Abstract
Objectives
The primary aim was to determine whether patients with RA recalled having discussions concerning lifestyle habits during their health-care visits. The secondary aim was to study the association between patients' reported lifestyle and their wish to discuss it.
Methods
A postal questionnaire sent to 1542 eligible patients from the Better Anti-Rheumatic Pharmacotherapy (BARFOT) study included questions on lifestyle habits (physical activity, diet, smoking and alcohol), on whether these were discussed during health-care visits and on whether there was an interest in such discussions.
Results
A total of 1061 patients (68%) responded [mean age 67 (s.d. 13) years, 73% women]. Half of the patients (49%) recalled discussions on physical activity, and 23% recalled discussions about diet. Those who reported health-enhancing levels of physical activity were more likely to discuss physical activity with their health professionals. Likewise, patients who reported having a non-traditional mixed diet were more likely to discuss diet. Smoking was discussed with 25% of the patients, more often with current smokers than with non-smokers (32 vs 17%; P < 0.001). Alcohol was discussed with 17% of the patients. Of those patients who reported having hazardous drinking habits, 77% had not discussed alcohol use with any health professional.
Conclusion
Discussions about lifestyle were recalled by half of the patients with established RA. There is a need for improvement, because lifestyle habits may affect the long-term outcome in a chronic disease, such as RA. Patient education concerning lifestyle habits should be an integral part of care management and an interactive process.
Keywords: rheumatoid arthritis, lifestyle, habits, physical activity, diet, smoking, alcohol, discussion
Key messages
Lifestyle habits are not discussed with all patients with RA, even though this is recommended.
Physical activity was the lifestyle habit most frequently discussed with RA patients.
Structured interventions to support behavioural change to healthy lifestyles are needed in RA care.
Introduction
Rheumatoid arthritis (RA) is a long-term autoimmune disease characterized by synovitis, systemic inflammation and production of autoantibodies [1]. The prevalence is 0.5‒1.0% in the western world [2], being higher in women and in older individuals [3]. Physical disability, pain, fatigue and sleep disturbances are some of the most pronounced symptoms, resulting in activity limitations that affect the patient’s quality of life [4]. Exactly as in the general population, in patients with RA an unhealthy lifestyle increases the risk of developing co-morbidities, such as cardiovascular diseases, which is why the EULAR has published general guidelines on risk management in patients with RA. In these guidelines, health professionals are encouraged to prioritize discussions with patients regarding their lifestyle [5].
Regular physical activity and exercise are evidence-based elements in the treatment of RA, and during the past decade, interventional trials have shown that physical activity is well tolerated and improves physical function in patients with established RA [6]. In healthy individuals, exercise leads to decreased levels of pro-inflammatory cytokines, and individuals who are physically active before the onset of the disease appear to present with a milder form of RA [7]. More recent studies have indicated that exercise may also have an anti-inflammatory effect on chronic inflammatory diseases [8, 9]. Diet and obesity are closely related, and obesity is associated with worse disease activity, worse function, more pain and worse general health in patients with RA [10]. It is well known that smoking is a modifiable risk factor with important negative effects on health [11]. In rheumatic diseases, smoking is associated with the onset of RA, with smokers being more likely to develop RA than non-smokers [12]. Current smokers of cigarettes are also less likely to respond to pharmacological treatment of RA [13].
Studies regarding alcohol have shown divergent results; some studies have supported the idea that alcohol intake may protect against development of RA [14] and that alcohol intake is associated with less radiographic progression [15], lower self-reported disease activity and better health-related quality of life [16]. On the contrary, over-consumption of alcohol has many negative effects on health [17], and there is a hepatotoxic risk with alcohol use in patients treated with MTX [18].
The assimilation of international and national recommendations promoting lifestyle discussions, in primary and in secondary health care, between health-care professionals and patients with RA has not been extensively studied from the patient’s point of view. There is a lack of information regarding whether these discussions occur in a structured and understandable way for the patients and whether the patients are receptible to these discussions.
