Abstract
Purpose.
Childbirth is a life-transforming event often followed by a time of heightened psychological vulnerability in the mother. There is growing recognition of the importance of obstetrics aspects in maternal wellbeing with the way of labor potentially influencing psychological adjustment following parturition or failure thereof. Empirical scrutiny on the association between mode of delivery and postpartum wellbeing remains limited.
Methods.
We studied 685 women who were on average three months following childbirth and collected information concerning mode of delivery and pre- and postpartum mental health.
Results.
Analysis of variance revealed that women who had cesarean section or vaginal instrumental delivery had higher somatization, obsessive compulsive, depression, and anxiety symptom levels than those who had natural or vaginal delivery as well as overall general distress, controlling for pre-morbid mental health, maternal age, education, primiparity, and medical complication in newborn. Women who underwent unplanned cesarean also had higher levels of childbirth-related PTSD symptoms excluding those with vaginal instrumental. The risk for endorsing psychiatric symptoms reflecting clinically relevant cases increased by 2-fold following unplanned cesarean and was 3-fold for probable childbirth-related PTSD.
Conclusions.
Maternal wellbeing following childbirth is associated with the experienced mode of delivery. Increasing awareness in routine care of the implications of operative delivery and obstetric interventions in delivery on a woman’s mental health is needed. Screening at-risk women could improve the quality of care and prevent enduring symptoms. Research is warranted on the psychological and biological factors implicated in the mode of delivery and their role in postpartum adjustment.
Keywords: Delivery Mode, Childbirth, Mental Health, Postpartum Depression, Postpartum PTSD
Introduction
Childbirth is a complex event. Although viewed as uniformly happy, the rapid psychophysiological changes during birth may render it stressogenic. About 85% of postpartum women experience some mood disturbance, which is usually short-lived and remits spontaneously (O’Hara et al. 1990; Reck et al. 2009). A considerable number of women are likely to suffer from more enduring symptoms subsequently manifested in various postpartum psychiatric illness (Campbell et al. 1992; O’Hara et al. 1991). While postpartum depression (PPD) is the most documented complication of childbirth (Dekel et al. 2019), current research shows other conditions can also occur, including anxiety and posttraumatic-stress related disorders (Ayers and Ford 2016; Dekel et al. 2017). Psychological disturbance in the mother can impair her functioning and wellbeing but also the mother-infant bond (Dekel et al. 2018; Moehler et al. 2006) and adversely modify the developmental trajectory of the offspring (Cicchetti et al. 1998; Petterson and Albers 2001). Postpartum psychopathology increases vulnerability to mental illness in the adult offspring (Netsi et al. 2018; Yehuda et al. 2008). These considerations raise the specter of intergenerational disease transmission with heavy public health costs.
In accord with a diathesis-stress model, individual characteristics must combine with an external stressor that is intense enough to trigger an illness (McKeever and Huff 2003). While premorbid (e.g., younger age, primiparity, history of mental illness) and peripartum factors (e.g., medical complications in the newborn) may increase risk for postpartum psychopathology (Andersen et al. 2012; Ayers et al. 2016), the possibility that the way of labor affects a woman’s psychological state has received growing attention. It has been suggested that obstetrics interventions in delivery – determined for life-saving purpose for mother and child – may negative effect mother’s wellbeing however empirical evidence remains inconclusive.
Existing studies document that cesarean delivery is associated with postpartum mental health disturbance mainly evident in PPD (Lobel and DeLuca, 2007). These findings may suggest a serious concern for obstetrics care, as cesarean rates are estimated at 32% in the US, exceeding the 15% rate considered the highest acceptable by the World Health Organization (Betràn et al. 2016). Higher prevalence of PPD symptoms above the suggested clinical cutoff score has been noted among women who underwent operations in comparison to those who had delivered infants vaginally (Chang et al. 2015; Chen et al. 2017; Rauh et al. 2012). Lowered sense of control and violation of childbirth expectations as well as disrupted regulation of oxytocin secretion in birth has been hypothesized to lower maternal mood (Chen et al. 2017; Lobel and DeLuca 2007).
In contrast, a body of other studies reveals no evidence that cesarean delivery increases the risk for mood disturbance assessed as far as the first postpartum year. This has been reported in a meta-analysis of 24 studies with over 27,000 postpartum women (Carter et al. 2006). For example, Murray and Cartwright (1993) show that pre-existing differences between women who have cesarean versus vaginal may account for the presumably negative affect of mode of delivery on maternal mental health. Post-delivery stressors that have to do with health complications in the newborn and are often seen in operative delivery may also account for the relationship (Villar et al. 2007).
Finally, a few studies suggest that cesarean delivery may actually protect from adverse postpartum psychological outcomes. Women undergoing vaginal delivery reported higher PPD symptoms than those who had a cesarean assessed several months post-birth (Chaaya et al 2002, Olieman et al., 2017). This has been hypothesized to be due to prenatal preparation for surgery and increase support after birth.
