Abstract
Background: Right ventricular (RV) adaptation to acute and chronic pulmonary hypertensive syndromes is a significant determinant of short- and long-term outcomes. Although remarkable progress has been made in the understanding of RV function and failure since the meeting of the NIH Working Group on Cellular and Molecular Mechanisms of Right Heart Failure in 2005, significant gaps remain at many levels in the understanding of cellular and molecular mechanisms of RV responses to pressure and volume overload, in the validation of diagnostic modalities, and in the development of evidence-based therapies.
Methods: A multidisciplinary working group of 20 international experts from the American Thoracic Society Assemblies on Pulmonary Circulation and Critical Care, as well as external content experts, reviewed the literature, identified important knowledge gaps, and provided recommendations.
Results: This document reviews the knowledge in the field of RV failure, identifies and prioritizes the most pertinent research gaps, and provides a prioritized pathway for addressing these preclinical and clinical questions. The group identified knowledge gaps and research opportunities in three major topic areas: 1) optimizing the methodology to assess RV function in acute and chronic conditions in preclinical models, human studies, and clinical trials; 2) analyzing advanced RV hemodynamic parameters at rest and in response to exercise; and 3) deciphering the underlying molecular and pathogenic mechanisms of RV function and failure in diverse pulmonary hypertension syndromes.
Conclusions: This statement provides a roadmap to further advance the state of knowledge, with the ultimate goal of developing RV-targeted therapies for patients with RV failure of any etiology.
Keywords: right ventricle, pulmonary hypertension, pulmonary embolism, acute respiratory distress syndrome, pulmonary circulation
Contents
Overview
Introduction
Topic Domain 1
Topic Domain 2
Topic Domain 3
Methods
Definition, Development, and Staging of RVF
Topic Domain 1: Optimizing the Methodology to Assess RV Function in Acute and Chronic Conditions in Preclinical Models, Human Studies, and Clinical Trials
Normative Indices of RV Morphology and Function
Optimization of RV Assessment in Clinical Research
Optimization of Animal Models of RVF
Animal Models for RVF in Group 2 and 3 PH
RV Responses to Pulmonary Embolism and Acute Respiratory Distress Syndrome
Differences between Acute and Chronic RV Responses
Regional Differences in RV Responses
Topic Domain 2: Analyzing Advanced RV Hemodynamic Parameters at Rest and in Response to Exercise
Rationale
Invasive and Noninvasive Phenotyping of RV Function
Prognostic Relevance of Measurements of RV Function
Assessment of RV Afterload
Assessment of RV–Pulmonary Arterial Coupling
Assessment of RV Diastolic Function
Assessment of RV–LV Interactions and Ventricular Interdependence
Emerging and Alternative Approaches
Topic Domain 3: Deciphering the Underlying Molecular and Pathogenic Mechanisms of RV Function and Failure
Assessment of Hypertrophy and Angiogenesis
Assessment of Fibrosis
Assessment of Cardiomyocyte Metabolism
Assessment of Cell Death
Assessment of Inflammation
Assessment of Oxidative Stress
Assessment of Contractile Signaling and Calcium Handling
Conclusions
Overview
Right ventricular (RV) function is the single most important prognostic determinant of survival in various forms of pulmonary hypertension (PH). Significant progress has been made since improving the understanding of RV function and failure was identified in 2005 as a major area of need in the field; however, many knowledge gaps remain. A better understanding of the mechanisms of RV adaptation and maladaptation to pulmonary hypertensive syndromes will advance the field toward the goals of defining physiological and pathophysiological RV responses, identifying biomarkers of RV function, and developing RV-directed therapies. This document lays the framework for addressing knowledge gaps in clinical and basic RV research and for identifying research opportunities and pathways forward.
-
•
The task force defined RV failure (RVF) as a complex clinical syndrome characterized by insufficient delivery of blood from the RV in the setting of elevated systemic venous pressure at rest or exercise.
-
•
RVF is a heterogeneous syndrome. Multiple RVF phenotypes exist.
-
•
The task force identified multiple knowledge gaps and research opportunities in the field. The four major research priorities that should be addressed in the next 5 years are:
-
1.
Enhancing mechanistic understandings of adaptive versus maladaptive RV responses to pulmonary vascular load. This includes, but is not limited to, understanding the roles of fibrosis, angiogenesis, inflammation and metabolic shifts. Genetic and epigenetic contributions to successful adaptation need to be identified.
-
2.
Deriving and validating a series of plasma and/or imaging biomarkers (by echocardiography and cardiac magnetic resonance imaging) for accurate evaluation of RV function, perfusion, and RV–pulmonary vascular coupling and to serve as endpoints in clinical trials.
-
3.
Developing and validating novel animal models and improving existing models of RVF in the setting of increased pulmonary vascular load to provide a platform for better understanding mechanisms of RVF and for testing novel RV-directed therapies.
-
4.
Developing novel therapies aimed at targeting RV myocardial contractility (e.g., calcium sensitizing agents) as a critical area of need that would be expected to improve patient outcomes.
-
1.
-
•
Increased availability to and methods to study human RV tissue will be critical in addressing these research priorities and in advancing the field.
Introduction
RV failure (sometimes also referred to as “right heart failure”) is increasingly recognized in acute and chronic pulmonary hypertensive syndromes, and RV adaptation to these disease states is a significant determinant of short- and long-term outcomes (1–5). An estimated 70 million individuals in the United States may have abnormal RV function (3, 4, 6–10).
Thirteen years have passed since the initial meeting of the NIH Working Group on Cellular and Molecular Mechanisms of Right Heart Failure (1). Although remarkable progress has been made in the intervening period, significant gaps remain at many levels in the understanding of cellular and molecular mechanisms of RV responses to pressure and volume overload, in the validation of diagnostic modalities, and in the development of evidence-based therapies (1, 2, 11, 12). RV function is the single most important prognostic determinant of survival in pulmonary arterial hypertension (PAH) (3) as well as in multiple highly prevalent chronic heart and lung diseases (4, 6, 7, 10); however, no consensus exists regarding the definition of RV failure (RVF). This deficiency reflects in part the current paucity of clinically available, specific biomarkers reflecting RV function. In addition, targeted therapy for RVF remains elusive. Most importantly, factors determining transition from adaptive (or compensated) to maladaptive (or decompensated) RV remodeling and predictors of RVF remain unknown.
The purpose of this document is to:
-
1.
Comprehensively elucidate the current understanding of RV function and its assessment in healthy individuals and those with preclinical, acute, and chronic diseases;
-
2.
Identify major knowledge gaps; and
-
3.
Outline specific strategies for addressing these gaps.
We sought to address these objectives across three topic domains:
Topic Domain 1
Optimizing the methodology to assess RV function in acute and chronic conditions in pre-clinical models, human studies, and clinical trials. This provides the basic framework for optimally assessing RV morphology, function, and failure in animal models of disease and in humans.
Topic Domain 2
Analyzing advanced RV hemodynamic parameters at rest and in response to exercise. Recommendations are provided for improving the understanding of RV contractile and diastolic function as well as RV–pulmonary vascular coupling in response to load and exercise in both preclinical and clinical models. This will further our understanding of RV dynamic function adaptation and functional reserve and will establish optimal measures to be used in clinical assessment of the RV.
Topic Domain 3
Deciphering the underlying molecular and pathogenic mechanisms of RV function and failure in diverse PH syndromes. Identifying pathophysiologically relevant adaptive and maladaptive processes (e.g., angiogenesis, inflammation, fibrosis) in preclinical models will set the stage for targeted therapy to be tested in clinical trials.
Findings and recommendations generated from these topic domains address the overarching questions and cross-cutting themes listed in Table 1.
Table 1.
Overarching Questions and Cross-Cutting Themes Addressed in This Document
| 1. What are the hallmarks of acute and chronic RVF? |
| 2. What are the mechanisms underlying transition from adaptive to maladaptive RV function? |
| 3. What are clinically relevant endpoints in RV research, and are they accurately assessed and validated? |
| 4. What are currently available tools in RV research, and what are their limitations? |
| 5. What are the current knowledge gaps in research assessing acute and chronic RV failure, and what are the suggested remedies? |
Definition of abbreviations: RV = right ventricular; RVF = right ventricular failure.
The intended audience of this report includes basic, translational, and clinical researchers in the fields of pulmonary circulation, cardiovascular medicine, respiratory and critical care medicine, research funding organizations, health policy experts, and pharmaceutical and device industries.
Methods
A working group of international experts from the American Thoracic Society (ATS) Assemblies on Pulmonary Circulation and Critical Care (18 ATS members and two external content experts) was convened, which included basic, translational, and clinical researchers with expertise in a broad range of areas within adult pulmonary and critical care medicine, cardiovascular medicine, cardiothoracic surgery, physiology, and pathology. The scope of the project was reviewed and approved by the ATS. Potential conflicts of interest were disclosed and managed in accordance with the policies and procedures of the ATS. No unresolvable conflict of interest was identified.
This task force met twice in person (ATS 2015 for a full-day workshop and ATS 2016 for a 2-hour summation) and multiple times in between by teleconference. Major focus areas were developed by semistructured systematic review of the literature, expert opinion, and consultation. During the initial workshop, goals and ground rules guiding the work group were established. Subjects to be discussed were suggested by the steering committee and agreed on by the group. Presentations by content experts were made in each of the three topic domains, followed by group discussion aimed at defining key areas of consensus and disagreement. Current knowledge state summaries were then developed and rigorously analyzed by the entire workgroup and in focus area subgroups. Structured knowledge gap analyses were conducted in all three topic domains.
The draft was circulated to the task force members with revisions at each step. Consensus was achieved through moderated discussion. Data cloud document management was used to coordinate version control and integrate components from the subgroups. The final report was peer reviewed, approved by the leadership of each of the sponsoring Assemblies, and ultimately approved by the ATS Board of Directors.
Definition, Development, and Staging of RVF
The task force defined RVF as a complex clinical syndrome characterized by insufficient delivery of blood from the RV and elevated systemic venous pressure at rest or exercise.
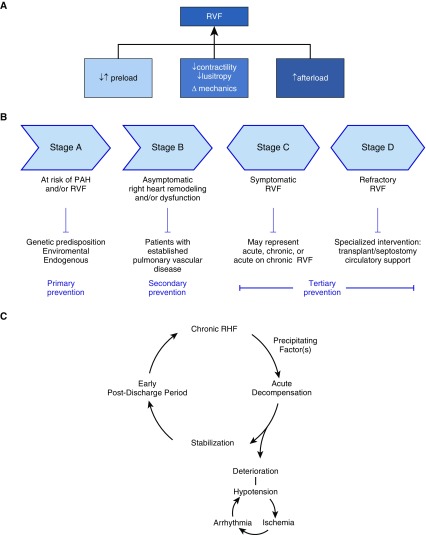
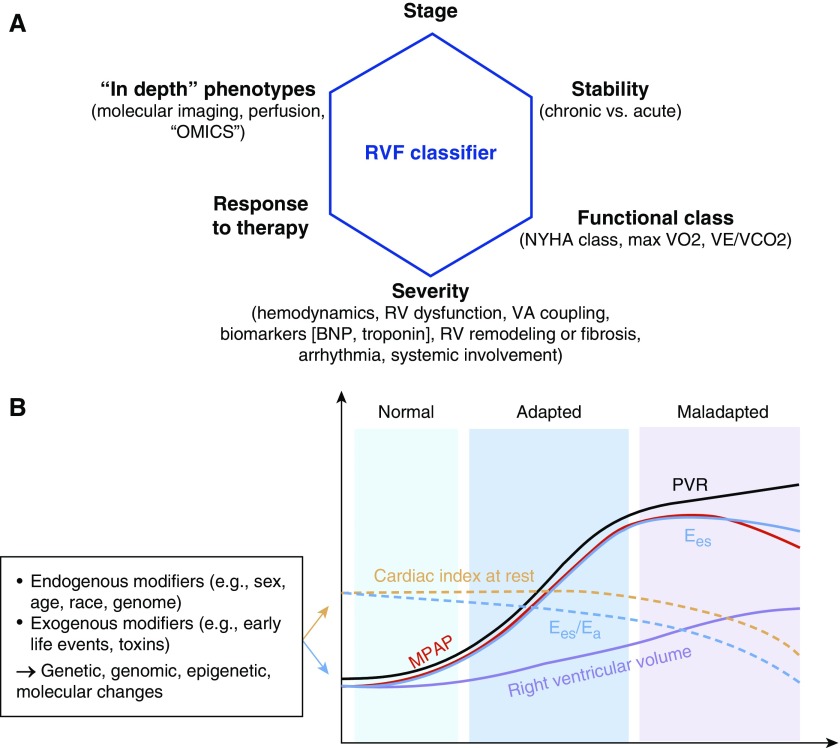
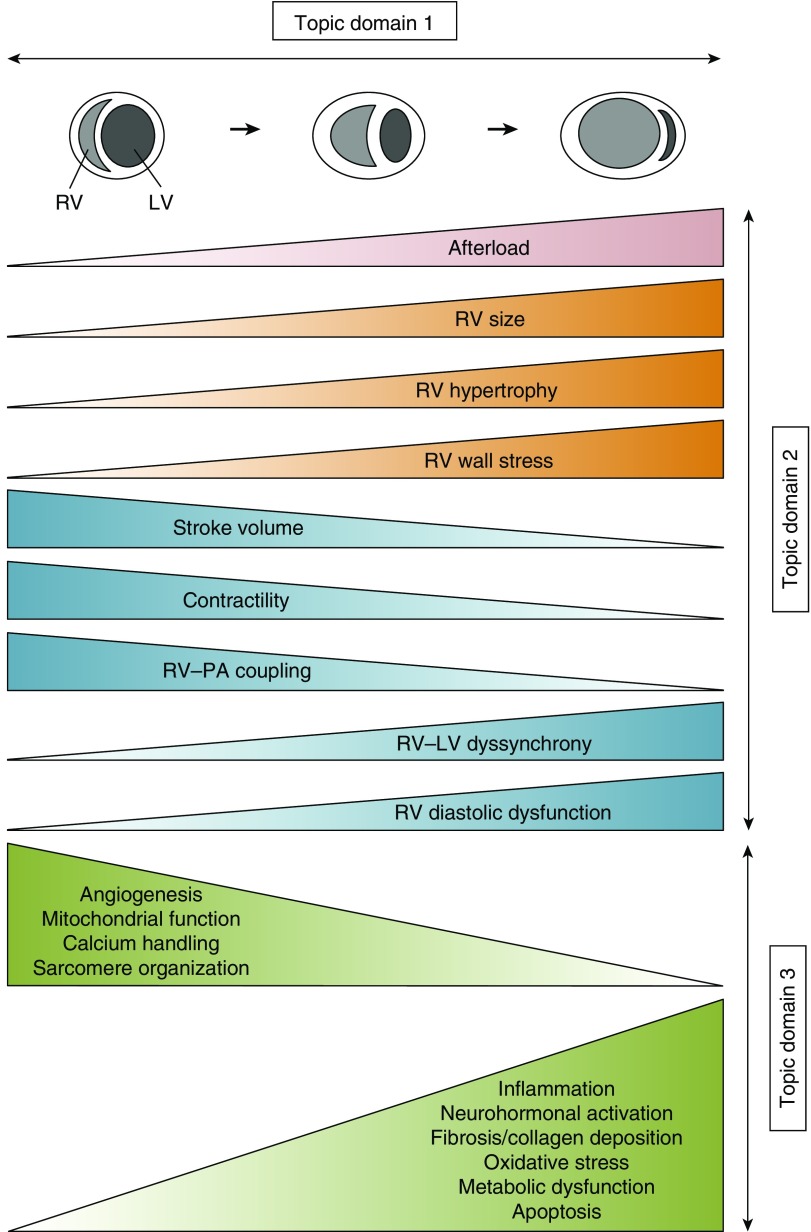
RVF occurs as a consequence of 1) alterations in preload; 2) changes in RV mechanics, lusitropy, and/or contractility; or 3) increases in afterload (Figure 1A). Similar to left ventricular (LV) failure, chronic RVF occurs in four distinct stages (Figure 1B). Some investigators use the term “RV dysfunction” to indicate structural RV changes in the absence of functional alterations. In this statement, we avoid this term, because such a constellation would qualify as “RV failure” according to the definition provided above. Although frequently progressive in character, with appropriate intervention(s), progression may stop at any of these stages or even be reversible. On the other hand, acute decompensation may develop at any of the four RVF stages. Once acute RVF develops, patients may deteriorate or stabilize (Figure 1C). Several clinically relevant modifiers of RV function exist (Figure 2A). PH is a syndrome commonly associated with RVF and is a prime example of how the RV responds to chronically elevated afterload (Figure 2B). With increases in pulmonary artery pressure (PAP), the RV exhibits compensatory mechanisms that include homeometric and heterometric adaptation as well as neurohormonal activation (2, 13). Adaptive RV hypertrophy (RVH) develops. It is believed, although not fully proven, that once the RV’s compensatory mechanisms are exhausted (purportedly as a result of transition from adaptive to maladaptive RVH), RVF develops. Genetic predispositions and early life events are putative modifiers of the RV compensatory response (Figure 2B). Figure 3 highlights key aspects of RVF pathophysiology addressed in this research statement.
Figure 1.
Etiologies and stages of right ventricular failure (RVF). (A) RVF occurs as a consequence of alterations in preload, changes in mechanics and/or decreases in contractility, or increases in afterload. (B) Classification of RVF according to stages of development in keeping with the recent classification of the American College of Cardiology Foundation/American Heart Association Task Force for Heart Failure (298, 299). Note that stages are not static and that stages C and D are potentially reversible with normalization or significant decrease in pulmonary vascular resistance (e.g., after pulmonary endarterectomy or lung transplantation) (300, 301). Symptomatic RVF (stage C) is usually managed pharmacologically, whereas refractory RVF (stage D) often requires specialized interventional or surgical measures. Preventive measures may be applied at any of the different stages of RVF. Decompensation may occur at any stage. (C) Cycle of acute on chronic decompensation of RVF. Acute decompensation is usually provoked by one or more precipitating factors (e.g., infection, pulmonary embolism, bleeding disorders) or by progression of the underlying disease (112). Patients frequently deteriorate and enter a vicious cycle of hypotension, ischemia, and decreased pump function or may stabilize and revert to more or less stable chronic RVF. However, mortality after hospital discharge remains high (35% at 12 mo [112]). PAH = pulmonary arterial hypertension; RHF = right heart failure.
Figure 2.
Classifiers and time course of right ventricular failure (RVF). (A) RV function is described using several characteristics, such as stage and acuity, as well as functional class (either by New York Heart Association [NYHA] classification or by cardiopulmonary exercise testing) and severity (using hemodynamic characteristics, markers of RV function, ventriculoatrial [VA] coupling, imaging or plasma biomarkers indicating RV remodeling, as well as presence or absence of arrhythmias [e.g., atrial fibrillation] and presence or absence of systemic involvement [e.g., liver congestion, renal impairment]) (2, 128, 162). Response to therapy (e.g., treatment-responsive vs. refractory RVF) is frequently used for classifying RV function as well. Novel classifiers and “deep” phenotyping tools include imaging approaches aimed at assessing perfusion, metabolism, and/or fibrosis, complemented by “omics” and “big data” approaches. (B) Time course of RVF development in the setting of chronic pressure overload from pulmonary vascular disease. See Reference 128 for detailed review of the supporting literature. Note that significant molecular and temporal heterogeneity exist in RV adaptation and maladaptation to pressure overload, possibly determined by genetic, genomic, epigenetic, and molecular changes due to endogenous and exogenous factors. For example, in scleroderma-associated pulmonary arterial hypertension (PAH), end-systolic elastance (Ees) is lower than in idiopathic PAH, and Ees/arterial elastance (Ea) decreases earlier than in other disease states (170). Cardiac output/cardiac index decreases as a result of transition from adaptive to maladaptive remodeling, because of either progression of the underlying disease or an additional insult. BNP = brain natriuretic peptide; MPAP = mean pulmonary arterial pressure; PVR = pulmonary vascular resistance. (B) Modified from Reference 302.
Figure 3.
Concept figure of changes in right ventricular (RV) structural, functional, and biochemical/molecular processes as the RV transitions from normal function to failure in the setting of increased afterload. Afterload increases can be acute (e.g., in cases of pulmonary embolism or acute respiratory distress syndrome) or chronic (e.g., in pulmonary arterial hypertension, pulmonary hypertension from chronic heart or lung disease, or chronic thromboembolic pulmonary hypertension). With progressive increases in RV afterload (top), RV size increases. In forms of chronic afterload increases, RV hypertrophy develops. RV stroke volume, RV contractility, and RV–pulmonary artery (PA) coupling are initially maintained (or even increased) but then progressively decrease. In parallel, RV diastolic dysfunction and RV–left ventricular (LV) dyssynchrony develop. At a molecular/biochemical level, these processes are accompanied by alterations in angiogenesis, calcium handling, mitochondrial function, and sarcomere organization, as well as progressive increases in inflammation, neurohormonal activation, fibrosis/collagen deposition, oxidative stress, metabolic dysfunction, and cardiomyocyte apoptosis. Note that for didactic purposes, long-term trajectories for all changes are shown as gradual increases or decreases, whereas in reality these changes may exhibit fluctuations and not develop in a parallel manner. Topic domain 1 of this research statement focuses on optimizing the methodology to assess RV function in acute and chronic conditions in preclinical models, human studies, and clinical trials. Structural and functional RV changes (shown in red, orange, and blue) are covered in topic domain 2; biochemical/molecular processes (in green) are discussed in topic domain 3.
Topic Domain 1: Optimizing the Methodology to Assess RV Function in Acute and Chronic Conditions in Preclinical Models, Human Studies, and Clinical Trials
Normative Indices of RV Morphology and Function
Rationale
Despite the high prevalence of RVF in the United States and throughout the world (3, 4, 6–10), there are no well-established biologic or clinical determinants of RV structure and function. Thus, there remains significant scientific and clinical justification for studying the structure and function of the RV in greater detail during health. Establishing normative values will enhance our understanding of subclinical changes in disease and may allow for early/preventative treatment. Unlike the LV, the thin-walled, compliant RV has difficulty accommodating increases in afterload, and even small increments or fluctuations in afterload may lead to adverse RV sequelae (13, 14), particularly if the increase in PAP is rapid. There is, however, great variability in the clinical trajectory of patients, who often present at later stages of disease, when RVF is overt (Figure 1B). Furthermore, observations from population-based cohorts may provide insight into important mechanistic pathways generalizable to RVF, regardless of etiology. Finally, targeting patients before the development of significant RVF may be more successful than instituting therapy after advanced disease is established.
Current state of knowledge
An ideal RV metric would be sensitive enough to capture subtle cardiac structural changes, reliable, reproducible, inexpensive, and easily obtained. It would be validated across settings and in different populations. Echocardiography can qualitatively assess RV function and can be used to measure ventricular volumes and wall motion. However, quantification requires geometric assumptions, and these are hindered by the crescentic, thin-walled shape of the normal RV and also by subject characteristics (e.g., body habitus), which could introduce bias. In contrast, cardiac magnetic resonance imaging (CMR) is a fundamentally safe and reliable modality from which quantitative data regarding RV size, function, and remodeling are acquired rapidly with limited artifact. However, it is relatively expensive in some settings and not universally available.
Measurement of RV ejection fraction (RVEF) and RV mass and volumes by CMR is highly accurate and reliable in normal subjects and in those with RV or LV failure (15–18). Thus, CMR is the standard of measuring imaging technique for RV assessment (although echocardiography is more practical in the unstable patient because it can be performed at the bedside). RVEF has been identified as a key determinant of outcome in RVF regardless of etiology, including PH due to LV failure (group 2 PH) or advanced lung disease (group 3 PH), and PAH (4, 6, 7) (group 1 PH). RVEF predicts outcome in PAH, and changes in RVEF mediate improvements in survival with disease-specific therapy, making it currently the most reliable surrogate RV endpoint (3, 19–22). Several other imaging techniques have been shown to measure RV function and predict outcome (e.g., tricuspid annular plane systolic excursion [TAPSE], speckle-tracking for strain imaging, three-dimensional [3D] echocardiography, fluorodeoxyglucose–positron emission tomography [PET]) but are less well validated, especially in health or early disease (23–27).
