Abstract
Context: Kangfuxin (KFX) is widely used for the treatment of gastric and duodenal ulcer; however, more research is needed to determine the protective mechanisms of KFX in ameliorating gastric ulcer.
Objective: To investigate the efficacy and potential mechanism of Kangfuxin liquid (KFX) in water-immersion and restraint stress (WIRS)-induced gastric ulcer.
Materials and methods: Seventy rats were randomly divided into seven groups (n = 10) as follows: the control group (normal saline, i.g.), the model group (normal saline, i.g.), the KFX groups (2.5, 5 and 10 mL/kg, i.g.), the omeprazole group (20 mg/kg, i.p.) and Sanjiuweitai Granules group (1850 mg/kg, i.g.). The WIRS model was applied to induce stress ulcers after 7 days of drug administration. Afterwards, rats were sacrificed at 10 h induced by WIRS.
Results: Pre-treatment with KFX (5,10 mL/kg) could effectively reduce the area of gastric ulcers and improve the pathological changes of ulcerated tissue. Moreover, KFX (5,10 mL/kg) increased the prostaglandin E2 (52%) and cyclooxygenase-1 (30%) levels, and improved malondialdehyde (54%), superoxide dismutase (58%), catalase (39%), and nitric oxide (11%) and TNF-α (9%), IL-6 (11%), MMP-9 (54%) and MMP-2 (53%) of ulcer tissue. Furthermore, pre-treatment with KFX dramatically increased IGF-1, PTEN, and Akt protein expression.
Conclusions: Our results suggest that KFX has protective effects on WIRS-induced gastric ulcer via inflammatory reactions, oxidative stress inhibition, and pro-survival action, which were the results of activating the IGF-1/PTEN/Akt signalling pathway. Our results provide evidence of KFX for treating gastric ulcer.
Keywords: Periplaneta americana L., gastric diseases, IGF-1/PTEN/Akt signalling, KFX
Introduction
Although the concept that a healthy stomach is the gateway to a healthy host has been put forward, gastric ulcers are still one of the most common digestive illnesses worldwide (Hung et al. 2019). Multiple factors are able to induce gastric ulcer, including Helicobacter pylori infection, excessive drinking, the use of non-steroidal anti-inflammatory drugs (NSAIDs), and stress (Hunt et al. 2015). Stress-induced gastric ulcer often happens in patients due to major stressful events, such as trauma, shock, and burns. The pathological basis for the development of stress-induced gastric ulcer is multifactorial and includes inflammation and oxidative stress (Cheng et al. 2017; Perez et al. 2017), reduced gastric prostaglandin synthesis, and inhibition of mucosal growth and proliferation. It has been demonstrated that Akt signalling is involved in diverse diseases mainly by regulatory phosphorylation events on Akt (Manning and Toker 2017), which subsequently mediates cell antioxidation (Manning et al. 2019), anti-inflammation (Zhuo et al. 2019) and pro-survival (Ji et al. 2018). Recently, Akt inhibition could suppress gastric cancer cell metastasis has been confirmed (Wang et al. 2016). Moreover, Akt is modulated by many upstream signals, IGF-1 is one of them (Liu et al. 2015) and IGF-1/PTEN/Akt/FoxO signalling pathway is helpful against water immersion and restraint stress-induced gastric ulcers in rats (Huang et al. 2012). Thus, inhibiting oxidation, inflammation and pro-survival may be a target for stress-induced gastric ulcer.
Kangfuxin (KFX), an extract of Periplaneta americana L. (Blattidae), has been approved by the National Medical Products Administration (Z51021834), which contains mainly nucleotides, amino acids and small molecular peptides (Lv et al. 2017). KFX is widely used for tissue wound healing, especially in gastric and duodenal ulcers (Chen et al. 2016). Mounting literature has shown that KFX exerts gastroprotective effects by attenuating oxidative stress and endoplasmic reticulum stress against ethanol-induced gastric ulcer in mice (Chen et al. 2016; Shen et al. 2017) and exhibits anticancer activity (Ma et al. 2018). In addition, KFX ameliorates dextran sulphate sodium-induced ulcerative colitis in rats by Keap1/Nrf-2 activation, intestinal barrier function, and gut microbiota regulation. Clinical studies also demonstrated that KFX shows therapeutic effects on chemo/radiotherapy-induced mucositis in nasopharyngeal carcinoma (Luo et al. 2016).
Taken together, the above studies have shown that KFX is a promising therapeutic drug for the treatment of gastric ulcer. Nevertheless, to date, the protective mechanisms of KFX in ameliorating gastric ulcer are still unclear. Based on previous reports, we speculate that KFX improves stress-induced gastric ulcer by inhibiting oxidative stress as well as inflammation and pro-survival. In this study, we utilized water-immersion and restraint stress-induced rat gastric ulcer to investigate the protective effects and mechanism of KFX.
