Abstract
Introduction
Obesity is a public health concern that is becoming increasingly more serious worldwide. Effective and sustainable childhood obesity prevention strategies may help to reduce the prevalence of obesity and may have an impact on lifelong health. However, few such strategies have been rigorously evaluated for Chinese children in different regions of China.
Methods and analysis
The Diet, ExerCIse and CarDiovascular hEalth-Children is a cluster-randomised controlled trial that aims to assess the effectiveness and sustainability of a school-based, multi-faceted intervention to prevent obesity among Grade 4 primary school students (8–10 years old) in China. Twenty-four schools (approximately 1200 students) from above average, average and below average developed regions in China will be randomised to an intervention (12 schools) or usual practice (12 schools) group. The intervention will last for one school year (9 months) and consists of activities towards students, parents and school environment. A smartphone application will be used to assist in providing information on, monitoring and providing feedback on the behaviours and body weight of the students. Data will be collected at baseline, 4 months, 9 months and 21 months. The primary outcome will be the difference between groups in the change in students’ body mass index at 9 months after the baseline investigation. The secondary outcomes will include the differences between groups in the changes in anthropometric measures, diet, physical activity levels and other measures at the follow-up visits. A variety of process evaluation methods will be used to evaluate the implementation process of the complex intervention.
Ethics and dissemination
This study was approved by the Peking University Institution Review Board (IRB00001052-18021). The results will be disseminated through publication in peer-reviewed journals, presentations at conferences and in lay summaries provided to school staff and participants.
Trial registration number
Keywords: pediatric obesity, cluster, prevention, randomised controlled trial
Strengths and limitations of this study.
This study will rigorously evaluate the effectiveness of a childhood obesity prevention programme in eastern, central and western regions with different levels of economic development in China.
We will employ a smartphone application to assist in providing information on, monitoring and providing feedback on the behaviours and body weight of the students.
We will include an explicit process evaluation plan for both the intervention and the control groups, which will evaluate the implementation process of the complex intervention.
A follow-up investigation will be conducted to evaluate the sustainability of the intervention.
This intervention is limited by a relatively short duration, but additional funding will be sought for the implementation of a long-term intervention in the future.
Introduction
Childhood obesity is a significant public health concern worldwide.1 2 In China, childhood obesity has dramatically increased as the economy has grown quickly over the past decades. The prevalence of obesity among 7- to 18-year-old Chinese children increased from 0.1% in 1985 to 7.3% in 2014.2 Childhood obesity is associated with not only adverse consequences on the physical and mental health of children in the short term,3 4 but also increases the risk of developing cardiovascular diseases in the long term.5 6 Accordingly, effective strategies to curb and reduce childhood obesity prevalence may help to prevent cardiovascular diseases in the whole population in the long term.
The development of childhood obesity is complex and may involve multi-factorial mechanisms, but in most cases, it essentially results from an imbalance between energy intake and energy expenditure. Children spend half of their waking hours at school and consume at least one-third of their daily calories at school; thus, school-based interventions are promising in preventing childhood obesity.7 In particular, multi-faceted interventions combining diet, physical activity and a family component have shown the highest effectiveness.7 8 However, there is a paucity of rigorously developed and evaluated prevention interventions for Chinese children.8 9 Moreover, not all school-based interventions have been effective in preventing excessive weight gain in children.10 11 One potential interpretation of this finding is that adherence to the intervention components was not guaranteed.11 It is thus crucial to increase our understanding of how and why these interventions work or do not work.12 To achieve this, a thorough process evaluation of the intervention implementation is necessary. Furthermore, socioeconomic development is associated with patterns of childhood obesity13 and may also affect the effectiveness of a childhood obesity intervention. Social disparities in the patterns of obesity differ between China and Western countries. In China, socioeconomic development has been positively associated with overweight and obesity prevalence in children.13 However, previous studies have been largely conducted in a single region, which limits the generalizability of study findings to other populations. Another weakness is that most studies examined outcomes only at the end of the intervention. Thus, it remains unclear whether healthy behaviours and a healthy weight are maintained beyond the period of the intervention.
School system in China
In primary schools in China, there are six grades in total, and the age of the students ranges from 6 to 11 years. The typical size of a Chinese class is fewer than 45 students, but varies in different schools, ranging from 30 to 60 students. There are two school policies that have been issued by the Chinese government that are particularly relevant to the prevention and management of childhood obesity. First, schools should have school doctors or healthcare teachers who provide in-house school healthcare. The routine practices include student health surveillance, health education for students and the prevention and control of common diseases in students. Second, schools should implement ‘One-Hour Physical Activity On Campus Every School Day’. That is, the total duration of physical activity (ie, physical education classes, exercises during breaks from class and extracurricular activities) per school day should be no less than 1 hour. However, the implementation of these policies in the school systems in China varies by region.14
Development of a childhood obesity intervention
To fill in research gaps, in accordance with the school systems in China, we underwent four stages to develop the intervention: (1) we systematically reviewed previous literature to identify intervention elements related to intervention effectiveness; (2) we conducted focus group discussions and interviews with key informants (children, parents, teachers, school principals, local health and education officials) to further revise and refine the intervention approaches; (3) we conducted a 3-month, before-after, pilot study at two primary schools in Beijing (one in an urban area and the other in a rural area) involving 58 Grade 4 students (mean age: 9.38±0.49 years) to test the feasibility of the proposed intervention15; and (4) we further discussed the proposed intervention with multiple experts. Based on all the work mentioned, we finally developed the intervention elements used for this study.