Current knowledge gaps
Normative values for RV size and function have been derived from the MESA-RV (Multi-Ethnic Study of Atherosclerosis–Right Ventricle) Study, the Framingham Heart Study, and other cohorts (28–35). However, these observations need to be validated 1) in health and disease, 2) longitudinally, and 3) in other populations. Racial, ethnic and socioeconomic differences need further exploration (28, 36, 37). Normal values for RV function are needed for physiological modifiers of the normal RV in pregnant subjects and athletes, and the effects of processes such as puberty, menopause, and aging merit study. The temporal evolution with early life events (e.g., prematurity) also requires further study (38–40). The definition and relevance of subclinical RV changes, and their role in the natural history of RVF, are also incompletely elucidated.
Recommendations/pathway for progress
Several knowledge gaps exist, which include a better understanding of the normative indices of RV morphology and function, the impact of key demographic characteristics (age, sex, race/ethnicity, and socioeconomic status) on the healthy RV, RV development throughout the life span, subclinical RV abnormalities, cardiopulmonary interactions under stress, and, finally, the impact of biventricular interactions. Such studies should include neonates and prematurely born babies, especially because the latter are at risk for developing RV abnormalities later in life (38).
Optimization of RV Assessment in Clinical Research
Rationale
Trials to detect differences in clinical worsening or survival generally require a substantial sample size, which can be difficult to complete in rare diseases such as PAH, especially when the intervention being studied is added to background therapy. A well-chosen RV surrogate endpoint in clinical trials may facilitate trial design, and ultimately drug approval, because RVF is the leading cause of death in PAH (3). An endpoint must be both accurate and precise, as measurement error can lead to bias and, therefore, erroneous conclusions.
Current state of knowledge
A given endpoint needs to satisfy a number of criteria to serve as a surrogate for “hard” clinical outcomes before incorporation into clinical trials (41–43). It should be reliable, integral to the disease causal pathway, and targeted by the intervention of interest, and be linked with a clinically important outcome, such as survival. Finally, a significant proportion of the treatment effect (50–75%) on clinical outcome should be explained by the effect of the intervention on the surrogate endpoint. The requirements for a disease surrogate are much more stringent than for a correlate, and in fact several long-held endpoints in PAH, such as 6-minute-walk distance (6MWD) and hemodynamics, are inadequate surrogates for short-term events (44–48).
Current knowledge gaps
A number of RV endpoints have been proposed, including biomarkers (e.g., BNP [brain natriuretic peptide] and troponin) as well as metrics obtained from traditional and novel imaging techniques (23–27, 49–52). Although there is currently no consensus on how to best measure RV function in clinical trials, there is some evidence that current PAH treatments may have unique effects on the RV (criterion #2 for a surrogate; as demonstrated in a limited way with sildenafil and simvastatin and RV mass, and with bosentan and RV stroke volume [53–55]). Up-front combination therapy with ambrisentan and tadalafil reduced RV mass and NT-pro-BNP levels and increased RV contractility as measured by TAPSE or speckle-tracking echocardiography in an open-label trial in scleroderma-associated PAH (56, 57). Small observational studies demonstrated that worsening RV performance is associated with poor outcomes independent of pulmonary vascular resistance (3, 53, 58). These observations, along with those that demonstrated classic endpoints (e.g., 6MWD and hemodynamics) to be inadequate, suggest we may not fully understand how currently approved PAH treatments work (e.g., by targeting the pulmonary circulation or the RV or through other systemic effects) (59). The study of patients with PH with a severe RVF phenotype independent of the etiology (i.e., WHO groups 1–5) may allow for larger and faster trials; however, such an approach has not yet been tested. CMR is accurate, reproducible, and allows for detecting small changes in RVEF (∼3%) in sample sizes that are modest. It is considered the standard of measure for RV morphology and function and has been shown to be more cost saving in PAH drug trials than echocardiography, as a result of its lower measurement variability (60). Although some investigators advocate that CMR should be routinely incorporated into clinical trials, wide-scale incorporation into trials and ultimately clinical practice may be limited in some centers by cost and technical expertise.
Recommendations/pathway for progress
Measurements of RV function should be routinely incorporated into observational studies and clinical trials in pulmonary vascular disease, even if not as the primary endpoint. Longer, time-to-event clinical trials are now being conducted in PAH using composite morbidity and mortality endpoints (61, 62), which is the ideal setting in which to validate potential RV-based surrogate endpoints. The validation of an RV surrogate in this setting would contribute greatly to the feasibility of smaller phase II trials to identify potentially promising therapies from ineffective ones. CMR has greater sensitivity and reproducibility than ultrasound and thus can rapidly detect an efficacy signal with a small sample size in a short period of time, potentially minimizing cost and avoiding trial futility (60). However, its routine use in clinical trials needs further validation.
Optimization of Animal Models of RVF
Rationale
Animal models of disease are critical to understanding the physiology and structural and molecular underpinnings of the human conditions they attempt to recapitulate. They facilitate therapy discovery and safety evaluation. For RVF, an animal model that recapitulates the mechanisms and prognostic implications of RVF in humans would minimize requirements for human tissues, and new understanding of molecular processes driving failure would accelerate the discovery and preclinical testing of potential drugs for RVF.
Current state of knowledge
An ideal RVF animal model would be reproducible by individual investigators over time, as well as reproducible across institutions. Such a model would also be inexpensive, feature relatively brisk disease development for rapid knowledge acquisition, and, most importantly, accurately represent physiologic and molecular characteristics of the human RVF phenotypes. Given the varied clinical conditions resulting in primary or secondary RVF, a single animal model fulfilling all these criteria is unlikely (63). Presently, there are several commonly used animal models of RVF (Table 2), all with limitations and none considered the single “best” model. With the exception of exposure to hypoxia and pulmonary artery banding (PAB), which can be done in mice, rats have been used predominantly, as they most reliably reproduce the vascular lesions characteristic of human PAH (64). Pulmonary vascular lesions generated in different models vary (64).
Table 2.
Commonly Used Animal Models of Right Ventricular Failure
| Monocrotaline | Hypoxia | Sugen/Hypoxia | PA Banding | |
|---|---|---|---|---|
| Method | Subcutaneous injection of alkaloid monocrotaline (40–60 mg/kg; lower dose results in milder phenotype) | Exposure to FiO2 10% (or 0.5 atmospheric pressure) for 3–5 wk | Subcutaneous injection of VEGFR2 antagonist Su5416 + hypoxia (3 wk) + room air (≥4 wk) | Suture or clip around main PA |
| RVSP, mm Hg | 40–60 | 30–40 | 60–80 | 60–80 |
| Cardiac output | Depressed | Maintained or slightly depressed | Severely depressed | Maintained or depressed (depending on tightness of band and duration of banding) |
| RV histology | Fibrosis, cardiomyocyte hypertrophy, possibly biventricular myocarditis (conflicting data on the latter) | Fibrosis (less than other models), cardiomyocyte hypertrophy | Fibrosis, cardiomyocyte hypertrophy, apoptosis | Fibrosis, cardiomyocyte hypertrophy |
| RV vascular effects | Vascular inflammation, decreased capillary density | Capillary proliferation | No angiogenesis, decreased capillary volume and density | Capillary volume and density maintained or slightly decreased |
| Type of RV remodeling | Maladaptive | Adaptive | Maladaptive | Adaptive or maladaptive (depending on tightness of band and duration of banding) |
| Pulmonary vascular effects | Yes | Yes | Yes | No |
| Systemic effects | Yes | Yes | Yes | No |
| Sex of animal tied to experimental phenotype | Yes (less PH in females) | Yes (less PH in females) | Yes (better RV function in females) | Yes (better RV function in females) |
| What is being modeled? | Inflammatory PAH and RV dysfunction | Chronic hypoxia, high altitude, some aspects of chronic lung disease | Pulmonary vascular endothelial cell injury with uncontrolled proliferation of remaining cells | RV afterload increase without pulmonary vascular injury |
| Modifications of model | Combination with pneumonectomy or aortocaval shunting to result in pulmonary vascular overflow and more pronounced remodeling | Extension of room air exposure associated with progressive pulmonary vascular remodeling and afterload increase |
Definition of abbreviations: PA = pulmonary artery; PAH = pulmonary arterial hypertension; PH = pulmonary hypertension; RV = right ventricle; RVSP = right ventricular systolic pressure; VEGFR2 = vascular endothelial growth factor receptor 2.
Current knowledge gaps
Whether the development of RVF in these preclinical models is purely a function of hemodynamic overload or specific lung and systemic vascular lesions in various models is unknown. PAB can be applied to both rats and mice and does not elicit pulmonary vascular disease, but it has technical limitations and variable effects on the RV. The comparison of pure RV pressure overload models (such as PAB) versus pressure overload syndromes due to pulmonary vascular disease (as induced by monocrotaline or Sugen plus hypoxia) suggests that the former model manifests adaptive RVH and may be relevant to congenital heart diseases (such as pulmonic stenosis), whereas the latter may be more reflective of the maladaptive RVH seen in most patients with WHO group 1 PH (65). However, it is believed, although not fully proven, that decreased cardiac output (CO) and maladaptive RVH can develop in this model as well, depending on the degree and duration of the banding (66). A need exists for models of pure RV volume overload. The role of alternative models of RVF, including large animal models (67, 68) and transgenic mouse models (69), needs to be defined further.
Recommendations/pathway for progress
We recommend matching the animal model to the experimental question asked. For instance, when the experimental question involves the etiology of RV fibrosis, monocrotaline or Sugen plus hypoxia may be relevant. Alternatively, when studying molecular mechanisms behind the progression from compensated RVH to RVF, PAB with various degrees and/or durations of banding is preferable. Corroboration of results in more than one model strengthens experimental findings (70). The RV Langendorff model is a useful ex vivo model to assess RV inotropy and lusitropy (71–73) and a useful adjunct to in vivo assessments of the RV, which are largely load dependent. Large animal models of RV pressure and volume overload (with and without pulmonary vascular disease) will likely be very helpful in the latter stages of preclinical testing of drugs and devices, before use in humans. RV volume overload could be generated by inducing compromising tricuspid valve insufficiency. The design of novel, translationally relevant models is dependent on a better molecular understanding of the unique determinants of human RVF. A better molecular understanding of the basis for RVF may lead to improved transgenic animal models or preference for one of the existing models with greater understanding of its implications. In the absence of these data, we recommend:
-
1.
Correlation of findings from animal models with human tissue.
-
2.
Consideration of sex and age in animal models of RVF.
-
3.
Incorporation of right heart catheterization (RHC) (thermodilution and/or pressure–volume analyses using high-fidelity conductance catheters), echocardiography, and/or CMR to measure CO, a marker of RV function.
-
4.
Combine CO measurements with other functional measurements (e.g., TAPSE and RV dilatation with echocardiography), RV volumes (CMR), and/or ventriculoarterial coupling (using pressure–volume loops).
Although optimization of animal models of RVF is of utmost importance in the field, these efforts should be paralleled by the development of new in vitro technologies, such as a “heart on a chip” approach and/or cardiomyocytes or cardiac endothelial cells differentiated from human-PH induced pluripotent stem cells. Such models could be used to study RV cardiomyocyte–endothelial cell interactions, screen drugs, and identify novel signaling pathways.
Animal Models for RVF in Group 2 and 3 PH
Rationale
The majority of PH cases worldwide are due to diseases such as chronic LV and lung disease, sleep-disordered breathing, or high altitude exposure (group 2 and 3 PH) (74–76). Treating the underlying condition is typically the goal; however, a significant number of patients may develop RVF, and there has been considerable interest in better understanding the mechanisms of RVF in affected individuals. Therefore, there is a need for adequate animal models of RVF resulting from group 2 and 3 PH.
Current state of knowledge
RVF generally does not develop in rodent models of hypoxia exposure but is present in the hypoxic newborn calf (77). In patients with chronic lung disease, the development of PH and/or RVF is not strictly linked to chronic hypoxia but may also develop because of hypercapnia, neurohormonal alterations, comorbid cardiovascular disease, and pulmonary vascular obstruction and obliteration (78). Rodents with Sugen- or cigarette smoke–induced emphysema as well as bleomycin- or adenoviral TGF-β–induced pulmonary fibrosis may exhibit RVH but do not exhibit significant RVF (79–83).
In models of LV disease, RVF may develop as an integral part of a global cardiac dysfunction (e.g., doxorubicin-induced biventricular failure) (84). In addition, isolated damage to the LV can directly impair RV function (85), even in the absence of PH (86). Development of secondary PH in models of LV failure induced by transverse aortic constriction is little studied. Indeed, a significant degree of lung vascular remodeling, PH, and RVF can develop as soon as 4 weeks after transverse aortic constriction in mice (87), suggesting this may be a model of combined pre- and postcapillary PH. Combined pre- and postcapillary PH and RVF in the setting of mitral stenosis or heart failure with preserved ejection fraction may be more aptly represented by a model of pulmonary vein banding (reported in swine [88], although with technical limitations for mechanistic studies). A model of PH due to LV diastolic dysfunction using Su5416 administration in obese ZSF1 rats has recently been published; this model exhibits moderate PH, but no overt RVF (89). Similarly, AKR/J mice fed with a high-fat diet develop increased LV end-diastolic pressure and biventricular hypertrophy, but it is unknown if they develop RVF (90). As in patients, animal models may require substantial time to develop RVF; this feature may be overlooked because of cost and time constraints, as well as arbitrary requirements by animal care committees that animals be killed if they become ill. Clinically relevant surrogate endpoints of failure to thrive (e.g., weight loss or decreased oral intake) may occur before overt RVF develops in these models.
Current knowledge gaps
Mechanisms of RVF development in group 2 and 3 PH are multifactorial, but the relative contributions of the various causes have not yet been fully elucidated and are difficult to mimic in small or large animals. Whether treating RVF would translate to improved clinical outcomes is currently unknown, particularly as PAH medications have largely been found to be ineffective or harmful in patients with group 2 and 3 PH.
Recommendations/pathway for progress
A better understanding of RV function in patients with group 2 or 3 PH will be critical for understanding the human disease and for optimizing animal models. Therefore, clinical studies should carefully phenotype patients with RVF from these syndromes, and studies should explore whether treating RVF improves clinically relevant outcomes. “Multiple hits” rather than a “single hit” likely contribute to human disease, and such multifactorial etiologies should be considered in animal models (89). Ultimately, even though the “perfect” animal model may not ever exist, the development of animal models mimicking group 2 and 3 PH with significant RVF would be a major milestone. Isolated cardiomyocytes may allow for mechanistic investigations of specific pathways. Animal studies of group 2 or 3 PH should be of sufficient duration to detect RVF. Ideally, more sophisticated RV endpoints including BNP levels, CO (measured by RHC and Doppler), and formal assessment of RV size and function should be incorporated. Studies in humans should focus on deep phenotyping and ideally involve the study of RV tissues.
RV Responses to Pulmonary Embolism and Acute Respiratory Distress Syndrome
Rationale
Both pulmonary embolism (PE) and acute respiratory distress syndrome (ARDS) cause relatively acute PH and RV injury; the ensuing RVF results in significant morbidity and mortality in both conditions. Causes of RV injury in both scenarios include increased afterload from PH and impaired subendocardial RV perfusion (91–94).
Current state of knowledge
Rapid increases in PAP and PVR, as occur in PE and ARDS, are poorly tolerated, and the RV will fail and develop conduction abnormalities that would not occur if the pressure increased slowly, allowing time for the development of compensatory RVH. Both large PE and severe ARDS result in uncoupling of the RV from the pulmonary circulation (defined and discussed in Assessment of RV–PA Coupling), and subsequent inefficient forward flow. The primary insult with PE comes from macrovessel occlusion, whereas ARDS results from microvessel occlusion with widespread but heterogeneous alveolar consolidation and elements of acute hypoxic pulmonary vasoconstriction. Both conditions shift the pulmonary vasoconstrictor–dilator balance toward an increase in afterload and result in chemokine and cytokine release, recruitment of inflammatory cells, and production of reactive oxygen species (95–101). LV diastolic dysfunction (i.e., stiffness) may arise after acute PE and persist despite PH resolution (102–104) but likely is not a main contributor to symptoms. Approximately 4% of acute PE survivors develop chronic thromboembolic PH (CTEPH) (105), making this one of the most common forms of PH. Uniquely, CTEPH has a high index of recovery after intervention.
Current knowledge gaps
Although RVF is an independent cause of increased mortality in ARDS (106), the impact of RVF prevention or treatment on prognosis in ARDS is unknown (107). Prone positioning improves survival and RV function in severe ARDS (108, 109); however, the optimal methods and modes of ventilation, as well as the roles of inotropic support, varying levels of sedation, and paralysis to protect the RV and limit RVF in patients with ARDS all remain poorly studied. Whether prone positioning is indicated in cases of RVF independent of decreases in PaO2/FiO2 remains to be evaluated as well. Despite extensive research on the mechanisms promoting lung injury and pulmonary vascular dysfunction in ARDS, no specific and effective targeted therapies have emerged. For PE, the role of catheter-directed fibrinolysis (vs. standard anticoagulation) for intermediate-risk PE requires large-scale randomized controlled trial investigation (110). Significant gaps exist in understanding the best ways to support the failing RV during these relatively acute RVF syndromes. The optimal intravenous inotrope for clinical use has not been identified. In animal models of chronic RVH, dobutamine appears superior for acute RV support (111), but it is unclear if this also pertains to acute RVF. Although use of inotropes in RVF in the face of PAH identifies a patient cohort at high risk (46%) of in-hospital mortality, it is unclear if this is a mere reflection of the severity of the underlying condition rather than an inotrope effect per se (112). It is also uncertain how best to prevent secondary inflammatory RV injury from PE and ARDS. Modulating LV stiffness in resuscitation remains unstudied for both conditions (102–104). Knowledge about vasoconstrictor–vasodilator balance, platelet hyperreactivity, and coagulation–fibrinolytic balance has not been adequately translated into early-phase clinical trials. Mechanisms of development of CTEPH after acute PE are incompletely understood and need further study. Recently developed rat and piglet models (113–115) will facilitate such studies.
Recommendations/pathway for progress
We recommend developing robust and translationally applicable animal models, designing RV-focused outcome studies to assign risk in large cohorts, and performing RV-focused randomized controlled trials, particularly at the phase I stage. Strategies aimed at understanding common mechanisms of lung injury caused by precapillary pulmonary vascular occlusion associated with PE and/or ARDS need to be identified. Goals should include identifying optimal mechanisms of enhancing CO while supporting systemic vascular tone. This should include studies modulating the β-adrenergic receptor in RV cardiomyocytes as well as studies of mechanical devices. In addition, this should include the unraveling of cause and effect interplay between small vessel occlusion by cells and vasospasm and inflammatory processes that can cause RV injury directly and indirectly. The roles of disordered coagulation, platelet activation, neutrophil-derived networks, and regulation of fibrinolysis need to be defined. For both PE and ARDS, existing evidence raises the hypothesis of a secondary inflammatory hit to the RV, initiated by either direct injury (e.g., shear stress or ischemia) or as collateral damage from systemic inflammation (116). The importance and magnitude of effect of this secondary hit require quantitative study. Priorities should focus on producing translatable knowledge in the laboratory and in clinical trials to enhance the pipeline of new therapies for both conditions. In addition, better data are required to determine the optimal duration of therapy. Guidelines should be developed to assess whether and when RV function should be assessed in patients who recover from acute PE or ARDS. Investigating whether CTEPH surveillance in survivors of a documented PE improves outcomes is therefore indicated. Mechanistic and therapeutic preclinical studies in recently developed CTEPH animal models will provide further knowledge that can be harnessed to improve outcomes of patients with CTEPH.
Differences between Acute and Chronic RV Responses
Rationale
Although identifying cellular and molecular mechanisms that underlie successful adaptation of the RV to chronic stress can lead to efforts to prevent RVF in patients with chronic RV pressure overload (RVPO), this may also lead to strategies that improve outcomes of acute PH. Similarly, a better understanding of mechanisms of acute RVF may lead to treatment strategies for chronic RVF. For example, a detailed knowledge of the mechanisms leading to—or protecting against—myocardial apoptosis in the acute setting could improve the management of patients suffering from both acute and chronic RVF.
Current state of knowledge
Acute RVPO causes wall stress, exhaustion of cardiomyocyte energy resources, impaired calcium handling, release of proinflammatory chemokines and cytokines, inflammatory cell infiltration, and generation of toxic reactive oxygen and nitrogen species, all of which contribute to cardiomyocyte death within hours or days and loss of pump function (96, 98, 100, 101). In contrast, chronic RVPO triggers a slower and more or less successful adaptation to pressure overload (96, 117), including complex alterations in energy metabolism (generally away from fatty acid oxidation [FAO] toward uncoupled glycolysis and carbohydrate oxidation) as well as hypoxemia, ischemia, inflammation, and oxidative stress (1, 2, 13, 118, 119). These changes are accompanied by macroscopic and microscopic structural remodeling of the myocardium and cardiac microcirculation. The remodeling of chronic RVPO includes cardiomyocyte hypertrophy and, in case of unsuccessful adaptation, fibrosis and capillary rarefaction (65). Failure of compensatory mechanisms is believed to trigger transition from adaptive to maladaptive RVH, with ischemia considered a major contributor (65, 120, 121).
Current knowledge gaps
It is likely that changes in metabolism vary among forms of RVF. For example, FAO is increased in PAB (and inhibiting FAO is beneficial to RV function) (122); conversely, in fawn hooded rats (which develop spontaneous PH), FAO is decreased (123). It is likely this disease heterogeneity, which is relatively chamber specific and primarily affecting the RV, is also seen in humans; however, this has not been systematically assessed. Other metabolic pathways are induced in RVH as well, including the de novo appearance of cardiomyocyte glutaminolysis (although this finding requires confirmation) (124). It is unknown if a “point of no return” exists in the transition from adaptive to maladaptive RV remodeling and whether certain failure components are more important than others (117). For example, if impaired FAO in cardiomyocytes is the root cause of RVF, other processes (e.g., apoptosis, inflammation, fibrosis) would be downstream consequences, and therapeutic interventions would need to aim at reversing impaired FAO. Furthermore, it is unclear whether inflammation, oxidative stress, neurohormonal activation, or metabolic alterations equally affect RV function in the acute versus chronic setting and whether targeting these processes has the same outcome in acute versus chronic RVF. The role of hematological factors (e.g., hypercoagulation, platelet activation, hypofibrinolysis) in initiating or propagating acute (and possibly even chronic) RVF is unknown. Furthermore, the contribution of pulmonary vasoconstriction to inducing and maintaining acute or chronic RVPO has not been well defined. Last, the role of the LV in the setting of RVPO needs further definition. Even with acute PH, the LV becomes compressed and stiffened by an enlarged RV, thereby contributing to reduced CO (102, 103).
Recommendations/pathway for progress
Targets and pathways important in acute RVF should be evaluated in chronic RVF (and vice versa), allowing for identification of common as well as unique targets and pathways in either setting. For example, in acute PE, hemolysis increases shear forces in the RV (125), and multiple sites in the coagulation cascade are believed to contribute to acute RVF development (126, 127). If these processes are identified as being unique to acute RVF, their study may lead to novel treatment targets. If a role in chronic RVF is established, these concepts could then be expanded to treating the chronically failing RV. Comparing acute with chronic RVF will allow for a better understanding of the transition from compensated RV remodeling. Phenotypic, genetic, and epigenetic determinants of adaptation in the acute or chronic setting should be studied. Comprehensive and integrated systems biology/-omics approaches are most likely to yield novel insights regarding the shared and divergent pathways and mechanisms between acute and chronic RVF.
Regional Differences in RV Responses
Rationale
Recent data indicate that RV responses to acute or chronic afterload stress vary between different regions of the RV. Uncovering these regional differences will help identity mechanisms of transition from adaptive to maladaptive RVH. Please see the online supplement for further details. LV involvement in RV disease and ventricular interdependence are covered in Assessment Of RV–LV Interactions and Ventricular Interdependence.