The aim was to determine whether patients with RA recalled having discussions concerning the lifestyle habits ‘physical activity’, ‘diet’, ‘smoking’ and ‘consumption of alcohol’ during their health-care visits. A secondary aim was to study the association between patients' reported lifestyle and their wish to discuss it.
Methods
Patients
This cross-sectional postal survey in 2017 included all 1542 still living patients from the Better Anti-Rheumatic Pharmacotherapy (BARFOT) study [19], which involved patients with early RA according to the ACR criteria 1987 (ACR 87) [20] who had been recruited in southern Sweden. In the BARFOT study, data from 2800 adult patients were registered (with consecutive inclusion between 1992 and 2006) at diagnosis (baseline), at 3, 6 and 12 months, and after 2, 5, 8 and 15 years. Details of the larger study have been published elsewhere [19]. All participants provided written informed consent. The present study was approved by the Ethical Review Board at Lund University, Sweden (DNR LU 2016/816) and was performed according to the ethical principles for medical research on human beings described in the Declaration of Helsinki.
Questionnaire
All the patients received a postal questionnaire in January 2017, including questions concerning lifestyle-related habits, sociodemographic data and questions on function and health status. We sent one reminder, and if necessary two, to those who did not respond to the first mailing.
The main outcome variables were based on questions that had been used previously in a national patient survey (Health on Equal Terms) [21]: ‘Did a medical doctor or other health professional discuss physical activity and exercise/diet/smoking/alcohol habits with you during any of your health-care visits, including the rheumatology department and the general practitioner?’ The response alternatives were: yes, during at least one health-care visit; yes, at my latest visit; and no. In this study, both ‘yes’ responses were treated as ‘yes’. For each of the four lifestyle-related habits, there was also a question regarding whether the patients wanted such a discussion, with an answer of either ‘yes’ or ‘no’. The questionnaire also included questions regarding their current physical activity level, their diet, their smoking habits and their alcohol consumption.
Physical activity
Physical activity was assessed with two questions concerning the frequency and duration during the previous 7 days (in minutes per week): vigorous intensity (jogging or intense exercise) and moderate intensity (walking, gardening or bicycling) [5]. The questions have acceptable validity and are used in other studies [22, 23]. The answers were categorized depending on whether or not they met the recommendations for health-enhancing physical activity. According to these recommendations, moderate-intensity physical activity should be performed regularly for a minimum of 30 min, ≥ 5 days a week (150 min/week) or substituted by 20 min of vigorous activity 3 days per week (60 min/week) [24].
Diet
Diet was assessed by giving eight options: traditional mixed, Mediterranean, low-glycaemic, vegetarian, vegetarian with seafood, vegan, gluten-free and other (free text). The dietary habits were dichotomized to a traditional mixed diet and non-traditional mixed diet (Mediterranean, low-glycaemic, vegetarian, vegetarian with seafood, vegan, gluten-free or other).
Smoking
Smoking habits were coded according to three possible descriptions: never smoker, previous smoker or current smoker [25]. These categories were later dichotomized into ever smoker (including both previous smokers and current smokers) and never smoker.
Alcohol consumption
Alcohol consumption was assessed with the Alcohol Use Disorders Identification Test Consumption (AUDIT-C) questionnaire, a validated subset of items from the full alcohol AUDIT [26], consisting of three questions concerning frequency per month, volume per occasion, and number of times with six or more drinks on one occasion. All questions are scored from zero to four (best to worst), with a total score of 0‒12 points. The limit for hazardous drinking according to the Swedish National Institute of Public Health is AUDIT-Cmore than four points for women and more than five points for men (www.fhi.se). Cut-offs that were also used in this study.
Clinical disease assessment
The questionnaire also included well-used and validated questionnaires on physical function and health status. Function was measured with the Stanford HAQ and scored from zero to three (best to worst) [27]. Health status was measured according to EuroQol-5 Dimensions (EQ-5D-3L) and scored from one to zero (best to worst) [28]. Patients’ global assessment (general health), pain and fatigue were assessed with numerical rating scales, from zero to 10 (best to worst) [29]. Self-administered assessment of the number of tender and swollen joints was based on the 28-joint count [30]. Self-reported treatment with conventional DMARDs (cDMARDs) and biologic DMARD (bDMARD) was also registered.