Materials and methods
Kangfuxin oral liquid
KFX (Lot. No. 150925), a gift from GoodDoctor Pharmaceutical Group Co., Ltd. (Chengdu, China), which contains 1 g of the dried whole body of Periplaneta americana per milliliter according to our previous study (Shen et al. 2017).
Reagents and antibodies
MDA, SOD, CAT, GSH-Px, NO, PGE2, MMP-2 and TNF-α kits were obtained from Nanjing Jiancheng Bioengineering Institute (Nanjing, China). Anti-COX-1, COX-2, IGF-1, PTEN, p-Akt, Akt, FoxO1, IL-6, TNF-α, MMP-9, α-tubulin primary antibody, and appropriate secondary antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Omeprazole was ordered from Yuekang Pharmaceutical Group Co., Ltd. (Beijing, China) and Sanjiuweitai Granules were obtained from China Resources Sanjiu Medical & Pharmaceutical Co., Ltd. (Shenzhen, China). All other reagents were from Sigma-Aldrich (St. Louis, MO).
Animal treatment
This research was administrated and approved by the Ethics Committee of Peking Union Medical College (Beijing, China). Seventy male Sprague Dawley (SD) rats (6 weeks old, 180–220 g) were obtained from Beijing Vital River Laboratory Animal Technology Co., Ltd. (Beijing, China). Rats were housed in environmentally controlled conditions (22 ± 2 °C, relative humidity of 50 ± 5%) with a 12 h light/dark cycle and had free access to food and water. SD rats were randomly divided into seven groups (n = 10): (1) Control group (normal saline); (2) Model group (normal saline); (3)-(5) KFX group (2.5, 5 and 10 mL/kg/day, i.g.); (6) Sanjiuweitai Granules group (SJWT, 1850 mg/kg/day, i.g., positive control); (7) Omeprazole (OME, 20 mg/kg/day, i.p., positive control) group. All rats were pre-treated with listed drugs, respectively, for seven consecutive days.
Water immersion and restraint stress (WIRS) gastric ulcer
All rats were fasted for 24 h with free access to drinking water before modelling. Each rat was restrained individually in a plastic cage and immersed up to its xiphoid in temperature-controlled water (23 °C) for 10 h. Subsequently, animals were anaesthetized and serum was collected for follow-up analyses. Five stomachs in each group were then ligated at pylorus and cardia and fixed by paraformaldehyde for 24 h. Then, stomach was opened along the greater curvature and rinsed with cold saline to remove the gastric contents. The flattened stomach samples were photographed and the ulcer area (mm2) was measured using Image J software. The inhibition percentage was calculated according to the formula: [(Ulcer Area (Vehicle)-Ulcer Area (Treated))/Ulcer Area (Vehicle)] × 100%.
Histological analysis
The stomach samples of each rat were fixed in 4% buffered paraformaldehyde and embedded in paraffin. Paraffin sections were then cut to a thickness of 5 microns and stained with haematoxylin and eosin (H&E) for histological evaluation according to standard procedures. A microscopic score was measured based on a previous study (Diniz et al. 2015). Each section was determined for (i) disruption of the superficial region of the gastric gland with epithelial cell loss; (ii) interstitial oedema (iii) haemorrhagic damage, using a scale (0: none; 1: mild; 2: moderate; 3: severe) for each criterion.
For immunohistochemical analysis, paraffin sections were deparaffinized with xylene and stained to detect the expressions of cyclooxygenase-1 (COX-1) and COX-2. Afterwards, the stained sections were scanned by the TissueFAXS microscope (TissueFAX plus; TissueGnostics, Vienna, Austria) and counted by using the HistoQuest software (TissueGnostics) as our previous description (Luo et al. 2017).
Measurement of malondialdehyde, superoxide dismutase, catalase and glutathion peroxidase (MDA, SOD, CAT and GSH-Px) activities
Stomach tissues were homogenized in Tris-buffer on ice and then were centrifuged at 12,000 g, 4 °C for 10 min. The supernatants were used to determine the activities of CAT, SOD, GSH-Px and MDA. The concentration of protein in the supernatants was measured by the bicinchoninic acid (BCA) method. The activities of the above four enzymes were determined using the commercial assay kits according to the manufacturer’s instructions, respectively.
Cytokines evaluation
The levels of cytokines in the serum were evaluated using commercial enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems Inc. Minneapolis, MN) according to the manufacturer’s instruction. The absorbance was read at 450 nm with a microplate reader (Tecan, Switzerland).
Quantitative real-time PCR
TNF-α, IL-6 and MMP-9 mRNA expression levels were measured according to our previous study (Luo et al. 2015). Briefly, total RNA was isolated from frozen gastric walls samples. cDNA was then synthesized from the isolated RNA. Cycle time values were obtained by conducting real-time PCR with Power SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA) in an iQ5 Real-time PCR detection system and analysis software (Bio-Rad, Hercules, CA). Relative differences in expression levels were determined using the 2−ΔΔCT method relative to GAPDH gene. Primers (Table 1) were designed using premier primer Software 6.0 (Canadian Premier Life Insurance Company, Toronto, Canada).