Aim and objectives
To develop effective lifestyle interventions for the prevention and control of cardiovascular disease in China, the Diet, ExerCIse and CarDiovascular hEalth (DECIDE) project was initiated in 2016. As one of five independent DECIDE studies, the DECIDE-Children study aims to develop a school-based, multi-faceted childhood obesity prevention programme targeting school children aged 8–10 years in three different regions of China and rigorously test its effectiveness in preventing excessive weight gain in Chinese primary school settings. The research objectives of the DECIDE-Children study were (1) to assess the effectiveness of the intervention compared with the usual practice in preventing childhood overweight and obesity; (2) to determine the sustainability of the intervention in preventing overweight and obesity; and (3) to evaluate the process and health economics of the intervention.
Methods and analysis
This protocol has been prepared in accordance with the Standard Protocol Items: Recommendations for Interventional Trials statement.16 17
Study design
DECIDE-Children is a cluster-randomised, parallel-group controlled trial. To accommodate the social and economic variations within the country, we will intentionally select schools from three different regions of China: the above average developed area in the east (Beijing), the average developed area in central China (Shanxi) and the below average developed area in the west (Xinjiang). A total of 24 primary schools (clusters) equally distributed among three regions will be selected. In Beijing, 4 schools will be selected from the Dongcheng district (located in the centre of the city), and four will be selected from the Mentougou district (located in a rural suburban area). In Xinjiang, all eight schools will be selected from Urumchi, the capital city of the autonomous region: four of the schools will be selected from the Shayiba district (an urban district) and the other four schools will be selected from the Shuimogou district (a rural district). In Shanxi, all eight schools will be selected from only one urban district, Changzhi, a small/medium-sized city in the province. The reason for excluding rural schools in Changzhi is that most of the rural schools are boarding schools, and parents are difficult to reach in boarding schools. Thus, a total of 24 primary schools from five sites in three regions will be selected and randomised into two groups, the obesity prevention intervention group and the usual practice group. The intervention will be implemented for one school year from late September 2018 to June 2019, and the study will continue with a 1-year follow-up investigation in June 2020. Figure 1 shows the flow of the study.
Figure 1.
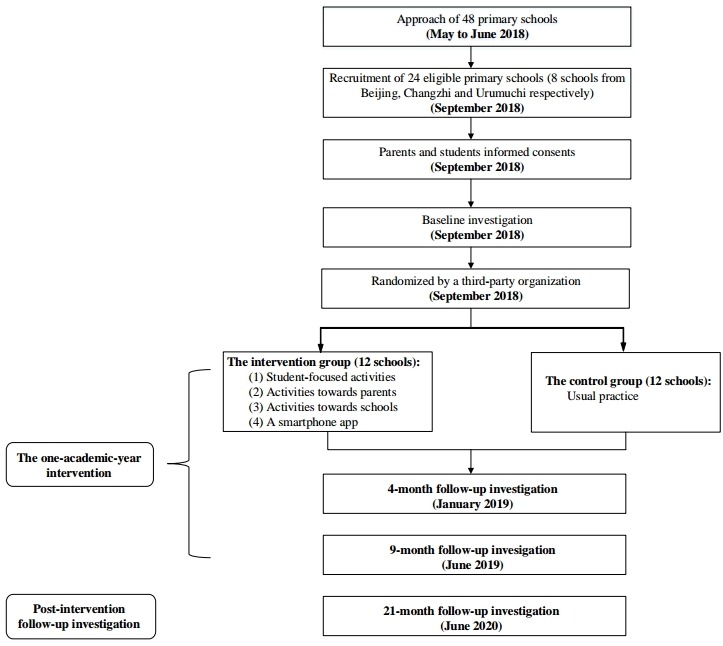
Flow chart of the Diet, ExerCIse and CarDiovascular hEalth-Children study.
Recruitment
Recruitment of the schools
This study will be carried out in Grade 4 students (8–10 years old), as they are sufficiently mature to understand health education information and are able to remain in the same school to complete the 2-year study before they graduate. For a school to be eligible, the school principal must agree with the randomisation procedure and comply with the study protocol. The total number of Grade 4 students must be greater than 50 in the school, and schools that have implemented or are planning to implement an obesity prevention intervention or similar intervention programme will not be eligible. Boarding schools and specialty schools for children with talents or minority ethnic groups will be excluded. Schools will also not be included if they have a definite plan for relocation or cancellation in the next 2 years. For the schools participating in the programme, the size of a class will vary between fewer than 30 children and approximately 60 children per class. If the number of students in each class is less than 50, we will recruit two classes from the school, and if the number of students is greater than 50, we will recruit one class to meet the sample size requirement. If there are more classes in one school than needed for the study, the school principal will recommend which classes we should select.
Three steps will be followed for the recruitment of the schools. First, project staff will contact the local education authorities to gain their opinion, support and approval of the study and basic information of the schools (type of schools and the number of students and teachers). Second, project staff will contact the schools by phone or visit the schools to determine the eligibility of the selected schools for the study. Third, the final list of eligible schools and classes will be made by the principal investigator and schools will be invited to participate in the study by local research partners.
