173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Wang VH, Min J, Xue H, et al. What factors may contribute to sex differences in childhood obesity prevalence in China? Public Health Nutr 2018; 21: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. O'Dea JA. Gender, ethnicity, culture and social class influences on childhood obesity among Australian schoolchildren: Implications for treatment, prevention and community education. Health Soc Care Community 2008; 16: 282–290. 10.1111/j.1365-2524.2008.00768.x. [DOI] [PubMed] [Google Scholar]
- 75. The GBD . 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med 2017; 377: 13–27. 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: A problem of the rich or the poor? BMC Public Health 2009; 9: 465 10.1186/1471-2458-9-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Mokhtar N, Elati J, Chabir R, et al. Diet Culture and Obesity in Northern Africa. J Nutr 2001; 131: S887–S892. [DOI] [PubMed] [Google Scholar]
- 78. Muthuri SK, Wachira LJ, Onywera VO, Tremblay MS. Correlates of objectively measured overweight/obesity and physical activity in Kenyan school children: results from ISCOLE‐Kenya. BMC Public Health 2014; 14: 436 10.1186/1471-2458-14-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hemmingsson E, Johansson K, Reynisdottir S. Effects of childhood abuse on adult obesity : a systematic review and meta‐analysis. Obes Rev 2014; 15: 1–12. 10.1111/obr.12216. [DOI] [PubMed] [Google Scholar]
- 80. Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta‐analysis. Mol Psychiatry 2014; 19: 544–554. 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- 81. Hawton K, Norris T, Crawley E, Bch BM, Shield JPH, Chb MB. Is Child Abuse Associated with Adolescent Obesity? A Population Cohort Study. Child Obes 2018; 14: 1–8. 10.1089/chi.2017.0141. [DOI] [PubMed] [Google Scholar]
- 82. Yu Z, Han S, Chu J, Xu Z, Zhu C, Guo X. Trends in Overweight and Obesity among Children and Adolescents in China from 1981 to 2010: A Meta‐Analysis. PLoS ONE 2012; 7 10.1371/journal.pone.0051949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Fruhstorfer BH, Mousoulis C, Uthman OA, Robertson W. Socio‐economic status and overweight or obesity among school‐age children in sub‐Saharan Africa ‐ a systematic review. Clin Obes 2016; 6: 19–32. 10.1111/cob.12130. [DOI] [PubMed] [Google Scholar]
- 84. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012; 70: 3–21. 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Akombi BJ, Agho KE, Hall JJ, Wali N, Renzaho AMN, Merom D. Stunting, wasting and underweight in Sub‐Saharan Africa: A systematic review. Int J Environ Res Public Health 2017; 14: 1–18. 10.3390/ijerph14080863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Johnson JA, Johnson AM. Urban‐Rural Differences in Childhood and Adolescent Obesity in the United States: A Systematic Review and Meta‐Analysis. Child Obes 2015; 11: 233–241. 10.1089/chi.2014.0085. [DOI] [PubMed] [Google Scholar]
- 87. WHO . Report of the commission on ending childhood obesity. 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Search strategy for PubMed
Table S2. PRISMA checklist
Table S3. Summary of the quality scores of the included studies
Table S4. Summary statistics from meta‐analyses of prevalence studies of overweight in African school going children using random effects model and arcsine transformations
Table S5. Summary statistics from meta‐analyses of prevalence studies of obesity in African school going children using random effects model and arcsine transformations
Fig S1. Forest plot showing the effect of omitting one study at a time on pooled prevalence and heterogeneity statistics from studies that used World Health Organisation (WHO) criteria to diagnose prevalent obesity (first panel) and overweight (second panel) in African school learners
Fig S2. Forest plot showing the effect of omitting one study at a time on pooled prevalence and heterogeneity statistics from studies that used International Obesity Task Force (IOTF, upper panels) and Centre for Diseases Control (CDC, lower panels) criteria to diagnose prevalent obesity (left panels) and overweight (right panels) in African school learners
Fig S3. Funnel plots for the assessment of publication bias in studies of prevalent overweight (upper panels) and obesity (lower panels) by the World Health organisation (left column), International Obesity Task Force (middle column) and Centre for Diseases Control (right column) criteria, in African school going children, after implementation of the trim & fill methods to correct for publication bias.
Fig. S4. Forest plots showing the effect of studies imputations on pooled prevalence estimates from trim and fill methods, for studies that used the World Health Organisation (WHO) criteria to diagnose obesity (first panel) or overweight (second panel) in African school going children
Fig. S5. Forest plots showing the effect of studies imputations on pooled prevalence estimates from trim and fill methods, for studies that used the International Obesity Task Force (IOTF, upper panels) or Centre for Diseases Control (CDC, lower panels) criteria to diagnose obesity (left panels) or overweight (right panels) in African school going children
Fig. S6. Prevalence of overweight by major diagnostic criteria in boys. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig.S7. Prevalence of overweight by major diagnostic criteria in girls. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig S8. Prevalence of obesity by major diagnostic criteria in boys. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S9. Prevalence of obesity by major diagnostic criteria in girls. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S10. Prevalence of overweight by major diagnostic criteria in urban studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S11. Prevalence of overweight by major diagnostic criteria in rural studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S12. Prevalence of overweight by major diagnostic criteria in urban and rural studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S13. Prevalence of obesity by major diagnostic criteria in urban studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S14. Prevalence of obesity by major diagnostic criteria in rural studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S15. Prevalence of overweight by major diagnostic criteria in public schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S16. Prevalence of overweight by major diagnostic criteria in private schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S17. Prevalence of obesity by major diagnostic criteria in public schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.
Fig. S18. Prevalence of obesity by major diagnostic criteria in private schools studies. Black boxes represent the effect estimates (prevalence) and the horizontal bars about are for the 95% confidence intervals (CIs). The diamond is for the pooled effect estimate and 95% CI.