An important factor to consider is the various psychiatric outcomes manifested in the postpartum period (Brockington 2004). Previous studies mainly focused on PPD and therefore less is known about the role of delivery mode in relation to anxiety and stress-related postpartum conditions. Moreover, existing research often examined postpartum outcomes by contrasting women following cesareans and vaginal deliveries (e.g., Mathisen et al. 2013; Sadat et al. 2014; Sword et al. 2011). Knowledge of postpartum mental health outcomes in relation to subtypes of delivery modes (i.e., planned vs. unplanned cesarean, and vaginal vs. instrumental vaginal) (e.g., Rowlands and Redshaw 2012), which each may involve different birth experiences, is limited.
To this end, we studied a large sample of women in the first months following birth, including some women who endorsed psychiatric symptoms in the postpartum period. We focused our analysis on the question of whether women who undergo different mode of deliveries also differ in regard to their mental health state following parturition. And second, whether differences in postpartum mental health exist even after accounting for possible confounding factors.
Materials and Methods
Participants
This study is part of a larger project on childbirth and psychological sequelae. Women who gave birth to a live baby in the last six months were recruited through web announcements on websites including postpartum-related sites (e.g., Postpartum Support) between November 2016 and April 2017. Exclusion criteria included stillbirth and being younger than 18 years of age. Women completed an anonymous survey in English concerning their childbirth and pre- and postpartum mental health. Partners Human Research Committee (PHRC) granted the project exemption (see, Dekel et al. 2018, for detailed information about the study sample).
846 women agreed to participate and among them 94% met inclusion criteria (N=795). We excluded a further 110 participants from the data set due to non-response on most measures, leaving a final sample of 685 women. This sample included women who on average were 31 years old (SD=4.80) and three months postpartum (SD=1.5). Around half were primiparas (56%). The majority had a planned pregnancy (74%), delivered at-term a healthy baby (79%), were also married (93%), had at least college education (71%), were middle class (median household income = $50,000 - $99,000), and resided in North America (66%).
Measures
Postpartum psychiatric symptoms were assessed with the commonly used Brief Symptom Inventory (BSI) targeting 53 symptoms and comprising 9 symptom clusters (somatization, obsessive compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) (Derogatis 1993). The inventory measures symptom intensity during the past week on a 5-point scale (0 – 4). It has adequate properties (Derogatis 1993) and used in postpartum samples (Örün et al. 2013; Ross et al. 2003). Reliability for the symptoms clusters was good (α between 0.77 and 0.92). We defined probable clinical cases as a score of 9 >= on at least two clusters (depression, anxiety, or obsessive compulsive) (Biggs et al. 2017). We calculated a single composite score of all items, i.e., the Global Severity Index (GSI), for global psychological distress.
Childbirth-related posttraumatic stress was assessed with the widely used PTSD checklist for DSM-5 (PCL-5; Weathers et al. 2013), with “recent childbirth” as the index event. This 20- item measures PTSD symptoms and their intensity over the past month on a 5-point scale (0 – 4). It has good psychometrics (Blevins et al. 2015), and has been used in postpartum samples (Scheepstra et al. 2017; Stramrood and Slade 2017; Van Heumen et al. 2018). In this study reliability was high (α = 0.95). Conforming to DSM-5 symptom criteria, probable childbirth-related PTSD was defined as symptom intensity of 2 >= to include at least 1 intrusion, 1 avoidance, 2 alterations in cognitions and mood, and 2 reactivity and hyperarousal.
Childbirth and demographic information was assessed using single items for the purpose of this study, including age, education, income, primiparity, gestation week, mode of delivery (natural delivery, i.e., without routine medical interventions including anesthesia; vaginal delivery; instrumental vaginal delivery, i.e., forceps-assisted delivery or vacuum-assisted delivery; planned or unplanned caesarean section), health complications in newborn resulting in neonatal intensive care (NICU) admission, and mental health problems before childbirth (mainly depression, anxiety, PTSD).
Statistical Analysis
Pattern of missing data was estimated using Little’s Missing Completely At Random (MCAR) test and handled using Multiple Imputation (Rubin 2009) where all variables were included. Analyses were performed with SPSS v.21. Differences in postpartum symptom severity by delivery mode were estimated using a multivariate analysis of variance (MANOVA) and an analysis of variance (ANOVA). We also employed multivariate analysis of covariate (MANCOVA) and analysis of covariance (ANCOVA) to assess the stability of these differences taking into account the contribution of age, primiparity (0 = no, 1 = yes), education level, general mental health problems before birth (0 = no, 1 = yes), premorbid-depression (0 = no, 1 = yes), anxiety (0 = no, 1 = yes), and PTSD (PTSD; 0 = no, 1 = yes), PPD (0 = no, 1 = yes), other premorbid mental health conditions (0 = no, 1 = yes), and medical complications in newborn (0 = no, 1 = yes). Šidák post-hoc analyses (Abdi 2007; Šidák 1967) were used to examine the source of significant differences. The MANOVA was followed by discriminant analysis (also known as canonical regression) to examine the relative difference between delivery groups by different symptom cluster. Differences in the prevalence of estimated clinically relevant cases of probable postpartum psychopathology and childbirth-related PTSD was examined by chi-square test for independence of measures, with Fisher’s exact test to estimate significance and relative risk to estimate effect size.