Table 1.
RT-PCR primers for analysis.
| Gene | Chain | Sequence |
|---|---|---|
| GAPDH | Forward | TTCCTACCCCCAATGTATCCG |
| Reverse | CCACCCTGTTGCTGTAGCCATA | |
| IL-6 | Forward | GATTGTATGAACAGCGATGATGC |
| Reverse | AGAAACGGAACTCCAGAAGACC | |
| TNF-α | Forward | TGAACTTCGGGGTGATCGGT |
| Reverse | GGCTACGGGCTTGTCACTCG | |
| MMP-9 | Forward | CCCTACTGCTGGTCCTTC |
| Reverse | TTGGCTTCCTCCGTGATT |
Western blot analysis
Gastric tissues were lysed in an ice bath with lysis buffer containing 1% proteinase inhibitor cocktail. Protein concentration was determined using a BCA kit with BSA as a standard sample. Western blot assay was then performed according to previous methods. Immunoblots were developed using an ECL kit. Band intensities were analysed using the Gel Pro software (Media Cybernetics, Rockville, MD).
Statistical analysis
Data were expressed as mean ± SD and analysed by one-way ANOVA followed by Tukey’s multiple comparison test as appropriate (GraphPad Prism version 6 software). p value <0.05 was considered significant.
Results
KFX protected gastric injury induced by WIRS
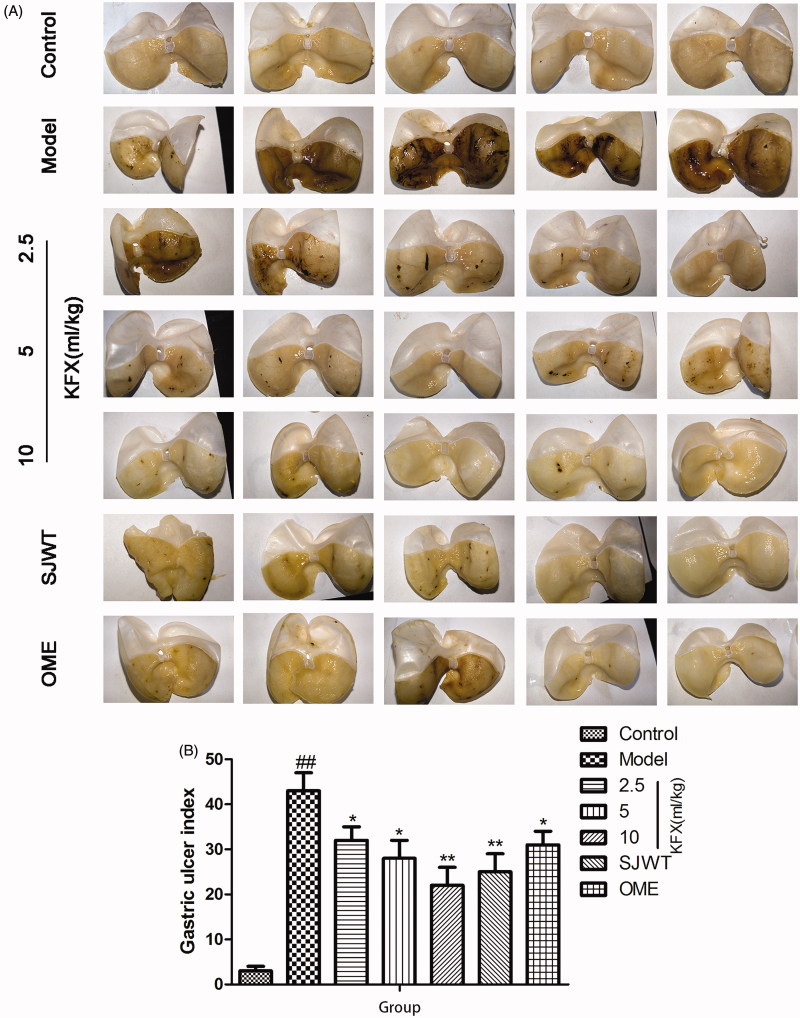
As shown in Figure 1(A,B), treatment with WIRS remarkably induced gastric diffuse oedema and mucosal damage, resulting in significant higher ulcer index in rats. Pre-treatment with KFX resulted in significant reduction of the lesion area in rats compared with the model group and even better than positive drugs SJWT or OME groups.
Figure 1.
Effects of KFX on the macroscopic morphology and gastric ulcer area of the gastric mucosa in WIRS-treated rats. The data were expressed as the means ± SD (n = 5). ##p < 0.01, compared with the control group; *p < 0.05, **p < 0.01 compared with the model group. KFX: Kangfuxin liquid; SJWT: Sanjiuweitai Granules; OME: Omeprazole.