Table 3 lists key knowledge gaps and solution approaches for topic domain 1.
Table 3.
Key Knowledge Gaps and Approaches to Improve Methodology to Assess Right Ventricular Function in Acute and Chronic Conditions in Preclinical Models, Human Studies, and Clinical Trials
| Key knowledge gaps |
| • What is the definition of “normal” and “abnormal” RV structure and function? How do key demographic characteristics such as age, sex, race/ethnicity, and socioeconomic status affect the definitions of “normal” and “abnormal”? |
| • How do aspects of RV development throughout the life span as well as cardiopulmonary interactions under stress and in response to critical exposures affect the definition of “normal” vs. “abnormal” RV function? |
| • What is the exact impact of existing and novel PAH therapies on RV function? |
| • Better animal and in vitro models are needed that allow study of RV function in all groups of PH. |
| • What are the mechanisms of RV dysfunction in acute PE and ARDS? Which interventions improve RV function in these settings? |
| Solution approaches/pathways forward |
| • After the identification of a critical set of RV biomarkers, a joint global effort is needed to replicate and validate prior findings and to determine effects of age, sex, race/ethnicity, exercise, and other exposures on these biomarkers in animal studies and human cohorts. |
| • Human RV specimens should be studied to improve understanding of human disease and determine to what extent experimental models may or may not recapitulate human disease. |
| • A small but unique set of biomarkers of RV function should be defined that can be used to quantify load-independent effects of medical and nonmedical PH treatment in clinical studies. |
| • While acknowledging that a single model reflecting RV function in all aspects and types of PH is unlikely to be developed, novel models (in vivo, in vitro [e.g., “heart on a chip,” iPSCs], and in silico) should be developed that replicate critical aspects of RVF in all groups of PH. |
| • Determine mechanisms of RVF in patient cohorts and in animal models of acute (and chronic) PE and ARDS. The effect of novel RV-directed therapies (e.g., prone positioning in ARDS) on RV function in these settings should be prospectively studied. |
Definition of abbreviations: ARDS = acute respiratory distress syndrome; iPSCs = induced pluripotent stem cells; PAH = pulmonary arterial hypertension; PE = pulmonary embolism; PH = pulmonary hypertension; RV = right ventricle; RVF = right ventricular failure.
Topic Domain 2: Analyzing Advanced RV Hemodynamic Parameters at Rest and in Response to Exercise
Rationale
Identification of knowledge gaps and solution approaches in hemodynamic phenotyping and prognostication requires a detailed understanding of the various tools used. This section, therefore, reviews strengths and weaknesses of commonly used tools, identification of knowledge gaps, and pathways for progress.
Invasive and Noninvasive Phenotyping of RV Function
Current state of knowledge and knowledge gaps
Comprehensive assessment of the RV requires a combination of RHC and RV imaging via echocardiography or CMR. Biomarkers and exercise testing serve as additional tools. RHC allows for a thorough (though not complete) description of RV function, with right atrial pressure to estimate RV end-diastolic volume, or preload, PAP, or PVR to estimate afterload, and stroke volume (SV) to reflect contractility. Imaging by echocardiography and/or CMR offers additional information. Both provide accurate (although sometimes imprecise) estimates of systolic, mean, and diastolic PAP, left atrial pressure (LAP), and CO, and derived calculations of PVR and pulmonary arterial (PA) compliance. More importantly, both techniques provide indices of RV systolic function, diastolic function and filling pressures, planar and volumetric estimations of dimensions, and quantifications of dyssynchrony (interregional inhomogeneity of contraction) and asynchrony (interventricular inhomogeneity of contraction) and RV volumes.
Recommendations/pathway for progress
RV function is often reported in a cursory fashion and frequently limited to an EF measurement. A physiologically sound definition of RVF (see Definition, Development, and Staging of RVF) should be implemented in biological and clinical studies, to avoid ambiguity in bench-to-bedside translation and epidemiology. Clinical studies can achieve this through an integrated imaging and invasive approach (e.g., RHC, imaging by echocardiography and/or CMR, and possibly PET [128]); preclinical investigations should use comprehensive hemodynamics and RV imaging studies (70).
Prognostic Relevance of Measurements of RV Function
Current state of knowledge and knowledge gaps
Table E1 in the online supplement provides an overview of the prognostic capabilities of RHC-, echocardiography-, and CMR-derived variables in various types of severe PH. Various combinations of these parameters have been used in prediction models (129, 130). RHC-derived predictors of outcomes include CO (measured or calculated from mixed venous blood oxygenation) (131–135), right atrial pressure (132–134, 136), PVR (135–137), and PAP (133). Echocardiographic predictors include pericardial effusion (138–141), right heart dimensions (139, 140, 142–144), estimated RV diastolic pressure (140, 145), tricuspid regurgitation (142), TAPSE (23, 140, 143, 146), maximum tissue velocity of isovolumic contraction (147), dP/dt (146), strain (evaluated by variable and evolving methodologies) (141, 148, 149), asynchrony and regional inhomogeneity of RV contraction (150), myocardial performance index (151, 152), RV fractional area change (130), right atrial size index (130), and RV contractile reserve (defined as the exercise-induced increase in the maximum velocity of tricuspid regurgitation) (153). These data suggest that echocardiography offers prognostication via measurements of RV systolic function (TAPSE, velocity of isovolumic contraction, dP/dt, strain, myocardial performance index, contractile reserve), dimensions, and estimates of filling pressures. CMR-derived predictors include SV (21, 154), end-diastolic volume (21, 155), RVEF (3, 154, 156), end-systolic volume (ESV) (129, 157), SV/ESV (3), and late gadolinium enhancement (158). The latter, however, is not uniformly confirmed (159). CMR therefore offers prognostication from measures of systolic function (ESV, EF, SV/ESV) and right heart dimensions. A recent CMR-based study used machine learning of patterns of RV motion for outcome prediction in PH (160). Because of their noninvasive nature, there has been particular interest in using imaging parameters to assess RV function. The current knowledge, knowledge gaps, and potential future roles of commonly used RV imaging parameters are listed in Table 4. As of now, CMR remains the standard of measurement, and RVEF is the most robustly validated parameter. Head-to-head comparisons of other imaging parameters with regard to superiority are lacking, and the appropriateness for use of one specific parameter rather than others in special clinical scenarios has not been well described. Please see the online supplement for further discussion of caveats pertinent to the use of RV function markers as prognosticators.
Table 4.
Current State of Knowledge, Knowledge Gaps, and Potential Future Roles of Commonly Used Right Ventricular Imaging Parameters
| Imaging Parameter | Current State | Disadvantages and Knowledge Gaps | Future Role |
|---|---|---|---|
| TAPSE | • Easy and quick assessment | • Less suitable for serial assessment (284, 285) | • 2D measures will still be used for assessment of RV function |
| • Cheap and widely available | • 2D measures are less suitable for serial assessment owing to the complex geometry of the RV | ||
| • High reproducibility (280, 281) | |||
| • Prognostic value at baseline (23, 141, 282, 283) | |||
| RVFAC | • Easy and quick assessment | • Less reproducible than TAPSE (280, 281, 285) | • See TAPSE |
| • Good relation with RVEF (280, 285, 286) | • Less suitable for serial assessment (285) | ||
| • Prognostic value at baseline in PAH (141, 282, 283) | |||
| Eccentricity index | • Easy and quick assessment | • Lack of information on serial assessment | • See TAPSE |
| • Prognostic value at baseline in PAH (282, 283) | |||
| Strain/strain rate | • Prognostic value in PAH (141, 283, 287) | • Strain assessment possible with echo (2D speckle tracking) and CMR (tagging) | • Shows potential to assess RV dysfunction in a very early stage |
| • Early detection of RV dysfunction; detects differences in RV function when other traditional measurements, including TAPSE, fail to do so (288) | • Tagging analyses time-consuming | ||
| Myocardial performance index (Tei index) | • No need to make geometric assumptions | • Doppler echocardiography only | • See TAPSE |
| • Prognostic value in PAH (141, 282) | |||
| RVEF | • Gold standard parameter for assessment of RV systolic function | • Assessment is time-consuming | • Likely to be useful in assessment of prognosis and treatment response |
| • RVEF is reproducible (289) | • Presence of tricuspid regurgitation can overestimate RVEF | • Automated assessment of RV volumes with CMR needed | |
| • Prognostic value at baseline and during follow-up (3, 21) | • Minimal clinical important difference unknown | • 3D echocardiography may enable accurate assessment; however, currently 3D echocardiography RV underestimates volumes and is less reproducible (290–294) | |
| RVSV/RVESV | • Prognostic value at baseline (129, 184) | • Assessment time-consuming | • May be an important parameter, although the measure shows a great similarity to RVEF |
| • Minimal clinical important difference unknown | |||
| • Reproducibility unknown | |||
| • Prognostic value of the change over time unknown | |||
| • Indexing to body size may be necessary but is not consistently done | |||
| RV volumes | • Prognostic value at baseline and at change during follow-up (3, 21, 157, 295) | • Assessment time-consuming | • Will play a role for assessment of prognosis and treatment response |
| • Minimal clinical important difference unknown (only assessed for RVSV [20]) | • Automated assessment of RV volumes with CMR needed | ||
| • Not consistently indexed to body size | • 3D echocardiography may enable accurate assessment; however, currently 3D echocardiography RV underestimates volumes and is less reproducible in comparison to CMR (290–294) | ||
| LGE | • LGE at interventricular insertion points and septum prognostic value at baseline (159). Possibility to assess myocardial pathologies (fibrosis) (296) | • MRI only | • LGE will probably be replaced by T1 mapping for assessment of myocardial pathologies in the future |
| • Need reference region of interest in myocardium, making LGE less suitable for assessing diffuse myocardial pathologies | |||
| Native T1 values | • Native T1 values at interventricular insertion points are related to measures of disease severity (227, 297) | • MRI only | • Shows potential to replace LGE |
| • Prognostic value unknown | • No administration of contrast agents needed for generating T1 maps | ||
| • Longitudinal changes unknown | • More suitable for detection of diffuse myocardial pathology | ||
| • Spatial resolution of T1 maps currently too low to assess total RV free wall (227) | • Future studies will need to assess its prognostic value | ||
| • Resolution and correction for partial volume effects (fat saturation pulse) in T1 mapping needs to be improved |
Definition of abbreviations: 2D = two-dimensional; 3D = three-dimensional; CMR = cardiac magnetic resonance imaging; LGE = late gadolinium enhancement; MRI = magnetic resonance imaging; PAH = pulmonary arterial hypertension; RV = right ventricular; RVEF = right ventricular ejection fraction; RVESV = right ventricular end-systolic volume; RVFAC = right ventricular fractional area change; RVSV = right ventricular stroke volume; TAPSE = tricuspid annular plane systolic excursion.
Recommendations/pathway for progress
Imaging or invasive measurements of RV function, identified as prognostic indicators in PAH, should be evaluated together in the framework of a multicenter trial and prediction scores constructed from rigorously identified independent predictors. A hierarchy of imaging parameters and their appropriateness for specific scenarios should be determined.
Assessment of RV Afterload
Current state of knowledge and knowledge gaps
With low-normal PVR, the contribution of the RV to pulmonary blood flow is modest at rest (evidenced after a Fontan operation). However, RV pump function is required in cases of increased afterload (e.g., in acute or chronic PH). RV afterload is affected by PVR, but there are several other equally valid contributors (161): 1) Maximum wall tension (an impractical parameter because of the irregular shape of the RV and regional inhomogeneities in contraction); 2) hydraulic power (WTOT; calculated from the integration of instantaneous pressure and flow waves, which is the sum of oscillatory power [WOSC] and steady power [WST = mPAP × CO]); 3) arterial elastance (Ea; calculated from an RV pressure–volume loop as end-systolic pressure [ESP]/SV), corresponding to a measurement of afterload as “seen” by the ventricle; and 4) pulmonary vascular impedance, which represents the most comprehensive assessment of RV afterload (although least accessible to the clinician) (162).
RV pressure–volume loops with preload reduction allow for identification of the end-systolic elastance (Ees; the standard of measure for load-independent contractility in vivo). Direct measurements of Ees and Ea allow for calculation of the Ees/Ea ratio as a measurement of the coupling of the RV to the pulmonary circulation (2, 161) (Figure 4). This concept was initially developed for the LV (163) but soon thereafter was shown to be applicable to the RV (164). Sagawa and colleagues demonstrated that optimal efficiency of ventriculoarterial coupling (allowing for flow output at minimal amount of energy cost) is achieved in either ventricle when maximal or end-systolic elastance is 1.5 to 2 times greater than Ea (165). In the RV, the amount of uncoupling associated with decreased maximum cardiac output and increased RV size with high filling pressures and systemic congestion is not exactly known (128). Although a coupling ratio of 1 at rest may still be associated with preserved RV dimensions, at this level of Ees/Ea, there is impaired contractile reserve, and exercise is associated with uncoupling and increased dimensions (166, 167). Furthermore, in experimental animal models of embolic PH, the RV starts to dilate when Ees/Ea is decreased to 0.7 to 1.0 (168, 169). Most investigators therefore consider “optimal” mechanical RV–arterial coupling to correspond to an Ees/Ea of 1 to 2. Interestingly, for a similar afterload, patients with scleroderma-PAH demonstrate lower Ees/Ea than patients with idiopathic PAH (1.0 vs. 2.1) (170), suggesting significant uncoupling in scleroderma-PAH.
Figure 4.
Methods used to estimate right ventricle–pulmonary artery (RV–PA) coupling and diastolic stiffness. In both (A) the volume method, and (B) the pressure method, arterial elastance (Ea) is calculated from the ratio of end-systolic pressure (ESP) to stroke volume (SV). End-systolic elastance (Ees) as an approximation of maximum elastance in the volume method is estimated by the ratio of ESP to end-systolic volume (ESV), which results in a simplified Ees/Ea of SV/ESV. In the pressure method, Pmax is estimated from the nonlinear extrapolation of the early systolic and diastolic portions of the RV pressure curve. Ees is the ratio of (Pmax − mPAP) divided by SV, which results in a simplified Ees/Ea of (Pmax/mPAP − 1). (C) The single-beat method calculates Ees as a straight line drawn from Pmax tangent to RV pressure–relative change in volume relationship. The approach relies on an estimate of Pmax determined from the extrapolation of early and late isovolumic portions of an RV pressure curve and synchronized absolute or relative volume measurements. Ees is then defined by a tangent from Pmax to the pressure–volume relationship, and Ea is defined by a line drawn from the Ees point to end-diastolic volume (EDV) (at zero pressure). (D) Diastolic stiffness (β) is calculated by fitting the nonlinear exponential P = α(eVβ − 1) to pressure and volume measured at the beginning of diastole (BDP, ESV) and the end of diastole (EDP, EDV). Adapted by permission from Reference 184. BDP = beginning diastolic pressure; EDP = end-diastolic pressure; Evol = Ees estimated by the volume method; mPAP = mean pulmonary arterial pressure; Pmax = RV maximum pressure; sRVP = peak systolic RV pressure.
Ea and WTOT are metrics of RV afterload, so it is understandable that these measurements of the pulmonary circulation emerge as prognostic markers of RVF in severe PH (171, 172). For example, increased stiffness of the proximal PA, mediated by excessive collagen accumulation, increases the pulsatile component of RV afterload (quantified by measurement of impedance [173]) and thus decreases RV–PA coupling and RV contractile reserve (defined as the ability of the RV to increase contractile function during exercise) (2, 153, 174). Consequently, PA compliance is an important predictor of mortality in PAH (2, 172, 174, 175).
The most comprehensive measure of RV afterload is pulmonary vascular impedance, which represents the opposition of the vascular bed to pulsatile flow generated by friction in small-diameter vessels, stiff vessels that do not accommodate pulsations, and branching and tapering vessels that generate wave reflections (162).
Recommendations/pathway for progress
Contributions of the various components of RV afterload to RV function and RV adaptive and maladaptive processes need better definition. Effects of PAH-targeted therapies on components of RV afterload require further study. Easy-to-obtain bedside measures of RV afterload would be of value.
Assessment of RV–PA Coupling
Current state of knowledge and knowledge gaps
The most accurate measurement of RV–PA coupling is Ees/Ea. However, the complex geometry of the RV makes functional evaluations with measurement of instantaneous volume changes technically difficult. In addition, manipulating systemic venous return to alter RV preload clinically is not practical. Accordingly, a single-beat method has been developed, allowing for determining Ees and Ea from instantaneous ventricular pressure and flow output (176) or volume (129) measurements (Figure 4). However, this method is controversial, as it relies on multiple assumptions (176).
RV–PA coupling has been assessed in several studies in patients with PAH or CTEPH, and in one case report of a patient with a systemic RV (129, 167, 170, 177–179). As shown in Table E2, Ees/Ea was either maintained or decreased at rest but consistently decreased at exercise. In aggregate, these results agree with the notion of homeometric adaptation of RV function to afterload, even though the results do not allow identification of critical levels of decoupling associated with onset of heterometric adaptation and congestion.
Recommendations/pathway for progress
RV–PA coupling measurement should be implemented in studies investigating the mechanisms of action of targeted therapies in PAH (which decrease RV afterload but may or may not have intrinsic myocardial effects), even if not as the primary endpoint. It is controversial whether Ees/Ea can be measured on a single-beat pressure–volume loop versus a family of such loops generated by a manipulation of venous return. A study comparing these methods in patients with various types of PH is urgently needed. Simplified surrogate measurements of Ees/Ea, such as SV/ESP (156, 180) and (RV maximum pressure/mPAP − 1) (181) (Figure 4), should be validated.
Assessment of RV Diastolic Function
Current state of knowledge and knowledge gaps
Coupling of RV function to afterload has an inevitable diastolic component (2, 161, 182). Diastolic stiffness may be a predictor of outcomes in severe PH (183, 184). Please see the online supplement for a summary of RV diastolic function assessment.
RV diastolic function has not been specifically explored by imaging studies. Its description is generally limited to the isovolumic relaxation time, the ratio of trans-tricuspid flow E wave to tricuspid annulus tissue Doppler imaging tricuspid e′, the deceleration of the E wave, estimated RV filling pressure from the inferior vena cava dimension and inspiratory collapse, and end-diastolic area or volume. However, these measurements have not been systematically confirmed with diastolic pressure–volume curves or, with the exception of occasional parameters (Table E1), been considered as prognostic markers.
Recommendations/pathway for progress
The relevance of RV diastolic elastance or its surrogate, the end-diastolic pressure–volume ratio, should be further assessed. Novel, noninvasive measurement techniques using echocardiographic or other imaging methods are needed.
Assessment of RV–LV Interactions and Ventricular Interdependence
Current state of knowledge and knowledge gaps
RV function needs to be understood in the context of its direct and indirect interactions with LV function. Direct interaction, or ventricular interdependence, is defined as the forces that are transmitted from one ventricle to the other through the myocardium, perivalvular fibrous annulus, and pericardium, independent of neural, humoral, or circulatory effects (185). Diastolic ventricular interaction refers to the competition for space within the indistensible pericardium when the RV dilates. RHC and imaging studies demonstrated that in patients with severe PH, mPAP and LV peak filling rate are altered in proportion to decreased RVEF (186). Systolic interaction refers to positive interaction between RV and LV contractions. For example, aortic constriction and the subsequent increase in LV contraction markedly improve RV function in animals with PAB (187). Similarly, in electrically isolated ventricular preparations, LV contraction contributes significantly (∼30%) to both RV contraction and pulmonary flow (187). This is explained by a mechanical entrainment effect, but also by LV systolic function determining systemic blood pressure (an essential determinant of RV coronary perfusion). This is important because increased RV filling pressures and excessive decrease in blood pressure have been linked to RV ischemia and decreased contractility (188).
An additional cause of negative ventricular interaction is regional and interventricular asynchrony with postsystolic contraction or “shortening.” This develops in parallel with increased PAP and contributes to altered RV systolic function and LV underfilling (189). RV regional asynchrony can be identified and quantified by echocardiography using two-dimensional (2D) or 3D speckle tracking (149, 156) (see Regional Differences in RV Responses for further details). Electrophysiologically, this phenomenon is reflected by increased QRS width and prolonged duration of the monophasic action potential of RV myocytes secondary to downregulation of repolarizing potassium channels (72). Interestingly, this is amenable to metabolic therapies (72). Likewise, QTc duration increases in patients with PAH and serves as a prognostic indicator that appears to be related to RV mass (190). LV abnormalities in patients with RVF are not limited to functional changes. In fact, fibrotic and inflammatory changes in LVs from patients with PAH were recently reported (191).
Recommendations/pathway for progress
Further insight into the functional significance and clinical relevance of dyssynchrony and asynchrony is needed. Because interventricular interdependence evolves in both acute and chronic RVF, studies in relevant preclinical models are needed to determine the relative contribution of this pathogenic mechanism in those conditions. Mechanisms of structural, biochemical and molecular LV abnormalities in patients with RVF require further study.
Emerging and Alternative Approaches
Please see the online supplement for a detailed discussion of this topic.
Table 5 lists key knowledge gaps and solution approaches for topic domain 2.
Table 5.
Key Knowledge Gaps and Solution Approaches for Analyzing Advanced Right Ventricular Hemodynamic Parameters at Rest and in Response to Exercise
| Key knowledge gaps |
| • What are the gold standard measurements of RV–arterial coupling (Ees/Ea) in various types and severities of PH? What is their relevance to functional state, exercise capacity, and outcomes? |
| • What is the natural history of RV–arterial uncoupling and RV dilatation/altered diastolic function and congestion? |
| • How can simplified pressure and volume methods to estimate RV–arterial coupling be validated? |
| • How can items on the currently growing list of echocardiographic and CMR measurements of systolic and diastolic dimensions and function be integrated and validated (e.g., what is the added value with respect to RHC)? Is there a need for scores? |
| • What are optimal* measures of RV afterload (e.g., WTOT, Ea, PA compliance, Ca, Zc, low-frequency PVZ, imaging of proximal stiffness, RV wall tension)? |
| • How can differences in definition, methodology (e.g., exercise, dobutamine) and relevance of RV contractile reserve measurements be resolved and harmonized? |
| Solution approaches/pathways forward |
| • Perform further monocentric expert physiological and clinical studies on RV–arterial function adaptation to PH using gold standard invasive methodology in various clinical circumstances. |
| • Further definition of the best compromise between gold standard and simplified imaging methods. |
| • Multicenter effort to investigate the hemodynamic, imaging, and CPET predictors of functional capacity and survival. |
| • Implement optimal invasive and noninvasive phenotyping measures of RV function in basic and human studies focusing on the biology of RVF. |
Definition of abbreviations: Ca = capacitance; CMR = cardiac magnetic resonance imaging; CPET = cardiopulmonary exercise testing; CTEPH = chronic thromboembolic pulmonary hypertension; Ea = arterial elastance; Ees = end-systolic elastance; PA = pulmonary artery; PAH = pulmonary arterial hypertension; PH = pulmonary hypertension; PVZ = pulmonary vascular impedance; RHC = right heart catheterization; RV = right ventricular; RVF = right ventricular failure; WTOT = hydraulic power; Zc = characteristic impedance.
The group notes that one should not expect to find one optimal measure of RV afterload. Rather, one measure may be better for diagnosis, and another may be better for prognosis; one may be better for CTEPH and one for scleroderma-associated PAH; etc.
Topic Domain 3: Deciphering the Underlying Molecular and Pathogenic Mechanisms of RV Function and Failure
Assessment of Hypertrophy and Angiogenesis
Rationale
Adaptive myocardial remodeling requires coordination of myocyte hypertrophy and angiogenesis to preserve ventricular function. Myocyte hypertrophy associated with a disproportional number of capillaries and/or endothelial cell (EC) dysfunction may ultimately promote RVF. Regulation of angiogenesis is complex (reviewed in Reference 192) and involves molecular cross-talk between myocytes and ECs (193, 194). Insight regarding molecular mechanisms linking RV myocyte hypertrophy and angiogenesis is limited. Further investigation is likely to identify new paradigms and therapeutic strategies.
