Abstract
Background
Balloon pulmonary angioplasty (BPA) has been demonstrated to improve cardiac function and exercise capacity in patients with inoperable chronic thromboembolic pulmonary hypertension (CTEPH), but its instant impact on cardiopulmonary function has seldom been evaluated. This study aims to determine the safety and efficacy of BPA and its immediate and lasting effects on cardiopulmonary function among CTEPH patients.
Methods
From May 2018 to January 2019, patients with inoperable CTEPH who underwent BPA sessions were consecutively enrolled. Hemodynamics were measured by right heart catheterization, selective pulmonary angiography and BPA were successively conducted. Hemodynamic variables, WHO functional class (WHO-FC), 6-min walk distance (6MWD) and serum NT-proBNP were evaluated before and after BPA sessions during hospitalization. Pulmonary function testing (PFT) and cardiopulmonary exercise testing (CPET) were performed within 1–3 days pre and post BPA to evaluate the effect of BPA on cardiopulmonary function.
Results
Twenty-five patients with inoperable CTEPH who underwent a total of forty BPA sessions were consecutively enrolled. A total of 183 segmental or subsegmental vessels (4.6 ± 1.9 vessels per session) in 137 segments (3.4 ± 1.6 segments per session) were dilated. No procedure-related complications occurred. Instant hemodynamics, WHO-FC, 6MWD and NT-proBNP were all significantly improved after a single BPA session. Significant improvement in cardiopulmonary function was also evident as assessed by PFT indexes (forced vital capacity, forced expiratory volume in the first second, maximal voluntary ventilation) and CPET parameters (peak work rate, peak VO2, oxygen uptake efficiency slope). Further analysis among ten CTEPH patients receiving multiple BPA sessions (2–4 sessions) indicated BPA resulted in lasting improvements in hemodynamics and cardiopulmonary function.
Conclusions
BPA, a safe and effective approach, can bring instant improvements after a single session and lasting benefits after multiple sessions to hemodynamics and cardiopulmonary function for patients with inoperable CTEPH.
Keywords: Balloon pulmonary angioplasty, Chronic thromboembolic pulmonary hypertension, Cardiopulmonary function
Background
Chronic thromboembolic pulmonary hypertension (CTEPH) is a chronic and progressive disease characterized by fibrous stenosis or obliteration of pulmonary vasculature caused by organized thrombus, leading to progressive increase of pulmonary vascular resistance, right heart failure and terminal death [1–4]. The pathogenesis of CTEPH remains largely unknown, coagulation and fibrinolysis dysfunction, immune and inflammatory disorders, genetic susceptibility, defective angiogenesis and vascular remodeling have been reported to collaboratively contribute to the occurrence and development of CTEPH [5]. Although recent years have witnessed tremendous progress in medical therapies, particularly in pulmonary hypertension (PH)-targeted therapies [6], CTEPH is still a serious disease with poor prognosis with 1-, 3-, and 5-year survival rates of 90.2%, 78.4, and 64.5% respectively amongst patients with not-operated CTEPH [7].
Pulmonary endarterectomy (PEA) is recommended as the method of choice for all eligible patients with CTEPH, yet not all can benefit from this potentially curable procedure due to surgical contraindications and potential complications [4, 8, 9]. Balloon pulmonary angioplasty (BPA) was firstly reported to improve cardiac function and 6-min walk distance (6MWD) in 2001 [10], but it was accompanied with fatal reperfusion pulmonary edema and mechanical ventilation requirement, thus being left on the shelf for more than 10 years. Encouragingly, BPA has once again burst into the limelight since three gratifying reports from Japanese centers in 2012, making it as a promising alternative approach to improve hemodynamics and clinical symptoms [11–13]. Targeted therapy with or without BPA has been proposed in the CTEPH treatment algorithm for patients with non-operable CTEPH [4, 14].
Cardiopulmonary exercise testing (CPET) is a useful and non-invasive tool to objectively and safely evaluate the cardiopulmonary function and exercise capacity [15]. Our previous studies have shown CTEPH is associated with impaired ventilation efficiency and exercise capacity which are independent prognostic predictors in patients with CTEPH [16–19]. Improved exercise capacity assessed by CPET 3 months after BPA has been described [20, 21], nevertheless, the assessment was determined late and might be confounded by rehabilitation training or medical therapies. Since there are no reports regarding BPA in China and its instant impact on cardiopulmonary function among hospitalized patients with inoperable CTEPH, this study aims to firstly evaluate the safety and efficacy of BPA in our center and to assess its early effects on cardiopulmonary function in CTEPH patients.
Methods
Study patients
We enrolled twenty-five consecutive patients with CTEPH who underwent BPA procedures in the Center for Pulmonary Vascular Diseases, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College from May 11, 2018 to January 4, 2019. The diagnosis criteria of CTEPH, as we previously described, was established as follows: 1) existing precapillary PH defined as mean pulmonary arterial pressure (mPAP) ≥ 25 mmHg and pulmonary arterial wedge pressure (PAWP) ≤ 15 mmHg at rest confirmed by right heart catheterization (RHC); 2) evidence of thromboembolic occlusion of the proximal or distal pulmonary vasculature detected by imaging techniques such as computed tomography, magnetic resonance imaging, ventilation/perfusion scintigraphy or pulmonary angiography; 3) the above conditions should be obtained after at least 3 months of effective anticoagulation therapy [22, 23]. Inclusion criteria for BPA procedures: all CTEPH patients who are not suitable or contraindicated for PEA after operability assessment by our multidisciplinary team including PEA surgeons, PH experts, BPA interventionists and radiologists; Those with age more than 80 years old, severe liver or kidney dysfunction, iodinated contrast agents allergy, oxygen saturation in peripheral blood < 80%, existence of foreign body such as tumor and thrombus in catheter path, severe bleeding and coagulation disorders, life-threatening hypotension and cardiac arrhythmias, and different types of tumors were excluded. Written informed consent was obtained from all patients, and this study was approved by the Fuwai Hospital Ethics Committee and conformed to the Declaration of Helsinki.
Clinical assessment
Demographic data (age, sex and body mass index), history of deep vein thrombosis (DVT), PH targeted drugs (endothelin receptor antagonists, phosphodiesterase-5 inhibitors, prostanoids, soluble guanylate cyclase stimulators) were fully assessed after admission among all patients. World Health Organization (WHO) functional class (WHO-FC), N-terminal pro-brain natriuretic peptide (NT-proBNP) levels, oxygen saturation (SaO2) measured by arterial blood gas, 6MWD, transthoracic echocardiography (TTE), pulmonary function testing (PFT), chest computed tomography and pulmonary ventilation/perfusion scintigraphy before and after each BPA session within 1–3 days were well documented. General TTE parameters such as left ventricular end-diastolic diameter (LVED), right ventricular end-diastolic diameter (RVED) and tricuspid annular plane systolic excursion (TAPSE) were recorded [24]. RHC was performed through the right femoral vein after local anesthesia, hemodynamic parameters included right atrial pressure (RAP), right ventricular pressure, PAP [systolic PAP (sPAP), diastolic PAP (dPAP) and mPAP], PAWP, cardiac output (calculated by indirect Fick’s principle) and oxygen saturation (vena cava, right atrium, right ventricle and pulmonary artery). Mixed venous oxygen saturation (SvO2), cardiac index (CI) and pulmonary vascular resistance (PVR) were calculated according to standard formulas [20, 24].
