Abstract
Background
The Nature Step to Respiratory Health was the overarching theme of the 12th General Meeting of the Global Alliance against Chronic Respiratory Diseases (GARD) in Helsinki, August 2018. New approaches are needed to improve respiratory health and reduce premature mortality of chronic diseases by 30% till 2030 (UN Sustainable Development Goals, SDGs). Planetary health is defined as the health of human civilization and the state of the natural systems on which it depends. Planetary health and human health are interconnected, and both need to be considered by individuals and governments while addressing several SDGs.
Results
The concept of the Nature Step has evolved from innovative research indicating, how changed lifestyle in urban surroundings reduces contact with biodiverse environments, impoverishes microbiota, affects immune regulation and increases risk of NCDs. The Nature Step calls for strengthening connections to nature. Physical activity in natural environments should be promoted, use of fresh vegetables, fruits and water increased, and consumption of sugary drinks, tobacco and alcohol restricted. Nature relatedness should be part of everyday life and especially emphasized in the care of children and the elderly. Taking “nature” to modern cities in a controlled way is possible but a challenge for urban planning, nature conservation, housing, traffic arrangements, energy production, and importantly for supplying and distributing food. Actions against the well-known respiratory risk factors, air pollution and smoking, should be taken simultaneously.
Conclusions
In Finland and elsewhere in Europe, successful programmes have been implemented to reduce the burden of respiratory disorders and other NCDs. Unhealthy behaviour can be changed by well-coordinated actions involving all stakeholders. The growing public health concern caused by NCDs in urban surroundings cannot be solved by health care alone; a multidisciplinary approach is mandatory.
Keywords: Nature, Biodiversity, Immune regulation, Lifestyle, Respiratory diseases, Environment, Planetary health, CRDs, NCDs, SDGs
Background
The 12th General Meeting of the Global Alliance against Chronic Respiratory Diseases (GARD) [1] was hosted by the Finnish Lung Health Association and the National Institute for Health and Welfare in Helsinki 30.8.-1.9.2018. It covered the theme The Nature Step to Respiratory Health discussing the influence of nature and natural elements on respiratory health and on NCDs in general. Prevention and management of chronic respiratory diseases need a fresh approach, especially as new data concerning health effects of environment, lifestyle and indigenous microbiota have emerged since previous GARD meetings. The meeting gathered around 100 opinion leaders from all continents and over 30 countries. It featured presentations on hot topics like environmental effects on respiratory health, determinants of immune balance and planetary health.
This paper outlines the recent findings in the area of improving contact with nature as a strategy for respiratory health and suggests action to combat the challenges of the modern world. To change our behaviour, we should first change our minds by adapting new knowledge [2].
The United Nations Sustainable Development Agenda 2030 was formulated by world leaders in 2015 at a historical summit in New York [3]. All countries were called to work on 17 sustainable development goals (SDGs) and end poverty, fight inequalities, tackle climate change and ensure that no one is left behind. These goals highlight that education, health, social protection, tackling climate change and restoring the natural resources of the Earth are important prerequisites to achieve economic balance and end poverty [4]. While the SDGs are not legally binding, governments and populations are urged to take ownership, show commitment, provide the necessary funding and monitor progress towards the goals within the timeframe of 11 years, by the year 2030.
Over the last few decades, premature mortality from non-communicable diseases (NCDs) before age 70 has dropped in almost all countries [5]. However, additional efforts are needed to achieve a further reduction of 30% by 2030. SDG Goal No. 3 on Good health and wellbeing promotes healthy living for all and lists a number of important targets to be achieved. For NCDs it aims to reduce premature mortality by one-third through prevention and treatment, and promote mental health. SDG Goal No. 15 on Life on Land proposes we take care of our planet. This includes stopping deforestation, land degradation and loss of animal and plant species, i.e. biodiversity loss. Contact with nature educates the human immune system and endorses tolerance against a variety of exposures being thus an essential determinant of health [6]. All the 17 goals are highly interconnected and in many cases progress in one depends on progress in some other goals. For example, biodiversity is a goal the progress of which several other goals depend on [7].
The concept of Nature Step
Urbanization and sedentary lifestyle
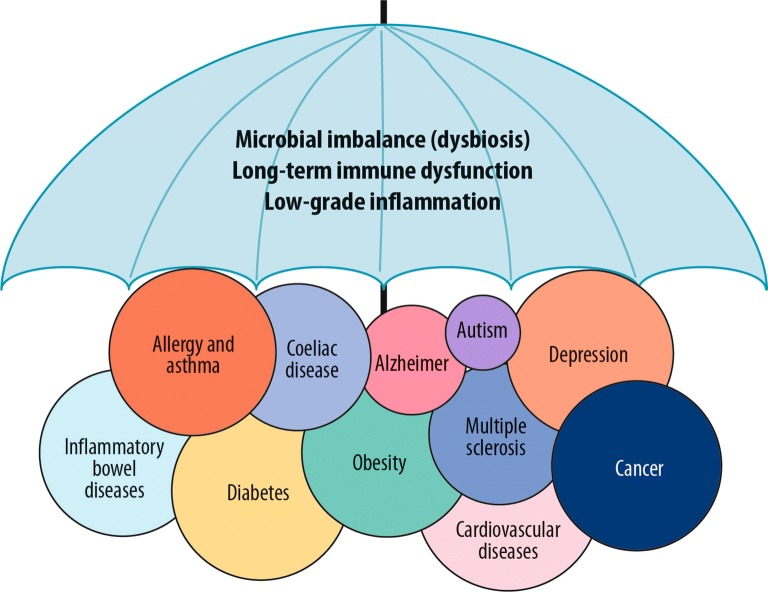
The world is urbanizing faster than ever, and the United Nations predicts that 68% of all human populations live in cities by 2050 [8]. At the same time many chronic conditions including respiratory, allergic, autoimmune, metabolic and mental diseases, are on the increase worldwide in urban environments [9, 10]. The human immune system has run into an adaptation crisis not having had time to adjust to the rapidly changing environment and lifestyles. Crucial elements in this context are the environmental as well as our indigenous microbiota [11] (Fig. 1).
Fig. 1.
Several non-communicable diseases have been suggested to share the same underlying risk factors such as microbial imbalance, long-term immune dysfunction and low-grade inflammation
Urban living in asphalt-covered environments with little green space may not provide us with the diverse microbial stimulation necessary for the development of a balanced immune function. This is augmented by the use of highly processed food, salty and fatty food, sugary drinks and alcohol and the lack of physical activity. Several chronic diseases mentioned above are linked to alteration in our indigenous microbiota and the disappearance of ancient species from these commensal communities [11].
Other environmental stressors like air pollution, common environmental chemicals, noise and behavioural changes like sedentary lifestyle add to the risks. People in urban settings spend more than 90% of their lives indoors. Sedentary lifestyle has indeed become a serious concern in modern societies [12]. The situation is particularly alarming among children. Recent observations link the lack of green surroundings to mental well-being and depression [13, 14]. The studies of residential surrounding greenness and proximity to green spaces on respiratory and allergic symptoms are not uniform, but the majority shows benefits [15–20]. In a recent study, green areas around school neighbourhoods had an effect even on students´ lung function [21]. Interestingly, this effect was partially mediated by the autonomic nervous system. In a nationally representative cohort of 20,000 subjects in England, at least 120 min weekly contact with natural environment was associated with good health and well-being [22].
Increasing surrounding greenness alone may be ineffective, if nutrition and physical activity remain unchanged. Moreover, green surrounding may be more of a surrogate marker of the lifestyle.