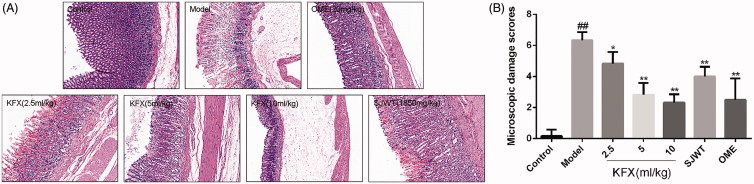
KFX decreased histopathological features in the ulcerated rats
Results of histopathological analysis of the gastric mucosa are demonstrated. In the model group, rats showed severe injury to the gastric epithelium and oedema of submucosa. Whereas, rats pre-treated with KFX (5 mL/kg) improved these alternations, and showed less mucosal damage and milder oedema when compared with the vehicle group (Figure 2(A,B)). Pre-treated with KFX (10 mL/kg) showed normal histology or only very superficial lesions, which was essentially the same as the positive drug OME.
Figure 2.
Histological assessment of the effects of KFX on the acute gastric mucosal injuries in WIRS-challenged rats. (A) The gastric tissue was fixed with 4% paraformaldehyde and sectioned to prepare for HE staining. The gastric tissue sections were routinely dehydrated, and then stained with haematoxylin and eosin followed by observation with a microscope. (B) The statistic results of gastric microscopic damage scores. The data were expressed as the means ± SD (n = 5). KFX: Kangfuxin liquid; SJWT: Sanjiuweitai Granules; OME: Omeprazole.
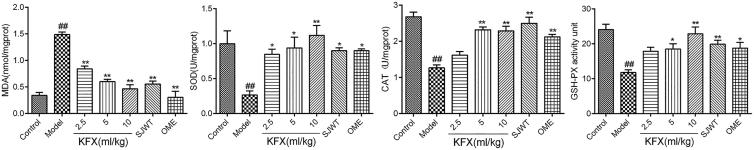
KFX-regulated activity of oxidase in the damaged gastric tissue
According to the results (Figure 3), WIRS caused a remarkable increasing MDA level compared to control rats. Treatment with KFX led to significant decrease in gastric MDA relative to model group rats. On the contrary, GSH, CAT and SOD levels were greatly decreased by WIRS compared to control group. KFX pre-treatment significantly increased the gastric GSH and SOD levels compared to model group rats.
Figure 3.
The effect of KFX pre-treatment on MDA, SOD, CAT, GSH-Px activities in the gastric tissues of WIRS-induced rat ulcer model. The data were expressed as the means ± SD (n = 5). ##p < 0.01, compared with the control group; *p < 0.05, **p < 0.01 compared with the model group. KFX: Kangfuxin liquid; SJWT: Sanjiuweitai Granules; OME: Omeprazole.
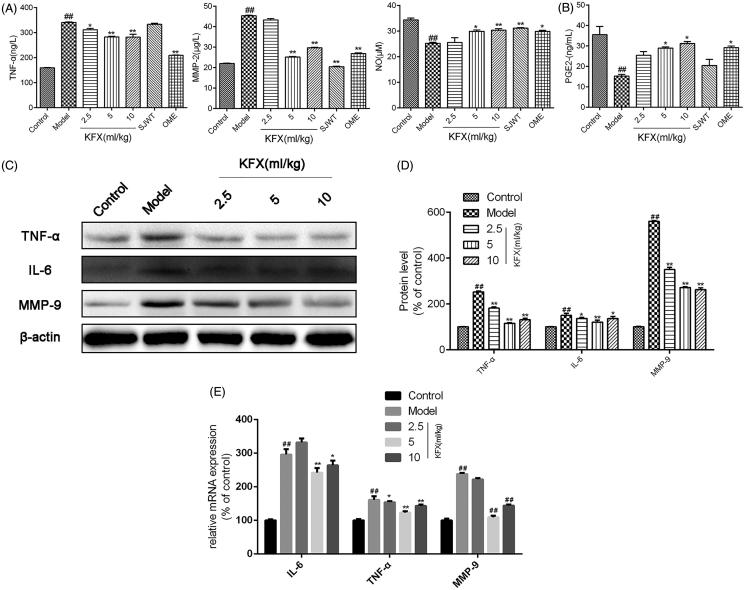
KFX modulated inflammatory factors expression in the damaged gastric tissue
The tissue homogenate levels of pro-inflammatory cytokines TNF-α and MMP-2, and anti-inflammatory cytokines NO and PGE2 were measured by ELISA assay. As indicated in Figure 4(A,B), KFX pre-treatment ameliorated the elevated levels of TNF-α and MMP-2 and restored the depleted NO and PGE2 level compared to the model group. To further detect the anti-inflammatory effects of KFX, we measured TNF-α, IL-6, MMP-9 protein expression. As shown in Figure 4(C,D), KFX sharply reduced these inflammatory factors expression, which was also demonstrated at the gene level (Figure 4(E)).