BPA procedures
Pulmonary angiography was performed selectively in anterior-posterior and lateral (45 degree) projections after RHC to acquire overall view about the position and degree of filling defect in combination with previous ventilation/perfusion scintigraphy. BPA was routinely performed via the right femoral vein by two interventional cardiologists (Operator: ZHZ; Assistant: TY). A 80 cm 7 Fr long sheath (Flexor® Check-Flo® Introducer; Cook Medical, Bloomington, IN, USA) was inserted into the lobar pulmonary artery to introduce a 6 Fr guiding catheter in order to prevent the guiding catheter from moving along with the beating heart as well as to facilitate the exchange of guiding catheter, wires and balloons. 6 Fr Multi-purpose (Cordis Corporation, Bridgewater, New Jersey, USA), Amplatz Left (mainly for anterior segments, especially A3; Terumo® Heartrail™ II; Terumo Corporation, Tokyo, Japan) or Judkins Right (Terumo® Heartrail™ II; Terumo Corporation, Tokyo, Japan) was selected as the guiding catheter. After introducing the guiding catheter, 2000 U unfractionated heparin was additionally infused, and oxygen was given at a flow rate of 5–8 L/min to all patients. Priority selection of target lesions was as follows: right lung > left lung, inferior lobe > superior or middle lobes, webs or bands > subtotal occlusion > chronic total occlusion > tortuous lesions. A 0.014-in. wire (Hi-Torque Pilot 50; Abbot, Santa Clara, CA, USA) was crossed to the target lesion, then appropriate balloon catheters (Mini Trek; Abbot, Santa Clara, CA, USA) were positioned over the selected lesion and inflated with iodinated contrast agents to pressures of 2–14 atm for 5–30 s. A small-sized balloon (2.0 × 20 mm) was firstly used regardless of the diameter of target vessels at initial dilation, smaller balloon may be selected to pass subtotal or total occlusion lesions, inflation pressure was dynamically adjusted according to balloon size and vessel size, and selective angiography with 1:1 mixture of saline and contrast agents was performed with deep breath holds in real time to confirm vascular filling and the presence of ruptured vessels. Dilations were repeated with unchanged or stepwise increased balloon size in case of unresponsive or poorly responsive target angiographic vessel. Hemodynamic parameters were once again measured by RHC at the end of each BPA session. A typical BPA session lasted for 1–2 h. Each session should not exceed 2000 mGy radiation exposure, 60 min fluoroscopy time, and 250 ml contrast medium. Complications including reperfusion pulmonary edema, vascular injury and hemoptysis were adjudicated by two interventional cardiologists and were well recorded.
Cardiopulmonary exercise testing
CPET was performed according to standardized protocol as we previously described [16, 17, 25, 26]. An incremental symptom-limited exercise test was performed on an upright cycle ergometer using the COSMED Quark CPET system (COSMED, Rome, Italy). CPET was carried out prior to RHC and after BPA respectively within 3 days, and the protocol used after BPA was identical to that used before RHC. Three minutes of rest was followed by 3 min of unloaded pedaling and increased exercise using a physician-supervised, progressively increasing work rate (WR) of 5 to 30 W/min (the work rate depended on the estimated exercise capacity of each patient) to a maximum tolerance on an electromagnetically braked cycle ergometer. Patients were encouraged to exercise unless they met indications for test termination (eg, inappropriate blood pressure response, severe arrhythmia, dyspnea and leg fatigue). Gas exchange measurements were made by a metabolic cart breath by breath and averaged over 10 s intervals. Patients were continuously monitored by a standard 12-lead ECG and pulse oximetry (SpO2). Blood pressure was recorded using a standard cuff sphygmomanometer every 3 min. Heart rate was measured at 1-min intervals. Peak VO2 was defined as the highest 30s average of oxygen consumption in the last minute of exercise. Anaerobic threshold (AT) was detected by a combination of the V-slope method and ventilatory equivalents. PeakVO2/HR was calculated as peak VO2 divided by peak heart rate, and ventilatory efficiency was evaluated by minute ventilation (VE)/VCO2 slope and PETCO2@AT. VE/VCO2 slope was determined by linear regression analysis (VE = a VCO2 + b, a = slope) of VE/VCO2 plot obtained during exercise. Oxygen uptake efficiency slope (OUES) represented the rate of increase in VO2 in response to a ten-fold increase in VE during incremental exercise (VO2 = a log10VE + b; a = OUES) [25].
Statistical analysis
All continuous variables were presented as mean ± SD or median (interquartile range) when appropriate, categorical variables were shown as counts or percentages. A paired t test was used to compare data from the same subject before and after BPA procedures. A two-sided P value < 0.05 was considered as statistically significant. Paired t test analysis was performed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA), and figures displaying changes of variables before and after BPA procedures were drawn using GraphPad Prism version 5.01 (GraphPad Software, San Diego, CA, USA).
Results
Study population
A total of 40 BPA sessions were performed in 25 consecutive patients (13 male, 12 female, 1.6 ± 0.9 sessions per patient) with inoperable CTEPH during the study period. Baseline clinical characteristics of CTEPH patients at the first admission, including hemodynamics measured by RHC before their initial BPA session and PH targeted therapies, were summarized in Table 1. Their mean age at baseline was 58.2 ± 9.8 years old, among these CTEPH patients, 8 (32%) had a past history of DVT. The median time from onset to admission was 3 years. 19 (76%) patients received PH targeted medications, 14 (56%) patients received monotherapy and 5 (20%) patients received combined therapy. Before the first BPA session, 12 (48%) subjects had symptoms of WHO-FC I/II while 13 (52%) were in WHO-FC III/IV. The overall CTEPH patients (n = 25) had a mean 6MWD of 331.8 ± 111.3 m at baseline, with a mPAP of 49.4 ± 13.4 mmHg and a mean PVR of 952.01 ± 375.38 dyn·s·cm− 5 .
Table 1.
Baseline characteristics of patients with inoperable CTEPH
| Variables | Values |
|---|---|
| Patients, n | 25 |
| Male/Female, n | 13/12 |
| Age, years | 58.2 ± 9.8 |
| BMI, kg/m2 | 23.6 ± 3.4 |
| WHO-FC I/II/III/IVa, n | 1/11/13/0 |
| DVT, n (%) | 8 (32%) |
| Duration from onset to admissiona, years | 3.0 (1.1–5.5) |
| SaO2a, % | 91.3 ± 2.3 |
| SvO2a, % | 68.9 ± 5.3 |
| mRAPa, mmHg | 7.4 ± 3.3 |
| mPAPa, mmHg | 49.4 ± 13.4 |
| PVRa, dyne·s·cm−5 | 952.01 ± 375.38 |
| CIa, l/min/m2 | 3.18 ± 0.74 |
| PAWPa, mmHg | 10.2 ± 3.0 |
| PH targeted medicationa, n (%) | 19 (76%) |
| Monotherapy, n (%) | 14 (56%) |
| ERAs | 2 (8%) |
| PDE-5is | 8 (32%) |
| sGCs | 4 (16%) |
| Combined therapy, n (%) | 5 (20%) |
| ERAs+PDE-5is, n (%) | 5 (20%) |
| 6MWDa, m | 331.8 ± 111.3 |
| Number of BPA sessions, n | 40 |
| Number of treated segments per session, n | 3.4 ± 1.6 |
| Number of treated vessels per session, n | 4.6 ± 1.9 |
| Number of balloons per session, n | 1.4 ± 0.5 |
BMI body mass index, WHO-FC WHO functional class, DVT deep vein thrombosis, SaO2 arterial oxygen saturation, SvO2 mixed venous oxygen saturation, mRAP mean right atrial pressure, mPAP mean pulmonary artery pressure, PVR pulmonary vascular resistance, CI cardiac index, PAWP pulmonary arterial wedge pressure, PH pulmonary hypertension, ERAs endothelin receptor antagonists, PDE-5is phosphodiesterase-5 inhibitors, sGCs soluble guanylate cyclase stimulators, 6MWD 6-min walk distance, BPA balloon pulmonary angioplasty
aData at the first admission
Efficacy and safety of BPA
A total of 183 segmental or subsegmental vessels (4.6 ± 1.9 vessels per session) in 137 segments (3.4 ± 1.6 segments per session) were dilated among 40 BPA sessions. These vessel lesions consisted of 146 webs or bands, 17 subtotal lesions, and 20 total occlusion lesions. After selective pulmonary angiography, a total of 55 balloons (1.4 ± 0.5 per session) matched to the vessel diameters were selected, and balloon diameters and number proportion used for dilation were as follows: 1.2 mm (2%), 1.5 mm (2%), 2.0 mm (47%), 2.5 mm (13%), 3 mm (18%), 3.5 mm (16%), 4 mm (2%). Representative images and videos pre-BPA and post-BPA sessions were displayed in Fig. 1 and Additional file 1. No patients died during the follow-up period till June 1, 2019, and no complications such as pulmonary edema and hemoptysis occurred. The changes in catheter hemodynamics, echocardiographic and clinical parameters before and after BPA sessions (n = 40) are shown in Table 2 and Fig. 2. After BPA, CTEPH patients got immediate and significant decreases in sPAP (84.4 ± 22.8 mmHg vs 74.7 ± 21.9 mmHg, P < 0.001), dPAP (29.4 ± 7.8 mmHg vs 25.5 ± 7.3 mmHg, P < 0.001) and mPAP (47.4 ± 11.9 mmHg vs 41.5 ± 10.7 mmHg, P < 0.001). However, no significant differences were observed in echocardiographic parameters such as LVED, RVED and TAPSE. Average level of NT-proBNP markedly reduced from 1161.8 pg/ml to 671.2 pg/ml (P = 0.001). Moreover, 6MWD dramatically increased from 350.0 ± 103.4 m to 403.6 ± 81.3 m after BPA treatment. Compared with baseline, WHO-FC improved with the number of patients in I, II, III, and IV changing from 1/26/13/0 to 8/30/2/0, respectively.