Recruitment of the students
After recruiting the schools and before conducting the baseline measurements, written informed consent will be provided by all students and their primary caregivers (parents in most cases) in the selected classes. Then, the parents who provide informed consent will be required to complete a questionnaire about the health status of their children. The project staff will collect the questionnaires and if a parent reports one of the following conditions, his or her children will be excluded: (1) medical history of heart disease, hypertension, diabetes, tuberculosis, asthma, hepatitis or nephritis; (2) obesity caused by endocrine diseases or side effects of drugs; (3) abnormal physical development like dwarfism or gigantism; (4) physical deformity such as severe scoliosis, pectus carinatum, limp, obvious O-leg or X-leg; (5) inability to participate in school sport activities; and (6) a loss in weight by vomiting or taking drugs during the past 3 months.
Randomisation procedures
The random sequence of allocation of the schools (clusters) to the intervention or control group will be stratified by the study sites. Schools in the same study site will be randomly allocated in a 1:1 ratio to either the intervention or control group using a computer-generated random number system (the simple random sampling method). Randomisation will be performed by an independent person at the central coordinating centre at Peking University Clinical Research Institute. The randomisation will take place only after the baseline measurements are completed to ensure allocation concealment.
Intervention
We used the social ecological model to identify intervention elements in this multi-faceted health promotion programme.18 As shown in figure 2, the programme will target the influencing factors of childhood obesity at both individual (student-focused activities) and environmental levels (a supportive family and school environment), with the intent to influence the knowledge, attitude and behaviours of school children.
Figure 2.
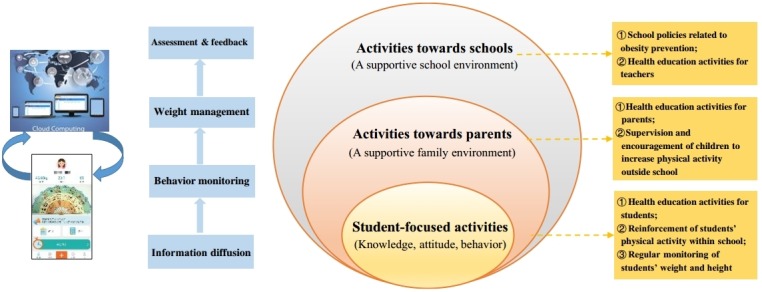
The social ecological model as applied to the Diet, ExerCIse and CarDiovascular hEalth-Children study.
Description of the intervention components
The intervention components are described in tables 1 and 2.
Table 1.
Description of the intervention components implemented in the DECIDE-Children study
| Intervention components | Descriptions of the content, frequency and duration | Person responsible |
| 1. Student-focused activities | ||
| Health education activities for students | (1) Frequency and duration
A total of ten activities (each lasting 40 min) will be provided once every two to 3 weeks (six activities will be arranged in the first semester, and four will be arranged in the second semester). (2) Different kinds of activities The ten activities will include seven health education lectures and three theme class meetings. The focus of the health education lectures will be on information diffusion, while the focus of theme class meetings will be on consolidation of the key messages learnt in health education lectures through interactive and interesting group work (eg, ‘Let me guess’). (3) Content 1) Information diffusion Key messages will include the benefits of healthy weight, measurements and assessments of weight, and methods of achieving a healthy weight (not eating excessively; not drinking sugar-sweetened beverage; eating less high-energy food; less sedentary behaviours; performing more physical activity). Health education books and ‘nutrition evaluation turnplate for Chinese primary and middle school students’ will be delivered to students. Health education messages will also be spread through posters on campus or in the classroom. 2) Promotion for translating knowledge into action ‘Small hand in big hand’ homework (eg, ‘challenge of 3 days away from screen’) will be arranged at the end of each health education activity. 3) Feedback and encouragement for BMI and behaviour change Feedback of regular monitoring results of students’ BMIs and behaviours will be provided in each health education activity. The students with good performance will be encouraged. |
The trained class teachers |
| Reinforcement of students’ physical activity within school | 1) Students will be instructed by physical education teachers to perform physical activities with moderate-to-vigorous intensity at school for at least 1 hour per school day (including physical education classes, class-break exercise, extracurricular activities). The aim of this component will be to improve the adherence to the Chinese national requirement for ‘One-Hour Physical Activity On Campus Every School Day’. If a school has met this requirement, no extra physical activities will be added at the school; otherwise, extra physical activities (ie, physical education classes, exercises during breaks in class or extracurricular activities) will be added to the school schedule. The monitoring of the implementation of these extra physical activities will be continuous within the intervention period for the intervention group; 2) Physical education teachers will be advised to teach students at least one sports game during each extracurricular activity. |
The trained physical education teachers |
| Regular monitoring of students’ weight and height |
1) Monthly monitoring
Students’ weight and height will be monitored monthly, and the data will then be input into the computer management system in a timely manner and shown in the smartphone app (described below); 2) Weekly monitoring Students’ weight will be monitored weekly by the students themselves in the classroom. |
The trained school doctors/healthcare teachers with the assistance of the trained project staff (for monthly monitoring); The trained project staff (for data input of monthly monitoring) Students (for weekly monitoring) |
| 2. Activities towards parents (providing a supportive family environment) | ||
| Health education activities for parents | 1) Frequency and duration
At least one activity (lasting for approximately 40–60 min) will be held at the beginning of each semester. One more activity will be held in the middle of the first semester. Another activity will also be held in the middle of the second semester if necessary (for example, if the fidelity of the data is unsatisfactory). 2) Contents
Key messages will be similar to those for the health education activities for students (described earlier). Parents will also be taught to use the smartphone app.