Biodiversity hypothesis
The 2018 Living Planet Report by the World Wildlife Fund gave a stunning message: “Wildlife populations show continuous decline, on average by 58% between 1970 and 2014 and are likely to reach 67% by the end of the decade” [23]. The human impact is overwhelming. According to the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES), 75% of the land surface and 66% of the ocean area are significantly altered [24]. Over 85% of wetlands have been lost.
Biodiversity loss may be the most dangerous megatrend, along with interlinked global warming [25, 26] and air pollution [27]. In 2015, for the first time, the UN recognized biodiversity as an essential determinant of human health [9] and included it in Goal No. 15 of the SDG 2030 Agenda [3]. Biodiversity loss in the wider environment was recognized to reduce diversity in human microbiota, contributing to immune dysfunction and disease. For example, environmental and lifestyle changes may affect microbial diversity of the fetal and infant gut microbiome impacting type I diabetes susceptibility [28].
The species on Earth are interlinked by complex interactions like antagonistic ones involving predation, herbivory and parasitism, or mutualistic ones, such as those involving the pollination of flowers by insects. Moreover, the metaphor hints that the interactions may be complex to the point of being impossible to fully elucidate [29]. Biodiversity can be broadly defined as the variety of life on Earth. It includes the genes in all living cells, populations, species and their communities, the habitats in which they occur, and the ecosystems they comprise [30].
The biodiversity hypothesis proposes simply that biodiversity loss leads to immune dysfunction and disease [31]. Reduced contact of people with natural diverse environments, including microbiota, adversely affects the assembly, composition and quality of human commensal microbiota and may thereby lead to inadequate and unbalanced stimulation of immunoregulatory circuits and ultimately to clinical disease [32–35].
The hypothesis is based on the concept that pathogen recognition receptor signalling and the regulatory network activation are needed throughout life for the balanced development and maintenance of immune regulation [6]. Beneficial effects of microbiota in the farming environment are known as it has been shown that children raised in farms with early life exposure to rich microbiota are protected against allergies and asthma [36–38]. However, the role of environmental microbiota by and large has been less explored and recognized. Increased risk in the farming environment may be massive and sudden exposure to microbes causing allergic alveolitis or long term exposure to pesticides [39].
Two layers of biodiversity
We are protected by two nested layers of biodiversity, consisting of microbes residing in our bodies and those of the environment we live in [40]. The diversity and composition of the inner layer are dependent largely on microbial colonisation from the outer layer, a process that depends on our environment and behaviour. Microbes are also transferred vertically, from mother to child. This route of microbial colonization has been discussed in detail elsewhere [41]. After a house move, the microbial community in the new house rapidly converged on the microbial community of the occupants’ former house, suggesting colonization by the family’s microbiota [42]. To preserve our inner biodiversity—which closely interacts with the immune system—we need to preserve the outer biodiversity and change our everyday practices. It is evident but poorly studied that everything we eat, drink, inhale and touch affects the composition and function of our microbiota and promotes a cross-talk of human DNA with the environmental metagenome [11, 43, 44].
The role of microbes in immune tolerance
During the last decade, human microbiota has become a central issue in health and disease. Microbes hold promise for new strategies of prevention and treatment of many inflammatory conditions [45, 46]. Altogether, several factors have been identified to be involved in poorly developed or broken immune tolerance. These include lack of natural microbial exposure, especially in early and late life, dietary factors, dwelling and its surrounding, lifestyles and the use of antibiotics. Broken tolerance is discussed thoroughly elsewhere and not reiterated here [6].
The number of bacteria in the body is about the same as the number of our own cells [47]. Around 3 million genes are encoded in the genome of our microbiota, compared to around 20,000–23,000 genes of the human genome. The microbiome can be regarded as our second genome, to which we have externalized many protective and life supporting functions [48]. The gut microbiome is being attributed an important role in diseases such as obesity, diabetes and metabolic disease [49].
Many urban environments appear to lack elements such as plants and trees necessary for the proper development of tolerance against foreign proteins [50]. People living in densely built urban areas are less exposed to diverse environmental microbiota than people living in more sparsely built areas [51]. A study comparing adolescents in Finnish and more rural Russian Karelia [52] showed that the skin and nasal microbiome of the Finnish and Russian adolescents were quite contrasting and directing immune responses to opposite routes [53]. The environmental microbiota may have profound effects on DNA methylation e.g. of CD14, which is a pattern-recognition receptor for lipopolysaccharides (LPS) and other bacterial wall-derived components [54]. Epigenetic regulation affects innate immune function and guides inflammatory pathways [55].
Cities are built and organized differently, and many have residential areas with a lot of green spaces. Practical actions for greener cities are increasing, and also promoted by United Nations [56]. Also, the GSDR 2019 calls upon fostering urban citizens relationship with nature by promoting green space, urban biodiversity and urban food production [7]. At the same time, the idea of Smart Cities with environmental priority is one of the central themes to be funded by the new EU Programme, Horizon Europe 2021–2027 [57].
Nature Step in practice
The Nature Step is still a hypothesis, but suggests practical actions to improve nature relatedness by: (i) strengthening connections with natural environments and increasing physical activity, (ii) increasing use of fresh vegetables and fruits and water, avoiding sugary drinks and consumption of tobacco and alcohol, (iii) linking with natural elements especially in the care of children and the elderly, and (iv) focusing research also on ecosystem services and their health effects to gain evidence to improve practices [58].
According to the World Health Organization (WHO), approximately 1.7 million (2.8%) of deaths worldwide are attributable to low fruit and vegetable consumption [59]. There is convincing evidence that consumption of high-energy foods, such as processed foods containing lot of fats and sugars, promotes obesity compared to low-energy foods such as fruits and vegetables, and even increase all-cause mortality [60]. The possible immunological effect of soil microbes in fresh food is a research priority, as in a recent mouse model study soil exposure modified the gut microbiota and supported immune tolerance [44]. Other research priorities in the field of chronic respiratory and allergic diseases have been outlined in a 2010 GARD publication [61].
At the urban society level, there is no return to the traditional farming life, but it is possible to integrate elements of nature into modern cities in a controlled way and foster the contact of humans and green elements through policy and practice. That is a challenge for policy makers responsible for city planning, housing, traffic arrangements, supplying energy, education, social services and especially for food production and distribution. Healthy behaviour may also be promoted by introducing taxes on unhealthy foods and sugary drinks, tobacco and alcohol. The impact of this approach on respiratory health and other NCDs—and reduction in health care costs—is a research priority.
While many of the points included in the Nature Step approach are part of the best buys strategy of the WHO to reduce the burden from NCDs, better understanding of the mechanisms of nature connection leading to interventions is needed to obtain evidence for societal actions. People must become aware that the link with nature is critical for their own health as well as for their communities.