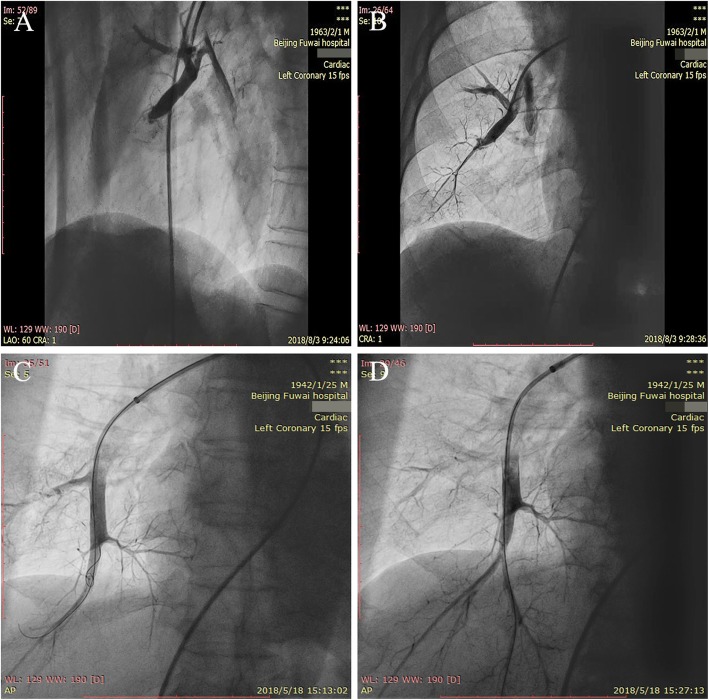
Fig. 1.
Selective pulmonary angiography in right lower lobe before and immediately after BPA. a Total occlusion in RA8 before BPA. b Improved blood flow in RA8 immediately after BPA. c Total occlusion in RA10 before BPA. d Improved blood flow in RA10 immediately after BPA
Table 2.
Hemodynamics and clinical parameters before and after a single BPA session and multiple BPA sessions
| Parameters | Single BPA session (n = 40) | Multiple BPA sessions (n = 10) | ||||
|---|---|---|---|---|---|---|
| Pre-BPA | Post-BPA | P value | Before-first BPA | After-last BPA | P value | |
| RHC | ||||||
| SvO2, % | 69.8 ± 5.1 | – | 68.14 ± 4.43 | 72.07 ± 2.97a | 0.019 | |
| SaO2, % | 91.4 ± 2.1 | 91.9 ± 2.7 | 0.262 | 90.2 ± 1.8 | 91.9 ± 1.6a | 0.01 |
| mRAP, mmHg | 7.4 ± 2.9 | – | 7.3 ± 3.9 | 8.1 ± 2.5a | 0.54 | |
| sPAP, mmHg | 84.4 ± 22.8 | 74.7 ± 21.9 | < 0.001 | 93.0 ± 26.0 | 81.2 ± 18.7a | 0.068 |
| dPAP, mmHg | 29.4 ± 7.8 | 25.5 ± 7.3 | < 0.001 | 31.9 ± 9.0 | 27.8 ± 4.3a | 0.089 |
| mPAP, mmHg | 47.4 ± 11.9 | 41.5 ± 10.7 | < 0.001 | 52.6 ± 14.1 | 44.8 ± 8.2a | 0.031 |
| PVR, dyne·s·cm−5 | 886.15 ± 342.04 | – | 1067.0 ± 410.4 | 758.0 ± 212.1a | 0.04 | |
| PAWP, mmHg | 9.8 ± 3.2 | – | 8.1 ± 2.8 | 10.7 ± 3.0a | 0.164 | |
| CI, l/min/m2 | 3.26 ± 0.78 | – | 3.07 ± 0.69 | 3.42 ± 0.70a | 0.202 | |
| TTE | ||||||
| LVED, mm | 41.1 ± 4.9 | 42.0 ± 5.1 | 0.203 | 41.4 ± 3.7 | 43.7 ± 3.8 | 0.048 |
| RVED, mm | 31.3 ± 7.4 | 30.2 ± 6.4 | 0.142 | 30.5 ± 4.0 | 28.1 ± 5.1 | 0.32 |
| TAPSE, mm | 16.5 ± 4.2 | 17.2 ± 3.5 | 0.296 | 16.2 ± 4.2 | 18.3 ± 1.5 | 0.304 |
| Pulmonary function testing | ||||||
| FVC, l | 3.11 ± 0.83 | 3.21 ± 0.93 | 0.037 | 3.22 ± 0.84 | 3.49 ± 1.01 | 0.01 |
| FVC% predicted, % | 90.7 ± 13.0 | 93.4 ± 14.5 | 0.041 | 95.8 ± 12.0 | 103.6 ± 11.2 | 0.004 |
| FEV1, l | 2.26 ± 0.64 | 2.32 ± 0.71 | 0.034 | 2.39 ± 0.69 | 2.55 ± 0.79 | 0.023 |
| FEV1% predicted, % | 80.8 ± 14.2 | 82.7 ± 16.1 | 0.045 | 87.9 ± 16.5 | 93.2 ± 15.4 | 0.038 |
| MVV, l/min | 89.4 ± 31.7 | 99.1 ± 34.7 | < 0.001 | 95.2 ± 37.7 | 114.1 ± 36.2 | 0.002 |
| MVV% predicted, % | 83.2 ± 24.0 | 92.4 ± 25.2 | < 0.001 | 89.0 ± 26.4 | 108.4 ± 26.0 | 0.005 |
| NT-proBNP, pg/ml | 1161.8 ± 1420.0 | 671.2 ± 753.0 | 0.001 | 1329.0 ± 1599.0 | 326.5 ± 601.0 | 0.022 |
| 6MWD, m | 350.0 ± 103.4 | 403.6 ± 81.3 | < 0.001 | 316.8 ± 120.2 | 443.9 ± 63.6 | 0.003 |
| WHO-FC I/II/III/IV | 2.3 ± 0.5 | 1.9 ± 0.5 | < 0.001 | 2.7 ± 0.5 | 2.0 ± 0 | 0.001 |
| I, n (%) | 1 (2.5%) | 8 (20%) | 0 (0%) | 0 (0%) | ||
| II, n (%) | 26 (65%) | 30 (75%) | 3 (30%) | 10 (100%) | ||
| III, n (%) | 13 (32.5%) | 2 (5%) | 7 (70%) | 0 (0%) | ||
| IV, n (%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
BPA balloon pulmonary angioplasty, RHC right heart catheterization, SvO2 mixed venous oxygen saturation, SaO2 arterial oxygen saturation, mRAP mean right atrial pressure, sPAP systolic pulmonary artery pressure, dPAP diastolic pulmonary artery pressure, mPAP mean pulmonary artery pressure, PVR pulmonary vascular resistance, PAWP pulmonary arterial wedge pressure, CI cardiac index, TTE transthoracic echocardiography, LVED left ventricular end-diastolic diameter, RVED right ventricular end-diastolic diameter, TAPSE tricuspid annular plane systolic excursion, FVC forced vital capacity, FEV1 forced expiratory volume in the first second, MVV maximal voluntary ventilation, NT-proBNP N-terminal pro-brain natriuretic peptide, 6MWD 6-min walk distance, WHO-FC WHO functional class
aData at RHC before the last BPA
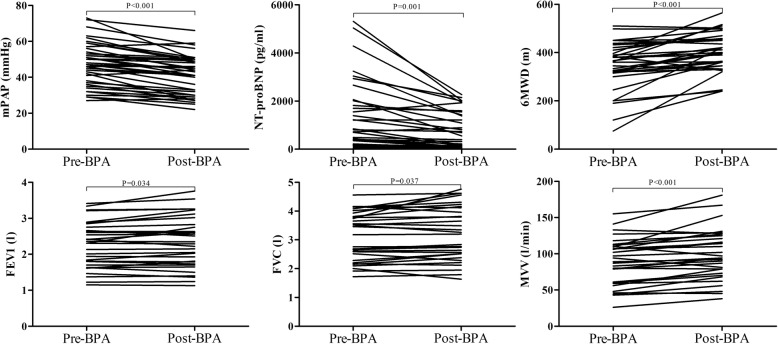
Fig. 2.
Hemodynamic and clinical parameters before and after a single BPA session
Cardiopulmonary function after a single BPA session
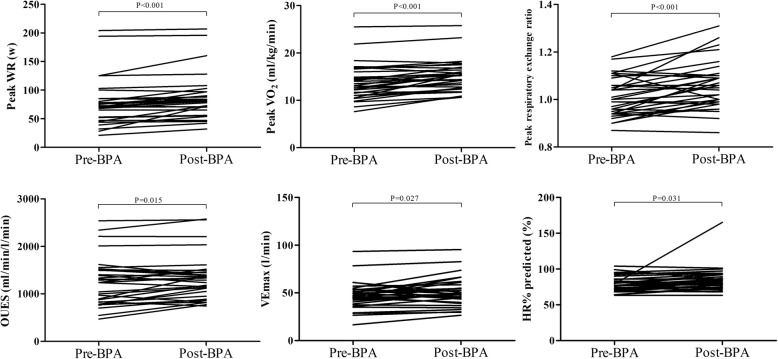
As for PFT, forced vital capacity (FVC), FVC% predicted, forced expiratory volume in the first second (FEV1), FEV1% predicted, maximal voluntary ventilation (MVV) and MVV% predicted all significantly improved post-BPA compared to those of pre-BPA (all P < 0.05; Fig. 2). As shown in Table 3 and Fig. 3, exercise performance as evaluated by several CPET parameters improved significantly after BPA. Compared to pre-BPA, Peak WR (78.0 ± 40.6 w vs 86.7 ± 39.8 w, P < 0.001), Peak VO2 (13.9 ± 3.7 ml/kg/min vs 15.2 ± 3.3 ml/kg/min, P < 0.001), Peak VO2% predicted (54.5 ± 16.8% vs 58.8 ± 15.3%, P < 0.001), peak respiratory exchange ratio (1.01 ± 0.08 vs 1.06 ± 0.10, P < 0.001), OUES (1250.5 ± 508.3 ml/min/l/min vs 1329.1 ± 466.6 ml/min/l/min, P = 0.015) and