Project staff will provide feedback about students’ weight status and behaviours to parents. Face-to-face group discussions will be established between the project staff and parents. |
The trained project staff |
| Reinforcement of students’ physical activity outside school | 1) Parents will be instructed to supervise and encourage students to perform physical activities outside of school for 30 min per weekday and 1 hour per weekend day; 2) Recommendations for physical activity outside of school will be provided through the smartphone app once every 2 months; 3) Students will be encouraged to participate in sports games outside of school that will be taught by their physical education teachers during extracurricular activities. |
Students’ parents |
| 3. Activities towards schools (providing a supportive school environment) | ||
| School policies related to obesity prevention | The following school policies will be suggested: 1) ‘Not selling’: Not selling unhealthy snacks* or sugar-sweetened beverages within school; 2) ‘Not eating’: Telling students not to eat unhealthy snacks or drink sugar-sweetened beverages at school; 3) ‘Not buying’: Students being educated by class teachers not to buy unhealthy snacks or sugar-sweetened beverages around school. |
The trained school principal; The trained class teachers |
| Health education activities for school teachers |
1) Frequency and duration
The activity will be held once (lasting for approximately 40 min) in the first month of the intervention. School teachers participating in this programme at each school (school principal, class teachers, school doctors/healthcare teachers and physical education teachers) will be required to attend the activity. 2) Content Key messages will be similar to those for the health education activities for students (described earlier). School teachers will also be taught to use the smartphone app. |
The trained project staff |
| 4. A smartphone app assisted in implementation of the intervention | ||
| The smartphone app (‘Eat Wisely, Move Happily’) |
1) Information diffusion (the BCT used: providing information on consequences of behaviours) The smartphone app will provide information to parents, class teachers and project staff in accordance with the health education activities. 2) Behaviour monitoring (the BCT used: prompting the self-monitoring of behaviours) Parents together with their children will be asked to record the diet and physical activity behaviours of students in the app weekly, and then they will receive individualised feedback related to these behaviours (described in table 2). 3) Weight management (the BCT used: prompting self-monitoring) According to the monthly monitoring of students’ weight and height (described earlier), parents, school teachers and project staff will view the recent weight status (categorised according to the BMI percentile criteria24), changes compared with previous records of the students and the individualised feedback related to weight management (described in table 2). 4) Assessment and feedback (the BCT used: providing feedback on performance) The smartphone app will also provide a synthetic and individualised assessment that will combine changes in the behaviours and weight status of the students. The four kinds of feedback are shown in table 2. |
The smartphone app (installed by parents, school teachers and project staff) and the computer management system (utilised by project staff) |
*‘Healthy snacks’ refer to dairy products, fresh vegetables or fruits and natural unprocessed nuts that are eaten at times other than at main meals. ‘Unhealthy snacks’ refer to snacks other than the three kinds of healthy snacks.
BCT, behaviour change technique; BMI, body mass index; DECIDE, Diet, ExerCIse and CarDiovascular hEalth.
Table 2.
The four kinds of regular evaluation feedback messages provided to all stakeholders by the smartphone mobile app on the basis of data from the regular monitoring of children’s weight, height and behaviours
| Results automatically judged according to the heights and weights measured at the regular monitoring intervals | |||
| Positive results (BMI decreases in students who are overweight or obese, or BMI increases in students who are underweight) |
Negative results (BMI increases in students who are overweight or obese, or BMI decreases in students who are underweight) |
||
| Results automatically judged according to the diet and physical activity behaviours recorded regularly | Full marks/getting better | Feedback 1: ‘Your child is doing a great job. The weight changes are consistent with the changes in the diet and physical activity behaviours. Keep it up!’ | Feedback 2: ‘Your child’s weight has not improved, but the diet and physical activity behaviours are good. It might be that weight improvement requires long-term adherence to a reasonable diet and physical activity behaviour, or that the behaviour records are inaccurate. Please continue to improve!’ |
| Unchanged/getting worse | Feedback 3: ‘Your child has improved or maintained a healthy body weight, but there is still room for improvement in the diet and physical activity behaviours. Keep working!’ | Feedback 4: ‘Your child’s weight has not improved, and the diet and physical activity behaviours also need improvement. Please continue to work hard!’ | |
BMI, body mass index.
Student-focused activities
These activities will include health education activities for students, the reinforcement of students’ physical activity at school and the regular monitoring of students’ weight and height.
Activities towards parents
These activities will include health education activities for parents and the supervision and encouragement of children to increase their physical activity level outside of school.
Activities towards schools
These activities will include school policies related to obesity prevention and health education activities for teachers.
The smartphone APP
Project staff, school teachers and parents will be suggested to install the app titled ‘Eat Wisely, Move Happily’. The app, which was developed based on behaviour change techniques,19 will aid in information diffusion, behaviour monitoring, weight management, assessment and feedback.