Current state of knowledge
In the LV, angiogenesis is necessary (195, 196) and sufficient (197, 198) for myocyte hypertrophy. The interplay between angiogenesis and myocyte hypertrophy is poorly defined in the RV, which has unique mechanisms to augment myocyte perfusion during increased myocardial demand (199). A detailed review of the topic was recently published (200). RV angiogenesis has been evaluated in animal models of PH, although most studies relied on counting capillary profiles in 2D sections. Some authors believe that this approach may lead to underestimation of effective capillary length and surface area (201) and unintentional sampling bias (201, 202) that may lead to inconsistent findings, even within the same model (203–208). Analysis of 2D sections in PH models associated with RVF demonstrated reduced RV capillary density (65, 124, 207), potentially reflecting capillary rarefaction. In the rat monocrotaline model, early microvascular expansion was reversed as RVF ensued (209). These data, obtained from several laboratories and consistent with data reporting vascular rarefaction in LV hypertrophy, suggest that a combination of cardiomyocyte hypertrophy (causing increased demand) and capillary rarefaction leads to clinically relevant RV ischemia in PAH (210). However, a recent analysis of human RV tissue by a stereological approach noted an increase in total vascular length in PAH RVs versus controls (211). Although the role of microvascular ischemia is still controversial, the role of macrovascular ischemia (reduced coronary perfusion pressure due to elevated RV end-diastolic pressure) is established (188).
Molecular regulators of RV angiogenesis and myocyte hypertrophy have received limited attention. In addition, whether molecular regulation is similar between the failing LV and RV is also incompletely understood. Animal models support potential roles for hypoxia-inducible factor and vascular endothelial growth factor (65, 207, 209), although these pathways may be impaired in RVF (64, 119). Recent studies identified additional potential proangiogenic regulators in the LV (e.g., PlGF, NF-κB [nuclear factor-κB], extracellular ubiquitin, STAT3, Nrf2, and Ang-2/Tie-2) (197, 212–216), but these have not been studied in the RV. A potential regulatory role for the proangiogenic microRNA miR-126 in RV capillary rarefaction was recently shown (217). Although several angiostatic factors were recently identified as unique biomarkers in PAH (218, 219), their role in regulating RV angiogenesis has not been explored.
Current knowledge gaps
Pivotal questions are whether RV angiogenesis is necessary for adaptive myocardial remodeling and whether EC dysfunction, insufficient angiogenesis, and/or capillary rarefaction lead to maladaptive remodeling and RVF. The quantitative and temporal relationship between myocyte hypertrophy and angiogenesis required to preserve RV function in PH has not been established. Better understanding of the molecular regulators of RVH and angiogenesis is needed to develop studies designed to investigate whether hypertrophy and successful adaptation depend on angiogenesis. The potential role of angiostatic/antiangiogenic factors (217, 218, 220) in counteracting initial angiogenic responses is incompletely understood. The applicability of any single animal model to human RV angiogenesis and hypertrophy in PH is uncertain, and differences between models require further characterization. Angiogenesis data from patients with PAH are extremely limited, and current noninvasive imaging modalities lack sufficient resolution.
Recommendations/pathway for progress
Studies focused on RV myocyte hypertrophy and angiogenesis that use standardized, quantitative metrics avoid unintentional sampling bias and produce physiologically relevant endpoints (stereological methods [221]) that will improve precision and significance of morphometric studies. Mechanistic studies, including both unbiased screens for angiogenic and angiostatic mediators and hypothesis-driven assessment of specific regulatory candidates during multiple stages of RV remodeling, will advance the field. Additional insight is likely to be gained by more advanced imaging techniques (micro–computed tomography, microsphere injection), although these will require comprehensive assessment of the entire RV or a rigorous, unbiased sampling strategy.
Table 6 lists several key recommendations for the study of molecular and pathogenic mechanisms of RV function, which are relevant for the study of RVH and angiogenesis but are also critical for the study of the other mechanisms listed in topic domain 3. RV vascularization should be measured in an unbiased fashion; however, there currently is no agreement on whether stereology is the only acceptable technique for this. At the very least, further studies are needed that compare stereological versus other techniques (e.g., two-photon confocal imaging with 3D reconstructions). We strongly recommend the inclusion of human samples for morphological studies, which may be facilitated by the development of central tissue repositories. RV biopsy is safe in patients with RVH at the time of surgery (e.g., in pulmonary endarterectomy for group 4 PH [222]). We recommend that preclinical studies evaluate hypertrophy and angiogenesis in multiple models, including both male and female subjects. Studies of sex and age as modifiers of hypertrophy and angiogenesis should be pursued to better understand these relevant modulators of RV function (30, 36, 223). The potential role of progenitor cells as modifiers of RVH and angiogenesis (224) requires further study. Next-generation sequencing techniques in humans and animals may help identify genetic contributors to hypertrophy development and angiogenesis. Development and validation of noninvasive imaging techniques with adequate resolution to assess RV myocyte hypertrophy and angiogenesis should be a priority.
Table 6.
Key Knowledge Gaps and Solution Approaches for Deciphering the Underlying Molecular and Pathogenic Mechanisms of Right Ventricular Function and Failure
| Key knowledge gaps |
| • Is angiogenesis and/or capillary maintenance necessary to preserve RV function during remodeling, and does capillary rarefaction cause maladaptive RV remodeling? |
| • Does myocardial fibrosis promote RVF, and can it be reversed? |
| • Are metabolic alterations necessary for transition from adaptive to maladaptive RV remodeling? If so, which changes are the most important ones in this process? Which alterations in myocardial metabolic pathways should be targeted therapeutically, and how? |
| • Are apoptosis and other forms of cellular death necessary for transition from adaptive to maladaptive RV remodeling? |
| • Are myocardial inflammation and oxidative stress causes or consequences of RVF? |
| • What is the role of circulating and resident progenitor cells in modulating RV hypertrophy, angiogenesis, fibrosis, metabolism, cell death, inflammation, oxidative stress, and contractile signaling? |
| • How do established and novel PAH therapies modulate RV hypertrophy, angiogenesis, fibrosis, metabolism, cell death, inflammation, oxidative stress, and contractile signaling? |
| • Are potential short-term detrimental effects on RV contractile function with neurohormonal modulators (e.g., β-adrenergic receptor antagonists) offset by long-term beneficial effects on other signaling pathways? |
| Solution approaches/pathways forward |
| • More human studies focused on identifying mechanisms of RVF and facilitated through RV biopsy samples, tissue repositories, and development of advanced imaging techniques. In order to enhance scientific impact, human subjects need to be well phenotyped |
| • Identification and validation of biomarkers of RV remodeling and dysfunction to facilitate human studies in PH-induced RV dysfunction |
| • Use of stereological methods in all morphometric analyses, including both human tissue and animal models |
| • More studies investigating the roles of sex and age as modifiers of RV function |
| • More studies investigating the roles of circulating and resident progenitor cells as modifiers of RV function |
| • Next-generation sequencing techniques in humans and animals to identify genetic contributors to RV adaptation and maladaptation |
| • Correlation of findings from cellular and animal studies with human phenotypes |
| • Identification/clarification of important mechanistic differences between preclinical models of RV adaptation and RVF |
| • Expanded use of RV working heart models and in vitro analyses of diverse myocardial cell types to evaluate specific regulatory pathways |
Definition of abbreviations: PAH = pulmonary arterial hypertension; PH = pulmonary hypertension; RV = right ventricular; RVF = right ventricular failure.
Assessment of Fibrosis
Rationale
Fibrosis is a common end result of various pathogenic processes (2, 119), resulting in contractile dysfunction, diastolic dysfunction, and arrhythmias (2, 119). Cardiac fibrosis can be detected using CMR; patients with PAH with late gadolinium uptake (indicating fibrosis) have a poor prognosis (158). Strategies aimed at decreasing fibrosis may attenuate RVF.
Current state of knowledge
Major mediators of fibrosis include angiotensin, aldosterone, transforming growth factor-β, and matrix metalloproteinases (119). In preclinical studies, fibrosis is typically quantified via histological methods (e.g., collagen staining with trichrome or picrosirius red). More indirect measures of fibrosis include hydroxyproline assays and measurements of collagen breakdown products in the urine. In clinical studies, the gold standard for fibrosis assessment is CMR with late gadolinium enhancement (225, 226). Native T1 mapping by magnetic resonance imaging (MRI) provides similar information without administration of gadolinium (227). A role for PET scans is emerging (e.g., with radiolabeled cyclic arginine-glycine-aspartic [RGD] peptides tracking α-v β-3 integrin expression [228]).
Current knowledge gaps
The clinical relevance of RV fibrosis in PAH is uncertain. Although late gadolinium enhancement at septal hinge points on CMR (corresponding to areas of increased mechanical stress) predicts increased mortality, findings of fibrosis among autopsy series vary, and less is known about patients with early disease. No biomarkers of RV fibrosis currently exist. The role of fibrosis in mediating transition from adaptive to maladaptive RV remodeling is unclear. Uncertainty exists about the possible role of circulating progenitor cells and resident progenitor cells in mediating RV fibrosis. Conversely, a better understanding of mechanisms mediating regression of fibrosis is needed. It is unclear how representative animal models are of RV fibrosis, and differences between models are not sufficiently characterized. Finally, it is unknown if therapies targeting RV inflammation, angiogenesis, and bioenergetics (229) or PAH-directed therapy will reduce RV fibrosis.
Recommendations/pathway for progress
Noninvasive studies of RV fibrosis and assessment of RV biopsy specimens will improve understanding of the mechanisms and consequences of RV fibrosis in human RVF. The routine use of gadolinium-enhanced CMR (already part of the monitoring algorithm in many centers) should be considered as a potential gold standard for noninvasive detection and quantification of RV fibrosis. Identification and validation of potential biomarkers of RV fibrosis would move the field forward. The study of isolated fibroblasts from normal and diseased RVs would provide novel mechanistic insights in fibrosis progression and regression. It will be important to know whether disorders found in pulmonary vascular cells and RV cardiomyocytes are also detected in RV cardiac fibroblasts. In vitro studies of PH-RV fibroblasts should confirm that these cells retain their disease phenotype in cell culture. Table 6 lists further recommendations regarding the study of human samples, stereology, biomarkers, progenitor cells, consideration of sex and age, and use of next-generation sequencing techniques.
Assessment of Cardiomyocyte Metabolism
Rationale
The normal adult RV relies primarily on primary FAO for ATP production (230). However, metabolic plasticity in the RV is seen at the time of birth and with disease states inducing RVH. RV myocytes engage in several maladaptive forms of metabolism during hypertrophy, including uncoupled glycolysis, dysregulated FAO, and glutaminolysis (reviewed in Reference 229). Because these alterations contribute to cardiomyocyte dysfunction (69, 72, 122, 231, 232), further insight into mechanisms of metabolic dysregulation is likely to identify new paradigms and new targets for therapeutic intervention.
Current state of knowledge
RV myocardial energetics are implicated in the regulation of RV function in experimental and clinical PAH, and metabolic therapies are well validated in preclinical models (65, 69, 72, 122, 231, 232). Metabolic changes may be (in part) elicited by ischemia and potentially genetic and epigenetic alterations (69, 233, 234). Epigenetic changes may be mediated by histone deacetylation, methylation of CpG islands (promoter regions with a high frequency of C-phosphate-G nucleotides), and miRNAs. Fluorodeoxyglucose F 18–PET studies have shed light on metabolism in humans, suggesting PAH-associated RVH is associated with increased glucose uptake. There are early, conflicting data regarding changes in FAO in the PAH-RV (235–239). Clinical trials are currently evaluating whether correction of metabolic alterations, such as reducing FAO or enhancing glucose oxidation, attenuates RVF (Clinicaltrials.gov identifiers NCT02102672 and NCT01083524).
Current knowledge gaps
Gaps exist in understanding the contribution of metabolic dysfunction to RVF, in particular the metabolic processes that drive transition from RV compensation to failure. Defining which metabolic changes are considered adaptive versus maladaptive will assist in testing metabolic therapies to prolong RV compensation and improve outcomes. Triggers of altered metabolism in the human RV, and whether correction of ischemia would reverse RV metabolic dysfunction, remain unknown. Moreover, it is unclear whether RV ECs or fibroblasts exhibit similar metabolic abnormalities to myocytes.
Recommendations/pathway for progress
Additional study of metabolic dysregulation in humans and human tissues is needed. Use of micropolarimetry would allow for direct measurement of metabolism in freshly isolated RV myocytes (reviewed in Reference 229). Such direct ex vivo studies, as well as use of in vivo confocal microscopy, would be important to avoid pharmacological inference from in vivo experiments as a basis for defining changes in the RV in PH. Metabolic imaging, using PET with conventional and novel radiotracers and MR spectroscopy, holds promise to enhance understanding of the in vivo metabolic RV phenotypes and defining the transition from compensation to decompensation. In preclinical studies, use of Langendorff and working heart models allows more definitive attribution of metabolic therapies to changes in RV function. In vivo, the use of high-fidelity catheters to measure pressure–volume relationships can help establish effects of metabolic therapies on the RV (240). Metabolic studies in skeletal muscle may be highly relevant in patients with PAH, because several metabolic abnormalities are also evident peripherally (241–243). Human samples, stereology, biomarkers, progenitor cells, sex and age, and sequencing techniques should be considered as outlined in Table 6.
Assessment of Cell Death
Rationale
Cardiomyocyte death is considered the common end result of various pathogenically relevant processes (e.g., ischemia, neurohormonal activation, inflammation, oxidative/nitrosative stress, mechanical stress, pressure overload) (2, 119). Consequences of cardiomyocyte death include fibrosis, contractile and diastolic dysfunction, and potentially arrhythmias (2, 119). Strategies aimed at decreasing cardiomyocyte death may prevent the transition from adaptive to maladaptive remodeling and may improve outcomes in RVF.
Current state of knowledge
The predominant type of cell death in the RV is considered to be apoptotic, affecting predominantly the cardiomyocyte (2, 119). Troponin levels are currently used for markers of myocyte damage and death (244). Apoptosis is assessed in animal studies by measuring abundance or activity of proapoptotic pathways (e.g., bax, caspase-3), terminal deoxynucleotidyl transferase dUTP nick-end labeling, and quantification of annexin V expression. In clinical studies, cell death is assessed indirectly via CMR or PET–computed tomography (using annexin-based probes) (225).
Current knowledge gaps
The role of cell death in RV cell types other than cardiomyocytes (e.g., cardiac ECs) remains unknown. Furthermore, the contribution of nonapoptotic types of cell death (e.g., autophagy, necroptosis [245–248]) is poorly defined. Uncertainty exists about the possible role of circulating progenitor cells and resident progenitor cells in modifying RV cell survival and death. The potential contributions of endoplasmic reticulum stress, mitophagy, as well as genetic and epigenetic contributors to RV cell death are unknown. Furthermore, the role of cell death in mediating transition from adaptive to maladaptive RV remodeling is unclear. Little is still known about the relevance of RV cell death in patients with PAH, as findings in autopsy series vary and are usually limited to patients with end-stage disease. It is unclear how representative animal models are of RV cell death, and differences between models have not been sufficiently characterized. Last, a better understanding of established and novel PAH therapies on RV cell death is needed.
Recommendations/pathway for progress
The role of cardiomyocyte or cardiac EC death as a driver from adaptive to maladaptive RV remodeling needs further study. In particular, more mechanistic studies in animal models and isolated RV cells focusing on initiators and modifiers of cell death of cardiomyocytes and other relevant cell types (e.g., cardiac ECs) and correlation of findings with human phenotypes will provide a better understanding of mechanisms of RV cell death. Studies of isolated cardiomyocytes and ECs (ideally from animal models of severe RVF and/or well-phenotyped human samples) would provide novel mechanistic insights in RV cell death initiation and progression. The contribution of endoplasmic reticulum stress, mitochondrial fusion and mitophagy (249), autophagy (245–247), and nonapoptotic types of cell death to RVF development requires further study. Identification and validation of cardiac troponins as markers of cardiomyocyte death (rather than damage) would move the field forward. Identification of novel targets and probes for apoptosis and cell death imaging will help study cell death in animals and in humans. Strategies and regulators listed in Table 6 also apply to the study of RV cell death.
Assessment of Inflammation
Rationale
Inflammation is an integral contributor to the development of both acute and chronic RVF (2, 95, 119, 229, 250). Strategies aimed at decreasing RV inflammation may prevent or delay the progression from adaptive to maladaptive RV remodeling and result in improved outcomes. Monitoring RV inflammation may serve as a “biomarker” of RV function and/or treatment responses.
Current state of knowledge
Inflammation, among other processes, likely contributes to RV fibrosis and contractile dysfunction. Influx of inflammatory cells and expression of proinflammatory cytokines and adhesion molecules is observed rapidly (within 2 h) after onset of RVPO (96, 98, 250). For example, in animal models of PE, an influx of neutrophils and M1 macrophages is seen in the RV outflow tract within 18 hours (95, 98, 250). On the other hand, 6 weeks after acute RVPO, secretory M2 macrophages predominate, likely contributing to RV repair processes (95). In chronic RVPO, abundant expression of proinflammatory cytokines is noted (223), although the degree of inflammation appears to be less in chronic RVF than in RVF from acute RVPO (96).
Current knowledge gaps
Whether inflammation is a cause or a consequence of RVF is unknown. Initiators of RV inflammation (e.g., ischemia, apoptosis, impaired efferocytosis, mitochondrial dysfunction, oxidative stress), and potential links between inflammation and fibrosis, apoptosis, and metabolic dysfunction need to be identified. Similarly, it is unknown whether a certain degree of inflammation is beneficial for repair (and if so, how much). In LV failure, distinct macrophage populations have been linked to adaptive and maladaptive responses (251); it is unclear whether such a dual macrophage function also plays a role in RVF. Detailed investigation in human RVs (especially from patients not in end-stage disease) are lacking. Mechanisms mediating regression of inflammation, and whether this translates into clinical improvement, are poorly understood. Last, a better understanding of effects of established and novel PAH therapies as well as specific antiinflammatory strategies (e.g., ketorolac [250]) on acute and chronic RV inflammation is needed.
Recommendations/pathway for progress
Further characterization of inflammatory processes in the RV using biopsy (222) and novel imaging approaches (225) targeting specific inflammatory mediators in various stages of RVF and in distinct PAH populations (e.g., idiopathic vs. scleroderma-associated) would provide a better understanding of the role of inflammation in RVF. Preclinical mechanistic loss- or gain-of-function studies focused on individual cell types, mediators, and signaling pathways would provide a better understanding of the inflammatory contribution to RVF. Studying isolated cardiomyocytes and other relevant cell types (e.g., cardiac ECs and fibroblasts) will provide novel mechanistic insights into inflammatory signaling, especially if the proinflammatory environment of the failing RV can be recapitulated in vitro. Identification of mediators of inflammation development and regression and correlation of findings with human phenotypes will provide a better understanding of mechanisms of RV inflammation. Human samples, stereology, biomarkers, progenitor cells, sex and age, and sequencing techniques should be studied as outlined in Table 6.
Assessment of Oxidative Stress
Rationale
Oxidative stress is a purported contributor to RV dysfunction, providing a strong rationale for studying the oxidant/antioxidant imbalance of the stressed myocardium in both acute and chronically failing RV tissue. Please see the online supplement for detailed discussion of this topic.
Assessment of Contractile Signaling and Calcium Handling
Rationale
The RV in PAH is characterized by hypertrophy and both systolic and diastolic dysfunction (182). Perturbations in calcium handling have been implicated in all of these processes. A better understanding of calcium signaling in the failing RV may lead to novel diagnostic and/or therapeutic interventions.
Current state of knowledge
The RV in PAH exhibits changes in both the passive and active portions of the contractile apparatus. Sarcomere stiffening was identified in isolated RV cardiomyocytes (182). Both increased collagen accumulation and intrinsic stiffening of RV cardiomyocyte sarcomeres contribute to RV myocardial stiffness. In mild RVF, increased myofibril stiffness predominantly contributes to myocardial stiffening, whereas in severe RVF, both myofibril- and fibrosis (collagen)-mediated stiffness contribute to increased RV myocardial stiffness (252). Sarcomere stiffening and RV diastolic dysfunction is caused by titin hypophosphorylation (182). In addition, there is dysfunction of active contractile regulator mechanisms. Downregulation of SERCA2a (sarcoplasmic reticulum Ca2 +-ATPase 2a) appears to play a critical role in the pulmonary vasculature in PAH (253). Although less is known about calcium handling in RV myocytes, recent data from a pig pulmonary vein banding model demonstrated downregulation of SERCA2a and endoplasmic reticulum stress (88). In a recent study, intracellular calcium recycling appeared similar to normal LVs in patients with idiopathic PAH but was depressed in patients with scleroderma-PAH (167). A follow-up study using skinned cardiomyocytes obtained from RV biopsies revealed significant sarcomere dysfunction in patients in scleroderma-PAH (254). Apelin, a potent proangiogenic and procontractile peptide that exerts critical effects in the LV (255), may also be of importance in the RV (223, 256).
Current knowledge gaps
More insight is needed regarding mechanisms of calcium homeostasis in the RV myocyte. The occurrence, timing, and pathologic relevance of changes in SERCA2a during RVH in PAH is unknown. Although selective pulmonary SERCA2a gene transfer may offer benefit as a therapeutic intervention for the vascular bed in PAH (253), it is unknown if cardiac-targeted SERCA2a therapy, an approach that was (so far, unsuccessfully) taken to treat patients with LV failure (257), would be beneficial for the RV. The role of mitochondrial calcium handling has not been assessed in RVF; this may be important, as the influx of calcium via the mitochondrial calcium uniporter is a major regulator of both cytosolic calcium and the intramitochondrial calcium stores, which regulate key enzymes in oxidative metabolism (258). Effects of neurohormonal modulators (e.g., inhibitors of the renin-angiotensin/aldosterone system) and β-adrenergic receptor antagonists on RV contractile function require further study. In particular, the effect of the latter is of great interest, because currently available studies yielded conflicting results of these drugs on clinical outcomes and RV function (259–263). RV inotropic agents may improve short- and/or long-term outcomes in acute and/or chronic PH, but their role (and potential for adverse events) is incompletely explored.
Recommendations/pathway for progress
More studies of the mitochondrial calcium uniporter and sarcoplasmic reticulum calcium handling system in preclinical models and humans are required. Studies of active and passive mechanisms that control RV diastolic and systolic function likely will identify new insights. In addition to addressing changes in fibrosis (which determines passive stiffness), more study of calcium pumps, gap junctions, and ion channels (which determine active stiffness) in RV myocytes is required. More studies focusing on the regulation of SERCA2a in RVF are needed. Acute and chronic effects of renin-angiotensin/aldosterone system inhibitors and β-blockers on RV contractile function require further study. The role of therapies aimed at enhancing RV myocardial contractility (e.g., apelin and calcium-sensitizing agents) needs to be explored in preclinical and clinical studies. Studies in skinned RV cardiomyocytes may allow for deciphering mechanisms of RV dysfunction and guide targeted therapies. General recommendations from Table 6 also pertain to the study of calcium and contractile signaling.
Conclusions
This research statement delineates areas of established knowledge in the field of RVF, identifies and prioritizes the most pertinent research gaps (Table 7), and provides a prioritized pathway for addressing these preclinical and clinical questions. By combining basic, translational, and clinical approaches in an integrative and multidisciplinary manner, investigators will be able to further advance the state of knowledge, with the ultimate goal of developing RV-targeted therapies for patients with RVF of any etiology. Such therapies are anticipated to prevent or reverse the progression from adaptive to maladaptive RV remodeling.
Table 7.