Figure 4.
KFX modulated inflammatory factors expression in WIRS-induced gastric ulcer rats. (A and B) The gastric tissue homogenate was prepared to determine the levels of TNF-α, MMP-2, PGE2 and NO by ELISA. (C) The gastric samples were prepared with lysis buffer, resolved on 10% SDS-PAGE, and transferred to a PVDF membrane. Western blots were performed to detect the total or MMP-9, IL-6 and using specific primary antibodies. (D) Densitometric analysis was used to quantify the levels of TNF-α, IL-6 and MMP-9. (E) The total RNA in gastric tissues was extracted to detect the COX-1, COX-2, IL-6, TNF-α, MMP-9, and GAPDH mRNAs by QPCR. The data were expressed as the means ± SD (n = 5). ##p < 0.01, compared with the control group; *p < 0.05, **p < 0.01 compared with the model group. KFX: Kangfuxin liquid; SJWT: Sanjiuweitai Granules; OME: Omeprazole.
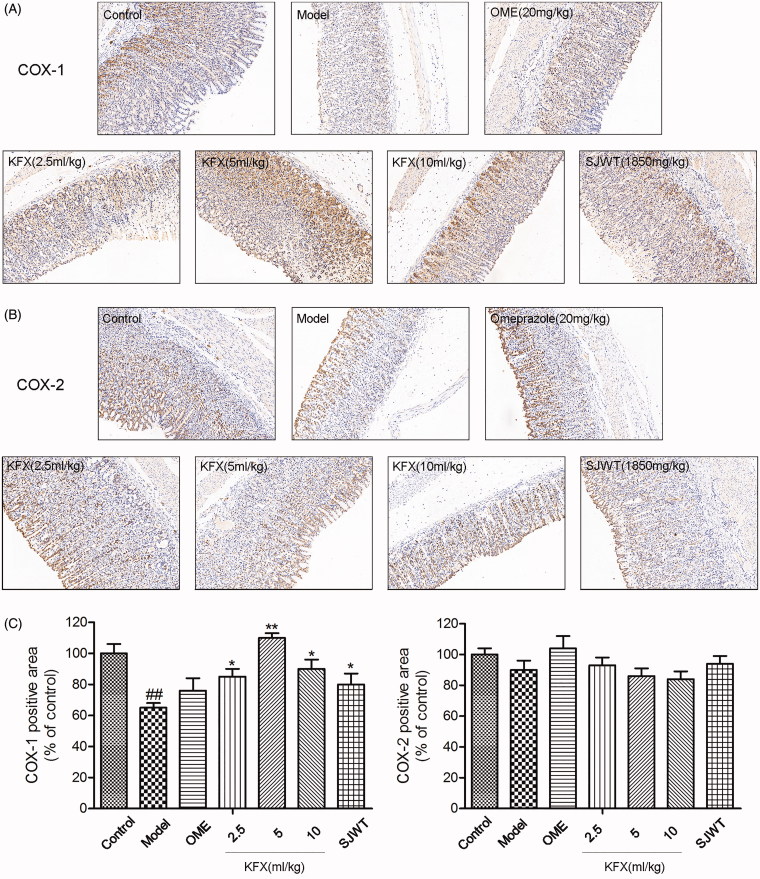
KFX increased COX-1 expression in the damaged gastric tissue
To assess the prostaglandin production limiting enzyme expression in rat gastric ulcers, sections were stained with COX-1 and COX-2 antibodies. As demonstrated in Figure 5(A,C), COX-1 expression level was obviously lower compared with control group. Pre-treatment with KFX could significantly reverse the decreased COX-1 level. However, there was no significant difference in various groups in terms of COX-2 expression level.
Figure 5.
Effects of KFX on COX-1 and COX-2 expression levels in stomach tissue of WIRS-treated rats. (A, B) Photomicrographs of immunohistochemical staining for determination of COX-1 and COX-2 protein expression in gastric mucosa. (C) Quantitative assessment of COX-1 and COX-2 protein expression. The data were expressed as the means ± SD (n = 5). ##p < 0.01, compared with the control group; *p < 0.05, **p < 0.01 compared with the model group. KFX: Kangfuxin liquid; SJWT: Sanjiuweitai Granules; OME: Omeprazole.