Quality control of the intervention
Two manuals (‘An Operation Manual for Project Staff Involved in the Multi-component Obesity Intervention among Primary School Students’ and ‘An Operation Manual for School Team Members Involved in the Multi-component Obesity Intervention among Primary School Students’) have been developed for implementing and managing this complex intervention. The manuals describe in detail the duties of project staff and school team members (school principals, class teachers, physical education teachers, school doctors/healthcare teachers) in delivering the intervention. The manuals also describe the detailed workflow of the implementation of each intervention component, that is, by whom, when, how and to what extent the specific intervention element should be delivered. All of the project staff and school team members will be required to conduct the intervention in accordance with the operation manuals.
During implementation of the intervention, regular field observations will be made and the smartphone app records will be checked. If it is found that schools are not complying with the study protocol, project staff will communicate with school team members in a timely manner and conduct follow-ups to improve the fidelity of the study results.
Control group
The 12 schools in the control group will not carry out any of the DECIDE-Children intervention components and will continue their usual practice according to their own teaching curriculum during the study period (from September 2018 to June 2020). Participants in the control group will receive the same health education materials that will have been delivered to those in the intervention group immediately after the 21-month follow-up investigation is completed in June 2020.
Outcome evaluation
Table 3 describes the study outcomes, including when and how the study outcomes will be evaluated. Baseline measurements will be conducted in September 2018 for both the intervention and the control groups. Follow-up measurements will be conducted 4 months after the baseline measurements are conducted in January (after one school semester and half way through the intervention), 9 months after the baseline measurements are conducted in June 2019 (after one school year and immediately after the whole intervention programme is completed) and 21 months after the baseline measurements are conducted in June 2020 (after two school years and 12 months after the intervention is completed).
Table 3.
Outcome measurements for the DECIDE-Children study
| Outcomes | Time | Device (Manufacturer, model) | Method | |||
| Baseline | 4 months after baseline | 9 months after baseline | 21 months after baseline | |||
| Anthropometric measures | ||||||
| Height | √ | √ | √ | √ | Stadiometer (Huateng GMCS-1) |
Measured to the nearest 0.1 cm at least twice |
| Weight | √ | √ | √ | √ | Lever scale (Wujin RGT-140) |
Measured to the nearest 0.1 kg at least twice |
| Waist circumference | √ | √ | √ | √ | Tape (MyoTape) |
Measured to the nearest 0.1 cm at least twice |
| Hip circumference | √ | √ | √ | √ | Tape (MyoTape) |
Measured to the nearest 0.1 cm at least twice |
| Systolic and diastolic blood pressures | √ | √ | √ | √ | Electronic sphygmomanometer (Omron HBP-1300) |
Measured to the nearest 1 mm Hg at least twice |
| Body fat percentage | √ | √ | Body component instrument (Tanita MC-780 MA) |
According to the standard procedure | ||
| Physical fitness measures | ||||||
| One-minute rope jumping | √ | √ | Physical fitness measures will be assessed by trained outcome assessors according to the standard procedure. | |||
| One-minute sit-up | √ | √ | ||||
| Long-standing jump | √ | √ | ||||
| Shuttle run (50 m×8) | √ | √ | ||||
| Behavioural measures and other measures | ||||||
| Students’ knowledge related to energy balance | √ | √ | We will use eight items to assess the change in students' knowledge related to energy balance. For example, we will ask students, ‘Is it correct that drinking sugar-sweetened beverage cannot substitute drinking water ?’ Three choices will be provided (right; wrong; not clear). Students should finish the questionnaires in the classroom in the presence of the trained outcome assessors, who can provide guidance and help. |
|||
| Students’ duration of moderate-to-vigorous physical activity | √ | √ | The questions were designed based on a validated 7-day PAQ (kappa values for test-retest results were 0.46~0.79 (different measures of activity), face validity and content validity were good based on experts’ evaluations, and the correlations between the PAQ and Caltrac motion sensor data ranged from 0.38 to 0.46 (different measures of activity) for boys).21
Students should finish the questionnaires in the classroom in the presence of the trained outcome assessors, who can provide guidance and help. |
|||
| Students’ eating behaviour | √ | √ | We will use the ‘Children Eating Behaviour Questionnaire’ to assess students' eating behaviours, including their responsiveness to food and enjoyment of food. This 35-item instrument has been shown to have relatively good reliability.22
The questionnaires should be self-reported by parents or other primary caregivers of the students. |
|||
| Students’ sedentary behaviour | √ | √ | We will use a self-designed questionnaire to determine the average duration of completing homework, watching television and playing electronic devices per day during the last week. Students should finish the questionnaires in the classroom in the presence of the trained outcome assessors, who can provide guidance and help. |
|||
| School policies for the prevention and management of childhood obesity | √ | √ | The questionnaires should be filled by the trained investigators after face-to-face interviews with school principals, doctors/healthcare teachers and physical education teachers. | |||
| Stage of readiness for behaviour change related to weight reduction | √ | √ | We will use two items for the assessment. First, we will ask ‘Have you taken action to reduce your weight during the last 3 months?’ Yes/no choices will be provided. In addition, we will ask ‘Do you currently intend to reduce your weight?’ Five choices ranging from ‘completely do not intend’ to ‘intend to very much’ will be provided. Students should finish the questionnaires in the classroom in the presence of the trained outcome assessors, who can provide guidance and help. |
|||
PAQ, physical activity questionnaire.