Research Priorities to Be Addressed in the Next 5 Years
| 1. Understand the mechanisms underlying adaptive vs. maladaptive RV adaptation to pulmonary vascular load, including role of fibrosis, angiogenesis, metabolic shifts |
| 2. Develop a series of plasma and/or imaging biomarkers (by echocardiography and CMR) that could be used to accurately evaluate RV function, perfusion, and RV–PA coupling and as endpoints in clinical trials |
| 3. Develop and validate or improve on current animal models of RV dysfunction in the setting of increased pulmonary vascular load |
| 4. Develop therapies aimed at targeting RV myocardial contractility (e.g., calcium-sensitizing agents targeting sarcoplasmic reticulum and/or sarcomere function) |
Definition of abbreviations: CMR = cardiac magnetic resonance imaging; PA = pulmonary artery; RV = right ventricular.
The list was generated by surveying working group members to identify their top five priorities. The most commonly mentioned topics and themes are included in the table.
Acknowledgments
This official statement was prepared by an ad hoc subcommittee of the ATS Assembly on Pulmonary Circulation.
Members of the subcommittee are as follows:
Tim Lahm, M.D. (Co-Chair)*
Paul M. Hassoun, M.D. (Co-Chair)*
Stephen L. Archer, M.D.
Harm J. Bogaard, M.D., Ph.D.
Naomi C. Chesler, Ph.D.
Ivor S. Douglas, M.D.*
Francois Haddad, M.D.
Anna R. Hemnes, M.D.
Steven M. Kawut, M.D.
Jeffrey A. Kline, M.D.
Todd M. Kolb, M.D., Ph.D.
Stephen C. Mathai, M.D., M.H.S.
Olaf Mercier, M.D., Ph.D.
Evangelos D. Michelakis, M.D.
Robert Naeije, M.D.
Rubin M. Tuder, M.D.
Corey E. Ventetuolo, M.D., M.S.
Antoine Vieillard-Baron, M.D., Ph.D.
Norbert F. Voelkel, M.D.
Anton Vonk-Noordegraaf, M.D., Ph.D.
*Steering committee member.
Acknowledgment
The authors thank Dr. Myriam Amsallem for her contributions to Figure 2B. They also thank the American Thoracic Society staff for their help in organizing working group meetings and conference calls, and Dr. Kevin Wilson for his guidance and advice.
Footnotes
This official research statement of the American Thoracic Society was approved May 2018
An Executive Summary of this document is available at http://www.atsjournals.org/doi/suppl/10.1164/rccm.201806-1160ST.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author Disclosures: T.L. served as a speaker for Bayer; served as a consultant for Actelion and Gilead; received research support from Eli Lilly, Gilead, and Pfizer; and served on an advisory committee for Gilead. I.S.D. served on an advisory committee for Accelerate Diagnostics. A.R.H. served as a consultant for Bayer, Actelion, United Therapeutics, and GlaxoSmithKline; served on an advisory committee for Actelion and United Therapeutics; received research support from United Therapeutics; and provided expert testimony for Pfizer. S.M.K. received travel support from Actelion, Bayer, Gilead, Lung Biotech, Mallinckrodt, and United Therapeutics. J.A.K. received research support from Ikaria, Janssen, and Pfizer; has a patent pending on fibrinolysis technology; and served on a steering committee for a clinical trial with Janssen and Bayer. S.C.M. served as a consultant for Bayer, Actelion, and Gilead; served on an advisory committee for Actelion; and received personal fees from United Therapeutics. E.D.M. served on an advisory committee for Medtelligence; and his institution served as a site for clinical trials for Bayer, Bellerophon, and United Therapeutics. C.E.V. served as a consultant for Acceleron, Bayer, United Therapeutics, and Maquet; received research support from Eiger, Actelion, and Pfizer; and served on an advisory committee for Actelion, Bayer, and United Therapeutics. A.V.-B. received travel support from GE Healthcare; and received grants and personal fees from GlaxoSmithKline. N.F.V. served as a consultant for Janssen and Actelion; and served on an advisory committee for Actelion. A.V.-N. served a speaker for Actelion and Merck Sharp & Dohme. P.M.H., S.L.A., H.J.B., N.C.C., F.H., T.M.K., O.M., R.N., and R.M.T. reported no relationships with relevant commercial interests.
Contributor Information
Collaborators: on behalf of the American Thoracic Society Assembly on Pulmonary Circulation
References
- 1.Voelkel NF, Quaife RA, Leinwand LA, Barst RJ, McGoon MD, Meldrum DR, et al. National Heart, Lung, and Blood Institute Working Group on Cellular and Molecular Mechanisms of Right Heart Failure. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114:1883–1891. doi: 10.1161/CIRCULATIONAHA.106.632208. [DOI] [PubMed] [Google Scholar]
- 2.Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62:D22–D33. doi: 10.1016/j.jacc.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 3.van de Veerdonk MC, Kind T, Marcus JT, Mauritz GJ, Heymans MW, Bogaard HJ, et al. Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol. 2011;58:2511–2519. doi: 10.1016/j.jacc.2011.06.068. [DOI] [PubMed] [Google Scholar]
- 4.Meyer P, Filippatos GS, Ahmed MI, Iskandrian AE, Bittner V, Perry GJ, et al. Effects of right ventricular ejection fraction on outcomes in chronic systolic heart failure. Circulation. 2010;121:252–258. doi: 10.1161/CIRCULATIONAHA.109.887570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riedel M, Stanek V, Widimsky J, Prerovsky I. Longterm follow-up of patients with pulmonary thromboembolism: late prognosis and evolution of hemodynamic and respiratory data. Chest. 1982;81:151–158. doi: 10.1378/chest.81.2.151. [DOI] [PubMed] [Google Scholar]
- 6.Mohammed SF, Hussain I, AbouEzzeddine OF, Takahama H, Kwon SH, Forfia P, et al. Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation. 2014;130:2310–2320. doi: 10.1161/CIRCULATIONAHA.113.008461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrison DA, Adcock K, Collins CM, Goldman S, Caldwell JH, Schwarz MI. Right ventricular dysfunction and the exercise limitation of chronic obstructive pulmonary disease. J Am Coll Cardiol. 1987;9:1219–1229. doi: 10.1016/s0735-1097(87)80459-x. [DOI] [PubMed] [Google Scholar]
- 8.Hyduk A, Croft JB, Ayala C, Zheng K, Zheng ZJ, Mensah GA. Pulmonary hypertension surveillance--United States, 1980-2002. MMWR Surveill Summ. 2005;54:1–28. [PubMed] [Google Scholar]
- 9.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. WRITING GROUP MEMBERS; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 10.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 11.Erzurum S, Rounds SI, Stevens T, Aldred M, Aliotta J, Archer SL, et al. Strategic plan for lung vascular research: an NHLBI-ORDR workshop report. Am J Respir Crit Care Med. 2010;182:1554–1562. doi: 10.1164/rccm.201006-0869WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dweik RA, Rounds S, Erzurum SC, Archer S, Fagan K, Hassoun PM, et al. ATS Committee on Pulmonary Hypertension Phenotypes. An official American Thoracic Society Statement: pulmonary hypertension phenotypes. Am J Respir Crit Care Med. 2014;189:345–355. doi: 10.1164/rccm.201311-1954ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117:1717–1731. doi: 10.1161/CIRCULATIONAHA.107.653584. [DOI] [PubMed] [Google Scholar]
- 14.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–1448. doi: 10.1161/CIRCULATIONAHA.107.653576. [DOI] [PubMed] [Google Scholar]
- 15.Sandstede J, Lipke C, Beer M, Hofmann S, Pabst T, Kenn W, et al. Age- and gender-specific differences in left and right ventricular cardiac function and mass determined by cine magnetic resonance imaging. Eur Radiol. 2000;10:438–442. doi: 10.1007/s003300050072. [DOI] [PubMed] [Google Scholar]
- 16.Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ. Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J. 2004;147:218–223. doi: 10.1016/j.ahj.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 17.Beygui F, Furber A, Delépine S, Helft G, Metzger J-P, Geslin P, et al. Routine breath-hold gradient echo MRI-derived right ventricular mass, volumes and function: accuracy, reproducibility and coherence study. Int J Cardiovasc Imaging. 2004;20:509–516. doi: 10.1007/s10554-004-1097-7. [DOI] [PubMed] [Google Scholar]
- 18.Kawut SM, Barr RG, Lima JAC, Praestgaard A, Johnson WC, Chahal H, et al. Right ventricular structure is associated with the risk of heart failure and cardiovascular death: the Multi-Ethnic Study of Atherosclerosis (MESA)--right ventricle study. Circulation. 2012;126:1681–1688. doi: 10.1161/CIRCULATIONAHA.112.095216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacobs W, van de Veerdonk MC, Trip P, de Man F, Heymans MW, Marcus JT, et al. The right ventricle explains sex differences in survival in idiopathic pulmonary arterial hypertension. Chest. 2014;145:1230–1236. doi: 10.1378/chest.13-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Wolferen SA, van de Veerdonk MC, Mauritz G-J, Jacobs W, Marcus JT, Marques KMJ, et al. Clinically significant change in stroke volume in pulmonary hypertension. Chest. 2011;139:1003–1009. doi: 10.1378/chest.10-1066. [DOI] [PubMed] [Google Scholar]
- 21.van Wolferen SA, Marcus JT, Boonstra A, Marques KM, Bronzwaer JG, Spreeuwenberg MD, et al. Prognostic value of right ventricular mass, volume, and function in idiopathic pulmonary arterial hypertension. Eur Heart J. 2007;28:1250–1257. doi: 10.1093/eurheartj/ehl477. [DOI] [PubMed] [Google Scholar]
- 22.Peacock AJ, Crawley S, McLure L, Blyth K, Vizza CD, Poscia R, et al. Changes in right ventricular function measured by cardiac magnetic resonance imaging in patients receiving pulmonary arterial hypertension-targeted therapy: the EURO-MR study. Circ Cardiovasc Imaging. 2014;7:107–114. doi: 10.1161/CIRCIMAGING.113.000629. [DOI] [PubMed] [Google Scholar]
- 23.Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006;174:1034–1041. doi: 10.1164/rccm.200604-547OC. [DOI] [PubMed] [Google Scholar]
- 24.Sachdev A, Villarraga HR, Frantz RP, McGoon MD, Hsiao JF, Maalouf JF, et al. Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest. 2011;139:1299–1309. doi: 10.1378/chest.10-2015. [DOI] [PubMed] [Google Scholar]
- 25.Hardegree EL, Sachdev A, Villarraga HR, Frantz RP, McGoon MD, Kushwaha SS, et al. Role of serial quantitative assessment of right ventricular function by strain in pulmonary arterial hypertension. Am J Cardiol. 2013;111:143–148. doi: 10.1016/j.amjcard.2012.08.061. [DOI] [PubMed] [Google Scholar]
- 26.Oikawa M, Kagaya Y, Otani H, Sakuma M, Demachi J, Suzuki J, et al. Increased [18F]fluorodeoxyglucose accumulation in right ventricular free wall in patients with pulmonary hypertension and the effect of epoprostenol. J Am Coll Cardiol. 2005;45:1849–1855. doi: 10.1016/j.jacc.2005.02.065. [DOI] [PubMed] [Google Scholar]
- 27.Can MM, Kaymaz C, Tanboga IH, Tokgoz HC, Canpolat N, Turkyilmaz E, et al. Increased right ventricular glucose metabolism in patients with pulmonary arterial hypertension. Clin Nucl Med. 2011;36:743–748. doi: 10.1097/RLU.0b013e3182177389. [DOI] [PubMed] [Google Scholar]
- 28.Kawut SM, Lima JAC, Barr RG, Chahal H, Jain A, Tandri H, et al. Sex and race differences in right ventricular structure and function: the multi-ethnic study of atherosclerosis-right ventricle study. Circulation. 2011;123:2542–2551. doi: 10.1161/CIRCULATIONAHA.110.985515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ventetuolo CE, Barr RG, Bluemke DA, Jain A, Delaney JA, Hundley WG, et al. Selective serotonin reuptake inhibitor use is associated with right ventricular structure and function: the MESA-right ventricle study. PLoS One. 2012;7:e30480. doi: 10.1371/journal.pone.0030480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ventetuolo CE, Ouyang P, Bluemke DA, Tandri H, Barr RG, Bagiella E, et al. Sex hormones are associated with right ventricular structure and function: the MESA-right ventricle study. Am J Respir Crit Care Med. 2011;183:659–667. doi: 10.1164/rccm.201007-1027OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aaron CP, Tandri H, Barr RG, Johnson WC, Bagiella E, Chahal H, et al. Physical activity and right ventricular structure and function: the MESA-Right Ventricle Study. Am J Respir Crit Care Med. 2011;183:396–404. doi: 10.1164/rccm.201003-0469OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foppa M, Arora G, Gona P, Ashrafi A, Salton CJ, Yeon SB, et al. Right ventricular volumes and systolic function by cardiac magnetic resonance and the impact of sex, age, and obesity in a longitudinally followed cohort free of pulmonary and cardiovascular disease: the Framingham Heart Study. Circ Cardiovasc Imaging. 2016;9:e003810. doi: 10.1161/CIRCIMAGING.115.003810. [DOI] [PubMed] [Google Scholar]
- 33.Hudsmith LE, Petersen SE, Francis JM, Robson MD, Neubauer S. Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J Cardiovasc Magn Reson. 2005;7:775–782. doi: 10.1080/10976640500295516. [DOI] [PubMed] [Google Scholar]
- 34.Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J. 2006;27:2879–2888. doi: 10.1093/eurheartj/ehl336. [DOI] [PubMed] [Google Scholar]
- 35.Alfakih K, Plein S, Thiele H, Jones T, Ridgway JP, Sivananthan MU. Normal human left and right ventricular dimensions for MRI as assessed by turbo gradient echo and steady-state free precession imaging sequences. J Magn Reson Imaging. 2003;17:323–329. doi: 10.1002/jmri.10262. [DOI] [PubMed] [Google Scholar]
- 36.Leary PJ, Kaufman JD, Barr RG, Bluemke DA, Curl CL, Hough CL, et al. Traffic-related air pollution and the right ventricle: the Multi-Ethnic Study of Atherosclerosis. Am J Respir Crit Care Med. 2014;189:1093–1100. doi: 10.1164/rccm.201312-2298OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Talwar A, Garcia JGN, Tsai H, Moreno M, Lahm T, Zamanian RT, et al. Pulmonary Circulation Assembly. Health disparities in patients with pulmonary arterial hypertension: a blueprint for action. An Official American Thoracic Society statement. Am J Respir Crit Care Med. 2017;196:e32–e47. doi: 10.1164/rccm.201709-1821ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lewandowski AJ, Bradlow WM, Augustine D, Davis EF, Francis J, Singhal A, et al. Right ventricular systolic dysfunction in young adults born preterm. Circulation. 2013;128:713–720. doi: 10.1161/CIRCULATIONAHA.113.002583. [DOI] [PubMed] [Google Scholar]
- 39.Goss KN, Cucci AR, Fisher AJ, Albrecht M, Frump A, Tursunova R, et al. Neonatal hyperoxic lung injury favorably alters adult right ventricular remodeling response to chronic hypoxia exposure. Am J Physiol Lung Cell Mol Physiol. 2015;308:L797–L806. doi: 10.1152/ajplung.00276.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goss KN, Kumari S, Tetri LH, Barton G, Braun RK, Hacker TA, et al. Postnatal hyperoxia exposure durably impairs right ventricular function and mitochondrial biogenesis. Am J Respir Cell Mol Biol. 2017;56:609–619. doi: 10.1165/rcmb.2016-0256OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fleming TR, DeMets DL. Surrogate end points in clinical trials: are we being misled? Ann Intern Med. 1996;125:605–613. doi: 10.7326/0003-4819-125-7-199610010-00011. [DOI] [PubMed] [Google Scholar]
- 42.Buyse M, Molenberghs G. Criteria for the validation of surrogate endpoints in randomized experiments. Biometrics. 1998;54:1014–1029. [PubMed] [Google Scholar]
- 43.Freedman LS, Graubard BI, Schatzkin A. Statistical validation of intermediate endpoints for chronic diseases. Stat Med. 1992;11:167–178. doi: 10.1002/sim.4780110204. [DOI] [PubMed] [Google Scholar]
- 44.Ventetuolo CE, Gabler NB, Fritz JS, Smith KA, Palevsky HI, Klinger JR, et al. Are hemodynamics surrogate end points in pulmonary arterial hypertension? Circulation. 2014;130:768–775. doi: 10.1161/CIRCULATIONAHA.114.009690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gabler NB, French B, Strom BL, Palevsky HI, Taichman DB, Kawut SM, et al. Validation of 6-minute walk distance as a surrogate end point in pulmonary arterial hypertension trials. Circulation. 2012;126:349–356. doi: 10.1161/CIRCULATIONAHA.112.105890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Savarese G, Musella F, D’Amore C, Losco T, Marciano C, Gargiulo P, et al. Haemodynamics, exercise capacity and clinical events in pulmonary arterial hypertension. Eur Respir J. 2013;42:414–424. doi: 10.1183/09031936.00123712. [DOI] [PubMed] [Google Scholar]
- 47.Savarese G, Paolillo S, Costanzo P, D’Amore C, Cecere M, Losco T, et al. Do changes of 6-minute walk distance predict clinical events in patients with pulmonary arterial hypertension? A meta-analysis of 22 randomized trials. J Am Coll Cardiol. 2012;60:1192–1201. doi: 10.1016/j.jacc.2012.01.083. [DOI] [PubMed] [Google Scholar]
- 48.Ventetuolo CE, Kawut SM. What’s the (end) point? Eur Respir J. 2015;45:853–854. doi: 10.1183/09031936.00191314. [DOI] [PubMed] [Google Scholar]
- 49.Fritz JS, Blair C, Oudiz RJ, Dufton C, Olschewski H, Despain D, et al. Baseline and follow-up 6-min walk distance and brain natriuretic peptide predict 2-year mortality in pulmonary arterial hypertension. Chest. 2013;143:315–323. doi: 10.1378/chest.12-0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vélez-Martínez M, Ayers C, Mishkin JD, Bartolome SB, García CK, Torres F, et al. Association of cardiac troponin I with disease severity and outcomes in patients with pulmonary hypertension. Am J Cardiol. 2013;111:1812–1817. doi: 10.1016/j.amjcard.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 51.Leary PJ, Kurtz CE, Hough CL, Waiss MP, Ralph DD, Sheehan FH. Three-dimensional analysis of right ventricular shape and function in pulmonary hypertension. Pulm Circ. 2012;2:34–40. doi: 10.4103/2045-8932.94828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ohyama Y, Ambale-Venkatesh B, Chamera E, Shehata ML, Corona-Villalobos CP, Zimmerman SL, et al. Comparison of strain measurement from multimodality tissue tracking with strain-encoding MRI and harmonic phase MRI in pulmonary hypertension. Int J Cardiol. 2015;182:342–348. doi: 10.1016/j.ijcard.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 53.Wilkins MR, Paul GA, Strange JW, Tunariu N, Gin-Sing W, Banya WA, et al. Sildenafil versus Endothelin Receptor Antagonist for Pulmonary Hypertension (SERAPH) study. Am J Respir Crit Care Med. 2005;171:1292–1297. doi: 10.1164/rccm.200410-1411OC. [DOI] [PubMed] [Google Scholar]
- 54.Chin KM, Kingman M, de Lemos JA, Warner JJ, Reimold S, Peshock R, et al. Changes in right ventricular structure and function assessed using cardiac magnetic resonance imaging in bosentan-treated patients with pulmonary arterial hypertension. Am J Cardiol. 2008;101:1669–1672. doi: 10.1016/j.amjcard.2008.01.055. [DOI] [PubMed] [Google Scholar]
- 55.Wilkins MR, Ali O, Bradlow W, Wharton J, Taegtmeyer A, Rhodes CJ, et al. Simvastatin Pulmonary Hypertension Trial (SiPHT) Study Group. Simvastatin as a treatment for pulmonary hypertension trial. Am J Respir Crit Care Med. 2010;181:1106–1113. doi: 10.1164/rccm.2009111-699OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hassoun PM, Zamanian RT, Damico R, Lechtzin N, Khair R, Kolb TM, et al. Ambrisentan and tadalafil up-front combination therapy in scleroderma-associated pulmonary arterial hypertension. Am J Respir Crit Care Med. 2015;192:1102–1110. doi: 10.1164/rccm.201507-1398OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mercurio V, Mukherjee M, Tedford RJ, Zamanian RT, Khair RM, Sato T, et al. Improvement in right ventricular strain with ambrisentan and tadalafil upfront therapy in scleroderma-associated pulmonary arterial hypertension. Am J Respir Crit Care Med. 2018;197:388–391. doi: 10.1164/rccm.201704-0789LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gan CT, Holverda S, Marcus JT, Paulus WJ, Marques KM, Bronzwaer JG, et al. Right ventricular diastolic dysfunction and the acute effects of sildenafil in pulmonary hypertension patients. Chest. 2007;132:11–17. doi: 10.1378/chest.06-1263. [DOI] [PubMed] [Google Scholar]
- 59.Rich S. The effects of vasodilators in pulmonary hypertension: pulmonary vascular or peripheral vascular? Circ Heart Fail. 2009;2:145–150. doi: 10.1161/CIRCHEARTFAILURE.108.805374. [DOI] [PubMed] [Google Scholar]
- 60.Addetia K, Bhave NM, Tabit CE, Gomberg-Maitland M, Freed BH, Dill KE, et al. Sample size and cost analysis for pulmonary arterial hypertension drug trials using various imaging modalities to assess right ventricular size and function end points. Circ Cardiovasc Imaging. 2014;7:115–124. doi: 10.1161/CIRCIMAGING.113.000932. [DOI] [PubMed] [Google Scholar]
- 61.Galiè N, Barberà JA, Frost AE, Ghofrani HA, Hoeper MM, McLaughlin VV, et al. AMBITION Investigators. Initial use of ambrisentan plus tadalafil in pulmonary arterial hypertension. N Engl J Med. 2015;373:834–844. doi: 10.1056/NEJMoa1413687. [DOI] [PubMed] [Google Scholar]
- 62.Pulido T, Adzerikho I, Channick RN, Delcroix M, Galiè N, Ghofrani HA, et al. SERAPHIN Investigators. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369:809–818. doi: 10.1056/NEJMoa1213917. [DOI] [PubMed] [Google Scholar]
- 63.Maarman G, Lecour S, Butrous G, Thienemann F, Sliwa K. A comprehensive review: the evolution of animal models in pulmonary hypertension research; are we there yet? Pulm Circ. 2013;3:739–756. doi: 10.1086/674770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stenmark KR, Meyrick B, Galie N, Mooi WJ, McMurtry IF. Animal models of pulmonary arterial hypertension: the hope for etiological discovery and pharmacological cure. Am J Physiol Lung Cell Mol Physiol. 2009;297:L1013–L1032. doi: 10.1152/ajplung.00217.2009. [DOI] [PubMed] [Google Scholar]
- 65.Bogaard HJ, Natarajan R, Henderson SC, Long CS, Kraskauskas D, Smithson L, et al. Chronic pulmonary artery pressure elevation is insufficient to explain right heart failure. Circulation. 2009;120:1951–1960. doi: 10.1161/CIRCULATIONAHA.109.883843. [DOI] [PubMed] [Google Scholar]
- 66.Kerbaul F, Brimioulle S, Rondelet B, Dewachter C, Hubloue I, Naeije R. How prostacyclin improves cardiac output in right heart failure in conjunction with pulmonary hypertension. Am J Respir Crit Care Med. 2007;175:846–850. doi: 10.1164/rccm.200611-1615OC. [DOI] [PubMed] [Google Scholar]