Results
8.6% of the data were missing; out of the total of 685 participants, 99.4% had 1 to 20 items missing (Mdn = 4 items; 0.6% of the sample had complete data in all variables). Little’s MCAR test had indicated that the data were missing completely at random, χ2(2654) = 1642.80, p = 1.00. To handle missing data, we used Multiple Imputation (Rubin 2009) with 10 imputed datasets.
Differences in mental health outcomes symptoms by mode of delivery
22.2% (N = 152) of participants had natural delivery (ND), 34.7% (N = 238) vaginal delivery (VD), 7.2% (N = 49) instrumental vaginal delivery (IVD), 19.3% (N = 132) planned cesarean section (PCS), and 16.6% (N = 114) unplanned caesarean section (UPCS). Groups differed on primiparity (χ2(4) = 66.51, p < .001), newborn complications (χ2(4) = 33.70, p < .001), and age (F(4,680) = 4.17, p = .002).
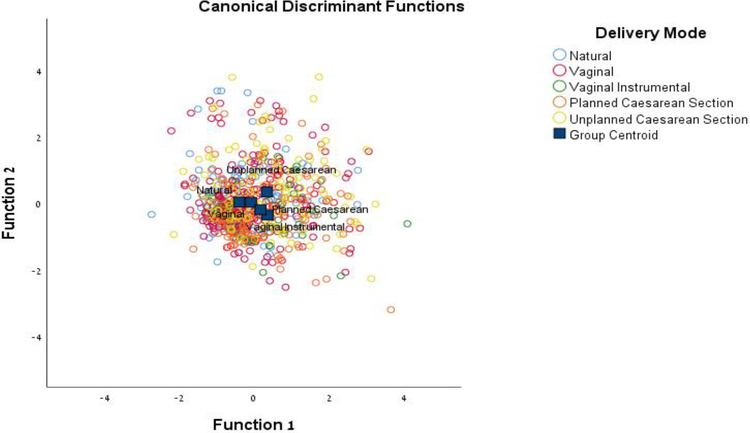
We examined differences in psychopathology-related symptoms (somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) severity by delivery mode by employing MANOVA followed by discriminant analysis (Table 1).
Table 1.
Means, standard deviations, univariate statistics and effect sizes for differences in postpartum psychopathology-related symptoms severity by delivery mode
| Natural | Vaginal | Assisted | Planned Cesarean | Unplanned Cesarean | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | F(4, 680) | ɳ2p | |
| Somatization | 0.54b | 0.68 | 0.66b, c | 0.67 | 0.90c | 0.77 | 0.87c | 0.67 | 0.93a, c | 0.87 | 7.42*** | .042 |
| Obsessive compulsive | 1.02b | 1.02 | 1.30 | 1.04 | 1.29 | 1.06 | 1.31 | 1.12 | 1.61a | 1.17 | 4.72*** | .027 |
| Interpersonal sensitivity | 0.9 9b | 1.00 | 1.27b | 1.10 | 1.30 | 1.19 | 1.28 | 1.11 | 1.66a | 1.28 | 5.78*** | .033 |
| Depression | 0.95b | 0.96 | 1.18b | 1.04 | 1.30 | 1.19 | 1.18b | 1.08 | 1.61a | 1.21 | 6.39*** | .036 |
| Anxiety | 0.77b | 0.86 | 1.04b, c | 0.97 | 1.04 | 0.92 | 1.16c | 0.98 | 1.37a | 1.03 | 6.72*** | .038 |
| Hostility | 0.72b | 0.76 | 0.91 | 0.80 | 0.88 | 0.87 | 0.99a | 0.87 | 1.09a | 0.90 | 3.82** | .022 |
| Phobic anxiety | 0.60b | 0.76 | 0.70b | 0.78 | 0.64 | 0.74 | 0.75 | 0.79 | 1.00a | 0.96 | 4.50*** | 0.26 |
| Paranoid ideation | 0.68 | 0.79 | 0.76 | 0.78 | 0.59 | 0.79 | 0.79 | 0.84 | 0.94 | 0.96 | 2.12 | 0.12 |
| Psychoticism | 0.63b | 0.75 | 0.80b | 0.78 | 0.78b | 0.73 | 0.85b | 0.80 | 1.18a | 0.93 | 7.83*** | 0.44 |
Note.
p < .05,
p < .05,
p < .001.