At the baseline and all follow-up visits, anthropometric measures (height, weight, waist and hip circumference, systolic and diastolic blood pressures, body fat percentage) and physical fitness measures (1-min rope jumping, 1-min sit-up, long-standing jump, shuttle run (50 m×8)) will be collected by the trained outcome assessors using the same device and/or forms according to the standard methods and procedures. The assessors measuring students’ height and weight will be blinded to the group allocation of the schools. We will use questionnaires to measure students’ behaviours (duration of moderate-to-vigorous physical activity, eating behaviour, sedentary behaviour), school policies for prevention and management of childhood obesity, and other potential moderators/mediators of the intervention (eg, stage of readiness for behaviour change related to weight reduction). The questionnaires were developed based on earlier studies and the pilot study. The questionnaires were found to be feasible for this study and acceptable to students and their parents.20–22
Outcomes
The primary outcome is the difference between groups in the change in students’ body mass index (BMI=weight (kg)/(height (m))2) immediately after the intervention completion (9 months after the baseline measurements are conducted). The secondary outcomes include the change in BMI 1 year after the intervention is completed (21 months after the baseline measurements are conducted). In addition, we will compare the following indices between groups at the follow-up visits: 1) change in students’ BMI z-score (SD score will be calculated based on the WHO criteria23); 2) change in prevalence and incidence of childhood overweight/obesity defined according to the criteria for Chinese children and adolescents24; 3) change in students’ waist circumference, waist-to-hip circumference ratio and systolic and diastolic blood pressures; and 4) change in students’ body fat percentage, physical fitness measures, behavioural outcomes (including students’ duration of moderate-to-vigorous physical activity, students’ eating behaviour and students’ sedentary behaviour) and other outcomes (including students’ knowledge related to energy balance, school policies for the prevention and management of childhood obesity and stage of readiness for behaviour change related to weight reduction).
Sample size estimation
We assumed that the difference between the two groups in the change in BMI (effect size) would be 0.50 kg/m2, the SD of the BMI would be 1.40 kg/m2, the intra-cluster correlation coefficient would be 0.05 and the rate of attrition would be 10% for the sample size calculation in our study. We aimed to recruit a total of 1200 students from 24 schools with an average cluster size of 50 students per school. This sample size will provide 88% power with a=0.05 to detect a mean difference of 0.50 kg/m2 in the change in BMI between groups after the intervention lasting one school year.
Statistical analyses
Statistical analyses will be performed using SAS V.9.4 (SAS Institute). All statistical tests will be two-sided at the 5% level of significance. Baseline characteristics at both the school and individual levels will be reported by using descriptive statistics.
The primary analysis will be based on the intention-to-treat principle and includes all students recruited with the baseline BMIs measured. Generalised linear mixed models will be used to compare the primary and secondary outcomes at 4, 9 and 21 months after the baseline measurements are conducted, and the models will adjust for the clustering effect and baseline outcome values. The missing data will be treated in the maximum likelihood estimates assuming they are missing at random. The intra-cluster correlation coefficient will also be estimated. Sensitivity analysis will be performed on the primary outcome using the last-value-carry-forward imputation if the percentage of missing data exceeds 5%. For continuous outcomes, we will report pre/post-intervention means for the intervention and control groups and model-adjusted mean differences between groups. For binary outcomes, we will report pre/post-intervention percentages for the intervention and control groups and adjusted ORs between groups. The 95% CIs and associated p values will be calculated. We will also examine whether the differences in the outcomes between the control and intervention groups vary by the three regions (Beijing, Shanxi, Xinjiang), the sex of children, socioeconomic status (mother’s education), BMI status at baseline and primary caregivers of the children (parents compared with non-parents).
Process evaluation
Based on the steps and principles described in the conceptual framework by Saunders et al,25 we will identify the process evaluation elements including fidelity (the extent to which the intervention will be implemented as initially planned), dose delivered (the frequency and intensity of the actual implementation of the programme), dose received (the extent to which students/primary caregivers (parents in most cases)/teachers will be exposed to the intervention, as well as the degree of their satisfaction with the intervention and materials), reach (the proportions and the characteristics of students/primary caregivers/teachers completing or dropping out of the intervention) and context (family environment and school policies related to obesity prevention and management).
The implementation process data collection procedure will include (1) direct regular field observation and records which will be collected for the quality control of the intervention (eg, quality and quantity of the intervention sessions and number of students attending the lectures) and will be recorded by the trained project staff; (2) the user logs (eg, frequency and duration) which will be collected by the smartphone app; (3) school policies related to obesity prevention and management, which will be collected by the questionnaires (table 3) in both the intervention and the control groups; and (4) interviews with participants (6–8 students per school) which will be conducted in both the intervention and the control groups.
Health economics evaluation
A cost-effectiveness analysis will be employed in the health economics evaluation, and a societal perspective will be used to examine whether the intervention is economically feasible. Intervention costs will include hours spent by project staff, school staff and students’ primary caregivers (parents in most cases) for all the intervention activities and material expenses. Only the time spent by the project staff in implementing the intervention will be included. Time costs will be based on personal employment compensations if available or average compensations in the local areas for similar types of employees. Material expenses will be based on the actual purchasing prices. An incremental cost-effectiveness ratio will be calculated and a sensitivity analysis will be used to vary key parameters to examine the robustness of the health economics results.