Statistical analysis
Statistical analyses were performed using SPSS statistical software v.21.0 (IBM Corp., Armonk, NY, USA). All significance tests were two tailed and conducted at the 5% significance level. Continuous data are given as the mean and s.d., whereas categorical data are shown as the frequency (percentage). To study differences between groups, the independent t-test was used for continuous variables and the χ2 test for proportions.
Results
Of the 1542 patients who were eligible, 1061 (68%) responded to the questionnaire. The mean age of the responders was 67 (s.d. 13) years, the mean duration of disease was 15 (s.d. 3.8) years, and 769 patients were women (73%). In total, 58% of the patients reported to have discussed any of the lifestyle habits, physical activity, diet, smoking or alcohol. Demographics, patient characteristics and treatment are given in Table 1.
Table 1.
Demographics and disease activity variables in the postal questionnaire
| Parameter | Treatment | All n = 1061 Mean (s.d.) | Women n = 769 (73%) Mean (s.d.) | Men n = 292 (27%) Mean (s.d.) | P-value |
|---|---|---|---|---|---|
| Age, years | 67 (13) | 66 (13) | 70 (12) | <0.001 | |
| Disease duration, years | 15 (3.8) | 16 (3.8) | 16 (3.8) | 0.6 | |
| HAQ (0‒3) | 0.5 (0.6) | 0.6 (0.6) | 0.4 (0.5) | <0.001 | |
| EQ-5D (0‒1) | 0.7 (0.2) | 0.7 (0.3) | 0.8 (0.2) | <0.001 | |
| NRS pain (0‒10, best to worst) | 3.5 (2.5) | 3.6 (2.5) | 3.0 (2.5) | <0.001 | |
| NRS fatigue (0‒10, best to worst) | 4.0 (2.8) | 4.4 (2.9) | 3.4 (2.6) | <0.001 | |
| NRS global health (0‒10, best to worst) | 3.0 (2.4) | 3.2 (2.5) | 2.8 (2.4) | 0.027 | |
| Tender joints, 28-joint counta | 5.6 (6.6) | 5.6 (6.8) | 4.3 (6.1) | 0.003 | |
| Swollen joints, 28-joint counta | 3.0 (4.9) | 3.3 (5.0) | 2.3 (4.5) | 0.002 | |
| Medical treatment | No DMARD | 23 | 23 | 24 | |
| cDMARD | 44 | 43 | 47 | 0.360 | |
| bDMARD | 33 | 34 | 29 |
Tender/swollen joints, self-administered assessment of number of tender and swollen joints based on the 28-joint count.
DMARD: biological DMARD; cDMARD: conventional DMARD; EQ-5D: EuroQol-5 dimensions; NRS: numerical rating scale.
Gender and age characteristics were not significantly different in the responders and non-responders. However, inclusion data from the BARFOT cohort showed that a lower proportion of patients who did not answer the questionnaire were RF positive (57 vs 66%; P = 0.002).