ɳ2p = partial eta-squared. Means with different superscript letters are significantly different at p < .05 based on Sidak adjustment. For example, the unplanned cesarean group had higher levels of depression compared with all the other groups (except for the planned cesarean group).
The analyses revealed a significant multivariate difference between delivery modes, Pillai’s T = .13, F(36, 2700) = 2.48, p < .0001, such that delivery mode accounted for 13% of the variance in symptoms severity. The analysis highlighted two discriminant functions (1) women who had UPCS, PCS or IVD were higher on somatization, obsessive compulsive, depression, anxiety, and hostility than women who had VD or ND; (2) women who had UPCS tended to be higher than the other groups on psychoticism and paranoid ideation (non-significant trend) (Figure 1).
Fig. 1.
Canonical discriminant functions analysis for examining the differences in postpartum psychopathology-related symptoms severity by delivery mode
We examined the stability of these patterns using MANCOVA adjusting the analysis based on the contribution of maternal age, primiparity, years of education, premorbid general mental health problems, premorbid mental health, and medical complications in newborn. The analysis revealed similar results.
We further conducted an additional one-way ANOVA with Sidak post-hoc analysis to examine differences in childbirth-related PTSD symptoms severity by delivery mode, which revealed significant results, F(4, 680) = 13.11, p < .0001, ɳ2 = .07. Women who had UPCS (M = 30.77, SD = 19.74) had higher PTSD symptom levels than women who did not have UPCS (PCS, M = 23.01, SD = 16.89; VD, M = 19.27, SD = 17.23; ND, M = 16.23, SD = 16.95), excluding the group of women who had VID (M = 25.04, SD = 16.90). Additionally, women who had VID or PCS had higher symptom levels than women who had ND or VD.
An ANCOVA controlling for the contribution of the factors noted above, found slightly different results: women who had gone UPCS had higher PTSD symptoms levels than all any others excluding those who had VID, but there were no significant differences between VID and PCS and the other groups.
Finally, we examined differences between the groups in regard to overall distress using one-way ANOVA with Sidak post-hoc analysis. The analysis was significant, F(4, 680) = 7.07, p < .001, ɳ2 = .04. Women who had UPCS (M = 1.28, SD = 0.88) were higher on GSI than women who had ND (M = 0.77, SD = 0.74) and VD (M = 0.96, SD = 0.75); women who had PCS (M = 1.03, SD = 0.78) were higher on GSI than women who had ND (M = 0.77, SD = 0.74).
Differences in the prevalence of estimated postpartum psychopathology and PTSD
We examined differences in the prevalence of endorsing clinical relevant postpartum cases (based on symptom severity) and probable childbirth-related PTSD. To this end, we conducted a series of chi-square tests for independence of measures with Fisher’s exact test for assessing significance, and relative risk scores for examining the relative risk of women who had UPCS for probable postpartum psychopathology and childbirth-PTSD in comparison to the reset. Results are summarized in Table 2.
Table 2.
Prevalence of childbirth-related PTSD and psychopathology endorsement by delivery mode
| Childbirth-related PTSD | Postpartum Psychopathology | |||||
|---|---|---|---|---|---|---|
| % | RR | χ2 | % | RR | χ2 | |
| Natural | 12.5 | 3.30 (2.05, 5.30) | 43.01*** | 21.1 | 2.13 (1.47,3.07) | 17.06** |
| Vaginal | 14.7 | 2.80 (1.92,4.08) | 31.9 | 1.40 (1.06, 1.85) | ||
| Assisted Vaginal | 24.5 | 1.68 (0.98,2.88) | 30.6 | 1.46 (0.91,2.33) | ||
| Planned cesarean | 17.4 | 2.37 (1.54,3.64) | 33.3 | 1.34 (0.98, 1.84) | ||
| Unplanned cesarean | 41.2 | 44.7 | ||||
Note. Childbirth-related PTSD refers to endorsement of probable PTSD in accord with DSM-5 symptom criteria. Postpartum psychopathology refers to endorsement of depression, anxiety or obsessive compulsive symptoms. RR = relative risk with Unplanned cesarean as the reference group; 95% confidence interval for RR are presented in parenthesis.
p < .01,
p < .001.
The analyses indicated that women who had UPCS are 2.13-times more likely to endorse clinical symptoms than women who had ND, and 1.4-times more likely than women who had VD. Regarding childbirth-related PTSD, we found that women who had UPCS are 3.3-times more likely to endorse probable childbirth-related PTSD than women who had ND, 2.8-times more than women who had VD, and 2.37-times more at risk than women who had PCS.