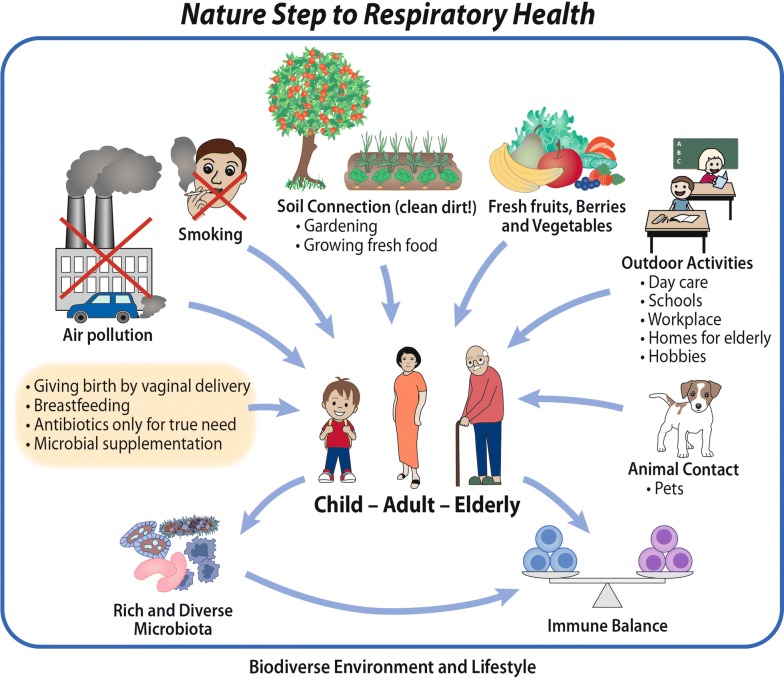
The Finnish Programme showing the way
The Finnish Allergy Programme (2008–2018) revisited the allergy and asthma paradigm and led to actions relevant to society and healthcare as a whole [62, 63]. Immune tolerance and allergy health were promoted through a Nature Step in trying to reset the connection between humans and the natural environment, the original home of Homo sapiens (Fig. 2). There is some direct evidence indicating that human microbiota can be modulated by nature contact, i.e. by handling soil and plant-based materials [64].
Fig. 2.
The Nature Step to Respiratory Health
In Finland, the burden of allergy and asthma has started to decline and there is less medicalisation, less allergy diets, and the severity of asthma has decreased. For example, in 2013–2015, the prevalence of use of allergy diets decreased by 43% in day care centres in the Helsinki Capital area [65]. The Finnish disease surveillance system is showing signs that the epidemic is slowing down as the asthma and allergic rhinitis prevalence is levelling off [66]. Experience shows that medical communities and societies can lessen the disability and costs caused by these disorders and improve public health.
Actions taken for allergy and asthma may also show the way to prevent many other NCDs which are on the rise everywhere in urban communities. An educational programme tackling diabetes, obesity and inflammatory bowel diseases, in addition to allergy and asthma, is planned to take off in Finland in 2020 [28, 67]. A Nature Step is also undertaken in day-care, where (i) diet is changed (less meat and more fresh fruits and vegetables), (ii) food waste is minimized, and (iii) connection to natural environments is increased. The project starts in 2019 and is funded by The Finnish Innovation Fund SITRA [68].
The Finnish Allergy Programme (2008–2018) implemented Nature Step both for primary and secondary (tertiary) prevention of allergy and asthma by emphasizing nature relatedness. Promoting physical exercise, reducing air pollution and stopping smoking were also central.
Human and planetary health—the grand challenges
Planetary health and global warming
According to recent projections, changes in climate will increase in the coming years [69]. Global warming represents a massive threat also to respiratory health by directly promoting or aggravating respiratory diseases, and by increasing exposure to risk factors [70]. Warming increases the exposure to pollen, allergens produced by plants, mould proliferation, ambient air ozone and particulate matter at ground level. The main respiratory concerns are allergic respiratory diseases, asthma, chronic rhinosinusitis (CRS), chronic obstructive pulmonary disease (COPD) and respiratory tract infections. Groups at higher risk of global warming include individuals with existing cardiopulmonary diseases or disadvantaged individuals. Adaptation and mitigation measures are needed.
Climate affects weather, air and water quality, local and national water and food supplies, economics and other critical health determinants. Observational evidence indicates that regional temperature increases affect a diverse set of physical and biological systems in many parts of the world, some of which are of concern for respiratory health. A rapid rise has been observed in the number of hot days, such as the 2003 heat wave resulting in 40,000 excess deaths across Europe, mostly for cardiopulmonary causes [71]. In 2018 another heat wave was experienced in many parts of the world, the effects of which have not been calculated yet. On the other hand, nature based solutions can help humans to adapt to heat waves in cities, e.g. by providing shelter in the form of trees [72].
In 2015, the report of a commission on planetary health created by the Lancet Commission and the Rockefeller Foundation proposed a new way of understanding the relationship between human health and the environment [73]. The view emerged from the realization that humanity is experiencing substantial improvements in life expectancy and health at a time when many ecosystems worldwide are degrading at unprecedented rates. Wealthy populations can use ecosystem services from other locations through access to markets widening health and ecological inequalities. The dependence of health on ecosystems is delayed and complex enough not to be detected with our current paradigms and methods [74, 75]. The current concept of health does not take into account whether health gains are achieved at the cost of eroding the Earth’s underpinning natural systems. To reconcile human health with the restauration of planet’s natural resources, Planetary Health is seen as the highest attainable standard of health and wellbeing; i.e. taking into account Earth’s natural systems limits within which humanity can flourish [73].
Air pollution
Ambient air pollution is a heavy burden in many industrialized and developing countries, especially in urbanized areas where it contributes to increased morbidity and mortality [76]. More than 90% of air pollution related deaths occur in low and middle-income countries According to WHO estimates, outdoor air pollution caused about 4.2 million deaths in 2016 and indoor air pollution from cooking with polluting technologies 3.8 million deaths in the same year [77]. As reported by the Lancet Commission on pollution and health, the global estimated annual deaths due to pollution risk factors ranges between 8.4 (according to the WHO best estimate) and 9.0 million (Global Burden of Diseases best estimate) [78].
Lungs and the cardiovascular system are affected by exposure to fine and ultrafine particles in polluted air, causing stroke, heart disease, cancer, COPD and respiratory infections such as pneumonia [79]. A joint ERS/ATS policy statement of the adverse effects of air pollution has been recently published [80]. Outdoor air pollution is a risk factor for asthma and COPD emergency visits [81, 82], and sleep apnoea [83].
For allergy and asthma, immune dysfunction poses the main risk, but heavy air pollution also contributes to inflammation and affects immune regulation, e.g. diesel fumes may promote allergic inflammation [84]. Epidemiological studies in Japan showed that the increase in cedar pollinosis was likely linked to Diesel exhaust [85]. Other outdoor air pollutants are associated with increased frequency of asthma exacerbations as well as symptoms that affect quality of life such as cough, wheezing and nasal drainage [86]. Nevertheless, there are situations like in Finland where ambient air pollution is minimal, even in cities, still asthma prevalence is high [87].
Smoking
Tobacco use is the main risk factor for all major NCDs. It is estimated by WHO that the tobacco epidemic kills more than 7 million people a year. Six million of these deaths are due to direct tobacco use and about 900,000 due to second-hand smoke [88].
For COPD and lung cancer, smoking is overwhelmingly the greatest risk, which is augmented by air pollutants. Global efforts for implementing the Framework Convention on Tobacco Control and using the WHO MPOWER package have led to better policies in tobacco control [89, 90]. In many countries, however, additional efforts are needed to achieve the UN Sustainable Goals. Moreover, since use of electronic cigarettes has rapidly escalated among youths and are strongly associated with the subsequent initiation of combustible tobacco products, control strategies at the national level are mandatory [91].
Furthermore, oriental water pipe (Narghile) smoking is alarmingly increasing in Europe and the Americas and becoming a pandemic [92]. The WHO Framework Convention on Tobacco Control Secretariat has worked to establish a network of six knowledge hubs for the tobacco MPOWER programme within academic institutions. Water pipe and smokeless tobacco use is one of the six hubs. Each of them specializes in a given area, such as taxation or research and surveillance, and assists parties in their implementation work and disseminating information.
Endgame for smoking
Of particular interest are tobacco endgame policies adopted by a few countries including Finland [93, 94]. The goal of the Tobacco-free Finland 2030 Network is to create a tobacco- and nicotine-free country [95]. In 2010, 23% of Finnish men and 16% of women smoked. Instead of restricting the harmful effects of smoking, the goal of the Tobacco Act aimed to end the consumption of tobacco products in Finland by the year 2030.