- 67.Bruns DR, Brown RD, Stenmark KR, Buttrick PM, Walker LA. Mitochondrial integrity in a neonatal bovine model of right ventricular dysfunction. Am J Physiol Lung Cell Mol Physiol. 2015;308:L158–L167. doi: 10.1152/ajplung.00270.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kitahori K, He H, Kawata M, Cowan DB, Friehs I, Del Nido PJ, et al. Development of left ventricular diastolic dysfunction with preservation of ejection fraction during progression of infant right ventricular hypertrophy. Circ Heart Fail. 2009;2:599–607. doi: 10.1161/CIRCHEARTFAILURE.109.862664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hemnes AR, Brittain EL, Trammell AW, Fessel JP, Austin ED, Penner N, et al. Evidence for right ventricular lipotoxicity in heritable pulmonary arterial hypertension. Am J Respir Crit Care Med. 2014;189:325–334. doi: 10.1164/rccm.201306-1086OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bonnet S, Provencher S, Guignabert C, Perros F, Boucherat O, Schermuly RT, et al. Translating research into improved patient care in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2017;195:583–595. doi: 10.1164/rccm.201607-1515PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nagendran J, Sutendra G, Paterson I, Champion HC, Webster L, Chiu B, et al. Endothelin axis is upregulated in human and rat right ventricular hypertrophy. Circ Res. 2013;112:347–354. doi: 10.1161/CIRCRESAHA.111.300448. [DOI] [PubMed] [Google Scholar]
- 72.Piao L, Fang YH, Cadete VJ, Wietholt C, Urboniene D, Toth PT, et al. The inhibition of pyruvate dehydrogenase kinase improves impaired cardiac function and electrical remodeling in two models of right ventricular hypertrophy: resuscitating the hibernating right ventricle. J Mol Med (Berl) 2010;88:47–60. doi: 10.1007/s00109-009-0524-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Neto-Neves EM, Frump AL, Vayl A, Kline JA, Lahm T. Isolated heart model demonstrates evidence of contractile and diastolic dysfunction in right ventricles from rats with sugen/hypoxia-induced pulmonary hypertension. Physiol Rep. 2017;5:e13438. doi: 10.14814/phy2.13438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Strange G, Playford D, Stewart S, Deague JA, Nelson H, Kent A, et al. Pulmonary hypertension: prevalence and mortality in the Armadale echocardiography cohort. Heart. 2012;98:1805–1811. doi: 10.1136/heartjnl-2012-301992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vachiéry JL, Adir Y, Barberà JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62:D100–D108. doi: 10.1016/j.jacc.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 76.Seeger W, Adir Y, Barberà JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension in chronic lung diseases. J Am Coll Cardiol. 2013;62:D109–D116. doi: 10.1016/j.jacc.2013.10.036. [DOI] [PubMed] [Google Scholar]
- 77.Walker LA, Walker JS, Glazier A, Brown DR, Stenmark KR, Buttrick PM. Biochemical and myofilament responses of the right ventricle to severe pulmonary hypertension. Am J Physiol Heart Circ Physiol. 2011;301:H832–H840. doi: 10.1152/ajpheart.00249.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bogaard HJ, Vonk Noordegraaf A, Voelkel NF.Right heart failure in chronic lung diseases and pulmonary arterial hypertension Crawford MH, DiMarco JP, Paulus WJ.Cardiology 3rd edSt. Louis: Elsevier; 20091159–1169 [Google Scholar]
- 79.Weissmann N, Lobo B, Pichl A, Parajuli N, Seimetz M, Puig-Pey R, et al. Stimulation of soluble guanylate cyclase prevents cigarette smoke-induced pulmonary hypertension and emphysema. Am J Respir Crit Care Med. 2014;189:1359–1373. doi: 10.1164/rccm.201311-2037OC. [DOI] [PubMed] [Google Scholar]
- 80.Kasahara Y, Tuder RM, Taraseviciene-Stewart L, Le Cras TD, Abman S, Hirth PK, et al. Inhibition of VEGF receptors causes lung cell apoptosis and emphysema. J Clin Invest. 2000;106:1311–1319. doi: 10.1172/JCI10259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Taraseviciene-Stewart L, Kasahara Y, Alger L, Hirth P, Mc Mahon G, Waltenberger J, et al. Inhibition of the VEGF receptor 2 combined with chronic hypoxia causes cell death-dependent pulmonary endothelial cell proliferation and severe pulmonary hypertension. FASEB J. 2001;15:427–438. doi: 10.1096/fj.00-0343com. [DOI] [PubMed] [Google Scholar]
- 82.Bryant AJ, Carrick RP, McConaha ME, Jones BR, Shay SD, Moore CS, et al. Endothelial HIF signaling regulates pulmonary fibrosis-associated pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2016;310:L249–L262. doi: 10.1152/ajplung.00258.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Farkas L, Farkas D, Ask K, Möller A, Gauldie J, Margetts P, et al. VEGF ameliorates pulmonary hypertension through inhibition of endothelial apoptosis in experimental lung fibrosis in rats. J Clin Invest. 2009;119:1298–1311. doi: 10.1172/JCI36136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Milano G, Raucci A, Scopece A, Daniele R, Guerrini U, Sironi L, et al. Doxorubicin and trastuzumab regimen induces biventricular failure in mice. J Am Soc Echocardiogr. 2014;27:568–579. doi: 10.1016/j.echo.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 85.Santamore WP, Lynch PR, Heckman JL, Bove AA, Meier GD. Left ventricular effects on right ventricular developed pressure. J Appl Physiol. 1976;41:925–930. doi: 10.1152/jappl.1976.41.6.925. [DOI] [PubMed] [Google Scholar]
- 86.Toldo S, Bogaard HJ, Van Tassell BW, Mezzaroma E, Seropian IM, Robati R, et al. Right ventricular dysfunction following acute myocardial infarction in the absence of pulmonary hypertension in the mouse. PLoS One. 2011;6:e18102. doi: 10.1371/journal.pone.0018102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chen Y, Guo H, Xu D, Xu X, Wang H, Hu X, et al. Left ventricular failure produces profound lung remodeling and pulmonary hypertension in mice: heart failure causes severe lung disease. Hypertension. 2012;59:1170–1178. doi: 10.1161/HYPERTENSIONAHA.111.186072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Aguero J, Ishikawa K, Hadri L, Santos-Gallego C, Fish K, Hammoudi N, et al. Characterization of right ventricular remodeling and failure in a chronic pulmonary hypertension model. Am J Physiol Heart Circ Physiol. 2014;307:H1204–H1215. doi: 10.1152/ajpheart.00246.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lai YC, Tabima DM, Dube JJ, Hughan KS, Vanderpool RR, Goncharov DA, et al. SIRT3-AMP-activated protein kinase activation by nitrite and metformin improves hyperglycemia and normalizes pulmonary hypertension associated with heart failure with preserved ejection fraction. Circulation. 2016;133:717–731. doi: 10.1161/CIRCULATIONAHA.115.018935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Meng Q, Lai YC, Kelly NJ, Bueno M, Baust JJ, Bachman TN, et al. Development of a mouse model of metabolic syndrome, pulmonary hypertension, and heart failure with preserved ejection fraction. Am J Respir Cell Mol Biol. 2017;56:497–505. doi: 10.1165/rcmb.2016-0177OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Smulders YM. Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. Cardiovasc Res. 2000;48:23–33. doi: 10.1016/s0008-6363(00)00168-1. [DOI] [PubMed] [Google Scholar]
- 92.Gold FL, Bache RJ. Transmural right ventricular blood flow during acute pulmonary artery hypertension in the sedated dog: evidence for subendocardial ischemia despite residual vasodilator reserve. Circ Res. 1982;51:196–204. doi: 10.1161/01.res.51.2.196. [DOI] [PubMed] [Google Scholar]
- 93.Sharma GV, Sasahara AA. Regional and transmural myocardial blood flow studies in experimental pulmonary embolism. Prog Cardiovasc Dis. 1974;17:191–198. doi: 10.1016/0033-0620(74)90043-7. [DOI] [PubMed] [Google Scholar]
- 94.Lahm T, McCaslin CA, Wozniak TC, Ghumman W, Fadl YY, Obeidat OS, et al. Medical and surgical treatment of acute right ventricular failure. J Am Coll Cardiol. 2010;56:1435–1446. doi: 10.1016/j.jacc.2010.05.046. [DOI] [PubMed] [Google Scholar]
- 95.Watts JA, Gellar MA, Obraztsova M, Kline JA, Zagorski J. Role of inflammation in right ventricular damage and repair following experimental pulmonary embolism in rats. Int J Exp Pathol. 2008;89:389–399. doi: 10.1111/j.1365-2613.2008.00610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Watts JA, Marchick MR, Kline JA. Right ventricular heart failure from pulmonary embolism: key distinctions from chronic pulmonary hypertension. J Card Fail. 2010;16:250–259. doi: 10.1016/j.cardfail.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 97.Iwadate K, Tanno K, Doi M, Takatori T, Ito Y. Two cases of right ventricular ischemic injury due to massive pulmonary embolism. Forensic Sci Int. 2001;116:189–195. doi: 10.1016/s0379-0738(00)00367-4. [DOI] [PubMed] [Google Scholar]
- 98.Watts JA, Zagorski J, Gellar MA, Stevinson BG, Kline JA. Cardiac inflammation contributes to right ventricular dysfunction following experimental pulmonary embolism in rats. J Mol Cell Cardiol. 2006;41:296–307. doi: 10.1016/j.yjmcc.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 99.Zagorski J, Obraztsova M, Gellar MA, Kline JA, Watts JA. Transcriptional changes in right ventricular tissues are enriched in the outflow tract compared with the apex during chronic pulmonary embolism in rats. Physiol Genomics. 2009;39:61–71. doi: 10.1152/physiolgenomics.00076.2009. [DOI] [PubMed] [Google Scholar]
- 100.Zagorski J, Gellar MA, Obraztsova M, Kline JA, Watts JA. Inhibition of CINC-1 decreases right ventricular damage caused by experimental pulmonary embolism in rats. J Immunol. 2007;179:7820–7826. doi: 10.4049/jimmunol.179.11.7820. [DOI] [PubMed] [Google Scholar]
- 101.Iwadate K, Doi M, Tanno K, Katsumura S, Ito H, Sato K, et al. Right ventricular damage due to pulmonary embolism: examination of the number of infiltrating macrophages. Forensic Sci Int. 2003;134:147–153. doi: 10.1016/s0379-0738(03)00138-5. [DOI] [PubMed] [Google Scholar]
- 102.Sullivan DM, Watts JA, Kline JA. Biventricular cardiac dysfunction after acute massive pulmonary embolism in the rat. J Appl Physiol (1985) 2001;90:1648–1656. doi: 10.1152/jappl.2001.90.5.1648. [DOI] [PubMed] [Google Scholar]
- 103.Gurudevan SV, Malouf PJ, Auger WR, Waltman TJ, Madani M, Raisinghani AB, et al. Abnormal left ventricular diastolic filling in chronic thromboembolic pulmonary hypertension: true diastolic dysfunction or left ventricular underfilling? J Am Coll Cardiol. 2007;49:1334–1339. doi: 10.1016/j.jacc.2007.01.028. [DOI] [PubMed] [Google Scholar]
- 104.Amà R, Leather HA, Segers P, Vandermeersch E, Wouters PF. Acute pulmonary hypertension causes depression of left ventricular contractility and relaxation. Eur J Anaesthesiol. 2006;23:824–831. doi: 10.1017/S0265021506000317. [DOI] [PubMed] [Google Scholar]
- 105.Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Thromboembolic Pulmonary Hypertension Study Group. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350:2257–2264. doi: 10.1056/NEJMoa032274. [DOI] [PubMed] [Google Scholar]
- 106.Mekontso Dessap A, Boissier F, Charron C, Bégot E, Repessé X, Legras A, et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42:862–870. doi: 10.1007/s00134-015-4141-2. [DOI] [PubMed] [Google Scholar]
- 107.Vieillard-Baron A, Matthay M, Teboul JL, Bein T, Schultz M, Magder S, et al. Experts’ opinion on management of hemodynamics in ARDS patients: focus on the effects of mechanical ventilation. Intensive Care Med. 2016;42:739–749. doi: 10.1007/s00134-016-4326-3. [DOI] [PubMed] [Google Scholar]
- 108.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 109.Vieillard-Baron A, Charron C, Caille V, Belliard G, Page B, Jardin F. Prone positioning unloads the right ventricle in severe ARDS. Chest. 2007;132:1440–1446. doi: 10.1378/chest.07-1013. [DOI] [PubMed] [Google Scholar]
- 110.Sista AK, Goldhaber SZ, Vedantham S, Kline JA, Kuo WT, Kahn SR, et al. Research priorities in submassive pulmonary embolism: proceedings from a multidisciplinary research consensus panel. J Vasc Interv Radiol. 2016;27:787–794. doi: 10.1016/j.jvir.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 111.Piao L, Fang YH, Parikh KS, Ryan JJ, D’Souza KM, Theccanat T, et al. GRK2-mediated inhibition of adrenergic and dopaminergic signaling in right ventricular hypertrophy: therapeutic implications in pulmonary hypertension. Circulation. 2012;126:2859–2869. doi: 10.1161/CIRCULATIONAHA.112.109868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Campo A, Mathai SC, Le Pavec J, Zaiman AL, Hummers LK, Boyce D, et al. Outcomes of hospitalisation for right heart failure in pulmonary arterial hypertension. Eur Respir J. 2011;38:359–367. doi: 10.1183/09031936.00148310. [DOI] [PubMed] [Google Scholar]
- 113.Neto-Neves EM, Brown MB, Zaretskaia MV, Rezania S, Goodwill AG, McCarthy BP, et al. Chronic embolic pulmonary hypertension caused by pulmonary embolism and vascular endothelial growth factor inhibition. Am J Pathol. 2017;187:700–712. doi: 10.1016/j.ajpath.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Noly PE, Guihaire J, Coblence M, Dorfmüller P, Fadel E, Mercier O. Chronic thromboembolic pulmonary hypertension and assessment of right ventricular function in the piglet. J Vis Exp. 2015;105:e53133. doi: 10.3791/53133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Guihaire J, Haddad F, Noly PE, Boulate D, Decante B, Dartevelle P, et al. Right ventricular reserve in a piglet model of chronic pulmonary hypertension. Eur Respir J. 2015;45:709–717. doi: 10.1183/09031936.00081314. [DOI] [PubMed] [Google Scholar]
- 116.Mekontso Dessap A, Voiriot G, Zhou T, Marcos E, Dudek SM, Jacobson JR, et al. Conflicting physiological and genomic cardiopulmonary effects of recruitment maneuvers in murine acute lung injury. Am J Respir Cell Mol Biol. 2012;46:541–550. doi: 10.1165/rcmb.2011-0306OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.van de Veerdonk MC, Bogaard HJ, Voelkel NF. The right ventricle and pulmonary hypertension. Heart Fail Rev. 2016;21:259–271. doi: 10.1007/s10741-016-9526-y. [DOI] [PubMed] [Google Scholar]
- 118.Ryan JJ, Archer SL. The right ventricle in pulmonary arterial hypertension: disorders of metabolism, angiogenesis and adrenergic signaling in right ventricular failure. Circ Res. 2014;115:176–188. doi: 10.1161/CIRCRESAHA.113.301129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bogaard HJ, Abe K, Vonk Noordegraaf A, Voelkel NF. The right ventricle under pressure: cellular and molecular mechanisms of right-heart failure in pulmonary hypertension. Chest. 2009;135:794–804. doi: 10.1378/chest.08-0492. [DOI] [PubMed] [Google Scholar]
- 120.Drake JI, Bogaard HJ, Mizuno S, Clifton B, Xie B, Gao Y, et al. Molecular signature of a right heart failure program in chronic severe pulmonary hypertension. Am J Respir Cell Mol Biol. 2011;45:1239–1247. doi: 10.1165/rcmb.2010-0412OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vogel-Claussen J, Skrok J, Shehata ML, Singh S, Sibley CT, Boyce DM, et al. Right and left ventricular myocardial perfusion reserves correlate with right ventricular function and pulmonary hemodynamics in patients with pulmonary arterial hypertension. Radiology. 2011;258:119–127. doi: 10.1148/radiol.10100725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Fang YH, Piao L, Hong Z, Toth PT, Marsboom G, Bache-Wiig P, et al. Therapeutic inhibition of fatty acid oxidation in right ventricular hypertrophy: exploiting Randle’s cycle. J Mol Med (Berl) 2012;90:31–43. doi: 10.1007/s00109-011-0804-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Piao L, Sidhu VK, Fang YH, Ryan JJ, Parikh KS, Hong Z, et al. FOXO1-mediated upregulation of pyruvate dehydrogenase kinase-4 (PDK4) decreases glucose oxidation and impairs right ventricular function in pulmonary hypertension: therapeutic benefits of dichloroacetate. J Mol Med (Berl) 2013;91:333–346. doi: 10.1007/s00109-012-0982-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Piao L, Fang YH, Parikh K, Ryan JJ, Toth PT, Archer SL. Cardiac glutaminolysis: a maladaptive cancer metabolism pathway in the right ventricle in pulmonary hypertension. J Mol Med (Berl) 2013;91:1185–1197. doi: 10.1007/s00109-013-1064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Helms CC, Marvel M, Zhao W, Stahle M, Vest R, Kato GJ, et al. Mechanisms of hemolysis-associated platelet activation. J Thromb Haemost. 2013;11:2148–2154. doi: 10.1111/jth.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kline JA, Marchick MR, Hogg MM. Reduction in plasma haptoglobin in humans with acute pulmonary embolism causing tricuspid regurgitation. J Thromb Haemost. 2009;7:1597–1599. doi: 10.1111/j.1538-7836.2009.03535.x. [DOI] [PubMed] [Google Scholar]
- 127.Insenser M, Montes-Nieto R, Martínez-García MA, Durán EF, Santiuste C, Gómez V, et al. Identification of reduced circulating haptoglobin concentration as a biomarker of the severity of pulmonary embolism: a nontargeted proteomic study. PLoS One. 2014;9:e100902. doi: 10.1371/journal.pone.0100902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Vonk Noordegraaf A, Westerhof BE, Westerhof N. The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol. 2017;69:236–243. doi: 10.1016/j.jacc.2016.10.047. [DOI] [PubMed] [Google Scholar]
- 129.Swift AJ, Capener D, Johns C, Hamilton N, Rothman A, Elliot C, et al. Magnetic resonance imaging in the prognostic evaluation of patients with pulmonary arterial hypertension. Am J Respir Crit Care Med. 2017;196:228–239. doi: 10.1164/rccm.201611-2365OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Haddad F, Spruijt OA, Denault AY, Mercier O, Brunner N, Furman D, et al. Right heart score for predicting outcome in idiopathic, familial, or drug- and toxin-associated pulmonary arterial hypertension. JACC Cardiovasc Imaging. 2015;8:627–638. doi: 10.1016/j.jcmg.2014.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fuster V, Steele PM, Edwards WD, Gersh BJ, McGoon MD, Frye RL. Primary pulmonary hypertension: natural history and the importance of thrombosis. Circulation. 1984;70:580–587. doi: 10.1161/01.cir.70.4.580. [DOI] [PubMed] [Google Scholar]
- 132.D’Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective registry. Ann Intern Med. 1991;115:343–349. doi: 10.7326/0003-4819-115-5-343. [DOI] [PubMed] [Google Scholar]
- 133.Sandoval J, Bauerle O, Palomar A, Gómez A, Martínez-Guerra ML, Beltrán M, et al. Survival in primary pulmonary hypertension: validation of a prognostic equation. Circulation. 1994;89:1733–1744. doi: 10.1161/01.cir.89.4.1733. [DOI] [PubMed] [Google Scholar]
- 134.McLaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation. 2002;106:1477–1482. doi: 10.1161/01.cir.0000029100.82385.58. [DOI] [PubMed] [Google Scholar]
- 135.Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation. 2010;122:156–163. doi: 10.1161/CIRCULATIONAHA.109.911818. [DOI] [PubMed] [Google Scholar]
- 136.Benza RL, Miller DP, Gomberg-Maitland M, Frantz RP, Foreman AJ, Coffey CS, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL) Circulation. 2010;122:164–172. doi: 10.1161/CIRCULATIONAHA.109.898122. [DOI] [PubMed] [Google Scholar]
- 137.Sitbon O, Humbert M, Nunes H, Parent F, Garcia G, Hervé P, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol. 2002;40:780–788. doi: 10.1016/s0735-1097(02)02012-0. [DOI] [PubMed] [Google Scholar]
- 138.Eysmann SB, Palevsky HI, Reichek N, Hackney K, Douglas PS. Two-dimensional and Doppler-echocardiographic and cardiac catheterization correlates of survival in primary pulmonary hypertension. Circulation. 1989;80:353–360. doi: 10.1161/01.cir.80.2.353. [DOI] [PubMed] [Google Scholar]
- 139.Raymond RJ, Hinderliter AL, Willis PW, Ralph D, Caldwell EJ, Williams W, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol. 2002;39:1214–1219. doi: 10.1016/s0735-1097(02)01744-8. [DOI] [PubMed] [Google Scholar]
- 140.Brierre G, Blot-Souletie N, Degano B, Têtu L, Bongard V, Carrié D. New echocardiographic prognostic factors for mortality in pulmonary arterial hypertension. Eur J Echocardiogr. 2010;11:516–522. doi: 10.1093/ejechocard/jeq011. [DOI] [PubMed] [Google Scholar]
- 141.Fine NM, Chen L, Bastiansen PM, Frantz RP, Pellikka PA, Oh JK, et al. Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging. 2013;6:711–721. doi: 10.1161/CIRCIMAGING.113.000640. [DOI] [PubMed] [Google Scholar]
- 142.Bustamante-Labarta M, Perrone S, De La Fuente RL, Stutzbach P, De La Hoz RP, Torino A, et al. Right atrial size and tricuspid regurgitation severity predict mortality or transplantation in primary pulmonary hypertension. J Am Soc Echocardiogr. 2002;15:1160–1164. doi: 10.1067/mje.2002.123962. [DOI] [PubMed] [Google Scholar]
- 143.Ghio S, Klersy C, Magrini G, D’Armini AM, Scelsi L, Raineri C, et al. Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol. 2010;140:272–278. doi: 10.1016/j.ijcard.2008.11.051. [DOI] [PubMed] [Google Scholar]
- 144.Ghio S, Pazzano AS, Klersy C, Scelsi L, Raineri C, Camporotondo R, et al. Clinical and prognostic relevance of echocardiographic evaluation of right ventricular geometry in patients with idiopathic pulmonary arterial hypertension. Am J Cardiol. 2011;107:628–632. doi: 10.1016/j.amjcard.2010.10.027. [DOI] [PubMed] [Google Scholar]
- 145.Utsunomiya H, Nakatani S, Nishihira M, Kanzaki H, Kyotani S, Nakanishi N, et al. Value of estimated right ventricular filling pressure in predicting cardiac events in chronic pulmonary arterial hypertension. J Am Soc Echocardiogr. 2009;22:1368–1374. doi: 10.1016/j.echo.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 146.Ameloot K, Palmers PJ, Vande Bruaene A, Gerits A, Budts W, Voigt JU, et al. Clinical value of echocardiographic Doppler-derived right ventricular dp/dt in patients with pulmonary arterial hypertension. Eur Heart J Cardiovasc Imaging. 2014;15:1411–1419. doi: 10.1093/ehjci/jeu134. [DOI] [PubMed] [Google Scholar]