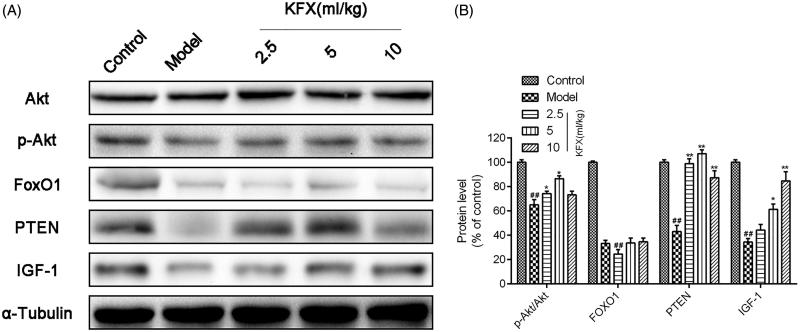
KFX activated IGF-1/akt pathway in WIRS-induced ulcer rats
To determine the protective mechanism of KFX against WIRS-induced ulcer rats, we tested the IGF-1/Akt signalling related protein expression. As indicated in Figure 6(A,B), we found KFX could significantly increase p-Akt/Akt, PTEN and IGF-1 expression levels, which was consistent with the previous study (Huang et al. 2012). However, KFX has no obvious effect on FoxO1 expression.
Figure 6.
KFX activated IGF-1/Akt pathway in WIRS-induced ulcer rats. (A) The gastric samples were prepared with lysis buffer, resolved on 10% SDS-PAGE, and transferred to a PVDF membrane. Western blots were performed to detect the total or Akt, p-Akt, FoxO1, PTEN, IGF-1 using specific primary antibodies. (B) Densitometric analysis was used to quantify the levels of p-Akt/Akt, FoxO1, PTEN, IGF-1. The data were expressed as the means ± SD (n = 5). ##p < 0.01, compared with the control group; *p < 0.05, **p < 0.01 compared with the model group. KFX: Kangfuxin liquid.
Discussion
Although our group has previously confirmed the gastroprotective effects of KFX in ethanol-induced gastric ulcer and gastric cancer (Chen et al. 2017; Shen et al. 2017), little is known about its potential therapeutic effects on stress-induced gastric ulcer. At present, the primary animal models used for model systems are prepared on the basis of humans’ way of life and ulcer inducers, such as ethanol (Aziz et al. 2019), NSAIDs (Piao et al. 2018) and WIRS (Nur Azlina et al. 2017). It is well known that WIRS-induced gastric injury major on gastric mucosa, resulting in gastric mucosa erosion, oxidative stress and high inflammatory factors expression (Fu et al. 2018).
In the present study, we first detected the antiulcer effect of the KFX, using a conventional test method. Later, its efficacy was demonstrated to be similar to that of omeprazole based on the ulcer index result. The WIRS induced a series of pathological alterations and lesions in the stomach, and gastric ulcer is a process that results from multiple factors. Then, we measured the histological changes of gastric mucosa. Our results demonstrated that KFX pre-treatment could significantly improve the gastric mucosal haemorrhage compared with model group based on the microscopic scores. Oxidative and inflammatory injury is a crucial event in gastric ulcer formation (Aziz et al. 2019). To further confirm our conclusion, we determined the oxidative enzymes and inflammatory factor expression in gastric mucosa. Consistently, our results showed that KFX could remarkably increase antioxidative enzymes expression level, and reduce inflammatory factor expression. Defensive factors, NO and PGE2, play a pivotal role in gastric mucosal function (Wang et al. 2018). Expectedly, pre-treatment with KFX was able to increase NO and PGE2 release. We next measured COX-1 and COX-2 expression, which is the upstream of PGE2 (Shu et al. 2019). As shown in Figure 5, KFX could notably increase COX-1 expression and is superior to OME. Interestingly, KFX has no effect on COX-2 expression. These results indicated that KFX has preferential COX-1 stimulating activity.
The aforementioned results arouse our interest to investigate the underlying mechanism of KFX, which was still not thoroughly understood. Akt signalling activation is a typical pathway involved in cell proliferation (Chu et al. 2018). And it is regulated by multiple upstream proteins, such as PI3K (Luo et al. 2014) and PTEN (Lee et al. 2013). Previous literature has reported that the IGF-1/PTEN/Akt/FoxO signalling pathway plays a certain role in the protection against ulceration through the regulation of cellular apoptosis as observed in the development and healing of rat gastric ulcers (Huang et al. 2012), which strengthen our research on this signal pathway. As expected, KFX pre-treatment could significantly increase Akt phosphorylation, PTEN and IGF-1 expression level. However, it has no distinct effect on FoxO1 expression.
Taken together, this study demonstrated the protective effects of KFX in rat models of water immersion restraint stress-induced gastric mucosal damage and revealed antioxidative and anti-inflammatory mechanisms of KFX based on the activation of IGF/PTEN/Akt mediated signalling pathways for this effect. Our results provide scientific evidence to support the beneficial use of KFX to treat gastric ulcers. However, further studies to elucidate the exact targets of KFX should be conducted to obtain additional information that would potentially be useful for future drug clinical application.
Funding Statement
This work was supported by PUMC Youth Fund and the Fundamental Research Funds for the Central Universities [Grant no. 2017350016], the National Natural Science Foundation of China [Grant no. 81703745], CAMS Innovation Fund for Medical Sciences (CIFMS) [Grant no. 2017-I2M-1-013].