In 2012, Finnish sales outlets were prohibited from displaying tobacco products. In 2014, the European Union passed the updated Tobacco Products Directive (2014/40/EC) stipulating that tobacco packaging must include health warnings containing image and text.
In 2015, 16% of Finnish men and 12% of women smoked. In 2016, the updated version of the Tobacco Act came into force. In 2020, the aim is to ban menthol as a flavouring of tobacco products. In 2030, when the objective of the Tobacco Act is hopefully met, less than 5% of the adult population should consume tobacco or nicotine products on a daily basis.
Under the framework of planetary health, fight against smoking and air pollution provides an opportunity to work both to protect human health and restore the natural resource of the Planet. For air pollution there is abundant evidence that active transportation policies can reduce greenhouse gas emissions and improve air quality and physical exercise [96]. In a similar way, eradication of smoking could not only result in unprecedented health benefits but also in reduction of deforestation and land degradation as well as in improvements of biodiversity in large tobacco production areas [97]. Recent studies have shown that vaping is also representing a risk for morbidity and mortality and needs to be urgently regulated [98].
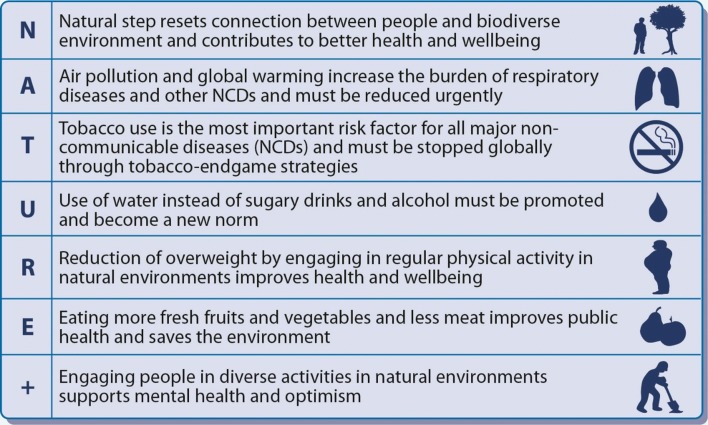
Future challenges
The epidemic of chronic respiratory diseases and other NCDs is the result of changes in lifestyle including reduced contact to natural environments, tobacco smoking and outdoor/indoor air pollution and unhealthy diets. Indoor life in buildings, reduced physical activity, diets using processed food and excessive meat consumption rather than plant-based diets [99, 100], sugary drinks, tobacco and alcohol [101] contribute to the risk. The relative importance of each of these factors varies between populations and living conditions, but they are all mainly caused by exponential growth of human populations leading to escalating urbanization worldwide.
Global, national and local action plans taking into account the local situation need to be constructed and implemented by engaging policy makers, governments, civil society and each individual. This will lead to a better understanding regarding the benefits of positive Steps living in and with Nature (Fig. 3).
Fig. 3.
Imperative actions to promote human health and conserve nature
Monitoring of the different determinants in urban surrounding and their effects on microbiome and immune regulation is difficult and only little studied. Basic questions remain unanswered. For example, what happens when we pick up a wild berry from the bush to the mouth? What is the microbiota of the berry, how does it transfer to our hands and skin, how to the mouth and gut, and how does it modulate human microbiota and regulate the immune system? If eating wild berries, “superfood”, reduces disease risk, by what mechanism? What is the dynamics of environmental microbiota affecting human microbiota? What is the composition of “healthy” human microbiota and what are the mechanisms of the cross-talk with human cells and gene expression? For example, Sberro et al. found recently thousands of previously unknown small proteins in the human microbiome, which may perform diverse functions including epigenetic modulation [102].
Furthermore, how are human microbiota affected by different diets, antibiotics or chemicals? What are the most important urban/rural microbial determinants influencing risk of NCDs, and what, altogether, is the relative importance of environment/lifestyle factors and hereditary dispositions? Is it possible partly to compensate the “lost nature connection” with artificial microbial supplementation? New information is urgently needed, and we strongly advocate both for controlled and real-life studies.
The logistic regression models to assess air pollution effects should be supplemented by biodiversity information, at least by land use data. Usually, air pollution effects are seen in big cities where biodiversity loss is also at its worst. Their interaction and confounding effects should be investigated in future epidemiological studies. Altogether, the respiratory effects of biodiversity loss and global warming may be enormous but have been insufficiently evaluated [31].
A large proportion of NCDs is preventable and changes in behaviour modify disease severity and outcome. This has been shown in Finland, where several successful public health programmes for chronic respiratory conditions and cardiovascular disease prevention have been implemented [103, 104]. In terms of air pollution, the Vilnius Declaration originating from a meeting by the European Forum for Research and Education in Allergies and Airway Diseases (EUFOREA) in March 2018 proposes several urgent actions to mitigate air pollution [105]. More recently, on September 2018, the United Nations High-level Meeting on Non-communicable Diseases has issued a declaration [106], in which the role of air pollution is outlined as a major risk factor to be combatted. Following this path, WHO has organized the First Global Conference on Air Pollution and Health, October 2018 [107].
While there is plenty of evidence that NCDs are preventable through policy changes such as tax increases for tobacco, unhealthy foods and drinks and individual behaviour change, implementing these measures is challenging as there is lack of funding for prevention programmes and opposition from industries with vested interests.
All governments need to address the health effects of major environmental threats on a regular basis to prompt timely and concrete actions. Indeed, the WHO 12th recommendation from the Declaration of the Health of People, Health of Planet and Our Responsibility: Climate Change, Air Pollution and Health Workshop 2017 states “Promote an alliance with society that brings together scientists, policy makers, healthcare providers, faith/spiritual leaders, communities, and foundations to foster the societal transformation necessary to achieve our goals in the spirit of Pope Francis’s encyclical Laudato si” [108].
The present paper is of importance to sustain Planetary Health and should be embedded in next-generation care pathways for respiratory diseases [109] for a change management strategy concerning CRDs [110]. On December 3–4, 2019, a high-level meeting will be organized during the Finnish Presidency of the EU Council to discuss the impact between Planetary and Human health. A focus will be made concerning biodiversity and the digital transformation of health.
Conclusive remark
New research suggests that reducing harmful exposures and strengthening immune tolerance could be promoted through a Nature Step, resetting the connection between humans and nature. This is also an imperative for nature conservation and safeguarding a peaceful planet.
The most urgent challenge is for the quickly urbanising developing countries as their NCDs epidemic is quite recent and worsening, and effective strategies for prevention and treatment have not been implemented. The pace of urbanization is fastest in Africa and South-East Asia, the exposure to nature in these populations is expected to fall dramatically [8].
Abbreviations
- ATS
American Thoracic Society
- COPD
chronic obstructive pulmonary disease
- CRDs
chronic respiratory diseases
- CRS
chronic rhinosinusitis
- ERS
European Respiratory Society
- EUFOREA
european forum for research and education in allergy and airway diseases
- EU
European Union
- FCTC
Framework Convention on Tobacco Control
- GARD
Global Alliance Against Chronic Respiratory Diseases
- GSDR
Global Sustainable Development Report
- IPBES
Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services
- MPOWER
monitor tobacco use and prevention policies, protect people from tobacco smoke, offer help to quit tobacco use, warn about the dangers of tobacco, enforce bans on tobacco advertising, promotion and sponsorship, raise taxes on tobacco
- NCDs
non-communicable diseases
- SDGs
sustainable development goals
- SITRA
Suomen itsenäisyyden juhlarahasto: Finnish Innovation Fund
- UN
United Nations
- WHO
World Health Organization
Authors’ contributions
TH, LvH and NEB drafted the first version of the manuscript and contributed to critical content revisions. JA, JB, EF, PJ, GV contributed to critical content revisions. All authors read and approved the final manuscript.