HR% predicted (78.5 ± 10.5% vs 84.9 ± 17.4%, P = 0.031) all significantly increased post-BPA. Similarly, notable increments were also identified in ventilation parameters VEmax (47.2 ± 14.4 l/min vs 50.7 ± 15.1 l/min, P = 0.027), VT@AT (1.19 ± 0.31 l vs 1.31 ± 0.34 l, P = 0.035) and VTmax (1.54 ± 0.38 l vs 1.67 ± 0.43 l, P < 0.001). HR@ AT (102.8 ± 18.3 bpm vs 108.1 ± 19.0 bpm, P = 0.056) and Peak VO2/HR% predicted (69.0 ± 17.9% vs 71.3 ± 15.3%, P = 0.068) before and after BPA reached a borderline statistical significance. VE/VCO2 slope, VE/VCO2 slope% predicted and Peak VE/VCO2 were on a downward trend, although no significant differences were found between pre-BPA and post-BPA.
Table 3.
CPET parameters before and after a single BPA session and multiple BPA sessions
| Parameters | Single BPA session (n = 40) | Multiple BPA sessions (n = 10) | ||||
|---|---|---|---|---|---|---|
| Pre-BPA | Post-BPA | P value | Before-first BPA | After-last BPA | P value | |
| Peak WR, w | 78.0 ± 40.6 | 86.7 ± 39.8 | < 0.001 | 77.3 ± 47.6 | 96.2 ± 40.2 | 0.024 |
| AT, ml/kg/min | 10.7 ± 3.2 | 11.7 ± 3.1 | 0.098 | 10.3 ± 3.2 | 11.4 ± 3.3 | 0.57 |
| Peak VO2, ml/kg/min | 13.9 ± 3.7 | 15.2 ± 3.3 | < 0.001 | 13.7 ± 4.5 | 16.1 ± 3.2 | 0.025 |
| Peak VO2% predicted, % | 54.5 ± 16.8 | 58.8 ± 15.3 | < 0.001 | 53.7 ± 18.1 | 63.9 ± 14.1 | 0.015 |
| Peak respiratory exchange ratio | 1.01 ± 0.08 | 1.06 ± 0.10 | < 0.001 | 1.04 ± 0.08 | 1.09 ± 0.10 | 0.046 |
| VE/VCO2 slope | 49.1 ± 15.3 | 45.3 ± 11.4 | 0.09 | 52.3 ± 16.7 | 44.0 ± 10.5 | 0.099 |
| VE/VCO2 slope% predicted, % | 181.4 ± 57.0 | 166.7 ± 40.6 | 0.079 | 191.4 ± 62.7 | 160.7 ± 37.8 | 0.098 |
| OUES, ml/min/l/min | 1250.5 ± 508.3 | 1329.1 ± 466.6 | 0.015 | 1205.0 ± 576.2 | 1341.0 ± 382.6 | 0.397 |
| VEmax, l/min | 47.2 ± 14.4 | 50.7 ± 15.1 | 0.027 | 52.4 ± 17.1 | 56.8 ± 15.4 | 0.197 |
| VT@AT, l | 1.19 ± 0.31 | 1.31 ± 0.34 | 0.035 | 1.20 ± 0.37 | 1.31 ± 0.33 | 0.422 |
| VTmax, l | 1.54 ± 0.38 | 1.67 ± 0.43 | < 0.001 | 1.66 ± 0.39 | 1.80 ± 0.45 | 0.051 |
| HR@AT, bpm | 102.8 ± 18.3 | 108.1 ± 19.0 | 0.056 | 102.3 ± 15.1 | 108.6 ± 14.4 | 0.388 |
| HRmax, bpm | 128.9 ± 19.5 | 132.9 ± 16.0 | 0.16 | 126.4 ± 17.0 | 141.8 ± 13.0 | < 0.001 |
| HR% predicted, % | 78.5 ± 10.5 | 84.9 ± 17.4 | 0.031 | 79.7 ± 9.8 | 88.7 ± 7.5 | < 0.001 |
| Peak VO2/HR, ml/bpm | 7.52 ± 2.88 | 7.66 ± 2.55 | 0.381 | 7.24 ± 3.37 | 7.73 ± 2.49 | 0.466 |
| Peak VO2/HR% predicted, % | 69.0 ± 17.9 | 71.3 ± 15.3 | 0.068 | 66.6 ± 18.9 | 71.8 ± 12.0 | 0.272 |
| Peak PetCO2, mmHg | 24.7 ± 6.3 | 24.6 ± 7.0 | 0.916 | 22.4 ± 5.3 | 24.4 ± 4.9 | 0.39 |
| Peak PetO2, mmHg | 125.0 ± 5.0 | 125.7 ± 4.9 | 0.253 | 126.8 ± 3.8 | 127.8 ± 3.8 | 0.454 |
| Peak VE/VO2 | 52.3 ± 12.6 | 51.6 ± 10.6 | 0.609 | 60.1 ± 14.4 | 54.4 ± 9.6 | 0.359 |
| Peak VE/VCO2 | 51.8 ± 12.9 | 49.6 ± 10.7 | 0.078 | 57.9 ± 13.5 | 50.5 ± 10.5 | 0.19 |
| Peak SpO2, % | 91.0 ± 5.1 | 92.4 ± 4.7 | 0.484 | 89.1 ± 4.6 | 90.9 ± 4.1 | 0.213 |
Peak WR peak work rate, AT anaerobic threshold, Peak VO2 peak oxygen consumption, VE/VCO2 minute ventilation/carbon dioxide production, OUES oxygen uptake efficiency slope, VEmax maximal minute ventilation, VT@AT tidal volume at the anaerobic threshold, VTmax maximum tidal volume, HR@AT heart rate at the anaerobic threshold, HRmax maximum heart rate, Peak VO2/HR peak oxygen consumption/peak heart rate, PetCO2 partial pressure of end-tidal carbon dioxide, PetO2 partial pressure of end-tidal oxygen, VE/VO2 minute ventilation/oxygen consumption, SpO2 pulse oxygen saturation
Fig. 3.
CPET parameters before and after a single BPA session
Hemodynamics and cardiopulmonary function after multiple BPA sessions
For ten CTEPH patients receiving repeated BPA sessions (2–4 sessions), a subgroup analysis was performed. The median time interval between the first and last BPA sessions was 14.4 (9.8–29.2) weeks. As described in Table 2, SaO2 (90.2 ± 1.8% vs 91.9 ± 1.6%, P = 0.01) and SvO2 (68.14 ± 4.43% vs 72.07 ± 2.97%, P = 0.019) were both significantly increased before the last BPA session when compared with those before the first BPA session. In addition, mPAP decreased from 52.6 ± 14.1 mmHg to 44.8 ± 8.2 mmHg (P = 0.031, Additional file 2: Figure S1), and PVR declined from 1067.0 ± 410.4 dyne·s·cm− 5 to 758.0 ± 212.1 dyne·s·cm− 5, while CI remained unchanged. LVED measured by TTE was significantly elevated from 41.4 ± 3.7 mm to 43.7 ± 3.8 mm. In contrast to data before first-BPA, all variables of PFT as was mentioned above augmented significantly after