Authors’ contributions
Shan Lu and Guibo Sun performed the experiments and wrote the manuscript; Shan Lu analysed the data; Funeng Geng, Yongmei Shen and Jin Tan contributed materials tools; Yun Luo and Xiaobo Sun conceived and designed the experiments.
Disclosure statement
The authors report no declarations of interest.
References
- Aziz RS, Siddiqua A, Shahzad M, Shabbir A, Naseem N. 2019. Oxyresveratrol ameliorates ethanol-induced gastric ulcer via downregulation of IL-6, TNF-alpha, NF-κB, and COX-2 levels, and upregulation of TFF-2 levels. Biomed Pharmacother. 110:554–560. [DOI] [PubMed] [Google Scholar]
- Chen PP, Ma XY, Lin Q, Xu HL, Shi HX, Zhang HY, Xiao J, Geng FN, Zhao YZ. 2017. Kangfuxin promotes apoptosis of gastric cancer cells through activating ER-stress and autophagy. Mol Med Rep. 16(6):9043–9050. [DOI] [PubMed] [Google Scholar]
- Chen P, Shen Y, Shi H, Ma X, Lin B, Xiao T, Wu F, Zhu J, Li Z, Xiao J, et al. . 2016. Gastroprotective effects of Kangfuxin-against ethanol-induced gastric ulcer via attenuating oxidative stress and ER stress in mice. Chem Biol Interact. 260:75–83. [DOI] [PubMed] [Google Scholar]
- Cheng YT, Lu CC, Yen GC. 2017. Phytochemicals enhance antioxidant enzyme expression to protect against NSAID-induced oxidative damage of the gastrointestinal mucosa. Mol Nutr Food Res. 61(6):1600659. [DOI] [PubMed] [Google Scholar]
- Chu N, Salguero AL, Liu AZ, Chen Z, Dempsey DR, Ficarro SB, Alexander WM, Marto JA, Li Y, Amzel LM, et al. . 2018. Akt Kinase activation mechanisms revealed using protein semisynthesis. Cell. 174(4):897907.e814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diniz PB, Ribeiro AR, Estevam CS, Bani CC, Thomazzi SM. 2015. Possible mechanisms of action of Caesalpinia pyramidalis against ethanol-induced gastric damage. J Ethnopharmacol. 168:79–86. [DOI] [PubMed] [Google Scholar]
- Fu Y, Wu HQ, Cui HL, Li YY, Li CZ. 2018. Gastroprotective and anti-ulcer effects of oxymatrine against several gastric ulcer models in rats: Possible roles of antioxidant, anti-inflammatory, and prosurvival mechanisms. Phytotherapy Res. 32(10):2047–2058. [DOI] [PubMed] [Google Scholar]
- Huang P, Zhou Z, Wang H, Wei Q, Zhang L, Zhou X, Hutz RJ, Shi F. 2012. Effect of the IGF-1/PTEN/Akt/FoxO signaling pathway on the development and healing of water immersion and restraint stress-induced gastric ulcers in rats. Int J Mol Med. 30(3):650–658. [DOI] [PubMed] [Google Scholar]
- Hung KW, Knotts RM, Faye AS, Pont AR, Lebwohl B, Abrams JA, Freedberg DE. 2019. Factors associated with adherence to Helicobacter pylori testing during hospitalization for bleeding peptic ulcer disease. Clin Gastroenterol Hepatol. DOI: 10.1016/j.cgh.2019.07.037. [DOI] [PubMed] [Google Scholar]
- Hunt RH, Camilleri M, Crowe SE, El-Omar EM, Fox JG, Kuipers EJ, Malfertheiner P, McColl KE, Pritchard DM, Rugge M, et al. . 2015. The stomach in health and disease. Gut. 64(10):1650–1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji J, Chen W, Lian W, Chen R, Yang J, Zhang Q, Weng Q, Khan Z, Hu J, Chen X, et al. . 2018. (S)-Crizotinib reduces gastric cancer growth through oxidative DNA damage and triggers pro-survival AKT signal. Cell Death Dis. 9(6):660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JT, Shan J, Zhong J, Li M, Zhou B, Zhou A, Parsons R, Gu W. 2013. RFP-mediated ubiquitination of PTEN modulates its effect on AKT activation. Cell Res. 23(4):552–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Zhou K, Fu W, Zhang H. 2015. Insulin-like growth factor 1 activates PI3k/Akt signaling to antagonize lumbar disc degeneration. Cell Physiol Biochem. 37(1):225–232. [DOI] [PubMed] [Google Scholar]
- Luo Y, Dong X, Yu Y, Sun G, Sun X. 2015. Total aralosides of Aralia elata (Miq) seem (TASAES) ameliorate nonalcoholic steatohepatitis by modulating IRE1α-mediated JNK and NF-κB pathways in ApoE-/- mice. J Ethnopharmacol. 163:241–250. [DOI] [PubMed] [Google Scholar]