Funding
No funding received.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tari Haahtela, Email: tari.haahtela@haahtela.fi.
Leena von Hertzen, Email: leena.vonhertzen@kolumbus.fi.
Josep M. Anto, Email: josepm.anto@isglobal.org
Chunxue Bai, Email: bai.chunxue@zs-hospital.sh.cn.
Abay Baigenzhin, Email: national_clinic@nnmc.kz.
Eric D. Bateman, Email: eric.bateman@uct.ac.za
Digambar Behera, Email: dirlrsi@gmail.com.
Kazi Bennoor, Email: bennoor@gmail.com.
Paulo Camargos, Email: pauloamcamargos@gmail.com.
Niels Chavannes, Email: n.h.chavannes@lumc.nl.
Jaime Correia de Sousa, Email: jaimecsousa@gmail.com.
Alvaro Cruz, Email: cruz.proar@gmail.com.
Maria Do Céu Teixeira, Email: teixeiramc@hotmail.com.
Marina Erhola, Email: marina.erhola@thl.fi.
Eeva Furman, Email: Eeva.Furman@ymparisto.fi.
Bilun Gemicioğlu, Email: bilung@gmail.com.
Sandra Gonzalez Diaz, Email: sandra.gonzalezd@uanl.mx.
Peter W. Hellings, Email: peter.hellings@icloud.com
Pekka Jousilahti, Email: pekka.jousilahti@thl.fi.
Nikolai Khaltaev, Email: khaltaevn@bluewin.ch.
Vitezslav Kolek, Email: vitezslav.kolek@fnol.cz.
Piotr Kuna, Email: pk@pta.med.pl.
Stefania La Grutta, Email: stefania.lagrutta@irib.cnr.it.
Le Thi Tuyet Lan, Email: tuyetlanyds@gmail.com.
Tamaz Maglakelidze, Email: tmaglak@gmail.com.
Mohamed R. Masjedi, Email: mrmasjedi@gmail.com
Florin Mihaltan, Email: mihaltan@starnets.ro.
Yousser Mohammad, Email: ccollaborating@gmail.com.
Elizabete Nunes, Email: dra.elizabete.nunes@gmail.com.
Arvid Nyberg, Email: arvid.enyberg@gmail.com.
Jorge Quel, email@haama.org.
Jose Rosado-Pinto, Email: rosadopinto@mail.telepac.pt.
Hironori Sagara, Email: sagarah@med.showa-u.ac.jp.
Boleslaw Samolinski, Email: boleslaw.samolinski@wum.edu.pl.
Dean Schraufnagel, Email: schrauf@uic.edu.
Talant Sooronbaev, Email: sooronbaev@yahoo.com.
Mohamed Tag Eldin, Email: mohamedawadtag@yahoo.com.
Teresa To, Email: teresa.to@sickkids.ca.
Arunas Valiulis, Email: arval2691@gmail.com.
Cherian Varghese, Email: varghesec@who.int.
Tuula Vasankari, Email: tuula.vasankari@filha.fi.
Giovanni Viegi, Email: giovanni.viegi@ibim.cnr.it.
Tonya Winders, Email: twinders@allergyasthmanetwork.org.
Anahi Yañez, Email: anahi.yanez@inaerargentina.org.
Arzu Yorgancioğlu, Email: arzuyo@hotmail.com.
Osman Yusuf, Email: allergypk@gmail.com.
Jean Bousquet, Email: jean.bousquet@orange.fr.
Nils E. Billo, Email: nilsericbillo@gmail.com
References
- 1.Bousquet J, Khaltaev N. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. Geneva: World Health Organization; 2007. [Google Scholar]
- 2.Marteau TM. Changing minds about changing behaviour. Lancet. 2018;391(10116):116–117. doi: 10.1016/S0140-6736(17)33324-X. [DOI] [PubMed] [Google Scholar]
- 3.Transforming our world: The 2030 agenda for sustainable development. A/RES/70/1. United Nations 2015.
- 4.United Nations. The Sustainable Development Goals (SDGs). https://www.un.org/sustainabledevelopment/sustainable-development-goals. Accessed 31 Mar 2019.
- 5.Time to deliver: report of the WHO independent high-level commission on non-communicable diseases.: World Health Organization; 2018.
- 6.von Hertzen L, Beutler B, Bienenstock J, Blaser M, Cani PD, Eriksson J, et al. Helsinki alert of biodiversity and health. Ann Med. 2015;47(3):218–225. doi: 10.3109/07853890.2015.1010226. [DOI] [PubMed] [Google Scholar]
- 7.Independent Group of Scientists appointed by the Secretary-General . Global sustainable development report 2019: the future is now—science for achieving sustainable development. New York: United Nations; 2019. [Google Scholar]
- 8.World Urbanization Prospects . The 2018 revision. Department of Economic and Social Affairs. New York: United Nations; 2018. [Google Scholar]
- 9.Connecting Global Priorities: Biodiversity and Human Health. A state of knowledge review 2015. World Health Organization and the Convention on Biological Diversity; 2015.
- 10.Maio S, Baldacci S, Carrozzi L, Pistelli F, Angino A, Simoni M, et al. Respiratory symptoms/diseases prevalence is still increasing: a 25-yr population study. Respir Med. 2016;110:58–65. doi: 10.1016/j.rmed.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Flandroy L, Poutahidis T, Berg G, Clarke G, Dao MC, Decaestecker E, et al. The impact of human activities and lifestyles on the interlinked microbiota and health of humans and of ecosystems. Sci Total Environ. 2018;627:1018–1038. doi: 10.1016/j.scitotenv.2018.01.288. [DOI] [PubMed] [Google Scholar]
- 12.George ES, Rosenkranz RR, Kolt GS. Chronic disease and sitting time in middle-aged Australian males: findings from the 45 and up study. Int J Behav Nutr Phys Act. 2013;10:20. doi: 10.1186/1479-5868-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomita A, Vandormael AM, Cuadros D, Di Minin E, Heikinheimo V, Tanser F, et al. Green environment and incident depression in South Africa: a geospatial analysis and mental health implications in a resource-limited setting. Lancet Planet Health. 2017;1(4):e152–e162. doi: 10.1016/S2542-5196(17)30063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarkar C, Webster C, Gallacher J. Residential greenness and prevalence of major depressive disorders: a cross-sectional, observational, associational study of 94 879 adult UK Biobank participants. Lancet Planet Health. 2018;2(4):e162–e173. doi: 10.1016/S2542-5196(18)30051-2. [DOI] [PubMed] [Google Scholar]
- 15.Louv R. Last child in the woods. London: Atlantic Books; 2009. [Google Scholar]
- 16.Lovasi GS, Quinn JW, Neckerman KM, Perzanowski MS, Rundle A. Children living in areas with more street trees have lower prevalence of asthma. J Epidemiol Community Health. 2008;62(7):647–649. doi: 10.1136/jech.2007.071894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuertes E, Markevych I, Bowatte G, Gruzieva O, Gehring U, Becker A, et al. Residential greenness is differentially associated with childhood allergic rhinitis and aeroallergen sensitization in seven birth cohorts. Allergy. 2016;71(10):1461–1471. doi: 10.1111/all.12915. [DOI] [PubMed] [Google Scholar]
- 18.Lovasi GS, O’Neil-Dunne JP, Lu JW, Sheehan D, Perzanowski MS, Macfaden SW, et al. Urban tree canopy and asthma, wheeze, rhinitis, and allergic sensitization to tree pollen in a New York City birth cohort. Environ Health Perspect. 2013;121(4):494–500. doi: 10.1289/ehp.1205513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dadvand P, Villanueva CM, Font-Ribera L, Martinez D, Basagana X, Belmonte J, et al. Risks and benefits of green spaces for children: a cross-sectional study of associations with sedentary behavior, obesity, asthma, and allergy. Environ Health Perspect. 2014;122(12):1329–1335. doi: 10.1289/ehp.1308038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cilluffo G, Ferrante G, Fasola S, Montalbano L, Malizia V, Piscini A, et al. Associations of greenness, greyness and air pollution exposure with children’s health: a cross-sectional study in Southern Italy. Environ Health. 2018;17(1):86. doi: 10.1186/s12940-018-0430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pacieência IRJ, Silva D, Martins C, Mendes F, Rama T, et al. School environment associates with lung function and autonomic nervous system activity in children: a crosssectional study. Sci Rep. 2019;9:15156. doi: 10.1038/s41598-019-51659-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White MP, Alcock I, Grellier J, Wheeler BW, Hartig T, Warber SL, et al. Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Sci Rep. 2019;9(1):7730. doi: 10.1038/s41598-019-44097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Living Planet Report—2018. In: Aiming higher. M Grooten, REA Almond, editors. WWF: Gland, Switzerland; 2018.