last-BPA. Furthermore, the average level of NT-proBNP fell significantly over time from 1329.0 pg/ml to 326.5 pg/ml, while 6MWD rose to 443.9 ± 63.6 m after the last BPA session (Additional file 2: Figure S1). Seven (70%) patients in WHO-FC III prior to the first BPA session improved to WHO-FC II after the final procedure. The changes of CPET parameters before-first and after-last BPA sessions were displayed in Table 3. Compared with baseline, Peak WR, Peak VO2, Peak VO2% predicted, peak respiratory exchange ratio and HR% predicted were still obviously elevated (Additional file 2: Figure S2). HRmax during exercise increased significantly from 126.4 ± 17.0 bpm to 141.8 ± 13.0 bpm (P < 0.001), yet differences of VTmax between before-first BPA and after-last BPA reached a marginal significance (P = 0.051). Non-significant increased trends in OUES, Peak VO2/HR and SpO2 were discerned.
Discussion
This is, to the best of our knowledge, the first study to investigate the safety and efficacy of BPA in China, as well as its instant effects on cardiopulmonary function in patients with inoperable CTEPH. The present study demonstrated BPA, as a safe and effective approach, brought instant and lasting benefits to hemodynamics and cardiopulmonary function for patients with inoperable CTEPH.
PEA is currently the only established curative treatment for patients with CTEPH [14]. Nevertheless, nearly 40% of subjects were considered inoperable because of lesion inaccessbility or possible comorbidities [4, 8], and 25–31% of CTEPH patients had residual PH after PEA surgery [27, 28]. Moreover, PEA surgery involves exquisite techniques and multidisciplinary collaboration, and can be performed only at a limited number of institutions. Riociguat, a soluble guanylate cyclase stimulator, is the only approved medical therapy indicated for patients with inoperable CTEPH based on the CHEST trials [6, 29, 30]. However, majorities of CTEPH patients cannot benefit from this drug for economic reasons in China.
BPA is an interventional technique which uses a balloon catheter to cross and dilate target lesions to relieve pulmonary vascular stenosis or obstruction. It was firstly attempted in 1983 to relieve pulmonary artery stenosis or hypoplasia, and brought significant hemodynamic improvements for children with congenital lesions [31]. The first case of BPA for CTEPH was reported by Voorburg et al. in 1988 [32]. Later in 2001, Feinstein described 18 CTEPH case series treated with BPA, showing improved hemodynamics and exercise tolerance. Unfortunately, 11 patients developed reperfusion pulmonary edema, and 3 patients required mechanical ventilation [10]. With continuous refinements from three Japanese institutions [11–13], BPA has been reported to significantly improve hemodynamics, exercise capacity and right ventricular function, with significantly lower rates of complications [33–36]. BPA is now recommended in the newly proposed CTEPH treatment algorithm for inoperable CTEPH patients at experienced centers [4], however, most of data with regard to BPA in CTEPH mainly come from Japan, Europe and USA, the safety and efficacy of BPA procedures in China have never been reported.
Our study demonstrated that BPA conferred significant improvements in instant hemodynamics as evidenced by decreased sPAP, dPAP and mPAP. However, differential structural changes in the heart evaluated by TTE were not observed after a single BPA session among our patients. In accordance with our results, Tsugu et al. [33] also noticed mPAP was significantly improved, and right ventricular basal, mid cavity and longitudinal diameters remained unchanged immediately after BPA, but left ventricular end-diastolic diameter and TAPSE obviously increased compared with baseline, the difference might be explained by relatively better right ventricular function and higher TAPSE of our patients. In order to exclude the effect of supplemental oxygen on pulmonary hemodynamics during BPA procedures, we compared catheterization hemodynamics before the first BPA and before the second BPA among patients receiving multiple BPA sessions which revealed mPAP decreased from 52.6 ± 14.1 mmHg to 44.5 ± 9.2 mmHg (P = 0.004) and PVR declined from 1067.0 ± 410.4 dyne·s·cm− 5 to 822.6 ± 272.4 dyne·s·cm− 5 (P = 0.025), definitely demonstrating a single BPA session was enough to improve hemodynamics. Except for hemodynamics, PFT indexes, 6MWD, NT-proBNP and WHO-FC all got improved after a single BPA session.