- 147.Ernande L, Cottin V, Leroux PY, Girerd N, Huez S, Mulliez A, et al. Right isovolumic contraction velocity predicts survival in pulmonary hypertension. J Am Soc Echocardiogr. 2013;26:297–306. doi: 10.1016/j.echo.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 148.Haeck ML, Scherptong RW, Marsan NA, Holman ER, Schalij MJ, Bax JJ, et al. Prognostic value of right ventricular longitudinal peak systolic strain in patients with pulmonary hypertension. Circ Cardiovasc Imaging. 2012;5:628–636. doi: 10.1161/CIRCIMAGING.111.971465. [DOI] [PubMed] [Google Scholar]
- 149.Smith BC, Dobson G, Dawson D, Charalampopoulos A, Grapsa J, Nihoyannopoulos P. Three-dimensional speckle tracking of the right ventricle: toward optimal quantification of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol. 2014;64:41–51. doi: 10.1016/j.jacc.2014.01.084. [DOI] [PubMed] [Google Scholar]
- 150.Badagliacca R, Poscia R, Pezzuto B, Papa S, Gambardella C, Francone M, et al. Right ventricular dyssynchrony in idiopathic pulmonary arterial hypertension: determinants and impact on pump function. J Heart Lung Transplant. 2015;34:381–389. doi: 10.1016/j.healun.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 151.Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, Tajik AJ, et al. Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr. 1996;9:838–847. doi: 10.1016/s0894-7317(96)90476-9. [DOI] [PubMed] [Google Scholar]
- 152.Yeo TC, Dujardin KS, Tei C, Mahoney DW, McGoon MD, Seward JB. Value of a Doppler-derived index combining systolic and diastolic time intervals in predicting outcome in primary pulmonary hypertension. Am J Cardiol. 1998;81:1157–1161. doi: 10.1016/s0002-9149(98)00140-4. [DOI] [PubMed] [Google Scholar]
- 153.Grünig E, Tiede H, Enyimayew EO, Ehlken N, Seyfarth HJ, Bossone E, et al. Assessment and prognostic relevance of right ventricular contractile reserve in patients with severe pulmonary hypertension. Circulation. 2013;128:2005–2015. doi: 10.1161/CIRCULATIONAHA.113.001573. [DOI] [PubMed] [Google Scholar]
- 154.Moledina S, Pandya B, Bartsota M, Mortensen KH, McMillan M, Quyam S, et al. Prognostic significance of cardiac magnetic resonance imaging in children with pulmonary hypertension. Circ Cardiovasc Imaging. 2013;6:407–414. doi: 10.1161/CIRCIMAGING.112.000082. [DOI] [PubMed] [Google Scholar]
- 155.Yamada Y, Okuda S, Kataoka M, Tanimoto A, Tamura Y, Abe T, et al. Prognostic value of cardiac magnetic resonance imaging for idiopathic pulmonary arterial hypertension before initiating intravenous prostacyclin therapy. Circ J. 2012;76:1737–1743. doi: 10.1253/circj.cj-11-1237. [DOI] [PubMed] [Google Scholar]
- 156.Brewis MJ, Bellofiore A, Vanderpool RR, Chesler NC, Johnson MK, Naeije R, et al. Imaging right ventricular function to predict outcome in pulmonary arterial hypertension. Int J Cardiol. 2016;218:206–211. doi: 10.1016/j.ijcard.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Swift AJ, Rajaram S, Campbell MJ, Hurdman J, Thomas S, Capener D, et al. Prognostic value of cardiovascular magnetic resonance imaging measurements corrected for age and sex in idiopathic pulmonary arterial hypertension. Circ Cardiovasc Imaging. 2014;7:100–106. doi: 10.1161/CIRCIMAGING.113.000338. [DOI] [PubMed] [Google Scholar]
- 158.Freed BH, Gomberg-Maitland M, Chandra S, Mor-Avi V, Rich S, Archer SL, et al. Late gadolinium enhancement cardiovascular magnetic resonance predicts clinical worsening in patients with pulmonary hypertension. J Cardiovasc Magn Reson. 2012;14:11. doi: 10.1186/1532-429X-14-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Swift AJ, Rajaram S, Capener D, Elliot C, Condliffe R, Wild JM, et al. LGE patterns in pulmonary hypertension do not impact overall mortality. JACC Cardiovasc Imaging. 2014;7:1209–1217. doi: 10.1016/j.jcmg.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 160.Dawes TJW, de Marvao A, Shi W, Fletcher T, Watson GMJ, Wharton J, et al. Machine learning of three-dimensional right ventricular motion enables outcome prediction in pulmonary hypertension: a cardiac MR imaging study. Radiology. 2017;283:381–390. doi: 10.1148/radiol.2016161315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vonk-Noordegraaf A, Westerhof N. Describing right ventricular function. Eur Respir J. 2013;41:1419–1423. doi: 10.1183/09031936.00160712. [DOI] [PubMed] [Google Scholar]
- 162.Kussmaul WG, Noordergraaf A, Laskey WK. Right ventricular-pulmonary arterial interactions. Ann Biomed Eng. 1992;20:63–80. doi: 10.1007/BF02368506. [DOI] [PubMed] [Google Scholar]
- 163.Suga H, Sagawa K, Shoukas AA. Load independence of the instantaneous pressure-volume ratio of the canine left ventricle and effects of epinephrine and heart rate on the ratio. Circ Res. 1973;32:314–322. doi: 10.1161/01.res.32.3.314. [DOI] [PubMed] [Google Scholar]
- 164.Maughan WL, Shoukas AA, Sagawa K, Weisfeldt ML. Instantaneous pressure-volume relationship of the canine right ventricle. Circ Res. 1979;44:309–315. doi: 10.1161/01.res.44.3.309. [DOI] [PubMed] [Google Scholar]
- 165.Sagawa K, Maughan L, Suga H, Sunagawa K. Cardiac contraction and the pressure-volume relationship. New York: Oxford Unversity Press; 1988. [Google Scholar]
- 166.Spruijt OA, de Man FS, Groepenhoff H, Oosterveer F, Westerhof N, Vonk-Noordegraaf A, et al. The effects of exercise on right ventricular contractility and right ventricular-arterial coupling in pulmonary hypertension. Am J Respir Crit Care Med. 2015;191:1050–1057. doi: 10.1164/rccm.201412-2271OC. [DOI] [PubMed] [Google Scholar]
- 167.Hsu S, Houston BA, Tampakakis E, Bacher AC, Rhodes PS, Mathai SC, et al. Right ventricular functional reserve in pulmonary arterial hypertension. Circulation. 2016;133:2413–2422. doi: 10.1161/CIRCULATIONAHA.116.022082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Fourie PR, Coetzee AR, Bolliger CT. Pulmonary artery compliance: its role in right ventricular-arterial coupling. Cardiovasc Res. 1992;26:839–844. doi: 10.1093/cvr/26.9.839. [DOI] [PubMed] [Google Scholar]
- 169.Ghuysen A, Lambermont B, Kolh P, Tchana-Sato V, Magis D, Gerard P, et al. Alteration of right ventricular-pulmonary vascular coupling in a porcine model of progressive pressure overloading. Shock. 2008;29:197–204. doi: 10.1097/SHK.0b013e318070c790. [DOI] [PubMed] [Google Scholar]
- 170.Tedford RJ, Mudd JO, Girgis RE, Mathai SC, Zaiman AL, Housten-Harris T, et al. Right ventricular dysfunction in systemic sclerosis-associated pulmonary arterial hypertension. Circ Heart Fail. 2013;6:953–963. doi: 10.1161/CIRCHEARTFAILURE.112.000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Mahapatra S, Nishimura RA, Oh JK, McGoon MD. The prognostic value of pulmonary vascular capacitance determined by Doppler echocardiography in patients with pulmonary arterial hypertension. J Am Soc Echocardiogr. 2006;19:1045–1050. doi: 10.1016/j.echo.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 172.Gan CT, Lankhaar JW, Westerhof N, Marcus JT, Becker A, Twisk JW, et al. Noninvasively assessed pulmonary artery stiffness predicts mortality in pulmonary arterial hypertension. Chest. 2007;132:1906–1912. doi: 10.1378/chest.07-1246. [DOI] [PubMed] [Google Scholar]
- 173.Tabima DM, Roldan-Alzate A, Wang Z, Hacker TA, Molthen RC, Chesler NC. Persistent vascular collagen accumulation alters hemodynamic recovery from chronic hypoxia. J Biomech. 2012;45:799–804. doi: 10.1016/j.jbiomech.2011.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ooi CY, Wang Z, Tabima DM, Eickhoff JC, Chesler NC. The role of collagen in extralobar pulmonary artery stiffening in response to hypoxia-induced pulmonary hypertension. Am J Physiol Heart Circ Physiol. 2010;299:H1823–H1831. doi: 10.1152/ajpheart.00493.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Stevens GR, Garcia-Alvarez A, Sahni S, Garcia MJ, Fuster V, Sanz J. RV dysfunction in pulmonary hypertension is independently related to pulmonary artery stiffness. JACC Cardiovasc Imaging. 2012;5:378–387. doi: 10.1016/j.jcmg.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 176.Brimioulle S, Wauthy P, Ewalenko P, Rondelet B, Vermeulen F, Kerbaul F, et al. Single-beat estimation of right ventricular end-systolic pressure-volume relationship. Am J Physiol Heart Circ Physiol. 2003;284:H1625–H1630. doi: 10.1152/ajpheart.01023.2002. [DOI] [PubMed] [Google Scholar]
- 177.Kuehne T, Yilmaz S, Steendijk P, Moore P, Groenink M, Saaed M, et al. Magnetic resonance imaging analysis of right ventricular pressure-volume loops: in vivo validation and clinical application in patients with pulmonary hypertension. Circulation. 2004;110:2010–2016. doi: 10.1161/01.CIR.0000143138.02493.DD. [DOI] [PubMed] [Google Scholar]
- 178.Wauthy P, Naeije R, Brimioulle S. Left and right ventriculo-arterial coupling in a patient with congenitally corrected transposition. Cardiol Young. 2005;15:647–649. doi: 10.1017/S1047951105001848. [DOI] [PubMed] [Google Scholar]
- 179.McCabe C, White PA, Hoole SP, Axell RG, Priest AN, Gopalan D, et al. Right ventricular dysfunction in chronic thromboembolic obstruction of the pulmonary artery: a pressure-volume study using the conductance catheter. J Appl Physiol (1985) 2014;116:355–363. doi: 10.1152/japplphysiol.01123.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sanz J, García-Alvarez A, Fernández-Friera L, Nair A, Mirelis JG, Sawit ST, et al. Right ventriculo-arterial coupling in pulmonary hypertension: a magnetic resonance study. Heart. 2012;98:238–243. doi: 10.1136/heartjnl-2011-300462. [DOI] [PubMed] [Google Scholar]
- 181.Trip P, Kind T, van de Veerdonk MC, Marcus JT, de Man FS, Westerhof N, et al. Accurate assessment of load-independent right ventricular systolic function in patients with pulmonary hypertension. J Heart Lung Transplant. 2013;32:50–55. doi: 10.1016/j.healun.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 182.Rain S, Handoko ML, Trip P, Gan CT, Westerhof N, Stienen GJ, et al. Right ventricular diastolic impairment in patients with pulmonary arterial hypertension. Circulation. 2013;128:2016–2025. doi: 10.1161/CIRCULATIONAHA.113.001873. [DOI] [PubMed] [Google Scholar]
- 183.Trip P, Rain S, Handoko ML, van der Bruggen C, Bogaard HJ, Marcus JT, et al. Clinical relevance of right ventricular diastolic stiffness in pulmonary hypertension. Eur Respir J. 2015;45:1603–1612. doi: 10.1183/09031936.00156714. [DOI] [PubMed] [Google Scholar]
- 184.Vanderpool RR, Pinsky MR, Naeije R, Deible C, Kosaraju V, Bunner C, et al. RV-pulmonary arterial coupling predicts outcome in patients referred for pulmonary hypertension. Heart. 2015;101:37–43. doi: 10.1136/heartjnl-2014-306142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Santamore WP, Dell’Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis. 1998;40:289–308. doi: 10.1016/s0033-0620(98)80049-2. [DOI] [PubMed] [Google Scholar]
- 186.Lazar JM, Flores AR, Grandis DJ, Orie JE, Schulman DS. Effects of chronic right ventricular pressure overload on left ventricular diastolic function. Am J Cardiol. 1993;72:1179–1182. doi: 10.1016/0002-9149(93)90990-t. [DOI] [PubMed] [Google Scholar]
- 187.Belenkie I, Horne SG, Dani R, Smith ER, Tyberg JV. Effects of aortic constriction during experimental acute right ventricular pressure loading: further insights into diastolic and systolic ventricular interaction. Circulation. 1995;92:546–554. doi: 10.1161/01.cir.92.3.546. [DOI] [PubMed] [Google Scholar]
- 188.van Wolferen SA, Marcus JT, Westerhof N, Spreeuwenberg MD, Marques KM, Bronzwaer JG, et al. Right coronary artery flow impairment in patients with pulmonary hypertension. Eur Heart J. 2008;29:120–127. doi: 10.1093/eurheartj/ehm567. [DOI] [PubMed] [Google Scholar]
- 189.Marcus JT, Gan CT, Zwanenburg JJ, Boonstra A, Allaart CP, Götte MJ, et al. Interventricular mechanical asynchrony in pulmonary arterial hypertension: left-to-right delay in peak shortening is related to right ventricular overload and left ventricular underfilling. J Am Coll Cardiol. 2008;51:750–757. doi: 10.1016/j.jacc.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 190.Rich JD, Thenappan T, Freed B, Patel AR, Thisted RA, Childers R, et al. QTc prolongation is associated with impaired right ventricular function and predicts mortality in pulmonary hypertension. Int J Cardiol. 2013;167:669–676. doi: 10.1016/j.ijcard.2012.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.van der Bruggen CE, Happé CM, Dorfmüller P, Trip P, Spruijt OA, Rol N, et al. Bone morphogenetic protein receptor type 2 mutation in pulmonary arterial hypertension: a view on the right ventricle. Circulation. 2016;133:1747–1760. doi: 10.1161/CIRCULATIONAHA.115.020696. [DOI] [PubMed] [Google Scholar]
- 192.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Oka T, Akazawa H, Naito AT, Komuro I. Angiogenesis and cardiac hypertrophy: maintenance of cardiac function and causative roles in heart failure. Circ Res. 2014;114:565–571. doi: 10.1161/CIRCRESAHA.114.300507. [DOI] [PubMed] [Google Scholar]
- 194.Walsh K, Shiojima I. Cardiac growth and angiogenesis coordinated by intertissue interactions. J Clin Invest. 2007;117:3176–3179. doi: 10.1172/JCI34126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Heineke J, Auger-Messier M, Xu J, Oka T, Sargent MA, York A, et al. Cardiomyocyte GATA4 functions as a stress-responsive regulator of angiogenesis in the murine heart. J Clin Invest. 2007;117:3198–3210. doi: 10.1172/JCI32573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Shiojima I, Sato K, Izumiya Y, Schiekofer S, Ito M, Liao R, et al. Disruption of coordinated cardiac hypertrophy and angiogenesis contributes to the transition to heart failure. J Clin Invest. 2005;115:2108–2118. doi: 10.1172/JCI24682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Jaba IM, Zhuang ZW, Li N, Jiang Y, Martin KA, Sinusas AJ, et al. NO triggers RGS4 degradation to coordinate angiogenesis and cardiomyocyte growth. J Clin Invest. 2013;123:1718–1731. doi: 10.1172/JCI65112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Tirziu D, Chorianopoulos E, Moodie KL, Palac RT, Zhuang ZW, Tjwa M, et al. Myocardial hypertrophy in the absence of external stimuli is induced by angiogenesis in mice. J Clin Invest. 2007;117:3188–3197. doi: 10.1172/JCI32024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zong P, Tune JD, Downey HF. Mechanisms of oxygen demand/supply balance in the right ventricle. Exp Biol Med (Maywood) 2005;230:507–519. doi: 10.1177/153537020523000801. [DOI] [PubMed] [Google Scholar]
- 200.Frump AL, Bonnet S, de Jesus Perez VA, Lahm T. The emerging role of angiogenesis in adaptive and maladaptive right ventricular remodeling in pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2018;314:L443–L460. doi: 10.1152/ajplung.00374.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hudlicka O, Brown M, Egginton S. Angiogenesis in skeletal and cardiac muscle. Physiol Rev. 1992;72:369–417. doi: 10.1152/physrev.1992.72.2.369. [DOI] [PubMed] [Google Scholar]
- 202.Kaneko N, Matsuda R, Toda M, Shimamoto K. Three-dimensional reconstruction of the human capillary network and the intramyocardial micronecrosis. Am J Physiol Heart Circ Physiol. 2011;300:H754–H761. doi: 10.1152/ajpheart.00486.2010. [DOI] [PubMed] [Google Scholar]
- 203.Kayar SR, Banchero N. Myocardial capillarity in acclimation to hypoxia. Pflugers Arch. 1985;404:319–325. doi: 10.1007/BF00585342. [DOI] [PubMed] [Google Scholar]
- 204.Miller AT, Jr, Hale DM. Increased vascularity of brain, heart, and skeletal muscle of polycythemic rats. Am J Physiol. 1970;219:702–704. doi: 10.1152/ajplegacy.1970.219.3.702. [DOI] [PubMed] [Google Scholar]
- 205.Turek Z, Grandtner M, Kreuzer F. Cardiac hypertrophy, capillary and muscle fiber density, muscle fiber diameter, capillary radius and diffusion distance in the myocardium of growing rats adapted to a simulated altitude of 3500 m. Pflugers Arch. 1972;335:19–28. doi: 10.1007/BF00586932. [DOI] [PubMed] [Google Scholar]
- 206.Clark DR, Smith P. Capillary density and muscle fibre size in the hearts of rats subjected to stimulated high altitude. Cardiovasc Res. 1978;12:578–584. doi: 10.1093/cvr/12.10.578. [DOI] [PubMed] [Google Scholar]
- 207.Partovian C, Adnot S, Eddahibi S, Teiger E, Levame M, Dreyfus P, et al. Heart and lung VEGF mRNA expression in rats with monocrotaline- or hypoxia-induced pulmonary hypertension. Am J Physiol. 1998;275:H1948–H1956. doi: 10.1152/ajpheart.1998.275.6.H1948. [DOI] [PubMed] [Google Scholar]
- 208.Turek Z, Hoofd LJ, Ringnalda BE, Rakusan K. Myocardial capillarity of rats exposed to simulated high altitude. Adv Exp Med Biol. 1985;191:249–255. doi: 10.1007/978-1-4684-3291-6_25. [DOI] [PubMed] [Google Scholar]
- 209.Sutendra G, Dromparis P, Paulin R, Zervopoulos S, Haromy A, Nagendran J, et al. A metabolic remodeling in right ventricular hypertrophy is associated with decreased angiogenesis and a transition from a compensated to a decompensated state in pulmonary hypertension. J Mol Med (Berl) 2013;91:1315–1327. doi: 10.1007/s00109-013-1059-4. [DOI] [PubMed] [Google Scholar]
- 210.Gómez A, Bialostozky D, Zajarias A, Santos E, Palomar A, Martínez ML, et al. Right ventricular ischemia in patients with primary pulmonary hypertension. J Am Coll Cardiol. 2001;38:1137–1142. doi: 10.1016/s0735-1097(01)01496-6. [DOI] [PubMed] [Google Scholar]
- 211.Graham BB, Koyanagi D, Kandasamy B, Tuder RM. Right ventricle vasculature in human pulmonary hypertension assessed by stereology. Am J Respir Crit Care Med. 2017;196:1075–1077. doi: 10.1164/rccm.201702-0425LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Chen JX, Stinnett A. Disruption of Ang-1/Tie-2 signaling contributes to the impaired myocardial vascular maturation and angiogenesis in type II diabetic mice. Arterioscler Thromb Vasc Biol. 2008;28:1606–1613. doi: 10.1161/ATVBAHA.108.169235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Javan H, Szucsik AM, Li L, Schaaf CL, Salama ME, Selzman CH. Cardiomyocyte p65 nuclear factor-κB is necessary for compensatory adaptation to pressure overload. Circ Heart Fail. 2015;8:109–118. doi: 10.1161/CIRCHEARTFAILURE.114.001297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kan J, Guo W, Huang C, Bao G, Zhu Y, Zhu YZ. S-propargyl-cysteine, a novel water-soluble modulator of endogenous hydrogen sulfide, promotes angiogenesis through activation of signal transducer and activator of transcription 3. Antioxid Redox Signal. 2014;20:2303–2316. doi: 10.1089/ars.2013.5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Steagall RJ, Daniels CR, Dalal S, Joyner WL, Singh M, Singh K. Extracellular ubiquitin increases expression of angiogenic molecules and stimulates angiogenesis in cardiac microvascular endothelial cells. Microcirculation. 2014;21:324–332. doi: 10.1111/micc.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Valcarcel-Ares MN, Gautam T, Warrington JP, Bailey-Downs L, Sosnowska D, de Cabo R, et al. Disruption of Nrf2 signaling impairs angiogenic capacity of endothelial cells: implications for microvascular aging. J Gerontol A Biol Sci Med Sci. 2012;67:821–829. doi: 10.1093/gerona/glr229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Potus F, Ruffenach G, Dahou A, Thebault C, Breuils-Bonnet S, Tremblay È, et al. Downregulation of microRNA-126 contributes to the failing right ventricle in pulmonary arterial hypertension. Circulation. 2015;132:932–943. doi: 10.1161/CIRCULATIONAHA.115.016382. [DOI] [PubMed] [Google Scholar]
- 218.Damico R, Kolb TM, Valera L, Wang L, Housten T, Tedford RJ, et al. Serum endostatin is a genetically determined predictor of survival in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2015;191:208–218. doi: 10.1164/rccm.201409-1742OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Hoffmann J, Marsh LM, Pieper M, Stacher E, Ghanim B, Kovacs G, et al. Compartment-specific expression of collagens and their processing enzymes in intrapulmonary arteries of IPAH patients. Am J Physiol Lung Cell Mol Physiol. 2015;308:L1002–L1013. doi: 10.1152/ajplung.00383.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Al-Husseini A, Kraskauskas D, Mezzaroma E, Nordio A, Farkas D, Drake JI, et al. Vascular endothelial growth factor receptor 3 signaling contributes to angioobliterative pulmonary hypertension. Pulm Circ. 2015;5:101–116. doi: 10.1086/679704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Weibel ER, Hsia CC, Ochs M. How much is there really? Why stereology is essential in lung morphometry. J Appl Physiol (1985) 2007;102:459–467. doi: 10.1152/japplphysiol.00808.2006. [DOI] [PubMed] [Google Scholar]
- 222.Bradley SP, Auger WR, Moser KM, Fedullo PF, Channick RN, Bloor CM. Right ventricular pathology in chronic pulmonary hypertension. Am J Cardiol. 1996;78:584–587. doi: 10.1016/s0002-9149(96)00372-4. [DOI] [PubMed] [Google Scholar]
- 223.Frump AL, Goss KN, Vayl A, Albrecht M, Fisher A, Tursunova R, et al. Estradiol improves right ventricular function in rats with severe angioproliferative pulmonary hypertension: effects of endogenous and exogenous sex hormones. Am J Physiol Lung Cell Mol Physiol. 2015;308:L873–L890. doi: 10.1152/ajplung.00006.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Wehman B, Sharma S, Pietris N, Mishra R, Siddiqui OT, Bigham G, et al. Mesenchymal stem cells preserve neonatal right ventricular function in a porcine model of pressure overload. Am J Physiol Heart Circ Physiol. 2016;310:H1816–H1826. doi: 10.1152/ajpheart.00955.2015. [DOI] [PubMed] [Google Scholar]
- 225.Vonk Noordegraaf A, Haddad F, Bogaard HJ, Hassoun PM. Noninvasive imaging in the assessment of the cardiopulmonary vascular unit. Circulation. 2015;131:899–913. doi: 10.1161/CIRCULATIONAHA.114.006972. [DOI] [PubMed] [Google Scholar]
- 226.Sanz J, Dellegrottaglie S, Kariisa M, Sulica R, Poon M, O’Donnell TP, et al. Prevalence and correlates of septal delayed contrast enhancement in patients with pulmonary hypertension. Am J Cardiol. 2007;100:731–735. doi: 10.1016/j.amjcard.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 227.Spruijt OA, Vissers L, Bogaard HJ, Hofman MB, Vonk-Noordegraaf A, Marcus JT. Increased native T1-values at the interventricular insertion regions in precapillary pulmonary hypertension. Int J Cardiovasc Imaging. 2016;32:451–459. doi: 10.1007/s10554-015-0787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Liu H, Wu Y, Wang F, Liu Z. Molecular imaging of integrin αvβ6 expression in living subjects. Am J Nucl Med Mol Imaging. 2014;4:333–345. [PMC free article] [PubMed] [Google Scholar]