Discussion
There is a controversy on whether the way of labor affects the psychological adjustment of women following childbirth. To address this issue we studied women who had undergone different modes of delivery and compared their wellbeing in the first postpartum months on various psychiatric outcomes, including symptoms of depression, anxiety, psychosis, and PTSD, and general distress. To better capture the association between mode of delivery and subsequent psychological adjustment, we controlled for the influence of premorbid factors which may affect postpartum adjustment, such as a woman’s mental health before childbirth, primiparity, maternal age as well as medical complications in the newborn.
Here we document across a range of psychiatric outcomes that the mode of delivery is implicated in a woman’s postpartum mental state. Women who had obstetric interventions (i.e., Caesarean or instrumental vaginal) had higher psychological distress following childbirth than women who had natural or vaginal delivery. Poorer psychological health was not limited to depression symptoms but rather obstetric interventions was related to somatization, obsessive compulsive, anxiety-related, and hostility symptoms. We also found that having an unplanned cesarean increases a woman’s vulnerability to suffer from clinically relevant psychiatric problems and probable PTSD evoked by childbirth by as much as three folds, suggesting that a stressogenic childbirth can pose significant threat to maternal wellbeing.
Caesarean sections have become increasingly common in developed and developing countries. Our findings support recommendations of the American College of Obstetricians and Gynecologists (ACOG) to minimize any unnecessary obstetric intervention in birth (American College of Obstetricians and Gynecologists 2017). Previous studies document increased risk following caesareans for severe maternal morbidities, complications in newborn medical health (Castillo-Ruiz et al. 2018; Zanardo et al. 2010), and also risk for complications in psychologically-derived factors such maternal bonding (Rowe-Murray and Fisher 2001). Increased psychological vulnerability following operative delivery may in part account for these negative outcomes.
It has been hypothesized that caesarean involves disruption of the normal labor physiology and the hormonal environment and oxytocin deficiency (Swain et al. 2008). Other related hormones that are mediators of stress reactivity, which peak in labor, such as cortisol (Stjernholm et al. 2016), could be dysregulated in caesarean delivery. A proper hormonal environment which promotes delivery and maternal bonding (Feldman et al. 2007) and mood (Jobst et al. 2016) may facilitate adaptive coping in the wake of the childbirth stressor, and disruption may result in risk for mental health problems, although other biological and psychological factors are likely at work (Dekel et al. 2017; Eckerdal et al. 2018).
The heightened risk of clinically relevant psychiatric symptoms following unplanned caesarean is worth noting. Prevalence of childbirth-related PTSD symptoms at a clinical level was evident in more than 1 out of 3 women. Although not all individuals with clinically relevant PTSD symptoms are likely to meet a PTSD diagnosis, sub-clinical PTSD may interfere with functioning (Marshall et al. 2001) and childbirth-related PTSD may interfere with maternal attachment (Davies et al. 2008; Dekel et al. 2018). A dose-response model underlies PTSD and posits a relationship between event magnitude and clinical outcome (Wyler et al. 1971). Accordingly, the increased risk for probable childbirth-related PTSD among women undergoing unplanned caesarean as others (Ryding et al. 1998; Sӧderquist et al. 2009) and we show here may reflect the magnitude of psychological and as biological stressors. This may relate to perceived (subjective) traumatic appraisal of the birth and acute disruption in biological processes accompanying natural birth.
Several limitations in this study should be noted. The cross-sectional study design does not allow cause and effect conclusions. While we obtained mental health assessment on average around three months postpartum – when symptoms become stable – ideally, we would conduct repeated assessments and collect birth information using medical records. We measured psychiatric symptoms with well-validated measures but did not include a clinical diagnostic assessment. Although we controlled for several factors to capture the link between mode of delivery and mental health, other factors may have been overlooked. Our sample, though large in size, was based on an internet sample. Incidences of clinical relevant cases are likely to be higher than in community.
In conclusion, the experienced mode of delivery appears to have an important role in maternal mental health as assessed in a large sample of women three months following childbirth. In contrast to having a vaginal delivery, obstetric interventions are associated with psychological distress in the mother, and clinically relevant psychiatry-related cases are highly increased following an unplanned cesarean section. Our findings support an holistic approach in perinatal care taking into account also psychological factors when determining obstetrics decisions and benefit vs. risk ratio concerning mother’s health. Monitoring at-risk women following parturition and implementing preventive interventions to lower the rates of postpartum psychological liability is warranted.
Acknowledgments
The authors would like to thank Ms. Shannon Hennig for her generous support in initiating this research project. We also would like to thank Gabriella Dishy for developing the online survey and Philip Mayopoulos for assisting with manuscript editing.
Funding: Dr. Dekel was supported by grant from the National Institute of Child Health and Human Development (R21 HD090396) and an award from the MGH Center for Faculty Development.
Footnotes
Declarations of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Partners (Massachusetts General Hospital) Human Research Committee granted this study exemption.