Physical activity
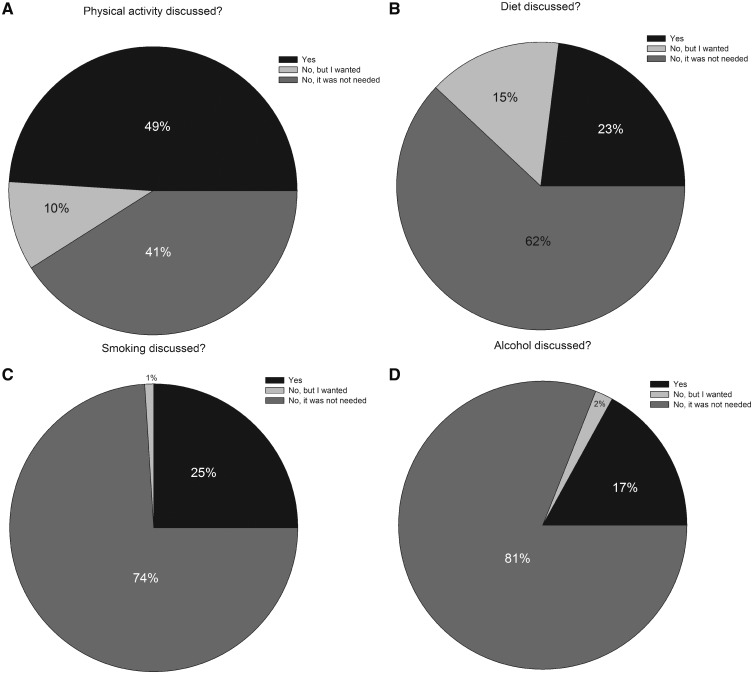
Physical activity was discussed with 49% of the patients, with no significant difference between women and men (48 vs 53%; P = 0.121). Ten per cent of the patients who did not recall having a discussion on physical activity with a health professional reported that they wanted to be involved in discussions of physical activity (Fig. 1A). Fifty-one per cent of the patients were physically active at a health-enhancing level. They also recalled having discussions on physical activity more often than those who did not fulfil the requirements for health-enhancing physical activity (54 vs 45%; P = 0.007). There was no significant difference between patients who fulfilled the requirements for health-enhancing physical activity and those who did not, regarding whether or not they wanted to be involved in discussions of physical activity (28 vs 27%; P = 0.592).
Fig. 1.
Rate of patients reporting that they had discussed lifestyle-related habits and whether they wanted such a discussion
(A) Physical activity. (B) Diet. (C) Smoking. (D) Alcohol consumption.
Diet
Diet was discussed with 23% of the patients, with no significant difference between women and men (22 vs 27%; P = 0.085). There were no differences in diet type between those who recalled vs did not recall dietary discussions. Fifteen per cent of the patients who did not recall a discussion wanted to be involved in dietary discussions (Fig. 1B). Most patients (81%) reported that they ate a traditional mixed diet. A higher proportion of patients who reported having a non-traditional mixed diet expressed that they wanted to be involved in dietary discussions than those who had a traditional mixed diet (31 vs 20%; P = 0.002).
Smoking
Smoking was discussed with 25% of the patients, with no significant difference between women and men (26 vs 27%; P = 0.731). Only 1% of the patients who could not recall a discussion wanted to be involved in discussions of smoking habits (Fig. 1C). Thirteen per cent reported that they were current smokers. A higher proportion of ever smokers than never smokers had discussed their smoking habits with health-care professionals (32 vs 17%; P = 0.000), and a higher proportion of the ever smokers wanted to be involved in discussions of smoking habits (7 vs 2%; P = 0.001). There was no significant difference in medical treatment between those who had discussed smoking and those who had not (P = 0.008).
Alcohol consumption
Alcohol consumption was discussed with 17% of the patients, and more commonly with men than with women (22 vs 15%; P = 0.008). Nineteen per cent reported having a hazardous drinking pattern, and of those, 77% did not recall any discussion regarding alcohol. Two per cent reported that they wanted to be involved in discussions of alcohol consumption (Fig. 1D). A higher proportion of those who reported having hazardous drinking habits wanted to be involved in discussions of alcohol consumption than the proportion of those who had non-hazardous drinking (8 vs 4%; P = 0.018). There was no significant difference in medical treatment between those who had discussed alcohol and those who had not (P = 0.610).
Discussion
This study, based on patient reporting, showed that lifestyle habits were not discussed with the patients according to international and national recommendations [5]. Physical activity was discussed at least once with half of the patients with established RA. However, diet, smoking and alcohol consumption were discussed with only about a quarter of the patients. Between 10 and 15% of the patients reported that they wanted to be involved in discussions regarding physical activity and diet, but only 1‒2% of the patients wanted to be involved in discussions regarding smoking and alcohol consumption. In the present study, the question did not refer to any specific health-care setting or health professional, and given that all the patients included are enrolled in the BARFOT study, they have had at least seven follow-ups at a rheumatology unit.