- 229.Ryan JJ, Archer SL. Emerging concepts in the molecular basis of pulmonary arterial hypertension: part I: metabolic plasticity and mitochondrial dynamics in the pulmonary circulation and right ventricle in pulmonary arterial hypertension. Circulation. 2015;131:1691–1702. doi: 10.1161/CIRCULATIONAHA.114.006979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease. Physiol Rev. 2010;90:207–258. doi: 10.1152/physrev.00015.2009. [DOI] [PubMed] [Google Scholar]
- 231.Piao L, Marsboom G, Archer SL. Mitochondrial metabolic adaptation in right ventricular hypertrophy and failure. J Mol Med (Berl) 2010;88:1011–1020. doi: 10.1007/s00109-010-0679-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Graham BB, Kumar R, Mickael C, Sanders L, Gebreab L, Huber KM, et al. Severe pulmonary hypertension is associated with altered right ventricle metabolic substrate uptake. Am J Physiol Lung Cell Mol Physiol. 2015;309:L435–L440. doi: 10.1152/ajplung.00169.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Archer SL, Marsboom G, Kim GH, Zhang HJ, Toth PT, Svensson EC, et al. Epigenetic attenuation of mitochondrial superoxide dismutase 2 in pulmonary arterial hypertension: a basis for excessive cell proliferation and a new therapeutic target. Circulation. 2010;121:2661–2671. doi: 10.1161/CIRCULATIONAHA.109.916098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Archer SL, Fang YH, Ryan JJ, Piao L. Metabolism and bioenergetics in the right ventricle and pulmonary vasculature in pulmonary hypertension. Pulm Circ. 2013;3:144–152. doi: 10.4103/2045-8932.109960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ohira H, deKemp R, Pena E, Davies RA, Stewart DJ, Chandy G, et al. Shifts in myocardial fatty acid and glucose metabolism in pulmonary arterial hypertension: a potential mechanism for a maladaptive right ventricular response. Eur Heart J Cardiovasc Imaging. 2016;17:1424–1431. doi: 10.1093/ehjci/jev136. [DOI] [PubMed] [Google Scholar]
- 236.Wong YY, Raijmakers P, van Campen J, van der Laarse WJ, Knaapen P, Lubberink M, et al. 11C-Acetate clearance as an index of oxygen consumption of the right myocardium in idiopathic pulmonary arterial hypertension: a validation study using 15O-labeled tracers and PET. J Nucl Med. 2013;54:1258–1262. doi: 10.2967/jnumed.112.115915. [DOI] [PubMed] [Google Scholar]
- 237.Fang W, Zhao L, Xiong CM, Ni XH, He ZX, He JG, et al. Comparison of 18F-FDG uptake by right ventricular myocardium in idiopathic pulmonary arterial hypertension and pulmonary arterial hypertension associated with congenital heart disease. Pulm Circ. 2012;2:365–372. doi: 10.4103/2045-8932.101651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Bokhari S, Raina A, Rosenweig EB, Schulze PC, Bokhari J, Einstein AJ, et al. PET imaging may provide a novel biomarker and understanding of right ventricular dysfunction in patients with idiopathic pulmonary arterial hypertension. Circ Cardiovasc Imaging. 2011;4:641–647. doi: 10.1161/CIRCIMAGING.110.963207. [DOI] [PubMed] [Google Scholar]
- 239.Sakao S, Miyauchi H, Voelkel NF, Sugiura T, Tanabe N, Kobayashi Y, et al. Increased right ventricular fatty acid accumulation in chronic thromboembolic pulmonary hypertension. Ann Am Thorac Soc. 2015;12:1465–1472. doi: 10.1513/AnnalsATS.201504-236LE. [DOI] [PubMed] [Google Scholar]
- 240.Urboniene D, Haber I, Fang YH, Thenappan T, Archer SL. Validation of high-resolution echocardiography and magnetic resonance imaging vs. high-fidelity catheterization in experimental pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2010;299:L401–L412. doi: 10.1152/ajplung.00114.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Malenfant S, Potus F, Mainguy V, Leblanc E, Malenfant M, Ribeiro F, et al. Impaired skeletal muscle oxygenation and exercise tolerance in pulmonary hypertension. Med Sci Sports Exerc. 2015;47:2273–2282. doi: 10.1249/MSS.0000000000000696. [DOI] [PubMed] [Google Scholar]
- 242.Malenfant S, Potus F, Fournier F, Breuils-Bonnet S, Pflieger A, Bourassa S, et al. Skeletal muscle proteomic signature and metabolic impairment in pulmonary hypertension. J Mol Med (Berl) 2015;93:573–584. doi: 10.1007/s00109-014-1244-0. [DOI] [PubMed] [Google Scholar]
- 243.Batt J, Ahmed SS, Correa J, Bain A, Granton J. Skeletal muscle dysfunction in idiopathic pulmonary arterial hypertension. Am J Respir Cell Mol Biol. 2014;50:74–86. doi: 10.1165/rcmb.2012-0506OC. [DOI] [PubMed] [Google Scholar]
- 244.Heresi GA, Tang WH, Aytekin M, Hammel J, Hazen SL, Dweik RA. Sensitive cardiac troponin I predicts poor outcomes in pulmonary arterial hypertension. Eur Respir J. 2012;39:939–944. doi: 10.1183/09031936.00067011. [DOI] [PubMed] [Google Scholar]
- 245.Gomez-Arroyo J, Sakagami M, Syed AA, Farkas L, Van Tassell B, Kraskauskas D, et al. Iloprost reverses established fibrosis in experimental right ventricular failure. Eur Respir J. 2015;45:449–462. doi: 10.1183/09031936.00188013. [DOI] [PubMed] [Google Scholar]
- 246.Lahm T, Frump AL, Albrecht ME, Fisher AJ, Cook TG, Jones TJ, et al. 17β-Estradiol mediates superior adaptation of right ventricular function to acute strenuous exercise in female rats with severe pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2016;311:L375–L388. doi: 10.1152/ajplung.00132.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Rawat DK, Alzoubi A, Gupte R, Chettimada S, Watanabe M, Kahn AG, et al. Increased reactive oxygen species, metabolic maladaptation, and autophagy contribute to pulmonary arterial hypertension-induced ventricular hypertrophy and diastolic heart failure. Hypertension. 2014;64:1266–1274. doi: 10.1161/HYPERTENSIONAHA.114.03261. [DOI] [PubMed] [Google Scholar]
- 248.Szobi A, Rajtik T, Carnicka S, Ravingerova T, Adameova A. Mitigation of postischemic cardiac contractile dysfunction by CaMKII inhibition: effects on programmed necrotic and apoptotic cell death. Mol Cell Biochem. 2014;388:269–276. doi: 10.1007/s11010-013-1918-x. [DOI] [PubMed] [Google Scholar]
- 249.Joshi SR, Dhagia V, Gairhe S, Edwards JG, McMurtry IF, Gupte SA. MicroRNA-140 is elevated and mitofusin-1 is downregulated in the right ventricle of the Sugen5416/hypoxia/normoxia model of pulmonary arterial hypertension. Am J Physiol Heart Circ Physiol. 2016;311:H689–H698. doi: 10.1152/ajpheart.00264.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Watts JA, Gellar MA, Stuart LK, Obraztsova M, Kline JA. Proinflammatory events in right ventricular damage during pulmonary embolism: effects of treatment with ketorolac in rats. J Cardiovasc Pharmacol. 2009;54:246–252. doi: 10.1097/FJC.0b013e3181b2b699. [DOI] [PubMed] [Google Scholar]
- 251.Lavine KJ, Epelman S, Uchida K, Weber KJ, Nichols CG, Schilling JD, et al. Distinct macrophage lineages contribute to disparate patterns of cardiac recovery and remodeling in the neonatal and adult heart Proc Natl Acad Sci USA 201411116029–16034.[Published erratum appears in Proc Natl Acad Sci USA 113:E1414.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Rain S, Andersen S, Najafi A, Gammelgaard Schultz J, da Silva Gonçalves Bós D, Handoko ML, et al. Right ventricular myocardial stiffness in experimental pulmonary arterial hypertension: relative contribution of fibrosis and myofibril stiffness. Circ Heart Fail. 2016;9:e002636. doi: 10.1161/CIRCHEARTFAILURE.115.002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Hadri L, Kratlian RG, Benard L, Maron BA, Dorfmüller P, Ladage D, et al. Therapeutic efficacy of AAV1.SERCA2a in monocrotaline-induced pulmonary arterial hypertension. Circulation. 2013;128:512–523. doi: 10.1161/CIRCULATIONAHA.113.001585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Hsu S, Kokkonen-Simon KM, Kirk JA, Kolb TM, Damico RL, Mathai SC, et al. Right ventricular myofilament functional differences in humans with systemic sclerosis-associated versus idiopathic pulmonary arterial hypertension. Circulation. 2018;137:2360–2370. doi: 10.1161/CIRCULATIONAHA.117.033147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Folino A, Montarolo PG, Samaja M, Rastaldo R. Effects of apelin on the cardiovascular system. Heart Fail Rev. 2015;20:505–518. doi: 10.1007/s10741-015-9475-x. [DOI] [PubMed] [Google Scholar]
- 256.Dai T, Ramirez-Correa G, Gao WD. Apelin increases contractility in failing cardiac muscle. Eur J Pharmacol. 2006;553:222–228. doi: 10.1016/j.ejphar.2006.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Greenberg B, Butler J, Felker GM, Ponikowski P, Voors AA, Desai AS, et al. Calcium upregulation by percutaneous administration of gene therapy in patients with cardiac disease (CUPID 2): a randomised, multinational, double-blind, placebo-controlled, phase 2b trial. Lancet. 2016;387:1178–1186. doi: 10.1016/S0140-6736(16)00082-9. [DOI] [PubMed] [Google Scholar]
- 258.Hong Z, Chen KH, DasGupta A, Potus F, Dunham-Snary K, Bonnet S, et al. MicroRNA-138 and microRNA-25 down-regulate mitochondrial calcium uniporter, causing the pulmonary arterial hypertension cancer phenotype Am J Respir Crit Care Med 2017195515–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Provencher S, Herve P, Jais X, Lebrec D, Humbert M, Simonneau G, et al. Deleterious effects of beta-blockers on exercise capacity and hemodynamics in patients with portopulmonary hypertension. Gastroenterology. 2006;130:120–126. doi: 10.1053/j.gastro.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 260.Grinnan D, Bogaard HJ, Grizzard J, Van Tassell B, Abbate A, DeWilde C, et al. Treatment of group I pulmonary arterial hypertension with carvedilol is safe. Am J Respir Crit Care Med. 2014;189:1562–1564. doi: 10.1164/rccm.201311-2025LE. [DOI] [PubMed] [Google Scholar]
- 261.van Campen JS, de Boer K, van de Veerdonk MC, van der Bruggen CE, Allaart CP, Raijmakers PG, et al. Bisoprolol in idiopathic pulmonary arterial hypertension: an explorative study. Eur Respir J. 2016;48:787–796. doi: 10.1183/13993003.00090-2016. [DOI] [PubMed] [Google Scholar]
- 262.Farha S, Saygin D, Park MM, Cheong HI, Asosingh K, Comhair SA, et al. Pulmonary arterial hypertension treatment with carvedilol for heart failure: a randomized controlled trial. JCI Insight. 2017;2:95240. doi: 10.1172/jci.insight.95240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Perros F, de Man FS, Bogaard HJ, Antigny F, Simonneau G, Bonnet S, et al. Use of β-blockers in pulmonary hypertension. Circ Heart Fail. 2017;10:e003703. doi: 10.1161/CIRCHEARTFAILURE.116.003703. [DOI] [PubMed] [Google Scholar]
- 264.Werchan PM, Summer WR, Gerdes AM, McDonough KH. Right ventricular performance after monocrotaline-induced pulmonary hypertension. Am J Physiol. 1989;256:H1328–H1336. doi: 10.1152/ajpheart.1989.256.5.H1328. [DOI] [PubMed] [Google Scholar]
- 265.Hessel MH, Steendijk P, den Adel B, Schutte CI, van der Laarse A. Characterization of right ventricular function after monocrotaline-induced pulmonary hypertension in the intact rat. Am J Physiol Heart Circ Physiol. 2006;291:H2424–H2430. doi: 10.1152/ajpheart.00369.2006. [DOI] [PubMed] [Google Scholar]
- 266.Schäfer S, Ellinghaus P, Janssen W, Kramer F, Lustig K, Milting H, et al. Chronic inhibition of phosphodiesterase 5 does not prevent pressure-overload-induced right-ventricular remodelling. Cardiovasc Res. 2009;82:30–39. doi: 10.1093/cvr/cvp002. [DOI] [PubMed] [Google Scholar]
- 267.Ostádal B, Urbanová D, Ressl J, Procházka J, Pelouch V, Widimský J. Changes of the right and left ventricles in rats exposed to intermittent high altitude hypoxia. Cor Vasa. 1981;23:111–120. [PubMed] [Google Scholar]
- 268.Sharma S, Taegtmeyer H, Adrogue J, Razeghi P, Sen S, Ngumbela K, et al. Dynamic changes of gene expression in hypoxia-induced right ventricular hypertrophy. Am J Physiol Heart Circ Physiol. 2004;286:H1185–H1192. doi: 10.1152/ajpheart.00916.2003. [DOI] [PubMed] [Google Scholar]
- 269.Gomez A, Mink S. Interaction between effects of hypoxia and hypercapnia on altering left ventricular relaxation and chamber stiffness in dogs. Am Rev Respir Dis. 1992;146:313–320. doi: 10.1164/ajrccm/146.2.313. [DOI] [PubMed] [Google Scholar]
- 270.Dias CA, Assad RS, Caneo LF, Abduch MC, Aiello VD, Dias AR, et al. Reversible pulmonary trunk banding: II. An experimental model for rapid pulmonary ventricular hypertrophy. J Thorac Cardiovasc Surg. 2002;124:999–1006. doi: 10.1067/mtc.2002.124234. [DOI] [PubMed] [Google Scholar]
- 271.Akhavein F, St-Michel EJ, Seifert E, Rohlicek CV. Decreased left ventricular function, myocarditis, and coronary arteriolar medial thickening following monocrotaline administration in adult rats. J Appl Physiol (1985) 2007;103:287–295. doi: 10.1152/japplphysiol.01509.2005. [DOI] [PubMed] [Google Scholar]
- 272.Abe K, Toba M, Alzoubi A, Ito M, Fagan KA, Cool CD, et al. Formation of plexiform lesions in experimental severe pulmonary arterial hypertension. Circulation. 2010;121:2747–2754. doi: 10.1161/CIRCULATIONAHA.109.927681. [DOI] [PubMed] [Google Scholar]
- 273.Bogaard HJ, Natarajan R, Mizuno S, Abbate A, Chang PJ, Chau VQ, et al. Adrenergic receptor blockade reverses right heart remodeling and dysfunction in pulmonary hypertensive rats. Am J Respir Crit Care Med. 2010;182:652–660. doi: 10.1164/rccm.201003-0335OC. [DOI] [PubMed] [Google Scholar]
- 274.Gomez-Arroyo JG, Farkas L, Alhussaini AA, Farkas D, Kraskauskas D, Voelkel NF, et al. The monocrotaline model of pulmonary hypertension in perspective. Am J Physiol Lung Cell Mol Physiol. 2012;302:L363–L369. doi: 10.1152/ajplung.00212.2011. [DOI] [PubMed] [Google Scholar]
- 275.Gomez-Arroyo J, Saleem SJ, Mizuno S, Syed AA, Bogaard HJ, Abbate A, et al. A brief overview of mouse models of pulmonary arterial hypertension: problems and prospects. Am J Physiol Lung Cell Mol Physiol. 2012;302:L977–L991. doi: 10.1152/ajplung.00362.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Okada K, Tanaka Y, Bernstein M, Zhang W, Patterson GA, Botney MD. Pulmonary hemodynamics modify the rat pulmonary artery response to injury: a neointimal model of pulmonary hypertension. Am J Pathol. 1997;151:1019–1025. [PMC free article] [PubMed] [Google Scholar]
- 277.Gomez-Arroyo J, Mizuno S, Szczepanek K, Van Tassell B, Natarajan R, dos Remedios CG, et al. Metabolic gene remodeling and mitochondrial dysfunction in failing right ventricular hypertrophy secondary to pulmonary arterial hypertension. Circ Heart Fail. 2013;6:136–144. doi: 10.1161/CIRCHEARTFAILURE.111.966127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Lahm T, Tuder RM, Petrache I. Progress in solving the sex hormone paradox in pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2014;307:L7–L26. doi: 10.1152/ajplung.00337.2013. [DOI] [PubMed] [Google Scholar]
- 279.Brown MB, Chingombe TJ, Zinn AB, Reddy JG, Novack RA, Cooney SA, et al. Novel assessment of haemodynamic kinetics with acute exercise in a rat model of pulmonary arterial hypertension. Exp Physiol. 2015;100:742–754. doi: 10.1113/EP085182. [DOI] [PubMed] [Google Scholar]
- 280.Shiran H, Zamanian RT, McConnell MV, Liang DH, Dash R, Heidary S, et al. Relationship between echocardiographic and magnetic resonance derived measures of right ventricular size and function in patients with pulmonary hypertension. J Am Soc Echocardiogr. 2014;27:405–412. doi: 10.1016/j.echo.2013.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Sato T, Tsujino I, Ohira H, Oyama-Manabe N, Yamada A, Ito YM, et al. Validation study on the accuracy of echocardiographic measurements of right ventricular systolic function in pulmonary hypertension. J Am Soc Echocardiogr. 2012;25:280–286. doi: 10.1016/j.echo.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 282.Grapsa J, Pereira Nunes MC, Tan TC, Cabrita IZ, Coulter T, Smith BC, et al. Echocardiographic and hemodynamic predictors of survival in precapillary pulmonary hypertension: seven-year follow-up. Circ Cardiovasc Imaging. 2015;8:e002107. doi: 10.1161/CIRCIMAGING.114.002107. [DOI] [PubMed] [Google Scholar]
- 283.Badagliacca R, Reali M, Poscia R, Pezzuto B, Papa S, Mezzapesa M, et al. Right intraventricular dyssynchrony in idiopathic, heritable, and anorexigen-induced pulmonary arterial hypertension: clinical impact and reversibility. JACC Cardiovasc Imaging. 2015;8:642–652. doi: 10.1016/j.jcmg.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 284.Mauritz GJ, Kind T, Marcus JT, Bogaard HJ, van de Veerdonk M, Postmus PE, et al. Progressive changes in right ventricular geometric shortening and long-term survival in pulmonary arterial hypertension. Chest. 2012;141:935–943. doi: 10.1378/chest.10-3277. [DOI] [PubMed] [Google Scholar]
- 285.Spruijt OA, Di Pasqua MC, Bogaard HJ, van der Bruggen CE, Oosterveer F, Marcus JT, et al. Serial assessment of right ventricular systolic function in patients with precapillary pulmonary hypertension using simple echocardiographic parameters: a comparison with cardiac magnetic resonance imaging. J Cardiol. 2017;69:182–188. doi: 10.1016/j.jjcc.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 286.Kind T, Mauritz GJ, Marcus JT, van de Veerdonk M, Westerhof N, Vonk-Noordegraaf A. Right ventricular ejection fraction is better reflected by transverse rather than longitudinal wall motion in pulmonary hypertension. J Cardiovasc Magn Reson. 2010;12:35. doi: 10.1186/1532-429X-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Okumura K, Humpl T, Dragulescu A, Mertens L, Friedberg MK. Longitudinal assessment of right ventricular myocardial strain in relation to transplant-free survival in children with idiopathic pulmonary hypertension. J Am Soc Echocardiogr. 2014;27:1344–1351. doi: 10.1016/j.echo.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 288.Mukherjee M, Mercurio V, Tedford RJ, Shah AA, Hsu S, Mullin CJ, et al. Right ventricular longitudinal strain is diminished in systemic sclerosis compared with idiopathic pulmonary arterial hypertension. Eur Respir J. 2017;50:1701436. doi: 10.1183/13993003.01436-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Bradlow WM, Hughes ML, Keenan NG, Bucciarelli-Ducci C, Assomull R, Gibbs JS, et al. Measuring the heart in pulmonary arterial hypertension (PAH): implications for trial study size. J Magn Reson Imaging. 2010;31:117–124. doi: 10.1002/jmri.22011. [DOI] [PubMed] [Google Scholar]
- 290.Grapsa J, O’Regan DP, Pavlopoulos H, Durighel G, Dawson D, Nihoyannopoulos P. Right ventricular remodelling in pulmonary arterial hypertension with three-dimensional echocardiography: comparison with cardiac magnetic resonance imaging. Eur J Echocardiogr. 2010;11:64–73. doi: 10.1093/ejechocard/jep169. [DOI] [PubMed] [Google Scholar]
- 291.Niemann PS, Pinho L, Balbach T, Galuschky C, Blankenhagen M, Silberbach M, et al. Anatomically oriented right ventricular volume measurements with dynamic three-dimensional echocardiography validated by 3-Tesla magnetic resonance imaging. J Am Coll Cardiol. 2007;50:1668–1676. doi: 10.1016/j.jacc.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 292.Ostenfeld E, Carlsson M, Shahgaldi K, Roijer A, Holm J. Manual correction of semi-automatic three-dimensional echocardiography is needed for right ventricular assessment in adults; validation with cardiac magnetic resonance. Cardiovasc Ultrasound. 2012;10:1. doi: 10.1186/1476-7120-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Shimada YJ, Shiota M, Siegel RJ, Shiota T. Accuracy of right ventricular volumes and function determined by three-dimensional echocardiography in comparison with magnetic resonance imaging: a meta-analysis study. J Am Soc Echocardiogr. 2010;23:943–953. doi: 10.1016/j.echo.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 294.van der Zwaan HB, Geleijnse ML, McGhie JS, Boersma E, Helbing WA, Meijboom FJ, et al. Right ventricular quantification in clinical practice: two-dimensional vs. three-dimensional echocardiography compared with cardiac magnetic resonance imaging. Eur J Echocardiogr. 2011;12:656–664. doi: 10.1093/ejechocard/jer107. [DOI] [PubMed] [Google Scholar]
- 295.van de Veerdonk MC, Marcus JT, Westerhof N, de Man FS, Boonstra A, Heymans MW, et al. Signs of right ventricular deterioration in clinically stable patients with pulmonary arterial hypertension. Chest. 2015;147:1063–1071. doi: 10.1378/chest.14-0701. [DOI] [PubMed] [Google Scholar]
- 296.McCann GP, Gan CT, Beek AM, Niessen HW, Vonk Noordegraaf A, van Rossum AC. Extent of MRI delayed enhancement of myocardial mass is related to right ventricular dysfunction in pulmonary artery hypertension. AJR Am J Roentgenol. 2007;188:349–355. doi: 10.2214/AJR.05.1259. [DOI] [PubMed] [Google Scholar]
- 297.Reiter U, Reiter G, Kovacs G, Adelsmayr G, Greiser A, Olschewski H, et al. Native myocardial T1 mapping in pulmonary hypertension: correlations with cardiac function and hemodynamics. Eur Radiol. 2017;27:157–166. doi: 10.1007/s00330-016-4360-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 299.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810–1852. doi: 10.1161/CIR.0b013e31829e8807. [DOI] [PubMed] [Google Scholar]
- 300.Surie S, Bouma BJ, Bruin-Bon RA, Hardziyenka M, Kloek JJ, Van der Plas MN, et al. Time course of restoration of systolic and diastolic right ventricular function after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. Am Heart J. 2011;161:1046–1052. doi: 10.1016/j.ahj.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 301.Katz WE, Gasior TA, Quinlan JJ, Lazar JM, Firestone L, Griffith BP, et al. Immediate effects of lung transplantation on right ventricular morphology and function in patients with variable degrees of pulmonary hypertension. J Am Coll Cardiol. 1996;27:384–391. doi: 10.1016/0735-1097(95)00502-1. [DOI] [PubMed] [Google Scholar]
- 302.Austin ED, Kawut SM, Gladwin MT, Abman SH. Pulmonary hypertension: NHLBI workshop on the primary prevention of chronic lung diseases. Ann Am Thorac Soc. 2014;11:S178–S185. doi: 10.1513/AnnalsATS.201312-443LD. [DOI] [PMC free article] [PubMed] [Google Scholar]