Informed consent: This study entailed an anonymous online survey, no personal identifiable information was collected. Participants were informed that by agreeing to complete the study survey, they are implying their consent to participate in the study.
References
- Abdi H (2007) Bonferroni and Šidák corrections for multiple comparisons In: Salkind NJ (ed) Encyclopedia of measurement and statistics. Sage, Thousand Oaks, pp. 284–290. [Google Scholar]
- American College of Obstetricians and Gynecologists (2017) Committee opinion No. 687:Approaches to limit intervention during labor and birth. Obstet Gynecol 129(2):e20–e28. 10.1097/AOG.0000000000001905 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association; (2013) Diagnostic and Statistical Manual of Mental Disorders (DSM-5). American Psychiatric Association, Arlington. [Google Scholar]
- Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS (2012) Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand 91(11): 1261–1272. 10.1111/j.1600-0412.2012.01476.x [DOI] [PubMed] [Google Scholar]
- Ayers S, Ford E (2016) Post-traumatic stress during pregnancy and the postpartum period In: Wenzel A (ed) Oxford handbook of perinatal psychology. Oxford University Press, Oxford, pp. 182–200. [Google Scholar]
- Ayers S, Bond R, Bertullies S, Wijma K (2016) The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol Med 46(6):1121–1134. 10.1017/S0033291715002706 [DOI] [PubMed] [Google Scholar]
- Betrán AP, Torloni MR, Zhang JJ, et al. (2016) WHO statement on caesarean section rates. BJOG 123(5):667–670. 10.1111/1471-0528.13526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs MA, Upadhyay UD, McCulloch CE, Foster DG (2017) Women’s mental health and well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry 74(2):169–178. 10.1001/jamapsychiatry.2016.3478 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL (2015) The posttraumatic stress disorder checklist for DSM–5 (PCL–5): development and initial psychometric evaluation. J Trauma Stress 28(6):489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Brockington I (2004) Postpartum psychiatric disorders. Lancet 363(9405):303–310. 10.1016/S0140-6736(03)15390-1 [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, Flanagan C, Popper S, Meyers T (1992) Course and correlates of postpartum depression during the transition to parenthood. Dev Psychopathol 4(1):29–47. 10.1017/S095457940000554X [DOI] [Google Scholar]
- Carter FA, Frampton CM, Mulder RT (2006) Cesarean section and postpartum depression: a review of the evidence examining the link. Psychosom Med 68(2):321–330. 10.1097/01.psy.0000204787.83768.0c [DOI] [PubMed] [Google Scholar]
- Castillo-Ruiz A, Mosley M, Jacobs AJ, Hoffiz YC, Forger NG (2018) Birth delivery mode alters perinatal cell death in the mouse brain. Proc Natl Acad Sci U S A 115(46):11826–11831. 10.1073/pnas.1811962115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaaya M, Campbell OMR, El Kak F, Shaar D, Harb H, Kaddour A (2002) Postpartum depression: prevalence and determinants in Lebanon. Arch Womens Ment Health 5(2):65–72. 10.1007/s00737-002-0140-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang SR, Chen KH, Ho HN, et al. (2015) Depressive symptoms, pain, and sexual dysfunction over the first year following vaginal or cesarean delivery: a prospective longitudinal study. Int J Nurs Stud 52(9):1433–1444. 10.1016/j.ijnurstu.2015.04.019 [DOI] [PubMed] [Google Scholar]
- Chen HH, Lai JCY, Hwang SJ, Huang N, Chou YJ, Chien LY (2017) Understanding the relationship between cesarean birth and stress, anxiety, and depression after childbirth: a nationwide cohort study. Birth 44(4):369–376. 10.1111/birt.12295 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL (1998) Maternal depressive disorder and contextual risk: contributions to the development of attachment insecurity and behavior problems in toddlerhood. Dev Psychopathol 10(2):283–300. 10.1017/S0954579498001618 [DOI] [PubMed] [Google Scholar]
- Davies J, Slade P, Wright I, Stewart P (2008) Posttraumatic stress symptoms following childbirth and mothers’ perceptions of their infants. Infant Ment Health J, 29(6):537–554. 10.1002/imhj.20197 [DOI] [PubMed] [Google Scholar]
- Dekel S, Ein-Dor T, Ruohomäki, et al. (2019) The dynamic course of peripartum depression across pregnancy and childbirth. J Psychiatr Res. 10.1016/j.jpsychires.2019.03.016 [DOI] [PubMed] [Google Scholar]