Patient and public involvement
We will conduct focus group discussions and interviews with key stakeholders (children, parents, teachers, school principals, local health and education officials) by refining the intervention approach. We will not involve any of the stakeholders in other aspects of the research study, including idea development, design of the study, implementation of the protocol, data collection and analysis and interpretation of the results. The results of the study will be disseminated through publication in peer-reviewed journals, presentations at conferences and in lay summaries provided to school staff, students and parents. The benefits and burden of the intervention will be assessed by children and their primary caregivers through self-reported questionnaires at the end of the intervention.
Trial status
The trial started and the recruitment of schools and children was completed in September 2018. Baseline measurements were conducted in the last few weeks in September 2018. The intervention lasting one school year started at the end of September 2018 and was completed in June 2019. The 4-month follow-up measurements started and were completed in January 2019. The 9-month follow-up measurements started and were completed in June 2019. The 21-month follow-up measurements will be completed in June 2020.
Ethics and dissemination
Any amendments to the study protocol will be submitted for IRB approval prior to implementation. Written informed consent will be obtained from all students and their parents. All data collected will be entered into an electronic database with de-identified information. The database will be accessed only by designated staff with a password. The results will be disseminated through publication in peer-reviewed journals, presentation at conferences and in lay summaries provided to school staff and participants. On completion of the trial and after the publication of these results, the data will be made available on request by contacting the corresponding author of this protocol.
Discussion
Non-communicable diseases, especially cardiovascular diseases, have contributed to the public health burden worldwide. Preventing childhood obesity in early life may have the greatest long-term effects in curbing this widespread burden. Although several childhood obesity intervention studies have been conducted in China, research gaps exist in terms of methodological flaws, process measures, and sustainability of the intervention. The DECIDE-Children study is based on theory-driven and systematic developments (eg, systematic review,8 qualitative interviews, panel discussions and a pilot study15) and serves as one of the first examples of a rigorously developed and evaluated childhood obesity prevention programme that will be implemented in eastern, central and western regions of China.
Our DECIDE-Children study can overcome poor adherence to the intervention components, which is a weakness of most previous studies, due to our favourable collaborations with local education authorities as well as the rigorous quality control of implementing the intervention. This study also has several other distinguishing features: (1) randomisation by an independent person not involved in the study, blinding of key outcome measures and a detailed process evaluation plan will help to provide study results of high quality; (2) a follow-up investigation will be conducted 1 year after the intervention is completed to determine the sustainability of the effects of the intervention; (3) a smartphone app will be employed to assist in providing information on, monitoring and providing feedback on the behaviours and body weight of the children; (4) three centres located in eastern, central and western regions of China will be involved in the study to reflect the different levels of economic development in China; and (5) most of the intervention components (school polices, regular monitoring of students’ weight and height, reinforcement of students’ physical activity at school, health education activities for students) will be integrated into the regular academic schedule of each intervention school.
Supplementary Material
Acknowledgments
We thank Jun-Shi Chen, Li-Ming Wen, Jun Ma, Guan-Sheng Ma, Ke-Ji Li, Yan-Fang Wang, Zheng-Zhen Wang, Hong-Juan Li, Qian Zhang and Yao Zhao for their support and advice in the study design and intervention development. We also thank the children and their parents, school principals and teachers for their participation in the research. We thank China Mobile Research Institute for their help in development of the smartphone application.
Footnotes
Collaborators: Study team of the DECIDE-Children study:
Beijing: Department of Maternal and Child Health, School of Public Health, Peking University (Hai-Jun Wang, Zheng Liu, Li-Zi Lin, Qiang Feng, Chen-Xiong Li, Shuang Zhou, Wen-Hao Li, Chu-Yao Jin, Qin Li, Yu Cheng, Di Wang, Lan Cheng, Yi Song, Hong Zhou, Xiang-Rong Xu, Jie-Yun Song); Dongcheng Primary and Secondary School Health Care Center, Beijing (Ai-Yu Gao, Hai-Hua Chen, Li-Jia Shang), Mentougou Primary and Secondary School Health Care Center, Beijing (Fang Zhang, Run-Ze Chen).
Changzhi: Changzhi Medical College (Xiang-Xian Feng, Jian-hui Yuan, Li-fen Duan).
Urumqi: Urumqi Primary and Secondary School Health Care Center, Xinjiang (Yi Lin, Chun-Xia Xu, Guo-Qin Yang, Zheng Zhang).
Contributors: HW and YW conceived the project. HW, ZL, YW, W-YN and H-JL were involved in design of the study and development of intervention materials. ZL wrote the first draft of the manuscript. XF, YL, AG and FZ contributed to implementation of the program. HF contributed to economic evaluation. PG contributed to statistical analysis plan. All authors approved the final manuscript.