Those receiving multiple BPA sessions got lasting hemodynamic improvements as evidenced by reduced mPAP and PVR together with elevated oxygen saturation before the last BPA session when compared with baseline values. However, CI did not show any significant changes but presented a rising trend after BPA sessions among our patients, while previous studies reported significant improvements in CI [20, 34, 37], which might be ascribed to limited sessions, short BPA intervals and small sample size of our study. Most importantly, LVED got significantly increased, reflecting structural recovery. The above hemodynamic and structural changes are only based on 2–4 BPA sessions, we believe there will be a more significant improvement after more BPA sessions. Furthermore, 6MWD and NT-proBNP got larger scale changes than those in a single BPA session, signifying more benefits brought by staged BPA sessions.
Previous studies reported the rates of lung injury, hemoptysis, and pulmonary artery perforation were 7.0–31.4%, 5.6–19.6%, and 0–8.0% respectively [35]. Occurrence of complications depends on target lesion types, guiding wire types, balloon size and interventionist experience, too many target vessels dilated per session or too large balloon are easy to cause aforementioned complications. No such complications occurred among our patients, we utilized pulmonary angiography and pulmonary perfusion scintigraphy before BPA procedures to facilitate the selection of target lesions, preferred to select smaller balloons (2 mm) at the initial BPA session no matter what lesions our patients had, and limited the total number of balloons (1–2 per session). As subtotal occlusion, total occlusion and tortuous lesions were accompanied with higher risks of complications such as wire injury [38], we started with “webs and bands” and performed balloon dilatation in a staged manner, indicating a relatively conservative approach may lower BPA complications.
CPET is an important clinical tool to evaluate exercise capacity and cardiopulmonary function. Peak VO2, an essential factor that mainly reflects exercise capacity and cardiac function, is currently an important index of risk stratification in patients with PAH [39, 40]. In patients with inoperable CTEPH, Peak VO2 is still a powerful predictor of mortality [41]. After a median 14.4-week interval between the first and last BPA, Peak VO2 and Peak VO2% predicted both strikingly increased among our patients receiving multiple BPA sessions, indicating a significantly lasting recovery in exercise capacity and cardiac function and possible improvement of prognosis, other similar parameters such as peak respiratory exchange ratio (respiratory quotient), HRmax and HR% predicted were also comparable to those before BPA, which is consistent with previous studies [20, 34]. VE/VCO2 slope, a sensitive variable that reflects exercise ventilatory efficiency, decreased greatly even in the early 1 month after PEA [42] as well as 3 months after BPA sessions [34]. However, VE/VCO2 slope showed a non-significantly declining tendency, which might be influenced by small population size.
Unlike earlier studies in which cardiopulmonary function was assessed late after interventions [20, 34], our study mainly focused on the early changes of hemodynamics and cardiopulmonary function within a week after BPA procedure, thus revealing immediate effectiveness of BPA. Peak WR, Peak VO2, Peak VO2% predicted significantly improved when assessed within 3 days following a single BPA session. OUES is a submaximal exercise parameter that represents the absolute rate of increase in oxygen consumption per 10-fold increase in ventilation, our previous study demonstrated OUES could predict poor outcome in patients with idiopathic PAH [25]. Herein, we observed early increase of OUES after a single BPA session, indicating instant improvement of submaximal exercise capacity. VE and VT are two good indicators of ventilation function, VEmax and VTmax were both evidently elevated, illustrating early ventilation improvements. FVC, FEV1, and MVV have been widely used clinically to evaluate pulmonary function in respiratory diseases, they all achieved instant and lasting correction after BPA procedure, which may be explained by ventilation improvement along with increased pulmonary blood flow so as to maintain the dynamic balance of ventilation and perfusion. In consistent with aforementioned ventilation improvement, CTEPH patients felt much better and breathed more deeper and easier even during BPA procedures in our real-world clinical practice. CPET could objectively, safely and repetitiously evaluate the cardiopulmonary function, exhibiting absolute advantages over subjective parameters such as WHO-FC and 6MWD as well as catherization hemodynamics which might be confounded by supplemental oxygen during BPA, CPET may exert as a sensitive and reliable indicator to assess the effects of BPA.
There are several limitations of this study. First, the sample size of this study is relatively small. Second, this study was implemented in a single center, although our center is the largest pulmonary vascular center and also one of the largest BPA centers in China. Large-scale, multicenter, prospective studies should be launched to investigate and confirm the long-term effects of BPA procedures for CTEPH patients. Third, we didn’t measure other parameters such as oxygen saturation after BPA for economic issues and procedure time, thus immediate PVR and CI were not obtained, leading to incomprehensive hemodynamics evaluation after a single BPA session.
Conclusion
BPA can safely and effectively improve the instant and lasting hemodynamics and cardiopulmonary function. Larger multicenter studies are needed to further investigate and confirm the role of BPA in CTEPH.
Supplementary information
Additional file 1. Representative videos before and immediately after BPA.
Additional file 2: Figure S1. Hemodynamic and clinical parameters before and after multiple BPA sessions. Figure S2. CPET parameters before and after multiple BPA sessions.
Acknowledgements
We thank Professor Hiromi Matsubara, Department of Clinical Science, National Hospital Organization Okayama Medical Center, Okayama, Japan, for his direction in BPA procedures.
Abbreviations
- 6MWD
6-min walk distance
- AT
Anaerobic threshold
- BPA
Balloon pulmonary angioplasty
- CI
Cardiac index
- CPET
Cardiopulmonary exercise testing
- CTEPH
Chronic thromboembolic pulmonary hypertension
- DVT
Deep vein thrombosis
- FEV1
Forced expiratory volume in the first second
- FVC
Forced vital capacity
- LVED
Left ventricular end-diastolic diameter
- mPAP
Mean pulmonary arterial pressure
- MVV
Maximal voluntary ventilation
- NT-proBNP
N-terminal pro-brain natriuretic peptide
- OUES
Oxygen uptake efficiency slope
- PAH
Pulmonary arterial hypertension.
- PAWP
Pulmonary arterial wedge pressure
- PEA
Pulmonary endarterectomy
- PH
Pulmonary hypertension
- PVR
Pulmonary vascular resistance
- RAP
Right atrium pressure
- RHC
Right heart catheterization
- RVED
Right ventricular end-diastolic diameter
- SaO2
Oxygen saturation
- SvO2
Mixed venous oxygen saturation
- TAPSE
Tricuspid annular plane systolic excursion
- TTE
Transthoracic echocardiography
- VE
Minute ventilation
- WHO-FC
World Health Organization functional class
- WR
Work rate
Authors’ contributions
JQ contributed to the conception and design of the study, analysis and interpretation of data, drafting and revising the manuscript. LQ, YT, ZQX and ZZH contributed to data collection and interpretation. JQ, YX, YL, ZY, ZQ, MXP and ACH contributed to data collection. XCM critically reviewed and revised the manuscript. ZZH and LZH conceived and designed the study, and helped revise the manuscript. All authors read and approved the final manuscript.
Funding
This paper is supported by National Natural Science Foundation of China (Grant Nos. 81370326, 81641005), Beijing Municipal Science and Technology Project (Z181100001718200) and National Precision Medical Research Program of China (2016YFC0905602).
Availability of data and materials
All data generated or analyzed during this study are included in this manuscript.
Ethics approval and consent to participate
The study was approved by the ethics committee of Fuwai Hospital and adhered to the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from patients in this study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhihui Zhao, Phone: +86 010-88396985, Email: 1250167892@qq.com.