- 24.Global assessment report on biodiversity and ecosystem services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services. In: ES Brondizio, J Settele, S Díaz, HT Ngo, editors. IPBES Secretariat: Bonn, Germany, 2019.
- 25.Rockstrom J, Steffen W, Noone K, Persson A, Chapin FS, 3rd, Lambin EF, et al. A safe operating space for humanity. Nature. 2009;461(7263):472–475. doi: 10.1038/461472a. [DOI] [PubMed] [Google Scholar]
- 26.Campbell-Lendrum D, Pruss-Ustun A. Climate change, air pollution and noncommunicable diseases. Bull World Health Organ. 2019;97(2):160–161. doi: 10.2471/BLT.18.224295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landrigan P, Fuller R, Haines A, Watts N, McCarthy G. Pollution prevention and climate change mitigation: measuring the health benefits of comprehensive interventions. Lancet Planet Health. 2018;2(12):e515–e516. doi: 10.1016/S2542-5196(18)30226-2. [DOI] [PubMed] [Google Scholar]
- 28.Kostic AD, Gevers D, Siljander H, Vatanen T, Hyotylainen T, Hamalainen AM, et al. The dynamics of the human infant gut microbiome in development and in progression toward type 1 diabetes. Cell Host Microbe. 2015;17(2):260–273. doi: 10.1016/j.chom.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montoya JM, Pimm SL, Sole RV. Ecological networks and their fragility. Nature. 2006;442(7100):259–264. doi: 10.1038/nature04927. [DOI] [PubMed] [Google Scholar]
- 30.Convention on Biological Diversity 1992. United Nations; 1992.
- 31.von Hertzen L, Hanski I, Haahtela T. Natural immunity. Biodiversity loss and inflammatory diseases are two global megatrends that might be related. EMBO Rep. 2011;12(11):1089–1093. doi: 10.1038/embor.2011.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanski I, von Hertzen L, Fyhrquist N, Koskinen K, Torppa K, Laatikainen T, et al. Environmental biodiversity, human microbiota, and allergy are interrelated. Proc Natl Acad Sci USA. 2012;109(21):8334–8339. doi: 10.1073/pnas.1205624109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haahtela T, Holgate S, Pawankar R, Akdis CA, Benjaponpitak S, Caraballo L, et al. The biodiversity hypothesis and allergic disease: world allergy organization position statement. World Allergy Organ J. 2013;6(1):3. doi: 10.1186/1939-4551-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rook GA. Regulation of the immune system by biodiversity from the natural environment: an ecosystem service essential to health. Proc Natl Acad Sci USA. 2013;110(46):18360–18367. doi: 10.1073/pnas.1313731110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haahtela T. A biodiversity hypothesis. Allergy. 2019;74(8):1445–1456. doi: 10.1111/all.13763. [DOI] [PubMed] [Google Scholar]
- 36.Martinez FD, Guerra S. Early origins of asthma. Role of microbial dysbiosis and metabolic dysfunction. Am J Respir Crit Care Med. 2018;197(5):573–579. doi: 10.1164/rccm.201706-1091PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kirjavainen PV, Karvonen AM, Adams RI, Taubel M, Roponen M, Tuoresmaki P, et al. Farm-like indoor microbiota in non-farm homes protects children from asthma development. Nat Med. 2019;25(7):1089–1095. doi: 10.1038/s41591-019-0469-4. [DOI] [PubMed] [Google Scholar]
- 38.Stein MM, Hrusch CL, Gozdz J, Igartua C, Pivniouk V, Murray SE, et al. Innate immunity and asthma risk in amish and hutterite farm children. N Engl J Med. 2016;375(5):411–421. doi: 10.1056/NEJMoa1508749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tjalvin G, Mikkelsen KE, Apelseth TO, Hollund BE, Svanes C, Van Do T. Hypersensitivity pneumonitis in farmers: improving etiologic diagnosis to optimize counselling. J Agromed. 2019 doi: 10.1080/1059924X.2019.1605954. [DOI] [PubMed] [Google Scholar]
- 40.Ruokolainen L, Lehtimaki J, Karkman A, Haahtela T, von Hertzen L, Fyhrquist N. Holistic view on health: two protective layers of biodiversity. Ann Zool Fenn. 2017;25(1–4):39–49. doi: 10.5735/086.054.0106. [DOI] [Google Scholar]
- 41.Rautava S, Luoto R, Salminen S, Isolauri E. Microbial contact during pregnancy, intestinal colonization and human disease. Nat Rev Gastroenterol Hepatol. 2012;9(10):565–576. doi: 10.1038/nrgastro.2012.144. [DOI] [PubMed] [Google Scholar]
- 42.Lax S, Smith DP, Hampton-Marcell J, Owens SM, Handley KM, Scott NM, et al. Longitudinal analysis of microbial interaction between humans and the indoor environment. Science. 2014;345(6200):1048–1052. doi: 10.1126/science.1254529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Karkman A, Lehtimaki J, Ruokolainen L. The ecology of human microbiota: dynamics and diversity in health and disease. Ann N Y Acad Sci. 2017;1399(1):78–92. doi: 10.1111/nyas.13326. [DOI] [PubMed] [Google Scholar]
- 44.Ottman N, Ruokolainen L, Suomalainen A, Sinkko H, Karisola P, Lehtimaki J, et al. Soil exposure modifies the gut microbiota and supports immune tolerance in a mouse model. J Allergy Clin Immunol. 2019;143(3):1198-206 e12. doi: 10.1016/j.jaci.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 45.Logan AC, Jacka FN, Prescott SL. Immune-microbiota interactions: dysbiosis as a global health issue. Curr Allergy Asthma Rep. 2016;16(2):13. doi: 10.1007/s11882-015-0590-5. [DOI] [PubMed] [Google Scholar]
- 46.Langella P, Guarner F, Martin R. Editorial: next-generation probiotics: from commensal bacteria to novel drugs and food supplements. Front Microbiol. 2019;10:1973. doi: 10.3389/fmicb.2019.01973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14(8):e1002533. doi: 10.1371/journal.pbio.1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grice EA, Segre JA. The human microbiome: our second genome. Annu Rev Genomics Hum Genet. 2012;13:151–170. doi: 10.1146/annurev-genom-090711-163814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harsch IA, Konturek PC. The role of gut microbiota in obesity and type 2 and type 1 diabetes mellitus: new insights into “old” diseases. Med Sci (Basel) 2018;6(2):32. doi: 10.3390/medsci6020032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.von Hertzen L, Haahtela T. Disconnection of man and the soil: reason for the asthma and atopy epidemic? J Allergy Clin Immunol. 2006;117(2):334–344. doi: 10.1016/j.jaci.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 51.Parajuli A, Gronroos M, Siter N, Puhakka R, Vari HK, Roslund MI, et al. Urbanization reduces transfer of diverse environmental microbiota indoors. Front Microbiol. 2018;9:84. doi: 10.3389/fmicb.2018.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haahtela T, Laatikainen T, Alenius H, Auvinen P, Fyhrquist N, Hanski I, et al. Hunt for the origin of allergy—comparing the Finnish and Russian Karelia. Clin Exp Allergy. 2015;45(5):891–901. doi: 10.1111/cea.12527. [DOI] [PubMed] [Google Scholar]
- 53.Ruokolainen L, Paalanen L, Karkman A, Laatikainen T, von Hertzen L, Vlasoff T, et al. Significant disparities in allergy prevalence and microbiota between the young people in Finnish and Russian Karelia. Clin Exp Allergy. 2017;47(5):665–674. doi: 10.1111/cea.12895. [DOI] [PubMed] [Google Scholar]
- 54.Song Y, Khoo SK, Lee KH, Makela M, Haahtela T, LeSouef P, et al. Dual responses of CD14 methylation to distinct environments: a role in asthma and allergy. Eur Respir J. 2017;50(6):1701228. doi: 10.1183/13993003.01228-2017. [DOI] [PubMed] [Google Scholar]
- 55.Zhang Q, Cao X. Epigenetic regulation of the innate immune response to infection. Nat Rev Immunol. 2019;19(7):417–432. doi: 10.1038/s41577-019-0151-6. [DOI] [PubMed] [Google Scholar]
- 56.Greener Cities Partnership (UN-Habitat and UN Environment). https://new.unhabitat.org/greener-cities-partnership. Accessed 2 Oct 2019.