The results from the present study suggest that discussions about physical activity have increased over the years; in 2013, less than one-third (28%) of the patients at a Swedish rheumatology outpatient clinic reported that they had discussed physical activity with their health professionals [31]. The Swedish national patient survey from 2018 found that 38% of patients in primary care had discussed physical activity, which is a lower proportion than in the present study [32]. One explanation for the higher proportion found in our study might be that most patients with RA meet a physiotherapist during the course of the disease, with numerous opportunities to discuss physical activity. This might also be the reason for physical activity being discussed more often than other lifestyle habits. Yet another explanation might be an increased understanding of the health benefits of physical activity in the general population.
Previous research has found that patients with RA often ask for dietary recommendations to improve their symptoms [33]. However, in 2013 only 8% (23% in the present study) of the patients at a rheumatology outpatient clinic reported that they had discussed diet [31]. Associations between diet and cardiovascular diseases, cancer and diabetes are well known and also apply to patients with rheumatic diseases [5, 34]. Whether or not a change of diet would influence the inflammatory activity in RA has been debated [35]. There are still no evidence-based dietary recommendations for patients with RA. In Sweden, patients with RA are encouraged to follow the same recommendations as the general population: increasing their intake of fruit and vegetables, increasing their intake of fish and shellfish to two or three times per week, choosing whole-grain products instead of refined-grain products, choosing low-fat dairy products instead of full-fat varieties and reducing their intake of red meat and refined sugar [36]. There is a need for further research on diet and its relationship to inflammation in RA. In the present study, a higher proportion of patients who reported having a non-traditional mixed diet (low-glycaemic, Mediterranean, vegetarian or vegan) wanted to be involved in dietary discussions. There is a well-known association between food intake and psychological well-being [37], which is why patients reporting a non-traditional mixed diet might have a personal interest in dietary impact on their health and the disease.
Given that environmental exposure has been implicated in the aetiology of RA [12] and that the most prominent risk factor for RA is smoking [38], discussions concerning smoking should be prioritized. In the present study, smoking was discussed with one-quarter of the patients, but a lower proportion of non-smokers recalled having any discussions, and they were also less interested in having them. This is worrying, because many patients are aware of the effects of smoking on general health but not the disease-specific effects on RA [39]. Cessation of smoking is important because of the negative response of smokers to disease-modifying anti-rheumatic therapy [13]. It is also important to discuss smoking habits with non-smokers, because smoking is an important environmental risk factor for RA, particularly in patients with specific genetics [38]. In the clinic, when introducing patients to medical treatment, counselling regarding smoking and alcohol habits [40] is recommended, and most rheumatologists (∼65%) do give advice on smoking cessation to patients with inflammatory diseases [41]. Yet another study found that half of the patients recalled some advice about smoking given by health professionals [42], a figure that is twice as high as in our study.
The definition of hazardous drinking patterns has varied in different surveys, but use of AUDIT-C indicated that 17% of the Swedish population reported having a hazardous drinking pattern in 2016, which is similar to the findings in the present study (19%) [5, 16]. In our study, alcohol consumption was seldom discussed, and patients with a hazardous drinking pattern often reported that they had not had any such discussion. Alcohol consumption is known to be one of the most challenging subjects for health-care professionals to bring up for discussion [43], but patients who take MTX and consume alcohol have an increased risk of developing liver disease [18]. The relationship between alcohol consumption and cardiovascular disease is complex. A population-based cohort study found conflicting associations between levels of alcohol consumption and initial presentations of a cardiovascular disease [44], which highlights the importance of counselling patients who are at high risk of cardiovascular disease, such as RA patients.
In the present study, a rather large proportion of the patients were not interested in discussing their lifestyle habits, which is a challenge. A goal in rheumatology care is to have well-informed and educated patients, to facilitate shared decision making. The EULAR-recommended patient-centred standards of care for RA encourage health professionals to prioritize discussions about lifestyle habits [45]. A limitation of the present study is that we lack information concerning the structure of the discussions from both the patients and the health professionals. In many clinics, these discussions are part of any regular visit, and special visits are not planned solely for lifestyle discussions. A structured intervention with a person-centred approach might be more effective [46, 47]. The suspected gap between health-care professionals’ and patients’ perceptions and expectations concerning lifestyle discussions in our study might indicate a lack of person centredness and shared decision making in the health-care system. Successful discussions must rely on a patient-centred approach and have more than information and facts, taking patients’ attitudes, motivations, goals, readiness for change, and social support into account [48]. More studies comparing different methods of initiating discussions about lifestyle are needed, and to determine why some patients decline such a conversation.