- Dekel S, Stuebe C, Dishy G (2017) Childbirth induced posttraumatic stress syndrome: a systematic review of prevalence and risk factors. Front Psychol 8:560 10.3389/fpsyg.2017.00560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekel S, Thiel F, Dishy G, Ashenfarb AL (2018) Is childbirth-induced PTSD associated with low maternal attachment?. Arch Womens Ment Health 1–4. 10.1007/s00737-018-0853-y [DOI] [PubMed] [Google Scholar]
- Derogatis LR (1993) BSI Brief Symptom Inventory: Administration, Scoring, and Procedure Manual, 4th edn. National Computer Systems, Minneapolis. [Google Scholar]
- Eckerdal P, Georgakis MK, Kollia N, Wikström AK, Högberg U, Skalkidou A (2018) Delineating the association between mode of delivery and postpartum depression symptoms: a longitudinal study. Acta Obstet Gynecol Scand 97(3):301–311. 10.1111/aogs.13275 [DOI] [PubMed] [Google Scholar]
- Feldman R, Weller A, Zagoory-Sharon O, Levine A (2007) Evidence for a neuroendocrinological foundation of human affiliation: plasma oxytocin levels across pregnancy and the postpartum period predict mother-infant bonding. Psychol Sci 18:965–97. 10.1111/j.1467-9280.2007.02010.x [DOI] [PubMed] [Google Scholar]
- Guintivano J, Sullivan PF, Stuebe AM, et al. (2018) Adverse life events, psychiatric history, and biological predictors of postpartum depression in an ethnically diverse sample of postpartum women. Psychological Med 48(7):1190–1200. 10.1017/S0033291717002641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobst A, Krause D, Maiwald C, et al. (2016) Oxytocin course over pregnancy and postpartum period and the association with postpartum depressive symptoms. Arch Womens Ment Health 19:571–579. 10.1007/s00737-016-0644-2 [DOI] [PubMed] [Google Scholar]
- Lobel M, DeLuca RS (2007) Psychosocial sequelae of cesarean delivery: review and analysis of their causes and implications. Soc Sci Med 64(11):2272–2284. 10.1016/j.socscimed.2007.02.028 [DOI] [PubMed] [Google Scholar]
- Marshall RD, Olfson M, Hellman F, Blanco C, Guardino M, Struening EL (2001) Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry 158(9):1467–1473. 10.1176/appi.ajp.158.9.1467 [DOI] [PubMed] [Google Scholar]
- Mathisen SE, Glavin K, Lien L, Lagerløv P (2013) Prevalence and risk factors for postpartum depressive symptoms in Argentina: a cross-sectional study. Int J Women’s Health 5:787–793. 10.2147/IJWH.S51436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeever VM, Huff ME (2003) A diathesis-stress model of posttraumatic stress disorder: ecological, biological, and residual stress pathways. Rev Gen Psychol 7(3):237–250. 10.1037/1089-2680.7.3.237 [DOI] [Google Scholar]
- Moehler E, Brunner R, Wiebel A, Reck C, Resch F (2006). Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother–child bonding. Arch Womens Ment Health 9(5):273–278. 10.1007/s00737-006-0149-5 [DOI] [PubMed] [Google Scholar]
- Murray L, Cartwright W (1993) The role of obstetric factors in postpartum depression. J Reprod Infant Psychol 11(4):215–219. 10.1080/02646839308403221 [DOI] [Google Scholar]
- Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A (2018) Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry 75(3):247–253. 10.1001/jamapsychiatry.2017.4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara MW, Schlechte JA, Lewis DA, Wright EJ (1991) Prospective study of postpartum blues: biologic and psychosocial factors. Arch Gen Psychiatry 48(9):801–806. 10.1001/archpsyc.1991.01810330025004 [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Zekoski EM, Philipps LH, Wright EJ (1990) Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 99(1):3–15. 10.1037/0021-843X.99.1.3 [DOI] [PubMed] [Google Scholar]
- Olieman RM, Siemonsma F, Bartens MA, Garthus-Niegel S, Scheele F, Honig A (2017) The effect of an elective cesarean section on maternal request on peripartum anxiety and depression in women with childbirth fear: a systematic review. BMC Pregnancy Childbirth 17(1):195 10.1186/s12884-017-1371-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Örün E, Yalçın SS, Mutlu B (2013) Relations of maternal psychopathologies, social-obstetrical factors and mother-infant bonding at 2-month postpartum: a sample of Turkish mothers. World J Pediatr 9(4):350–355. 10.1007/s12519-013-0432-2 [DOI] [PubMed] [Google Scholar]
- Petterson SM, Albers AB (2001) Effects of poverty and maternal depression on early child development. Child Dev 72(6):1794–1813. 10.1111/1467-8624.00379 [DOI] [PubMed] [Google Scholar]
- Rauh C, Beetz A, Burger P, et al. (2012) Delivery mode and the course of pre- and postpartum depression. Arch Gynecol Obstet 286:1407–1412. 10.1007/s00404-012-2470-8 [DOI] [PubMed] [Google Scholar]