- 57.EU Commission H2020 programme. https://ec.europa.eu/inea/en/horizon-2020/smart-cities-communities. Accessed 30 Sept 2019.
- 58.Haahtela T, Hanski I, von Hertzen L, Jousilahti P, Laatikainen T, Makela M, et al. “ Nature step” to prevent noncommunicable inflammatory disease. Duodecim. 2017;133(1):19–26. [PubMed] [Google Scholar]
- 59.Global strategy on diet, physical activity and health—2004. Geneva: World Health Organization; 2004.
- 60.Rico-Campa A, Martinez-Gonzalez MA, Alvarez-Alvarez I, Mendonca RD, de la Fuente-Arrillaga C, Gomez-Donoso C, et al. Association between consumption of ultra-processed foods and all cause mortality: sUN prospective cohort study. BMJ. 2019;365:l1949. doi: 10.1136/bmj.l1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bousquet J, Kiley J, Bateman ED, Viegi G, Cruz AA, Khaltaev N, et al. Prioritised research agenda for prevention and control of chronic respiratory diseases. Eur Respir J. 2010;36(5):995–1001. doi: 10.1183/09031936.00012610. [DOI] [PubMed] [Google Scholar]
- 62.Haahtela T, von Hertzen L, Makela M, Hannuksela M, Allergy Programme Working G Finnish allergy programme 2008–2018—time to act and change the course. Allergy. 2008;63(6):634–645. doi: 10.1111/j.1398-9995.2008.01712.x. [DOI] [PubMed] [Google Scholar]
- 63.von Hertzen LC, Savolainen J, Hannuksela M, Klaukka T, Lauerma A, Makela MJ, et al. Scientific rationale for the Finnish Allergy Programme 2008–2018: emphasis on prevention and endorsing tolerance. Allergy. 2009;64(5):678–701. doi: 10.1111/j.1398-9995.2009.02024.x. [DOI] [PubMed] [Google Scholar]
- 64.Gronroos M, Parajuli A, Laitinen OH, Roslund MI, Vari HK, Hyoty H, et al. Short-term direct contact with soil and plant materials leads to an immediate increase in diversity of skin microbiota. Microbiologyopen. 2019;8(3):e00645. doi: 10.1002/mbo3.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Haahtela T, Valovirta E, Bousquet J, Makela M. The Finnish allergy programme 2008–2018 works. Eur Respir J. 2017;49(6):1700470. doi: 10.1183/13993003.00470-2017. [DOI] [PubMed] [Google Scholar]
- 66.Hisinger-Molkanen H, Pallasaho P, Haahtela T, Lindqvist A, Sovijarvi A, Piirila P. The increase of asthma prevalence has levelled off and symptoms decreased in adults during 20 years from 1996 to 2016 in Helsinki, Finland. Respir Med. 2019;155:121–126. doi: 10.1016/j.rmed.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 67.Saaristo T, Peltonen M, Keinanen-Kiukaanniemi S, Vanhala M, Saltevo J, Niskanen L, et al. National type 2 diabetes prevention programme in Finland: FIN-D2D. Int J Circumpolar Health. 2007;66(2):101–112. doi: 10.3402/ijch.v66i2.18239. [DOI] [PubMed] [Google Scholar]
- 68.Mikola M. Taste classes support children’s growth into confident experimenters and consumers. https://www.sitra.fi/en/articles/markku-mikola-taste-classes-support-childrens-growth-confident-experimenters/. Accessed 12 July 2019.
- 69.Hegerl G, Stott P. Atmospheric science. From past to future warming. Science. 2014;343(6173):844–845. doi: 10.1126/science.1249368. [DOI] [PubMed] [Google Scholar]
- 70.Haines A, Ebi K. The imperative for climate action to protect health. N Engl J Med. 2019;380(3):263–273. doi: 10.1056/NEJMra1807873. [DOI] [PubMed] [Google Scholar]
- 71.Haines A, Kovats RS, Campbell-Lendrum D, Corvalan C. Climate change and human health: impacts, vulnerability, and mitigation. Lancet. 2006;367(9528):2101–2109. doi: 10.1016/S0140-6736(06)68933-2. [DOI] [PubMed] [Google Scholar]
- 72.Baro F, Chaparro L, Gomez-Baggethun E, Langemeyer J, Nowak DJ, Terradas J. Contribution of ecosystem services to air quality and climate change mitigation policies: the case of urban forests in Barcelona, Spain. Ambio. 2014;43(4):466–479. doi: 10.1007/s13280-014-0507-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet. 2015;386(10007):1973–2028. doi: 10.1016/S0140-6736(15)60901-1. [DOI] [PubMed] [Google Scholar]
- 74.Myers SS, Gaffikin L, Golden CD, Ostfeld RS, Redford KH, Ricketts TH, et al. Human health impacts of ecosystem alteration. Proc Natl Acad Sci USA. 2013;110(47):18753–18760. doi: 10.1073/pnas.1218656110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Raudsepp-Hearne C, Peterson GD, Bennett EM. Ecosystem service bundles for analyzing tradeoffs in diverse landscapes. Proc Natl Acad Sci USA. 2010;107(11):5242–5247. doi: 10.1073/pnas.0907284107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ambient (outdoor) air quality and health. WHO fact sheet. https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. Accessed 12 July 2019.