Conclusion
Physical activity was discussed at least once with half of the patients with established RA. Diet, smoking and alcohol consumption were discussed with only about one-quarter of them. Although these are higher figures than has been reported previously, there is a need for further improvement, because lifestyle habits are especially important in a long-standing disease, such as RA. Patient education concerning lifestyle issues should be an integral part of care management and an interactive process between patients and health professionals.
Supplementary Material
Acknowledgements
We thank the patients for generously sharing their experiences, and the BARFOT study group (for all members, see Supplementary material, available at Rheumatology Advances in Practice online).
Funding: This research was supported by grants from the Swedish Rheumatism Association, the County Council of Halland Research Fund and the Norrbacka-Eugenia Foundation.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1. Scott DL, Wolfe F, Huizinga TW.. Rheumatoid arthritis. Lancet 2010;376:1094–108. [DOI] [PubMed] [Google Scholar]
- 2. Englund M, Joud A, Geborek P. et al. Prevalence and incidence of rheumatoid arthritis in southern Sweden 2008 and their relation to prescribed biologics. Rheumatology 2010;49:1563–9. [DOI] [PubMed] [Google Scholar]
- 3. Cross M, Smith E, Hoy D. et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014;73:1316–22. [DOI] [PubMed] [Google Scholar]
- 4. Uhlig T, Moe RH, Kvien TK.. The burden of disease in rheumatoid arthritis. Pharmacoeconomics 2014;32:841–51. [DOI] [PubMed] [Google Scholar]
- 5. Agca R, Heslinga SC, Rollefstad S. et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis 2017;76:17–28. [DOI] [PubMed] [Google Scholar]
- 6. Hurkmans E, van der Giesen FJ, Vliet Vlieland TP, Schoones J, Van den Ende EC.. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev 2009;(4):CD006853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sandberg ME, Wedrén S, Klareskog L. et al. Patients with regular physical activity before onset of rheumatoid arthritis present with milder disease. Ann Rheum Dis 2014;73:1541–4. [DOI] [PubMed] [Google Scholar]
- 8. Benatti FB, Pedersen BK.. Exercise as an anti-inflammatory therapy for rheumatic diseases—myokine regulation. Nat Rev Rheumatol 2015;11:86–97. [DOI] [PubMed] [Google Scholar]
- 9. Gleeson M, Bishop NC, Stensel DJ. et al. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 2011;11:607–15. [DOI] [PubMed] [Google Scholar]
- 10. Ajeganova S, Andersson ML, Hafström I; BARFOT study group. Association of obesity with worse disease severity in rheumatoid arthritis as well as with comorbidities: a long-term followup from disease onset. Arthritis Care Res 2013;65:78–87. [DOI] [PubMed] [Google Scholar]
- 11.WHO. The world health report 2002: reducing risk, promoting healthy life. 2002. https://www.who.int/whr/2002/en/ (18 March 2019, date last accessed). [Google Scholar]
- 12. Lundberg K, Bengtsson C, Kharlamova N. et al. Genetic and environmental determinants for disease risk in subsets of rheumatoid arthritis defined by the anticitrullinated protein/peptide antibody fine specificity profile. Ann Rheum Dis 2013;72:652–8. [DOI] [PubMed] [Google Scholar]
- 13. Saevarsdottir S, Wedrén S, Seddighzadeh M. et al. Patients with early rheumatoid arthritis who smoke are less likely to respond to treatment with methotrexate and tumor necrosis factor inhibitors: observations from the Epidemiological Investigation of Rheumatoid Arthritis and the Swedish Rheumatology Register cohorts. Arthritis Rheum 2011;63:26–36. [DOI] [PubMed] [Google Scholar]
- 14. Maxwell JR, Gowers IR, Moore DJ, Wilson AG.. Alcohol consumption is inversely associated with risk and severity of rheumatoid arthritis. Rheumatology 2010;49:2140–6. [DOI] [PubMed] [Google Scholar]