- Reck C, Stehle E, Reinig K, Mundt C (2009) Maternity blues as a predictor of DSM-IV depression and anxiety disorders in the first three months postpartum. J Affect Disord 113(1–2):77–87. 10.1016/j.jad.2008.05.003 [DOI] [PubMed] [Google Scholar]
- Ross LE, Evans SG, Sellers EM, Romach MK (2003) Measurement issues in postpartum depression part 1: anxiety as a feature of postpartum depression. Arch Womens Ment Health 6(1):51–57. 10.1007/s00737-002-0155-1 [DOI] [PubMed] [Google Scholar]
- Rowe-Murray HJ, Fisher JR (2001) Operative intervention in delivery is associated with compromised early mother-infant interaction. BJOG 108(10):1068–1075. 10.1111/j.1471-0528.2001.00242.x [DOI] [PubMed] [Google Scholar]
- Rowlands IJ, Redshaw M (2012) Mode of birth and women’s psychological and physical wellbeing in the postnatal period. BMC Pregnancy Childbirth 12(1):138 10.1186/1471-2393-12-138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB (2009) Multiple imputation for nonresponse in surveys, Vol 307 John Wiley & Sons, Hoboken. [Google Scholar]
- Ryding EL, Wijma K, Wijma B (1998) Psychological impact of emergency cesarean section in comparison with elective cesarean section, instrumental and normal vaginal delivery. J Psychosom Obstet Gynecol 19(3):135–144. 10.3109/01674829809025691 [DOI] [PubMed] [Google Scholar]
- Sadat Z, Kafaei Atrian M, Masoudi Alavi N, et al. (2014) Effect of mode of delivery on postpartum depression in Iranian women. J Obstet Gynaecol Res 40(1):172–177. 10.1111/jog.12150 [DOI] [PubMed] [Google Scholar]
- Scheepstra KWF, van Steijn ME, Dijksman LM, van Pampus MG (2017) Post-traumatic stress disorder in women and their partners, following severe post-partum hemorrhage: a study protocol for a prospective cohort study. Cogent Med 4(1):1278840 10.1080/2331205X.2017.1278840 [DOI] [Google Scholar]
- Šidák Z (1967) Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc 62(318):626–633. 10.1080/01621459.1967.10482935 [DOI] [Google Scholar]
- Söderquist J, Wijma B, Thorbert G, Wijma K (2009) Risk factors in pregnancy for post-traumatic stress and depression after childbirth. BJOG 116(5):672–680. 10.1111/j.1471-0528.2008.02083.x [DOI] [PubMed] [Google Scholar]
- Stjernholm YV, Nyberg A, Cardell M, Höybye C (2016) Circulating maternal cortisol levels during vaginal delivery and elective cesarean section. Arch Gynecol Obstet 294(2):267–271. 10.1007/s00404-015-3981-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stramrood C, Slade P (2017) A woman afraid of becoming pregnant again: posttraumatic stress disorder following childbirth In: Paarlberg K, van de Wiel H (eds) Bio-psycho-social obstetrics and gynecology. Springer, Cham, pp. 33–49. [Google Scholar]
- Swain JE, Tasgin E, Mayes LC, Feldman R, Todd Constable R, Leckman JF (2008) Maternal brain response to own baby-cry is affected by cesarean section delivery. J Child Psychol Psychiatry 49:1042–1052. 10.1111/j.1469-7610.2008.01963.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sword W, Kurtz Landy C, Thabane L, et al. (2011) Is mode of delivery associated with postpartum depression at 6 weeks: a prospective cohort study. BJOG 118(8):966–977. 10.1111/j.1471-0528.2011.02950.x [DOI] [PubMed] [Google Scholar]
- Van Heumen MA, Hollander MH, van Pampus MG, van Dillen J, Stramrood CA (2018) Psychosocial predictors of postpartum posttraumatic stress disorder in women with a traumatic childbirth experience. Front Psychiatry 9:348 10.3389/fpsyt.2018.00348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villar J, Carroli G, Zavaleta N, et al. (2007) Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ 335(7628):1025 10.1136/bmj.39363.706956.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP (2013) The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Wyler AR, Masuda M, Holmes TH (1971) Magnitude of life events and seriousness of illness. Psychosom Med 33(2):115–122. 10.1097/00006842-197103000-00003 [DOI] [PubMed] [Google Scholar]
- Yehuda R, Bell A, Bierer LM, Schmeidler J (2008) Maternal, not paternal, PTSD is related to increased risk for PTSD in offspring of Holocaust survivors. J Psychiatr Res 42(13):1104–1111. 10.1016/j.jpsychires.2008.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanardo V, Svegliado G, Cavallin F, et al. (2010) Elective cesarean delivery: does it have an effect on breastfeeding? Birth 37(4):275–279. 10.1111/j.1523-536X.2010.00421.x [DOI] [PubMed] [Google Scholar]