Zhihong Liu, Phone: +86 010-88396985, Email: zhihongliufuwai@163.com.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12931-019-1211-y.
References
- 1.Hoeper MM, Mayer E, Simonneau G, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Circulation. 2006;113:2011–2020. doi: 10.1161/CIRCULATIONAHA.105.602565. [DOI] [PubMed] [Google Scholar]
- 2.Kim NH, Delcroix M, Jenkins DP, Channick R, Dartevelle P, Jansa P, Lang I, Madani MM, Ogino H, Pengo V, Mayer E. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62:D92–D99. doi: 10.1016/j.jacc.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 3.Mahmud E, Madani MM, Kim NH, Poch D, Ang L, Behnamfar O, Patel MP, Auger WR. Chronic thromboembolic pulmonary hypertension: evolving therapeutic approaches for operable and inoperable disease. J Am Coll Cardiol. 2018;71:2468–2486. doi: 10.1016/j.jacc.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Kim Nick H., Delcroix Marion, Jais Xavier, Madani Michael M., Matsubara Hiromi, Mayer Eckhard, Ogo Takeshi, Tapson Victor F., Ghofrani Hossein-Ardeschir, Jenkins David P. Chronic thromboembolic pulmonary hypertension. European Respiratory Journal. 2019;53(1):1801915. doi: 10.1183/13993003.01915-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yan Lu, Li Xin, Liu Zhihong, Zhao Zhihui, Luo Qin, Zhao Qin, Jin Qi, Yu Xue, Zhang Yi. Research progress on the pathogenesis of CTEPH. Heart Failure Reviews. 2019;24(6):1031–1040. doi: 10.1007/s10741-019-09802-4. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Yi, Yu Xue, Jin Qi, Luo Qin, Zhao Zhihui, Zhao Qing, Yan Lu, Liu Zhihong. Advances in targeted therapy for chronic thromboembolic pulmonary hypertension. Heart Failure Reviews. 2019;24(6):949–965. doi: 10.1007/s10741-019-09798-x. [DOI] [PubMed] [Google Scholar]
- 7.Taniguchi Yu, Jaïs Xavier, Jevnikar Mitja, Boucly Athénaïs, Weatherald Jason, Brenot Philippe, Planche Olivier, Parent Florence, Savale Laurent, Fadel Elie, Montani David, Humbert Marc, Sitbon Olivier, Simonneau Gérald. Predictors of survival in patients with not-operated chronic thromboembolic pulmonary hypertension. The Journal of Heart and Lung Transplantation. 2019;38(8):833–842. doi: 10.1016/j.healun.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Pepke-Zaba J, Delcroix M, Lang I, Mayer E, Jansa P, Ambroz D, Treacy C, D'Armini AM, Morsolini M, Snijder R, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation. 2011;124:1973–1981. doi: 10.1161/CIRCULATIONAHA.110.015008. [DOI] [PubMed] [Google Scholar]
- 9.Yandrapalli S, Tariq S, Kumar J, Aronow WS, Malekan R, Frishman WH, Lanier GM. Chronic thromboembolic pulmonary hypertension: epidemiology, diagnosis, and management. Cardiol Rev. 2018;26:62–72. doi: 10.1097/CRD.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 10.Feinstein JA, Goldhaber SZ, Lock JE, Ferndandes SM, Landzberg MJ. Balloon pulmonary angioplasty for treatment of chronic thromboembolic pulmonary hypertension. Circulation. 2001;103:10–13. doi: 10.1161/01.CIR.103.1.10. [DOI] [PubMed] [Google Scholar]
- 11.Sugimura K, Fukumoto Y, Satoh K, Nochioka K, Miura Y, Aoki T, Tatebe S, Miyamichi-Yamamoto S, Shimokawa H. Percutaneous transluminal pulmonary angioplasty markedly improves pulmonary hemodynamics and long-term prognosis in patients with chronic thromboembolic pulmonary hypertension. Circ J. 2012;76:485–488. doi: 10.1253/circj.CJ-11-1217. [DOI] [PubMed] [Google Scholar]
- 12.Kataoka M, Inami T, Hayashida K, Shimura N, Ishiguro H, Abe T, Tamura Y, Ando M, Fukuda K, Yoshino H, Satoh T. Percutaneous transluminal pulmonary angioplasty for the treatment of chronic thromboembolic pulmonary hypertension. Circ Cardiovasc Interv. 2012;5:756–762. doi: 10.1161/CIRCINTERVENTIONS.112.971390. [DOI] [PubMed] [Google Scholar]
- 13.Mizoguchi H, Ogawa A, Munemasa M, Mikouchi H, Ito H, Matsubara H. Refined balloon pulmonary angioplasty for inoperable patients with chronic thromboembolic pulmonary hypertension. Circ Cardiovasc Interv. 2012;5:748–755. doi: 10.1161/CIRCINTERVENTIONS.112.971077. [DOI] [PubMed] [Google Scholar]
- 14.Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) Eur Respir J. 2015;46:903–975. doi: 10.1183/13993003.01032-2015. [DOI] [PubMed] [Google Scholar]
- 15.Albouaini K, Egred M, Alahmar A, Wright DJ. Cardiopulmonary exercise testing and its application. Postgrad Med J. 2007;83:675–682. doi: 10.1136/hrt.2007.121558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao ZH, Liu ZH, Gu Q, Luo Q, Zhao Q, Xiong CM, Ni XH. Application of cardiopulmonary exercise testing in patients with chronic thromboembolic pulmonary hypertension. Zhonghua Yi Xue Za Zhi. 2013;93:1687–1690. [PubMed] [Google Scholar]
- 17.Xi Q, Zhao Z, Liu Z, Ma X, Luo Q, Liu W. The lowest VE/VCO(2) ratio best identifies chronic thromboembolic pulmonary hypertension. Thromb Res. 2014;134:1208–1213. doi: 10.1016/j.thromres.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Condliffe R, Kiely DG, Gibbs JS, Corris PA, Peacock AJ, Jenkins DP, Goldsmith K, Coghlan JG, Pepke-Zaba J. Prognostic and aetiological factors in chronic thromboembolic pulmonary hypertension. Eur Respir J. 2009;33:332–338. doi: 10.1183/09031936.00092008. [DOI] [PubMed] [Google Scholar]
- 19.Schwaiblmair M, Faul C, von Scheidt W, Berghaus TM. Ventilatory efficiency testing as prognostic value in patients with pulmonary hypertension. BMC Pulm Med. 2012;12:23. doi: 10.1186/1471-2466-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andreassen AK, Ragnarsson A, Gude E, Geiran O, Andersen R. Balloon pulmonary angioplasty in patients with inoperable chronic thromboembolic pulmonary hypertension. Heart. 2013;99:1415–1420. doi: 10.1136/heartjnl-2012-303549. [DOI] [PubMed] [Google Scholar]
- 21.Akizuki M, Serizawa N, Ueno A, Adachi T, Hagiwara N. Effect of balloon pulmonary angioplasty on respiratory function in patients with chronic thromboembolic pulmonary hypertension. Chest. 2017;151:643–649. doi: 10.1016/j.chest.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Yu X, Huang Z, Zhang Y, Liu Z, Luo Q, Zhao Z, Zhao Q, Gao L, Jin Q, Yan L. Obstructive sleep apnea in patients with chronic thromboembolic pulmonary hypertension. J Thorac Dis. 2018;10:5804–5812. doi: 10.21037/jtd.2018.09.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xi Q, Liu Z, Liu W, Zhao Z, Luo Q, Huang Z. Chronic thromboembolic pulmonary hypertension is not associated with iron overload. Cardiovasc Pathol. 2015;24:76–79. doi: 10.1016/j.carpath.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 24.Yu X, Luo Q, Liu Z, Zhao Z, Zhao Q, An C, Huang Z, Jin Q, Gao L, Yan L. Prevalence of iron deficiency in different subtypes of pulmonary hypertension. Heart Lung. 2018;47:308–313. doi: 10.1016/j.hrtlng.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Tang Y, Luo Q, Liu Z, Ma X, Zhao Z, Huang Z, Gao L, Jin Q, Xiong C, Ni X. Oxygen uptake efficiency slope predicts poor outcome in patients with idiopathic pulmonary arterial hypertension. J Am Heart Assoc. 2017;6:e005037. [DOI] [PMC free article] [PubMed]