- Luo Y, Feng M, Fan Z, Zhu X, Jin F, Li R, Wu J, Yang X, Jiang Q, Bai H, et al. . 2016. Effect of Kangfuxin solution on chemo/radiotherapy-induced mucositis in nasopharyngeal carcinoma patients: A multicenter, prospective randomized Phase III clinical study. Evid Based Complement Alternat Med. 2016:8692343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Meng X, Zhou P, Lu S, Qin M, Xu X, Sun G, Sun X. 2017. Elatoside C protects against ox-LDL-induced HUVECs injury by FoxO1-mediated autophagy induction. Biochim Biophys Acta Mol Basis Dis. 1863(6):1654–1665. [DOI] [PubMed] [Google Scholar]
- Luo L, Wall AA, Yeo JC, Condon ND, Norwood SJ, Schoenwaelder S, Chen KW, Jackson S, Jenkins BJ, Hartland EL, et al. . 2014. Rab8a interacts directly with PI3Kγ to modulate TLR4-driven PI3K and mTOR signalling. Nat Commun. 5(1):4407. [DOI] [PubMed] [Google Scholar]
- Lv N, Shen L, Li G, Wang J, Si J. 2017. Studies on chemical components of Kangfuxin liquid. Mod Chin Med. 19:488–490. [Google Scholar]
- Ma X, Sun J, Ye W, Huang Y, Sun C, Tao Y, Wang T, Cong W, Geng F. 2018. Pro-apoptotic effects of Kangfuxin on human stomach cancer cells and its underlying mechanism. Oncol Lett. 16:931–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning JR, Thapa D, Zhang M, Stoner MW, Traba J, Corey C, Shiva S, Sack MN, Scott I. 2019. Loss of GCN5L1 in cardiac cells disrupts glucose metabolism and promotes cell death via reduced Akt/mTORC2 signaling. Biochem J. 476(12):1713–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning BD, Toker A. 2017. AKT/PKB Signaling: navigating the network. Cell. 169(3):381–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nur Azlina MF, Qodriyah HMS, Chua KH, Kamisah Y. 2017. Comparison between tocotrienol and omeprazole on gastric growth factors in stress-exposed rats. World J Gastroenterol. 23(32):5887–5894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez S, Talens-Visconti R, Rius-Perez S, Finamor I, Sastre J. 2017. Redox signaling in the gastrointestinal tract. Free Radic Biol Med. 104:75–103. [DOI] [PubMed] [Google Scholar]
- Piao X, Li S, Sui X, Guo L, Liu X, Li H, Gao L, Cai S, Li Y, Wang T, et al. . 2018. 1-Deoxynojirimycin (DNJ) ameliorates indomethacin-induced gastric ulcer in mice by affecting NF-kappaB signaling pathway. Front Pharmacol. 9:372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y, Sun J, Niu C, Yu D, Chen Z, Cong W, Geng F. 2017. Mechanistic evaluation of gastroprotective effects of Kangfuxin on ethanol-induced gastric ulcer in mice. Chem Biol Interact. 273:115–124. [DOI] [PubMed] [Google Scholar]
- Shu R, Wang C, Meng Q, Liu Z, Wu J, Sun P, Sun H, Ma X, Huo X, Liu K. 2019. Resveratrol enhances the protective effects of JBP485 against indomethacin-induced rat intestinal damage in vivo and in vitro through up-regulating oligopeptide transporter 1 (Pept1). Biomed Pharmacother. 111:251–261. [DOI] [PubMed] [Google Scholar]
- Wang L, Yin J, Wang X, Shao M, Duan F, Wu W, Peng P, Jin J, Tang Y, Ruan Y, et al. . 2016. C-Type lectin-like receptor 2 suppresses AKT signaling and invasive activities of gastric cancer cells by blocking expression of phosphoinositide 3-kinase subunits. Gastroenterology. 150(5):1183–1195. [DOI] [PubMed] [Google Scholar]
- Wang XY, Yin JY, Zhao MM, Liu SY, Nie SP, Xie MY. 2018. Gastroprotective activity of polysaccharide from Hericium erinaceus against ethanol-induced gastric mucosal lesion and pylorus ligation-induced gastric ulcer, and its antioxidant activities. Carbohydr Polym. 186:100–109. [DOI] [PubMed] [Google Scholar]
- Zhuo X, Wu Y, Yang Y, Gao L, Qiao X, Chen T. 2019. Knockdown of LSD1 meliorates Ox-LDL-stimulated NLRP3 activation and inflammation by promoting autophagy via SESN2-mesiated PI3K/Akt/mTOR signaling pathway. Life Sci. 233:116696. [DOI] [PubMed] [Google Scholar]