- 78.Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu NN, et al. The Lancet Commission on pollution and health. Lancet. 2018;391(10119):462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- 79.Du Y, Xu X, Chu M, Guo Y, Wang J. Air particulate matter and cardiovascular disease: the epidemiological, biomedical and clinical evidence. J Thorac Dis. 2016;8(1):E8–E19. doi: 10.3978/j.issn.2072-1439.2015.11.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Thurston GD, Kipen H, Annesi-Maesano I, Balmes J, Brook RD, Cromar K, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J. 2017;49(1):1600419. doi: 10.1183/13993003.00419-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Orellano P, Quaranta N, Reynoso J, Balbi B, Vasquez J. Effect of outdoor air pollution on asthma exacerbations in children and adults: systematic review and multilevel meta-analysis. PLoS ONE. 2017;12(3):e0174050. doi: 10.1371/journal.pone.0174050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li J, Sun S, Tang R, Qiu H, Huang Q, Mason TG, et al. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2016;11:3079–3091. doi: 10.2147/COPD.S122282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Weinreich G, Wessendorf TE, Pundt N, Weinmayr G, Hennig F, Moebus S, et al. Association of short-term ozone and temperature with sleep disordered breathing. Eur Respir J. 2015;46(5):1361–1369. doi: 10.1183/13993003.02255-2014. [DOI] [PubMed] [Google Scholar]
- 84.Behrendt H, Alessandrini F, Buters J, Kramer U, Koren H, Ring J. Environmental pollution and allergy: historical aspects. Chem Immunol Allergy. 2014;100:268–277. doi: 10.1159/000359918. [DOI] [PubMed] [Google Scholar]
- 85.Ozawa K, Furuta M, Miyao M, Terao C, Kimura M, Sugata K, et al. Medical consultation rate of allergic rhinitis and pollinosis surveillance in Aichi, Japan. Nagoya J Med Sci. 1994;57(1–4):51–60. [PubMed] [Google Scholar]
- 86.Wendling ZA, Emerson JW, Esty DC, Levy MA, de Sherbinin A, et al. 2018 Environmental performance index. New Haven, CT: Yale Center for Environmental Law & Policy. Yale Center for Environmental Law & Policy, Yale University; 2018. https://epi.yale.edu/.
- 87.Pelkonen MK, Notkola IK, Laatikainen TK, Jousilahti P. 30-year trends in asthma and the trends in relation to hospitalization and mortality. Respir Med. 2018;142:29–35. doi: 10.1016/j.rmed.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 88.WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. World Health Organization; 2017.
- 89.MPOWER in action. Defeating the global epidemic. https://www.who.int/tobacco/mpower/publications/brochure_2013/en/. Accessed 12 July 2019.
- 90.Jiang XQ, Mei XD, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis. 2016;8(1):E31–E40. doi: 10.3978/j.issn.2072-1439.2015.11.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ferkol TW, Farber HJ, La Grutta S, Leone FT, Marshall HM, Neptune E, et al. Electronic cigarette use in youths: a position statement of the Forum of International Respiratory Societies. Eur Respir J. 2018;51(5):1800278. doi: 10.1183/13993003.00278-2018. [DOI] [PubMed] [Google Scholar]
- 92.Advisory Note. Waterpipe tobacco smoking: health effects, research needs and recommended actions for regulators. 2nd edition.: WHO Study Group on Tobacco Product Regulation (TobReg). World Health Organization; 2015.
- 93.Branston JR, Sweanor D. Big tobacco, E-cigarettes, and a road to the smoking endgame. Int J Drug Policy. 2016;29:14–18. doi: 10.1016/j.drugpo.2015.12.023. [DOI] [PubMed] [Google Scholar]
- 94.Timberlake DS, Laitinen U, Kinnunen JM, Rimpela AH. Strategies and barriers to achieving the goal of Finland’s tobacco endgame. Tob Control. 2019 doi: 10.1136/tobaccocontrol-2018-054779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tobacco-Free Finland 2020. https://svautonsuomi.fi/en/. Accessed 12 July 2019.
- 96.Nieuwenhuijsen MJ, Khreis H, Triguero-Mas M, Gascon M, Dadvand P. Fifty shades of green: pathway to healthy urban living. Epidemiology. 2017;28(1):63–71. doi: 10.1097/EDE.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 97.Tobacco and its enviromental impact: an overview. World Health Organization 2017. Report No.: 978-92-4-151249-7.
- 98.Carlos WG, Crotty Alexander LE, Gross JE, Dela Cruz CS, Keller JM, Pasnick S, et al. Vaping-associated pulmonary illness (VAPI) Am J Respir Crit Care Med. 2019;200(7):P13–P14. doi: 10.1164/rccm.2007P13. [DOI] [PubMed] [Google Scholar]
- 99.Springmann M, Clark M, Mason-D’Croz D, Wiebe K, Bodirsky BL, Lassaletta L, et al. Options for keeping the food system within environmental limits. Nature. 2018;562(7728):519–525. doi: 10.1038/s41586-018-0594-0. [DOI] [PubMed] [Google Scholar]
- 100.Yip CSC, Chan W, Fielding R. The associations of fruit and vegetable intakes with burden of diseases: a systematic review of meta-analyses. J Acad Nutr Diet. 2019;119(3):464–481. doi: 10.1016/j.jand.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 101.Collaborators GBDA. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10152):1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sberro H, Fremin BJ, Zlitni S, Edfors F, Greenfield N, Snyder MP, et al. Large-scale analyses of human microbiomes reveal thousands of small, novel genes. Cell. 2019;178(5):1245-59 e14. doi: 10.1016/j.cell.2019.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Erhola M, Vasankari T, Jormanainen V, Toppila-Salmi S, Herrala J, Haahtela T. 25 years of respiratory health in Finland. Lancet Respir Med. 2019;7(5):e16. doi: 10.1016/S2213-2600(19)30122-5. [DOI] [PubMed] [Google Scholar]
- 104.Vartiainen E. The North Karelia Project: cardiovascular disease prevention in Finland. Glob Cardiol Sci Pract. 2018;2018(2):13. doi: 10.21542/gcsp.2018.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Valiulis A, Bousquet J, Veryga A, Suprun U, Sergeenko D, Cebotari S, et al. Vilnius Declaration on chronic respiratory diseases: multisectoral care pathways embedding guided self-management, mHealth and air pollution in chronic respiratory diseases. Clin Transl Allergy. 2019;9:7. doi: 10.1186/s13601-019-0242-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Political declaration of the third high-level meeting of the General Assembly on the prevention and control of non-communicable diseases.: United Nations; 2018. A/RES/73/2.
- 107.First WHO Global Conference on air pollution and health. Improving air quality, combatting climate change- saving lives.: World Health Organization; 2018.
- 108.Ramanathan V, Samet J, Neira M, Sorondo MS. Air pollution, climate change, and health: a declaration from the Vatican. Ann Am Thorac Soc. 2018;15(9):1027–1029. doi: 10.1513/AnnalsATS.201805-319ED. [DOI] [PubMed] [Google Scholar]
- 109.Bousquet J, Bedbrook A, Czarlewski W, Onorato GL, Arnavielhe S, Laune D, et al. Guidance to 2018 good practice: ARIA digitally-enabled, integrated, person-centred care for rhinitis and asthma. Clin Transl Allergy. 2019;9:16. doi: 10.1186/s13601-019-0252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bousquet J, Hellings PW, Agache I, Amat F, Annesi-Maesano I, Ansotegui IJ, et al. Allergic rhinitis and its impact on asthma (ARIA) phase 4 (2018): change management in allergic rhinitis and asthma multimorbidity using mobile technology. J Allergy Clin Immunol. 2019;143(3):864–879. doi: 10.1016/j.jaci.2018.08.049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.