- 26.Tang Y, Yao L, Liu Z, Xie W, Ma X, Luo Q, Zhao Z, Huang Z, Gao L, Jin Q, et al. Peak circulatory power is a strong prognostic factor in patients with idiopathic pulmonary arterial hypertension. Respir Med. 2018;135:29–34. doi: 10.1016/j.rmed.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 27.Freed DH, Thomson BM, Berman M, Tsui SS, Dunning J, Sheares KK, Pepke-Zaba J, Jenkins DP. Survival after pulmonary thromboendarterectomy: effect of residual pulmonary hypertension. J Thorac Cardiovasc Surg. 2011;141:383–387. doi: 10.1016/j.jtcvs.2009.12.056. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh WC, Jansa P, Huang WC, Niznansky M, Omara M, Lindner J. Residual pulmonary hypertension after pulmonary endarterectomy: a meta-analysis. J Thorac Cardiovasc Surg. 2018;156:1275–1287. doi: 10.1016/j.jtcvs.2018.04.110. [DOI] [PubMed] [Google Scholar]
- 29.Ghofrani HA, D'Armini AM, Grimminger F, Hoeper MM, Jansa P, Kim NH, Mayer E, Simonneau G, Wilkins MR, Fritsch A, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med. 2013;369:319–329. doi: 10.1056/NEJMoa1209657. [DOI] [PubMed] [Google Scholar]
- 30.Simonneau G, D'Armini AM, Ghofrani HA, Grimminger F, Jansa P, Kim NH, Mayer E, Pulido T, Wang C, Colorado P, et al. Predictors of long-term outcomes in patients treated with riociguat for chronic thromboembolic pulmonary hypertension: data from the CHEST-2 open-label, randomised, long-term extension trial. Lancet Respir Med. 2016;4:372–380. doi: 10.1016/S2213-2600(16)30022-4. [DOI] [PubMed] [Google Scholar]
- 31.Lock JE, Castaneda-Zuniga WR, Fuhrman BP, Bass JL. Balloon dilation angioplasty of hypoplastic and stenotic pulmonary arteries. Circulation. 1983;67:962–967. doi: 10.1161/01.CIR.67.5.962. [DOI] [PubMed] [Google Scholar]
- 32.Voorburg JA, Cats VM, Buis B, Bruschke AV. Balloon angioplasty in the treatment of pulmonary hypertension caused by pulmonary embolism. Chest. 1988;94:1249–1253. doi: 10.1378/chest.94.6.1249. [DOI] [PubMed] [Google Scholar]
- 33.Tsugu T, Murata M, Kawakami T, Minakata Y, Kanazawa H, Kataoka M, Endoh J, Tsuruta H, Itabashi Y, Maekawa Y, et al. Changes in right ventricular dysfunction after balloon pulmonary angioplasty in patients with chronic thromboembolic pulmonary hypertension. Am J Cardiol. 2016;118:1081–1087. doi: 10.1016/j.amjcard.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 34.Fukui S, Ogo T, Goto Y, Ueda J, Tsuji A, Sanda Y, Kumasaka R, Arakawa T, Nakanishi M, Fukuda T, et al. Exercise intolerance and ventilatory inefficiency improve early after balloon pulmonary angioplasty in patients with inoperable chronic thromboembolic pulmonary hypertension. Int J Cardiol. 2015;180:66–68. doi: 10.1016/j.ijcard.2014.11.187. [DOI] [PubMed] [Google Scholar]
- 35.Tanabe N, Kawakami T, Satoh T, Matsubara H, Nakanishi N, Ogino H, Tamura Y, Tsujino I, Ogawa A, Sakao S, et al. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension: a systematic review. Respir Investig. 2018;56:332–341. doi: 10.1016/j.resinv.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 36.Khan Muhammad Shahzeb, Amin Emaan, Memon Muhammad Mustafa, Yamani Naser, Siddiqi Tariq Jamal, Khan Safi U., Murad Mohammad Hassan, Mookadam Farouk, Figueredo Vincent M., Doukky Rami, Benza Raymond L., Krasuski Richard A. Meta-analysis of use of balloon pulmonary angioplasty in patients with inoperable chronic thromboembolic pulmonary hypertension. International Journal of Cardiology. 2019;291:134–139. doi: 10.1016/j.ijcard.2019.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Araszkiewicz A, Darocha S, Pietrasik A, Pietura R, Jankiewicz S, Banaszkiewicz M, Slawek-Szmyt S, Biederman A, Mularek-Kubzdela T, Lesiak M, et al. Balloon pulmonary angioplasty for the treatment of residual or recurrent pulmonary hypertension after pulmonary endarterectomy. Int J Cardiol. 2019;278:232–237. doi: 10.1016/j.ijcard.2018.10.066. [DOI] [PubMed] [Google Scholar]
- 38.Kawakami T, Ogawa A, Miyaji K, Mizoguchi H, Shimokawahara H, Naito T, Oka T, Yunoki K, Munemasa M, Matsubara H. Novel angiographic classification of each vascular lesion in chronic thromboembolic pulmonary hypertension based on selective angiogram and results of balloon pulmonary angioplasty. Circ Cardiovasc Interv. 2016;9:e003318. [DOI] [PubMed]
- 39.Wensel R, Opitz CF, Anker SD, Winkler J, Hoffken G, Kleber FX, Sharma R, Hummel M, Hetzer R, Ewert R. Assessment of survival in patients with primary pulmonary hypertension: importance of cardiopulmonary exercise testing. Circulation. 2002;106:319–324. doi: 10.1161/01.CIR.0000022687.18568.2A. [DOI] [PubMed] [Google Scholar]
- 40.Wensel R, Francis DP, Meyer FJ, Opitz CF, Bruch L, Halank M, Winkler J, Seyfarth HJ, Glaser S, Blumberg F, et al. Incremental prognostic value of cardiopulmonary exercise testing and resting haemodynamics in pulmonary arterial hypertension. Int J Cardiol. 2013;167:1193–1198. doi: 10.1016/j.ijcard.2012.03.135. [DOI] [PubMed] [Google Scholar]
- 41.Richter MJ, Pader P, Gall H, Reichenberger F, Seeger W, Mayer E, Guth S, Kramm T, Grimminger F, Ghofrani HA, Voswinckel R. The prognostic relevance of oxygen uptake in inoperable chronic thromboembolic pulmonary hypertension. Clin Respir J. 2017;11:682–690. doi: 10.1111/crj.12399. [DOI] [PubMed] [Google Scholar]
- 42.Iwase T, Nagaya N, Ando M, Satoh T, Sakamaki F, Kyotani S, Takaki H, Goto Y, Ohkita Y, Uematsu M, et al. Acute and chronic effects of surgical thromboendarterectomy on exercise capacity and ventilatory efficiency in patients with chronic thromboembolic pulmonary hypertension. Heart. 2001;86:188–192. doi: 10.1136/heart.86.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Representative videos before and immediately after BPA.
Additional file 2: Figure S1. Hemodynamic and clinical parameters before and after multiple BPA sessions. Figure S2. CPET parameters before and after multiple BPA sessions.
Data Availability Statement
All data generated or analyzed during this study are included in this manuscript.