- 15. Nissen MJ, Gabay C, Scherer A, Finckh A; Swiss Clinical Quality Management Project in Rheumatoid Arthritis. The effect of alcohol on radiographic progression in rheumatoid arthritis. Arthritis Rheum 2010;62:1265–72. [DOI] [PubMed] [Google Scholar]
- 16. Bergman S, Symeonidou S, Andersson ML, Söderlin MK; BARFOT study group. Alcohol consumption is associated with lower self-reported disease activity and better health-related quality of life in female rheumatoid arthritis patients in Sweden: data from BARFOT, a multicenter study on early RA. BMC Musculoskelet Disord 2013;14:218.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Klatsky AL. Alcohol and cardiovascular diseases: where do we stand today? J Intern Med 2015;278:238–50. [DOI] [PubMed] [Google Scholar]
- 18. Kremer JM, Weinblatt ME.. Quantifying the hepatotoxic risk of alcohol consumption in patients with rheumatoid arthritis taking methotrexate. Ann Rheum Dis 2018;77:e4. [DOI] [PubMed] [Google Scholar]
- 19. Andersson ML, Forslind K, Hafström I.. Comparing five year out-come in two cohorts of patients with early rheumatoid arthritis – a BARFOT study. Open Rheumatol J 2015;9:8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arnett FC, Edworthy SM, Bloch DA. et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. [DOI] [PubMed] [Google Scholar]
- 21.Swedish State Institute of Public Health. National health survey: health on equal terms. Merging of data from the period 2007–2010. https://snd.gu.se/en/catalogue/study/ext0114 (18 March 2019, date last accessed).
- 22. Haglund E, Bergman S, Petersson IF. et al. Differences in physical activity patterns in patients with spondylarthritis. Arthritis Care Res 2012;64:1886–94. [DOI] [PubMed] [Google Scholar]
- 23. Olsson SJG, Ekblom Ö, Andersson E, Börjesson M, Kallings LV.. Categorical answer modes provide superior validity to open answers when asking for level of physical activity: A cross-sectional study. Scand J Public Health 2016;44:70–6. [DOI] [PubMed] [Google Scholar]
- 24. Haskell WL, Lee I-M, Pate RR. et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007;39:1423–34. [DOI] [PubMed] [Google Scholar]
- 25. Söderlin MK, Petersson IF, Bergman S, Svensson B; BARFOT study group. Smoking at onset of rheumatoid arthritis (RA) and its effect on disease activity and functional status: experiences from BARFOT, a long-term observational study on early RA. Scand J Rheumatol 2011;40:249–55. [DOI] [PubMed] [Google Scholar]
- 26. Fleming MF, Barry KL, MacDonald R.. The alcohol use disorders identification test (AUDIT) in a college sample. Int J Addict 1991;26:1173–85. [DOI] [PubMed] [Google Scholar]
- 27. Ekdahl C, Eberhardt K, Andersson SI, Svensson B.. Assessing disability in patients with rheumatoid arthritis. Use of a Swedish version of the Stanford Health Assessment Questionnaire. Scand J Rheumatol 1988;17:263–71. [DOI] [PubMed] [Google Scholar]
- 28. Hurst NP, Kind P, Ruta D, Hunter M, Stubbings A.. Measuring health-related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D). Br J Rheumatol 1997;36:551–9. [DOI] [PubMed] [Google Scholar]
- 29. Joos E, Peretz A, Beguin S, Famaey JP.. Reliability and reproducibility of visual analogue scale and numeric rating scale for therapeutic evaluation of pain in rheumatic patients. J Rheumatol 1991;18:1269–70. [PubMed] [Google Scholar]
- 30. Fries JF, Spitz P, Kraines RG, Holman HR.. Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137–45. [DOI] [PubMed] [Google Scholar]
- 31. Bergman S, Bremander A.. Lifestyle factors were seldom discussed with patients visiting a rheumatology clinic. Arthritis Rheum 2013;65:S982–3. [Google Scholar]
- 32.The Public Health Agency of Sweden. Health on equal terms. 2018. www.npe.skl.se (18 March 2019, date last accessed).