Funding: This work was supported by National Key R&D Program of China (2016YFC1300200-4), the China Postdoctoral Science Foundation (2019M650391) and the National Natural Science Foundation of China (81903343).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
the study team for the DECIDE-children study:
Hai-Jun Wang, Zheng Liu, Li-Zi Lin, Qiang Feng, Chen-Xiong Li, Shuang Zhou, Wen-Hao Li, Chu-Yao Jin, Qin Li, Yu Cheng, Lan Cheng Di Wang, Yi Song, Hong Zhou, Xiang-Rong Xu, Jie-Yun Song, Ai-Yu Gao, Hai-Hua Chen, Li-Jia Shang, Fang Zhang, Run-Ze Chen, Xiang-Xian Feng, Jian-hui Yuan, Li-fen Duan, Yi Lin, Chun-Xia Xu, Guo-Qin Yang, and Zheng Zhang
Collaborators: the study team for the DECIDE-children study
References
- 1. Ng M, Fleming T, Robinson M, et al. . Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. The Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang S, Dong YH, Wang ZH, et al. . [Trends in overweight and obesity among Chinese children of 7-18 years old during 1985-2014]. Zhonghua Yu Fang Yi Xue Za Zhi 2017;51:300–5. 10.3760/cma.j.issn.0253-9624.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 3. Booth JN, Tomporowski PD, Boyle JME, et al. . Obesity impairs academic attainment in adolescence: findings from ALSPAC, a UK cohort. Int J Obes 2014;38:1335–42. 10.1038/ijo.2014.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther 2013;35:A18–32. 10.1016/j.clinthera.2012.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Twig G, Yaniv G, Levine H, et al. . Body-Mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016;374:2430–40. 10.1056/NEJMoa1503840 [DOI] [PubMed] [Google Scholar]
- 6. Gunnell DJ, Frankel SJ, Nanchahal K, et al. . Childhood obesity and adult cardiovascular mortality: a 57-year follow-up study based on the Boyd Orr cohort. Am J Clin Nutr 1998;136:664–72. [DOI] [PubMed] [Google Scholar]
- 7. Bleich SN, Vercammen KA, Zatz LY, et al. . Interventions to prevent global childhood overweight and obesity: a systematic review. Lancet Diabetes Endocrinol 2018;6:332–46. 10.1016/S2213-8587(17)30358-3 [DOI] [PubMed] [Google Scholar]
- 8. Feng L, Wei D-M, Lin S-T, et al. . Systematic review and meta-analysis of school-based obesity interventions in mainland China. PLoS One 2017;12:e0184704 10.1371/journal.pone.0184704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li B, Liu WJ, Adab P, et al. . Cluster-Randomised controlled trial to assess the effectiveness and cost-effectiveness of an obesity prevention programme for Chinese primary school-aged children: the CHIRPY dragon study protocol. BMJ Open 2017;7:e018415 10.1136/bmjopen-2017-018415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang Z, Xu F, Ye Q, et al. . Childhood obesity prevention through a community-based cluster randomized controlled physical activity intervention among schools in China: the health legacy project of the 2nd world summer youth Olympic Games (YOG-Obesity study). Int J Obes 2018;42:625–33. 10.1038/ijo.2017.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu Z, Li Q, Maddison R, et al. . A school-based comprehensive intervention for childhood obesity in China: a cluster randomized controlled trial. Child Obes 2019;15:105–15. 10.1089/chi.2018.0251 [DOI] [PubMed] [Google Scholar]
- 12. JaKa MM, Haapala JL, Trapl ES, et al. . Reporting of treatment fidelity in behavioural paediatric obesity intervention trials: a systematic review. Obes Rev 2016;17:1287–300. 10.1111/obr.12464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dong Y, Jan C, Ma Y, et al. . Economic development and the nutritional status of Chinese school-aged children and adolescents from 1995 to 2014: an analysis of five successive national surveys. Lancet Diabetes Endocrinol 2019;7:288–99. 10.1016/S2213-8587(19)30075-0 [DOI] [PubMed] [Google Scholar]
- 14. Yao H, Zhu G, Zhang X, et al. . Current situation and analysis of school physicians in primary and secondary schools in 16 provinces in China.. Chin J Sch Health 2018;39:1455–-8.. [Google Scholar]
- 15. Lin L, Li C, Gao A, et al. . Effect of a comprehensive school-based intervention on childhood obesity. Chin J Sch Health 2018;39:1505–8. [Google Scholar]
- 16. Chan A-W, Tetzlaff JM, Altman DG, et al. . Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. . Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sallis J, Owen N, Fisher E. Ecological models of health behavior : Glanz K, Rimer B, Viswanath K, Health behavior and health education. San Francisco, CA: Jossey-Bass, A Wiley Imprint, 2008: 465–85. [Google Scholar]
- 19. Martin J, Chater A, Lorencatto F. Effective behaviour change techniques in the prevention and management of childhood obesity. Int J Obes 2013;37:1287–94. 10.1038/ijo.2013.107 [DOI] [PubMed] [Google Scholar]
- 20. Hunsberger M, O'Malley J, Block T, et al. . Relative validation of block kids food screener for dietary assessment in children and adolescents. Matern Child Nutr 2015;11:260–70. 10.1111/j.1740-8709.2012.00446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu A-L, Ma G-S, Zhang Q, et al. . [Reliability and validity of a 7-day physical activity questionnaire for elementary students]. Zhonghua Liu Xing Bing Xue Za Zhi 2003;24:901–4. [PubMed] [Google Scholar]
- 22. Wardle J, Guthrie CA, Sanderson S, et al. . Development of the children's eating behaviour questionnaire. J Child Psychol & Psychiat 2001;42:963–70. 10.1111/1469-7610.00792 [DOI] [PubMed] [Google Scholar]
- 23. de Onis M, Onyango A, Borghi E. Development of a who growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7. 10.2471/BLT.07.043497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. National Health Commission of the People's Republic of China Screening for overweight and obesity among school-age children and adolescents (WS/T 586-2018). Beijing, China; 2018. [Google Scholar]
- 25. Saunders RP, Evans MH, Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot Pract 2005;6:134–47. 10.1177/1524839904273387 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