- 33. Tedeschi SK, Frits M, Cui J. et al. Diet and rheumatoid arthritis symptoms: survey results from a rheumatoid arthritis registry. Arthritis Care Res 2017;69:1920–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Michaud K, Wolfe F.. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol 2007;21:885–906. [DOI] [PubMed] [Google Scholar]
- 35. Winkvist A, Bärebring L, Gjertsson I, Ellegård L, Lindqvist HM.. A randomized controlled cross-over trial investigating the effect of anti-inflammatory diet on disease activity and quality of life in rheumatoid arthritis: the Anti-inflammatory Diet In Rheumatoid Arthritis (ADIRA) study protocol. Nutr J 2018;17:44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Swedish National Board of Welfare (Socialstyrelsen). National guidlines for prevention and treatment of unhealthy lifestyle (Nationella riktlinjer för prevention och behandling vid ohälsosamma levnasvanor). 2018. www.socialstyrelsen.se/regler-och-riktlinjer/nationella-riktlinjer/slutliga-riktlinjer/levnadsvanor (18 March 2019, date last accessed).
- 37. Lee YH, Shelley M, Liu CT, Chang YC.. Assessing the association of food preferences and self-reported psychological well-being among middle-aged and older adults in contemporary China-results from the China Health and Nutrition Survey. Int J Environ Res Public Health 2018;15:E463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. van Wesemael TJ, Ajeganova S, Humphreys J. et al. Smoking is associated with the concurrent presence of multiple autoantibodies in rheumatoid arthritis rather than with anti-citrullinated protein antibodies per se: a multicenter cohort study. Arthritis Res Ther 2016;18:285.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Malm K, Bremander A, Arvidsson B. et al. The influence of lifestyle habits on quality of life in patients with established rheumatoid arthritis-A constant balancing between ideality and reality. Int J Qual Stud Health Well-being 2016;11:30534.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tedeschi SK, Costenbader KH.. Is there a role for diet in the therapy of rheumatoid arthritis? Curr Rheumatol Rep 2016;18:23.. [DOI] [PubMed] [Google Scholar]
- 41. Naranjo A, Khan NA, Cutolo M. et al. Smoking cessation advice by rheumatologists: results of an international survey. Rheumatology 2014;53:1825–9. [DOI] [PubMed] [Google Scholar]
- 42. Aimer P, Stamp L, Stebbings S. et al. Identifying barriers to smoking cessation in rheumatoid arthritis. Arthritis Care Res 2015;67:607–15. [DOI] [PubMed] [Google Scholar]
- 43. Hörnsten Å, Lindahl K, Persson K, Edvardsson K.. Strategies in health-promoting dialogues – primary healthcare nurses' perspectives – a qualitative study. Scand J Caring Sci 2014;28:235–44. [DOI] [PubMed] [Google Scholar]
- 44. Bell S, Daskalopoulou M, Rapsomaniki E. et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ 2017;356:j909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Stoffer MA, Smolen JS, Woolf A. et al. Development of patient-centred standards of care for rheumatoid arthritis in Europe: the eumusc.net project. Ann Rheum Dis 2014;73:902–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pinto RZ, Ferreira ML, Oliveira VC. et al. Patient-centred communication is associated with positive therapeutic alliance: a systematic review. J Physiother 2012;58:77–87. [DOI] [PubMed] [Google Scholar]
- 47. Primdahl J, Clausen J, Hørslev-Petersen K.. Results from systematic screening for cardiovascular risk in outpatients with rheumatoid arthritis in accordance with the EULAR recommendations. Ann Rheum Dis 2013;72:1771–6. [DOI] [PubMed] [Google Scholar]
- 48. Knittle K, De Gucht V, Maes S.. Lifestyle- and behaviour-change interventions in musculoskeletal conditions. Best Pract Res Clin Rheumatol 2012;26:293–304. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.